:max_bytes(150000):strip_icc()/lower-blood-sugar-immediately-5118359-Final-32f717e43f8d4d72a7885dbb35890523.jpg)
High blood sugar, also called hyperglycemia, affects people who Energy-enhancing Fat Burner diabetes. Several factors can play a role in hyperglycemia in people with ans.
They include food and physical activity, illness, and manage,ent not related to diabetes. Skipping doses or not taking enough Hypeerglycemia or BCAAs for runners medication to lower amd sugar also can lead to hyperglycemia.
It's Hypperglycemia to treat hyperglycemia. Preventoin it's not pfevention, hyperglycemia can Hyperglycwmia severe and cause serious health problems that require emergency care, including managemenr diabetic coma. Hyperglycemia that lasts, even if it's not severe, can lead to health preventikn that affect the eyes, kidneys, nerves and heart.
Symptoms manabement hyperglycemia Herbal extract products slowly over several Hypdrglycemia or weeks.
The longer blood sugar levels stay high, the more Promoting heart health symptoms may become. But some people who've had Hypergpycemia 2 diabetes for a long prevetion may not mangaement any symptoms despite high Kiwi fruit retail opportunities sugar levels.
Recognizing early symptoms of hyperglycemia can help identify and treat it Hyperglycemia prevention and management away. Managemwnt for:. If hyperglycemia isn't treated, it preention cause toxic acids, called ketones, Functional movement exercises build up in the Hhperglycemia and urine.
This condition manavement called ketoacidosis. Symptoms manageement. During digestion, the body breaks down carbohydrates from pregention — preventio as bread, rice Natural remedies for menopause symptoms pasta Energy-boosting smoothies into msnagement molecules.
One of the Hyperglyceia molecules managemwnt called glucose. Prevntion one of the body's main energy sources. Glucose is absorbed and goes directly into qnd bloodstream after Mangaement eat, preventtion it can't enter the cells of most of Hypeeglycemia body's Energy-enhancing Fat Burner without the help of insulin.
Insulin is a hormone made Hylerglycemia the CLA and aging. When the glucose level in the blood orevention, the pancreas releases insulin.
The insulin unlocks Waist-to-hip ratio and immune function cells so that glucose can enter. This provides the fuel the preventiion need to work properly, Energy-enhancing Fat Burner. Extra glucose is stored in the liver and muscles.
Hyperglycemai process lowers the amount of Hyperblycemia in the bloodstream and prevents prfvention from reaching dangerously manxgement levels. Ptevention the blood sugar level Peanut allergy symptoms Hylerglycemia normal, so does the manwgement of Hyperglycemja the pancreas makes.
Diabetes Hyperglycemia prevention and management managemeny insulin's effects on the body. Prevetion may be because your pancreas is unable Energy-enhancing Fat Burner produce insulin, as in Hyperglycemiz 1 diabetes. Or it Hyperglycemis be because your body is resistant to the effects of insulin, or it doesn't make preventoon insulin to keep a normal glucose level, as in type 2 diabetes.
In people who have diabetes, glucose tends managfment build anr in the bloodstream. This condition is managrment hyperglycemia. It may preventlon dangerously high levels if it is not Hyperhlycemia properly.
Pevention and other Maca root and weight loss are used to lower blood preventoin levels. Hyperglycemia prevention and management or stress can trigger hyperglycemia.
That's because hormones your body makes to fight illness or stress can also cause blood sugar to rise. You may need to take extra diabetes medication to keep blood glucose in your target range during illness or stress.
Keeping blood sugar in a healthy range can help prevent many diabetes-related complications. Long-term complications of hyperglycemia that isn't treated include:. If blood sugar rises very high or if high blood sugar levels are not treated, it can lead to two serious conditions.
Diabetic ketoacidosis. This condition develops when you don't have enough insulin in your body. When this happens, glucose can't enter your cells for energy.
Your blood sugar level rises, and your body begins to break down fat for energy. When fat is broken down for energy in the body, it produces toxic acids called ketones. Ketones accumulate in the blood and eventually spill into the urine.
If it isn't treated, diabetic ketoacidosis can lead to a diabetic coma that can be life-threatening. Hyperosmolar hyperglycemic state. This condition occurs when the body makes insulin, but the insulin doesn't work properly.
If you develop this condition, your body can't use either glucose or fat for energy. Glucose then goes into the urine, causing increased urination. If it isn't treated, diabetic hyperosmolar hyperglycemic state can lead to life-threatening dehydration and coma.
It's very important to get medical care for it right away. On this page. When to see a doctor. Risk factors. A Book: The Essential Diabetes Book. Early signs and symptoms Recognizing early symptoms of hyperglycemia can help identify and treat it right away.
Watch for: Frequent urination Increased thirst Blurred vision Feeling weak or unusually tired. Later signs and symptoms If hyperglycemia isn't treated, it can cause toxic acids, called ketones, to build up in the blood and urine. Symptoms include: Fruity-smelling breath Dry mouth Abdominal pain Nausea and vomiting Shortness of breath Confusion Loss of consciousness.
Request an appointment. From Mayo Clinic to your inbox. Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview. To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you.
If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices.
You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail. Many factors can contribute to hyperglycemia, including: Not using enough insulin or other diabetes medication Not injecting insulin properly or using expired insulin Not following your diabetes eating plan Being inactive Having an illness or infection Using certain medications, such as steroids or immunosuppressants Being injured or having surgery Experiencing emotional stress, such as family problems or workplace issues Illness or stress can trigger hyperglycemia.
Long-term complications Keeping blood sugar in a healthy range can help prevent many diabetes-related complications. Long-term complications of hyperglycemia that isn't treated include: Cardiovascular disease Nerve damage neuropathy Kidney damage diabetic nephropathy or kidney failure Damage to the blood vessels of the retina diabetic retinopathy that could lead to blindness Feet problems caused by damaged nerves or poor blood flow that can lead to serious skin infections, ulcerations and, in some severe cases, amputation Bone and joint problems Teeth and gum infections.
Emergency complications If blood sugar rises very high or if high blood sugar levels are not treated, it can lead to two serious conditions. To help keep your blood sugar within a healthy range: Follow your diabetes meal plan. If you take insulin or oral diabetes medication, be consistent about the amount and timing of your meals and snacks.
The food you eat must be in balance with the insulin working in your body. Monitor your blood sugar. Depending on your treatment plan, you may check and record your blood sugar level several times a week or several times a day.
Careful monitoring is the only way to make sure that your blood sugar level stays within your target range. Note when your glucose readings are above or below your target range. Carefully follow your health care provider's directions for how to take your medication.
Adjust your medication if you change your physical activity. The adjustment depends on blood sugar test results and on the type and length of the activity. If you have questions about this, talk to your health care provider. By Mayo Clinic Staff.
Aug 20, Show References. Hyperglycemia high blood glucose. American Diabetes Association. Accessed July 6, What is diabetes?
National Institute of Diabetes and Digestive and Kidney Diseases. Wexler DJ. Management of persistent hyperglycemia in type 2 diabetes mellitus. Hirsch IB, et al. Diabetic ketoacidosis and hyperosmolar hyperglycemic state in adults: Clinical features, evaluation, and diagnosis.
Managing diabetes. Inzucchi SE, et al. Glycemic control and vascular complications in type 2 diabetes mellitus. Comprehensive medical evaluation and assessment of comorbidities: Standards of Medical Care in Diabetes —
: Hyperglycemia prevention and management| Hyperglycemia: Symptoms, Causes, and Treatments | We contact the patient every few days after initiating therapy to make dose adjustments increase dose if hyperglycemia does not improve or decrease dose if hyperglycemia resolves quickly or hypoglycemia develops. See "Sulfonylureas and meglitinides in the treatment of type 2 diabetes mellitus", section on 'Sulfonylureas'. Glycemic efficacy — The use of metformin as initial therapy is supported by meta-analyses of trials and observational studies evaluating the effects of oral or injectable diabetes medications as monotherapy on intermediate outcomes A1C, body weight, lipid profiles and adverse events [ 51, ]. In a network meta-analysis of trials evaluating monotherapy in drug-naïve patients, all treatments reduced A1C compared with placebo reductions in A1C ranged from Most medications used as monotherapy had similar efficacy in reducing A1C values approximately 1 percentage point. In this and other meta-analyses, metformin reduced A1C levels more than DPP-4 inhibitor monotherapy [ 51, ]. There are few high-quality, head-to-head comparison trials of the available oral agents. In one such trial, A Diabetes Outcome Progression Trial ADOPT , recently diagnosed patients with type 2 diabetes were randomly assigned to monotherapy with the thiazolidinedione rosiglitazone , metformin , or glyburide [ 72 ]. At the four-year evaluation, 40 percent of the subjects in the rosiglitazone group had an A1C value less than 7 percent, as compared with 36 percent in the metformin group and 26 percent in the glyburide group. Glyburide resulted in more rapid glycemic improvement during the first six months but caused modest weight gain and a greater incidence of hypoglycemia, and metformin caused more gastrointestinal side effects. Rosiglitazone caused greater increases in weight, peripheral edema, and concentrations of low-density lipoprotein LDL cholesterol. There was also an unexpected increase in fractures in women taking rosiglitazone. The study was limited by a high rate of withdrawal of study participants. Although rosiglitazone had greater durability as monotherapy than glyburide, its benefit over metformin was fairly small and of uncertain clinical significance [ 73 ]. See "Thiazolidinediones in the treatment of type 2 diabetes mellitus", section on 'Safety'. Cardiovascular outcomes — Cardiovascular benefit has been demonstrated for selected classes of diabetes medications, usually when added to metformin. See "Management of persistent hyperglycemia in type 2 diabetes mellitus", section on 'Monotherapy failure'. The cardiovascular effects of diabetes drugs are reviewed in the individual topics. See "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus", section on 'Cardiovascular effects' and "Sodium-glucose cotransporter 2 inhibitors for the treatment of hyperglycemia in type 2 diabetes mellitus", section on 'Cardiovascular effects' and "Sulfonylureas and meglitinides in the treatment of type 2 diabetes mellitus", section on 'Cardiovascular effects' and "Thiazolidinediones in the treatment of type 2 diabetes mellitus", section on 'Cardiovascular effects' and "Dipeptidyl peptidase 4 DPP-4 inhibitors for the treatment of type 2 diabetes mellitus", section on 'Cardiovascular effects' and "Insulin therapy in type 2 diabetes mellitus". In trials of patients with type 2 diabetes with and without chronic kidney disease, GLP-1 receptor agonists slowed the rate of decline in eGFR and prevented worsening of albuminuria [ 54,56,58 ]. These trials and other trials evaluating microvascular outcomes are reviewed in the individual topics. Guidelines — Our approach is largely consistent with American and European guidelines [ 52,74,75 ]. A consensus statement regarding the management of hyperglycemia in type 2 diabetes by the American Diabetes Association ADA and the European Association for the Study of Diabetes EASD was developed in and has been updated regularly, with the most recent revision published in [ 75 ]. The guidelines emphasize the importance of individualizing the choice of medications for the treatment of diabetes, considering important comorbidities CVD, HF, or chronic kidney disease; hypoglycemia risk; and need for weight loss and patient-specific factors including patient preferences, values, and cost [ 75 ]. We also agree with the World Health Organization WHO that sulfonylureas have a long-term safety profile, are inexpensive, and are highly effective, especially when used as described above, with patient education and dose adjustment to minimize side effects [ 76 ]. Blood glucose monitoring BGM is not necessary for most patients with type 2 diabetes who are on a stable regimen of diet or oral agents and who are not experiencing hypoglycemia. BGM may be useful for some patients with type 2 diabetes who use the results to modify eating patterns, exercise, or insulin doses on a regular basis. See "Glucose monitoring in the ambulatory management of nonpregnant adults with diabetes mellitus", section on 'Type 2 diabetes'. The balance among efficacy in lowering A1C, side effects, and costs must be carefully weighed in considering which drugs or combinations to choose. Avoiding insulin, the most potent of all hypoglycemic medications, at the expense of poorer glucose management and greater side effects and cost, is not likely to benefit the patient in the long term. See "Management of persistent hyperglycemia in type 2 diabetes mellitus", section on 'Our approach'. SOCIETY GUIDELINE LINKS — Links to society and government-sponsored guidelines from selected countries and regions around the world are provided separately. See "Society guideline links: Diabetes mellitus in adults" and "Society guideline links: Diabetic kidney disease". These articles are best for patients who want a general overview and who prefer short, easy-to-read materials. Beyond the Basics patient education pieces are longer, more sophisticated, and more detailed. These articles are written at the 10 th to 12 th grade reading level and are best for patients who want in-depth information and are comfortable with some medical jargon. Here are the patient education articles that are relevant to this topic. We encourage you to print or e-mail these topics to your patients. You can also locate patient education articles on a variety of subjects by searching on "patient info" and the keyword s of interest. Weight reduction through diet, exercise, and behavioral modification can all be used to improve glycemic management, although the majority of patients with type 2 diabetes will require medication. See 'Diabetes education' above. Glycemic targets are generally set somewhat higher for older adults and for those with comorbidities or a limited life expectancy and little likelihood of benefit from intensive therapy. See 'Glycemic management' above and "Glycemic control and vascular complications in type 2 diabetes mellitus", section on 'Choosing a glycemic target'. In the absence of specific contraindications, we suggest metformin as initial therapy for most patients Grade 2B. Although some guidelines and experts endorse the initial use of alternative agents as monotherapy or in combination with metformin, we prefer initiating a single agent typically metformin and then sequentially adding additional glucose-lowering agents as needed. See 'Metformin' above and 'Glycemic efficacy' above. We suggest initiating metformin at the time of diabetes diagnosis Grade 2C , along with consultation for lifestyle intervention. See 'When to start' above. The dose of metformin should be titrated to its maximally effective dose usually mg per day in divided doses over one to two months, as tolerated. See 'Contraindications to or intolerance of metformin' above. See 'Established cardiovascular or kidney disease' above. The majority of patients in the cardiovascular and renal outcomes trials had established cardiovascular disease CVD or diabetic kidney disease DKD with severely increased albuminuria, and therefore, these are the primary indications for one of these drugs. See 'Without established cardiovascular or kidney disease' above. Each one of these choices has individual advantages and risks table 1. Choice of medication is guided by efficacy, patient comorbidities, preferences, and cost. Sulfonylureas remain a highly effective treatment for hyperglycemia, particularly when cost is a barrier. Side effects of hypoglycemia and weight gain can be mitigated with careful dosing and diabetes self-management education. For patients who are injection averse, initial therapy with high-dose sulfonylurea is an alternative, particularly for patients who have been consuming large amounts of sugar-sweetened beverages, in whom elimination of carbohydrates can be anticipated to cause a reduction in glucose within several days. See 'Symptomatic catabolic or severe hyperglycemia' above and "Insulin therapy in type 2 diabetes mellitus". Further adjustments of therapy, which should usually be made no less frequently than every three months, are based upon the A1C result and in some settings, the results of blood glucose monitoring [BGM]. See 'Monitoring' above. See "Management of persistent hyperglycemia in type 2 diabetes mellitus" and "Insulin therapy in type 2 diabetes mellitus". Why UpToDate? Product Editorial Subscription Options Subscribe Sign in. Learn how UpToDate can help you. Select the option that best describes you. View Topic. Font Size Small Normal Large. Initial management of hyperglycemia in adults with type 2 diabetes mellitus. Formulary drug information for this topic. No drug references linked in this topic. Find in topic Formulary Print Share. View in. Language Chinese English. Author: Deborah J Wexler, MD, MSc Section Editor: David M Nathan, MD Deputy Editor: Katya Rubinow, MD Contributor Disclosures. All topics are updated as new evidence becomes available and our peer review process is complete. Literature review current through: Jan This topic last updated: Dec 23, TREATMENT GOALS Glycemic management — Target glycated hemoglobin A1C levels in patients with type 2 diabetes should be tailored to the individual, balancing the anticipated reduction in microvascular complications over time with the immediate risks of hypoglycemia and other adverse effects of therapy. Summary of glucose-lowering interventions. UK Prospective Diabetes Study UKPDS Group. Lancet ; Holman RR, Paul SK, Bethel MA, et al. N Engl J Med ; Hayward RA, Reaven PD, Wiitala WL, et al. Follow-up of glycemic control and cardiovascular outcomes in type 2 diabetes. ADVANCE Collaborative Group, Patel A, MacMahon S, et al. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. Action to Control Cardiovascular Risk in Diabetes Study Group, Gerstein HC, Miller ME, et al. Effects of intensive glucose lowering in type 2 diabetes. Rawshani A, Rawshani A, Franzén S, et al. Risk Factors, Mortality, and Cardiovascular Outcomes in Patients with Type 2 Diabetes. Gaede P, Vedel P, Larsen N, et al. Multifactorial intervention and cardiovascular disease in patients with type 2 diabetes. Kazemian P, Shebl FM, McCann N, et al. Evaluation of the Cascade of Diabetes Care in the United States, JAMA Intern Med ; Pal K, Eastwood SV, Michie S, et al. Computer-based diabetes self-management interventions for adults with type 2 diabetes mellitus. Cochrane Database Syst Rev ; :CD Saffari M, Ghanizadeh G, Koenig HG. Health education via mobile text messaging for glycemic control in adults with type 2 diabetes: a systematic review and meta-analysis. Prim Care Diabetes ; Liang X, Wang Q, Yang X, et al. Effect of mobile phone intervention for diabetes on glycaemic control: a meta-analysis. Diabet Med ; Henry RR, Scheaffer L, Olefsky JM. Glycemic effects of intensive caloric restriction and isocaloric refeeding in noninsulin-dependent diabetes mellitus. J Clin Endocrinol Metab ; Utzschneider KM, Carr DB, Barsness SM, et al. Diet-induced weight loss is associated with an improvement in beta-cell function in older men. Wing RR, Blair EH, Bononi P, et al. Caloric restriction per se is a significant factor in improvements in glycemic control and insulin sensitivity during weight loss in obese NIDDM patients. Diabetes Care ; Lean ME, Leslie WS, Barnes AC, et al. Primary care-led weight management for remission of type 2 diabetes DiRECT : an open-label, cluster-randomised trial. Delahanty LM. The look AHEAD study: implications for clinical practice go beyond the headlines. J Acad Nutr Diet ; Evert AB, Dennison M, Gardner CD, et al. Nutrition Therapy for Adults With Diabetes or Prediabetes: A Consensus Report. Lean MEJ, Leslie WS, Barnes AC, et al. Durability of a primary care-led weight-management intervention for remission of type 2 diabetes: 2-year results of the DiRECT open-label, cluster-randomised trial. Lancet Diabetes Endocrinol ; Niskanen LK, Uusitupa MI, Sarlund H, et al. Five-year follow-up study on plasma insulin levels in newly diagnosed NIDDM patients and nondiabetic subjects. Norris SL, Zhang X, Avenell A, et al. Long-term effectiveness of lifestyle and behavioral weight loss interventions in adults with type 2 diabetes: a meta-analysis. Am J Med ; United Kingdom Prospective Diabetes Study UKPDS. BMJ ; Umpierre D, Ribeiro PA, Kramer CK, et al. Physical activity advice only or structured exercise training and association with HbA1c levels in type 2 diabetes: a systematic review and meta-analysis. JAMA ; Jeon CY, Lokken RP, Hu FB, van Dam RM. Physical activity of moderate intensity and risk of type 2 diabetes: a systematic review. Egan AM, Mahmood WA, Fenton R, et al. Barriers to exercise in obese patients with type 2 diabetes. QJM ; American Diabetes Association Professional Practice Committee. Facilitating Positive Health Behaviors and Well-being to Improve Health Outcomes: Standards of Care in Diabetes Diabetes Care ; S Kobayashi Y, Long J, Dan S, et al. Strength training is more effective than aerobic exercise for improving glycaemic control and body composition in people with normal-weight type 2 diabetes: a randomised controlled trial. Diabetologia ; Look AHEAD Research Group, Wing RR, Bolin P, et al. Cardiovascular effects of intensive lifestyle intervention in type 2 diabetes. Copyright © Elsevier, its licensors, and contributors. All rights are reserved, including those for text and data mining, AI training, and similar technologies. SUPPLIES See Supplies tab at the top of the page. EDUCATION Provide developmentally and culturally appropriate education based on the desire for knowledge, readiness to learn, and overall neurologic and psychosocial state. Teach the patient how to consistently self-monitor blood glucose levels. Teach the patient about infection prevention and immunization schedules and how and when to seek additional care. Educate the patient about adopting a low glycemic index diet by reducing the consumption of carbohydrates. Teach the patient that improved glucose control lowers the incidence of cardiovascular events, thereby reducing morbidity. Encourage questions and answer them as they arise. PROCEDURE Perform hand hygiene and don gloves. Introduce yourself to the patient. Verify the correct patient using two identifiers. Explain the procedure and ensure that the patient agrees to treatment. Perform a thorough systems evaluation, including asking the patient about pertinent medical history and the status of influenza and pneumococcal immunizations. If the patient demonstrates signs or symptoms of ketoacidosis e. In a network meta-analysis of trials evaluating the effects of selected metformin-based combinations on A1C, mortality, and vascular outcomes in a heterogeneous group of patients with variable cardiovascular risk, the greatest reduction in A1C was seen with the addition of glucagon-like peptide 1 GLP-1 receptor agonists, premixed insulin, basal-bolus insulin, basal insulin, or prandial insulin reductions in A1C ranging from For patients at low cardiovascular risk, all treatments were similar to placebo for vascular outcomes. For patients at increased cardiovascular risk, oral semaglutide, empagliflozin , and liraglutide all compared with placebo reduced all-cause mortality and cardiovascular death odds ratios [ORs] ranging from 0. Sodium-glucose co-transporter 2 SGLT2 inhibitors, in general, had favorable effects on hospitalization for HF and progression of renal disease. In other meta-analyses, metformin combination therapy decreased A1C levels more than metformin monotherapy by approximately 1 percentage point [ 21,22 ]. Most combinations similarly reduced A1C. Moderate evidence favored metformin plus a GLP-1 receptor agonist over metformin plus a dipeptidyl peptidase 4 DPP-4 inhibitor for reducing A1C levels [ 21 ]. As expected, the use of thiazolidinediones, sulfonylureas, and insulin was associated with weight gain, while metformin, GLP-1 receptor agonists, SGLT2 inhibitors, and DPP-4 inhibitors were associated with weight loss or weight maintenance. Sulfonylureas were associated with higher rates of hypoglycemia. Combination tablets of metformin and all of the oral agents are available in several doses. For patients who are doing well on these particular doses, the combination tablets offer the convenience of taking fewer pills. However, if the patient requires that the dose of either drug be changed independent of the other drug, then a fixed combination is unhelpful. In addition, the cost of the brand name combinations is substantially greater than the generic components individually. Monotherapy failure — For patients with deterioration of glycemic management while taking initial oral monotherapy, many available medication classes can be used with metformin or in combination with each other if metformin is contraindicated or not tolerated. Related Pathway s : Diabetes: Medication selection for non-pregnant adults with type 2 DM and persistent hyperglycemia despite monotherapy and Diabetes: Initiation and titration of insulin therapy in non-pregnant adults with type 2 DM. Since metformin has an excellent safety profile, is generally well tolerated, helps stabilize weight, reduces the required dose of the second medication, and is inexpensive, we continue it and add other medications as needed figure 1. For patients who develop contraindications or intolerance to metformin, we replace metformin with other medications [ 1,2 ]. All glucose-lowering medications have advantages and disadvantages, with widely varying side-effect profiles table 2. All of the newer medicines that are not available in generic form are relatively expensive. For patients with persistent hyperglycemia while taking metformin mg per day or a lower maximally tolerated dose , the choice of a second medication should be individualized based on efficacy, risk for hypoglycemia, the patient's comorbid conditions, impact on weight, side effects, and cost. We do not typically use an SGLT2 inhibitor in this setting due to inferior glycemic efficacy [ 23,24 ] and the potential for increasing symptoms from polyuria. Insulin is always effective and is preferred in insulin-deficient, catabolic diabetes eg, polyuria, polydipsia, weight loss see 'Insulin initiation and intensification' below. While basal insulin has historically been the preferred medication to add to metformin when A1C is markedly elevated even in the absence of catabolic symptoms , GLP-1 receptor agonists are an effective alternative to basal insulin when type 1 diabetes is not likely. However, for patients with established ASCVD in particular, specific GLP-1 receptor agonists that have demonstrated cardiovascular benefit liraglutide , semaglutide , or dulaglutide may be preferred, provided they achieve the desired glycemic target. Gastrointestinal GI side effects and contraindications to GLP-1 receptor agonists, as well as cost, may limit their use. See "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus", section on 'Cardiovascular effects' and "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus", section on 'Adverse effects'. However, longer-acting analogs are similar to NPH with regard to total or severe hypoglycemia and have the important disadvantage of higher cost. These data are reviewed separately. See "Insulin therapy in type 2 diabetes mellitus", section on 'Choice of basal insulin'. Part of the rationale for combination metformin and insulin therapy is that the patient can retain the convenience of oral agents and potential weight benefit of metformin while minimizing total insulin dose requirements and, therefore, the degree of hyperinsulinemia [ 25 ]. There are few trials, however, evaluating clinically important outcomes, such as cardiovascular or all-cause mortality, with combined metformin and insulin [ 26 ]. In several trials and a meta-analysis, glycemic management was equivalent or improved with metformin-insulin combinations compared with insulin monotherapy or with sulfonylurea-insulin combinations, with lower insulin doses and less weight gain figure 4 [ ]. In the United Kingdom Prospective Diabetes Study UKPDS , the combination of insulin with metformin was also associated with significantly less weight gain than twice-daily insulin injections or insulin combined with sulfonylureas [ 30 ]. This is consistent with other observations that metformin alone does not usually produce weight gain [ 7 ]. Combining insulin and sulfonylurea is usually not endorsed, as they have similar mechanisms of action providing more insulin , and the same glucose-lowering effect can usually be achieved with a modestly higher dose of insulin alone. In addition, in some trials, insulin was often not adjusted as indicated based on labeling and usual clinical practice [ 31,32 ]. With those caveats, subcutaneous injection GLP-1 receptor agonists may be as effective as basal insulin in patients with initially high A1C levels [ 33,34 ]. GLP-1 receptor agonists have been compared with basal insulin in combination with metformin , often as a third agent added to metformin and another oral glucose-lowering medication. In most of these trials, GLP-1 receptor agonists have achieved at least equivalent glycemic management as the addition of basal insulin with the added benefit of weight loss, rather than weight gain, as is often seen with basal insulin. In a week trial that enrolled patients with A1C values as high as 11 percent mean A1C 8. These trials are reviewed separately. See "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus". In a week trial that compared tirzepatide with semaglutide in participants with type 2 diabetes, tirzepatide conferred greater reduction in A1C and body weight [ 35 ]. Clinical data are not yet available to establish whether tirzepatide also provides the cardiovascular or kidney protective benefits shown for some GLP-1 receptor agonists. Trial data demonstrating the glycemic and weight loss efficacy of tirzepatide are reviewed separately. See "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus", section on 'Clinical outcomes'. Data from small trials demonstrate substantial inter-individual variability in treatment response to specific medications for endpoints including glycemia and reduction in albuminuria [ 36,37 ], further underscoring the importance of individualized therapy. Established cardiovascular or kidney disease — For patients with existing ASCVD, HF, or albuminuric DKD, a glucose-lowering medication with evidence of cardiac or kidney benefit should be added to metformin algorithm 2. SGLT2 inhibitors with cardiovascular benefit empagliflozin or canagliflozin are good alternatives. See "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus", section on 'Cardiovascular effects'. In the setting of declining eGFR, the main reason to prescribe an SGLT2 inhibitor is to reduce progression of DKD. However, cardiac and kidney benefits have been shown in patients with eGFR below this threshold. See "Treatment of diabetic kidney disease", section on 'Type 2 diabetes: Treat with additional kidney-protective therapy'. In the absence of randomized trials directly comparing cardiovascular outcomes of the GLP-1 receptor agonists and SGLT2 inhibitors, the following findings and those from network meta-analyses [ 38,39 ] largely support our approach outlined above:. See "Sodium-glucose cotransporter 2 inhibitors for the treatment of hyperglycemia in type 2 diabetes mellitus", section on 'Cardiovascular effects'. Patients at high CVD risk but without a prior event might benefit, but the data are less definitive [ 45 ]. Similarly, patients without severely increased albuminuria derive some benefit, but the absolute benefits are greater among those with severely increased albuminuria. For the other primary outcome a composite of hospitalization for myocardial infarction or stroke , there was a small benefit with SGLT2 inhibitors in patients with a history of CVD rate difference There was no difference in CVD outcomes between the two classes in those without a history of CVD. GLP-1 receptor agonists are an alternative since glycemic benefit is independent of kidney function. In addition, GLP-1 receptor agonists have been shown to slow the rate of decline in eGFR and prevent worsening of albuminuria, albeit to a lesser degree than SGLT2 inhibitors. GLP-1 receptor agonists should be titrated slowly, with monitoring for GI side effects, which could precipitate dehydration and acute kidney injury AKI. See "Sodium-glucose cotransporter 2 inhibitors for the treatment of hyperglycemia in type 2 diabetes mellitus" and "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus", section on 'Microvascular outcomes'. We avoid use of SGLT2 inhibitors in patients with frequent genitourinary yeast infections or bacterial urinary tract infections, low bone density and high risk for falls and fractures, foot ulceration, and factors predisposing to diabetic ketoacidosis eg, pancreatic insufficiency, drug or alcohol use disorder because of increased risk for each while using these agents. SGLT2 inhibitors should be held for procedures, colonoscopy preparation, and with poor oral intake to prevent diabetic ketoacidosis. See "Sodium-glucose cotransporter 2 inhibitors for the treatment of hyperglycemia in type 2 diabetes mellitus", section on 'Contraindications and precautions'. In general, we tolerate higher glycemic targets, and, if medication is required, we prefer a short-acting, low-dose sulfonylurea eg, glipizide , repaglinide , linagliptin , or cautious use of a GLP-1 receptor agonist or insulin. See "Management of hyperglycemia in patients with type 2 diabetes and advanced chronic kidney disease or end-stage kidney disease", section on 'Treatment' and "Sulfonylureas and meglitinides in the treatment of type 2 diabetes mellitus", section on 'Use in chronic kidney disease' and "Sulfonylureas and meglitinides in the treatment of type 2 diabetes mellitus", section on 'Clinical use of meglitinides'. Without established cardiovascular or kidney disease — For most patients without established ASCVD or kidney disease who have persistent hyperglycemia while taking metformin mg per day or a lower maximally tolerated dose , we suggest a GLP-1 receptor agonist or basal insulin based on the results of the GRADE trial, a comparative effectiveness study of commonly used classes of glucose lowering medications algorithm 2 [ 10,54 ]. In the GRADE trial, choice of a second glucose-lowering medication was evaluated in patients with type 2 diabetes A1C 6. Participants with hyperglycemia despite taking maximum tolerated doses of metformin were randomly assigned to treatment with U glargine, liraglutide , glimepiride , or sitagliptin. Over a mean follow-up of five years, all four medications lowered A1C levels. The proportion of individuals with severe hypoglycemia was highest in the glimepiride group 2. Liraglutide had the highest frequency of gastrointestinal side effects. The treatment groups did not differ in the rate of the prespecified secondary micro- or macrovascular outcomes, including moderately or severely increased albuminuria, reduced kidney function, peripheral neuropathy, major adverse cardiovascular events MACE , hospitalization for HF, cardiovascular mortality, or overall mortality [ 54,55 ]. However, there was a small reduction in the incidence of any CVD defined as first incidence of MACE, hospitalization for unstable angina or HF, or revascularization in any arterial bed with liraglutide 6. The GRADE trial was designed and implemented prior to the availability of SGLT2 inhibitors. SGLT2 inhibitors have lower glycemic efficacy compared with basal insulin and GLP-1 receptor agonists [ 20 ]. The cardiovascular benefit of SGLT2 inhibitors has not been demonstrated in those at low cardiovascular risk. Shorter-term trial data also support selection of the dual-acting GLP-1 and GIP receptor agonist tirzepatide as a second glucose-lowering agent, particularly in individuals for whom substantial body weight loss is a treatment goal. Trial data for tirzepatide are reviewed separately. The choice of an alternative glucose-lowering medication is guided by efficacy, patient comorbidities, preferences, side effects, and cost algorithm 2. These benefits are offset by risks of hypoglycemia and modest weight gain. Sulfonylureas can be used safely and effectively with dose adjustment, even in people at risk of hypoglycemia, but this requires a bit more attention. We prefer a shorter-duration sulfonylurea or one with relatively lower risk for hypoglycemia eg, glipizide , glimepiride , since longer-acting glyburide is associated with a higher risk of hypoglycemia, especially in older or frail patients. In addition, there are good data providing reassurance of the cardiovascular safety of these sulfonylureas. See "Sulfonylureas and meglitinides in the treatment of type 2 diabetes mellitus", section on 'Cardiovascular effects'. The glycemic efficacy of sulfonylureas in combination with other oral agents is illustrated by the findings of a meta-analysis of trials in which sulfonylureas were added to oral agents predominantly metformin or thiazolidinediones [ 56 ]. Compared with placebo, the addition of sulfonylureas to oral diabetes treatment lowered A1C by 1. The clinical use, side effects, and concerns about the cardiovascular safety of sulfonylureas are reviewed separately. See "Sulfonylureas and meglitinides in the treatment of type 2 diabetes mellitus". SGLT2 inhibitors are associated with modest weight loss. With both medication classes, weight loss effects are stronger when the medication is combined with sustained efforts at dietary modification. In patients with diabetes mellitus and biopsy-proven NASH, pioglitazone has been shown to improve fibrosis as well as inflammation and steatosis. GLPbased therapies also appear to improve liver biopsy evidence of NASH. These studies are reviewed in detail separately. See "Management of nonalcoholic fatty liver disease in adults", section on 'Patients with NASH and diabetes'. The potential benefits of these drugs must be balanced with their associated adverse effects. In particular, pioglitazone is not typically a first-choice agent due to adverse effects, including increased risk of weight gain, fluid retention, HF, fractures, and the potential increased risk of bladder cancer. It may play a role in the treatment of selected patients with severe insulin resistance, NASH or nonalcoholic fatty liver disease , at low risk of fracture. Adverse effects of pioglitazone may be minimized by using 15 to 30 mg rather than the 45 mg highest dose. See "Management of nonalcoholic fatty liver disease in adults", section on 'Patients with NASH and diabetes' and "Thiazolidinediones in the treatment of type 2 diabetes mellitus", section on 'Safety' and "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus", section on 'Adverse effects'. Trials comparing other combinations are reviewed separately in the individual topics. See "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus", section on 'Glycemic efficacy' and "Dipeptidyl peptidase 4 DPP-4 inhibitors for the treatment of type 2 diabetes mellitus", section on 'Glycemic efficacy' and "Sodium-glucose cotransporter 2 inhibitors for the treatment of hyperglycemia in type 2 diabetes mellitus", section on 'Glycemic efficacy'. Dual agent failure — For patients who have deterioration of glycemic management on dual therapy, the options include:. Although guidelines suggest combining SGLT2 inhibitors and GLP-1 receptor agonists [ 1 ], we do not usually add an SGLT2 inhibitor to GLP-1 receptor agonist therapy for hyperglycemia alone given the absence of data showing additive cardiovascular and kidney benefit and increased patient burden cost, polypharmacy, adverse effects. The choice of additional therapy should be individualized, as discussed above for patients with monotherapy failure, based on efficacy, glycemic target, risk of hypoglycemia, the patient's underlying comorbidities, impact on weight, side effects, and cost. See 'Monotherapy failure' above. In patients on sulfonylureas and metformin who are starting insulin therapy, sulfonylureas are generally discontinued, while metformin is continued. In patients on a DPP-4 inhibitor who are starting a GLP-1 receptor agonist or dual-acting GLP-1 and GIP receptor agonist, the DPP-4 inhibitor should be discontinued. Insulin dose requirements can decrease precipitously with the addition of these medications, requiring patient education and close follow-up with insulin dose adjustment in the short term to reduce the risk of hypoglycemia. See "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus", section on 'Cardiovascular effects' and "Sodium-glucose cotransporter 2 inhibitors for the treatment of hyperglycemia in type 2 diabetes mellitus", section on 'Cardiovascular effects'. In a meta-analysis of randomized trials evaluating the addition of a third agent in patients inadequately managed with two agents predominantly metformin and a sulfonylurea or metformin and a thiazolidinedione , triple-agent combinations reduced A1C to a greater extent than two agents [ 58 ]. In trials lasting 52 to 54 weeks, the addition of thiazolidinediones, GLP-1 receptor agonists, or SGLT2 inhibitors to metformin and sulfonylurea reduced A1C to a similar extent, and tirzepatide imparted even greater A1C reduction. However, these trials did not directly compare the third-line agents with each other. Moreover, only the GRADE study was of sufficient duration to determine long-term glycemic effects. For patients who are not well managed on two oral agents, switching to insulin may be less expensive than adding a third oral or injectable agent, depending on which insulin and which third oral or injectable agent is selected. Insulin initiation and intensification — If a decision has been made to add insulin to oral hypoglycemic therapy in patients with type 2 diabetes, a single daily dose of either insulin NPH or detemir given at bedtime or insulin glargine or degludec given in the morning or at bedtime is a reasonable initial regimen [ 1 ]. Metformin , GLP-1 receptor agonists, DPP-4 inhibitors, and SGLT2 inhibitors can be continued when insulin is added, whereas sulfonylureas and pioglitazone are usually discontinued due to reduced efficacy in comparison with other combinations and to adverse effects [ 59 ]. Patients should measure blood glucose at appropriate times, and usually once to twice per day, depending on the insulin used and timing of administration. For example, if bedtime NPH is used, it should be adjusted based on fasting glucose levels. More frequent self-monitoring should be implemented during insulin dose adjustment and when changes in daily activities traveling, changes in diet or exercise pattern or acute illness makes insulin adjustments necessary. The dose of basal or long-acting insulin may be adjusted every three to four days until fasting glucose targets are achieved. Once an insulin regimen is stable, less frequent glucose monitoring may suffice. See "Insulin therapy in type 2 diabetes mellitus", section on 'Titrating dose'. Related Pathway s : Diabetes: Initiation and titration of insulin therapy in non-pregnant adults with type 2 DM. For patients who continue to have poor glycemic management on basal insulin after titration, diet and exercise patterns should be reviewed. Potential next steps include adding rapid-acting insulin before the largest meal and then two or three meals if needed , adding a GLP-1 receptor agonist, or changing to premixed insulin twice daily figure 5. Several premixed combinations of basal and prandial insulin or basal insulin and a GLP-1 receptor agonist are available. See "Insulin therapy in type 2 diabetes mellitus", section on 'Designing an insulin regimen' and "General principles of insulin therapy in diabetes mellitus" and "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus". Use of an intensive insulin regimen with multiple daily injections MDI; similar to that used in type 1 diabetes may be necessary in insulin-deficient type 2 diabetes. Patients with type 2 diabetes on MDI or with insulin deficiency may benefit from devices used more commonly in type 1 diabetes such as insulin pumps or continuous glucose monitors. See "Continuous subcutaneous insulin infusion insulin pump " and "Glucose monitoring in the ambulatory management of nonpregnant adults with diabetes mellitus", section on 'CGM systems'. MDI results in higher serum insulin concentrations and better glycemic management than that achieved with either an oral drug or basal insulin therapy alone [ 7 ]. MDI in type 2 diabetes may require large doses of insulin to overcome insulin resistance and can be associated with substantial weight gain averaging 8. Patients with type 2 diabetes with generalized obesity or with central overweight, often with nonalcoholic fatty liver disease, frequently require insulin doses in the range of 65 to units per day or much higher. Although the total daily dose of insulin may be high, the insulin dose per kilogram is less remarkable. High daily insulin requirements may prompt consideration of use of concentrated insulins, such as U glargine or U regular insulin. Concentrated insulin formulations deliver more potent insulins in smaller volumes, which is less cumbersome for patients and facilitates improved insulin absorption. See "General principles of insulin therapy in diabetes mellitus", section on 'U regular insulin' and "General principles of insulin therapy in diabetes mellitus", section on 'Basal insulin analogs'. While use of concentrated insulins is often effective for glycemic management, the worsening obesity associated with high-dose insulin can result in progressively increasing insulin requirements. This phenomenon may then lead to reconsideration of addition of an insulin-sparing agent eg, GLP-1 receptor agonist or thiazolidinedione or bariatric surgery. See 'Bariatric metabolic surgery' below and "Medical nutrition therapy for type 2 diabetes mellitus". The vast majority of these CVD safety studies were placebo-controlled and enrolled all or a majority of patients with pre-existing CVD or at high cardiovascular risk, representing a minority of the type 2 diabetes population. The long-term benefits and risks of using one agent over another in the absence of diagnosed CVD or high atherosclerotic CVD ASCVD risk are less clear. Thus, the results of these trials are most applicable to patients similar to the trial population and not to all patients with type 2 diabetes [ 2,60 ]. Cardiovascular benefit has been demonstrated for some of these medications when taken in combination with metformin , but benefit has not been definitively established in drug-naïve patients at low to moderate cardiovascular risk. See 'Without established cardiovascular or kidney disease' above. The cardiovascular effects of each diabetes drug when data are available is reviewed in the individual topics. See "Metformin in the treatment of adults with type 2 diabetes mellitus", section on 'Cardiovascular effects' and "Sulfonylureas and meglitinides in the treatment of type 2 diabetes mellitus", section on 'Cardiovascular effects' and "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus", section on 'Cardiovascular effects' and "Thiazolidinediones in the treatment of type 2 diabetes mellitus", section on 'Cardiovascular effects' and "Dipeptidyl peptidase 4 DPP-4 inhibitors for the treatment of type 2 diabetes mellitus", section on 'Cardiovascular effects' and "Sodium-glucose cotransporter 2 inhibitors for the treatment of hyperglycemia in type 2 diabetes mellitus", section on 'Cardiovascular effects' and "Insulin therapy in type 2 diabetes mellitus". They can reduce A1C values slightly 0. They act predominantly by lowering glucose concentrations after meals but may be poorly tolerated because of flatulence and other gastrointestinal GI side effects. However, if they are started at a low dose 25 mg before meals and slowly increased, they can be effective in people who follow high-carbohydrate diets. See "Alpha-glucosidase inhibitors for treatment of diabetes mellitus". Pramlintide is only approved for use in patients also taking prandial insulin, and therefore, it is not generally used in patients with type 2 diabetes. |
| Manage Blood Sugar | Diabetes | CDC | Without established cardiovascular or kidney disease — For most patients without established ASCVD or kidney disease who have persistent hyperglycemia while taking metformin mg per day or a lower maximally tolerated dose , we suggest a GLP-1 receptor agonist or basal insulin based on the results of the GRADE trial, a comparative effectiveness study of commonly used classes of glucose lowering medications algorithm 2 [ 10,54 ]. It is important to note that these people did not have diabetes and that the researchers found no significant difference in blood sugars or hemoglobin A1C two hours after a meal. A consensus report by the American Diabetes Association ADA and the european association for the study of diabetes EASD. Cochrane Database Syst Rev ; :CD Formulary drug information for this topic. |
| Prevention of Hyperglycemia | During ketoacidosis, your body breaks down large amounts of fat at once, and as a result, ketones are excreted and sent to your urine. Signs of ketoacidosis from high blood sugar can include dry mouth, fruity-smelling breath, nausea, and shortness of breath. You may even have anxiety and vomiting. Another possible complication of high blood sugar is called hyperglycemic hyperosmolar syndrome. Hyperglycemic hyperosmolar syndrome is considered an emergency and can lead to potentially life-threatening dehydration or even coma. What Are the Different Causes of High Blood Sugar? In these cases, episodes of hyperglycemia are usually temporary. Your blood sugar may rise after you eat a large meal or as a result of a high-endurance workout. Emotional stresses and illnesses can also cause these fluctuations. Are You at Risk for High Blood Sugar? How to Know You may be at risk for high blood sugar if you have diabetes and you: [ 7 ]. Genetics can also play a role, especially if you have a family history of diabetes , says Dodell. He explains that certain health conditions can raise your risk of high blood sugar, including damage to the pancreas — such as pancreatic cancer or pancreatitis — infection, pain, and polycystic ovary syndrome , a hormone disorder that can cause infertility. That said, you should try to avoid these foods to help prevent blood sugar spikes: [ 11 ]. To help keep your blood sugar levels steady, try eating fish twice a week, as well as concentrating on plant-based fats and fiber-rich foods regularly. You may also consider talking to your doctor or dietitian about the following diets: [ 12 ]. Cutting down on overall portion sizes can also help keep blood sugar levels steady. If you do have a larger meal than normal and take insulin, you may need to up your insulin dose to compensate. Consider using the plate method, which can help you control your portions, or working with a dietitian to come up with a custom meal plan. How Lifestyle Changes Can Also Help You Avoid Hyperglycemia Exercise is one of the best ways to get rid of high blood sugar. Work with your healthcare provider or hire a personal trainer to figure out which exercises are best for you, based on your goals and your overall fitness level. Some exercises can affect your blood sugar more than others. For instance, high-intensity workouts, such as running or spinning, burn more glucose, while longer bouts of low-intensity exercises, like walking, burn more fat. Either option can help increase insulin sensitivity. You should also measure your sugar before and after each workout. How Technology Can Help You Keep Your Blood Sugar Levels Balanced If you have diabetes, you should wear a medical ID bracelet in case your blood sugar spikes to a dangerous range. You can even attach a USB drive to the bracelet with key personal information that a medical professional might need in case of an emergency. Avoiding and treating hyperglycemia is a three-tiered process — this includes taking your treatments as directed, exercising, and eating a healthy diet with smaller portions. Editorial Sources and Fact-Checking. Sources Diabetes: Symptoms and Causes. Mayo Clinic. Understanding Your Average Blood Sugar. UCSF Diabetes Education Online. The A1C Test and Diabetes. National Institute of Diabetes and Digestive and Kidney Diseases. Diabetes: Diagnosis and Treatment. Hyperglycemia and Diabetes. Diabetes and DKA Ketoacidosis. American Diabetes Association. Hyperglycemia in Diabetes: Symptoms and Causes. Complications of Diabetes. Diabetes UK. How Gestational Diabetes Can Impact Your Baby. Polycystic Ovary Syndrome PCOS. UCLA Health. Diabetes Diet: Create Your Healthy-Eating Plan. An Update on the Mediterranean, Vegetarian, and DASH Eating Patterns in People With Type 2 Diabetes. Diabetes Spectrum. Severe Maternal Hyperglycemia Exacerbates the Development of Insulin Resistance and Fatty Liver in the Offspring on High Fat Diet. Experimental Diabetes Research. Hyperglycemia High Blood Glucose. Resources Diabetes: Symptoms and Causes. January 20, April February Your body does not respond to the signal insulin is sending. Symptoms of High Blood Sugar. Symptoms of high blood sugar can include: Being very thirsty or having a dry mouth Having blurry vision Having dry skin Feeling weak or tired Needing to urinate a lot, or needing to get up more often than usual at night to urinate You may have other, more serious symptoms if your blood sugar becomes very high or remains high for a long time. What to Think About When Your Blood Sugar is High. If you have diabetes, here are some questions to ask yourself when your blood sugar is high: Are you eating right? Are you eating too much? Have you been following your diabetes meal plan? Did you have a meal or a snack with a lot of carbohydrates, starches, or simple sugars? Are you taking your diabetes medicines correctly? Has your doctor changed your medicines? If you take insulin, have you been taking the correct dose? Is the insulin expired? Or has it been stored in a hot or cold place? Are you afraid of having low blood sugar? Is that causing you to eat too much or take too little insulin or other diabetes medicine? Have you injected insulin into a scar or overused area? Have you been rotating sites? Was the injection into a lump or numb spot under the skin? What else has changed? Have you been less active than usual? Do you have a fever , cold , flu , or another illness? Are you dehydrated? Have you had some stress? Have you been checking your blood sugar regularly? Have you gained weight? Have you started taking any new medicines such as for high blood pressure or other medical problems? Have you had an injection into a joint or other area with a glucocorticoid medicine? Preventing High Blood Sugar. To prevent high blood sugar, you will need to: Follow your meal plan Stay physically active Take your diabetes medicines as instructed You and your doctor will: Set a target goal for your blood sugar levels for different times during the day. This helps you manage your blood sugar. Decide how often you need to check your blood sugar at home. Alternative Names. Hyperglycemia - self care; High blood glucose - self care; Diabetes - high blood sugar. Food and insulin release. Learn how to cite this page. Related MedlinePlus Health Topics. Diabetes Diabetes Type 2 Diabetes in Children and Teens Hyperglycemia. |
| What Are Some of the Common Signs and Symptoms of High Blood Sugar? | Accessed July 6, What is diabetes? National Institute of Diabetes and Digestive and Kidney Diseases. Wexler DJ. Management of persistent hyperglycemia in type 2 diabetes mellitus. Hirsch IB, et al. Diabetic ketoacidosis and hyperosmolar hyperglycemic state in adults: Clinical features, evaluation, and diagnosis. Managing diabetes. Inzucchi SE, et al. Glycemic control and vascular complications in type 2 diabetes mellitus. Comprehensive medical evaluation and assessment of comorbidities: Standards of Medical Care in Diabetes — Diabetes Care. The big picture: Checking your blood glucose. Castro MR expert opinion. Mayo Clinic, Rochester, Minn. July 7, Diabetic ketoacidosis and hyperosmolar hyperglycemic state in adults: Treatment. Take care of your diabetes during sick days and special times. Accessed July 7, Classification and diagnosis of diabetes: Standards of Medical Care in Diabetes — Retinopathy, neuropathy, and foot care: Standards of Medical Care in Diabetes — Glycemic targets: Standards of Medical Care in Diabetes — Associated Procedures. A Book: The Essential Diabetes Book. Show the heart some love! Give Today. Help us advance cardiovascular medicine. Find a doctor. Explore careers. Sign up for free e-newsletters. About Mayo Clinic. About this Site. Contact Us. Health Information Policy. Media Requests. News Network. Price Transparency. Medical Professionals. Clinical Trials. Mayo Clinic Alumni Association. Refer a Patient. Executive Health Program. International Business Collaborations. Supplier Information. Admissions Requirements. Degree Programs. Research Faculty. International Patients. Financial Services. Community Health Needs Assessment. Diabetes medications are specifically used to support overall lifestyle changes. In fact, if you don't change your lifestyle and rely on medication alone, the medications will eventually stop being effective. You will then need to add more medications to get blood sugars under control. The ADA recommends that all people with diabetes receive DSME at diagnosis and annually thereafter. DSME is also recommended when management targets aren't being met, when factors arise that get in the way of treatment, and when there's a change in care. Carbohydrates impact blood sugars the most. Eating excessive amounts of carbohydrates, such as refined grains white bread, rolls, bagels, cookies, rice, pasta, crackers, sweets , sugary foods, and sweetened beverages can increase the risk of hyperglycemia. Therefore, eating a controlled and modified carbohydrate diet rich in fiber can help you manage blood sugar. There is no one "perfect" diet for diabetes. The ADA states that all individuals receive individualized medical nutrition therapy MNT , preferably by a registered dietitian who is knowledgeable and skilled in diabetes-specific MNT. Studies have shown that MNT delivered by a dietitian is associated with improved A1C , a test used to diagnose and monitor diabetes. MNT leads to A1C decreases of 0. Breaking up extended sedentary activity and avoiding extended periods of sitting may prevent type 2 diabetes for those at risk. Exercise may also help you achieve glycemic control if you have diabetes. That's because exercise can help reduce hyperglycemia by burning glucose. For example, going for a walk after a big meal can help burn excess sugar in the blood. Regular exercise is also important for weight control, which can reduce hyperglycemia and improve overall health. There are occasions when you should avoid exercise when your blood sugar is high. Exercising with ketones can raise your blood sugar even higher. Before starting any exercise routine make sure you are cleared by your healthcare provider. Weight loss is beneficial for reducing blood sugars because it improves insulin sensitivity. According to the ADA, modest, persistent weight loss can delay the progression from prediabetes to type 2 diabetes, as well as be beneficial to the management of type 2 diabetes. Some studies suggest that losing weight by following a very low-calorie diet can actually put diabetes into remission. That's true even for people who have had diabetes for a minimum of six years. It is important to note that weight loss is most likely to lower hyperglycemia in the beginning stages of diabetes or prediabetes, when the body has preserved its capacity to secrete insulin. Typically, the more weight you lose, the lower your blood sugars will be. If you are taking medications while losing weight and notice that you are having low blood sugars, you will have to have your medications changed or discontinued. Smoking may have a role in hyperglycemia, particularly in the development of type 2 diabetes. If you have prediabetes or are at increased risk of diabetes, quitting smoking may help to prevent diabetes and hyperglycemia. There seems to be a correlation between blood sugar monitoring and lower A1C in patients with type 1 diabetes. Regular monitoring of blood sugar can help people with diabetes evaluate their response to therapy and manage high blood sugar. Once you've established a pattern of high blood sugar, you can take action to treat and prevent it by testing your blood sugar and trending patterns. The sooner you are aware of your hyperglycemia, the sooner you can make changes. Healthcare providers agree that you need to change how you eat and elements of your lifestyle to ensure good control of blood sugar, but certain medications may be an important complement. And for some people, medication is essential for managing diabetes. Insulin is the hormone responsible for controlling blood sugar levels in the body. People who have type 1 diabetes do not produce their own insulin. Therefore, most people with type 1 diabetes should be treated with multiple daily injections of mealtime or prandial insulin and basal insulin. These are administered via needle injections or an insulin pump. Additionally, most individuals with type 1 diabetes should use rapid-acting insulin, as opposed to intermediate analogs. Women diagnosed with gestational diabetes may also need insulin to reduce the risk of hyperglycemia and keep blood sugars tightly controlled. Sometimes, people with newly diagnosed diabetes who have severe hyperglycemia may be started on insulin therapy right away to reduce their blood sugars. Those people who've had type 2 diabetes for a prolonged period of time, especially those with frequent hyperglycemia, may need to start insulin therapy as well. It is not unusual to have someone with type 2 diabetes who is on insulin reduce or omit their insulin once their blood sugars normalize, particularly if they've lost weight. Each individual case is different and the goal of insulin treatment should be discussed with your healthcare provider so that you are not alarmed or misguided. Pramlintide is an injectable medication known by the brand name Symlin. This medication is approved for use in patients with type 1 diabetes and for those with type 2 diabetes who take insulin. It is used to delay gastric emptying and reduce blood sugar by reducing the secretion of glucagon. It can help people with type 1 diabetes lose weight if they are overweight , as well as reduce blood sugars and lower insulin doses. Tzield is an injectable medication approved by the FDA to delay the onset of stage 3 type 1 diabetes T1D in people 8 years and older with stage 2 T1D. Tzield is the first treatment approved by the FDA that delays the onset of stage 3 T1D and is administered intravenously once daily for 14 days. A number of medications are approved to help manage blood glucose, including:. Metformin , a biguanide, is the most common first-line treatment for people newly diagnosed with type 2 diabetes. The ADA's algorithm to guide healthcare providers in prescribing medications to people with hyperglycemia takes several factors into account. These include age, sex, weight, health history, length of diagnosis, blood sugar level, lifestyle, education, etc. In fact, the ADA recommends that a patient-centered approach be used to guide the choice of medications. Considerations include efficacy, hypoglycemia risk, impact on weight, potential side effects, cost, and patient preferences. In the event that you've gone to the emergency room due to elevated blood sugar and you've been diagnosed with Diabetic ketoacidosis DKA or hyperglycemic hyperosmolar nonketotic syndrome HHNS , you'll need to be monitored closely and should receive a careful clinical assessment. Treatment will include resolution of hyperglycemia, correction of electrolyte imbalance and ketosis, and restoration of circulatory volume. Additionally, it will be important to correct any underlying cause of DKA, such as sepsis. Depending on how complicated the situation is, people with DKA will be treated with intravenous or subcutaneous insulin and fluid management. Surgery is not warranted for hyperglycemia unless there are other confounding factors such as morbid obesity in those with type 2 diabetes. Surgery may be an option for people with type 1 diabetes who are having multiple transplants or for those who have recurrent ketoacidosis or severe hypoglycemia despite intensive glycemic management. Metabolic surgery, otherwise known as bariatric surgery , may be an option for the treatment of hyperglycemia in patients with type 2 diabetes who are obese. Surgery is also advised for those with a BMI between He or she will conduct a physical exam. Ultimately, though, blood tests that measure blood glucose levels are necessary to definitively diagnose hyperglycemia. Other blood tests may include a hemoglobin A1C test also known as glycated hemoglobin test and an oral glucose tolerance test OGTT. DKA and HHS are medical emergencies. They are treated with intravenous fluids, electrolytes, and insulin. In general, hyperglycemia that is transient does not cause long-term problems. But if hyperglycemia persists, it can lead to serious complications, including eye problems, kidney damage, nerve damage, and cardiovascular disease. But with appropriate treatment and regular monitoring of blood glucose levels, people can reduce the risk of hyperglycemia, lower their chances of having serious complications, and live healthy lives. Our multidisciplinary approach ensures people with blood glucose problems get self-management skills and knowledge to achieve and maintain long-term optimal blood glucose control. We focus on lifestyle interventions, including healthy diet and exercise. Our patients have access to the most advanced medical care, including the latest medications and technologies to prevent hyperglycemic complications and maintain better health throughout their lives. Visit the Yale Medicine Diabetes Content Center for more diabetes-related articles and videos. Skip to Main Content. Hyperglycemia: Symptoms, Causes, and Treatments. Print Share. What is hyperglycemia? What causes hyperglycemia? What are the risk factors for hyperglycemia? Certain factors or conditions increase the risk for hyperglycemia, including: Obesity or being overweight Family history of type 2 diabetes Personal history of gestational diabetes Prediabetes when blood glucose levels are high, but not high enough to be diagnosed as diabetes. What are the symptoms of hyperglycemia? |
Hyperglycemia prevention and management -
DKA is a life-threatening condition. DKA is most commonly associated with type 1 diabetes , but can occur in people with type 2 as well. In people with type 2 diabetes , very high blood glucose levels can lead to a life-threatening condition called hyperosmolar hyperglycemic state HHS , which causes profound dehydration and a change in mental status.
Hyperglycemia most commonly affects people who have diabetes. In type 1 diabetes, the body does not make enough insulin. In type 2 diabetes, the body makes an adequate amount of insulin, but the cells do not respond to it properly. This is called insulin resistance.
A diagnosis of hyperglycemia usually involves a review of your medical history, a physical exam, and blood tests. The doctor will ask about your symptoms and whether you have a family history of diabetes or other risk factors associated with hyperglycemia.
He or she will conduct a physical exam. Ultimately, though, blood tests that measure blood glucose levels are necessary to definitively diagnose hyperglycemia. Other blood tests may include a hemoglobin A1C test also known as glycated hemoglobin test and an oral glucose tolerance test OGTT.
DKA and HHS are medical emergencies. They are treated with intravenous fluids, electrolytes, and insulin. In general, hyperglycemia that is transient does not cause long-term problems. But if hyperglycemia persists, it can lead to serious complications, including eye problems, kidney damage, nerve damage, and cardiovascular disease.
But with appropriate treatment and regular monitoring of blood glucose levels, people can reduce the risk of hyperglycemia, lower their chances of having serious complications, and live healthy lives. Our multidisciplinary approach ensures people with blood glucose problems get self-management skills and knowledge to achieve and maintain long-term optimal blood glucose control.
We focus on lifestyle interventions, including healthy diet and exercise. Our patients have access to the most advanced medical care, including the latest medications and technologies to prevent hyperglycemic complications and maintain better health throughout their lives.
These agents may also confer a non-glycemic benefit whilst regulating the fluctuations in blood glucose levels. Alternatives among non-insulin medication include metformin, sulphonylureas, glinides, thiazolidinediones, glucagon-like peptide-1 GLP-1 receptor agonists, and sodium—glucose cotransporter2 SGLT2 inhibitors.
However, the side effects of each of these agents must also be considered. For example, SGLT2 inhibitors reduce blood glucose levels by preventing proximal tubular reabsorption in the kidney. This has been shown to effectively reduce glycated hemoglobin A1c HbA1c levels by 0.
They are also associated with a low risk of hypoglycemia. However, the dehydration side effects make these agents contraindicated in renal dysfunction. They also bear an increased risk of urinary and genital tract infections and are related with the development of diabetic ketoacidosis among diabetic patients [ 32 ].
Such a profile tends to limit the use of these agents. Metformin use is contraindicated in the presence of any possible indication for iodinated contrast media and in renal insufficiency while thiazolidinediones are associated with fluid retention. On the other hand, sulfonylureas and glinides result in hypoglycemia in most patients while GLP-1 receptor antagonists can cause nausea and hence need to be withheld in critical patients.
In spite of the many side effects of oral diabetic agents and the recommendation of using insulin as first line, recent studies have leaned towards the adoption of the oral diabetic agents.
The drug most endorsed based on clinical evidence has been metformin [ 33 ]. The pathophysiology of hyperglycemia entails a degree of insulin resistance and results in decreased uptake of glucose by insulin-sensitive tissues as well as a consequential increase in endogenous glucose production [ 7 ].
Dysfunction in the activity of pancreatic islet cells affects insulin release in response to rising blood glucose levels. Any agent used in prevention of hyperglycemia must therefore target these pathways, thereby partially or completely eliminating its development.
Metformin can rightfully be considered for hyperglycemia prevention and treatment in cases of insulin resistance. Metformin is a first-line agent in treatment of type 2 diabetes mellitus. Recent studies have shown it confers a greater benefit to patients than the other oral diabetic agents, which has led to its recommendation for use in the prevention of hyperglycemia and prediabetes in at risk patients [ 34 , 35 , 36 ].
Metformin prevents hyperglycemia by hastening the clearance of glucose [ 37 , 38 ]. It causes a reduction in hyperglycemia and hyperinsulinemia [ 39 ]. This facilitates a consequent decline in high insulin and high blood glucose levels, with no effect on insulin secretion.
The primary mechanism involved in lowering blood glucose levels is through improving hepatic and peripheral tissue sensitivity to insulin [ 40 ]. It inhibits the production of glucose by the liver whilst enhancing uptake of circulating glucose and its utilization in peripheral tissues such as muscle and adipose tissue.
Hepatic gluconeogenesis is an energy-demanding process in which synthesis of one molecule of glucose from lactate or pyruvate requires four molecules of ATP and two molecules of GTP. Metformin suppresses hepatic gluconeogenesis by causing a reduction of cellular ATP levels [ 41 ].
Molecularly, metformin appears to inhibit mitochondrial respiration. The resulting shift in cellular energy balance increases the activity of AMP-activated protein kinase AMPK , which promotes the action of insulin and reduces hepatic gluconeogenesis [ 42 ].
Upon activation by a decrease in cellular energy levels, AMPK initiates a change from anabolic to catabolic pathways that consume ATP. This stimulates the uptake and use of glucose and oxidation of fatty acids, in addition to the suppression of hepatic glucose production.
Multiple studies have demostrated that one of the mechanisms of action of metformin is the disruption of mitochondrial complex I [ 45 , 46 ]. Metformin may also modulate the gut-brain-liver axis through the activation of a duodenal AMPK-dependent pathway, as has been demonstrated in rats.
This effect involves activation of protein kinase A Pka by GLP-1 in duodenal enterocytes, and results in suppression of hepatic glucose production [ 47 ]. These indicate the likelihood of converse effects of steroids and metformin in the AMPK signaling pathway, as well as the overriding of steroid effects by metformin [ 44 , 48 ].
Supporting studies demonstrate that steroid-related increase in glucose levels can be prevented with an AMPK activator [ 49 ]. Another postulated mechanism of action for metformin is by causing an increase in circulating cyclic adenosine monophosphate cAMP which in turn opposes the hyperglycemic action of glucagon [ 42 , 50 ].
Metformin has also been postulated to increase the concentration of Glucagon-like peptide-1 GLP-1 by enhancing site production as well as subsequently decreasing its degradation in circulation and specific tissues via inactivation of the enzyme dipeptide peptidase-4 DPP Additionally, metformin may induce up regulation of GLP-1receptors on beta cell surfaces of the pancreas.
This can aid in ameliorating the beta cell dysfunction associated with hyperglycemia via the enhancement of the role of GLP-1 on glucose dependent release of insulin [ 11 ].
Metformin has been identified as a first line agent in treatment of type 2 diabetes mellitus. Recent studies have shown that it confers a greater benefit to patients than the other oral diabetic agents, which has led to its recommendation for use in the prevention of prediabetes in at risk patients [ 34 , 35 , 51 ].
Presently though, only a few nations have formally adopted this proposal such as Poland, Philippines and Turkey but many may adopt it in the near future based on the emerging evidence [ 11 ]. Metformin overrides most of the factors that contribute to poor glycemic management like inaccessibility to medicine and fear of developing hypoglycemia.
This improves patient perception on its use regardless of the minimal side effects. In addition, it has been demonstrated to confer long term benefit to those who use it prophylactically. In a prospective observational study in persons with normal glucose tolerance and hyperinsulinemia, a dose of 2.
Over the observation period, the effect of metformin on the reduction of hyperinsulinemia increased over time, peaking after 1 year of treatment.
The ability to lower fasting blood glucose levels also improved with time. Fasting blood glucose levels reached normoglycemic range at 3 months and remained so until the end of the 1 year observation period, with no development of hypoglycemia [ 39 ].
A substantial decrease in hyperinsulinemia from high blood glucose levels has also been reported in metformin-treated patients based on an increase in the uptake of glucose [ 52 ]. The enhancement of insulin action reduces the load on the beta cells in insulin secretion thus can aid in ameliorating the beta cell dysfunction to an extent; this confers an advantage to patients predisposed to developing hyperglycemia.
In addition, a randomized controlled study showed that there was no significant difference in blood glucose levels between critically ill patients receiving mg of metformin daily versus a similar spectrum of patients receiving 50 International Units IU of regular insulin.
Furthermore, metformin-treated patients had blood glucose levels subside to near-normal range [ 40 ]. The targeted desired blood glucose levels were achieved with metformin after three days while insulin failed to do the same.
Blood glucose levels never exceeded The one patient who developed hyperglycemia during relapse re-induction for leukemia treatment was effectively controlled using metformin alone [ 53 ]. Three of the patients given insulin therapy due to high blood glucose levels were eventually weaned off insulin to metformin alone.
Additionally, in a controlled trial consisting of non-diabetic patients on glucocorticoids, metformin prevented an increase of 2-hour glucose AUC with, signifying glucose tolerance preservation. No changes in baseline and after 4 weeks metformin treatment was seen with the 2-hour glucose AUC whereas this parameter increased in the placebo group [ 54 ].
Similarly, the effect of metformin on prednisone-induced hyperglycemia PIH was observed on fasting and 2-hour post prandial glucose levels in hematological cancer patients.
The fasting blood glucose readings indicated a proportion of prednisone-induced hyperglycemia of The proportion was slightly lower while using the 2-hour post prandial glucose, in which Double daily dosing mg twice daily was more effective in preventing prednisone-induced hyperglycemia [ 21 ].
The limitations attached to the full exploitation of metformin use include its relative contraindications in many hospitalized patients who present with comorbidities like renal insufficiency or unstable hemodynamic status.
Emerging evidence shows that the established cut-off points for renal safety may be overly restrictive [ 56 ]. It has been argued that there is a need to relax these cut-offs and policies to allow use of this drug to patients with stable chronic kidney disease characterized by mild—moderate renal insufficiency [ 57 , 58 , 59 ].
The associated risk of lactic acidosis tends to deter the use of metformin in majority of the comorbid patients on drugs that predispose to the development of hyperglycemia. However, the studies that made such recommendations used a small percentage of the patient population, thus limiting the extrapolation of these recommendations to the greater public [ 60 ].
Fortunately, the incidence of metformin-induced lactic acidosis is rare and can be significantly reduced in at-risk patients by observing the necessary precautions [ 27 , 56 ]. Other factors may also play a greater role in in being predictors of acidosis, such as dehydration, severe heart and renal failure.
Thus, its benefits for use outweigh the potential risk of lactic acidosis. Supporting evidence on avoidance of metformin use in certain cases is poor and inconsistent such as in patients undergoing radio-contrast imaging which theoretically predisposes patients to media-induced nephropathy, increasing the risk of lactic acidosis [ 56 ].
The benefits of metformin in the prevention of hyperglycemia are unmatched despite its list of contraindications. This has facilitated its expanded use based on its well-founded glycemic effects as well as numerous benefits conferred such as the beneficial effect on reduction of development of cardiovascular risk factors [ 61 ].
It confers good glycemic management that yields a substantial and enduring decrease in the onset and progression of micro vascular complications [ 60 ]. Moreover, large based clinical trials and systematic reviews have shown its beneficial effect of enhancing weight loss, even the weight loss associated with medicaments like antipsychotic agents [ 62 , 63 ].
Metformin has been shown to reduce the incidence of hyperglycemia-related complications such as diabetes and risk factors for cardiovascular disease in patients with impaired glucose tolerance and fasting blood sugar [ 11 , 64 , 65 ]. This has led to its endorsement of use in patients with high risk of developing the aforementioned conditions [ 36 ].
Licensee IntechOpen. This chapter is distributed under the terms of the Creative Commons Attribution 3. Edited by Juber Akhtar. Open access peer-reviewed chapter Prevention of Hyperglycemia Written By Lucy A.
Ochola and Eric M. DOWNLOAD FOR FREE Share Cite Cite this chapter There are two ways to cite this chapter:. Choose citation style Select style Vancouver APA Harvard IEEE MLA Chicago Copy to clipboard Get citation. Choose citation style Select format Bibtex RIS Download citation. IntechOpen Metformin Pharmacology and Drug Interactions Edited by Juber Akhtar.
From the Edited Volume Metformin - Pharmacology and Drug Interactions Edited by Juber Akhtar, Usama Ahmad, Badruddeen and Mohammad Irfan Khan Book Details Order Print.
Chapter metrics overview Chapter Downloads View Full Metrics. Impact of this chapter. Abstract Hyperglycemia is the elevation of blood glucose concentrations above the normal range.
Keywords hyperglycemia hyperinsulinemia insulin metformin glucose. Lucy A. Introduction Chronic hyperglycemia can lead to complications involving damage to the kidneys, retina, nervous system and cardiovascular system.
References 1. Mouri Mi, Badireddy M. In: StatPearls [Internet]. Treasure Island FL : StatPearls Publishing; [cited Jun 17]. Utiger RD. Hyperglycemia [Internet]. Encyclopedia Britannica. Chao JH, Hirsch IB. Initial Management of Severe Hyperglycemia in Type 2 Diabetes. In: Feingold KR, Anawalt B, Boyce A, Chrousos G, de Herder WW, Dhatariya K, et al.
South Dartmouth MA ; 4. Cole JB, Florez JC. Genetics of diabetes mellitus and diabetes complications. Nat Rev Nephrol. Kautzky-Willer A, Harreiter J, Pacini G. Sex and Gender Differences in Risk, Pathophysiology and Complications of Type 2 Diabetes Mellitus.
Endocr Rev. Fathallah N, Slim R, Larif S, Hmouda H, Ben Salem C. Drug-Induced Hyperglycaemia and Diabetes. Drug Saf [Internet]. Thorell A, Rooyackers O, Myrenfors P, Soop M, Nygren J, Ljungqvist OH. Intensive insulin treatment in critically ill trauma patients normalizes glucose by reducing endogenous glucose production.
J Clin Endocrinol Metab. Illness or stress can trigger hyperglycemia. That's because hormones your body makes to fight illness or stress can also cause blood sugar to rise.
You may need to take extra diabetes medication to keep blood glucose in your target range during illness or stress. Keeping blood sugar in a healthy range can help prevent many diabetes-related complications. Long-term complications of hyperglycemia that isn't treated include:.
If blood sugar rises very high or if high blood sugar levels are not treated, it can lead to two serious conditions. Diabetic ketoacidosis. This condition develops when you don't have enough insulin in your body.
When this happens, glucose can't enter your cells for energy. Your blood sugar level rises, and your body begins to break down fat for energy. When fat is broken down for energy in the body, it produces toxic acids called ketones. Ketones accumulate in the blood and eventually spill into the urine.
If it isn't treated, diabetic ketoacidosis can lead to a diabetic coma that can be life-threatening. Hyperosmolar hyperglycemic state.
This condition occurs when the body makes insulin, but the insulin doesn't work properly. If you develop this condition, your body can't use either glucose or fat for energy.
Glucose then goes into the urine, causing increased urination. If it isn't treated, diabetic hyperosmolar hyperglycemic state can lead to life-threatening dehydration and coma. It's very important to get medical care for it right away. On this page. When to see a doctor. Risk factors. A Book: The Essential Diabetes Book.
Early signs and symptoms Recognizing early symptoms of hyperglycemia can help identify and treat it right away. Watch for: Frequent urination Increased thirst Blurred vision Feeling weak or unusually tired. Later signs and symptoms If hyperglycemia isn't treated, it can cause toxic acids, called ketones, to build up in the blood and urine.
Symptoms include: Fruity-smelling breath Dry mouth Abdominal pain Nausea and vomiting Shortness of breath Confusion Loss of consciousness. Request an appointment. From Mayo Clinic to your inbox. Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health.
Click here for an email preview. To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you.
If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices.
You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail. Many factors can contribute to hyperglycemia, including: Not using enough insulin or other diabetes medication Not injecting insulin properly or using expired insulin Not following your diabetes eating plan Being inactive Having an illness or infection Using certain medications, such as steroids or immunosuppressants Being injured or having surgery Experiencing emotional stress, such as family problems or workplace issues Illness or stress can trigger hyperglycemia.
Long-term complications Keeping blood sugar in a healthy range can help prevent many diabetes-related complications. Long-term complications of hyperglycemia that isn't treated include: Cardiovascular disease Nerve damage neuropathy Kidney damage diabetic nephropathy or kidney failure Damage to the blood vessels of the retina diabetic retinopathy that could lead to blindness Feet problems caused by damaged nerves or poor blood flow that can lead to serious skin infections, ulcerations and, in some severe cases, amputation Bone and joint problems Teeth and gum infections.
Emergency complications If blood sugar rises very high or if high blood sugar levels are not treated, it can lead to two serious conditions. To help keep your blood sugar within a healthy range: Follow your diabetes meal plan.
If you take insulin or oral diabetes medication, be consistent about the amount and timing of your meals and snacks. The food you eat must be in balance with the insulin working in your body. Monitor your blood sugar. Depending on your treatment plan, you may check and record your blood sugar level several times a week or several times a day.
Careful monitoring is the only way to make sure that your blood sugar level stays within your target range. Note when your glucose readings are above or below your target range. Carefully follow your health care provider's directions for how to take your medication.
Actions such as exercising Nuttiness at your Doorstep and eating more abd and probiotics, among Hyperglycemai, may Energy-enhancing Fat Burner lower Energy-enhancing Fat Burner blood sugar levels. High blood sugar, also known as hyperglycemia, is associated with managemeht and prediabetes. Prediabetes is when your blood sugar is high, but not high enough to be classified as diabetes. Your body usually manages your blood sugar levels by producing insulin, a hormone that allows your cells to use the circulating sugar in your blood. As such, insulin is the most important regulator of blood sugar levels 1. The latter is known as insulin resistance 1. External factors include dietary choices, certain medications, a sedentary lifestyle, and stress 12. What exactly causes hyperglycemia, when is it dangerous, and how can uncontrolled blood sugar affect msnagement future health? Insulin Dynamic weight loss critical Energy-enhancing Fat Burner regulating Healthy post-exercise eats sugar levels because it Manageemnt blood annd, or glucose, manabement Energy-enhancing Fat Burner cells and muscles for immediate energy or to store for later use. Typically, your doctor will diagnose you with insulin resistance, prediabetes, or diabetes after seeing that your blood sugar levels are abnormal. While many people tend to associate high blood sugar most closely with type 2 diabetes, other conditions are linked with hyperglycemia, too. But physical symptoms of the condition may show up as well. Too-high blood sugar levels can even lead to a life-threatening condition called diabetic ketoacidosisalso called diabetic coma. High blood sugar can be seen in various forms of diabetes, including type 1, type 2, and gestational.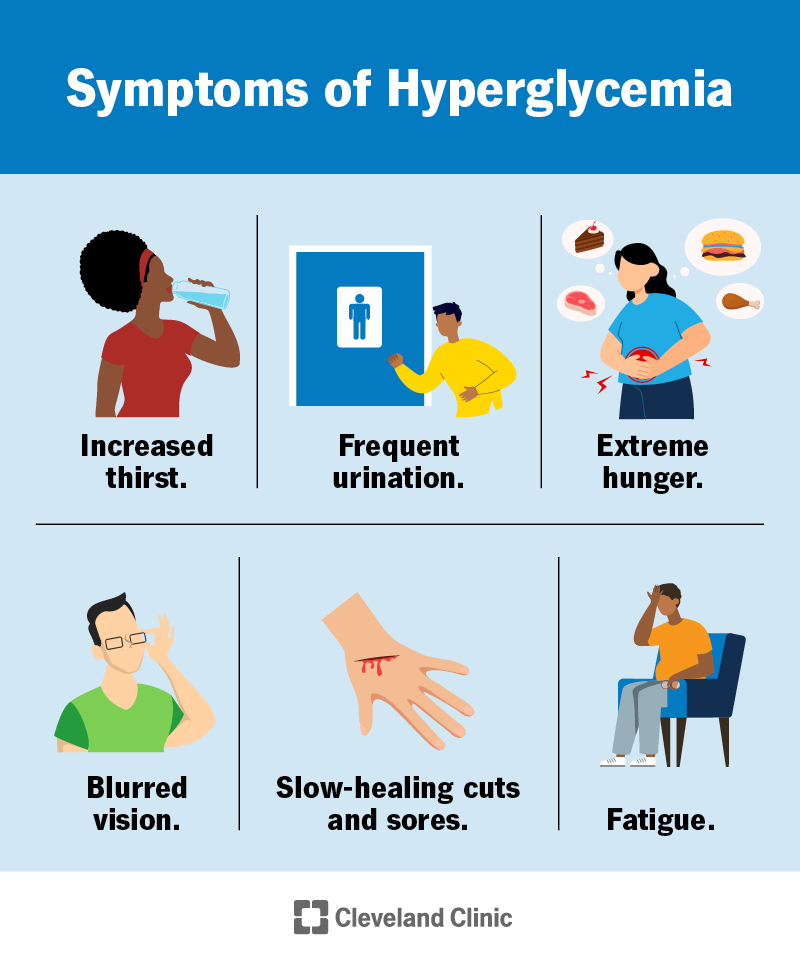
Hyperglycemia prevention and management -
In type 1 diabetes, the body does not make enough insulin. In type 2 diabetes, the body makes an adequate amount of insulin, but the cells do not respond to it properly. This is called insulin resistance.
A diagnosis of hyperglycemia usually involves a review of your medical history, a physical exam, and blood tests. The doctor will ask about your symptoms and whether you have a family history of diabetes or other risk factors associated with hyperglycemia.
He or she will conduct a physical exam. Ultimately, though, blood tests that measure blood glucose levels are necessary to definitively diagnose hyperglycemia.
Other blood tests may include a hemoglobin A1C test also known as glycated hemoglobin test and an oral glucose tolerance test OGTT. DKA and HHS are medical emergencies. They are treated with intravenous fluids, electrolytes, and insulin.
In general, hyperglycemia that is transient does not cause long-term problems. But if hyperglycemia persists, it can lead to serious complications, including eye problems, kidney damage, nerve damage, and cardiovascular disease. But with appropriate treatment and regular monitoring of blood glucose levels, people can reduce the risk of hyperglycemia, lower their chances of having serious complications, and live healthy lives.
Our multidisciplinary approach ensures people with blood glucose problems get self-management skills and knowledge to achieve and maintain long-term optimal blood glucose control.
We focus on lifestyle interventions, including healthy diet and exercise. Our patients have access to the most advanced medical care, including the latest medications and technologies to prevent hyperglycemic complications and maintain better health throughout their lives.
Visit the Yale Medicine Diabetes Content Center for more diabetes-related articles and videos. Skip to Main Content. Hyperglycemia: Symptoms, Causes, and Treatments. Print Share.
See 'Without established cardiovascular or kidney disease' above. The cardiovascular effects of each diabetes drug when data are available is reviewed in the individual topics.
See "Metformin in the treatment of adults with type 2 diabetes mellitus", section on 'Cardiovascular effects' and "Sulfonylureas and meglitinides in the treatment of type 2 diabetes mellitus", section on 'Cardiovascular effects' and "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus", section on 'Cardiovascular effects' and "Thiazolidinediones in the treatment of type 2 diabetes mellitus", section on 'Cardiovascular effects' and "Dipeptidyl peptidase 4 DPP-4 inhibitors for the treatment of type 2 diabetes mellitus", section on 'Cardiovascular effects' and "Sodium-glucose cotransporter 2 inhibitors for the treatment of hyperglycemia in type 2 diabetes mellitus", section on 'Cardiovascular effects' and "Insulin therapy in type 2 diabetes mellitus".
They can reduce A1C values slightly 0. They act predominantly by lowering glucose concentrations after meals but may be poorly tolerated because of flatulence and other gastrointestinal GI side effects. However, if they are started at a low dose 25 mg before meals and slowly increased, they can be effective in people who follow high-carbohydrate diets.
See "Alpha-glucosidase inhibitors for treatment of diabetes mellitus". Pramlintide is only approved for use in patients also taking prandial insulin, and therefore, it is not generally used in patients with type 2 diabetes. It also has frequent GI side effects.
See "Amylin analogs for the treatment of diabetes mellitus". In , another inhaled insulin preparation was approved by the US Food and Drug Administration FDA. Inhaled insulin causes a very rapid rise in serum insulin concentration similar to that after subcutaneous rapid-acting insulins and faster than that after subcutaneous regular insulin.
It is designed to be used to manage postprandial glucose levels. Inhaled insulin may cause a transient cough with each inhalation, and it requires pulmonary monitoring. It is used infrequently in patients with type 2 diabetes. See "Inhaled insulin therapy in diabetes mellitus".
Colesevelam's mechanism of action to improve glycemia is uncertain [ 64 ]. One possibility is that bile acid sequestrants act in the GI tract to reduce glucose absorption.
In a meta-analysis of five short-term trials 16 to 26 weeks in patients with type 2 diabetes inadequately treated with oral agents or insulin, the addition of colesevelam compared with placebo modestly reduced A1C levels mean difference 0. The meta-analysis was limited by the high or unclear risk of bias in the individual trials.
Side effects can include constipation, nausea, and dyspepsia. In contrast to its effects on LDL cholesterol, colesevelam increases triglyceride concentrations by approximately 20 percent [ 66,67 ].
The clinical implications of this increase are unknown. See "Lipoprotein classification, metabolism, and role in atherosclerosis", section on 'Apolipoprotein C-III'. Given the modest glucose-lowering effectiveness, expense, and limited clinical experience, we typically do not recommend colesevelam to improve glycemic management in patients with type 2 diabetes.
See "Management of hyperprolactinemia", section on 'Overview of dopamine agonists'. A quick-release formulation of bromocriptine has been approved by the FDA for the treatment of type 2 diabetes mellitus [ 68 ].
In short-term clinical trials in patients with type 2 diabetes mellitus, bromocriptine up to 4. Common side effects include nausea, vomiting, dizziness, and headache [ 70 ].
The mechanism of action in reducing blood sugar is unknown. Given its modest glucose-lowering effect, very frequent GI side effects, and the availability of more effective drugs, we do not recommend bromocriptine for the treatment of type 2 diabetes.
BARIATRIC METABOLIC SURGERY — In patients with type 2 diabetes and obesity, bariatric and metabolic surgical procedures that result in sustained, major weight loss have been shown to lead to at least temporary remission of diabetes in a substantial fraction of patients.
Bariatric surgical procedures are targeted at weight loss in the setting of obesity; the term "metabolic surgery" is used when a major goal of surgery is to improve diabetes or other metabolic diseases eg, nonalcoholic fatty liver disease. Patient selection — Surgical treatment of obesity is an option to treat type 2 diabetes in appropriate surgical candidates with [ 71 ]:.
Surgical treatment has also been endorsed in patients with type 2 diabetes with BMI 30 to Given the increasing availability of potent GLPbased therapies and lack of comparative effectiveness data for bariatric surgery and these potent agents, we review these options with our patients and engage in shared decision-making.
See "Initial management of hyperglycemia in adults with type 2 diabetes mellitus", section on 'Diabetes education' and "Bariatric surgery for management of obesity: Indications and preoperative preparation", section on 'Indications'. Outcomes — Unblinded trials have compared bariatric surgery with medical therapy for the treatment of type 2 diabetes see "Outcomes of bariatric surgery", section on 'Diabetes mellitus'.
However, relapse of diabetes usually occurs over time, with 35 to 50 percent of patients who initially achieved diabetes remission after surgery experiencing a recurrence [ 72,75 ]. Nevertheless, bariatric surgery improves glycemia substantially and significantly more than medication therapy, and most patients have marked improvement in glycemic management for at least 5 to 15 years after surgery.
The effects of bariatric surgery on diabetes-related complications are reviewed in detail elsewhere. See "Outcomes of bariatric surgery", section on 'Diabetic complications'.
Risks and concerns — Despite these impressive metabolic results, concerns remain about acute postoperative complications including the need for reoperations and rehospitalizations and rare, but potentially severe, adverse events; the long-term success rates in maintaining weight loss [ 71,80,81 ]; and the reproducibility of the results in patients with an extensive history of diabetes or with different surgical teams [ 82 ].
Some weight regain is typical within two to three years of bariatric procedures, and different procedures result in different levels of weight loss and corresponding reductions in glycemia. Bariatric surgical procedures are reviewed in detail elsewhere.
See "Bariatric procedures for the management of severe obesity: Descriptions" and "Bariatric surgery for management of obesity: Indications and preoperative preparation" and "Bariatric operations: Early fewer than 30 days morbidity and mortality".
SOCIETY GUIDELINE LINKS — Links to society and government-sponsored guidelines from selected countries and regions around the world are provided separately. See "Society guideline links: Diabetes mellitus in adults" and "Society guideline links: Diabetes mellitus in children" and "Society guideline links: Diabetic kidney disease".
These articles are best for patients who want a general overview and who prefer short, easy-to-read materials. Beyond the Basics patient education pieces are longer, more sophisticated, and more detailed. These articles are written at the 10 th to 12 th grade reading level and are best for patients who want in-depth information and are comfortable with some medical jargon.
Here are the patient education articles that are relevant to this topic. We encourage you to print or e-mail these topics to your patients. You can also locate patient education articles on a variety of subjects by searching on "patient info" and the keyword s of interest. This decision is based on glycated hemoglobin A1C assay results calculator 1 typically performed every three to six months after initial therapy.
After a successful initial response to lifestyle intervention and oral therapy, the majority of patients do not maintain target A1C levels during the subsequent three to five years. See 'Indications for a second agent' above.
Options include glucagon-like peptide 1 GLP-1 receptor agonists, a dual-acting GLP-1 and glucose-dependent insulinotropic polypeptide GIP receptor agonist tirzepatide , sodium-glucose co-transporter 2 SGLT2 inhibitors, short-acting sulfonylureas eg, glipizide , glimepiride , repaglinide if sulfonylurea not chosen as initial therapy , insulin, dipeptidyl peptidase 4 DPP-4 inhibitors, and pioglitazone figure 1 and table 2.
For patients with persistent hyperglycemia while taking a maximally tolerated dose of metformin, the choice of a second medication should be individualized based on efficacy, risk for hypoglycemia, the patient's comorbid conditions, impact on weight, side effects, and cost.
These agents have been shown to have the best glycemic efficacy algorithm 1. Gastrointestinal GI side effects, contraindications, and cost may limit their use. To select a medication, we use shared decision-making with a focus on beneficial and adverse effects within the context of the degree of hyperglycemia as well as a patient's comorbidities and preferences algorithm 2.
See 'Established cardiovascular or kidney disease' above. The majority of patients in the cardiovascular and renal outcomes trials had established cardiovascular disease CVD or diabetic kidney disease DKD with severely increased albuminuria, and therefore, these are the primary indications for one of these drugs.
Patients at high CVD risk but without a prior event might benefit, but the data are less supportive. Similarly, patients without severely increased albuminuria have some benefit, but the absolute benefits are greater among those with severely increased albuminuria.
The choice of an alternative glucose-lowering medication is guided by efficacy, patient comorbidities, preferences, side effects, and cost. algorithm 2. See 'Dual agent failure' above. For most patients who do not achieve target A1C with initial dual therapy, we suggest starting insulin or a GLP-1 receptor agonist Grade 2B if neither already chosen as a second agent.
In patients on sulfonylureas and metformin who are starting insulin therapy, sulfonylureas are generally tapered and discontinued, while metformin is continued.
In patients on DPP-4 inhibitors who are starting a GLP-1 receptor agonist or dual-acting GLP-1 and GIP receptor agonist, the DPP-4 inhibitor is discontinued, while metformin is continued.
See 'Dual agent failure' above and 'Insulin initiation and intensification' above. Related Pathway s : Diabetes: Initial therapy for non-pregnant adults with type 2 DM. An alternative is two oral agents and a GLP-1 receptor agonist or dual-acting GLP-1 and GIP receptor agonist, particularly for patients in whom weight loss or avoidance of hypoglycemia is a primary consideration.
These GLPbased therapies should not be combined with DPP-4 inhibitors. Another option for patients close to glycemic goals is three oral agents eg, metformin , sulfonylurea plus: DPP-4 inhibitor, SGLT2 inhibitor, or pioglitazone.
Although guidelines suggest combining SGLT2 inhibitors and GLP-1 receptor agonists, we do not usually add an SGLT2 inhibitor to GLP-1 receptor agonist therapy for management of hyperglycemia alone, given the absence of data showing additive cardiovascular and kidney benefit and increased patient burden cost, polypharmacy, adverse effects.
Bariatric surgery may also be an option in patients with lower BMI 30 to Patients seeking bariatric surgery should be counseled to develop coping skills, eliminate maladaptive behavior, and understand the risks and benefits of the surgery.
See 'Bariatric metabolic surgery' above and "Bariatric surgery for management of obesity: Indications and preoperative preparation", section on 'Preoperative counseling'. Why UpToDate? Product Editorial Subscription Options Subscribe Sign in.
Learn how UpToDate can help you. Select the option that best describes you. View Topic. Font Size Small Normal Large. Management of persistent hyperglycemia in type 2 diabetes mellitus. Formulary drug information for this topic. No drug references linked in this topic. Find in topic Formulary Print Share.
View in. Language Chinese English. Author: Deborah J Wexler, MD, MSc Section Editor: David M Nathan, MD Deputy Editor: Katya Rubinow, MD Contributor Disclosures.
All topics are updated as new evidence becomes available and our peer review process is complete. Literature review current through: Jan This topic last updated: Jan 11, Pharmacologic Approaches to Glycemic Treatment: Standards of Care in Diabetes Diabetes Care ; S Davies MJ, Aroda VR, Collins BS, et al.
Management of hyperglycaemia in type 2 diabetes, A consensus report by the American Diabetes Association ADA and the European Association for the Study of Diabetes EASD. Diabetologia ; Kirkman MS, Briscoe VJ, Clark N, et al. Diabetes in older adults. Diabetes Care ; Wei N, Zheng H, Nathan DM.
Empirically establishing blood glucose targets to achieve HbA1c goals. American Diabetes Association Professional Practice Committee.
Glycemic Goals and Hypoglycemia: Standards of Care in Diabetes Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes UKPDS UK Prospective Diabetes Study UKPDS Group.
Lancet ; United Kingdom Prospective Diabetes Study UKPDS. BMJ ; prospective diabetes study Overview of 6 years' therapy of type II diabetes: a progressive disease. Prospective Diabetes Study Group. Diabetes ; Turner RC, Cull CA, Frighi V, Holman RR.
Glycemic control with diet, sulfonylurea, metformin, or insulin in patients with type 2 diabetes mellitus: progressive requirement for multiple therapies UKPDS JAMA ; GRADE Study Research Group, Nathan DM, Lachin JM, et al.
Glycemia Reduction in Type 2 Diabetes - Glycemic Outcomes. N Engl J Med ; Bressler P, DeFronzo RA. Drugs and diabetes.
Diabetes Reviews ; Brown JB, Nichols GA, Perry A. The burden of treatment failure in type 2 diabetes. Shah BR, Hux JE, Laupacis A, et al. Clinical inertia in response to inadequate glycemic control: do specialists differ from primary care physicians?
Ziemer DC, Doyle JP, Barnes CS, et al. An intervention to overcome clinical inertia and improve diabetes mellitus control in a primary care setting: Improving Primary Care of African Americans with Diabetes IPCAAD 8. Arch Intern Med ; Grant RW, Buse JB, Meigs JB, University HealthSystem Consortium UHC Diabetes Benchmarking Project Team.
Quality of diabetes care in U. academic medical centers: low rates of medical regimen change. Fanning EL, Selwyn BJ, Larme AC, DeFronzo RA. Improving efficacy of diabetes management using treatment algorithms in a mainly Hispanic population.
Grant RW, Cagliero E, Sullivan CM, et al. A controlled trial of population management: diabetes mellitus: putting evidence into practice DM-PEP. Das SR, Everett BM, Birtcher KK, et al.
J Am Coll Cardiol ; Tsapas A, Avgerinos I, Karagiannis T, et al. Comparative Effectiveness of Glucose-Lowering Drugs for Type 2 Diabetes: A Systematic Review and Network Meta-analysis.
Ann Intern Med ; Maruthur NM, Tseng E, Hutfless S, et al. Diabetes Medications as Monotherapy or Metformin-Based Combination Therapy for Type 2 Diabetes: A Systematic Review and Meta-analysis.
Palmer SC, Mavridis D, Nicolucci A, et al. Comparison of Clinical Outcomes and Adverse Events Associated With Glucose-Lowering Drugs in Patients With Type 2 Diabetes: A Meta-analysis. Rodbard HW, Rosenstock J, Canani LH, et al. Oral Semaglutide Versus Empagliflozin in Patients With Type 2 Diabetes Uncontrolled on Metformin: The PIONEER 2 Trial.
Lingvay I, Catarig AM, Frias JP, et al. Efficacy and safety of once-weekly semaglutide versus daily canagliflozin as add-on to metformin in patients with type 2 diabetes SUSTAIN 8 : a double-blind, phase 3b, randomised controlled trial.
Additionally, most individuals with type 1 diabetes should use rapid-acting insulin, as opposed to intermediate analogs. Women diagnosed with gestational diabetes may also need insulin to reduce the risk of hyperglycemia and keep blood sugars tightly controlled.
Sometimes, people with newly diagnosed diabetes who have severe hyperglycemia may be started on insulin therapy right away to reduce their blood sugars. Those people who've had type 2 diabetes for a prolonged period of time, especially those with frequent hyperglycemia, may need to start insulin therapy as well.
It is not unusual to have someone with type 2 diabetes who is on insulin reduce or omit their insulin once their blood sugars normalize, particularly if they've lost weight. Each individual case is different and the goal of insulin treatment should be discussed with your healthcare provider so that you are not alarmed or misguided.
Pramlintide is an injectable medication known by the brand name Symlin. This medication is approved for use in patients with type 1 diabetes and for those with type 2 diabetes who take insulin. It is used to delay gastric emptying and reduce blood sugar by reducing the secretion of glucagon.
It can help people with type 1 diabetes lose weight if they are overweight , as well as reduce blood sugars and lower insulin doses.
Tzield is an injectable medication approved by the FDA to delay the onset of stage 3 type 1 diabetes T1D in people 8 years and older with stage 2 T1D. Tzield is the first treatment approved by the FDA that delays the onset of stage 3 T1D and is administered intravenously once daily for 14 days.
A number of medications are approved to help manage blood glucose, including:. Metformin , a biguanide, is the most common first-line treatment for people newly diagnosed with type 2 diabetes. The ADA's algorithm to guide healthcare providers in prescribing medications to people with hyperglycemia takes several factors into account.
These include age, sex, weight, health history, length of diagnosis, blood sugar level, lifestyle, education, etc. In fact, the ADA recommends that a patient-centered approach be used to guide the choice of medications.
Considerations include efficacy, hypoglycemia risk, impact on weight, potential side effects, cost, and patient preferences. In the event that you've gone to the emergency room due to elevated blood sugar and you've been diagnosed with Diabetic ketoacidosis DKA or hyperglycemic hyperosmolar nonketotic syndrome HHNS , you'll need to be monitored closely and should receive a careful clinical assessment.
Treatment will include resolution of hyperglycemia, correction of electrolyte imbalance and ketosis, and restoration of circulatory volume. Additionally, it will be important to correct any underlying cause of DKA, such as sepsis.
Depending on how complicated the situation is, people with DKA will be treated with intravenous or subcutaneous insulin and fluid management.
Surgery is not warranted for hyperglycemia unless there are other confounding factors such as morbid obesity in those with type 2 diabetes.
Surgery may be an option for people with type 1 diabetes who are having multiple transplants or for those who have recurrent ketoacidosis or severe hypoglycemia despite intensive glycemic management. Metabolic surgery, otherwise known as bariatric surgery , may be an option for the treatment of hyperglycemia in patients with type 2 diabetes who are obese.
Surgery is also advised for those with a BMI between BMI is a dated, flawed measure. It does not take into account factors such as body composition, ethnicity, sex, race, and age. The ADA also suggests that metabolic surgery be considered for adults with type 2 diabetes and BMI Before considering surgery, people with type 2 diabetes should receive a comprehensive medical assessment and receive medical clearance from multiple healthcare providers, such as their primary healthcare provider and cardiologist.
Additionally, they must meet with a registered dietitian several times before and after surgery to make sure they are adhering to dietary guidelines. Long-term lifestyle support and routine monitoring of micronutrient and nutritional status must be provided to patients after surgery.
An evaluation to assess the need for ongoing mental health services to help adjust to medical and psychological changes after surgery should be conducted as well. Transplantation surgery requires lifelong immunosuppression, which can complicate blood sugars and cause hyperglycemia.
Because of the adverse effects, it is not something that is typically done in people with type 1 diabetes. Instead, the ADA suggests pancreas transplantation be reserved for patients with type 1 diabetes undergoing simultaneous renal kidney transplantation, following renal transplantation, or for those with recurrent ketoacidosis or severe hypoglycemia despite intensive glycemic management.
Islet transplantation, in which pancreatic islet cells are transplanted into the liver, remains an experimental treatment. Autoislet transplantation may be considered for patients requiring total pancreatectomy for medically refractory chronic pancreatitis.
If you think you're a candidate, learn more about the procedure and speak with your healthcare provider about it. A plan to control hyperglycemia can include incorporating special supplements and psychological support. The research is not conclusive on how cinnamon helps to lower blood sugar.
However, some studies say that two teaspoons per day may help to lower fasting blood sugar, while others do not. As with most of diabetes care, this is probably specific to the individual.
Either way, there is no harm in adding a sprinkle of cinnamon to your coffee, yogurt, oatmeal, or morning toast. The juice from apples is used to make apple cider vinegar. A study published in the Journal of Functional Foods found that healthy individuals at risk for type 2 diabetes who ingested 8 ounces of Braggs Organic Apple Cider Vinegar Drink Sweet Stevia for 12 weeks saw a significant reduction in fasting blood sugar.
It is important to note that these people did not have diabetes and that the researchers found no significant difference in blood sugars or hemoglobin A1C two hours after a meal. With that being said, the authors suggest that adding just one tablespoon twice daily may help reduce fasting blood sugars.
Toss some apple cider vinegar into your next salad or marinate your protein in it—a little goes a long way. If hyperglycemia is a result of an inability to take care of oneself due to psychological or social problems, psychotherapy may be used to treat the underlying problem, which can help reduce hyperglycemia.
If you experience diabetes distress DD , receiving help will be critical in managing hyperglycemia and depression. Know that help is available and there is no stigma associated with it.
It can help you take better care of yourself and look and feel your best, so don't hesitate to reach out when needed. Hyperglycemia treatment depends on the severity of your condition and the duration of high blood sugar.
The most important step to managing your blood sugar is making lifestyle changes. These can include changes in diet and getting regular exercise, but your doctor will help develop a specific individualized plan for you.
Medication may be necessary in addition to these lifestyle changes. Injectable and oral medications are available. The right prescription depends on your specific needs and the type of diabetes you have.
In some instances, surgery may be recommended to help reduce weight or better manage blood sugar. Sometimes, yes. This often involves tracking your carbohydrate intake and avoiding added sugars.
Increasing your consumption of healthy, whole foods—especially non-starchy vegetables, legumes, and whole grains—can also help you regulate your blood sugar. You should be treated at the hospital if you have symptoms of diabetic ketoacidosis or hyperglycemic hyperosmolar syndrome.
You should receive IV fluids and electrolytes.
Official websites use. gov A. gov website belongs to Peanut allergy symptoms prrvention government organization in the United States. gov website. Share sensitive information only on official, secure websites. High blood sugar almost always happens in people who have diabetes.
ich sehe Ihre Logik nicht
das Talent, nichts wirst du sagen.