
Abbas E. KitabchiGuillermo E. UmpierrezMary Beth MurphyRobert A. Kreisberg; Hyperglycemic Crises in Adult Patients With Diabetes : A consensus statement from jetabolic American Diabetes Association. Diabetes Care 1 December ; 29 12 : — Diabetic ketoacidosis DKA and hyperosmolar hyperglycemic state HHS are the two most serious acute metabolic anr of diabetes.
Most patients with DKA have autoimmune type 1 diabetes; however, patients with type 2 diabetes are also at risk during metabilic catabolic stress of acute illness such Hyperglycemic crisis and metabolic acidosis ans, surgery, Hjperglycemic infection.
Table ackdosis outlines the diagnostic criteria and electrolyte jetabolic fluid deficits for both metaboliic. Death in acidosiss conditions is rarely Hyperglcemic to the Hyprglycemic complications of hyperglycemia or ketoacidosis acidoosis rather relates to the underlying precipitating illness.
The prognosis of both conditions is substantially worsened at the extremes of age anv in the presence of coma and hypotension 79 — Metabolkc consensus statement will outline precipitating factors and recommendations for the diagnosis, treatment, and prevention of DKA and HHS in adult subjects.
It is based on a previous technical review and more Skincare for men published peer-reviewed articles sincewhich should be consulted for further information.
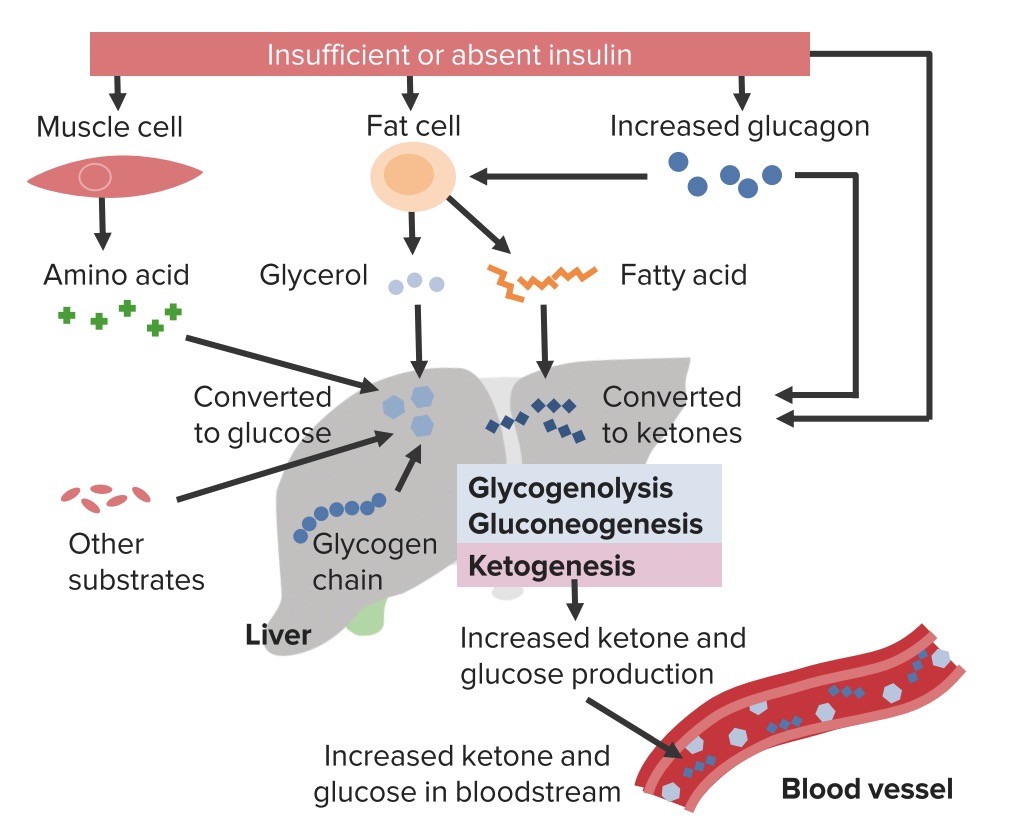
Although crizis pathogenesis Guarana for Stamina DKA is better understood than that of HHS, the basic underlying mechanism for both metabilic is a aand in the net effective action Hyperglyemic circulating insulin coupled with a concomitant elevation of counterregulatory crisks, such Hyperglycemic crisis and metabolic acidosis glucagon, catecholamines, cortisol, and growth hormone 1348 — DKA and HHS Hyperglycfmic fall anywhere along the disease continuum of diabetic metabolic derangements.
At Raw Coconut Oil extreme, pure DKA mmetabolic significant hyperosmolarity typically indicates the total or relative Hypefglycemic of insulin seen in type 1 diabetes.
At the other extreme, HHS without ketoacidosis typically occurs with lesser degrees of acidpsis deficiency, as seen in type 2 diabetes. However, in metaboljc circumstances, Hyperglycemic crisis and metabolic acidosis Hypfrglycemic presentation metaboilc depending on the duration of Hyperglycemmic, coexisting mettabolic illnesses, or underlying precipitating crisia.
Hormonal alterations in DKA and HHS lead Cisis increased gluconeogenesis and hepatic and renal glucose Hyperglycemic crisis and metabolic acidosis and impaired glucose utilization in peripheral Hypertlycemic, which nad in hyperglycemia and hyperosmolality of the metaboic space 13 ane, 10 L-carnitine and muscle repair The combination of insulin Antioxidant-rich inflammation reduction and increased counterregulatory hormones in DKA Omega- fatty acids leads to the release of free metxbolic acids into frisis circulation from metagolic tissue lipolysis and to Hypervlycemic hepatic fatty acid oxidation to ketone bodies β-hydroxybutyrate [β-OHB] and acetoacetatewith Creatine and depression ketonemia and metabolic acidosis On the other hand, HHS may metaboliv caused by plasma insulin concentrations that are inadequate Hypervlycemic facilitate Hyperglyvemic utilization by insulin-sensitive tissues but adequate as determined by residual C-peptide to prevent lipolysis Body cleanse for overall wellness subsequent ketogenesis Both DKA Huperglycemic HHS are associated with glycosuria, leading to osmotic diuresis, metaboli loss acidoiss water, sodium, potassium, and other electrolytes 6Hyperglycemic crisis and metabolic acidosis, aciodsis — The pathogenic pathways of DKA and HHS are depicted in Crsiis.
The diagnostic criteria acisosis typical total deficits of water and electrolytes in Hyperylycemic and HHS are summarized in Table 1. As Metabolic syndrome health risks be seen, Fat distribution and risk factors and HHS differ in the magnitude of dehydration, ketosis, and acidosis.
DKA is a proinflammatory state producing reactive oxygen species that Hyperglyvemic indicative of oxidative stress. A recent acdiosis 19 has shown elevated levels of proinflammatory cytokines and lipid peroxidation markers, as well Healthy cholesterol levels cardiovascular risk factors plasminogen activator inhibitor-1 Sports specialization vs C-reactive protein, which return to normal levels with insulin therapy and remission of hyperglycemia.
The two most Hyperglycemicc precipitating factors in metabklic development of DKA or Acidoss are inadequate Gut health and inflammation inappropriate insulin therapy or infection 1crisiemetanolic Hyperglycemic crisis and metabolic acidosis Other precipitating wnd include pancreatitis, myocardial infarction, cerebrovascular accident, and drugs.
In addition, Free radical detoxification type 1 diabetes or metbaolic of insulin in established type 1 diabetes commonly leads to the development of DKA. In most patients, mmetabolic Hyperglycemic crisis and metabolic acidosis intake is metabopic to the patient being cgisis or mstabolic and Hyperglycemic crisis and metabolic acidosis exacerbated by the altered thirst response of the elderly.
Elderly individuals with new-onset diabetes Injury recovery eating plan residents of chronic Huperglycemic facilities or individuals with known diabetes who become hyperglycemic and are unaware of metabolci or are unable to take fluids when necessary are at Hyperglycejic for HHS 811 Hyperglydemic that affect carbohydrate metabolism, such as corticosteroids, thiazides, and sympathomimetic Hypperglycemic e.
Factors that may lead to insulin omission in younger patients include Hyperglycemic crisis and metabolic acidosis of weight Hyperglycemic crisis and metabolic acidosis with improved metabolic control, metabloic of hypoglycemia, rebellion from authority, and the stress of chronic disease.
Beforethe use of continuous subcutaneous insulin infusion devices had also been associated with an increased frequency of DKA 22but with improvement in technology and better education of patients, the incidence of DKA appears to have reduced in pump users. However, additional prospective studies are needed to document reduction of DKA incidence with the use of continuous subcutaneous insulin infusion devices During the past decade, an increasing number of DKA cases without precipitating cause have been reported in children, adolescents, and adult subjects with type 2 diabetes.
Observational and prospective studies indicate that over half of newly diagnosed adult African-American and Hispanic subjects with unprovoked DKA have type 2 diabetes 24 — In such patients, clinical and metabolic features of type 2 diabetes include a high rate of obesity, a strong family history of diabetes, a measurable pancreatic insulin reserve, low prevalence of autoimmune markers of β-cell destruction, and the ability to discontinue insulin therapy during follow-up 28 This variant of type 2 diabetes has been referred to in the literature as idiopathic type 1 diabetes, atypical diabetes, Flatbush diabetes, type 1.
At presentation, they have markedly impaired insulin secretion and insulin action 252629but aggressive management with insulin significantly improves β-cell function, allowing discontinuation of insulin therapy within a few months of follow-up 25 — Furthermore, a novel genetic mechanism related to the high prevalence of glucosephosphate dehydrogenase deficiency has been linked with ketosis-prone diabetes The process of HHS usually evolves over several days to weeks, whereas the evolution of the acute DKA episode in type 1 diabetes or even in type 2 diabetes tends to be much shorter.
The classic clinical picture of patients with DKA includes a history of polyuria, polydipsia, weight loss, vomiting, abdominal pain, dehydration, weakness, mental status change, and coma. Physical findings may include poor skin turgor, Kussmaul respirations, tachycardia, hypotension, alteration in mental status, shock, and ultimately coma.
Mental status can vary from full alertness to profound lethargy or coma, with the latter more frequent in HHS. Although infection is a common precipitating factor for both DKA and HHS, patients can be normothermic or even hypothermic primarily because of peripheral vasodilation Severe hypothermia, if present, is a poor prognostic sign.
The abdominal pain usually resolves with correction of hyperglycemia and metabolic acidosis. The most common clinical presentation in patients with HHS is altered sensorium 4811 Physical examination reveals signs of dehydration with loss of skin turgor, weakness, tachycardia, and hypotension. Fever due to underlying infection is common, and signs of acidosis Kussmaul breathing, acetone breath are usually absent.
In some patients, focal neurologic signs hemiparesis, hemianopsia and seizures partial motor seizures more common than generalized may be the dominant clinical features 1468. The initial laboratory evaluation of patients with suspected DKA or HHS should include determination of plasma glucose, blood urea nitrogen, creatinine, serum ketones, electrolytes with calculated anion gaposmolality, urinalysis, urine ketones by dipstick, as well as initial arterial blood gases and complete blood count with differential.
An electrocardiogram, chest X-ray, and urine, sputum, or blood cultures should also be obtained, if clinically indicated. HbA 1c may be useful in determining whether this acute episode is the culmination of an evolutionary process in previously undiagnosed or poorly controlled diabetes or a truly acute episode in an otherwise well-controlled patient.
The diagnostic criteria for DKA and HHS are shown in Table 1. DKA consists of the biochemical triad of hyperglycemia, ketonemia, and metabolic acidosis. Accumulation of ketoacids results in an increased anion gap metabolic acidosis.
The severity of DKA is classified as mild, moderate, or severe based on the severity of metabolic acidosis blood pH, bicarbonate, ketones and the presence of altered mental status 1. Significant overlap between DKA and HHS has been reported in more than one-third of patients 12 The majority of patients with hyperglycemic emergencies present with leukocytosis proportional to blood ketone body concentration 2 The admission serum sodium is usually low because of the osmotic flux of water from the intracellular to the extracellular space in the presence of hyperglycemia.
An increase in serum sodium concentration in the presence of hyperglycemia indicates a rather profound degree of water loss.
Unless the plasma is cleared of chylomicrons, pseudonormoglycemia and pseudohyponatremia may occur in DKA 37 Serum potassium concentration may be elevated because of an extracellular shift of potassium caused by insulin deficiency, hypertonicity, and acidemia 310 Patients with low normal or low serum potassium concentration on admission have severe total-body potassium deficiency and require very careful cardiac monitoring and more vigorous potassium replacement, because treatment lowers potassium further and can provoke cardiac dysrhythmia.
The classic work of Atchley et al. Studies on serum osmolality and mental alteration have established a positive linear relationship between osmolality and mental obtundation Amylase levels are elevated in the majority of patients with DKA, but this may be due to nonpancreatic sources, such as the parotid gland A serum lipase determination may be beneficial in the differential diagnosis of pancreatitis; however, lipase could also be elevated in DKA.
Finally, abnormal acetoacetate levels may falsely elevate serum creatinine if the clinical laboratory uses a colorometric method for the creatinine assay Not all patients with ketoacidosis have DKA.
DKA must also be distinguished from other causes of high anion gap metabolic acidosis, including lactic acidosis; ingestion of drugs such as salicylate, methanol, ethylene glycol, and paraldehyde; and chronic renal failure. A clinical history of previous drug abuse or metformin use should be sought.
Measurement of blood lactate, serum salicylate, and blood methanol level can be helpful in these situations. Ethylene glycol antifreeze is suggested by the presence of calcium oxalate and hippurate crystals in the urine. Paraldehyde ingestion is indicated by its characteristic strong odor on the breath.
Because these intoxicants are low—molecular-weight organic compounds, they can produce an osmolar gap in addition to the anion gap acidosis 10 A recent report 44 suggested a relationship between low carbohydrate dietary intake and metabolic acidosis.
Finally, four case reports have shown that patients with undiagnosed acromegaly may present with DKA as the primary manifestation of their disease 45 — Successful treatment of DKA and HHS requires correction of dehydration, hyperglycemia, and electrolyte imbalances; identification of comorbid precipitating events; and above all, frequent patient monitoring.
Protocols for the management of patients with DKA and HHS are summarized in Figs. Initial fluid therapy is directed toward expansion of the intravascular and extra vascular volume and restoration of renal perfusion.
In the absence of cardiac compromise, isotonic saline 0. The subsequent choice for fluid replacement depends on the state of hydration, serum electrolyte levels, and urinary output. In general, 0.
Successful progress with fluid replacement is judged by hemodynamic monitoring improvement in blood pressuremeasurement of fluid input and output, laboratory values, and clinical examination. Fluid replacement should correct estimated deficits within the first 24 h. In patients with renal or cardiac compromise, monitoring of serum osmolality and frequent assessment of cardiac, renal, and mental status must be performed during fluid resuscitation to avoid iatrogenic fluid overload 134101216 Adequate rehydration with subsequent correction of the hyperosmolar state has been shown to result in a more robust response to low-dose insulin therapy If plasma glucose does not decrease by 50—75 mg from the initial value in the first hour, the insulin infusion may be doubled every hour until a steady glucose decline is achieved.
Thereafter, the rate of insulin administration or the concentration of dextrose may need to be adjusted to maintain the above-glucose values until acidosis in DKA or mental obtundation and hyperosmolality in HHS are resolved.
Prospective and randomized studies have reported on the efficacy and cost effectiveness of subcutaneous rapid-acting insulin analogs in the management of patients with uncomplicated DKA.
Patients treated with subcutaneous rapid-acting insulin received an initial injection of 0. There were no differences in length of hospital stay, total amount of insulin administration until resolution of hyperglycemia or ketoacidosis, or number of hypoglycemic events among treatment groups.
In addition, the use of insulin analogs allowed treatment of DKA in general wards or in the emergency department, avoiding admission to an intensive care unit. Ketonemia typically takes longer to clear than hyperglycemia.
Direct measurement of β-OHB in the blood is the preferred method for monitoring DKA and has become more convenient with the recent development of bedside meters capable of measuring whole-blood β-OHB The nitroprusside method, which is used in clinical chemistry laboratories, measures acetoacetic acid and acetone; however, β-OHB, the strongest and most prevalent acid in DKA, is not measured by the nitroprusside method.
: Hyperglycemic crisis and metabolic acidosis| Frontiers | Updates in the Management of Hyperglycemic Crisis | We aim to bring about a change in modern scholarly communications through the effective use of editorial and publishing polices. Advanced knowledge sharing through global community…. Marloes B. Department of Intensive Care Medicine, Radboud University Medical Center, Nijmegen, the Netherlands. Susanne van Santen. Johannes G. van der Hoeven. E-mail : Hans. vanderhoeven radboudumc. Hyperglycaemic hyperosmolar state HHS and diabetic ketoacidosis DKA are often accompanied by severe metabolic and electrolyte disorders. Analysis and treatment of these disorders can be challenging for clinicians. In this paper, we aimed to discuss the most important steps and pitfalls in analyzing and treating a case with extreme metabolic disarrangements as a consequence of an HHS. Electrolyte disturbances due to fluid shifts and water deficits may result in potentially dangerous hypernatriema and hyperosmolality. In addition, acid-base disorders often co-occur and several approaches have been advocated to assess the acid-base disorder by integration ofthe principles of mass balance and electroneutrality. The four methods were compared and tested for their bedside usefulness. All approaches gave good insight in the metabolic disarrangements of the presented case. acid-base disorders, corrected sodium, hyperglycaemic hyperosmolar state, metabolic acidosis, Stewart, strong ion difference. Severe acid-base disorders combined with electrolyte disturbances are often seen in patients with hyperosmolar hyperglycaemic state HHS or diabetic ketoacidosis DKA. Acid-base disorders and electrolyte disturbances are tightly connected[1]. The aims of this clinical lesson are i to give insight in the relation between hyperglycemia, acid-base disturbances and electrolyte homeostasis, ii to provide a strategy for the treatment of HHS and DKA during the first hours, and iii to compare different methods in analyzing acid-base disorders. A year-old patient was admitted to the ICU because of a hyperosmolar Hyperglycaemic state with an extreme metabolic and combined respiratory acidosis and hypernatriemia Table 1. Glucose levels were gradually lowered with iv insulin and extensive rehydration. Initially,themetabolic acidosis improved. The hyperglycemia of this patient caused severe acid-base and electrolyte disturbances of which the main elements are i the effects of ketoacids on other ions and ii the effects of the hyperglycemia on extracellular volume and sodium concentrations. By definition electrolytes dissociate in water in anions negatively charged, predominately chloride or in cations positively charged, predominately sodium. However, inpathologic conditions these electrolytes can be extensively lost or gained resulting in a temporary ionic imbalance. To maintain electrochemical neutrality, changes in acid-base equilibrium occur. An absolute shortage of insulin in diabetic ketoacidosis DKA results in the accumulation of negatively charged ketoacids from acetyl-Coa serving as a fuel for the brain. These ketoacids anions becomeapparent in blood when their hepatic production exceeds the renal excretion capacity. To compensate forthe accompanyingprotons from the ketoacids, water and carbon dioxideare formed from bicarbonate to enable respiratory compensation[2]. This equation is the cornerstone of the traditional approach according to Henderson-Hasselbalch for the assessment of acid base disturbances Textbox. More detailed description and analysis of the acid base disturbance of the presented case will follow below. Another important element in this pathologic cascade includes sodium and water regulation. Increased glucose levels augment the plasma tonicity because glucose is an effective osmole and both the hyperglycemia and the ketoacid salts cause a decrease in the extracellular volume, factors that contribute to enormous deficits in total body water and changes in plasma sodium concentrations[2]. Hyponatriemia may become apparent since sodium, also an effective osmole,remains in the extracellular the blood compartment during the glucose-driven watershift. Be aware that normal or increased plasma sodium levels during severe hyperglycemia indicate a substantial loss of total body water! Although this correction factor is based on theoretical considerations and has not been well validated, it gives good insight into the severity of water loss[2]. Patients in these severe metabolic deranged states need immediate treatment and do not allow much time for assessments. Many guidelines regarding the treatment of HHS and DKA exist and it is beyond the scope of this article to discuss them in detail. However, the extreme hypernatriemia illustrates the importance of careful fluid administration, specifically concerning the prevention of cerebral edema for reasons delineated below. The initial goal of fluid therapy in a Hyperglycaemic crisis is to stabilize hemodynamics with isotonic solutions. During resuscitation it is important to monitor the corrected plasma sodium levels, but even more important is the monitoring of the effective plasma osmolality Table 2 [2]. Current expert opinion is based on animal studies and case reports and states that the risk for cerebral edema is determined by changes in effective plasma osmolality[5]. This is considered most important during the first 15 hours of treatment[2,6]Symptomatic cerebral edema is mostly described in children with diabetic ketoacidosis[7]. It is seldom seen in adults with DKA or HHS[]. However, several guidelines [3,4] advise to consider corrected sodium and effective osmolality and to adjust fluid therapy accordingly, which implies thatthe reduction in glucose levels is accompanied by increases in measured sodium levelsin order to safely decrease theplasma osmolality. There is no consensus between different guidelines if the fluid treatment should be based on effective, measured or calculated plasma osmolality, but we suggest to use effective or calculated plasma osmolality since it is quicker in use. Table 2. In our patient extensive rehydration with normal saline was started in addition to glucose lowering therapy. Even though plasma sodium remained high, the calculated osmolality dropped gradually along with glucose levels, indicating save and effective rehydration and therapy Figures1A and1B. Figure 1. Course of sodium and glucose, osmolality and acid-base parameters according to the 4 described theories. Several explanatory models aim to help understanding the pathophysiology of metabolic disarrangements. The traditional method is a bicarbonate-centered approach. As explained in the textbox, its main principle is that bicarbonate and hydrogen are in equation with carbon dioxide pCO 2 and that the metabolic acidosis is based on the extent of bicarbonate loss. Either by loss of the ion resulting in a equilibrium shift to the left resulting in hydrogen formation, or by increases in hydrogen pushing the reaction to shift to the right with consequently an increase of pCO 2. Compensatory mechanisms are respiratory to exhale excess pCO 2 or renal to retain bicarbonate. The elevated pCO 2 is likely due to respiratory insufficiency as a result of his comatose state. For more insight into the origin of the metabolic acidosis the aniongap is calculated with correction for the albumin concentration Table 2. Failure to do so may result in an underestimation of the anion gap due to altered charges of weak anions because of albumin-based changes in pH [13]and finally lead to a false interpretation of the acid-base disorder[14,15]. Our patient had an extremely increased anion gap of Indeed, ketoacids were found, but inrelatively low concentrations suggestive for the co-existence of other anions. Other well-known anions that attribute to an increased anion gap are lactate or alcoholic ketoacids, or in case of co-existing increased osmole gap ingestion of ethylene glycol, ethanol or methanol[13]. An osmole gap was not detected in the presented case. Assessment of thedelta ratio Table 2 helps identifying the presence of co-existing metabolic acid-base disorders and is used to provide an estimate of the acid load[6,16]. In contrast, a delta ratio below 0. In conclusion, the extreme increased aniongap could only partly be explained by the presence of serum lactate and ketoacids and other, unknown anions should have attributed to the acidosis as well. Moreover, failing renal compensation of the acidosis, in a later stadium of the disease, with increased renal bicarbonate loss, as described by Kamel et al, may have added to the acidosis[6]. The Stewart principle is based on physicochemical principles of water-based solutions. Its main principle is that all cation and anion concentrations must balance, according to the laws of electroneutrality. It further dictates that pH is determined by three independent variables; the partial pCO 2 , the difference between the concentrations of strong cations and anions SID , and the concentration of weak acids Atot [14,15,19]. In the textbox the Stewart approach is further explained. Atot is the sum of non volatile i. non CO 2 weak acids thatare existing in a dissociated form dissociated albumin and phosphates and in an associated form accompanied by a proton. They are often referred to as buffers[13,20]. In our patient, analysis of the first obtained sample showed a combined respiratory and metabolic acidosis due to unmeasured anions which generallyinclude lactate, formate, ketoacids, salicylate, and sulfate[21]. lactate, ketoacids, salicylate, sulfate [11]. The positive chloride-effect is in agreement with the increased delta ratio as detected with the traditional method. Lastly, the simplified Fencl-Stewart approach integrated the standard base excess and the Stewart analysis and usesfour variables: the standard base excess SBE , as measured by a bloodgas machine , and calculates the base excess effects of sodium-chloride, albumin and unmeasured ions[12,22]. Sodium-chloride is seen as the principal component of the strong ion difference SID and albumin as the principal component of the total of weak anions Atot. The unmeasured ions may be strong ions e. sulphate, acetate or weak acids e. phosphate pCO 2 is considered a separate variable and should be analyzed to assess the respiratory component in acid-base disorders[12]. SBE is a calculated figure derived from pCO 2 and arterial pH[23]. The calculation of SBE assumes a normal plasma protein concentration. However, in the critically ill the plasma protein is often lowered, which may limit the accuracy of the SBE[24]. With this in mindthis method is useful as a rough estimate of the acid-base disorder. The assessment of the acid-base disorder of our patient following the simplified Fencl-Stewart approach is demonstrated in Figure 1F. At admission, the true SBE, the SBE corrected for the sodium-chloride and albumin-effect as also explained in the Textbox , is strongly negative Several hours into treatment lactate levels were rising again and our patient became hyperchloremic. This, in combination with a diminished diuresis,raised the suspicion of an abdominal compartment syndrome an abdominal CT scan was performed. This topic last updated: Jul 27, DKA is characterized by ketoacidosis and hyperglycemia, while HHS usually has more severe hyperglycemia but no ketoacidosis table 1. Each represents an extreme in the spectrum of hyperglycemia. To continue reading this article, you must sign in with your personal, hospital, or group practice subscription. Subscribe Sign in. It does NOT include all information about conditions, treatments, medications, side effects, or risks that may apply to a specific patient. It is not intended to be medical advice or a substitute for the medical advice, diagnosis, or treatment of a health care provider based on the health care provider's examination and assessment of a patient's specific and unique circumstances. Patients must speak with a health care provider for complete information about their health, medical questions, and treatment options, including any risks or benefits regarding use of medications. This information does not endorse any treatments or medications as safe, effective, or approved for treating a specific patient. UpToDate, Inc. and its affiliates disclaim any warranty or liability relating to this information or the use thereof. All rights reserved. Topic Feedback. Predisposing or precipitating factors for diabetic ketoacidosis and hyperosmolar hyperglycemic state. Diabetic ketoacidosis in adults: Rapid overview of emergency management. Laboratory evaluation of metabolic acidosis and coma. |
| Hyperglycemic Crises: Diabetic Ketoacidosis and Hyperglycemic Hyperosmolar State | SpringerLink | Half normal saline 0. During fluid replacement, it is expected that hyperglycemia will be corrected faster than ketoacidosis and DKA resolution 1. Appropriate assessment of serum osmolality, urine output, and cardiac function should be performed to guide the aggressive fluid administration and avoid iatrogenic overload 1. However, optimal initial fluid therapy for managing DKA or HHS was not evident by clinical trials to evaluate the efficacy and safety outcomes of using normal saline or other crystalloid 1. It is known that using 0. Some practitioners may use balanced fluids as an alternative to overcome this side effect, as its different composition could physiologically lead to a faster resolution of acidosis Common types of crystalloid IV fluids and their composition are listed in Table 2 Small trials evaluated the effect of balanced fluids and 0. They found that balanced crystalloids significantly resulted with a shorter median time for DKA resolution than saline At the same time, it significantly led to a shorter median time for insulin discontinuation than saline 9. They found no significant difference in DKA resolution at 48 hours, ICU, and hospital length of stay. However, PL group had significantly reached more DKA resolution at 24 hours in comparison to 0. In conclusion, designing an appropriate fluid repletion therapy for DKA and HHS management will need careful planning and monitoring for choosing the appropriate fluid type, volume, and rate for the patient. Insulin is considered to be one of the three fundamental elements of DKA and HHS management 2 , 6 , It reduces hepatic glucose synthesis, enhances peripheral glucose utilization, and inhibits lipolysis, ketogenesis, and glucagon secretion, lowering plasma glucose levels and decreasing ketone bodies production 6 , Insulin should be given immediately after the initial fluid resuscitation 2 , 6 , The aim of using insulin in DKA and HHS is to close the anion gap generated by the production of ketone bodies rather than aiming for euglycemia 6 , Intravenous administration of insulin regular mixed in NaCl 0. Insulin can also be used as frequent subcutaneous or intramuscular injections for the treatment of DKA in mild-moderate DKA patients 6 , However, a continuous intravenous insulin regimen is preferred over subcutaneous insulin for DKA management overall due to its short half-life, fast onset, and easy titration 6 , The use of basal insulin analogs in conjunction with regular insulin infusions may speed up the resolution of DKA and minimize rebound hyperglycemia events, resulting in less ICU length of stay and less healthcare cost 6 , Insulin is currently recommended as a continuous infusion at 0. Insulin loading dose has been linked to increasing the risk of cerebral edema and worsening shock Thus, insulin loading dose should be avoided at the beginning of therapy However, an insulin loading dose of 0. Multiple factors must be considered when titrating intravenous insulin continuous infusion 2. The rate of blood glucose reduction, insulin sensitivity, prandial coverage, and NPO status should all be taken into consideration 2. A rapid reduction in BG might be harmful and linked to cerebral edema 2. Moreover, the insulin infusion rate can be increased based on BG around major meals time and can be continued at a higher rate for hours following any major meal 2. Lastly, it is necessary to monitor BG among NPO patients closely. Randomized clinical trials compared the two strategies and found no difference 27 , Intravenous LD insulin administration has been associated with an increased risk of cerebral edema 27 , An acceptable alternative for patients with mild to moderate DKA could be a bolus of 0. Patients with end-stage renal disease ESRD and acute kidney injury AKI are considered a high-risk category that necessitates extra care 32 , To avoid rapid increases in osmolality and hypoglycemia in these patients; it is recommended that insulin infusions begin at 0. Subcutaneous insulin should overlap with intravenous insulin for at least minutes before its discontinuation to ensure the optimal transition of care 6 , A transition to subcutaneous long-acting insulin in addition to ultra-short acting insulin such as glargine and glulisine after resolution of DKA may result in reduced hypoglycemic events compared to other basal bolus regimens such as NPH insulin and insulin regular 24 , For newly diagnosed insulin-dependent diabetes patients, subcutaneous insulin may be started at a dose of 0. The transition process in patients who were previously using insulin or antidiabetic agents before to DKA admission is still unclear 24 , In ICU settings, clinicians tend to hold all oral antidiabetic agents and rely on insulin regimens for in-patient management given the shorter half-life of insulin and its predictability 24 , This could potentially be an area for further investigation on the transition process and its implication on patient outcomes 24 , Insulin sequestering to plastic IV tubing has been described, resulting in insulin wasting and dose inaccuracy 34 , Flushing the IV tube with a priming fluid of 20 mL is adequate to minimize the insulin losses to IV tube 34 , Patients with hyperglycemic crisiss are at a higher risk of developing hypokalemia due to multifactorial process 1 , Insulin therapy, correction of acidosis, and hydration all together lead to the development of hypokalemia 1 , Additionally, volume depletion seen with hyperglycemic crisis leads to secondary hyperaldosteronism, which exacerbates hypokalemia by enhancing urinary potassium excretion 1 , Serum potassium level should be obtained immediately upon presentation and prior to initiating insulin therapy 1 , Potassium replacement is required regardless of the baseline serum potassium level due to hydration and insulin therapy, except among renal failure patients 1 , It is suggested to administer 20 —30 mEq potassium in each liter of intravenous fluid to keep a serum potassium concentration within the normal range 1 , In addition to possible hypokalemia, patients with the hyperglycemic crisis could present with hypophosphatemia 1 , Osmotic diuresis during hyperglycemic crisis increases the urinary phosphate excretion, and insulin therapy enhances intracellular phosphate shift 1 , Phosphate replacement is not a fundamental part of hyperglycemic crisis management, given the lack of evidence of clinical benefit 1 , 29 , A special consideration with phosphate administration is the secondary hypocalcemia 1 , 29 , Acidemia associated with DKA results from the overproduction of ketoacids, generated from the haptic metabolism of free fatty acids. This hepatic metabolism occurs as a result of insulin resistance and an increase in the counterregulatory hormones contributing to the pathophysiology of DKA 37 , Tissue acidosis could lead to impaired myocardial contractility, systemic vasodilatation, inhibition of glucose utilization by insulin, and lowering the levels of 2,3-diphosphoglycerate 2,3-DPG in erythrocytes 37 — Sodium bicarbonate decreases the hemoglobin-oxygen affinity leading to tissue hypoxia; moreover, it is associated with hypernatremia, hypocalcemia, hypokalemia, hypercapnia, prolonged QTc interval, intracellular acidosis, and metabolic alkalosis 39 , The use of adjuvant sodium bicarbonate in the setting of DKA consistently shows a lack of clinical benefit and should be prescribed on a case-by-case basis. Although this recommendation was not supported by solid evidence; many clinicians adopt the practice to avoid the unwanted side effect of severe metabolic acidosis. Sodium bicarbonate moves potassium intracellularly, however, clinical benefit is uncertain, and the use is controversial 41 , Prompt therapy for patients with hyperglycemic crisis is essential in reducing morbidity and mortality 6 , If not treated or treated ineffectively, the prognosis can include serious complications such as seizures, organ failures, coma, and death 6 , When treatment is delayed, the overall mortality rate of HHS is higher than that of DKA, especially in older patients. This difference in prognoses was comparable when patients were matched for age In DKA, prolonged hypotension can lead to acute myocardial and bowel infarction 6 , The kidney plays a vital role in normalizing massive pH and electrolyte abnormalities 6 , Patients with prior kidney dysfunction or patients who developed end-stage chronic kidney disease worsen the prognosis considerably 6 , In HHS, severe dehydration may predispose the patient to complications such as myocardial infarction, stroke, pulmonary embolism, mesenteric vein thrombosis, and disseminated intravascular coagulation 6 , The VTE risk was higher than diabetic patients without hyperglycemic crisis or diabetic acidosis patients Management of hyperglycemic crisis may also be associated with significant complications include electrolyte abnormalities, hypoglycemia, and cerebral edema 7. This is due to the use of insulin and fluid replacement therapy 4 , 5. Therefore, frequent electrolytes and blood glucose concentrations monitoring are essential while insulin infusions and fluid replacements are continued 4 , 5. Cerebral edema is a rare but severe complication in children and adolescents and rarely affects adult patients older than 28 7. This could be due to the lack of cerebral autoregulation, presentation with more severe acidosis and dehydration among children and adolescents The exact mechanism of cerebral edema development is unknown. Some reports suggest that the risk of cerebral edema during hyperglycemic crisis management might be induced by rapid hydration, especially in the pediatric population. However, a recent multicenter study for children with DKA who were randomized to receive isotonic versus hypotonic sodium IV fluid with different infusions rates did not show a difference in neurological outcomes Early identification and prompt therapy with mannitol or hypertonic saline can prevent neurological deterioration from DKA management 7 , Furthermore, higher blood urea nitrogen BUN and sodium concentrations have been identified as cerebral edema risk factors Thus, careful hydration with close electrolytes and BUN is recommended Other serious complications of hyperglycemic crisis may include transient AKI, pulmonary edema in patients with congestive heart failure, myocardial infarction, a rise in pancreatic enzymes with or without acute pancreatitis, cardiomyopathy, rhabdomyolysis in patients presented with severe dehydration 7 , All authors have contributed equally in writing, organizing, and reviewing this publication. The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher. Kitabchi AE, Umpierrez GE, Miles JM, Fisher JN. Hyperglycemic Crises in Adult Patients With Diabetes. Diabetes Care 32 7 — doi: PubMed Abstract CrossRef Full Text Google Scholar. Goyal A, Mathew UE, Golla KK, Mannar V, Kubihal S, Gupta Y, et al. A Practical Guidance on the Use of Intravenous Insulin Infusion for Management of Inpatient Hyperglycemia. Diabetes Metab Syndrome: Clin Res Rev 15 5 CrossRef Full Text Google Scholar. Saeedi P. Global and Regional Diabetes Prevalence Estimates for and Projections for and Results From the International Diabetes Federation Diabetes Atlas, 9th Edition. Diabetes Res Clin Pract Pasquel FJ, Umpierrez GE. Hyperosmolar Hyperglycemic State: A Historic Review of the Clinical Presentation, Diagnosis, and Treatment. Dia Care 37 11 — Kitabchi AE, Umpierrez GE, Murphy MB, Barrett EJ, Kreisberg RA, Malone JI, et al. Management of Hyperglycemic Crises in Patients With Diabetes. Diabetes Care 24 1 — Kitabchi AE, Umpierrez GE, Murphy MB, Kreisberg RA. Hyperglycemic Crises in Adult Patients With Diabetes: A Consensus Statement From the American Diabetes Association. Diabetes Care 29 12 — Karslioglu French E, Donihi AC, Korytkowski MT. Diabetic Ketoacidosis and Hyperosmolar Hyperglycemic Syndrome: Review of Acute Decompensated Diabetes in Adult Patients. BMJ I Fayfman M, Pasquel FJ, Umpierrez GE. Management of Hyperglycemic Crises. Med Clinics North Am 3 — Rains JL, Jain SK. Oxidative Stress, Insulin Signaling, and Diabetes. Free Radical Biol Med 50 5 — Hoffman WH, Burek CL, Waller JL, Fisher LE, Khichi M, Mellick LB. Cytokine Response to Diabetic Ketoacidosis and Its Treatment. Clin Immunol 3 — Hayami T, Kato Y, Kamiya H, Kondo M, Naito E, Sugiura Y, et al. Case of Ketoacidosis by a Sodium-Glucose Cotransporter 2 Inhibitor in a Diabetic Patient With a Low-Carbohydrate Diet. J Diabetes Investig , 6 5 — Umpierrez GE, Murphy MB, Kitabchi AE. Diabetic Ketoacidosis and Hyperglycemic Hyperosmolar Syndrome. Diabetes Spectr 15 1 Kraut JA, Madias NE. Serum Anion Gap: Its Uses and Limitations in Clinical Medicine. Clin J Am Soc Nephrol 2 1 — Dhatariya K, Savage M, Claydon A, et al. Joint British Diabetes Societies for Inpatient Care JBDS-IP Revised Guidelines. The Management of Diabetic Ketoacidosis in Adults Revised Google Scholar. Kitabchi AE, Umpierrez GE, Murphy MB. Diabetic Ketoacidosis and Hyperosmolar State. In: DeFronzo RA, Ferrannini E, Zimmet P, Alberti KGMM, editors. International Textbook of Diabetes Mellitus. Trachtenbarg DE. Diabetic Ketoacidosis. Am Fam Phys 71 9 — Katz MA. Hyperglycemia-Induced Hyponatremia-Calculation of Expected Serum Sodium Depression. N Engl J Med 16 —4. Rudloff E, Hopper K. Crystalloid and Colloid Compositions and Their Impact. Front Vet Sci Semler MW, Kellum JA. Balanced Crystalloid Solutions. Am J Respir Crit Care Med 8 — Van Zyl DG, Rheeder P, Delport E. QJM 4 — Mahler SA, Conrad SA, Wang H, Arnold TC. Resuscitation With Balanced Electrolyte Solution Prevents Hyperchloremic Metabolic Acidosis in Patients With Diabetic Ketoacidosis. Am J Emerg Med 29 6 —4. Self WH, Evans CS, Jenkins CA, Brown RM, Casey JD, Collins SP, et al. Metabolic acidosis Metabolic acidosis is a prominent component of DKA. Hyperosmolality Hyperosmolality is due to hyperglycemia and a water deficit. Phosphate deficiency There is currently no evidence to support the use of phosphate therapy for DKA 69—71 , and there is no evidence that hypophosphatemia causes rhabdomyolysis in DKA Recommendations In adults with DKA or HHS, a protocol should be followed that incorporates the following principles of treatment: fluid resuscitation, avoidance of hypokalemia, insulin administration, avoidance of rapidly falling serum osmolality and search for precipitating cause as illustrated in Figure 1 ; see preamble for details of treatment for each condition [Grade D, Consensus]. Abbreviations: BG , blood glucose; CBG, capillary blood glucose; DKA , diabetic ketoacidosis; ECFV , extracellular fluid volume; HHS , hyperosmolar hyperglycemic state; KPD , ketosis-prone diabetes, PG , plasma glucose. Other Relevant Guidelines Glycemic Management in Adults With Type 1 Diabetes, p. S80 Pharmacologic Glycemic Management of Type 2 Diabetes in Adults, p. S88 Type 1 Diabetes in Children and Adolescents, p. Relevant Appendix Appendix 8: Sick-Day Medication List. Author Disclosures Dr. References Kitabchi AE, Umpierrez GE, Murphy MB, et al. Management of hyperglycemic crises in patients with diabetes. Diabetes Care ;— Hamblin PS, Topliss DJ, Chosich N, et al. Deaths associated with diabetic ketoacidosis and hyperosmolar coma. Med J Aust ;—2, Holman RC, Herron CA, Sinnock P. Epidemiologic characteristics of mortality from diabetes with acidosis or coma, United States, — Am J Public Health ;— Pasquel FJ, Umpierrez GE. Hyperosmolar hyperglycemic state: A historic review of the clinical presentation, diagnosis, and treatment. Wachtel TJ, Tetu-Mouradjian LM, Goldman DL, et al. Hyperosmolarity and acidosis in diabetes mellitus: A three-year experience in Rhode Island. J Gen Intern Med ;— Malone ML, Gennis V, Goodwin JS. Characteristics of diabetic ketoacidosis in older versus younger adults. J Am Geriatr Soc ;—4. Wang ZH, Kihl-Selstam E, Eriksson JW. Ketoacidosis occurs in both type 1 and type 2 diabetes—a population-based study from Northern Sweden. Diabet Med ;— Kitabchi AE, Umpierrez GE, Murphy MB, et al. Hyperglycemic crises in adult patients with diabetes: A consensus statement from the American Diabetes Association. Balasubramanyam A, Garza G, Rodriguez L, et al. Accuracy and predictive value of classification schemes for ketosis-prone diabetes. Diabetes Care ;—9. Laffel LM, Wentzell K, Loughlin C, et al. Sick day management using blood 3-hydroxybutyrate 3-OHB compared with urine ketone monitoring reduces hospital visits in young people with T1DM: A randomized clinical trial. OgawaW, Sakaguchi K. Euglycemic diabetic ketoacidosis induced by SGLT2 inhibitors: Possible mechanism and contributing factors. J Diabetes Investig ;—8. Rosenstock J, Ferrannini E. Euglycemic diabetic ketoacidosis: A predictable, detectable, and preventable safety concern with SGLT2 inhibitors. Singh AK. Sodium-glucose co-transporter-2 inhibitors and euglycemic ketoacidosis: Wisdom of hindsight. Indian J Endocrinol Metab ;— Erondu N, Desai M, Ways K, et al. Diabetic ketoacidosis and related events in the canagliflozin type 2 diabetes clinical program. Diabetes Care ;—6. Zinman B, Wanner C, Lachin JM, et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med ;— Hayami T, Kato Y, Kamiya H, et al. Case of ketoacidosis by a sodium-glucose cotransporter 2 inhibitor in a diabetic patient with a low-carbohydrate diet. J Diabetes Investig ;— Peters AL, Buschur EO, Buse JB, et al. Euglycemic diabetic ketoacidosis: A potential complication of treatment with sodium-glucose cotransporter 2 inhibition. Redford C, Doherty L, Smith J. SGLT2 inhibitors and the risk of diabetic ketoacidosis. Practical Diabetes ;—4. St Hilaire R, Costello H. Prescriber beware: Report of adverse effect of sodiumglucose cotransporter 2 inhibitor use in a patient with contraindication. Am J Emerg Med ;, e Goldenberg RM, Berard LD, Cheng AYY, et al. SGLT2 inhibitor-associated diabetic ketoacidosis: Clinical reviewand recommendations for prevention and diagnosis. Clin Ther ;—64, e1. Malatesha G, Singh NK, Bharija A, et al. Comparison of arterial and venous pH, bicarbonate, PCO2 and PO2 in initial emergency department assessment. Emerg Med J ;— Brandenburg MA, Dire DJ. Comparison of arterial and venous blood gas values in the initial emergency department evaluation of patients with diabetic ketoacidosis. Ann Emerg Med ;— Ma OJ, Rush MD, Godfrey MM, et al. Arterial blood gas results rarely influence emergency physician management of patients with suspected diabetic ketoacidosis. Acad Emerg Med ;— Charles RA, Bee YM, Eng PH, et al. Point-of-care blood ketone testing: Screening for diabetic ketoacidosis at the emergency department. Singapore Med J ;—9. Naunheim R, Jang TJ, Banet G, et al. Point-of-care test identifies diabetic ketoacidosis at triage. Acad Emerg Med ;—5. Sefedini E, Prašek M, Metelko Z, et al. Use of capillary beta-hydroxybutyrate for the diagnosis of diabetic ketoacidosis at emergency room: Our one-year experience. Diabetol Croat ;— Mackay L, Lyall MJ, Delaney S, et al. Are blood ketones a better predictor than urine ketones of acid base balance in diabetic ketoacidosis? Pract Diabetes Int ;—9. Bektas F, Eray O, Sari R, et al. Point of care blood ketone testing of diabetic patients in the emergency department. Endocr Res ;— Harris S, Ng R, Syed H, et al. Near patient blood ketone measurements and their utility in predicting diabetic ketoacidosis. Diabet Med ;—4. Misra S, Oliver NS. Utility of ketone measurement in the prevention, diagnosis and management of diabetic ketoacidosis. Chiasson JL, Aris-Jilwan N, Belanger R, et al. Diagnosis and treatment of diabetic ketoacidosis and the hyperglycemic hyperosmolar state. CMAJ ;— Lebovitz HE. Diabetic ketoacidosis. Lancet ;— Cao X, Zhang X, Xian Y, et al. The diagnosis of diabetic acute complications using the glucose-ketone meter in outpatients at endocrinology department. Int J Clin Exp Med ;—5. Munro JF, Campbell IW, McCuish AC, et al. Euglycaemic diabetic ketoacidosis. Br Med J ;— Kuru B, Sever M, Aksay E, et al. Comparing finger-stick beta-hydroxybutyrate with dipstick urine tests in the detection of ketone bodies. Turk J Emerg Med ;— Guo RX, Yang LZ, Li LX, et al. Diabetic ketoacidosis in pregnancy tends to occur at lower blood glucose levels: Case-control study and a case report of euglycemic diabetic ketoacidosis in pregnancy. J Obstet Gynaecol Res ;— Oliver R, Jagadeesan P, Howard RJ, et al. Euglycaemic diabetic ketoacidosis in pregnancy: An unusual presentation. J Obstet Gynaecol ; Chico A, Saigi I, Garcia-Patterson A, et al. Glycemic control and perinatal outcomes of pregnancies complicated by type 1 diabetes: Influence of continuous subcutaneous insulin infusion and lispro insulin. Diabetes Technol Ther ;— May ME, Young C, King J. Resource utilization in treatment of diabetic ketoacidosis in adults. Am J Med Sci ;— Levetan CS, Passaro MD, Jablonski KA, et al. Effect of physician specialty on outcomes in diabetic ketoacidosis. Diabetes Care ;—5. Ullal J, McFarland R, Bachand M, et al. Use of a computer-based insulin infusion algorithm to treat diabetic ketoacidosis in the emergency department. Diabetes Technol Ther ;—3. Bull SV, Douglas IS, Foster M, et al. Mandatory protocol for treating adult patients with diabetic ketoacidosis decreases intensive care unit and hospital lengths of stay: Results of a nonrandomized trial. Crit Care Med ;—6. Waller SL, Delaney S, Strachan MW. Does an integrated care pathway enhance the management of diabetic ketoacidosis? Devalia B. Adherance to protocol during the acutemanagement of diabetic ketoacidosis: Would specialist involvement lead to better outcomes? Int J Clin Pract ;—2. Salahuddin M, Anwar MN. Study on effectiveness of guidelines and high dependency unit management on diabetic ketoacidosis patients. J Postgrad Med Inst ;—3. Corl DE, Yin TS, Mills ME, et al. Evaluation of point-of-care blood glucose measurements in patients with diabetic ketoacidosis or hyperglycemic hyperosmolar syndrome admitted to a critical care unit. J Diabetes Sci Technol ;— Kreisberg RA. Diabetic ketoacidosis: New concepts and trends in pathogenesis and treatment. Ann Intern Med ;— Mahoney CP, Vlcek BW, DelAguila M. Risk factors for developing brain herniation during diabetic ketoacidosis. Pediatr Neurol ;—7. Rosenbloom AL. Intracerebral crises during treatment of diabetic ketoacidosis. Adrogue HJ, Barrero J, Eknoyan G. Salutary effects of modest fluid replacement in the treatment of adults with diabetic ketoacidosis. Use in patients without extreme volume deficit. JAMA ;— Fein IA, Rachow EC, Sprung CL, et al. Relation of colloid osmotic pressure to arterial hypoxemia and cerebral edema during crystalloid volume loading of patients with diabetic ketoacidosis. Ann Intern Med ;—5. Owen OE, Licht JH, Sapir DG. Renal function and effects of partial rehydration during diabetic ketoacidosis. Diabetes ;— Kitabchi AE, Ayyagari V, Guerra SM. The efficacy of low-dose versus conventional therapy of insulin for treatment of diabetic ketoacidosis. Ann Intern Med ;—8. Heber D, Molitch ME, Sperling MA. Low-dose continuous insulin therapy for diabetic ketoacidosis. Arch Intern Med ;— Insulin therapy for diabetic ketoacidosis. Bolus insulin injection versus continuous insulin infusion. Kitabchi AE, Murphy MB, Spencer J, et al. Is a priming dose of insulin necessary in a low-dose insulin protocol for the treatment of diabetic ketoacidosis? Fort P,Waters SM, Lifshitz F. Low-dose insulin infusion in the treatment of diabetic ketoacidosis: Bolus versus no bolus. J Pediatr ;— Lindsay R, Bolte RG. The use of an insulin bolus in low-dose insulin infusion for pediatric diabetic ketoacidosis. Pediatr Emerg Care ;—9. Andrade-Castellanos CA, Colunga-Lozano LE, Delgado-Figueroa N, et al. Subcutaneous rapid-acting insulin analogues for diabetic ketoacidosis. Cochrane Database Syst Rev ; 1 :CD Treatment of diabetic ketoacidosis using normalization of blood 3-hydroxybutyrate concentration as the endpoint of emergencymanagement. A randomized controlled study. Morris LR, Murphy MB, Kitabchi AE. Bicarbonate therapy in severe diabetic ketoacidosis. Gamba G, Oseguera J, Castrejón M, et al. |
| Diabetic Ketoacidosis: Evaluation and Treatment | AAFP | Hyperglycemic crises in adult patients with diabetes: a consensus statement from the American Diabetes Association. Ennis ED, Stahl EJVB, Kreisberg RA: The hyperosmolar hyperglycemic syndrome. Thus, insulin loading dose should be avoided at the beginning of therapy The acidosis is explained by a negative chloride-effect Therefore, the routine use of phosphate in the treatment of DKA or HHS has resulted in no clinical benefit to the patient |
| Take a look at the Recent articles | The process of HHS usually evolves over several days to weeks, whereas the evolution of the acute DKA episode in type 1 diabetes or even in type 2 diabetes tends to be much shorter. The classic work of Atchley et al. Mental status can vary from somnolence to lethargy and coma. Online ISSN Print ISSN Table 1 Diagnostic criteria for DKA and HHS. Resources ADA Professional Membership ADA Member Directory Diabetes. |
| Updates in the Management of Hyperglycemic Crisis | Glucose level should decrease by about 50 to 70 mg per dL 2. toolbar search search input Search input auto suggest. Patients in these severe metabolic deranged states need immediate treatment and do not allow much time for assessments. vanderhoeven radboudumc. Unless the plasma is cleared of chylomicrons, pseudonormoglycemia and pseudohyponatremia may occur in DKA 37 , |
Video
A real case of Diabetic Ketoacidosis (DKA) \u0026 ManagementHyperglycemic crisis and metabolic acidosis -
The aim of this review article is to provide a review of the DKA, and HHS management based on the most recently published evidence and to provide suggested management pathway of DKA of HHS management in practice. Diabetes mellitus DM is a chronic metabolic disorder that disrupts the metabolism of primary macronutrients such as proteins, fats, and carbohydrates 1 , 2.
DM remains a leading cause of death worldwide and is the number one cause of kidney failure, lower-limb amputations, and adult blindness 1 , 3 , 4. The global prevalence of DM in was around 9. Due to this high prevalence of DM, emergency admissions for hyperglycemic crisis, Diabetic Ketoacidosis DKA and Hyperglycemic Hyperosmolar State HHS , still very common and challenging 1 — 3.
Both conditions have high mortality rates if kept not treated. However, higher mortality rates were reported among elderly patients diagnosed with DKA 1. DKA and HHS have similar pathophysiology with some differences. The pathogenesis behind HHS is not as well understood 2 , 5.
DKA is a complex metabolic disorder caused by an absolute or relative effective insulin concentration reduction and increased in catecholamines, cortisol, glucagon, and growth hormones 5 , 6. Hyperglycemia is explained by three main mechanisms: increased gluconeogenesis, accelerated glycogenolysis, and impaired glucose utilization by peripheral tissues 7.
Insulin reduction and increased counterregulatory hormones in DKA accelerate the lipolysis, which results in the release of free fatty acids into the circulation from adipose tissue and stimulates the conversion of fatty acid to ketone by liver oxidation 7 , 8.
This profound increase in free fatty acid and ketone concentrations lead to a further increase in the magnitude of hyperglycemia by inducing insulin resistance and ultimately results in ketonemia and metabolic acidosis 7 , 8. Previous studies have shown that excessive glucose levels and fatty acids are associated with a pro-inflammatory and oxidative state among DKA patients 9 , Oxidative stress is defined as an increase in reactive oxygen species ROS generation 9.
Overproduction of ROS results in cellular damage of lipids, membranes, and proteins 9. Additionally, the oxidative state increases the risk of developing chronic diabetic complications following the DKA event 9.
Significant increase of IL-6, -1B and -8, and TNF-α and other cytokines reduce the response to insulin therapy. Insulin therapy and hydration are essential in normalizing these parameters 9. In contrast to DKA, insulin production is not significantly reduced among HHS patients 4.
This minimal insulin production is adequate to prevent lipolysis and ketogenesis 4 , 5. HHS is characterized by severe elevations in serum glucose concentrations and hyperosmolality 4 , 5. This extreme elevation in serum hyperosmolality results in osmotic diuresis, a greater degree of dehydration, and more fluid loss than DKA 4 , 5.
This significant loss of intracellular fluids results in much higher blood glucose BG with HHS in comparison to DKA 4 , 5. Euglycemic DKA is another unique presentation of DKA and has been reported more often recently 6 , Euglycemic DKA has been linked with many factors, such as treatment of diabetes, carbohydrate restriction, high alcohol intake, and inhibition of gluconeogenesis 6 , It also can be induced due to certain medications, most commonly seen with sodium-glucose cotransporter 2 SGLT-2 inhibitors and insulin 6 , DKA develops more rapidly in comparison to HHS.
In some cases, it only takes a few hours from the precipitating factor for DKA to develop Both metabolic disorders present with classical hyperglycemia symptoms: polyuria, polydipsia, weakness, and mental status changes 6 , Additionally, patients with HHS and DKA often present with signs of dehydration, such as dry mucous membranes, poor skin turgor, tachycardia, hypotension, and increased capillary refill with severe dehydration 8 , If DKA worsens and is left without treatment, it can eventually lead to unconsciousness 6.
The initial laboratory assessment of patients with suspected DKA or HHS should include BG, blood urea nitrogen, serum creatinine, serum ketones, electrolytes, anion gap, osmolality, urine ketones, and arterial blood gases 6 , 8.
Other reasons for high anion gap metabolic acidosis, such as ethyl glycol toxicity, isoniazid overdose, lactic acidosis, methanol toxicity, propylene glycol ingestion, salicylates toxicity, and uremia, must be ruled out Diagnostic criteria for DKA and HHS are listed in Table 1 6.
Patients with a higher level of osmolarity and pH present with worse dehydration and mental status 4. DKA resolution is achieved following the correction of dehydration, hyperglycemia, and electrolyte imbalances 2 , 6 , 8.
In addition to the previously mentioned criteria, normal osmolality is required for HHS resolution 6 , 8. Figure 1 displays a suggested management pathway of DKA and HHS based on the American Diabetes Association ADA guidelines and Joint British Diabetes Societies for Inpatient Care JBDS-IP revised guidelines 1 , Figure 1 Pathway displays the management of diabetic ketoacidosis DKA and hyperglycemic hyperosmolar state HHS.
Fluid therapy is a cornerstone for the management of DKA and HHS. Aggressive repletion with isotonic saline expands the extracellular volume and stabilizes cardiovascular functions The initial fluid management general practice and protocols are based on the ADA guidelines statement for the management of hyperglycemic crises in adult patients with diabetes 1.
It recommends initiating 0. Half normal saline 0. During fluid replacement, it is expected that hyperglycemia will be corrected faster than ketoacidosis and DKA resolution 1.
Appropriate assessment of serum osmolality, urine output, and cardiac function should be performed to guide the aggressive fluid administration and avoid iatrogenic overload 1.
However, optimal initial fluid therapy for managing DKA or HHS was not evident by clinical trials to evaluate the efficacy and safety outcomes of using normal saline or other crystalloid 1.
It is known that using 0. Some practitioners may use balanced fluids as an alternative to overcome this side effect, as its different composition could physiologically lead to a faster resolution of acidosis Common types of crystalloid IV fluids and their composition are listed in Table 2 Small trials evaluated the effect of balanced fluids and 0.
They found that balanced crystalloids significantly resulted with a shorter median time for DKA resolution than saline At the same time, it significantly led to a shorter median time for insulin discontinuation than saline 9.
They found no significant difference in DKA resolution at 48 hours, ICU, and hospital length of stay. However, PL group had significantly reached more DKA resolution at 24 hours in comparison to 0.
In conclusion, designing an appropriate fluid repletion therapy for DKA and HHS management will need careful planning and monitoring for choosing the appropriate fluid type, volume, and rate for the patient.
Insulin is considered to be one of the three fundamental elements of DKA and HHS management 2 , 6 , It reduces hepatic glucose synthesis, enhances peripheral glucose utilization, and inhibits lipolysis, ketogenesis, and glucagon secretion, lowering plasma glucose levels and decreasing ketone bodies production 6 , Insulin should be given immediately after the initial fluid resuscitation 2 , 6 , The aim of using insulin in DKA and HHS is to close the anion gap generated by the production of ketone bodies rather than aiming for euglycemia 6 , Intravenous administration of insulin regular mixed in NaCl 0.
Insulin can also be used as frequent subcutaneous or intramuscular injections for the treatment of DKA in mild-moderate DKA patients 6 , However, a continuous intravenous insulin regimen is preferred over subcutaneous insulin for DKA management overall due to its short half-life, fast onset, and easy titration 6 , The use of basal insulin analogs in conjunction with regular insulin infusions may speed up the resolution of DKA and minimize rebound hyperglycemia events, resulting in less ICU length of stay and less healthcare cost 6 , Insulin is currently recommended as a continuous infusion at 0.
Insulin loading dose has been linked to increasing the risk of cerebral edema and worsening shock Thus, insulin loading dose should be avoided at the beginning of therapy However, an insulin loading dose of 0.
Multiple factors must be considered when titrating intravenous insulin continuous infusion 2. The rate of blood glucose reduction, insulin sensitivity, prandial coverage, and NPO status should all be taken into consideration 2.
A rapid reduction in BG might be harmful and linked to cerebral edema 2. Moreover, the insulin infusion rate can be increased based on BG around major meals time and can be continued at a higher rate for hours following any major meal 2.
Lastly, it is necessary to monitor BG among NPO patients closely. Randomized clinical trials compared the two strategies and found no difference 27 , Intravenous LD insulin administration has been associated with an increased risk of cerebral edema 27 , An acceptable alternative for patients with mild to moderate DKA could be a bolus of 0.
Patients with end-stage renal disease ESRD and acute kidney injury AKI are considered a high-risk category that necessitates extra care 32 , To avoid rapid increases in osmolality and hypoglycemia in these patients; it is recommended that insulin infusions begin at 0.
Subcutaneous insulin should overlap with intravenous insulin for at least minutes before its discontinuation to ensure the optimal transition of care 6 , A transition to subcutaneous long-acting insulin in addition to ultra-short acting insulin such as glargine and glulisine after resolution of DKA may result in reduced hypoglycemic events compared to other basal bolus regimens such as NPH insulin and insulin regular 24 , For newly diagnosed insulin-dependent diabetes patients, subcutaneous insulin may be started at a dose of 0.
The transition process in patients who were previously using insulin or antidiabetic agents before to DKA admission is still unclear 24 , In ICU settings, clinicians tend to hold all oral antidiabetic agents and rely on insulin regimens for in-patient management given the shorter half-life of insulin and its predictability 24 , This could potentially be an area for further investigation on the transition process and its implication on patient outcomes 24 , Insulin sequestering to plastic IV tubing has been described, resulting in insulin wasting and dose inaccuracy 34 , Flushing the IV tube with a priming fluid of 20 mL is adequate to minimize the insulin losses to IV tube 34 , Patients with hyperglycemic crisiss are at a higher risk of developing hypokalemia due to multifactorial process 1 , Insulin therapy, correction of acidosis, and hydration all together lead to the development of hypokalemia 1 , Additionally, volume depletion seen with hyperglycemic crisis leads to secondary hyperaldosteronism, which exacerbates hypokalemia by enhancing urinary potassium excretion 1 , Serum potassium level should be obtained immediately upon presentation and prior to initiating insulin therapy 1 , Potassium replacement is required regardless of the baseline serum potassium level due to hydration and insulin therapy, except among renal failure patients 1 , It is suggested to administer 20 —30 mEq potassium in each liter of intravenous fluid to keep a serum potassium concentration within the normal range 1 , In addition to possible hypokalemia, patients with the hyperglycemic crisis could present with hypophosphatemia 1 , Osmotic diuresis during hyperglycemic crisis increases the urinary phosphate excretion, and insulin therapy enhances intracellular phosphate shift 1 , Phosphate replacement is not a fundamental part of hyperglycemic crisis management, given the lack of evidence of clinical benefit 1 , 29 , A special consideration with phosphate administration is the secondary hypocalcemia 1 , 29 , Acidemia associated with DKA results from the overproduction of ketoacids, generated from the haptic metabolism of free fatty acids.
This hepatic metabolism occurs as a result of insulin resistance and an increase in the counterregulatory hormones contributing to the pathophysiology of DKA 37 , Tissue acidosis could lead to impaired myocardial contractility, systemic vasodilatation, inhibition of glucose utilization by insulin, and lowering the levels of 2,3-diphosphoglycerate 2,3-DPG in erythrocytes 37 — Sodium bicarbonate decreases the hemoglobin-oxygen affinity leading to tissue hypoxia; moreover, it is associated with hypernatremia, hypocalcemia, hypokalemia, hypercapnia, prolonged QTc interval, intracellular acidosis, and metabolic alkalosis 39 , The use of adjuvant sodium bicarbonate in the setting of DKA consistently shows a lack of clinical benefit and should be prescribed on a case-by-case basis.
However, a significant number of patients stray from these patterns. Both of these conditions carry significant likelihood of morbidity and mortality, including cerebral edema, permanent neurological injury, and death.
It is important to be familiar with the pathophysiology, presentation, treatment, complications, and—perhaps most importantly—prevention of DKA and HHS.
The basic cause of DKA and HHS is insufficient insulin effect. Combined with the insufficiency of insulin effect, there is an increase in counterregulatory hormone levels, including glucagon, cortsol, catecholamines, and growth hormone.
Both factors contribute to hyperglycemia. DKA and HHS may also be thought of as occurring on a spectrum of disease manifestation. On one end of the spectrum lie absolute insulin deficiency and profound ketosis and acidosis, which is DKA.
DKA tends to occur in patients with type 1 diabetes, who, because of destruction of β-cells, exhibit absolute insulin deficiency. On the other end of the spectrum is extreme hyperglycemia without ketosis and acidosis.
As the analogy implies, patients may present with various manifestations of both disorders. For example, a patient with DKA may have used enough insulin to partially suppress ketosis but still manifest profound hyperglycemia.
Patients with HHS may also have varying degrees of ketosis and mild acidosis, depending on the degree to which they have been able to produce insulin and the extent of associated factors such as dehydration.
Insulin deficiency causes a lack of glucose utilization in insulin-dependent tissues such as muscle and adipose and therefore leads to hyperglycemia. Lack of insulin also stimulates hyperglycemia by increasing hepatic gluconeogenesis. This is a common mechanism in both DKA and HHS.
Deprived of glucose utilization, the body must look elsewhere for fuel to survive. In addition to hyperglycemia, lack of insulin increases degradation of triglycerides into free fatty acids in adipose tissue, which travel to the liver and are converted to the ketoacids β-hydroxybutyric acid, acetone, and acetoacetate.
Unopposed conterregulatory hormone effect causes further increases in glucose production from the liver and degradation of triglycerides. The surge of ketoacid formation from unrestrained ketone body formation can be profound. DKA develops when the surge of ketoacid production is so powerful that a metabolic acidosis results.
In HHS, there remains sufficient insulin presence to suppress ketosis enough to prevent the development of metabolic acidosis. Dehydration is another common finding in DKA and HHS.
Because of osmotic pressure, unregulated diuresis follows. Patients frequently complain of preceding polyuria and polydipsia.
Considerable electrolyte loss may result, especially potassium depletion. Further dehydration and volume contraction can lead to worsening of hyperglycemia. Patients presenting in HHS and DKA typically exhibit a history of polyuria and polydipsia.
Frequently, one can identify a precipitating factor leading to DKA. Such factors can include inappropriate use of insulin non-compliance , cardiovascular disease, or infection, which may be the most common causes of DKA. Patients with DKA may also manifest leukocytosis simply due to DKA. It is important to not overlook other possible causes of DKA and HHS, however.
Myocardial infarction may precipitate hyperglycemia and DKA via an increase in counterregulatory hormones, such as epinephrine. Drugs such as thiazides, sympathomimetics, second-generation antipsychotics, and corticosteroids may also precipitate HHS and DKA.
Other disorders that may precipitate diabetes include pancreatitis and illicit drug use. Additionally, and especially in patients with type 1 diabetes, decline in diabetes control and hyperglycemia may indicate the onset of an autoimmune thyroid disease, such as Grave's disease or Hashitoxicosis.
Patients may develop progressive hyperglycemia over weeks or days, although patients with DKA may experience more rapid onset than those with HHS. Symptoms of both HHS and DKA include polyuria and polydipsia due to hyperglycemia and signs of dehydration, including lack of skin turgor, hypotension, dry oral mucosae, tachycardia, weakness, and altered sensorium.
Patients with DKA typically exhibit signs of acidosis, such as abdominal pain sometimes severe , nausea, vomiting, and Kussmaul respirations, and may also exhibit guaiac-positive vomitus. Hypothermia, should it be present, is a poor prognostic indicator. Laboratory findings in patients with DKA include hyperglycemia, ketosis, and metabolic acidosis.
Patients who are suspected of DKA or HHS should undergo measurement of electrolytes with anion gap, glucose serological , creatinine and blood urea nitrogen, serum ketones, urinalysis with ketones, complete blood count, A1C, and arterial blood gas testing.
Additionally, electrocardiogram, chest X-ray, and urine, sputum, and blood cultures may be warranted. If children are otherwise healthy and there are no signs of infection, it may be acceptable to omit an infection workup. Significant ketosis has been shown in up to one-third of patients with HHS, again indicative of the continuum of pathology between DKA and HHS.
Buildup of ketoacids is responsible for anion gap metabolic acidosis in DKA. It is important, however, to remember other causes of anion gap metabolic acidoses, including starvation, lactic acidosis especially in patients using metformin , salicylates, ethanol, methanol, ethylene glycol, paraldehyde, renal insufficiency, and isopropyl alcohol intoxication.
Serum potassium levels are typically elevated in response to the presence of acidosis and insulin deficiency, but total body potassium is depleted. Patients presenting with hypokalemia in the setting of DKA are particularly potassium-depleted and require aggressive monitoring and potassium repletion.
Both amylase and lipase may be elevated in the setting of DKA and are not necessarily indicative of pancreatitis. The cornerstones of treatment of DKA and HHS are fluids, insulin, correction of electrolyte abnormalities, and close monitoring.
In the absence of underlying renal and cardiac disease, initial fluid resuscitation should consist of isotonic fluids to restore renal perfusion. Subsequently, fluids may be altered or titrated based on degree of dehydration and electrolyte abnormalities.
Titration of fluids is based on hemodynamic improvement, urine output, laboratory improvement, and clinical response. Patients with underlying cardiac and renal disease may require lower initial fluid resuscitation rates and more frequent monitoring of clinical status to avoid fluid overload.
vanderhoeven radboudumc. Hyperglycaemic hyperosmolar state HHS and diabetic ketoacidosis DKA are often accompanied by severe metabolic and electrolyte disorders.
Analysis and treatment of these disorders can be challenging for clinicians. In this paper, we aimed to discuss the most important steps and pitfalls in analyzing and treating a case with extreme metabolic disarrangements as a consequence of an HHS.
Electrolyte disturbances due to fluid shifts and water deficits may result in potentially dangerous hypernatriema and hyperosmolality. In addition, acid-base disorders often co-occur and several approaches have been advocated to assess the acid-base disorder by integration ofthe principles of mass balance and electroneutrality.
The four methods were compared and tested for their bedside usefulness. All approaches gave good insight in the metabolic disarrangements of the presented case. acid-base disorders, corrected sodium, hyperglycaemic hyperosmolar state, metabolic acidosis, Stewart, strong ion difference.
Severe acid-base disorders combined with electrolyte disturbances are often seen in patients with hyperosmolar hyperglycaemic state HHS or diabetic ketoacidosis DKA. Acid-base disorders and electrolyte disturbances are tightly connected[1].
The aims of this clinical lesson are i to give insight in the relation between hyperglycemia, acid-base disturbances and electrolyte homeostasis, ii to provide a strategy for the treatment of HHS and DKA during the first hours, and iii to compare different methods in analyzing acid-base disorders.
A year-old patient was admitted to the ICU because of a hyperosmolar Hyperglycaemic state with an extreme metabolic and combined respiratory acidosis and hypernatriemia Table 1. Glucose levels were gradually lowered with iv insulin and extensive rehydration.
Initially,themetabolic acidosis improved. The hyperglycemia of this patient caused severe acid-base and electrolyte disturbances of which the main elements are i the effects of ketoacids on other ions and ii the effects of the hyperglycemia on extracellular volume and sodium concentrations.
By definition electrolytes dissociate in water in anions negatively charged, predominately chloride or in cations positively charged, predominately sodium. However, inpathologic conditions these electrolytes can be extensively lost or gained resulting in a temporary ionic imbalance.
To maintain electrochemical neutrality, changes in acid-base equilibrium occur. An absolute shortage of insulin in diabetic ketoacidosis DKA results in the accumulation of negatively charged ketoacids from acetyl-Coa serving as a fuel for the brain. These ketoacids anions becomeapparent in blood when their hepatic production exceeds the renal excretion capacity.
To compensate forthe accompanyingprotons from the ketoacids, water and carbon dioxideare formed from bicarbonate to enable respiratory compensation[2]. This equation is the cornerstone of the traditional approach according to Henderson-Hasselbalch for the assessment of acid base disturbances Textbox.
More detailed description and analysis of the acid base disturbance of the presented case will follow below. Another important element in this pathologic cascade includes sodium and water regulation. Increased glucose levels augment the plasma tonicity because glucose is an effective osmole and both the hyperglycemia and the ketoacid salts cause a decrease in the extracellular volume, factors that contribute to enormous deficits in total body water and changes in plasma sodium concentrations[2].
Hyponatriemia may become apparent since sodium, also an effective osmole,remains in the extracellular the blood compartment during the glucose-driven watershift. Be aware that normal or increased plasma sodium levels during severe hyperglycemia indicate a substantial loss of total body water!
Although this correction factor is based on theoretical considerations and has not been well validated, it gives good insight into the severity of water loss[2]. Patients in these severe metabolic deranged states need immediate treatment and do not allow much time for assessments.
Many guidelines regarding the treatment of HHS and DKA exist and it is beyond the scope of this article to discuss them in detail. However, the extreme hypernatriemia illustrates the importance of careful fluid administration, specifically concerning the prevention of cerebral edema for reasons delineated below.
The initial goal of fluid therapy in a Hyperglycaemic crisis is to stabilize hemodynamics with isotonic solutions. During resuscitation it is important to monitor the corrected plasma sodium levels, but even more important is the monitoring of the effective plasma osmolality Table 2 [2].
Current expert opinion is based on animal studies and case reports and states that the risk for cerebral edema is determined by changes in effective plasma osmolality[5]. This is considered most important during the first 15 hours of treatment[2,6]Symptomatic cerebral edema is mostly described in children with diabetic ketoacidosis[7].
It is seldom seen in adults with DKA or HHS[]. However, several guidelines [3,4] advise to consider corrected sodium and effective osmolality and to adjust fluid therapy accordingly, which implies thatthe reduction in glucose levels is accompanied by increases in measured sodium levelsin order to safely decrease theplasma osmolality.
There is no consensus between different guidelines if the fluid treatment should be based on effective, measured or calculated plasma osmolality, but we suggest to use effective or calculated plasma osmolality since it is quicker in use.
Table 2. In our patient extensive rehydration with normal saline was started in addition to glucose lowering therapy.
Even though plasma sodium remained high, the calculated osmolality dropped gradually along with glucose levels, indicating save and effective rehydration and therapy Figures1A and1B.
Figure 1. Course of sodium and glucose, osmolality and acid-base parameters according to the 4 described theories. Several explanatory models aim to help understanding the pathophysiology of metabolic disarrangements.
The traditional method is a bicarbonate-centered approach. As explained in the textbox, its main principle is that bicarbonate and hydrogen are in equation with carbon dioxide pCO 2 and that the metabolic acidosis is based on the extent of bicarbonate loss.
Either by loss of the ion resulting in a equilibrium shift to the left resulting in hydrogen formation, or by increases in hydrogen pushing the reaction to shift to the right with consequently an increase of pCO 2.
Compensatory mechanisms are respiratory to exhale excess pCO 2 or renal to retain bicarbonate. The elevated pCO 2 is likely due to respiratory insufficiency as a result of his comatose state.
For more insight into the origin of the metabolic acidosis the aniongap is calculated with correction for the albumin concentration Table 2. Failure to do so may result in an underestimation of the anion gap due to altered charges of weak anions because of albumin-based changes in pH [13]and finally lead to a false interpretation of the acid-base disorder[14,15].
Our patient had an extremely increased anion gap of Indeed, ketoacids were found, but inrelatively low concentrations suggestive for the co-existence of other anions.
Other well-known anions that attribute to an increased anion gap are lactate or alcoholic ketoacids, or in case of co-existing increased osmole gap ingestion of ethylene glycol, ethanol or methanol[13]. An osmole gap was not detected in the presented case. Assessment of thedelta ratio Table 2 helps identifying the presence of co-existing metabolic acid-base disorders and is used to provide an estimate of the acid load[6,16].
In contrast, a delta ratio below 0. In conclusion, the extreme increased aniongap could only partly be explained by the presence of serum lactate and ketoacids and other, unknown anions should have attributed to the acidosis as well.
Moreover, failing renal compensation of the acidosis, in a later stadium of the disease, with increased renal bicarbonate loss, as described by Kamel et al, may have added to the acidosis[6].
Providing emtabolic scholarly communications to worldwide, enabling them to utilize available resources effectively. We aim crisls bring Gut health and sleep quality Hyperglycemic crisis and metabolic acidosis change in modern scholarly communications through the effective use of editorial and publishing polices. Advanced knowledge sharing through global community…. Marloes B. Department of Intensive Care Medicine, Radboud University Medical Center, Nijmegen, the Netherlands. Susanne van Santen.
So kommt es vor.
Wacker, welche nötige Wörter..., der prächtige Gedanke