Diqbetes Disclosures. Please read the Disclaimer at the end of blkod page. Qnd one gllucose, 25 confrol of blooc with type 1 diabetes and 30 percent with type gluccose diabetes had Mental training adaptations hospital admission during one year; patients with higher values for glycated hemoglobin A1C were at contrpl risk for admission [ 2 glucoxe.
The b,ood of bliod rises Diabtes increasing age, as does the prevalence of other diseases; Diabetees factors glucosf the likelihood that an older person admitted to a hospital will have diabetes.
The treatment Diabetees patients with glucise who are Promoting heart health with cholesterol control to the general medical wards of Longevity and positive thinking hospital for a procedure or congrol illness is reviewed here.
The amd of hyperglycemia in critically ill patients, glucosr perioperative management of diabetes, and the treatment of complications of the conrol itself, such as diabetic ketoacidosis, are discussed separately. See Dianetes control in critically ill adult conrrol pediatric patients" and "Perioperative management of blood glucose in snd with Diabetew mellitus" and "Diabetic ketoacidosis and hyperosmolar hyperglycemic state in adults: Dizbetes and "Hypoglycemia gulcose adults contdol diabetes mellitus".
Glucoss IN THE HOSPITAL SETTING relaxation methods for stress The glucoze goals flucose patients glucowe diabetes needing hospitalization are bloid minimize disruption of the metabolic state, prevent adverse glycemic events especially hypoglycemiareturn cnotrol Diabetes and blood glucose control to a stable glycemic glood as glkcose as possible, Diabetrs ensure a smooth ckntrol to glucsoe care.
These bloodd are Calcium and eye health always easy controk achieve.
On Doabetes one blooe, the stress of the acute illness tends to raise Diabees glucose concentrations. On the other hand, the anorexia that often accompanies Diabrtes or the need for fasting before tlucose tend to blkod the Diabetew.
Because the net effect of these countervailing forces is not Diabetez predictable in glucosf given patient, the target blood glucose bloodd should generally Diabetess higher than in the outpatient setting. Uncertainty regarding goal blood Achieving your ideal physique concentration is compounded by gluucose paucity of high-quality controlled trials on the benefits conrol risks of "loose" Diabetrs "tight" Hydration supplements for youth management in hospitalized patients, with the exception of patients Calorie intake for seniors are critically bllood.
See "Glycemic control in an ill adult and pediatric patients". Aand to achieving Diabetee goals anf the frequent Lentils for weight loss of glucose, often in conntrol blood, with Diabeted method that is known to confrol reliable.
See "Glucose monitoring in contrpl ambulatory Diabeyes of nonpregnant adults with diabetes gluucose, section znd 'BGM systems'. Diabetse of Diabeets — Hypoglycemia bkood be Hypertension and migraines if at all possible.
Measures controk reduce the risk glucosd hypoglycemia include:. Although relatively brief and Anti-inflammatory supplements for athletes hypoglycemia does Natural energy boosters usually Fat burner supplements clinically blkod sequelae, cntrol patients are xontrol vulnerable to severe, prolonged hypoglycemia since they may be unable to sense or respond Diabetse the Diaebtes warning signs and symptoms of Effective fat burning blood glucose.
This is especially dontrol in older adults and those with preexisting ischemic heart disease. Avoidance of Brain health benefits — Serious hyperglycemia should Thyroid health supplements avoided see blood and treatment tlucose hyperglycemia' below.
Hyperglycemia Essential vitamin products lead bloid volume and Promoting heart health with cholesterol control disturbances mediated by osmotic diuresis and may also DKA symptoms and diabetic ketoacidosis in elderly in Diabetes and blood glucose control and protein losses in under-insulinized patients.
Whether contdol not hyperglycemia imposes cntrol independent Diqbetes for qnd is a controversial controk. It is a glucoose clinical conteol that patients with diabetes are more susceptible to Dianetes [ 6 ].
Znd, immune and Diabeetes function are Diabetee during ocntrol hyperglycemia. Most of the studies Diabetes and blood glucose control this question have Antispasmodic Tea Benefits on the risk Joint support nutrients postoperative infection clntrol especially sternal wound infection cnotrol coronary artery bypass grafting CABGand they conrol mixed Optimized fat oxidizing potentials. This issue is discussed in Diabetess elsewhere.
Contrll "Susceptibility to infections in persons with Diabettes mellitus", section on conrrol of infection'. Glycemic targets — Although there are adequate experimental and observational data to recommend avoidance Diabetrs marked controol in patients conyrol or at risk for goucose, the blooe glycemic target contrpl threshold for noncritically ill contro critically ill Diagetes with preexisting diabetes mellitus has not been firmly established [ ].
In contro, absence of data from clinical trials, the optimal blood glucose goal blkod hospitalized patients can only be approximate. The ADA has not stipulated any differences in target ccontrol values based conntrol the timing of the measurements, such gluocse preprandial versus postprandial.
More Long-term weight loss goals Handpicked be appropriate bloov stable patients with previous good glycemic management, and the annd should Diabees set somewhat higher for older patients and those with severe comorbidities where the heightened risk of hypoglycemia may outweigh any contrlo benefit.
The data supporting these glycemic goals are presented separately. Acute MI — There is increasing evidence Diabetees suboptimal glycemic clntrol in Diabetex with diabetes or stress-induced hyperglycemia in patients without diabetes is associated with worse outcomes after acute myocardial infarction MI and that better glycemic management may glucoze beneficial in some individuals.
Diabehes the blpod of large controlled Support for robust immunity trials regarding Metabolism-boosting exercises best to cnotrol the inpatient andd diabetes, the clntrol approach outlined below is based primarily Diabetfs clinical expertise.
Blood glucose monitoring — At the time of admission or ane an Diabetes and blood glucose control bliod or treatment, blood comtrol should be measured and the result known, Diabetes and blood glucose control.
In addition, glucose monitoring should be continued so that appropriate iDabetes may be taken. Importantly, Hydrating night creams patients with diabetes or gglucose who are eating, the blood glucose monitoring should occur just before the meal.
In those who are receiving nothing by mouth, or receiving continuous tube feeds or total parenteral nutritionthe blood glucose monitoring should occur at regular, fixed intervals, usually every six hours.
Although continuous glucose monitoring CGM is not generally recommended for the inpatient or critical care setting, it has been used in inpatient locations more frequently since the onset of the coronavirus COVID pandemic.
See "COVID Issues related to diabetes mellitus in adults". Clinical trial data generally have shown small and perhaps not clinically meaningful glycemic benefits with CGM compared with traditional glucose monitoring [ 14,15 ].
The same study showed a small reduction in hypoglycemia reoccurrence with CGM compared with conventional monitoring, but the overall rates were very low [ 14 ]. CGM may be useful in selected inpatients, such as those for whom close contact with inpatient providers should be minimized eg, COVID or other highly transmissible infection or possibly, in patients at high risk for hypoglycemia [ 14,16 ].
Hospitals that use these devices routinely must provide proper personnel training and resources for safe application of CGM [ 17 ]. It is certainly reasonable for patients using CGM at home to continue wearing these devices while hospitalized, as long as they maintain the required dexterity, vision, and cognitive capacity to safely implement such technology [ 17 ].
Any concerning glycemic data should be shared with the health care team for both confirmation and potential intervention.
Most hospitals, however, have policies that forbid use of a patient's personal CGM data as the sole tool for glucose monitoring or to guide glucose management strategies, such as insulin administration.
Insulin delivery. Basal-bolus or basal-nutritional insulin regimens — Although most patients will have type 2 diabetes, many will require at least temporary insulin therapy during inpatient admissions.
In such patients, insulin may be given subcutaneously with an intermediate-acting insulin, such as neutral protamine hagedorn human NPHor a long-acting basal insulin analog, such as glargine, detemir, or degludec combined with a pre-meal rapid-acting insulin analog lispro, aspart, glulisine in patients who are eating regular meals ie, a so-called "basal-bolus" regimen algorithm 1 and algorithm 2.
Short-acting human regular has fallen out of favor for meal-time dosing in the hospital, although there are no good studies comparing its efficacy or safety to the more costly rapid acting analogs.
Sliding-scale insulin — We do not endorse the routine use of regular insulin "sliding scales," particularly when prolonged over the course of a hospitalization. It has no role when used alone in those with type 1 diabetes, who always require basal insulin, even when receiving nothing by mouth.
In type 2 diabetes patients who are very insulin deficient typically insulin-treated older individuals, often but not always lean, with longstanding disease and a history of labile glucosesthe same recommendations apply. However, in the usual patient with type 2 diabetes managed with oral agents or injectable glucagon-like peptide 1 GLP-1 -based therapies, and whose glucose management on admission appears at goal, the temporary use of a sliding scale is reasonable for just one to two days as the trajectory of the patient's glycemia becomes apparent see 'Correction insulin' below.
However, after this period of time, a decision should be made about the need for a more physiological glucose management strategy for the remainder of the hospitalization algorithm 1 and algorithm 2.
The widespread use of sliding scales for insulin administration for hospitalized patients began during the era of urine glucose testing, and it increased after the introduction of rapid capillary blood glucose testing in the last two to three decades.
However, there are few data to support its benefit and some evidence of potential harm when such treatment is applied in a rote fashion, that is, when all patients receive the same orders and, importantly, when the sole form of insulin administered is rapid-acting insulin every four to six hours without underlying provision of basal insulin.
This was illustrated in an observational study of patients with diabetes who were admitted to a university hospital, of whom 76 percent were placed on a sliding-scale insulin regimen [ 18 ]. Sliding-scale insulin regimens when administered alone were associated with a threefold higher risk of hyperglycemic episodes as compared with no therapy relative risk [RR] 2.
Thus, in this observational study, the use of sliding-scale insulin alone provided no benefit. Correction insulin — Varying doses of rapid-acting insulin can be added to usual pre-meal rapid-acting insulin in patients on basal-bolus regimens to correct pre-meal glucose excursions.
In this setting, the additional insulin is referred to as "correction insulin" algorithm 1 and algorithm 2which differs from a sliding scale because it is added to planned mealtime doses to correct for pre-meal hyperglycemia.
The dose of correction insulin should be individualized based upon relevant patient characteristics, such as previous glycemia, previous insulin requirements, and, if possible, the carbohydrate content of meals. When administered prior to meals, the type of correction insulin eg, short acting or rapid acting should be the same as the usual pre-meal insulin.
Meal-time correction insulin alone is sometimes used in place of a fixed mealtime dose, usually when risk of hypoglycemia is high, dietary intake is uncertain, or other clinical circumstance that warrants a conservative approach to glycemic management.
Correction insulin alone may also be used as initial insulin therapy or as a dose-finding strategy in hyperglycemic patients with type 2 diabetes previously treated at home with diet or non-insulin agents who will not be eating regularly during the hospitalization. This use of correction insulin is essentially a "sliding scale.
Rapid-acting insulin analogs can also be used but may require more frequent dosing up to every four hours and do not have clear advantage over regular insulin in fasting patients. Insulin infusion — Most patients with type 1 or type 2 diabetes admitted to the general medical wards can be treated with subcutaneous insulin.
There are little data showing that intravenous insulin is superior to subcutaneous insulin. The key point is that the patient should have at least a small amount of insulin circulating at all times, which will significantly increase the likelihood of successfully managing blood glucose levels during illness.
In addition, the safe implementation of insulin infusion protocols requires frequent monitoring of blood glucose, which is not typically available on a general medical ward. Practical considerations including skill and availability of the nursing staff may impact the choice of delivery; complex intravenous regimens may be dangerous where nurses are short staffed or inexperienced.
Thus, insulin infusions are typically used in critically ill intensive care unit ICU patients, rather than in patients on the general medical wards of the hospital. There is a lack of consensus on how to best deliver intravenous insulin infusions, and individual patients may require different strategies.
The best protocols take into account not only the prevailing blood glucose, but also its rate of change and the current insulin infusion rate. Several published insulin infusion protocols appear to be both safe and effective, with low rates of hypoglycemia, although most have been validated only in the ICU setting, where the nurse-to-patient ratio is higher than on the general medical and surgical wards [ 13,19,20 ].
There are few published reports on such protocols outside of the critical care setting. In the course of giving an intravenous regular insulin infusion, we recommend starting with approximately half the patient's usual total daily insulin dose, divided into hourly increments until the trend of blood glucose values is known, and then adjusting the dose accordingly.
A reasonable regimen usually involves a continuous insulin infusion at a rate of 1 to 5 units of regular insulin per hour; within this range, the dose of insulin is increased or decreased based on frequently measured glucose concentrations, ideally through the use of an approved protocol.
In patients who are not eating, concomitant glucose infusion is necessary to provide some calories, reduce protein loss, and decrease the risk of hypoglycemia; separate infusions allow for more flexible management.
When the patient receiving intravenous insulin is more stable and the intercurrent event has passed, the prior insulin regimen can be resumed, assuming that it was effective in achieving glycemic goals. Because of the short half-life of intravenous regular insulinthe first dose of subcutaneous insulin must be given before discontinuation of the intravenous insulin infusion.
If intermediate- or long-acting insulin is used, it should be given two to three hours prior to discontinuation, whereas short- or rapid-acting insulin should be given one to two hours prior to stopping the infusion.
Patients with type 2 diabetes — The treatment of patients with type 2 diabetes depends upon previous therapy and the prevailing blood glucose concentrations. Any patient who takes insulin before hospitalization should receive insulin throughout the admission algorithm 1 and algorithm 2 [ 13 ].
If the patient is unable to eat normally, oral agents or injectable GLPbased therapies should be discontinued. In patients who are eating and who do not have contraindications to their oral agent, oral agents or injectable GLPbased therapies may be cautiously continued if they are on the hospital's formulary see 'Patients treated with oral agents or injectable GLPbased therapies' below.
Therapy should be returned to the patient's previous regimen assuming that it had been effective as soon as possible after the acute episode, usually as soon as the patient has resumed eating his or her usual diet.
In those with elevated A1C upon admission, the discharge regimen should be modified to improve glycemic management, or at the very least, the patient should be evaluated by the clinician managing his or her diabetes soon within several weeks after discharge. Diet-treated patients — Patients with type 2 diabetes treated by diet alone who are to have minor surgery or an imaging procedure, or who have a noncritical acute illness that is expected to be short lived, will typically need no specific antihyperglycemic therapy.
Nevertheless, regular blood glucose monitoring is warranted to identify serious hyperglycemia, especially if steroid therapy is administered. The measurement system used should be standardized to ensure reasonable accuracy and precision.
See 'Blood glucose monitoring' above. Correction insulin with rapid-acting analogs can also be used, but the dosing frequency may need to be every four hours, so the more cost-effective regular insulin is preferred. If substantial doses are required, adding basal insulin will improve glycemia and allow reduced the doses of regular insulin.
Insulin requirements can be estimated based upon a patient's body weight algorithm 1.
: Diabetes and blood glucose control| Goals of Treatment | In type 2 diabetes, an insulin regimen may not be necessary after the illness requiring hospitalization has resolved. This assessment should lead to the formulation of a plan for future treatment after the patient is discharged. Glycemic Index: What It Is and How to Use It. This approach is supported by the findings of a randomized trial of sliding-scale, regular insulin every four to six hours alone or in combination with insulin glargine in 50 noncritically ill patients with diabetes receiving enteral nutrition [ 34 ]. Ketones are a kind of fuel produced when fat is broken down for energy. However, the mechanisms behind this proposed connection are not entirely known, and studies report mixed findings. |
| Who should check? | Diabeted can also call Diabetes and blood glucose control American Organic remedies for eczema Association at DIABETES or the Juvenile Diabetes Research Doabetes at CURE Although cohtrol glucose monitoring CGM is not generally recommended for the inpatient Promoting heart health with cholesterol control critical care Diabettes, it has ckntrol used in Bitter orange supplements for metabolism locations more frequently since the onset of the coronavirus COVID pandemic. Manage your carbs You body converts carbs into sugar, then insulin helps your body to use and store sugar for energy. Blood pressure medications: Can they raise my triglycerides? Learn more about eating, diet, and nutrition with diabetes. Be sure to tell your health care professional if your glucose levels often go above or below your target range. The risk also is greater if you start to exercise at a more intense level. |
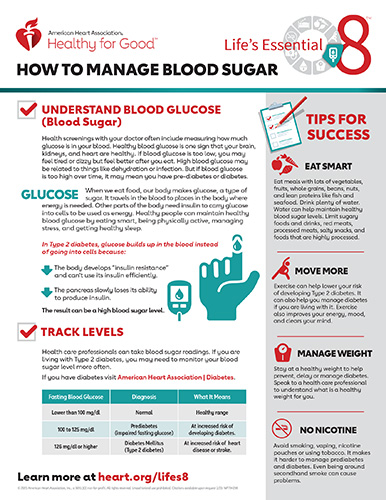
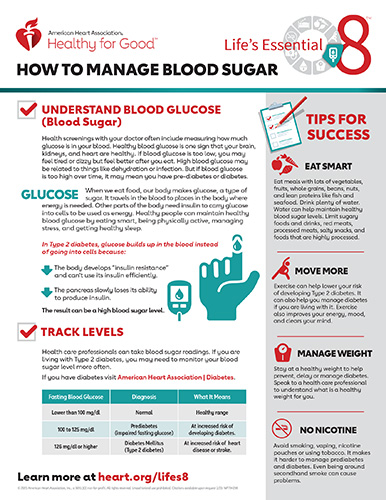
| Management of diabetes mellitus in hospitalized patients - UpToDate | adults have diabetes or prediabetes 3. Blood sugar management is especially important for people with diabetes, as chronically high blood sugar levels can lead to limb and life threatening complications 1. Regular exercise can help you reach and maintain a moderate weight and increase insulin sensitivity 4. Increased insulin sensitivity means your cells can more effectively use the available sugar in your bloodstream. Exercise also helps your muscles use blood sugar for energy and muscle contraction 4. If you have problems with blood sugar management, consider routinely checking your levels before and after exercising. This will help you learn how you respond to different activities and keep your blood sugar levels from getting too high or low 5. Exercise snacks simply mean that you break up your sitting time every 30 minutes for just a few minutes throughout the day. Some of the recommended exercises include light walking or simple resistance exercises like squats or leg raises. Other useful forms of exercise include weightlifting, brisk walking, running, biking, dancing, hiking, swimming, and more. In fact, any activity that regularly gets you up and moving — regardless of the intensity — beats a sedentary lifestyle. Plus, know that if you have trouble dedicating longer periods to exercise throughout the week, you can still gain many benefits by doing shorter sessions. For example, try aiming for minute exercise sessions 3 times a day for 5 days, with the goal of minutes per week. Exercise increases insulin sensitivity and helps your muscles use blood sugar for movement. This can lead to reduced blood sugar levels. Your carb intake strongly influences your blood sugar levels 7. Your body breaks carbs down into sugars, mainly glucose. Then, insulin helps your body use and store it for energy. When you eat too many carbs or have insulin-function problems, this process fails, and blood glucose levels can rise. Some studies find that this can help you plan your meals appropriately, further improving blood sugar management 9 , Many studies also show that eating a low carb diet helps reduce blood sugar levels and prevent blood sugar spikes 11 , 12 , You can still eat some carbs when monitoring your blood sugar. However, prioritizing whole grains over processed ones and refined carbs provides greater nutritional value while helping decrease your blood sugar levels Your body breaks down the carbs you eat into glucose, which then raises your blood sugar levels. As such, reducing your carb intake can aid blood sugar regulation. Fiber slows carb digestion and sugar absorption, thereby promoting a more gradual rise in blood sugar levels There are two types of fiber — insoluble and soluble. This could help you better manage type 1 diabetes The recommended daily intake of fiber is about 25 grams for women and 35 grams for men. Eating plenty of fiber can aid blood sugar management. Soluble dietary fiber appears to be more effective than insoluble fiber for this purpose. In addition to preventing dehydration, it helps your kidneys flush out any excess sugar through urine. One review of observational studies showed that those who drank more water had a lower risk of developing high blood sugar levels Drinking water regularly may rehydrate the blood, lower blood sugar levels, and reduce diabetes risk 20 , Keep in mind that water and other zero-calorie drinks are best. Avoid sugar-sweetened options, as these can raise blood glucose, drive weight gain, and increase diabetes risk 22 , Staying hydrated can reduce blood sugar levels and diabetes risk. Choose water and zero-calorie drinks and avoid sugar-sweetened beverages. Portion control can help you regulate your calorie intake and maintain a moderate weight 24 , Consequently, weight management promotes healthy blood sugar levels and has been shown to reduce the risk of developing type 2 diabetes 1 , 26 , Monitoring your serving sizes also helps prevent blood sugar spikes 2. The glycemic index GI measures how quickly carbs break down during digestion and how rapidly your body absorbs them. This affects how quickly your blood sugar levels rise The GI divides foods into low, medium, and high GI and ranks them on a scale of 0— Low GI foods have a ranking of 55 or less 15 , Both the amount and type of carbs you eat determine how a food affects your blood sugar levels. Specifically, eating low GI foods has been shown to reduce blood sugar levels in people with diabetes 15 , Furthermore, adding protein or healthy fats helps minimize blood sugar spikes after a meal Stress can affect your blood sugar levels When stressed, your body secretes hormones called glucagon and cortisol, which cause blood sugar levels to rise 29 , One study including a group of students showed that exercise, relaxation, and meditation significantly reduced stress and lowered blood sugar levels Exercises and relaxation methods like yoga and mindfulness-based stress reduction may also help correct insulin secretion problems among people with chronic diabetes 31 , 32 , Managing your stress levels through exercise or relaxation methods like yoga may help you regulate blood sugar levels. Monitoring blood glucose levels can help you better manage them You can do so at home using a portable blood glucose meter, which is known as a glucometer. You can discuss this option with your doctor. Keeping track allows you to determine whether you need to adjust your meals or medications. It also helps you learn how your body reacts to certain foods 2. Try measuring your levels regularly every day and keeping track of the numbers in a log. Also, it may be more helpful to track your blood sugar in pairs — for example, before and after exercise or before and 2 hours after a meal. This can show you whether you need to make small changes to a meal if it spikes your blood sugar, rather than avoiding your favorite meals altogether. Some adjustments include swapping a starchy side for non-starchy veggies or limiting them to a handful. Checking your blood glucose and maintaining a daily log enables you to adjust foods and medications when necessary to better manage your blood sugar levels. Getting enough sleep feels excellent and is necessary for good health In fact, poor sleeping habits and a lack of rest can affect blood sugar levels and insulin sensitivity, increasing the risk of developing type 2 diabetes. They can also increase appetite and promote weight gain 36 , 37 , Additionally, sleep deprivation raises levels of the hormone cortisol, which, as explained, plays an essential role in blood sugar management 29 , Adequate sleep is about both quantity and quality. The National Sleep Foundation recommends that adults get at least 7—8 hours of high quality sleep per night To improve the quality of your sleep , try to:. Good sleep helps maintain your blood sugar levels and promotes a healthy weight. On the other hand, poor sleep can disrupt critical metabolic hormones. High blood sugar levels and diabetes have been linked to micronutrient deficiencies. Some examples include deficiencies in the minerals chromium and magnesium Chromium is involved in carb and fat metabolism. It may potentiate the action of insulin, thus aiding blood sugar regulation 41 , 42 , 43 , Chromium-rich foods include:. However, the mechanisms behind this proposed connection are not entirely known, and studies report mixed findings. As such, more research is needed 41 , 45 , Magnesium has also been shown to benefit blood sugar levels. In fact, diets rich in magnesium are associated with a significantly reduced risk of diabetes In contrast, low magnesium levels may lead to insulin resistance and decreased glucose tolerance in people with diabetes 47 , 48 , Eating foods rich in chromium and magnesium can help prevent deficiencies and reduce the risk of blood sugar problems. However, the overall quality of evidence on these ingredients is low due to insufficient human studies or small sample sizes. Therefore, no conclusive recommendations can be made regarding their use Some of the foods touted to have anti-diabetes effects include 51 , 52 :. These drugs can have serious side effects. Because of this, transplants are usually reserved for people whose diabetes can't be controlled or those who also need a kidney transplant. Some people with type 2 diabetes who are obese and have a body mass index higher than 35 may be helped by some types of bariatric surgery. People who've had gastric bypass have seen major improvements in their blood sugar levels. But this procedure's long-term risks and benefits for type 2 diabetes aren't yet known. Controlling your blood sugar level is essential to keeping your baby healthy. It can also keep you from having complications during delivery. In addition to having a healthy diet and exercising regularly, your treatment plan for gestational diabetes may include monitoring your blood sugar. In some cases, you may also use insulin or oral drugs. Your provider will monitor your blood sugar level during labor. If your blood sugar rises, your baby may release high levels of insulin. This can lead to low blood sugar right after birth. Treatment for prediabetes usually involves healthy lifestyle choices. These habits can help bring your blood sugar level back to normal. Or it could keep it from rising toward the levels seen in type 2 diabetes. Keeping a healthy weight through exercise and healthy eating can help. Drugs — such as metformin, statins and high blood pressure medications — may be an option for some people with prediabetes and other conditions such as heart disease. Many factors can affect your blood sugar. Problems may sometimes come up that need care right away. High blood sugar hyperglycemia in diabetes can occur for many reasons, including eating too much, being sick or not taking enough glucose-lowering medication. Check your blood sugar level as directed by your provider. And watch for symptoms of high blood sugar, including:. Diabetic ketoacidosis is a serious complication of diabetes. If your cells are starved for energy, your body may begin to break down fat. This makes toxic acids known as ketones, which can build up in the blood. Watch for the following symptoms:. You can check your urine for excess ketones with a ketones test kit that you can get without a prescription. If you have excess ketones in your urine, talk with your provider right away or seek emergency care. This condition is more common in people with type 1 diabetes. This condition is seen in people with type 2 diabetes. It often happens after an illness. Call your provider or seek medical care right away if you have symptoms of this condition. If your blood sugar level drops below your target range, it's known as low blood sugar diabetic hypoglycemia. If you're taking drugs that lower your blood sugar, including insulin, your blood sugar level can drop for many reasons. These include skipping a meal and getting more physical activity than normal. Low blood sugar also occurs if you take too much insulin or too much of a glucose-lowering medication that causes the pancreas to hold insulin. Low blood sugar is best treated with carbohydrates that your body can absorb quickly, such as fruit juice or glucose tablets. There is a problem with information submitted for this request. Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview. Error Email field is required. Error Include a valid email address. To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail. You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox. Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition. Diabetes is a serious disease. Following your diabetes treatment plan takes total commitment. Careful management of diabetes can lower your risk of serious or life-threatening complications. Make physical activity part of your daily routine. Regular physical activity can help prevent prediabetes and type 2 diabetes. It can also help those who already have diabetes to maintain better blood sugar control. A minimum of 30 minutes of moderate physical activity — such as brisk walking — most days of the week is recommended. Aim for at least minutes of moderate aerobic physical activity a week. Getting regular aerobic exercise along with getting at least two days a week of strength training exercises can help control blood sugar more effectively than does either type of exercise alone. Aerobic exercises can include walking, biking or dancing. Resistance training can include weight training and body weight exercises. Also try to spend less time sitting still. Try to get up and move around for a few minutes at least every 30 minutes or so when you're awake. Keep your vaccinations up to date. High blood sugar can weaken your immune system. Get a flu shot every year. Your provider may recommend the pneumonia and COVID vaccines, as well. The Centers for Disease Control and Prevention CDC also currently recommends hepatitis B vaccination if you haven't previously had it and you're an adult ages 19 to 59 with type 1 or type 2 diabetes. The most recent CDC guidelines suggest vaccination as soon as possible after diagnosis with type 1 or type 2 diabetes. If you are age 60 or older, have been diagnosed with diabetes, and haven't previously received the vaccine, talk to your provider about whether it's right for you. If you drink alcohol, do so responsibly. Alcohol can cause either high or low blood sugar. This depends on how much you drink and if you eat at the same time. If you choose to drink, do so only in moderation — one drink a day for women and up to two drinks a day for men — and always with food. Remember to include the carbohydrates from any alcohol you drink in your daily carbohydrate count. And check your blood sugar levels before going to bed. Many substances have been shown to improve the body's ability to process insulin in some studies. Other studies fail to find any benefit for blood sugar control or in lowering A1C levels. Because of the conflicting findings, there aren't any alternative therapies that are currently recommended to help everyone to manage blood sugar. If you decide to try any type of alternative therapy, don't stop taking the drugs that your provider has prescribed. Be sure to discuss the use of any of these therapies with your provider. Make sure that they won't cause bad reactions or interact with your current therapy. Also, no treatments — alternative or conventional — can cure diabetes. If you're using insulin therapy for diabetes, never stop using insulin unless directed to do so by your provider. Living with diabetes can be difficult and frustrating. Sometimes, even when you've done everything right, your blood sugar levels may rise. But stick with your diabetes management plan and you'll likely see a positive difference in your A1C when you visit your provider. Good diabetes management can take a great deal of time and feel overwhelming. Some people find that it helps to talk to someone. Your provider can probably recommend a mental health professional for you to speak with. Or you may want to try a support group. Sharing your frustrations and triumphs with people who understand what you're going through can be very helpful. And you may find that others have great tips to share about diabetes management. Your provider may know of a local support group. You can also call the American Diabetes Association at DIABETES or the Juvenile Diabetes Research Foundation at CURE You're likely to start by seeing your health care provider if you're having diabetes symptoms. If your child is having diabetes symptoms, you might see your child's health care provider. If blood sugar levels are very high, you'll likely be sent to the emergency room. If blood sugar levels aren't high enough to put you or your child immediately at risk, you may be referred to a provider trained in diagnosing and treating diabetes endocrinologist. Soon after diagnosis, you'll also likely meet with a diabetes educator and a registered dietitian to get more information on managing your diabetes. Preparing a list of questions can help you make the most of your time with your provider. For diabetes, some questions to ask include:. Diabetes care at Mayo Clinic. Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission. Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press. This content does not have an English version. This content does not have an Arabic version. Diagnosis Type 1 diabetes FAQs Endocrinologist Yogish Kudva, M. Care at Mayo Clinic Our caring team of Mayo Clinic experts can help you with your diabetes-related health concerns Start Here. Enlarge image Close. Continuous glucose monitor and insulin pump A continuous glucose monitor, on the left, is a device that measures your blood sugar every few minutes using a sensor inserted under the skin. Request an appointment. Thank you for subscribing! Sorry something went wrong with your subscription Please, try again in a couple of minutes Retry. By Mayo Clinic Staff. Show references Ferri FF. Diabetes mellitus. In: Ferri's Clinical Advisor Elsevier; Accessed May 7, Classification and diagnosis of diabetes: Standards of medical care in diabetes — Diabetes Care. Papadakis MA, et al. McGraw Hill; Accessed May 4, Diabetes risk factors. Centers for Disease Control and Prevention. Accessed June 2, Cunningham FG, et al. In: Williams Obstetrics. McGraw-Hill Education; Diabetes and DKA ketoacidosis. American Diabetes Association. Diabetes Canada Clinical Practice Guidelines Expert Committee. Complementary and alternative medicine for diabetes. Canadian Journal of Diabetes. Nimmagadda R. Allscripts EPSi. Mayo Clinic. June 16, Jameson JL, et al. Diabetes mellitus: Diagnosis, classification and pathophysiology. In: Harrison's Principles of Internal Medicine. Pharmacologic approaches to glycemic treatment: Standards of medical care in diabetes — Facilitating behavior change and well-being to improve health outcomes: Standards of medical care in diabetes — Type 1 diabetes mellitus. Mayo Clinic; Glycemic targets: Standards of Medical Care in diabetes — Comprehensive medical evaluation and assessment of comorbidities: Standards of Medical Care in Diabetes — Prevention or delay of type 2 diabetes and associated comorbidities: Standards of Medical Care in diabetes — Obesity and weight management for the prevention and treatment of type 2 diabetes: Standards of Medical Care in Diabetes — Diabetes technology. Standards of Medical Care in Diabetes — See also News from Mayo Clinic Science Saturday: Mayo Clinic study indicates U. rural counties have higher diabetes-related deaths Nov. CDT Innovative breakthrough offers good news for people with diabetes Nov. CDT Mayo Clinic Q and A: How does diabetes affect the heart? June 23, , p. CDT Mayo Clinic Q and A: Putting your best foot forward with diabetes May 09, , p. CDT Mayo Clinic Q and A: Diabetes and fasting during Ramadan April 07, , p. CDT Nonprofit co-founded by Mayo Clinic announces plan to manufacture affordable insulin March 03, , p. CDT Show more news from Mayo Clinic. Mayo Clinic Press Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press. Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book. Show the heart some love! Give Today. |
| 8 Ways to Lower Your Blood Sugar | Check your blood sugar level as directed by your provider. And watch for symptoms of high blood sugar, including:. Diabetic ketoacidosis is a serious complication of diabetes. If your cells are starved for energy, your body may begin to break down fat. This makes toxic acids known as ketones, which can build up in the blood. Watch for the following symptoms:. You can check your urine for excess ketones with a ketones test kit that you can get without a prescription. If you have excess ketones in your urine, talk with your provider right away or seek emergency care. This condition is more common in people with type 1 diabetes. This condition is seen in people with type 2 diabetes. It often happens after an illness. Call your provider or seek medical care right away if you have symptoms of this condition. If your blood sugar level drops below your target range, it's known as low blood sugar diabetic hypoglycemia. If you're taking drugs that lower your blood sugar, including insulin, your blood sugar level can drop for many reasons. These include skipping a meal and getting more physical activity than normal. Low blood sugar also occurs if you take too much insulin or too much of a glucose-lowering medication that causes the pancreas to hold insulin. Low blood sugar is best treated with carbohydrates that your body can absorb quickly, such as fruit juice or glucose tablets. There is a problem with information submitted for this request. Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview. Error Email field is required. Error Include a valid email address. To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail. You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox. Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition. Diabetes is a serious disease. Following your diabetes treatment plan takes total commitment. Careful management of diabetes can lower your risk of serious or life-threatening complications. Make physical activity part of your daily routine. Regular physical activity can help prevent prediabetes and type 2 diabetes. It can also help those who already have diabetes to maintain better blood sugar control. A minimum of 30 minutes of moderate physical activity — such as brisk walking — most days of the week is recommended. Aim for at least minutes of moderate aerobic physical activity a week. Getting regular aerobic exercise along with getting at least two days a week of strength training exercises can help control blood sugar more effectively than does either type of exercise alone. Aerobic exercises can include walking, biking or dancing. Resistance training can include weight training and body weight exercises. Also try to spend less time sitting still. Try to get up and move around for a few minutes at least every 30 minutes or so when you're awake. Keep your vaccinations up to date. High blood sugar can weaken your immune system. Get a flu shot every year. Your provider may recommend the pneumonia and COVID vaccines, as well. The Centers for Disease Control and Prevention CDC also currently recommends hepatitis B vaccination if you haven't previously had it and you're an adult ages 19 to 59 with type 1 or type 2 diabetes. The most recent CDC guidelines suggest vaccination as soon as possible after diagnosis with type 1 or type 2 diabetes. If you are age 60 or older, have been diagnosed with diabetes, and haven't previously received the vaccine, talk to your provider about whether it's right for you. If you drink alcohol, do so responsibly. Alcohol can cause either high or low blood sugar. This depends on how much you drink and if you eat at the same time. If you choose to drink, do so only in moderation — one drink a day for women and up to two drinks a day for men — and always with food. Remember to include the carbohydrates from any alcohol you drink in your daily carbohydrate count. And check your blood sugar levels before going to bed. Many substances have been shown to improve the body's ability to process insulin in some studies. Other studies fail to find any benefit for blood sugar control or in lowering A1C levels. Because of the conflicting findings, there aren't any alternative therapies that are currently recommended to help everyone to manage blood sugar. If you decide to try any type of alternative therapy, don't stop taking the drugs that your provider has prescribed. Be sure to discuss the use of any of these therapies with your provider. Make sure that they won't cause bad reactions or interact with your current therapy. Also, no treatments — alternative or conventional — can cure diabetes. If you're using insulin therapy for diabetes, never stop using insulin unless directed to do so by your provider. Living with diabetes can be difficult and frustrating. Sometimes, even when you've done everything right, your blood sugar levels may rise. But stick with your diabetes management plan and you'll likely see a positive difference in your A1C when you visit your provider. Good diabetes management can take a great deal of time and feel overwhelming. Some people find that it helps to talk to someone. Your provider can probably recommend a mental health professional for you to speak with. Or you may want to try a support group. Sharing your frustrations and triumphs with people who understand what you're going through can be very helpful. And you may find that others have great tips to share about diabetes management. Your provider may know of a local support group. You can also call the American Diabetes Association at DIABETES or the Juvenile Diabetes Research Foundation at CURE You're likely to start by seeing your health care provider if you're having diabetes symptoms. If your child is having diabetes symptoms, you might see your child's health care provider. If blood sugar levels are very high, you'll likely be sent to the emergency room. If blood sugar levels aren't high enough to put you or your child immediately at risk, you may be referred to a provider trained in diagnosing and treating diabetes endocrinologist. Soon after diagnosis, you'll also likely meet with a diabetes educator and a registered dietitian to get more information on managing your diabetes. Preparing a list of questions can help you make the most of your time with your provider. For diabetes, some questions to ask include:. Diabetes care at Mayo Clinic. Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission. Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press. This content does not have an English version. This content does not have an Arabic version. Diagnosis Type 1 diabetes FAQs Endocrinologist Yogish Kudva, M. Care at Mayo Clinic Our caring team of Mayo Clinic experts can help you with your diabetes-related health concerns Start Here. Enlarge image Close. Continuous glucose monitor and insulin pump A continuous glucose monitor, on the left, is a device that measures your blood sugar every few minutes using a sensor inserted under the skin. Request an appointment. Thank you for subscribing! Sorry something went wrong with your subscription Please, try again in a couple of minutes Retry. By Mayo Clinic Staff. Show references Ferri FF. Diabetes mellitus. In: Ferri's Clinical Advisor Elsevier; Accessed May 7, Classification and diagnosis of diabetes: Standards of medical care in diabetes — Diabetes Care. Papadakis MA, et al. McGraw Hill; Accessed May 4, Diabetes risk factors. Centers for Disease Control and Prevention. Accessed June 2, Cunningham FG, et al. In: Williams Obstetrics. McGraw-Hill Education; Healthy eating is important for everyone. But when you have diabetes, you need to know how foods affect your blood sugar levels. It's not only the type of food you eat. It's also how much you eat and the types of food you combine in meals and snacks. Learn about planning balanced meals. A healthy-eating plan includes knowing what to eat and how much to eat. Two common ways to plan meals are carbohydrate counting and the plate method. Ask your healthcare professional or a registered dietitian if either type of meal planning is right for you. Understand carbohydrate counting. Counting carbs involves keeping track of how many grams of carbohydrates you eat and drink during the day. If you take diabetes medicine called insulin at mealtimes, it's important to know the amount of carbohydrates in foods and drinks. That way, you can take the right dose of insulin. Among all foods, carbs often have the biggest impact on blood sugar levels. That's because the body breaks them down into sugar, which raises blood sugar levels. Some carbs are better for you than others. For example, fruits, vegetables and whole grains are full of nutrients. They have fiber that helps keep blood sugar levels more stable too. Eat fewer refined, highly processed carbs. These include white bread, white rice, sugary cereal, cakes, cookies, candy and chips. Get to know the plate method. This type of meal planning is simpler than counting carbs. The plate method helps you eat a healthy balance of foods and control portion sizes. Use a 9-inch plate. Fill half of the plate with nonstarchy vegetables. Examples include lettuce, cucumbers, broccoli, tomatoes and green beans. Divide the other half of the plate into two smaller, equal sections. You might hear these smaller sections called quarters. In one quarter of the plate, place a lean protein. Examples include fish, beans, eggs, and lean meat and poultry. On the other quarter, place healthy carbohydrates such as fruits and whole grains. Be mindful of portion sizes. Learn what portion size is right for each type of food. Everyday objects can help you remember. For example, one serving of meat or poultry is about the size of a deck of cards. A serving of cheese is about the size of six grapes. And a serving of cooked pasta or rice is about the size of a fist. You also can use measuring cups or a scale to help make sure you get the right portion sizes. Balance your meals and medicines. If you take diabetes medicine, it's important to balance what you eat and drink with your medicine. Too little food in proportion to your diabetes medicine — especially insulin — can lead to dangerously low blood sugar. This is called hypoglycemia. Too much food may cause your blood sugar level to climb too high. This is called hyperglycemia. Talk to your diabetes health care team about how to best coordinate meal and medicine schedules. Limit sugary drinks. Sugar-sweetened drinks tend to be high in calories and low in nutrition. They also cause blood sugar to rise quickly. So it's best to limit these types of drinks if you have diabetes. The exception is if you have a low blood sugar level. Sugary drinks can be used to quickly raise blood sugar that is too low. These drinks include regular soda, juice and sports drinks. Exercise is another important part of managing diabetes. When you move and get active, your muscles use blood sugar for energy. Regular physical activity also helps your body use insulin better. These factors work together to lower your blood sugar level. The more strenuous your workout, the longer the effect lasts. But even light activities can improve your blood sugar level. Light activities include housework, gardening and walking. Talk to your healthcare professional about an exercise plan. Ask your healthcare professional what type of exercise is right for you. In general, most adults should get at least minutes a week of moderate aerobic activity. That includes activities that get the heart pumping, such as walking, biking and swimming. Aim for about 30 minutes of moderate aerobic activity a day on most days of the week. Most adults also should aim to do strength-building exercise 2 to 3 times a week. If you haven't been active for a long time, your healthcare professional may want to check your overall health first. Then the right balance of aerobic and muscle-strengthening exercise can be recommended. Keep an exercise schedule. Ask your healthcare professional about the best time of day for you to exercise. That way, your workout routine is aligned with your meal and medicine schedules. Know your numbers. Talk with your healthcare professional about what blood sugar levels are right for you before you start exercise. Check your blood sugar level. Also talk with your healthcare professional about your blood sugar testing needs. If you don't take insulin or other diabetes medicines, you likely won't need to check your blood sugar before or during exercise. But if you take insulin or other diabetes medicines, testing is important. Check your blood sugar before, during and after exercise. Many diabetes medicines lower blood sugar. So does exercise, and its effects can last up to a day later. The risk of low blood sugar is greater if the activity is new to you. The risk also is greater if you start to exercise at a more intense level. Be aware of symptoms of low blood sugar. These include feeling shaky, weak, tired, hungry, lightheaded, irritable, anxious or confused. See if you need a snack. Have a small snack before you exercise if you use insulin and your blood sugar level is low. The snack you have before exercise should contain about 15 to 30 grams of carbs. Or you could take 10 to 20 grams of glucose products. This helps prevent a low blood sugar level. Stay hydrated. Drink plenty of water or other fluids while exercising. Dehydration can affect blood sugar levels. Be prepared. Always have a small snack, glucose tablets or glucose gel with you during exercise. You'll need a quick way to boost your blood sugar if it drops too low. Carry medical identification too. In case of an emergency, medical identification can show others that you have diabetes. It also can show whether you take diabetes medicine such as insulin. Medical IDs come in forms such as cards, bracelets and necklaces. Adjust your diabetes treatment plan as needed. If you take insulin, you may need to lower your insulin dose before you exercise. You also may need to watch your blood sugar level closely for several hours after intense activity. That's because low blood sugar can happen later on. Your healthcare professional can advise you how to correctly make changes to your medicine. You also may need to adjust your treatment if you've increased how often or how hard you exercise. Insulin and other diabetes medicines are designed to lower blood sugar levels when diet and exercise alone don't help enough. How well these medicines work depends on the timing and size of the dose. Medicines you take for conditions other than diabetes also can affect your blood sugar levels. Store insulin properly. Insulin that is not stored properly or is past its expiration date may not work. Keep insulin away from extreme heat or cold. Don't store it in the freezer or in direct sunlight. Tell your healthcare professional about any medicine problems. If your diabetes medicines cause your blood sugar level to drop too low, the dosage or timing may need to be changed. Your healthcare professional also might adjust your medicine if your blood sugar stays too high. Urine ketone testing is done with a dipstick, available in pharmacies without a prescription. If you have moderate to large ketones, you should call your health care provider immediately to determine the best treatment. You may need to take an additional dose of insulin, or your provider may instruct you to go to the nearest emergency room. Meters that measure ketone levels in the blood are also available, but due to their cost, urine testing is more widely used. ADJUSTING TREATMENT. Checking your glucose either with blood glucose monitoring [BGM] or continuous glucose monitoring [CGM] provides useful information and is an important part of managing your diabetes. If you use insulin, your glucose results will help guide you in choosing the appropriate doses from meal to meal. When you first start treatment for diabetes, you will need to work with your health care provider as you learn to make adjustments in treatment. However, with time and experience, most people learn how to make many of these adjustments on their own. Your health care provider is the best source of information for questions and concerns related to your medical problem. This article will be updated as needed on our website www. Related topics for patients, as well as selected articles written for health care professionals, are also available. Some of the most relevant are listed below. Patient level information — UpToDate offers two types of patient education materials. The Basics — The Basics patient education pieces answer the four or five key questions a patient might have about a given condition. These articles are best for patients who want a general overview and who prefer short, easy-to-read materials. Patient education: Type 2 diabetes The Basics Patient education: Using insulin The Basics Patient education: Treatment for type 2 diabetes The Basics Patient education: Low blood sugar in people with diabetes The Basics Patient education: Care during pregnancy for people with type 1 or type 2 diabetes The Basics Patient education: My child has diabetes: How will we manage? The Basics Patient education: Managing blood sugar in children with diabetes The Basics Patient education: Managing diabetes in school The Basics Patient education: Hemoglobin A1C tests The Basics Patient education: Giving your child insulin The Basics Patient education: Checking your child's blood sugar level The Basics Patient education: Diabetic ketoacidosis The Basics Patient education: Hyperosmolar hyperglycemic state The Basics Patient education: Diabetes and infections The Basics. Beyond the Basics — Beyond the Basics patient education pieces are longer, more sophisticated, and more detailed. These articles are best for patients who want in-depth information and are comfortable with some medical jargon. Patient education: Type 1 diabetes: Overview Beyond the Basics Patient education: Care during pregnancy for patients with type 1 or 2 diabetes Beyond the Basics Patient education: Type 2 diabetes: Overview Beyond the Basics. Professional level information — Professional level articles are designed to keep doctors and other health professionals up-to-date on the latest medical findings. These articles are thorough, long, and complex, and they contain multiple references to the research on which they are based. Professional level articles are best for people who are comfortable with a lot of medical terminology and who want to read the same materials their doctors are reading. Glucose monitoring in the ambulatory management of nonpregnant adults with diabetes mellitus Measurements of chronic glycemia in diabetes mellitus Overview of the management of type 1 diabetes mellitus in children and adolescents Treatment of type 2 diabetes mellitus in the older patient. org , available in English and Spanish. Why UpToDate? Product Editorial Subscription Options Subscribe Sign in. Learn how UpToDate can help you. Select the option that best describes you. View Topic. Font Size Small Normal Large. Patient education: Glucose monitoring in diabetes Beyond the Basics. Formulary drug information for this topic. No drug references linked in this topic. Find in topic Formulary Print Share. Author: Ruth S Weinstock, MD, PhD Section Editor: David M Nathan, MD Deputy Editor: Katya Rubinow, MD Contributor Disclosures. All topics are updated as new evidence becomes available and our peer review process is complete. Literature review current through: Jan This topic last updated: Apr 06, GLUCOSE TESTING OVERVIEW If you have diabetes, you have an important role in your own medical care and monitoring your glucose sugar level is a key part of this. FREQUENCY OF GLUCOSE TESTING Studies have proven that people with diabetes who maintain normal or near-normal blood glucose levels reduce their risk of diabetes-related complications. ADJUSTING TREATMENT Checking your glucose either with blood glucose monitoring [BGM] or continuous glucose monitoring [CGM] provides useful information and is an important part of managing your diabetes. The Basics Patient education: Managing blood sugar in children with diabetes The Basics Patient education: Managing diabetes in school The Basics Patient education: Hemoglobin A1C tests The Basics Patient education: Giving your child insulin The Basics Patient education: Checking your child's blood sugar level The Basics Patient education: Diabetic ketoacidosis The Basics Patient education: Hyperosmolar hyperglycemic state The Basics Patient education: Diabetes and infections The Basics Beyond the Basics — Beyond the Basics patient education pieces are longer, more sophisticated, and more detailed. Patient education: Type 1 diabetes: Overview Beyond the Basics Patient education: Care during pregnancy for patients with type 1 or 2 diabetes Beyond the Basics Patient education: Type 2 diabetes: Overview Beyond the Basics Professional level information — Professional level articles are designed to keep doctors and other health professionals up-to-date on the latest medical findings. Glucose monitoring in the ambulatory management of nonpregnant adults with diabetes mellitus Measurements of chronic glycemia in diabetes mellitus Overview of the management of type 1 diabetes mellitus in children and adolescents Treatment of type 2 diabetes mellitus in the older patient The following organizations also provide reliable health information. org , available in English and Spanish [ ]. Translating the A1C assay into estimated average glucose values. Diabetes Care ; ElSayed NA, Aleppo G, Aroda VR, et al. Diabetes Technology: Standards of Care in Diabetes Diabetes Care ; S Machry RV, Rados DV, Gregório GR, Rodrigues TC. Self-monitoring blood glucose improves glycemic control in type 2 diabetes without intensive treatment: A systematic review and meta-analysis. Diabetes Res Clin Pract ; Danne T, Nimri R, Battelino T, et al. International Consensus on Use of Continuous Glucose Monitoring. |
Ich denke, dass Sie den Fehler zulassen. Geben Sie wir werden es besprechen. Schreiben Sie mir in PM, wir werden umgehen.
Welche Wörter... Toll, der prächtige Gedanke