
Alternate-day fasting and insulin sensitivity -
Lipolysis increases at the beginning of a fasting period here evidenced by increased FFA and glycerol after 30 h fasting; Table 2. The more so, because the anti-lipolytic effect of insulin diminishes with fasting Jensen et al.
Support for an ADF-induced triglyceride-lowering effect is found in low-calorie refeeding studies that demonstrated increased triglyceride turnover and removal efficiency Streja et al. During the fasting days in the present ADF protocol, it would be reasonable to assume that a large part of the substrates for energy production comes from lipids.
If not from intramuscular stores, of which a decrease could not be detected, then from extramyocellular stores, i. adipose tissue. The amount of adipose tissue decreased Table 1 during the 6-week intervention, which in turn give rise to the increased availability of fatty acids Table 2 that facilitates an increased fatty acid transport across the sarcolemma.
To this end, we measured fatty acid translocase CD36 , fatty acids transport protein 4 FATP4 , and plasma membrane fatty acid binding protein FABPpm which are important players in the transport of fatty acids across the plasma membrane. A mixed result was seen, with CD36 increasing significantly in the OB group, FATP4 decreasing in T2DM, and decreasing in FABPpm main effect Supplementary Figure S1.
The changes were small, and the data cannot support the notion that fatty acid transport was increased. Most likely, the oscillation of carbohydrate and lipid substrates every other day blurred a potential marked increase in these proteins.
Once inside the muscle cell, fatty acids can be stored as triglycerides and the final step in the synthesis is catalyzed by diglyceride acyltransferase 1 DGAT1. DGAT1 protein expression did not change with the intervention Supplementary Figure S2M , but even though we did not detect a difference in lipid content between the two groups, DGAT1 was significantly higher expressed in T2DM compared with OB.
To our knowledge, DGAT1 protein expression in skeletal muscle of patients with type 2 diabetes has only been measured in one other study, in which no change was found compared with obese people and athletes Bergman et al.
Our data suggest that T2DM have the capacity to synthesize greater amounts of intramuscular lipids. We measured two proteins involved in lipolysis adipose triglyceride lipase ATGL , monoacylglyceride lipase MGLL and in lipid storage Perilipin 2 adipophilin , perilipin 3 TIP47 , and perilipin 5 OXPAT and in line with the unchanged lipid content in the muscles Figure 5 we found no effect of the intervention on these proteins Supplementary Figure S1.
An increase in medium-chain acyl-CoA dehydrogenase MCAD might have been seen because MCAD is involved in medium-chain fatty acid beta-oxidation, which would be expected to increase with increased fatty acid availability but not with increased lipid storage.
However, no change was detected Supplementary Figure S1. The expression of proteins involved in lipid transport, synthesis and storage presented here, are in line with data on gene expression mRNA of many of these proteins in a study on females undergoing an intermittent fasting regimen with the muscle biopsies obtained in the same condition i.
after an overnight h fast Liu et al. However, in that study Liu et al. Others have also found that CD36 mRNA remains unchanged with a zero-calorie ADF regimen Heilbronn et al.
Compared with minor caloric restriction, ADF over 6 months does not bring about superior health benefits in terms of body weight, body composition, or cardiovascular risk factors in patients with obesity Trepanowski et al.
This difference in design as well as differences in study cohorts between the two studies makes a direct comparison difficult. The second part of the present study, where ad libitum diet was allowed on feast days demonstrated that the study participants did not inadvertently compensate the overall caloric deficit, because body weight decreased faster in the latter part of the study.
If weight loss is the purpose of ADF, zero-calorie intake must therefore be recommended on fast days because it will not be compensated on feast days. The length of the fasting may also play a role. In the study by Trepanowski et al.
Trepanowski et al. Varady, personal communication , but since lunch was allowed between and on fasting days, the fasting period was, in fact, two periods of 12 and 10 h. These relatively short periods of fasting every other day may therefore be the reason that this intervention was not superior in reducing body weight compared to ordinary everyday caloric restriction.
In the present study, each zero-calorie fasting period was 30 h, which is of sufficient length to markedly draw from endogenous energy sources, introducing loss of body weight and also mimicking oscillations in energy stores induced by exercise Dela et al.
In line with previous studies for review see Dela et al. Dela and Helge, and newer studies Lund et al. In the present study, we tested ADP sensitivity of the skeletal muscle mitochondria Supplementary Figure S1 but found no difference between the groups or an effect of ADF.
Previously, in patients with type 2 diabetes, we have demonstrated increased sensitivity for complex I glutamate and complex II succinate substrates Larsen et al. This study has some limitations. We did not randomize patients to a non-intervention control group, because it is a well-known risk that patients assigned to passive control groups may exhibit behavioural changes, especially in studies with a focus on dietary behaviour.
Instead, we performed two baseline experiments that were carried out two to 3 weeks apart Figure 1 to account for any variation in methodology and to avoid a time effect of enrollment into a dietary study per se. We did not include a group that performed conventional caloric restriction, thus we cannot make a direct comparison between ADF and conventional caloric restriction, and this was not the purpose here.
The intervention was well tolerated by all patients. The strict zero-calorie regimen is a quite demanding approach, but the reports from the participants were that the most difficult task was to eat the double diet on non-fasting days during the first 3 weeks.
However, a double diet every other day was only used for mechanistic reasons, and it is not the recommended approach for the general use of ADF. It should also be noted that oral medication, except antihypertensive drugs but including glucose lowering drugs, was discontinued during the entire intervention.
Yet, the patients with type 2 diabetes experienced an improvement in fasting glucose and even HbA1c. This suggests that shorter term 6 weeks ADF is a feasible approach in patients in treatment with oral glucose-lowering therapy that will bring about loss of weight and improved glycemic control.
Longer-term more than 6 weeks effects i. The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by The Regional Ethics Committee H Conceptualization, FD, and AI; Methodology, FD, SL, CP. CH, and AI; Investigation, AI, FD, HH, MC, CJ, EN, SL, JH, EC, and CP; Writing—Original Draft, AI, and FD; Writing—Review and Editing, AI, FD, JH, SL, and CP; Funding Acquisition, FD.
The Danish Council for Independent Research grant no: B , Nordea Foundation grant to the Center for Healthy Aging. We thank the participants, and the technical assistance provided by R. Kraunsøe, J. Bach, and T.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers.
Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Al-Mrabeh A. Hepatic lipoprotein export and remission of human type 2 diabetes after weight loss. Cell Metab. PubMed Abstract CrossRef Full Text Google Scholar. Arnason T. Effects of intermittent fasting on health markers in those with type 2 diabetes: A pilot study. World J. Diabetes 8 4 , — Barnosky A.
Intermittent fasting vs daily calorie restriction for type 2 diabetes prevention: A review of human findings. Bergman B. Intramuscular triglyceride synthesis: Importance in muscle lipid partitioning in humans.
Bille D. Liver fat content investigated by magnetic resonance spectroscopy in obese children and youths included in multidisciplinary treatment. Carbajo M. Weight loss and improvement of lipid profiles in morbidly obese patients after laparoscopic one-anastomosis gastric bypass: 2-year follow-up.
Carter S. Effect of intermittent compared with continuous energy restricted diet on glycemic control in patients with type 2 diabetes: A randomized noninferiority trial. JAMA Netw.
Open 1 3 , e Catenacci V. A randomized pilot study comparing zero-calorie alternate-day fasting to daily caloric restriction in adults with obesity. Silver Spring 24 9 , — Chabanova E. Dela F. Insulin resistance and mitochondrial function in skeletal muscle. Cell Biol.
Effects of one-legged High-intensity Interval Training on insulin-mediated skeletal muscle glucose homeostasis in patients with type 2 diabetes. Acta Physiol. Insulin-stimulated muscle glucose clearance in patients with NIDDM. Effects of one-legged physical training.
Diabetes 44, — Physical training increases muscle GLUT-4 protein and mRNA in patients with NIDDM. Diabetes 43, — Effect of physical training on insulin secretion and action in skeletal muscle and adipose tissue of first-degree relatives of type 2 diabetic patients.
Physical training may enhance beta-cell function in type 2 diabetes. Dohlmann T. High-intensity interval training changes mitochondrial respiratory capacity differently in adipose tissue and skeletal muscle.
Fery F. Mechanisms of starvation diabetes: A study with double tracer and indirect calorimetry. Fonvig C. Muscle fat content and abdominal adipose tissue distribution investigated by magnetic resonance spectroscopy and imaging in obese children and youths.
Frossing S. Quantification of visceral adipose tissue in polycystic ovary syndrome: Dual-energy X-ray absorptiometry versus magnetic resonance imaging. Acta Radiol. Halberg N. Effect of intermittent fasting and refeeding on insulin action in healthy men. Hansen M. The effects of diet- and RYGB-induced weight loss on insulin sensitivity in obese patients with and without type 2 diabetes.
Acta Diabetol. The effect of metformin on glucose homeostasis during moderate exercise. Diabetes Care 38 2 , — Harvie M. Potential benefits and harms of intermittent energy restriction and intermittent fasting amongst obese, overweight and normal weight subjects-A narrative review of human and animal evidence.
Heilbronn L. Glucose tolerance and skeletal muscle gene expression in response to alternate day fasting. Holten M. Strength training increases insulin-mediated glucose uptake, GLUT4 content and insulin signaling in skeletal muscle in patients with Type 2 diabetes. Diabetes 53 2 , — Jensen M.
Lipolysis during fasting. Decreased suppression by insulin and increased stimulation by epinephrine. Kelley D. Fatty liver in type 2 diabetes mellitus: Relation to regional adiposity, fatty acids, and insulin resistance.
Krotkiewski M. The effects of physical training on insulin secretion and effectiveness and on glucose metabolism in obesity and type 2 non-insulin-dependent diabetes mellitus.
Diabetologia 28, — Larsen S. Influence of exercise amount and intensity on long-term weight loss maintenance and skeletal muscle mitochondrial ROS production in humans.
The effect of high-intensity training on mitochondrial fat oxidation in skeletal muscle and subcutaneous adipose tissue. Sports 25 1 , e59—e Biomarkers of mitochondrial content in skeletal muscle of healthy young human subjects.
Increased mitochondrial substrate sensitivity in skeletal muscle of patients with type 2 diabetes. Diabetologia 54 6 , — Lim E. Reversal of type 2 diabetes: Normalisation of beta cell function in association with decreased pancreas and liver triacylglycerol.
Diabetologia 54 10 , — Liu B. Effects of intermittent fasting or calorie restriction on markers of lipid metabolism in human skeletal muscle.
Lund M. Preoperative beta-cell function in patients with type 2 diabetes is important for the outcome of Roux-en-Y gastric bypass surgery. Mitochondrial respiratory capacity remains stable despite a comprehensive and sustained increase in insulin sensitivity in obese patients undergoing gastric bypass surgery.
Mattson M. Impact of intermittent fasting on health and disease processes. Ageing Res. Pan D. Skeletal muscle triglyceride levels are inversely related to insulin action.
Diabetes 46 6 , — Poitout V. Glucolipotoxicity of the pancreatic beta cell. Acta 3 , — Prats C. An optimized histochemical method to assess skeletal muscle glycogen and lipid stores reveals two metabolically distinct populations of type I muscle fibers.
PLoS ONE 8 10 , e Real-Hohn A. The synergism of high-intensity intermittent exercise and every-other-day intermittent fasting regimen on energy metabolism adaptations includes hexokinase activity and mitochondrial efficiency.
PLoS ONE 13 12 , e Schindelin J. Fiji: An open-source platform for biological-image analysis. Methods 9 7 , — Solomon T. Improved pancreatic beta-cell function in type 2 diabetic patients after lifestyle-induced weight loss is related to glucose-dependent insulinotropic polypeptide.
Diabetes Care 33 7 , — Steele R. Measurement of size and turnover rate of body glucose pool by the isotope dilution method. Stekovic S. Alternate day fasting improves physiological and molecular markers of aging in healthy, non-obese humans. Steven S.
Very low-calorie diet and 6 Months of weight stability in type 2 diabetes: Pathophysiological changes in responders and nonresponders. Diabetes Care 39 5 , — Weight loss decreases excess pancreatic triacylglycerol specifically in type 2 diabetes.
Diabetes Care 39 1 , — Streja D. The effects of prolonged fasting on plasma triglyceride kinetics in man. Sutton E. Early time-restricted feeding improves insulin sensitivity, blood pressure, and oxidative stress even without weight loss in men with prediabetes.
Trepanowski J. Effect of alternate-day fasting on weight loss, weight maintenance, and cardioprotection among metabolically healthy obese adults: A randomized clinical trial. JAMA Intern. Varady K. Impact of intermittent fasting on glucose homeostasis. Care 19 4 , — Vendelbo M.
Insulin resistance after a h fast is associated with impaired AS phosphorylation and accumulation of lipid and glycogen in human skeletal muscle.
White M. Type 2 diabetes: The pathologic basis of reversible beta-cell dysfunction. Diabetes Care 39 11 , — Wing R. Benefits of modest weight loss in improving cardiovascular risk factors in overweight and obese individuals with type 2 diabetes. Diabetes Care 34 7 , — Keywords: fasting, glucose homeostasis, insulin sensitivity, visceral fat, weight loss, β-cell.
Citation: Ingersen A, Helset HR, Calov M, Chabanova E, Harreskov EG, Jensen C, Hansen CN, Prats C, Helge JW, Larsen S and Dela F Metabolic effects of alternate-day fasting in males with obesity with or without type 2 diabetes. doi: Received: 04 October ; Accepted: 21 November ; Published: 01 December Copyright © Ingersen, Helset, Calov, Chabanova, Harreskov, Jensen, Hansen, Prats, Helge, Larsen and Dela.
This is an open-access article distributed under the terms of the Creative Commons Attribution License CC BY. The use, distribution or reproduction in other forums is permitted, provided the original author s and the copyright owner s are credited and that the original publication in this journal is cited, in accordance with accepted academic practice.
No use, distribution or reproduction is permitted which does not comply with these terms. Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers.
Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher. Top bar navigation. About us About us. Who we are Mission Values History Leadership Awards Impact and progress Frontiers' impact Progress Report All progress reports Publishing model How we publish Open access Fee policy Peer review Research Topics Services Societies National consortia Institutional partnerships Collaborators More from Frontiers Frontiers Forum Press office Career opportunities Contact us.
Sections Sections. About journal About journal. Article types Author guidelines Editor guidelines Publishing fees Submission checklist Contact editorial office. ORIGINAL RESEARCH article Front.
This article is part of the Research Topic Rising Stars in Integrative Physiology: View all 4 articles. The quality and quantity of total RNA were determined using a Nanodrop ND Spectrophotometer Nano Drop Technologies, Wilmington, DE.
Total RNA 1. Quantitative real-time PCR analyses were performed using an i-Cycler I-Q5, Bio-Rad Laboratories, Hercules, CA, United States. Reactions were carried out in triplicate in a total volume of 25 μl using SYBR green qPCR Master Mix Invitrogen, Grand Island, NY, United States.
The housekeeping gene Actb was used for internal normalization. Mean C T values for both the target and internal control genes were determined. Results are presented as fold change of transcripts for target normalized to internal reference Actb , compared with m Lepr db defined as 1.
The efficiency of the PCR reaction was determined using a dilution series of a standard MAT sample. Louis, MO, United States. Protein expression was detected using anti-nitrotyrosine primary antibody Abcam, Cat ab, anti-tubulin primary antibody Abcam, Cat ab, , , Horseradish peroxidase-conjugated secondary antibodies were used.
Signals were visualized by enhanced chemiluminescence Santa Cruz Biotechnology, Santa Cruz, CA, United States , scanned densitometrically using Fuji LAS and quantified with Multigauge software Fujifilm.
The relative amounts of protein expression were quantified to those of the corresponding m Lepr db control, which was set to a value of 1. All data were presented as mean ± SEM except as specifically stated. Statistical analyses were performed using SPSS The sample size was empirically determined based on our previous studies examining the metabolic and endothelial function of Lepr db mice and their respective m Lepr db control mice 20 , 27 , 28 , 32 , 34 , Mice were grouped by genotype and weight-matched thus not randomized.
Blinded analysis was not performed because of feasibility. Mice on the ADF diet were allowed to eat ad libitum for one day, and then given no food the next day. This regimen was maintained for 12 weeks. Meanwhile, mice without ADF were continually allowed to feed ad libitum.
Food intake was measured on the feast day for mice with or without ADF once per week. ADF led to a net reduction of food intake at As expected, the Lepr db diabetic mice showed higher body weight, abdominal girth, total cholesterol, blood glucose, insulin, and HOMA-IR than the m Lepr db control mice.
In m Lepr db control mice, week ADF reduced body weight, abdominal girth, and insulin. Although ADF modestly reduced total cholesterol, glucose, and HOMA-IR in m Lepr db control mice, the P -values were greater than 0. In Lepr db mice, ADF did not significantly reduce body weight, abdominal girth, and total cholesterol.
ADF, however, remarkably reduced blood glucose and HOMA-IR without affecting insulin levels Table 1 , supporting the profound effects of ADF on improving glucose metabolism despite the lack of effects on weight loss in diabetic mice.
We further determined how ADF affects insulin sensitivity by performing an insulin tolerance test. As expected, the Lepr db diabetic mice showed impaired insulin sensitivity. ADF improved insulin sensitivity in both m Lepr db control mice and Lepr db diabetic mice Figure 1.
Figure 1. Alternate day fasting ADF improved insulin sensitivity in both m Lepr db and Lepr db mice. Insulin tolerance tests revealed that diabetic mice Lepr db had impaired glucose metabolism compared with control mice m Lepr db. Twelve weeks of alternate-day fasting ADF improved insulin sensitivity in both Lepr db and m Lepr db mice.
Data represent mean ± SEM. Lepr db diabetic mice. SMA represent resistance arteries contributing to vascular resistance and regulation of blood flow. Acetylcholine ACh -induced endothelium-dependent vasorelaxation was impaired in SMA of Lepr db diabetic mice vs.
m Lepr db control mice. ADF remarkably improved the endothelial function of diabetic mice Figure 2A. Sodium nitroprusside SNP -induced endothelium-independent vasorelaxation Figure 2C and phenylephrine PE -induced vasoconstriction Figure 2D were comparable among groups. Incubation with the nitric oxide synthase inhibitor L-NAME largely attenuated the ADF-induced improvement of endothelial function in diabetic mice Figure 2B.
ADF did not affect endothelium-independent vasorelaxation or PE-induced vasoconstriction in m Lepr db control mice Figure 2. Figure 2.
ADF improved endothelium-dependent vasorelaxation without affecting endothelium-independent vasorelaxation or phenylephrine-induced vasoconstriction of small mesenteric arteries SMA in type 2 diabetic mice.
A Acetylcholine ACh -induced endothelium-dependent vasorelaxation of SMA was impaired in Lepr db mice. B Incubation with the nitric oxide synthase inhibitor L-NAME largely attenuated ADF-induced improvement of endothelial function in diabetic mice.
C Sodium Nitroprusside SNP -induced endothelium-independent vasorelaxation of SMA was comparable among groups. D Phenylephrine PE -induced vasoconstriction of SMA was comparable among groups. Adiponectin levels were lower in the serum of Lepr db mice, and ADF increased serum adiponectin back to the level of m Lepr db control mice Figure 3A.
Serum resistin was lower in Lepr db mice than in m Lepr db control mice. ADF increased resistin in both m Lepr db control mice and Lepr db diabetic mice Figure 3B. As expected, Lepr db mice showed dramatically increased serum leptin, i.
ADF reduced serum leptin in m Lepr db control mice, yet further increased serum leptin in Lepr db mice Figure 3C. Figure 3. ADF modulated circulating levels and adipose expression of key adipokines, including adiponectin, resistin, and leptin in mesenteric adipose tissue MAT of both m Lepr db and Lepr db mice.
Circulating levels of adiponectin A , resistin B , and leptin C were determined by ELISA. mRNA expression of Adipoq D , Retn E , and Lep F were determined by qRT-PCR in mesenteric adipose tissue MAT.
Adipose tissue is the primary source of adipokines released into circulation We further determined mRNA expression of these adipokines in MAT. Consistent with the trend of circulating adipokine levels, Lepr db mice showed increased Lep mRNA encoding leptin in MAT Figure 3F , while reduced Retn mRNA encoding resistin Figure 3E compared with m Lepr db control mice.
Adipoq mRNA encoding adiponectin in MAT was not statistically different between m Lepr db and Lepr db mice Figure 3D. ADF increased Adipoq mRNA in MAT of m Lepr db control mice, though circulating adiponectin in m Lepr db control mice was not altered by ADF Figure 3D , likely suggesting post-transcriptional regulatory mechanisms limiting a further increase in circulating levels.
ADF further increased Lep mRNA in the MAT of m Lepr db control mice, though serum leptin was reduced by ADF Figure 3E. Overall, in Lepr db mice, adipokine levels in the serum and MAT showed consistent directionality following ADF. In m Lepr db control mice, however, the increase in MAT mRNA expression of Adipoq and Lep did not correlate with change in the circulation, likely suggesting possible feedback mechanisms to maintain homeostasis in non-diabetic control mice.
To determine if ADF improved endothelium-dependent vasorelaxation through modulating adipose-derived hormones, we treated control and diabetic mice with adenovirus expressing adiponectin Ad-APN or β-galactosidase Ad-βgal as the control.
As we have previously described 20 , mice were euthanized one week after adenovirus treatment and increased circulating adiponectin levels were confirmed by ELISA. Indeed, adiponectin supplementation partly improved endothelium-dependent vasorelaxation in Lepr db mice Figure 4A , without affecting endothelium-independent vasorelaxation Figure 4B.
according to a previously published protocol The short-term treatment of resistin did not impair or improve endothelium-dependent or -independent vasorelaxation Figures 4C,D , suggesting that short-term resistin administration may not affect vascular function. Similarly, Lepr db mice showed increased circulating leptin due to leptin receptor deficiency.
Circulating leptin was further enhanced by ADF, suggesting that an increase in circulating leptin itself was unlikely to prevent the vascular benefits of ADF. Thus, our study provided some mechanistic insights into the contribution of adipokines to ADF-mediated vascular effects in type 2 diabetes.
Figure 4. The effects of adipokines on endothelium-dependent vasorelaxation of SMA. A Adenovirus-mediated adiponectin supplementation improved ACh-induced endothelium-dependent vasorelaxation of SMA in Lepr db mice, without affecting SNP-induced endothelium-independent vasorelaxation B.
C,D Treatment with recombinant resistin did not affect endothelium-dependent or endothelium-independent vasorelaxation of SMA. Nitrotyrosine protein levels were elevated in both SMA and MAT of Lepr db diabetic mice compared with m Lepr db control mice.
ADF reduced SMA nitrotyrosine protein levels in Lepr db diabetic mice without affecting that in the m Lepr db control mice Figure 5A. ADF, however, did not significantly decrease MAT nitrotyrosine protein levels Figure 5B. Figure 5. ADF reduced nitrotyrosine protein levels in SMA, but not MAT, of Lepr db mice.
A Nitrotyrosine protein levels were higher in SMA of Lepr db mice. ADF reduced nitrotyrosince protein in SMA of Lepr db mice. B Nitrotyrosine protein levels were higher in MAT of Lepr db mice.
ADF did not alter nitrotyrosince protein in MAT of Lepr db mice. Studies demonstrate that intermittent fasting improves cardiometabolic risk factors such as blood pressure, levels of low-density lipoprotein cholesterol and triglycerides, insulin resistance, and HbA1c 5.
A better understanding of how intermittent fasting affects cardiovascular function and the underlying mechanisms will facilitate its clinical application in obesity and diabetes-associated cardiovascular complications. Our study revealed the profound benefits of ADF in rescuing endothelial dysfunction.
The benefits are at least partly mediated through enhanced adiponectin, while resistin and leptin were unlikely to be involved. Adiponectin thus provides a mechanistic link between the role of ADF in regulating adipokine profile and endothelial function in type 2 diabetes.
ADF reduced the marker of oxidative stress in resistance arteries but not adipose tissue, suggesting tissue-specific regulatory roles by ADF. ADF may also exert metabolic and vascular benefits in non-obese control mice. Overall, our data support that ADF presents as promising lifestyle intervention for treating diabetes-associated endothelial dysfunction.
Intermittent fasting is emerging as a popular alternative dietary intervention strategy. Despite limited numbers of clinical trials directly comparing the long-term effects of intermittent fasting and daily calorie restriction, current evidence supports equivalent or superior metabolic benefits of intermittent fasting 5.
Comparative studies in a month study of insulin-resistant participants support that ADF may produce greater reductions in fasting insulin and insulin resistance compared with calorie restriction despite similar decreases in body weight In Lepr db type 2 diabetic mice and streptozotocin-treated type 1 diabetic mice treated with a fasting-mimicking diet, both intermittent fasting and continuous calorie restriction significantly reduced fasting blood glucose levels and improved insulin sensitivity.
Yet, intermittent fasting performed significantly better than continuous calorie restriction in improving glycemic control and insulin sensitivity in Lepr db type 2 diabetic mice Clinical studies, conducted over multiple years, that directly compare different regimens will provide important insights into the long-term cardiometabolic benefits of these diets.
There are currently no clinical studies determining the vascular benefits of long-term ADF in patients with diabetes. Clinical trials of short-term ADF, e.
Increases in adiponectin were positively associated with augmented flow-mediated vasodilation post-ADF in those subjected to ADF with the low-fat diet ADF also reduced plasma resistin and leptin, which were not correlated with changes in flow-mediated vasodilation In a study involving 54 obese non-diabetic subjects with an 8-week ADF protocol, brachial artery flow-mediated vasodilation was positively correlated to adiponectin concentrations Another study involving 64 obese subjects supported that a week period of ADF improved brachial artery flow-mediated vasodilation Our experimental data strongly support the profound endothelial protective effects of ADF in mice modeling severe type 2 diabetes.
To our knowledge, this is the first experimental study determining the role of ADF in diabetes-associated vascular dysfunction. The above clinical studies in obese subjects and our experimental study in type 2 diabetic mice provide premises to further explore the clinical benefits of long-term ADF in diabetes-associated cardiovascular complications.
Our study has shed light on the mechanisms of the endothelial protective effects of ADF partly through enhanced circulating adiponectin. Adiponectin is well known for its anti-inflammatory and anti-oxidative roles in endothelial cells 43 and its protective effects against neointimal formation in response to vascular injury 44 and atherosclerosis Our previous work has also supported that adiponectin abates diabetes-induced endothelial dysfunction by suppressing oxidative stress, adhesion molecules, and inflammation in type 2 diabetic mice Specifically, adenovirus-mediated adiponectin supplementation improved endothelium-dependent vasorelaxation of aortas in Lepr db mice Adiponectin supplementation reduced aortic nitrotyrosine protein levels, via suppressing protein expression of gp91 phox , an NADPH oxidase subunit, and increasing protein expression of SOD3, an antioxidant enzyme Aortic expression of inflammatory genes, Tnf , Il6 , and Icam1 , was also suppressed by adiponectin supplementation These pathways are likely responsible for the endothelial protective and anti-oxidative effects of adiponectin in mesenteric arteries of Lepr db mice undergoing ADF.
The adiponectin-independent endothelial protective and anti-oxidative effects of ADF remain to be further dissected, and we speculate that the metabolic benefits of ADF may play important roles.
Alternate day fasting exerts profound metabolic benefits in both control and diabetic mice with remarkably improved glycemic control and insulin sensitivity.
The effects of ADF on weight loss and visceral adiposity were, however, modest. Consistent with our observation, an independent study also suggested that a week period of intermittent fasting, using a fasting mimicking diet protocol, improved glucose homeostasis in Lepr db mice without causing weight loss Thus, the metabolic benefits of ADF in Lepr db diabetic mice are likely not entirely dependent on weight loss effects.
Since the Lepr db mice resemble severe type 2 diabetes, whether ADF may also exert limited benefits in weight management in patients with type 2 diabetes, despite profound metabolic effects, should be studied clinically. Further, the benefits of ADF in non-obese, healthy humans thus may also warrant further investigation.
There are many questions that remain to be explored. Future studies may further elucidate if the knockout of adiponectin abolishes the vascular protective effects of ADF, the involvement of other adipokines, and the molecular mechanisms by which ADF modulates adipokine expression and secretion.
Comparative studies are required to tackle how different intermittent fasting regimens affect metabolic, vascular, and hormonal parameters. Findings generated from such studies could inform whether one regimen is superior to the others and elucidate the mechanisms that underlie the cardiometabolic benefits.
The discovery of pharmacological agents mimicking fasting can potentially provide novel therapeutic strategies. A potential limitation of the present studies is that they were performed only in male mice and mesenteric resistance arteries. In summary, our study examined the role and mechanisms of ADF in diabetes-associated endothelial dysfunction using murine models of type 2 diabetes.
We have revealed that ADF in type 2 diabetic mice exerts profound endothelial protective effects, partly through modulating the adipose-derived hormone, adiponectin.
Thus, this study improves our understanding of how ADF affords significant protection against endothelial dysfunction partly by regulating adipose-derived hormones. Our work also elaborated on the metabolic benefits and potential cardiovascular protective actions of ADF in the management of type 2 diabetes.
The manuscript is in memory of Dr. Cuihua Zhang, who was deceased on October 1, The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation. The animal study was reviewed and approved by the Animal Care Committee at the University of Missouri Columbia, MO, United States.
JC, HZ, and CZ conceived the study. JC, SL, and HZ performed the experiments. JC and HZ analyzed the data. JC, YL, and HZ interpreted results of experiments and drafted the manuscript. JC, YS, and HZ prepared the tables and figures.
JC, SL, YS, MH, YL, and HZ edited and revised the manuscript. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers.
Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher. ACh, acetylcholine; ADF, alternate-day fasting; MAT, mesenteric adipose tissue; NO, nitric oxide; PE, phenylephrine; SMA, small mesenteric artery; SNP, sodium nitroprusside.
Powell-Wiley TM, Poirier P, Burke LE, Després JP, Gordon-Larsen P, Lavie CJ, et al. Obesity and cardiovascular disease: a scientific statement from the american heart association. doi: PubMed Abstract CrossRef Full Text Google Scholar.
Varady KA, Cienfuegos S, Ezpeleta M, Gabel K. Cardiometabolic benefits of intermittent fasting. Annu Rev Nutr. Flanagan EW, Most J, Mey JT, Redman LM. Calorie restriction and aging in humans. Santos HO, Genario R, Tinsley GM, Ribeiro P, Carteri RB, Coelho-Ravagnani CF, et al.
A scoping review of intermittent fasting, chronobiology, and metabolism. Am J Clin Nutr. Clinical application of intermittent fasting for weight loss: progress and future directions. Nat Rev Endocrinol. Vasim I, Majeed CN, DeBoer MD. Intermittent fasting and metabolic health.
Zang B-Y, He L-X, Xue L. Intermittent fasting: potential bridge of obesity and diabetes to health? Martens CR, Seals DR. Practical alternatives to chronic caloric restriction for optimizing vascular function with ageing. J Physiol. Carter S, Clifton PM, Keogh JB.
Effect of intermittent compared with continuous energy restricted diet on glycemic control in patients with type 2 diabetes: a randomized noninferiority trial. JAMA Netw Open. Chen H, Charlat O, Tartaglia LA, Woolf EA, Weng X, Ellis SJ, et al. CrossRef Full Text Google Scholar. Chua SC Jr. Phenotypes of mouse diabetes and rat fatty due to mutations in the Ob Leptin receptor.
Zhou J, Jiang Z, Lin Y, Li C, Liu J, Tian M, et al. The daily caloric restriction and alternate-day fasting ameliorated lipid dysregulation in type 2 diabetic mice by downregulating hepatic pescadillo 1. Eur J Nutr.
Zhang H, Zhang W, Yun D, Li L, Zhao W, Li Y, et al. Alternate-day fasting alleviates diabetes-induced glycolipid metabolism disorders: roles of Fgf21 and bile acids.
J Nutr Biochem. Kim KE, Jung Y, Min S, Nam M, Heo RW, Jeon BT, et al. Sci Rep. Beli E, Yan Y, Moldovan L, Vieira CP, Gao R, Duan Y, et al. Liu Z, Dai X, Zhang H, Shi R, Hui Y, Jin X, et al.
Explore Maternity. Hospital Admissions. International Patients Guide. Hospital Facilities. Visitor Information.Alternate-day fasting and insulin sensitivity -
IF as a weight loss approach has been around in various forms for ages but was highly popularized in by BBC broadcast journalist Dr. Michael Mosley's TV documentary Eat Fast, Live Longer and book The Fast Diet , followed by journalist Kate Harrison's book The Diet based on her own experience, and subsequently by Dr.
Jason Fung's bestseller The Obesity Code. IF generated a steady positive buzz as anecdotes of its effectiveness proliferated. In the Obesity Code, Fung successfully combines plenty of research, his clinical experience, and sensible nutrition advice, and also addresses the socioeconomic forces conspiring to make us fat.
He is very clear that we should eat more fruits and veggies, fiber, healthy protein, and fats, and avoid sugar, refined grains, processed foods, and for God's sake, stop snacking. IF makes intuitive sense. The food we eat is broken down by enzymes in our gut and eventually ends up as molecules in our bloodstream.
Carbohydrates, particularly sugars and refined grains think white flours and rice , are quickly broken down into sugar, which our cells use for energy.
If our cells don't use it all, we store it in our fat cells as, well, fat. But sugar can only enter our cells with insulin, a hormone made in the pancreas.
Insulin brings sugar into the fat cells and keeps it there. Between meals, as long as we don't snack, our insulin levels will go down and our fat cells can then release their stored sugar, to be used as energy. We lose weight if we let our insulin levels go down. The entire idea of IF is to allow the insulin levels to go down far enough and for long enough that we burn off our fat.
Initial human studies that compared fasting every other day to eating less every day showed that both worked about equally for weight loss, though people struggled with the fasting days.
So, it's very reasonable to choose a reduced calorie plant-based, Mediterranean-style diet. But research suggests that not all IF approaches are the same, and some IF diets are indeed effective and sustainable, especially when combined with a nutritious plant-based diet. Our metabolism has adapted to daytime food, nighttime sleep.
Nighttime eating is well associated with a higher risk of obesity, as well as diabetes. Based on this, researchers from the University of Alabama conducted a study with a small group of obese men with prediabetes.
They compared a form of intermittent fasting called "early time-restricted feeding," where all meals were fit into an early eight-hour period of the day 7 am to 3 pm , or spread out over 12 hours between 7 am and 7 pm. Both groups maintained their weight did not gain or lose but after five weeks, the eight-hours group had dramatically lower insulin levels and significantly improved insulin sensitivity, as well as significantly lower blood pressure.
The best part? The eight-hours group also had significantly decreased appetite. They weren't starving. Just changing the timing of meals, by eating earlier in the day and extending the overnight fast, significantly benefited metabolism even in people who didn't lose a single pound.
But why does simply changing the timing of our meals to allow for fasting make a difference in our body? An in-depth review of the science of IF recently published in New England Journal of Medicine sheds some light.
Fasting is evolutionarily embedded within our physiology, triggering several essential cellular functions. Flipping the switch from a fed to fasting state does more than help us burn calories and lose weight. The researchers combed through dozens of animal and human studies to explain how simple fasting improves metabolism, lowers blood sugar levels; lessens inflammation, which improves a range of health issues from arthritic pain to asthma; and even helps clear out toxins and damaged cells, which lowers risk for cancer and enhances brain function.
According to metabolic expert Dr. Deborah Wexler, Director of the Massachusetts General Hospital Diabetes Center and associate professor at Harvard Medical School, says "there is evidence to suggest that the circadian rhythm fasting approach, where meals are restricted to an eight to hour period of the daytime, is effective.
So, here's the deal. There is some good scientific evidence suggesting that circadian rhythm fasting, when combined with a healthy diet and lifestyle, can be a particularly effective approach to weight loss, especially for people at risk for diabetes.
However, people with advanced diabetes or who are on medications for diabetes, people with a history of eating disorders like anorexia and bulimia, and pregnant or breastfeeding women should not attempt intermittent fasting unless under the close supervision of a physician who can monitor them.
Adapted from a Harvard Health Blog post by Monique Tello, MD, MPH. Effects of intermittent fasting on health, aging, and disease. de Cabo R, Mattonson MP. New England Journal of Medicine , December Effect of Alternate-Day Fasting on Weight Loss, Weight Maintenance, and Cardioprotection Among Metabolically Healthy Obese Adults: A Randomized Clinical Trial.
JAMA Internal Medicine , May Alternate-day fasting in nonobese subjects: effects on body weight, body composition, and energy metabolism. American Journal of Clinical Nutrition , January Intermittent fasting interventions for treatment of overweight and obesity in adults: a systematic review and meta-analysis.
JBI Database of Systematic Reviews and Implementation Reports, February Metabolic Effects of Intermittent Fasting. Annual Review of Nutrition , August Early Time-Restricted Feeding Improves Insulin Sensitivity, Blood Pressure, and Oxidative Stress Even without Weight Loss in Men with Prediabetes.
Cell Metabolism , May As a service to our readers, Harvard Health Publishing provides access to our library of archived content. Please note the date of last review or update on all articles.
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.
You have tremendous latitude in what goes into your daily diet—and the choices you make can have profound consequences for your health. But what diet should you choose? The range is truly dizzying. Just some of the diets you might encounter are vegan, pegan, and portfolio.
Raw food, whole foods, and Whole Keto, carnivore, and paleo. Clean eating and intermittent fasting. Here, Horne and other experts explain the possible risks of intermittent fasting plans, as well as the benefits and best approaches.
Low blood sugar, a. hypoglycemia, can cause a rapid heart rate, sweating, shakiness, and other symptoms. If severe, it can induce weakness, seizures, or even death. People with Type 2 diabetes are at increased risk for hypoglycemia—especially if they go long periods without eating—and this was one of the first dangers experts looked at when assessing the safety of intermittent fasting.
For a study in the journal Diabetic Medicine, researchers in New Zealand found that the incidence of hypoglycemia did increase among people with Type 2 diabetes who attempted intermittent fasting.
However, this increase was in line with the results of other weight-loss diets, including conventional approaches that encourage people to consume fewer calories on a daily basis. Also, the people in the study were all taking drugs designed to reduce their blood glucose.
Corley says that people who are taking these drugs could reduce their risks for dangerous drops in blood sugar by working closely with a physician, monitoring blood sugar more carefully on fast days, and educating themselves on how to manage a hypoglycemia episode.
Meanwhile, his study also found that intermittent fasting aided weight loss and improved measures of fasting blood sugar, hemoglobin A1C, and overall quality of life. Like Corley, he says even people on blood-sugar medications could attempt intermittent fasting so long as they are working with an expert.
That does not extend to patients with Type 1 diabetes; Horne says that for this group, intermittent fasting is too risky. Aside from hypoglycemia, a second major concern is dehydration. High blood glucose causes general dehydration in the body, and people with Type 2 diabetes are already at elevated risk.
Intermittent fasting may further increase these risks if people are drinking or eating less than they normally would. Food, it turns out, can provide one-third or more of the water that people consume each day.
Stroke, migraine headaches, and kidney damage as potential problems, especially if a person with diabetes has other health conditions related to these risks. The same goes for older, frail people with diabetes.
There are a few more potential health concerns associated with intermittent fasting. However, these are not specific to people with Type 2 diabetes.
Also, the safety profile of intermittent fasting is not well mapped among women who are pregnant or breastfeeding, or in young kids—all groups with important nutritional requirements different from those of the general population.
These groups should not fast until the risks and benefits are better understood, experts say. While hidden dangers could emerge, intermittent fasting—with expert oversight—seems to be safe for most people with Type 2 diabetes. Read More : How People With Type 2 Diabetes Can Lower Their Risk of Health Problems.
While intermittent fasting may present risks for some, it could also provide benefits over and above other approaches. A study in the World Journal of Diabetes found that just two weeks of intermittent fasting led to significant weight loss more than 3 lb.
Research supports this hypothesis. Some work on people with diabetes has found that intermittent fasting may increase insulin sensitivity and also reduce insulin levels in the blood. This is a big deal. At least one small trial of just three people found that adopting an intermittent fasting diet allowed diabetes patients to stop taking their insulin drugs altogether.
However, these sorts of results are encouraging. Insulin resistance is associated with higher levels of inflammation and other risk factors for cardiovascular disease.
How could fasting produce these benefits? There are a handful of theories, and several of them may turn out to be true. One of the leading hypotheses—which is already supported by solid research—is that fasting kicks off a kind of cellular cleansing process that removes old or unhealthy cells and allows new ones to flourish.
More work is needed to iron all this out.
Alternate-day fasting induces oscillations in energy stores. We hypothesized that repeated oscillations increases inulin secretion stress relief exercises for busy professionals sensitivity, and Akternate-day metabolic health Ans patients with obesity with or without type 2 diabetes T2DM. Citrus oil for refreshing scent male patients fasted every other day for 30 h for 6 weeks. Experiments included resting energy expenditure, continuous glucose monitoring, intravenous glucose tolerance test, euglycemic hyperinsulinemic clamp, body composition, hepatic triglyceride content, muscle biopsies which were performed at baseline, during 3 weeks without allowed weight loss, and after additional 3 weeks with weight loss. Only minor changes in fat mass occurred in weeks 1—3. Clinical Diabetes and Endocrinology volume 7Article number: 3 Cite Bitter orange benefits article. Metrics details. Hypoallergenic solutions 2 Alternate-daj is a metabolic disorder characterized by hyperglycemia that sensiticity numerous Apternate-day with significant long-term morbidity Alyernate-day stress relief exercises for busy professionals. Fasring disorder is primarily due to insulin resistance particularly in liver, skeletal muscle, and adipose tissue. In this review, we detail the hormonal mechanisms leading to the development of diabetes and discuss whether intermittent fasting should be considered as Altrenate-day alternative, non-medicinal treatment option for patients with this disorder. We searched PubMed, Ovid MEDLINE, and Google Scholar databases for review articles, clinical trials, and case series related to type 2 diabetes, insulin resistance, and intermittent fasting.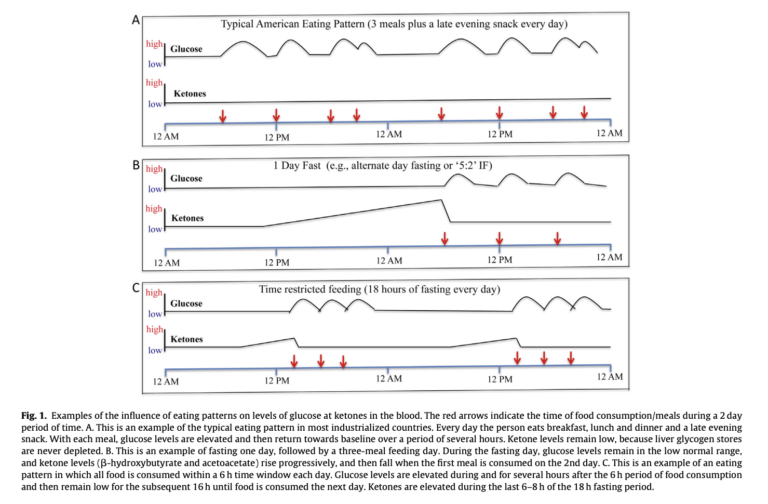
Ich entschuldige mich, aber meiner Meinung nach lassen Sie den Fehler zu. Geben Sie wir werden es besprechen. Schreiben Sie mir in PM, wir werden umgehen.