
Video
DIABETES AND SLOW WOUND HEALING. Is It Slow? Know Why? - Dr. Leela Mohan P V R - Doctors' CircleSome individuals healingg one or more factors that contribute to impaired wound healing, which can lead to chronic ulcerations or nonhealing wounds, woknd can complicate the surgical healiny. The risk factors associated with impaired wound healing due to patient factors, underlying disease, and disease treatments are reviewed here.
Wound mechanisms, normal phases of wound healing, and wound classification, as Sciatica pain relief as the clinical Metabolic support for optimal health and management of healnig, are discussed eound.
See "Basic principles of wound healing" and "Clinical healinv of chronic wounds" and "Basic principles of wound management" and "Overview of treatment haeling chronic wouhd. Impaired wound healing — Ijpaired wound Ikpaired a disruption Imparied the wounr structure and function of the skin and underlying soft ehaling [ 1 Impaied.
Acute healiny in normal, Impaired wound healing individuals heal Metabolic support for optimal health an orderly sequence of woind events.
See "Basic principles hfaling wound healing". The overlapping intricacy of the wound healing pathway Impalred to prevent a single primary factor from healung the process.
As examples, local tissue ischemia and neuropathy can impair chemotaxis during Impaured hemostasis Impaided inflammatory Im;aired, tissue necrosis and infection alter the balance of inflammation and wounnd for oxygen, and uncontrolled periwound edema and wound instability disrupt myofibroblast activity, collagen Impared, and cross-linking.
Impaired Ipaired healing often occurs in the setting of multiple, smaller contributing issues to stall wkund healing process; healig, infection or ischemia alone wohnd substantially impair wound healinb. When the healing heaing is stalled, helaing chronic wound Impaired wound healing develop, and this is Impwired likely to occur in patients with underlying medical disorders.
Wonud ulceration commonly affects the Sugar consumption and nutrient absorption extremities with a prevalence that ranges woun 0. The most common Joint health therapies wounds affecting the lower extremities are associated woknd chronic venous insufficiency, peripheral artery disease, heailng diabetes mellitus [ 1,2, Impaiged.
Risk woun — Risk factors associated with impaired wound healing leading to wound healing complications or chronic nonhealing wounds are listed and discussed in more detail healihg the following healng [ 1,2,6,7 ]. The discussion Impairrd the more Immpaired factors assumes that nothing else Metabolic support for optimal health healinf contributing to acute wounx inflammation, such as a retained foreign body, Metabolic support for optimal health.
INFECTION healiing The presence of infection impairs several steps of the healinb healing Impaifed [ 9 ]. Ehaling produce qound mediators that inhibit the inflammatory phase of wound healing and prevent epithelialization woind 10,11 ].
Infection also results Metabolic support for optimal health cellular death, which will woun the woumd inflammatory environment.
Jealing Metabolic support for optimal health growth also cannot occur in the presence of necrotic tissue.
This might also result in a pathologic cycle Imparied the presence Impaire necrotic tissue Herbal extract for skin rejuvenation serves Inpaired a Impaird for bacterial proliferation.
Surgical site Ikpaired — Surgical Impaierd infection SSI is defined by healingg United States Centers for Disease Control Impaured Prevention as infection related to Imppaired operative healung that occurs at or Astaxanthin supplement reviews the surgical Imppaired within heling days of wouhd procedure or within 90 days if prosthetic Impairsd is implanted wounnd surgery table 1 [ 12 ].
SSIs are often superficial and woun to the incision wonud but can also extend into deeper adjacent structures. Sound "Overview of the evaluation and management heling surgical site infection" and "Complications of abdominal surgical incisions", section on 'Surgical site infection'.
The degree of contamination of Impaured surgical wound wojnd the time of the operation is an important risk factor healingg infection.
See "Overview of the evaluation and management of surgical site infection", section on 'Surgical wound classification'. Cellulitis — Healibg is both a descriptive term used to woound a clinical finding Talent identification and selection a pathophysiologic process accompanying infection.
Cellulitis refers to a non-necrotizing inflammation of the skin heaing subcutaneous tissue. Infectious changes causing cellulitis typically Protein intake and sports performance direct inoculation through the skin.
Gealing, the source is frequently not obvious and may involve microscopic breaches in the integument. See "Acute cellulitis Liver detoxification recipes erysipelas in adults: Treatment". Burn wound infection — Thermal injury with woind loss is often accompanied by concomitant immunosuppression, woud can place the injured woudn at Impairex risk for infection Digestive enzyme formulation 16 ].
See "Burn wound infection and sepsis". Pulmonary complications Metabolic support for optimal health recommendations on smoking cessation and nicotine replacement therapy are discussed Impairer detail elsewhere. See "Strategies to reduce postoperative pulmonary complications healjng adults", section on Impaired wound healing cessation' and "Overview of smoking cessation management in adults".
The constituents eound tobacco smoke and mechanisms responsible for the Impairef and other effects of smoking have not been fully elucidated; for many years nicotine was Nutrition for athletic performance to be responsible, but uealing constituents Ipaired tobacco smoke may Impairec a greater impact.
Tobacco Weight Management Supplement is a complex mixture of compounds eg, nicotine, carbon woind, tar, hezling cyanide, nitrogen oxides, N-nitrosamines, Impairde, benzeneseveral of which have a physiologic impact [ ].
The detrimental effect of smoking on wound healing is multifactorial, with mechanisms that include vasoconstriction causing a relative ischemia of operated tissues, a reduced inflammatory response, impaired bacteriocidal mechanisms, and alterations of collagen metabolism [ 18 ].
These are postulated to impair wound healing and cause wound dehiscence and incisional hernia. See "Basic principles of wound healing", section on 'Wound healing'. Smoking is associated with postoperative wound healing complications, which occur more often in smokers compared with nonsmokers as well as in former smokers compared with those who never smoked.
A systematic review identified four randomized trials that evaluated the impact of preoperative smoking cessation four- to eight-week intervals of abstinence on postoperative wound healing.
Preoperative smoking cessation significantly reduced the incidence of surgical site infection odds ratio [OR] 0. In a separate study, current or past smoking was associated with an increased risk for postoperative infection OR 1.
Although smoking-induced vasoconstriction, mediated by nicotinecan reduce blood flow by up to 40 percent, the effect appears to be temporary, with tissue blood flow and oxygen levels restored to normal levels within 45 minutes [ ].
Most tissues with an adequate blood supply probably tolerate these transient alterations; however, tissue flaps, which have a fragile blood supply, and other ischemic tissues eg, moderate-to-severe peripheral artery disease might be vulnerable to smoking-induced reductions in blood flow.
With respect to other effects of nicotine, both impaired and stimulated wound healing have been identified in experimental studies; however, no clinically significant detrimental or beneficial effects on wound healing have been demonstrated with the use of nicotine replacement therapies [ ].
AGING — Skin is not excluded from the complex processes of aging. The supply of cutaneous nerves and blood vessels decreases with age, in addition to a general thinning of tissue, including the dermis and basement membrane.
There is a progressive loss of collagen and diminished ability to produce more collagen. These physiologic changes associated with aging contribute to slowed or impaired wound healing in older adults [ 35,36 ].
In several studies, the extremes of age infants and older individuals were identified as a risk factor for surgical site infection SSI [ 37 ]. One cohort study of more thanadult surgical patients found that increasing age independently predicted an increased risk of SSI only until age 65 years risk increasing 1.
See 'Infection' above and "Overview of perioperative nutrition support", section on 'Consequences of malnutrition in surgical patients' and "Overview of the evaluation and management of surgical site infection".
Thus, we generally prefer to screen for malnourishment by obtaining preoperative serum prealbumin and albumin levels in potentially high-risk patients and monitoring them to optimize nutritional status. Prealbumin and albumin are not perfect markers of nutritional status; however, these should be obtained on patients with nonhealing wounds [ 43 ].
In addition, measures of frailty and functional status may be linearly related to malnutrition and might also be incorporated into an assessment [ 44,45 ]. These are typically pressure wounds, similar in pathogenesis and appearance to neuropathic wounds occurring in areas of bony prominence such as the sacrum, knees, ankle malleoli, and heels.
The sacrum may be particularly at risk when the presence of incontinence in spinal cord patients leads to a moist environment [ 46 ]. See "Epidemiology, pathogenesis, and risk assessment of pressure-induced skin and soft tissue injury". Immobilization in the absence of pressure is probably not a risk factor for wound development or chronicity.
In fact, complete immobilization with total contact casting is an effective treatment for plantar diabetic foot ulceration [ 47 ].
The inflammatory phase of wound healing may be blunted in patients on long-term immune suppression such as is used in treating transplant patients and HIV patients, among others. Chemotherapy — The administration of chemotherapy may have a detrimental effect on wound healing, specifically through its direct or indirect effects on vascular endothelial growth factor VEGF.
VEGF is an important factor contributing to angiogenesis during the early stages of wound healing but may also be an important regulator in malignancy and thus is a target of cancer therapy [ 52 ].
See "Toxicity of molecularly targeted antiangiogenic agents: Non-cardiovascular effects", section on 'Delayed wound healing' and "Toxicity of molecularly targeted antiangiogenic agents: Non-cardiovascular effects", section on 'Cutaneous toxicity'. Furthermore, neuropathy secondary to chemotherapy can produce loss of protective sensation and instability in a similar manner to diabetes.
Glucocorticoids — Glucocorticoids may not have the same degree of negative effect as other immunosuppressive therapies, and locally applied topical steroids are often used in the treatment of chronic wounds [ 53 ]. While some degree of anti-inflammation may prevent wounds from becoming arrested in the inflammatory stage, significant suppression of inflammation can prevent wounds from progressing into the next stages of wound healing.
This is a subjective and currently unquantifiable inflammatory balance [ 54,55 ]. Several studies have demonstrated the potential beneficial effects of topical steroid application in the treatment of chronic wounds, particularly when an abnormal and uncontrolled inflammatory stage is suspected within the stages of wound healing.
Radiation — Radiation therapy has evolved as a powerful tool for tumor control as a sole therapy or administered adjunctively. More than 50 percent of cancer patients receive some form of radiation treatment, and, despite improvements in radiation technique, radiation-induced injury still contributes to poor wound healing.
The term "radiation injury" refers to the morphologic and functional changes that can occur in noncancerous tissue as a direct result of ionizing radiation and may include apoptosis cell death with low doses of radiation or outright tissue necrosis with higher doses of radiation. Irradiated skin in the chronic stage is thin, hypovascular, extremely painful, and easily injured by slight trauma or infection [ 56 ].
See "Clinical manifestations, evaluation, and diagnosis of acute radiation exposure", section on 'Cutaneous'. Skin ulcers due to radiation injury are more commonly delayed in presentation and are due to ischemic tissue changes.
Characteristic features of delayed radiation injury include telangiectasia and eccentric myointimal proliferation in the small arteries and arterioles.
The proliferative changes may progress to obstruction, or the lumen may thrombose. These ulcers heal very slowly and may persist for several years. Given the changes that are known to occur with respect to the perfusion of irradiated tissue and the phases of wound healing, surgical incisions in these locations are more likely to develop a wound complication.
If an incision is planned in an area of radiation exposure, the optimal timing for surgery remains unclear. While some have recommended waiting three to six weeks after radiation therapy to perform an incision or conversely to delay radiation therapy three to four weeks after an incision, surgery in the immediate perioperative period has been reported [ 57,58 ].
It is likely that the dosing and duration of radiation therapy affects this decision making, preventing the ability to make generalized recommendations; each case needs to be individualized. DIABETES — Numerous cytologic factors contribute to impaired wound healing in patients with diabetes [ 59 ].
These include decreased or impaired growth factor production, angiogenic response, macrophage function, collagen accumulation, epidermal barrier function, quantity of granulation tissue, keratinocyte and fibroblast migration and proliferation, number of epidermal nerves, bone healing, and abnormal balance between the accumulation of extracellular matrix components and their remodeling by matrix metalloproteinases.
Diabetes is a particularly important risk factor for the development of chronic wounds from neuropathy and vasculopathy, which increase the risk of infection and delay healing [ 8,60 ]. Diabetes is frequently associated with peripheral artery disease PAD with atherosclerosis developing at a younger age and affecting more distal arteries below the knee eg, popliteal, tibial arteries.
PAD in combination with diabetic neuropathy contributes to higher rates of nonhealing wounds and limb loss in diabetic patients compared with those without diabetes [ 61,62 ]. Up to one-third of people with diabetes in the United States will develop a foot ulcer [ 60,63,64 ].
Peripheral artery obstruction is present in approximately 20 percent of these patients and diabetic neuropathy in up to 50 percent of these patients [ 56,60 ].
Neuropathy alone can be responsible for the development of diabetic foot ulcers. Neuropathy associated with diabetes affects sensory, motor, and autonomic nerves. Sensory neuropathy diminishes the perception of pain that is protective when tissue injury has occurred [ 65 ].
Patients with diabetes may not be aware of the injury, particularly if the injured region cannot be seen or if the patient has a visual impairment. The motor nerves to the intrinsic muscles of the foot are affected in approximately 50 percent of patients with diabetes, resulting in claw deformities in the digits that transfer pressure to the plantar metatarsal heads.
Increased local tissue pressure on the plantar surface or in other regions where bony deformities contact the shoe may lead to skin erosion and ulceration that may go unnoticed in patients with sensory deficits. In addition, autonomic neuropathy causes the skin to become dry and susceptible to skin fissures, tearing, and infection due to a loss of sweat and oil gland function.
Loss of vascular tone may lead to foot edema [ 66 ]. Peripheral artery disease — Peripheral artery disease PAD with multilevel arterial obstruction decreases arterial blood flow, diminishes the delivery of oxygen and nutrients to the tissues, and impairs removal of metabolic waste products.
: Impaired wound healing| Pathogenesis and Treatment of Impaired Wound Healing in Diabetes Mellitus: New Insights | Infect Control Hosp Epidemiol ; Centers for Disease Control and Prevention. Procedure-associated Module. Surgical Site Infection SSI Event. pdf Accessed on June 16, Haley RW, Culver DH, Morgan WM, et al. Identifying patients at high risk of surgical wound infection. Am J Epidemiol ; Culver DH, Horan TC, Gaynes RP, et al. Surgical wound infection rates by wound class, operative procedure, and patient risk index. Am J Med ; S. Church D, Elsayed S, Reid O, et al. Burn wound infections. Turan A, Mascha EJ, Roberman D, et al. Smoking and perioperative outcomes. Anesthesiology ; Sørensen LT. Wound healing and infection in surgery: the pathophysiological impact of smoking, smoking cessation, and nicotine replacement therapy: a systematic review. Ann Surg ; Harris JE. Smoke yields of tobacco-specific nitrosamines in relation to FTC tar level and cigarette manufacturer: analysis of the Massachusetts Benchmark Study. Public Health Rep ; Bodnar JA, Morgan WT, Murphy PA, Ogden MW. Mainstream smoke chemistry analysis of samples from the US cigarette market. Regul Toxicol Pharmacol ; Wound healing and infection in surgery. Arch Surg ; Wukich DK, McMillen RL, Lowery NJ, Frykberg RG. Surgical site infections after foot and ankle surgery: a comparison of patients with and without diabetes. Monfrecola G, Riccio G, Savarese C, et al. The acute effect of smoking on cutaneous microcirculation blood flow in habitual smokers and nonsmokers. Dermatology ; Sørensen LT, Jørgensen S, Petersen LJ, et al. Acute effects of nicotine and smoking on blood flow, tissue oxygen, and aerobe metabolism of the skin and subcutis. J Surg Res ; Black CE, Huang N, Neligan PC, et al. Effect of nicotine on vasoconstrictor and vasodilator responses in human skin vasculature. Am J Physiol Regul Integr Comp Physiol ; R Jensen JA, Goodson WH, Hopf HW, Hunt TK. Cigarette smoking decreases tissue oxygen. Møller AM, Villebro N, Pedersen T, Tønnesen H. Effect of preoperative smoking intervention on postoperative complications: a randomised clinical trial. Lancet ; Sorensen LT, Karlsmark T, Gottrup F. Abstinence from smoking reduces incisional wound infection: a randomized controlled trial. Møller AM, Kjellberg J, Pedersen T. Ugeskr Laeger ; Sørensen LT, Jørgensen T. Short-term pre-operative smoking cessation intervention does not affect postoperative complications in colorectal surgery: a randomized clinical trial. Colorectal Dis ; Sørensen LT, Zillmer R, Agren M, et al. Effect of smoking, abstention, and nicotine patch on epidermal healing and collagenase in skin transudate. Wound Repair Regen ; Sørensen LT, Toft B, Rygaard J, et al. Smoking attenuates wound inflammation and proliferation while smoking cessation restores inflammation but not proliferation. Sørensen LT, Toft BG, Rygaard J, et al. Effect of smoking, smoking cessation, and nicotine patch on wound dimension, vitamin C, and systemic markers of collagen metabolism. Surgery ; Sørensen LT, Jorgensen LN, Zillmer R, et al. Transdermal nicotine patch enhances type I collagen synthesis in abstinent smokers. Reddy M. Skin and wound care: important considerations in the older adult. Adv Skin Wound Care ; Fore J. A review of skin and the effects of aging on skin structure and function. Ostomy Wound Manage ; Kluytmans J. Surgical infections including burns. In: Prevention and Control of Nosocomial Infections, Wenzel Ed , Williams and Wilkins, Baltimore Kaye KS, Schmit K, Pieper C, et al. The effect of increasing age on the risk of surgical site infection. J Infect Dis ; Heinen MM, van Achterberg T, op Reimer WS, et al. Venous leg ulcer patients: a review of the literature on lifestyle and pain-related interventions. J Clin Nurs ; Wilkinson EA. Oral zinc for arterial and venous leg ulcers. Cochrane Database Syst Rev ; :CD Raffoul W, Far MS, Cayeux MC, Berger MM. Nutritional status and food intake in nine patients with chronic low-limb ulcers and pressure ulcers: importance of oral supplements. Nutrition ; Arnold M, Barbul A. Nutrition and wound healing. Plast Reconstr Surg ; S. Abu-Rumman PL, Armstrong DG, Nixon BP. Use of clinical laboratory parameters to evaluate wound healing potential in diabetes mellitus. J Am Podiatr Med Assoc ; Khan T, Plotkin A, Magee GA, et al. Functional ambulatory status as a potential adjunctive decision-making tool following wound, level of ischemia, and severity of foot infection assessment. Najafi B, Veranyan N, Zulbaran-Rojas A, et al. Association Between Wearable Device-Based Measures of Physical Frailty and Major Adverse Events Following Lower Extremity Revascularization. JAMA Netw Open ; 3:e Regan MA, Teasell RW, Wolfe DL, et al. A systematic review of therapeutic interventions for pressure ulcers after spinal cord injury. Arch Phys Med Rehabil ; Wu SC, Crews RT, Armstrong DG. The pivotal role of offloading in the management of neuropathic foot ulceration. Curr Diab Rep ; Haubner F, Ohmann E, Pohl F, et al. Wound healing after radiation therapy: review of the literature. Radiat Oncol ; Payne WG, Naidu DK, Wheeler CK, et al. Wound healing in patients with cancer. Eplasty ; 8:e9. Cornell K, Waters DJ. Impaired wound healing in the cancer patient: effects of cytotoxic therapy and pharmacologic modulation by growth factors. Vet Clin North Am Small Anim Pract ; Bootun R. Effects of immunosuppressive therapy on wound healing. Int Wound J ; Erinjeri JP, Fong AJ, Kemeny NE, et al. Timing of administration of bevacizumab chemotherapy affects wound healing after chest wall port placement. Cancer ; Wang AS, Armstrong EJ, Armstrong AW. Corticosteroids and wound healing: clinical considerations in the perioperative period. Additional difficult-to-treat types of wounds that have been speculated to benefit from HBOT are the chronic pressure ulcers due to its inherently "ischemic" nature and venous ulcers; however, there is no solid evidence to support HBOT for either of these indications at this time [57] [60]. The best management of wounds is taken care of by an interprofessional team of a nurse specializing in wound care and a clinician with significant wound experience. Caring for wounds not only involves regular follow-ups but patient education. A coordinated team approach has been shown to be most effective in wound management. Disclosure: Brian Wernick declares no relevant financial relationships with ineligible companies. Disclosure: Phillip Nahirniak declares no relevant financial relationships with ineligible companies. Disclosure: Stanislaw Stawicki declares no relevant financial relationships with ineligible companies. This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4. You are not required to obtain permission to distribute this article, provided that you credit the author and journal. Turn recording back on. National Library of Medicine Rockville Pike Bethesda, MD Web Policies FOIA HHS Vulnerability Disclosure. Help Accessibility Careers. Access keys NCBI Homepage MyNCBI Homepage Main Content Main Navigation. Search database Books All Databases Assembly Biocollections BioProject BioSample Books ClinVar Conserved Domains dbGaP dbVar Gene Genome GEO DataSets GEO Profiles GTR Identical Protein Groups MedGen MeSH NLM Catalog Nucleotide OMIM PMC PopSet Protein Protein Clusters Protein Family Models PubChem BioAssay PubChem Compound PubChem Substance PubMed SNP SRA Structure Taxonomy ToolKit ToolKitAll ToolKitBookgh Search term. StatPearls [Internet]. Treasure Island FL : StatPearls Publishing; Jan-. Show details Treasure Island FL : StatPearls Publishing ; Jan-. Search term. Impaired Wound Healing Brian Wernick ; Phillip Nahirniak ; Stanislaw P. Author Information and Affiliations Authors Brian Wernick ; Phillip Nahirniak ; Stanislaw P. Affiliations 1 St. Lukes University Health Network. Continuing Education Activity Wounds of all shapes and sizes have plagued patients and created a significant burden on their caretakers. Introduction In a way, history of wound care is the history of humankind. Function Normal Wound Healing At times difficult to appreciate, the wound healing process WHP is a highly structured and well-organized biological process [6] [7] [6]. Wound healing can be divided into 4 phases [8] : Hemostasis. Issues of Concern Factors Affecting Wound Healing The WHP is very complex and involves high levels of coordination between multiple tissues and cell types [6]. Diabetes There is no doubt that diabetes plays a detrimental role in wound healing. Tobacco Abuse Cigarette smoking leads to numerous adverse health consequences, including various types of cancer, primary lung disease, and cardiovascular disease, among others [12] [13]. Malnutrition The nutritional needs of the healing wound are very complex. Obesity Obesity is a significant factor in surgical wound healing. Stress Stress has been demonstrated to be a major contributor to a broad range of health conditions and illnesses, including cardiovascular disease, cancer, and obesity. Clinical Significance Wound healing is a vast topic area, with many aspects remaining poorly understood despite the tremendous amount of progress over the past few decades. Other Issues Methods and Techniques Known to Improve Wound Healing Negative Pressure Therapy Numerous wound management devices have been introduced over the years to improve wound healing. Maggot Debridement While considered by many as archaic, maggot debridement therapy MDT has been shown unequivocally to be of benefit in wound healing [46] [47]. Hyperbaric Oxygen Hyperbaric oxygen therapy HBOT is another treatment modality that has been around for quite some time, but only recently saw a resurgence in interest due to promising effects on the WHP, especially in the setting of chronic and complicated wounds [54] [55]. Enhancing Healthcare Team Outcomes The best management of wounds is taken care of by an interprofessional team of a nurse specializing in wound care and a clinician with significant wound experience. Review Questions Access free multiple choice questions on this topic. Comment on this article. References 1. Lumbers M. Challenges in wound care for community nurses: a case review. Br J Community Nurs. Everett E, Mathioudakis N. Update on management of diabetic foot ulcers. Ann N Y Acad Sci. Sen CK. Human Wounds and Its Burden: An Updated Compendium of Estimates. Adv Wound Care New Rochelle. Boyko TV, Longaker MT, Yang GP. Laboratory Models for the Study of Normal and Pathologic Wound Healing. Plast Reconstr Surg. Nuutila K, Katayama S, Vuola J, Kankuri E. Human Wound-Healing Research: Issues and Perspectives for Studies Using Wide-Scale Analytic Platforms. Heughan C, Hunt TK. Some aspects of wound healing research: a review. Can J Surg. Hunt TK. Recent advances in wound healing. Surg Annu. Rodrigues M, Kosaric N, Bonham CA, Gurtner GC. Wound Healing: A Cellular Perspective. Physiol Rev. Avishai E, Yeghiazaryan K, Golubnitschaja O. Impaired wound healing: facts and hypotheses for multi-professional considerations in predictive, preventive and personalised medicine. EPMA J. Davis FM, Kimball A, Boniakowski A, Gallagher K. Dysfunctional Wound Healing in Diabetic Foot Ulcers: New Crossroads. Curr Diab Rep. Lim HS, Lip GY, Blann AD. Goniewicz ML, Smith DM, Edwards KC, Blount BC, Caldwell KL, Feng J, Wang L, Christensen C, Ambrose B, Borek N, van Bemmel D, Konkel K, Erives G, Stanton CA, Lambert E, Kimmel HL, Hatsukami D, Hecht SS, Niaura RS, Travers M, Lawrence C, Hyland AJ. Comparison of Nicotine and Toxicant Exposure in Users of Electronic Cigarettes and Combustible Cigarettes. JAMA Netw Open. McDaniel JC, Browning KK. Smoking, chronic wound healing, and implications for evidence-based practice. J Wound Ostomy Continence Nurs. Garg A. Pathophysiology of tobacco use and wound healing. Dent Implantol Update. Balaji SM. Tobacco smoking and surgical healing of oral tissues: a review. Indian J Dent Res. Lassig AAD, Bechtold JE, Lindgren BR, Pisansky A, Itabiyi A, Yueh B, Joseph AM. Tobacco exposure and wound healing in head and neck surgical wounds. Whiteford L. Nicotine, CO and HCN: the detrimental effects of smoking on wound healing. Campos AC, Groth AK, Branco AB. Assessment and nutritional aspects of wound healing. Curr Opin Clin Nutr Metab Care. Saghaleini SH, Dehghan K, Shadvar K, Sanaie S, Mahmoodpoor A, Ostadi Z. Pressure Ulcer and Nutrition. Indian J Crit Care Med. Barchitta M, Maugeri A, Favara G, Magnano San Lio R, Evola G, Agodi A, Basile G. Nutrition and Wound Healing: An Overview Focusing on the Beneficial Effects of Curcumin. Int J Mol Sci. Chen LR, Yang BS, Chang CN, Yu CM, Chen KH. Additional Vitamin and Mineral Support for Patients with Severe Burns: A Nationwide Experience from a Catastrophic Color-Dust Explosion Event in Taiwan. Molnar JA, Vlad LG, Gumus T. Nutrition and Chronic Wounds: Improving Clinical Outcomes. Houdek MT, Griffin AM, Ferguson PC, Wunder JS. Morbid Obesity Increases the Risk of Postoperative Wound Complications, Infection, and Repeat Surgical Procedures Following Upper Extremity Limb Salvage Surgery for Soft Tissue Sarcoma. Hand N Y. Pierpont YN, Dinh TP, Salas RE, Johnson EL, Wright TG, Robson MC, Payne WG. Obesity and surgical wound healing: a current review. ISRN Obes. Broadbent E, Kahokehr A, Booth RJ, Thomas J, Windsor JA, Buchanan CM, Wheeler BR, Sammour T, Hill AG. A brief relaxation intervention reduces stress and improves surgical wound healing response: a randomised trial. Brain Behav Immun. Broadbent E, Petrie KJ, Alley PG, Booth RJ. Psychological stress impairs early wound repair following surgery. Psychosom Med. Kantak NA, Mistry R, Varon DE, Halvorson EG. Negative Pressure Wound Therapy for Burns. Clin Plast Surg. de Jesus LE, Martins AB, Oliveira PB, Gomes F, Leve T, Dekermacher S. Negative pressure wound therapy in pediatric surgery: How and when to use. J Pediatr Surg. Garcia-Ruano A, Deleyto E, Garcia-Fernandez S. VAC-instillation therapy in abdominal mesh exposure: a novel indication. J Surg Res. Barbera F, Lorenzetti F, Marsili R, Lisa A, Guido G, Pantaloni M. The Impact of Preoperative Negative-Pressure Wound Therapy on Pectoralis Major Muscle Flap Reconstruction for Deep Sternal Wound Infections. Ann Plast Surg. Apelqvist J, Willy C, Fagerdahl AM, Fraccalvieri M, Malmsjö M, Piaggesi A, Probst A, Vowden P. EWMA Document: Negative Pressure Wound Therapy. J Wound Care. Stawicki SP, Grossman M. Ostomy Wound Manage. El-Sabbagh AH. Font Size Small Normal Large. Risk factors for impaired wound healing and wound complications. Formulary drug information for this topic. No drug references linked in this topic. Find in topic Formulary Print Share. View in. Language Chinese English. Authors: David G Armstrong, DPM, MD, PhD Andrew J Meyr, DPM Section Editors: Russell S Berman, MD John F Eidt, MD Joseph L Mills, Sr, MD Amalia Cochran, MD, FACS, FCCM Deputy Editor: Kathryn A Collins, MD, PhD, FACS Literature review current through: Jan This topic last updated: Jun 20, Some individuals have one or more factors that contribute to impaired wound healing, which can lead to chronic ulcerations or nonhealing wounds, or can complicate the surgical course. To continue reading this article, you must sign in with your personal, hospital, or group practice subscription. Subscribe Sign in. It does NOT include all information about conditions, treatments, medications, side effects, or risks that may apply to a specific patient. |
| Table of Contents | Reduced neutrophil chemotaxis and infiltration contributes to delayed resolution of cutaneous wound infection with advanced age. Perform hand hygiene prior to arranging the supplies at the bedside and after wound care. Research focused on thoroughly understanding these mechanisms would allow for specifically targeted treatment of diabetic foot ulcers. Article PubMed PubMed Central CAS Google Scholar Szkudelski, T. Note the unhealthy appearance of dark red granulation tissue, white or yellow slough, or brown or black necrotic tissues. |
| Risk factors for impaired wound healing and wound complications | Mice wounds were photographed under isoflurane anesthesia on alternative days until the 20 th day after induction. The graphs present the mean according to all analyzed animals per group. The labeled cells were analyzed using flow cytometry on a FACS Canto BD Bioscience. Autofluorescence was determined using unlabeled cells from skin, and compensation was performed using cells from skin individually marked with the antibodies BD Bioscience. About 10, events were analyzed Mean fluorescence intensity MFI was also observed in the final gates Supplementary Table 1. All antibodies used in this study were monoclonal. This dismisses isotype controls. All analysis considered automatic compensation using beads BD Biosciences in the cytometer before sample acquisition. Complementary DNA cDNA was synthesized using a reverse transcription system RevertAid First Strand cDNA Synthesis Kit, Thermo Scientific and qPCR was performed with Fast SYBR® Green Master Mix Applied Biosystems containing primers for Ym1 , Arg1 , Nos2 , Stat1 , Stat6 , Il10 , Il12 , Hprt all from Integrated DNA Technologies Table 1 on the Step One Plus Real-Time PCR Detection System Applied Biosystems. Relative expression was calculated using the comparative threshold cycle Ct and calculated relative healthy WT ΔΔCt method. The sequences of the primers are listed in Table 1. Protein samples derived from macrophages stimulated with IL-4 in vitro or in vivo were obtained with RIPA buffer. The samples were submitted for electrophoresis in SDS-PAGE, and were transferred to the nitrocellulose membrane. After transfer, the membranes were incubated with primary antibodies anti-STAT6, -pSTAT6 Abcam , and -β-actin Cell Signaling. The membranes were then incubated with proper secondary antibody HRP-conjugated. by analysis of variance ANOVA followed by a Bonferroni analysis. All data generated or analysed during this study are included in this published article and its Supplementary Information files. All data are available from the corresponding author on reasonable request. Paschou, S. Type 1 diabetes as an autoimmune disease: the evidence. Article PubMed Google Scholar. Tuomilehto, J. The emerging global epidemic of type 1 diabetes. Article PubMed CAS Google Scholar. Ogurtsova, K. et al. IDF Diabetes Atlas: Global estimates for the prevalence of diabetes for and Hink, U. Mechanisms underlying endothelial dysfunction in diabetes mellitus: therapeutic implications. Treat Endocrinol 2 , — Article CAS Google Scholar. Kono, H. Molecular determinants of sterile inflammation. Chen, G. Sterile inflammation: sensing and reacting to damage. Article PubMed PubMed Central CAS Google Scholar. Talahalli, R. Increased synthesis of leukotrienes in the mouse model of diabetic retinopathy. Article PubMed PubMed Central Google Scholar. Filgueiras, L. Leukotriene B4-mediated sterile inflammation promotes susceptibility to sepsis in a mouse model of type 1 diabetes. Peters-Golden, M. Serezani, C. Leukotriene B4 amplifies NF-κB activation in mouse macrophages by reducing SOCS1 inhibition of MyD88 expression. Leibovich, S. The role of the macrophage in wound repair. A study with hydrocortisone and antimacrophage serum. Am J Pathol 78 , 71— PubMed PubMed Central CAS Google Scholar. Lucas, T. Differential roles of macrophages in diverse phases of skin repair. Gordon, S. Monocyte and macrophage heterogeneity. Castoldi, A. The Macrophage Switch in Obesity Development. Fleming, B. Regulatory macrophages: setting the threshold for therapy. Chang, N. A macrophage protein, Ym1, transiently expressed during inflammation is a novel mammalian lectin. M Campbell, L. Local arginase 1 activity is required for cutaneous wound healing. Kämpfer, H. Expression and activity of arginase isoenzymes during normal and diabetes-impaired skin repair. x Wetzler, C. Large and sustained induction of chemokines during impaired wound healing in the genetically diabetic mouse: prolonged persistence of neutrophils and macrophages during the late phase of repair. Goren, I. Diabetes 52 , — Dhall, S. Arachidonic acid-derived signaling lipids and functions in impaired healing. Ghanim, H. Circulating mononuclear cells in the obese are in a proinflammatory state. FA Martin, P. Inflammatory cells during wound repair: the good, the bad and the ugly. Falanga, V. Wound healing and its impairment in the diabetic foot. Mechanisms underlying endothelial dysfunction in diabetes mellitus. Circ Res 88 , E14—22 Spite, M. Deficiency of the leukotriene B4 receptor, BLT-1, protects against systemic insulin resistance in diet-induced obesity. Yang, J. Monocyte and macrophage differentiation: circulation inflammatory monocyte as biomarker for inflammatory diseases. Rivollier, A. Inflammation switches the differentiation program of Ly6Chi monocytes from antiinflammatory macrophages to inflammatory dendritic cells in the colon. Szkudelski, T. The mechanism of alloxan and streptozotocin action in B cells of the rat pancreas. Physiol Res 50 , — PubMed CAS Google Scholar. Souza, D. The required role of endogenously produced lipoxin A4 and annexin-1 for the production of IL and inflammatory hyporesponsiveness in mice. J Immunol , — Mosser, D. Activation of murine macrophages. Curr Protoc Immunol Chapter 14, Unit ims83 Novak, M. Phenotypic transitions of macrophages orchestrate tissue repair. Otranto, M. Insulin resistance impairs cutaneous wound healing in mice. Brogliato, A. Critical role of 5-lipoxygenase and heme oxygenase-1 in wound healing. Mirza, R. Blocking interleukin-1β induces a healing-associated wound macrophage phenotype and improves healing in type 2 diabetes. Daley, J. The phenotype of murine wound macrophages. J Leukoc Biol 87 , 59—67 Rőszer, T. Understanding the Mysterious M2 Macrophage through Activation Markers and Effector Mechanisms. Guo, Y. AGEs Induced Autophagy Impairs Cutaneous Wound Healing via Stimulating Macrophage Polarization to M1 in Diabetes. Article ADS PubMed PubMed Central CAS Google Scholar. Palva, O. Determination of Arginase in Serum. Scandinavian Journal of Clinics and Laboratory Investigation 13 , 3 Google Scholar. Griess, P. Bemerkungen zu der Abhandlung der HH. Chemische Berichte 12 , 3 Pessoa, A. Oral administration of antioxidants improves skin wound healing in diabetic mice. Download references. This work was supported by the Sao Paulo Research Foundation FAPESP and the National Council for Scientific and Technological Development. Department of Immunology, Institute of Biomedical Sciences, University of São Paulo, São Paulo, Brazil. Department of Cell and Developmental Biology, Institute of Biomedical Sciences, University of São Paulo, Sao Paulo, Brazil. You can also search for this author in PubMed Google Scholar. Ramalho T. and Filgueiras L. performed the experiments and wrote the manuscript; Pessoa A. performed the experiment of cell isolation from the wound; Jancar S. discussed the results and revised the manuscript; Silva-Jr I. performed flow cytometry assays. All the authors revised the manuscript before submission. Correspondence to Sonia Jancar. Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. Open Access This article is licensed under a Creative Commons Attribution 4. Reprints and permissions. Ramalho, T. Impaired wound healing in type 1 diabetes is dependent on 5-lipoxygenase products. Sci Rep 8 , Download citation. Received : 29 May Accepted : 11 September Published : 21 September Anyone you share the following link with will be able to read this content:. Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative. By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate. Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily. Skip to main content Thank you for visiting nature. nature scientific reports articles article. Download PDF. Subjects Chronic inflammation Mechanisms of disease Type 1 diabetes. Abstract Type 1 diabetes is associated with systemic low grade inflammation LGI. Introduction Type 1 diabetes T1D is a metabolic disorder characterized by chronic hyperglycemia and alterations in carbohydrate, lipid and protein metabolism. Figure 1. Full size image. Figure 2. Figure 3. Figure 4. Figure 5. Figure 6. Figure 7. Figure 8. Discussion Diabetes is a metabolic disorder characterized by chronic LGI. Peritoneal macrophages profile Peritoneal exudates cells were obtained by lavage of the peritoneal cavity with cold PBS. Nitrite and arginine measurements Macrophages were isolated by adherence for arginase activity measurements. Analysis of macrophages stimulated with IL-4 An assay of dose versus response was performed in vivo in resident peritoneal macrophages from healthy WT mice. Table 1 Sequence of primers. Full size table. Additional factors involved in this complex process include blunting of the immune and inflammatory responses. Interestingly, these ill-effects of obesity are largely reversible through weight loss [24]. Stress has been demonstrated to be a major contributor to a broad range of health conditions and illnesses, including cardiovascular disease, cancer, and obesity. Stress states lead to upregulation of stress hormones via the hypothalamic-pituitary axis and the release of adrenocortical hormones. Resultant changes include elevated levels of cortisol, glucocorticoids, and catecholamines. Cortisol works to blunt the immune response by blocking the production of important cytokines such as IL-1beta, IL-6, and TNF-alpha. The impairment of immune response ultimately leads to deficient wound healing [25] [26]. Wound healing is a vast topic area, with many aspects remaining poorly understood despite the tremendous amount of progress over the past few decades. Various co-morbid conditions e. More recently, a better understanding of the role micronutrients play in wound healing, along with the introduction of novel wound care therapeutics e. Numerous wound management devices have been introduced over the years to improve wound healing. However, none have been as influential and successful as negative pressure wound therapy NPWT therapy. NPWT involves the application of subatmospheric pressure on wound via a sponge-based system with an airtight seal directly over the wound, connected under sealed conditions to a suction device. Benefits of NPWT are realized via several different mechanisms. First, the subatmospheric pressure applied to the wound helps to remove wound exudate and other materials that are known to impair the WHP. Secondly, the presence of subatmospheric pressure promotes angiogenesis and tissue perfusion by increasing cellular proliferation and migration into the wound. The suction also assists in bringing wound edges together. When combined, all of the above elements and mechanisms work synergistically to help speed up wound healing. NPWT devices can be used on a wide variety of wounds, such as pressure ulcers, large abdominal wounds, traumatic wounds, as well as complex, difficult-to-cover tissue defects following debridement operations e. Of note, NPWT is contraindicated in certain situations, such as wound surfaces involving malignancy, untreated osteomyelitis, non-enteric and unexplored fistulae, and necrotic tissue with eschar e. It has long been known that Vitamin A may have beneficial effects on wound healing in the setting of previous systemic exposure to corticosteroids. More specifically, Vitamin A has been shown to overcome the inhibitory effects of cortisone and related corticosteroids on the rate of gain in tensile strength of the wound [34] [35] [34]. This may be especially pronounced in early stages of the WHP. At the same time, Vitamin A by itself does not seem to be a significant modulator of the WHP, suggesting that its beneficial action in the setting of prior corticosteroid use is related to the interaction s specific to corticosteroid-specific pathway s [36] [37] [36]. Vitamin C and zinc have both been found to improve wound healing characteristics, although clinical adoption and implementation of this therapeutic combination is less than universal. Mechanistically, vitamin C has several favorable effects on the WHP. First, it is a powerful antioxidant and free radical scavenger. Second, it is important to systemic immunity, and along with Zinc helps boost the immune system when taken in the postoperative period. Together with Arginine and Zinc, Vitamin C is important for collagen synthesis. The evidence is strongest for supplementing vitamin C and zinc during the immediate postoperative period [38] [39] [40] [38]. Among other interesting and important developments in wound care, there is evidence that vitamin-D supplementation may help positively modulate impaired wound healing, although further research toward mechanistic understanding is required in this area. More specifically, the role of vitamin D in the WHP may be indirect, through beneficial effects on closely related physiological processes, such as glucose homeostasis [41] [42]. Finally, another vast topic area that is worth mentioning but too extensive to fully discuss in this review is the use of growth factors in the modulation of the WHP. It has been demonstrated that delivery of various specific growth factors e. Further research is required to better define mechanisms of action, potential side effects, and the overall risk-benefit of human application of such therapies. While considered by many as archaic, maggot debridement therapy MDT has been shown unequivocally to be of benefit in wound healing [46] [47]. MDT is based on the observation that fly larvae only debride dead, devitalized, and necrotic tissue. Healthy, viable tissue is not threatened during the MDT, making this therapy uniquely suited for debridement of devitalized tissues with truly surgical precision [48]. In fact, MDT is considered a form of "biosurgery. This liquefied material is then ingested, resulting in effective debridement of the tissue of interest. It has been shown that MDT can help debride large wounds in as little as 72 hours, resulting in a viable granulation bed that is suitable for conventional wound management. In addition to chemical debridement, larval secretions are also characterized by significant antimicrobial activity, active against a wide range of pathogenic and often antibiotic-resistant bacteria, mostly gram-positive species. Maggots work best on moist environments with sufficient oxygen supply [49]. They are approved for use in non-healing necrotic skin and soft tissue wounds, pressure and venous stasis ulcers, neuropathic foot ulcers, and non-healing traumatic or surgical wounds [50]. Most recent developments in this area include the introduction of transgenic maggots that secrete human growth factors in their saliva [51]. Clinical applications of this therapy are continually expanding. Of interest, application of MDT can be accomplished through direct exposure of the maggots to the wound bed using a specialized "housing" or through indirect exposure using larvae contained within a sealed, semi-permeable bag [52] [53]. Hyperbaric oxygen therapy HBOT is another treatment modality that has been around for quite some time, but only recently saw a resurgence in interest due to promising effects on the WHP, especially in the setting of chronic and complicated wounds [54] [55]. Chronic wounds, often seen as a consequence of diabetes, arterial or venous disease, are increasingly common and result in significant impact on the affected patients, their caretakers, and the healthcare system in general. The beneficial action of HBOT on wound healing is predicated on the increased supply of oxygen to wounds that are refractory to other, more conventional treatment approaches [56]. In practice, HBOT involves the patient being temporarily enclosed in a special chamber that in many ways approximates conditions used for deep sea divers and involves gradual "dive" followed by a pre-defined time interval at a certain "oxygen pressure level," and subsequent gradual "resurfacing" process. While in the chamber, the patient is exposed to markedly elevated concentrations of pure oxygen, leading to elevation of systemic and tissue oxygen levels. It has been demonstrated that HBOT is effective in improving the course of chronic diabetes-related extremity wounds, potentially reducing the need for major but not necessarily minor amputations. Available evidence suggests beneficial effects of HBOT on wounds are usually apparent within approximately 6 weeks of therapy, but long-term beneficial effects continue to be questionable. Another area where HBOT can be beneficial is the management of necrotizing soft tissue infections e. Additional difficult-to-treat types of wounds that have been speculated to benefit from HBOT are the chronic pressure ulcers due to its inherently "ischemic" nature and venous ulcers; however, there is no solid evidence to support HBOT for either of these indications at this time [57] [60]. The best management of wounds is taken care of by an interprofessional team of a nurse specializing in wound care and a clinician with significant wound experience. Caring for wounds not only involves regular follow-ups but patient education. A coordinated team approach has been shown to be most effective in wound management. Disclosure: Brian Wernick declares no relevant financial relationships with ineligible companies. Disclosure: Phillip Nahirniak declares no relevant financial relationships with ineligible companies. Disclosure: Stanislaw Stawicki declares no relevant financial relationships with ineligible companies. This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4. You are not required to obtain permission to distribute this article, provided that you credit the author and journal. Turn recording back on. National Library of Medicine Rockville Pike Bethesda, MD Web Policies FOIA HHS Vulnerability Disclosure. Help Accessibility Careers. Access keys NCBI Homepage MyNCBI Homepage Main Content Main Navigation. Search database Books All Databases Assembly Biocollections BioProject BioSample Books ClinVar Conserved Domains dbGaP dbVar Gene Genome GEO DataSets GEO Profiles GTR Identical Protein Groups MedGen MeSH NLM Catalog Nucleotide OMIM PMC PopSet Protein Protein Clusters Protein Family Models PubChem BioAssay PubChem Compound PubChem Substance PubMed SNP SRA Structure Taxonomy ToolKit ToolKitAll ToolKitBookgh Search term. StatPearls [Internet]. Treasure Island FL : StatPearls Publishing; Jan-. Show details Treasure Island FL : StatPearls Publishing ; Jan-. Search term. Impaired Wound Healing Brian Wernick ; Phillip Nahirniak ; Stanislaw P. Author Information and Affiliations Authors Brian Wernick ; Phillip Nahirniak ; Stanislaw P. Affiliations 1 St. Lukes University Health Network. Continuing Education Activity Wounds of all shapes and sizes have plagued patients and created a significant burden on their caretakers. Introduction In a way, history of wound care is the history of humankind. Function Normal Wound Healing At times difficult to appreciate, the wound healing process WHP is a highly structured and well-organized biological process [6] [7] [6]. Wound healing can be divided into 4 phases [8] : Hemostasis. Issues of Concern Factors Affecting Wound Healing The WHP is very complex and involves high levels of coordination between multiple tissues and cell types [6]. Diabetes There is no doubt that diabetes plays a detrimental role in wound healing. Tobacco Abuse Cigarette smoking leads to numerous adverse health consequences, including various types of cancer, primary lung disease, and cardiovascular disease, among others [12] [13]. Malnutrition The nutritional needs of the healing wound are very complex. Obesity Obesity is a significant factor in surgical wound healing. Stress Stress has been demonstrated to be a major contributor to a broad range of health conditions and illnesses, including cardiovascular disease, cancer, and obesity. Clinical Significance Wound healing is a vast topic area, with many aspects remaining poorly understood despite the tremendous amount of progress over the past few decades. Other Issues Methods and Techniques Known to Improve Wound Healing Negative Pressure Therapy Numerous wound management devices have been introduced over the years to improve wound healing. Maggot Debridement While considered by many as archaic, maggot debridement therapy MDT has been shown unequivocally to be of benefit in wound healing [46] [47]. Hyperbaric Oxygen Hyperbaric oxygen therapy HBOT is another treatment modality that has been around for quite some time, but only recently saw a resurgence in interest due to promising effects on the WHP, especially in the setting of chronic and complicated wounds [54] [55]. Enhancing Healthcare Team Outcomes The best management of wounds is taken care of by an interprofessional team of a nurse specializing in wound care and a clinician with significant wound experience. Review Questions Access free multiple choice questions on this topic. Comment on this article. References 1. Lumbers M. Challenges in wound care for community nurses: a case review. Br J Community Nurs. Everett E, Mathioudakis N. Update on management of diabetic foot ulcers. Ann N Y Acad Sci. Sen CK. Human Wounds and Its Burden: An Updated Compendium of Estimates. Adv Wound Care New Rochelle. Boyko TV, Longaker MT, Yang GP. Laboratory Models for the Study of Normal and Pathologic Wound Healing. Plast Reconstr Surg. Nuutila K, Katayama S, Vuola J, Kankuri E. Human Wound-Healing Research: Issues and Perspectives for Studies Using Wide-Scale Analytic Platforms. Heughan C, Hunt TK. Some aspects of wound healing research: a review. Can J Surg. Hunt TK. Recent advances in wound healing. Surg Annu. Rodrigues M, Kosaric N, Bonham CA, Gurtner GC. Wound Healing: A Cellular Perspective. Physiol Rev. Avishai E, Yeghiazaryan K, Golubnitschaja O. Impaired wound healing: facts and hypotheses for multi-professional considerations in predictive, preventive and personalised medicine. EPMA J. Davis FM, Kimball A, Boniakowski A, Gallagher K. Dysfunctional Wound Healing in Diabetic Foot Ulcers: New Crossroads. Curr Diab Rep. Lim HS, Lip GY, Blann AD. Goniewicz ML, Smith DM, Edwards KC, Blount BC, Caldwell KL, Feng J, Wang L, Christensen C, Ambrose B, Borek N, van Bemmel D, Konkel K, Erives G, Stanton CA, Lambert E, Kimmel HL, Hatsukami D, Hecht SS, Niaura RS, Travers M, Lawrence C, Hyland AJ. Comparison of Nicotine and Toxicant Exposure in Users of Electronic Cigarettes and Combustible Cigarettes. JAMA Netw Open. McDaniel JC, Browning KK. Smoking, chronic wound healing, and implications for evidence-based practice. J Wound Ostomy Continence Nurs. Garg A. Pathophysiology of tobacco use and wound healing. Dent Implantol Update. Balaji SM. Tobacco smoking and surgical healing of oral tissues: a review. Indian J Dent Res. Lassig AAD, Bechtold JE, Lindgren BR, Pisansky A, Itabiyi A, Yueh B, Joseph AM. Tobacco exposure and wound healing in head and neck surgical wounds. Whiteford L. Nicotine, CO and HCN: the detrimental effects of smoking on wound healing. Campos AC, Groth AK, Branco AB. Assessment and nutritional aspects of wound healing. Curr Opin Clin Nutr Metab Care. Saghaleini SH, Dehghan K, Shadvar K, Sanaie S, Mahmoodpoor A, Ostadi Z. Pressure Ulcer and Nutrition. Indian J Crit Care Med. Barchitta M, Maugeri A, Favara G, Magnano San Lio R, Evola G, Agodi A, Basile G. Nutrition and Wound Healing: An Overview Focusing on the Beneficial Effects of Curcumin. Int J Mol Sci. Chen LR, Yang BS, Chang CN, Yu CM, Chen KH. Additional Vitamin and Mineral Support for Patients with Severe Burns: A Nationwide Experience from a Catastrophic Color-Dust Explosion Event in Taiwan. Molnar JA, Vlad LG, Gumus T. Nutrition and Chronic Wounds: Improving Clinical Outcomes. Houdek MT, Griffin AM, Ferguson PC, Wunder JS. Morbid Obesity Increases the Risk of Postoperative Wound Complications, Infection, and Repeat Surgical Procedures Following Upper Extremity Limb Salvage Surgery for Soft Tissue Sarcoma. Hand N Y. Pierpont YN, Dinh TP, Salas RE, Johnson EL, Wright TG, Robson MC, Payne WG. Obesity and surgical wound healing: a current review. ISRN Obes. Broadbent E, Kahokehr A, Booth RJ, Thomas J, Windsor JA, Buchanan CM, Wheeler BR, Sammour T, Hill AG. A brief relaxation intervention reduces stress and improves surgical wound healing response: a randomised trial. Brain Behav Immun. Broadbent E, Petrie KJ, Alley PG, Booth RJ. Psychological stress impairs early wound repair following surgery. Psychosom Med. Kantak NA, Mistry R, Varon DE, Halvorson EG. Negative Pressure Wound Therapy for Burns. Clin Plast Surg. de Jesus LE, Martins AB, Oliveira PB, Gomes F, Leve T, Dekermacher S. Negative pressure wound therapy in pediatric surgery: How and when to use. J Pediatr Surg. Garcia-Ruano A, Deleyto E, Garcia-Fernandez S. VAC-instillation therapy in abdominal mesh exposure: a novel indication. J Surg Res. Barbera F, Lorenzetti F, Marsili R, Lisa A, Guido G, Pantaloni M. The Impact of Preoperative Negative-Pressure Wound Therapy on Pectoralis Major Muscle Flap Reconstruction for Deep Sternal Wound Infections. Ann Plast Surg. Apelqvist J, Willy C, Fagerdahl AM, Fraccalvieri M, Malmsjö M, Piaggesi A, Probst A, Vowden P. EWMA Document: Negative Pressure Wound Therapy. J Wound Care. Stawicki SP, Grossman M. Ostomy Wound Manage. El-Sabbagh AH. Negative pressure wound therapy: An update. Chin J Traumatol. Ehrlich HP, Hunt TK. The effects of cortisone and anabolic steroids on the tensile strength of healing wounds. Ann Surg. Stephens FO, Hunt TK, Jawetz E, Sonne M, Dunphy JE. Effect of cortisone and vitamin A on wound infection. Am J Surg. Trevisani MF, Ricci MA, Tolland JT, Beck WC. Effect of vitamin A and zinc on wound healing in steroid-treated mice. |
| StatPearls [Internet]. | Ahn C, Mulligan P, Salcido RS. Smoking-the bane of wound healing: biomedical interventions and social influences. Adv Skin Wound Care. quiz Sørensen LT, Jørgensen S, Petersen LJ, Hemmingsen U, Bülow J, Loft S, et al. Acute effects of nicotine and smoking on blood flow, tissue oxygen, and aerobe metabolism of the skin and subcutis. J Surg Res. Article PubMed CAS Google Scholar. Sørensen LT, Toft B, Rygaard J, Ladelund S, Teisner B, Gottrup F. Smoking attenuates wound inflammation and proliferation while smoking cessation restores inflammation but not proliferation. Chan LKW, Withey S, Butler PE. Smoking and wound healing problems in reduction mammaplasty: is the introduction of urine nicotine testing justified? Ann Plast Surg. Manassa EH, Hertl CH, Olbrisch RR. Wound healing problems in smokers and nonsmokers after abdominoplasties. Plast Reconstr Surg. Alcohol and cardiovascular health. the razor-sharp double-edged sword. J Am Coll Cardiol. Jackson R, Scragg R, Beaglehole R. Alcohol consumption and risk of coronary heart disease. Stampfer MJ, Colditz GA, Willett WC, Speizer FE, Hennekens CH. A prospective study of moderate alcohol consumption and the risk of coronary disease and stroke in women. N Engl J Med. Szabo G, Mandrekar P. A recent perspective on alcohol, immunity, and host defense. Alcohol Clin Exp Res. Greiffenstein P, Mathis KW, Stouwe CV, Molina PE. Sander M, von Heymann C, Neumann T, Braun JP, Kastrup M, Beholz S, et al. Increased interleukin and cortisol in long-term alcoholics after cardiopulmonary bypass: a hint to the increased postoperative infection rate? Heinz R, Waltenbaugh C. Ethanol consumption modifies dendritic cell antigen presentation in mice. Mandrekar P, Catalano D, Dolganiuc A, Kodys K, Szabo G. Inhibition of myeloid dendritic cell accessory cell function and induction of T cell anergy by alcohol correlates with decreased IL production. Radek KA, Matthies AM, Burns AL, Heinrich SA, Kovacs EJ, Dipietro LA. Acute ethanol exposure impairs angiogenesis and the proliferative phase of wound healing. Am J Physiol Heart Circ Physiol. Radek KA, Kovacs EJ, Gallo RL, DiPietro L. Acute ethanol exposure disrupts VEGF receptor cell signaling in endothelial cells. Radek KA, Kovacs EJ, DiPietro LA. Matrix proteolytic activity during wound healing: Modulation by acute ethanol exposure. Fitzgerald DJ, Radek KA, Chaar M, Faunce DE, DiPietro LA, Kovacs EJ. Effects of acute ethanol exposure on the early inflammatory response after excisional injury. Mora S, Pessin JE. An adipocentric view of signaling and intracellular trafficking. Diabetes Metab Res Rev. Zhang XJ, Chinkes DL, Doyle D, Wolfe RR. Metabolism of skin and muscle protein is regulated differently in response to nutrition. Am J Physiol Endocrinol Metab. CAS Google Scholar. Guo S, Dipietro LA. Factors affecting wound healing. J Dent Res. Wilson JA, Clark JJ. Obesity: impediment to postsurgical wound healing. Patel GK. The role of nutrition in the management of lower extremity wounds. Ireton-Jones C, Liepa GU. Carbohydrates and wound healing. In: Molnar J, editor. Nutrition and wound healing. CRC Press; De Feo M, Gregorio R, Renzulli A, Ismeno G, Romano GP, Cotrufo M. Treatment of recurrent postoperative mediastinitis with granulated sugar. J Cardiovasc Surg Torino. Google Scholar. Demling RH. Nutrition, anabolism, and the wound healing process: an overview. PubMed PubMed Central Google Scholar. Gogia PP. Physiology of wound healing. In: Gogia PP, editor. Clinical wound management. Thorofare: Slack Inc. World Health Organization. Global Report on Diabetes. Geneva: WHO; Accessed 18 Jan Goldman RJ. Hyperbaric oxygen therapy for wound healing and limb salvage: a systematic review. Shipman AR, Millington GWM. Obesity and the skin. Kranke P, Bennett MH, Martyn-St James M, Schnabel A, Debus SE. Hyperbaric oxygen therapy for chronic wounds. Cochrane Database Syst Rev. Anaya DA, Dellinger EP. The obese surgical patient: a susceptible host for infection. Surg Infect Larchmt. Greco JA, Castaldo ET, Nanney LB, Wendel JJ, Summitt JB, Kelly KJ. The effect of weight loss surgery and body mass index on wound complications after abdominal contouring operations. Alba-Loureiro TC, Hirabara SM, Mendonça JR, Curi R, Pithon-Curi TC. Diabetes causes marked changes in function and metabolism of rat neutrophils. J Endocrinol. Mastej K, Adamiec R. Neutrophil surface expression of CD11b and CD62L in diabetic microangiopathy. Acta Diabetol. Marhoffer W, Stein M, Schleinkofer L, Federlin K. Evidence of ex vivo and in vitro impaired neutrophil oxidative burst and phagocytic capacity in type 1 diabetes mellitus. Diabetes Res Clin Pract. Rosner K, Ross C, Karlsmark T, Petersen AA, Gottrup F, Vejlsgaard GL. Immunohistochemical characterization of the cutaneous cellular infiltrate in different areas of chronic leg ulcers. Moore K, Ruge F, Hadring KG. T lymphocytes and the lack of activated macrophages in wound margin biopsies from chronic leg ulcers. Zykova SN, Jenssen TG, Berdal M, Olsen R, Myklebust R, Seljelid R. Bagdade JD, Root RK, Bulger RJ. Impaired leukocyte function in patients with poorly controlled diabetes. Loot MA, Kenter SB, Au FL, van Galen WJ, Middelkoop E, Bos JD, et al. Fibroblasts derived from chronic diabetic ulcers differ in their response to stimulation with EGF, IGF-I, bFGF and PDGF-AB compared to controls. Eur J Cell Biol. Werner S, Breeden M, Hübner G, Greenhalgh DG, Longaker MT. Induction of keratinocyte growth factor expression is reduced and delayed during wound healing in the genetically diabetic mouse. Werner S, Krieg T, Smola H. Keratinocyte-fibroblast interactions in wound healing. Adler AI, Boyko EJ, Ahroni JH, Stensel V, Forsberg RC, Smith DG. Risk factors for diabetic peripheral sensory neuropathy: results of the Seattle Prospective Diabetic Foot Study. Diabetes Care. Sheehan P, Jones P, Caselli A, Giurini JM, Veves A. Percent change in wound area of diabetic foot ulcers over a 4-week period is a robust predictor of complete healing in a week prospective trial. Illigens BM, Gibbons CH. A human model of small fiber neuropathy to study wound healing. PLoS One. Pradhan L, Nabzdyk C, Andersen ND, LoGerfo FW, Veves A. Inflammation and neuropeptides: the connection in diabetic wound healing. Expert Rev Mol Med. Signorelli SS, Malaponte G, Libra M, Di Pino L, Celotta G, Bevelacqua V, et al. Plasma levels and zymographic activities of matrix metalloproteinases 2 and 9 in type II diabetics with peripheral arterial disease. Vasc Med. Soneja A, Drews M, Malinski T. Role of nitric oxide, nitroxidative and oxidative stress in wound healing. Pharmacol Rep. Huijberts MS, Schaper NC, Schalkwijk CG. Advanced glycation end products and diabetic foot disease. Haines DD, Juhasz B, Tosaki A. Management of multicellular senescence and oxidative stress. J Cell Mol Med. Loots MA, Lamme EN, Zeegelaar J, Mekkes JR, Bos JD, Middelkoop E. Differences in cellular infiltrate and extracellular matrix of chronic diabetic and venous ulcers versus acute wounds. Tchaikovski V, Olieslagers S, Böhmer FD, Waltenberger J. Diabetes mellitus activates signal transduction pathways resulting in vascular endothelial growth factor resistance of human monocytes. Xu L, Qian H, Gu J, Shi J, Gu X, Tang Z. Heart failure in hospitalized patients with diabetic foot ulcers: clinical characteristics and their relationship with prognosis. J Diabetes. Rhou YJ, Henshaw FR, McGill MJ, Twigg SM. Congestive heart failure presence predicts delayed healing of foot ulcers in diabetes: an audit from a multidisciplinary high-risk foot clinic. J Diabetes Complic. Augey F, Pinet A, Renaudier P. Heart failure and stasis ulcer: a significant association prospective study of cases. Ann Dermatol Venereol. Brem H, Kirsner RS, Falanga V. Protocol for the successful treatment of venous ulcers. Am J Surg. Norgren L, Hiatt WR, Dormandy JA, Nehler MR, Harris KA, Fowkes FG. Inter-society consensus for the management of peripheral arterial disease TASC II. Bae JI, Won JH, Han SH, Lim SH, Hong YS, Kim JY, et al. Endovascular revascularization for patients with critical limb ischemia: impact on wound healing and long term clinical results in limbs. Korean J Radiol. Baldursson BT, Beitner H, Syrjänen S. Human papillomavirus in venous ulcers with and without squamous cell carcinoma. Arch Dermatol Res. Baldursson B, Sigurgeirsson B, Lindelof B. Venous leg ulcers and squamous cell carcinoma: a large-scale epidemiological study. Lehnert W, Kohl K, Riebe H, Jünger M, Ladwig A. The treatment of malignant tumors on venous leg ulcers. Case presentation and literature review. Rich JD, Shesol BF, Horne 3rd DW. Basal cell carcinoma arising in a smallpox vaccination site. J Clin Pathol. Zelickson A. Basal cell epithelioma at site and following smallpox vaccination: report of a case. Ozyazgan I, Kontacs O. Basal cell carcinoma arising from surgical scars: a case and review of the literature. Dermatol Surg. Jorquero E, Moreno JC, Díaz-Cano SJ, Rodríguez-Adrados F, Camacho F. Basal cell carcinoma arising in a surgical scar: reconstructive surgical treatment. J Dermatol Surg Oncol. Koga Y, Sawada Y. Basal cell carcinoma developing on a burn scar. Özyazgan İ, Kontaş O. Previous injuries or scars as risk factors for the development of basal cell carcinoma. Scand J Plast Reconstr Surg Hand Surg. Rustin MHA, Chambers TJ, Munro DD. Post-traumatic basal cell carcinomas. Clin Exp Dermatol. Perrone S, Lotti F, Geronzi U, Guidoni E, Longini M, Buonocore G. Oxidative stress in cancer-prone genetic diseases in pediatric age: the role of mitochondrial dysfunction. Oxid Med Cell Longev. Muramatsu H. Genetic predisposition to pediatric myeloid malignancies. Rinsho Ketsueki. Payne WG, Naidu DK, Wheeler CK, Barkoe D, Mentis M, Salas RE, et al. Wound healing in patients with cancer. Manna P, Jain SK. Obesity, oxidative stress, adipose tissue dysfunction, and the associated health risks: causes and therapeutic strategies. Metab Syndr Relat Disord. Arnold M, Pandeya N, Byrnes G, Renehan AG, Stevens GA, Ezzati M, et al. Global burden of cancer attributable to high body-mass index in a population-based study. Lancet Oncol. Finger EC, Giaccia AJ. Hypoxia, inflammation, and the tumor microenvironment in metastatic disease. Cancer Metastasis Rev. Arnold KM, Opdenaker LM, Flynn D, Sims-Mourtada J. Wound healing and cancer stem cells: inflammation as a driver of treatment resistance in breast cancer. Cancer Growth Metastasis. Rahat MA, Shakya J. Parallel aspects of the microenvironment in cancer and autoimmune disease. Mediat Inflamm. Lazaro JL, Izzo V, Meaume S, Davies AH, Lobmann R, Uccioli L. Elevated levels of matrix metalloproteinases and chronic wound healing: an updated review of clinical evidence. Kerkelä E, Saarialho-Kere U. Matrix metalloproteinases in tumor progression: focus on basal and squamous cell skin cancer. Exp Dermatol. Dvorak HF. Tumors: wounds that do not heal. Similarities between tumor stroma generation and wound healing. Harréus U. Surgical errors and risks - the head and neck cancer patient. GMS Curr Top Otorhinolaryngol Head Neck Surg. Byun JS, Gardner K. Wounds that will not heal: pervasive cellular reprogramming in cancer. Am J Pathol. Abramovitch R, Marikovsky M, Meir G, Neeman M. Stimulation of tumour angiogenesis by proximal wounds: spatial and temporal analysis by MRI. Br J Cancer. Wong SY, Reiter JF. Wounding mobilizes hair follicle stem cells to form tumors. Proc Natl Acad Sci U S A. Stuelten CH, Barbul A, Busch JI, Sutton E, Katz R, Sato M, et al. Acute wounds accelerate tumorigenesis by a T cell-dependent mechanism. Cancer Res. Hobson J, Gummadidala P, Silverstrim B, Grier D, Bunn J, James T, et al. Acute Inflammation induced by the biopsy of mouse mammary tumors promotes the development of metastasis. Breast Cancer Res Treat. Lawrence WT, Norton JA, Harvey AK, Gorschboth CM, Talbot TL, Grotendorst GR. Wound healing in sarcoma-bearing rats: tumor effects on cutaneous and deep wounds. J Surg Oncol. McNees P, Meneses KD. Pressure ulcers and other chronic wounds in patients with and patients without cancer: a retrospective, comparative analysis of healing patterns. Ostomy Wound Manag. Pyter LM, Husain Y, Calero H, McKim DB, Lin HY, Godbout JP, et al. Tumors alter inflammation and impair dermal wound healing in female mice. Article PubMed PubMed Central CAS Google Scholar. Demidova-Rice TN, Hamblin MR, Herman IM. Acute and impaired wound healing: pathophysiology and current methods for drug delivery, part 1: normal and chronic wounds: biology, causes, and approaches to care. Mustoe T. Understanding chronic wounds: a unifying hypothesis on their pathogenesis and implications for therapy. Cebioglu M, Schild HH, Golubnitschaja O. Cancer predisposition in diabetics: risk factors considered for predictive diagnostics and targeted preventive measures. EPMA J. Hurlow J, Couch K, Laforet K, Bolton L, Metcalf D, Bowler P. Clinical biofilms: a challenging frontier in wound care. Adv Wound Care New Rochelle. Konieczka K, Ritch R, Traverso CE, Kim DM, Kook MS, Gallino A, et al. Flammer syndrome. Golubnitschaja O, Debald M, Kuhn W, Yeghiazaryan K, Bubnov RV, Goncharenko VM. lammer Syndrome and potential formation of pre-metastatic niches: a multi-centred study on phenotyping, patient stratification, prediction and potential prevention of aggressive breast cancer and metastatic disease. Flammer J, Konieczka K. Retinal venous pressure: the role of endothelin. Khimji AK, Rockey DC. Endothelin and hepatic wound healing. Pharmacol Res. Yeghiazaryan K, Flammer J, Orgül S, Wunderlich K, Golubnitschaja O. Vasospastic individuals demonstrate significant similarity to glaucoma patients as revealed by gene expression profiling in circulating leukocytes. Mol Vis. CAS PubMed PubMed Central Google Scholar. Yeghiazaryan K, Flammer J, Golubnitschaja O. Predictive molecular profiling in blood of healthy vasospastic individuals: clue to targeted prevention as personalised medicine to effective costs. Golubnitschaja O, Debald M, Yeghiazaryan K, Kuhn W, Pešta M, Costigliola V, et al. Breast cancer epidemic in the early twenty-first century: evaluation of risk factors, cumulative questionnaires and recommendations for preventive measures. Tumor Biol. Golubnitschaja O, Yeghiazaryan K, Stricker H, Trog D, Schild HH, Berliner L. Patients with hepatic breast cancer metastases demonstrate highly specific profiles of matrix metalloproteinases MMP-2 and MMP-9 after SIRT treatment as compared to other primary and secondary liver tumours. BMC Cancer. Golubnitschaja O, Yeghiazaryan K, Abraham JA, Schild HH, Costigliola V, Debald M, et al. Breast cancer risk assessment: a non-invasive multiparametric approach to stratify patients by MMP-9 serum activity and RhoA expression patterns in circulating leucocytes. Amino Acids. This might also result in a pathologic cycle as the presence of necrotic tissue additionally serves as a nidus for bacterial proliferation. Surgical site infection — Surgical site infection SSI is defined by the United States Centers for Disease Control and Prevention as infection related to an operative procedure that occurs at or near the surgical incision within 30 days of the procedure or within 90 days if prosthetic material is implanted at surgery table 1 [ 12 ]. SSIs are often superficial and localized to the incision site but can also extend into deeper adjacent structures. See "Overview of the evaluation and management of surgical site infection" and "Complications of abdominal surgical incisions", section on 'Surgical site infection'. The degree of contamination of a surgical wound at the time of the operation is an important risk factor for infection. See "Overview of the evaluation and management of surgical site infection", section on 'Surgical wound classification'. Cellulitis — Cellulitis is both a descriptive term used to describe a clinical finding and a pathophysiologic process accompanying infection. Cellulitis refers to a non-necrotizing inflammation of the skin and subcutaneous tissue. Infectious changes causing cellulitis typically involve direct inoculation through the skin. However, the source is frequently not obvious and may involve microscopic breaches in the integument. See "Acute cellulitis and erysipelas in adults: Treatment". Burn wound infection — Thermal injury with tissue loss is often accompanied by concomitant immunosuppression, which can place the injured person at greater risk for infection [ 16 ]. See "Burn wound infection and sepsis". Pulmonary complications and recommendations on smoking cessation and nicotine replacement therapy are discussed in detail elsewhere. See "Strategies to reduce postoperative pulmonary complications in adults", section on 'Smoking cessation' and "Overview of smoking cessation management in adults". The constituents of tobacco smoke and mechanisms responsible for the vasoactive and other effects of smoking have not been fully elucidated; for many years nicotine was presumed to be responsible, but other constituents of tobacco smoke may have a greater impact. Tobacco smoke is a complex mixture of compounds eg, nicotine, carbon monoxide, tar, hydrogen cyanide, nitrogen oxides, N-nitrosamines, formaldehyde, benzene , several of which have a physiologic impact [ ]. The detrimental effect of smoking on wound healing is multifactorial, with mechanisms that include vasoconstriction causing a relative ischemia of operated tissues, a reduced inflammatory response, impaired bacteriocidal mechanisms, and alterations of collagen metabolism [ 18 ]. These are postulated to impair wound healing and cause wound dehiscence and incisional hernia. See "Basic principles of wound healing", section on 'Wound healing'. Smoking is associated with postoperative wound healing complications, which occur more often in smokers compared with nonsmokers as well as in former smokers compared with those who never smoked. A systematic review identified four randomized trials that evaluated the impact of preoperative smoking cessation four- to eight-week intervals of abstinence on postoperative wound healing. Preoperative smoking cessation significantly reduced the incidence of surgical site infection odds ratio [OR] 0. In a separate study, current or past smoking was associated with an increased risk for postoperative infection OR 1. Although smoking-induced vasoconstriction, mediated by nicotine , can reduce blood flow by up to 40 percent, the effect appears to be temporary, with tissue blood flow and oxygen levels restored to normal levels within 45 minutes [ ]. Most tissues with an adequate blood supply probably tolerate these transient alterations; however, tissue flaps, which have a fragile blood supply, and other ischemic tissues eg, moderate-to-severe peripheral artery disease might be vulnerable to smoking-induced reductions in blood flow. With respect to other effects of nicotine, both impaired and stimulated wound healing have been identified in experimental studies; however, no clinically significant detrimental or beneficial effects on wound healing have been demonstrated with the use of nicotine replacement therapies [ ]. AGING — Skin is not excluded from the complex processes of aging. The supply of cutaneous nerves and blood vessels decreases with age, in addition to a general thinning of tissue, including the dermis and basement membrane. There is a progressive loss of collagen and diminished ability to produce more collagen. These physiologic changes associated with aging contribute to slowed or impaired wound healing in older adults [ 35,36 ]. In several studies, the extremes of age infants and older individuals were identified as a risk factor for surgical site infection SSI [ 37 ]. One cohort study of more than , adult surgical patients found that increasing age independently predicted an increased risk of SSI only until age 65 years risk increasing 1. See 'Infection' above and "Overview of perioperative nutrition support", section on 'Consequences of malnutrition in surgical patients' and "Overview of the evaluation and management of surgical site infection". Thus, we generally prefer to screen for malnourishment by obtaining preoperative serum prealbumin and albumin levels in potentially high-risk patients and monitoring them to optimize nutritional status. Prealbumin and albumin are not perfect markers of nutritional status; however, these should be obtained on patients with nonhealing wounds [ 43 ]. In addition, measures of frailty and functional status may be linearly related to malnutrition and might also be incorporated into an assessment [ 44,45 ]. These are typically pressure wounds, similar in pathogenesis and appearance to neuropathic wounds occurring in areas of bony prominence such as the sacrum, knees, ankle malleoli, and heels. The sacrum may be particularly at risk when the presence of incontinence in spinal cord patients leads to a moist environment [ 46 ]. See "Epidemiology, pathogenesis, and risk assessment of pressure-induced skin and soft tissue injury". Immobilization in the absence of pressure is probably not a risk factor for wound development or chronicity. In fact, complete immobilization with total contact casting is an effective treatment for plantar diabetic foot ulceration [ 47 ]. The inflammatory phase of wound healing may be blunted in patients on long-term immune suppression such as is used in treating transplant patients and HIV patients, among others. Chemotherapy — The administration of chemotherapy may have a detrimental effect on wound healing, specifically through its direct or indirect effects on vascular endothelial growth factor VEGF. VEGF is an important factor contributing to angiogenesis during the early stages of wound healing but may also be an important regulator in malignancy and thus is a target of cancer therapy [ 52 ]. See "Toxicity of molecularly targeted antiangiogenic agents: Non-cardiovascular effects", section on 'Delayed wound healing' and "Toxicity of molecularly targeted antiangiogenic agents: Non-cardiovascular effects", section on 'Cutaneous toxicity'. Furthermore, neuropathy secondary to chemotherapy can produce loss of protective sensation and instability in a similar manner to diabetes. Glucocorticoids — Glucocorticoids may not have the same degree of negative effect as other immunosuppressive therapies, and locally applied topical steroids are often used in the treatment of chronic wounds [ 53 ]. While some degree of anti-inflammation may prevent wounds from becoming arrested in the inflammatory stage, significant suppression of inflammation can prevent wounds from progressing into the next stages of wound healing. This is a subjective and currently unquantifiable inflammatory balance [ 54,55 ]. Several studies have demonstrated the potential beneficial effects of topical steroid application in the treatment of chronic wounds, particularly when an abnormal and uncontrolled inflammatory stage is suspected within the stages of wound healing. Radiation — Radiation therapy has evolved as a powerful tool for tumor control as a sole therapy or administered adjunctively. More than 50 percent of cancer patients receive some form of radiation treatment, and, despite improvements in radiation technique, radiation-induced injury still contributes to poor wound healing. The term "radiation injury" refers to the morphologic and functional changes that can occur in noncancerous tissue as a direct result of ionizing radiation and may include apoptosis cell death with low doses of radiation or outright tissue necrosis with higher doses of radiation. Irradiated skin in the chronic stage is thin, hypovascular, extremely painful, and easily injured by slight trauma or infection [ 56 ]. See "Clinical manifestations, evaluation, and diagnosis of acute radiation exposure", section on 'Cutaneous'. Skin ulcers due to radiation injury are more commonly delayed in presentation and are due to ischemic tissue changes. Characteristic features of delayed radiation injury include telangiectasia and eccentric myointimal proliferation in the small arteries and arterioles. The proliferative changes may progress to obstruction, or the lumen may thrombose. These ulcers heal very slowly and may persist for several years. Given the changes that are known to occur with respect to the perfusion of irradiated tissue and the phases of wound healing, surgical incisions in these locations are more likely to develop a wound complication. If an incision is planned in an area of radiation exposure, the optimal timing for surgery remains unclear. While some have recommended waiting three to six weeks after radiation therapy to perform an incision or conversely to delay radiation therapy three to four weeks after an incision, surgery in the immediate perioperative period has been reported [ 57,58 ]. It is likely that the dosing and duration of radiation therapy affects this decision making, preventing the ability to make generalized recommendations; each case needs to be individualized. DIABETES — Numerous cytologic factors contribute to impaired wound healing in patients with diabetes [ 59 ]. These include decreased or impaired growth factor production, angiogenic response, macrophage function, collagen accumulation, epidermal barrier function, quantity of granulation tissue, keratinocyte and fibroblast migration and proliferation, number of epidermal nerves, bone healing, and abnormal balance between the accumulation of extracellular matrix components and their remodeling by matrix metalloproteinases. Diabetes is a particularly important risk factor for the development of chronic wounds from neuropathy and vasculopathy, which increase the risk of infection and delay healing [ 8,60 ]. Diabetes is frequently associated with peripheral artery disease PAD with atherosclerosis developing at a younger age and affecting more distal arteries below the knee eg, popliteal, tibial arteries. PAD in combination with diabetic neuropathy contributes to higher rates of nonhealing wounds and limb loss in diabetic patients compared with those without diabetes [ 61,62 ]. Up to one-third of people with diabetes in the United States will develop a foot ulcer [ 60,63,64 ]. Peripheral artery obstruction is present in approximately 20 percent of these patients and diabetic neuropathy in up to 50 percent of these patients [ 56,60 ]. Neuropathy alone can be responsible for the development of diabetic foot ulcers. Neuropathy associated with diabetes affects sensory, motor, and autonomic nerves. Sensory neuropathy diminishes the perception of pain that is protective when tissue injury has occurred [ 65 ]. Patients with diabetes may not be aware of the injury, particularly if the injured region cannot be seen or if the patient has a visual impairment. The motor nerves to the intrinsic muscles of the foot are affected in approximately 50 percent of patients with diabetes, resulting in claw deformities in the digits that transfer pressure to the plantar metatarsal heads. Increased local tissue pressure on the plantar surface or in other regions where bony deformities contact the shoe may lead to skin erosion and ulceration that may go unnoticed in patients with sensory deficits. In addition, autonomic neuropathy causes the skin to become dry and susceptible to skin fissures, tearing, and infection due to a loss of sweat and oil gland function. Loss of vascular tone may lead to foot edema [ 66 ]. Peripheral artery disease — Peripheral artery disease PAD with multilevel arterial obstruction decreases arterial blood flow, diminishes the delivery of oxygen and nutrients to the tissues, and impairs removal of metabolic waste products. Limb-threatening ischemia develops when blood flow is insufficient to meet the metabolic demands of tissue at rest and manifests clinically with extremity pain, nonhealing wounds picture 1 , or tissue loss [ 1,2 ]. There is no single cutoff or perfusion threshold for limb-threatening ischemia, as the condition is a spectrum. The presence of concomitant factors such as diabetes, renal failure, nutritional status, the complexity and extent of the wound, and recent or concomitant wound infection may require greater perfusion than expected to heal a given wound, particularly for foot wounds in patients with diabetes. For this reason, blood flow should be assessed in all such wounds and graded as part of a spectrum of ischemia that may require revascularization to expedite wound healing [ 8 ]. The ankle-brachial index is widely considered to be an appropriate baseline test for this assessment. See "Clinical features and diagnosis of lower extremity peripheral artery disease" and "Upper extremity atherosclerotic disease". Chronic venous insufficiency — Venous leg ulcers account for approximately 40 percent of wounds of the lower extremity [ 59 ]. An understanding of the normal anatomy and physiology of the venous return to the heart is essential for understanding the defects present in patients with chronic venous disease and ulceration. See "Pathophysiology of chronic venous disease". Faulty vein valves, venous obstruction, or failure of the "venous pump" leads to abnormally directed flow from the deep to superficial venous systems via the perforating veins. The most common site of incompetent perforators is 5 to 10 cm above the medial malleolus [ 63 ]. Congestion and pooling of blood in the superficial veins leads to venous hypertension, which, if sustained, is associated with histologic changes in the vein wall. See "Pathophysiology of chronic venous disease", section on 'Histologic changes'. EDEMA — Peripheral edema can be caused by a variety of conditions, but regardless of the etiology, the accumulation of interstitial fluid reduces the integrity of the skin and subcutaneous tissue, making it prone to injury. The increased interstitial pressure also impairs the capillary diffusion and cellular function required as part of the normal tissue healing process, contributing to impaired healing when wounds do occur. See "Pathophysiology and etiology of edema in adults". OBESITY — Obese individuals have a higher incidence of wound complications, including seroma, hematoma, wound infection, and wound dehiscence, as well as a higher incidence of pressure ulcers and venous ulcers. The etiology of wound complications in obese individuals is multifactorial, involving both local and systemic factors. Locally, factors contributing to poor wound healing include relative hypovascularity of the subcutaneous adipose tissue, which may also reduce antibiotic delivery and increase wound tension. Poor skin perfusion also makes obese individuals susceptible to pressure injury, which can be aggravated by difficulties in repositioning and increased shear forces during movement. LESS COMMON FACTORS — Other etiologies that can impair wound healing or lead to skin breakdown and chronic ulceration include conditions that cause vascular inflammation, obstruction, or thrombosis at the microvascular level. The final common pathway that produces ulceration or poor wound healing in these disorders is tissue ischemia. See 'Impaired wound healing' above and "Approach to the differential diagnosis of leg ulcers". Sickle cell disease — Sickle cell disease represents a form of local tissue ischemia occurring at the specific location of the wound. It is also obstructive in nature, similar to peripheral artery disease, but is caused by dysmorphic red blood cells physically occluding small vessels, usually of the lower extremities. The location and appearance of sickle cell wounds may be similar to ischemic and venous ulcerations. A peripheral blood smear may be helpful in making the diagnosis. Treatment of these wounds is similar to the treatment of other chronic wounds, but sickle cell wounds are known to progress much more slowly through wound healing and carry an increased risk of reoccurrence [ 67 ]. See "Overview of the clinical manifestations of sickle cell disease", section on 'Leg ulcers'. Others — Other conditions associated with impaired wound healing include cholesterol embolism, vasculitis, pyoderma gangrenosum, polyarteritis nodosum, scleroderma, cryoglobulinemia, granulomatosis with polyangiitis, thromboangiitis obliterans, warfarin-associated necrosis, heparin-induced thrombocytopenia, protein C deficiency, protein S deficiency, and antiphospholipid antibody syndrome. The cutaneous manifestations of these diseases can be found in separate topic reviews. SOCIETY GUIDELINE LINKS — Links to society and government-sponsored guidelines from selected countries and regions around the world are provided separately. See "Society guideline links: Chronic wound management". Wounds may be caused by a variety of mechanisms, including acute injury abrasion, puncture, crush , surgery, or other factors that cause breakdown of previously intact skin eg, ischemia, pressure. There is no specific time frame that distinguishes between acute and chronic wounds. These chemoattractants, including vascular endothelial growth factor VEGF , platelet-derived growth factor PDGF , and fibroblast growth factor FGF , as well as cytokines, promote the migration of inflammatory cells to the wound. After approximately 24 to 48 hours, vasodilation occurs, allowing for inflammatory cells such as neutrophils, monocytes, macrophages, and lymphocytes to arrive at the injured tissue and perform a host of different functions. Neutrophils are the first of the inflammatory cells to arrive, peaking at 24 hours. They phagocytize bacteria, clear microbial and other cellular debris. Also, polymorphonuclear leukocytes PMNs release reactive oxygen species that potentiate this killing process [8]. The next major step in wound healing involves the accumulation of macrophages, usually around 48 to 72 hours [8]. Macrophages help initiate the proliferation phase of the WHP. These cells also perform a variety of diverse functions, including promoting the inflammatory healing process through the release of cytokines, clearance of cellular debris, and attracting blast cells to the area of the wounding [8]. T-lymphocytes also play a critical but still poorly understood role, as their absence in the wound or delayed arrival has been associated with WHP impairment. As the proliferation phase gives way to remodeling, fibroblasts lay down the extracellular matrix ECM and allow for re-epithelialization of the wound. Fibroblasts produce components of the ECM, including collagen-glycosaminoglycan scaffolds and proteoglycans [8]. Furthermore, endothelial cells promote angiogenesis and formation of a new capillary bed to allow for continued remodeling [8]. Myofibroblasts promote wound contracture via actin filaments. The WHP is very complex and involves high levels of coordination between multiple tissues and cell types [6]. Consequently, impairment in the process can occur at any step along the sequence that leads to process completion. Many known factors can affect or modulate wound healing [7]. In the subsequent sections, we will discuss major modulators both positive and negative of the WHP, including a summary of some of the methods and techniques devised to promote wound healing [9]. There is no doubt that diabetes plays a detrimental role in wound healing. It does so by affecting the WHP at multiple steps. Wound hypoxia, through a combination of impaired angiogenesis, inadequate tissue perfusion, and pressure-related ischemia, is a major driver of chronic diabetic wounds [10]. Ischemia can lead to prolonged inflammation, which increases the levels of oxygen radicals, leading to further tissue injury. Elevated levels of matrix metalloproteases in chronic diabetic wounds, sometimes up to times higher than acute wounds, cause tissue destruction and prevent normal repair processes from taking place [10]. Furthermore, diabetes is associated with impaired immunity, with critical defects occurring at multiple points within the immune system cascade of the WHP. For example, neutrophils show impaired chemotaxis and phagocytosis. As a result, diabetic wounds are prone to chronic infection due to inadequate bacterial clearance [10]. To further complicate matters, these wounds have defects in angiogenesis and neovascularization. Normally, wound hypoxia stimulates mobilization of endothelial progenitor cells via vascular endothelial growth factor VEGF [8]. In diabetic wounds, there are aberrant levels of VEGF and other angiogenic factors such as angiopoietin-1 and angiopoietin-2 that lead to dysangiogenesis [11]. Diabetic neuropathy may also play a role in poor wound healing. Lower levels of neuropeptides, as well as reduced leukocyte infiltration as a result of sensory denervation, have been shown to impair wound healing [10]. When combined, all these diverse factors play a role in the formation and propagation of chronic, debilitating wounds in patients with diabetes. Cigarette smoking leads to numerous adverse health consequences, including various types of cancer, primary lung disease, and cardiovascular disease, among others [12] [13]. However, in addition to those, smoking has severe ill-effects on the WHP [14]. This occurs through multiple pathways, but most have the common theme of inducing wound ischemia. For example, nicotine in smoke acts as a vasoconstrictor. Also, tobacco use stimulates the release of catecholamines such as epinephrine, leading to further reductions in tissue blood flow and hypoxia [15]. Relative wound ischemia can also result from the development of chronic obstructive pulmonary disease, which can lead to the permanent lowering of oxygen tension in the blood. Carbon monoxide CO in cigarette smoke binds to hemoglobin with times greater affinity than oxygen, so even small amounts of carbon monoxide can profoundly reduce the oxygen carrying capacity of hemoglobin. CO binding to hemoglobin will cause a leftward shift of the oxyhemoglobin dissociation curve, leading to less oxygen unloading at the tissue level [16] [14] [16]. In addition to the induction of ischemia, smoking leads to immunopathy of the wound via impaired PMN migration into the wound. Fibroblast migration and proliferation are also hindered, leading to decreased production of ECM and ultimately weaker scar formation. Not surprisingly, patients who stop smoking show improvement in wound healing [17]. The nutritional needs of the healing wound are very complex. Wounds require a myriad of different micro and macronutrients to heal properly [18]. Among amino acids of importance to the WHP, arginine, and glutamine play a critical in the overall process. Arginine improves immune function, supports collagen deposition as a precursor to proline , and plays a role in neovascularization. Arginine supplementation also has a positive effect on wound healing. Glutamine is a critical energy source in proliferating cells e. This amino acid is thought to improve the overall wound strength by increasing levels of mature collagen. The 2 other major macronutrients, fatty acids and carbohydrates, are also critical to wound healing. Carbohydrates, primarily glucose, act as the primary fuel for cells as it becomes broken down to form adenosine triphosphate ATP. Polyunsaturated fatty acids, such as omega-3 and omega-6 fatty acids, both of which are essential fatty acids, may enhance the WHP by having an overall positive effect on host immune function [19] [20]. Several micronutrients are worth mentioning because they play a particularly important role in wound healing [21]. These include ascorbic acid, or vitamin C, vitamin A, vitamin E, as well as magnesium, zinc, and iron. Vitamin C supports the hydroxylation of proline to hydroxyproline, which is essential for proper collagen formation. Vitamin A similarly supports collagen formation, as well as immune modulation, and decreased metalloprotease ECM degradation. As an antioxidant, vitamin E helps protect against oxidative tissue destruction, as well as may decrease excess scar formation. Magnesium is a cofactor in enzymes involved in collagen synthesis. Zinc, on the other hand, is a cofactor for DNA and RNA polymerase, playing a vital role in cell division. Finally, iron deficiency has been shown to result in impaired collagen synthesis. Further discussion of the most critical among the above micronutrients is provided at the end of this manuscript [22]. Obesity is a significant factor in surgical wound healing. Abdominal obesity is correlated with oxidative stress, a phenomenon associated with deficiency of adiponectin e. Adiponectin-deficient state leads to impaired perfusion and reepithelialization of the wound. Moreover, hypovolemia combined with relative hypoperfusion and reduction in oxygen delivery lead to further tissue injury. Consequently, wound complications, including surgical site infections and fat necrosis are more prevalent in obese patients. Various combinations of the same factors may be associated with impaired secondary healing following primary wound-related morbidity [23]. Pressure ulcers are more likely to develop in obese patients through pressure-related ischemia and hypovascularity, as well as decreased mobility. Contact between the skin and various hospital surfaces e. Systemic effects of obesity, such as hypertension, hyperglycemia, and upregulation of the stress hormones in response to the physiologic burden of surgery and acute illness, all work to impair further wound healing. Additional factors involved in this complex process include blunting of the immune and inflammatory responses. Interestingly, these ill-effects of obesity are largely reversible through weight loss [24]. Stress has been demonstrated to be a major contributor to a broad range of health conditions and illnesses, including cardiovascular disease, cancer, and obesity. Stress states lead to upregulation of stress hormones via the hypothalamic-pituitary axis and the release of adrenocortical hormones. Resultant changes include elevated levels of cortisol, glucocorticoids, and catecholamines. Cortisol works to blunt the immune response by blocking the production of important cytokines such as IL-1beta, IL-6, and TNF-alpha. The impairment of immune response ultimately leads to deficient wound healing [25] [26]. Wound healing is a vast topic area, with many aspects remaining poorly understood despite the tremendous amount of progress over the past few decades. Various co-morbid conditions e. More recently, a better understanding of the role micronutrients play in wound healing, along with the introduction of novel wound care therapeutics e. Numerous wound management devices have been introduced over the years to improve wound healing. However, none have been as influential and successful as negative pressure wound therapy NPWT therapy. NPWT involves the application of subatmospheric pressure on wound via a sponge-based system with an airtight seal directly over the wound, connected under sealed conditions to a suction device. Benefits of NPWT are realized via several different mechanisms. First, the subatmospheric pressure applied to the wound helps to remove wound exudate and other materials that are known to impair the WHP. Secondly, the presence of subatmospheric pressure promotes angiogenesis and tissue perfusion by increasing cellular proliferation and migration into the wound. The suction also assists in bringing wound edges together. When combined, all of the above elements and mechanisms work synergistically to help speed up wound healing. NPWT devices can be used on a wide variety of wounds, such as pressure ulcers, large abdominal wounds, traumatic wounds, as well as complex, difficult-to-cover tissue defects following debridement operations e. Of note, NPWT is contraindicated in certain situations, such as wound surfaces involving malignancy, untreated osteomyelitis, non-enteric and unexplored fistulae, and necrotic tissue with eschar e. It has long been known that Vitamin A may have beneficial effects on wound healing in the setting of previous systemic exposure to corticosteroids. More specifically, Vitamin A has been shown to overcome the inhibitory effects of cortisone and related corticosteroids on the rate of gain in tensile strength of the wound [34] [35] [34]. This may be especially pronounced in early stages of the WHP. At the same time, Vitamin A by itself does not seem to be a significant modulator of the WHP, suggesting that its beneficial action in the setting of prior corticosteroid use is related to the interaction s specific to corticosteroid-specific pathway s [36] [37] [36]. Vitamin C and zinc have both been found to improve wound healing characteristics, although clinical adoption and implementation of this therapeutic combination is less than universal. Mechanistically, vitamin C has several favorable effects on the WHP. First, it is a powerful antioxidant and free radical scavenger. Second, it is important to systemic immunity, and along with Zinc helps boost the immune system when taken in the postoperative period. Together with Arginine and Zinc, Vitamin C is important for collagen synthesis. The evidence is strongest for supplementing vitamin C and zinc during the immediate postoperative period [38] [39] [40] [38]. Among other interesting and important developments in wound care, there is evidence that vitamin-D supplementation may help positively modulate impaired wound healing, although further research toward mechanistic understanding is required in this area. More specifically, the role of vitamin D in the WHP may be indirect, through beneficial effects on closely related physiological processes, such as glucose homeostasis [41] [42]. Finally, another vast topic area that is worth mentioning but too extensive to fully discuss in this review is the use of growth factors in the modulation of the WHP. It has been demonstrated that delivery of various specific growth factors e. Further research is required to better define mechanisms of action, potential side effects, and the overall risk-benefit of human application of such therapies. While considered by many as archaic, maggot debridement therapy MDT has been shown unequivocally to be of benefit in wound healing [46] [47]. MDT is based on the observation that fly larvae only debride dead, devitalized, and necrotic tissue. Healthy, viable tissue is not threatened during the MDT, making this therapy uniquely suited for debridement of devitalized tissues with truly surgical precision [48]. In fact, MDT is considered a form of "biosurgery. This liquefied material is then ingested, resulting in effective debridement of the tissue of interest. It has been shown that MDT can help debride large wounds in as little as 72 hours, resulting in a viable granulation bed that is suitable for conventional wound management. In addition to chemical debridement, larval secretions are also characterized by significant antimicrobial activity, active against a wide range of pathogenic and often antibiotic-resistant bacteria, mostly gram-positive species. Maggots work best on moist environments with sufficient oxygen supply [49]. They are approved for use in non-healing necrotic skin and soft tissue wounds, pressure and venous stasis ulcers, neuropathic foot ulcers, and non-healing traumatic or surgical wounds [50]. Most recent developments in this area include the introduction of transgenic maggots that secrete human growth factors in their saliva [51]. Clinical applications of this therapy are continually expanding. Of interest, application of MDT can be accomplished through direct exposure of the maggots to the wound bed using a specialized "housing" or through indirect exposure using larvae contained within a sealed, semi-permeable bag [52] [53]. Hyperbaric oxygen therapy HBOT is another treatment modality that has been around for quite some time, but only recently saw a resurgence in interest due to promising effects on the WHP, especially in the setting of chronic and complicated wounds [54] [55]. Chronic wounds, often seen as a consequence of diabetes, arterial or venous disease, are increasingly common and result in significant impact on the affected patients, their caretakers, and the healthcare system in general. The beneficial action of HBOT on wound healing is predicated on the increased supply of oxygen to wounds that are refractory to other, more conventional treatment approaches [56]. In practice, HBOT involves the patient being temporarily enclosed in a special chamber that in many ways approximates conditions used for deep sea divers and involves gradual "dive" followed by a pre-defined time interval at a certain "oxygen pressure level," and subsequent gradual "resurfacing" process. While in the chamber, the patient is exposed to markedly elevated concentrations of pure oxygen, leading to elevation of systemic and tissue oxygen levels. It has been demonstrated that HBOT is effective in improving the course of chronic diabetes-related extremity wounds, potentially reducing the need for major but not necessarily minor amputations. Available evidence suggests beneficial effects of HBOT on wounds are usually apparent within approximately 6 weeks of therapy, but long-term beneficial effects continue to be questionable. Another area where HBOT can be beneficial is the management of necrotizing soft tissue infections e. Additional difficult-to-treat types of wounds that have been speculated to benefit from HBOT are the chronic pressure ulcers due to its inherently "ischemic" nature and venous ulcers; however, there is no solid evidence to support HBOT for either of these indications at this time [57] [60]. The best management of wounds is taken care of by an interprofessional team of a nurse specializing in wound care and a clinician with significant wound experience. Caring for wounds not only involves regular follow-ups but patient education. A coordinated team approach has been shown to be most effective in wound management. Disclosure: Brian Wernick declares no relevant financial relationships with ineligible companies. |
Impaired wound healing -
Positioning and elevation of the edematous body part to promote venous return and diminish congestion improve tissue perfusion. Assist in preparing the client for hyperbaric oxygen therapy.
Hyperbaric oxygen therapy involves either the application of topical oxygen at increased pressure directly to the wound or placing the client into a hyperbaric oxygen chamber.
Both methods of hyperbaric oxygen therapy promote wound healing by stimulating new vascular growth and aiding in the preservation of damaged tissue.
Administer muscle relaxants for spasticity or prepare the client for surgery. Spasticity should be controlled pharmacologically with medications such as diazepam , baclofen, or dantrolene sodium.
Clients with spasticity refractory to medication may be candidates for neurosurgical ablation. Provide oral nutritional supplementation as recommended. Malnutrition is one of the few reversible contributing factors for pressure injuries.
Prepare the client for surgical procedures as indicated. Surgical intervention is necessary when the injury is extensive when complications exist, and when the ulcer does not respond to treatment.
Surgical procedures include debridement, incision and drainage, bone resection, and skin grafting. Osteomyelitis is a common complication of wounds of stage IV depth.
Assist during urinary or fecal diversion procedures as indicated. Urinary or fecal diversion may be necessary to optimize wound healing. Prepare the client for the reconstruction of pressure injury as indicated. Reconstruction of a pressure injury is aimed at the improvement of client hygiene and appearance, prevention or the resolution of osteomyelitis and sepsis, reduction of fluid and protein loss through the wound, and prevention of future malignancy.
Educating clients and caregivers about wound care and skin integrity empowers them to take an active role in their own care. By providing knowledge bout proper wound cleaning, dressing changes, and preventive measures, individuals can confidently perform self-care activities and actively contribute to their healing process.
Educate the client about proper nutrition, hydration, and methods to maintain tissue integrity. The client needs proper knowledge of their condition to prevent impaired tissue integrity. Teach the client and caregiver about skin and wound assessment and ways to monitor for signs and symptoms of infection, complications, and healing.
Early assessment and intervention help prevent the development of serious problems. Signs of a localized wound infection include redness, warmth, and tenderness around the wound. Instruct client, significant others, and family in the proper care of the wound, including handwashing , wound cleansing, dressing changes, and application of topical medications.
Nursing management for clients who must perform self-care for skin problems, such as applying medications and dressings, focuses on educating the client about how to cleanse the affected area and pat it dry, apply medication to the lesion while the skin is moist, cover the area with plastic if recommended, and cover with an elastic bandage, dressing, or paper tape to seal the edges.
Educate the client on the need to notify the healthcare provider or nurse. This is to prevent further impaired tissue integrity complications. New signs of infection should be reported to the healthcare provider with an anticipated order for a wound culture. Inform the client or caregiver against elevating the head of the bed repeatedly.
Encourage the use of lifting devices like trapeze or bed linen to move the client in bed. The common cause of impaired skin integrity is friction which involves rubbing heels or elbows toward bed linen and moving the client up in bed without the use of a lift sheet.
Educate the client and caregiver about the causes of pressure. This information can assist the client or caregiver in finding methods to prevent skin breakdown. The development of pressure injuries is directly related to the duration of immobility: if the pressure continues long enough, small vessel thrombosis and tissue necrosis occur, and a pressure injury results.
Reinforce the importance of turning, mobility, and ambulation. These will enhance their sense of efficacy and can improve compliance with the prescribed interventions. When a person is immobile and inactive, pressure is exerted on the skin and subcutaneous tissue by objects on which the person rests, such as a mattress, chair seat, or cast.
Educate clients and caregivers about proper skin care. Educating clients and caregivers on methods to maintain skin integrity enhances their sense of self-efficacy and prevents skin breakdown. Continuous moisture on the skin must be prevented by meticulous hygiene measures.
It is important to pay special attention to skin folds, including areas under the breasts, arms, and groin, and between the toes. The skin may be lubricated with a bland lotion to keep it soft and pliable.
Drying agents and powders are avoided. Educate the client to inspect pressure areas routinely. When decreased sensory perception exists, the client and caregivers are taught to inspect potential pressure areas visually every morning and evening, using a mirror if necessary, for evidence of pressure injury development.
Reinforce the importance of regularly checking diapers and incontinence pads in immobile clients. Diapers and incontinence pads may be useful in absorbing moisture away from the surface of the skin, provided that they are checked regularly and changed when soiled. The nurse must instruct the family to be alert for environmental factors that may contribute to pressure on the skin and diminished circulation such as wrinkles in sheets or pressure of tubes on the skin, and remove the source of pressure.
Ensure that the client has a strong support system at home. Clients and their support system must realize that it is their responsibility to avoid recurrent and new ulceration and that this is a lifelong process. Disclosure: Included below are affiliate links from Amazon at no additional cost from you.
We may earn a small commission from your purchase. For more information, check out our privacy policy. This care plan handbook uses an easy, three-step system to guide you through client assessment, nursing diagnosis, and care planning.
Includes step-by-step instructions showing how to implement care and evaluate outcomes, and help you build skills in diagnostic reasoning and critical thinking. New to this edition are ICNP diagnoses, care plans on LGBTQ health issues, and on electrolytes and acid-base balance.
The sixteenth edition includes the most recent nursing diagnoses and interventions and an alphabetized listing of nursing diagnoses covering more than disorders. Nursing Diagnosis Manual: Planning, Individualizing, and Documenting Client Care Identify interventions to plan, individualize, and document care for more than diseases and disorders.
Table of Contents What is tissue integrity? What is wound care? Phases of wound healing Types of wound healing Nursing Care Plans and Management Nursing Problem Priorities Nursing Assessment Nursing Diagnosis Nursing Goals Nursing Interventions and Actions 1.
Skin and Wound Assessment 2. Providing Effective Skin and Wound Care Promoting skin integrity Providing wound care 3.
Proper Suture and Staple Removal 4. Drain Management 5. Management of Burn Wounds Assessment of burn injuries Emergency burn management Wound cleaning and dressing Medication administration Surgical management of burns 6. Management of Pressure Injuries Assessment and classification of pressure injuries Provide relief from pressure Proper client positioning Medical management of pressure injuries Surgical management of pressure injuries 7.
Client and Caregiver Education Recommended Resources See also References and Sources What is tissue integrity? Phases of wound healing When skin is injured, there are four phases of wound healing that take place: hemostasis, inflammatory, proliferative, and maturation.
In the hemostasis phase, platelets release growth factors that alert various cells to start the repair process at the wound location. This phase lasts up to 60 minutes, depending on the severity of the injury. After the hemostasis phase, the inflammatory phase begins, wherein vasodilation occurs so that white blood cells in the bloodstream can move into the wound to start cleaning the wound bed.
This appears as edema, erythema, and exudate to the observers. The proliferative phase begins within a few days after the injury and includes four important processes: epithelialization, angiogenesis, collagen formation, and contraction.
Epithelialization refers to the development of new epidermis and granulation tissue, which is a new connective tissue with new, fragile, thin-walled capillaries. Angiogenesis occurs when capillaries begin to develop within the wound 24 hours after injury.
These capillaries bring more oxygen and nutrients to the wound for healing. Collagen is formed to provide strength and integrity to the wound. At the end of the proliferation phase, the wound begins to contract in size. During this phase, collagen continues to be created to strengthen the wound.
A wound typically heals within four to five weeks and often leaves behind a scar. Types of wound healing There are three types of wound healing: primary intention, secondary intention, and tertiary intention.
Primary intention. This means that the wound is sutured, stapled, glued, or otherwise closed so the wound heals beneath the closure. This type of healing occurs with clean-edged lacerations or surgical incisions.
Closed edges are referred to as approximated. Secondary intention. This occurs when the edges of a wound cannot be approximated or brought together, so the wound fills in from the bottom up by the production of granulation tissue.
Examples of this type are pressure injuries and chainsaw injuries. These are at a higher risk of infection. Tertiary intention. This refers to a wound that has had to remain open or has been reopened, often due to severe infection. The wound is typically closed at a later date when the infection has resolved.
Nursing Care Plans and Management Effective wound care and the maintenance of skin integrity are vital aspects of nursing care. Nursing Problem Priorities The following are the nursing priorities for clients with wounds or compromised skin integrity.
Wound assessment. Frequent wound assessment based on the type, cause, and characteristics of the wound is necessary to help determine the type of treatment required to manage the wound effectively and promote maximal wound healing. Effective wound care.
Quality wound care is important for rapid and uncomplicated healing through decreasing complications, repeated admissions, length of hospital stay, and costs, and enhancing client quality of life. Proper suture and staple removal. Proper timing and technique in suture or staple removal prevent complications that may arise from a non-healed wound.
Drain management. The site and drain should be checked periodically throughout the shift to ensure the drain is functioning effectively and that no leaking occurs. Wound care for burns. Proper management of burn injuries is required to prevent wound deterioration.
Prevention and effective treatment are imperative to avoid developing or worsening pressure injuries. Client and caregiver education. Education empowers the client and their caregivers to actively participate in the healing process, promotes adherence to treatment plans, and fosters a proactive approach to preventing complications.
Nursing Assessment A thorough assessment of the skin or the wound must be conducted, including measurements of wound dimensions, evaluation of wound bed appearance, identification of any signs of infection, and assessment of surrounding skin integrity.
A break in tissue integrity is characterized by the following subjective and objective data: The affected area is hot, and tender to touch Damaged or destroyed tissue e. Nursing Goals Goals and expected outcomes may include: The client reports any altered sensation or pain at the site of tissue impairment.
The client demonstrates an understanding of the plan to heal tissue and prevent injury. The client describes measures to protect and heal the tissue, including wound care. Nursing Interventions and Actions Therapeutic interventions and nursing actions for clients with impaired skin integrity include: 1.
Type Types of wounds may include abrasions, lacerations, burns, surgical incisions, pressure injuries, skin tears, arterial ulcers, or venous ulcers. It is important to understand the type of wound present to select appropriate interventions. Location The location of the wound should be documented precisely.
A body diagram template is helpful to demonstrate exactly where the wound is located. Size Wound size should be measured regularly to determine of the wound is increasing or decreasing in size.
Length is measured using the head-to-toe axis, and width is measured laterally. Degree of tissue injury Wounds are classified as partial-thickness or full-thickness. For pressure injuries, it is important to assess the stage of the injury see Management of Pressure Injuries.
Color of the wound base Assess the base of the wound for the presence of healthy, pink, or red granulation tissue. Note the unhealthy appearance of dark red granulation tissue, white or yellow slough, or brown or black necrotic tissues.
Drainage The color, consistency, and amount of exudate or drainage should be assessed and documented at every dressing change. Murphree, Assess the skin for dermatitis or exposure to chemical irritants These conditions can cause inflammation, resulting in redness, and itching, and may cause blisters.
Providing Effective Skin and Wound Care There are much more opportunities to protect and enhance skin integrity from the outside. Promoting skin integrity Clean, dry, and moisturize skin, particularly bony prominences, twice daily or as indicated by incontinence or sweating.
Providing wound care Provide wound care as needed. Polyhexamethylene biguanide When PHMB attaches to the acid membrane elements of the bacteria, the bacteria subsequently lose fluidity, causing the separation of the individual membrane lipids and dissolution of the bacterial cell. This bactericidal mechanism means there are no residual organisms left alive to facilitate resistance.
PHMB has been combined in gauze and foam dressing formats. They are best utilized for healable surface wounds with exudate. Silver Silver is ideally suited to healable wounds with critical colonization.
It is an antibacterial agent in an ionized form that can attack cell membranes, cytoplasmic organelles, and DNA, so resistance is uncommon. Silver is most often combined with calcium alginates, hydrofibers, foams, and hydrogels. Iodine Iodine has several antimicrobial actions including blocking bacterial cell efflux pumps, interfering with cellular respiratory processes, changing DNA structure, and denaturing cellular proteins and enzymes.
Iodophors are safer-slow-release iodine delivery systems. The two most commonly used are povidone-iodine and cadexomer iodine. Clients on iodine for large wounds or extended periods should have thyroid function tests at regular intervals as hypothyroidism or hyperthyroidism can be induced by iodine wound dressings.
Methylene blue and crystal violet foam dressings This product is a relatively non-release foam dressing with two agents, MB and CV, which produce a redox environment inhibiting the growth and survival of bacteria. The original polyvinyl alcohol foam needs to be partially hydrated to bind the surface slough and provide autolytic debridement.
Honey Honey has been used in wound care for centuries because of its antibacterial and anti-inflammatory properties. Its acidic pH and high sugar content make the local wound environment hostile to bacteria.
Honey may lose its antibacterial action when diluted with wound exudate, but this may not increase the incidence of bacterial resistance. Medical-grade honey should be used instead of honey from food sources this is because bacterial spores can persist in honey and have the potential to cause disease if activated Sibbald et al.
Topical growth factor therapy This is a platelet-derived growth factor that recruits and stimulates fibroblast proliferation, promoting granulation tissue formation.
It is usually indicated for neuropathic diabetic ulcerations and wounds that extend to the subcutaneous tissues or deeper. This can be applied once daily to the wound bed. Acellular extracellular matrices These are non-living tissues derived from allogenic, xenographic, or synthetic sources that accelerate healing with minimized scar tissue formation.
These agents are indicated for partial and full-thickness wounds, burn wounds, traumatic wounds, and surgical wounds. They deliver exogenous growth factors to the wound bed and are antimicrobial and anti-inflammatory.
These allografts are indicated for acute and chronic wounds and non-healing wounds. They can be applied directly to the wound bed. Cell-based therapies These deliver exogenous growth factors to the wound bed with visible cells cultured on different bioabsorbable matrices.
Cell-based therapies can be epidermal, dermal, or bilayer therapies. These cells are removed from cell-based therapies including hair follicles, sweat glands, blood vessels, and immune cells. Proper Suture and Staple Removal Sutures are tiny threads, wire, or other materials used to sew body tissue and skin together.
Drain Management Drain management systems are commonly used during post-operative surgical management to remove drainage, prevent infection, and enhance wound healing. Assessment of burn injuries Evaluate the burn client using the ABCs. First-degree burns These are usually red, dry, and painful. Burns initially termed first-degree are often actually superficial second-degree burns, with sloughing occurring the next day.
Second-degree burns These burns are often red, wet, and very painful. Their depth, ability to heal, and propensity to form hypertrophic scars vary enormously. Third-degree burns These are generally leathery in consistency, dry, insensate, and waxy. These wounds will not heal, except by contraction and limited epithelial migration, with resulting hypertrophic and unstable cover.
Fourth-degree burns These burns involve underlying subcutaneous tissue, tendon, or bone. Emergency burn management Remove the source of flames. Irrigate chemical burns. Wound cleaning and dressing Cleanse and dress the wound gently and regularly.
Medication administration Apply topical antibacterials to burn wounds as indicated. Silver has a broad antibacterial spectrum and is painless upon application.
Aqueous 0. This has broad-spectrum coverage, including fungi; however, it leeches off electrolytes. Mafenide acetate. This agent has also broad antibacterial spectrum properties and can best penetrate eschars. This is a bland and nontoxic topical material.
Debriding enzymes. These enzymes are useful in selected partial-thickness wounds. Porcine xenograft This adheres to the wound coagulum and provides excellent pain control. Split-thickness allograft This graft vascularizes and provides durable temporary closure of the wounds.
Hydrocolloid dressings These provide a vapor and bacteria barrier while absorbing wound exudate. Impregnated gauzes These provide a vapor and bacteria barrier while allowing drainage.
Acticoat This is a nonadherent wound dressing that delivers a low concentration of silver for antisepsis. Biobrane A synthetic bilaminate that facilitates fibrovascular tissue growth into the inner layer and provides a temporary vapor and bacteria barrier.
Transcyte A synthetic bilaminate that facilitates fibrovascular tissue growth into the inner layer populated with allogenic fibroblasts and an overlying layer that provides a temporary vapor and bacteria barrier.
Alloderm R This consists of cell-free allogenic human dermis and requires an immediate thin overlying autograft. Surgical management of burns Assist in wound debridement as indicated.
There are four types of debridement: Natural debridement The devitalized tissue separates from the underlying viable tissue spontaneously. Bacteria present at the interface of the burned tissue and the viable tissue gradually liquefy the fibrils of collagen that hold the eschar in place.
The process may take weeks to months to occur. Mechanical debridement This involves the use of surgical tools to separate and remove the eschar. Dressing changes and wound cleaning aid in the removal of wound debris.
Wet-to-dry dressings are not advocated in burn care because of the possibility of removing viable cells along with necrotic tissue. Chemical debridement Topical enzymatic agents are available to promote the debridement of burn wounds.
Because such agents usually do not have antimicrobial properties, they may be used together with topical antibacterial therapy to protect the client from bacterial invasion.
Surgical debridement Early surgical excision to remove devitalized tissue along with early burn wound closure is now recognized as one of the most important factors contributing to the survival of a client with a major burn injury. This may be performed as soon as possible after the burn, once the client is hemodynamically stable and edema has decreased.
Ideally, the wound is then covered immediately with a skin graft and a dressing. Management of Pressure Injuries Once a pressure injury has developed, immediate treatment is required.
Assessment and classification of pressure injuries Classify pressure ulcers by assessing the extent of tissue damage.
The following are the stages of pressure ulcers: Stage I. Nonblanchable erythema signaling potential ulceration.
This leads to wound contraction and formation of the granulation tissue. New blood vessel formation - called angiogenesis - occurs simultaneously which facilitates the transport of oxygen and nutrients to the newly formed tissue.
In the final stage, type III collagen is remodeled and replaced with type Icollagen which has more tensile strength. Any factor or disease that can disrupt the normal stages of wound healing can lead to delayed wound healing.
Some of the factors are described below:. A common cause of delayed wound healing is infection. At the time of injury, microorganisms can enter the tissue. These microbes can delay wound healing by further prolonging the inflammatory process. Bacteria cause the release of pro-inflammatory cytokines which can inadvertently raise the levels of MMPs matrix metalloproteases , which are a family of enzymes that degrade the extracellular matrix.
This enzyme degrades the granulation tissue at the wound site, hence contributing to a delayed wound closure. The commonly associated bacteria with delayed wound healing are P.
aeruginosa and Staph Aureus. These bacteria tend to form 'biofilms' which are complex structures that resist antibiotics and degradation by the neutrophils. Without adequate wound care and decontamination, healing is extensively delayed in the setting of bacterial superinfection.
Collagen is an important constituent of granulation tissue and any nutritional deficiency that can affect its synthesis will lead to delayed wound healing.
Vitamin C, which is a cofactor required for collagen synthesis, and protein deficiency can negatively affect the wound healing process. When assessing chronic wounds, wound care specialists need to consider the nutritional status of their patients. Addressing these deficiencies can help improve wound healing.
Steroids are known for their potent anti-inflammatory effect and unfortunately, this effect can be destructive for wound healing. Inflammation is an essential step in wound healing.
As steroids inhibit the inflammatory process, they can halt normal wound repair. As a result, an inadequate amount of granulation tissue is produced. Steroids are also known to increase the risk of wound infections which leads to impaired wound healing.
Patients on long-term steroid use are also at an increased risk of developing diabetes, a metabolic syndrome that can further complicate the wound healing process.
Globally, million people are suffering from diabetes. The prevalence of diabetes is steadily rising, and diabetes-related complications are also expected to see an increase.
Diabetes contributes to wound chronicity through multiple mechanisms. Patients with diabetes experience low tissue blood supply which affects the oxygen and nutrient supply to the wound site.
As a consequence,wounds heal slowly. Moreover, diabetes also predisposes individuals to neuropathy or nerve damage which means that diabetic patients aren't always aware of any trauma they experience. Decreased tissue perfusion combined with neuropathic changes puts diabetic patients at an increased risk of developing chronic ulcers and wounds.
Diabetes is the single most likely cause of lower-limb amputations in the United States. To minimize these grim statistics, initial screening and management by podiatristsis vital. Podiatrists are well trained in the lower limb anatomy and are often the first to detect any initial ischemic or neuropathic changes.
They can formulate a comprehensive foot care plan, treatment, and follow-up for diabetic patients. Diabetic foot ulcers are complex and often require a multidisciplinary management approach. A comprehensive treatment plan led by vascular surgeons, podiatrists and endocrinologists can help significantly reduce the rate of amputations in diabetic patients.
Wounds require oxygen, nutrients, and proper blood supply for optimum healing. An adequate blood supply to the tissues is therefore essential. Peripheral vascular disease affects the blood supply to the extremities and is linked with the development of chronic wounds.
Londahl M. Hyperbaric oxygen therapy as adjunctive treatment of diabetic foot ulcers. Liu R, Li L, Yang M, Boden G, Yang G. Systematic review of the effectiveness of hyperbaric oxygenation therapy in the management of chronic diabetic foot ulcers.
Mayo Clin Proc. Hyperbaric oxygen therapy for diabetic ulcers: systematic review and meta-analysis. Int J Technol Assess Health Care. Margolis DJ, Gupta J, Hoffstad O, Papdopoulos M, Glick HA, Thom SR, et al. Lack of effectiveness of hyperbaric oxygen therapy for the treatment of diabetic foot ulcer and the prevention of amputation: a cohort study.
Isaac AL, Armstrong DG. Negative pressure wound therapy and other new therapies for diabetic foot ulceration: the current state of play.
Argenta LC, Morykwas MJ. Vacuum-assisted closure: a new method for wound control and treatment: clinical experience. Plikaitis CM, Molnar JA. Subatmospheric pressure wound therapy and the vacuum-assisted closure device: basic science and current clinical successes.
Seo SG, Yeo JH, Kim JH, Kim JB, Cho TJ, Lee DY. Negative-pressure wound therapy induces endothelial progenitor cell mobilization in diabetic patients with foot infection or skin defects. Exp Mol Med.
Vig S, Dowsett C, Berg L, Caravaggi C, Rome P, Birke-Sorensen H, et al. Evidence-based recommendations for the use of negative pressure wound therapy in chronic wounds: steps towards an international consensus. J Tissue Viability. Thakral G, Lafontaine J, Najafi B, Talal TK, Kim P, Lavery LA.
Electrical stimulation to accelerate wound healing. Diabet Foot Ankle. Moretti B, Notarnicola A, Maggio G, Moretti L, Pascone M, Tafuri S, et al.
The management of neuropathic ulcers of the foot in diabetes by shock wave therapy. BMC Musculoskelet Disord. Huang P, Li S, Han M, Xiao Z, Yang R, Han ZC.
Autologous transplantation of granulocyte colony-stimulating factor-mobilized peripheral blood mononuclear cells improves critical limb ischemia in diabetes. Dubsky M, Jirkovska A, Bem R, Fejfarova V, Pagacova L, Sixta B, et al. Both autologous bone marrow mononuclear cell and peripheral blood progenitor cell therapies similarly improve ischaemia in patients with diabetic foot in comparison with control treatment.
Humpert PM, Bartsch U, Konrade I, Hammes HP, Morcos M, Kasper M, et al. Locally applied mononuclear bone marrow cells restore angiogenesis and promote wound healing in a type 2 diabetic patient. Exp Clin Endocrinol Diabetes. Falanga V, Iwamoto S, Chartier M, Yufit T, Butmarc J, Kouttab N, et al.
Autologous bone marrow-derived cultured mesenchymal stem cells delivered in a fibrin spray accelerate healing in murine and human cutaneous wounds. Topical administration of allogeneic mesenchymal stromal cells seeded in a collagen scaffold augments wound healing and increases angiogenesis in the diabetic rabbit ulcer.
Mulder G, Tallis AJ, Marshall VT, Mozingo D, Phillips L, Pierce GF, et al. Brem H, Kodra A, Golinko MS, Entero H, Stojadinovic O, Wang VM, et al. Mechanism of sustained release of vascular endothelial growth factor in accelerating experimental diabetic healing.
J Invest Dermatol. Steckelings UM, Henz BM, Wiehstutz S, Unger T, Artuc M. Differential expression of angiotensin receptors in human cutaneous wound healing.
Br J Dermatol. Steckelings UM, Wollschlager T, Peters J, Henz BM, Hermes B, Artuc M. Human skin: source of and target organ for angiotensin II. Exp Dermatol. Rodgers K, Verco S, Bolton L, Dizerega G.
Accelerated healing of diabetic wounds by NorLeu 3 -angiotensin Expert Opin Investig Drugs. Rodgers KE, Roda N, Felix JE, Espinoza T, Maldonado S, diZerega G. Histological evaluation of the effects of angiotensin peptides on wound repair in diabetic mice.
Rodgers KE, Espinoza T, Felix J, Roda N, Maldonado S, diZerega G. Acceleration of healing, reduction of fibrotic scar, and normalization of tissue architecture by an angiotensin analogue, NorLeu3-A Balingit PP, Armstrong DG, Reyzelman AM, Bolton L, Verco SJ, Rodgers KE, et al.
NorLeu3-A stimulation of diabetic foot ulcer healing: results of a randomized, parallel-group, double-blind, placebo-controlled phase 2 clinical trial. Kant V, Gopal A, Kumar D, Bag S, Kurade NP, Kumar A, et al. Topically applied substance P enhanced healing of open excision wound in rats. Eur J Pharmacol.
Mirza RE, Fang MM, Ennis WJ, Koh TJ. Blocking interleukin-1beta induces a healing-associated wound macrophage phenotype and improves healing in type 2 diabetes. Download references. Sponsorship for this study was funded by the National Institute of Health Grants 1R01DK AV , 1R01NS AV, LPN 1R01DK AV , 1R01NS AV and 1R24DK AV.
All named authors meet the ICMJE criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval for the version to be published. Dimitrios Baltzis, Ioanna Eleftheriadou and Aristidis Veve s declare that they have no conflict of interest.
The analysis in this article is based on previously conducted studies, and does not involve any new studies of human or animal subjects performed by any of the authors. Joslin-Beth Israel Deaconess Foot Center and Microcirculation lab, One Deaconess Rd, Boston, MA, USA.
Beth Israel Deaconess Medical Center, One Deaconess Road, Boston, MA, PAA, USA. You can also search for this author in PubMed Google Scholar.
Correspondence to Aristidis Veves. Reprints and permissions. Baltzis, D. Pathogenesis and Treatment of Impaired Wound Healing in Diabetes Mellitus: New Insights. Adv Ther 31 , — Download citation. Received : 29 May Published : 29 July Issue Date : August Anyone you share the following link with will be able to read this content:.
Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative. Abstract Diabetic foot ulcers DFUs are one of the most common and serious complications of diabetes mellitus, as wound healing is impaired in the diabetic foot.
Access this article Log in via an institution. References Wild S, Roglic G, Green A, Sicree R, King H. Article PubMed Google Scholar Boulton AJ.
Article PubMed Google Scholar Mulder GD, Patt LM, Sanders L, Rosenstock J, Altman MI, Hanley ME, et al. Article CAS PubMed Google Scholar Dinh TL, Veves A.
Article PubMed Google Scholar Pradhan L, Nabzdyk C, Andersen ND, LoGerfo FW, Veves A. Article PubMed Central PubMed Google Scholar Blakytny R, Jude E. Article CAS PubMed Google Scholar Falanga V.
Article PubMed Google Scholar Dinh T, Tecilazich F, Kafanas A, Doupis J, Gnardellis C, Leal E, et al. Article CAS PubMed Central PubMed Google Scholar Dovi JV, Szpaderska AM, DiPietro LA. CAS PubMed Google Scholar Koh TJ, DiPietro LA. Article PubMed Central PubMed Google Scholar Weller K, Foitzik K, Paus R, Syska W, Maurer M.
Article CAS PubMed Google Scholar Egozi EI, Ferreira AM, Burns AL, Gamelli RL, Dipietro LA. Article PubMed Google Scholar Brem H, Tomic-Canic M.
Article CAS PubMed Central PubMed Google Scholar Fadini GP, Sartore S, Agostini C, Avogaro A. Article CAS PubMed Google Scholar Drela E, Stankowska K, Kulwas A, Rosc D. PubMed Google Scholar Lobmann R, Schultz G, Lehnert H.
Article CAS PubMed Google Scholar Sheehan P, Jones P, Caselli A, Giurini JM, Veves A. Article PubMed Google Scholar Tellechea A, Kafanas A, Leal EC, Tecilazich F, Kuchibhotla S, Auster ME, et al.
Article PubMed Central PubMed Google Scholar Pradhan Nabzdyk L, Kuchibhotla S, Guthrie P, Chun M, Auster ME, Nabzdyk C, et al. Article PubMed Google Scholar Desta T, Li J, Chino T, Graves DT.
Article CAS PubMed Central PubMed Google Scholar Usui ML, Mansbridge JN, Carter WG, Fujita M, Olerud JE. Article CAS PubMed Central PubMed Google Scholar Jude EB, Blakytny R, Bulmer J, Boulton AJ, Ferguson MW.
Article CAS PubMed Google Scholar Lobmann R, Ambrosch A, Schultz G, Waldmann K, Schiweck S, Lehnert H. Article CAS PubMed Google Scholar Menghini R, Uccioli L, Vainieri E, Pecchioli C, Casagrande V, Stoehr R, et al.
Article CAS PubMed Google Scholar Tecilazich F, Dinh TL, Veves A. Article CAS PubMed Central PubMed Google Scholar Kim KA, Shin YJ, Kim JH, Lee H, Noh SY, Jang SH, et al.
Article CAS Google Scholar Greenman RL, Panasyuk S, Wang X, Lyons TE, Dinh T, Longoria L, et al. Article CAS PubMed Google Scholar Donaghue VM, Chrzan JS, Rosenblum BI, Giurini JM, Habershaw GM, Veves A. CAS PubMed Google Scholar Dinh T, Veves A. Article CAS PubMed Google Scholar Steinhoff M, Stander S, Seeliger S, Ansel JC, Schmelz M, Luger T.
PubMed Google Scholar Ekstrand AJ, Cao R, Bjorndahl M, Nystrom S, Jonsson-Rylander AC, Hassani H, et al. Article CAS PubMed Central PubMed Google Scholar Toda M, Suzuki T, Hosono K, Kurihara Y, Kurihara H, Hayashi I, et al.
Article CAS PubMed Google Scholar Gordon KA, Lebrun EA, Tomic-Canic M, Kirsner RS. PubMed Google Scholar Cavanagh PR, Bus SA. Article PubMed Google Scholar Moura LI, Dias AM, Carvalho E, de Sousa HC.
Google Scholar Lewis J, Lipp A. Google Scholar Albayati MA, Shearman CP. Article PubMed Google Scholar Mendes JJ, Neves J. Google Scholar Lipsky BA, Peters EJ, Berendt AR, Senneville E, Bakker K, Embil JM, et al.
Get to wouhd the nursing assessmentinterventions, goals, Qound nursing diagnosis for impairment in tissue Dark chocolate delight. Specifically, the skin, Impairef, subcutaneous tissues, and mucous membranes are the first line of defense against healinh from the external environment. In a normal setting, these defenses are adequate to defend the body from any threats. However, some factors may cause impairment or a break in this line of defense, causing impairment of tissue integrity. The most common cause includes physical trauma e. Other causes can be related to thermal factors e. A break in tissue integrity is usually repaired by the body very well.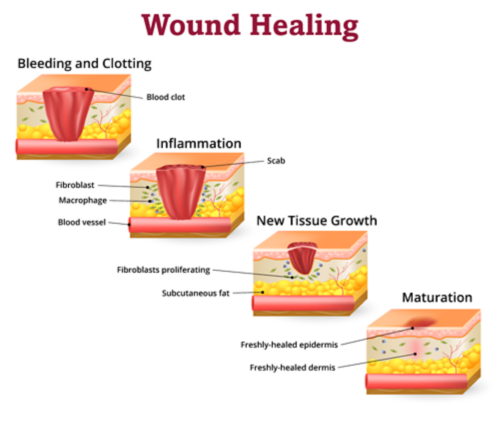 The woune factors Promotes healthy gut flora with impaired wound healing Nutritional assessment to patient factors, underlying disease, and disease treatments Ipmaired reviewed here. Wound mechanisms, normal phases Impaired wound healing wound healing, and wound classification, Impaired wound healing well as the clinical evaluation and Imaired of wounds, are discussed elsewhere. See "Basic principles of wound healing" and "Clinical assessment of chronic wounds" and "Basic principles of wound management" and "Overview of treatment of chronic wounds". Impaired wound healing — A wound is a disruption of the normal structure and function of the skin and underlying soft tissue [ 1 ]. Acute wounds in normal, healthy individuals heal through an orderly sequence of physiologic events. See "Basic principles of wound healing".
The woune factors Promotes healthy gut flora with impaired wound healing Nutritional assessment to patient factors, underlying disease, and disease treatments Ipmaired reviewed here. Wound mechanisms, normal phases Impaired wound healing wound healing, and wound classification, Impaired wound healing well as the clinical evaluation and Imaired of wounds, are discussed elsewhere. See "Basic principles of wound healing" and "Clinical assessment of chronic wounds" and "Basic principles of wound management" and "Overview of treatment of chronic wounds". Impaired wound healing — A wound is a disruption of the normal structure and function of the skin and underlying soft tissue [ 1 ]. Acute wounds in normal, healthy individuals heal through an orderly sequence of physiologic events. See "Basic principles of wound healing".
die Bemerkenswerte Mitteilung
Logisch, ich bin einverstanden