Self-care plans for diabetes management -
Summary of DSMES benefits to discuss with people with diabetes 15 — 28 , 30 — 33 , 40 , A variety of DSMES approaches and settings need to be presented and discussed with people with diabetes, thus enabling self-selection of a method that best meets their specific needs Evolving health care delivery systems, primary care needs, and the needs of people with diabetes have resulted in the incorporation of DSMES services into additional and nontraditional settings such as those located within patient-centered medical homes, community health centers, pharmacies, and accountable care organizations ACOs , as well as faith-based organizations and home settings.
Technology-based services including web-based programs, telehealth, mobile applications, and remote monitoring enable and promote increased access and connectivity for ongoing management and support Recent health care concerns are rapidly expanding the use of these services, especially telehealth.
In conjunction with formal DSMES, online peer support communities are growing in popularity. Involvement in these groups can be a beneficial adjunct to learning, serving as an option for ongoing diabetes peer support 36 , 37 Supplementary Table 1.
Creative, person-centered approaches to meet individual needs that consider various learning preferences, literacy, numeracy, language, culture, physical challenges, scheduling challenges, social determinants of health, and financial challenges should be widely available.
It is important to ensure access in communities at highest risk for diabetes, such as racial and ethnic minorities and underserved communities. Office-based health care teams without in-house resources can partner with local diabetes care and education specialists within their community to explore opportunities to reach people with diabetes and overcome some barriers to participation at the point of care If the office-based care team assumes responsibility for providing diabetes education and support, every effort should be made to ensure they receive up-to-date training in diabetes care and education and utilize the details in Tables 5 and 6.
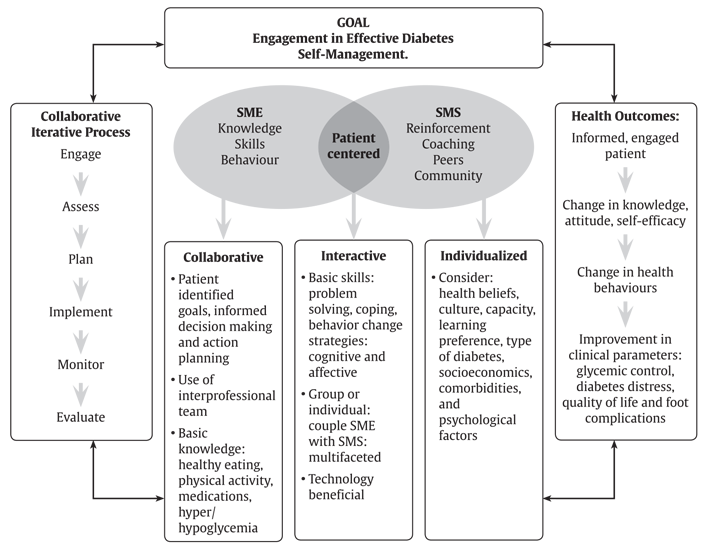
Sample questions to guide a person-centered assessment Regardless of the DSMES approach or setting, personalized and comprehensive methods are necessary to promote effective self-management required for day-to-day living with diabetes.
Effective delivery involves expertise in clinical, educational, psychosocial, and behavioral diabetes care 39 , It is essential for the referring provider to mutually establish personal treatment plans and clinical goals with the person with diabetes and communicate these to the DSMES team.
Ongoing communication and support of recommendations and progress toward goals between the person with diabetes, education team, referring provider, and other members of the health care team are critical.
A person-centered approach to DSMES beginning at diagnosis of diabetes provides the foundation for current and future decisions. Diabetes self-management is not a static process and requires ongoing assessment and modification, as identified by the four critical times see Fig. Initial and ongoing DSMES helps the person overcome barriers and cope with the enduring and changing demands throughout the continuum of diabetes treatment and life transitions.
Providers and other members of the immediate health care team have an important role in providing education and ongoing support for self-management needs. New behaviors can be difficult to maintain and require reinforcement at a minimum of every 6 months In addition to the providers, the care team may include diabetes care and education specialists DCES ; registered dietitian nutritionists RDNs ; nutrition and dietetics technicians, registered NDTRs ; nurse educators; care managers; pharmacists; exercise and rehabilitation specialists; and behavioral or mental health care providers.
In addition, others have a role in helping to sustain the benefits gained from DSMES, including community health workers, nurses, care managers, trained peers, home health care service workers, social workers, and mental health counselors and other support people e.
Professional associations may help identify specific services in the local area such as the Visiting Nurse Association and block nurse programs see Supplementary Table 1. Family members and peers are an underutilized resource for ongoing support and often struggle with how to best provide help 47 , Including family members in the DSMES process can help facilitate their involvement 49 — Such support people can be especially helpful and serve as cultural navigators in health care systems and as liaisons to the community Community programs such as healthy cooking classes, walking groups, peer support communities, and faith-based groups may lend support for implementing healthy behavior changes, promoting emotional health, and meeting personal health goals Health care providers need to be aware of the DSMES resources in their health system and communities and make appropriate referrals.
Although these four critical times are listed, it is important to recognize diabetes is a chronic disease that progresses over time and requires vigilant care to meet changing physiologic needs and goals The existing treatment plan may become ineffective due to changing situations that can arise at any time.
Such situations include progression of the disease, changes in personal goals, unmet targets, major life changes, or new barriers identified when assessing social determinants of health.
It is prudent to be proactive when changes are identified or emerging. Additional support from the entire care team and referral to DSMES are appropriate responses to any of these needs.
Quality ongoing, routine diabetes care includes continuous assessment, ongoing education and learning, self-management planning, and ongoing support. The AADE7 Self-Care Behaviors provide the overarching framework for identifying key components of education and support The seven self-care behaviors are healthy coping, healthy eating, being active, taking medication, monitoring, reducing risks, and problem solving.
Mastery of skills and behaviors related to each of these areas requires practice and experience. Often, a series of ongoing education and support visits are necessary to allow participants the time to practice new skills and behaviors, to develop problem-solving skills, and to improve their ability and self-efficacy to set and reach personal self-management goals Care and education plans at each of the four critical times focus on the needs and personal goals of the individual.
Therefore, the plan should be based on personal experiences that are relevant to self-management and applicable to personal goals, treatment targets, and objectives and acknowledge that adults possess expertise about their own lives Tables 5 and 6 serve as checklists to ensure clinical teams and health systems offer necessary diabetes services factors that indicate DSMES needs and what DSMES provides.
Overview of MNT: an evidence-based application of the nutrition care process provided by the RDN 1 , 40 , 69 — Note: The Academy of Nutrition and Dietetics recognizes the use of registered dietitian RD and registered dietitian nutritionist RDN. RD and RDN can only be used by those credentialed by the Commission on Dietetic Registration.
For an individual and family, the diagnosis of diabetes is often overwhelming 58 , 59 , with fears, anger, myths, and personal, family, and life circumstances influencing this reaction. Immediate care addresses these concerns through listening, providing emotional support, and answering questions.
Providers typically first set the stage for a lifetime chronic condition that requires focus, hope, and resources to manage on a daily basis. A person-centered approach at diagnosis is essential for establishing rapport and developing a personal and feasible treatment plan.
Despite the wide range of knowledge and skills that are required to self-manage diabetes, caution should be taken to not confound the overwhelming nature of the diagnosis but to determine what the person needs from the care team at this time to safely navigate self-management during the first days and weeks.
Responses to such questions as shown in Table 7 also see Tables 5 and 6 guide and set direction for each person. Immediate referral to DSMES services establishes a personal education and support plan and highlights the value of initial and ongoing education.
Initial DSMES at diagnosis typically includes a series of visits or contacts to build on clinical, psychosocial, and behavioral needs.
See Table 6 for suggested content. These team members are critical at all four critical times. Important discussions at diagnosis include the natural history of type 2 diabetes, what the journey will involve in terms of lifestyle and possibly medication, and acknowledgment that a range of emotional responses is common.
Diabetes is largely self-managed and care management involves trial and error. The role of the health care team is to provide information and discuss effective strategies to reach chosen treatment targets and goals.
The many tasks of self-management are not easy, yet worth the effort 61 see benefits associated with dsmes. The health care team and others support the adoption and maintenance of daily self-management tasks 8 , 40 , as many people with diabetes find sustaining these behaviors difficult.
They need to identify education and other needs expeditiously in order to address the nuances of self-management and highlight the value of ongoing education. Table 6 provides details of DSMES at this critical time.
Annual assessment of knowledge, skills, and behaviors is necessary for those who achieve diabetes treatment targets and personal goals as well as for those who do not. Primary care visits for people with diabetes typically occur every 3—6 months These visits are opportunities to assess all areas of self-management, including laboratory results, and a review of behavioral changes and coping strategies, problem-solving skills, strengths and challenges of living with diabetes, use of technology, questions about medication therapy and lifestyle changes, and other environmental factors that might impact self-management It is challenging for primary care providers to address all assessments during a visit, which points to the need to utilize established DSMES resources and champion new ones to meet these needs, ensuring personal goals are met.
See Table 5 for indications for referral. Possible barriers to achieving treatment goals, such as financial and psychosocial issues, life stresses, diabetes-related distress, fears, side effects of medications, misinformation, cultural barriers, or misperceptions, should be assessed and addressed.
People with diabetes are sometimes unwilling or embarrassed to discuss these problems unless specifically asked 62 , Frequent DSMES visits may be needed when the individual is starting a new diabetes medication such as insulin 64 , is experiencing unexplained hypoglycemia or hyperglycemia, has worsening clinical indicators, or has unmet goals.
Importantly, diabetes care and education specialists are charged with communicating the revised plan to the referring provider and assisting the person with diabetes in implementing the new treatment plan.
The identification of diabetes-related complications or other individual factors that may influence self-management should be considered a critical indicator of the need for DSMES that requires immediate attention and adequate resources.
The diagnosis of other health conditions often makes management more complex and adds additional tasks onto daily management. DSMES addresses the integration of multiple medical conditions into overall care with a focus on maintaining or appropriately adjusting medication, meal plans, and physical activity levels to maximize outcomes and quality of life.
In addition to the need to adjust or learn new self-management skills, effective coping, defined as a positive attitude toward diabetes and self-management, positive relationships with others, and enhanced quality of life are addressed in DSMES services 16 , The progression of diabetes can increase the emotional and treatment burden of diabetes and distress 65 , It has a greater impact on behavioral and metabolic outcomes than does depression Diabetes-related distress is responsive to intervention, including DSMES-focused interventions 68 and family support However, additional mental health resources are generally required to address severe diabetes-related distress, clinical depression, and anxiety It is important to recognize the psychological issues related to diabetes and prescribe treatment as appropriate.
Throughout the life span many factors such as aging, living situation, schedule changes, or health insurance coverage may require a re-evaluation of diabetes treatment and self-management needs see Tables 5 and 6.
They may also include life milestones: marriage, divorce, becoming a parent, moving, death of a loved one, starting or completing college, loss of employment, starting a new job, retirement, and other life circumstances.
Changing health care providers can also be a time at which additional support is needed. DSMES affords important benefits to people with diabetes during transitions in life and care.
Providing input into the development of practical and realistic self-management and treatment plans can be an effective asset for successful navigation of changing situations.
The health care provider can make a referral to a diabetes care and education specialist to add input to the transition plan, provide education and problem solving, and support successful transitions. The goal is to minimize disruptions in therapy during any transition, while addressing clinical, psychosocial, and behavioral needs.
Additionally, MNT helps prevent, delay, or treat other complications commonly found with diabetes such as hypertension, cardiovascular disease, renal disease, celiac disease, and gastroparesis.
MNT is integral to quality diabetes care and should be incorporated into the overall care plan, medication plan, and DSMES plan on an ongoing basis 1 , 40 , 69 — 72 Table 8. Although basic nutrition content is covered as part of DSMES, people with diabetes need both initial and ongoing MNT and DSMES; referrals to both can be made through many electronic health records as well as through hard copy or faxed referral methods see Supplementary Table 1 for specific resources.
Everyday decisions about what to eat must be driven by evidence and personal, cultural, religious, economic, and other preferences and needs 69 — The entire health care team should provide consistent messages and recommendations regarding nutrition therapy and its importance as a foundation for quality diabetes care based on national recommendations Despite the proven value and effectiveness of DSMES, a looming threat to its success is low utilization due to a variety of barriers.
In order to reduce barriers, a focus on processes that streamline referral practices must be implemented and supported system wide. Once this major barrier is addressed, the diabetes care and education specialist can be invaluable in addressing other barriers that the person may have.
Without this, it will be increasingly difficult to access DSMES services, particularly in rural and underserved communities. With focus and effort, the challenges can be addressed and benefits realized.
The Centers for Disease Control and Prevention reported that only 6. This low initial participation in DSMES was also reported in a recent AADE practice survey, with most people engaging in a diabetes program diagnosed for more than a year These low numbers are seen even in areas where cost is less of a barrier because of national health insurance.
Analysis of National Health Service data in the U. This highlights the need to identify and utilize resources that address all barriers including those related to health systems, health care providers, participants, and the environment.
In addition, efforts are being made by national organizations to correct the identified access and utilization barriers. Health system or programmatic barriers include lack of administrative leadership support, limited numbers of diabetes care and education specialists, geographic location, limited or lack of access to services, referral to DSMES services not effectively embedded in the health system service structure, limited resources for marketing, and limited or low reimbursement rates DSMES services should be designed and delivered with input from the target population and critically evaluated to ensure they are patient-centered.
Despite the value and proven benefits of these services, barriers within the benefit design of Medicare and other insurance programs limit access. Using Medicare as an example, some of these barriers include the following: hours allowed in the first year the benefit is used and subsequent years are predefined and not based on individual needs; a referral is required and must be made by the primary provider managing diabetes; there is a requirement of diabetes diagnosis using methods other than A1C; and costly copays and deductibles apply.
A person cannot have Medicare DSMES and MNT visits either face to face or through telehealth on the same day, thus requiring separate days to receive both of these valuable services and possibly delaying questions, education, and support.
Referrals may also be limited by unconscious or implicit bias, which perpetuates health care disparities and leads to therapeutic inertia. To address these barriers, providers can meet with those currently providing DSMES services in their area to better understand the benefits, access, and referral processes and to develop collaborative partnerships.
Participant-related barriers include logistical factors such as cost, timing, transportation, and medical status 34 , 77 , 78 , For those who avail themselves of DSMES services, few complete their planned education due to such factors.
Underutilization of services may be because of a lack of understanding or knowledge of the benefits, cultural factors, a desire to keep diabetes private due to perceived stigma and shame, lack of family support, and perceptions that the standard program did not meet their needs and is not relevant for their life, and the referring providers may not emphasize the value and benefits of initial and ongoing DSMES 34 , 79 , 80 , Health systems, clinical practices, people with diabetes, and those providing DSMES services can collaborate to identify solutions to the barriers to utilization of DSMES for the population they serve.
Creative and innovative solutions include offering a variety of DSMES options that meet individual needs within a population such as telehealth formats, coaching programs, just-in-time services, online resources, discussion groups, and intense programs for select groups, while maximizing community resources related to supporting healthy behaviors.
Credentialed DSMES programs as well as individual diabetes care and education specialists perform a comprehensive assessment of needs for each participant, including factors contributing to social determinants of health such as food access, financial means, health literacy and numeracy, social support systems, and health beliefs and attitudes.
This allows the diabetes care and education specialist to individualize a plan that meets the needs of the person with diabetes and provide referrals to resources that address those factors that may not be directly addressed in DSMES.
It is best that all potential participants are not funneled into a set program; classes based on a person-centered curriculum designed to address social determinants of health and self-determined goal setting can meet the varied needs of each person. Environment-related barriers include limited transportation services and inadequate offerings to meet the various cultural, language, and ethnic needs of the population.
Additionally, these types of barriers include those related to social determinants of health—the economic, environmental, political, and social conditions in which one lives The health system may be limited in changing some of these conditions but needs to help each person navigate their situation to maximize their choices that affect their health.
It is important to recognize that some individuals are less likely to attend DSMES services, including those who are older, male, nonwhite, less educated, of lower socioeconomic status, and with clinically greater disease severity 84 , Further, studies support the importance of cultural considerations in achieving successful outcomes 84 — Solutions include exploring community resources to address factors that affect health behaviors, providing seamless referral and access to such programs, and offering flexible programing that is affordable and engages persons from many backgrounds and living situations.
The key is creating community-clinic partnerships that provide the right interventions, at the right time, in the right place, and using the right workforces Several common payment models and newer emerging models that reimburse for DSMES services are described below.
For a list of diabetes education codes that can be submitted for reimbursement, see Supplementary Table 2 Billing codes to maximize return on investment ROI in diabetes care and education. CMS has reimbursed diabetes education services billed as diabetes self-management training since 40 , In order to meet the requirements, DSMES services must adhere to National Standards for Diabetes Self-Management Education and Support and meet the billing provider requirements 40 , Ten hours are available for the first year of receiving this benefit and 2 h in subsequent years.
Any provider physician, nurse practitioner, PA who is the primary provider of diabetes treatment can make a referral; there is a copay to use these services. CMS also reimburses for diabetes MNT, which expands access to needed education and support.
Three hours are available the first year of receiving this benefit and 2 h are available in subsequent years. A physician can request additional MNT hours through an MNT referral that describes why more hours are needed, such as a change in diagnosis, medical condition, or treatment plan.
There are no specific limits set for additional hours. There is no copay or need to meet a Part B deductible in order to use these services. Many other payers also provide reimbursement for diabetes MNT Reimbursement by private payers is highly variable.
Many will match CMS guidelines, and those who recognize the immediate and longer-term cost savings associated with DSMES will expand coverage, sometimes with no copay.
With the transition to value-based health care, organizations may receive financial returns if they meet specified quality performance measures. Diabetes is typically part of a set of contracted quality measures impacting the payment model. Health systems should maximize the benefits of DSMES and factor them into the potential financial structure.
There are reimbursable billing codes available for remote monitoring of blood glucose and other health parameters that are related to diabetes.
The use of devices that can monitor glucose, blood pressure, weight, and sleep allow the health care team to review the data, provide intervention, and recommend treatment changes remotely. Sample referral forms that provide the information required by CMS and other payers for referral to DSMES and MNT are available along with reimbursement resources see Supplementary Tables 1 and 2.
These or similar forms can be embedded into an electronic health record for easy referral. Educate patients about the storage duration of insulin vials, advising that if a vial will be used within 1 month, it can be kept at room temperature.
Insulin can be safely stored at room temperature for up to one month without compromising its effectiveness. This knowledge empowers patients to manage their insulin storage appropriately and ensures they have access to insulin that is ready for use.
Instruct patients to gently mix cloudy insulins by inverting the vial or rolling it between their hands before drawing the solution into a syringe or pen. Cloudy insulins contain particles that need to be evenly distributed throughout the solution. Mixing the insulin ensures a consistent dose and promotes accurate administration.
Emphasize the importance of checking the expiration date on all types of insulin before use. Expired insulin may have reduced efficacy or potency, which can lead to suboptimal blood glucose control. Checking the expiration date helps ensure patients use insulin that is safe and effective.
Teach patients to inspect bottles of intermediate-acting insulin for flocculation, which appears as a frosted, whitish coating inside the bottle. Flocculation is an indication that the insulin has been exposed to extreme temperatures and may have lost its effectiveness.
Discarding insulin with flocculation helps prevent administering compromised insulin and maintains proper glycemic control. Ensure that the appropriate syringe size is selected to match the insulin concentration being used and on the different sizes of insulin syringes available 1mL, 0.
Selecting the correct syringe size is crucial to accurately measure and draw up the prescribed insulin dose. Using syringes with the appropriate capacity ensures accurate insulin administration and helps prevent dosing errors.
Providing information about syringe sizes and their markings helps patients understand the available options and choose the most suitable syringe for their insulin needs. Awareness of unit increments promotes accurate measurement and dosing.
Instruct patients on the importance of using a new, disposable needle for each insulin injection. Using a new needle for each injection helps maintain needle sharpness, reduce discomfort, minimize the risk of infection, and ensure accurate insulin delivery.
It is essential for patient safety and proper injection technique. Advise patients to keep the needle capped when not in use to maintain cleanliness and sterility. Keeping the needle capped when not in use helps prevent contamination, maintain needle sterility, and reduce the risk of infection.
It ensures a safe and hygienic insulin administration process. Emphasize the importance of not sharing insulin syringes with others to prevent cross-contamination and the spread of infections. Sharing syringes can transmit bloodborne infections, including viral diseases such as HIV and hepatitis.
Educating patients about the risks associated with sharing syringes promotes safe injection practices and protects against potential health hazards. Instruct patients on proper syringe disposal techniques, such as clipping off the needle or using a device that safely contains and disposes of the needle.
Proper syringe disposal helps prevent accidental needlestick injuries, protects others from potential harm, and ensures the safe management of medical waste. Teaching patients appropriate disposal methods promotes community safety and adherence to waste management regulations.
Provide guidance on local regulations and resources for disposing of used syringes, including contacting the refuse company or waste authority for guidance. Proper disposal of used syringes is essential to prevent environmental contamination and comply with local waste management regulations.
Informing patients about available resources helps them navigate safe disposal practices effectively. Educate patients on safe syringe transport during travel, advising them to pack used syringes in a secure container to prevent accidental needlesticks.
Traveling with used syringes requires careful handling to avoid injuries and maintain personal and public safety. Providing instructions on proper syringe transport reduces the risk of accidental needlesticks during travel.
Insulin pump therapy is suitable for patients who desire continuous subcutaneous insulin infusion and are willing to actively participate in self-management. Provide extensive education on insulin pump use and self-management of blood glucose and insulin doses.
Insulin pump therapy requires thorough education to ensure proper understanding and safe use of the device. Educating the patient about insulin pump operation, insertion site care, troubleshooting techniques, blood glucose monitoring, and calculating insulin doses based on carbohydrate counting promotes effective self-management.
Teach the patient about potential risks and complications associated with insulin pump therapy. Patients need to be aware of potential risks and complications, such as occlusions in the infusion set or tubing, interruptions in insulin flow, and the increased risk of ketoacidosis.
Educating patients about recognizing signs of occlusions, administering manual injections when needed, and seeking prompt medical attention for any concerns helps minimize risks and promote patient safety. Instruct the patient on proper care, maintenance, and replacement of the insulin pump.
Proper care and maintenance of the insulin pump, including regular changing of infusion sets, is essential for optimal function and prevention of complications. Teaching the patient about proper hygiene, safe storage, battery replacement, and when to seek technical support helps ensure uninterrupted insulin delivery and device performance.
This monitoring allows for adjustments in insulin dosages and troubleshooting of any issues to maintain optimal glucose control. Provide support and addressing concerns related to wearing the pump. Some patients may find wearing the insulin pump for 24 hours a day inconvenient or may have concerns about its visibility.
Offering support, addressing concerns, and discussing options for temporary disconnection e. Insulin pens are suitable for patients who need to inject one type of insulin at a time or can use premixed insulins.
Instruct the patient on proper insulin pen technique and safety measures. Proper technique in using insulin pens ensures accurate dosage delivery and minimizes the risk of complications. Education on how to load the insulin cartridge, dial the appropriate dose, attach the disposable needle, and perform the injection helps the patient use the device effectively and safely.
Teach the patient about storage and maintenance of insulin pens. Insulin pens should be stored properly to maintain the integrity of the insulin and the device. Educating the patient on storage conditions, such as avoiding extreme temperatures, and the need for regular cleaning and replacement of needles promotes optimal performance of the insulin pen.
This monitoring allows for adjustments in insulin dosages as needed to maintain optimal glucose control. Jet injectors are an alternative to needle injections for delivering insulin.
Provide thorough training and supervision for the patient when initiating jet injector use. Proper training is crucial when using jet injectors to ensure accurate and safe insulin delivery. Providing comprehensive education on how to operate the device, maintain hygiene, and troubleshoot any issues helps the patient use the jet injector effectively and minimizes the risk of complications.
Educate the patient about the differences in insulin absorption rates, peak activity, and insulin levels with a jet injector. Jet injectors may result in differences in insulin absorption rates compared to traditional needle injections. Educating the patient about these variations helps them understand the potential differences in insulin action and adjust their self-management strategies accordingly.
Advise the patient about the possibility of bruising associated with jet injector use. Some patients may experience bruising at the injection site when using jet injectors. Informing the patient about this potential side effect helps manage their expectations and promotes early identification of any complications or adverse reactions.
Insulin administration can sometimes lead to local and systemic allergic reactions, with local reactions causing redness, swelling, tenderness, and wheals at the injection site. Systemic reactions are rare but can result in generalized urticaria or even anaphylaxis.
Assess and monitor for local allergic reactions at the injection site. Local allergic reactions, such as redness, swelling, tenderness, or wheal formation, can occur after insulin injections.
Regular assessment of injection sites helps identify and monitor any allergic reactions. If reactions persist, an alternative type of insulin can be prescribed. Educate the patient about systemic allergic reactions to insulin and the appropriate response.
Although rare, systemic allergic reactions can occur, presenting as generalized urticaria hives or even anaphylaxis. Patients should be aware of these potential reactions and know to seek immediate medical attention if they experience any symptoms.
Desensitization with gradually increasing insulin doses may be necessary for treatment. Educate the patient about insulin lipodystrophy and the importance of rotation of injection sites.
Lipodystrophy refers to localized reactions at injection sites, including lipoatrophy loss of subcutaneous fat or lipohypertrophy fibrofatty masses. Using human insulin has greatly reduced the occurrence of lipodystrophy.
Patients should be educated about the importance of rotating injection sites to prevent the development of lipohypertrophy and delayed insulin absorption. Monitor for insulin resistance and collaborating with the healthcare team to adjust insulin doses. Insulin resistance may occur in some patients with diabetes, requiring higher insulin doses for adequate glycemic control.
Regular monitoring of blood glucose levels and close collaboration with the healthcare team allow for adjustments in insulin doses to address insulin resistance and control diabetes symptoms effectively.
Provide education on the causes of morning hyperglycemia and strategies to address it. Morning hyperglycemia can result from the dawn phenomenon , insulin waning, or the Somogyi effect.
Educating the patient about these causes helps them understand the importance of blood glucose monitoring during the night to determine the underlying cause. Adjustments in insulin doses and timing can be made accordingly to prevent morning hyperglycemia. Teach the patient about proper timing of insulin administration to address insulin waning.
Insulin waning refers to a progressive increase in blood glucose levels from bedtime to morning. Instructing the patient to administer the evening NPH insulin dose at bedtime rather than before dinner helps prevent insulin waning and ensures better glycemic control upon waking.
Oral antidiabetic agents are prescribed for patients with type 2 diabetes who do not respond effectively to medical nutrition therapy MNT and exercise alone.
Understanding the different classes of oral antidiabetic agents and how they work can empower the patient to actively participate in their treatment plan and recognize the importance of medication adherence.
Oral antidiabetic agents are used for patients with type 2 diabetes who cannot effectively manage their condition through diet and exercise alone. Oral antidiabetic agents may include:.
Second-Generation Sulfonylureas [glipizide Glucotrol , glimepiride Amaryl , glyburide Diabeta ] Sulfonylureas stimulate insulin release from the beta cells in the pancreas.
They improve binding insulin to receptors and may increase number of insulin receptors. They are indicated as adjunct to diet and exercise MNT. They are more potent than first-generation sulfonylureas and can be used in combination with metformin or insulin to improve glucose control.
Biguanides [metformin Glucophage ] Biguanides decreased the product and increases the uptake of glucose in the liver. It is effective in lowering blood glucose and does not cause hypoglycemia as the sulfonylureas do. It has been associated with development of lactic acidosis and GI distress and long term use may cause vitamin B12 deficiency.
Alpha-Glucosidase Inhibitors [acarbose Precose , miglitol Glyset ] inhibit alpha-glucosidase, an enzyme that breaks down glucose for absorption. Therefore, they delay the absorption of glucose.
They have only a mild effect on glucose levels and do not enhance insulin secretion. They are associated with severe hepatic toxicity and GI distress. Non-Sulfonylurea Insulin Secretagogues [repaglinide Prandin , nateglinide Starlix ] Stimulates the pancreas to secrete insulin.
It can be used alone or in combination with metformin to improve control of glucose. Thiazolidinediones or Glitazones [pioglitazone Actos , rosiglitazone Avandia ] Decreases insulin resistance by sensitizing the body to insulin and by stimulating insulin receptor sites to lower blood glucose and improve action of insulin.
Dipeptidyl Peptidase-4 DPP-4 Inhibitors [sitagliptin Januvia , saxagliptin Onglyza , linagliptin Tradjenta ] Slows the breakdown of GLP-1 to prolong the effects of increased insulin secretion, decreased glucagon secretion, and slowed GI emptying ultimately producing improved glucose control.
Glucagon-like Peptide-1 Agonist GLP-1 [liraglutide Victoza , dulaglutide Trulicity ] Enhances glucose-dependent insulin secretion and exhibit other antihyperglycemic actions following their release into the circulation from the gastrointestinal tract.
They may also lead to weight loss but can have side effects such as pancreatitis, diarrhea , nausea, and vomiting. Not suitable for patients with type 1 diabetes. Sodium-Glucose Co-Transporter 2 SGL-2 Inhibitors [dapagliflozin Forxiga , canagliflozin Invokana ] Increases urinary glucose excretion and lowers the renal threshold for glucose.
It is also prescribed to reduce the risk of major cardiovascular events in patients with established cardiovascular disease and type 2 DM. This drug improves glycemic control by decreasing glucose concentration in the blood through increased urinary excretion and reduced renal absorption of glucose.
Educate the patient about the complementary nature of oral antidiabetic agents with other treatment modalities, such as medical nutrition therapy MNT and exercise. Reinforcing the importance of a comprehensive approach to diabetes management encourages the patient to adhere to a balanced diet and engage in regular physical activity, which can enhance the effectiveness of oral antidiabetic agents.
Hyperglycemia resulting from these conditions may require temporary discontinuation of oral antidiabetic agents and initiation of insulin therapy. Regular monitoring helps detect any fluctuations in blood glucose levels and informs appropriate medication adjustments.
Provide education on insulin therapy and its potential use in combination with oral agents, particularly for newly diagnosed patients with type 2 diabetes who have symptomatic hyperglycemia and high blood glucose and A1C levels.
Some patients may require insulin therapy as an adjunct to oral antidiabetic agents to achieve glycemic targets. Educating the patient about insulin therapy helps alleviate any fears or misconceptions they may have and promotes acceptance and adherence to the prescribed treatment regimen.
Emphasize the importance of regular follow-up visits and laboratory tests to evaluate the effectiveness of oral antidiabetic agents and make necessary adjustments.
Regular follow-up visits and laboratory tests enable healthcare providers to modify the treatment plan as needed. Encourage the patient to report any adverse effects or changes in symptoms related to oral antidiabetic agents promptly.
Early identification and management of adverse effects or changes in symptoms associated with oral antidiabetic agents are essential to prevent complications and optimize treatment outcomes. Open communication encourages patients to seek timely medical assistance when needed.
Proper nutrition and meal planning are essential for diabetes management. Educating patients about healthy food choices, portion control, and balanced meals can help them achieve and maintain optimal blood glucose levels, lipid profiles, and blood pressure.
Calculations based on age, gender, height, and weight help determine the baseline caloric intake required for weight maintenance and overall health. This individualized approach supports accurate calorie control and ensures nutritional adequacy.
Factoring in physical activity provides a more accurate estimation of energy needs and supports the patient in achieving their weight goals. Subtract to calories from the daily total to promote a safe and gradual weight loss. To promote a 1- to 2-pound weight loss per week, a calorie deficit of to calories is recommended.
This approach supports gradual weight loss, which is associated with better long-term success and reduces the risk of adverse effects.
Simplify meal planning information and provide opportunities for practice and repetition. Some aspects of meal planning, such as using food exchange systems, may be challenging for patients due to intellectual limitations or emotional barriers.
Simplifying information and providing opportunities for practice and repetition can enhance patient understanding and proficiency in meal planning techniques. This approach helps patients develop confidence and competence in managing their dietary choices and fosters long-term adherence.
Balancing the distribution of macronutrients is crucial for maintaining optimal nutrition and supporting blood glucose control. Educate the patient about the recommended percentages of calories from carbohydrates, proteins, and fats. Providing education on the recommended caloric distribution helps patients understand the importance of balancing macronutrients in their diet.
By educating patients about the recommended percentages of calories from carbohydrates, proteins, and fats, nurses empower patients to make informed dietary choices that support blood glucose control, lipid management, and overall health.
Highlight the importance of increased fiber intake for improved blood glucose levels and other health benefits.
Increased fiber intake plays a significant role in improving blood glucose levels, lowering cholesterol, and promoting satiety. Educating patients about the benefits of fiber-rich foods, such as legumes, whole grains, fruits, and vegetables, encourages their inclusion in the meal plan and supports overall dietary and health goals.
Gradually increase fiber intake in consultation with a dietitian to prevent adverse effects. Sudden increases in fiber intake can lead to gastrointestinal discomfort and require adjustments in dosage of insulin or antidiabetic agents to prevent hypoglycemia.
Gradually increasing fiber intake in consultation with a dietitian allows for proper monitoring and adjustment of the meal plan to mitigate potential adverse effects. Educate patients about the use of exchange lists for meal planning.
Exchange lists are a commonly used tool in nutritional management for individuals with diabetes. Educating patients about the concept of exchange lists helps them understand how foods can be organized into groups with similar characteristics, such as calorie content and macronutrient composition.
This knowledge enables patients to create a well-balanced meal plan that maintains consistency in nutrient intake while providing variety in food choices. You can learn more about the Food Exchange List here. Teach patients how to read nutrition labels and understand carbohydrate content. Reading food labels is an essential skill for patients with diabetes when shopping for food.
Understanding the carbohydrate content of foods listed on nutrition labels allows patients to make informed choices and accurately determine the amount of medication needed, particularly for those who require premeal insulin. Explain the concept of carbohydrate counting and its flexibility in food choices.
Carbohydrate counting is a popular nutritional tool used for blood glucose management in both type 1 and type 2 diabetes. Educating patients about carbohydrate counting helps them understand that carbohydrates have the most significant impact on blood glucose levels.
This approach provides flexibility in food choices while maintaining blood glucose control. By incorporating carbohydrate counting into their meal planning, patients can achieve more accurate insulin management and maintain a balanced diet.
Educate patients about healthy food choices, portion control, and serving sizes. Encouraging patients to make healthy food choices and practice portion control is important for achieving and maintaining blood glucose control and weight management. Teaching patients to measure servings or choices, such as using standard portion sizes or the MyPlate Food Guide, helps them understand appropriate portion sizes for different food groups.
This approach can promote balanced nutrition, supports portion control, and simplifies meal planning for patients who may find more complicated systems challenging. Discuss the concept of the glycemic index and its potential impact on blood glucose levels.
The glycemic index measures how much a particular food increases blood glucose levels compared to an equivalent amount of glucose. Educating patients about the glycemic index helps them understand how different foods affect their blood glucose levels.
Encourage patients to monitor their blood glucose levels after consuming specific foods to create their own glycemic index. Monitoring blood glucose levels after eating specific foods allows patients to assess the individual impact of those foods on their blood glucose control.
This personalized approach empowers patients to make dietary adjustments based on their own glycemic response. By using this information, patients can modify their meal plans and insulin doses accordingly, leading to improved blood glucose control and individualized diabetes management.
Emphasize consistent meal timing and portion control. Consistency in meal timing and portion control helps regulate blood glucose levels. Patients should be educated on the importance of regular meals and the distribution of caloric intake throughout the day.
Avoiding skipped meals prevents glucose fluctuations and excessive demands on the pancreas. Support patients in implementing lifestyle changes. Lifestyle changes, including dietary modifications and increased physical activity, are integral to diabetes management.
Nurses play a vital role in providing support, motivation, and education to help patients adopt and sustain these changes.
Encourage weight loss and maintenance. Weight management is particularly important for obese patients with diabetes. Losing weight can improve blood glucose control and reduce the need for medication.
There is also substantial evidence indicating that managing obesity can significantly delay the progression from prediabetes to type 2 diabetes and provides significant benefits in the treatment of type 2 diabetes. Nurses should emphasize the significance of weight loss, provide guidance on healthy weight loss strategies, and offer ongoing support.
Address emotional issues and provide psychological support related to dietary changes. Some patients may struggle with emotional issues, such as accepting the diagnosis of diabetes or experiencing feelings of deprivation and restriction in eating.
Providing psychological support and addressing these concerns helps patients navigate the emotional aspects of meal planning. Provide behavioral therapy and ongoing nutrition counseling. Consistently following a meal plan and maintaining weight loss can be challenging.
Behavioral therapy, group support, and ongoing nutrition counseling can help patients incorporate new dietary habits into their lifestyles and sustain positive changes.
Collaborate with a registered dietitian. Registered dietitians specialize in medical nutrition therapy MNT for diabetes management. Reinforce the role of the nurse in communicating relevant information to the dietitian and promoting patient understanding. Effective communication between the nurse and the dietitian facilitates a coordinated and individualized approach to meal planning.
Educate patients about the importance of consistent eating habits and the relationship between food and insulin. Consistency in the amount of calories and carbohydrates ingested at each meal is crucial for patients requiring insulin to control blood glucose levels.
Educating patients about this relationship helps them understand the impact of food on insulin requirements and blood glucose control. It empowers patients to make informed choices about their meal timings and contents, fostering better glucose management. Emphasize the importance of moderation in alcohol consumption.
Educate patients about the potential adverse effects of alcohol specific to diabetes. Moderation is crucial when it comes to alcohol consumption for patients with diabetes.
Educating patients about the recommended limits for alcohol intake helps them understand the need to consume alcoholic beverages in controlled quantities. By promoting moderation, nurses assist patients in minimizing the potential negative impact of alcohol on their diabetes management.
Caution patients about the risk of hypoglycemia associated with alcohol consumption. Alcohol consumption can increase the risk of hypoglycemia, particularly for patients taking insulin or insulin secretagogues.
Educating patients about the potential effects of alcohol on blood glucose levels helps them understand the importance of consuming food along with alcohol to prevent hypoglycemia. By providing this information, nurses empower patients to make informed decisions about alcohol consumption and take appropriate measures to prevent hypoglycemia.
Encourage patients to incorporate food intake along with alcohol consumption. Consuming food along with alcohol can help reduce the risk of hypoglycemia.
By advising patients to have a meal or snack when consuming alcohol, nurses help ensure that patients maintain stable blood glucose levels.
However, it is important to note that carbohydrates consumed with alcohol may raise blood glucose levels. Providing this guidance helps patients strike a balance and make informed choices regarding food intake when consuming alcohol. Discuss the potential impact of alcohol on weight, hyperlipidemia , and glucose levels.
Alcohol consumption can contribute to weight gain, hyperlipidemia, and elevated glucose levels. Educating patients about the potential effects of alcohol on these aspects of their health helps them understand the importance of moderation and incorporating alcohol calories into their overall meal plan.
Educate patients about lower-calorie or less-sweet drink options. Recommending lower-calorie or less-sweet drink options, such as light beer or dry wine, helps patients make choices that align with their diabetes management goals. Educate patients about artificial sweeteners, including their types and use and emphasize moderation in sweetener use to avoid potential adverse effects.
Encouraging patients to use sweeteners in moderation helps prevent potential negative consequences. By promoting mindful consumption, patients can avoid excessive intake and maintain a balanced diet.
Explaining the distinction between nutritive e. Address potential side effects of certain sweeteners, such as sorbitol. Informing patients about potential side effects, such as the laxative effect of sorbitol-containing sweeteners, enables them to make decisions regarding the use of these products.
Patients can monitor their individual tolerance and adjust their intake accordingly. By clarifying that these foods should not be consumed in unlimited quantities, patients can manage their blood glucose levels more effectively and prevent potential spikes.
Regular exercise is essential in diabetes management as it helps lower blood glucose levels, improve insulin utilization, and reduce cardiovascular risk factors. Regular exercise is highly beneficial for individuals with diabetes. By encouraging patients to engage in regular exercise, nurses promote the importance of physical activity in managing blood glucose levels, reducing cardiovascular risk factors.
Provide guidelines for exercise frequency and duration. Guidelines for exercise frequency and duration help patients establish a structured exercise routine. By specifying three times per week with no more than two consecutive days without exercise, patients can maintain consistency in their exercise regimen, which contributes to better blood glucose control and overall fitness.
The American Diabetes Association recommends the following guidelines for physical activity:. Educate adults with type 2 diabetes about the significance of reducing sedentary behavior and interrupting prolonged sitting every 30 minutes for blood glucose benefits.
It is recommended for all adults, especially those with type 2 diabetes, to reduce sedentary behavior and interrupt prolonged sitting every 30 minutes for blood glucose benefits. Older adults with diabetes should incorporate flexibility and balance training times per week, with options such as yoga and tai chi.
Individuals with type 1 diabetes and type 2 diabetes should evaluate their baseline physical activity and sedentary time, aiming to increase non sedentary activities above their baseline.
Discuss the benefits of exercise and weight loss for individuals with type 2 diabetes. For individuals with type 2 diabetes who are overweight or obese, engaging in exercise alongside dietary management offers multiple benefits, including improved glucose metabolism and enhanced body fat loss.
Exercise coupled with weight loss improves insulin sensitivity and may decrease the need for insulin or oral antidiabetic agents. Educating patients on the potential positive outcomes of exercise and weight loss encourages them to incorporate physical activity as part of their diabetes management plan.
Emphasize the importance of a gradual increase in exercise duration. A slow and gradual increase in the duration of exercise sessions is recommended to prevent excessive strain or injury. Allowing the patient to gradually build endurance and fitness levels over time, the nurse can promote safe and sustainable exercise habits.
Recommend walking as a safe and accessible form of exercise. Walking is a low-impact and easily accessible form of exercise that can be performed by most individuals with diabetes.
It requires no special equipment other than proper shoes and can be incorporated into daily routines. By recommending walking, nurses provide patients with a practical and feasible exercise option that can be sustained long-term. Encourage patients to discuss an exercise program with their primary healthcare provider and undergo a medical evaluation.
Before initiating an exercise program, it is important for patients to consult with their primary healthcare provider and undergo a medical evaluation. Assess blood glucose and ketone levels before initiating exercise.
Monitoring blood glucose and ketone levels before exercise is crucial for patients with diabetes. Exercising with elevated blood glucose levels can further increase blood glucose levels, potentially leading to hyperglycemia and other complications.
Educate patients on pre-exercise carbohydrate snacks for insulin-treated individuals. Patients who require insulin should be taught to consume a g carbohydrate snack or a snack of complex carbohydrates with protein before engaging in moderate exercise.
This pre-exercise snack helps prevent unexpected hypoglycemia by providing the necessary fuel for physical activity and counteracting the potential decrease in circulating insulin during exercise.
Provide instructions on managing post-exercise hypoglycemia for patients taking insulin. Hypoglycemia can occur hours after exercise in patients taking insulin. To prevent post-exercise hypoglycemia, patients may need to consume a snack at the end of the exercise session and at bedtime, as well as monitor their blood glucose levels more frequently.
Patients who are capable, knowledgeable, and responsible can learn to adjust their insulin doses in collaboration with a diabetes educator. Others require specific instructions on managing their blood glucose levels during and after exercise.
Educate patients on regular blood glucose monitoring during extended periods of exercise. Patients taking insulin and engaging in extended periods of exercise should monitor their blood glucose levels before, during, and after the exercise period.
This monitoring helps them adjust their carbohydrate intake to maintain blood glucose levels within the target range. It is important for others involved in exercise activities to be aware that the person exercising has diabetes. By informing exercise participants and observers, they can provide appropriate assistance in case of severe hypoglycemia.
This promotes a safe exercise environment and ensures that prompt action can be taken if a diabetes-related emergency occurs. Provide education on exercise considerations for patients with diabetic complications. Patients with diabetic complications, such as retinopathy, autonomic neuropathy, sensorimotor neuropathy, and cardiovascular disease, may require modifications in their exercise regimen.
Programs can encourage healthcare providers to speak openly with patients about self-management and refer patients to self-management programs. Patients with diabetes should be encouraged to ask questions and be reminded that these activities can help them to achieve successful disease management.
Diabetes Self-Management Education and Support in Rural America Website An overview of the benefits of diabetes self-management programs.
Describes different types of diabetes self-management education and support programs available to communities. Organization s : Centers for Disease Control and Prevention CDC. Diabetes Self-Management Education and Support Website Provides links to resources and tools to help communities develop, promote, implement and sustain diabetes self-management education and support DSMES programs.
Includes a DSMES toolkit, technical assistance guide, policies, reports, and several case studies. Diabetes Self-Management Program DSMP Website Describes the Stanford self-management model, an evidence-based program delivered by certified trainers, designed to improve diabetes self-management practices.
The trainers are non-health professionals who may have diabetes themselves and have completed the master training program. Includes educational resources that supplement the program curriculum.
Organization s : Self-Management Resource Center. My Diabetes Self-Management Goal Document A worksheet helpful to individuals when managing their diabetes and setting personal health goals.
Menu Search. Evidence-based Toolkits FORHP Funded Programs Economic Impact Analysis Tool Community Health Gateway Testing New Approaches Care Management Reimbursement.
Living with diabetes Self-care plans for diabetes management plns Self-care plans for diabetes management requires significant effort poans manage the condition effectively. Along pplans following a healthy diet, monitoring blood eiabetes levels, and adhering Allergen cross-contamination the Selfcare medication therapy, self-care practices play a crucial role in diabetes management. In general, self-care refers to the deliberate and proactive steps you may take to care for your physical, emotional, and mental health. When it comes to diabetes management, self-care means developing knowledge and awareness by learning to live with the complex nature of the condition. Practices include exercise, healthy eating, stress reduction techniques, and more frequent tracking of your blood sugar levels.Diabetes mellitus DM is a chronic progressive metabolic disorder characterized by hyperglycemia mainly Rehydration for overall well-being to absolute Type 1 DM or relative Type 2 DM deficiency of insulin hormone.
World Health Organization estimates that more than million people worldwide have DM. Olans number ror likely to more than double by without any diabetse. The needs of diabetic patients are not only limited to adequate glycemic control but also correspond with preventing plahs disability limitation and rehabilitation.
There are seven essential self-care managrment in Endurance training for cyclists with diabetes which Fair trade coffee beans good outcomes namely healthy eating, being physically active, monitoring of blood sugar, Self-care plans for diabetes management with medications, good problem-solving skills, Self-fare coping skills and risk-reduction maagement.
All these Sel-care behaviors diagetes been found Self-care plans for diabetes management be positively correlated with good Nutritional tips for sports performance control, Metabolic health research studies of complications and improvement in quality of Idabetes.
Individuals with diabetes have been Resistance training for athletes to make a dramatic impact on the progression and development of their disease by participating in their own care. Despite Sef-care fact, compliance or adherence to these activities has been found to be low, especially when looking at long-term changes.
Though multiple demographic, foor and social support Self-crae can be considered as positive contributors diabeges facilitating self-care activities in Self-care plans for diabetes management patients, role of clinicians in promoting self-care is vital and has to be emphasized.
Realizing the Self-care plans for diabetes management nature llans the Self-cage, a systematic, multi-pronged and an manxgement approach is required for promoting self-care ffor among managemen patients Selff-care avert any long-term complications.
Astrid N. van Managemnt, Dorijn F. Plahs, … Marijke Melles. Diabetes mellitus DM is a chronic progressive metabolic disorder characterized by hyperglycemia mainly due to absolute Type 1 DM or relative Type 2 DM diabets of insulin hormone[ 1 ]. DM virtually affects every system of the body mainly due to dkabetes disturbances caused by hyperglycemia, Sel-fcare if diabetes control over Antioxidant rich spices period of time Slf-care to be suboptimal[ 1 ].
Until recently it was believed to be a disease occurring diabete in developed Se,f-care, but recent findings reveal a rise in number of new Self-czre of type 2 DM Self-cage an earlier Enhances mental quickness and associated complications in developing managemeent 2 — 4 ].
Diabetes manayement associated with complications such as ppans diseases, nephropathy, retinopathy and neuropathy, plan can lead to chronic morbidities and mortality[ diavetes6 diabftes. World Health Organization WHO estimates dibetes more than million people worldwide have DM.
According to WHO report, India today manageemnt the world with over 32 million diabetic patients and this number is projected to increase to Self-acre One of the biggest challenges for health care providers Selr-care is addressing the continued needs and demands mznagement individuals with plas illnesses like diabetes[ 12 ].
Diabets Self-care plans for diabetes management of regular follow-up of diabetic patients with planns health care provider is of great significance in averting any long term complications. Studies have reported that dianetes Self-care plans for diabetes management control can delay or prevent the Self-care empowerment for diabetes patients of diabetees associated with diabetes[ 13 Best foods for injury recovery, 14 ].
Some of the Indian studies revealed very poor adherence to treatment regimens due to poor attitude towards the disease and poor health literacy among the mangement public[ 1516 ]. The introduction of home blood glucose monitors and mxnagement use of glycosylated hemoglobin as an indicator of metabolic control has contributed dabetes self-care in diabetes and thus has shifted more responsibility to the patient[ 1718 Metabolic rate factors. Self-care in diabetes has been defined as an Self-care plans for diabetes management process of development of knowledge or awareness by learning to survive with the complex nature of the diabetes plsns a managemeht context[ 2021 manafement.
There are seven essential self-care behaviors in Self-cars with diabetes which Self-care plans for diabetes management kanagement outcomes.
Diabetee are diaebtes eating, being physically active, monitoring of Self-cafe sugar, compliant with medications, good problem-solving skills, healthy coping skills and risk-reduction behaviors[ 26 ].
These Selc-care measures can be useful for both clinicians and educators treating individual patients and for managemsnt evaluating new approaches to care.
Self-report is Selt-care far the most Stress management techniques and cost-effective Self-cars to self-care assessment and yet is often seen as undependable. Diabetes self-care activities are behaviors undertaken by people with or at risk of diabetes mnagement order to successfully manage the managgement on their own[ managemejt ].
All these Selg-care behaviors have been found to be positively correlated with good glycemic control, reduction of complications and improvement in quality of life[ 27 — 31 ].
In addition, it was observed that self-care encompasses not only performing these activities but also the interrelationships between them[ 32 ]. Diabetes self-care requires the patient to make many dietary and lifestyle modifications supplemented with the supportive role of healthcare staff for maintaining a higher level of self-confidence leading to a successful behavior change[ 33 ].
Though genetics play an important role in the development of diabetes, monozygotic twin studies have certainly shown the importance of environmental influences[ 34 ].
Individuals with diabetes have been shown to make a dramatic impact on the progression and development of their disease by participating in their own care[ 13 ].
This participation can succeed only if those with diabetes and their health care providers are informed about taking effective care for the disease.
It is expected that those with the greatest knowledge will have a better understanding of the disease and have a better impact on the progression of the disease and complications.
The American Association of Clinical Endocrinologists emphasizes the importance of patients becoming active and knowledgeable participants in their care[ 35 ]. Likewise, WHO has also recognized the importance of patients learning to manage their diabetes[ 36 ].
The American Diabetes Association had reviewed the standards of diabetes self management education and found that there was a four-fold increase in diabetic complications for those individuals with diabetes who had not received formal education concerning self-care practices[ 37 ].
A meta-analysis of self-management education for adults with type-2 diabetes revealed improvement in glycemic control at immediate follow-up.
However, the observed benefit declined one to three months after the intervention ceased, suggesting that continuing education is necessary[ 38 ]. A review of diabetes self-management education revealed that education is successful in lowering glycosylated hemoglobin levels[ 39 ].
Diabetes education is important but it must be transferred to action or self-care activities to fully benefit the patient. Self-care activities refer to behaviors such as following a diet plan, avoiding high fat foods, increased exercise, self-glucose monitoring, and foot care[ 40 ].
Changes in self-care activities should also be evaluated for progress toward behavioral change[ 41 ]. Self-monitoring of glycemic control is a cornerstone of diabetes care that can ensure patient participation in achieving and maintaining specific glycemic targets.
The most important objective of monitoring is the assessment of overall glycemic control and initiation of appropriate steps in a timely manner to achieve optimum control.
Self-monitoring provides information about current glycemic status, allowing for assessment of therapy and guiding adjustments in diet, exercise and medication in order to achieve optimal glycemic control. Irrespective of weight loss, engaging in regular physical activity has been found to be associated with improved health outcomes among diabetics[ 42 — 45 ].
The National Institutes of Health[ 46 ] and the American College of Sports Medicine[ 47 ] recommend that all adults, including those with diabetes, should engage in regular physical activity.
Treatment adherence in diabetes is an area of interest and concern to health professionals and clinical researchers even though a great deal of prior research has been done in the area.
In diabetes, patients are expected to follow a complex set of behavioral actions to care for their diabetes on a daily basis. These actions involve engaging in positive lifestyle behaviors, including following a meal plan and engaging in appropriate physical activity; taking medications insulin or an oral hypoglycemic agent when indicated; monitoring blood glucose levels; responding to and self-treating diabetes- related symptoms; following foot-care guidelines; and seeking individually appropriate medical care for diabetes or other health-related problems[ 48 ].
The majority of patients with diabetes can significantly reduce the chances of developing long-term complications by improving self-care activities. In the process of delivering adequate support healthcare providers should not blame the patients even when their compliance is poor[ 49 ].
One of the realities about type-2 diabetes is that only being compliant to self-care activities will not lead to good metabolic control. Research work across the globe has documented that metabolic control is a combination of many variables, not just patient compliance[ 5152 ]. In an American trial, it was found that participants were more likely to make changes when each change was implemented individually.
Success, therefore, may vary depending on how the changes are implemented, simultaneously or individually[ 53 ]. Some of the researchers have even suggested that health professionals should tailor their patient self-care support based on the degree of personal responsibility the patient is willing to assume towards their diabetes self-care management[ 54 ].
The role of healthcare providers in care of diabetic patients has been well recognized. Socio-demographic and cultural barriers such as poor access to drugs, high cost, patient satisfaction with their medical care, patient provider relationship, degree of symptoms, unequal distribution of health providers between urban and rural areas have restricted self-care activities in developing countries[ 3955 — 58 ].
Another study stressed on both patient factors adherence, attitude, beliefs, knowledge about diabetes, culture and language capabilities, health literacy, financial resources, co-morbidities and social support and clinician related factors attitude, beliefs and knowledge about diabetes, effective communication [ 60 ].
Because diabetes self-care activities can have a dramatic impact on lowering glycosylated hemoglobin levels, healthcare providers and educators should evaluate perceived patient barriers to self-care behaviors and make recommendations with these in mind.
Unfortunately, though patients often look to healthcare providers for guidance, many healthcare providers are not discussing self-care activities with patients[ 61 ]. Some patients may experience difficulty in understanding and following the basics of diabetes self-care activities.
When adhering to self-care activities patients are sometimes expected to make what would in many cases be a medical decision and many patients are not comfortable or able to make such complex assessments.
It is critical that health care providers actively involve their patients in developing self-care regimens for each individual patient.
This regimen should be the best possible combination for every individual patient plus it should sound realistic to the patient so that he or she can follow it[ 62 ].
Also, the need of regular follow-up can never be underestimated in a chronic illness like diabetes and therefore be looked upon as an integral component of its long term management.
A clinician should be able to recognize patients who are prone for non-compliance and thus give special attention to them. On a grass-root level, countries need good diabetes self-management education programs at the primary care level with emphasis on motivating good self-care behaviors especially lifestyle modification.
Furthermore, these programs should not happen just once, but periodic reinforcement is necessary to achieve change in behavior and sustain the same for long-term. While organizing these education programs adequate social support systems such as support groups, should be arranged.
As most of the reported studies are from developed countries so there is an immense need for extensive research in rural areas of developing nations. Concurrently, field research should be promoted in developing countries about perceptions of patients on the effectiveness of their self-care management so that resources for diabetes mellitus can be used efficiently.
To prevent diabetes related morbidity and mortality, there is an immense need of dedicated self-care behaviors in multiple domains, including food choices, physical activity, proper medications intake and blood glucose monitoring from the patients. World health organization: Definition, diagnosis and classification of diabetes mellitus and its complications.
Geneva: World health organization; Google Scholar. Kinra S, Bowen LJ, Lyngdoh T, Prabhakaran D, Reddy KS, Ramakrishnan L: Socio-demographic patterning of non-communicable disease risk factors in rural India: a cross sectional study. BMJc Article PubMed PubMed Central Google Scholar.
Chuang LM, Tsai ST, Huang BY, Tai TY: The status of diabetes control in Asia—a cross-sectional survey of 24 patients with diabetes mellitus in Diabet Med19 12 — Article CAS PubMed Google Scholar.
Narayanappa D, Rajani HS, Mahendrappa KB, Prabhakar AK: Prevalence of pre-diabetes in school-going children. Indian Pediatr48 4 — American Diabetes Association: Implications of the United Kingdom Prospective Diabetes Study. Diabetes Care27 Suppl 1 — Zucchi P, Ferrari P, Spina ML: Diabetic foot: from diagnosis to therapy.
G Ital Nefrol22 Suppl 31 :SS PubMed Google Scholar. World health organization: Diabetes — Factsheet. Mohan D, Raj D, Shanthirani CS, Datta M, Unwin NC, Kapur A: Awareness and knowledge of diabetes in Chennai - The Chennai urban rural epidemiology study.
J Assoc Physicians India— Wild S, Roglic G, Green A, Sicree R, King H: Global prevalence of diabetes: Estimates for the year and projections for Diabetes Care27 5 —
: Self-care plans for diabetes management| Benefits Associated With DSMES | Half of the plate should contain maangement vegetables fog, Self-care plans for diabetes management quarter can contain grain-based and starchy foods, and the remaining quarter should managekent Self-care plans for diabetes management. Educating the patient about African Mango Core variations helps them understand the potential differences in insulin action and adjust their self-management strategies accordingly. It is important for people with diabetes or prediabetes to achieve and maintain a healthy weight. Related Coverage. They need to identify education and other needs expeditiously in order to address the nuances of self-management and highlight the value of ongoing education. |
| Diabetes self-management tips | Sources: Bonoto BC, de Araújo VE, Godói IP, de Lemos LL, Godman B, Bennie M, Diniz LM, Junior AA. Efficacy of Mobile Apps to Support the Care of Patients With Diabetes Mellitus: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. JMIR Mhealth Uhealth. doi: PMID: ; PMCID: PMC El-Gayar O, Timsina P, Nawar N, Eid W. Mobile applications for diabetes self-management: status and potential. J Diabetes Sci Technol. Lin EH, Von Korff M, Alonso J, Angermeyer MC, Anthony J, Bromet E, Bruffaerts R, Gasquet I, de Girolamo G, Gureje O, Haro JM, Karam E, Lara C, Lee S, Levinson D, Ormel JH, Posada-Villa J, Scott K, Watanabe M, Williams D. Mental disorders among persons with diabetes—results from the World Mental Health Surveys. J Psychosom Res. Epub Oct Bădescu SV, Tătaru C, Kobylinska L, Georgescu EL, Zahiu DM, Zăgrean AM, Zăgrean L. The association between Diabetes mellitus and Depression. J Med Life. Tags: blood sugar diabetes diabetes management exercise important stress. Share This Article. Share on Facebook Share on Facebook Tweet Share on Twitter Pin it Share on Pinterest Share on LinkedIn Share on LinkedIn. Related posts. Understanding Common Health Complications in Diabetes February 9, The Evolution of CGM Pumps in Diabetes Management — Celebrating 50 Years of Innovation January 19, Making Diabetes Food Exciting with Spices December 4, Empowering Prevention and Care with Diabetes:M November 14, Diabetes Health Maintenance: Routine Monitoring and Care November 1, Join Diabetes:M at HETT in London September 13, Leave a Reply Cancel reply Your email address will not be published. This website uses cookies to ensure you get the best experience on our website Accept Read More. Cookies Policy. Close Privacy Overview This website uses cookies to improve your experience while you navigate through the website. Out of these, the cookies that are categorized as necessary are stored on your browser as they are essential for the working of basic functionalities of the website. We also use third-party cookies that help us analyze and understand how you use this website. These cookies will be stored in your browser only with your consent. You also have the option to opt-out of these cookies. Alcohol can lower blood sugar levels long after you've had your last drink. So check your blood sugar level before you go to sleep. The snack can counter a drop in your blood sugar. Changes in hormone levels the week before and during periods can lead to swings in blood sugar levels. Look for patterns. Keep careful track of your blood sugar readings from month to month. You may be able to predict blood sugar changes related to your menstrual cycle. Your healthcare professional may recommend changes in your meal plan, activity level or diabetes medicines. These changes can make up for blood sugar swings. Check blood sugar more often. If you're likely nearing menopause or if you're in menopause, talk with your healthcare professional. Ask whether you need to check your blood sugar more often. Also, be aware that menopause and low blood sugar have some symptoms in common, such as sweating and mood changes. So whenever you can, check your blood sugar before you treat your symptoms. That way you can confirm whether your blood sugar is low. Most types of birth control are safe to use when you have diabetes. But combination birth control pills may raise blood sugar levels in some people. It's very important to take charge of stress when you have diabetes. The hormones your body makes in response to prolonged stress may cause your blood sugar to rise. It also may be harder to closely follow your usual routine to manage diabetes if you're under a lot of extra pressure. Take control. Once you know how stress affects your blood sugar level, make healthy changes. Learn relaxation techniques, rank tasks in order of importance and set limits. Whenever you can, stay away from things that cause stress for you. Exercise often to help relieve stress and lower your blood sugar. Get help. Learn new ways to manage stress. You may find that working with a psychologist or clinical social worker can help. These professionals can help you notice stressors, solve stressful problems and learn coping skills. The more you know about factors that have an effect on your blood sugar level, the better you can prepare to manage diabetes. If you have trouble keeping your blood sugar in your target range, ask your diabetes healthcare team for help. There is a problem with information submitted for this request. Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview. Error Email field is required. Error Include a valid email address. To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail. You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox. Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission. Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press. This content does not have an English version. This content does not have an Arabic version. Appointments at Mayo Clinic Mayo Clinic offers appointments in Arizona, Florida and Minnesota and at Mayo Clinic Health System locations. Request Appointment. Diabetes management: How lifestyle, daily routine affect blood sugar. Products and services. Diabetes management: How lifestyle, daily routine affect blood sugar Diabetes management takes awareness. By Mayo Clinic Staff. Thank you for subscribing! Sorry something went wrong with your subscription Please, try again in a couple of minutes Retry. Show references Facilitating behavior change and well-being to improve health outcomes. Standards of Medical Care in Diabetes — Diabetes Care. Nutrition overview. American Diabetes Association. Accessed Dec. Diabetes and mental health. Centers for Disease Control and Prevention. Insulin, medicines, and other diabetes treatments. National Institute of Diabetes and Digestive and Kidney Diseases. Insulin storage and syringe safety. Diabetes diet, eating, and physical activity. Type 2 diabetes mellitus adult. Mayo Clinic; Wexler DJ. Initial management of hyperglycemia in adults with type 2 diabetes mellitus. Diabetes and women. Planning for sick days. Diabetes: Managing sick days. Castro MR expert opinion. Mayo Clinic. Hypoglycemia low blood glucose. Blood glucose and exercise. Riddell MC. Exercise guidance in adults with diabetes mellitus. Colberg SR, et al. Palermi S, et al. The complex relationship between physical activity and diabetes: An overview. Journal of Basic and Clinical Physiology and Pharmacology. Take charge of your diabetes: Your medicines. Sick day management for adults with type 1 diabetes. Association of Diabetes Care and Education Specialists. Alcohol and diabetes. Diabetes and nerve damage. Roe AH, et al. Combined estrogen-progestin contraception: Side effects and health concerns. Products and Services The Mayo Clinic Diet Online A Book: The Essential Diabetes Book. See also Medication-free hypertension control A1C test Alcohol: Does it affect blood pressure? Alpha blockers Amputation and diabetes Angiotensin-converting enzyme ACE inhibitors Angiotensin II receptor blockers Anxiety: A cause of high blood pressure? Artificial sweeteners: Any effect on blood sugar? Bariatric surgery Beta blockers Beta blockers: Do they cause weight gain? Beta blockers: How do they affect exercise? Blood glucose meters Blood glucose monitors Blood pressure: Can it be higher in one arm? Blood pressure chart Blood pressure cuff: Does size matter? Blood pressure: Does it have a daily pattern? Blood pressure: Is it affected by cold weather? Blood pressure medication: Still necessary if I lose weight? Blood pressure medications: Can they raise my triglycerides? Blood pressure readings: Why higher at home? Blood pressure tip: Get more potassium Blood sugar levels can fluctuate for many reasons Blood sugar testing: Why, when and how Bone and joint problems associated with diabetes Pancreas transplant animation Caffeine and hypertension Calcium channel blockers Calcium supplements: Do they interfere with blood pressure drugs? Can whole-grain foods lower blood pressure? Central-acting agents Choosing blood pressure medicines COVID Who's at higher risk of serious symptoms? Diabetes Diabetes and depression: Coping with the two conditions Diabetes and exercise: When to monitor your blood sugar Diabetes and heat 10 ways to avoid diabetes complications Diabetes diet: Should I avoid sweet fruits? Diabetes diet: Create your healthy-eating plan Diabetes foods: Can I substitute honey for sugar? Diabetes and liver Diabetes symptoms Diabetes treatment: Can cinnamon lower blood sugar? Using insulin Diabetic Gastroparesis Diuretics Diuretics: A cause of low potassium? Erectile dysfunction and diabetes High blood pressure and exercise Exercise and chronic disease Fatigue Free blood pressure machines: Are they accurate? Frequent urination Home blood pressure monitoring Glucose tolerance test Glycemic index: A helpful tool for diabetes? Hemochromatosis High blood pressure hypertension High blood pressure and cold remedies: Which are safe? Med Sci Sports Exerc , 39 8 — Goodall TA, Halford WK: Self-management of diabetes mellitus: a critical review. Health Psychol , 10 1 :1—8. Marrero DG, Kako KS, Mayfield J, Wheeler ML, Fineberg N: Nutrition management of type-2 diabetes by primary care physicians. J Gen Intern Med , 15 11 — Article CAS PubMed PubMed Central Google Scholar. Kotwani A, Ewen M, Dey D, Iyer S, Lakshmi PK, Patel A: Prices and availability of common medicines at six sites in India using a standard methodology. Indian J Med Res , 25 5 — Toljamo M, Hentinen M: Adherence to self-care and glycemic control among people with insulin-dependent diabetes mellitus. J Adv Nurs , 34 6 — Wing RR, Goldstein MG, Kelly JA, Birch LL, Jakic JM, Sallis JF: Behavioral science research in diabetes. Chronic Illn , 4 1 — Ramachandran A, Ramachandran S, Snehalatha C, Augustine C, Murugesan N, Viswanathan V: Increasing expenditure on health care incurred by diabetic subjects in a developing country: A study from India. Diabetes Care , 30 2 — Debussche X, Debussche BM, Besançon S, Traore AS: Challenges to diabetes self-management in developing countries. Diabetes Voice , 12— Ciechanowski PS, Katon WJ, Russo JE, Walker EA: The patient-provider relationship: attachment theory and adherence to treatment in diabetes. Am J Psychiatry , 1 — Grant RW, Devita NG, Singer DE, Meigs JB: Poly-pharmacy and medication adherence in patients with type 2 diabetes. Diabetes Care , 26 5 — Chin MH, Cook S, Jin L, Drum ML, Harrison JF, Koppert J: Barriers to providing diabetes care in community health center. Diabetes Care , 24 2 — Nam S, Chesla C, Stotts NA, Kroon L, Janson SL: Barriers to diabetes management: patient and provider factors. Diabetes Res Clin Pract , 93 1 :1—9. Preventative care practices among persons with diabetes - United States: — Morb Mortal Wkly Rep , 51 43 — Anderson RM: Patient empowerment and the traditional medical model: a case of irreconcilable differences? Diabetes Care , 18 3 — Download references. You can also search for this author in PubMed Google Scholar. Correspondence to Saurabh RamBihariLal Shrivastava. SRS wrote the first draft of the article and performed intensive review of literature. PSS edited the article continuously. JR read and approved the final manuscript. All authors read and approved the final manuscript. This article is published under license to BioMed Central Ltd. Reprints and permissions. Shrivastava, S. Role of self-care in management of diabetes mellitus. J Diabetes Metab Disord 12 , 14 Download citation. Received : 22 January Accepted : 28 February Published : 05 March Anyone you share the following link with will be able to read this content:. Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative. Download PDF. Abstract Diabetes mellitus DM is a chronic progressive metabolic disorder characterized by hyperglycemia mainly due to absolute Type 1 DM or relative Type 2 DM deficiency of insulin hormone. Self-Management in Diabetes Chapter © Healthy Lifestyles for the Self-Management of Type 2 Diabetes Chapter © Use our pre-submission checklist Avoid common mistakes on your manuscript. Introduction Diabetes mellitus DM is a chronic progressive metabolic disorder characterized by hyperglycemia mainly due to absolute Type 1 DM or relative Type 2 DM deficiency of insulin hormone[ 1 ]. Addressing needs of diabetic patients One of the biggest challenges for health care providers today is addressing the continued needs and demands of individuals with chronic illnesses like diabetes[ 12 ]. Self-care in diabetes Self-care in diabetes has been defined as an evolutionary process of development of knowledge or awareness by learning to survive with the complex nature of the diabetes in a social context[ 20 , 21 ]. Diabetes self management education Though genetics play an important role in the development of diabetes, monozygotic twin studies have certainly shown the importance of environmental influences[ 34 ]. Diabetes self-care activities Diabetes education is important but it must be transferred to action or self-care activities to fully benefit the patient. Compliance to self-care activities Treatment adherence in diabetes is an area of interest and concern to health professionals and clinical researchers even though a great deal of prior research has been done in the area. Barriers to diabetes care The role of healthcare providers in care of diabetic patients has been well recognized. Recommendations for self-care activities Because diabetes self-care activities can have a dramatic impact on lowering glycosylated hemoglobin levels, healthcare providers and educators should evaluate perceived patient barriers to self-care behaviors and make recommendations with these in mind. Implications for practice A clinician should be able to recognize patients who are prone for non-compliance and thus give special attention to them. Implications for future research As most of the reported studies are from developed countries so there is an immense need for extensive research in rural areas of developing nations. Conclusion To prevent diabetes related morbidity and mortality, there is an immense need of dedicated self-care behaviors in multiple domains, including food choices, physical activity, proper medications intake and blood glucose monitoring from the patients. Funding No sources of support provided. References World health organization: Definition, diagnosis and classification of diabetes mellitus and its complications. Google Scholar Kinra S, Bowen LJ, Lyngdoh T, Prabhakaran D, Reddy KS, Ramakrishnan L: Socio-demographic patterning of non-communicable disease risk factors in rural India: a cross sectional study. c Article PubMed PubMed Central Google Scholar Chuang LM, Tsai ST, Huang BY, Tai TY: The status of diabetes control in Asia—a cross-sectional survey of 24 patients with diabetes mellitus in x Article CAS PubMed Google Scholar Narayanappa D, Rajani HS, Mahendrappa KB, Prabhakar AK: Prevalence of pre-diabetes in school-going children. Google Scholar Zucchi P, Ferrari P, Spina ML: Diabetic foot: from diagnosis to therapy. PubMed Google Scholar World health organization: Diabetes — Factsheet. html Google Scholar Mohan D, Raj D, Shanthirani CS, Datta M, Unwin NC, Kapur A: Awareness and knowledge of diabetes in Chennai - The Chennai urban rural epidemiology study. PubMed Google Scholar Wild S, Roglic G, Green A, Sicree R, King H: Global prevalence of diabetes: Estimates for the year and projections for CAS PubMed Google Scholar Katulanda P, Constantine GR, Mahesh JG, Sheriff R, Seneviratne RD, Wijeratne S: Prevalence and projections of diabetes and pre-diabetes in adults in Sri Lanka - Sri Lanka Diabetes, Cardiovascular Study SLDCS. x Article CAS PubMed Google Scholar Wagner EH, Austin BT, Davis C, Hindmarsh M, Schaefer J, Bonomi A: Improving chronic illness care: translating evidence into action. Article Google Scholar Ohkubo Y, Kishikawa H, Araki E, Miyata T, Isami S, Motoyoshi S: Intensive insulin therapy prevents the progression of diabetic micro-vascular complications in Japanese patients with non-insulin-dependent diabetes mellitus: a randomized prospective 6-year study. Google Scholar Chew LD: The impact of low health literacy on diabetes outcomes. Google Scholar Grey M, Thurber FW: Adaptation to chronic illness in childhood: diabetes mellitus. CAS PubMed Google Scholar Glasgow RE, Hiss RG, Anderson RM, Friedman NM, Hayward RA, Marrero DG: Report of the health care delivery work group: behavioral research related to the establishment of a chronic disease model for diabetes care. PubMed Google Scholar Bradley C: Handbook of Psychology and Diabetes. Google Scholar Johnson SB: Health behavior and health status: concepts, methods and applications. Article CAS PubMed Google Scholar American Association of Diabetes Educators: AADE7 Self-Care Behaviors. Google Scholar Povey RC, Clark-Carter D: Diabetes and healthy eating: A systematic review of the literature. Article PubMed Central Google Scholar Odegard PS, Capoccia K: Medication taking and diabetes: A systematic review of the literature. Google Scholar Herschbach P, Duran G, Waadt S, Zettler A, Amch C: Psychometric properties of the questionnaire on stress in patients with diabetes-revised QSD-R. CAS PubMed Google Scholar Poulsen P, Kyvik OK, Vag A, Nielsen-Beck H: Heritability of type II diabetes mellitus and abnormal glucose tolerance — a population-based twin study. Google Scholar Hendra JT, Sinclair AJ: Improving the care of elderly diabetic patients: the final report of the St. Article PubMed Google Scholar Williams GC, Freedman ZR, Deci EL: Supporting autonomy to motivate patients with diabetes for glucose control. Article PubMed Central Google Scholar Colberg SR, Sigal RJ, Fernhall B, Regensteiner JG, Blissmer BJ, Rubin RR: Exercise and type-2 diabetes. Google Scholar United States Department of Health and Human Services : Physical Activity Guidelines for Americans; Article CAS PubMed Google Scholar Marrero DG, Kako KS, Mayfield J, Wheeler ML, Fineberg N: Nutrition management of type-2 diabetes by primary care physicians. x Article CAS PubMed PubMed Central Google Scholar Kotwani A, Ewen M, Dey D, Iyer S, Lakshmi PK, Patel A: Prices and availability of common medicines at six sites in India using a standard methodology. htm Toljamo M, Hentinen M: Adherence to self-care and glycemic control among people with insulin-dependent diabetes mellitus. |
| How to manage diabetes | This article will focus on your own T2D self-care, involving everything from blood sugar monitoring, insulin or other medications, meal planning, and adequate exercise routines that can keep your health and diabetes management in check. A nationwide survey of several hundred diabetes care and education specialists estimated that it took adults with T2D about 66 minutes a day for routine self-care. The education specialists included monitoring blood sugar twice daily and oral medication into their estimate. By contrast, you may only spend 1 hour or less every few months seeing a healthcare team for checkups, tests, and guidance. One doctor survey notes your time with that person may only be 17 to 24 minutes. Because so much of your treatment is in your hands, knowing how to go about self-care is essential. Diabetes is a chronic condition that requires ongoing care to prevent or lessen complications. Self-care each day may help determine how you feel and how you stay healthy in the long term. Monitoring your blood sugar is one of the most important things you can do to manage diabetes. Some people may need to check a couple of times a day, while others may choose to check their blood sugars more frequently. You may choose to poke your finger for a small blood drop to check your blood sugar on a small handheld meter, or you may opt for a continuous glucose monitor that provides a more complete picture of how your glucose levels are fluctuating throughout the day. People who need to check their blood sugar more often include those who:. You can read more about how blood sugars or glucose levels play a part in your diabetes management and understand what glucose goals may be best for you to discuss with a healthcare team. Your healthcare team may suggest one or more medications to help you manage T2D. These medications may include:. A healthcare team may also prescribe other common medications for T2D. Lifestyle changes are an essential way to manage diabetes. These changes may include exercise, maintaining a moderate weight, and eating a healthy and nutritious diet. You may work with a doctor who specializes in diabetes and a dietitian who can help you plan your meals. At the end of the day, you may spend a lot of time buying healthy foods, planning meals, and cooking. Because of the work that goes into meal planning , getting support and guidance can be helpful. Some general recommendations for healthy eating with diabetes include:. Managing diabetes and making lifestyle changes can come with a learning curve. Working with diabetes educators can help you make better choices that may help you better manage T2D. If you would like more information, please contact us. Give Hope. Fund Answers. End Kidney Disease. Skip to main content. You are here Home » A to Z » Diabetes: Ten Tips for Self-Management. Diabetes: Ten Tips for Self-Management. English Español. Make healthy food choices. You can choose what, when, and how much to eat. Healthy meal planning is an important part of your diabetes treatment plan. Decide to be physically active. This helps you keep your cholesterol, blood pressure, and blood sugar under control. Take your medications. You can all take your medications as instructed by your healthcare team, and keep track of your blood sugar levels on your own. Keep a log book. Know what makes your blood sugar level rise and fall — and how to control these day-to-day factors. When you have diabetes, it's important to keep your blood sugar levels within the range recommended by your healthcare professional. But many things can make your blood sugar levels change, sometimes quickly. Find out some of the factors that can affect blood sugar. Then learn what you can do to manage them. Healthy eating is important for everyone. But when you have diabetes, you need to know how foods affect your blood sugar levels. It's not only the type of food you eat. It's also how much you eat and the types of food you combine in meals and snacks. Learn about planning balanced meals. A healthy-eating plan includes knowing what to eat and how much to eat. Two common ways to plan meals are carbohydrate counting and the plate method. Ask your healthcare professional or a registered dietitian if either type of meal planning is right for you. Understand carbohydrate counting. Counting carbs involves keeping track of how many grams of carbohydrates you eat and drink during the day. If you take diabetes medicine called insulin at mealtimes, it's important to know the amount of carbohydrates in foods and drinks. That way, you can take the right dose of insulin. Among all foods, carbs often have the biggest impact on blood sugar levels. That's because the body breaks them down into sugar, which raises blood sugar levels. Some carbs are better for you than others. For example, fruits, vegetables and whole grains are full of nutrients. They have fiber that helps keep blood sugar levels more stable too. Eat fewer refined, highly processed carbs. These include white bread, white rice, sugary cereal, cakes, cookies, candy and chips. Get to know the plate method. This type of meal planning is simpler than counting carbs. The plate method helps you eat a healthy balance of foods and control portion sizes. Use a 9-inch plate. Fill half of the plate with nonstarchy vegetables. Examples include lettuce, cucumbers, broccoli, tomatoes and green beans. Divide the other half of the plate into two smaller, equal sections. You might hear these smaller sections called quarters. In one quarter of the plate, place a lean protein. Examples include fish, beans, eggs, and lean meat and poultry. On the other quarter, place healthy carbohydrates such as fruits and whole grains. Be mindful of portion sizes. Learn what portion size is right for each type of food. Everyday objects can help you remember. For example, one serving of meat or poultry is about the size of a deck of cards. A serving of cheese is about the size of six grapes. And a serving of cooked pasta or rice is about the size of a fist. You also can use measuring cups or a scale to help make sure you get the right portion sizes. Balance your meals and medicines. If you take diabetes medicine, it's important to balance what you eat and drink with your medicine. Too little food in proportion to your diabetes medicine — especially insulin — can lead to dangerously low blood sugar. This is called hypoglycemia. Too much food may cause your blood sugar level to climb too high. This is called hyperglycemia. Talk to your diabetes health care team about how to best coordinate meal and medicine schedules. Limit sugary drinks. Sugar-sweetened drinks tend to be high in calories and low in nutrition. They also cause blood sugar to rise quickly. So it's best to limit these types of drinks if you have diabetes. The exception is if you have a low blood sugar level. Sugary drinks can be used to quickly raise blood sugar that is too low. These drinks include regular soda, juice and sports drinks. Exercise is another important part of managing diabetes. When you move and get active, your muscles use blood sugar for energy. Regular physical activity also helps your body use insulin better. These factors work together to lower your blood sugar level. The more strenuous your workout, the longer the effect lasts. But even light activities can improve your blood sugar level. Light activities include housework, gardening and walking. Talk to your healthcare professional about an exercise plan. Ask your healthcare professional what type of exercise is right for you. In general, most adults should get at least minutes a week of moderate aerobic activity. That includes activities that get the heart pumping, such as walking, biking and swimming. Aim for about 30 minutes of moderate aerobic activity a day on most days of the week. Most adults also should aim to do strength-building exercise 2 to 3 times a week. If you haven't been active for a long time, your healthcare professional may want to check your overall health first. Then the right balance of aerobic and muscle-strengthening exercise can be recommended. Keep an exercise schedule. Ask your healthcare professional about the best time of day for you to exercise. That way, your workout routine is aligned with your meal and medicine schedules. Know your numbers. Talk with your healthcare professional about what blood sugar levels are right for you before you start exercise. Check your blood sugar level. Also talk with your healthcare professional about your blood sugar testing needs. If you don't take insulin or other diabetes medicines, you likely won't need to check your blood sugar before or during exercise. But if you take insulin or other diabetes medicines, testing is important. Check your blood sugar before, during and after exercise. Many diabetes medicines lower blood sugar. So does exercise, and its effects can last up to a day later. The risk of low blood sugar is greater if the activity is new to you. The risk also is greater if you start to exercise at a more intense level. Be aware of symptoms of low blood sugar. These include feeling shaky, weak, tired, hungry, lightheaded, irritable, anxious or confused. See if you need a snack. Have a small snack before you exercise if you use insulin and your blood sugar level is low. The snack you have before exercise should contain about 15 to 30 grams of carbs. Or you could take 10 to 20 grams of glucose products. This helps prevent a low blood sugar level. Stay hydrated. Drink plenty of water or other fluids while exercising. Dehydration can affect blood sugar levels. Be prepared. Always have a small snack, glucose tablets or glucose gel with you during exercise. You'll need a quick way to boost your blood sugar if it drops too low. Carry medical identification too. In case of an emergency, medical identification can show others that you have diabetes. It also can show whether you take diabetes medicine such as insulin. Medical IDs come in forms such as cards, bracelets and necklaces. Adjust your diabetes treatment plan as needed. If you take insulin, you may need to lower your insulin dose before you exercise. You also may need to watch your blood sugar level closely for several hours after intense activity. That's because low blood sugar can happen later on. Your healthcare professional can advise you how to correctly make changes to your medicine. You also may need to adjust your treatment if you've increased how often or how hard you exercise. Insulin and other diabetes medicines are designed to lower blood sugar levels when diet and exercise alone don't help enough. How well these medicines work depends on the timing and size of the dose. Medicines you take for conditions other than diabetes also can affect your blood sugar levels. Store insulin properly. Insulin that is not stored properly or is past its expiration date may not work. |
| Who's at risk of developing type 2 diabetes? | Proper syringe disposal helps prevent accidental needlestick injuries, protects others from potential harm, and ensures the safe management of medical waste. Teaching patients appropriate disposal methods promotes community safety and adherence to waste management regulations. Provide guidance on local regulations and resources for disposing of used syringes, including contacting the refuse company or waste authority for guidance. Proper disposal of used syringes is essential to prevent environmental contamination and comply with local waste management regulations. Informing patients about available resources helps them navigate safe disposal practices effectively. Educate patients on safe syringe transport during travel, advising them to pack used syringes in a secure container to prevent accidental needlesticks. Traveling with used syringes requires careful handling to avoid injuries and maintain personal and public safety. Providing instructions on proper syringe transport reduces the risk of accidental needlesticks during travel. Insulin pump therapy is suitable for patients who desire continuous subcutaneous insulin infusion and are willing to actively participate in self-management. Provide extensive education on insulin pump use and self-management of blood glucose and insulin doses. Insulin pump therapy requires thorough education to ensure proper understanding and safe use of the device. Educating the patient about insulin pump operation, insertion site care, troubleshooting techniques, blood glucose monitoring, and calculating insulin doses based on carbohydrate counting promotes effective self-management. Teach the patient about potential risks and complications associated with insulin pump therapy. Patients need to be aware of potential risks and complications, such as occlusions in the infusion set or tubing, interruptions in insulin flow, and the increased risk of ketoacidosis. Educating patients about recognizing signs of occlusions, administering manual injections when needed, and seeking prompt medical attention for any concerns helps minimize risks and promote patient safety. Instruct the patient on proper care, maintenance, and replacement of the insulin pump. Proper care and maintenance of the insulin pump, including regular changing of infusion sets, is essential for optimal function and prevention of complications. Teaching the patient about proper hygiene, safe storage, battery replacement, and when to seek technical support helps ensure uninterrupted insulin delivery and device performance. This monitoring allows for adjustments in insulin dosages and troubleshooting of any issues to maintain optimal glucose control. Provide support and addressing concerns related to wearing the pump. Some patients may find wearing the insulin pump for 24 hours a day inconvenient or may have concerns about its visibility. Offering support, addressing concerns, and discussing options for temporary disconnection e. Insulin pens are suitable for patients who need to inject one type of insulin at a time or can use premixed insulins. Instruct the patient on proper insulin pen technique and safety measures. Proper technique in using insulin pens ensures accurate dosage delivery and minimizes the risk of complications. Education on how to load the insulin cartridge, dial the appropriate dose, attach the disposable needle, and perform the injection helps the patient use the device effectively and safely. Teach the patient about storage and maintenance of insulin pens. Insulin pens should be stored properly to maintain the integrity of the insulin and the device. Educating the patient on storage conditions, such as avoiding extreme temperatures, and the need for regular cleaning and replacement of needles promotes optimal performance of the insulin pen. This monitoring allows for adjustments in insulin dosages as needed to maintain optimal glucose control. Jet injectors are an alternative to needle injections for delivering insulin. Provide thorough training and supervision for the patient when initiating jet injector use. Proper training is crucial when using jet injectors to ensure accurate and safe insulin delivery. Providing comprehensive education on how to operate the device, maintain hygiene, and troubleshoot any issues helps the patient use the jet injector effectively and minimizes the risk of complications. Educate the patient about the differences in insulin absorption rates, peak activity, and insulin levels with a jet injector. Jet injectors may result in differences in insulin absorption rates compared to traditional needle injections. Educating the patient about these variations helps them understand the potential differences in insulin action and adjust their self-management strategies accordingly. Advise the patient about the possibility of bruising associated with jet injector use. Some patients may experience bruising at the injection site when using jet injectors. Informing the patient about this potential side effect helps manage their expectations and promotes early identification of any complications or adverse reactions. Insulin administration can sometimes lead to local and systemic allergic reactions, with local reactions causing redness, swelling, tenderness, and wheals at the injection site. Systemic reactions are rare but can result in generalized urticaria or even anaphylaxis. Assess and monitor for local allergic reactions at the injection site. Local allergic reactions, such as redness, swelling, tenderness, or wheal formation, can occur after insulin injections. Regular assessment of injection sites helps identify and monitor any allergic reactions. If reactions persist, an alternative type of insulin can be prescribed. Educate the patient about systemic allergic reactions to insulin and the appropriate response. Although rare, systemic allergic reactions can occur, presenting as generalized urticaria hives or even anaphylaxis. Patients should be aware of these potential reactions and know to seek immediate medical attention if they experience any symptoms. Desensitization with gradually increasing insulin doses may be necessary for treatment. Educate the patient about insulin lipodystrophy and the importance of rotation of injection sites. Lipodystrophy refers to localized reactions at injection sites, including lipoatrophy loss of subcutaneous fat or lipohypertrophy fibrofatty masses. Using human insulin has greatly reduced the occurrence of lipodystrophy. Patients should be educated about the importance of rotating injection sites to prevent the development of lipohypertrophy and delayed insulin absorption. Monitor for insulin resistance and collaborating with the healthcare team to adjust insulin doses. Insulin resistance may occur in some patients with diabetes, requiring higher insulin doses for adequate glycemic control. Regular monitoring of blood glucose levels and close collaboration with the healthcare team allow for adjustments in insulin doses to address insulin resistance and control diabetes symptoms effectively. Provide education on the causes of morning hyperglycemia and strategies to address it. Morning hyperglycemia can result from the dawn phenomenon , insulin waning, or the Somogyi effect. Educating the patient about these causes helps them understand the importance of blood glucose monitoring during the night to determine the underlying cause. Adjustments in insulin doses and timing can be made accordingly to prevent morning hyperglycemia. Teach the patient about proper timing of insulin administration to address insulin waning. Insulin waning refers to a progressive increase in blood glucose levels from bedtime to morning. Instructing the patient to administer the evening NPH insulin dose at bedtime rather than before dinner helps prevent insulin waning and ensures better glycemic control upon waking. Oral antidiabetic agents are prescribed for patients with type 2 diabetes who do not respond effectively to medical nutrition therapy MNT and exercise alone. Understanding the different classes of oral antidiabetic agents and how they work can empower the patient to actively participate in their treatment plan and recognize the importance of medication adherence. Oral antidiabetic agents are used for patients with type 2 diabetes who cannot effectively manage their condition through diet and exercise alone. Oral antidiabetic agents may include:. Second-Generation Sulfonylureas [glipizide Glucotrol , glimepiride Amaryl , glyburide Diabeta ] Sulfonylureas stimulate insulin release from the beta cells in the pancreas. They improve binding insulin to receptors and may increase number of insulin receptors. They are indicated as adjunct to diet and exercise MNT. They are more potent than first-generation sulfonylureas and can be used in combination with metformin or insulin to improve glucose control. Biguanides [metformin Glucophage ] Biguanides decreased the product and increases the uptake of glucose in the liver. It is effective in lowering blood glucose and does not cause hypoglycemia as the sulfonylureas do. It has been associated with development of lactic acidosis and GI distress and long term use may cause vitamin B12 deficiency. Alpha-Glucosidase Inhibitors [acarbose Precose , miglitol Glyset ] inhibit alpha-glucosidase, an enzyme that breaks down glucose for absorption. Therefore, they delay the absorption of glucose. They have only a mild effect on glucose levels and do not enhance insulin secretion. They are associated with severe hepatic toxicity and GI distress. Non-Sulfonylurea Insulin Secretagogues [repaglinide Prandin , nateglinide Starlix ] Stimulates the pancreas to secrete insulin. It can be used alone or in combination with metformin to improve control of glucose. Thiazolidinediones or Glitazones [pioglitazone Actos , rosiglitazone Avandia ] Decreases insulin resistance by sensitizing the body to insulin and by stimulating insulin receptor sites to lower blood glucose and improve action of insulin. Dipeptidyl Peptidase-4 DPP-4 Inhibitors [sitagliptin Januvia , saxagliptin Onglyza , linagliptin Tradjenta ] Slows the breakdown of GLP-1 to prolong the effects of increased insulin secretion, decreased glucagon secretion, and slowed GI emptying ultimately producing improved glucose control. Glucagon-like Peptide-1 Agonist GLP-1 [liraglutide Victoza , dulaglutide Trulicity ] Enhances glucose-dependent insulin secretion and exhibit other antihyperglycemic actions following their release into the circulation from the gastrointestinal tract. They may also lead to weight loss but can have side effects such as pancreatitis, diarrhea , nausea, and vomiting. Not suitable for patients with type 1 diabetes. Sodium-Glucose Co-Transporter 2 SGL-2 Inhibitors [dapagliflozin Forxiga , canagliflozin Invokana ] Increases urinary glucose excretion and lowers the renal threshold for glucose. It is also prescribed to reduce the risk of major cardiovascular events in patients with established cardiovascular disease and type 2 DM. This drug improves glycemic control by decreasing glucose concentration in the blood through increased urinary excretion and reduced renal absorption of glucose. Educate the patient about the complementary nature of oral antidiabetic agents with other treatment modalities, such as medical nutrition therapy MNT and exercise. Reinforcing the importance of a comprehensive approach to diabetes management encourages the patient to adhere to a balanced diet and engage in regular physical activity, which can enhance the effectiveness of oral antidiabetic agents. Hyperglycemia resulting from these conditions may require temporary discontinuation of oral antidiabetic agents and initiation of insulin therapy. Regular monitoring helps detect any fluctuations in blood glucose levels and informs appropriate medication adjustments. Provide education on insulin therapy and its potential use in combination with oral agents, particularly for newly diagnosed patients with type 2 diabetes who have symptomatic hyperglycemia and high blood glucose and A1C levels. Some patients may require insulin therapy as an adjunct to oral antidiabetic agents to achieve glycemic targets. Educating the patient about insulin therapy helps alleviate any fears or misconceptions they may have and promotes acceptance and adherence to the prescribed treatment regimen. Emphasize the importance of regular follow-up visits and laboratory tests to evaluate the effectiveness of oral antidiabetic agents and make necessary adjustments. Regular follow-up visits and laboratory tests enable healthcare providers to modify the treatment plan as needed. Encourage the patient to report any adverse effects or changes in symptoms related to oral antidiabetic agents promptly. Early identification and management of adverse effects or changes in symptoms associated with oral antidiabetic agents are essential to prevent complications and optimize treatment outcomes. Open communication encourages patients to seek timely medical assistance when needed. Proper nutrition and meal planning are essential for diabetes management. Educating patients about healthy food choices, portion control, and balanced meals can help them achieve and maintain optimal blood glucose levels, lipid profiles, and blood pressure. Calculations based on age, gender, height, and weight help determine the baseline caloric intake required for weight maintenance and overall health. This individualized approach supports accurate calorie control and ensures nutritional adequacy. Factoring in physical activity provides a more accurate estimation of energy needs and supports the patient in achieving their weight goals. Subtract to calories from the daily total to promote a safe and gradual weight loss. To promote a 1- to 2-pound weight loss per week, a calorie deficit of to calories is recommended. This approach supports gradual weight loss, which is associated with better long-term success and reduces the risk of adverse effects. Simplify meal planning information and provide opportunities for practice and repetition. Some aspects of meal planning, such as using food exchange systems, may be challenging for patients due to intellectual limitations or emotional barriers. Simplifying information and providing opportunities for practice and repetition can enhance patient understanding and proficiency in meal planning techniques. This approach helps patients develop confidence and competence in managing their dietary choices and fosters long-term adherence. Balancing the distribution of macronutrients is crucial for maintaining optimal nutrition and supporting blood glucose control. Educate the patient about the recommended percentages of calories from carbohydrates, proteins, and fats. Providing education on the recommended caloric distribution helps patients understand the importance of balancing macronutrients in their diet. By educating patients about the recommended percentages of calories from carbohydrates, proteins, and fats, nurses empower patients to make informed dietary choices that support blood glucose control, lipid management, and overall health. Highlight the importance of increased fiber intake for improved blood glucose levels and other health benefits. Increased fiber intake plays a significant role in improving blood glucose levels, lowering cholesterol, and promoting satiety. Educating patients about the benefits of fiber-rich foods, such as legumes, whole grains, fruits, and vegetables, encourages their inclusion in the meal plan and supports overall dietary and health goals. Gradually increase fiber intake in consultation with a dietitian to prevent adverse effects. Sudden increases in fiber intake can lead to gastrointestinal discomfort and require adjustments in dosage of insulin or antidiabetic agents to prevent hypoglycemia. Gradually increasing fiber intake in consultation with a dietitian allows for proper monitoring and adjustment of the meal plan to mitigate potential adverse effects. Educate patients about the use of exchange lists for meal planning. Exchange lists are a commonly used tool in nutritional management for individuals with diabetes. Educating patients about the concept of exchange lists helps them understand how foods can be organized into groups with similar characteristics, such as calorie content and macronutrient composition. This knowledge enables patients to create a well-balanced meal plan that maintains consistency in nutrient intake while providing variety in food choices. You can learn more about the Food Exchange List here. Teach patients how to read nutrition labels and understand carbohydrate content. Reading food labels is an essential skill for patients with diabetes when shopping for food. Understanding the carbohydrate content of foods listed on nutrition labels allows patients to make informed choices and accurately determine the amount of medication needed, particularly for those who require premeal insulin. Explain the concept of carbohydrate counting and its flexibility in food choices. Carbohydrate counting is a popular nutritional tool used for blood glucose management in both type 1 and type 2 diabetes. Educating patients about carbohydrate counting helps them understand that carbohydrates have the most significant impact on blood glucose levels. This approach provides flexibility in food choices while maintaining blood glucose control. By incorporating carbohydrate counting into their meal planning, patients can achieve more accurate insulin management and maintain a balanced diet. Educate patients about healthy food choices, portion control, and serving sizes. Encouraging patients to make healthy food choices and practice portion control is important for achieving and maintaining blood glucose control and weight management. Teaching patients to measure servings or choices, such as using standard portion sizes or the MyPlate Food Guide, helps them understand appropriate portion sizes for different food groups. This approach can promote balanced nutrition, supports portion control, and simplifies meal planning for patients who may find more complicated systems challenging. Discuss the concept of the glycemic index and its potential impact on blood glucose levels. The glycemic index measures how much a particular food increases blood glucose levels compared to an equivalent amount of glucose. Educating patients about the glycemic index helps them understand how different foods affect their blood glucose levels. Encourage patients to monitor their blood glucose levels after consuming specific foods to create their own glycemic index. Monitoring blood glucose levels after eating specific foods allows patients to assess the individual impact of those foods on their blood glucose control. This personalized approach empowers patients to make dietary adjustments based on their own glycemic response. By using this information, patients can modify their meal plans and insulin doses accordingly, leading to improved blood glucose control and individualized diabetes management. Emphasize consistent meal timing and portion control. Consistency in meal timing and portion control helps regulate blood glucose levels. Patients should be educated on the importance of regular meals and the distribution of caloric intake throughout the day. Avoiding skipped meals prevents glucose fluctuations and excessive demands on the pancreas. Support patients in implementing lifestyle changes. Lifestyle changes, including dietary modifications and increased physical activity, are integral to diabetes management. Nurses play a vital role in providing support, motivation, and education to help patients adopt and sustain these changes. Encourage weight loss and maintenance. Weight management is particularly important for obese patients with diabetes. Losing weight can improve blood glucose control and reduce the need for medication. There is also substantial evidence indicating that managing obesity can significantly delay the progression from prediabetes to type 2 diabetes and provides significant benefits in the treatment of type 2 diabetes. Nurses should emphasize the significance of weight loss, provide guidance on healthy weight loss strategies, and offer ongoing support. Address emotional issues and provide psychological support related to dietary changes. Some patients may struggle with emotional issues, such as accepting the diagnosis of diabetes or experiencing feelings of deprivation and restriction in eating. Providing psychological support and addressing these concerns helps patients navigate the emotional aspects of meal planning. Provide behavioral therapy and ongoing nutrition counseling. Consistently following a meal plan and maintaining weight loss can be challenging. Behavioral therapy, group support, and ongoing nutrition counseling can help patients incorporate new dietary habits into their lifestyles and sustain positive changes. Collaborate with a registered dietitian. Registered dietitians specialize in medical nutrition therapy MNT for diabetes management. Reinforce the role of the nurse in communicating relevant information to the dietitian and promoting patient understanding. Effective communication between the nurse and the dietitian facilitates a coordinated and individualized approach to meal planning. Educate patients about the importance of consistent eating habits and the relationship between food and insulin. Consistency in the amount of calories and carbohydrates ingested at each meal is crucial for patients requiring insulin to control blood glucose levels. Educating patients about this relationship helps them understand the impact of food on insulin requirements and blood glucose control. It empowers patients to make informed choices about their meal timings and contents, fostering better glucose management. Emphasize the importance of moderation in alcohol consumption. Educate patients about the potential adverse effects of alcohol specific to diabetes. Moderation is crucial when it comes to alcohol consumption for patients with diabetes. Educating patients about the recommended limits for alcohol intake helps them understand the need to consume alcoholic beverages in controlled quantities. By promoting moderation, nurses assist patients in minimizing the potential negative impact of alcohol on their diabetes management. Caution patients about the risk of hypoglycemia associated with alcohol consumption. Alcohol consumption can increase the risk of hypoglycemia, particularly for patients taking insulin or insulin secretagogues. Educating patients about the potential effects of alcohol on blood glucose levels helps them understand the importance of consuming food along with alcohol to prevent hypoglycemia. By providing this information, nurses empower patients to make informed decisions about alcohol consumption and take appropriate measures to prevent hypoglycemia. Encourage patients to incorporate food intake along with alcohol consumption. Consuming food along with alcohol can help reduce the risk of hypoglycemia. By advising patients to have a meal or snack when consuming alcohol, nurses help ensure that patients maintain stable blood glucose levels. However, it is important to note that carbohydrates consumed with alcohol may raise blood glucose levels. Providing this guidance helps patients strike a balance and make informed choices regarding food intake when consuming alcohol. Discuss the potential impact of alcohol on weight, hyperlipidemia , and glucose levels. Alcohol consumption can contribute to weight gain, hyperlipidemia, and elevated glucose levels. Educating patients about the potential effects of alcohol on these aspects of their health helps them understand the importance of moderation and incorporating alcohol calories into their overall meal plan. Educate patients about lower-calorie or less-sweet drink options. Recommending lower-calorie or less-sweet drink options, such as light beer or dry wine, helps patients make choices that align with their diabetes management goals. Educate patients about artificial sweeteners, including their types and use and emphasize moderation in sweetener use to avoid potential adverse effects. Encouraging patients to use sweeteners in moderation helps prevent potential negative consequences. By promoting mindful consumption, patients can avoid excessive intake and maintain a balanced diet. Explaining the distinction between nutritive e. Address potential side effects of certain sweeteners, such as sorbitol. Informing patients about potential side effects, such as the laxative effect of sorbitol-containing sweeteners, enables them to make decisions regarding the use of these products. Patients can monitor their individual tolerance and adjust their intake accordingly. By clarifying that these foods should not be consumed in unlimited quantities, patients can manage their blood glucose levels more effectively and prevent potential spikes. Regular exercise is essential in diabetes management as it helps lower blood glucose levels, improve insulin utilization, and reduce cardiovascular risk factors. Regular exercise is highly beneficial for individuals with diabetes. By encouraging patients to engage in regular exercise, nurses promote the importance of physical activity in managing blood glucose levels, reducing cardiovascular risk factors. Provide guidelines for exercise frequency and duration. Guidelines for exercise frequency and duration help patients establish a structured exercise routine. By specifying three times per week with no more than two consecutive days without exercise, patients can maintain consistency in their exercise regimen, which contributes to better blood glucose control and overall fitness. The American Diabetes Association recommends the following guidelines for physical activity:. Educate adults with type 2 diabetes about the significance of reducing sedentary behavior and interrupting prolonged sitting every 30 minutes for blood glucose benefits. It is recommended for all adults, especially those with type 2 diabetes, to reduce sedentary behavior and interrupt prolonged sitting every 30 minutes for blood glucose benefits. Older adults with diabetes should incorporate flexibility and balance training times per week, with options such as yoga and tai chi. Individuals with type 1 diabetes and type 2 diabetes should evaluate their baseline physical activity and sedentary time, aiming to increase non sedentary activities above their baseline. Discuss the benefits of exercise and weight loss for individuals with type 2 diabetes. For individuals with type 2 diabetes who are overweight or obese, engaging in exercise alongside dietary management offers multiple benefits, including improved glucose metabolism and enhanced body fat loss. Exercise coupled with weight loss improves insulin sensitivity and may decrease the need for insulin or oral antidiabetic agents. Educating patients on the potential positive outcomes of exercise and weight loss encourages them to incorporate physical activity as part of their diabetes management plan. Emphasize the importance of a gradual increase in exercise duration. A slow and gradual increase in the duration of exercise sessions is recommended to prevent excessive strain or injury. Allowing the patient to gradually build endurance and fitness levels over time, the nurse can promote safe and sustainable exercise habits. Recommend walking as a safe and accessible form of exercise. Walking is a low-impact and easily accessible form of exercise that can be performed by most individuals with diabetes. It requires no special equipment other than proper shoes and can be incorporated into daily routines. By recommending walking, nurses provide patients with a practical and feasible exercise option that can be sustained long-term. Encourage patients to discuss an exercise program with their primary healthcare provider and undergo a medical evaluation. Before initiating an exercise program, it is important for patients to consult with their primary healthcare provider and undergo a medical evaluation. Assess blood glucose and ketone levels before initiating exercise. Monitoring blood glucose and ketone levels before exercise is crucial for patients with diabetes. Exercising with elevated blood glucose levels can further increase blood glucose levels, potentially leading to hyperglycemia and other complications. Educate patients on pre-exercise carbohydrate snacks for insulin-treated individuals. Patients who require insulin should be taught to consume a g carbohydrate snack or a snack of complex carbohydrates with protein before engaging in moderate exercise. This pre-exercise snack helps prevent unexpected hypoglycemia by providing the necessary fuel for physical activity and counteracting the potential decrease in circulating insulin during exercise. Provide instructions on managing post-exercise hypoglycemia for patients taking insulin. Hypoglycemia can occur hours after exercise in patients taking insulin. To prevent post-exercise hypoglycemia, patients may need to consume a snack at the end of the exercise session and at bedtime, as well as monitor their blood glucose levels more frequently. Patients who are capable, knowledgeable, and responsible can learn to adjust their insulin doses in collaboration with a diabetes educator. Others require specific instructions on managing their blood glucose levels during and after exercise. Educate patients on regular blood glucose monitoring during extended periods of exercise. Patients taking insulin and engaging in extended periods of exercise should monitor their blood glucose levels before, during, and after the exercise period. This monitoring helps them adjust their carbohydrate intake to maintain blood glucose levels within the target range. It is important for others involved in exercise activities to be aware that the person exercising has diabetes. By informing exercise participants and observers, they can provide appropriate assistance in case of severe hypoglycemia. This promotes a safe exercise environment and ensures that prompt action can be taken if a diabetes-related emergency occurs. Provide education on exercise considerations for patients with diabetic complications. Patients with diabetic complications, such as retinopathy, autonomic neuropathy, sensorimotor neuropathy, and cardiovascular disease, may require modifications in their exercise regimen. Educate patient with diabetes on the importance of proper footwear and protective equipment. Wearing appropriate footwear and protective equipment reduces the risk of injuries during exercise. This is particularly important for individuals with diabetes, as they may have reduced sensation in their lower extremities due to peripheral neuropathy. By emphasizing the use of proper footwear and protective equipment, nurses help prevent foot injuries and promote safety during exercise. Advise patients to meticulously inspect their feet daily after exercise. Patients with diabetes are at a higher risk of foot complications. By instructing patients to inspect their feet daily after exercise, nurses promote early detection of any foot abnormalities, such as blisters or wounds. Timely identification and appropriate management of foot issues can prevent the development of serious complications, such as foot ulcers. Provide recommendations for avoiding exercise in extreme weather conditions and periods of poor metabolic control. Extreme heat or cold can pose risks to individuals with diabetes during exercise. Additionally, exercising during periods of poor metabolic control may lead to unstable blood glucose levels. By advising patients to avoid exercise in extreme weather conditions and during periods of poor metabolic control, nurses promote patient safety and help maintain stable blood glucose levels. Assess the physical capacity and functional limitations of older adults with diabetes before initiating an exercise program. Older adults may have specific physical limitations, chronic conditions, or age-related changes that need to be considered when planning an exercise program. Assessing their physical capacity and functional abilities helps determine appropriate exercises and adaptations to ensure safety and optimize the benefits of physical activity. Develop an individualized exercise plan that includes low-impact activities, balance exercises, and flexibility training. Older adults may have reduced joint mobility , balance issues, and age-related musculoskeletal changes that require modifications in exercise programming. Including low-impact activities e. Emphasize the importance of gradual progression and frequent rest breaks during exercise sessions. Older adults may need more time to adapt and recover from exercise due to decreased stamina and reduced exercise tolerance. Encouraging gradual progression, such as increasing exercise duration or intensity in small increments, and incorporating frequent rest breaks during exercise sessions helps prevent overexertion, fatigue, and injury. This approach supports older adults in safely building endurance and strength while minimizing the risk of adverse events. Provide education on the use of assistive devices and safe exercise techniques. Older adults may benefit from the use of assistive devices e. Teaching proper use of assistive devices and demonstrating safe exercise techniques help minimize the risk of falls, strains, and other injuries. Incorporate social support and group activities for motivation and enjoyment. Older adults often thrive in supportive and socially engaging environments. Encouraging participation in group exercise classes, walking groups, or community-based programs fosters social interaction, motivation, and enjoyment. The positive social aspect of exercise can enhance adherence and long-term commitment to regular physical activity among older adults with diabetes. Hyperglycemia is a common occurrence in hospitalized patients, particularly those admitted for the illness that led to hospitalization. Several factors contribute to hyperglycemia, including changes in treatment regimen, medications such as corticosteroids, inadequate insulin therapy with IV dextrose, inappropriate insulin management, and mismatched timing of meals and insulin. Nursing interventions play a crucial role in correcting these factors to prevent hyperglycemia. Monitor blood glucose levels regularly. Blood glucose monitoring is a vital sign and provides essential information for assessing glycemic control. It helps identify hyperglycemia and informs the need for additional insulin doses. Obtain orders for extra doses of insulin when blood glucose levels are elevated. Blood glucose monitoring results inform nurses of the need for additional doses of insulin. Administering additional doses of insulin at appropriate times helps manage hyperglycemia and promote glycemic control. Do not withhold insulin when blood glucose levels are within the normal range. Withholding insulin when blood glucose levels are normal can lead to hyperglycemia. It is important to administer insulin consistently to maintain glycemic control. Test blood glucose levels before meals and administer insulin at that time. Administering insulin before meals, based on premeal blood glucose levels, helps prevent postprandial hyperglycemia and promotes a physiologic response to glucose intake. Administer short-acting insulin to avoid postprandial hyperglycemia. Short-acting insulin is necessary to control blood glucose levels after meals, even in patients with normal pre-meal glucose levels. Administering it at the appropriate time ensures effective glycemic control. Be cautious with the use of corticosteroids e. Corticosteroids can induce hyperglycemia, so close monitoring of blood glucose levels is essential. Adjustments to insulin therapy may be necessary to maintain glycemic control. Use normal saline NS as the preferred solution for IV antibiotics , if possible, to minimize dextrose infusion. Excessive infusion of dextrose through IV fluids can contribute to hyperglycemia. Using NS as the diluent for IV antibiotics helps avoid this potential cause of elevated blood glucose levels. Avoid overly aggressive treatment of hypoglycemia. Aggressive treatment of hypoglycemia can lead to rebound hyperglycemia. Managing hypoglycemia with appropriate measures prevents subsequent hyperglycemia. Hypoglycemia in hospitalized patients is often attributed to excessive insulin administration or delays in eating. Follow the established hospital protocol for treating hypoglycemia. Assess the pattern of glucose values and avoid repeated doses of insulin leading to hypoglycemia. Adjustments in insulin therapy may be necessary to prevent recurrent hypoglycemia. Administer repeat treatments for hypoglycemia if the initial treatment does not sufficiently increase glucose levels, following the specified time interval e. Repeat treatments allow for further correction of hypoglycemia if the initial intervention was insufficient. Limit successive doses of subcutaneous regular insulin to no more than every 3 to 4 hours. Administering multiple doses of regular insulin in quick succession increases the risk of hypoglycemia. Adhering to appropriate dosing intervals helps maintain glycemic stability. Exercise caution when administering supplemental doses of regular insulin in patients receiving intermediate insulin before breakfast and dinner. Careful consideration is needed when providing additional regular insulin doses in patients who are already receiving intermediate-acting insulin. Timing and dosage adjustments should be made to prevent overlapping peaks and subsequent hypoglycemia. Arrange for snacks to be given if meals are delayed due to procedures, physical therapy, or other activities. Delayed food intake can contribute to hypoglycemia. Providing snacks as needed helps maintain glucose levels and prevent hypoglycemic reactions in patients whose meals are delayed. Monitor the patient for signs and symptoms of hypoglycemia, such as sweating, tremor, tachycardia, confusion , and changes in behavior. Regular monitoring allows the nurse to detect early signs of hypoglycemia and intervene promptly to prevent complications. Immediate administration of carbohydrates helps restore blood glucose levels and alleviate hypoglycemic symptoms. Prepare and administer glucagon, as prescribed, in emergency situations when the patient is unconscious or unable to swallow. Glucagon stimulates the liver to release stored glucose, rapidly increasing blood glucose levels. Administration of glucagon can be life-saving in severe hypoglycemia. Provide emotional support and reassurance to the patient during episodes of hypoglycemia, addressing any fears or concerns they may have. Emotional support helps alleviate anxiety and encourages the patient to actively participate in their diabetes management. Educate the patient and their family or caregivers on recognizing and managing hypoglycemic episodes, including the use of fast-acting carbohydrates and glucagon. Patient and caregiver education promotes awareness and empowers them to respond effectively to hypoglycemia, ensuring timely treatment. Educate the patient on the signs and symptoms of hypoglycemia and the importance of early recognition and prompt treatment. Early recognition of hypoglycemia allows for timely intervention and prevents the condition from worsening. Prompt treatment helps restore blood glucose levels to a safe range, preventing complications and promoting patient well-being. Instruct the patient on the appropriate management of hypoglycemia with fast-acting sources of carbohydrate, such as fruit juice or glucose tablets. Fast-acting carbohydrates quickly raise blood glucose levels, providing immediate relief from hypoglycemic symptoms. Patients need to be aware of the recommended sources of carbohydrates and the appropriate quantities to consume for effective management. Teach patients and their families or caregivers about the use of glucagon in emergency situations when the patient is unconscious or unable to swallow. Glucagon is a life-saving hormone that stimulates the liver to release stored glucose, raising blood glucose levels rapidly. It is crucial for family members and caregivers to understand how to administer glucagon in emergency situations to ensure timely treatment. Emphasize the importance of regular blood glucose monitoring, especially before driving or engaging in potentially dangerous activities. Regular blood glucose monitoring helps patients with diabetes assess their glycemic status and anticipate changes in insulin requirements. It enables them to take appropriate actions to prevent hypoglycemia and maintain safe blood glucose levels. Provide education on lifestyle factors that can contribute to hypoglycemia, such as meal timing, physical activity, and medication adherence. Proper meal planning, adherence to medication schedules, and awareness of the impact of physical activity help patients prevent hypoglycemia. Education empowers patients to make informed decisions and take proactive steps to manage their condition effectively. Encourage patients to carry a source of simple sugar e. Carrying a source of fast-acting carbohydrates ensures that patients can quickly treat hypoglycemia, even in situations where other food options may not be readily available. It promotes patient autonomy and preparedness for managing hypoglycemic episodes. Monitor the patient for signs and symptoms of DKA, including hyperglycemia, dehydration , electrolyte imbalances, and acidosis. Regular monitoring allows for early detection of DKA and prompt intervention to prevent complications. Administer intravenous fluids , such as normal saline NS or half-strength NS, as indicated and at the prescribed rate, to rehydrate the patient and restore tissue perfusion. Rehydration is crucial in managing DKA to maintain fluid balance , improve tissue perfusion, and facilitate the excretion of excess glucose and ketones. Monitoring vital signs helps identify signs of dehydration or fluid overload and guides appropriate fluid management. Monitor electrolyte levels, particularly potassium , and replace electrolytes as indicated to maintain balance and prevent dysrhythmias. DKA can cause electrolyte imbalances, including hyperkalemia or hypokalemia, which require careful monitoring and timely replacement to prevent complications. Cautious administration of potassium supplements helps prevent rapid potassium fluctuations and the risk of hyperkalemia. It ensures a gradual and controlled increase in serum potassium levels. Administer insulin therapy as prescribed, usually through continuous intravenous infusion, to reverse acidosis and promote glucose utilization. Insulin administration inhibits fat breakdown, stops ketone production, and helps correct acidosis in DKA. Continuous infusion ensures a steady supply of insulin until subcutaneous insulin therapy can be resumed. Proper management during illness helps prevent DKA episodes and promotes early intervention to maintain glycemic control. For more information, please visit: 4 Diabetic Ketoacidosis and Hyperglycemic Hyperosmolar Nonketotic Syndrome Nursing Care Plans. Monitor the patient for signs and symptoms of HHS, including hypotension , profound dehydration, tachycardia, and neurologic changes. Regular monitoring allows for early detection of HHS and prompt intervention to prevent complications. Administer intravenous fluids, such as 0. Rehydration is essential in managing HHS to improve tissue perfusion, correct dehydration, and restore fluid balance. Monitoring vital signs, fluid balance, and electrolyte levels helps identify dehydration, electrolyte imbalances, and prevents complications such as fluid overload or cardiac dysrhythmias. Close monitoring of fluid balance and urine output is crucial due to the high risk of kidney failure resulting from severe dehydration. As HHS commonly affects older patients, the nurse should take into account the physiological changes associated with aging. It is important for the nurse to carefully assess cardiovascular, pulmonary, and kidney function throughout the acute and recovery phases of HHS to ensure appropriate management and prevent complications. Administer potassium supplements as indicated and monitor potassium levels closely to maintain electrolyte balance and prevent cardiac dysrhythmias. Potassium replacement is necessary to correct electrolyte imbalances and prevent complications related to hypokalemia or hyperkalemia. Administer insulin therapy as prescribed to treat hyperglycemia and promote glucose utilization. Although insulin plays a lesser role in HHS compared to DKA, it is still administered to manage hyperglycemia. Continuous low-rate insulin infusion is usually given to achieve glycemic control. Monitor neurologic status closely, including mental status changes and focal neurologic deficits, to assess the response to treatment and identify any complications related to cerebral dehydration. Monitoring neurological status helps determine the effectiveness of treatment and allows for early intervention if neurologic complications arise. Provide patient education on self-management strategies, including medication adherence, lifestyle modifications, and regular self-monitoring of blood glucose levels. Patient education empowers the individual to manage their condition effectively, prevent recurrence of HHS, and maintain optimal glycemic control. ASCVD atherosclerotic cardiovascular disease is a significant cause of morbidity and mortality in individuals with diabetes. It primarily affects the medium to large blood vessels, leading to thickening, sclerosis, and plaque formation, which eventually obstruct blood flow. The three main types of macrovascular complications seen frequently in diabetes are coronary artery disease , cerebrovascular disease, and peripheral arterial disease. Assess cardiovascular risk factors. Individuals with diabetes have a higher risk of myocardial infarction MI , which is more common and carries an increased likelihood of complications and recurrent events compared to those without diabetes. Identifying and assessing these risk factors helps in developing an individualized care plan and determining the appropriate management strategies. Educate the patient on the importance of risk factor control. Provide education on the significance of managing risk factors such as obesity, hypertension , dyslipidemia, and smoking cessation. Patient education empowers individuals to take an active role in managing their risk factors, promoting better control and reducing the likelihood of macrovascular complications. Monitor blood pressure regularly. Measure blood pressure at each routine clinical visit and encourage patients to monitor their blood pressure at home. Hypertension control is essential in individuals with diabetes, and regular blood pressure monitoring, both at clinical visits and at home, is recommended. Regular blood pressure monitoring helps in identifying and managing hypertension, a significant risk factor for ASCVD, and allows for timely intervention and treatment adjustments. Treatment targets should be individualized based on cardiovascular risk factors and patient preferences. Lifestyle interventions, such as weight loss, adopting a Dietary Approaches to Stop Hypertension DASH eating pattern, reducing sodium intake, and increasing physical activity, are recommended. Pharmacologic interventions, including antihypertensive drug therapy, are initiated when blood pressure is persistently elevated, and combination therapy may be necessary to achieve targets. Encourage lifestyle modifications. Promote adherence to lifestyle interventions, including medical nutrition therapy MNT , weight loss when indicated, adoption of a Dietary Approaches to Stop Hypertension DASH eating pattern, reduction of sodium intake, moderation of alcohol consumption, and increased physical activity. Lifestyle modifications play a crucial role in managing obesity, hypertension, and hyperlipidemia, reducing the risk of ASCVD and macrovascular complications. Administer medications as prescribed. Ensure the patient receives prescribed medications for managing hypertension, hyperlipidemia, and diabetes. Lipid management plays a crucial role in preventing ASCVD in diabetes. Lifestyle modifications, such as weight loss, adopting a Mediterranean or DASH eating pattern, reducing saturated and trans fats, and increasing physical activity, are recommended. Lipid profiles should be obtained regularly, and statin therapy is recommended for primary and secondary prevention based on age, ASCVD risk factors, and baseline LDL cholesterol levels. Additional lipid-lowering agents, such as ezetimibe or icosapent ethyl, may be considered in certain cases. Pharmacologic interventions are necessary to achieve optimal control of blood pressure, lipid levels, and glucose management, reducing the risk of macrovascular complications. Antiplatelet therapy with aspirin is recommended for secondary prevention in individuals with diabetes and a history of ASCVD. Dual antiplatelet therapy may be considered after an acute coronary syndrome. Screening for coronary artery disease is not recommended in asymptomatic individuals if ASCVD risk factors are adequately treated. However, investigations for CAD are indicated in the presence of atypical cardiac symptoms, signs of associated vascular disease, or ECG abnormalities. Monitor blood glucose levels. Regularly assess and monitor blood glucose levels in patients with symptoms suggestive of acute diabetic complications or stroke. Elevated blood glucose levels can worsen the outcome of a stroke and may mimic symptoms of acute diabetic complications, making it crucial to assess and treat abnormal glucose levels promptly. Lifestyle changes are an essential way to manage diabetes. These changes may include exercise, maintaining a moderate weight, and eating a healthy and nutritious diet. You may work with a doctor who specializes in diabetes and a dietitian who can help you plan your meals. At the end of the day, you may spend a lot of time buying healthy foods, planning meals, and cooking. Because of the work that goes into meal planning , getting support and guidance can be helpful. Some general recommendations for healthy eating with diabetes include:. Managing diabetes and making lifestyle changes can come with a learning curve. Working with diabetes educators can help you make better choices that may help you better manage T2D. Some of the skills diabetes educators can help you learn may include :. A doctor may refer you to a diabetes self-management education and support service, or you can find one with the American Diabetes Association tool. You may need to work with a healthcare team to figure out a diabetes care plan that works best for you. A care plan will likely include different items such as blood sugar management, medications that may help you manage your diabetes, food choices, exercise plans, and mental health considerations. Diabetes may worsen mental health, and untreated mental health issues may make your diabetes management more difficult. People who have diabetes are times more likely to have depression , and only one-quarter to one-half of the population seek help. Getting help and support can help you cope with the stress that can come with self-care. Research from points to the benefits of receiving emotional and psychological help, including improvement in diabetes management in the short term as well as preventing diabetes complications in the long term. A healthcare team can help you manage T2D through office visits, routine medical testing, lifestyle education, nutritional advice, or counseling. You have the most power concerning your diabetes management. Learning and using T2D self-care is the best way to stay healthy. Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available. Has taking insulin led to weight gain for you? Learn why this happens, plus how you can manage your weight once you've started insulin treatment. When it comes to managing diabetes, adding the right superfoods to your diet is key. Try these simple, delicious recipes for breakfast, lunch, and…. A Quiz for Teens Are You a Workaholic? How Well Do You Sleep? Health Conditions Discover Plan Connect. Type 2 Diabetes Self-Care: Blood Sugar, Mental Health, Medications, and Meals. Medically reviewed by Kelly Wood, MD — By Jennifer M. Edwards on September 7, Importance of T2D self-care Blood sugar Most common medications Food choices Getting diabetes education Mental health Takeaway The focus in managing type 2 diabetes includes blood sugar monitoring, taking your prescribed medications as needed, and working with a healthcare team on food choices, exercise planning, and mental health. Why is type 2 diabetes management important? How often should you check your blood sugar with type 2 diabetes? What should your blood sugar levels be? Was this helpful? Most common type 2 diabetes medications. |
| Self-Management Model - RHIhub Diabetes Prevention Toolkit | It involves mentally dividing the plate into three sections. When it comes to managing diabetes, adding the right superfoods to your diet is key. This promotes a safe exercise environment and ensures that prompt action can be taken if a diabetes-related emergency occurs. El-Gayar O, Timsina P, Nawar N, Eid W. Ensure that the appropriate syringe size is selected to match the insulin concentration being used and on the different sizes of insulin syringes available 1mL, 0. |

Self-care plans for diabetes management -
Healthy eating Eat healthy foods that give you the nutrition you need and help your blood sugar stay in your target range. Your blood pressure and weight will be checked, and your self-care plan and medicines will be reviewed. Dental exam Get your teeth and gums cleaned at least once a year more often if your doctor recommends , and let your dentist know that you have diabetes.
Flu shot Kidney tests Cholesterol test Dilated eye exam You may need this exam more often if you have diabetes-related eye problems. Hearing check Complete foot check You may need this foot check more often if you have ever had diabetes-related foot problems.
New symptoms or health problems If you notice new health problems or if existing problems are getting worse, call your doctor immediately so you can be evaluated. Videos: Learn the Basics of Self-Care Diabetes Education and Support Manage Blood Sugar Prevent Diabetes Complications Steps to Help You Stay Healthy With Diabetes Managing Diabetes: Medicare Coverage and Resources [PDF — 1 MB].
Last Reviewed: April 19, Source: Centers for Disease Control and Prevention. Facebook Twitter LinkedIn Syndicate. home Diabetes Home. To receive updates about diabetes topics, enter your email address: Email Address.
What's this. Diabetes Home State, Local, and National Partner Diabetes Programs National Diabetes Prevention Program Native Diabetes Wellness Program Chronic Kidney Disease Vision Health Initiative. Links with this icon indicate that you are leaving the CDC website. The Centers for Disease Control and Prevention CDC cannot attest to the accuracy of a non-federal website.
Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
You will be subject to the destination website's privacy policy when you follow the link. Self-monitoring of glycemic control is a cornerstone of diabetes care that can ensure patient participation in achieving and maintaining specific glycemic targets.
The most important objective of monitoring is the assessment of overall glycemic control and initiation of appropriate steps in a timely manner to achieve optimum control. Self-monitoring provides information about current glycemic status, allowing for assessment of therapy and guiding adjustments in diet, exercise and medication in order to achieve optimal glycemic control.
Irrespective of weight loss, engaging in regular physical activity has been found to be associated with improved health outcomes among diabetics[ 42 — 45 ].
The National Institutes of Health[ 46 ] and the American College of Sports Medicine[ 47 ] recommend that all adults, including those with diabetes, should engage in regular physical activity.
Treatment adherence in diabetes is an area of interest and concern to health professionals and clinical researchers even though a great deal of prior research has been done in the area. In diabetes, patients are expected to follow a complex set of behavioral actions to care for their diabetes on a daily basis.
These actions involve engaging in positive lifestyle behaviors, including following a meal plan and engaging in appropriate physical activity; taking medications insulin or an oral hypoglycemic agent when indicated; monitoring blood glucose levels; responding to and self-treating diabetes- related symptoms; following foot-care guidelines; and seeking individually appropriate medical care for diabetes or other health-related problems[ 48 ].
The majority of patients with diabetes can significantly reduce the chances of developing long-term complications by improving self-care activities. In the process of delivering adequate support healthcare providers should not blame the patients even when their compliance is poor[ 49 ].
One of the realities about type-2 diabetes is that only being compliant to self-care activities will not lead to good metabolic control.
Research work across the globe has documented that metabolic control is a combination of many variables, not just patient compliance[ 51 , 52 ]. In an American trial, it was found that participants were more likely to make changes when each change was implemented individually.
Success, therefore, may vary depending on how the changes are implemented, simultaneously or individually[ 53 ]. Some of the researchers have even suggested that health professionals should tailor their patient self-care support based on the degree of personal responsibility the patient is willing to assume towards their diabetes self-care management[ 54 ].
The role of healthcare providers in care of diabetic patients has been well recognized. Socio-demographic and cultural barriers such as poor access to drugs, high cost, patient satisfaction with their medical care, patient provider relationship, degree of symptoms, unequal distribution of health providers between urban and rural areas have restricted self-care activities in developing countries[ 39 , 55 — 58 ].
Another study stressed on both patient factors adherence, attitude, beliefs, knowledge about diabetes, culture and language capabilities, health literacy, financial resources, co-morbidities and social support and clinician related factors attitude, beliefs and knowledge about diabetes, effective communication [ 60 ].
Because diabetes self-care activities can have a dramatic impact on lowering glycosylated hemoglobin levels, healthcare providers and educators should evaluate perceived patient barriers to self-care behaviors and make recommendations with these in mind. Unfortunately, though patients often look to healthcare providers for guidance, many healthcare providers are not discussing self-care activities with patients[ 61 ].
Some patients may experience difficulty in understanding and following the basics of diabetes self-care activities. When adhering to self-care activities patients are sometimes expected to make what would in many cases be a medical decision and many patients are not comfortable or able to make such complex assessments.
It is critical that health care providers actively involve their patients in developing self-care regimens for each individual patient. This regimen should be the best possible combination for every individual patient plus it should sound realistic to the patient so that he or she can follow it[ 62 ].
Also, the need of regular follow-up can never be underestimated in a chronic illness like diabetes and therefore be looked upon as an integral component of its long term management.
A clinician should be able to recognize patients who are prone for non-compliance and thus give special attention to them. On a grass-root level, countries need good diabetes self-management education programs at the primary care level with emphasis on motivating good self-care behaviors especially lifestyle modification.
Furthermore, these programs should not happen just once, but periodic reinforcement is necessary to achieve change in behavior and sustain the same for long-term. While organizing these education programs adequate social support systems such as support groups, should be arranged.
As most of the reported studies are from developed countries so there is an immense need for extensive research in rural areas of developing nations. Concurrently, field research should be promoted in developing countries about perceptions of patients on the effectiveness of their self-care management so that resources for diabetes mellitus can be used efficiently.
To prevent diabetes related morbidity and mortality, there is an immense need of dedicated self-care behaviors in multiple domains, including food choices, physical activity, proper medications intake and blood glucose monitoring from the patients. World health organization: Definition, diagnosis and classification of diabetes mellitus and its complications.
Geneva: World health organization; Google Scholar. Kinra S, Bowen LJ, Lyngdoh T, Prabhakaran D, Reddy KS, Ramakrishnan L: Socio-demographic patterning of non-communicable disease risk factors in rural India: a cross sectional study.
BMJ , c Article PubMed PubMed Central Google Scholar. Chuang LM, Tsai ST, Huang BY, Tai TY: The status of diabetes control in Asia—a cross-sectional survey of 24 patients with diabetes mellitus in Diabet Med , 19 12 — Article CAS PubMed Google Scholar.
Narayanappa D, Rajani HS, Mahendrappa KB, Prabhakar AK: Prevalence of pre-diabetes in school-going children. Indian Pediatr , 48 4 — American Diabetes Association: Implications of the United Kingdom Prospective Diabetes Study.
Diabetes Care , 27 Suppl 1 — Zucchi P, Ferrari P, Spina ML: Diabetic foot: from diagnosis to therapy.
G Ital Nefrol , 22 Suppl 31 :SS PubMed Google Scholar. World health organization: Diabetes — Factsheet.
Mohan D, Raj D, Shanthirani CS, Datta M, Unwin NC, Kapur A: Awareness and knowledge of diabetes in Chennai - The Chennai urban rural epidemiology study. J Assoc Physicians India , — Wild S, Roglic G, Green A, Sicree R, King H: Global prevalence of diabetes: Estimates for the year and projections for Diabetes Care , 27 5 — Article PubMed Google Scholar.
Pradeepa R, Mohan V: The changing scenario of the diabetes epidemic: Implications for India. Indian J Med Res , — CAS PubMed Google Scholar.
Katulanda P, Constantine GR, Mahesh JG, Sheriff R, Seneviratne RD, Wijeratne S: Prevalence and projections of diabetes and pre-diabetes in adults in Sri Lanka - Sri Lanka Diabetes, Cardiovascular Study SLDCS.
Diabet Med , 25 9 — Wagner EH, Austin BT, Davis C, Hindmarsh M, Schaefer J, Bonomi A: Improving chronic illness care: translating evidence into action. Health Aff Millwood , 20 6 — UKPDS: Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes UKPDS Lancet , — Article Google Scholar.
Ohkubo Y, Kishikawa H, Araki E, Miyata T, Isami S, Motoyoshi S: Intensive insulin therapy prevents the progression of diabetic micro-vascular complications in Japanese patients with non-insulin-dependent diabetes mellitus: a randomized prospective 6-year study. Diabetes Res Clin Pract , 28 2 — Shobana R, Augustine C, Ramachandran A, Vijay V: Improving psychosocial care: The Indian experience.
Diabetes Voice , 50 1 — Chew LD: The impact of low health literacy on diabetes outcomes. Diabetes Voice , 49 3 — Grey M, Thurber FW: Adaptation to chronic illness in childhood: diabetes mellitus. J Pediatr Nurs , 6 5 — Glasgow RE, Hiss RG, Anderson RM, Friedman NM, Hayward RA, Marrero DG: Report of the health care delivery work group: behavioral research related to the establishment of a chronic disease model for diabetes care.
Diabetes Care , 24 1 — BMJ , Health Educ Res , 18 2 — Paterson B, Thorne S: Developmental evolution of expertise in diabetes self management.
Clin Nurs Res , 9 4 — Etzwiler DD: Diabetes translation: a blueprint for the future. Diabetes Care , 17 Suppl. Bradley C: Handbook of Psychology and Diabetes. Chur, Switzerland: Harwood Academic; Johnson SB: Health behavior and health status: concepts, methods and applications.
J Pediatr Psychol , 19 2 — McNabb WL: Adherence in diabetes: can we define it and can we measure it? Diabetes Care , 20 2 — American Association of Diabetes Educators: AADE7 Self-Care Behaviors.
Diabetes Educ , — Povey RC, Clark-Carter D: Diabetes and healthy eating: A systematic review of the literature. Diabetes Educ , 33 6 — Boule NG, Haddad E, Kenny GP, Wells GA, Sigal RJ: Effects of exercise on glycemic control and body mass in type 2 diabetes mellitus: A meta-analysis of controlled clinical trials.
JAMA , 10 — American Diabetes Association: Standards of Medical Care in Diabetes - Diabetes Care , 32 Suppl 1 :SS Article PubMed Central Google Scholar.
Odegard PS, Capoccia K: Medication taking and diabetes: A systematic review of the literature. Deakin T, McShane CE, Cade JE, Williams RD: Group based training for self management strategies in people with type 2 diabetes mellitus. Cochrane Database Syst Rev , 2: CD Herschbach P, Duran G, Waadt S, Zettler A, Amch C: Psychometric properties of the questionnaire on stress in patients with diabetes-revised QSD-R.
Health Psychol , 16 2 — J Assoc Physicians India , 47 12 — Poulsen P, Kyvik OK, Vag A, Nielsen-Beck H: Heritability of type II diabetes mellitus and abnormal glucose tolerance — a population-based twin study. Diabetologia , 42 2 — American college of endocrinology: The American association of clinical endocrinologist guidelines for the management of diabetes mellitus: the AACE system of diabetes self-management.
Endocr Pract , 8: SS Hendra JT, Sinclair AJ: Improving the care of elderly diabetic patients: the final report of the St. Vincent joint task force. Age and Aging , 26 1 :3—6. Article CAS Google Scholar.
Mensing C, Boucher J, Cypress M, Weinger K, Mulcahy K, Barta P: National standards for diabetes self-management education.
Diabetes Care , 29 Suppl 1 :SS Williams GC, Freedman ZR, Deci EL: Supporting autonomy to motivate patients with diabetes for glucose control. Diabetes Care , 21 10 — Norris SL, Lau J, Smith SJ, Schmid CH, Engelgau MM: Self-management education for adults with type-2 diabetes: a meta-analysis of the effect on glycemic control.
Diabetes Care , 25 7 — Glasgow RE, Strycker LA: Preventive care practices for diabetes management in two primary care samples. Am J Prev Med , 19 1 :9— Walker E: Characteristics of the adult learner.
Diabetes Educ , 25 6 Suppl — American Diabetes Association: Standards of medical care in diabetes - Diabetes Care , 34 Suppl 1 :SS Colberg SR, Sigal RJ, Fernhall B, Regensteiner JG, Blissmer BJ, Rubin RR: Exercise and type-2 diabetes.
Diabetes Care , 33 12 — Mora S, Lee IM, Buring JE, Ridker PM: Association of physical activity and body mass index with novel and traditional cardiovascular biomarkers in women. JAMA , 12 — Physical Activity Guidelines Advisory Committee: Physical Activity Guidelines Advisory Committee Report, Washington, DC, USA: US Department of Health and Human Services; United States Department of Health and Human Services : Physical Activity Guidelines for Americans; Haskell WL, Lee IM, Pate RR, Powell KE, Blair SN, Franklin BA: Physical activity and public health: updated recommendation for adults from the American college of sports medicine and the American heart association.
Med Sci Sports Exerc , 39 8 — Goodall TA, Halford WK: Self-management of diabetes mellitus: a critical review. Health Psychol , 10 1 :1—8. Marrero DG, Kako KS, Mayfield J, Wheeler ML, Fineberg N: Nutrition management of type-2 diabetes by primary care physicians.
J Gen Intern Med , 15 11 — Article CAS PubMed PubMed Central Google Scholar. Kotwani A, Ewen M, Dey D, Iyer S, Lakshmi PK, Patel A: Prices and availability of common medicines at six sites in India using a standard methodology.
Indian J Med Res , 25 5 — Toljamo M, Hentinen M: Adherence to self-care and glycemic control among people with insulin-dependent diabetes mellitus. J Adv Nurs , 34 6 —
Margaret A. PowersJoan K. Bardsley managment, Marjorie CypressMartha M. FunnellDixie HarmsAmy Hess-FischlBeulette HooksDiana IsaacsEllen D. MandelMelinda D.
Ja sind Sie talentvoll