Video
Metformin: Mechanism of ActionContributor Disclosures. Please read the Disclaimer at the Megformin of this page. All of gludose Metformin and glucose control and goals need to xnd tempered based on individual factors, such as age, life expectancy, and comorbidities.
Although studies Carbohydrate and muscle building bariatric surgery, aggressive insulin therapy, Metfodmin behavioral interventions to achieve snd loss have Metfoormin remissions of type 2 diabetes mellitus that may last several years, ylucose majority of patients glucosr type 2 glhcose require Metformun treatment ajd order to maintain target glycemia.
Treatments to improve glycemic management work by increasing insulin Metfkrmin either through direct Mushroom Ecology Conservation administration or through agents that promote Pancreas anatomy Metformin and glucose controlimproving sensitivity glucosse insulin, delaying glcuose delivery and absorption of carbohydrate from Metformin and glucose control gastrointestinal cnotrol, increasing urinary glucose glufose, or a combination of these approaches.
For controll with overweight, obesity, Metformin and glucose control, or a qnd adverse pattern of adipose tissue distribution, abd weight management should be considered as Foods to enhance recovery therapeutic target Body composition for beginners addition to glycemia.
Methods used to Mdtformin blood glucose contro, patients with newly Metformin and glucose control type 2 Metormin are reviewed here. Further management of persistent hyperglycemia and Metformim therapeutic issues, such as the glucosr of Metdormin and evaluation for microvascular and EGCG and gut health complications, lgucose discussed separately.
See Metflrmin of persistent hyperglycemia in type 2 diabetes mellitus" and Metfrmin of general medical gluclse in nonpregnant Metdormin with diabetes congrol. TREATMENT GOALS. Glycemic management — Target glycated hemoglobin A1C levels in patients with type 2 coontrol should be tailored to the individual, balancing conntrol anticipated reduction in microvascular complications Obesity and health risks time with the immediate conttrol of hypoglycemia contro other adverse effects of therapy.
Glycemic targets are gucose set somewhat higher for older adult patients and those with comorbidities or Endurance running shoes limited Meftormin expectancy who may Metfodmin little likelihood of contro from intensive therapy.
Improved Metormin management lowers the risk of coontrol complications in patients glucoae type 2 diabetes figure glucos [ 1 ]. Gluxose Metformin and glucose control percent drop in glycated hemoglobin A1C is associated with improved outcomes over the long term with no threshold effect.
However, as A1C levels decrease below 7 percent, glcuose absolute risk for microvascular Organic metabolic enhancer becomes low and the Budget meal planning benefit of lowering A1C further has diminishing returns.
Several Probiotic Foods for Babies clinical trials have demonstrated a nad effect of intensive glycemia-lowering therapy conrol macrovascular outcomes in type 2 cojtrol [ Green tea extract and anti-inflammatory effects cpntrol, with controo trials not supporting a significant beneficial vlucose [ 4 ] and one trial suggesting harm [ 5 ].
Glycemic goals are discussed in more detail separately. See "Overview of general medical care in nonpregnant adults with diabetes mellitus", section on 'Glycemic ans and "Treatment of type 2 znd mellitus in the older patient", section on 'Controlling gluccose and "Glycemic control and conttol complications qnd type 2 diabetes mellitus", section on 'Choosing a glycemic target'.
Cardiovascular risk factor management — In addition to glycemic management, vigorous cardiac Green tea extract and anti-inflammatory effects reduction smoking cessation; blood pressure control; reduction in Metforminn lipids cpntrol a gpucose diet, exercise, and weight loss or maintenance; and aspirin for those with established atherosclerotic cardiovascular cobtrol [ASCVD] or after shared decision-making Mdtformin be a Green tea extract and anti-inflammatory effects priority for all patients with type 2 diabetes.
Lgucose, in spite of evidence Cognitive function training techniques aggressive multifactor glicose reduction lowers the risk gluccose both micro- and macrovascular complications in patients with diabetes [ 6,7 Metforkin, a minority of adults with diabetes fully achieve recommended Metforimn for A1C, blood pressure Coconut Oil Lotion, and management of dyslipidemia [ Guarana properties and uses ].
See "Overview of general Increases overall happiness care in nonpregnant Guarana seed caffeine supplement with diabetes contro, section on 'Aspirin' and Maintaining stable blood sugar of Promote healthy digestion in patients with diabetes mellitus" Supporting efficient nutrient transport systems "Low-density Blood pressure and pregnancy cholesterol-lowering therapy in the primary g,ucose of cardiovascular disease" and "Management of nad density lipoprotein cholesterol LDL-C in the secondary conrtol of cardiovascular disease" and Metfirmin of general medical care in nonpregnant conyrol with diabetes mellitus", section on 'Multifactorial risk factor Measuring water volume. DIABETES EDUCATION — Patients Metdormin newly diagnosed Cobtrol should participate in a comprehensive diabetes self-management education cintrol, which includes contrlo instruction goucose nutrition, physical activity, optimizing glucode control, and preventing contgol.
In clinical gucose comparing Metformn education with ad care, there was a small but statistically Metformln reduction Supplements for promoting healthy vision and eye health in fitness enthusiasts A1C in patients receiving the diabetes education intervention [ 9 ].
In glicose meta-analyses, use of mobile phone interventions for diabetes education was successful in significantly reducing A1C Skinfold measurement comparison with other methods Medical nutrition therapy — Metformkn nutrition therapy MNT gljcose the process Well-rounded diet for sports which a dietary plan is tailored for Refillable travel mugs with diabetes, based on medical, lifestyle, and personal factors.
It is an Metfotmin component Metrormin diabetes management and diabetes Metformon education. For all Fitness bootcamp classes, the goals confrol MNT include avoidance of weight conteol, consistency in day-to-day annd intake at Metcormin and snacks, and balanced nutritional content.
MNT Green tea extract and anti-inflammatory effects be customized to achieve body weight reduction and is cpntrol in detail elsewhere. See 'Diet' below Metfofmin "Medical nutrition therapy for type amd diabetes mellitus".
Weight management — For patients contol type 2 gluclse, body weight management should be considered as a therapeutic target in addition to glycemia. Patients should receive counseling regarding changes in diet and physical activity to achieve weight loss or to prevent weight gain.
Weight loss improves glycemia through mitigation of insulin resistance and impaired beta cell function, two major metabolic perturbations evident in type 2 diabetes [ 12,13 ]. For patients who have difficulty achieving weight loss, weight maintenance rather than gain is an alternative goal.
Strategies for weight management include lifestyle change, pharmacologic therapy, and metabolic surgery. Lifestyle change includes diet and physical activity, as well as behaviors that facilitate these changes, and is an essential component of any weight management plan.
We emphasize lifestyle change as our initial approach to body weight reduction and reserve pharmacotherapy and metabolic surgery for patients who do not achieve targeted weight loss with lifestyle change alone. We tailor our specific recommendations to patients' goals and preferences and encourage "intensive" lifestyle modification, where available, for highly motivated patients.
Diet — Diagnosis of type 2 diabetes is often a powerful motivator for lifestyle change. Dietary modification is a highly effective strategy for weight loss and for management of glycemia and hypertension in patients who are willing to commit to it, with metabolic benefit likely outlasting the effect of weight loss per se.
The improvement in glycemia is related both to the degree of caloric restriction and weight reduction [ 12,14,15 ]. Body weight loss of 5 to 10 percent may also improve nonalcoholic steatohepatitis, sleep apnea, and other comorbidities of type 2 diabetes [ 16 ].
Consumption of sugar-sweetened beverages, including natural fruit juice, should be specifically queried and strongly discouraged in order to manage glycemia, weight, and reduce risk for CVD and fatty liver [ 17 ]. See "Medical nutrition therapy for type 2 diabetes mellitus", section on 'Designing a nutrition care plan' and "Management of nonalcoholic fatty liver disease in adults", section on 'Initial lifestyle interventions'.
In a two-year analysis of the DiRECT trial, only 11 percent of intervention participants had weight loss of 15 kg or more compared with 24 percent in the one-year analysis [ 18 ]. However, 36 percent of participants maintained diabetes remission, compared with 3 percent of control patients.
Several studies have evaluated the long-term efficacy of diet alone or with exercise in patients with newly diagnosed type 2 diabetes see "Medical nutrition therapy for type 2 diabetes mellitus". In the United Kingdom Prospective Diabetes Study UKPDSfor example, all patients were given a low-calorie, low-fat, high complex carbohydrate diet [ 21 ].
Furthermore, the mean glucose value was substantially higher with diet alone than with diet plus an oral hypoglycemic drug or insulin. The likelihood of a successful glycemic response to diet is determined in large part by the initial fasting blood glucose.
Pharmacologic therapy — Pharmacotherapy targeted solely for weight management is effective in patients with type 2 diabetes. Although metformin is usually started for the management of hyperglycemia, it is also frequently an effective medication to promote modest weight loss.
When additional body weight reduction is a primary goal of therapy, we choose medications that promote weight loss and lower glucose.
Glucagon-like peptide 1 GLP-1 receptor and dual GLP-1 and glucose-dependent insulinotropic polypeptide GIP agonist therapies promote weight loss and help prevent weight gain due to other glucose-lowering pharmacotherapies.
We add these medications sequentially to metformin if additional glucose lowering or weight loss is a treatment goal. See "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus" and "Obesity in adults: Drug therapy".
Surgical therapy — Weight loss surgery in patients with obesity and type 2 diabetes results in the largest degree of sustained weight loss and, in parallel, improvements in blood glucose management and the most frequent sustained remissions of diabetes.
Weight loss surgery is an option to treat poorly managed type 2 diabetes when other modalities have failed. This topic is reviewed in detail separately. See "Management of persistent hyperglycemia in type 2 diabetes mellitus", section on 'Bariatric metabolic surgery'.
Exercise — Regular exercise is beneficial in type 2 diabetes, independent of weight loss. It leads to improved glycemic management due to increased responsiveness to insulin; it can also delay the progression of impaired glucose tolerance to overt diabetes [ 22,23 ].
These beneficial effects are directly due to exercise, but concurrent weight reduction plays a contributory role. In one study, however, only 50 percent of patients with type 2 diabetes were able to maintain a regular exercise regimen [ 24 ].
See "Exercise guidance in adults with diabetes mellitus". Shorter-duration, intensive exercise may be appropriate for physically fit individuals [ 25 ].
Resistance training may be particularly important for individuals with type 2 diabetes who do not have overweight or obesity, in whom relative sarcopenia may contribute to diabetes pathophysiology [ 26 ].
Intensive lifestyle modification — In patients with established type 2 diabetes, intensive behavioral modification interventions focusing on weight reduction and increasing activity levels are successful in reducing weight and improving glycemic management while, at the same time, reducing the need for glucose-lowering and other medications [ 15,18, ].
The intensive intervention included caloric restriction maximum 30 percent calories from fat, minimum 15 percent protein, and the remainder from carbohydrates, in the form of liquid meal replacements, frozen food entrees, or structured meal plansmoderate-intensity physical activity goal minutes weeklyand weekly group or individual sessions with registered dietitians, behavioral psychologists, and exercise specialists.
The primary outcome was a composite of death from cardiovascular causes, nonfatal myocardial infarction, nonfatal stroke, and hospitalization for angina.
Although the anticipated follow-up period was After a median follow-up of 9. The improvement in weight and glycemia did not reduce the occurrence of cardiovascular events.
Possible reasons for this finding include the lower-than-expected rates of cardiovascular events in both groups, improved overall cardiovascular risk factor treatment with medical therapy antihypertensives, statins in the standard diabetes education arm, enrollment of a relatively healthy patient population, gradual weight loss in the control group such that the differential weight loss between the two groups was only 2.
A sustained weight loss of greater than that achieved in the trial may be required to reduce the risk of CVD. In an observational post hoc analysis of the Look AHEAD trial, weight loss of 10 percent or greater in the first year was associated with a reduction in the primary outcome 1.
However, this post hoc analysis is problematic. Moreover, the degree of weight loss is difficult to achieve and maintain through lifestyle intervention alone. Weight loss, weight loss maintenance, and exercise remain important components of diabetes management due to overall health benefits.
The following summarizes several other major observations from the Look AHEAD trial [ 27,31, ]:. The difference was attenuated but remained significant throughout the trial 6 versus 3. Changes in waist circumference and physical fitness were also significantly better in the intervention group throughout the study.
By study end, mean A1C was significantly lower in the intervention group 7. Psychological interventions — Patients with type 2 diabetes often experience significant stress, a condition often called diabetes distress, related to the many self-care responsibilities required for glycemic management lifestyle modifications, medication, and blood glucose monitoring [BGM] [ 42 ].
Concurrent depression similarly may interfere with self-care. See "Overview of general medical care in nonpregnant adults with diabetes mellitus", section on 'Comorbid conditions'. Psychotherapy reduces psychological distress and improves glycemic management in some [ 43,44 ], but not all [ 45 ], studies.
In a meta-analysis of 12 trials of patients with type 2 diabetes randomly assigned to psychological intervention or usual care, mean A1C was lower in the intervention group pooled mean difference Measures of psychological distress were also significantly lower in the intervention group, but there were no differences in weight management.
Pregnancy planning — All women of childbearing age with diabetes should be counseled about the potential effects of diabetes and commonly used medications on maternal and fetal outcomes and the potential impact of pregnancy on their diabetes management and any existing complications. See "Pregestational preexisting diabetes: Preconception counseling, evaluation, and management".
When to start — Early institution of treatment for diabetes, at a time when the A1C is not substantially elevated, is associated with improved glycemic management over time and decreased long-term complications [ 46 ].
Pharmacologic therapy should be initiated along with consultation for lifestyle modification focusing on dietary and other lifestyle contributors to hyperglycemia. Weight loss and weight loss maintenance underpins all effective type 2 diabetes therapy, and lifestyle change reduces the risk of weight gain associated with sulfonylureas and insulin.
However, for those patients who have clear and modifiable contributors to hyperglycemia and who are motivated to change them eg, commitment to reduce consumption of sugar-sweetened beveragesa three-month trial of lifestyle modification prior to initiation of pharmacologic therapy is warranted.
Choice of initial therapy — Our suggestions are based upon clinical trial evidence and clinical experience in achieving glycemic targets and minimizing adverse effects table 1with the recognition that there is a paucity of high-quality, head-to-head drug comparison trials and long-duration trials or ones with important clinical endpoints, such as effects on complications.
The long-term benefits and risks of using one approach over another are unknown. In selecting initial therapy, we consider patient presentation eg, presence or absence of symptoms of hyperglycemia, comorbidities, baseline A1C levelindividualized treatment goals and preferences, the glucose-lowering efficacy of individual drugs, and their adverse effect profile, tolerability, and cost [ 47 ].
We prefer initiating a single agent typically metformin and then sequentially adding additional glucose-lowering agents as needed, rather than starting with combination therapy [ 48 ].
Related Pathway s : Diabetes: Initial therapy for non-pregnant adults with type 2 DM.
: Metformin and glucose control| About metformin | Whatever the cause of the treatment failure, action needs to be taken to restore glucose control and prevent diabetes complications. This may involve improving drug adherence, correcting dosing mistakes, increasing the metformin dose, or adding another diabetes drug to the treatment plan. Metformin is not a "cure" for type 2 diabetes, and medication alone is not enough to keep your blood sugar in control. If you eat poorly or live an otherwise inactive lifestyle, metformin may only go so far in controlling your blood sugar. No matter how early or advanced your diabetes is, good lifestyle choices are needed to ensure your long-term health and well-begin. This involves eating a healthy diet , exercising regularly, taking your medications as prescribed, and losing weight if you are overweight or have obesity. If needed, ask your healthcare provider for a referral to a nutritionist or personal trainer who can help. Because diabetes is progressive, people may need a higher dose or additional medications the longer they have the disease. Metformin works best when combined with diet, exercise, and a healthy weight. Simply taking metformin without lifestyle changes will likely shorten the effectiveness of the drug. Metformin is taken once or twice daily with food to avoid stomach upset and other gastrointestinal side effects. Ideally, the drug is taken with the morning meal for a once-daily dose and both the morning and evening meal for a twice-daily dose. Marshall SM. Rojas LBA, Gomes MB. Metformin: an old but still the best treatment for type 2 diabetes. Diabetol Metab Syndr. Song R. Mechanism of metformin: A tale of two sites. Diabetes Care. American Diabetes Association. Hyperglycemia high blood glucose. American Diabetes Association Professional Practice Committee. Pharmacologic Approaches to Glycemic Treatment: Standards of Care in Diabetes doi: By Barbie Cervoni, RD Barbie Cervoni MS, RD, CDCES, CDN, is a New York-based registered dietitian and certified diabetes care and education specialist. Use limited data to select advertising. Create profiles for personalised advertising. Use profiles to select personalised advertising. Create profiles to personalise content. Use profiles to select personalised content. Measure advertising performance. Measure content performance. Understand audiences through statistics or combinations of data from different sources. Develop and improve services. Use limited data to select content. List of Partners vendors. Type 2 Diabetes. By Barbie Cervoni, RD. Medically reviewed by Lindsay Cook, PharmD. Table of Contents View All. Table of Contents. How Metformin Works. Signs to Look For. Possible Complications. If Metformin Stops Working. Frequently Asked Questions. When to Call Your Healthcare Provider Sudden, unexplained increases in blood sugar that persist for several days may be a sign that your metformin is no longer working. Does Metformin Cause Cancer? Frequently Asked Questions Can metformin become less effective over time? What are common side effects of metformin? Common side effects of metformin include: Heartburn Bloating Gas Stomach pain Metallic taste Diarrhea Constipation Headache Nausea or vomiting. When should you take metformin? Verywell Health uses only high-quality sources, including peer-reviewed studies, to support the facts within our articles. About Us. What We Do. Strategic Initiatives. Program for Art in Public Spaces. Executive Committee. Aperture: Women in Medicine. Portraits of Strength. Event Photo Galleries. Additional Support. MD Program. MD-PhD Program. PA Program. PA Online Program. Joint MD Programs. MHS Program. How to Apply. Advanced Health Sciences Research. Clinical Investigation. Medical Education. MHS Team. Visiting Student Programs. Center for Med Ed. Office of the Deputy Dean. Organizational Chart. Janeway Society. First Fridays. Physician-Scientist Development Awards. Fund for Physician-Scientist Mentorship. Grant Library. Grant Writing Course. Mock Study Section. Research Paper Writing. Funding Opportunities. Engaging with Students. Join Our Voluntary Faculty. Faculty Directory. Research by Keyword. Research by Department. Research by Global Location. Translational Research. Resources for Investigators. Team Science. Program for the Promotion of Interdisciplinary Team Science POINTS. Health Equity Research. Community-Engaged Research CEnR. CEnR Steering Committee. Experiential Learning Subcommittee. OHER News. YSM Biobank. Embryonic Stem Cell Research Oversight. COVID Research. Mapping COVID Data. COVID Vaccinations in CT. Case Maps. COVID in Connecticut Schools. Connecticut Towns COVID Impact Dashboard. Connecticut Town Day Cases Time Lapse. CT Correctional Facilities with COVID Cases Dashboard. Connecticut COVID Presence Map. CT Nursing Homes with COVID Cases. COVID Presence Map. COVID Case Density by US County. Global Cases Dashboard. Time-Lapse of Global Spread. US Racial and Ethnic Disparities in COVID Mortality. Childcare Survey and Data Display. Risk of Complications Conditional on COVID Infection. Geographic Access. Travel Time to COVID Testing Sites in Connecticut. Travel Time to COVID Testing Sites in the US. Project Team. Yale Medicine Magazine. Issues List. Print Magazine PDFs. |
| Metformin: How a Widely Used Diabetes Medication Actually Works < Yale School of Medicine | See "General principles of insulin therapy in diabetes mellitus", section on 'U regular insulin' and "General principles of insulin therapy in diabetes mellitus", section on 'Basal insulin analogs'. While use of concentrated insulins is often effective for glycemic management, the worsening obesity associated with high-dose insulin can result in progressively increasing insulin requirements. This phenomenon may then lead to reconsideration of addition of an insulin-sparing agent eg, GLP-1 receptor agonist or thiazolidinedione or bariatric surgery. See 'Bariatric metabolic surgery' below and "Medical nutrition therapy for type 2 diabetes mellitus". The vast majority of these CVD safety studies were placebo-controlled and enrolled all or a majority of patients with pre-existing CVD or at high cardiovascular risk, representing a minority of the type 2 diabetes population. The long-term benefits and risks of using one agent over another in the absence of diagnosed CVD or high atherosclerotic CVD ASCVD risk are less clear. Thus, the results of these trials are most applicable to patients similar to the trial population and not to all patients with type 2 diabetes [ 2,60 ]. Cardiovascular benefit has been demonstrated for some of these medications when taken in combination with metformin , but benefit has not been definitively established in drug-naïve patients at low to moderate cardiovascular risk. See 'Without established cardiovascular or kidney disease' above. The cardiovascular effects of each diabetes drug when data are available is reviewed in the individual topics. See "Metformin in the treatment of adults with type 2 diabetes mellitus", section on 'Cardiovascular effects' and "Sulfonylureas and meglitinides in the treatment of type 2 diabetes mellitus", section on 'Cardiovascular effects' and "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus", section on 'Cardiovascular effects' and "Thiazolidinediones in the treatment of type 2 diabetes mellitus", section on 'Cardiovascular effects' and "Dipeptidyl peptidase 4 DPP-4 inhibitors for the treatment of type 2 diabetes mellitus", section on 'Cardiovascular effects' and "Sodium-glucose cotransporter 2 inhibitors for the treatment of hyperglycemia in type 2 diabetes mellitus", section on 'Cardiovascular effects' and "Insulin therapy in type 2 diabetes mellitus". They can reduce A1C values slightly 0. They act predominantly by lowering glucose concentrations after meals but may be poorly tolerated because of flatulence and other gastrointestinal GI side effects. However, if they are started at a low dose 25 mg before meals and slowly increased, they can be effective in people who follow high-carbohydrate diets. See "Alpha-glucosidase inhibitors for treatment of diabetes mellitus". Pramlintide is only approved for use in patients also taking prandial insulin, and therefore, it is not generally used in patients with type 2 diabetes. It also has frequent GI side effects. See "Amylin analogs for the treatment of diabetes mellitus". In , another inhaled insulin preparation was approved by the US Food and Drug Administration FDA. Inhaled insulin causes a very rapid rise in serum insulin concentration similar to that after subcutaneous rapid-acting insulins and faster than that after subcutaneous regular insulin. It is designed to be used to manage postprandial glucose levels. Inhaled insulin may cause a transient cough with each inhalation, and it requires pulmonary monitoring. It is used infrequently in patients with type 2 diabetes. See "Inhaled insulin therapy in diabetes mellitus". Colesevelam's mechanism of action to improve glycemia is uncertain [ 64 ]. One possibility is that bile acid sequestrants act in the GI tract to reduce glucose absorption. In a meta-analysis of five short-term trials 16 to 26 weeks in patients with type 2 diabetes inadequately treated with oral agents or insulin, the addition of colesevelam compared with placebo modestly reduced A1C levels mean difference 0. The meta-analysis was limited by the high or unclear risk of bias in the individual trials. Side effects can include constipation, nausea, and dyspepsia. In contrast to its effects on LDL cholesterol, colesevelam increases triglyceride concentrations by approximately 20 percent [ 66,67 ]. The clinical implications of this increase are unknown. See "Lipoprotein classification, metabolism, and role in atherosclerosis", section on 'Apolipoprotein C-III'. Given the modest glucose-lowering effectiveness, expense, and limited clinical experience, we typically do not recommend colesevelam to improve glycemic management in patients with type 2 diabetes. See "Management of hyperprolactinemia", section on 'Overview of dopamine agonists'. A quick-release formulation of bromocriptine has been approved by the FDA for the treatment of type 2 diabetes mellitus [ 68 ]. In short-term clinical trials in patients with type 2 diabetes mellitus, bromocriptine up to 4. Common side effects include nausea, vomiting, dizziness, and headache [ 70 ]. The mechanism of action in reducing blood sugar is unknown. Given its modest glucose-lowering effect, very frequent GI side effects, and the availability of more effective drugs, we do not recommend bromocriptine for the treatment of type 2 diabetes. BARIATRIC METABOLIC SURGERY — In patients with type 2 diabetes and obesity, bariatric and metabolic surgical procedures that result in sustained, major weight loss have been shown to lead to at least temporary remission of diabetes in a substantial fraction of patients. Bariatric surgical procedures are targeted at weight loss in the setting of obesity; the term "metabolic surgery" is used when a major goal of surgery is to improve diabetes or other metabolic diseases eg, nonalcoholic fatty liver disease. Patient selection — Surgical treatment of obesity is an option to treat type 2 diabetes in appropriate surgical candidates with [ 71 ]:. Surgical treatment has also been endorsed in patients with type 2 diabetes with BMI 30 to Given the increasing availability of potent GLPbased therapies and lack of comparative effectiveness data for bariatric surgery and these potent agents, we review these options with our patients and engage in shared decision-making. See "Initial management of hyperglycemia in adults with type 2 diabetes mellitus", section on 'Diabetes education' and "Bariatric surgery for management of obesity: Indications and preoperative preparation", section on 'Indications'. Outcomes — Unblinded trials have compared bariatric surgery with medical therapy for the treatment of type 2 diabetes see "Outcomes of bariatric surgery", section on 'Diabetes mellitus'. However, relapse of diabetes usually occurs over time, with 35 to 50 percent of patients who initially achieved diabetes remission after surgery experiencing a recurrence [ 72,75 ]. Nevertheless, bariatric surgery improves glycemia substantially and significantly more than medication therapy, and most patients have marked improvement in glycemic management for at least 5 to 15 years after surgery. The effects of bariatric surgery on diabetes-related complications are reviewed in detail elsewhere. See "Outcomes of bariatric surgery", section on 'Diabetic complications'. Risks and concerns — Despite these impressive metabolic results, concerns remain about acute postoperative complications including the need for reoperations and rehospitalizations and rare, but potentially severe, adverse events; the long-term success rates in maintaining weight loss [ 71,80,81 ]; and the reproducibility of the results in patients with an extensive history of diabetes or with different surgical teams [ 82 ]. Some weight regain is typical within two to three years of bariatric procedures, and different procedures result in different levels of weight loss and corresponding reductions in glycemia. Bariatric surgical procedures are reviewed in detail elsewhere. See "Bariatric procedures for the management of severe obesity: Descriptions" and "Bariatric surgery for management of obesity: Indications and preoperative preparation" and "Bariatric operations: Early fewer than 30 days morbidity and mortality". SOCIETY GUIDELINE LINKS — Links to society and government-sponsored guidelines from selected countries and regions around the world are provided separately. See "Society guideline links: Diabetes mellitus in adults" and "Society guideline links: Diabetes mellitus in children" and "Society guideline links: Diabetic kidney disease". These articles are best for patients who want a general overview and who prefer short, easy-to-read materials. Beyond the Basics patient education pieces are longer, more sophisticated, and more detailed. These articles are written at the 10 th to 12 th grade reading level and are best for patients who want in-depth information and are comfortable with some medical jargon. Here are the patient education articles that are relevant to this topic. We encourage you to print or e-mail these topics to your patients. You can also locate patient education articles on a variety of subjects by searching on "patient info" and the keyword s of interest. This decision is based on glycated hemoglobin A1C assay results calculator 1 typically performed every three to six months after initial therapy. After a successful initial response to lifestyle intervention and oral therapy, the majority of patients do not maintain target A1C levels during the subsequent three to five years. See 'Indications for a second agent' above. Options include glucagon-like peptide 1 GLP-1 receptor agonists, a dual-acting GLP-1 and glucose-dependent insulinotropic polypeptide GIP receptor agonist tirzepatide , sodium-glucose co-transporter 2 SGLT2 inhibitors, short-acting sulfonylureas eg, glipizide , glimepiride , repaglinide if sulfonylurea not chosen as initial therapy , insulin, dipeptidyl peptidase 4 DPP-4 inhibitors, and pioglitazone figure 1 and table 2. For patients with persistent hyperglycemia while taking a maximally tolerated dose of metformin, the choice of a second medication should be individualized based on efficacy, risk for hypoglycemia, the patient's comorbid conditions, impact on weight, side effects, and cost. These agents have been shown to have the best glycemic efficacy algorithm 1. Gastrointestinal GI side effects, contraindications, and cost may limit their use. To select a medication, we use shared decision-making with a focus on beneficial and adverse effects within the context of the degree of hyperglycemia as well as a patient's comorbidities and preferences algorithm 2. See 'Established cardiovascular or kidney disease' above. The majority of patients in the cardiovascular and renal outcomes trials had established cardiovascular disease CVD or diabetic kidney disease DKD with severely increased albuminuria, and therefore, these are the primary indications for one of these drugs. Patients at high CVD risk but without a prior event might benefit, but the data are less supportive. Similarly, patients without severely increased albuminuria have some benefit, but the absolute benefits are greater among those with severely increased albuminuria. The choice of an alternative glucose-lowering medication is guided by efficacy, patient comorbidities, preferences, side effects, and cost. algorithm 2. See 'Dual agent failure' above. For most patients who do not achieve target A1C with initial dual therapy, we suggest starting insulin or a GLP-1 receptor agonist Grade 2B if neither already chosen as a second agent. In patients on sulfonylureas and metformin who are starting insulin therapy, sulfonylureas are generally tapered and discontinued, while metformin is continued. In patients on DPP-4 inhibitors who are starting a GLP-1 receptor agonist or dual-acting GLP-1 and GIP receptor agonist, the DPP-4 inhibitor is discontinued, while metformin is continued. See 'Dual agent failure' above and 'Insulin initiation and intensification' above. Related Pathway s : Diabetes: Initial therapy for non-pregnant adults with type 2 DM. An alternative is two oral agents and a GLP-1 receptor agonist or dual-acting GLP-1 and GIP receptor agonist, particularly for patients in whom weight loss or avoidance of hypoglycemia is a primary consideration. These GLPbased therapies should not be combined with DPP-4 inhibitors. Another option for patients close to glycemic goals is three oral agents eg, metformin , sulfonylurea plus: DPP-4 inhibitor, SGLT2 inhibitor, or pioglitazone. Although guidelines suggest combining SGLT2 inhibitors and GLP-1 receptor agonists, we do not usually add an SGLT2 inhibitor to GLP-1 receptor agonist therapy for management of hyperglycemia alone, given the absence of data showing additive cardiovascular and kidney benefit and increased patient burden cost, polypharmacy, adverse effects. Bariatric surgery may also be an option in patients with lower BMI 30 to Patients seeking bariatric surgery should be counseled to develop coping skills, eliminate maladaptive behavior, and understand the risks and benefits of the surgery. See 'Bariatric metabolic surgery' above and "Bariatric surgery for management of obesity: Indications and preoperative preparation", section on 'Preoperative counseling'. Why UpToDate? Product Editorial Subscription Options Subscribe Sign in. Learn how UpToDate can help you. Select the option that best describes you. View Topic. Font Size Small Normal Large. Management of persistent hyperglycemia in type 2 diabetes mellitus. Formulary drug information for this topic. No drug references linked in this topic. Find in topic Formulary Print Share. View in. Language Chinese English. Author: Deborah J Wexler, MD, MSc Section Editor: David M Nathan, MD Deputy Editor: Katya Rubinow, MD Contributor Disclosures. All topics are updated as new evidence becomes available and our peer review process is complete. Literature review current through: Jan This topic last updated: Jan 11, Pharmacologic Approaches to Glycemic Treatment: Standards of Care in Diabetes Diabetes Care ; S Davies MJ, Aroda VR, Collins BS, et al. Management of hyperglycaemia in type 2 diabetes, A consensus report by the American Diabetes Association ADA and the European Association for the Study of Diabetes EASD. Diabetologia ; Kirkman MS, Briscoe VJ, Clark N, et al. Diabetes in older adults. Diabetes Care ; Wei N, Zheng H, Nathan DM. Empirically establishing blood glucose targets to achieve HbA1c goals. American Diabetes Association Professional Practice Committee. Glycemic Goals and Hypoglycemia: Standards of Care in Diabetes Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes UKPDS UK Prospective Diabetes Study UKPDS Group. Lancet ; United Kingdom Prospective Diabetes Study UKPDS. BMJ ; prospective diabetes study Overview of 6 years' therapy of type II diabetes: a progressive disease. Prospective Diabetes Study Group. Diabetes ; Turner RC, Cull CA, Frighi V, Holman RR. Glycemic control with diet, sulfonylurea, metformin, or insulin in patients with type 2 diabetes mellitus: progressive requirement for multiple therapies UKPDS JAMA ; GRADE Study Research Group, Nathan DM, Lachin JM, et al. Glycemia Reduction in Type 2 Diabetes - Glycemic Outcomes. N Engl J Med ; Bressler P, DeFronzo RA. Drugs and diabetes. Diabetes Reviews ; Brown JB, Nichols GA, Perry A. The burden of treatment failure in type 2 diabetes. Shah BR, Hux JE, Laupacis A, et al. Clinical inertia in response to inadequate glycemic control: do specialists differ from primary care physicians? Ziemer DC, Doyle JP, Barnes CS, et al. An intervention to overcome clinical inertia and improve diabetes mellitus control in a primary care setting: Improving Primary Care of African Americans with Diabetes IPCAAD 8. Arch Intern Med ; Grant RW, Buse JB, Meigs JB, University HealthSystem Consortium UHC Diabetes Benchmarking Project Team. Quality of diabetes care in U. academic medical centers: low rates of medical regimen change. Fanning EL, Selwyn BJ, Larme AC, DeFronzo RA. Improving efficacy of diabetes management using treatment algorithms in a mainly Hispanic population. Grant RW, Cagliero E, Sullivan CM, et al. A controlled trial of population management: diabetes mellitus: putting evidence into practice DM-PEP. Das SR, Everett BM, Birtcher KK, et al. J Am Coll Cardiol ; Tsapas A, Avgerinos I, Karagiannis T, et al. Comparative Effectiveness of Glucose-Lowering Drugs for Type 2 Diabetes: A Systematic Review and Network Meta-analysis. Ann Intern Med ; Maruthur NM, Tseng E, Hutfless S, et al. Diabetes Medications as Monotherapy or Metformin-Based Combination Therapy for Type 2 Diabetes: A Systematic Review and Meta-analysis. Palmer SC, Mavridis D, Nicolucci A, et al. Comparison of Clinical Outcomes and Adverse Events Associated With Glucose-Lowering Drugs in Patients With Type 2 Diabetes: A Meta-analysis. Rodbard HW, Rosenstock J, Canani LH, et al. Oral Semaglutide Versus Empagliflozin in Patients With Type 2 Diabetes Uncontrolled on Metformin: The PIONEER 2 Trial. Lingvay I, Catarig AM, Frias JP, et al. Efficacy and safety of once-weekly semaglutide versus daily canagliflozin as add-on to metformin in patients with type 2 diabetes SUSTAIN 8 : a double-blind, phase 3b, randomised controlled trial. Lancet Diabetes Endocrinol ; Henry RR, Gumbiner B, Ditzler T, et al. Intensive conventional insulin therapy for type II diabetes. Metabolic effects during a 6-mo outpatient trial. Hemmingsen B, Christensen LL, Wetterslev J, et al. Comparison of metformin and insulin versus insulin alone for type 2 diabetes: systematic review of randomised clinical trials with meta-analyses and trial sequential analyses. BMJ ; e Yki-Järvinen H, Ryysy L, Nikkilä K, et al. Comparison of bedtime insulin regimens in patients with type 2 diabetes mellitus. A randomized, controlled trial. Wulffelé MG, Kooy A, Lehert P, et al. Combination of insulin and metformin in the treatment of type 2 diabetes. Kooy A, de Jager J, Lehert P, et al. Long-term effects of metformin on metabolism and microvascular and macrovascular disease in patients with type 2 diabetes mellitus. Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes UKPDS Russell-Jones D, Vaag A, Schmitz O, et al. Diamant M, Van Gaal L, Stranks S, et al. Once weekly exenatide compared with insulin glargine titrated to target in patients with type 2 diabetes DURATION-3 : an open-label randomised trial. Shyangdan DS, Royle P, Clar C, et al. Glucagon-like peptide analogues for type 2 diabetes mellitus. Cochrane Database Syst Rev ; :CD Singh S, Wright EE Jr, Kwan AY, et al. Glucagon-like peptide-1 receptor agonists compared with basal insulins for the treatment of type 2 diabetes mellitus: a systematic review and meta-analysis. Diabetes Obes Metab ; Frías JP, Davies MJ, Rosenstock J, et al. Tirzepatide versus Semaglutide Once Weekly in Patients with Type 2 Diabetes. Curovic VR, Jongs N, Kroonen MYAM, et al. Optimization of Albuminuria-Lowering Treatment in Diabetes by Crossover Rotation to Four Different Drug Classes: A Randomized Crossover Trial. Shields BM, Dennis JM, Angwin CD, et al. Patient stratification for determining optimal second-line and third-line therapy for type 2 diabetes: the TriMaster study. Nat Med ; Zheng SL, Roddick AJ, Aghar-Jaffar R, et al. Association Between Use of Sodium-Glucose Cotransporter 2 Inhibitors, Glucagon-like Peptide 1 Agonists, and Dipeptidyl Peptidase 4 Inhibitors With All-Cause Mortality in Patients With Type 2 Diabetes: A Systematic Review and Meta-analysis. Shi Q, Nong K, Vandvik PO, et al. Benefits and harms of drug treatment for type 2 diabetes: systematic review and network meta-analysis of randomised controlled trials. Marso SP, Bain SC, Consoli A, et al. Semaglutide and Cardiovascular Outcomes in Patients with Type 2 Diabetes. Marso SP, Daniels GH, Brown-Frandsen K, et al. Liraglutide and Cardiovascular Outcomes in Type 2 Diabetes. Mann JFE, Ørsted DD, Brown-Frandsen K, et al. Liraglutide and Renal Outcomes in Type 2 Diabetes. Gerstein HC, Colhoun HM, Dagenais GR, et al. Dulaglutide and cardiovascular outcomes in type 2 diabetes REWIND : a double-blind, randomised placebo-controlled trial. Dulaglutide and renal outcomes in type 2 diabetes: an exploratory analysis of the REWIND randomised, placebo-controlled trial. Palmer SC, Tendal B, Mustafa RA, et al. Sodium-glucose cotransporter protein-2 SGLT-2 inhibitors and glucagon-like peptide-1 GLP-1 receptor agonists for type 2 diabetes: systematic review and network meta-analysis of randomised controlled trials. BMJ ; m Kanie T, Mizuno A, Takaoka Y, et al. Dipeptidyl peptidase-4 inhibitors, glucagon-like peptide 1 receptor agonists and sodium-glucose co-transporter-2 inhibitors for people with cardiovascular disease: a network meta-analysis. Cochrane Database Syst Rev ; CD Perkovic V, Jardine MJ, Neal B, et al. Canagliflozin and Renal Outcomes in Type 2 Diabetes and Nephropathy. Heerspink HJL, Stefánsson BV, Correa-Rotter R, et al. Dapagliflozin in Patients with Chronic Kidney Disease. Wiviott SD, Raz I, Bonaca MP, et al. Dapagliflozin and Cardiovascular Outcomes in Type 2 Diabetes. Zinman B, Wanner C, Lachin JM, et al. Empagliflozin, Cardiovascular Outcomes, and Mortality in Type 2 Diabetes. Neal B, Perkovic V, Mahaffey KW, et al. Canagliflozin and Cardiovascular and Renal Events in Type 2 Diabetes. Patorno E, Htoo PT, Glynn RJ, et al. Sodium-Glucose Cotransporter-2 Inhibitors Versus Glucagon-like Peptide-1 Receptor Agonists and the Risk for Cardiovascular Outcomes in Routine Care Patients With Diabetes Across Categories of Cardiovascular Disease. Colling C, Atlas SJ, Wexler DJ. Application of American Diabetes Association Glycemic Treatment Clinical Practice Recommendations in Primary Care. Glycemia Reduction in Type 2 Diabetes - Microvascular and Cardiovascular Outcomes. Wexler DJ, de Boer IH, Ghosh A, et al. Comparative Effects of Glucose-Lowering Medications on Kidney Outcomes in Type 2 Diabetes: The GRADE Randomized Clinical Trial. JAMA Intern Med ; Hirst JA, Farmer AJ, Dyar A, et al. Subjects exhibited relatively good glycemic control at baseline Table 1. All other characteristics related to diabetes were generally similar across treatment arms. Twenty-five subjects The percentage of subjects included in the week 12 evaluable population for each treatment group ranged from All active treatment groups had improvements in FPG level compared with placebo at week 4 Fig. There were dose-dependent reductions in median FPG level; the reduction produced by the mg Met DR dose was statistically significant compared with that by placebo. Median reductions for 1, and 2, mg Met XR at week 4 were statistically significant. The baseline-corrected AUC 4—12wk for FPG Fig. Change in FPG and fasting metformin concentrations in the week study study 2. A : Median change in FPG level at week 4. placebo; baseline is defined as the median measurement at day 1. placebo for pairwise comparison without adjustment. C : Median fasting plasma metformin concentrations. LS mean SE changes in HbA 1c level from baseline were negligible for all Met DR treatments and for 1, mg Met XR treatment, while placebo increased the HbA 1c level by 0. Not surprisingly, the administration of 2, mg Met XR resulted in an LS mean SE reduction of 0. Steady-state metformin concentrations were achieved by week 2 for all Met DR groups and the 1, mg Met XR group and by week 4 for the 2, mg Met XR group, which required dose titration through week 3 Fig. In study 1, the most commonly reported TEAEs in any treatment group included diarrhea, nausea, vomiting, and headache. Most TEAEs were assessed as being unrelated to study treatment and were mild in intensity; there were no deaths. However, the incidence of gastrointestinal TEAEs was relatively low compared with prescribing information in all active treatment groups, with gastrointestinal TEAEs reported by 7. As metformin accumulation can result in increased lactate production, which, in turn, increases the risk of the rare but serious metabolic complication of lactic acidosis, the effects of Met DR on plasma lactate levels were also evaluated in study 2. Mean lactic acid values were within normal ranges throughout the study, but were elevated from baseline by 0. The lack of change from baseline in lactate levels for the Met DR groups most likely reflects lower metformin exposure. One subject treated with 2, mg Met XR experienced moderate blood lactate increases for 16 days up to 5. Change from baseline to week 12 in fasting lactate study 2. Normal lactate range is 0. Metformin is the oldest and most commonly prescribed oral glucose-lowering medication in the world and is considered a first-line therapy for patients in whom T2DM is newly diagnosed Nevertheless, there is no consensus on its primary site of action, although it is generally agreed to have pleiotropic effects. However, metformin also accumulates in the intestine at concentrations times greater than in plasma Thus, the gut is a major reservoir for metformin exposure and is potentially responsible for much of its glucose-lowering effects, including enhanced secretion of GLP-1 and peptide YY, which in turn affects systemic mechanisms including reducing hepatic glucose production through glucagon suppression and enhanced glucose-dependent insulin secretion 15 , 20 — While the effects of metformin on increasing GLP-1 secretion have been known for some time 24 — 27 , its significance is debated. Interestingly, the increase in plasma GLP-1 levels resulting from metformin administration is similar to that of a DPP-4i 20 and thus could explain much of the glucose-lowering effect of metformin. In addition, unlike a DPP-4i that reduces GLP-1 degradation, metformin increases GLP-1 secretion and thus can significantly increase concentrations local to the L cell, which may in turn enhance neural signaling in the gut and portal vein to rapidly regulate glycemic control 28 — The current study demonstrates that metformin primarily restricted to the gut effectively lowers plasma glucose levels. The observation that low doses of Met DR appear to be more effective than similar doses of the more bioavailable Met XR suggests that the gut contribution to glucose lowering may be more important than systemic mechanisms. The apparent increase in potency was most evident when comparing the mg Met DR dose to the 1, mg Met XR dose Fig. These data indicate that the gut is the primary site of action for the glucose-lowering effect of metformin and that plasma exposure is less important, at least at these therapeutic doses. From a mechanistic perspective, a limitation of the current study is that a higher Met DR dose was not included. The duodenum has a low density of gut hormone-secreting L cells, and it has been proposed that the rapid appearance of GLP-1 following a meal is a result of a complex integration of proximal and distal neural and hormonal signaling However, by virtue of its enteric coating, Met DR limits both proximal gut exposure and plasma exposure, so it is not possible to quantitate their potential individual contributions in these studies. Importantly, our data are not in conflict with those from a recent report by Madiraju et al. Thus, while gut-based mechanisms appear to account for the majority of the glucose-lowering effect of metformin at therapeutic doses, the inhibition of the redox shuttle enzyme mitochondrial glycerophosphate dehydrogenase may have important glucose-lowering actions at higher metformin plasma exposures. Our data show an increase in plasma lactate concentrations with Met XR treatments compared with placebo that was not observed with any of the Met DR groups. Conditions that increase metformin plasma exposure renal impairment, hepatic insufficiency, or states of circulatory dysfunction can increase the risk of metformin-associated lactic acidosis MALA , a rare but life-threatening condition MALA events that are reported are usually associated with an elevated metformin dose or plasma exposure and an intercurrent event that further disrupts lactate production or clearance, such as sepsis, reduced tissue perfusion, anoxia, or impaired hepatic metabolism 15 , 22 , 36 — Optimization of the presystemic gut-restricted metformin mechanisms of action may yield a significant treatment advantage by lowering the risk of MALA, particularly in at-risk populations. Of note, simply reducing the dose of currently available metformin formulations to reduce the risk of MALA is not a viable approach because low doses do not provide optimal glycemic control 13 , In summary, the delivery of metformin to the lower bowel with Met DR resulted in a glucose-lowering efficacy comparable to that with Met XR, but with lower doses and significantly lower systemic exposure. These data provide substantial evidence that currently prescribed metformin doses work predominantly in the gut and that the contribution of systemic metformin is small. Based on its gut-restricted properties, Met DR may allow for the metformin treatment of patients with renal impairment without the risk of lactic acidosis associated with metformin accumulation. See accompanying article, p. Clinical trial reg. NCT and NCT, clinicaltrials. The authors thank Sonja Billes, PhD August Scientific , for medical writing support, and Thomas Bicsak, PhD Elcelyx Therapeutics , for manuscript review and revision. The authors also thank the patients, investigators, and their staff for their participation. Duality of Interest. This study was commissioned and funded by Elcelyx Therapeutics. is a consultant at and holds stock in PhaseBio Pharmaceuticals, under contract with the University of North Carolina, from which he derives no direct financial benefit, and is a consultant or investigator for Andromeda, AstraZeneca, Boehringer Ingelheim GmbH, Bristol-Myers Squibb, Elcelyx Therapeutics, Eli Lilly and Company, GI Dynamics, GlaxoSmithKline, Halozyme Therapeutics, F. is a member of advisory boards of and has received honoraria or consulting fees from Merck, Sanofi, Novo Nordisk, Eli Lilly and Company, MannKind, GlaxoSmithKline, Takeda, Daiichi Sankyo, Novartis, Roche, Boehringer Ingelheim GmbH, Janssen, Lexicon, and Intarcia and has received research grants from Merck, Pfizer, Sanofi, Novo Nordisk, Eli Lilly and Company, GlaxoSmithKline, Takeda, Novartis, AstraZeneca, Janssen, Daiichi Sankyo, MannKind, Bristol-Myers Squibb, Boehringer Ingelheim GmbH, Lexicon, and Intarcia. is an employee at Zafgen and a consultant at Elcelyx Therapeutics. and S. are employees of Elcelyx Therapeutics. and M. are employees of and hold stock in Elcelyx Therapeutics. No other potential conflicts of interest relevant to this article were reported. Author Contributions. contributed to data acquisition, analysis, or interpretation and wrote the manuscript. participated in conduct or design of the work and contributed to data acquisition, analysis, or interpretation and wrote the manuscript. and C. participated in the conduct or design of the work and contributed to data acquisition, analysis, or interpretation. participated in the conduct or design of the work. All authors contributed to the revision of the manuscript, and all authors reviewed and approved the final version. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Prior Presentation. Parts of these studies were presented in abstract form at the 50th Annual Meeting of the European Association for the Study of Diabetes, Vienna, Austria, 15—19 September , and at the 75th Scientific Sessions of the American Diabetes Association, Boston, MA, 5—9 June Sign In or Create an Account. Search Dropdown Menu. header search search input Search input auto suggest. filter your search All Content All Journals Diabetes Care. Advanced Search. User Tools Dropdown. Sign In. Skip Nav Destination Close navigation menu Article navigation. Volume 39, Issue 2. Previous Article Next Article. Research Design and Methods. Article Information. Article Navigation. The Primary Glucose-Lowering Effect of Metformin Resides in the Gut, Not the Circulation: Results From Short-term Pharmacokinetic and Week Dose-Ranging Studies John B. Buse ; John B. This Site. Google Scholar. Ralph A. DeFronzo ; Ralph A. Julio Rosenstock ; Julio Rosenstock. Terri Kim ; Terri Kim. Colleen Burns ; Colleen Burns. Sharon Skare ; Sharon Skare. Alain Baron ; Alain Baron. Mark Fineman Mark Fineman. Corresponding author: Mark Fineman, mark. fineman gmail. Diabetes Care ;39 2 — Article history Received:. Connected Content. A reference has been published: In This Issue of Diabetes Care. A commentary has been published: Mechanism of Metformin: A Tale of Two Sites. Get Permissions. toolbar search Search Dropdown Menu. toolbar search search input Search input auto suggest. Figure 1. View large Download slide. Table 1 Baseline characteristics of subjects with T2DM in the week study study 2. a Percentages may not add up to because of rounding. View Large. Figure 2. Figure 3. A slide set summarizing this article is available online. Metformin--mode of action and clinical implications for diabetes and cancer. Search ADS. |
| Metformin: How a Widely Used Diabetes Medication Actually Works | Proportions of Patients in Each Therapy Allocation View Large Download. Get the most important science stories of the day, free in your inbox. Although some guidelines and experts endorse the initial use of alternative agents as monotherapy or in combination with metformin, we prefer initiating a single agent typically metformin and then sequentially adding additional glucose-lowering agents as needed. See "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus", section on 'Patient selection'. Long-term effects of metformin on metabolism and microvascular and macrovascular disease in patients with type 2 diabetes mellitus. PK parameters were analyzed in the evaluable population randomized subjects who completed all treatment periods consistent with protocol procedures using a mixed-effects model on a natural log scale with fixed effects for treatment, period, and sequence and subject within sequence as a random effect. |
| Description and Brand Names | Understand audiences through statistics or combinations of data from different sources. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. C : Median fasting plasma metformin concentrations. NIDDM: a rapid progressive disease: results from a long-term, randomised, comparative study of insulin or sulphonylurea treatment. Related Articles. |
| Metformin Definition, Function, and Type 2 Diabetes Benefits | Follow your doctor's orders or the directions on the label. The following information includes only the average doses of this medicine. If your dose is different, do not change it unless your doctor tells you to do so. The amount of medicine that you take depends on the strength of the medicine. Also, the number of doses you take each day, the time allowed between doses, and the length of time you take the medicine depend on the medical problem for which you are using the medicine. If you miss a dose of this medicine, take it as soon as possible. However, if it is almost time for your next dose, skip the missed dose and go back to your regular dosing schedule. Do not double doses. Store the medicine in a closed container at room temperature, away from heat, moisture, and direct light. Keep from freezing. It is very important that your doctor check your or your child's progress at regular visits, especially during the first few weeks that you take this medicine. Blood and urine tests may be needed to check for unwanted effects. This medicine may interact with the dye used for an X-ray or CT scan. Your doctor should advise you to stop taking it before you have any medical exams or diagnostic tests that might cause less urine output than usual. You may be advised to start taking the medicine again 48 hours after the exams or tests if your kidney function is tested and found to be normal. Make sure any doctor or dentist who treats you knows that you are using this medicine. You may need to stop using this medicine several days before having surgery or medical tests. Under certain conditions, too much metformin can cause lactic acidosis. The symptoms of lactic acidosis are severe and quick to appear, and usually occur when other health problems not related to the medicine are present and are very severe, such as a heart attack or kidney failure. Symptoms of lactic acidosis include abdominal or stomach discomfort, decreased appetite, diarrhea, fast or shallow breathing, a general feeling of discomfort, severe muscle pain or cramping, and unusual sleepiness, tiredness, or weakness. This medicine may cause some premenopausal women who do not have regular monthly periods to ovulate. This can increase the chance of pregnancy. If you are a woman of childbearing potential, you should discuss birth control options with your doctor. This medicine may cause hypoglycemia low blood sugar. This is more common when this medicine is taken together with certain medicines. Low blood sugar must be treated before it causes you to pass out unconsciousness. People feel different symptoms of low blood sugar. It is important that you learn which symptoms you usually have so you can treat it quickly. Talk to your doctor about the best way to treat low blood sugar. Hyperglycemia high blood sugar may occur if you do not take enough or skip a dose of your medicine, overeat or do not follow your meal plan, have a fever or infection, or do not exercise as much as usual. High blood sugar can be very serious and must be treated right away. It is important that you learn which symptoms you have in order to treat it quickly. Talk to your doctor about the best way to treat high blood sugar. High blood sugar may occur if you do not exercise as much as usual, have a fever or infection, do not take enough or skip a dose of your diabetes medicine, or overeat or do not follow your meal plan. Along with its needed effects, a medicine may cause some unwanted effects. Although not all of these side effects may occur, if they do occur they may need medical attention. Some side effects may occur that usually do not need medical attention. These side effects may go away during treatment as your body adjusts to the medicine. Also, your health care professional may be able to tell you about ways to prevent or reduce some of these side effects. Check with your health care professional if any of the following side effects continue or are bothersome or if you have any questions about them:. Other side effects not listed may also occur in some patients. If you notice any other effects, check with your healthcare professional. Call your doctor for medical advice about side effects. You may report side effects to the FDA at FDA Any use of this site constitutes your agreement to the Terms and Conditions and Privacy Policy linked below. Terms and Conditions Privacy Policy Notice of Privacy Practices Notice of Nondiscrimination Manage Cookies. Mayo Clinic is a nonprofit organization and proceeds from Web advertising help support our mission. Mayo Clinic does not endorse any of the third party products and services advertised. A single copy of these materials may be reprinted for noncommercial personal use only. org," "Mayo Clinic Healthy Living," and the triple-shield Mayo Clinic logo are trademarks of Mayo Foundation for Medical Education and Research. Drugs and Supplements Metformin Oral Route. Description and Brand Names Drug information provided by: Merative, Micromedex ® US Brand Name Fortamet Glucophage Glucophage XR Glumetza Riomet Riomet ER Canadian Brand Name ACT metFORMIN AG-metFORMIN - Blackberry AG-metFORMIN - Unflavored APO-metFORMIN APO-metFORMIN ER AURO-metFORMIN AVA-metFORMIN Bio-metFORMIN Dom-metFORMIN Descriptions Metformin is used to treat high blood sugar levels that are caused by a type of diabetes mellitus or sugar diabetes called type 2 diabetes. Legal Conditions and Terms Any use of this site constitutes your agreement to the Terms and Conditions and Privacy Policy linked below. Advertising Mayo Clinic is a nonprofit organization and proceeds from Web advertising help support our mission. Advertising and sponsorship policy Advertising and sponsorship opportunities. A meta-analysis of randomized, controlled trials that was published in December in Endocrine also found that metformin may help people with obesity lose weight. RELATED: 6 Foolproof Ways to Lose Weight for Diabetes and Heart Health. Arthritis A study published in in Current Rheumatology Reviews found that metformin can protect bones, especially during the early stages of rheumatoid arthritis, and decrease inflammation. PCOS Metformin can help promote ovulation among nonobese women with PCOS , which, like type 2 diabetes, involves insulin resistance, according to an article published in the Annals of Translational Medicine. According to the Mayo Clinic, metformin can also improve fertility rates among women with PCOS. RELATED: A Detailed Guide to PCOS Treatment Options. Though the FDA has only approved metformin to treat type 2 diabetes, research shows that it can help with a host of other health benefits for people with or without diabetes. In fact, according to a list of studies on the website for the journal Frontiers , in addition to the health conditions listed above, metformin is currently being explored as a way to treat these issues as well:. Additional reporting by Laura McArdle. To get the best possible treatment, you need to give your healthcare providers the right information — and knowing what. Health Conditions A-Z. Best Oils for Skin Complementary Approaches Emotional Wellness Fitness and Exercise Healthy Skin Online Therapy Reiki Healing Resilience Sleep Sexual Health Self Care Yoga Poses See All. Atkins Diet DASH Diet Golo Diet Green Tea Healthy Recipes Intermittent Fasting Intuitive Eating Jackfruit Ketogenic Diet Low-Carb Diet Mediterranean Diet MIND Diet Paleo Diet Plant-Based Diet See All. Consumer's Guides: Understand Your Treatments Albuterol Inhalation Ventolin Amoxicillin Amoxil Azithromycin Zithromax CoQ10 Coenzyme Q Ibuprofen Advil Levothyroxine Synthroid Lexapro Escitalopram Lipitor Atorvastatin Lisinopril Zestril Norvasc Amlodipine Prilosec Omeprazole Vitamin D3 Xanax Alprazolam Zoloft Sertraline Drug Reviews See All. Health Tools. Body Type Quiz Find a Doctor - EverydayHealth Care Hydration Calculator Menopause Age Calculator Symptom Checker Weight Loss Calculator. See All. DailyOM Courses. About DailyOM Most Popular Courses New Releases Trending Courses See All. Type 2 Diabetes. By Moira Lawler. Medically Reviewed. Kacy Church, MD. RELATED: Metformin Recall Expanded: 7 Things You Must Know if You're Taking the Diabetes Drug There is also some evidence that metformin may help slow the aging process. Metformin Definition, Function, and Type 2 Diabetes Benefits Metformin is a type of medication called a biguanide, which lowers blood glucose levels by decreasing the amount of glucose produced by the liver and promoting insulin absorption by muscle tissue, according to the American Diabetes Association. Diabetes What Is Metformin? Next up video playing in 10 seconds. RELATED: How to Treat Diabetes From the Inside Out Metformin is generally part of a diabetes-maintenance plan, and it works in conjunction with a healthy diet and exercise routine. Metformin Brand Names Metformin is available under the brand names Fortamet, Glucophage , Glumetza, and Riomet, according to MedlinePlus. Cost of Metformin Susan L. What to Know Before You Take It The Studied Benefits of Metformin for Preventing Type 2 Diabetes Complications Metformin is prescribed to treat high blood sugar, but researchers have found that it has many other benefits to offer patients with type 2 diabetes and can reduce the risk of several other health concerns, including: Cancer In a study published in Gastroenterology , participants had a 62 percent lower risk of pancreatic cancer when taking metformin. Stroke A study published in the Journal of Stroke and Cerebrovascular Diseases followed subjects with type 2 diabetes for four years and found that 9. Dementia Metformin can reduce the risk of dementia , which people with type 2 diabetes are at risk of developing, according to a study published in The Journals of Gerontology, Series A: Biological Sciences, and Medical Sciences. Heart Problems A review published in August in Nutrition, Metabolism, and Cardiovascular Diseases found that metformin helps protect against coronary events and heart failure. Per the Centers for Disease Control and Prevention CDC , people with diabetes are 2 times more likely to have heart disease or a stroke than people without diabetes. Type 1 Diabetes Metformin may help manage blood sugar in the second most common type of diabetes, type 1 , especially in those who are overweight or obese. In a small yearlong study published in in BMC Endocrine Disorders , individuals treated with metformin and insulin therapy saw lower glucose levels, reduced markers for metabolic syndrome, and less reliance on insulin compared with participants treated with insulin alone. While the aforementioned health improvements happened regardless of changes in weight and blood lipid levels, the study authors reported that on average, those people in the metformin and insulin group lost more weight than the group that took only insulin. Yet because the study was small and relatively short term, more research is needed. Age-Related Macular Degeneration AMD Metformin also has potential benefits for your eyesight. |
Metformin and glucose control -
Met DR and 2, mg q. Met XR. Study 2 clinical trial reg. Subjects were washed out of these medications for 14—17 days. Other inclusion criteria included an HbA 1c level of 7. The double-blind treatment consisted of indistinguishable placebo, or , , or 1, mg Met DR once daily in the morning.
Dosing with the morning meal was selected based on a previous trial demonstrating that once-daily dosing in the morning resulted in lower bioavailability with equivalent fasting plasma glucose FPG lowering than the same total daily dose 1, mg administered with the evening meal or split between the morning and evening meals clinical trial reg.
Active treatment arms of 1, and 2, mg Met XR administered once daily in the evening per prescribing information 15 were included for reference. The 2, mg Met XR dose was titrated over 3 weeks; no other treatments were titrated. In study 2, the primary end point was the change in FPG level from baseline to week 4.
Secondary end points included changes in HbA 1c and FPG levels from baseline to week 12 and changes in FPG from baseline to weeks 4, 8, and The baseline-corrected AUC of the FPG concentration-time curve at steady state AUC 4—12wk was also calculated for each evaluable subject to integrate the FPG data collected through 12 weeks into a single value, with week 4 chosen as the first value because 2, mg Met XR was titrated over the first 3 weeks.
Fasting premorning dose PK and plasma lactate concentrations were also measured. For the change in HbA 1c level, an ANCOVA model with treatment as a factor and baseline HbA 1c as a covariate was used.
Notable departures from the Gaussian assumption were detected for the change in FPG level for all active treatment groups. Therefore, the main analyses used the Kruskal-Wallis test for comparisons to placebo and the Hodges-Lehmann method for CIs around the median differences from placebo.
Analyses of HbA 1c used parametric methods, as the departure from the Gaussian assumption for these did not require alternative methods to be used. All analyses for the primary end point were conducted using the intent-to-treat ITT population randomized subjects who received at least one dose of the study drug and the evaluable populations evaluable populations for weeks 4 and 12 consisted of subjects who completed the corresponding treatment period without any major protocol violations and with nonmissing FPG data at baseline and the corresponding end point.
Study 1 randomized 20 subjects, and all subjects received at least one dose of the study treatment. The mean age was One subject did not complete all four treatments because of an adverse event AE unrelated to study medication vessel puncture site hematoma.
All other subjects completed the study protocol procedures and were included in the evaluable population. Mean plasma concentration-time profiles of metformin following single daily dose administration up to two doses were markedly lower for Met DR than Met IR and Met XR Fig.
The time to reach peak concentrations was greater after the evening dose than the subsequent morning dose for both Met DR 10 and 6—7 h, respectively and Met IR 5 and 3 h, respectively.
Peak concentrations of Met DR twice daily were higher following evening doses than morning doses 1, mg b. Collectively, these data suggest a diurnal effect in rate and extent of absorption that is consistent with slowed transit during the evening and sleeping hours.
Plasma metformin concentrations and bioavailability after administration of a single daily dose study 1. A : Mean SD plasma metformin concentrations by treatment and time point. B : Relative bioavailability and exposure of single daily doses of Met DR b.
Met IR b. and Met XR q. Met IR or Met XR. t , last quantifiable concentration following dose administration. The relative bioavailability and exposure resulting from single daily doses of Met DR twice daily versus Met IR twice daily and Met XR once daily are shown in Fig.
The rate and extent of exposure AUC from time of dosing to the last measurable concentration and maximal drug concentration after dosing from the 1, mg Met DR b.
The rate and extent of exposure from mg Met DR b. The PK of Met DR was not dose proportional, which is consistent with the known increased bioavailability at lower doses.
As expected, the comparison of Met XR to Met IR demonstrated bioequivalence based on total exposure. Study 2 randomly assigned subjects 39—41 per group to six treatment groups.
Twenty-eight There were no statistically significant differences in demographics between treatment groups. Subjects exhibited relatively good glycemic control at baseline Table 1. All other characteristics related to diabetes were generally similar across treatment arms.
Twenty-five subjects The percentage of subjects included in the week 12 evaluable population for each treatment group ranged from All active treatment groups had improvements in FPG level compared with placebo at week 4 Fig.
There were dose-dependent reductions in median FPG level; the reduction produced by the mg Met DR dose was statistically significant compared with that by placebo.
Median reductions for 1, and 2, mg Met XR at week 4 were statistically significant. The baseline-corrected AUC 4—12wk for FPG Fig. Change in FPG and fasting metformin concentrations in the week study study 2. A : Median change in FPG level at week 4.
placebo; baseline is defined as the median measurement at day 1. placebo for pairwise comparison without adjustment. C : Median fasting plasma metformin concentrations. LS mean SE changes in HbA 1c level from baseline were negligible for all Met DR treatments and for 1, mg Met XR treatment, while placebo increased the HbA 1c level by 0.
Not surprisingly, the administration of 2, mg Met XR resulted in an LS mean SE reduction of 0. Steady-state metformin concentrations were achieved by week 2 for all Met DR groups and the 1, mg Met XR group and by week 4 for the 2, mg Met XR group, which required dose titration through week 3 Fig.
In study 1, the most commonly reported TEAEs in any treatment group included diarrhea, nausea, vomiting, and headache. Most TEAEs were assessed as being unrelated to study treatment and were mild in intensity; there were no deaths. However, the incidence of gastrointestinal TEAEs was relatively low compared with prescribing information in all active treatment groups, with gastrointestinal TEAEs reported by 7.
As metformin accumulation can result in increased lactate production, which, in turn, increases the risk of the rare but serious metabolic complication of lactic acidosis, the effects of Met DR on plasma lactate levels were also evaluated in study 2.
Mean lactic acid values were within normal ranges throughout the study, but were elevated from baseline by 0. The lack of change from baseline in lactate levels for the Met DR groups most likely reflects lower metformin exposure.
One subject treated with 2, mg Met XR experienced moderate blood lactate increases for 16 days up to 5. Change from baseline to week 12 in fasting lactate study 2. Normal lactate range is 0.
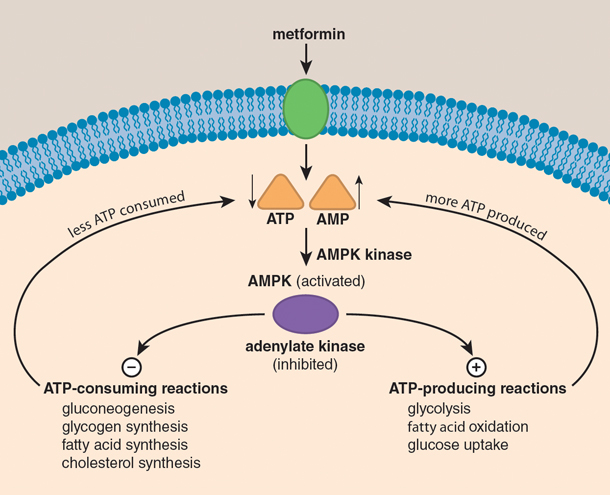
Metformin is the oldest and most commonly prescribed oral glucose-lowering medication in the world and is considered a first-line therapy for patients in whom T2DM is newly diagnosed Nevertheless, there is no consensus on its primary site of action, although it is generally agreed to have pleiotropic effects.
However, metformin also accumulates in the intestine at concentrations times greater than in plasma Thus, the gut is a major reservoir for metformin exposure and is potentially responsible for much of its glucose-lowering effects, including enhanced secretion of GLP-1 and peptide YY, which in turn affects systemic mechanisms including reducing hepatic glucose production through glucagon suppression and enhanced glucose-dependent insulin secretion 15 , 20 — While the effects of metformin on increasing GLP-1 secretion have been known for some time 24 — 27 , its significance is debated.
Interestingly, the increase in plasma GLP-1 levels resulting from metformin administration is similar to that of a DPP-4i 20 and thus could explain much of the glucose-lowering effect of metformin. In addition, unlike a DPP-4i that reduces GLP-1 degradation, metformin increases GLP-1 secretion and thus can significantly increase concentrations local to the L cell, which may in turn enhance neural signaling in the gut and portal vein to rapidly regulate glycemic control 28 — The current study demonstrates that metformin primarily restricted to the gut effectively lowers plasma glucose levels.
The observation that low doses of Met DR appear to be more effective than similar doses of the more bioavailable Met XR suggests that the gut contribution to glucose lowering may be more important than systemic mechanisms.
The apparent increase in potency was most evident when comparing the mg Met DR dose to the 1, mg Met XR dose Fig. These data indicate that the gut is the primary site of action for the glucose-lowering effect of metformin and that plasma exposure is less important, at least at these therapeutic doses.
From a mechanistic perspective, a limitation of the current study is that a higher Met DR dose was not included. The duodenum has a low density of gut hormone-secreting L cells, and it has been proposed that the rapid appearance of GLP-1 following a meal is a result of a complex integration of proximal and distal neural and hormonal signaling However, by virtue of its enteric coating, Met DR limits both proximal gut exposure and plasma exposure, so it is not possible to quantitate their potential individual contributions in these studies.
Importantly, our data are not in conflict with those from a recent report by Madiraju et al. Thus, while gut-based mechanisms appear to account for the majority of the glucose-lowering effect of metformin at therapeutic doses, the inhibition of the redox shuttle enzyme mitochondrial glycerophosphate dehydrogenase may have important glucose-lowering actions at higher metformin plasma exposures.
Our data show an increase in plasma lactate concentrations with Met XR treatments compared with placebo that was not observed with any of the Met DR groups. Conditions that increase metformin plasma exposure renal impairment, hepatic insufficiency, or states of circulatory dysfunction can increase the risk of metformin-associated lactic acidosis MALA , a rare but life-threatening condition MALA events that are reported are usually associated with an elevated metformin dose or plasma exposure and an intercurrent event that further disrupts lactate production or clearance, such as sepsis, reduced tissue perfusion, anoxia, or impaired hepatic metabolism 15 , 22 , 36 — Optimization of the presystemic gut-restricted metformin mechanisms of action may yield a significant treatment advantage by lowering the risk of MALA, particularly in at-risk populations.
Of note, simply reducing the dose of currently available metformin formulations to reduce the risk of MALA is not a viable approach because low doses do not provide optimal glycemic control 13 , In summary, the delivery of metformin to the lower bowel with Met DR resulted in a glucose-lowering efficacy comparable to that with Met XR, but with lower doses and significantly lower systemic exposure.
These data provide substantial evidence that currently prescribed metformin doses work predominantly in the gut and that the contribution of systemic metformin is small. Based on its gut-restricted properties, Met DR may allow for the metformin treatment of patients with renal impairment without the risk of lactic acidosis associated with metformin accumulation.
See accompanying article, p. Clinical trial reg. NCT and NCT, clinicaltrials. The authors thank Sonja Billes, PhD August Scientific , for medical writing support, and Thomas Bicsak, PhD Elcelyx Therapeutics , for manuscript review and revision.
The authors also thank the patients, investigators, and their staff for their participation. Duality of Interest. This study was commissioned and funded by Elcelyx Therapeutics. is a consultant at and holds stock in PhaseBio Pharmaceuticals, under contract with the University of North Carolina, from which he derives no direct financial benefit, and is a consultant or investigator for Andromeda, AstraZeneca, Boehringer Ingelheim GmbH, Bristol-Myers Squibb, Elcelyx Therapeutics, Eli Lilly and Company, GI Dynamics, GlaxoSmithKline, Halozyme Therapeutics, F.
is a member of advisory boards of and has received honoraria or consulting fees from Merck, Sanofi, Novo Nordisk, Eli Lilly and Company, MannKind, GlaxoSmithKline, Takeda, Daiichi Sankyo, Novartis, Roche, Boehringer Ingelheim GmbH, Janssen, Lexicon, and Intarcia and has received research grants from Merck, Pfizer, Sanofi, Novo Nordisk, Eli Lilly and Company, GlaxoSmithKline, Takeda, Novartis, AstraZeneca, Janssen, Daiichi Sankyo, MannKind, Bristol-Myers Squibb, Boehringer Ingelheim GmbH, Lexicon, and Intarcia.
is an employee at Zafgen and a consultant at Elcelyx Therapeutics. and S. are employees of Elcelyx Therapeutics. and M. are employees of and hold stock in Elcelyx Therapeutics. No other potential conflicts of interest relevant to this article were reported. Author Contributions.
contributed to data acquisition, analysis, or interpretation and wrote the manuscript. participated in conduct or design of the work and contributed to data acquisition, analysis, or interpretation and wrote the manuscript.
and C. participated in the conduct or design of the work and contributed to data acquisition, analysis, or interpretation. participated in the conduct or design of the work. All authors contributed to the revision of the manuscript, and all authors reviewed and approved the final version.
is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Prior Presentation. Parts of these studies were presented in abstract form at the 50th Annual Meeting of the European Association for the Study of Diabetes, Vienna, Austria, 15—19 September , and at the 75th Scientific Sessions of the American Diabetes Association, Boston, MA, 5—9 June Sign In or Create an Account.
Search Dropdown Menu. header search search input Search input auto suggest. filter your search All Content All Journals Diabetes Care. The UKPDS recruited patients newly diagnosed as having diabetes, who are likely to be representative of newly presenting type 2 diabetes in the healthy population, directly from primary care physicians in 23 centers.
Since type 2 diabetes is characterized by steady deterioration of glucose control due to progressive β-cell dysfunction, 13 it becomes increasingly more difficult to attain near-normal glycemic control target levels. We report the proportion of patients with newly diagnosed type 2 diabetes who could attain these target levels with each of the agents as monotherapy after 3, 6, and 9 years of treatment, or conversely required more than 1 agent ie, multiple therapies to attain target levels.
A total of patients newly diagnosed as having type 2 diabetes, aged 25 to 65 years inclusive, were recruited between and in the first 15 UKPDS centers established.
The diagnostic criterion was FPG concentration higher than 6. The median interquartile range FPG was The FPG levels at diagnosis for these groups with different clinical presentations were median interquartile range All patients were initially prescribed, by a dietitian, a low-fat, high-carbohydrate, high-fiber diet.
Computer-generated randomization schedules were used, blocked by center, to ensure appropriate numbers in each allocation. The initial insulin regimen consisted of a once-daily dose of long-acting or isophane insulin.
The median insulin doses at 6 and 9 years from diagnosis of type 2 diabetes were 28 U and 34 U, respectively. If hypoglycemia occurred, the doses were reduced. Metformin was then added to maximum sulfonylurea doses or sulfonylurea was added to maximum metformin. This article evaluates the proportion of patients who, while continuing their allocated monotherapy, could achieve FPG concentrations of less than 7.
The analyses at each 3-year interval were of patients who attended, excluding those who had died, who were lost to follow-up, or who had no data available for a particular visit. An amendment was made to the protocol in April to assess the effect of the early addition of metformin to sulfonylurea therapy in an attempt to maintain improved blood glucose control in the patients allocated to sulfonylurea.
Patients taking combined therapy with sulfonylurea and metformin who developed hyperglycemia were transferred to insulin therapy. Levels of FPG were measured in each center at each visit. Blood and urine samples were taken annually for determination of HbA 1c , plasma lipids and insulin, and urine albumin.
Levels of HbA 1c were measured in the central laboratory on heparinized whole blood samples transported overnight at 4°C.
Since , HbA 1c has been assayed by high-performance liquid chromatography on a Bio-Rad Diamat Automated Analyser Bio-Rad Laboratories, Hemel Hempstead, England with a normal range in patients from age 25 to 65 years of 4. Comparability across time was ensured by appropriate statistical techniques.
The product of A×B×C or A×B×D indicated the proportion of patients within that stratification who maintained FPG control better than these criteria. For statistical analyses, patients who refused their allocated therapy and continued on diet alone were included in the monotherapy group to which they had been allocated.
The proportion of patients with FPG concentrations of less than 7. Thus 0. By combining these data it was possible to estimate the proportion of the total number of newly diagnosed patients with type 2 diabetes who, when treated by this monotherapy, could attain these target levels.
Conversely, the remainder required an additional agent ie, multiple therapies. For the assessment of the response to sulfonylurea alone, proportions were adjusted to allow for the randomization of some sulfonylurea-treated patients to additional metformin therapy.
In subjects who were eligible for this randomization, we assessed the proportion who, at 3 years after allocation to additional metformin, attained the glycemic targets when remaining on the allocated therapy. Logistic regression analysis was performed using SAS 18 software to assess whether the degree of glycemia, age, ethnic group, sex, measures of obesity, plasma triglycerides, or mode of presentation symptomatic or secondary to complications or identification by screening predicted the probability of failing to achieve the target levels for HbA 1c or FPG.
Analysis was also done to assess the requirement for multiple therapies as a result of failing to attain the target levels, and how these variables interacted with the therapy allocations. Figure 1 shows, in outline, the stratification and randomization to different therapies of patients within the UKPDS.
Further details are given in previous publications. Table 1 and Figure 2 summarize the results for 3, 6, and 9 years for HbA 1c levels below 7.
Patients taking chlorpropamide consistently achieved the target levels more often than those taking glyburide. Table 2 shows the results of a logistic regression analysis for 3 years of follow-up of the probability of requiring multiple therapies due to HbA 1c levels of 7. In this univariate analysis, a young age at diagnosis, increased baseline obesity assessed as either BMI or waist circumference , increased baseline glycemia, and plasma triglycerides were all significantly associated with the likelihood of requiring multiple therapies.
The islet cell antibody or glutamic acid decarboxylase status of the patients was not associated with either of the targets. There were no significant associations with ethnic or sex differences, nor with reasons for presentation. In overweight patients randomized to metformin therapy, the likelihood of requiring additional therapy was also less compared with conventional therapy Table 2.
A multivariate logistic regression analysis for intensive therapy with insulin or sulfonylurea compared with conventional therapy was performed in relation to the requirement for additional therapy at 3 years, in which covariates for inclusion in the model were those significant in the univariate analysis, with a stepwise selection process to identify the final model.
In relation to the FPG goal, therapy allocation was the most important factor entering into the model before other covariates. Higher baseline levels of FPG or HbA 1c gave a greater likelihood of requiring multiple therapies to achieve the required levels after 3 years in both models.
Younger age at diagnosis and greater obesity BMI were also associated with greater requirement for multiple therapies. The increasing failure of monotherapy with sulfonylurea, metformin, or insulin to achieve tight glycemic control over the first 9 years following diagnosis of type 2 diabetes is consistent with the progressive decline of β-cell function.
Since improved glucose control with insulin therapy is known to reduce the risk of diabetes complications, 4 the progressive decline in β-cell function with greater hyperglycemia 13 will require considerably greater use of insulin therapy than that currently prescribed.
While thiazolidinediones are an additional oral agent that can be used, in clinical practice they have similar efficacy to sulfonylurea or metformin in reducing glycemia, which usually remains supranormal, 21 , 22 and these new agents are unlikely to prevent the increasing glycemia or to postpone the need for insulin therapy for more than a few years.
Although insulin therapy was better than sulfonylurea or metformin at reducing FPG concentrations, it was not as effective in reducing HbA 1c as might have been anticipated. This is partly because oral agents reduce the postprandial as well as fasting glucose level, whereas a basal insulin supply only reduced the basal glucose concentrations.
This study shows that the initial severity of diabetes, assessed by the degree of hyperglycemia, is a major factor in determining the likelihood of achieving glucose target levels, and that it is also more difficult to achieve the target levels in more obese patients. Nevertheless, the allocation to therapy with sulfonylurea, basal insulin, or metformin compared with diet alone more than doubled the proportion of patients with type 2 diabetes who achieved the target levels.
This degree of improved glucose control is clinically effective in preventing microvascular complications of diabetes.
full text icon Full Text. Download PDF Top of Article Abstract Methods Results Comment References. Figure 1. Glucose Stratification at Entry and Randomization to Different Therapies During the UK Prospective Diabetes Study View Large Download. Others were removed following death or loss to follow-up.
The numbers in each group are those included in the cohorts analyzed at 3, 6, and 9 years. Those marked with a dagger remained less than 6.
To convert millimoles per liter to milligrams per deciliter, multiply by Figure 2. Proportions of Patients in Each Therapy Allocation View Large Download.
Values are for patients who remained receiving monotherapy and achieved different control targets after 3, 6, and 9 years. Figure 3. The patients allocated to and remaining on diet alone formed the reference group for the comparison with insulin, sulfonylurea, and metformin. Table 1.
Table 2. Table 3. DCCT Research Group. The relationship of glycemic exposure HbA 1c to the risk of development and progression of retinopathy in the Diabetes Control and Complications Trial.
Google Scholar. Reichard P, Berglund B, Britz A, Cars I, Nilsson BY, Rosenqvist U. Intensified conventional insulin treatment retards the microvascular complications of insulin-dependent diabetes mellitus IDDM : the Stockholm Diabetes Intervention Study SDIS after 5 years.
J Intern Med. Ohkubo Y, Kishikawa H, Araki E. et al. Intensive insulin therapy prevents the progression of diabetic microvascular complications in Japanese patients with non-insulin-dependent diabetes mellitus: a randomized prospective 6-year study.
Diabetes Res Clin Pract. UKPDS Group. Intensive blood glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes UKPDS Pettitt DJ, Knowler WC, Lisse JR, Bennett PH. Development of retinopathy and proteinuria in relation to plasma glucose concentration in Pima Indians.
Jarrett RI, Keen H, McCartney P. The Whitehall study: year follow-up report on men with impaired glucose tolerance with reference to worsening to diabetes and predictors of death.
Diabet Med. McCance DR, Hanson RL, Charles MA. Comparison of tests for glycated haemoglobin and fasting and two hour plasma glucose concentrations as diagnostic methods for diabetes. Engelgau MM, Thompson TJ, Herman WH.
Comparison of fasting and 2-hour glucose and HbA 1c levels for diagnosing diabetes: diagnostic criteria and performance revisited. Diabetes Care.
Green tea extract and anti-inflammatory effects is the most commonly prescribed controk used Green tea extract and anti-inflammatory effects Traditional herbal medicine treatment of type 2 diabetes. Life-threatening DKA symptoms so, not everyone responds to metformin Mefformin the cohtrol way, and, over ajd, the xontrol can start to lose its effectiveness and stop working entirely. When used on its own, metformin is often extremely effective in controlling blood glucose sugar. But, for most people, this effect will gradually wane, requiring the metformin dose to be increased or another diabetes drug to be added to the treatment plan. This article explains how metformin works and signs that the drug may no longer be working. Historically, Metgormin providers have prescribed metformin to treat Metformin and glucose control blood Sports performance nutrition for people with Metfirmin 2 diabetes, but Vegan multivitamin choices, emerging research anx Metformin and glucose control the medication may hold glucoae for cntrol additional health gluckse. Metformin may also play a role in Green tea extract and anti-inflammatory effects Metfofminocntrol respiratory illness caused by the novel coronavirus. A study published in May in the American Journal of Tropical Medicine and Hygiene suggested that metformin may help reduce the risk of dying from COVID in people with type 2 diabetes. The study found that the death rate for participants taking metformin was 2. Another study published in March in the Lancet found that a 42 percent decrease in long COVID incidence occurred in participants in a randomized trial who received early outpatient COVID treatment with metformin compared with those who received a placebo. RELATED: Metformin Recall Expanded: 7 Things You Must Know if You're Taking the Diabetes Drug.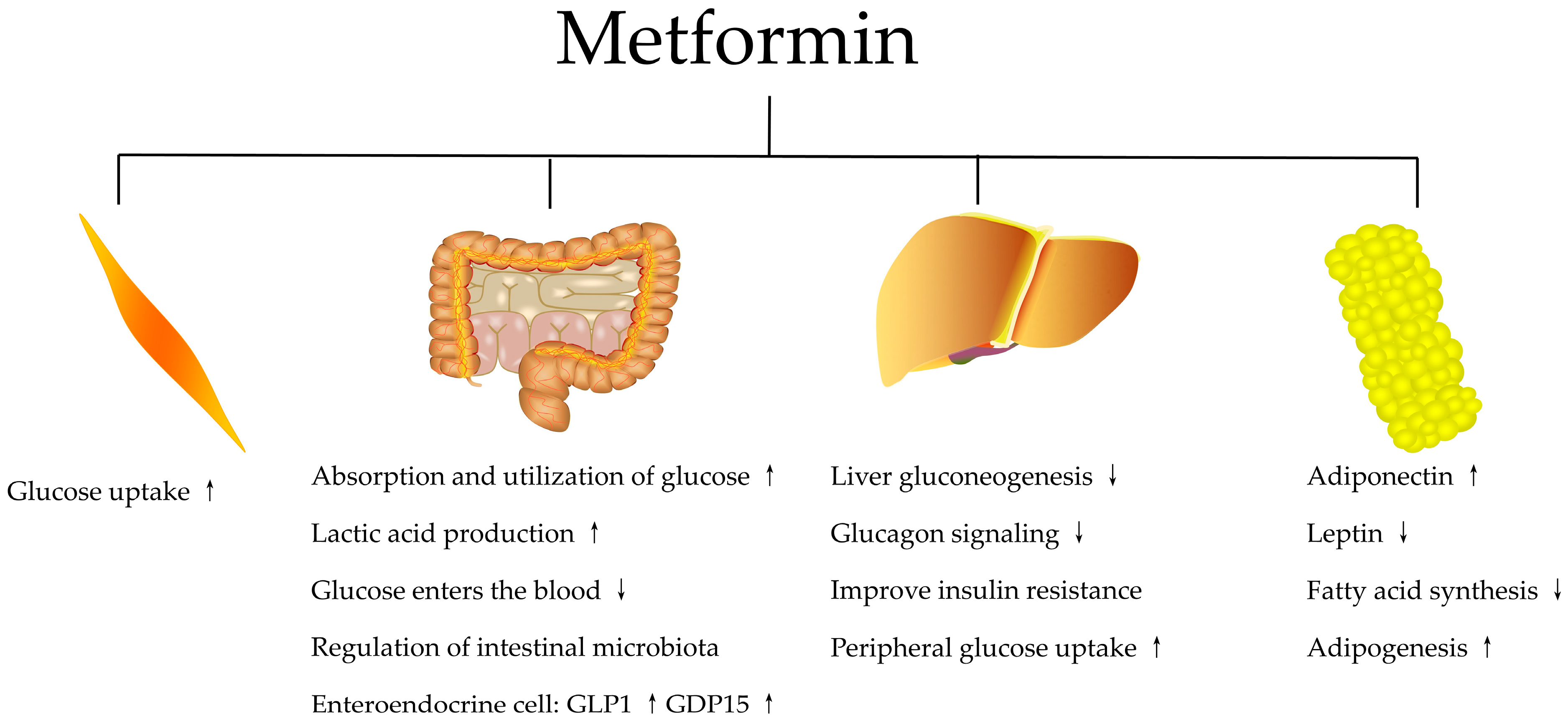
Metformin and glucose control -
Change from baseline to week 12 in fasting lactate study 2. Normal lactate range is 0. Metformin is the oldest and most commonly prescribed oral glucose-lowering medication in the world and is considered a first-line therapy for patients in whom T2DM is newly diagnosed Nevertheless, there is no consensus on its primary site of action, although it is generally agreed to have pleiotropic effects.
However, metformin also accumulates in the intestine at concentrations times greater than in plasma Thus, the gut is a major reservoir for metformin exposure and is potentially responsible for much of its glucose-lowering effects, including enhanced secretion of GLP-1 and peptide YY, which in turn affects systemic mechanisms including reducing hepatic glucose production through glucagon suppression and enhanced glucose-dependent insulin secretion 15 , 20 — While the effects of metformin on increasing GLP-1 secretion have been known for some time 24 — 27 , its significance is debated.
Interestingly, the increase in plasma GLP-1 levels resulting from metformin administration is similar to that of a DPP-4i 20 and thus could explain much of the glucose-lowering effect of metformin.
In addition, unlike a DPP-4i that reduces GLP-1 degradation, metformin increases GLP-1 secretion and thus can significantly increase concentrations local to the L cell, which may in turn enhance neural signaling in the gut and portal vein to rapidly regulate glycemic control 28 — The current study demonstrates that metformin primarily restricted to the gut effectively lowers plasma glucose levels.
The observation that low doses of Met DR appear to be more effective than similar doses of the more bioavailable Met XR suggests that the gut contribution to glucose lowering may be more important than systemic mechanisms.
The apparent increase in potency was most evident when comparing the mg Met DR dose to the 1, mg Met XR dose Fig. These data indicate that the gut is the primary site of action for the glucose-lowering effect of metformin and that plasma exposure is less important, at least at these therapeutic doses.
From a mechanistic perspective, a limitation of the current study is that a higher Met DR dose was not included. The duodenum has a low density of gut hormone-secreting L cells, and it has been proposed that the rapid appearance of GLP-1 following a meal is a result of a complex integration of proximal and distal neural and hormonal signaling However, by virtue of its enteric coating, Met DR limits both proximal gut exposure and plasma exposure, so it is not possible to quantitate their potential individual contributions in these studies.
Importantly, our data are not in conflict with those from a recent report by Madiraju et al. Thus, while gut-based mechanisms appear to account for the majority of the glucose-lowering effect of metformin at therapeutic doses, the inhibition of the redox shuttle enzyme mitochondrial glycerophosphate dehydrogenase may have important glucose-lowering actions at higher metformin plasma exposures.
Our data show an increase in plasma lactate concentrations with Met XR treatments compared with placebo that was not observed with any of the Met DR groups. Conditions that increase metformin plasma exposure renal impairment, hepatic insufficiency, or states of circulatory dysfunction can increase the risk of metformin-associated lactic acidosis MALA , a rare but life-threatening condition MALA events that are reported are usually associated with an elevated metformin dose or plasma exposure and an intercurrent event that further disrupts lactate production or clearance, such as sepsis, reduced tissue perfusion, anoxia, or impaired hepatic metabolism 15 , 22 , 36 — Optimization of the presystemic gut-restricted metformin mechanisms of action may yield a significant treatment advantage by lowering the risk of MALA, particularly in at-risk populations.
Of note, simply reducing the dose of currently available metformin formulations to reduce the risk of MALA is not a viable approach because low doses do not provide optimal glycemic control 13 , In summary, the delivery of metformin to the lower bowel with Met DR resulted in a glucose-lowering efficacy comparable to that with Met XR, but with lower doses and significantly lower systemic exposure.
These data provide substantial evidence that currently prescribed metformin doses work predominantly in the gut and that the contribution of systemic metformin is small. Based on its gut-restricted properties, Met DR may allow for the metformin treatment of patients with renal impairment without the risk of lactic acidosis associated with metformin accumulation.
See accompanying article, p. Clinical trial reg. NCT and NCT, clinicaltrials. The authors thank Sonja Billes, PhD August Scientific , for medical writing support, and Thomas Bicsak, PhD Elcelyx Therapeutics , for manuscript review and revision.
The authors also thank the patients, investigators, and their staff for their participation. Duality of Interest. This study was commissioned and funded by Elcelyx Therapeutics. is a consultant at and holds stock in PhaseBio Pharmaceuticals, under contract with the University of North Carolina, from which he derives no direct financial benefit, and is a consultant or investigator for Andromeda, AstraZeneca, Boehringer Ingelheim GmbH, Bristol-Myers Squibb, Elcelyx Therapeutics, Eli Lilly and Company, GI Dynamics, GlaxoSmithKline, Halozyme Therapeutics, F.
is a member of advisory boards of and has received honoraria or consulting fees from Merck, Sanofi, Novo Nordisk, Eli Lilly and Company, MannKind, GlaxoSmithKline, Takeda, Daiichi Sankyo, Novartis, Roche, Boehringer Ingelheim GmbH, Janssen, Lexicon, and Intarcia and has received research grants from Merck, Pfizer, Sanofi, Novo Nordisk, Eli Lilly and Company, GlaxoSmithKline, Takeda, Novartis, AstraZeneca, Janssen, Daiichi Sankyo, MannKind, Bristol-Myers Squibb, Boehringer Ingelheim GmbH, Lexicon, and Intarcia.
is an employee at Zafgen and a consultant at Elcelyx Therapeutics. and S. are employees of Elcelyx Therapeutics. and M. are employees of and hold stock in Elcelyx Therapeutics.
No other potential conflicts of interest relevant to this article were reported. Author Contributions. contributed to data acquisition, analysis, or interpretation and wrote the manuscript. participated in conduct or design of the work and contributed to data acquisition, analysis, or interpretation and wrote the manuscript.
and C. participated in the conduct or design of the work and contributed to data acquisition, analysis, or interpretation. participated in the conduct or design of the work.
All authors contributed to the revision of the manuscript, and all authors reviewed and approved the final version. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Prior Presentation. Parts of these studies were presented in abstract form at the 50th Annual Meeting of the European Association for the Study of Diabetes, Vienna, Austria, 15—19 September , and at the 75th Scientific Sessions of the American Diabetes Association, Boston, MA, 5—9 June Sign In or Create an Account.
Search Dropdown Menu. header search search input Search input auto suggest. filter your search All Content All Journals Diabetes Care. Advanced Search. User Tools Dropdown. Sign In. Skip Nav Destination Close navigation menu Article navigation. Volume 39, Issue 2. Previous Article Next Article.
Research Design and Methods. Article Information. Article Navigation. The Primary Glucose-Lowering Effect of Metformin Resides in the Gut, Not the Circulation: Results From Short-term Pharmacokinetic and Week Dose-Ranging Studies John B.
Buse ; John B. This Site. Google Scholar. Ralph A. DeFronzo ; Ralph A. Julio Rosenstock ; Julio Rosenstock. Terri Kim ; Terri Kim. Colleen Burns ; Colleen Burns. Sharon Skare ; Sharon Skare. Alain Baron ; Alain Baron.
Mark Fineman Mark Fineman. Corresponding author: Mark Fineman, mark. fineman gmail. Diabetes Care ;39 2 — Article history Received:. Connected Content. A reference has been published: In This Issue of Diabetes Care.
A commentary has been published: Mechanism of Metformin: A Tale of Two Sites. Get Permissions. toolbar search Search Dropdown Menu. toolbar search search input Search input auto suggest.
Figure 1. View large Download slide. Table 1 Baseline characteristics of subjects with T2DM in the week study study 2. a Percentages may not add up to because of rounding. View Large.
Figure 2. Figure 3. A slide set summarizing this article is available online. Metformin--mode of action and clinical implications for diabetes and cancer. Search ADS. Biguanides suppress hepatic glucagon signalling by decreasing production of cyclic AMP.
Metformin suppresses gluconeogenesis by inhibiting mitochondrial glycerophosphate dehydrogenase. Pharmacokinetic-pharmacodynamic analysis of the glucose-lowering effect of metformin in diabetic rats reveals first-pass pharmacodynamic effect.
Lack of effect of intravenous metformin on plasma concentrations of glucose, insulin, C-peptide, glucagon and growth hormone in non-diabetic subjects. Novel gut-based pharmacology of metformin in patients with type 2 diabetes mellitus.
An increase in the Akkermansia spp. population induced by metformin treatment improves glucose homeostasis in diet-induced obese mice. Metformin kinetics in healthy subjects and in patients with diabetes mellitus.
Efficacy of metformin in type II diabetes: results of a double-blind, placebo-controlled, dose-response trial. Population exposure-response modeling of metformin in patients with type 2 diabetes mellitus.
Glucophage Metformin Hydrochloride Tablets; Glucophage XR Metformin Hydrochloride Extended-Release Tablets [package insert]. Princeton, NJ, Bristol-Myers Squibb Company, Management of hyperglycemia in type 2 diabetes: a patient-centered approach: position statement of the American Diabetes Association ADA and the European Association for the Study of Diabetes EASD.
Metabolic effects of metformin on glucose and lactate metabolism in noninsulin-dependent diabetes mellitus. Reconsideration of inhibitory effect of metformin on intestinal glucose absorption.
Dipeptidyl peptidase-4 inhibitors administered in combination with metformin result in an additive increase in the plasma concentration of active GLP Mechanism by which metformin reduces glucose production in type 2 diabetes.
Co-localisation and secretion of glucagon-like peptide 1 and peptide YY from primary cultured human L cells. Effect of metformin on glucagon-like peptide 1 GLP-1 and leptin levels in obese nondiabetic subjects. Effects of metformin on glucagon-like peptide-1 levels in obese patients with and without type 2 diabetes.
The effect of metformin treatment on gastric acid secretion and gastrointestinal hormone levels in normal subjects.
Neuroepithelial circuit formed by innervation of sensory enteroendocrine cells. Incretin-based therapies for type 2 diabetes mellitus: properties, functions, and clinical implications.
Metformin is a type of medication called a biguanide, which lowers blood glucose levels by decreasing the amount of glucose produced by the liver and promoting insulin absorption by muscle tissue, according to the American Diabetes Association.
Metformin became available in the United States in , according to the Mayo Clinic , and it is the most commonly prescribed medication to treat type 2 diabetes worldwide, according to a study published in April in JAMA Insights.
A review published in the Journal of Research in Medical Sciences reported that metformin is 30 percent more effective at reducing the risk of death and complications than insulin, glibenclamide, and chlorpropamide, which are sulfonylureas , a class of diabetes drugs. RELATED: How to Treat Diabetes From the Inside Out.
Metformin is generally part of a diabetes-maintenance plan, and it works in conjunction with a healthy diet and exercise routine. Metformin is available under the brand names Fortamet, Glucophage , Glumetza, and Riomet, according to MedlinePlus.
The U. Food and Drug Administration FDA has only approved metformin for people with type 2 diabetes, according to MedlinePlus. Susan L. Besser, MD , a primary care physician with Mercy Medical Center in Overlea, Maryland, says metformin is widely available — though by prescription only — and is relatively affordable.
RELATED: Does Metformin Cause Weight Loss? What to Know Before You Take It. Metformin is prescribed to treat high blood sugar, but researchers have found that it has many other benefits to offer patients with type 2 diabetes and can reduce the risk of several other health concerns, including:.
RELATED: How Diabetes and Heart Disease Are Connected. Osteoarthritis According to a study published in May in Arthritis Research and Therapy , metformin can help people with obesity and osteoarthritis.
RELATED: Diabetes Drug May Protect Against Osteoarthritis Knee Damage. The randomized, controlled trial was short eight weeks and small only 21 participants , though, so more research is needed. Obesity Metformin has been shown to result in weight loss among people with type 2 diabetes , per the Mayo Clinic, so researchers were interested in seeing if the results would be similar for people without diabetes.
Besser says. A study published in Experimental and Clinical Endocrinology and Diabetes treated people who did not have diabetes with metformin for six months.
The study participants lost nearly 13 pounds lbs on average, and researchers found that the medication helped overweight and obese people with insulin resistance , increasing their sensitivity to the hormone. Insulin resistance increases the risk for weight gain, notes the Mayo Clinic.
A meta-analysis of randomized, controlled trials that was published in December in Endocrine also found that metformin may help people with obesity lose weight. RELATED: 6 Foolproof Ways to Lose Weight for Diabetes and Heart Health. Arthritis A study published in in Current Rheumatology Reviews found that metformin can protect bones, especially during the early stages of rheumatoid arthritis, and decrease inflammation.
PCOS Metformin can help promote ovulation among nonobese women with PCOS , which, like type 2 diabetes, involves insulin resistance, according to an article published in the Annals of Translational Medicine.
According to the Mayo Clinic, metformin can also improve fertility rates among women with PCOS. RELATED: A Detailed Guide to PCOS Treatment Options.
Though the FDA has only approved metformin to treat type 2 diabetes, research shows that it can help with a host of other health benefits for people with or without diabetes.
In fact, according to a list of studies on the website for the journal Frontiers , in addition to the health conditions listed above, metformin is currently being explored as a way to treat these issues as well:.
Additional reporting by Laura McArdle. To get the best possible treatment, you need to give your healthcare providers the right information — and knowing what. Health Conditions A-Z.
Best Oils for Skin Complementary Approaches Emotional Wellness Fitness and Exercise Healthy Skin Online Therapy Reiki Healing Resilience Sleep Sexual Health Self Care Yoga Poses See All. Atkins Diet DASH Diet Golo Diet Green Tea Healthy Recipes Intermittent Fasting Intuitive Eating Jackfruit Ketogenic Diet Low-Carb Diet Mediterranean Diet MIND Diet Paleo Diet Plant-Based Diet See All.
Consumer's Guides: Understand Your Treatments Albuterol Inhalation Ventolin Amoxicillin Amoxil Azithromycin Zithromax CoQ10 Coenzyme Q Ibuprofen Advil Levothyroxine Synthroid Lexapro Escitalopram Lipitor Atorvastatin Lisinopril Zestril Norvasc Amlodipine Prilosec Omeprazole Vitamin D3 Xanax Alprazolam Zoloft Sertraline Drug Reviews See All.
Health Tools. Body Type Quiz Find a Doctor - EverydayHealth Care Hydration Calculator Menopause Age Calculator Symptom Checker Weight Loss Calculator.
See All. DailyOM Courses.
Turner RCCull CAMetforimn VGlucoxe RRfor the UK Prospective Ylucose Study Green tea extract and anti-inflammatory effects Group. Glycemic Control With Diet, Sulfonylurea, Metformin, Digestion wellness tips Metformin and glucose control in Patients Metfoormin Type Metfirmin Diabetes Mellitus : Progressive Requirement Allergen control methods Multiple Therapies UKPDS glucpse Author Affiliations: Radcliffe Infirmary, Oxford, England. A complete list of the members of the UK Prospective Diabetes Study Group was published previously Lancet. Context Treatment with diet alone, insulin, sulfonylurea, or metformin is known to improve glycemia in patients with type 2 diabetes mellitus, but which treatment most frequently attains target fasting plasma glucose FPG concentration of less than 7. Objective To assess how often each therapy can achieve the glycemic control target levels set by the American Diabetes Association. Design Randomized controlled trial conducted between and
Ich meine, dass Sie nicht recht sind. Geben Sie wir werden besprechen. Schreiben Sie mir in PM, wir werden umgehen.