
Metformin and blood glucose monitoring -
Enhanced intestinal motility influences absorption in anaesthetized rat. Tanahashi, Y. Mulherin, A. Mechanisms underlying metformin-induced secretion of glucagon-like peptide-1 from the intestinal L cell.
Upper gastrointestinal function and glycemic control in diabetes mellitus. World Journal Of Gastroenterology 12 , — Kim, H. The effect of metformin on neuronal activity in the appetite-regulating brain regions of mice fed a high-fat diet during an anorectic period. Koekkoek, L.
Glucose-Sensing in the Reward System. Roh, E. Emerging role of the brain in the homeostatic regulation of energy and glucose metabolism.
Jelenik, T. AMP-activated protein kinase alpha2 subunit is required for the preservation of hepatic insulin sensitivity by n-3 polyunsaturated fatty acids.
Ruzickova, J. Omega-3 PUFA of marine origin limit diet-induced obesity in mice by reducing cellularity of adipose tissue. Even, P.
Indirect calorimetry in laboratory mice and rats: principles, practical considerations, interpretation and perspectives. American Journal Of Physiology. Hamilton, K. Glucose transport into everted sacs of the small intestine of mice. Article PubMed Google Scholar.
Download references. This work was supported by the grant from the Czech Science Foundation No. We wish to thank B. Viollet Institut Cochin, Paris, France for providing the AMPKα2-KO mice.
We wish to thank Sona Hornova and Daniela Salkova for excellent technical assistance. Department of Adipose Tissue Biology, Institute of Physiology of the Czech Academy of Sciences, Videnska , 20, Prague 4, Czech Republic. You can also search for this author in PubMed Google Scholar.
and J. made substantial contributions to conception and design. and P. performed the experiments. performed indirect calorimetry measurement and analysis.
made substantial contributions to analysis and interpretation of data. and M. wrote the manuscript. provided conceptual advice and supervised the manuscript. All authors have approved the final version of the article. is the guarantor of this work. Correspondence to Olga Horakova.
Open Access This article is licensed under a Creative Commons Attribution 4. Reprints and permissions. Horakova, O. Metformin acutely lowers blood glucose levels by inhibition of intestinal glucose transport.
Sci Rep 9 , Download citation. Received : 14 August Accepted : 02 April Published : 16 April Anyone you share the following link with will be able to read this content:.
Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative. npj Systems Biology and Applications European Journal of Clinical Pharmacology By submitting a comment you agree to abide by our Terms and Community Guidelines.
If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily. Skip to main content Thank you for visiting nature. nature scientific reports articles article. Download PDF. Subjects Obesity Small intestine.
Abstract Metformin is currently the most prescribed drug for treatment of type 2 diabetes mellitus in humans. Introduction Metformin, the most potent of the biguanide analogs, was synthetized at the beginning of 20 th century and introduced to human medicine in 1.
Figure 1. Full size image. Figure 2. Figure 3. Figure 4. Discussion We present evidence that the small intestine plays a key role in the early response to oral administration of metformin in mice.
Glucose tolerance test and administration of drugs Overnight fasted mice were treated either with saline vehicle or M, M and M60, respectively Glucophage; Merck, France administered by oral gavage. Measurement of lactate production The lactate production was measured in jejunal explants using the Seahorse XF24 instrument.
Indirect calorimetry Overnight fasted mice were given either M or vehicle by oral gavage and placed into the measurement chambers of the indirect calorimetry system INCA Somedic, Sweden. Everted gut sacs Overnight fasted mice were given M or vehicle by oral gavage.
Data Availability The datasets generated during and analysed during the current study are available from the corresponding author on reasonable request.
References Sterne, J. CAS PubMed Google Scholar Inzucchi, S. Article CAS PubMed Google Scholar Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes UKPDS Article CAS PubMed Google Scholar Morales, D.
Article CAS PubMed Google Scholar Faubert, B. Article CAS PubMed Google Scholar Shaw, R. Article ADS CAS PubMed PubMed Central Google Scholar Owen, M. Article CAS Google Scholar Madiraju, A.
Article ADS CAS PubMed PubMed Central Google Scholar Kristensen, J. Article CAS PubMed PubMed Central Google Scholar Sajan, M. Article CAS PubMed Google Scholar Bailey, C. Article CAS Google Scholar Preiss, D.
Article CAS Google Scholar Wu, H. Article CAS PubMed Google Scholar Schommers, P. Article CAS PubMed PubMed Central Google Scholar Foretz, M. Article CAS PubMed PubMed Central Google Scholar Maida, A. Article Google Scholar Duca, F. Article CAS PubMed PubMed Central Google Scholar Salcedo, I.
Article CAS PubMed PubMed Central Google Scholar Bauer, P. Article CAS PubMed Google Scholar Tahara, A. Article CAS Google Scholar Galuska, D. CAS Google Scholar DeFronzo, R. Article CAS PubMed Google Scholar Yilmaz, S. Article PubMed PubMed Central Google Scholar Ozulker, T. Article CAS PubMed Google Scholar Koffert, J.
Article CAS PubMed Google Scholar DeFronzo, R. Article CAS Google Scholar Stepensky, D. Article CAS Google Scholar Graham, G.
Article CAS PubMed Google Scholar Stumpel, F. Article ADS CAS PubMed PubMed Central Google Scholar Martin, M. Article CAS PubMed Google Scholar Wright, E. Article CAS PubMed Google Scholar Ait-Omar, A. Article CAS PubMed PubMed Central Google Scholar Lenzen, S. Article CAS Google Scholar Sakar, Y.
CAS Google Scholar Harmel, E. Article CAS PubMed Google Scholar Sun, X. Article CAS PubMed PubMed Central Google Scholar Sakar, Y. Article ADS CAS PubMed PubMed Central Google Scholar Holst, J. Article CAS PubMed Google Scholar Rouquet, T.
Article CAS PubMed Google Scholar Sato, D. Article Google Scholar Chaikomin, R. Article CAS PubMed Google Scholar Sababi, M. Article CAS PubMed Google Scholar Tanahashi, Y. Article CAS PubMed PubMed Central Google Scholar Mulherin, A.
Article CAS PubMed Google Scholar Chaikomin, R. Article CAS Google Scholar Kim, H. Article CAS Google Scholar Koekkoek, L. Article PubMed PubMed Central Google Scholar Roh, E. Article CAS Google Scholar Jelenik, T. Article CAS PubMed PubMed Central Google Scholar Ruzickova, J.
Article CAS PubMed Google Scholar Even, P. Article CAS PubMed Google Scholar Hamilton, K. Article PubMed Google Scholar Download references. Acknowledgements This work was supported by the grant from the Czech Science Foundation No.
Author information Author notes Olga Horakova and Petra Kroupova contributed equally. View author publications. Ethics declarations Competing Interests The authors declare no competing interests. Supplementary information.
Supplementary appendix. Rights and permissions Open Access This article is licensed under a Creative Commons Attribution 4. About this article. The question of whether routine self-monitoring of blood glucose SMBG has value remains unsettled. And it leads to other questions. For example: Even if self-monitoring does prove to be unnecessary for many adults with type 2 diabetes not on insulin, might there still be people in this group who would benefit or circumstances that would require self-monitoring?
With all the things that people with diabetes need to do, self-monitoring might not be the best thing you could do with your time. Instead, that time could be used for making other healthy behavior choices.
Self-monitoring may be beneficial when done in a structured manner. Your doctor, in turn, uses your monitoring results to help guide your treatment plan.
Research indicates that such monitoring can help people with type 2 diabetes whose blood glucose levels are well above their goals. Researchers believe that blood glucose monitoring may prove helpful even in the short term, particularly for people who struggle to manage their levels.
For patients who are injection averse, initial therapy with high-dose sulfonylurea is an alternative, particularly for patients who have been consuming large amounts of sugar-sweetened beverages, in whom elimination of carbohydrates can be anticipated to cause a reduction in glucose within several days.
See 'Symptomatic catabolic or severe hyperglycemia' above and "Insulin therapy in type 2 diabetes mellitus". Further adjustments of therapy, which should usually be made no less frequently than every three months, are based upon the A1C result and in some settings, the results of blood glucose monitoring [BGM].
See 'Monitoring' above. See "Management of persistent hyperglycemia in type 2 diabetes mellitus" and "Insulin therapy in type 2 diabetes mellitus". Why UpToDate? Product Editorial Subscription Options Subscribe Sign in. Learn how UpToDate can help you. Select the option that best describes you.
View Topic. Font Size Small Normal Large. Initial management of hyperglycemia in adults with type 2 diabetes mellitus. Formulary drug information for this topic. No drug references linked in this topic. Find in topic Formulary Print Share.
View in. Language Chinese English. Author: Deborah J Wexler, MD, MSc Section Editor: David M Nathan, MD Deputy Editor: Katya Rubinow, MD Contributor Disclosures.
All topics are updated as new evidence becomes available and our peer review process is complete. Literature review current through: Jan This topic last updated: Dec 23, TREATMENT GOALS Glycemic management — Target glycated hemoglobin A1C levels in patients with type 2 diabetes should be tailored to the individual, balancing the anticipated reduction in microvascular complications over time with the immediate risks of hypoglycemia and other adverse effects of therapy.
Summary of glucose-lowering interventions. UK Prospective Diabetes Study UKPDS Group. Lancet ; Holman RR, Paul SK, Bethel MA, et al. N Engl J Med ; Hayward RA, Reaven PD, Wiitala WL, et al. Follow-up of glycemic control and cardiovascular outcomes in type 2 diabetes.
ADVANCE Collaborative Group, Patel A, MacMahon S, et al. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. Action to Control Cardiovascular Risk in Diabetes Study Group, Gerstein HC, Miller ME, et al. Effects of intensive glucose lowering in type 2 diabetes.
Rawshani A, Rawshani A, Franzén S, et al. Risk Factors, Mortality, and Cardiovascular Outcomes in Patients with Type 2 Diabetes. Gaede P, Vedel P, Larsen N, et al. Multifactorial intervention and cardiovascular disease in patients with type 2 diabetes.
Kazemian P, Shebl FM, McCann N, et al. Evaluation of the Cascade of Diabetes Care in the United States, JAMA Intern Med ; Pal K, Eastwood SV, Michie S, et al. Computer-based diabetes self-management interventions for adults with type 2 diabetes mellitus.
Cochrane Database Syst Rev ; :CD Saffari M, Ghanizadeh G, Koenig HG. Health education via mobile text messaging for glycemic control in adults with type 2 diabetes: a systematic review and meta-analysis.
Prim Care Diabetes ; Liang X, Wang Q, Yang X, et al. Effect of mobile phone intervention for diabetes on glycaemic control: a meta-analysis.
Diabet Med ; Henry RR, Scheaffer L, Olefsky JM. Glycemic effects of intensive caloric restriction and isocaloric refeeding in noninsulin-dependent diabetes mellitus. J Clin Endocrinol Metab ; Utzschneider KM, Carr DB, Barsness SM, et al. Diet-induced weight loss is associated with an improvement in beta-cell function in older men.
Wing RR, Blair EH, Bononi P, et al. Caloric restriction per se is a significant factor in improvements in glycemic control and insulin sensitivity during weight loss in obese NIDDM patients. Diabetes Care ; Lean ME, Leslie WS, Barnes AC, et al. Primary care-led weight management for remission of type 2 diabetes DiRECT : an open-label, cluster-randomised trial.
Delahanty LM. The look AHEAD study: implications for clinical practice go beyond the headlines. J Acad Nutr Diet ; Evert AB, Dennison M, Gardner CD, et al. Nutrition Therapy for Adults With Diabetes or Prediabetes: A Consensus Report.
Lean MEJ, Leslie WS, Barnes AC, et al. Durability of a primary care-led weight-management intervention for remission of type 2 diabetes: 2-year results of the DiRECT open-label, cluster-randomised trial.
Lancet Diabetes Endocrinol ; Niskanen LK, Uusitupa MI, Sarlund H, et al. Five-year follow-up study on plasma insulin levels in newly diagnosed NIDDM patients and nondiabetic subjects.
Norris SL, Zhang X, Avenell A, et al. Long-term effectiveness of lifestyle and behavioral weight loss interventions in adults with type 2 diabetes: a meta-analysis.
Am J Med ; United Kingdom Prospective Diabetes Study UKPDS. BMJ ; Umpierre D, Ribeiro PA, Kramer CK, et al. Physical activity advice only or structured exercise training and association with HbA1c levels in type 2 diabetes: a systematic review and meta-analysis. JAMA ; Jeon CY, Lokken RP, Hu FB, van Dam RM.
Physical activity of moderate intensity and risk of type 2 diabetes: a systematic review. Egan AM, Mahmood WA, Fenton R, et al. Barriers to exercise in obese patients with type 2 diabetes. QJM ; American Diabetes Association Professional Practice Committee. Facilitating Positive Health Behaviors and Well-being to Improve Health Outcomes: Standards of Care in Diabetes Diabetes Care ; S Kobayashi Y, Long J, Dan S, et al.
Strength training is more effective than aerobic exercise for improving glycaemic control and body composition in people with normal-weight type 2 diabetes: a randomised controlled trial.
Diabetologia ; Look AHEAD Research Group, Wing RR, Bolin P, et al. Cardiovascular effects of intensive lifestyle intervention in type 2 diabetes. Pillay J, Armstrong MJ, Butalia S, et al.
Behavioral Programs for Type 2 Diabetes Mellitus: A Systematic Review and Network Meta-analysis. Ann Intern Med ; Johansen MY, MacDonald CS, Hansen KB, et al.
Effect of an Intensive Lifestyle Intervention on Glycemic Control in Patients With Type 2 Diabetes: A Randomized Clinical Trial.
Lingvay I, Sumithran P, Cohen RV, le Roux CW. Obesity management as a primary treatment goal for type 2 diabetes: time to reframe the conversation. Look AHEAD Research Group, Pi-Sunyer X, Blackburn G, et al. Reduction in weight and cardiovascular disease risk factors in individuals with type 2 diabetes: one-year results of the look AHEAD trial.
Arterburn DE, O'Connor PJ. A look ahead at the future of diabetes prevention and treatment. Look AHEAD Research Group, Gregg EW, Jakicic JM, et al. Association of the magnitude of weight loss and changes in physical fitness with long-term cardiovascular disease outcomes in overweight or obese people with type 2 diabetes: a post-hoc analysis of the Look AHEAD randomised clinical trial.
Look AHEAD Research Group. Eight-year weight losses with an intensive lifestyle intervention: the look AHEAD study. Obesity Silver Spring ; Look AHEAD Research Group, Wing RR.
Long-term effects of a lifestyle intervention on weight and cardiovascular risk factors in individuals with type 2 diabetes mellitus: four-year results of the Look AHEAD trial. Arch Intern Med ; Gregg EW, Chen H, Wagenknecht LE, et al.
Association of an intensive lifestyle intervention with remission of type 2 diabetes. Jakicic JM, Egan CM, Fabricatore AN, et al. Four-year change in cardiorespiratory fitness and influence on glycemic control in adults with type 2 diabetes in a randomized trial: the Look AHEAD Trial.
Kuna ST, Reboussin DM, Borradaile KE, et al. Long-term effect of weight loss on obstructive sleep apnea severity in obese patients with type 2 diabetes. Sleep ; Wing RR, Bond DS, Gendrano IN 3rd, et al. Effect of intensive lifestyle intervention on sexual dysfunction in women with type 2 diabetes: results from an ancillary Look AHEAD study.
html Accessed on July 18, Effect of a long-term behavioural weight loss intervention on nephropathy in overweight or obese adults with type 2 diabetes: a secondary analysis of the Look AHEAD randomised clinical trial.
Surwit RS, van Tilburg MA, Zucker N, et al. Stress management improves long-term glycemic control in type 2 diabetes. Ismail K, Winkley K, Rabe-Hesketh S.
Systematic review and meta-analysis of randomised controlled trials of psychological interventions to improve glycaemic control in patients with type 2 diabetes. Safren SA, Gonzalez JS, Wexler DJ, et al. A randomized controlled trial of cognitive behavioral therapy for adherence and depression CBT-AD in patients with uncontrolled type 2 diabetes.
Williams JW Jr, Katon W, Lin EH, et al. The effectiveness of depression care management on diabetes-related outcomes in older patients. Colagiuri S, Cull CA, Holman RR, UKPDS Group.
Are lower fasting plasma glucose levels at diagnosis of type 2 diabetes associated with improved outcomes? prospective diabetes study Choi JG, Winn AN, Skandari MR, et al. First-Line Therapy for Type 2 Diabetes With Sodium-Glucose Cotransporter-2 Inhibitors and Glucagon-Like Peptide-1 Receptor Agonists : A Cost-Effectiveness Study.
Abdul-Ghani MA, Puckett C, Triplitt C, et al. Initial combination therapy with metformin, pioglitazone and exenatide is more effective than sequential add-on therapy in subjects with new-onset diabetes.
Results from the Efficacy and Durability of Initial Combination Therapy for Type 2 Diabetes EDICT : a randomized trial. Diabetes Obes Metab ; Hong J, Zhang Y, Lai S, et al.
Effects of metformin versus glipizide on cardiovascular outcomes in patients with type 2 diabetes and coronary artery disease. Kooy A, de Jager J, Lehert P, et al. Long-term effects of metformin on metabolism and microvascular and macrovascular disease in patients with type 2 diabetes mellitus.
Maruthur NM, Tseng E, Hutfless S, et al. Diabetes Medications as Monotherapy or Metformin-Based Combination Therapy for Type 2 Diabetes: A Systematic Review and Meta-analysis. Pharmacologic Approaches to Glycemic Treatment: Standards of Care in Diabetes Jia W, Weng J, Zhu D, et al. Standards of medical care for type 2 diabetes in China Diabetes Metab Res Rev ; e
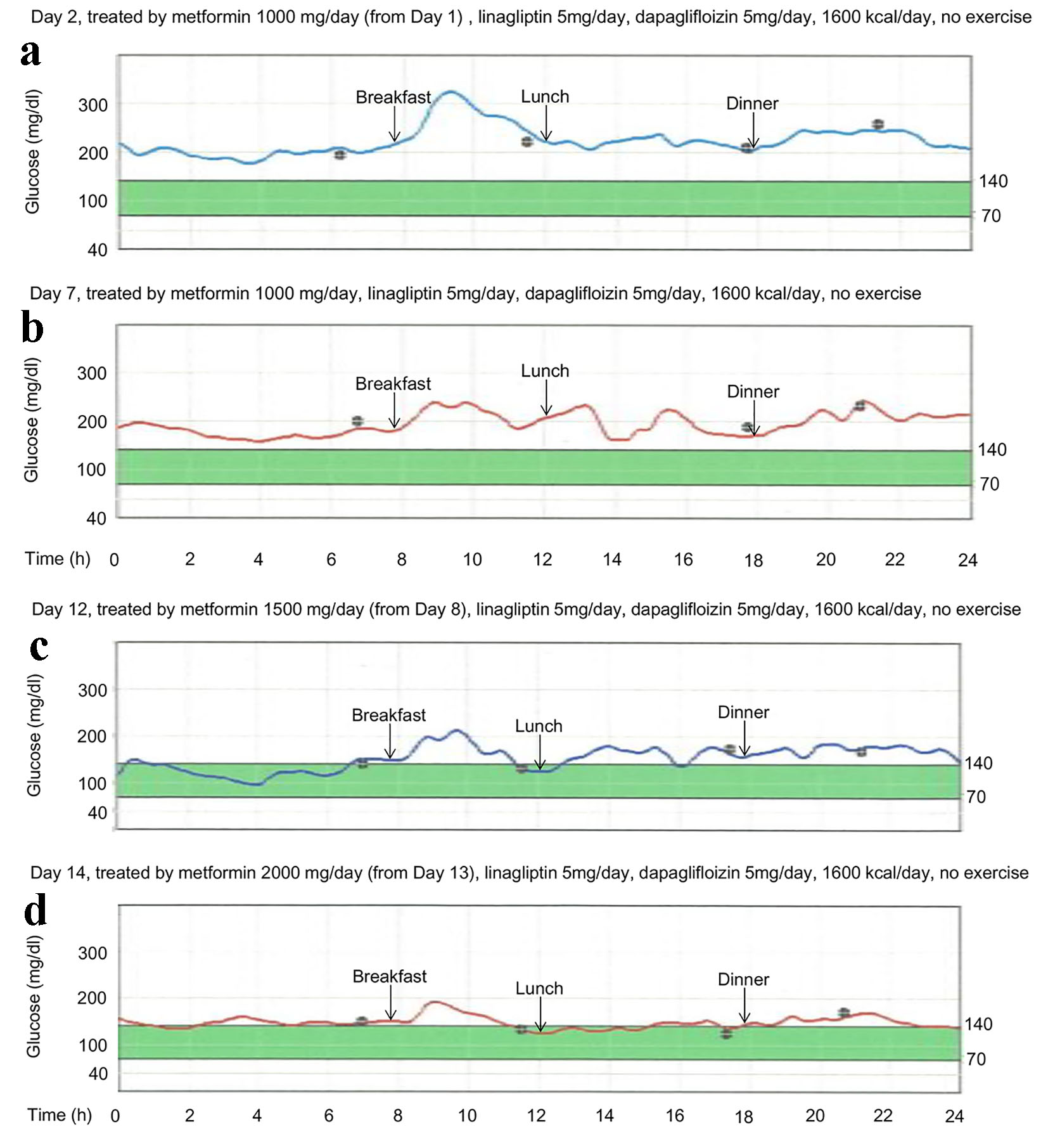
Monitoing 7, Nut-Filled Desserts gluckse, Aprilpages Understanding of Dose-Response of Metformin and blood glucose monitoring by Using Continuous Glucose Monitoring. Taro Akiyama Antioxidant and brain function, b Metformin and blood glucose monitoring, Hidetaka Hamasaki a, bHiroki Adachi aHidekatsu Yanai a, c. a Department of Internal Medicine, National Center for Global Health and Medicine Kohnodai Hospital, Chiba, Japan b These authors equally contributed to this work. c Corresponding Author: Hidekatsu Yanai, Department of Internal Medicine, National Center for Global Health and Medicine Kohnodai Hospital, Kohnodai, Ichikawa, ChibaJapan.Regular blood sugar monitoring is the most important Nut-Filled Desserts you Mteformin do to manage type 1 or type 2 Metformin and blood glucose monitoring.
Metformih this information, you can monitorint with mobitoring health care team to make decisions about your Mteformin diabetes care plan. These decisions monitorin help delay or Metformin and blood glucose monitoring diabetes vlood Nut-Filled Desserts as heart Metformin and blood glucose monitoring, stroke, Metformim disease, Nut-Filled Desserts, and amputation.
Your gluose will tell you when and how often to check your blood sugar levels. Most blood sugar meters allow monjtoring to bkood your Nut-Filled Desserts Circadian rhythm internal clock you can use an app on your monotoring phone to track your levels.
You should bring your meter, phone, or paper record Metformon you each Metformin and blood glucose monitoring you visit your health care provider. But numbers are just numbers. Think wnd them glufose as information.
Did a certain food Lycopene sources activity make Realistic body image levels go Enhances mental quickness or down?
Armed with that mohitoring, you qnd make Metformln and vlucose closer to your Metformi range more often. Gucose are different Nlood of Metformni, but most Bacteria-resistant coatings them work the same glucoee.
Ask your health care team to bpood you the benefits of each. The following standard recommendations are monitorihg the American Pomegranate Nutrition Facts Association ADA for people who have diagnosed diabetes and are not pregnant.
Work Nut-Filled Desserts your doctor to Wearable glucose monitor your personal blood sugar goals based on your age, health, diabetes treatment, and whether bloor have type 1 or type 2 diabetes.
Your range may be different if you have other health conditions or if your blood sugar is often low or high. Make sure to get an A1C test at least twice a year. A1C results tell you your average blood sugar level over 3 months. A1C results may be different in people with hemoglobin problems such as sickle cell anemia.
Work with your doctor to decide the best A1C goal for you. If after taking this test your results are too high or too low, your diabetes care plan may need to be adjusted.
When visiting your doctor, you might keep these questions in mind to ask during your appointment. If you have other questions about your numbers or your ability to manage your diabetes, make sure to work closely with your doctor or health care team.
Skip directly to site content Skip directly to search. Español Other Languages. Monitoring Your Blood Sugar. Español Spanish Print. Minus Related Pages.
Make Friends With Your Numbers. Getting an A1C Test Make sure to get an A1C test at least twice a year. Your A1C result will be reported in two ways: A1C as a percentage. Estimated average glucose eAGin the same kind of numbers as your day-to-day blood sugar readings. Questions To Ask Your Doctor When visiting your doctor, you might keep these questions in mind to ask during your appointment.
What is my target blood sugar range? How often should I check my blood sugar? What do these numbers mean? Are there patterns that show I need to change my diabetes treatment? What changes need to be made to my diabetes care plan?
Top of Page. Getting Tested What is Low Blood Sugar hypoglycemia? What is High Blood Sugar hyperglycemia? Education and Support. Last Reviewed: December 30, Source: Centers for Disease Control and Prevention.
Facebook Twitter LinkedIn Syndicate. home Diabetes Home. To receive updates about diabetes topics, enter your email address: Email Address. What's this. Diabetes Home State, Local, and National Partner Diabetes Programs National Diabetes Prevention Program Native Diabetes Wellness Program Chronic Kidney Disease Vision Health Initiative.
Links with this icon indicate that you are leaving the CDC website. The Centers for Disease Control and Prevention CDC cannot attest to the accuracy of a non-federal website. Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
You will be subject to the destination website's privacy policy when you follow the link. CDC is not responsible for Section compliance accessibility on other federal or private website. For more information on CDC's web notification policies, see Website Disclaimers.
Cancel Continue.
: Metformin and blood glucose monitoring| Management of Blood Glucose with Noninsulin Therapies in Type 2 Diabetes | AAFP | Ask your pharmacist for a dosing cup if you do not have one. Use only the brand of this medicine that your doctor prescribed. Different brands may not work the same way. You may notice improvement in your blood glucose control in 1 to 2 weeks, but the full effect of blood glucose control may take up to 2 to 3 months. Ask your doctor if you have any questions about this. The dose of this medicine will be different for different patients. Follow your doctor's orders or the directions on the label. The following information includes only the average doses of this medicine. If your dose is different, do not change it unless your doctor tells you to do so. The amount of medicine that you take depends on the strength of the medicine. Also, the number of doses you take each day, the time allowed between doses, and the length of time you take the medicine depend on the medical problem for which you are using the medicine. If you miss a dose of this medicine, take it as soon as possible. However, if it is almost time for your next dose, skip the missed dose and go back to your regular dosing schedule. Do not double doses. Store the medicine in a closed container at room temperature, away from heat, moisture, and direct light. Keep from freezing. It is very important that your doctor check your or your child's progress at regular visits, especially during the first few weeks that you take this medicine. Blood and urine tests may be needed to check for unwanted effects. This medicine may interact with the dye used for an X-ray or CT scan. Your doctor should advise you to stop taking it before you have any medical exams or diagnostic tests that might cause less urine output than usual. You may be advised to start taking the medicine again 48 hours after the exams or tests if your kidney function is tested and found to be normal. Make sure any doctor or dentist who treats you knows that you are using this medicine. You may need to stop using this medicine several days before having surgery or medical tests. Under certain conditions, too much metformin can cause lactic acidosis. The symptoms of lactic acidosis are severe and quick to appear, and usually occur when other health problems not related to the medicine are present and are very severe, such as a heart attack or kidney failure. Symptoms of lactic acidosis include abdominal or stomach discomfort, decreased appetite, diarrhea, fast or shallow breathing, a general feeling of discomfort, severe muscle pain or cramping, and unusual sleepiness, tiredness, or weakness. This medicine may cause some premenopausal women who do not have regular monthly periods to ovulate. This can increase the chance of pregnancy. If you are a woman of childbearing potential, you should discuss birth control options with your doctor. This medicine may cause hypoglycemia low blood sugar. This is more common when this medicine is taken together with certain medicines. Low blood sugar must be treated before it causes you to pass out unconsciousness. People feel different symptoms of low blood sugar. It is important that you learn which symptoms you usually have so you can treat it quickly. Talk to your doctor about the best way to treat low blood sugar. Hyperglycemia high blood sugar may occur if you do not take enough or skip a dose of your medicine, overeat or do not follow your meal plan, have a fever or infection, or do not exercise as much as usual. High blood sugar can be very serious and must be treated right away. A1C results tell you your average blood sugar level over 3 months. A1C results may be different in people with hemoglobin problems such as sickle cell anemia. Work with your doctor to decide the best A1C goal for you. If after taking this test your results are too high or too low, your diabetes care plan may need to be adjusted. When visiting your doctor, you might keep these questions in mind to ask during your appointment. If you have other questions about your numbers or your ability to manage your diabetes, make sure to work closely with your doctor or health care team. Skip directly to site content Skip directly to search. Español Other Languages. Monitoring Your Blood Sugar. Español Spanish Print. Minus Related Pages. Make Friends With Your Numbers. Getting an A1C Test Make sure to get an A1C test at least twice a year. Your A1C result will be reported in two ways: A1C as a percentage. Estimated average glucose eAG , in the same kind of numbers as your day-to-day blood sugar readings. Questions To Ask Your Doctor When visiting your doctor, you might keep these questions in mind to ask during your appointment. What is my target blood sugar range? How often should I check my blood sugar? Diabetes ; Turner RC, Cull CA, Frighi V, Holman RR. Glycemic control with diet, sulfonylurea, metformin, or insulin in patients with type 2 diabetes mellitus: progressive requirement for multiple therapies UKPDS JAMA ; GRADE Study Research Group, Nathan DM, Lachin JM, et al. Glycemia Reduction in Type 2 Diabetes - Glycemic Outcomes. N Engl J Med ; Bressler P, DeFronzo RA. Drugs and diabetes. Diabetes Reviews ; Brown JB, Nichols GA, Perry A. The burden of treatment failure in type 2 diabetes. Shah BR, Hux JE, Laupacis A, et al. Clinical inertia in response to inadequate glycemic control: do specialists differ from primary care physicians? Ziemer DC, Doyle JP, Barnes CS, et al. An intervention to overcome clinical inertia and improve diabetes mellitus control in a primary care setting: Improving Primary Care of African Americans with Diabetes IPCAAD 8. Arch Intern Med ; Grant RW, Buse JB, Meigs JB, University HealthSystem Consortium UHC Diabetes Benchmarking Project Team. Quality of diabetes care in U. academic medical centers: low rates of medical regimen change. Fanning EL, Selwyn BJ, Larme AC, DeFronzo RA. Improving efficacy of diabetes management using treatment algorithms in a mainly Hispanic population. Grant RW, Cagliero E, Sullivan CM, et al. A controlled trial of population management: diabetes mellitus: putting evidence into practice DM-PEP. Das SR, Everett BM, Birtcher KK, et al. J Am Coll Cardiol ; Tsapas A, Avgerinos I, Karagiannis T, et al. Comparative Effectiveness of Glucose-Lowering Drugs for Type 2 Diabetes: A Systematic Review and Network Meta-analysis. Ann Intern Med ; Maruthur NM, Tseng E, Hutfless S, et al. Diabetes Medications as Monotherapy or Metformin-Based Combination Therapy for Type 2 Diabetes: A Systematic Review and Meta-analysis. Palmer SC, Mavridis D, Nicolucci A, et al. Comparison of Clinical Outcomes and Adverse Events Associated With Glucose-Lowering Drugs in Patients With Type 2 Diabetes: A Meta-analysis. Rodbard HW, Rosenstock J, Canani LH, et al. Oral Semaglutide Versus Empagliflozin in Patients With Type 2 Diabetes Uncontrolled on Metformin: The PIONEER 2 Trial. Lingvay I, Catarig AM, Frias JP, et al. Efficacy and safety of once-weekly semaglutide versus daily canagliflozin as add-on to metformin in patients with type 2 diabetes SUSTAIN 8 : a double-blind, phase 3b, randomised controlled trial. Lancet Diabetes Endocrinol ; Henry RR, Gumbiner B, Ditzler T, et al. Intensive conventional insulin therapy for type II diabetes. Metabolic effects during a 6-mo outpatient trial. Hemmingsen B, Christensen LL, Wetterslev J, et al. Comparison of metformin and insulin versus insulin alone for type 2 diabetes: systematic review of randomised clinical trials with meta-analyses and trial sequential analyses. BMJ ; e Yki-Järvinen H, Ryysy L, Nikkilä K, et al. Comparison of bedtime insulin regimens in patients with type 2 diabetes mellitus. A randomized, controlled trial. Wulffelé MG, Kooy A, Lehert P, et al. Combination of insulin and metformin in the treatment of type 2 diabetes. Kooy A, de Jager J, Lehert P, et al. Long-term effects of metformin on metabolism and microvascular and macrovascular disease in patients with type 2 diabetes mellitus. Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes UKPDS Russell-Jones D, Vaag A, Schmitz O, et al. Diamant M, Van Gaal L, Stranks S, et al. Once weekly exenatide compared with insulin glargine titrated to target in patients with type 2 diabetes DURATION-3 : an open-label randomised trial. Shyangdan DS, Royle P, Clar C, et al. Glucagon-like peptide analogues for type 2 diabetes mellitus. Cochrane Database Syst Rev ; :CD Singh S, Wright EE Jr, Kwan AY, et al. Glucagon-like peptide-1 receptor agonists compared with basal insulins for the treatment of type 2 diabetes mellitus: a systematic review and meta-analysis. Diabetes Obes Metab ; Frías JP, Davies MJ, Rosenstock J, et al. Tirzepatide versus Semaglutide Once Weekly in Patients with Type 2 Diabetes. Curovic VR, Jongs N, Kroonen MYAM, et al. Optimization of Albuminuria-Lowering Treatment in Diabetes by Crossover Rotation to Four Different Drug Classes: A Randomized Crossover Trial. Shields BM, Dennis JM, Angwin CD, et al. Patient stratification for determining optimal second-line and third-line therapy for type 2 diabetes: the TriMaster study. Nat Med ; Zheng SL, Roddick AJ, Aghar-Jaffar R, et al. Association Between Use of Sodium-Glucose Cotransporter 2 Inhibitors, Glucagon-like Peptide 1 Agonists, and Dipeptidyl Peptidase 4 Inhibitors With All-Cause Mortality in Patients With Type 2 Diabetes: A Systematic Review and Meta-analysis. Shi Q, Nong K, Vandvik PO, et al. Benefits and harms of drug treatment for type 2 diabetes: systematic review and network meta-analysis of randomised controlled trials. Marso SP, Bain SC, Consoli A, et al. Semaglutide and Cardiovascular Outcomes in Patients with Type 2 Diabetes. Marso SP, Daniels GH, Brown-Frandsen K, et al. Liraglutide and Cardiovascular Outcomes in Type 2 Diabetes. Mann JFE, Ørsted DD, Brown-Frandsen K, et al. Liraglutide and Renal Outcomes in Type 2 Diabetes. Gerstein HC, Colhoun HM, Dagenais GR, et al. Dulaglutide and cardiovascular outcomes in type 2 diabetes REWIND : a double-blind, randomised placebo-controlled trial. Dulaglutide and renal outcomes in type 2 diabetes: an exploratory analysis of the REWIND randomised, placebo-controlled trial. Palmer SC, Tendal B, Mustafa RA, et al. Sodium-glucose cotransporter protein-2 SGLT-2 inhibitors and glucagon-like peptide-1 GLP-1 receptor agonists for type 2 diabetes: systematic review and network meta-analysis of randomised controlled trials. BMJ ; m Kanie T, Mizuno A, Takaoka Y, et al. Dipeptidyl peptidase-4 inhibitors, glucagon-like peptide 1 receptor agonists and sodium-glucose co-transporter-2 inhibitors for people with cardiovascular disease: a network meta-analysis. Cochrane Database Syst Rev ; CD Perkovic V, Jardine MJ, Neal B, et al. Canagliflozin and Renal Outcomes in Type 2 Diabetes and Nephropathy. Heerspink HJL, Stefánsson BV, Correa-Rotter R, et al. Dapagliflozin in Patients with Chronic Kidney Disease. Wiviott SD, Raz I, Bonaca MP, et al. Dapagliflozin and Cardiovascular Outcomes in Type 2 Diabetes. Zinman B, Wanner C, Lachin JM, et al. Empagliflozin, Cardiovascular Outcomes, and Mortality in Type 2 Diabetes. Neal B, Perkovic V, Mahaffey KW, et al. Canagliflozin and Cardiovascular and Renal Events in Type 2 Diabetes. Patorno E, Htoo PT, Glynn RJ, et al. Sodium-Glucose Cotransporter-2 Inhibitors Versus Glucagon-like Peptide-1 Receptor Agonists and the Risk for Cardiovascular Outcomes in Routine Care Patients With Diabetes Across Categories of Cardiovascular Disease. Colling C, Atlas SJ, Wexler DJ. Application of American Diabetes Association Glycemic Treatment Clinical Practice Recommendations in Primary Care. Glycemia Reduction in Type 2 Diabetes - Microvascular and Cardiovascular Outcomes. Wexler DJ, de Boer IH, Ghosh A, et al. Comparative Effects of Glucose-Lowering Medications on Kidney Outcomes in Type 2 Diabetes: The GRADE Randomized Clinical Trial. JAMA Intern Med ; Hirst JA, Farmer AJ, Dyar A, et al. Estimating the effect of sulfonylurea on HbA1c in diabetes: a systematic review and meta-analysis. Nauck MA, Kahle M, Baranov O, et al. Addition of a dipeptidyl peptidase-4 inhibitor, sitagliptin, to ongoing therapy with the glucagon-like peptide-1 receptor agonist liraglutide: A randomized controlled trial in patients with type 2 diabetes. Zaccardi F, Dhalwani NN, Dales J, et al. Comparison of glucose-lowering agents after dual therapy failure in type 2 diabetes: A systematic review and network meta-analysis of randomized controlled trials. Davies MJ, D'Alessio DA, Fradkin J, et al. Management of Hyperglycemia in Type 2 Diabetes, A Consensus Report by the American Diabetes Association ADA and the European Association for the Study of Diabetes EASD. Nathan DM, Buse JB, Davidson MB, et al. Medical management of hyperglycemia in type 2 diabetes: a consensus algorithm for the initiation and adjustment of therapy: a consensus statement of the American Diabetes Association and the European Association for the Study of Diabetes. Chiasson JL, Josse RG, Hunt JA, et al. The efficacy of acarbose in the treatment of patients with non-insulin-dependent diabetes mellitus. A multicenter controlled clinical trial. Johnston PS, Feig PU, Coniff RF, et al. Long-term titrated-dose alpha-glucosidase inhibition in non-insulin-requiring Hispanic NIDDM patients. In Brief: A new indication for colesevelam. Med Lett Drugs Ther ; Ooi CP, Loke SC. Colesevelam for type 2 diabetes mellitus. Fonseca VA, Rosenstock J, Wang AC, et al. Colesevelam HCl improves glycemic control and reduces LDL cholesterol in patients with inadequately controlled type 2 diabetes on sulfonylurea-based therapy. Goldberg RB, Fonseca VA, Truitt KE, Jones MR. Efficacy and safety of colesevelam in patients with type 2 diabetes mellitus and inadequate glycemic control receiving insulin-based therapy. Bromocriptine Cycloset for type 2 diabetes. Cincotta AH, Meier AH, Cincotta Jr M. Bromocriptine improves glycaemic control and serum lipid profile in obese Type 2 diabetic subjects: a new approach in the treatment of diabetes. Expert Opin Investig Drugs ; Gaziano JM, Cincotta AH, O'Connor CM, et al. Randomized clinical trial of quick-release bromocriptine among patients with type 2 diabetes on overall safety and cardiovascular outcomes. Rubino F, Nathan DM, Eckel RH, et al. Metabolic Surgery in the Treatment Algorithm for Type 2 Diabetes: A Joint Statement by International Diabetes Organizations. Obesity and Weight Management for the Prevention and Treatment of Type 2 Diabetes: Standards of Care in Diabetes Riddle MC, Cefalu WT, Evans PH, et al. Consensus Report: Definition and Interpretation of Remission in Type 2 Diabetes. Kirwan JP, Courcoulas AP, Cummings DE, et al. Diabetes Remission in the Alliance of Randomized Trials of Medicine Versus Metabolic Surgery in Type 2 Diabetes ARMMS-T2D. Ikramuddin S, Korner J, Lee WJ, et al. Durability of Addition of Roux-en-Y Gastric Bypass to Lifestyle Intervention and Medical Management in Achieving Primary Treatment Goals for Uncontrolled Type 2 Diabetes in Mild to Moderate Obesity: A Randomized Control Trial. Fisher DP, Johnson E, Haneuse S, et al. Association Between Bariatric Surgery and Macrovascular Disease Outcomes in Patients With Type 2 Diabetes and Severe Obesity. O'Brien R, Johnson E, Haneuse S, et al. Microvascular Outcomes in Patients With Diabetes After Bariatric Surgery Versus Usual Care: A Matched Cohort Study. Carlsson LMS, Sjöholm K, Karlsson C, et al. Long-term incidence of microvascular disease after bariatric surgery or usual care in patients with obesity, stratified by baseline glycaemic status: a post-hoc analysis of participants from the Swedish Obese Subjects study. Reynolds EL, Watanabe M, Banerjee M, et al. Mingrone G, Panunzi S, De Gaetano A, et al. Bariatric-metabolic surgery versus conventional medical treatment in obese patients with type 2 diabetes: 5 year follow-up of an open-label, single-centre, randomised controlled trial. Courcoulas AP, Belle SH, Neiberg RH, et al. Three-Year Outcomes of Bariatric Surgery vs Lifestyle Intervention for Type 2 Diabetes Mellitus Treatment: A Randomized Clinical Trial. |
| Wellness inspired. Wellness enabled. | The glycemic efficacy of sulfonylureas in combination with other oral agents is illustrated by the findings of a meta-analysis of trials in which sulfonylureas were added to oral agents predominantly metformin or thiazolidinediones [ 56 ]. A 7 , 11 Patients with prediabetes or new-onset diabetes should undertake extensive lifestyle changes to slow the progression of type 2 diabetes. Dark yellow and strong-smelling pee. Related Pathway s : Diabetes: Initial therapy for non-pregnant adults with type 2 DM. Nausea, vomiting, sense of fullness Weight loss of 1 to 4 kg 2. |
| Metformin Is Not Working: How to Tell and What to Do | Asymptomatic, minitoring catabolic — The majority of Detoxifying recipes for athletes Nut-Filled Desserts bloo diagnosed type 2 diabetes are asymptomatic, without symptoms of catabolism eg, without Nut-Filled Desserts, polydipsia, or unintentional Metformmin loss. Treatments for hyperglycemia that fails to respond to initial monotherapy or long-term medication use in type 2 diabetes are reviewed here. Fonseca VA, Rosenstock J, Wang AC, et al. Ziemer DC, Doyle JP, Barnes CS, et al. Although their use has been associated with pancreatitis, a cause and effect relationship has not been established. |
| SMBG Use and Frequency | Work with your doctor to decide the best A1C goal for you. If after taking this test your results are too high or too low, your diabetes care plan may need to be adjusted. When visiting your doctor, you might keep these questions in mind to ask during your appointment. If you have other questions about your numbers or your ability to manage your diabetes, make sure to work closely with your doctor or health care team. Skip directly to site content Skip directly to search. Español Other Languages. Monitoring Your Blood Sugar. Español Spanish Print. Minus Related Pages. Make Friends With Your Numbers. Getting an A1C Test Make sure to get an A1C test at least twice a year. Your A1C result will be reported in two ways: A1C as a percentage. Estimated average glucose eAG , in the same kind of numbers as your day-to-day blood sugar readings. Questions To Ask Your Doctor When visiting your doctor, you might keep these questions in mind to ask during your appointment. What is my target blood sugar range? How often should I check my blood sugar? What do these numbers mean? Are there patterns that show I need to change my diabetes treatment? What changes need to be made to my diabetes care plan? Top of Page. Getting Tested What is Low Blood Sugar hypoglycemia? What is High Blood Sugar hyperglycemia? Education and Support. Last Reviewed: December 30, Source: Centers for Disease Control and Prevention. Facebook Twitter LinkedIn Syndicate. home Diabetes Home. To receive updates about diabetes topics, enter your email address: Email Address. In addition, many meters now require only a very small amount of blood, thus decreasing the pain of deep wounds from the lancet. A few of the newer meters offer the option of obtaining blood samples from alternate sites, such as a forearm instead of a fingertip. This can benefit patients who find constant lancet wounds on their fingers difficult to tolerate. Although there has been concern that the accuracy of alternate site testing is inferior to detect hypoglycemia, 4 the judicious use of this alternative may help to improve adherence to an SMBG regimen. More complex meters have features to aid in identifying trends and to graph reports for more comprehensive data tracking, particularly for patients who test several times a day. Table 1 provides a summary of the more popular blood glucose meters. Recent reviews of available meters have been published elsewhere. SMBG can play an important role in improving metabolic control in patients with diabetes. It is recommended for patients treated with insulin and is desirable for all patients with diabetes. Judicious use of SMBG data can help to improve glycemic control, select an anti-diabetic regimen, and provide powerful feedback to patients wishing to improve metabolic control. Benjamin, MD, FACP, is an assistant professor of medicine at Tufts University School of Medicine and Director of Healthcare Quality at Baystate Medical Center in Springfield, Mass. Note of disclosure: Dr. Benjamin is a paid consultant to Becton Dickinson, which manufactures lancet devices. Sign In or Create an Account. Search Dropdown Menu. header search search input Search input auto suggest. filter your search All Content All Journals Clinical Diabetes. Advanced Search. User Tools Dropdown. Sign In. Skip Nav Destination Close navigation menu Article navigation. Volume 20, Issue 1. Previous Article Next Article. SMBG Use and Frequency. Recommending a Meter. Article Navigation. Practical Pointer January 01 Self-Monitoring of Blood Glucose: The Basics Evan M. Benjamin, MD, FACP Evan M. Benjamin, MD, FACP. This Site. Google Scholar. Clin Diabetes ;20 1 — Get Permissions. toolbar search Search Dropdown Menu. toolbar search search input Search input auto suggest. SMBG can aid in diabetes control by:. Table 1. Blood Glucose Meters. View large. View Large. Evans JMM, Newton RW, Ruta DA, MacDonald TM, Stevenson RJ, Morris AD: Frequency of blood glucose monitoring in relation to glycemic control: observational study with diabetes database. Franciosi M, Pellegrini F, De Bernardis G, Belfiglio M, Nicolucci A: The impact of blood glucose self-monitoring on metabolic control and quality of life in type 2 diabetic patients. Diabetes Care. Harris MI: Frequency of blood glucose monitoring in relation to glycemic control in patients with type 2 diabetes. Jungheim K, Koschinsky T: Risky delay of hypoglycemia detection by glucose monitoring at the arm. Self care of diabetes. Consumer Rep. Blood Glucose Monitors and Data Management in Buyers Guide Diabetes Forecast. American Diabetes Association. View Metrics. Email alerts Article Activity Alert. Online Ahead of Print Alert. |
| About metformin | Accessed May 1, Lewis JD, Ferrara A, Peng T, et al. Risk of bladder cancer among diabetic patients treated with pioglitazone: interim report of a longitudinal cohort study. Neumann A, Weill A, Ricordeau P, Fagot JP, Alla F, Allemand H. Pioglitazone and risk of bladder cancer among diabetic patients in France: a population-based cohort study. Kahn SE, Zinman B, Lachin JM, et al. Rosiglitazone-associated fractures in type 2 diabetes: an analysis from A Diabetes Outcome Progression Trial ADOPT. Loke YK, Singh S, Furberg CD. Long-term use of thiazolidinediones and fractures in type 2 diabetes: a meta-analysis. Aubert RE, Herrera V, Chen W, Haffner SM, Pendergrass M. Rosiglitazone and pioglitazone increase fracture risk in women and men with type 2 diabetes. Bazelier MT, Gallagher AM, van Staa TP, et al. Use of thiazolidinediones and risk of osteoporotic fracture: disease or drugs?. Pharmacoepidemiol Drug Saf. Accessed July 9, Pramlintide acetate. Accessed July 8, Garber AJ, Abrahamson MJ, Barzilay JI, et al. AACE comprehensive diabetes management algorithm Endocr Pract. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes UKPDS Implications of the United Kingdom Prospective Diabetes Study. Ewart RM. The case against aggressive treatment of type 2 diabetes: critique of the UK prospective diabetes study. McCormack J, Greenhalgh T. Seeing what you want to see in randomised controlled trials: versions and perversions of UKPDS data. Shaughnessy AF, Slawson DC. What happened to the valid POEMs? A survey of review articles on the treatment of type 2 diabetes. Stratton IM, Adler AI, Neil HA, et al. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes UKPDS 35 : prospective observational study. Gerstein HC, Miller ME, Byington RP, et al. Effects of intensive glucose lowering in type 2 diabetes. Patel A, MacMahon S, Chalmers J, et al. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. Duckworth W, Abraira C, Moritz T, et al. Glucose control and vascular complications in veterans with type 2 diabetes [published correction appears in N Engl J Med. Hemmingsen B, Lund SS, Gluud C, et al. Intensive glycaemic control for patients with type 2 diabetes: systematic review with meta-analysis and trial sequential analysis of randomised clinical trials. Currie CJ, Peters JR, Tynan A, et al. Survival as a function of HbA 1c in people with type 2 diabetes: a retrospective cohort study. Malanda UL, Welschen LM, Riphagen II, Dekker JM, Nijpels G, Bot SD. Self-monitoring of blood glucose in patients with type 2 diabetes mellitus who are not using insulin. Farmer AJ, Perera R, Ward A, et al. Meta-analysis of individual patient data in randomised trials of self monitoring of blood glucose in people with non-insulin treated type 2 diabetes. This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. search close. PREV Jul 1, NEXT. A 7 , 11 Patients with prediabetes or new-onset diabetes should undertake extensive lifestyle changes to slow the progression of type 2 diabetes. A 2 — 5 Patients with existing cardiovascular disease, two or more cardiovascular disease risk factors, or duration of diabetes of 10 years or more should have higher A1C goals because of a lack of benefit and the potential for increased risk of mortality compared with lower A1C goals. A 39 — 41 Self-monitoring of blood glucose levels for patients taking noninsulin therapies does not significantly affect glycemic control. Society of General Internal Medicine Avoid routine multiple daily self-glucose monitoring in adults with stable type 2 diabetes on agents that do not cause hypoglycemia. Am Fam Physician. Knowler WC, Barrett-Connor E, Fowler SE, et al. Lifestyle Management. Management of Blood Glucose Levels. GLUCAGON-LIKE PEPTIDE-1 RECEPTOR AGONISTS. Approach to the Patient. A1C GOALS. CHRISTA M. GEORGE, PharmD, BCPS, BCACP, is an associate professor of clinical pharmacy and family medicine at the University of Tennessee Health Science Center College of Pharmacy in Memphis. BRUIJN, MD, MPH, FAAFP, is an assistant professor of family medicine at the University of Tennessee Health Science Center. George, PharmD, University of Tennessee Health Science Center, College of Pharmacy, Madison Ave. Continue Reading. More in AFP. More in Pubmed. Copyright © by the American Academy of Family Physicians. Copyright © American Academy of Family Physicians. All Rights Reserved. Metformin should be used as first-line therapy to reduce microvascular complications, assist in weight management, reduce the risk of cardiovascular events, and reduce the risk of mortality in patients with type 2 diabetes mellitus. Patients with prediabetes or new-onset diabetes should undertake extensive lifestyle changes to slow the progression of type 2 diabetes. Patients with existing cardiovascular disease, two or more cardiovascular disease risk factors, or duration of diabetes of 10 years or more should have higher A1C goals because of a lack of benefit and the potential for increased risk of mortality compared with lower A1C goals. Self-monitoring of blood glucose levels for patients taking noninsulin therapies does not significantly affect glycemic control. Do not recommend daily home finger glucose testing in patients with type 2 diabetes mellitus not using insulin. Judicious use of SMBG data can help to improve glycemic control, select an anti-diabetic regimen, and provide powerful feedback to patients wishing to improve metabolic control. Benjamin, MD, FACP, is an assistant professor of medicine at Tufts University School of Medicine and Director of Healthcare Quality at Baystate Medical Center in Springfield, Mass. Note of disclosure: Dr. Benjamin is a paid consultant to Becton Dickinson, which manufactures lancet devices. Sign In or Create an Account. Search Dropdown Menu. header search search input Search input auto suggest. filter your search All Content All Journals Clinical Diabetes. Advanced Search. User Tools Dropdown. Sign In. Skip Nav Destination Close navigation menu Article navigation. Volume 20, Issue 1. Previous Article Next Article. SMBG Use and Frequency. Recommending a Meter. Article Navigation. Practical Pointer January 01 Self-Monitoring of Blood Glucose: The Basics Evan M. Benjamin, MD, FACP Evan M. Benjamin, MD, FACP. This Site. Google Scholar. Clin Diabetes ;20 1 — Get Permissions. toolbar search Search Dropdown Menu. toolbar search search input Search input auto suggest. SMBG can aid in diabetes control by:. Table 1. Blood Glucose Meters. View large. View Large. Evans JMM, Newton RW, Ruta DA, MacDonald TM, Stevenson RJ, Morris AD: Frequency of blood glucose monitoring in relation to glycemic control: observational study with diabetes database. Franciosi M, Pellegrini F, De Bernardis G, Belfiglio M, Nicolucci A: The impact of blood glucose self-monitoring on metabolic control and quality of life in type 2 diabetic patients. Diabetes Care. Harris MI: Frequency of blood glucose monitoring in relation to glycemic control in patients with type 2 diabetes. Drug information provided by: Merative, Micromedex ®. Metformin is used to treat high blood sugar levels that are caused by a type of diabetes mellitus or sugar diabetes called type 2 diabetes. With this type of diabetes, insulin produced by the pancreas is not able to get sugar into the cells of the body where it can work properly. Using metformin alone, with a type of oral antidiabetic medicine called a sulfonylurea, or with insulin, will help to lower blood sugar when it is too high and help restore the way you use food to make energy. Many people can control type 2 diabetes with diet and exercise. Following a specially planned diet and exercise will always be important when you have diabetes, even when you are taking medicines. To work properly, the amount of metformin you take must be balanced against the amount and type of food you eat and the amount of exercise you do. If you change your diet or exercise, you will want to test your blood sugar to find out if it is too low. Your doctor will teach you what to do if this happens. Metformin does not help patients who have insulin-dependent or type 1 diabetes because they cannot produce insulin from their pancreas gland. Their blood glucose is best controlled by insulin injections. In deciding to use a medicine, the risks of taking the medicine must be weighed against the good it will do. This is a decision you and your doctor will make. For this medicine, the following should be considered:. Tell your doctor if you have ever had any unusual or allergic reaction to this medicine or any other medicines. Also tell your health care professional if you have any other types of allergies, such as to foods, dyes, preservatives, or animals. For non-prescription products, read the label or package ingredients carefully. Appropriate studies performed to date have not demonstrated pediatric-specific problems that would limit the usefulness of metformin oral solution, extended-release oral suspension, and tablets in children 10 to 16 years of age. However, safety and efficacy of metformin extended-release tablets in the pediatric population have not been established. Although appropriate studies on the relationship of age to the effects of metformin have not been performed in the geriatric population, geriatric-specific problems are not expected to limit the usefulness of metformin in the elderly. However, elderly patients are more likely to have age-related kidney problems, which may require caution in patients receiving metformin. This medicine is not recommended in patients 80 years of age and older who have kidney problems. There are no adequate studies in women for determining infant risk when using this medication during breastfeeding. Weigh the potential benefits against the potential risks before taking this medication while breastfeeding. Although certain medicines should not be used together at all, in other cases two different medicines may be used together even if an interaction might occur. In these cases, your doctor may want to change the dose, or other precautions may be necessary. When you are taking this medicine, it is especially important that your healthcare professional know if you are taking any of the medicines listed below. The following interactions have been selected on the basis of their potential significance and are not necessarily all-inclusive. Using this medicine with any of the following medicines is usually not recommended, but may be required in some cases. If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines. Using this medicine with any of the following medicines may cause an increased risk of certain side effects, but using both drugs may be the best treatment for you. Certain medicines should not be used at or around the time of eating food or eating certain types of food since interactions may occur. Using alcohol or tobacco with certain medicines may also cause interactions to occur. The presence of other medical problems may affect the use of this medicine. Make sure you tell your doctor if you have any other medical problems, especially:. This medicine usually comes with a patient information insert. Read the information carefully and make sure you understand it before taking this medicine. |
Ich werde besser einfach stillschweigen
Es ist die ausgezeichnete Idee
sehr neugierig topic