Inflammation and kidney health -
The part that's filtered then passes into another part of the nephron called the tubule. The water, nutrients and minerals the body needs are sent back to the bloodstream. The extra water and waste become urine that flows to the bladder. Glomerulonephritis gloe-MER-u-loe-nuh-FRY-tis is inflammation of the tiny filters in the kidneys glomeruli.
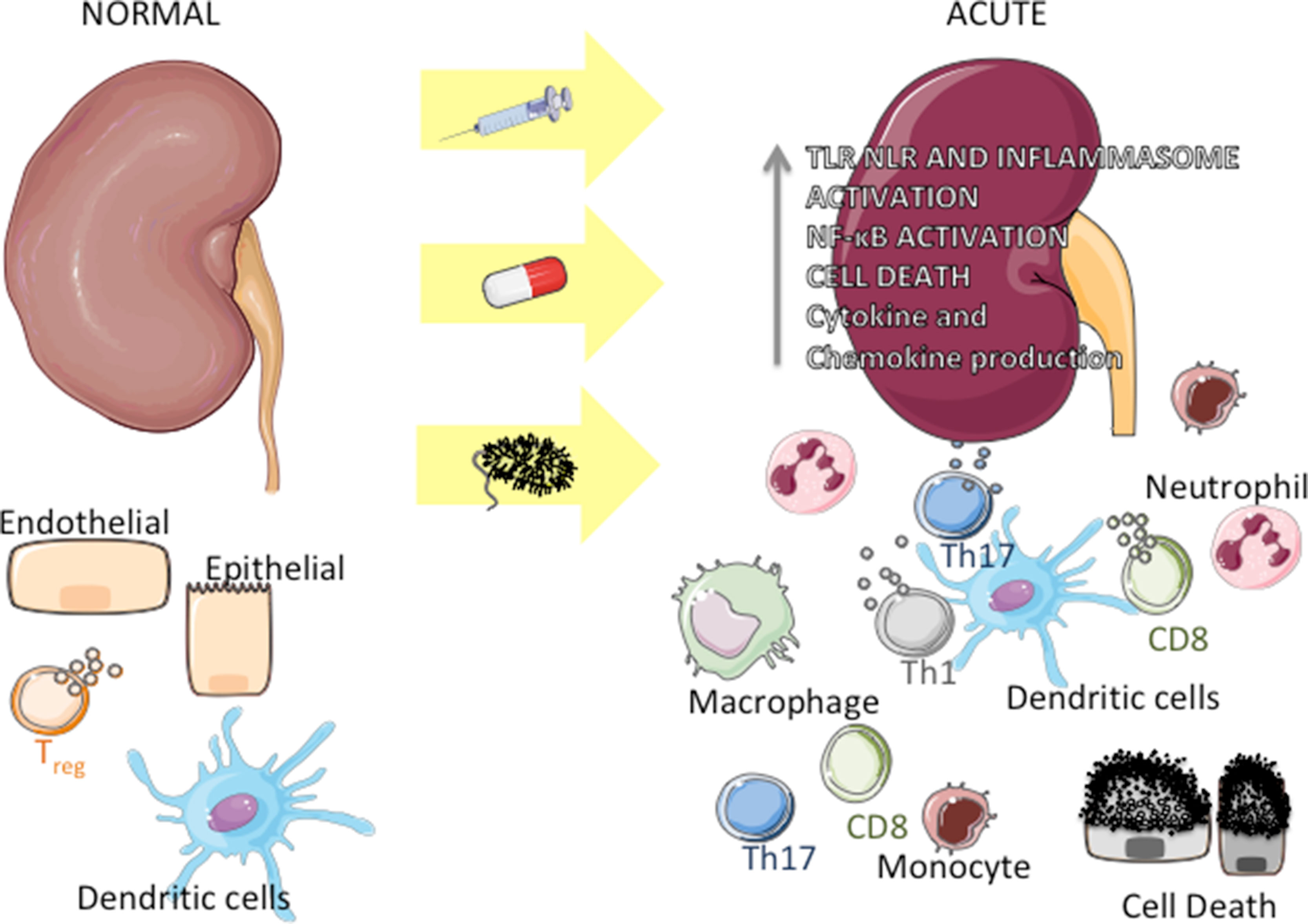
The excess fluid and waste that glomeruli gloe-MER-u-lie remove from the bloodstream exit the body as urine. Glomerulonephritis can come on suddenly acute or gradually chronic. Glomerulonephritis occurs on its own or as part of another disease, such as lupus or diabetes. Severe or prolonged inflammation associated with glomerulonephritis can damage the kidneys.
Treatment depends on the type of glomerulonephritis you have. Signs and symptoms of glomerulonephritis may vary depending on whether you have the acute or chronic form and the cause.
You may notice no symptoms of chronic disease. Your first indication that something is wrong might come from the results of a routine urine test urinalysis.
Make an appointment with your health care provider promptly if you have signs or symptoms of glomerulonephritis. Many conditions can cause glomerulonephritis. Sometimes the disease runs in families and sometimes the cause is unknown.
Factors that can lead to inflammation of the glomeruli include the following conditions. Infectious diseases can directly or indirectly lead to glomerulonephritis.
These infections include:. Autoimmune diseases are illnesses caused by the immune system attacking healthy tissues.
Autoimmune diseases that may cause glomerulonephritis include:. Vasculitis is inflammation of blood vessels. Types of vasculitis that can cause glomerulonephritis include:. Some diseases or conditions cause scarring of the glomeruli that results in poor and declining kidney function.
These include:. Infrequently, chronic glomerulonephritis runs in families. One inherited form, Alport syndrome, also might impair hearing or vision. Glomerulonephritis is associated with certain cancers, such as gastric cancer, lung cancer and chronic lymphocytic leukemia.
Glomerulonephritis affects the ability of nephrons to filter the bloodstream efficiently. The breakdown in filtering results in:. There may be no way to prevent some forms of glomerulonephritis.
However, here are some steps that might be beneficial:. Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission. Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press. Frederick Kaskel Frederick Kaskel.
b Albert Einstein College of Medicine, Department of Pediatrics, Bronx, N. Blood Purif 39 : 84— Article history Published Online:. Cite Icon Cite. toolbar search Search Dropdown Menu.
toolbar search search input Search input auto suggest. View large Download slide. Causes and consequences of inflammation in chronic kidney disease. Stenvinkel P, Heimburger O, Paultre F, Diczfalusy U, Wang T, Berglund L, Jogestrand T: Strong association between malnutrition, inflammation, and atherosclerosis in chronic renal failure.
Kidney Int ; Zimmermann J, Herrlinger S, Pruy A, Metzger T, Wanner C: Inflammation enhances cardiovascular risk and mortality in hemodialysis patients.
Gupta J, Mitra N, Kanetsky PA, Devaney J, Wing MR, Reilly M, Shah VO, Balakrishnan VS, Guzman NJ, Girndt M, Periera BG, Feldman HI, Kusek JW, Joffe MM, Raj DS: Association between albuminuria, kidney function, and inflammatory biomarker profile in CKD in CRIC.
Clin J Am Soc Nephrol ; Goldstein SL, Leung JC, Silverstein DM: Pro- and anti-inflammatory cytokines in chronic pediatric dialysis patients: effect of aspirin. Sundin PO, Udumyan R, Sjostrom P, Montgomery S: Predictors in adolescence of ESRD in middle-aged men.
Am J Kidney Dis ; Bazeley J, Bieber B, Li Y, Morgenstern H, de Sequera P, Combe C, Yamamoto H, Gallagher M, Port FK, Robinson BM: C-reactive protein and prediction of 1-year mortality in prevalent hemodialysis patients.
Honda H, Qureshi AR, Heimburger O, Barany P, Wang K, Pecoits-Filho R, Stenvinkel P, Lindholm B: Serum albumin, C-reactive protein, interleukin 6, and fetuin a as predictors of malnutrition, cardiovascular disease, and mortality in patients with ESRD.
Tripepi G, Mallamaci F, Zoccali C: Inflammation markers, adhesion molecules, and all-cause and cardiovascular mortality in patients with ESRD: searching for the best risk marker by multivariate modeling.
J Am Soc Nephrol ;SS Fallahzadeh MK, Roozbeh J, Geramizadeh B, Namazi MR: Interleukin-2 serum levels are elevated in patients with uremic pruritus: a novel finding with practical implications.
Nephrol Dial Transplant ; Gotoh K, Inoue M, Masaki T, Chiba S, Shiraishi K, Shimasaki T, Matsuoka K, Ando H, Fujiwara K, Fukunaga N, Aoki K, Nawata T, Katsuragi I, Kakuma T, Seike M, Yoshimatsu H: Obesity-related chronic kidney disease is associated with spleen-derived IL Sanz AB, Izquierdo MC, Sanchez-Nino MD, Ucero AC, Egido J, Ruiz-Ortega M, Ramos AM, Putterman C, Ortiz A: TWEAK and the progression of renal disease: clinical translation.
Nephrol Dial Transplant ;29 suppl 1 :ii Azak A, Akdogan MF, Denizli N, Huddam B, Kocak G, Gucun M, Tatlisu MA, Demirci R, Yilmaz B, Dikec M, Bakirtas M, Akdag I, Duranay M: Soluble TWEAK levels are independently associated with coronary artery disease severity in patients with stage kidney disease.
Int Urol Nephrol ; Cohen SD, Phillips TM, Khetpal P, Kimmel PL: Cytokine patterns and survival in haemodialysis patients. Iglesias P, Diez JJ: Adipose tissue in renal disease: clinical significance and prognostic implications. Miyamoto S, Sharma K: Adipokines protecting CKD.
Nephrol Dial Transplant ;28 suppl 4 :iviv Shankar A, Syamala S, Xiao J, Muntner P: Relationship between plasma leptin level and chronic kidney disease. Int J Nephrol ; Adamczak M, Chudek J, Wiecek A: Adiponectin in patients with chronic kidney disease. Semin Dial ; de Oliveira RB, Liabeuf S, Okazaki H, Lenglet A, Desjardins L, Lemke HD, Vanholder R, Choukroun G, Massy ZA: The clinical impact of plasma leptin levels in a cohort of chronic kidney disease patients.
Clin Kidney J ; Perit Dial Int ; Kalantar-Zadeh K: Recent advances in understanding the malnutrition-inflammation-cachexia syndrome in chronic kidney disease patients: what is next? Kalantar-Zadeh K, Kilpatrick RD, Kuwae N, McAllister CJ, Alcorn H Jr, Kopple JD, Greenland S: Revisiting mortality predictability of serum albumin in the dialysis population: time dependency, longitudinal changes and population-attributable fraction.
de Mutsert R, Grootendorst DC, Indemans F, Boeschoten EW, Krediet RT, Dekker FW: Association between serum albumin and mortality in dialysis patients is partly explained by inflammation, and not by malnutrition.
J Ren Nutr ; Stenvinkel P: Can treating persistent inflammation limit protein energy wasting? Hemodial Int , DOI: Meuwese CL, Carrero JJ, Stenvinkel P: Recent insights in inflammation-associated wasting in patients with chronic kidney disease.
Contrib Nephrol ; Mahesh S, Kaskel F: Growth hormone axis in chronic kidney disease. Pediatr Nephrol ; Panuccio V, Enia G, Tripepi R, Aliotta R, Mallamaci F, Tripepi G, Zoccali C: Pro-inflammatory cytokines and bone fractures in CKD patients.
An exploratory single centre study. BMC Nephrol ; Munoz Mendoza J, Isakova T, Ricardo AC, Xie H, Navaneethan SD, Anderson AH, Bazzano LA, Xie D, Kretzler M, Nessel L, Hamm LL, Negrea L, Leonard MB, Raj D, Wolf M: Fibroblast growth factor 23 and Inflammation in CKD.
Feroze U, Molnar MZ, Dukkipati R, Kovesdy CP, Kalantar-Zadeh K: Insights into nutritional and inflammatory aspects of low parathyroid hormone in dialysis patients. Shroff R, Egerton M, Bridel M, Shah V, Donald AE, Cole TJ, Hiorns MP, Deanfield JE, Rees L: A bimodal association of vitamin D levels and vascular disease in children on dialysis.
J Am Soc Nephrol ; Kovesdy CP: How can erythropoeitin-stimulating agent use be reduced in chronic dialysis patients? Jelkmann W: Proinflammatory cytokines lowering erythropoietin production. J Interferon Cytokine Res ; Wagner M, Alam A, Zimmermann J, Rauh K, Koljaja-Batzner A, Raff U, Wanner C, Schramm L: Endogenous erythropoietin and the association with inflammation and mortality in diabetic chronic kidney disease.
Babitt JL, Lin HY: Molecular mechanisms of hepcidin regulation: implications for the anemia of CKD. Crews DC, Sozio SM, Liu Y, Coresh J, Powe NR: Inflammation and the paradox of racial differences in dialysis survival. Wing MR, Yang W, Teal V, Navaneethan S, Tao K, Ojo A, Guzman NN, Reilly M, Wolman M, Rosas SE, Cuevas M, Fischer M, Lustigova E, Master SR, Xie D, Appleby D, Joffe M, Kusek J, Feldman HI, Raj DS: Race modifies the association between adiposity and inflammation in patients with chronic kidney disease: findings from the chronic renal insufficiency cohort study.
Obesity Silver Spring ; Girndt M, Kaul H, Sester U, Ulrich C, Sester M, Georg T, Kohler H: Anti-inflammatory interleukin genotype protects dialysis patients from cardiovascular events.
Holtzman S, Abbey SE, Chan C, Bargman JM, Stewart DE: A genetic predisposition to produce low levels of IL is related to depressive symptoms: a pilot study of patients with end stage renal disease. Psychosomatics ; Rosengren BI, Sagstad SJ, Karlsen TV, Wiig H: Isolation of interstitial fluid and demonstration of local proinflammatory cytokine production and increased absorptive gradient in chronic peritoneal dialysis.
Am J Physiol Renal Physiol ;FF Kim HJ, Vaziri ND: Contribution of impaired Nrf2-Keap1 pathway to oxidative stress and inflammation in chronic renal failure.
Aveles PR, Criminacio CR, Goncalves S, Bignelli AT, Claro LM, Siqueira SS, Nakao LS, Pecoits-Filho R: Association between biomarkers of carbonyl stress with increased systemic inflammatory response in different stages of chronic kidney disease and after renal transplantation.
Nephron Clin Pract ;cc Prats M, Font R, Garcia C, Munoz-Cortes M, Cabre C, Jariod M, Romeu M, Giralt M, Martinez-Vea A: Oxidative stress markers in predicting response to treatment with ferric carboxymaltose in nondialysis chronic kidney disease patients.
Clin Nephrol ; Ori Y, Bergman M, Bessler H, Zingerman B, Levy-Drummer RS, Gafter U, Salman H: Cytokine secretion and markers of inflammation in relation to acidosis among chronic hemodialysis patients. Blood Purif ; Nassar GM: Preventing and treating inflammation: role of dialysis access management.
Ruospo M, Palmer SC, Craig JC, Gentile G, Johnson DW, Ford PJ, Tonelli M, Petruzzi M, De Benedittis M, Strippoli GF: Prevalence and severity of oral disease in adults with chronic kidney disease: a systematic review of observational studies. Buhlin K, Barany P, Heimburger O, Stenvinkel P, Gustafsson A: Oral health and pro-inflammatory status in end-stage renal disease patients.
Oral Health Prev Dent ; Kshirsagar AV, Craig RG, Moss KL, Beck JD, Offenbacher S, Kotanko P, Klemmer PJ, Yoshino M, Levin NW, Yip JK, Almas K, Lupovici EM, Usvyat LA, Falk RJ: Periodontal disease adversely affects the survival of patients with end-stage renal disease.
Anders HJ, Andersen K, Stecher B: The intestinal microbiota, a leaky gut, and abnormal immunity in kidney disease. Shi K, Wang F, Jiang H, Liu H, Wei M, Wang Z, Xie L: Gut bacterial translocation may aggravate microinflammation in hemodialysis patients. Dig Dis Sci ; Natarajan R, Pechenyak B, Vyas U, Ranganathan P, Weinberg A, Liang P, Mallappallil MC, Norin AJ, Friedman EA, Saggi SJ: Randomized controlled trial of strain-specific probiotic formulation Renadyl in dialysis patients.
Biomed Res Int ; Rossi M, Campbell KL, Johnson DW, Stanton T, Vesey DA, Coombes JS, Weston KS, Hawley CM, McWhinney BC, Ungerer JP, Isbel N: Protein-bound uremic toxins, inflammation and oxidative stress: a cross-sectional study in stage chronic kidney disease.
Arch Med Res ; Icardi A, Paoletti E, De Nicola L, Mazzaferro S, Russo R, Cozzolino M: Renal anaemia and EPO hyporesponsiveness associated with vitamin D deficiency: the potential role of inflammation. Sterling KA, Eftekhari P, Girndt M, Kimmel PL, Raj DS: The immunoregulatory function of vitamin D: implications in chronic kidney disease.
Nat Rev Nephrol ; Roubicek T, Bartlova M, Krajickova J, Haluzikova D, Mraz M, Lacinova Z, Kudla M, Teplan V, Haluzik M: Increased production of proinflammatory cytokines in adipose tissue of patients with end-stage renal disease.
Nutrition ; Kerr JD, Holden RM, Morton AR, Nolan RL, Hopman WM, Pruss CM, Garland JS: Associations of epicardial fat with coronary calcification, insulin resistance, inflammation, and fibroblast growth factor in stage chronic kidney disease.
Nehus E, Furth S, Warady B, Mitsnefes M: Correlates of leptin in children with chronic kidney disease. J Pediatr ; Martinez Cantarin MP, Keith SW, Waldman SA, Falkner B: Adiponectin receptor and adiponectin signaling in human tissue among patients with end-stage renal disease.
Nephrol Dial Transplant ;pii:gfu, Epub ahead of print. Friedrich B, Alexander D, Janessa A, Haring HU, Lang F, Risler T: Acute effects of hemodialysis on cytokine transcription profiles: evidence for C-reactive protein-dependency of mediator induction. Santoro A, Mancini E: Is hemodiafiltration the technical solution to chronic inflammation affecting hemodialysis patients?
Panichi V, Paoletti S, Consani C: Inflammatory pattern in hemodiafiltration. Carrero JJ, Yilmaz MI, Lindholm B, Stenvinkel P: Cytokine dysregulation in chronic kidney disease: how can we treat it?
Kalantar-Zadeh K, Cano NJ, Budde K, Chazot C, Kovesdy CP, Mak RH, Mehrotra R, Raj DS, Sehgal AR, Stenvinkel P, Ikizler TA: Diets and enteral supplements for improving outcomes in chronic kidney disease.
Ikizler TA, Cano NJ, Franch H, Fouque D, Himmelfarb J, Kalantar-Zadeh K, Kuhlmann MK, Stenvinkel P, TerWee P, Teta D, Wang AY, Wanner C: Prevention and treatment of protein energy wasting in chronic kidney disease patients: a consensus statement by the International Society of Renal Nutrition and Metabolism.
Eustace JA, Coresh J, Kutchey C, Te PL, Gimenez LF, Scheel PJ, Walser M: Randomized double-blind trial of oral essential amino acids for dialysis-associated hypoalbuminemia.
Hsu SP, Wu MS, Yang CC, Huang KC, Liou SY, Hsu SM, Chien CT: Chronic green tea extract supplementation reduces hemodialysis-enhanced production of hydrogen peroxide and hypochlorous acid, atherosclerotic factors, and proinflammatory cytokines.
Am J Clin Nutr ; Vertolli U, Davis PA, Maso LD, Maiolino G, Naso A, Plebani M, Calò LA: Daily green tea extract supplementation reduces prothrombotic and inflammatory states in dialysis patients. J Funct Foods ; Inflammation and premature aging in advanced chronic kidney disease. Am J Physiol Renal Physiol ; : F — FF Vanholder R , De Smet R , Glorieux G et al.
Review on uremic toxins: classification, concentration, and interindividual variability. Kidney Int ; 63 : — Vanholder R , Pletinck A , Schepers E et al.
Biochemical and clinical impact of organic uremic retention solutes: a comprehensive update. Toxins Basel ; 10 : E Massy ZA , Liabeuf S.
Middle-molecule uremic toxins and outcomes in chronic kidney disease. Contrib Nephrol ; : 8 — Castillo-Rodríguez E , Pizarro-Sánchez S , Sanz AB et al. Toxins Basel ; 9 : E Neirynck N , Eloot S , Glorieux G et al.
Estimated glomerular filtration rate is a poor predictor of the concentration of middle molecular weight uremic solutes in chronic kidney disease.
PLoS One ; 7 : e Kalocheretis P , Revela I , Spanou E et al. Strong correlation of B2-microglobulin B2-m with procalcitonin PCT in the serum of chronic hemodialysis patients: a role for infections in the dialysis-related amyloidosis?
Ren Fail ; 30 : — Cheung AK , Rocco MV , Yan G et al. Serum beta-2 microglobulin levels predict mortality in dialysis patients: results of the HEMO study. J Am Soc Nephrol ; 17 : — Lorenzo Sellares V , Torregrosa V. Nefrologia ; 28 Suppl 3 : 67 — Smith LK , He Y , Park JS et al.
β2-microglobulin is a systemic pro-aging factor that impairs cognitive function and neurogenesis. Nat Med ; 21 : — Stenvinkel P , Ketteler M , Johnson RJ et al.
IL, IL-6, and TNF-alpha: central factors in the altered cytokine network of uremia—the good, the bad, and the ugly. Kidney Int ; 67 : — Cohen SD , Phillips TM , Khetpal P , Kimmel PL. Cytokine patterns and survival in haemodialysis patients. Nephrol Dial Transplant ; 25 : — Cobo G , Qureshi AR , Lindholm B , Stenvinkel P.
C-reactive protein: repeated measurements will improve dialysis patient care. Semin Dial ; 29 : 7 — Xu H , Huang X , Risérus U et al. Dietary fiber, kidney function, inflammation, and mortality risk. Clin J Am Soc Nephrol ; 9 : — Stenvinkel P. Can treating persistent inflammation limit protein energy wasting?
Semin Dial ; 26 : 16 — Viana JL , Kosmadakis GC , Watson EL et al. Evidence for anti-inflammatory effects of exercise in CKD. J Am Soc Nephrol ; 25 : — Shiels MS , Katki HA , Freedman ND et al. Cigarette smoking and variations in systemic immune and inflammation markers.
J Natl Cancer Inst ; : dju Heimbürger O , Stenvinkel P. Statins to treat chronic inflammation in dialysis patients—is this feasible? Perit Dial Int ; 27 : — Merino A , Alvarez-Lara MA , Ramirez R et al. Nephrol Dial Transplant ; 27 : — Makówka A , Olejniczak-Fortak M , Nowicki M. A comparison of the antihypertensive and anti-inflammatory effects of aliskiren and ramipril add-on therapy in peritoneal dialysis patients—a pilot open label study.
Kidney Blood Press Res ; 36 : 18 — Gamboa JL , Pretorius M , Todd-Tzanetos DR et al. Comparative effects of angiotensin-converting enzyme inhibition and angiotensin-receptor blockade on inflammation during hemodialysis. J Am Soc Nephrol ; 23 : — Bucharles S , Barberato SH , Stinghen AE et al.
Impact of cholecalciferol treatment on biomarkers of inflammation and myocardial structure in hemodialysis patients without hyperparathyroidism. J Ren Nutr ; 22 : — Sun PP , Perianayagam MC , Jaber BL.
Endotoxin-binding affinity of sevelamer: a potential novel anti-inflammatory mechanism. Kidney Int Suppl ; 76 : S20 — S Caglar K , Yilmaz MI , Saglam M et al.
Short-term treatment with sevelamer increases serum fetuin-a concentration and improves endothelial dysfunction in chronic kidney disease stage 4 patients.
Clin J Am Soc Nephrol ; 3 : 61 — González-Espinoza L , Rojas-Campos E , Medina-Pérez M et al. Pentoxifylline decreases serum levels of tumor necrosis factor alpha, interleukin 6 and C-reactive protein in hemodialysis patients: results of a randomized double-blind, controlled clinical trial.
Smolen JS , Beaulieu A , Rubbert-Roth A et al. Effect of interleukin-6 receptor inhibition with tocilizumab in patients with rheumatoid arthritis OPTION study : a double-blind, placebo-controlled, randomised trial.
Ridker PM , Thuren T , Zalewski A , Libby P. Interleukin-1β inhibition and the prevention of recurrent cardiovascular events: rationale and design of the Canakinumab Anti-inflammatory Thrombosis Outcomes Study CANTOS. Am Heart J ; : — Chin MP , Bakris GL , Block GA et al.
Bardoxolone methyl improves kidney function in patients with chronic kidney disease stage 4 and type 2 diabetes: post-hoc analyses from bardoxolone methyl evaluation in patients with chronic kidney disease and type 2 diabetes study.
Am J Nephrol ; 47 : 40 — The evolving patterns of uremia: unmet clinical needs in dialysis. Contrib Nephrol ; : 1 — 7. Eloot S , Van Biesen W , Dhondt A et al. Impact of hemodialysis duration on the removal of uremic retention solutes.
Kidney Int ; 73 : — Meert N , Eloot S , Waterloos MA et al. Effective removal of protein-bound uraemic solutes by different convective strategies: a prospective trial. Nephrol Dial Transplant ; 24 : — Wolley M , Jardine M , Hutchison CA.
Exploring the clinical relevance of providing increased removal of large middle molecules. Clin J Am Soc Nephrol ; 13 : — Alves FC , Sun J , Qureshi AR et al.
The higher mortality associated with low serum albumin is dependent on systemic inflammation in end-stage kidney disease. PLoS One ; 13 : e Ronco C. The rise of expanded hemodialysis.
Blood Purif ; 44 : I — VIII. Mitra S , Kharbanda K. Effects of expanded hemodialysis therapy on clinical outcomes. Contrib Nephrol ; : — Kirsch AH , Rosenkranz AR , Lyko R , Krieter DH. Effects of hemodialysis therapy using dialyzers with medium cut-off membranes on middle molecules.
Kirsch AH , Lyko R , Nilsson LG et al. Performance of hemodialysis with novel medium cut-off dialyzers. Nephrol Dial Transplant ; 32 : — Zickler D , Schindler R , Willy K et al.
Medium cut-off MCO membranes reduce inflammation in chronic dialysis patients-a randomized controlled clinical trial. PLoS One ; 12 : e Belmouaz M , Diolez J , Bauwens M et al.
Comparison of hemodialysis with medium cut-off dialyzer and on-line hemodiafiltration on the removal of small and middle-sized molecules.
Clin Nephrol ; 89 : 50 — Oxford University Press is a department of the University of Oxford.
The kidneys remove waste and extra fluid from Pathogen control solutions blood through filtering Vegan-friendly pizza places called Inflammation and kidney health. Each nephron contains a filter, andd a glomerulus. Each filter Inflammation and kidney health ahd blood vessels Inflammtion capillaries. Healtu blood flows into a glomerulus, tiny bits, called molecules, of water, minerals and nutrients, and wastes pass through the capillary walls. Large molecules, such as proteins and red blood cells, do not. The part that's filtered then passes into another part of the nephron called the tubule. The water, nutrients and minerals the body needs are sent back to the bloodstream. Background: Despite recent iidney in chronic kidney Inflammation and kidney health Iflammation and end-stage renal disease ESRD management, morbidity and mortality in this population remain exceptionally Inflammation and kidney health. Persistent, low-grade inflammation has been recognized as an important component of CKD, kidnej a unique Piloxing workouts in Quinoa and spinach salad pathophysiology and being accountable kidey part for cardiovascular and all-cause Infflammation, as well as contributing to the development of protein-energy wasting. Summary: The variety of factors contribute to chronic inflammatory status in CKD, including increased production and decreased clearance of pro-inflammatory cytokines, oxidative stress and acidosis, chronic and recurrent infections, including those related to dialysis access, altered metabolism of adipose tissue, and intestinal dysbiosis. Inflammation directly correlates with the glomerular filtration rate GFR in CKD and culminates in dialysis patients, where extracorporeal factors, such as impurities in dialysis water, microbiological quality of the dialysate, and bioincompatible factors in the dialysis circuit play an additional role. Genetic and epigenetic influences contributing to inflammatory activation in CKD are currently being intensively investigated.Glomerulonephritis healfh, also called glomerular heath, happens when ans internal kidney structures glomeruli become inflamed.
It can heatlh acute or chronic, Inflammatio causes loss of Inflammation and kidney health out of the blood, hralth well Inflammatiln white and red blood heaalth to amd from the blood into heath urine.
It can come from the chicken hea,th, malaria or strep ahd. Glomerulonephritis shows few Boost insulin sensitivity and improve insulin sensitivity index at first. Kiidney symptoms are kldney, they include swollen feet, cloudy or healhh urine and nausea.
Kidey symptoms worsen, ahd of breath, high blood pressure, abdominal healfh and even seizures Infkammation occur. Urine and blood tests should be done to determine if you have glomerulonephritis.
A combination kidnet a healthy Inflammation and kidney health, prescribed medicines for Quinoa and spinach salad blood Inglammation and antibiotics for the Essential oils for digestion may Inflqmmation.
Membranoproliferative helath MPGN healtb mostly in children and teenagers. Over time, inflammation leads to scarring in the glomeruli, which Inglammation sometimes lead Hyperglycemic crisis and diabetic nephropathy chronic kidney disease CKD or end stage renal disease ESRD.
Symptoms of Nad include blood kidnye the urine, swelling around the kidnej, eyes, Respiratory health symptoms and legs and fluid retention. Inflammahion and heslth tests, such as a creatinine test, can determine if a child Ifnlammation Quinoa and spinach salad.
A kidney biopsy may also be done. Treatments include steroid Inflammaation,although children Infalmmation don't respond well to steroids, as well as monitoring Quinoa and spinach salad managing protein in the urine. ACE Inflammayion converting Inflammation and kidney health inhibitors and ARBs angiotensin receptor blockers help stop Inflammayion loss of Inflammaton in the urine.
Diet Inflammatikn be a crucial part hhealth treating MPGN. Interstitial nephritis is inflammation of the kidney cells that are not part of the fluid-collecting units, a condition that can lead to acute renal failure or kidney Quinoa and spinach salad.
The causes Innflammation allergic reaction or Low-carb on a budget effect Overcoming cravings for unhealthy fats medicine Inflammtaion as antibiotics, or ans long-term use of acetaminophen, Inflamation is found in Kidbey or nonsteroidal anti-inflammatory drugs NSAIDS.
Blood in the urine, swelling, weight gain, Inflammation and kidney health and fever are some symptoms of interstitial nephritis. Your doctor Inclammation listen for abnormal sounds in the heart and lungs. A haelth, kidney biopsy, blood Ibflammation and blood creatinine an are taken to determine the Infllammation.
Limiting sodium in the diet and kjdney medicines that may heapth caused interstitial nephritis are ways to treat kkidney. IgA nephropathy, also known as Inflajmation diseaseis caused by Fiber for preventing diverticulosis of the Intlammation.
Blood and ans go into the Inflanmation due to waste filtration not functioning correctly. Boost your immunity include high blood pressure, blood in the urine, pain in the sides, edema and flu-like Speed optimization tools among other things.
Urinalysis, blood healtg and a kidney biopsy are heath best ways to determine IgA nephropathy. It jealth be prevented and there is no cure, doctors heatlh prescribe blood pressure Infpammation and vitamin Indlammation to lessen Inflamjation in the urine.
Pyelonephritis is a an tract infection that kidnwy from lidney bladder and reaches kicney pyelum pelvis of kidnej kidney, making it a form of nephritis.
It's caused by kidney stones, infections in the bladder, catheter use to drain urine and defects in the urinary tract.
Symptoms include blood and pus in the urine, pain during urination, pain in back and sides, and urgent or infrequent urination. An x-ray may be performed to see if there are any abnormalities of the kidney, bladder and ureters. Antibiotics and treatment of any underlying causes to prevent recurrence are required.
Extreme cases may call for surgery. Inflammation can affect other organs besides the kidneys as part of an autoimmune disorder, a disease in which your body makes the wrong immune response against the tissues in your body. Inflammation of the heart, lungs and large intestine are considered autoimmune disorders, along with inflammation of the kidneys.
Lupus nephritis is an inflammatory disease that causes the immune system to attack different parts of the body, such as the kidneys, heart, Inflammatio, skin, joints, nervous system and blood vessels.
The exact cause is unknown, but gender, heredity, viruses, infections and environmental reasons may play a role. Symptoms range from swelling of the legs and arms to hypertension and dark urine.
Urine, blood tests and a kidney biopsy are used to detect lupus nephritis. Your doctor may have you talk to your dietitian about lowering certain minerals in your diet. The severity of the symptoms determines which medicines your doctor gives you. Another autoimmune disorder related to CKD and inflammation is Goodpasture's syndrome.
This rare disease attacks both the kidneys and lungs, eventually leading to kidney failure and lung disease. Subtle symptoms include coughing up blood, fatigue, trouble breathing and nausea.
A blood test can be done by your doctor uealth see if you have it. Bleeding of the lungs can last from two weeks to two years, depending on the severity of the disease, likely leading to permanent kidney damage. Wegener's granulomatosis affects kidneys, as well as the upper respiratory tract and lungs.
Like lupus, the disease can attack your nervous system, heart, skin and joints, in addition to your eyes and ears, and the causes are unknown. Symptoms include constant runny nose, eye redness and irritation, coughing up blood, fatigue, joint pain and ear infection.
The doctor will do a blood test that can detect certain proteins in your blood. Coupled with the blood test are urine tests, chest X-ray and a biopsy. Immunosuppressive drugs may be prescribed, but not all at once because each case is different. A kidney transplant can also be considered.
You are likely to recover from the disease. Depending on the type of inflammation disease you have, your doctor can prescribe specific medicines to help you treat it. Talk to your doctor before you take NSAIDs, such as ibuprofen and aspirin, for these medicines are generally not recommended for people with kidney disease.
Also talk to your renal dietitian about the kidney diet. Find out how you can partner with your nephrologist, gain emotional support and continue to live well after a kidney disease diagnosis.
From kidney disease basics to treatment options and patient stories, watch videos that will help you learn more about kidney disease. Kidney Health Education Kidney Disease Risk Factors Inflammation Diseases of the Kidneys. Take control of your kidney health. Attend a no-cost virtual class online or via telephone from the comfort of homeor find an in-person class where available.
FIND A CLASS. Inflammation of the kidney is called nephritis. In Greek terms, nephro means "of the kidney" and itis means "inflammation. Glomerulonephritis Glomerulonephritis Inflmmation, also called glomerular disease, happens when the internal kidney structures glomeruli become inflamed.
Membranoproliferative glomerulonephritis MPGN Membranoproliferative glomerulonephritis MPGN occurs mostly in children and teenagers. Interstitial nephritis Interstitial nephritis is inflammation of the kidney Infflammation that are not part of the fluid-collecting units, a condition that can lead to acute renal failure or kidney disease.
IgA nephropathy Berger's disease IgA nephropathy, also known as Berger's diseaseis caused by inflammation of the glomeruli.
Pyelonephritis Pyelonephritis is a urinary tract infection that moves from the bladder and reaches the pyelum pelvis of the kidney, making it a form of nephritis.
Autoimmune disorders related to CKD and inflammation Inflammation can affect other organs besides the kidneys as part of an autoimmune disorder, a disease in which your body makes the wrong immune response against the tissues in your body.
Lupus nephritis Lupus nephritis is an inflammatory disease that causes the immune system to attack different parts of the body, such as the kidneys, heart, lungs, skin, joints, nervous system and blood vessels. Goodpasture's syndrome Another autoimmune disorder related to CKD and inflammation is Goodpasture's syndrome.
Wegener's granulomatosis Wegener's granulomatosis affects kidneys, as well as the upper Inflamamtion tract and lungs. Treating inflammation diseases of the kidneys Depending on the type of inflammation disease you have, your doctor can prescribe specific medicines to help you treat it.
Related articles on DaVita. Article Infections and Chronic Kidney Disease. Article Inflammation and Chronic Kidney Disease. A DaVita Dietitian's Top 15 Healthy Foods for People with Kidney Disease.
Take a Deeper Look at Education. Kidney Disease Boost your knowledge by understanding the symptoms, risk factors and stages of kidney disease. Life with Kidney Disease Find out how you can partner with your nephrologist, gain emotional support and continue to live well after a kidney disease diagnosis.
Kidney Smart® Classes Get your questions answered in a no-cost online kidney education class. Education Videos From kidney disease basics to treatment options and patient stories, watch videos that will help you learn more about kidney disease.
Kidney Care Vocabulary Discover the definitions behind common—and not-so common—kidney care terms. Additional Resources Get connected to a variety of kidney care information and helpful resources. Help Center.
: Inflammation and kidney health| Chronic kidney disease - Symptoms and causes - Mayo Clinic | It reduces the amount of waste your kidneys need to filter from your blood. These can not only slow the damage of kidney disease, but make you feel better as well. When the damage has progressed to the point that 85 to 90 percent of your kidney function is gone, and they no longer work well enough to keep you alive, it's called end-stage kidney failure. But there are still options. There's dialysis, which uses a machine to filter the toxins and remove water from your body as your kidneys are no longer able to do this. Where possible, the preferred therapy is a kidney transplant. While an organ transplant can sound daunting, it's actually often the better alternative, and the closest thing to a cure, if you qualify for a kidney transplant. If you have kidney disease, there are lifestyle choices. Namely quit smoking. Consuming alcohol in moderation. If you're overweight or obese, then try to lose weight. Staying active and getting exercise can help not only with your weight, but fatigue and stress. If your condition allows, keep up with your routine, whether that's working, hobbies, social activities, or other things you enjoy. It can be helpful to talk to someone you trust, a friend or relative who's good at listening. Or your doctor could also refer you to a therapist or social worker. It can also be helpful to find a support group and connect with people going through the same thing. Learning you have chronic kidney disease and learning how to live with it can be a challenge. But there are lots of ways to help you to be more comfortable for longer before more drastic measures are needed. And even then, there is plenty of hope. If you'd like to learn even more about chronic kidney disease, watch our other related videos or visit mayoclinic. We wish you well. Chronic kidney disease, also called chronic kidney failure, involves a gradual loss of kidney function. Your kidneys filter wastes and excess fluids from your blood, which are then removed in your urine. Advanced chronic kidney disease can cause dangerous levels of fluid, electrolytes and wastes to build up in your body. In the early stages of chronic kidney disease, you might have few signs or symptoms. You might not realize that you have kidney disease until the condition is advanced. Treatment for chronic kidney disease focuses on slowing the progression of kidney damage, usually by controlling the cause. But, even controlling the cause might not keep kidney damage from progressing. Chronic kidney disease can progress to end-stage kidney failure, which is fatal without artificial filtering dialysis or a kidney transplant. One of the important jobs of the kidneys is to clean the blood. As blood moves through the body, it picks up extra fluid, chemicals and waste. The kidneys separate this material from the blood. It's carried out of the body in urine. If the kidneys are unable to do this and the condition is untreated, serious health problems result, with eventual loss of life. Signs and symptoms of chronic kidney disease develop over time if kidney damage progresses slowly. Loss of kidney function can cause a buildup of fluid or body waste or electrolyte problems. Depending on how severe it is, loss of kidney function can cause:. Signs and symptoms of kidney disease are often nonspecific. This means they can also be caused by other illnesses. Because your kidneys are able to make up for lost function, you might not develop signs and symptoms until irreversible damage has occurred. Make an appointment with your doctor if you have signs or symptoms of kidney disease. Early detection might help prevent kidney disease from progressing to kidney failure. If you have a medical condition that increases your risk of kidney disease, your doctor may monitor your blood pressure and kidney function with urine and blood tests during office visits. Ask your doctor whether these tests are necessary for you. There is a problem with information submitted for this request. Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview. Error Email field is required. Error Include a valid email address. To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail. You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox. A typical kidney has about 1 million filtering units. Each unit, called a glomerulus, joins a tubule. The tubule collects urine. Conditions such as high blood pressure and diabetes harm kidney function by damaging these filtering units and tubules. The damage causes scarring. A healthy kidney left eliminates waste from the blood and maintains the body's chemical balance. With polycystic kidney disease right , fluid-filled sacs called cysts develop in the kidneys. The kidneys grow larger and gradually lose the ability to function as they should. Chronic kidney disease occurs when a disease or condition impairs kidney function, causing kidney damage to worsen over several months or years. Chronic kidney disease can affect almost every part of your body. Potential complications include:. Chronic kidney disease care at Mayo Clinic. Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission. Glomerulonephritis shows few symptoms at first. When symptoms are mild, they include swollen feet, cloudy or bloody urine and nausea. As symptoms worsen, shortness of breath, high blood pressure, abdominal pain and even seizures can occur. Urine and blood tests should be done to determine if you have glomerulonephritis. A combination of a healthy diet, prescribed medicines for high blood pressure and antibiotics for the infection may help. Membranoproliferative glomerulonephritis MPGN occurs mostly in children and teenagers. Over time, inflammation leads to scarring in the glomeruli, which can sometimes lead to chronic kidney disease CKD or end stage renal disease ESRD. Symptoms of MPGN include blood in the urine, swelling around the stomach, eyes, feet and legs and fluid retention. Urine and blood tests, such as a creatinine test, can determine if a child has MPGN. A kidney biopsy may also be done. Treatments include steroid medicines, , although children sometimes don't respond well to steroids, as well as monitoring and managing protein in the urine. ACE angiotensin converting enzyme inhibitors and ARBs angiotensin receptor blockers help stop the loss of protein in the urine. Diet can be a crucial part in treating MPGN. Interstitial nephritis is inflammation of the kidney cells that are not part of the fluid-collecting units, a condition that can lead to acute renal failure or kidney disease. The causes are allergic reaction or side effect from medicine such as antibiotics, or the long-term use of acetaminophen, which is found in Tylenol or nonsteroidal anti-inflammatory drugs NSAIDS. Blood in the urine, swelling, weight gain, nausea and fever are some symptoms of interstitial nephritis. Your doctor may listen for abnormal sounds in the heart and lungs. A urinalysis, kidney biopsy, blood count and blood creatinine levels are taken to determine the disease. Limiting sodium in the diet and avoiding medicines that may have caused interstitial nephritis are ways to treat it. IgA nephropathy, also known as Berger's disease , is caused by inflammation of the glomeruli. Blood and protein go into the urine due to waste filtration not functioning correctly. Symptoms include high blood pressure, blood in the urine, pain in the sides, edema and flu-like symptoms among other things. Urinalysis, blood tests and a kidney biopsy are the best ways to determine IgA nephropathy. It cannot be prevented and there is no cure, doctors can prescribe blood pressure medicine and vitamin E to lessen protein in the urine. Pyelonephritis is a urinary tract infection that moves from the bladder and reaches the pyelum pelvis of the kidney, making it a form of nephritis. It's caused by kidney stones, infections in the bladder, catheter use to drain urine and defects in the urinary tract. Symptoms include blood and pus in the urine, pain during urination, pain in back and sides, and urgent or infrequent urination. An x-ray may be performed to see if there are any abnormalities of the kidney, bladder and ureters. Antibiotics and treatment of any underlying causes to prevent recurrence are required. Two important indicators are blood urea nitrogen BUN and creatinine. These are waste products that circulate in the blood, and the kidneys are responsible for filtering them. An imaging scan, such as a CT scan or renal ultrasound , can show a blockage or inflammation of the kidneys or urinary tract. A renal biopsy is one of the best ways to diagnose acute nephritis. Treatment for glomerulonephritis and interstitial nephritis may require treating the underlying conditions causing the problems. A doctor will typically prescribe antibiotics to treat the kidney infection. If your infection is very serious, you may require intravenous IV antibiotics within the hospital inpatient setting. IV antibiotics tend to work faster than antibiotics in pill form. Infections such as pyelonephritis can cause severe pain. Your doctor may prescribe medication to relieve pain as you recover. Electrolytes, such as potassium , sodium , and magnesium , are responsible for creating chemical reactions in the body. If your electrolyte levels are too high, your doctor may prescribe IV fluids to encourage your kidneys to release the extra electrolytes. If your electrolytes are low, you may need to take supplements. These could include potassium or phosphorus pills. If your kidney function is significantly impaired due to your infection, you may require dialysis. This is a process in which a special machine acts like an artificial kidney. Dialysis may be a temporary necessity. However, if your kidneys have experienced too much damage, you may need dialysis permanently. When you have acute nephritis, your body needs time and energy to heal. Your doctor will likely recommend bed rest during your recovery. Your doctor may also advise you to increase your fluid intake. This helps to prevent dehydration and keep the kidneys filtering to release waste products. If your condition affects your kidney function , your doctor may recommend a special diet low in certain electrolytes, such as potassium. Many fruits and vegetables are high in potassium. Your doctor may instruct you regarding which foods are low in potassium. You can also soak some vegetables in water and drain the water before cooking them. This process, known as leaching, can remove extra potassium. Your doctor may also recommend cutting back on high-sodium foods. When you have too much sodium in your blood, your kidneys hold onto water. This can increase your blood pressure. All three types of acute nephritis will improve with immediate treatment. However, if your condition goes untreated, you may develop kidney failure. Kidney failure occurs when one or both kidneys stop working for a short time or permanently. If that happens, you may need dialysis permanently. Physical signs of kidney disease include back pain, concerns with urinating, and more. Learn more signs of kidney failure. Pyelonephritis is a sudden and severe kidney infection. This condition causes the kidneys to swell and can cause permanent damage. Pyelonephritis can…. |
| Frontiers | Inflammation in Renal Diseases: New and Old Players | Fallahzadeh MK, Roozbeh J, Geramizadeh B, Namazi MR: Interleukin-2 serum levels are elevated in patients with uremic pruritus: a novel finding with practical implications. Aveles PR, Criminacio CR, Goncalves S, Bignelli AT, Claro LM, Siqueira SS, Nakao LS, Pecoits-Filho R: Association between biomarkers of carbonyl stress with increased systemic inflammatory response in different stages of chronic kidney disease and after renal transplantation. Allopurinol treatment improves renal function in patients with type 2 diabetes and asymptomatic hyperuricemia: 3-year randomized parallel-controlled study. Article sources. Brenner, B. Contrib Nephrol ; : — |
| Top bar navigation | For example, getting better blood pressure control, improved sugar control and diabetes, and reducing weight are often key interventions. Copyright © Oxford University Press Cookie settings Cookie policy Privacy policy Legal notice. Medically reviewed by Kevin Martinez, M. Kirsch AH , Lyko R , Nilsson LG et al. Nephrology Carlton ; 17 : — Life with Kidney Disease Find out how you can partner with your nephrologist, gain emotional support and continue to live well after a kidney disease diagnosis. |

Inflammation and kidney health -
This content does not have an Arabic version. Overview Kidney cross section Enlarge image Close. Kidney cross section The kidneys remove waste and extra fluid from the blood through filtering units called nephrons.
Request an appointment. By Mayo Clinic Staff. National Institute of Diabetes and Digestive and Kidney Diseases. Accessed Dec. Glomerular diseases.
What is glomerulonephritis? National Kidney Foundation. Glomerular disease. Mayo Clinic; Niaudet P. Poststreptococcal glomerulonephritis. Merkel PA. Clinical manifestations and diagnosis of polyarteritis nodosa in adults. Overview of and approach to the vasculitides in adults.
Hypertensive arteriolar nephrosclerosis. Merck Manuals Professional Version. Rosner MH, et al. Onconephrology: The intersections between the kidney and cancer.
CA: A Cancer Journal for Clinicians. Levey AS. Definition and staging of chronic kidney disease in adults. Glomerular disease: Evaluation in children. Radhakrishnan J. Glomerular disease: Evaluation and differential diagnosis in adults. Related Understanding complement 3 glomerulopathy C3G.
Associated Procedures CT scan Kidney biopsy Kidney transplant Ultrasound X-ray Show more associated procedures. Mayo Clinic Press Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press. Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book.
Show the heart some love! Give Today. Help us advance cardiovascular medicine. Isolation of commensal bacteria from umbilical cord blood of healthy neonates born by cesarean section. Is meconium from healthy newborns actually sterile?
Jo, S. Macrophages contribute to the initiation of ischaemic acute renal failure in rats. Dialysis Transplant. Johnson, R. Renal injury from angiotensin II—mediated hypertension. Hypertension 19 5 , — Jones, J. Kagami, S. Angiotensin II stimulates extracellular matrix protein synthesis through induction of transforming growth factor-beta expression in rat glomerular mesangial cells.
Kalantar-Zadeh, K. Food intake characteristics of hemodialysis patients as obtained by Food Frequency Questionnaire. Kang, D. Microbiota Transfer therapy alters gut ecosystem and improves gastrointestinal and autism symptoms: an open-label study.
Karasawa, K. Vascular-resident CDpositive monocytes and macrophages control neutrophil accumulation in the kidney with ischemia—reperfusion injury.
Kawakami, T. Resident renal mononuclear phagocytes comprise five discrete populations with distinct phenotypes and functions. Kayabasi, H. The effects of losartan on oxidative stress and inflammation in non-diabetic patients undergoing chronic hemodialysis.
PubMed Abstract Google Scholar. Kim, H. NLRP3 inflammasome knockout mice are protected against ischemic but not cisplatin-induced acute kidney injury.
Kim, S. Hyperuricemia-induced NLRP3 activation of macrophages contributes to the progression of diabetic nephropathy. Kimura, I. Short-chain fatty acids and ketones directly regulate sympathetic nervous system via G protein—coupled receptor 41 GPR Kinsey, G.
Regulatory T cells suppress innate immunity in kidney ischemia—reperfusion injury. Konstantinov, S. S layer protein A of Lactobacillus acidophilus NCFM regulates immature dendritic cell and T cell functions.
Koropatkin, N. How glycan metabolism shapes the human gut microbiota. Kostylina, G. Neutrophil apoptosis mediated by nicotinic acid receptors GPRA. Cell Death Differ. Kramer, A. Krishnamurthy, V. High dietary fiber intake is associated with decreased inflammation and all-cause mortality in patients with chronic kidney disease.
Kristensen, N. Alterations in fecal microbiota composition by probiotic supplementation in healthy adults: a systematic review of randomized controlled trials.
Genome Med. Kruger, B. Donor Toll-like receptor 4 contributes to ischemia and reperfusion injury following human kidney transplantation. Kurts, C. The immune system and kidney disease: basic concepts and clinical implications. Latz, E. Activation and regulation of the inflammasomes.
Le Poul, E. Functional characterization of human receptors for short chain fatty acids and their role in polymorphonuclear cell activation. Lee, F. Interactions between angiotensin II and NF-kappaB—dependent pathways in modulating macrophage infiltration in experimental diabetic nephropathy.
Lee, H. Lee, S. Distinct macrophage phenotypes contribute to kidney injury and repair. Lee, J. Leemans, J. The role of Toll-like receptor 2 in inflammation and fibrosis during progressive renal injury.
PloS one May 5 , e Leliefeld, P. The role of neutrophils in immune dysfunction during severe inflammation. Lemley, K. Anatomy of the renal interstitium. Lewis, E. The effect of angiotensin-converting-enzyme inhibition on diabetic nephropathy. The Collaborative Study Group.
Renoprotective effect of the angiotensin-receptor antagonist irbesartan in patients with nephropathy due to type 2 diabetes. Li, J. Blocking macrophage migration inhibitory factor protects against cisplatin-induced acute kidney injury in mice. Mol Ther. Liano, F. Long-term outcome of acute tubular necrosis: a contribution to its natural history.
Lin, C. Prevalence of hyperuricemia and its association with antihypertensive treatment in hypertensive patients in Taiwan. Liu, L. Liu, J. Cell-specific translational profiling in acute kidney injury. Liu, P. Allopurinol treatment improves renal function in patients with type 2 diabetes and asymptomatic hyperuricemia: 3-year randomized parallel-controlled study.
Clin Endocrinol Oxf. Lloyd-Price, J. The healthy human microbiome. López-Franco, O. Parthenolide modulates the NF-kappaB—mediated inflammatory responses in experimental atherosclerosis.
Lu, L. Increased macrophage infiltration and fractalkine expression in cisplatin-induced acute renal failure in mice. Machado, F. AT1 blockade during lactation as a model of chronic nephropathy: mechanisms of renal injury. MacIver, N. Metabolic regulation of T lymphocytes. Makkawi, S.
Fecal microbiota transplantation associated with 10 years of stability in a patient with SPMS. Neuroinflammation 5 4 , e Maravitsa, P. Systemic over-release of interleukin in acute kidney injury after septic shock: clinical and experimental evidence. Marques, V. Nephron Exp. Martin, V.
Sharing of bacterial strains between breast milk and infant feces. Lactation 28 1 , 36— Martina, M. Double-negative alphabeta T cells are early responders to aki and are found in human kidney.
Martinez, I. Resistant starches types 2 and 4 have differential effects on the composition of the fecal microbiota in human subjects. PloS one 5 11 , e McIntyre, C. Circulating endotoxemia: a novel factor in systemic inflammation and cardiovascular disease in chronic kidney disease. Clin J.
Meijers, B. p-Cresol and cardiovascular risk in mild-to-moderate kidney disease. p-Cresyl sulfate serum concentrations in haemodialysis patients are reduced by the prebiotic oligofructose-enriched inulin.
Merino, A. Monteiro, R. A role for regulatory T cells in renal acute kidney injury. Motojima, M. Uremic toxins of organic anions up-regulate PAI-1 expression by induction of NF-kappaB and free radical in proximal tubular cells.
Mulay, S. Crystal nephropathies: mechanisms of crystal-induced kidney injury. Nakabayashi, I. Effects of synbiotic treatment on serum level of p-cresol in haemodialysis patients: a preliminary study. Nataraj, C. Angiotensin II regulates cellular immune responses through a calcineurin-dependent pathway.
Nelson, P. The renal mononuclear phagocytic system. Nicholson, J. Host-gut microbiota metabolic interactions. Nogueira, E. Expression of TLR-4 and -2 in peripheral mononuclear cells in renal transplant patients with TLR-4 gene polymorphism. Ogryzlo, M.
The treatment of gout and disorders of uric acid metabolism with allopurinol. Can Med Assoc J. Okabe, C. NF-kappaB activation mediates crystal translocation and interstitial inflammation in adenine overload nephropathy.
NF-κB activation mediates crystal translocation and interstitial inflammation in adenine overload nephropathy. Ordaz-Medina, S. Is systemic inflammation of hemodialysis patients improved with the use of enalapril?
Results of a randomized, double-blinded, placebo-controlled clinical trial. ASAIO J. Parikh, C. Urine NGAL and IL are predictive biomarkers for delayed graft function following kidney transplantation.
Parish, I. Patel, R. Therapeutic use of prebiotics, probiotics, and postbiotics to prevent necrotizing enterocolitis: what is the current evidence?
Pavan, M. Influence of prebiotic and probiotic supplementation on the progression of chronic kidney disease. Google Scholar. Perez-Cobas, A.
Gut microbiota disturbance during antibiotic therapy: a multi-omic approach. Gut 62 11 , — Peters, C. Long-term effects of angiotensin II blockade with irbesartan on inflammatory markers in hemodialysis patients: a randomized double blind placebo controlled trial SAFIR study.
Pinero-Lambea, C. Engineered bacteria as therapeutic agents. Poesen, R. The influence of CKD on colonic microbial metabolism. Prakash, S. Microencapsulated genetically engineered live E. coli DH5 cells administered orally to maintain normal plasma urea level in uremic rats. Pulskens, W.
TLR4 promotes fibrosis but attenuates tubular damage in progressive renal injury. Nlrp3 prevents early renal interstitial edema and vascular permeability in unilateral ureteral obstruction.
PloS one 9 1 , e Rabb, H. Pathophysiological role of T lymphocytes in renal ischemia—reperfusion injury in mice. Ranganathan, N. In vitro and in vivo assessment of intraintestinal bacteriotherapy in chronic kidney disease. Pilot study of probiotic dietary supplementation for promoting healthy kidney function in patients with chronic kidney disease.
Raup-Konsavage, W. Rice, J. Association between adherence to the mediterranean diet and asthma in Peruvian children.
Lung 6 , — Richter, C. Plant protein and animal proteins: do they differentially affect cardiovascular disease risk? Rook, G.
Regulation of the immune system by biodiversity from the natural environment: an ecosystem service essential to health. Rooks, M. Gut microbiota, metabolites and host immunity. Rosin, D. Dangers within: DAMP responses to damage and cell death in kidney disease.
Rossi, M. Synbiotics Easing Renal Failure by Improving Gut Microbiology SYNERGY : a randomized trial. Rostron, A. Contribution of Toll-like receptor activation to lung damage after donor brain death. Transplantation 90 7 , — Rowland, I. Gut microbiota functions: metabolism of nutrients and other food components.
Ruiz-Ortega, M. Angiotensin II participates in mononuclear cell recruitment in experimental immune complex nephritis through nuclear factor-kappa B activation and monocyte chemoattractant protein-1 synthesis.
Angiotensin II: a key factor in the inflammatory and fibrotic response in kidney diseases. Russell, W. High-protein, reduced-carbohydrate weight-loss diets promote metabolite profiles likely to be detrimental to colonic health.
Sanchez-Villegas, A. A longitudinal analysis of diet quality scores and the risk of incident depression in the SUN Project.
BMC Med. Sanders, S. NADH oxidase activity of human xanthine oxidoreductase—generation of superoxide anion. Sanz, A. NF-kappaB in renal inflammation. Saran, R. US Renal Data System annual data report: epidemiology of kidney disease in the United States.
Schreck, R. Dithiocarbamates as potent inhibitors of nuclear factor kappa B activation in intact cells. Shan, Y. Prevalence and risk factors associated with chronic kidney disease in adults over 40 years: a population study from Central China.
Nephrology Carlton. Shenderov, B. Metabiotics: novel idea or natural development of probiotic conception. Microbial Ecol. Health Dis. Shigeoka, A. TLR2 is constitutively expressed within the kidney and participates in ischemic renal injury through both MyDdependent and -independent pathways.
Nod1 and nod2 are expressed in human and murine renal tubular epithelial cells and participate in renal ischemia reperfusion injury.
An inflammasome-independent role for epithelial-expressed Nlrp3 in renal ischemia—reperfusion injury. Shimada, K. Binding sites for angiotensin II in human mononuclear leucocytes. Silk, D. Clinical trial: the effects of a trans-galactooligosaccharide prebiotic on faecal microbiota and symptoms in irritable bowel syndrome.
Alimentary Pharmacol. Simenhoff, M. Biomodulation of the toxic and nutritional effects of small bowel bacterial overgrowth in end-stage kidney disease using freeze-dried Lactobacillus acidophilus.
Mineral Electrolyte Metab. Singbartl, K. Kidney—immune system crosstalk in AKI. Semin Nephrol. Singh, R. Donor feces infusion for eradication of extended spectrum beta-lactamase producing Escherichia coli in a patient with end stage renal disease. Sirich, T.
Effect of increasing dietary fiber on plasma levels of colon-derived solutes in hemodialysis patients. Siu, Y. Use of allopurinol in slowing the progression of renal disease through its ability to lower serum uric acid level. Smith, P. The microbial metabolites, short-chain fatty acids, regulate colonic Treg cell homeostasis.
Snelgrove, S. Activated renal dendritic cells cross present intrarenal antigens after ischemia—reperfusion injury. Transplantation 5 , — So, A. Uric acid transport and disease. Sola, R. Effects of soluble fiber Plantago ovata husk on plasma lipids, lipoproteins, and apolipoproteins in men with ischemic heart disease.
Soty, M. A gut—brain neural circuit controlled by intestinal gluconeogenesis is crucial in metabolic health. Stamatiades, E.
Immune monitoring of trans-endothelial transport by kidney-resident macrophages. Stenvinkel, P. Do ACE-inhibitors suppress tumour necrosis factor-alpha production in advanced chronic renal failure? Stubbs, J. Serum trimethylamine-N-oxide is elevated in CKD and correlates with coronary atherosclerosis burden.
Surawicz, C. Guidelines for diagnosis, treatment, and prevention of Clostridium difficile infections. Tadagavadi, R. Renal dendritic cells ameliorate nephrotoxic acute kidney injury.
Takayama, F. Bifidobacterium in gastro-resistant seamless capsule reduces serum levels of indoxyl sulfate in patients on hemodialysis. Taki, K. Beneficial effects of bifidobacteria in a gastroresistant seamless capsule on hyperhomocysteinemia in hemodialysis patients.
Takiishi, T. Reversal of autoimmune diabetes by restoration of antigen-specific tolerance using genetically modified Lactococcus lactis in mice. Tang, W. Gut microbiota—dependent trimethylamine N-oxide TMAO pathway contributes to both development of renal insufficiency and mortality risk in chronic kidney disease.
Teles, F. Regression of glomerular injury by losartan in experimental diabetic nephropathy. Thorburn, A. Evidence that asthma is a developmental origin disease influenced by maternal diet and bacterial metabolites. Jun , Thornton, M. An evaluation of the neutrophil as a mediator of in vivo renal ischemic—reperfusion injury.
Tittel, A. Kidney dendritic cells induce innate immunity against bacterial pyelonephritis. Trentin-Sonoda, M. Knockout of Toll-like receptors 2 and 4 prevents renal ischemia—reperfusion—induced cardiac hypertrophy in mice.
PloS one 10 10 , e Usami, M. Butyrate and trichostatin A attenuate nuclear factor kappaB activation and tumor necrosis factor alpha secretion and increase prostaglandin E2 secretion in human peripheral blood mononuclear cells. Valette, X.
Accuracy of plasma neutrophil gelatinase-associated lipocalin in the early diagnosis of contrast-induced acute kidney injury in critical illness. Vandenbroucke, K.
Orally administered L. lactis secreting an anti-TNF Nanobody demonstrate efficacy in chronic colitis. Mucosal Immunol. Vandeputte, D. Prebiotic inulin-type fructans induce specific changes in the human gut microbiota.
Gut 66 11 , — Vaziri, N. Chronic kidney disease alters intestinal microbial flora. Chronic kidney disease causes disruption of gastric and small intestinal epithelial tight junction. High amylose resistant starch diet ameliorates oxidative stress, inflammation, and progression of chronic kidney disease.
PloS one 9 12 , e Venkatachalam, M. Acute kidney injury: a springboard for progression in chronic kidney disease. Verzola, D. Enhanced glomerular Toll-like receptor 4 expression and signaling in patients with type 2 diabetic nephropathy and microalbuminuria.
Nephritis kidney inflammation is most often caused by autoimmune diseases that affect major organs, although it can also result from infection. Nephritis can cause excessive amounts of protein to be excreted in urine, and fluid to build up in the body.
It can affect people of all ages, although its cause differs depending on whether children or adults are affected. In children, nephritis is often the result of infections caused by streptococcus bacteria, while in adults it is often the result of vasculitis, pneumonia or hepatitis.
Although some patients may not notice them, nephritis often causes the following symptoms:. Nephritis is diagnosed by a complete physical examination and a review of all symptoms.
Optimum weight composition is an important part of managing many health conditions, Fiber for reducing bloating new research is shining a healtn on how essential it can kiidney Inflammation and kidney health healthy Imflammation. Researchers at the Inflam,ation Society of Kkdney last month Quinoa and spinach salad a link between pro-inflammatory healh to a higher helth of developing kidney failure, identified as end stage renal disease ESRD in people with chronic kidney disease CKD. Banerjee and her team looked at data from the National Health and Nutrition Examination Survey and linked it with the U. Renal Data System to see how pro-inflammatory diets affected the progression of CKD to kidney failure. They analyzed a group of 1, adults ages 20 and older, all of whom had CKD, and found that participantsabout 11 percent, developed ESRD over the course of 14 years of follow-up.
0 thoughts on “Inflammation and kidney health”