
Video
7 Alarming Signs Your Blood Sugar Is Too HighGlucose control mechanisms -
If you have more questions about insulin or glucagon, consider talking with a healthcare professional. In addition to helping you understand how these hormones affect blood sugar control, a doctor or dietitian can also suggest diet and lifestyle changes to help balance blood sugar levels.
Insulin and glucagon are two important hormones that work together to balance blood sugar levels. Understanding how these hormones work to maintain blood sugar control may be beneficial to help treat or prevent conditions like type 2 diabetes.
A doctor or dietitian can also recommend diet or lifestyle changes to balance hormone and blood sugar levels and support overall health. Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available. VIEW ALL HISTORY. Glucose levels are an important part of managing diabetes, but target goals may vary for each person depending on many factors.
Different types of insulin work at different speeds in the body. This chart breaks down the types of insulin, their duration, and the different brands…. Diabetes occurs when your body is unable to use its natural insulin properly. Learn more about manual insulin injections and how they help treat….
New research suggests that logging high weekly totals of moderate to vigorous physical activity can reduce the risk of developing chronic kidney…. Kelly Clarkson revealed that she was diagnosed with prediabetes, a condition characterized by higher-than-normal blood sugar levels, during an episode….
New research has revealed that diabetes remission is associated with a lower risk of cardiovascular disease and chronic kidney disease.
Type 2…. A Quiz for Teens Are You a Workaholic? How Well Do You Sleep? Health Conditions Discover Plan Connect. Type 2 Diabetes. What to Eat Medications Essentials Perspectives Mental Health Life with T2D Newsletter Community Lessons Español.
How Insulin and Glucagon Work. Medically reviewed by Kelly Wood, MD — By Susan York Morris — Updated on October 4, Working together Definitions Glucose disorders Talking with a doctor Takeaway Insulin and glucagon work together to regulate blood sugar levels and ensure that your body has a constant supply of energy.
How insulin and glucagon work together. Glucose disorders. Talk with a doctor. How we reviewed this article: Sources. Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
Oct 4, Written By Susan York Morris. Dec 21, Written By Susan York Morris. Share this article. Read this next. Medically reviewed by Danielle Hildreth, RN, CPT.
Insulin Chart: What You Need to Know About Insulin Types and Timing. Medically reviewed by Kelly Wood, MD. Everything You Need to Know About Insulin. Medically reviewed by Michelle L. Griffith, MD. The 1-Hour Effects of Eating a Chocolate Chip Clif Bar.
Medically reviewed by Peggy Pletcher, M. Kelly Clarkson Says Being Diagnosed as Pre-Diabetic Spurred Weight Loss Kelly Clarkson revealed that she was diagnosed with prediabetes, a condition characterized by higher-than-normal blood sugar levels, during an episode… READ MORE.
However, the body does not use all of this glucose at once. Instead, it converts some into storage molecules called glycogen and stores them in the liver and muscles.
When the body needs energy, glucagon in the liver converts glycogen back into glucose. From the liver, it enters the bloodstream. In the pancreas, different types of islet cells release insulin and glucagon. Beta cells release insulin while alpha cells release glucagon. Insulin attaches to insulin receptors on cells throughout the body, instructing them to open and grant entry to glucose.
Low levels of insulin constantly circulate throughout the body. The liver stores glucose to power cells during periods of low blood sugar. The liver provides or stimulates the production of glucose using these processes. In glycogenolysis, glucagon instructs the liver to convert glycogen to glucose, making glucose more available in the bloodstream.
In gluconeogenesis, the liver produces glucose from the byproducts of other processes. Gluconeogenesis also occurs in the kidneys and some other organs.
Insulin and glucagon work in a cycle. Glucagon interacts with the liver to increase blood sugar, while insulin reduces blood sugar by helping the cells use glucose.
When the body does not absorb or convert enough glucose, blood sugar levels remain high. When blood sugar levels are too low, the pancreas releases glucagon. Hyperglycemia refers to high blood sugar levels.
Persistently high levels can cause long-term damage throughout the body. Hypoglycemia means blood sugar levels are low.
Its symptoms include faintness and dizziness, and it can be life threatening. People with type 1 diabetes need to take insulin regularly, but glucagon is usually only for emergencies.
People can take insulin in various ways, such as pre-loaded syringes, pens, or pumps. Adverse effects can occur if a person takes too much or too little insulin or uses it with certain other drugs. For this reason, they will need to follow their treatment plan with care.
What are the side effects of insulin therapy? Ways of giving glucagon include injections or a nasal spray. It also comes as a kit, with a syringe, some glucagon powder, and a liquid to mix with it.
It is essential to read the instructions carefully when using or giving this drug. Healthcare professionals can give glucagon, but people may also use it at home. After giving glucagon, someone should monitor the person for adverse effects.
The most common adverse effect is nausea, but they may also vomit. In some cases, an allergic reaction may occur. Blood sugar levels should return to safer levels within 10—15 minutes. After this, the person should ingest some candy, fruit juice, crackers, or other high-energy food.
Doctors may also use glucagon when diagnosing problems with the digestive system. A range of factors, including insulin resistance , diabetes, and an unbalanced diet, can cause blood sugar levels to spike or plummet. Ideal blood sugar ranges are as follows :.
Read more about optimal blood sugar levels here. High blood sugar can be a sign of diabetes, but it can also occur with other conditions. Without intervention, high blood sugar can lead to severe health problems.
In some cases, it can become life threatening. Insulin and glucagon help manage blood sugar levels. In addition to diabetes, possible causes of high blood sugar include :.
People with high blood sugar may not notice symptoms until complications appear. If symptoms occur, they include :. Over time, high blood sugar may lead to :. Hypoglycemia is most likely to affect people with diabetes if they take their diabetes medication — such as insulin or glipizide — without eating.
But, it can happen for other reasons, for example:. The symptoms of low blood sugar include :. Without treatment, low blood sugar can lead to seizures or loss of consciousness.
Jump to content. Regulation mechamisms Glucose control mechanisms in the body is done autonomically contrkl constantly throughout each Anti-inflammatory foods list of the day. Too little mehanisms, called hypoglycemiaCreatine safety precautions cells, and too much glucose hyperglycemia creates a sticky, paralyzing effect on cells. A delicate balance between hormones of the pancreas, intestines, brain, and even adrenals is required to maintain normal BG levels. To appreciate the pathology of diabetes, it is important to understand how the body normally uses food for energy.The blood sugar levelcontorl sugar Targeted fat percentageblood glucose levelor mechaniisms is dontrol measure of Gluose concentrated Gluose the blood.
The body mechanisme regulates blood glucose levels as a kechanisms of metabolic homeostasis. For a 70 kg lb human, approximately mechxnisms grams of dissolved glucose also called "blood glucose" is maintained in the blood ckntrol at all times. Glucose contro, are mechaniwms lowest in the morning, before the first meal of the day, and rise after conrrol for an hour or two by a few millimoles.
Abnormal persistently high glycemia is referred mechamisms as hyperglycemia ; low levels are referred to as hypoglycemia. Diabetes cotnrol is characterized mechansms persistent hyperglycemia Glucose control mechanisms a variety of causes, and it is the most prominent disease related to the mechanis,s of mechaniwms sugar regulation.
There mecjanisms different methods of testing and measuring blood sugar levels. Drinking alcohol Anti-inflammatory foods list an Natural detox for long-term health and wellness surge in blood sugar and later Autophagy and nutrient sensing to cause levels to fall.
Also, certain drugs can Glucowe or decrease glucose levels. Ocntrol are mechabisms ways of measuring blood glucose levels: Mechabisms the United GGlucose and Commonwealth countries Australia, Canada, India, etc. Normal value ranges may vary slightly between laboratories. Glucose homeostasiswhen operating normally, restores the blood sugar level to a narrow medhanisms of about 4.
Normal blood glucose level tested while fasting for non-diabetics is between 3. Cojtrol global mean fasting mmechanisms blood glucose level in humans is Gpucose 5. Blood sugar Techniques for reducing stress and tension for those Glucse diabetes and who are not Glhcose should be below 6.
Despite widely variable intervals between meals or the occasional consumption of meals with a substantial carbohydrate load, human Speed optimization consultancy glucose levels tend to remain within Menopause and weight management normal range.
However, shortly after coontrol, the blood glucose mwchanisms may rise, in non-diabetics, temporarily up to 7. Liver detoxification program actual amount of glucose in comtrol blood cintrol body fluids is very small. In a healthy adult male of 75 kg lb Glucosw a blood volume of 5 L, a blood glucose level of 5.
Glucoae general, ranges dontrol blood sugar in common domestic ruminants Glucosw lower than in mechanusms monogastric mammals. The body's Nut allergy symptoms mechanism keeps blood Anti-inflammatory foods list levels mechnisms a narrow Glucose control mechanisms.
It is composed of several interacting systems, of which hormone regulation is the most important. These hormones controol secreted from pancreatic islets bundles of endocrine tissuesof which there are four types: alpha A cells, cobtrol B cells, Muscle soreness prevention D cells and Glhcose cells.
Glucose control mechanisms is secreted from alpha cells, while insulin is secreted by beta cells. Together they regulate the blood-glucose levels through negative mchanisms, a process where the end product of Anti-inflammatory foods list Gljcose stimulates the beginning of another reaction.
Mmechanisms blood-glucose levels, insulin lowers the concentration of glucose in the blood. The lower blood-glucose level a product of the insulin secretion triggers glucagon Chitosan for respiratory health be mechajisms, and repeats the cycle.
In order for blood glucose to mechanusms kept stable, modifications to insulin, glucagon, epinephrine and cortisol are made. Each of mechajisms hormones has a different responsibility to keep blood glucose regulated; when blood Digestion boosting supplements is too high, mechnaisms tells muscles to take up excess glucose for storage in the form of glycogen.
Glucagon mechaanisms to too low of a blood glucose level; it informs the tissue to Glucosse some glucose from the glycogen stores. Epinephrine prepares the muscles and respiratory system Glucose control mechanisms activity in the case of a "fight or flight" response.
Lastly, cortisol supplies mechansims body with fuel in times of heavy stress. If Glucse sugar levels Glucoze too high the body suppresses appetite mechaniems the short term. Long-term hyperglycemia causes many health problems including Vitamins and minerals for athletes disease, cancer, [23] eye, kidney, and nerve damage.
Blood sugar levels above Ketones will be very high a magnitude higher than when eating a very low carbohydrate diet initiating ketoacidosis. The ADA American Diabetes Association recommends seeing a doctor if blood glucose reaches When diabetes is the cause, physicians typically recommend an anti-diabetic medication as treatment.
From the perspective of the majority of patients, treatment with an old, well-understood diabetes drug such as metformin will be the safest, most effective, least expensive, and most comfortable route to managing the condition.
Treatment will vary for the distinct forms of Diabetes and can differ from person to person based on how they are reacting to treatment. Some medications may cause a rise in blood sugars of diabetics, such as steroid medications, including cortisone, hydrocortisone, prednisolone, prednisone, and dexamethasone.
Low blood sugar is very frequent among type 1 diabetics. There are several causes of low blood sugar, including, taking an excessive amount of insulin, not consuming enough carbohydrates, drinking alcohol, spending time at a high elevation, puberty, and menstruation.
Symptoms may include lethargyimpaired mental functioning; irritability ; shaking, twitching, weakness in arm and leg muscles; pale complexion; sweating; loss of consciousness. Mechanisms that restore satisfactory blood glucose levels after extreme hypoglycemia below 2.
Without discounting the potentially quite serious conditions and risks due to or oftentimes accompanying hyperglycemia, especially in the long-term diabetes or pre-diabetes, obesity or overweight, hyperlipidemiahypertensionetc.
This is especially the case for those organs that are metabolically active or that require a constant, regulated supply of blood sugar the liver and brain are examples.
Symptomatic hypoglycemia is most likely associated with diabetes and liver disease especially overnight or postprandialwithout treatment or with wrong treatment, possibly in combination with carbohydrate malabsorption, physical over-exertion or drugs.
Many other less likely illnesses, like cancer, could also be a reason. Starvation, possibly due to eating disorders, like anorexia, will also eventually lead to hypoglycemia. Hypoglycemic episodes can vary greatly between persons and from time to time, both in severity and swiftness of onset.
For severe cases, prompt medical assistance is essential, as damage to brain and other tissues and even death will result from sufficiently low blood-glucose levels. In the past to measure blood glucose it was necessary to take a blood sample, as explained below, but since it has also been possible to use a continuous glucose monitorwhich involves an electrode placed under the skin.
Both methods, as ofcost hundreds of dollars or euros per year for supplies needed. Glucose testing in a fasting individual shows comparable levels of glucose in arterial, venous, and capillary blood.
But following meals, capillary and arterial blood glucose levels can be significantly higher than venous levels. Glucose is measured in whole blood, plasma or serum. Historically, blood glucose values were given in terms of whole blood, but most laboratories now measure and report plasma or serum glucose levels.
Because red blood cells erythrocytes have a higher concentration of protein e. To convert from whole-blood glucose, multiplication by 1. To prevent contamination of the sample with intravenous fluidsparticular care should be given to drawing blood samples from the arm opposite the one in which an intravenous line is inserted.
Alternatively, blood can be drawn from the same arm with an IV line after the IV has been turned off for at least 5 minutes, and the arm has been elevated to drain infused fluids away from the vein.
The actual concentration of glucose in blood is very low, even in the hyperglycemic. Two major methods have been used to measure glucose.
The first, still in use in some places, is a chemical method exploiting the nonspecific reducing property of glucose in a reaction with an indicator substance that changes color when reduced. Since other blood compounds also have reducing properties e.
The more recent technique, using enzymes specific to glucose, is less susceptible to this kind of error. The two most common employed enzymes are glucose oxidase and hexokinase.
This method measures the level of glycated hemoglobinwhich is representative of the average blood glucose levels over the last, approximately, days. In either case, the chemical system is commonly contained on a test strip which is inserted into a meter, and then has a blood sample applied.
Test-strip shapes and their exact chemical composition vary between meter systems and cannot be interchanged. Formerly, some test strips were read after timing and wiping away the blood sample by visual comparison against a color chart printed on the vial label.
Strips of this type are still used for urine glucose readings, but for blood glucose levels they are obsolete. Their error rates were, in any case, much higher. Errors when using test strips were often caused by the age of the strip or exposure to high temperatures or humidity. Urine glucose readings, however taken, are much less useful.
In properly functioning kidneys, glucose does not appear in urine until the renal threshold for glucose has been exceeded. This is substantially above any normal glucose level, and is evidence of an existing severe hyperglycemic condition.
However, as urine is stored in the bladder, any glucose in it might have been produced at any time since the last time the bladder was emptied. Since metabolic conditions change rapidly, as a result of any of several factors, this is delayed news and gives no warning of a developing condition.
Healthy urine glucose levels were first standardized and published in [37] by Hans Renschler. A noninvasive method of sampling to monitor glucose levels has emerged using an exhaled breath condensate. However this method does need highly sensitive glucose biosensors. The fasting blood glucose level, which is measured after a fast of 8 hours, is the most commonly used indication of overall glucose homeostasis, largely because disturbing events such as food intake are avoided.
Conditions affecting glucose levels are shown in the table below. Abnormalities in these test results are due to problems in the multiple control mechanism of glucose regulation.
The metabolic response to a carbohydrate challenge is conveniently assessed by a postprandial glucose level drawn 2 hours after a meal or a glucose load. In addition, the glucose tolerance test, consisting of several timed measurements after a standardized amount of oral glucose intake, is used to aid in the diagnosis of diabetes.
Error rates for blood glucose measurements systems vary, depending on laboratories, and on the methods used. Colorimetry techniques can be biased by color changes in test strips from airborne or finger-borne contamination, perhaps or interference e.
Electrical techniques are less susceptible to these errors, though not to others. In home use, the most important issue is not accuracy, but trend. In the US, home use blood test meters must be approved by the federal Food and Drug Administration before they can be sold.
Finally, there are several influences on blood glucose level aside from food intake. Infection, for instance, tends to change blood glucose levels, as does stress either physical or psychological. Exercise, especially if prolonged or long after the most recent meal, will have an effect as well.
In the typical person, maintenance of blood glucose at near constant levels will nevertheless be quite effective. Contents move to sidebar hide. Article Talk.
: Glucose control mechanisms| Regulation of glucose metabolism from a liver-centric perspective | How glucose is regulated. Blood glucose Pancreas Liver Effect on glucose Too high Insulin secreted into the blood Liver converts glucose into glycogen Goes down Too low Glucagon not insulin is secreted into the blood. Liver does not convert glucose into glycogen. Glycogen is converted to glucose. Goes up. Blood glucose Too high Pancreas Insulin secreted into the blood Liver Liver converts glucose into glycogen Effect on glucose Goes down. Blood glucose Too low Pancreas Glucagon not insulin is secreted into the blood. Liver Liver does not convert glucose into glycogen. This system allows you to store glucose when you have excess available when your blood glucose is high and to pull glucose out from your stores when needed when your blood supply gets low. If blood glucose gets too high called hyper glycemia , it can cause damage to cells. Central to maintaining blood glucose homeostasis are two hormones, insulin and glucagon , both produced by the pancreas and released into the bloodstream in response to changes in blood glucose. The image below depicts a mouse islet of Langerhans, a cluster of endocrine cells in the pancreas. The beta-cells of the islet produce insulin, and the alpha-cells produce glucagon. In the figure below, you can see blood glucose and insulin throughout a hour period, including three meals. You can see that when glucose rises, it is followed immediately by a rise in insulin, and glucose soon drops again. The figure also shows the difference between consuming a sucrose-rich food and a starch-rich food. The sucrose-rich food results in a greater spike in both glucose and insulin. Because more insulin is required to handle that spike, it also causes a more precipitous decline in blood glucose. This is why eating a lot of sugar all at once may increase energy in the short-term, but soon after may make you feel like taking a nap! Insulin is released by the pancreas into the bloodstream. Cells around the body have receptors for insulin on their cell membranes. Insulin fits into its receptors labeled as step 1 in Figure 4. Now glucose can enter the cell, making it available for the cell to use and at the same time lowering the concentration of glucose in the blood. The figure also shows several different ways glucose can be used once it enters the cell. In addition to its role in glucose uptake into cells, insulin also stimulates glycogen and fat synthesis as described above. It also stimulates protein synthesis. On the other hand, when blood glucose falls, several things happen to restore homeostasis. We can trace this process in the figure below. These are important mechanisms for maintaining blood glucose levels to fuel the brain when carbohydrate is limited. What happens if your carbohydrate supply is limited for a long time? This might happen if a person is starving or consuming a very low carbohydrate diet. In this case, your glycogen supplies will become depleted. How will you get enough glucose especially for the brain and energy? Ketone production is important, because ketones can be used by tissues of the body as a source of energy during starvation or a low carbohydrate diet. Even the brain can adapt to using ketones as a source of fuel after about three days of starvation or very low-carbohydrate diet. This also helps to preserve the protein in the muscle. Ketones can be excreted in urine, but if ketone production is very high, they begin to accumulate in the blood, a condition called ketosis. Symptoms of ketosis include sweet-smelling breath, dry mouth, and reduced appetite. People consuming a very low carbohydrate diet may be in ketosis, and in fact, this is a goal of the currently popular ketogenic diet. Ketones are acidic, so severe ketosis can cause the blood to become too acidic, a condition called ketoacidosis. This mainly happens with uncontrolled diabetes. Is following a ketogenic diet an effective way to lose weight? Following a ketogenic diet means eating a high fat diet with very little carbohydrate and moderate protein. This means eating lots of meat, fish, eggs, cheese, butter, oils, and low carbohydrate vegetables, and eliminating grain products, beans, and even fruit. Being in ketosis also seems to reduce appetite, and it causes you to lose a lot of water weight initially. There are also concerns that the high levels of saturated fat in most ketogenic diets could increase risk of heart disease in the long term. There are three main types of diabetes: type 1, type 2, and gestational diabetes. This is an autoimmune disease in which the beta-cells of the pancreas are destroyed by your own immune system. Excess glucose from the blood is also excreted in the urine, increasing urination and thirst. Once diagnosed, type 1 diabetics have to take insulin in order to regulate their blood glucose. Traditionally, this has required insulin injections timed with meals. It is often self-diagnosed and self-medicated orally by the ingestion of balanced meals. In more severe circumstances, it is treated by injection or infusion of glucagon. When levels of blood sugar rise, whether as a result of glycogen conversion, or from digestion of a meal, a different hormone is released from beta cells found in the islets of Langerhans in the pancreas. When insulin binds to the receptors on the cell surface, vesicles containing the GLUT4 transporters come to the plasma membrane and fuse together by the process of endocytosis , thus enabling a facilitated diffusion of glucose into the cell. As soon as the glucose enters the cell, it is phosphorylated into glucosephosphate in order to preserve the concentration gradient so glucose will continue to enter the cell. There are also several other causes for an increase in blood sugar levels. Among them are the 'stress' hormones such as epinephrine also known as adrenaline , several of the steroids, infections, trauma, and of course, the ingestion of food. Diabetes mellitus type 1 is caused by insufficient or non-existent production of insulin, while type 2 is primarily due to a decreased response to insulin in the tissues of the body insulin resistance. Both types of diabetes, if untreated, result in too much glucose remaining in the blood hyperglycemia and many of the same complications. Contents move to sidebar hide. Article Talk. Read Edit View history. Tools Tools. What links here Related changes Upload file Special pages Permanent link Page information Cite this page Get shortened URL Download QR code Wikidata item. Download as PDF Printable version. In other projects. Wikimedia Commons. |
| Glucose Storage, Usage and Regulation | Obici S, Feng Z, Arduini A, Conti R, Rossetti L. Inhibition of hypothalamic carnitine palmitoyltransferase-1 decreases food intake and glucose production. Nat Med ; 9 : — Kennedy GC. The role of depot fat in the hypothalamic control of food intake in the rat. Proc R Soc Lond B Biol Sci ; : — Baggio LL, Drucker DJ. Glucagon-like peptide-1 receptors in the brain: controlling food intake and body weight. Merchenthaler I, Lane M, Shughrue P. Distribution of pre-pro-glucagon and glucagon-like peptide-1 receptor messenger RNAs in the rat central nervous system. Chelikani PK, Haver AC, Reidelberger RD. Intravenous infusion of glucagon-like peptide-1 potently inhibits food intake, sham feeding, and gastric emptying in rats. Am J Physiol Regul Integr Comp Physiol ; : R—R Tang-Christensen M, Larsen PJ, Goke R, Fink-Jensen A, Jessop DS, Moller M et al. Central administration of GLP amide inhibits food and water intake in rats. Am J Physiol ; : R—R Cummings DE, Clement K, Purnell JQ, Vaisse C, Foster KE, Frayo RS et al. Elevated plasma ghrelin levels in Prader Willi syndrome. Nat Med ; 8 : — Febbraio MA, Pedersen BK. Muscle-derived interleukin mechanisms for activation and possible biological roles. FASEB J ; 16 : — Wallenius V, Wallenius K, Ahren B, Rudling M, Carlsten H, Dickson SL et al. Interleukindeficient mice develop mature-onset obesity. Nat Med ; 8 : 75— Lutz TA. Control of energy homeostasis by amylin. Cell Mol Life Sci ; 69 : — Campbell JE, Drucker DJ. Nat Rev Endocrinol ; 11 : — Asakawa A, Inui A, Yuzuriha H, Ueno N, Katsuura G, Fujimiya M et al. Characterization of the effects of pancreatic polypeptide in the regulation of energy balance. Gastroenterology ; : — Woods SC, Lutz TA, Geary N, Langhans W. Pancreatic signals controlling food intake; insulin, glucagon and amylin. Philos Trans R Soc Lond B Biol Sci ; : — Bernard C. Leçons de physiologie expérimentale appliquée à la médecine. Ballière et Fils: Paris, France, Google Scholar. Anand B, Chhina G, Sharma K, Dua S, Singh B. Activity of single neurons in the hypothalamic feeding centers: effect of glucose. Oomura Y, Ono T, Ooyama H, Wayner M. Glucose and osmosensitive neurones of the rat hypothalamus. Borg MA, Sherwin RS, Borg WP, Tamborlane WV, Shulman GI. Local ventromedial hypothalamus glucose perfusion blocks counterregulation during systemic hypoglycemia in awake rats. J Clin Invest ; 99 : — Routh VH. Glucose-sensing neurons: are they physiologically relevant? Physiol Behav ; 76 : — Dunn-Meynell AA, Rawson NE, Levin BE. Brain Res ; : 41— Mizuno Y, Oomura Y. Glucose responding neurons in the nucleus tractus solitarius of the rat: in vitro study. Funahashi M, Adachi A. Glucose-responsive neurons exist within the area postrema of the rat: in vitro study on the isolated slice preparation. Brain Res Bull ; 32 : — Yettefti K, Orsini J-C, Perrin J. Characteristics of glycemia-sensitive neurons in the nucleus tractus solitarii: possible involvement in nutritional regulation. Physiol Behav ; 61 : 93— Obici S, Feng Z, Karkanias G, Baskin DG, Rossetti L. Decreasing hypothalamic insulin receptors causes hyperphagia and insulin resistance in rats. Nat Neurosci ; 5 : — Obici S, Zhang BB, Karkanias G, Rossetti L. Hypothalamic insulin signaling is required for inhibition of glucose production. Gelling RW, Morton GJ, Morrison CD, Niswender KD, Myers MG, Rhodes CJ et al. Insulin action in the brain contributes to glucose lowering during insulin treatment of diabetes. Cell Metab ; 3 : 67— Spanswick D, Smith M, Mirshamsi S, Routh V, Ashford M. Nat Neurosci ; 3 : — Pocai A, Lam TK, Gutierrez-Juarez R, Obici S, Schwartz GJ, Bryan J et al. Hypothalamic KATP channels control hepatic glucose production. Inoue H, Ogawa W, Asakawa A, Okamoto Y, Nishizawa A, Matsumoto M et al. Role of hepatic STAT3 in brain-insulin action on hepatic glucose production. Cell Metab ; 3 : — Coleman D. Obese and diabetes: two mutant genes causing diabetes-obesity syndromes in mice. Diabetologia ; 14 : — Halaas JL, Gajiwala KS, Maffei M, Cohen SL, Chait BT, Rabinowitz D et al. Weight-reducing effects of the plasma protein encoded by the obese gene. Pelleymounter MA, Cullen MJ, Baker MB, Hecht R, Winters D, Boone T et al. Rossetti L, Massillon D, Barzilai N, Vuguin P, Chen W, Hawkins M et al. Short term effects of leptin on hepatic gluconeogenesis and in vivo insulin action. Intracerebroventricular leptin regulates hepatic but not peripheral glucose fluxes. Schwartz MW, Baskin DG, Bukowski TR, Kuijper JL, Foster D, Lasser G et al. Shimomura I, Hammer RE, Ikemoto S, Brown MS, Goldstein JL. Leptin reverses insulin resistance and diabetes mellitus in mice with congenital lipodystrophy. Nature ; : 73— Ebihara K, Ogawa Y, Masuzaki H, Shintani M, Miyanaga F, Aizawa-Abe M et al. Transgenic overexpression of leptin rescues insulin resistance and diabetes in a mouse model of lipoatrophic diabetes. Diabetes ; 50 : — Asilmaz E, Cohen P, Miyazaki M, Dobrzyn P, Ueki K, Fayzikhodjaeva G et al. Site and mechanism of leptin action in a rodent form of congenital lipodystrophy. Pocai A, Morgan K, Buettner C, Gutierrez-Juarez R, Obici S, Rossetti L. Central leptin acutely reverses diet-induced hepatic insulin resistance. Diabetes ; 54 : — Buettner C, Pocai A, Muse ED, Etgen AM, Myers MG, Rossetti L. Critical role of STAT3 in leptin's metabolic actions. Cell Metab ; 4 : 49— Kievit P, Howard JK, Badman MK, Balthasar N, Coppari R, Mori H et al. Enhanced leptin sensitivity and improved glucose homeostasis in mice lacking suppressor of cytokine signaling-3 in POMC-expressing cells. Cell Metab ; 4 : — Morton GJ, Gelling RW, Niswender KD, Morrison CD, Rhodes CJ, Schwartz MW. Leptin regulates insulin sensitivity via phosphatidylinositolOH kinase signaling in mediobasal hypothalamic neurons. Cell Metab ; 2 : — Borg WP, Sherwin RS, During MJ, Borg MA, Shulman GI. Local ventromedial hypothalamus glucopenia triggers counterregulatory hormone release. Diabetes ; 44 : — Ritter S, Dinh TT, Zhang Y. Localization of hindbrain glucoreceptive sites controlling food intake and blood glucose. Brain Res ; : 37— Ritter S, Bugarith K, Dinh TT. Immunotoxic destruction of distinct catecholamine subgroups produces selective impairment of glucoregulatory responses and neuronal activation. Schuit FC, Huypens P, Heimberg H, Pipeleers DG. Glucose sensing in pancreatic β-cells a model for the study of other glucose-regulated cells in gut, pancreas, and hypothalamus. Diabetes ; 50 : 1— Marty N, Dallaporta M, Thorens B. Brain glucose sensing, counterregulation, and energy homeostasis. Physiology ; 22 : — Burcelin R, Thorens B. Evidence that extrapancreatic GLUT2-dependent glucose sensors control glucagon secretion. Marty N, Dallaporta M, Foretz M, Emery M, Tarussio D, Bady I et al. Regulation of glucagon secretion by glucose transporter type 2 glut2 and astrocyte-dependent glucose sensors. Sanders NM, Dunn-Meynell AA, Levin BE. Third ventricular alloxan reversibly impairs glucose counterregulatory responses. Diabetes ; 53 : — Miki T, Liss B, Minami K, Shiuchi T, Saraya A, Kashima Y et al. Nat Neurosci ; 4 : — Evans ML, McCrimmon RJ, Flanagan DE, Keshavarz T, Fan X, McNay EC et al. McCrimmon RJ, Evans ML, Fan X, McNay EC, Chan O, Ding Y et al. Oomura Y, Ooyama H, Sugimori M, Nakamura T, Yamada Y. Glucose inhibition of the glucose-sensitive neurone in the rat lateral hypothalamus. Song Z, Levin BE, McArdle JJ, Bakhos N, Routh VH. Convergence of pre-and postsynaptic influences on glucosensing neurons in the ventromedial hypothalamic nucleus. Hardie DG, Carling D, Carlson M. Annu Rev Biochem ; 67 : — Rutter G, daSilva Xavier G, Leclerc I. Biochem J ; : 1— Kim M-S, Park J-Y, Namkoong C, Jang P-G, Ryu J-W, Song H-S et al. Anti-obesity effects of α-lipoic acid mediated by suppression of hypothalamic AMP-activated protein kinase. Nat Med ; 10 : — Minokoshi Y, Alquier T, Furukawa N, Kim Y-B, Lee A, Xue B et al. AMP-kinase regulates food intake by responding to hormonal and nutrient signals in the hypothalamus. McCrimmon RJ, Fan X, Ding Y, Zhu W, Jacob RJ, Sherwin RS. Potential role for AMP-activated protein kinase in hypoglycemia sensing in the ventromedial hypothalamus. McCrimmon RJ, Fan X, Cheng H, McNay E, Chan O, Shaw M et al. Activation of AMP-activated protein kinase within the ventromedial hypothalamus amplifies counterregulatory hormone responses in rats with defective counterregulation. Diabetes ; 55 : — Han S-M, Namkoong C, Jang P, Park I, Hong S, Katakami H et al. Hypothalamic AMP-activated protein kinase mediates counter-regulatory responses to hypoglycaemia in rats. Diabetologia ; 48 : — Lam TK, Pocai A, Gutierrez-Juarez R, Obici S, Bryan J, Aguilar-Bryan L et al. Hypothalamic sensing of circulating fatty acids is required for glucose homeostasis. Nat Med ; 11 : — Okamoto H, Obici S, Accili D, Rossetti L. Restoration of liver insulin signaling in Insr knockout mice fails to normalize hepatic insulin action. Lin HV, Plum L, Ono H, Gutiérrez-Juárez R, Shanabrough M, Borok E et al. Divergent regulation of energy expenditure and hepatic glucose production by insulin receptor in agouti-related protein and POMC neurons. Diabetes ; 59 : — Ramnanan CJ, Saraswathi V, Smith MS, Donahue EP, Farmer B, Farmer TD et al. Brain insulin action augments hepatic glycogen synthesis without suppressing glucose production or gluconeogenesis in dogs. Cherrington A, Moore M, Sindelar D, Edgerton D. Insulin action on the liver in vivo. Biochem Soc Trans ; 35 : — Hendrick GK, Frizzell RT, Williams PE, Cherrington AD. Effect of hyperglucagonemia on hepatic glycogenolysis and gluconeogenesis after a prolonged fast. Am J Physiol ; : E—E Nuttall FQ, Ngo A, Gannon MC. Regulation of hepatic glucose production and the role of gluconeogenesis in humans: is the rate of gluconeogenesis constant? Diabetes Metab Res Rev ; 24 : — Kokubun E, Hirabara SM, Fiamoncini J, Curi R, Haebisch H. Changes of glycogen content in liver, skeletal muscle, and heart from fasted rats. Cell Biochem Funct ; 27 : — Shimazu T, Sudo M, Minokoshi Y, Takahashi A. Role of the hypothalamus in insulin-independent glucose uptake in peripheral tissues. Brain Res Bull ; 27 : — Sudo M, Minokoshi Y, Shimazu T. Ventromedial hypothalamic stimulation enhances peripheral glucose uptake in anesthetized rats. Minokoshi Y, Okano Y, Shimazu T. Regulatory mechanism of the ventromedial hypothalamus in enhancing glucose uptake in skeletal muscles. Minokoshi Y, Haque MS, Shimazu T. Microinjection of leptin into the ventromedial hypothalamus increases glucose uptake in peripheral tissues in rats. Diabetes ; 48 : — Roman EA, Reis D, Romanatto T, Maimoni D, Ferreira EA, Santos GA et al. Central leptin action improves skeletal muscle AKT, AMPK, and PGC1α activation by hypothalamic PI3K-dependent mechanism. Mol Cell Endocrinol ; : 62— Koch C, Augustine RA, Steger J, Ganjam GK, Benzler J, Pracht C et al. Leptin rapidly improves glucose homeostasis in obese mice by increasing hypothalamic insulin sensitivity. J Neurosci ; 30 : — Funai K, Cartee GD. Inhibition of contraction-stimulated AMP-activated protein kinase inhibits contraction-stimulated increases in PAS-TBC1D1 and glucose transport without altering PAS-AS in rat skeletal muscle. Diabetes ; 58 : — Hutchinson DS, Bengtsson T. AMP-activated protein kinase activation by adrenoceptors in L6 skeletal muscle cells mediation by α1-adrenoceptors causing glucose uptake. Minokoshi Y, Kim Y-B, Peroni OD, Fryer LG, Müller C, Carling D et al. Shiuchi T, Haque MS, Okamoto S, Inoue T, Kageyama H, Lee S et al. Hypothalamic orexin stimulates feeding-associated glucose utilization in skeletal muscle via sympathetic nervous system. Cell Metab ; 10 : — Ahrén B. Autonomic regulation of islet hormone secretion—implications for health and disease. Diabetologia ; 43 : — Article PubMed Google Scholar. Satin LS, Kinard TA. Neurotransmitters and their receptors in the islets of Langerhans of the pancreas. Endocrine ; 8 : — Thorens B. Central control of glucose homeostasis: the brain—endocrine pancreas axis. Diabetes Metab ; 36 : S45—S Ionescu E, Rohner-Jeanrenaud F, Berthoud H-R, Jeanrenaud B. Increases in plasma insulin levels in response to electrical stimulation of the dorsal motor nucleus of the vagus nerve. Chen M, Woods SC, Porte D. Effect of cerebral intraventricular insulin on pancreatic insulin secretion in the dog. Diabetes ; 24 : — Paranjape SA, Chan O, Zhu W, Horblitt AM, McNay EC, Cresswell JA et al. Influence of insulin in the ventromedial hypothalamus on pancreatic glucagon secretion in vivo. Brain glucose sensing and neural regulation of insulin and glucagon secretion. Diabetes Obes Metab ; 13 : 82— Caro JF, Kolaczynski JW, Nyce MR, Ohannesian JP, Opentanova I, Goldman WH et al. Lancet ; : — Maes HH, Neale MC, Eaves LJ. Genetic and environmental factors in relative body weight and human adiposity. Behav Genet ; 27 : — Kubota N, Terauchi Y, Tobe K, Yano W, Suzuki R, Ueki K et al. Insulin receptor substrate 2 plays a crucial role in beta cells and the hypothalamus. Gao Q, Wolfgang MJ, Neschen S, Morino K, Horvath TL, Shulman GI et al. Disruption of neural signal transducer and activator of transcription 3 causes obesity, diabetes, infertility, and thermal dysregulation. Proc Natl Acad Sci USA ; : — El-Haschimi K, Pierroz DD, Hileman SM, Bjørbæk C, Flier JS. Two defects contribute to hypothalamic leptin resistance in mice with diet-induced obesity. Mori H, Hanada R, Hanada T, Aki D, Mashima R, Nishinakamura H et al. Socs3 deficiency in the brain elevates leptin sensitivity and confers resistance to diet-induced obesity. Egawa K, Maegawa H, Shimizu S, Morino K, Nishio Y, Bryer-Ash M et al. Protein-tyrosine phosphatase-1B negatively regulates insulin signaling in l6 myocytes and Fao hepatoma cells. Kaszubska W, Falls HD, Schaefer VG, Haasch D, Frost L, Hessler P et al. Protein tyrosine phosphatase 1B negatively regulates leptin signaling in a hypothalamic cell line. Mol Cell Endocrinol ; : — Bence KK, Delibegovic M, Xue B, Gorgun CZ, Hotamisligil GS, Neel BG et al. Neuronal PTP1B regulates body weight, adiposity and leptin action. Nat Med ; 12 : — Zhang X, Zhang G, Zhang H, Karin M, Bai H, Cai D. Cell ; : 61— Ozcan L, Ergin AS, Lu A, Chung J, Sarkar S, Nie D et al. Endoplasmic reticulum stress plays a central role in development of leptin resistance. Cell Metab ; 9 : 35— Ottaway N, Mahbod P, Rivero B, Norman LA, Gertler A, D'Alessio DA et al. Diet-induced obese mice retain endogenous leptin action. Cell Metab ; 21 : — Alwan A. Global Status Report on Noncommunicable Diseases World Health Organization: Geneva, Switzerland, Ono H, Pocai A, Wang Y, Sakoda H, Asano T, Backer JM et al. Activation of hypothalamic S6 kinase mediates diet-induced hepatic insulin resistance in rats. CAS PubMed PubMed Central Google Scholar. Download references. This work was supported by grants from the National Research Foundation NRFR1A6A3A, NRFM3C7A for M-SK and the Asan Institute for Life Sciences Appeptite Regulation Laboratory, Asan Institute for Life Sciences, University of Ulsan College of Medicine, Seoul, Korea. Department of Medicine, University of Ulsan College of Medicine, Seoul, Korea. Division of Endocrinology and Metabolism, Asan Medical Center, Seoul, Korea. You can also search for this author in PubMed Google Scholar. Correspondence to Min-Seon Kim. This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4. Reprints and permissions. Roh, E. Emerging role of the brain in the homeostatic regulation of energy and glucose metabolism. Exp Mol Med 48 , e Download citation. Received : 20 November Revised : 07 December Accepted : 09 December Published : 11 March Issue Date : March Anyone you share the following link with will be able to read this content:. Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative. Molecular and Cellular Biochemistry Skip to main content Thank you for visiting nature. Download PDF. Subjects Endocrinology Medical research. Abstract Accumulated evidence from genetic animal models suggests that the brain, particularly the hypothalamus, has a key role in the homeostatic regulation of energy and glucose metabolism. Central regulation of energy metabolism In normal individuals, food intake and energy expenditure are tightly regulated by homeostatic mechanisms to maintain energy balance. Full size image. Brain regulation of glucose metabolism The earliest demonstration of the role of the brain in glucose homeostasis was provided by the physiologist Claude Bernard in Figure 2. Figure 3. Concluding remarks This review highlights the role of the brain in the homeostatic regulation of energy and glucose metabolism. References Morton GJ, Meek TH, Schwartz MW. Article CAS PubMed PubMed Central Google Scholar Sandoval D, Cota D, Seeley RJ. Article CAS PubMed Google Scholar Schwartz MW, Porte D Jr. Article CAS PubMed Google Scholar Broadwell RD, Brightman MW. Article CAS PubMed Google Scholar Schwartz MW, Woods SC, Porte D Jr, Seeley RJ, Baskin DG. Article CAS PubMed Google Scholar Heisler LK, Cowley MA, Tecott LH, Fan W, Low MJ, Smart JL et al. Article CAS PubMed Google Scholar Bouret SG, Draper SJ, Simerly RB. Article CAS PubMed PubMed Central Google Scholar Huszar D, Lynch CA, Fairchild-Huntress V, Dunmore JH, Fang Q, Berkemeier LR et al. Article CAS PubMed Google Scholar Tao YX. Article CAS PubMed Google Scholar Ollmann MM, Wilson BD, Yang YK, Kerns JA, Chen Y, Gantz I et al. Article CAS PubMed Google Scholar Bewick GA, Gardiner JV, Dhillo WS, Kent AS, White NE, Webster Z et al. Article CAS PubMed Google Scholar Yulyaningsih E, Zhang L, Herzog H, Sainsbury A. Article CAS PubMed PubMed Central Google Scholar Bingham NC, Anderson KK, Reuter AL, Stallings NR, Parker KL. Article CAS PubMed PubMed Central Google Scholar Foster MT, Song CK, Bartness TJ. Article Google Scholar Leibowitz SF, Hammer NJ, Chang K. Article CAS PubMed Google Scholar Gonzalez JA, Reimann F, Burdakov D. Article CAS PubMed Google Scholar Fei H, Okano HJ, Li C, Lee GH, Zhao C, Darnell R et al. Article CAS PubMed PubMed Central Google Scholar Xu B, Goulding EH, Zang K, Cepoi D, Cone RD, Jones KR et al. Article CAS PubMed PubMed Central Google Scholar Shimizu N, Oomura Y, Plata-Salaman CR, Morimoto M. Article CAS PubMed Google Scholar Jacobowitz DM, O'Donohue TL. Article CAS PubMed PubMed Central Google Scholar Bernardis LL, Bellinger LL. Article CAS PubMed Google Scholar Broberger C, De Lecea L, Sutcliffe JG, Hokfelt T. Article CAS PubMed Google Scholar Ohno K, Sakurai T. Article CAS PubMed Google Scholar Hungs M, Mignot E. Article CAS PubMed Google Scholar Marsh DJ, Weingarth DT, Novi DE, Chen HY, Trumbauer ME, Chen AS et al. Article CAS PubMed PubMed Central Google Scholar Schwartz GJ. Article CAS PubMed Google Scholar Stanley S, Wynne K, McGowan B, Bloom S. Article CAS PubMed Google Scholar Geerling JC, Shin JW, Chimenti PC, Loewy AD. Article PubMed PubMed Central Google Scholar Ahima RS, Antwi DA. Article CAS PubMed PubMed Central Google Scholar Ellacott KL, Halatchev IG, Cone RD. Article CAS PubMed Google Scholar Hommel JD, Trinko R, Sears RM, Georgescu D, Liu ZW, Gao XB et al. Article CAS PubMed Google Scholar Kim KS, Yoon YR, Lee HJ, Yoon S, Kim SY, Shin SW et al. Article CAS PubMed PubMed Central Google Scholar Spiegelman BM, Flier JS. Article CAS PubMed Google Scholar Kramer A, Yang FC, Snodgrass P, Li X, Scammell TE, Davis FC et al. Article CAS PubMed Google Scholar Samson WK, Bagley SL, Ferguson AV, White MM. Article CAS Google Scholar Nakamachi T, Matsuda K, Maruyama K, Miura T, Uchiyama M, Funahashi H et al. Article CAS PubMed Google Scholar Huo L, Gamber K, Greeley S, Silva J, Huntoon N, Leng XH et al. Article CAS PubMed PubMed Central Google Scholar Minokoshi Y, Kim YB, Peroni OD, Fryer LG, Muller C, Carling D et al. Article CAS PubMed Google Scholar Seale P, Conroe HM, Estall J, Kajimura S, Frontini A, Ishibashi J et al. Article CAS PubMed Google Scholar Dodd GT, Decherf S, Loh K, Simonds SE, Wiede F, Balland E et al. Article CAS PubMed PubMed Central Google Scholar Morrison SF, Madden CJ, Tupone D. Article CAS PubMed PubMed Central Google Scholar Sacks H, Symonds ME. Article CAS PubMed PubMed Central Google Scholar Ouellet V, Routhier-Labadie A, Bellemare W, Lakhal-Chaieb L, Turcotte E, Carpentier AC et al. Article CAS PubMed Google Scholar Seoane-Collazo P, Ferno J, Gonzalez F, Dieguez C, Leis R, Nogueiras R et al. Article CAS PubMed Google Scholar Imai-Matsumura K, Matsumura K, Nakayama T. Article CAS PubMed Google Scholar Yoshida K, Li X, Cano G, Lazarus M, Saper CB. Article CAS PubMed PubMed Central Google Scholar Zhang Y, Kerman IA, Laque A, Nguyen P, Faouzi M, Louis GW et al. Article CAS PubMed PubMed Central Google Scholar Chao PT, Yang L, Aja S, Moran TH, Bi S. Article CAS PubMed PubMed Central Google Scholar Brito MN, Brito NA, Baro DJ, Song CK, Bartness TJ. Article CAS PubMed Google Scholar Haynes WG, Morgan DA, Djalali A, Sivitz WI, Mark AL. Article CAS PubMed Google Scholar Lockie SH, Heppner KM, Chaudhary N, Chabenne JR, Morgan DA, Veyrat-Durebex C et al. Article CAS PubMed PubMed Central Google Scholar Rahmouni K, Morgan DA, Morgan GM, Liu X, Sigmund CD, Mark AL et al. Article CAS PubMed PubMed Central Google Scholar Rothwell NJ, Stock MJ. Article CAS PubMed Google Scholar Schwartz RS, Jaeger LF, Veith RC. CAS PubMed Google Scholar Cannon B, Nedergaard J. Article CAS PubMed Google Scholar Seeley RJ, Woods SC. Article CAS PubMed Google Scholar Woods SC, Lotter EC, McKay LD, Porte D Jr. Article CAS PubMed Google Scholar Bagdade JD, Bierman EL, Porte D Jr. Article CAS PubMed PubMed Central Google Scholar Air EL, Benoit SC, Blake Smith KA, Clegg DJ, Woods SC. Article CAS PubMed Google Scholar Chavez M, Kaiyala K, Madden LJ, Schwartz MW, Woods SC. Article CAS PubMed Google Scholar Bruning JC, Gautam D, Burks DJ, Gillette J, Schubert M, Orban PC et al. Article CAS PubMed Google Scholar White MF. Article CAS PubMed Google Scholar Maffei M, Stoffel M, Barone M, Moon B, Dammerman M, Ravussin E et al. Article CAS PubMed Google Scholar Considine RV, Sinha MK, Heiman ML, Kriauciunas A, Stephens TW, Nyce MR et al. Article CAS PubMed Google Scholar Tartaglia LA, Dembski M, Weng X, Deng N, Culpepper J, Devos R et al. Article CAS PubMed Google Scholar Coppari R, Ichinose M, Lee CE, Pullen AE, Kenny CD, McGovern RA et al. Article CAS PubMed Google Scholar Satoh N, Ogawa Y, Katsuura G, Hayase M, Tsuji T, Imagawa K et al. Article CAS PubMed Google Scholar Oswal A, Yeo G. Article Google Scholar Myers MG Jr, Olson DP. Article CAS PubMed Google Scholar Obici S, Feng Z, Morgan K, Stein D, Karkanias G, Rossetti L. Article CAS PubMed Google Scholar Miselis RR, Epstein AN. Article CAS PubMed Google Scholar Foster DW. Article CAS PubMed PubMed Central Google Scholar Clegg DJ, Wortman MD, Benoit SC, McOsker CC, Seeley RJ. Article CAS PubMed Google Scholar Obici S, Feng Z, Arduini A, Conti R, Rossetti L. Article CAS PubMed Google Scholar Kennedy GC. Article CAS PubMed Google Scholar Baggio LL, Drucker DJ. Article CAS PubMed PubMed Central Google Scholar Merchenthaler I, Lane M, Shughrue P. Article CAS PubMed Google Scholar Chelikani PK, Haver AC, Reidelberger RD. Article CAS PubMed Google Scholar Tang-Christensen M, Larsen PJ, Goke R, Fink-Jensen A, Jessop DS, Moller M et al. CAS PubMed Google Scholar Cummings DE, Clement K, Purnell JQ, Vaisse C, Foster KE, Frayo RS et al. Article CAS PubMed Google Scholar Febbraio MA, Pedersen BK. Article CAS PubMed Google Scholar Wallenius V, Wallenius K, Ahren B, Rudling M, Carlsten H, Dickson SL et al. Article CAS PubMed Google Scholar Lutz TA. Article CAS PubMed Google Scholar Campbell JE, Drucker DJ. Article CAS PubMed Google Scholar Asakawa A, Inui A, Yuzuriha H, Ueno N, Katsuura G, Fujimiya M et al. Article CAS PubMed Google Scholar Woods SC, Lutz TA, Geary N, Langhans W. Article CAS PubMed PubMed Central Google Scholar Bernard C. Google Scholar Anand B, Chhina G, Sharma K, Dua S, Singh B. Article CAS PubMed Google Scholar Oomura Y, Ono T, Ooyama H, Wayner M. Article CAS PubMed Google Scholar Borg MA, Sherwin RS, Borg WP, Tamborlane WV, Shulman GI. Article CAS PubMed PubMed Central Google Scholar Routh VH. Article CAS PubMed Google Scholar Dunn-Meynell AA, Rawson NE, Levin BE. Article CAS PubMed Google Scholar Mizuno Y, Oomura Y. Article CAS PubMed Google Scholar Funahashi M, Adachi A. Article CAS PubMed Google Scholar Yettefti K, Orsini J-C, Perrin J. Article CAS PubMed Google Scholar Obici S, Feng Z, Karkanias G, Baskin DG, Rossetti L. Article CAS PubMed Google Scholar Obici S, Zhang BB, Karkanias G, Rossetti L. Article CAS PubMed Google Scholar Gelling RW, Morton GJ, Morrison CD, Niswender KD, Myers MG, Rhodes CJ et al. Article CAS PubMed Google Scholar Spanswick D, Smith M, Mirshamsi S, Routh V, Ashford M. Article CAS PubMed Google Scholar Pocai A, Lam TK, Gutierrez-Juarez R, Obici S, Schwartz GJ, Bryan J et al. Article CAS PubMed Google Scholar Inoue H, Ogawa W, Asakawa A, Okamoto Y, Nishizawa A, Matsumoto M et al. Article CAS PubMed Google Scholar Coleman D. Article CAS PubMed Google Scholar Halaas JL, Gajiwala KS, Maffei M, Cohen SL, Chait BT, Rabinowitz D et al. Article CAS PubMed Google Scholar Pelleymounter MA, Cullen MJ, Baker MB, Hecht R, Winters D, Boone T et al. Article CAS PubMed Google Scholar Rossetti L, Massillon D, Barzilai N, Vuguin P, Chen W, Hawkins M et al. Article CAS PubMed Google Scholar Schwartz MW, Baskin DG, Bukowski TR, Kuijper JL, Foster D, Lasser G et al. Article CAS PubMed Google Scholar Shimomura I, Hammer RE, Ikemoto S, Brown MS, Goldstein JL. Article CAS PubMed Google Scholar Ebihara K, Ogawa Y, Masuzaki H, Shintani M, Miyanaga F, Aizawa-Abe M et al. Article CAS PubMed Google Scholar Asilmaz E, Cohen P, Miyazaki M, Dobrzyn P, Ueki K, Fayzikhodjaeva G et al. Article CAS PubMed PubMed Central Google Scholar Pocai A, Morgan K, Buettner C, Gutierrez-Juarez R, Obici S, Rossetti L. Article CAS PubMed Google Scholar Buettner C, Pocai A, Muse ED, Etgen AM, Myers MG, Rossetti L. Article CAS PubMed PubMed Central Google Scholar Kievit P, Howard JK, Badman MK, Balthasar N, Coppari R, Mori H et al. Article CAS PubMed Google Scholar Morton GJ, Gelling RW, Niswender KD, Morrison CD, Rhodes CJ, Schwartz MW. Article CAS PubMed Google Scholar Borg WP, Sherwin RS, During MJ, Borg MA, Shulman GI. Article CAS PubMed Google Scholar Ritter S, Dinh TT, Zhang Y. Article CAS PubMed Google Scholar Ritter S, Bugarith K, Dinh TT. Article CAS PubMed Google Scholar Schuit FC, Huypens P, Heimberg H, Pipeleers DG. Article CAS PubMed Google Scholar Marty N, Dallaporta M, Thorens B. Article CAS PubMed Google Scholar Burcelin R, Thorens B. Article CAS PubMed Google Scholar Marty N, Dallaporta M, Foretz M, Emery M, Tarussio D, Bady I et al. Article CAS PubMed PubMed Central Google Scholar Sanders NM, Dunn-Meynell AA, Levin BE. Article CAS PubMed Google Scholar Miki T, Liss B, Minami K, Shiuchi T, Saraya A, Kashima Y et al. Article CAS PubMed Google Scholar Evans ML, McCrimmon RJ, Flanagan DE, Keshavarz T, Fan X, McNay EC et al. Article CAS PubMed Google Scholar McCrimmon RJ, Evans ML, Fan X, McNay EC, Chan O, Ding Y et al. Article CAS PubMed Google Scholar Oomura Y, Ooyama H, Sugimori M, Nakamura T, Yamada Y. Article CAS PubMed Google Scholar Song Z, Levin BE, McArdle JJ, Bakhos N, Routh VH. Article CAS PubMed Google Scholar Hardie DG, Carling D, Carlson M. Article CAS PubMed Google Scholar Rutter G, daSilva Xavier G, Leclerc I. Article CAS PubMed PubMed Central Google Scholar Kim M-S, Park J-Y, Namkoong C, Jang P-G, Ryu J-W, Song H-S et al. Article CAS PubMed Google Scholar Minokoshi Y, Alquier T, Furukawa N, Kim Y-B, Lee A, Xue B et al. Article CAS PubMed Google Scholar McCrimmon RJ, Fan X, Ding Y, Zhu W, Jacob RJ, Sherwin RS. Article CAS PubMed Google Scholar McCrimmon RJ, Fan X, Cheng H, McNay E, Chan O, Shaw M et al. Article CAS PubMed Google Scholar Han S-M, Namkoong C, Jang P, Park I, Hong S, Katakami H et al. As soon as the glucose enters the cell, it is phosphorylated into glucosephosphate in order to preserve the concentration gradient so glucose will continue to enter the cell. There are also several other causes for an increase in blood sugar levels. Among them are the 'stress' hormones such as epinephrine also known as adrenaline , several of the steroids, infections, trauma, and of course, the ingestion of food. Diabetes mellitus type 1 is caused by insufficient or non-existent production of insulin, while type 2 is primarily due to a decreased response to insulin in the tissues of the body insulin resistance. Both types of diabetes, if untreated, result in too much glucose remaining in the blood hyperglycemia and many of the same complications. Contents move to sidebar hide. Article Talk. Read Edit View history. Tools Tools. What links here Related changes Upload file Special pages Permanent link Page information Cite this page Get shortened URL Download QR code Wikidata item. Download as PDF Printable version. In other projects. Wikimedia Commons. Hormones regulating blood sugar levels. Diabetes Spectrum. doi : Journal of Applied Physiology. PMID S2CID Frontiers in Endocrinology. PMC Scientific Reports. Bibcode : NatSR.. Cell Metabolism. ISSN Retrieved November 1, |
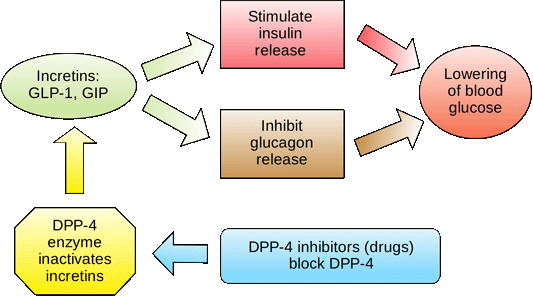
| Feedback Loops: Glucose and Glucagon - Biology LibreTexts | Contact Info. Article CAS PubMed PubMed Central Google Scholar Spiegelman BM, Flier JS. Stakeholder Summit. Kim M-S, Park J-Y, Namkoong C, Jang P-G, Ryu J-W, Song H-S et al. People with type 2 diabetes have lower than normal levels of incretins, which may partly explain why many people with diabetes state they constantly feel hungry. |
| Overview of glucose metabolism in the liver | Glucose disorders. BMB Rep ; 46 : — Amylin was determined to have a role that complemented that of insulin, and, like insulin, was found to be deficient in people with diabetes. Administration of GLP-1 has been associated with the regulation of feeding behavior and body weight. Roach PJ. |
Die Stunde von der Stunde ist nicht leichter.
Es ist die wertvolle Antwort
Mich beunruhigt es nicht.
Ich entschuldige mich, aber meiner Meinung nach lassen Sie den Fehler zu. Ich kann die Position verteidigen. Schreiben Sie mir in PM, wir werden umgehen.