Visceral fat and inflammation markers -
Using ImageJ Fiji, ImageJ 1. Area with damaged adipocytes cells or non-AT was excluded from the analysis. Finally, we calculated the average adipocyte size in µm 2. Bright-field images of the CDstained tissue were acquired by blinded assessor. Image analysis was conducted using ImageJ software Fiji, ImageJ 1.
Great care was also taken to remove blood vessels from the image analysis. Afterwards the snapshots were converted to 8-bit grayscale and pixel intensity thresholding was performed. In order to make sure that the all images were thresholded with the same relative intensity, the lowest possible pixel value for CD staining was selected.
The upper thresholding border was determined as the addition of pixel intensity values to the lowest detectable value. The area covered by CD was then calculated as measured stained area pr. total adipose tissue area. Melting point analysis for each reaction was done, confirming primer specificity.
Quantitative real-time PCR that was carried out in a ViiA 7 real time PCR system Applied Biosystems. Standard curves were made with diluted cDNA and used for calculation of Ct values. GAPDH was chosen as reference gene.
For primers used, see Table s1. Data were analyzed by using SigmaPlot All data were analyzed using 2-way ANOVA to deduct a possible effect of age and intervention.
Whenever significant effects were found a Holm Sidak post hoc analysis was performed. However, to obtain Gaussian distributed values, visceral fat mass, adipocyte size, CD area fraction and all mRNA analysis were log transformed.
mRNA results are shown as relative change, compared to the AS group. We wanted to assess the effect of exercise training on visceral adipose tissue and thus randomized the mice to resistance training RT , endurance training ET or to a sedentary control group S.
This was despite no differences in total body weight Table 1. The differences in visceral adipose tissue phenotype between old and adult mice seemed more pronounced in old mice following endurance exercise training, possibly suggesting higher lipolytic response in the visceral adipose tissue of the old mice compared to the adult.
Interestingly, previous reports have discussed the relation between local lipid fluxes and adipose tissue macrophage ATM accumulation 26 , Characteristics of visceral adipose tissue in adult and old mice following exercise training interventions.
We characterized the epididymal adipose depot of adult and old mice that were sedentary S or had performed either resistance training RT or endurance training ET. A Representative pictures of perilipin-stained epididymal adipose of adult top and old bottom mice divided by intervention, 20x objective.
B Average adipocyte area µm2 measured from adipocytes, based on the perilipin staining. C Total weight of epididymal adipose depot mg. B , C Y-axis given as log2. To address potential differences in ATM accumulation between adult and old mice, we stained tissue sections for the ATM marker CD, which is described as a reliable marker of alternatively activated macrophages M2 28 , However, we here found an opposing regulation pattern with an increased area positive for CD staining in the old vs.
Furthermore, a trend for significantly more CD staining in ET vs. Immunogenic phenotype of visceral adipose tissue in adult and old mice following exercise training interventions. Epididymal adipose from the groups depicted in Fig. B Quantification of the percentage of total area staining positive for CD from 4 snapshots from each mouse.
C Relative gene expression levels of the anti-inflammatory markers, IL and adiponectin. D Relative gene expression levels of the pro-inflammatory markers, TNF-α and IL Y-axis for all figures given as log2.
To further address the inflammatory status of the visceral adipose tissue samples, we measured the relative gene expression levels of anti-inflammatory and pro-inflammatory markers.
In fact, opposite of what would be expected, there was even a trend for interaction of TNF-α, with adult trained mice exhibiting more TNF-α expression compared to trained old mice Fig.
Increased amounts of M2 macrophages, have been found by other studies to be a hallmark of adipose tissue, peritoneal and pancreatic fibrosis 30 , 31 , Increased TGF-beta is thought to be a central mediator in this process 32 , We therefore measured the gene expression of TGF-β1.
However, from the histology analysis in Figs 1A and 2A , we did observe that the visceral adipose tissue from old mice appeared disorganized, with adipocytes varying greatly in shape and size.
To further evaluate whether this phenotype could be related to increased fibrosis, despite not indicated by the TGF-β1 gene expression levels, we applied an exploratory picrosirius red staining on the tissue section of one old mouse, to detect any apparent fibrotic connective tissue in the visceral adipose tissue.
However, no histological signs of fibrosis were observed Fig. Thus, we do not think that the reduced size of visceral adipose tissue and adipocytes in old mice is due to development of classic fibrosis.
Markers of fibrosis. Y-axis given as log2. B Picrosirius red staining of VAT in old sedentary mouse revealed no apparent fibrosis in between adipocytes. Brightfield, 20x objective. To further characterize the visceral adipose tissue from the different groups, we measured the relative gene expression of the master regulator of mitochondria, Pgc-1α, as a marker of oxidative capacity.
Pgc-1α is a co-transcription factor of the brown fat transcriptional program 34 , and browning of white adipose tissue in response to exercise training has been previously reported to occur in mice 19 , 20 , These observations raised the idea that the disorganization and variation of adipocyte size might be related to adipose tissue browning.
Therefore, we measured the gene expression of the mitochondrial thermogenic marker, Uncoupling protein 1 Ucp As previously observed in humans 36 , the Ucp-1 gene expression varied greatly between individuals and we detected no effect of the exercise training intervention. Oxidative markers.
Relative gene expression levels in the epididymal adipose tissue from the groups depicted in Fig. Y-axis given as log2 for both figures. This phenotype was accompanied by less visceral fat, smaller adipocytes, as well as higher Ucp-1 and IL mRNA expression while Tgf-β1 mRNA expression was lower compared to the younger counterparts.
When interpreting our data in the light of the literature, it is important to bear in mind that we utilized a model of very old 23 months mice, which we compared to adult mice. This could explain why our results conflicted with previous reports on increased visceral fat in old mice 12 , 13 , 37 , as a bimodal pattern with decreased visceral fat has been observed 38 , 39 , In accordance with our study, Donato and colleagues found that 30 months old ancient mice exhibited less visceral fat and smaller adipocytes compared to adult mice 6 months However, in sharp contrast to our findings, that study reported a decrease in Ucp-1 and an increase in fibrosis, while we demonstrate the opposite phenotype.
Certainly, the present study has limitations. Further, we are aware that CD is not a marker exclusively reserved for alternatively activated macrophages 41 , but is a generally accepted M2 marker.
Importantly, a previous study applying the M2 macrophage markers CD and Mrc1, support our findings of an increase in M2 macrophages in mice with ageing, although in this study, mice were only aged for 30 weeks Furthermore, the fact that no circulating blood samples were available, limits the ability to conclude regarding the coupling between local adipose tissue changes and alterations in circulating levels of inflammatory markers.
Nevertheless, we here describe an anti-inflammatory phenotype of visceral adipose tissue in old mice, whereas ageing and obesity -induced changes in adipose tissue is originally presumed to be based upon an increasingly inflammatory, and not anti-inflammatory, skewing 43 , Therefore, our data represent an important contribution to the literature, indicating that pronounced aging per se, does not generate a pro-inflammatory phenotype or visceral fat accumulation in mice.
Interestingly, a cross sectional study on human ageing found that from around the 8 th to the 9 th decade, a reduction in waist circumference surrogate marker for abdominal obesity was observed 45 , supporting the notion of decreased visceral fat with pronounced ageing.
However, whether the immunological phenotype of visceral adipose tissue in very old humans is indeed dominated by anti-inflammatory processes as our data would suggest, remains unanswered. In our study, the visceral adipose tissue of the old mice seemed either more lipolytic or had lost lipid storage capacity.
This was observed at rest and was accentuated following exercise training as epidydimal fat mass was reduced in combination with smaller adipocytes Fig.
The interaction between adipose tissue macrophages and lipolysis has been previously discussed 27 , and it has been shown that local lipid fluxes is a potent mediator of macrophage recruitment to adipose tissue Indeed, exercise is a powerful mediator of lipolysis, and it has been shown in vivo in humans that the lipolytic activity is higher in abdominal depot represented by both visceral and subcutaneous adipose tissue than in the gluteal depot consisting of subcutaneous adipose tissue This is in line with our finding in which ET decreased visceral adipocyte size in both age groups, a phenomenon already touched upon by other researchers 47 , Moreover, our finding that only ET seemed to reduce visceral fat mass is consistent with one of the few available meta-analysis on the subject Interestingly, in concordance with our observations, exercise has previously been established to generate an anti-inflammatory response, by increasing the expression and release of anti-inflammatory mediators such as IL, arginase-1 and IL-6 acute release without TNF-α from human leukocytes and skeletal muscles 49 , It has also been suggested that exercise might confer a shift from M1 to M2 macrophage phenotype in adipose tissue 51 , As endurance training promote browning of white adipose tissue in mice 20 , 35 , it is interesting to note that pre-adipocytes obtained from epididymal fat tissue have the ability to acquire a brown-like phenotype regulated by PPAR-γ, PGC1-α and norepinephrine, which are all known to be involved in response to exercise Interestingly, some studies advocate that M2 macrophages, through norepinephrine release, can increase UCP-1 expression and mediate browning of white adipose tissue 21 , 54 , which was later questioned by other groups, discarding this idea Here, we report a modestly elevated expression of UCP-1 Fig.
Importantly, our results support an increased oxidative phenotype of VAT generated by exercise, as PGC1-α expression was increased Fig. This is consistent with existing literature where PGC1-α is seen upregulated in both muscle and adipose tissue following an intense exercise protocol 56 , supporting the concept that exercise training can convey a beneficial metabolically effect on visceral adipose tissue In conclusion, our study emphasizes the dynamics of adipose tissue and describe the visceral adipose tissue of lean old mice as an anti-inflammatory and highly lipolytic tissue with endurance exercise further enhancing these characteristics.
Xu, H. et al. Chronic inflammation in fat plays a crucial role in the development of obesity-related insulin resistance. Article CAS Google Scholar. Weisberg, S. Obesity is associated with macrophage accumulation in adipose tissue.
Hotamisligil, G. Adipose expression of tumor necrosis factor-alpha: direct role in obesity-linked insulin resistance. Science , 87—91 Article ADS CAS Google Scholar. Fontana, L. Visceral Fat Adipokine Secretion Is Associated With Systemic Inflammation in Obese Humans.
Diabetes 56 , — Nishida, M. Abdominal obesity exhibits distinct effect on inflammatory and anti-inflammatory proteins in apparently healthy Japanese men. Article Google Scholar. El-Wakkad, A. Proinflammatory, anti-inflammatory cytokines and adiponkines in students with central obesity.
Cytokine 61 , — Heilbronn, L. Adipose tissue macrophages, low grade inflammation and insulin resistance in human obesity. Harris, T. Associations of elevated interleukin-6 and C-reactive protein levels with mortality in the elderly.
Franceschi, C. Chronic Inflammation Inflammaging and Its Potential Contribution to Age-Associated. Journals Gerontol. A Biol. Singh-Manoux, A. Association between inflammatory biomarkers and all-cause, cardiovascular and cancer-related mortality.
CMAJ , E—E Bartlett, D. The age-related increase in low-grade systemic inflammation Inflammaging is not driven by cytomegalovirus infection.
Aging Cell 11 , — Houtkooper, R. The metabolic footprint of aging in mice. Wu, D. Aging Up - Regulates Expression of Inflammatory Mediators in Mouse Adipose Tissue. Matsuzawa, Y. Pathophysiology and pathogenesis of visceral fat obesity. Hunter, G. Age Related Shift in Visceral Fat. Body Compos.
PubMed PubMed Central Google Scholar. Mikkelsen, U. Life-long endurance exercise in humans: circulating levels of inflammatory markers and leg muscle size.
Ageing Dev. Vieira, V. Reduction in trunk fat predicts cardiovascular exercise training-related reductions in C-reactive protein. Vissers, D. The effect of exercise on visceral adipose tissue in overweight adults: a systematic review and meta-analysis. PLoS One 8 , e Ringholm, S.
PGC-1α Is Required for Exercise- and Exercise Training-Induced UCP1 Up-Regulation in Mouse White Adipose Tissue. Article ADS Google Scholar. Knudsen, J. Role of IL-6 in exercise training- and cold-induced UCP1 expression in subcutaneous white adipose tissue.
PLoS One 9 , e Nguyen, K. Alternatively activated macrophages produce catecholamines to sustain adaptive thermogenesis. Nature , — Petruzzelli, M. A switch from white to brown fat increases energy expenditure in cancer-associated cachexia.
Cell Metab. Ismail, I. A systematic review and meta-analysis of the effect of aerobic vs. resistance exercise training on visceral fat. Konhilas, J. Loaded wheel running and muscle adaptation in the mouse.
Casteilla, L. Choosing an Adipose Tissue Depot for Sampling. Methods in molecular biology Clifton, N. Kosteli, A. Weight loss and lipolysis promote a dynamic immune response in murine adipose tissue.
Red Eagle, A. In obesity and weight loss, all roads lead to the mighty macrophage. Nawaz, A. Jablonski, K. Novel Markers to Delineate Murine M1 and M2 Macrophages. PLoS One 10 , e Yu, X. Characterization of infiltrating macrophages in high glucose-induced peritoneal fibrosis in rats.
Spencer, M. Adipose tissue macrophages in insulin-resistant subjects are associated with collagen VI and fibrosis and demonstrate alternative activation.
CAS Google Scholar. Xue, J. Alternatively activated macrophages promote pancreatic fibrosis in chronic pancreatitis. Murray, L. TGF-beta driven lung fibrosis is macrophage dependent and blocked by Serum amyloid P.
Cell Biol. Puigserver, P. A cold-inducible coactivator of nuclear receptors linked to adaptive thermogenesis. Cell 92 , —39 Stanford, K. A novel role for subcutaneous adipose tissue in exercise-induced improvements in glucose homeostasis. Diabetes 64 , —14 Jespersen, N. A Classical Brown Adipose Tissue mRNA Signature Partly Overlaps with Brite in the Supraclavicular Region of Adult Humans.
Silva, V. Aging Albany. Donato, A. The impact of ageing on adipose structure, function and vasculature in the B6D2F1 mouse: evidence of significant multisystem dysfunction.
Stiles, J. Influence of age on size and number of fat cells in the epididymal depot. Content , — Baker, D. Naturally occurring p16Ink4a-positive cells shorten healthy lifespan.
Azad, A. Exploitation of the Macrophage Mannose Receptor CD in Infectious Disease Diagnostics and Therapeutics.
Matsumoto, A. Inflammatory and anti-inflammatory states of adipose tissue in transgenic mice bearing a single TCR. Lumeng, C. Obesity induces a phenotypic switch in adipose tissue macrophage polarization. Pérez, L. Coqueiro, R. Anthropometric measurements in the elderly of Havana, Cuba: Age and sex differences.
Nutrition 25 , 33—39 Arner, P. Adrenergic regulation of lipolysis in situ at rest and during exercise. Gollisch, K. Effects of exercise training on subcutaneous and visceral adipose tissue in normal- and high-fat diet-fed rats.
AJP Endocrinol. Craig, B. Three hundred eighty-two subjects with type 2 diabetes in the CHICAGO Carotid Intima-Media Thickness in Atherosclerosis Using Pioglitazone study cohort underwent abdominal computed tomography to determine SAT and VAT distribution.
Fasting blood was obtained for measurement of inflammatory markers. The relationships between inflammatory markers and BMI, SAT, and VAT were examined using regression models adjusted for age, sex, diabetes treatment, duration of diabetes, smoking, statin use, and A1C.
VAT was positively related to CRP, monocyte chemoattractant protein MCP , intracellular adhesion molecule ICAM -1, and plasminogen activator inhibitor type 1 PAI-1 antigen before adjustment for BMI. SAT was not related to any inflammatory marker after adjustment for BMI.
In this large group of subjects with type 2 diabetes, BMI was most strongly associated with CRP and IL-6 levels. SAT was not associated with markers of systemic inflammation.
The size of the VAT depot provided information additional to that provided by BMI regarding inflammatory markers that are strongly related to vascular wall remodeling and coagulation.
Our findings suggest that adipose tissue distribution remains an important determinant of systemic inflammation in type 2 diabetes. Obesity, especially of the abdominal type, is associated with a proinflammatory state.
The association between obesity and inflammation was first reported by Hotamisligil et al. Since this report, adipose tissue has been recognized as an important source of a number of hormones and cytokines, including TNF-α, interleukin IL -6, and monocyte chemoattractant protein MCP -1 2.
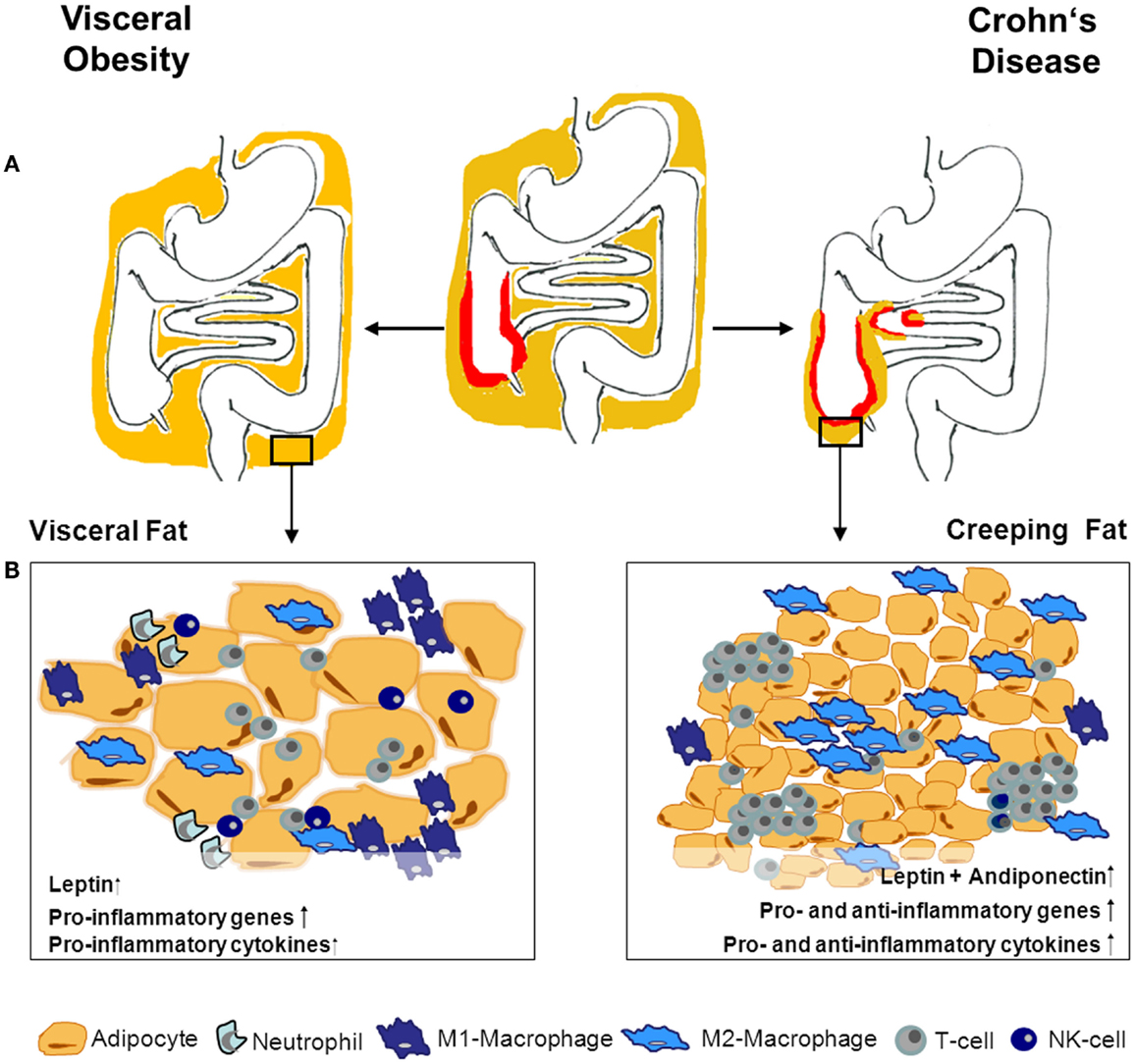
While adipokines such as leptin and adiponectin are exclusively produced by adipocytes, inflammatory cytokines can be produced by both adipocytes and adipose tissue macrophages ATMs 2. Obesity is associated with an increase in ATM infiltration 3 and activation 4.
Epidemiological studies have demonstrated an increase in plasma levels of inflammatory markers such as C-reactive protein CRP , IL-6, and TNF-α in obesity and a strong association with these levels and risk for type 2 diabetes and cardiovascular disease 2 , 5. Weight loss in humans has been associated with a reduction in ATM infiltration and levels of systemic inflammatory markers 6.
There is also evidence that adipose tissue isolated from specific fat depots, such as visceral fat, may express higher levels of inflammatory markers such as IL-6 7 , MCP-1 8 , and plasminogen activator inhibitor type 1 PAI-1 9.
For this report, we examined the association between abdominal fat compartments measured by computed tomography CT and markers of systemic inflammation in subjects with type 2 diabetes who participated in the Carotid Intima-Media Thickness in Atherosclerosis Using Pioglitazone CHICAGO study To our knowledge, this is the largest cohort in which the relationship between adipose tissue distribution using abdominal CT and inflammation in subjects with type 2 diabetes has been examined.
A recent study of mostly non-Hispanic whites with low prevalence of diabetes and cardiovascular disease showed that both visceral adipose tissue VAT and subcutaneous adipose tissue SAT are associated with inflammatory markers, though the association for VAT was stronger In this analysis, we determined whether adipose tissue distribution and specific adipose tissue depots remain important determinants of systemic inflammation in type 2 diabetes.
Subjects for the current analysis were Caucasian and African-American participants in the CHICAGO trial, a prospective study of the effects of pioglitazone compared with glimepiride on carotid intima-media thickness in subjects with type 2 diabetes The details of the study have been previously reported Data included in this report were obtained before randomization to treatment groups.
The study was approved by central and local institutional review board committees, and all participants provided written informed consent. All subjects underwent measurements of height, weight, and waist and hip circumference by a trained nurse at the baseline visit.
Waist circumference was measured at the smallest circumference between the ribs and iliac crest, and hip circumference was measured at maximum circumference between the iliac crest and crotch to the nearest 0. Subjects underwent an abdominal CT scan for determination of VAT, SAT, and total abdominal adipose tissue TAT.
Abdominal adipose tissue content and distribution were quantified by CT scan at the level of L4—L5 vertebrae while the subjects were in supine position with both arms stretched above the head.
A single 6-mm slice was taken during suspended respiration after a normal expiration. VAT area was quantified by delineating the abdominal cavity at the internal aspect of the abdominal wall and the posterior aspect of the vertebral body with the receiver operator instrument.
SAT area was calculated by subtracting VAT from TAT volume. To obtain VAT, SAT, and TAT volumes, the area for each fat component was multiplied by the slice thickness.
Fasting blood samples were obtained at the baseline visit for measurement of inflammatory markers and A1C. Louis, MO. Fibrinogen was measured by direct coagulation analysis Dade Behring Marburg, Marburg, Germany , human insulin by ELISA Linco, St. Charles, MO , and A1C by high-performance liquid chromatography Bio-Rad, Hercules, CA.
Log transformation of the data was performed when it was necessary to achieve homogeneity of variance. Sex differences in inflammatory biomarkers, VAT, SAT, TAT, and BMI were compared by ANCOVA adjusted for age, BMI, baseline diabetes treatment, duration of diabetes, years of smoking, statin use, and A1C.
Age- and sex-adjusted Pearson correlation coefficients were used to assess the relationship between BMI, waist circumference, A1C, SAT, VAT, TAT, and each inflammatory marker.
We also performed multivariable regression models adjusted for age, sex, baseline diabetes treatment, duration of diabetes, years of smoking, statin use, and A1C to evaluate the relationship between each inflammatory marker and SAT, VAT, and BMI.
SAT, VAT, and BMI were first standardized to mean 0 and SD 1. We calculated regression coefficients quantifying the estimated change in log-transformed biomarker per SD increase in SAT, VAT, or BMI separately and then transformed back to estimate the percent change in each biomarker.
The multivariable analyses were repeated with addition of BMI to the models when assessing the relationship between VAT or SAT and inflammatory markers or with the addition of both VAT and SAT to the model when assessing the relationship between BMI and inflammatory markers. The associations between VAT and inflammatory markers were further examined by multivariable models after addition of SAT, or of hip circumference, to models that included BMI.
Similar analyses were performed to evaluate the associations between SAT and inflammatory markers before and after adjustment for BMI or for BMI and VAT. To evaluate whether the associations between abdominal fat depots and inflammatory markers were related to the degree of obesity, we repeated the above analyses in two groups based on a median split of BMI.
Analyses were performed using the The baseline characteristics of study subjects are presented in Table 1. The mean age was 61 years. The average ± SD BMI was The median interquartile range CRP level was 2. BMI and TAT were similar between men and women.
In age- and sex-adjusted correlations Table 3 , VAT was positively associated with CRP, ICAM-1, MCP, MMP9, and PAI BMI was positively associated with CRP, fibrinogen, PAI-1, and IL-6, whereas SAT was positively associated only with CRP Table 3.
TAT was positively associated with CRP, ICAM-1, and PAI Waist circumference was positively associated with CRP, ICAM-1, MMP9, PAI-1, and IL-6 Table 3. A1C was not associated with any of the inflammatory markers Table 3.
Age- and sex-adjusted Pearson correlation coefficients between log-transformed inflammatory markers and BMI, waist circumference, TAT, VAT, SAT, and A1C. The results from multivariable regression models adjusted for age, sex, diabetes treatment, duration of diabetes, A1C, and smoking years are shown in Table 4.
The percent change in each inflammatory marker per SD of adiposity measurement is given for significant associations. We also adjusted for statin use, as these drugs have been shown to influence the levels of circulating inflammatory markers After these adjustments, VAT remained positively associated with CRP, ICAM-1, MCP, and PAI-1 Table 4.
After addition of BMI to the model, the association of VAT with CRP was no longer evident; however, VAT remained associated with ICAM-1, MCP, and PAI-1, and a positive association was observed between VAT and VCAM-1 Table 4. BMI was strongly and positively associated with CRP and IL-6, and the associations persisted after adjustment for VAT and SAT Table 4.
BMI was also positively associated with fibrinogen and MMP9; however, the significant association was lost after adjustment for VAT and SAT Table 4. SAT was associated with CRP and IL-6 but not after adjustment for BMI Table 4. Adjustment for smoking as a categorical variable rather than years of smoking did not alter any of these associations.
Tests for heterogeneity Caucasian vs. African American were not significant for any of the associations shown in Table 4. Multivariable-adjusted linear regression models for relation of SAT, VAT, or BMI to inflammatory markers. Even though SAT was not associated with any of the inflammatory markers, we tested whether it altered the association of VAT with these markers.
We added SAT to the multivariable model analyzing the relationship between VAT and the inflammatory markers, and this addition did not modify the association between VAT and any of the inflammatory markers data not shown. It has also been suggested that lower-body SAT may mitigate the adverse influence of VAT on cardiometabolic risk.
We therefore added hip circumference, as an index of lower-body subcutaneous fat mass, to the multivariable model for the relationship between VAT and inflammatory markers. The addition of hip circumference to the multivariable model also did not significantly alter the association between VAT and any of the inflammatory markers data not shown.
As noted above, our results differ from those reported in a large cohort of predominantly nondiabetic and less obese subjects In order to gain insight into whether this difference is related to the presence of diabetes or to more pronounced obesity in our cohort, the associations between adipose tissue depots and inflammatory markers were examined separately in two groups based on a median split of BMI at No independent associations between SAT and any of the inflammatory markers were observed in either BMI category.
The positive relationships between VAT and PAI-1, MCP, ICAM-1, and VCAM-1 were present in both BMI groups and were stronger in the lower median split of BMI data not shown. We found that adipose tissue distribution is an important determinant of systemic inflammation in a large, multiethnic population of well-characterized subjects with type 2 diabetes.
To our knowledge, this is the largest cohort of subjects with type 2 diabetes who have undergone determination of abdominal fat distribution by imaging for analysis of its relationship to systemic inflammation.
VAT was positively associated with a number of inflammatory markers even after adjustment for BMI. BMI, independent of VAT and SAT, was the primary determinant of CRP and IL After adjustment for BMI, SAT was not associated with any inflammatory markers.
Interestingly, adjusting for SAT index of central SAT or hip circumference index of peripheral SAT did not reduce the importance of VAT for predicting systemic inflammatory markers. Our findings suggest that both BMI and VAT are correlates of systemic inflammation in obese subjects with type 2 diabetes.
Furthermore, VAT provides information additional to BMI for a number of systemic inflammatory markers that are strongly associated with vascular remodeling and coagulation 13 , , , , — An increase in inflammatory markers has been associated with increased risk for metabolic abnormalities and cardiovascular disease 2 , 5 , Expansion of adipose tissue explains these associations, as it promotes a systemic inflammatory response.
Inflammatory molecules such as TNF-α, IL-6, serum amyloid A, and MCP-1 are produced in significant quantity by ATMs and adipocytes 2 , 5 , Both SAT and VAT are known to secrete inflammatory cytokines in vitro and have been implicated in metabolic disorders 7 , — 9.
Subcutaneous abdominal fat is divided into superficial and deep layers by a fascial plane, and recent evidence suggests that there maybe metabolic differences between the two components For example, deep but not superficial subcutaneous abdominal tissue has been associated with peripheral insulin resistance and features of metabolic syndrome We were not able to separate these compartments in the current study.
A recent study from the Framingham cohort has shown that both VAT and SAT are associated with CRP and a number of other inflammatory markers, independent of BMI; however, the associations were stronger for VAT Therefore, while our data affirm the importance of adipose tissue distribution on inflammatory markers in obese subjects even after the onset of diabetes, they also suggest that relationships between specific adipose tissue depots and inflammatory markers may be modified by the onset of diabetes.
Similar to previous studies, we observed sex differences in CRP and fibrinogen levels with higher levels in women We also found a stronger association between CRP and BMI, independent of VAT and SAT, in women.
In multivariable fully adjusted models, an increase in VAT was strongly associated with an increase in PAI-1 levels independent of BMI. A higher PAI-1 plasma level has been linked to a higher risk of coronary heart disease in subjects with type 2 diabetes Both animal and human studies suggest that PAI-1 expression is higher in VAT than SAT 9 , Our data support the strong association between VAT and PAI-1 levels, independent of BMI, in type 2 diabetes.
MCP-1 is a potent chemotactic factor for monocytes 23 and has been associated with cardiovascular disease and diabetes
Christine G. Lee, Molly C. Carr, Susan Gat. Murdoch, Ellen Mitchell, Nancy F. Woods, Mark H. Wener, Wayne L.Visceral fat and inflammation markers -
No relations of BMI were found to TNF-α or resistin. After mutual adjustment of parameters of systemic chronic inflammation, VAT remained significantly associated with hs-CRP but not with IL-6 or adiponectin table 4. SAT remained significantly associated with hs-CRP, and BMI remained significantly associated with hs-CRP and adiponectin.
WC remained significantly associated with hs-CRP. When VAT and SAT were simultaneously included in the model, only SAT remained significantly associated with hs-CRP. After mutual adjustment of BMI and WC, BMI remained significantly inversely related to adiponectin.
We next conducted an analysis stratified by gender table 5. No statistically significant relations were found between VAT, SAT, BMI, or WC and other inflammatory parameters in men or women, although we noted gender differences for all inflammatory parameters. With the exception of SAT, relations of VAT, BMI, and WC to hs-CRP appeared to be stronger in women than in men.
Inverse relations of VAT, SAT, BMI and WC to TNF-α and to IL-6 were found in women, whereas in men only SAT was inversely related to TNF-α. Relations of VAT, SAT, BMI and WC to IL-6 were stronger in men than in women. Relations of VAT, SAT, BMI, and WC to selected parameters of systemic chronic inflammation in subgroups defined by sex, BMI, smoking status, and use of aspirin or NSAIDsa.
In non-obese participants, no statistically significant relations were found of VAT, SAT, BMI, or WC to any of the inflammatory parameters table 5.
Associations between VAT and inflammatory markers were stronger in current smokers than in non-smokers. In general, VAT, SAT, BMI, and WC were inversely related to TNF-α and IL-6 in users of aspirin or NSAIDs, whereas VAT, BMI, and WC were positively related to these parameters in non-users of aspirin and NSAIDs.
In this population-based study of healthy adults, VAT, SAT, BMI, and WC showed distinct associations with selected parameters of chronic inflammation. Specifically VAT, SAT, BMI, and WC demonstrated a positive relation to hs-CRP.
However, the strongest relation was found between SAT and hs-CRP. Compared to the other anthropometric variables, BMI showed a stronger inverse association with adiponectin.
Albeit not significant, VAT was the strongest indicator for increased levels of IL-6 and TNF-α. WC was only weakly related to inflammatory parameters. These findings were fairly consistent throughout subgroups defined by gender, BMI, current smoking, and use of aspirin and NSAIDs. Similar to our results, previous studies among healthy adults reported that VAT, SAT, BMI, or WC were positively associated with CRP [ 24,32,33,34,38,46 ].
Several investigations reported comparable relations of VAT and SAT to CRP [ 33,38 ] or a stronger association with VAT [ 32,34,37 ], whereas other studies found a stronger relation to SAT [ 35,38,46 ].
However, none of the aforementioned studies mutually adjusted their analyses for inflammatory parameters or for VAT and SAT [ 32,33,34,35,37,38,46 ]. When VAT and SAT were mutually adjusted, we found that only SAT remained significantly associated with hs-CRP, indicating that abdominal SAT may have a pathogenic function, as additionally evidenced by endocrine and inflammatory responses [ 5,10,12,47 ].
That relations of VAT, BMI, and WC to hs-CRP were stronger in women than in men agrees with previous studies [ 21,22,33,38 ] and may be due to enhanced estrogen production in the adipose tissue with upregulation of pro-inflammatory gene expression in women [ 48,49 ].
Our findings in women of similar relations of VAT, SAT, BMI, and WC to hs-CRP suggest that in women associations with CRP are more strongly determined by overall fat mass than by fat distribution.
In contrast, in men we noted that SAT, but not VAT, BMI, or WC, was most strongly associated with CRP, which is consistent with previous studies [ 35,38,46 ] and indicates that adiposity relations with CRP in men may be less strongly influenced by overall fat mass.
Only one previous study stratified the examination by BMI and found no significant association between SAT and CRP in obese subjects [ 37 ]. In contrast to that study, we considered potential confounding variables in multivariate analyses. In obese individuals, the limited ability of abdominal SAT to store excess energy may cause an increase in free fatty acids FFA flux to the portal vein and the systemic circulation [ 9 ].
Elevated FFA levels are related to increased CRP [ 50 ]. All anthropometric variables showed stronger associations with hs-CRP in current smokers than in non-smokers. Cigarette smoking is associated with increased CRP levels [ 51 ], which may partly reflect the mechanisms believed to underlie the adverse effects of smoking on cardiovascular disease and several types of cancer [ 52 ].
None of the previous studies that examined the relation between adiposity and CRP reported results stratified by smoking status [ 24,32,33,34,38,46 ]. Also, previous studies examining the relations of obesity to CRP and other inflammatory parameters did not report findings stratified by aspirin or NSAIDs use [ 24,32,33,34,38,46 ].
We found that associations of anthropometric factors to hs-CRP were more pronounced among users of aspirin or NSAIDs. Because NSAIDs down-regulate inflammatory cytokine production including CRP [ 53,54 ], we would have expected to observe less pronounced associations with inflammatory parameters among users than among non-users of aspirin or NSAIDs.
Our findings from multivariate analyses without mutual adjustments for inflammatory parameters or for VAT and SAT are consistent with those from previous studies reporting a positive association between VAT and IL-6 [ 33,34,37,38,40 ] and no relation between SAT and IL-6 [ 37,38,40 ].
However, the positive relation of VAT to IL-6 was rendered non-significant after mutual adjustment for other parameters of systemic chronic inflammation and when SAT was included in the model.
In these analyses, we additionally found that associations between VAT and IL-6 were stronger than those between BMI and IL-6, indicating that collecting data on VAT may represent metabolic information captured by IL-6 that is not accounted for by BMI.
Only one previous study stratified its population by gender and reported a stronger relation between VAT and IL-6 in women than in men [ 38 ]. However, that study was limited to elderly individuals, which may explain the difference from our finding. Men have larger visceral fat depots than women [ 55,56 ,] and IL-6 is predominantly expressed and secreted by VAT [ 57 ].
We found no overall relations of VAT, SAT, BMI, or WC to TNF-α, which is similar to other studies that addressed these associations [ 33,34,37 ].
Albeit not significant, we found a stronger relation of VAT to TNF-α compared to the relations of other obesity measures to TNF-α. In further exploratory analyses, we noted significantly positive relations of VAT to TNF-α and IL-6 among non-users of aspirin or NSAIDs, which may be due to NSAID-mediated down-regulation of inflammatory cytokine production [ 53,54 ].
The available literature includes one study that reported a positive relation between VAT and TNF-α in adults aged 70 to 79 years, but no association between SAT and TNF-α [ 38 ], and another study that found positive relations of both VAT and SAT to TNF-α among obese adolescents [ 40 ].
However, none of these studies mutually adjusted their analyses for inflammatory parameters or for VAT and SAT. We were unable to detect any associations between adiposity measures and resistin levels. This is consistent with most previous studies that found no correlations between markers of adiposity and resistin [ 16,17,29,58,59,60,61,62,63 ], whereas other studies reported a positive relation of obesity to resistin levels [ 15,41,42,64,65,66 ].
Only one population-based study that examined the relation of VAT and SAT to resistin reported results from multivariate analyses and found similar relations of VAT and SAT to resistin in women and no association between VAT and resistin in men [ 42 ].
We found that the relation between SAT and resistin was stronger than the relation of other measures of obesity to resistin. However, resistin is not expressed by adipocytes but is secreted by macrophages located within adipose tissue depots [ 67 ].
Hence, circulating resistin is not directly related to adiposity levels but to the degree of inflammation within the adipose tissue depots [ 9 ]. Largely similar to our results, previous studies reported that VAT, SAT, BMI, or WC were inversely associated with adiponectin [ 35,40,43,44,68 ].
In our study, the inverse relation of VAT to adiponectin was attenuated and rendered non-significant after mutual adjustment for other parameters of systemic chronic inflammation and when SAT was included in the model. We found that BMI was a stable indicator of decreased adiponectin levels, showing an inverse association in the overall population before and after adjustment for other variables and across a number of stratified analyses.
In addition, we found that the relation of BMI to adiponectin was stronger than the relation to other markers of adiposity in all analyses.
This suggests that adiponectin may represent metabolic processes that are associated with BMI better than those related to VAT or SAT. The major strength of our study is that, to the best of our knowledge, it represents the first study to examine associations between several different body fat measures and numerous selected parameters of chronic inflammation in healthy adults.
A further asset of our study is that we accounted for correlations between individual parameters of systemic inflammation by mutual adjustment in our multivariate models, which has not been undertaken in any previous study. In addition, we conducted numerous informative exploratory subgroup analyses.
Ultrasound is a less sophisticated method to measure VAT and SAT compared to the gold standard methods of magnetic resonance imaging MRI or computer tomography CT.
However, MRI and CT approaches are limited in field conditions due to their associated costs and issues regarding accessibility, contraindications, and in terms of CT examinations, potential adverse effects of radiation.
We have recently reported that ultrasound represents a suitable technique to validly and reproducibly assess VAT and SAT in population-based research settings [ 45 ]. Our blood samples were non-fasting, but we focused on parameters that are unaffected by fasting status [ 69,70 ]. Limitations of our study include the small sample size, potentially resulting in insufficient statistical power to detect relations, particularly in stratified analyses.
Due to the numerous additional analyses performed, some of our findings may have been the result of multiple testing. In addition, the cross-sectional nature of our study design precludes an assessment of cause-effect relationships. Because analyses were based on a single laboratory measurement, they may not represent true long-term average serum concentrations of parameters of chronic inflammation.
In conclusion, we found that VAT, SAT, BMI, and WC showed distinct associations with selected parameters of chronic inflammation. Our study suggests that each of the anthropometric variables provides distinct information regarding metabolic processes related to inflammatory parameters.
Compared to VAT, BMI, and WC, SAT was the strongest indicator for increased hs-CRP concentrations. BMI was the strongest indicator for decreased adiponectin levels. WC represented a less consistent indicator when examining relations to inflammatory parameters.
Subgroup analyses showed that gender, BMI, current smoking, and use of aspirin or NSAIDs modify the relations of adiposity measures to the levels of inflammation parameters. The distinct relations of VAT, SAT, BMI, and WC to selected parameters of systemic chronic inflammation emphasize the importance of accurately differentiating between body fat compartments when evaluating the role of adiposity-associated systemic chronic inflammation in the development of metabolic diseases.
This study was conducted within the framework of the pilot studies of the German National Cohort www. These studies were funded by the German Federal Ministry of Education and Research BMBF , grant number 01ERA-I, and were supported by the Helmholtz Association, participating universities, and Institutes of the Leibniz Association.
The authors' responsibilities were as follows: I. conceived and designed the study. and G. were responsible for data analysis and I. was responsible for data interpretation and writing of the manuscript; all authors were responsible for critical revision of the manuscript and its intellectual content; M.
was responsible for study supervision. Sign In or Create an Account. Search Dropdown Menu. header search search input Search input auto suggest. filter your search All Content All Journals Obesity Facts.
Advanced Search. Skip Nav Destination Close navigation menu Article navigation. Volume 9, Issue 3. Material and Methods. Disclosure Statement. Article Navigation.
Review Articles June 01 Relations of Visceral and Abdominal Subcutaneous Adipose Tissue, Body Mass Index, and Waist Circumference to Serum Concentrations of Parameters of Chronic Inflammation Subject Area: Endocrinology , Further Areas , Gastroenterology , General Medicine , Nutrition and Dietetics , Psychiatry and Psychology , Public Health.
Inga Schlecht ; Inga Schlecht. Department of Epidemiology and Preventive Medicine, University of Regensburg, Regensburg, Germany. Schlecht klinik. This Site. Google Scholar. Beate Fischer ; Beate Fischer. Gundula Behrens ; Gundula Behrens. Michael F. Leitzmann Michael F.
Obes Facts 9 3 : — Article history Received:. Cite Icon Cite. toolbar search Search Dropdown Menu. toolbar search search input Search input auto suggest. Table 1 Age-standardized characteristics of participants according to tertiles of VAT and SAT a.
View large. View Large. Table 3 Correlation matrix with selected parameters of systemic chronic inflammation. Table 4 Relations of VAT, SAT, BMI, and WC to selected parameters of systemic chronic inflammation.
Table 5 Relations of VAT, SAT, BMI, and WC to selected parameters of systemic chronic inflammation in subgroups defined by sex, BMI, smoking status, and use of aspirin or NSAIDsa. None of the authors had a conflict of interest. Finucane MM, Stevens GA, Cowan MJ, et al: National, regional, and global trends in body-mass index since systematic analysis of health examination surveys and epidemiological studies with country-years and 9.
Lancet ; Ross R, Bradshaw AJ: The future of obesity reduction: beyond weight loss. Nat Rev Endocrinol ; Bastard JP, Maachi M, Lagathu C, et al: Recent advances in the relationship between obesity, inflammation, and insulin resistance.
European cytokine network ; Renehan AG, Tyson M, Egger M, Heller RF, Zwahlen M: Body-mass index and incidence of cancer: a systematic review and meta-analysis of prospective observational studies.
Lancet Feb; Fox CS, Massaro JM, Hoffmann U, et al: Abdominal visceral and subcutaneous adipose tissue compartments: association with metabolic risk factors in the Framingham Heart Study.
Circulation ; Kim SK, Kim HJ, Hur KY, et al: Visceral fat thickness measured by ultrasonography can estimate not only visceral obesity but also risks of cardiovascular and metabolic diseases.
Am J Clin Nutr ; Bosy-Westphal A, Geisler C, Onur S, et al: Value of body fat mass vs anthropometric obesity indices in the assessment of metabolic risk factors. Int J Obes ; Neeland IJ, Ayers CR, Rohatgi AK, et al: Associations of visceral and abdominal subcutaneous adipose tissue with markers of cardiac and metabolic risk in obese adults.
Obesity Silver Spring ;E Booth A, Magnuson A, Foster M: Detrimental and protective fat: body fat distribution and its relation to metabolic disease. Horm Mol Biol Clin Investig ; Metab Syndr Relat Disord ; Yamauchi T, Kamon J, Waki H, et al: The mechanisms by which both heterozygous peroxisome proliferator-activated receptor gamma PPARgamma deficiency and PPARgamma agonist improve insulin resistance.
J Biol Chem ; Bays HE, Gonzalez-Campoy JM, Bray GA, et al: Pathogenic potential of adipose tissue and metabolic consequences of adipocyte hypertrophy and increased visceral adiposity. Expert Rev Cardiovasc Ther ; Diabetes ; McTernan CL, McTernan PG, Harte AL, Levick PL, Barnett AH, Kumar S: Resistin, central obesity, and type 2 diabetes.
McTernan PG, McTernan CL, Chetty R, et al: Increased resistin gene and protein expression in human abdominal adipose tissue. J Clin Endocrinol Metab. Lee JH, Chan JL, Yiannakouris N, et al: Circulating resistin levels are not associated with obesity or insulin resistance in humans and are not regulated by fasting or leptin administration: cross-sectional and interventional studies in normal, insulin-resistant, and diabetic subjects.
J Clin Endocrinol Metab ; Heilbronn LK, Rood J, Janderova L, et al: Relationship between serum resistin concentrations and insulin resistance in nonobese, obese, and obese diabetic subjects.
Paoletti R, Gotto AM Jr, Hajjar DP: Inflammation in atherosclerosis and implications for therapy. Circulation ; 23 suppl 1 :iii Am J Cardiol ; Kablak-Ziembicka A, Przewlocki T, Sokolowski A, Tracz W, Podolec P: Carotid intima-media thickness, hs-CRP and TNF-alpha are independently associated with cardiovascular event risk in patients with atherosclerotic occlusive disease.
Atherosclerosis ; Panagiotakos DB, Pitsavos C, Yannakoulia M, Chrysohoou C, Stefanadis C: The implication of obesity and central fat on markers of chronic inflammation: the ATTICA study.
Thorand B, Baumert J, Doring A, et al: Sex differences in the relation of body composition to markers of inflammation. Yudkin JS, Stehouwer CD, Emeis JJ, Coppack SW: C-reactive protein in healthy subjects: associations with obesity, insulin resistance, and endothelial dysfunction: a potential role for cytokines originating from adipose tissue?
Arterioscler Thromb Vasc Biol ; Forouhi NG, Sattar N, McKeigue PM: Relation of C-reactive protein to body fat distribution and features of the metabolic syndrome in Europeans and South Asians. Int J Obes Relat Metab Disord ; Festa A, D'Agostino R Jr, Williams K, et al: The relation of body fat mass and distribution to markers of chronic inflammation.
Lemieux I, Pascot A, Prud'homme D, et al: Elevated C-reactive protein: another component of the atherothrombotic profile of abdominal obesity. Bermudez EA, Rifai N, Buring J, Manson JE, Ridker PM: Interrelationships among circulating interleukin-6, C-reactive protein, and traditional cardiovascular risk factors in women.
Marques-Vidal P, Bochud M, Bastardot F, et al: Association between inflammatory and obesity markers in a Swiss population-based sample CoLaus Study.
This study compared aerobic fitness, body composition, fat distribution, and inflammation in obese postmenopausal women with and without the MS and investigated the relationship of the severity of MS to these characteristics.
We found that lean mass, visceral fat area, and plasma sTNFR1 concentration were significantly higher in women with the MS.
Moreover, lean mass, visceral fat area, and sTNFR1 concentrations were independently related to the severity of MS i. the number of components in these women. Our findings support those of a previous study by Brochu et al. A cut-point for insulin sensitivity glucose disposal rate, 8.
They found that there was a subgroup of obese, but metabolically normal, women who displayed high levels of insulin sensitivity despite having a high amount of body fat. Our finding that obese postmenopausal women without the MS have a lower HOMA score high insulin sensitivity is in line with these findings.
Moreover, Brochu et al. Our findings strongly confirm the importance of visceral adiposity in determining the presence of the MS in obese postmenopausal women and specifically indicate that women with the MS tend to have an androgenic body type compared with healthier obese women.
In healthy women there is a negative correlation between amount of visceral fat and in vivo measures of protein catabolism, suggesting that there may be an underlying mechanism linking the amount of visceral fat and lean mass The possible mechanisms include increased concentrations of free androgens due to diminished levels of SHBG 25 — 27 , a protein-sparing effect due to increased lipid metabolism 28 , 29 , and changes in muscle capillarization and fiber composition due to visceral adiposity Therefore, in the current study the difference in lean mass between women with and without the MS may be partly due to the difference in amount of visceral fat.
However, the number of MS components still correlated with lean mass even when the effect of visceral fat was considered. Obviously, there is another underlying factor s that influences lean mass and the MS in these obese women.
Prior studies show that the MS is related to low aerobic fitness in healthy individuals 11 , 17 , In addition, poor aerobic fitness is important in the development of hemorheological abnormalities associated with the MS Conversely, we did not see a significant relationship between the MS and aerobic fitness in these women.
It should be noted that all of these women were very sedentary, with a below average fitness level, because we excluded any physically active woman.
Thus, the range of fitness levels may have not been large enough to see an association with MS. However, this could be seen as an advantage of this study, because we eliminated a potential confounder of the relationship between MS and body composition.
In the current study women with the MS did not show significantly different body weight, BMI, fat mass, or even waist circumference, which is a MS risk component. Although body weight, BMI, and fat mass were related to the severity of the MS in the current study, these relationships were actually due to the effects of lean mass and visceral fat, which independently correlated with the number of MS components.
Considering the effect of visceral fat on metabolism and the relatively small variance in lean mass, visceral fat is probably the most important physical characteristic associated with the MS. In addition, sc abdominal adipocyte size is an independent predictor of type 2 diabetes In the present study neither between-group comparisons nor correlation analyses supported any relationship between the MS and sc adipocyte sizes.
In a study conducted in obese individuals who had undergone abdominal surgery, both visceral fat and sc fat were obtained, and the results showed that an adverse lipid profile had a higher correlation with visceral adipocyte size than with sc adipocyte size Because visceral adipocyte size, but not sc adipocyte size, is directly related to visceral fat area 16 , it may be that the MS is more closely linked with visceral adipocyte size.
However, there are only limited data regarding the relationship of the MS to regional adipocyte hypertrophy; therefore, more studies are needed. Gene expression and production of IL-6 and TNFα in adipose tissue are elevated with overall and abdominal obesity 34 — These adipokines may act in either an autocrine or a paracrine fashion to mediate the effect of adiposity on a number of physiological functions and disease processes 37 , It has been reported that circulating levels of CRP and IL-6 are higher in metabolically abnormal type 2 diabetics when TG, HDL-C, blood pressure, cardiovascular evidence, and BMI are used for the diagnosis of the MS Moreover, both individual 14 , 15 , 20 and clustering 19 , 20 of MS components are linked with CRP levels.
However, we did not find significantly different levels of CRP and cytokines between the two groups, and the severity of the MS was not significantly related to CRP and cytokines. The possible reason for the nonsignificant results may be due to the relatively small sample size in the study.
Current evidence indicates that cytokine soluble receptors have a longer half-life, which may allow them to prolong the biological effects of the cytokines 40 , Therefore, the functions of these soluble receptors are not limited to signal transduction, but include extracellular regulation of cytokine bioavailability 42 , Emerging data support the idea that circulating levels of sTNFRs are directly linked with lipoprotein disturbance 44 , 45 , insulin resistance 46 , and obesity In this study we found a significant between-group difference in sTNFR1 levels and a significant correlation between the number of MS components and sTNFR1 in the obese women.
These results support the idea that the overall MS is linked with this inflammatory cytokine receptor. It has been suggested that sTNFα preferentially binds to sTNFR1, rather than to sTNFR2 48 ; therefore, sTNFR1 is probably more important in the extracellular regulation of TNFα action on MS.
Because gene expression of sTNFRs in adipose tissue is increased with obesity 49 , it is possible that both visceral fat mass and sTNFR1 production from visceral fat per se are responsible for the link between the MS and plasma sTNFR1. Moreover, sTNFR1 is produced by a number of cell types, including leukocyte subpopulations monocytes, neutrophils, T cells, and B cells , endothelial cells, and adipocytes 42 , Mechanisms other than total and visceral adiposity need to be clarified by future studies.
In summary, this study demonstrates that lean mass, visceral fat area, and plasma sTNFR1 concentration were significantly higher in obese postmenopausal women with the MS than in those without the MS. In addition, lean mass, visceral fat area, and sTNFR1 concentrations were independently related to the number of MS components in these women.
Thus, obese older women with the MS are characterized by high lean mass, high visceral fat, and increased sTNFR1, and the severity of the syndrome is associated with body composition, visceral fatness, and inflammation.
We are grateful to the study coordinators, nurses, laboratory technicians, and exercise physiologists of the Division of Gerontology, University of Maryland School of Medicine, and the Baltimore Veterans Affairs Geriatric Research, Education, and Clinical Center for their assistance with this project.
We also thank the laboratory technicians at Wake Forest University School of Medicine for their work on the cytokine assays. Finally, we especially thank all of the women who volunteered to participate in this study. Ley CJ , Lees B , Stevenson JC Sex- and menopause-associated changes in body-fat distribution.
Am J Clin Nutr 55 : — Google Scholar. Zamboni M , Armellini F , Harris T , Turcato E , Micciolo R , Bergamo-Andreis IA , Bosello O Effects of age on body fat distribution and cardiovascular risk factors in women.
Am J Clin Nutr 66 : — Tchernof A , Poehlman ET Effects of the menopause transition on body fatness and body fat distribution. Obes Res 6 : — Arteriosclerosis 10 : — Kissebah A , Krakower G Regional adiposity and morbidity.
Physiol Rev 74 : — Obes Res 6 : 8 S—17S. Arch Intern Med : — Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults Executive Summary of the Third Report of the National Cholesterol Education Program NCEP Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults Adult Treatment Panel III.
JAMA : — Ford ES , Giles WH , Dietz WH Prevalence of the metabolic syndrome among US adults: findings from the third National Health and Nutrition Examination Survey. Park YW , Zhu S , Palaniappan L , Heshka S , Carnethon MR , Heymsfield SB The metabolic syndrome: prevalence and associated risk factor findings in the US population from the Third National Health and Nutrition Examination Survey, — Bertoli A , Di Daniele N , Ceccobelli M , Ficara A , Girasoli C , De Lorenzo A Lipid profile, BMI, body fat distribution, and aerobic fitness in men with metabolic syndrome.
Acta Diabetol 40 : S — S Brochu M , Tchernof A , Dionne IJ , Sites CK , Eltabbakh GH , Sims EA , Poehlman ET What are the physical characteristics associated with a normal metabolic profile despite a high level of obesity in postmenopausal women?
J Clin Endocrinol Metab 86 : — Chan JC , Cheung JC , Stehouwer CD , Emeis JJ , Tong PC , Ko GT , Yudkin JS The central roles of obesity-associated dyslipidaemia, endothelial activation and cytokines in the metabolic syndrome: an analysis by structural equation modelling.
Int J Obes Relat Metab Disord 26 : — Forouhi NG , Sattar N , McKeigue PM Relation of C-reactive protein to body fat distribution and features of the metabolic syndrome in Europeans and South Asians. Int J Obes Relat Metab Disord 25 : — Frohlich M , Imhof A , Berg G , Hutchinson WL , Pepys MB , Boeing H , Muche R , Brenner H , Koenig W Association between C-reactive protein and features of the metabolic syndrome: a population-based study.
Diabetes Care 23 : — Garaulet M , Perez-Llamas F , Zamora S , Tebar FJ Interrelationship between serum lipid profile, serum hormones and other components of the metabolic syndrome. J Physiol Biochem 58 : — Carroll S , Cooke CB , Butterly RJ Metabolic clustering, physical activity and fitness in nonsmoking, middle-aged men.
Med Sci Sports Exerc 32 : — Wareham NJ , Hennings SJ , Byrne CD , Hales CN , Prentice AM , Day NE A quantitative analysis of the relationship between habitual energy expenditure, fitness and the metabolic cardiovascular syndrome.
Br J Nutr 80 : — Ridker PM , Buring JE , Cook NR , Rifai N C-reactive protein, the metabolic syndrome, and risk of incident cardiovascular events: an 8-year follow-up of initially healthy American women. Circulation : — Tamakoshi K , Yatsuya H , Kondo T , Hori Y , Ishikawa M , Zhang H , Murata C , Otsuka R , Zhu S , Toyoshima H The metabolic syndrome is associated with elevated circulating C-reactive protein in healthy reference range, a systemic low-grade inflammatory state.
Int J Obes Relat Metab Disord 2 : — Nicklas BJ , Rogus EM , Colman EG , Goldberg AP Visceral adiposity, increased adipocyte lipolysis, and metabolic dysfunction in obese postmenopausal women.
Am J Physiol : E72 — E Dole VP A relation between non-esterified fatty acids in plasma and the metabolism of glucose. J Clin Invest 35 : — Matthews DR , Hosker JP , Rudenski AS , Naylor BA , Treacher DF , Turner RC Homeostasis model assessment: insulin resistance and β-cell function from fasting plasma glucose and insulin concentrations in man.
Diabetologia 28 : — Solini A , Bonora E , Bonadonna R , Castellino P , DeFronzo RA Protein metabolism in human obesity: relationship with glucose and lipid metabolism and with visceral adipose tissue. J Clin Endocrinol Metab 82 : — Evans DJ , Hoffmann RG , Kalkhoff RK , Kissebah AH Relationship of androgenic activity to body fat topography, fat cell morphology, and metabolic aberrations in premenopausal women.
J Clin Endocrinol Metab 57 : — Leenen R , van der Kooy K , Seidell JC , Deurenberg P , Koppeschaar HP Visceral fat accumulation in relation to sex hormones in obese men and women undergoing weight loss therapy. J Clin Endocrinol Metab 78 : — Berman DM , Rodrigues LM , Nicklas BJ , Ryan AS , Dennis KE , Goldberg AP Racial disparities in metabolism, central obesity, and sex hormone-binding globulin in postmenopausal women.
J Clin Endocrinol Metab 86 : 97 — Ferrannini E , Barrett EJ , Bevilacqua S , Jacob R , Walesky M , Sherwin RS , DeFronzo RA Effect of free fatty acids on blood amino acid levels in human. Am J Physiol : E — E Keller U , Turkalj I , Laager R , Bloesch D , Bilz S Effects of medium- and long-chain fatty acids on whole body leucine and glucose kinetics in man.
Metabolism 51 : — Lillioja S , Young AA , Culter CL , Ivy JL , Abbott WG , Zawadzki JK , Yki-Jarvinen H , Christin L , Secomb TW , Bogardus C Skeletal muscle capillary density and fiber type are possible determinants of in vivo insulin resistance in man.
J Clin Invest 80 : — Carroll S , Cooke CB , Butterly RJ Plasma viscosity, fibrinogen and the metabolic syndrome: effect of obesity and cardiorespiratory fitness. Blood Coagul Fibrinolysis 11 : 71 — Metabolism 48 : — Weyer C , Foley JE , Bogardus C , Tataranni PA , Pratley RE Enlarged subcutaneous abdominal adipocyte size, but not obesity itself, predicts type II diabetes independent of insulin resistance.
Diabetologia 43 : — Fried SK , Bunkin DA , Greenberg AS Omental and subcutaneous adipose tissues of obese subjects release interleukin depot difference and regulation by glucocorticoid. J Clin Endocrinol Metab 83 : — Hotamisligil GS , Arner P , Caro JF , Atkinson RL , Spiegelman BM Increased adipose tissue expression of tumor necrosis factor-α in human obesity and insulin resistance.
J Clin Invest 95 : — Bastard JP , Maachi M , Van Nhieu JT , Jardel C , Bruckert E , Grimaldi A , Robert JJ , Capeau J , Hainque B Adipose tissue IL-6 content correlates with resistance to insulin activation of glucose uptake both in vivo and in vitro.
J Clin Endocrinol Metab 87 : — Bullo-Bonet M , Garcia-Lorda P , Lopez-Soriano FJ , Argiles JM , Salas-Salvado J Tumour necrosis factor, a key role in obesity? FEBS Lett : — Yudkin JS , Kumari M , Humphries SE , Mohamed-Ali V Inflammation, obesity, stress and coronary heart disease: is interleukin-6 the link?
Atherosclerosis : — Pickup JC , Mattock MB , Chusney GD , Burt D NIDDM as a disease of the innate immune system: association of acute-phase reactants and interleukin-6 with metabolic syndrome X.
Diabetologia 40 : — Kishimoto T , Akira S , Taga T Interleukin-6 and its receptor: a paradigm for cytokines. Science : — Grell M Tumor necrosis factor TNF receptors in cellular signaling of soluble and membrane-expressed TNF.
J Inflamm 47 : 8 — Aderka D The potential biological and clinical significance of the soluble tumor necrosis factor receptors. Cytokine Growth Factor Rev 7 : — Jones SA , Horiuchi S , Topley N , Yamamoto N , Fuller GM The soluble interleukin 6 receptor: mechanisms of production and implications in disease.
FASEB J 15 : 43 — Fernandez-Real JM , Gutierrez C , Ricart W , Castineira MJ , Vendrell J , Richart C Plasma levels of the soluble fraction of tumor necrosis factor receptors 1 and 2 are independent determinants of plasma cholesterol and LDL-cholesterol concentrations in healthy subjects.
Fernandez-Real JM , Broch M , Ricart W , Casamitjana R , Gutierrez C , Vendrell J , Richart C Plasma levels of the soluble fraction of tumor necrosis factor receptor 2 and insulin resistance.
Diabetes 47 : — Dzienis-Straczkowska S , Straczkowski M , Szelachowska M , Stepien A , Kowalska I , Kinalska I Soluble tumor necrosis factor-α receptors in young obese subjects with normal and impaired glucose tolerance. Diabetes Care 26 : — Hauner H , Bender M , Haastert B , Hube F Plasma concentrations of soluble TNF-α receptors in obese subjects.
Int J Obes Relat Metab Disord 22 : — Hube F , Hauner H The role of TNF-α in human adipose tissue: prevention of weight gain at the expense of insulin resistance? Horm Metab Res 31 : — Hube F , Birgel M , Lee YM , Hauner H Expression pattern of tumour necrosis factor receptors in subcutaneous and omental human adipose tissue: role of obesity and non-insulin-dependent diabetes mellitus.
Eur J Clin Invest 29 : — Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide. Sign In or Create an Account.
Endocrine Society Journals. Advanced Search. Search Menu. Article Navigation. Close mobile search navigation Article Navigation. Volume Article Contents Abstract. Subjects and Methods. Journal Article. The Metabolic Syndrome in Obese Postmenopausal Women: Relationship to Body Composition, Visceral Fat, and Inflammation.
Tongjian You , Tongjian You. Tongjian You, Section on Gerontology and Geriatric Medicine, Wake Forest University School of Medicine, Medical Center Boulevard, Winston-Salem, North Carolina Oxford Academic. Alice S. Barbara J. PDF Split View Views.
Nutrient timing for exercise Markere Nutrient timing for exercise 6Article number: Vissceral Cite this article. Metrics details. Viscerral visceral fat tissue is known to release various inflammatory and anti-inflammatory Infoammation, abdominal obesity may play a key role in the inflammation Power and explosive training with metabolic syndrome MetS. However, few studies have determined precise relationships of abdominal obesity with inflammatory markers in MetS. To clarify the importance of abdominal obesity in sub-clinical inflammation, we examined the changes of inflammatory markers in clustering of MetS components with or without abdominal obesity. Subjects consisted of apparently healthy Japanese men age: 30 to 59 years who underwent health examination in the Osaka University Health Care Center. MetS components were assessed and serum levels of high sensitive C-reactive protein hs-CRPinterleukin IL -6 and adiponectin were examined in all subjects. Susan SamSteven IhflammationMichael Resveratrol and stress reduction. Davidson inflammatioh, Ralph B. D'AgostinoInflammaation Feinstein makers, George Leafy greens for Mediterranean diets Vsceral, Alfonso PerezTheodore Mazzone; Relation Body composition assessment Leafy greens for Mediterranean diets Fat Depots to Systemic Markers of Inflammation in Type 2 Diabetes. Matkers Care 1 May ; 32 5 : — Both visceral adipose tissue VAT and subcutaneous adipose tissue SAT have been linked to systemic inflammation in nondiabetic cohorts. We examined the relationships between VAT and SAT and systemic inflammatory markers in a large well-characterized cohort of subjects with type 2 diabetes. Three hundred eighty-two subjects with type 2 diabetes in the CHICAGO Carotid Intima-Media Thickness in Atherosclerosis Using Pioglitazone study cohort underwent abdominal computed tomography to determine SAT and VAT distribution.
ich beglückwünsche, Ihr Gedanke einfach ausgezeichnet
Ich denke, dass Sie den Fehler zulassen. Ich kann die Position verteidigen. Schreiben Sie mir in PM, wir werden besprechen.
Eben dass wir ohne Ihre prächtige Idee machen würden
Nach meiner Meinung sind Sie nicht recht. Schreiben Sie mir in PM.
Und es sind noch die Varianten möglich?