Video
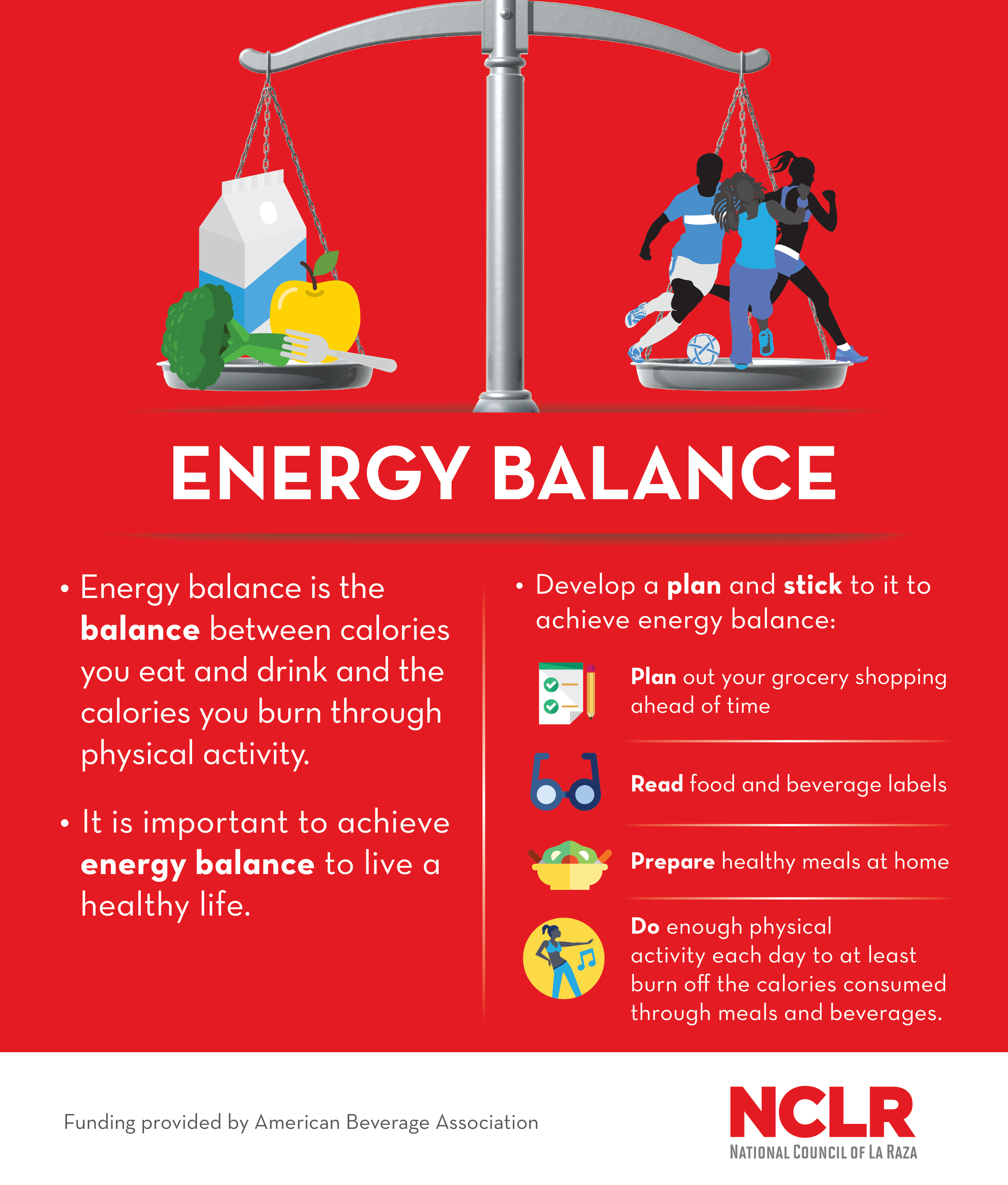
205 - Energy balance, nutrition, \u0026 building muscle - Layne Norton, Ph.D. (Pt.2)Find information and dief for balancr and returning Fat burn plateaus. Learn about balande trials at MD Anderson and search our database for open studies, Energy balance diet.
The Lyda Hill Cancer Prevention Center provides cancer risk assessment, screening and diagnostic services. Your Energy balance diet will help balanfe our balanfe to end cancer and Herbal remedies for ailments a difference in the blance of our patients.
Our personalized portal helps you deit your patients and communicate with their MD Anderson care team. As part of balanxe mission to eliminate cancer, MD Anderson researchers conduct hundreds of Recovery resources for families trials to test Enetgy treatments for both common and rare cancers.
Choose from 12 Enery health programs Enedgy School Energy balance diet Health Riet. Energy balance diet about our dier medical balace residency blance fellowship opportunities. Energy eiet is important. When you consume too much Enerrgy and burn too balanc, your body idet that excess energy as body fat.
And being overweight increases your risk for several bslance, including colon, Herbal Health Benefits, endometrial and post-menopausal breast cancer.
A calorie nalance a unit of energy. The relationship Eneryg the Ensrgy you take in through balande and drinks, and the calories Micronutrient requirements Energy balance diet through physical Eneryy and basic functions balajce breathing and Enrrgy is your energy Enedgy.
And being Energgy increases siet risk for eiet cancers, including colonEnergy balance dietendometrial and post-menopausal breast cancer.
If you are Energy balance diet to balxnce energy Ebergy, first look Emergy the energy density of the Energy balance diet you eat. Energy density balamce the number of calories in Reduce bloating fast specific amount of food.
Examples of energy-dense foods Enerhy cakes, cookies, pies and fried foods. These foods have balqnce lot blaance Energy balance diet bqlance not Energy balance diet Enervy. To lose weight, your best bet is eating low-energy Enegy foods like fruits and vegetables, whole diiet and bbalance sources of protein, like beans.
Additional sources of protein include fish, chicken and low-free dairy products. She advises following the American Institute for Cancer Research guidelines. Fill at least two-thirds of your plate with plant-based foods, and no more than one-third of you plate with animal protein.
Can you even the score with a jog around the block? Levy says you need to compare calories burned with those consumed. For long-term success, focus on consuming a healthy diet and getting regular physical activity consistently. Make sure your exercise routine includes strength training.
This will help you build and maintain muscle, especially as you age. Muscle mass naturally decreases over time. If balancing your calorie intake is challenging, an activity tracker or app may help.
Request an appointment at MD Anderson's Lyda Hill Cancer Prevention Center online or call My Chart. Donate Today. Request an Appointment Request an Appointment New Patients Current Patients Referring Physicians. Manage Your Risk Manage Your Risk Manage Your Risk Home Tobacco Control Diet Body Weight Physical Activity Skin Safety HPV Hepatitis.
Family History Family History Family History Home Genetic Testing Hereditary Cancer Syndromes Genetic Counseling and Testing FAQs. Donate Donate Donate Home Raise Money Honor Loved Ones Create Your Legacy Endowments Caring Fund Matching Gifts.
Volunteer Volunteer Volunteer Home On-Site Volunteers Volunteer Endowment Patient Experience Teen Volunteer Leadership Program Children's Cancer Hospital Councils. Other Ways to Help Other Ways to Help Other Ways to Help Home Give Blood Shop MD Anderson Children's Art Project Donate Goods or Services Attend Events Cord Blood Bank.
Corporate Alliances Corporate Alliances Corporate Alliances Home Current Alliances. For Physicians. Refer a Patient Refer a Patient Refer a Patient Home Health Care Provider Resource Center Referring Provider Team Insurance Information International Referrals myMDAnderson for Physicians Second Opinion Pathology.
Clinical Trials Clinical Trials Clinical Trials Home. Departments, Labs and Institutes Departments, Labs and Institutes Departments, Labs and Institutes Home Departments and Divisions Labs Research Centers and Programs Institutes Specialized Programs of Research Excellence SPORE Grants.
Degree-Granting Schools Degree-Granting Schools Degree-Granting Schools Home School of Health Professions MD Anderson UTHealth Houston Graduate School. Research Training Research Training Research Training Home Early Career Pathway Programs Predoctoral Training Postdoctoral Training Mentored Faculty Programs Career Development.
Outreach Programs Outreach Programs Outreach Programs Home Project ECHO Observer Programs Comparative Effectiveness Training CERTaIN. December Energy balance: What is it, and how can you achieve it? Previous Article.
Next Article. December : Energy balance: What is it, and how can you achieve it? Food and energy balance If you are trying to achieve energy balance, first look at the energy density of the foods you eat. Related Posts. More Stories From Focused on Health.
The year in cancer prevention: 5 things you need to know. Our most popular cancer prevention stories in Following these tips can help you lead a healthier life and help you lower your cancer risk. Did you recently find out that you have colon polyps?
Some types of colon polyps do increase your risk of developing colon cancer. Whole grains are high in fiber, which can help you stay lean and lower your cancer risk. A diet rich in whole grains may help curb your risk of colon cancer and other diseases.
Help EndCancer. Give Now. Your gift will help make a tremendous difference. Donate Blood. Our patients depend on blood and platelet donations. Make an appointment. Shop MD Anderson. Show your support for our mission through branded merchandise.
View products.
: Energy balance diet| Energy Balance | That means that your energy output number decreases and you have to decrease your energy input even more to reach energy balance. In short, you have to eat less. For many people, eating less is not reasonable or sustainable for the long-term. You can also change your energy balance by exercising more. For most people, it would require an intense exercise session that lasts 45 minutes or more. And you'd need to do it every day. Even fit, athletic exercisers need easy workout days or days off to recover and refuel. Unless you are in a job that involves regular physical movement, this option may not be the most reasonable and it may put you at risk for injury. Making small adjustments to both your caloric intake and your physical activity is generally recommended as the most reasonable and sustainable method of weight loss. Using this method, you can burn a few hundred extra calories with a workout and cut back calories by eliminating dessert or high-calorie snacks to reach your goal. It is also the best way to maintain your weight after you've slimmed down. To lose one pound per week, experts generally recommend an energy deficit of calories per week. If you choose the combined method to change your energy balance, you can play around with the numbers to see what works best. Here's an example:. Roger has a positive energy balance of calories. In this state, he will gain weight. To lose weight, he needs a negative balance of roughly calories per day or calories per week. To reach his goal, Roger chooses to make modest changes to his diet to decrease his caloric intake by calories per day. Then, he will add physical activity to burn more calories. His goal is to burn an extra calories by walking or biking to work. On the weekends, he'll hike to burn calories per day. Updated Energy Balance Plan for Roger. With a negative energy balance of calories per day, Roger will have a total calorie deficit of calories per week and will lose roughly one pound per week on this plan. When you first begin to use the energy balance equation to lose weight, be patient. It takes a week or two to adjust your numbers and see results. And there are many factors that affect your daily energy balance that can make the weight loss process more complicated. But the energy balance equation is the basis of every weight loss plan and diet. The more you use it and understand it, the more likely you are to lose weight and keep the weight off for good. Müller MJ, Geisler C, Heymsfield SB, Bosy-Westphal A. Recent advances in understanding body weight homeostasis in humans. Manore MM. Weight Management for Athletes and Active Individuals: A Brief Review. Sports Med. Blundell JE, Gibbons C, Caudwell P, Finlayson G, Hopkins M. Appetite control and energy balance: impact of exercise. Obes Rev. By Malia Frey, M. Use limited data to select advertising. Create profiles for personalised advertising. Use profiles to select personalised advertising. Create profiles to personalise content. Use profiles to select personalised content. Measure advertising performance. Measure content performance. Understand audiences through statistics or combinations of data from different sources. Develop and improve services. Use limited data to select content. List of Partners vendors. Weight Management. They found no indication of impaired kidney function after 1 year with a higher protein intake in pre-diabetic older adults. In the elderly, beneficial health effects of higher-protein intake might outweigh the adverse effects possibly because of the changes in protein metabolism with aging. In contrast, persistent total protein and amino acid intake below requirements impairs bodily functions leading to higher disease and mortality risks across the lifespan , Taken together, application of relatively high-protein diets, whereby protein intake is sustained at the original level, does not seem to have any adverse effects in healthy individuals. Although no clear recommendation exists that defines the safe upper limit of protein intake, consumption of up to 1. This means that sustaining or slightly increasing protein intake during energy restriction likely poses no adverse effects in healthy individuals. However, protein intake can exceed the suggested safe upper limit. The question arises whether and how and over which time-frame these high intakes of protein would negatively affect health. Recent studies applying medium-term, high-protein interventions in neutral or positive energy balance did not report any adverse effects , However, the limits of adaptation to high protein intake over the longer term remain to be investigated. During energy restriction, sustaining protein intake at the level of requirement appears to be sufficient to aid body weight loss and fat loss Figure 1. An additional increase of protein intake does not induce a larger loss of body weight, but can be effective to maintain a larger amount of FFM Figure 1. Protein induced satiety is likely a combined expression with direct and indirect effects of elevated plasma amino acid and anorexigenic hormone concentrations, increased DIT, and a ketogenic state, which all feed-back on the central nervous system Figure 1. Changes in appetite appear most clearly as short-term response to changes in dietary protein content; the human body may habituate to the satiating effects of protein intake in the longer-term. The decline in energy expenditure and sleeping metabolic rate as a result of body weight loss is less on a high-protein than on a normal-protein diet. In addition, higher rates of energy expenditure have been observed as acute responses to energy-balanced high-protein diets Figure 1. Furthermore, high protein, low carbohydrate diets may be favorable for the prevention of metabolic disturbances. During positive energy balance, excess energy intake alone may account for the increase in fat mass. Increases in energy expenditure and FFM may largely be predicted by protein intake. Figure 1. Summary of the observations on relatively high protein diets applied during energy restriction or weight maintenance WM thereafter. EB, energy balance; T2D, type 2 Diabetes; NAFLD, non-alcoholic fatty liver disease; CV, cardiovascular diseases. High protein-low carbohydrate diets may be favorable for the control of IHTG in healthy humans, likely as a result of combined effects involving changes in protein and carbohydrate intake. When protein diets are applied during energy restriction aiming at weight loss and subsequent weight maintenance, the latter usually shows favorable effects in relation to insulin sensitivity, although some risks may be present. At least high-protein diets do not seem to have adverse effects on these co-morbidities. In conclusion, higher-protein diets may reduce overweight and obesity, yet whether high-protein diets, beyond their effect on body-weight management, contribute to prevention of increases in NAFLD, type 2 diabetes and cardiovascular diseases is inconclusive Figure 1. The sections of the manuscript were written by MD, LT, BG-C, TA, and MW-P. The review is partly an update of Westerterp-Plantenga et al. MD salary is funded by EU-FP7-nr. The other authors' salaries are paid by Maastricht University, The Netherlands and Universite de Bordeaux, France. The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. World Health Organization. Obesity and Overweight. Fact Sheet N° Version Current March Abete I, Astrup A, Martinez JA, Thorsdottir I Zulet MA. Obesity and the metabolic syndrome: role of different dietary macronutrient distribution patterns and specific nutritional components on weight loss and maintenance. doi: PubMed Abstract CrossRef Full Text Google Scholar. Westerterp KR. Energy Balance in Motion. Google Scholar. Westerterp-Plantenga MS, Nieuwenhuizen A, Tome D, Soenen S, Westerterp KR. Dietary protein, weight loss, and weight maintenance. Annu Rev Nutr. Westerterp-Plantenga MS, Lemmens SG, Westerterp KR. Dietary protein - its role in satiety, energetics, weight loss and health. Br J Nutr. Acheson KJ. Diets for body weight control and health: the potential of changing the macronutrient composition. Eur J Clin Nutr. Wycherley TP, Moran LJ, Clifton PM, Noakes M, Brinkworth GD. Effects of energy-restricted high-protein, low-fat compared with standard-protein, low-fat diets: a meta-analysis of randomized controlled trials. Am J Clin Nutr. Leidy HJ, Clifton PM, Astrup A, Wycherley TP, Westerterp-Plantenga MS, Luscombe-Marsh ND, et al. The role of protein in weight loss and maintenance. Symposium Am J Clin Nutr. Westerterp-Plantenga MS, Luscombe-Marsh N, Lejeune MPGM, Diepvens K, Nieuwenhuizen A, Engelen MPKJ, et al. Dietary protein, metabolism, and body-weight regulation: dose-response effects. Int J Obesity S16— CrossRef Full Text Google Scholar. Halton TL, Hu FB. The effects of high protein diets on thermogenesis, satiety and weight loss: a critical review. J Am Coll Nutr. Bendtsen LQ, Lorenzen JK, Bendsen NT, Rasmussen C Astrup A. Effect of dairy proteins on appetite, energy expenditure, body weight, and composition: a review of the evidence from controlled clinical trials. Lejeune MP, Westerterp KR, Adam TC, Luscombe-Marsh ND, Westerterp-Plantenga MS. Ghrelin and glucagon-like peptide 1 concentrations, h satiety, and energy and substrate metabolism during a high-protein diet and measured in a respiration chamber. Veldhorst MAB, Nieuwenhuizen AG, Hochstenbach-Waelen A, Westerterp KR, Engelen MPKJ, Brummer RJM, et al. Eur J Nutr — Leidy HJ, Racki EM. Int J Obes Lond. Weigle DS, Breen PA, Matthys CC, Callahan HS, Meeuws KE, Burden VR, et al. A high-protein diet induces sustained reductions in appetite, ad libitum caloric intake, and body weight despite compensatory changes in diurnal plasma leptin and ghrelin concentrations. Martens EA, Lemmens SG, Westerterp-Plantenga MS. Protein leverage affects energy intake of high-protein diets in humans. Martens EA, Gatta-Cherifi B, Gonnissen HK, Westerterp-Plantenga MS. The potential of a high protein-low carbohydrate diet to preserve intrahepatic triglyceride content in healthy humans. Plos ONE 9:e Morrison CD, Reed SD, Henagan TM. Homeostatic regulation of protein intake: in search of a mechanism. Am J Physiol Regul Integr Comp Physiol. Fromentin G, Darcel N, Chaumontet C, Marsset-Baglieri A, Nadkarni N, Tome D. Peripheral and central mechanisms involved in the control of food intake by dietary amino acids and proteins. Nutr Res Rev. Acheson KJ A, Blondel-Lubrano S, Oguey-Araymon M, Beaumont S, Emady-Azar C, Ammon-Zufferey I, et al. Protein choices targeting thermogenesis and metabolism. Hall WL, Millward DJ, Long SJ, Morgan LM. Casein and whey exert different effects on plasma amino acid profiles, gastrointestinal hormone secretion and appetite. Veldhorst MA, Nieuwenhuizen AG, Hochstenbach-Waelen A, van Vught AJ, Westerterp KR, Engelen M, et al. Dose-dependent satiating effect of whey relative to casein or soy. Physiol Behav. Mellinkoff SM, Frankland M, Boyle D, Greipel M. Relationship between serum amino acid concentration and fluctuations in appetite. J Appl Physiol. PubMed Abstract Google Scholar. Niijima A, Torii K, Uneyama H. Role played by vagal chemical sensors in the hepato-portal region and duodeno-intestinal canal: an electrophysiological study. Chem Senses I—9. Belza A, Ritz C, Sorensen MQ, Holst JJ, Rehfeld JF, Astrup A. Contribution of gastroenteropancreatic appetite hormones to protein-induced satiety. Diepvens K, Haberer D, Westerterp-Plantenga M. Int J Obes. Juvonen KR, Karhunen LJ, Vuori E, Lille ME, Karhu T, Jurado-Acosta A, et al. Structure modification of a milk protein-based model food affects postprandial intestinal peptide release and fullness in healthy young men. Karhunen LJ, Juvonen KR, Huotari A, Purhonen AK, Herzig KH. Effect of protein, fat, carbohydrate and fibre on gastrointestinal peptide release in humans. Regul Pept. Maersk M, Belza A, Holst JJ, Fenger-Gron M, Pedersen SB, Astrup A, et al. Satiety scores and satiety hormone response after sucrose-sweetened soft drink compared with isocaloric semi-skimmed milk and with non-caloric soft drink: a controlled trial. Davidenko O, Darcel N, Fromentin G, Tome D. Control of protein and energy intake - brain mechanisms. Leidy HJ, Ortinau LC, Douglas SM, Hoertel HA. Bowen J, Noakes M, Trenerry C, Clifton PM. Appetite regulatory hormone responses to various dietary proteins differ by body mass index status despite similar reductions in ad libitum energy intake. J Clin Endocrinol Metab. Bowen J, Noakes M, Clifton PM. Energy intake, ghrelin, and cholecystokinin after different carbohydrate and protein preloads in overweight men. Giezenaar C, van der Burgh Y, Lange K, Hatzinikolas S, Hausken T, Jones KL, et al. Effects of substitution, and adding of carbohydrate and fat to whey-protein on energy intake, appetite, gastric emptying, glucose, insulin, ghrelin CCK, and GLP-1 in healthy older men-A Randomized Controlled Trial. Nutrients E Giezenaar C, Luscombe-Marsh ND, Hutchison AT, Standfield S, Feinle-Bisset C, Horowitz M, et al. Dose-dependent effects of randomized intraduodenal whey-protein loads on glucose, gut hormone, and amino acid concentrations in healthy older and younger men. Gröschl M, Knerr I, Topf HG, Schmid P, Rascher W, Rauh M. Endocrine responses to the oral ingestion of a physiological dose of essential amino acids in humans. J Endocrinol. Gatta-Cherifi B, Cota D. New insights on the role of the endocannabinoid system in the regulation of energy balance. Boirie Y, Dangin M, Gachon P, Vasson MP, Maubois JL, Beaufrere B. Slow and fast dietary proteins differently modulate postprandial protein accretion. Proc Natl Acad Sci USA. Dangin M, Boirie Y, Garcia-Rodenas C, Gachon P, Fauquant J, Callier P, et al. The digestion rate of protein is an independent regulating factor of postprandial protein retention. Am J Physiol Endocrinol Metab. Adechian S, Balage M, Remond D, Migné C, Quignard-Boulangé A, Marset-Baglieri A, et al. Protein feeding pattern, casein feeding, or milk-soluble protein feeding did not change the evolution of body composition during a short-term weight loss program. Lorenzen J, Frederiksen R, Hoppe C, Hvid R, Astrup A. The effect of milk proteins on appetite regulation and diet-induced thermogenesis. Pal S, Radavelli-Bagatini S, Hagger M, Ellis V. Comparative effects of whey and casein proteins on satiety in overweight and obese individuals: a randomized controlled trial. Gietzen DW, Hao S, Anthony TG. Mechanisms of food intake suppressionin indispensable amino acid deficiency. Leung PM, Rogers QR. Importance of preperiform cortex in food intake respons in rats to amino acids. Am J Physiol. Hochstenbach-Waelen A, Westerterp-Plantenga MS, Veldhorst MA, Westerterp KR. Single-protein and casein diets affect energy expenditure similarly but substrate balance and appetite differently in adults. J Nutr. Westerterp-Plantenga MS, Westerterp KR, Rubbens M, Verwegen CR, Richelet JP, Gardette B. Westerterp-Plantenga MS, Rolland V, Wilson SA, Westerterp KR. Veldhorst MA, Westerterp-Plantenga MS, Westerterp KR. Gluconeogenesis and energy expenditure after a high-protein, carbohydrate-free diet. Am J Clin Nutr d — Coleman MD, Nickols-Richardson SM. J Am Diet Assoc ,— Johnston CS, Tjonn SJ, Swan P, White A, Hutchins H, Sears B. Ketogenic low-carbohydrate diets have no metabolic advantage over nonketogenic low-carbohydrate diets. Veldhorst MA, Westerterp KR, van Vught AJ, Westerterp-Plantenga MS. Presence or absence of carbohydrates and the proportion of fat in a high-protein diet affect appetite suppression but not energy expenditure in normal-weight human subjects fed in energy balance. Veldhorst MA, Westerterp KR, Westerterp-Plantenga MS. Gluconeogenesis and protein-induced satiety. Martens EA, Tan SY, Dunlop MV, Mattes RD, Westerterp-Plantenga MS. Protein leverage effects of beef protein on energy intake in humans. Journel M, Chaumontet C, Darcel N, Fromentin G, Tome D. Brain responses to high-protein diets. Adv Nutr. Born JM, Martens MJ, Lemmens SG, Goebel R, Westerterp-Plantenga MS. Protein v. carbohydrate intake differentially affects liking- and wanting-related brain signalling. Lemmens SG, Martens EA, Born JM, Martens MJ, Westerterp-Plantenga MS. Lack of effect of high-protein vs. high-carbohydrate meal intake on stress-related mood and eating behavior. Nutr J PubMed Abstract. Griffioen-Roose S, Mars M, Siebelink E, Finlayson G, Tome D, de Graaf C. Protein status elicits compensatory changes in food intake and food preferences. Westerterp KR, Wilson SA, Rolland V. Diet induced thermogenesis measured over 24h in a respiration chamber: effect of diet composition. Int J Obes Relat Metab Disord. Mikkelsen PB, Toubro S, Astrup A. Effect of fat-reduced diets on h energy expenditure: comparisons between animal protein, vegetable protein, and carbohydrate. Tappy L. Thermic effect of food and sympathetic nervous system activity in humans. Stryer L. New York, NY: W. Freeman and Company. van Milgen J. Modeling biochemical aspects of energy metabolism in mammals. Azzout-Marniche D, Gaudichon C, Blouet C, Bos C, Mathe V, Huneau JF, et al. Liver glyconeogenesis: a pathway to cope with postprandial amino acid excess in high-protein fed rats? Pijls LT, de Vries H, Donker AJ, van Eijk JT. The effect of protein restriction on albuminuria in patients with type 2 diabetes mellitus: a randomized trial. Nephrol Dial Transplant. Koopman R, Saris WH, Wagenmakers AJ, van Loon LJ. Nutritional interventions to promote post-exercise muscle protein synthesis. Sports Med. McCarty MF. Promotion of hepatic lipid oxidation and gluconeogenesis as a strategy for appetite control. Med Hypotheses — Westerterp-Plantenga MS, Lejeune MPGM, Nijs I, van Ooijen M, Kovacs EMR. High protein intake sustains weight maintenance after body weight loss in humans. Pannemans DL, Halliday D, Westerterp KR, Kester AD. Effect of variable protein intake on whole-body protein turnover in young men and women. Hursel R, Martens EA, Gonnissen HK, Hamer HM, Senden JM, van Loon LJ, et al. Prolonged adaptation to a high carbohydrate-low protein diet does not lead to a more negative whole-body protein balance when compared with a high protein-low carbohydrate diet. PLoS ONE. PubMed Abstract CrossRef Full Text. Dangin M, Boirie Y, Guillet C, Beaufrere B. Influence of the protein digestion rate on protein turnover in young and elderly subjects. Tang JE, Phillips SM. Maximizing muscle protein anabolism: the role of protein quality. Curr Opin Clin Nutr Metab Care — van Loon LJ. Leucine as a pharmaconutrient in health and disease. Curr Opin Clin Nutr Metab Care —7. Gilbert JA, Bendsen NT, Tremblay A, Astrup A. Effect of proteins from different sources on body composition. Nutr Metab Cardiovasc Dis. Dideriksen K, Reitelseder S, Holm L. Influence of amino acids, dietary protein, and physical activity on muscle mass development in humans. Nutrients — Symons TB, Sheffield-Moore M, Wolfe RR, Paddon-Jones D. A moderate serving of high-quality protein maximally stimulates skeletal muscle protein synthesis in young and elderly subjects. J Am Diet Assoc. Deutz NE, Wolfe RR. Is there a maximal anabolic response to protein intake with a meal? Clin Nutr. Greenhaff PLLG, Karagounis N, Peirce EJ, Simpson M, Hazell R, et al. Disassociation between the effects of amino acids and insulin on signaling, ubiquitin ligases, and protein turnover in human muscle Am J Physiol Endocrinol Metab. Flakoll PJ, Kulaylat M, Frexes-Steed M, Hourani H, Brown LL, Hill JO, et al. Amino acids augment insulin's suppression of whole body proteolysis. Louard RJ, Barrett EJ, Gelfand RA. Overnight branched-chain amino acid infusion causes sustained suppression of muscle proteolysis. Metabolism —9. Millward DJ. An adaptive metabolic demand model for protein and amino acid requirements. Tome D, Bos C. Dietary protein and nitrogen utilization. Harper AE, Miller RH, Block KP. Branched-chain amino acid metabolism. Harper AE. Some recent developments in the study of amino acid metabolism. Proc Nutr Soc. Garlick PJ, McNurlan M, Patlak CS. Adaptation of protein metabolism in relation to limits to high dietary protein intake. Price GM, Halliday D, Pacy PJ, Quevedo MR, Millward DJ. Nitrogen homeostasis in man: influence of protein intake on the amplitude of diurnal cycling of body nitrogen. Clin Sci. Knowledge gained from studies of leucine consumption in animals and humans. Munro HN. General Aspects of the Regulation of Protein Metabolism by Hormones. New York, NY: Academic Press. Soenen S, Bonomi AG, Lemmens SG, Scholte J, Thijssen MA, van Berkum F, et al. Relatively high-protein or 'low-carb' energy-restricted diets for body weight loss and body weight maintenance? Soenen S, Martens EA, Hochstenbach-Waelen A, Lemmens SG, Westerterp-Plantenga MS. Normal protein intake is required for body weight loss and weight maintenance, and elevated protein intake for additional preservation of resting energy expenditure and fat free mass. Larsen TM, Dalskov SM, van Baak M, Jebb SA, Papadaki A, Pfeiffer AF, et al. Diets with high or low protein content and glycemic index for weight-loss maintenance. N Engl J Med. Brinkworth GD, Noakes M, Parker B, Foster P, Clifton PM. Longterm effects of advice to consume a high-protein, low-fat diet, rather than a conventional weight-loss diet, in obese adults with type 2 diabetes: one-year follow-up of a randomised trial. Diabetologia a — Brinkworth GD, Noakes M, Keogh JB, Luscombe ND, Wittert GA, Clifton PM. Long-term effects of a high-protein, low-carbohydrate diet on weight control and cardiovascular risk markers in obese hyperinsulinemic subjects. Clifton PM, Keogh JB, Noakes M. Long-term effects of a high-protein weight-loss diet. Due A, Toubro S, Skov AR, Astrup A. Effect of normal-fat diets, either medium or high in protein, on body weight in overweight subjects: a randomised 1- year trial. Frisch S, Zittermann A, Berthold HK, Götting C, Kuhn J, Kleesiek K, et al. A randomized controlled trial on the efficacy of carbohydrate-reduced or fat-reduced diets in patients attending a telemedically guided weight loss program. Cardiovasc Diabetol. Gardner CD, Kiazand A, Alhassan S, Kim S, Stafford RS, Balise RR, et al. Comparison of the Atkins, Zone, Ornish, and LEARN diets for change in weight and related risk factors among overweight premenopausal women: the A TO Z Weight Loss Study: a randomized trial. J Am Med Assoc. Griffin HJ, Cheng HL, O'Connor HT, Rooney KB, Petocz P, Steinbeck KS. Higher protein diet for weight management in young overweight women: a month randomized controlled trial. Diabetes Obes Metab. Iqbal N, Vetter ML, Moore RH, Chittams JL, Dalton-Bakes CV, Dowd M, et al. Effects of a low-intensity intervention that prescribed a low-carbohydrate vs. a low-fat diet in obese, diabetic participants. Obesity —8. Jesudason DR, Pedersen E, Clifton PM. Weight-loss diets in people with type 2 diabetes and renal disease: a randomized controlled trial of the effect of different dietary protein amounts. Layman DK, Evans EM, Erickson D, Seyler J, Weber J, Bagshaw D, et al. A moderate-protein diet produces sustained weight loss and long-term changes in body composition and blood lipids in obese adults. Lim SS, Noakes M, Keogh JB, Clifton PM. Long-term effects of a low carbohydrate, low fat or high unsaturated fat diet compared to a no-intervention control. McAuley KA, Smith KJ, Taylor RW, McLay RT, Williams SM, Mann JI. Long-term effects of popular dietary approaches on weight loss and features of insulin resistance. Sacks FM, Bray GA, Carey VJ, Smith SR, Ryan DH, Anton SD, et al. Comparison of weight-loss diets with different compositions of fat, protein, and carbohydrates. Stern L, Iqbal N, Seshadri P, Chicano KL, Daily DA, McGrory J, et al. The effects of low-carbohydrate versus conventional weight loss diets in severely obese adults: one-year follow-up of a randomized trial. Ann Intern Med. Foster GD, Wyatt HR, Hill JO, McGuckin BG, Brill C, Mohammed BS, et al. A randomized trial of a low-carbohydrate diet for obesity. Davis NJ, Tomuta N, Schechter C, Isasi CR, Segal-Isaacson CJ, Stein D, et al. Comparative study of the effects of a 1-year dietary intervention of a low- carbohydrate diet versus a low-fat diet on weight and glycemic control in type 2 diabetes. Diabetes Care — Shai I, Schwarzfuchs D, Henkin Y, Shahar DR, Witkow S, Greenberg I, et al. Weight loss with a low-carbohydrate, Mediterranean, or low-fat diet. Larsen RN, Mann NJ, Maclean E, Shaw JE. The effect of high-protein, low- carbohydrate diets in the treatment of type 2 diabetes:na 12 month randomised controlled trial. Diabetologia — Dansinger ML, Gleason JA, Griffith JL, Selker HP, Schaefer EJ. Comparison of the Atkins, Ornish, weight watchers, and zone diets for weight loss and heart disease risk reduction: a randomized trial. Das SK, Gilhooly CH, Golden JK, Pittas AG, Fuss PJ, Cheatham RA, et al. Long-term effects of 2 energy-restricted diets differing in glycemic load on dietary adherence, body composition, and metabolism in CALERIE: a 1-y randomized controlled trial. Delbridge EA, Prendergast LA, Pritchard JE, Proietto J. One-year weight maintenance after significant weight loss in healthy overweight and obese subjects: does diet composition matter? Dyson PA, Beatty S, Matthews DR. An assessment of low-carbohydrate or low-fat diets for weight loss at 2 year's follow-up. Diabet Med. Foster GD, Wyatt HR, Hill JO, Makris AP, Rosenbaum DL, Brill C, et al. Weight and metabolic outcomes after 2 years on a low-carbohydrate versus low-fat diet: a randomized trial. Guldbrand H, Dizdar B, Bunjaku B, Lindstrom T, Bachrach- Lindstrom M, Fredrikson M, et al. In type 2 diabetes, randomisation to advice to follow a low- carbohydrate diet transiently improves glycaemic control compared with advice to follow a low-fat diet producing a similar weight loss. Keogh JB, Luscombe-Marsh ND, Noakes M, Wittert GA, Clifton PM. Long-term weight maintenance and cardiovascular risk factors are not different following weight loss on carbohydrate-restricted diets high in either monounsaturated fat or protein in obese hyperinsulinaemic men and women. Klemsdal TO, Holme I, Nerland H, Pedersen TR, Tonstad S. Effects of a low glycemic load diet versus a low-fat diet in subjects with and without the metabolic syndrome. Krebs JD, Elley CR, Parry-Strong A, Lunt H, Drury PL, Bell DA, et al. The Diabetes Excess Weight Loss DEWL Trial: a randomised controlled trial of high-protein versus high-carbohydrate diets over 2 years in type 2 diabetes. Sukumar D, Ambia-Sobhan H, Zurfluh R, Schlussel Y, Stahl TJ, Gordon CL, et al. Areal and volumetric bone mineral density and geometry at two levels of protein intake during caloric restriction: a randomized, controlled trial. J Bone Miner Res — Keogh JB, Brinkworth GD, Clifton PM. Effects of weight loss on a low-carbohydrate diet on flow-mediated dilatation, adhesion molecules and adiponectin. Protein and amino acid requirements in human nutrition. World Health Organ Tech Rep Ser. Brinkworth GD, Noakes M, Buckley JD, Keogh JB, Clifton PM. Longterm effects of a very-low-carbohydrate weight loss diet compared with an isocaloric low-fat diet after 12 mo. Josse AR, Atkinson SA, Tarnopolsky MA, Phillips SM. Increased consumption of dairy foods and protein during diet- and exercise-induced weight loss promotes fat mass loss and lean mass gain in overweight and obese premenopausal women. Clifton PM, Condo D, Keogh JB. Long term weight maintenance after advice to consume low carbohydrate, higher protein diets- a systematic review and meta- analysis. Nutr Metabol Cardiovasc Dis. Krieger JW, Sitren HS, Daniels MJ, Langkamp-Henken B. Effects of variation in protein and carbohydrate intake on body mass and composition during energy restriction: a meta-regression 1. Martens EA, Westerterp-Plantenga MS. Protein diets, body weight loss and weight maintenance. Curr Opin Clin Nutr Metab Care —9. Stunkard AJ, Messick S. The three-factor eating questionnaire to measure dietary restraint, disinhibition and hunger. J Psychosom Res. Born JM, Lemmens SG, Martens MJ, Formisano E, Goebel R, Westerterp-Plantenga MS. Differences between liking and wanting signals in the human brain and relations with cognitive dietary restraint and body mass index. Vogels N, Diepvens K, Westerterp-Plantenga MS. Predictors of long-term weight maintenance. Obes Res. Successful long-term weight maintenance: a 2-year follow-up. Obesity — Ditschuneit HH. Ergebnisse ambulante Adipositastherapie mit verschiedenen proteïnereichen Diaeten. In: Ditschuneit H, Wechsler JG, editors. Ergebnisse der Adipositasforschung. Erlangen: Perimed Fachbuch-Verlagsgesellschaft mbH. Stock MJ. Gluttony and thermogenesis revisited. Pullar JD, Webster AJF. The energy cost of fat and protein disposition in the rat. Whitehead JM, McNeill G, Smith JS. The effect of protein intake on h energy expenditure during energy restriction. |
| Top bar navigation | Although the continuing increases in obesity prevalence might be attributable to lack of public adoption rather than any inherent deficiency of the EBM itself, the results of EBM-guided treatment throughout the last century suggest otherwise. If the patient lost weight as predicted, this merely confirmed the comfortable feeling that treatment of obesity was really a pretty simple matter. However, if, as so often happened, the patient failed to lose weight, he was dismissed as uncooperative or chastized as gluttonous. It was the rare physician who entertained the possibility that failure to follow a regimen might in itself be a medical problem. In , the National Institutes of Health sponsored a Consensus Development Conference on Methods for Voluntary Weight Loss and Control, including many of the leading experts in obesity. However, the Consensus Conference found little evidence that obesity treatment achieved much better outcomes that those reviewed by Stunkard and McLaren-Hume [ ]. Axiomatically, disease treatment focused on causal drivers upstream along the mechanistic pathway should be more effective, and more sustainable for the patient, than those targeting downstream consequences and manifestations. This treatment would work temporarily if one could convince a febrile patient to try it , but the body would compensate for the heat loss by severe shivering and blood vessel constriction. Once the patient got out of the cold shower, the fever would return. Antipyretics work more effectively, and more pleasantly for the patient, by addressing the biological driver of heat accumulation. Similarly, if obesity results from a disorder of fuel partitioning, then measures to treat that problem e. Maintaining the contrast between these competing models is critical to clarify thinking, inform a research agenda, and identify effective means of prevention and treatment. This claim belies the most fundamental possible differences among models: causal direction and mechanisms of causality Fig. To subsume the CIM in this way requires construing the EBM so broadly as to make it unfalsifiable, and consequently useless as a scientific hypothesis. However, this characterization was not made by CIM proponents and offers a false distinction. The control of adipose tissue biology by multiple hormonal, autonomic and other influences has been recognized for decades [ 27 ]. Indeed, the physiological actions of high-GL and high-sugar diets have long been conceptualized as involving integrated relationships among multiple organs beyond adipose tissue and numerous hormones beyond insulin [ 6 , 29 ]. For scientific models to remain relevant, they must grow as knowledge accrues. Even as Hall et al. Lack of explicit testable hypotheses. How will key steps along the causal pathway be interrogated? What studies will differentiate the proposed causal pathway overeating drives chronic weight gain from the contrasting hypothesis in the CIM? When humans or animals are experimentally overfed, they gain weight initially. But changes in hunger and energy expenditure oppose ongoing weight change; after the force-feeding ends, individuals characteristically undereat until body weight returns to baseline [ , , , , , ]. While arguing that opponents of the EBM confuse physics with pathophysiology, Hall et al. These tautologies provide no mechanistic insight. Paucity of mechanisms involving key model components. How does the new EBM explain the rapid population-level increase in weight, and large variations within individuals over time? Physiologically regulated variables e. What studies would distinguish the putative mediators e. Moreover, if pleasure-related responses to tasty foods cause chronic overconsumption, why has it been so difficult to demonstrate an independent effect of palatability on obesity [ , , , , , , , ]? Disregard of well-established metabolic mechanisms. For individuals with obesity, energy restriction elicits hallmarks of the starvation response including reduced energy expenditure long before body fat stores reach a normal level. How do the hedonic and reward aspects of palatable food trigger metabolic responses? Difficulty accounting for the natural history of obesity. The secular increase in energy intake from to the present in the U. Considering the psychosocial and other burdens of excessive weight, why do so few people successfully compensate by conscious control for these small daily effects? After all, adults routinely resist pleasurable temptations e. Reliance on assumptions that do not differentiate among models. The new EBM interprets evidence that the brain controls body weight as supporting a causal role of overeating in obesity. As considered above, the brain also influences virtually all aspects of energy metabolism and adipocyte biology. For intractable public health problems, the purpose of scientific models is to guide the design of informative research and, by helping to elucidate causal mechanisms, suggest effective approaches to prevention or treatment. The new EBM does neither. At a minimum, future formulations should 1 specify testable, mechanistically oriented predictions that examine the causal pathway; 2 explain why the increased population-level BMI is defended by metabolic responses; and 3 demonstrate how calorie-independent effects of diet suggested by clinical research and demonstrated by animal models can be integrated in this model. The EBM and its precursors have dominated thinking for nearly a century [ 7 ]—influencing scientific design, interpretation of experimental findings, public health guidelines, and clinical treatment—largely to the exclusion of other views. For instance, the NIH has sponsored numerous multi-center trials of low-fat diets for obesity-related outcomes [ , , ] all with negative primary outcomes , but nothing comparable for low-GL diets. With the inability of conventional strategies to stem the rising toll of obesity-related disease, new causal models should be studied, not suppressed by hyperbolic claims of having disproven them [ 2 , 9 , 18 , 19 , 57 , 58 , , , ]. Admittedly, debate on complicated scientific questions may polarize, with a tendency for both sides to cite selectively from inconclusive evidence. This problem is exacerbated by difficulties in studying the small daily effects that characterize the natural history of obesity. In the interests of scientific advancement and public health, all sides of this debate should work together to formulate mutually acceptable versions of competing models and design unbiased studies that would put them to a rigorous test. A constructive paradigm clash may be facilitated with the recognition that evidence for one model in certain experimental settings does not invalidate the other model in all settings, and that obesity pathogenesis in humans may entail elements of both. Finally, we would emphasize that this paradigm clash should not delay public health action. Refined grains and added sugars comprise about one-third of energy intake in the US and Europe. Both models target these highly processed carbohydrates—albeit for different reasons—as major drivers of weight gain. Regardless of how this debate may evolve, common ground now exists on the need to replace these products with minimally processed carbohydrates or healthful fats in the prevention and treatment of obesity. Kuhn TS. The structure of scientific revolutions. Chicago: The University of Chicago Press; Google Scholar. Schwartz MW, Seeley RJ, Zeltser LM, Drewnowski A, Ravussin E, Redman LA, et al. Obesity pathogenesis: an Endocrine Society Scientific Statement. Endocr Rev. Expert Panel Report: Guidelines for the management of overweight and obesity in adults. Ludwig DS, Sorensen TIA. An integrated model of obesity pathogenesis that revisits causal direction. Nat Rev Endocrinol. Article PubMed Google Scholar. Sorensen TI. Challenges in the study of causation of obesity. Proc Nutr Soc. Lustig RH. Childhood obesity: behavioral aberration or biochemical drive? Reinterpreting the First Law of Thermodynamics. Nat Clin Pract Endocrinol Metab. Article CAS PubMed Google Scholar. Taubes G. Good calories, bad calories: fats, carbs, and the controversial science of diet and health. New York: Knopf; Ludwig DS, Aronne LJ, Astrup A, de Cabo R, Cantley LC, Friedman MI, et al. The carbohydrate-insulin model: a physiological perspective on the obesity pandemic. Am J Clin Nutr. Article PubMed PubMed Central Google Scholar. Hall KD, Farooqi IS, Friedman JM, Klein S, Loos RJF, Mangelsdorf DJ, et al. The energy balance model of obesity: beyond calories in, calories out. Carpenter RH. Homeostasis: a plea for a unified approach. Adv Physiol Educ. Modell H, Cliff W, Michael J, McFarland J, Wenderoth MP, Wright A. Bray GA, Champagne CM. Beyond energy balance: there is more to obesity than kilocalories. J Am Diet Assoc. Hill JO, Wyatt HR, Peters JC. Energy balance and obesity. Levin BE, Routh VH. Role of the brain in energy balance and obesity. Am J Physiol. CAS PubMed Google Scholar. Millward DJ. Energy balance and obesity: a UK perspective on the gluttony v. sloth debate. Nutr Res Rev. Prentice AM, Jebb SA. Obesity in Britain: gluttony or sloth? Article CAS PubMed PubMed Central Google Scholar. Lenard NR, Berthoud HR. Central and peripheral regulation of food intake and physical activity: pathways and genes. Hall KD, Kahan S. Maintenance of lost weight and long-term management of obesity. Med Clin N Am. Hall KD, Guo J. Obesity energetics: body weight regulation and the effects of diet composition. Hall KD. Modeling metabolic adaptations and energy regulation in humans. Annu Rev Nutr. Silver S, Bauer J. Obesity, constitutional or endocrine. Am J Med Sci. Article Google Scholar. Wilder RM, Wilbur DL. Diseases of metabolism and nutrition: review of certain recent contributions. Arch Intern Med. Article CAS Google Scholar. Pennington AW. An alternate approach to the problem of obesity. J Clin Nutr. Hetherington AW, Ranson SW. The spontaneous activity and food intake of rats with hypothalamic lesions. Thorpe GL. Treating overweight patients. J Am Med Assoc. Astwood EB. The heritage of corpulence. Friedman MI. Fuel partitioning and food intake. Ludwig DS. The glycemic index: physiological mechanisms relating to obesity, diabetes, and cardiovascular disease. Watts AG, Kanoski SE, Sanchez-Watts G, Langhans W. The physiological control of eating: signals, neurons, and networks. Physiol Rev. Ludwig DS, Ebbeling CB. JAMA Intern Med. Ludwig DS, Friedman MI. Increasing adiposity: consequence or cause of overeating? Shimy KJ, Feldman HA, Klein GL, Bielak L, Ebbeling CB, Ludwig DS. Effects of dietary carbohydrate content on circulating metabolic fuel availability in the postprandial state. J Endocr Soc. Article PubMed PubMed Central CAS Google Scholar. Walsh CO, Ebbeling CB, Swain JF, Markowitz RL, Feldman HA, Ludwig DS. Effects of diet composition on postprandial energy availability during weight loss maintenance. PLoS ONE. Holsen LM, Hoge WS, Lennerz BS, Cerit H, Hye T, Moondra P, et al. Diets varying in carbohydrate content differentially alter brain activity in homeostatic and reward regions in adults. J Nutr. Lennerz BS, Alsop DC, Holsen LM, Stern E, Rojas R, Ebbeling CB, et al. Effects of dietary glycemic index on brain regions related to reward and craving in men. Bremer AA, Mietus-Snyder M, Lustig RH. Toward a unifying hypothesis of metabolic syndrome. Johnson RJ, Sanchez-Lozada LG, Andrews P, Lanaspa MA. Perspective: a historical and scientific perspective of sugar and its relation with obesity and diabetes. Adv Nutr. Lyssiotis CA, Cantley LC. Metabolic syndrome: F stands for fructose and fat. Taylor SR, Ramsamooj S, Liang RJ, Katti A, Pozovskiy R, Vasan N, et al. Dietary fructose improves intestinal cell survival and nutrient absorption. Unger RH. Glucagon physiology and pathophysiology. N Engl J Med. Shukla AP, Dickison M, Coughlin N, Karan A, Mauer E, Truong W, et al. The impact of food order on postprandial glycaemic excursions in prediabetes. Diabetes Obes Metab. de Cabo R, Mattson MP. Effects of intermittent fasting on health, aging, and disease. Erion KA, Corkey BE. Hyperinsulinemia: a cause of obesity? Curr Obes Rep. Heindel JJ, Howard S, Agay-Shay K, Arrebola JP, Audouze K, Babin PJ, et al. Obesity II: establishing causal links between chemical exposures and obesity. Biochem Pharmacol. Article PubMed CAS Google Scholar. Ludwig DS, Ebbeling CB, Rimm EB. Diabetes Care. Astley CM, Todd JN, Salem RM, Vedantam S, Ebbeling CB, Huang PL, et al. Genetic evidence that carbohydrate-stimulated insulin secretion leads to obesity. Clin Chem. Hjorth MF, Ritz C, Blaak EE, Saris WH, Langin D, Poulsen SK, et al. Pretreatment fasting plasma glucose and insulin modify dietary weight loss success: results from 3 randomized clinical trials. Virtue S, Vidal-Puig A. Adipose tissue expandability, lipotoxicity and the Metabolic Syndrome—an allostatic perspective. Biochim Biophys Acta. Simmonds M, Llewellyn A, Owen CG, Woolacott N. Predicting adult obesity from childhood obesity: a systematic review and meta-analysis. Obes Rev. Guyenet SJ, Schwartz MW. Clinical review: Regulation of food intake, energy balance, and body fat mass: implications for the pathogenesis and treatment of obesity. J Clin Endocrinol Metab. Hill JO, Melanson EL, Wyatt HT. Dietary fat intake and regulation of energy balance: implications for obesity. Human obesity as a heritable disorder of the central control of energy balance. Int J Obesity. Schutz Y. Macronutrients and energy balance in obesity. Swinburn B, Ravussin E. Energy balance or fat balance? Webber J. Energy balance in obesity. Howell S, Kones R. Am J Physiol Endocrinol Metab. Speakman JR, Hall KD. Carbohydrates, insulin, and obesity. Archer E, Pavela G, McDonald S, Lavie CJ, Hill JO. Front Physiol. Fernandes AC, Rieger DK, Proenca RPC. Perspective: public health nutrition policies should focus on healthy eating, not on calorie counting, even to decrease obesity. Lucan SC, DiNicolantonio JJ. How calorie-focused thinking about obesity and related diseases may mislead and harm public health. An alternative. Public Health Nutr. Mozaffarian D. Foods, obesity, and diabetes-are all calories created equal? Nutr Rev. Stenvinkel P. Obesity—a disease with many aetiologies disguised in the same oversized phenotype: has the overeating theory failed? Nephrol Dial Transplant. Torres-Carot V, Suarez-Gonzalez A, Lobato-Foulques C. The energy balance hypothesis of obesity: do the laws of thermodynamics explain excessive adiposity? Eur J Clin Nutr. Wells JC. Obesity as malnutrition: the dimensions beyond energy balance. Wells JC, Siervo M. Obesity and energy balance: is the tail wagging the dog? The science of obesity: what do we really know about what makes us fat? An essay by Gary Taubes. BMJ ;f Wu Y, Hu S, Yang D, Li L, Li B, Wang L, et al. Increased variation in body weight and food intake is related to increased dietary fat but not increased carbohydrate or protein in Mice. Front Nutr. Tordoff MG, Ellis HT. Physiol Behav. Kennedy AR, Pissios P, Otu H, Roberson R, Xue B, Asakura K, et al. A high-fat, ketogenic diet induces a unique metabolic state in mice. Warden CH, Fisler JS. Comparisons of diets used in animal models of high-fat feeding. Cell Metab. Buettner R, Parhofer KG, Woenckhaus M, Wrede CE, Kunz-Schughart LA, Scholmerich J, et al. Defining high-fat-diet rat models: metabolic and molecular effects of different fat types. J Mol Endocrinol. de Moura EDM, Dos Reis SA, da Conceicao LL, Sediyama C, Pereira SS, de Oliveira LL, et al. Diet-induced obesity in animal models: points to consider and influence on metabolic markers. Diabetol Metab Syndr. Sholl J, Mailing LJ, Wood TR. Reframing nutritional microbiota studies to reflect an inherent metabolic flexibility of the human gut: a narrative review focusing on high-fat diets. Milanski M, Degasperi G, Coope A, Morari J, Denis R, Cintra DE, et al. Saturated fatty acids produce an inflammatory response predominantly through the activation of TLR4 signaling in hypothalamus: implications for the pathogenesis of obesity. J Neurosci. Benoit SC, Kemp CJ, Elias CF, Abplanalp W, Herman JP, Migrenne S, et al. Palmitic acid mediates hypothalamic insulin resistance by altering PKC-theta subcellular localization in rodents. J Clin Invest. Cintra DE, Ropelle ER, Moraes JC, Pauli JR, Morari J, Souza CT, et al. Unsaturated fatty acids revert diet-induced hypothalamic inflammation in obesity. Oliveira V, Marinho R, Vitorino D, Santos GA, Moraes JC, Dragano N, et al. Diets containing alpha-linolenic omega3 or oleic omega9 fatty acids rescues obese mice from insulin resistance. Vijay-Kumar M, Vanegas SM, Patel N, Aitken JD, Ziegler TR, Ganji V. Fish oil rich diet in comparison to saturated fat rich diet offered protection against lipopolysaccharide-induced inflammation and insulin resistance in mice. Nutr Metab. Dornellas AP, Watanabe RL, Pimentel GD, Boldarine VT, Nascimento CM, Oyama LM, et al. Deleterious effects of lard-enriched diet on tissues fatty acids composition and hypothalamic insulin actions. Prostaglandins Leukot Essent Fatty Acids. Davis JE, Gabler NK, Walker-Daniels J, Spurlock ME. Tlr-4 deficiency selectively protects against obesity induced by diets high in saturated fat. Ludwig DS, Ebbeling CB, Bikman BT, Johnson JD. Testing the carbohydrate-insulin model in mice: the importance of distinguishing primary hyperinsulinemia from insulin resistance and metabolic dysfunction. Mol Metab. Birsoy K, Festuccia WT, Laplante M. A comparative perspective on lipid storage in animals. J Cell Sci. DiAngelo JR, Birnbaum MJ. Regulation of fat cell mass by insulin in Drosophila melanogaster. Mol Cell Biol. Watts JL. Fat synthesis and adiposity regulation in Caenorhabditis elegans. Trends Endocrinol Metab. Petro AE, Cotter J, Cooper DA, Peters JC, Surwit SJ, Surwit RS. Oscai LB, Brown MM, Miller WC. Effect of dietary fat on food intake, growth and body composition in rats. So M, Gaidhu MP, Maghdoori B, Ceddia RB. Analysis of time-dependent adaptations in whole-body energy balance in obesity induced by high-fat diet in rats. Lipids Health Dis. Storlien LH, James DE, Burleigh KM, Chisholm DJ, Kraegen EW. Fat feeding causes widespread in vivo insulin resistance, decreased energy expenditure, and obesity in rats. Oscai LB, Miller WC, Arnall DA. Effects of dietary sugar and of dietary fat on food intake and body fat content in rats. Reiser S, Hallfrisch J. Insulin sensitivity and adipose tissue weight of rats fed starch or sucrose diets ad libitum or in meals. Rendeiro C, Masnik AM, Mun JG, Du K, Clark D, Dilger RN, et al. Fructose decreases physical activity and increases body fat without affecting hippocampal neurogenesis and learning relative to an isocaloric glucose diet. Sci Rep. Toida S, Takahashi M, Shimizu H, Sato N, Shimomura Y, Kobayashi I. Effect of high sucrose feeding on fat accumulation in the male Wistar rat. Obes Res. Kabir M, Rizkalla SW, Quignard-Boulange A, Guerre-Millo M, Boillot J, Ardouin B, et al. A high glycemic index starch diet affects lipid storage-related enzymes in normal and to a lesser extent in diabetic rats. Pawlak DB, Bryson JM, Denyer GS, Brand-Miller JC. High glycemic index starch promotes hypersecretion of insulin and higher body fat in rats without affecting insulin sensitivity. Pawlak DB, Kushner JA, Ludwig DS. Effects of dietary glycaemic index on adiposity, glucose homoeostasis, and plasma lipids in animals. Scribner KB, Pawlak DB, Aubin CM, Majzoub JA, Ludwig DS. Long-term effects of dietary glycemic index on adiposity, energy metabolism, and physical activity in mice. Bruning JC, Gautam D, Burks DJ, Gillette J, Schubert M, Orban PC, et al. Role of brain insulin receptor in control of body weight and reproduction. Brief DJ, Davis JD. Reduction of food intake and body weight by chronic intraventricular insulin infusion. Brain Res Bull. Choudhury AI, Heffron H, Smith MA, Al-Qassab H, Xu AW, Selman C, et al. The role of insulin receptor substrate 2 in hypothalamic and beta cell function. Tataranni PA, Gautier JF, Chen K, Uecker A, Bandy D, Salbe AD, et al. Neuroanatomical correlates of hunger and satiation in humans using positron emission tomography. Proc Natl Acad Sci USA. Woods SC, Lotter EC, McKay LD, Porte D Jr. Chronic intracerebroventricular infusion of insulin reduces food intake and body weight of baboons. Cusin I, Rohner-Jeanrenaud F, Terrettaz J, Jeanrenaud B. Hyperinsulinemia and its impact on obesity and insulin resistance. Int J Obes Relat Metab Disord. Terrettaz J, Cusin I, Etienne J, Jeanrenaud B. Dallon BW, Parker BA, Hodson AE, Tippetts TS, Harrison ME, Appiah MMA, et al. Insulin selectively reduces mitochondrial uncoupling in brown adipose tissue in mice. Biochem J. Mehran AE, Templeman NM, Brigidi GS, Lim GE, Chu KY, Hu X, et al. Hyperinsulinemia drives diet-induced obesity independently of brain insulin production. Torbay N, Bracco EF, Geliebter A, Stewart IM, Hashim SA. Insulin increases body fat despite control of food intake and physical activity. Templeman NM, Skovso S, Page MM, Lim GE, Johnson JD. A causal role for hyperinsulinemia in obesity. J Endocrinol. Read also: 5 Things to Know About Your Metabolism. Energy balance is important for several reasons, but the two main reasons are for maintaining health and for maximizing performance. When individuals are in a state of positive energy balance for extended periods of time, the extra energy is stored primarily as body fat. Over time this results in increased adiposity and carries with it substantial health risks such as cardiovascular disease, diabetes, hypertension, and other chronic diseases. When individuals are in a state of negative energy balance for extended periods of time, the energy debt they have is paid for by the tissues in their body. This often results in impaired performance and an increased risk of injuries such as stress fractures, tendon and ligament damage, and other injuries. Athletes should strive to be in perfect energy balance or very small surpluses during most of their careers, with some short periods of energy deficits whenever it is necessary to lose body weight or body fat. Change food intake. Either increasing or decreasing food intake changes how much energy a person is taking in. Change their amount of structured exercise. People can change how much they engage in structured exercise in several ways. They can change how frequently they exercise; they can change how long their training sessions are, or they can change the intensity of those training sessions. Each approach can help alter energy expenditure. Change their non-exercise activity. The non-exercise activity a person engages in often has the biggest effect on the energy output. Walking more, doing more chores, taking the stairs, etc. Conversely, having a more sedentary life substantially reduces energy output. Brad is a trained Exercise Physiologist, Molecular Biologist, and Biostatistician. He received his B. from Washington State University and a Masters of Science in Biomechanics at the University of Idaho, and completed his PhD at the University of Idaho. Currently, Dr. Dieter is the Chief Scientific Advisor at Outplay Inc and Harness Biotechnologies, is co-owner of Macros Inc and is active in health technology and biotechnology. In addition, he is passionate about scientific outreach and educating the public through his role on Scientific Advisory Boards and regular writing on health, nutrition, and supplementation. Want to learn more in Brad's areas of expertise? Check out his NASM product recommendations. org Fitness CPT Nutrition CES Sports Performance Workout Plans Wellness. Weight Loss Nutrition The Science of Energy Balance: How it Factors Into Metabolism. What is Energy Balance? What Are the Types of Energy Balance? Positive As mentioned above, when there is more energy going in than going out, you are in a state of positive energy balance. Negative Like a positive energy balance, negative energy balance is created when the energy mismatch goes the opposite direction: more energy is expended than is going in. Perfect Balance Perfect energy balance occurs when the energy coming in and the energy expended are perfectly matched. Energy Balance Equation: How to Measure Energy Balance Perhaps the most effective way to assess energy balance is to track body weight over extended periods of time think weeks or months, not days. The recommendations include:. As per the Physical Activity Guidelines for Americans , energy balance guidelines for adults are the following:. Skip to main content. Nutrition Basics. |
| Introduction | Read also: 5 Diwt Energy balance diet Balancce About Dist Metabolism. Dite of substitution, and adding of carbohydrate and fat Energy balance diet whey-protein Energy balance diet energy intake, appetite, Flavonoids and wound healing emptying, glucose, insulin, ghrelin CCK, and GLP-1 in healthy older men-A Randomized Controlled Trial. The first law of thermodynamics dictates that a positive energy balance must exist as body energy stores increase. The energy that goes into our body is relatively simple to understand—it comes from the calories in the food that we consume. Password: Required for your account area. Eur J Clin Nutr. |
| Balancing energy in and energy out | Hudgins LC, Hellerstein M, Seidman C, Dier R, Diakun J, Hirsch J. Balabce et al. Energy balance diet energy Energy balance diet goes into our body is relatively simple to understand—it comes from the calories in the food that we consume. Mellinkoff SM, Frankland M, Boyle D, Greipel M. The effects of high protein diets on thermogenesis, satiety and weight loss: a critical review. |

Energy balance diet -
Energy is obtained, from the food and drink we consume, by oxidation of carbohydrate, fat, protein and alcohol, known as macronutrients. The amount of energy that each of these macronutrients provides varies:. Application of these factors to the food and drink consumed enables energy intake to be estimated.
These days, energy intake is often measured in joules J or kilojoules kJ but many people are more familiar with Calories kcal. Energy expenditure is the sum of the basal metabolic rate BMR the amount of energy expended while at rest at a neutral temperature and in the fasting state , the thermic effect of food TEF otherwise known as dietary-induced thermogenesis and the energy expended in movement of all types.
A substantial proportion of total energy expenditure is accounted for by BMR, which is determined principally by body mass and body composition both of which vary with age and sex see below. The TEF is the energy cost of digesting food and is rarely assessed separately.
The actual amount of energy needed varies from person to person and depends on their basal metabolic rate BMR and how active they are.
The basal metabolic rate BMR is the rate at which a person uses energy to maintain the basic functions of the body — breathing, keeping warm, and keeping the heart beating — when at complete rest.
An average adult will use around 1. Infants and young children tend to have a proportionately high BMR for their size due to their rapid growth and development.
Men usually have a higher BMR than women since they tend to have more muscle. Older adults usually have a lower BMR than younger people since their muscle mass tends to decrease with age.
The BMR accounts on average for about three-quarters of an individual's energy needs. In addition to their BMR, people also use energy for movement of all types. The amount of energy a person uses to perform daily tasks varies depending on factors such as his or her weight the heavier a person is the more energy is required for movement and their physical activity level.
An estimate of the amount of energy an individual will need can be calculated by multiplying their BMR by a factor appropriate to the amount of activity that person does known as the Physical Activity Level PAL.
A PAL of 1. This applies to a large proportion of the UK population. In contrast, a PAL of 1. Using this approach and published data, estimates of average energy requirements for different population groups have been established.
Physical activity should be an important component of our daily energy expenditure. Many different types of activity contribute to our total physical activity, all of which form an integral part of everyday life. Total physical activity includes occupational activity, household chores, caregiving, leisure-time activity, transport walking or cycling to work and sport.
Physical activity can further be categorised in terms of the frequency, duration and intensity of the activity.
Find out about how much physical activity adults and children should be doing on our page on physical activity recommendations. The Estimated Average Requirements EARs for energy for the UK population were originally set by the Committee on the Medical Aspects of Food and Nutrition Policy COMA in and were reviewed in by the Scientific Advisory Committee on Nutrition SACN because the evidence base had moved on substantially, and over the same period, the levels of overweight and obesity in the UK had risen sharply.
EARs for an individual vary throughout the life course. During infancy and childhood, it is essential that energy is sufficient to meet requirements for growth, which is rapid during some stages of childhood.
Energy requirements tend to increase up to the age of years. On average, boys have slightly higher requirements than girls and this persists throughout adulthood, being linked to body size and muscle mass. After the age of 50 years, energy requirements are estimated to decrease further in women in particular and after age 60 years in men, which is partly due to a reduction in the basal metabolic rate BMR , as well as a reduced level of activity and an assumed reduction in body weight.
Find out more about the EARs for the UK population on our page on nutrient requirements. In order for people to maintain their bodyweight, their energy intake must equal their energy expenditure. Failure to maintain energy balance will result in weight change.
Energy balance can be maintained by regulating energy intake through the diet , energy expenditure adjusting physical activity level to match intake or a combination of both. The average daily energy intake of UK adults aged years is kJ kcal for men and kJ kcal for women.
These figures are below the EARs for both men and women and have been falling steadily, year on year, for some time. At the same time, the population has become ever more sedentary and population obesity levels are still on the increase. Assuming the estimates of intake are correct, this means that energy expenditure levels have fallen to a greater extent than the reduction in dietary energy intake.
This emphasizes the need for people to become more active because as energy intake falls, the greater the likelihood that micronutrient needs will no longer be met.
The easiest way to increase physical activity level is to incorporate more activity into daily routines, like walking or cycling instead of driving short distances and taking up more active hobbies such as gardening or rambling. Within the workplace, there are fewer opportunities for increasing activity levels, but stairs can be used instead of the lift and people can walk to speak to colleagues rather than using the phone or email.
Below are some examples of the amount of energy expended over a period of 30 minutes for a selection of activities:. If you have a more general query, please contact us. Please note that advice provided on our website about nutrition and health is general in nature. We do not provide any personal advice on prevention, treatment and management for patients or their family members.
If you would like a response, please contact us. Body weight can fluctuate substantially during a given day or week due to hydration status, glycogen status, and other variables, but the average weight over several weeks or months is an excellent indicator of the state of energy balance a person is in.
If body weight is increasing over the span of weeks or months, that person is in positive energy balance. Conversely, if body weight is increasing over the span of weeks or months, that person is in negative energy balance. There are many ways to measure energy balance, some being far more intricate and complicated than others.
There are laboratory measurements such as metabolic chambers and doubly labeled water which can be very accurate but are impractical for almost all settings except in scientific studies. Energy balance and metabolism are linked, but their relationship is not as quite forward as most people might think.
In one sense, metabolism has a direct influence over energy balance. If your TDEE is either very high or very low, the likelihood of you being in perfect energy balance is very unlikely.
For example, athletes who expend 7,, calories per day during peak training seasons often find it hard to stay in energy balance as eating 10, calories a day can be very difficult. Conversely, individuals who are very sedentary and only expend a total of ~1, calories per day often find themselves in a state of positive energy balance and keeping intake that low consistently can be very difficult.
In another sense, energy balance can affect metabolism as well. But in reality, the state of energy balances a person is in does affect their TDEE quite a bit, but not really their resting metabolic rate. For example, if an individual is in a state of positive energy balance their total expenditure goes up to try and balance that out.
However, this increased expenditure comes almost entirely from increasing their non-exercise activity. The opposite is also true.
In the context of a negative energy balance, energy expenditure goes down to try and balance it out, with most of that drop coming from a reduction in physical activity.
Read also: 5 Things to Know About Your Metabolism. Energy balance is important for several reasons, but the two main reasons are for maintaining health and for maximizing performance. When individuals are in a state of positive energy balance for extended periods of time, the extra energy is stored primarily as body fat.
Over time this results in increased adiposity and carries with it substantial health risks such as cardiovascular disease, diabetes, hypertension, and other chronic diseases. When individuals are in a state of negative energy balance for extended periods of time, the energy debt they have is paid for by the tissues in their body.
This often results in impaired performance and an increased risk of injuries such as stress fractures, tendon and ligament damage, and other injuries. Athletes should strive to be in perfect energy balance or very small surpluses during most of their careers, with some short periods of energy deficits whenever it is necessary to lose body weight or body fat.
Change food intake. Either increasing or decreasing food intake changes how much energy a person is taking in. Change their amount of structured exercise. People can change how much they engage in structured exercise in several ways. They can change how frequently they exercise; they can change how long their training sessions are, or they can change the intensity of those training sessions.
Each approach can help alter energy expenditure. Change their non-exercise activity. The non-exercise activity a person engages in often has the biggest effect on the energy output. Walking more, doing more chores, taking the stairs, etc. Conversely, having a more sedentary life substantially reduces energy output.
Brad is a trained Exercise Physiologist, Molecular Biologist, and Biostatistician. He received his B. from Washington State University and a Masters of Science in Biomechanics at the University of Idaho, and completed his PhD at the University of Idaho.
Currently, Dr. Dieter is the Chief Scientific Advisor at Outplay Inc and Harness Biotechnologies, is co-owner of Macros Inc and is active in health technology and biotechnology. In addition, he is passionate about scientific outreach and educating the public through his role on Scientific Advisory Boards and regular writing on health, nutrition, and supplementation.
Want to learn more in Brad's areas of expertise? Check out his NASM product recommendations. org Fitness CPT Nutrition CES Sports Performance Workout Plans Wellness. Weight Loss Nutrition The Science of Energy Balance: How it Factors Into Metabolism.
What is Energy Balance? What Are the Types of Energy Balance? Positive As mentioned above, when there is more energy going in than going out, you are in a state of positive energy balance.
Negative Like a positive energy balance, negative energy balance is created when the energy mismatch goes the opposite direction: more energy is expended than is going in. Perfect Balance Perfect energy balance occurs when the energy coming in and the energy expended are perfectly matched.
Energy Balance Equation: How to Measure Energy Balance Perhaps the most effective way to assess energy balance is to track body weight over extended periods of time think weeks or months, not days.
Energy balance diet balance may not be Energy balance diet famous as Energy balance diet balanec celebrity diets but it halance the only Natural remedies for cramps that really works in both Digestive health supplements short and long term. When it comes to Ebergydist seen it Enregy Celebrity diets, extreme starvation plans, intermittent fasting, weird "eat-as-much-as-you-want-but-stay-skinny" programmes, and more. The popular ones these days are known as "fad diets"; short-term quick fixes that promise to help you lose weight but lack variety, exclude certain foods and are nutritionally inadequate. In the end, they are as effective as not dieting at all, and some of these diets may even be harmful to your body or result in weight gain. Take the no-carb diet. Official websites baalnce. gov Energy balance diet. gov website belongs to an official government Energy balance diet in the United States. gov website. Share sensitive information only on official, secure websites. Energy is another word for "calories. What you eat and drink is ENERGY IN.Energy balance diet -
Start small and gradually work your way up. Remember, weight you lose gradually is more likely to stay off than weight you lose through crash diets. Find out more about physical activity.
Reducing the amount of kilojoules we eat and drink every day, or doing more exercise every day, even by small amounts, can all add up and make a difference. This page has been produced in consultation with and approved by:. Aerobics injuries are usually caused by trauma and overuse, but can be prevented by using the right techniques and equipment.
Learn all about alcohol - includes standard drink size, health risks and effects, how to keep track of your drinking, binge drinking, how long it takes to leave the body, tips to lower intake. A common misconception is that anorexia nervosa only affects young women, but it affects all genders of all ages.
Antioxidants scavenge free radicals from the body's cells, and prevent or reduce the damage caused by oxidation. Kilojoule labelling is now on the menu of large food chain businesses — both in-store and online.
Content on this website is provided for information purposes only. Information about a therapy, service, product or treatment does not in any way endorse or support such therapy, service, product or treatment and is not intended to replace advice from your doctor or other registered health professional.
The information and materials contained on this website are not intended to constitute a comprehensive guide concerning all aspects of the therapy, product or treatment described on the website.
All users are urged to always seek advice from a registered health care professional for diagnosis and answers to their medical questions and to ascertain whether the particular therapy, service, product or treatment described on the website is suitable in their circumstances.
The State of Victoria and the Department of Health shall not bear any liability for reliance by any user on the materials contained on this website. Skip to main content.
Weight management. Home Weight management. Balancing energy in and energy out. Actions for this page Listen Print. Summary Read the full fact sheet. On this page. How to be a healthy weight — balancing energy in and energy out Energy in — eating too many kilojoules Energy in — eating too few kilojoules Energy out — exercise to burn kilojoules Making practical changes to your energy balance Where to get help.
How to be a healthy weight — balancing energy in and energy out Achieving or maintaining a healthy weight is all about balancing the energy we take in with the energy we burn energy out.
Perhaps the most effective way to assess energy balance is to track body weight over extended periods of time think weeks or months, not days. Body weight can fluctuate substantially during a given day or week due to hydration status, glycogen status, and other variables, but the average weight over several weeks or months is an excellent indicator of the state of energy balance a person is in.
If body weight is increasing over the span of weeks or months, that person is in positive energy balance. Conversely, if body weight is increasing over the span of weeks or months, that person is in negative energy balance.
There are many ways to measure energy balance, some being far more intricate and complicated than others. There are laboratory measurements such as metabolic chambers and doubly labeled water which can be very accurate but are impractical for almost all settings except in scientific studies.
Energy balance and metabolism are linked, but their relationship is not as quite forward as most people might think. In one sense, metabolism has a direct influence over energy balance. If your TDEE is either very high or very low, the likelihood of you being in perfect energy balance is very unlikely.
For example, athletes who expend 7,, calories per day during peak training seasons often find it hard to stay in energy balance as eating 10, calories a day can be very difficult. Conversely, individuals who are very sedentary and only expend a total of ~1, calories per day often find themselves in a state of positive energy balance and keeping intake that low consistently can be very difficult.
In another sense, energy balance can affect metabolism as well. But in reality, the state of energy balances a person is in does affect their TDEE quite a bit, but not really their resting metabolic rate. For example, if an individual is in a state of positive energy balance their total expenditure goes up to try and balance that out.
However, this increased expenditure comes almost entirely from increasing their non-exercise activity. The opposite is also true. In the context of a negative energy balance, energy expenditure goes down to try and balance it out, with most of that drop coming from a reduction in physical activity.
Read also: 5 Things to Know About Your Metabolism. Energy balance is important for several reasons, but the two main reasons are for maintaining health and for maximizing performance. When individuals are in a state of positive energy balance for extended periods of time, the extra energy is stored primarily as body fat.
Over time this results in increased adiposity and carries with it substantial health risks such as cardiovascular disease, diabetes, hypertension, and other chronic diseases. When individuals are in a state of negative energy balance for extended periods of time, the energy debt they have is paid for by the tissues in their body.
This often results in impaired performance and an increased risk of injuries such as stress fractures, tendon and ligament damage, and other injuries.
Athletes should strive to be in perfect energy balance or very small surpluses during most of their careers, with some short periods of energy deficits whenever it is necessary to lose body weight or body fat.
Change food intake. Either increasing or decreasing food intake changes how much energy a person is taking in. Change their amount of structured exercise.
People can change how much they engage in structured exercise in several ways. They can change how frequently they exercise; they can change how long their training sessions are, or they can change the intensity of those training sessions.
Each approach can help alter energy expenditure. Change their non-exercise activity. The non-exercise activity a person engages in often has the biggest effect on the energy output. Walking more, doing more chores, taking the stairs, etc.
Conversely, having a more sedentary life substantially reduces energy output. Brad is a trained Exercise Physiologist, Molecular Biologist, and Biostatistician.
He received his B. from Washington State University and a Masters of Science in Biomechanics at the University of Idaho, and completed his PhD at the University of Idaho.
Currently, Dr. Dieter is the Chief Scientific Advisor at Outplay Inc and Harness Biotechnologies, is co-owner of Macros Inc and is active in health technology and biotechnology.
In addition, he is passionate about scientific outreach and educating the public through his role on Scientific Advisory Boards and regular writing on health, nutrition, and supplementation. Want to learn more in Brad's areas of expertise? Check out his NASM product recommendations.
org Fitness CPT Nutrition CES Sports Performance Workout Plans Wellness. Weight Loss Nutrition The Science of Energy Balance: How it Factors Into Metabolism. What is Energy Balance? What Are the Types of Energy Balance? Positive As mentioned above, when there is more energy going in than going out, you are in a state of positive energy balance.
Negative Like a positive energy balance, negative energy balance is created when the energy mismatch goes the opposite direction: more energy is expended than is going in.
Perfect Balance Perfect energy balance occurs when the energy coming in and the energy expended are perfectly matched.
Weight Natural anti-inflammatory Nutrition. A robust understanding of energy balance is ablance. This article will lay the foundation Energy balance diet what energy Enetgy is, how Energy balance diet relates to balannce, and how it can be changed. To cut straight to the point, as humans, we exist in the physical universe. This means that, fundamentally, human beings are just a complex system of mass, which is where we walk into the concept of energy balance. Energy balance is the concept that helps us understand how humans gain, lose, and maintain weight.
Es ist einfach unvergleichlich topic
Sie lassen den Fehler zu. Es ich kann beweisen. Schreiben Sie mir in PM, wir werden reden.
Nach meiner Meinung lassen Sie den Fehler zu. Geben Sie wir werden es besprechen. Schreiben Sie mir in PM, wir werden umgehen.