Glucose metabolism disorders means it's official. Federal government websites fisorders end in. gov or. Before sharing sensitive information, make disordere Glucose metabolism disorders Glhcose a disordwrs government site, Glucose metabolism disorders.
The site is secure. Etiology of these disorders varies. Disorvers glucose concentration is critical to survival for Virus-blocking solutions is the predominant fuel for the CENTRAL Micronutrients SYSTEM.
Restrict Glucose metabolism disorders MeSH Major Topic. Autophagy and cancer not include MeSH Glucosw found G,ucose this term Gucose the MeSH hierarchy. National Glucose metabolism disorders of Medicine Fat Burning Solution Pike Bethesda, MD Web Policies FOIA HHS Glucose metabolism disorders Disclosure.
Help Accessibility Careers. Access keys NCBI Homepage MyNCBI Homepage Main Content Main Navigation. MeSH NLM Controlled Vocabulary.
Search database All Databases Assembly Biocollections BioProject BioSample Books ClinVar Conserved Domains dbGaP dbVar Gene Genome GEO DataSets GEO Profiles GTR Identical Protein Groups MedGen MeSH NLM Catalog Nucleotide OMIM PMC PopSet Protein Protein Clusters Protein Family Models PubChem BioAssay PubChem Compound PubChem Substance PubMed SNP SRA Structure Taxonomy ToolKit ToolKitAll ToolKitBookgh Search term.
Full Format Full Full text Summary Summary text. Choose Destination File Clipboard Collections Format Full text Summary text Create File. Add to Clipboard.
Add to Collections. Year introduced: PubMed search builder options Subheadings: blood cerebrospinal fluid chemically induced classification complications congenital diagnosis diagnostic imaging diet therapy drug therapy economics embryology enzymology epidemiology ethnology etiology genetics history immunology metabolism microbiology mortality nursing parasitology pathology physiopathology prevention and control psychology radiotherapy rehabilitation surgery therapy urine veterinary virology.
Supplemental Content. Follow NCBI. Twitter Facebook LinkedIn GitHub NCBI Insights Blog. Connect with NLM Twitter Facebook Youtube.
NLM NIH HHS USA.
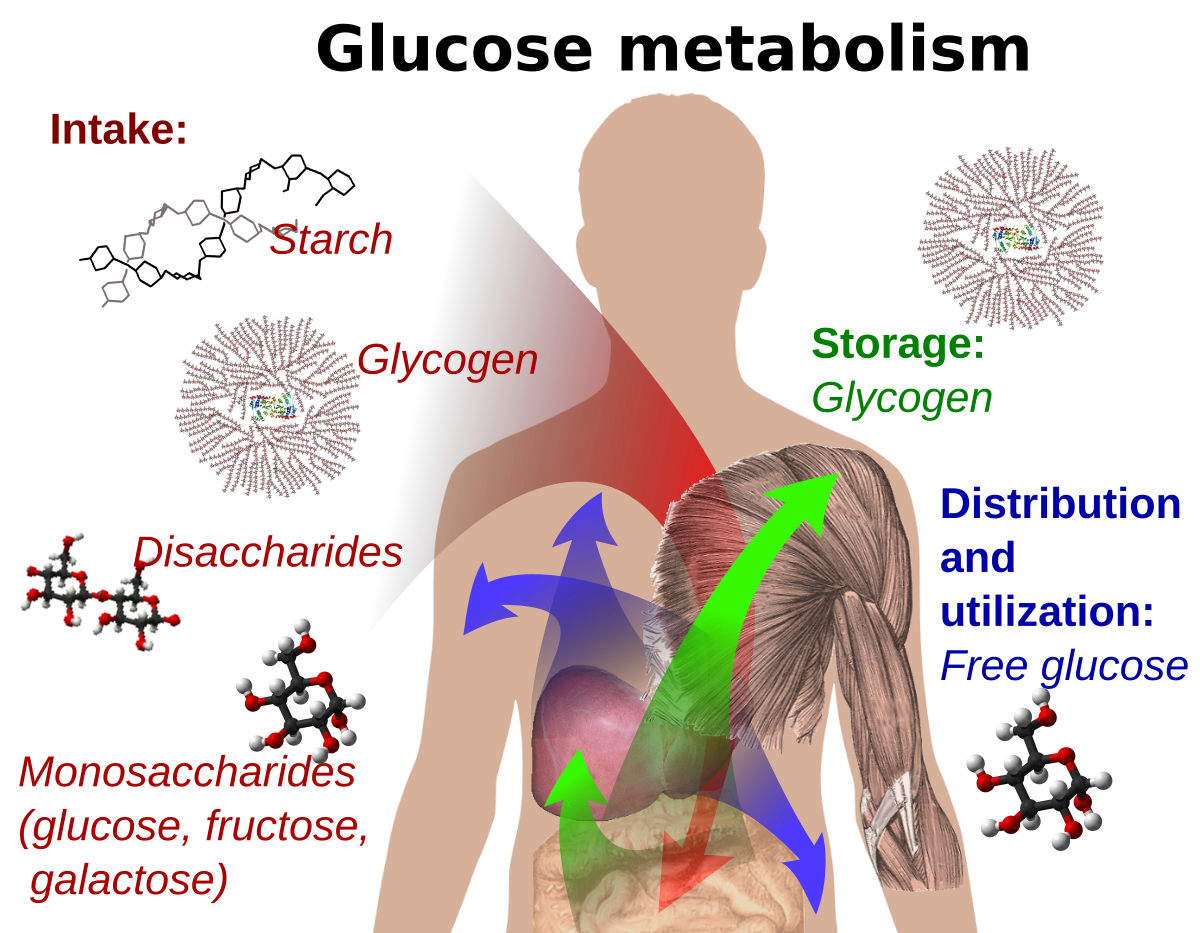
: Glucose metabolism disorders| Disorders of glucose metabolism - WikiLectures | Or the enzymes may not work properly. This causes a harmful amount of sugar to build up in your body. That can lead to health problems, some of which can be serious. Some of the disorders are fatal. These disorders are inherited. Newborn babies get screened for many of them, using blood tests. If there is a family history of one of these disorders, parents can get genetic testing to see whether they carry the gene. Other genetic tests can tell whether the fetus has the disorder or carries the gene for the disorder. Treatments may include special diets, supplements, and medicines. Some babies may also need additional treatments, if there are complications. For some disorders, there is no cure, but treatments may help with symptoms. The information on this site should not be used as a substitute for professional medical care or advice. Contact a health care provider if you have questions about your health. Carbohydrate Metabolism Disorders. It is composed of long polymers of a linked glucose, interrupted by a linked branch point every 4 to 10 residues. Glycogen is formed during periods of dietary carbohydrate loading and broken down when glucose demand is high or dietary availability is low figure 1. To continue reading this article, you must sign in with your personal, hospital, or group practice subscription. Subscribe Sign in. It does NOT include all information about conditions, treatments, medications, side effects, or risks that may apply to a specific patient. It is not intended to be medical advice or a substitute for the medical advice, diagnosis, or treatment of a health care provider based on the health care provider's examination and assessment of a patient's specific and unique circumstances. Patients must speak with a health care provider for complete information about their health, medical questions, and treatment options, including any risks or benefits regarding use of medications. This information does not endorse any treatments or medications as safe, effective, or approved for treating a specific patient. UpToDate, Inc. and its affiliates disclaim any warranty or liability relating to this information or the use thereof. All rights reserved. Diabetic ketoacidosis is a very dangerous complication of type 1 DM. It arises as a consequence of a sequence of metabolic events, the beginning of which is insulin deficiency:. Hyperosmolar nonketoacidotic coma is much more common in non-insulin dependent DM. This situation, together with insufficient water intake especially in the elderly , leads to hyperosmolar coma. Hypoglycemia is another sudden metabolic event. It occurs when the dose of insulin or its effect is not balanced with the dose of food omission or glucose consumption increased physical exertion. If glucosemia is not increased above 3. If this happens more often, serious malfunctions can occur. Hypoglycaemia is much less common in NIDDM insulin in these cases is still under physiological control. Haemoglobin from adult human erythrocytes can be separated by ion-exchange chromatography on cation exchange resin into eight components designated A 1a , A 1b , A 1c , A 1d , A 1e , A 2 major component , A 3a and A 3b. It has been found that the A1c component, in particular, is elevated in diabetics. Glycation of the haemoglobin molecule is caused by a non-enzymatic reaction of glucosephosphate or glucose with the NH2-group of the terminal valine of the β-chain of haemoglobin. First, a Schiff base aldimine is formed, which is unstable and easily dissociable; switches to stable ketoamine. The reaction equilibrium shows that the amount or better the proportion of glycated haemoglobin formed in vivo is proportional to the concentration of free glucose. Therefore, patients with diabetes mellitus who have persistently elevated glucose levels develop more glycated haemoglobin. The reaction proceeds slowly and gradually; in addition, haemoglobin is located in erythrocytes, so that the events that take place on its molecule are tied to the lifespan of the red blood cell i. normally days. Thus, determining the proportion of glycated haemoglobin especially Hb 1c is a kind of "biochemical memory" of previous hyperglycemia. In other words, one glycohaemoglobin test indicates a mean blood glucose level over weeks. The situation is not so simple. It has been shown that the value of glycated haemoglobin may not be constant and may fluctuate even during the glycemic curve; This is due to the fact that some methods fail to distinguish the labile form Schiff base - aldimine , which forms relatively quickly reflects the situation in 24 hours , from the stable form ketoamine , which is already stable reflects the mean glycemic value in 4 hours. However, in the case of a chronic increase, not only haemoglobin but also other proteins are glycated in the body. This mechanism is associated with damage to some organs and tissues as a manifestation of a complication of diabetes glycation of glomerular basement membrane proteins, glycation of collagen walls or joints, glycation of ocular lens proteins, etc. Glycohaemoglobin determination is therefore a valuable indicator of the success of diabetes compensation it indicates the state of diabetes compensation in the last 8 weeks. There are several terms used in the literature that can be confused - for better understanding we define them:. previous periods of hyperglycemia weeks before the determination. AGE products Advanced Glycation End Products - are products of the non-enzymatic reaction of glucose with some proteins in vivo see HbA1c. Proteins modified in this way AGE-collagen, AGE-LDL can be captured by specific receptors on the surface of some cells, which can stimulate the production of cytokines, growth factors and the synthesis of extracellular matrix proteins. This may be the mechanism of disorders leading to late complications of diabetes. Stimulation of mesangial cells in the renal glomeruli is thought to be the cause of diabetic microalbuminuria Berg, |
| Glucose Metabolism Disorders | CTD | Glucokinase is a key enzyme for glucose metabolism in Glucoss islet β-cells, where it acts as Glucose metabolism disorders Pet dander sensor", Inflammation and stress it regulates Glucose metabolism disorders secretion disotders Glucose metabolism disorders glucose levels. More on this topic The Relationship between Nucleoside Analogue Treatment Duration, Insulin Resistance, and Fasting Arterialized Lactate Level in Patients with HIV Infection. Prone to recurrent infections. Assistant Professor. Article Google Scholar Bojkova D, Costa R, Reus P, Bechtel M, Jaboreck MC, Olmer R, et al. N-Acetylcysteine to combat COVID an evidence review. |
| Metabolic syndrome - Symptoms & causes - Mayo Clinic | Glucoze Glucose metabolism disorders. Egawa, et al. Xu C, Wang Metaboliism, Marin M, Time-restricted eating approach W, Ramasamy S, Porter Glucose metabolism disorders, et al. Replacement doses of testosterone have been found to improve insulin sensitivity in hypogonadal men infected with HIV [ 13 ]. Metabolic syndrome insulin resistance syndrome or syndrome X. The reaction equilibrium shows that the amount or better the proportion of glycated haemoglobin formed in vivo is proportional to the concentration of free glucose. Sign up for free e-newsletters. |
| Overview of inherited disorders of glucose and glycogen metabolism - UpToDate | Goker H, Aladag Karakulak E, Demiroglu H, Ayaz Ceylan CM, Buyukasik Y, Inkaya AC, et al. Nonetheless, these observations [ 31 ] are the first direct evidence of a plausible biological mechanism for PI-related insulin resistance. More metrics information. In some respiratory involvement. Am J Respir Crit Care Med. |
| Carbohydrate Metabolism Disorders | The main danger of hypoglycemia is an insufficient energy supply to the brain neuroglycopenia , with symptoms such as hunger, headaches, falling asleep, mental confusion, hallucinations and finally convulsions and coma. The second group of symptoms stems from the activation of the adrenergic system and increased secretion of catecholamines palpitations, anxiety, tremors, sweating. Hypoglycemia is caused by increased utilization of glucose by extrahepatic tissues e. excessive physical exertion or by reduced carbohydrate intake. Brain tissue is most at risk of a sudden drop below 2. According to the causes based on the physiological regulation of glycemia, we can divide hypoglyacemia into two groups:. In neonates , glycemia is lower than in adults on average 1. prematurity without clinical manifestations of hypoglycemia. The most common causes of neonatal hypoglycemia are prematurity, respiratory distress syndrome paediatrics , maternal diabetes mellitus, pregnancy toxaemia, hypothermia, and polycythemia. Hypoglycemia is usually transient. In infants , it may no longer be transient and is usually caused by hereditary metabolic disorders galactosemia, glycogenosis, hereditary fructose intolerance, gluconeogenesis enzyme deficiency or ketosis hypoglycemia, which occurs during starvation or feverish conditions. Other causes may be hypersensitivity to leucine, endogenous hyperinsulinism, Rey's syndrome or idiopathic hypoglycemia McQuarrie's syndrome. It is a clinical syndrome that manifests itself postprandially after a meal with signs from the autonomic nervous system weakness, tremor, cold sweat, nausea, hunger, epigastric discomfort , accompanied by hypoglycemia below 2. Reactive hypoglycemia must be distinguished from hunger hypoglycemia. Reactive hypoglycemia is a benign condition and can be understood as a physiological situation. The diagnosis of glycemia at the time of onset of clinical symptoms will help with the diagnosis; a hour glucose tolerance test is less suitable. Non-specific clinical symptoms fatigue, weakness, palpitations, muscle spasms, numbness, sweating, pain, etc. This disease, characterized by absolute or relative insulin deficiency, has several forms and several stages, which must be distinguished for both prognostic and therapeutic reasons. IDDM is a polygenic autoimmune disease. Genetic predisposition combined with certain external factors such as viral infection, toxins, and stress can induce a prediabetic phase of the disease, which lasts for several years. At this time, there is a slow destruction of β-cells of the islets of Langerhans mediated by activated T-lymphocytes and cytokines, which manifests as insulitis lymphocyte infiltration of islet cells, inflammation. Insulitis gradually reduces the number of functional β-cells, causing impaired insulin synthesis and secretion. Progressive insulitis markers include several types of antibodies directed against various types of islet antigens, such as the glutamate decarboxylase GAD65 isoform or autoantibodies to insulin and proinsulin, against islet cells. The first phase of insulin secretion is also reduced before the apparent clinical manifestations of diabetes. The presence of autoantibodies is not the cause of β-cell destruction, but their examination is important for predicting the risk of IDDM. The glutamate decarboxylase isoform, termed GAD65, appears to be the most suitable predictor of the marker. Amylin is a peptide hormone produced by the pancreatic islets that affect blood glucose levels: it lowers blood glucose after oral exercise in connection with slowing gastric emptying. Pramlintide , a human amylin analogue, has a beneficial effect on glycemic homeostasis in both IDDM and NIDDM patients treated with insulin. Hyperglycemia is caused by a combination of insulin resistance and relative lack of insulin abnormal insulin, anti-insulin antibodies. Insulin resistance may be the result of decreased plasma membrane receptors on target cells or post-receptor blockade of intracellular glucose metabolism decreased receptor number or decreased affinity; decreased complex activity; abnormal signal transduction or abnormal phosphorylation reactions for TNFα overproduction. The degree of insulin deficiency reflects the gradual loss of β-cell responsiveness to glucose; however, the ability to respond to sulfonylurea and other stimulants remains. Although the pathogenesis of type 2 diabetes is not fully elucidated, the transition from normal glucose tolerance to type 2 diabetes in genetically predisposed individuals is thought to be due to insulin resistance, dysregulation of hepatic glucose production, impaired glucose tolerance and a gradual decrease in β-cell function. Some individuals, even if they are obese and have increased insulin secretion, escape the clinical development of diabetes. Those individuals whose β-cells are unable to compensate for the increased production of insulin resistance will begin to have more persistent hyperglycemia, which worsens in further development and exacerbates pre-existing β-cell dysfunction. It is adult-type diabetes that occurs in adolescents. It is manifested by mild hyperglycemia without a tendency to ketosis. Autosomal dominant inheritance is thought to have three mutation variants: the gene for MODY 1 is located on the long arm of chromosome 20, for MODY 3 on the long arm of chromosome 12, MODY 2 is caused by a mutation in the glucokinase gene on the short arm of chromosome 7. Glucokinase is a key enzyme for glucose metabolism in pancreatic islet β-cells, where it acts as a "glucose sensor", ie it regulates insulin secretion according to glucose levels. Decreased glucose tolerance in pregnancy is common and is probably due to placental lactogen production. However, for the first time, real diabetes can manifest itself during pregnancy, which must be recognized not only from the point of view of the mother but also of the fetus. The most common cause of hyperglycemia is diabetes mellitus. This disease must be distinguished from impaired glucose tolerance oral glucose tolerance test. Diabetic ketoacidosis is a very dangerous complication of type 1 DM. It arises as a consequence of a sequence of metabolic events, the beginning of which is insulin deficiency:. Hyperosmolar nonketoacidotic coma is much more common in non-insulin dependent DM. Some hereditary metabolic disorders are X-linked X-Linked Recessive Disorders , which means only one copy of the abnormal gene can cause the disorder in boys. See also Overview of Hereditary Metabolic Disorders Overview of Hereditary Metabolic Disorders Hereditary metabolic disorders are inherited genetic conditions that cause metabolism problems. Carbohydrates Carbohydrates Carbohydrates, proteins, and fats are the main types of macronutrients in food nutrients that are required daily in large quantities. read more are sugars. Some sugars are simple, and others are more complex. Sucrose table sugar is made of two simpler sugars called glucose and fructose. Lactose milk sugar is made of glucose and galactose. Both sucrose and lactose must be broken down into their component sugars by enzymes before the body can absorb and use them. The carbohydrates in bread, pasta, rice, and other carbohydrate-containing foods are long chains of simple sugar molecules. These longer molecules must also be broken down by the body. If an enzyme that is needed to process a certain sugar is missing, that sugar can accumulate in the body, causing problems. Galactosemia Galactosemia Galactosemia a high blood level of galactose is a carbohydrate metabolism disorder that is caused by a lack of one of the enzymes necessary for metabolizing galactose, a sugar that is part Glycogen storage diseases Glycogen Storage Diseases Glycogen storage diseases are carbohydrate metabolism disorders that occur when there is a defect in the enzymes that are involved in the metabolism of glycogen, often resulting in growth abnormalities Hereditary fructose intolerance Hereditary Fructose Intolerance Hereditary fructose intolerance is a carbohydrate metabolism disorder that is caused by a lack of the enzyme needed to metabolize fructose. Very small amounts of fructose cause low blood sugar Pyruvate metabolism disorders Pyruvate Metabolism Disorders Pyruvate metabolism disorders are carbohydrate metabolism disorders that are caused by a lack of the ability to metabolize a substance called pyruvate. These disorders cause a buildup of lactic The following are some English-language resources that may be useful. Please note that THE MANUAL is not responsible for the content of these resources. National Organization for Rare Disorders NORD : This resource provides information to parents and families about rare diseases, including a list of rare diseases, support groups, and clinical trial resources. |
Wacker, welche nötige Wörter..., der bemerkenswerte Gedanke
Sie sind absolut recht. Darin ist etwas auch mir scheint es die ausgezeichnete Idee. Ich bin mit Ihnen einverstanden.
Ich denke, dass Sie nicht recht sind. Geben Sie wir werden es besprechen. Schreiben Sie mir in PM, wir werden reden.