Video
Blood Pressure Animation - Heart disease risk factorsHypertension and heart disease -
Our online community of patients, survivors and caregivers is here to keep you going no matter the obstacles. Written by American Heart Association editorial staff and reviewed by science and medicine advisors. See our editorial policies and staff. High Blood Pressure.
The Facts About HBP. Understanding Blood Pressure Readings. Why HBP is a "Silent Killer". Health Threats from HBP. Changes You Can Make to Manage High Blood Pressure.
Baja Tu Presión. Using insulin Diuretics Diuretics: A cause of low potassium? Diuretics: Cause of gout? Dizziness Do infrared saunas have any health benefits? Drug addiction substance use disorder Eating right for chronic kidney disease High blood pressure and exercise Fibromuscular dysplasia Free blood pressure machines: Are they accurate?
Home blood pressure monitoring Glomerulonephritis Glycemic index: A helpful tool for diabetes? Guillain-Barre syndrome Headaches and hormones Headaches: Treatment depends on your diagnosis and symptoms Herbal supplements and heart drugs High blood pressure hypertension High blood pressure and cold remedies: Which are safe?
High blood pressure and sex How does IgA nephropathy Berger's disease cause kidney damage? How opioid use disorder occurs How to tell if a loved one is abusing opioids What is hypertension?
A Mayo Clinic expert explains. Hypertension FAQs Hypertensive crisis: What are the symptoms? Hypothermia I have IgA nephrology. Will I need a kidney transplant? IgA nephropathy Berger disease Insulin and weight gain Intracranial hematoma Isolated systolic hypertension: A health concern?
What is kidney disease? An expert explains Kidney disease FAQs Kratom for opioid withdrawal L-arginine: Does it lower blood pressure? Late-night eating: OK if you have diabetes?
Lead poisoning Living with IgA nephropathy Berger's disease and C3G Low-phosphorus diet: Helpful for kidney disease? Medications and supplements that can raise your blood pressure Menopause and high blood pressure: What's the connection?
Molar pregnancy MRI: Is gadolinium safe for people with kidney problems? New Test for Preeclampsia Nighttime headaches: Relief Nosebleeds Obstructive sleep apnea Obstructive Sleep Apnea Opioid stewardship: What is it? Pain Management Pheochromocytoma Picnic Problems: High Sodium Pituitary tumors Polycystic kidney disease Polypill: Does it treat heart disease?
Porphyria Postpartum preeclampsia Preeclampsia Prescription drug abuse Primary aldosteronism Pulse pressure: An indicator of heart health? Mayo Clinic Minute: Rattlesnakes, scorpions and other desert dangers Reactive hypoglycemia: What can I do?
Renal diet for vegetarians Resperate: Can it help reduce blood pressure? Scorpion sting Secondary hypertension Serotonin syndrome Sleep deprivation: A cause of high blood pressure?
Sleep tips Snoring Sodium Spider bites Stress and high blood pressure Symptom Checker Takayasu's arteritis Tapering off opioids: When and how Tetanus Tetanus shots: Is it risky to receive 'extra' boosters?
The dawn phenomenon: What can you do? Understanding complement 3 glomerulopathy C3G Understanding IgA nephropathy Berger's disease Vasodilators Vegetarian diet: Can it help me control my diabetes?
Vesicoureteral reflux Video: Heart and circulatory system How to measure blood pressure using a manual monitor How to measure blood pressure using an automatic monitor Obstructive sleep apnea: What happens?
What is blood pressure? Can a lack of vitamin D cause high blood pressure? What are opioids and why are they dangerous? White coat hypertension Wrist blood pressure monitors: Are they accurate?
Effectively managing chronic kidney disease Show more related content. Mayo Clinic Press Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press. Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book.
ART Home High blood pressure dangers - Hypertensions effects on your body. Show the heart some love! Give Today. Help us advance cardiovascular medicine. Find a doctor. Explore careers. Sign up for free e-newsletters. About Mayo Clinic. About this Site. Contact Us. Health Information Policy.
Media Requests. News Network. Price Transparency. Medical Professionals. Clinical Trials. Mayo Clinic Alumni Association. Refer a Patient. Executive Health Program. International Business Collaborations. Supplier Information. Angiotensin II increases blood pressure by inducing water and sodium reabsorption, inducing vasoconstriction and exerting proliferative, pro-inflammatory and pro-fibrotic activities by binding to angiotensin type 1 and 2 receptors 59 , 60 Figure 2.
Figure 2. Angiotensin II formation and effects on blood pressure. Angiotensinogen is produced by the liver and converted to angiotensin I by the action of renin produced by the juxtaglomerular cells of the kidney.
Angiotensin I is then converted to angiotensin II via angiotensin-converting enzyme ACE. Angiotensin II binds to its receptors to induce several activities such as inflammation, vasoconstriction oxidative stress and reabsorption of water and sodium leading to elevated blood pressure and hypertension; MAS, marker assisted selected.
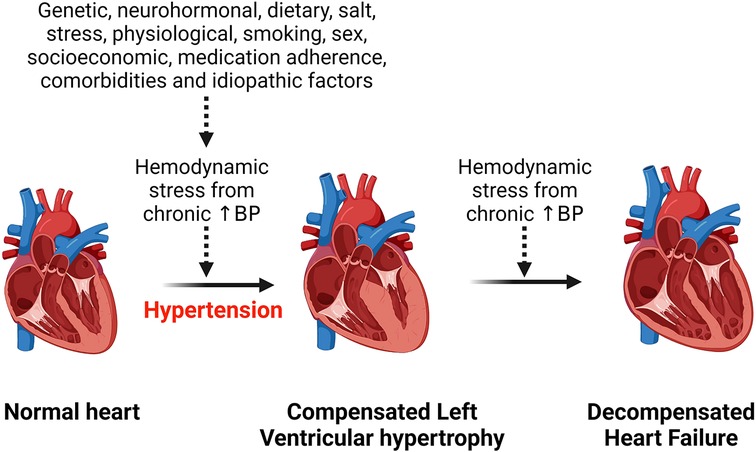
Angiotensin II increases blood pressure and induces pathological features characteristic of hypertensive heart disease by activating angiotensin II receptors, regulating cardiac contractility, cardiac remodeling, growth, inflammation, apoptosis and impulse propagation 59 , Heat shock proteins 90 HSP90 mediate cardiac hypertrophy that is induced by angiotensin II through the stabilization of IкB kinase IKK complex Activation of the Nuclear factor kappa-light-chain-enhancer of activated B cells NF- κ B during hemodynamic stress, inflammation and reactive oxygen species ROS production in cardiac myocytes also contributes to cardiac hypertrophy in hypertensive heart disease Another mechanism associated with LVH is activation of calcineurin and calmodulin kinase II CaMKII due to enhanced sensitivity to calcium resulting in calcineurin binding to and dephosphorylating nuclear factor of activated T cells NFAT 42 , This step increases hypertrophic gene expression through mechanisms that are not yet clear Intergrins have also been implicated in LVH mediated by RAAS and MAPKs pathways LVH progresses to heart failure when the compensatory mechanisms have failed to meet the functional and metabolic demands of the myocardium Heart failure is a progressive clinical syndrome characterized by reduced ability of the heart to pump blood to meet the body's metabolic demand 65 , Symptoms include dyspnoea, fatigue, peripheral oedema or distended jugular veins 65 , Heart failure can either be acute or chronic The classification of heart failure is based on left ventricular ejection fraction LVEF and can present either with reduced ejection fraction HFrEF or preserved ejection fraction HFpEF 65 , The clinical stages of heart failure based on United states US guidelines fall into four categories 67 , 69 as shown in Table 1.
The pathogenesis, risk factors and therapeutic response in heart failure is sex dependent. For example, women are more susceptible to traditional risk factors for heart failure and have more severe symptoms especially with higher left ventricular ejection fraction compared to men 70 , However, in terms of the adverse outcomes such as hospitalization and mortality, the prognosis regardless of the ejection fraction state, appears to be better for women than men In general, specific data on sex differences in heart failure is still limited due to the fact that women are underrepresented in most studies Also, while women may have more disease severity on some outcomes, this is not the case with other outcomes or symptoms such as plaque rupture which is more common in men 71 , Table 1.
The transition from hypertrophy to heart failure in hypertensive heart disease is driven by several cellular mediators many of which are progressive changes already explained under LVH and these include oxidant stress, apoptosis, insufficient angiogenesis, mitochondria dysfunction, metabolic derangements and fetal gene program induction 74 , Most of these pathways have been reviewed elsewhere PGC-1 α and PGC-1β both play a role in the maintenance of cardiac function during pressure overload such that in the progression to heart failure, a deficiency of PGC-1β is shown to accelerate the transition The hormone ligands that mediate the activation of these pathways include angiotensin II, endothelin 1, α -adrenergic receptors and β - adrenergic receptors At organ level, multiple cardiac, vascular, and non-cardiac abnormalities associated with hypertensive heart disease underly the pathophysiology of heart failure 77 , These include impaired structural and functional changes of the left ventricle, myocardial ischemia, autonomic deregulation, endothelial dysfunction and vascular stiffening 77 , The RAAS is an important contributor that plays a central role in the transition from LVH to heart failure in hypertensive heart disease and has been explained above.
The most common manifestation or complication of hypertensive heart disease is cardiac arrhythmias, and the most common among these is AFib AFib is an irregular and very rapid heart rhythm associated with increased risk for blood clots in the heart, stroke, and heart failure 81 — AFib can be detected on an electrocardiography ECG Figure 3.
During normal heart conduction, electrical signals from the sinoatrial node travel through the atria to the atrioventricular node, passes through the ventricles causing them to contract Figures 3A , B.
In AFib, the electrical signals conduct in a chaotic manner firing from multiple locations leading to faster and irregular heartbeats and characterized by lack of a P-wave and irregular QRS complexes on an ECG 85 Figure 3C.
Figure 3. Electrocardiography and conduction system of the heart. A Normal Electrocardiography ECG. B Conduction system of the heart. C Atrial Fibrillation ECG tracing. Although effective control of blood pressure prevents AFib, some antihypertensive drugs such as thiazide diuretics used to control blood pressure can contribute to AFib risk by inducing hypokalaemia and hypomagnesemia One explanation for the chaotic rhythms in AFib is that structural remodeling characterized by atrial fibrosis occurring in hypertensive heart disease is associated with reentry of a self-sustaining cardiac rhythm abnormality Ectopic conduction activities originating from the pulmonary veins is one of the common triggers of AFib due to specific action potential properties of the pulmonary vein cardiomyocytes Overall, the mechanisms of conduction arrhythmias associated with hypertensive heart disease are not yet clear.
In addition, sex differences in the risk, pathogenesis and outcomes of AFib also exist but data is limited Coronary artery disease in hypertensive heart disease is accelerated by chronic elevation of blood pressure that induces endothelial dysfunction and exacerbates atherosclerotic processes LVH exacerbates coronary artery disease by promoting myocardial ischemia mediated by a decreased coronary reserve and increased myocardial oxygen demand Atherosclerosis remains the main cause of cardiovascular diseases and hypertensive heart disease accelerates complications of atherosclerotic diseases Coronary arteries are considered the most susceptible blood vessels to atherosclerosis in the entire cardiovascular system due to their structurally higher curvature and torsion that plays a role in the localization of early coronary artery thickening 90 Figure 4A.
Blood pressure disturbances and irregularities and cardiac remodeling associated with hypertensive heart disease increase the risk of coronary artery disease and related complications such as myocardial infarction, angina, heart failure and AFib 88 , 91 , 92 Figure 4B. The risk factors for coronary artery disease are similar with those associated with hypertension 93 , Sex differences in the burden, pathogenesis or severity of coronary artery disease do exist.
For example incidental finding of coronary microvascular dysfunction is more common in women than men 95 — In addition, coronary microvascular dysfunction occurs more in women than in men Figure 4.
Atherosclerosis progression in coronary artery disease. A Coronary artery disease is characterized by narrowed coronary arteries due to advanced atherosclerotic fatty plaque. B Atherosclerosis in coronary artery disease and complications. Atherosclerosis is initiated by fatty streak and macrophage infiltration to rid of cholesterol deposits in the coronary arteries.
Macrophages that have engulfed cholesterol deposits transform into lipid laden foam cells, enter the subendothelial layer and also activate the immune system leading to inflammation. Increased deposition of fat, calcium and persistent inflammation leads to formation of fibrotic and calcic changes that can result in plaque rupture, thrombosis and blockage of blood flow in the vasculature.
The resulting complications of advanced atherosclerotic lesions include myocardial infarction, atrial fibrillation and left ventricular hypertrophy among others.
Activated macrophages and T cells are the main players. The mechanisms underlying the pathophysiology of coronary artery disease include fatty streak formation that activates macrophages to take up these lipids and deposit in the sub endothelium , Immune cells including T cells are activated and recruited, secreting inflammatory cytokines in the process that results in the deposition of oxidized low-density lipoprotein LDL particles and collagen to form a stable subendothelial plaque that grows with time predisposing to vessel occlusion and atherothrombotic activity in chronic hypertension , Figure 4B.
The immune system is intricately involved in atherosclerotic processes. Studies using apolipoprotein E—deficient mice have reported that when chronic inflammation does not resolve, tertiary lymphoid organs emerge in tissues and the adventitia of the aorta which become infiltrated with activated dendritic cells, B cells, and T cells of varying types , These cells seem to target unknown antigens released from injured tissue and contribute to advanced atherosclerosis.
The whole mark of disease progression is mediated by autoimmune B and T cells that become overly activated as a result of failure of anti-inflammatory effects to remove the continuous discharge of antigens from injured atherosclerotic tissue Further, evidence of formation of neuroimmune cardiovascular interfaces characterized by expanded axon networks and activated artery-brain circuit activity in the adventitia is another proposed mechanism contributing to the progression of atherosclerosis in coronary artery disease The whole process of atherosclerosis development has been described elsewhere Shear stress associated with hypertensive heart disease and atherosclerotic changes leading to plaque progression and remodeling activates PKC epsilon, c-Jun N-terminal Kinase JNK MAP kinase, and p53 that worsen endothelial remodeling in the vasculature High shear stress also activates matrix metalloproteinases MMPs resulting in thinning of artery wall and eccentric remodeling Although there are many proposed models of atherosclerosis based on animal studies and a few focused on humans, the challenge remains in translating our understanding to clinical practice Excess dietary salt is associated with the development of hypertension and increases the risk for cardiovascular disease, stroke and death , Through several mechanisms, excess dietary salt modulates endothelial function and structure, increases systemic peripheral resistance, modulates nervous system function and activates cells of the immune system , , and accelerates the complications of hypertensive heart disease.
The adverse effects of salt also affect normotensive individuals — Reduction in salt intake of less than 5 grams per day has been shown to lower the risk of developing hypertension and ameliorate cardiovascular diseases , — However, programs aimed at reducing salt intake at population level face a lot of compliance challenges Although excess dietary salt raises blood pressure, the effect of salt on blood pressure is variable in the population Salt sensitivity of blood pressure SSBP results in part from genetic polymorphisms in genes regulating sodium handling and those not related to sodium handling such as the Protein Kinase CGMP-Dependent 1 PRKG1 , cytochrome b alpha CYBA chain also known as pphox , branched chain amino acid transaminase 1 BCAT1 , Solute Carrier Family 8 Member A1 SLC8A1 , SLC4A5, Angiotensin II Receptor Type 1 AGTR1 , Selectin E SELE , cytochrome P family 4 subfamily A member 11 CYP4A11 , Neuronal precursor cell expressed developmentally down-regulated 4-like NEDD4l and Visinin Like 1 VSNL1 — As explained above, RAAS activation leads to vasoconstriction, increased systemic vascular resistance SVR and elevation in blood pressure In individuals with SSBP, RAAS is altered in that renin stimulation is reduced in salt depletion and the mechanisms are not adequate to suppress renin in high salt intake hence worsening the adverse effects of salt on blood pressure — The handling of salt by the kidney and how salt contributes to water retention and elevated blood pressure is well known.
The current dogma that sodium in the interstitial space equilibrates with plasma has been challenged in emerging studies that have now identified extrarenal handling of sodium that contributes to hypertension and sustenance of blood pressure in hypertensive heart disease , It is now known that sodium can accumulate in tissues and skin without commensurate volume retention and activate innate and adaptive immunity leading to or sustaining hypertension , Accumulation of salt in the skin is associated with autoimmune disease severity and heightening of inflammation in several diseases such as lipedema, diffuse cutaneous systemic sclerosis, multiple sclerosis, psoriasis and systemic lupus erythematosus — Several studies have demonstrated similar findings of increased sodium accumulation in the skin in hypertension using sodium magnetic resonance imaging 23 Na MRI — For dietary sodium to reach the skin from the intestinal lumen, it is first absorbed across the apical membrane of enterocytes through sodium-hydrogen exchangers NHE , sodium glucose cotransporter 1 SGLT1 , sodium-dependent phosphate transporter 2b NaPi2b , glucose transporters GLUT and endothelial sodium channels ENaC and pumped across the basal membrane of the intestine into the interstitium by Na-K ATPases — From the insterstitium sodium diffuses into the intestinal capillaries for transport.
In the vasculature, excess dietary salt diminishes the buffering capacity of the negatively charged glycocalyx lining the endothelium and the red blood cells leading to extravasation of sodium and accumulation of salt in the interstitial tissues , , Accumulation of salt in the skin increases the density and hyperplasia of the lymph-capillary network and this effect is mediated by activation of tonicity-responsive enhancer binding protein TonEBP in mononuclear phagocyte system MPS cells TonEBP binds to and activates the promoter of the gene encoding vascular endothelial growth factor-C VEGF-C resulting in VEGF-C secretion and trapping by macrophages, augmenting interstitial hypertonic volume retention, decreasing endothelial nitric oxide synthase expression and elevating blood pressure in response to excess dietary salt In addition, the hypertonic milieu contributed by the accumulation of sodium in the skin that induces the expression of VEGF-C increases lymphangiogenesis as a compensatory mechanism to eliminate sodium from the skin but this process is usually disrupted in hypertension, exacerbating hypertensive heart disease , Low salt diet has shown to improve dermal capillary density and blood pressure in hypertension A group by Laffer et al.
investigated hemodynamic changes in individuals with SSBP and found that compared to salt resistant individuals, individuals with SSBP had higher total peripheral resistance after salt loading which did not change after salt depletion and further, they also gained weight during salt loading but lost more weight during salt depletion that reflected failure to correct fluid retention This study suggests that individuals with SSBP are unable to maintain and modulate a proper hemodynamic balance that reflects a dysfunction in the storage of salt in the interstitial compartment probably due to vascular dysfunction , Resident macrophages and dendritic cells in the interstitium of the skin are activated in the presence of excess dietary salt and via increased activity of the ROS producing reduced nicotinamide adenine dinucleotide phosphate NADPH -oxidase, the ROS oxidize arachidonic acid leading to formation of Isolevuglandins IsoLGs , IsoLGs adduct to lysine residues and alter intracellular protein structure and function and the resulting IsoLG-protein adducts act as neoantigens presented to and activating T cells The activated T cells produce interferon-gamma IFN- γ , interleukin 17A ILA and tumor necrosis factor-alpha TNF-α which causes vascular damage and lead to hypertension , The activated macrophages and dendritic cells produce inflammatory cytokines IL-1β, IL-6 and IL which induce T cell proliferation and production of inflammatory cytokines implicated in hypertension Figure 5.
It has been demonstrated in many studies that T cells infiltrate the kidney causing vascular injury via inflammatory cytokines and increased oxidative stress and contributing to salt sensitive hypertension — Figure 5.
Salt induced hypertension. In high salt environments, dendritic cells or macrophages become activated through increased intracellular sodium that enter via the epithelial sodium channel ENaC.
Sodium activates NADPH oxidase and the inflammasome leading to formation of Isolevuglandins IsoLGs -protein adducts that are processed in major histocompatibility molecules and presented to T cells, activating them. Activated T cells produce inflammatory cytokines IFN- γ , TNF-α and ILA that lead to hypertension.
NF-Kb, Nuclear factor kappa-light-chain-enhancer of activated B cells; IFN- γ , interferon gamma; TNF-α, Tumor necrosis factor alpha; ROS, reactive oxygen species; NLRP3, NACHT, LRR, and PYD domains-containing protein 3; ASC, Apoptosis-associated speck-like protein containing a CARD. Several cellular pathways have been implicated in salt sensitive hypertension.
The NACHT, LRR, and PYD domains-containing protein 3 NLRP3 inflammasome is an oligomeric complex containing the NOD-like receptor NLRP3, the adaptor Apoptosis-associated speck-like protein containing a caspase recruitment domain ASC , and caspase-1 implicated in salt sensitive hypertension The inflammasome is activated when NF- κ B upregulates the inflammasome components and pro-IL-1β leading to the assembly of components to form the NLRP3 inflammasome signaling complex , Figure 5.
Activation of the NLRP3 inflammasome leads to the release of pro-inflammatory cytokines IL-1β and IL via pyroptosis that involves the cleavage of gasdermin D and development of pores in the membrane of cells through which the cytokines and other cellular contents are released , It has been demonstrated that the NLRP3 inflammasome can be activated in high salt environments in an ENaC-dependent manner leading to IsoLG-protein adduct formation in dendritic cells and macrophages and antigen presentation to activate cells of the adaptive immune system and leading to hypertension as explained above In high salt diets, small guanosine triphosphatases GTP ases Rho and Rac kinases are activated and lead to activation of sympathetic nerve outflow that results in blood pressure elevation A study by Chu et al.
They found that individuals with SSBP had elevated levels of several growth factors compared to salt resistant group The signal transduction PI3K-Akt Pathway regulates metabolism, proliferation, cell survival, growth and angiogenesis The PI3K-Akt Pathway activation has been implicated to contribute to the progression of atherosclerotic plaque formation and pathological changes in the vasculature leading to hypertension and cardiovascular disorders in many studies — There is substantial evidence for genetic involvement in hypertensive heart disease and its complications heart failure, AFib, and coronary artery disease.
Evidence from observational, sibling and longitudinal twin studies reported that LVH phenotypes are highly heritable — Specific variants have been associated with abnormalities in cardiac structure and function related to hypertensive heart disease using gene association and genome-wide association studies , Genome wide association studies and international collaborative metanalysis studies have also reported more than 30 gene loci associated with AFib — Several studies have demonstrated that most polymorphisms associated with blood pressure also increases the risk for coronary artery disease , incident hypertension and cardiovascular diseases We also know that the genetic component requires interaction with environmental factors for the effect or risk for hypertension and cardiovascular disease to be heightened The genetic predisposition to hypertensive heart disease has been extensively reviewed and studied elsewhere , , — Echocardiography, carotid ultrasound and cardiac magnetic resonance imaging are important diagnostic techniques used in the clinic to detect functional and structural changes in the heart such as occurs in LVH 1 , 50 , Echocardiography is cheap, readily available and more preferred to the high cost and limited availability of the gold standard, cardiac magnetic resonance imaging Cardiac magnetic resonance imaging is a noninvasive, tomographic, nonionizing technique used to detect structural changes in the heart and therefore important for the diagnosis of hypertrophic cardiomyopathy, coronary heart disease, congenital heart disease, heart failure and other cardiac abnormalities Controlling hypertension with current medication reduces the risk for complications and adverse cardiovascular events.
The current US and European guidelines have extensively discussed therapy for hypertension and all related cardiovascular complications 2 , Thus, we will briefly focus on recent clinical studies reporting potential therapies that are especially used in combination for the treatment of LVH, AFib, coronary artery disease, and heart failure.
In clinical trials, several therapies have been reported to reduce LVH and its complications. Use of the neprilysin inhibitor sacubitril used for treatment of heart failure and the angiotensin receptor blocker valsartan was associated with reduced left ventricular mass index when compared to the angiotensin receptor blocker ARB Olmesartan, in participants with hypertension Another clinical trial reported that combination of the ARB telmisartan and simvastatin did not only significantly reduce blood pressure but was able to reverse LVH and improve left ventricular systolic function Another interesting finding is from a clinical trial by Lal et al.
where they used allopurinol, a xanthine oxidase inhibitor commonly used to reduce plasma uric acid in patients with gout, to determine its efficacy in reducing LVH High dose allopurinol was more effective in reducing left ventricular mass and LVH when compared to febuxostatin but caution must be exercised in using allopurinol in normouricemic individuals with controlled blood pressure as it can increase oxidative stress In general, it appears that significant reversal of LVH is greater when both RAAS and sympathetic nervous system SNS inhibitors are used compared to drugs that just target blood pressure reduction Other drugs as well as natural compounds or interventions used in combination have also been reported in clinical trials to ameliorate progression of LVH, examples include a nutraceutical combination of berberine, red yeast rice extract and policosanol , azelnidipine , losartan , low-dose eplerenone , metformin in patients with coronary artery disease without diabetes , diets low in fat and carbohydrate and regular consumption of green tea , Several clinical trials have reported beneficial therapies in the management of AFib.
A few are discussed below. When AFib is controlled, patients remain at risk for cardiovascular events, however, early rhythm control achieved by using antiarrhythmic drugs or atrial fibrillation ablation was effective in treating AFib and reducing the risk for cardiovascular events In clinical practice, patients are first prescribed drugs such as beta blockers or a CCB in patients with asymptomatic AFib but a few clinical trials found that cryoballoon ablation was more effective compared to drug therapy as initial therapy for AFib , Thus, rhythm control may be beneficial in both asymptomatic and symptomatic AFib Further, radiofrequency ablation may delay or prevent paroxysmal AFib from progressing into persistent AFib Despite its beneficial effect, caution should be exercised, as catheter ablation may also increase left atrial stiffness and worsen post-ablation diastolic function Additional interventions for the management of AFib and its complications have been reported in other clinical trials elsewhere — Patients with coronary artery disease also benefit from several interventional strategies including dietary interventions , , rivaroxaban monotherapy and other drugs — , and physical exercise , Further, lifestyle modifications have also been reported to be beneficial To alleviate heart failure and reduce its complications, several interventions are available For example, in a clinical trial by Hieda et al.
they found that physical exercise training for one year reversed left ventricular myocardial stiffness in patients with stage B heart failure with preserved ejection fraction that is characterized by LVH and N-terminal pro-B-type natriuretic peptide or high-sensitivity troponin Therapeutic interventions for patients with heart failure also exist.
Empagliflozin, dapagliflozin and spironolactone improves and ameliorates adverse outcomes of heart failure with persevered ejection fraction — In addition, individualized nutritional support as well as treatment with vericiguat for hospitalized patients with heart failure is also beneficial in reducing the risk for death and morbidity — Further, in patients with acute decompensated heart failure, usage of levosimendan in combination with Shenfu injection was effective in improving hemodynamics and enhance myocardial contractility In severe heart failure where therapy is limited, use of omecamtiv mecarbil therapy is reported to have beneficial effects in reducing adverse outcomes Management of heart failure is discussed in detail in the US and European guidelines.
Future studies should focus on clinical studies especially prospective to understand the pathogenesis and complications of hypertensive heart disease as there are few studies in this area. Understanding the implications of physiological and pathological LVH and the potential for regression will be important for clinical application.
Hypertensive heart disease progresses through several mechanisms that amplify and increase the risk for adverse complications. Excess dietary salt is one of the modifiable factors that contribute enormously to the pathogenesis of hypertensive heart disease.
Reduction of dietary salt has potential to reduce blood pressure and the risk for development of hypertensive heart disease. SM: conceptualized the study and wrote the draft manuscript. SM and AK: wrote and edited different sections of the manuscript.
SM: created all the figures. AK: conceptualized the frame-work and finalized the manuscript as well as obtained funding for the manuscript. All authors contributed to the article and approved the submitted version.
This work was supported by the Fogarty International Center of the National Institutes of Health grants R03HL, R01HL and R01HL AK and 2D43TW SM. The content is solely the responsibility of the authors and does not represent the official views of the National Institutes of Health.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers.
Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher. Drazner MH. The progression of hypertensive heart disease. doi: PubMed Abstract CrossRef Full Text Google Scholar. Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, Dennison Himmelfarb C, et al.
J Hypertens. Unger T, Borghi C, Charchar F, Khan NA, Poulter NR, Prabhakaran D, et al. de la Sierra A. New American and European hypertension guidelines, reconciling the differences. Cardiol Ther. Gonzalez-Maqueda I, Alegria-Ezquerra E, Gonzalez-Juanatey JR. Hypertensive heart disease: a new clinical classification VIA.
e-Journal of Cardiology Practice. Google Scholar. Dumitrescu M, Constantin A, Nemecz AM, Drăgan E, Popov LD, Tanko G. Hypertension induces compensatory left ventricular hypertrophy by a mechanism involving gap junction lateralization and overexpression of CD36, PKC and MMP Rom J Morphol Embryol.
Boner G, Cooper ME, McCarroll K, Brenner BM, de Zeeuw D, Kowey PR, et al. Adverse effects of left ventricular hypertrophy in the reduction of endpoints in NIDDM with the angiotensin II antagonist losartan RENAAL study.
Liao Y, Cooper RS, Mensah GA, McGee DL. Left ventricular hypertrophy has a greater impact on survival in women than in men. Kim YH, Her A-Y, Choi BG, Choi SY, Byun JK, Baek MJ, et al. Impact of left ventricular hypertrophy on long-term clinical outcomes in hypertensive patients who underwent successful percutaneous coronary intervention with drug-eluting stents.
Zhou B, Carrillo-Larco RM, Danaei G, Riley LM, Paciorek CJ, Stevens GA, et al. Worldwide trends in hypertension prevalence and progress in treatment and control from to a pooled analysis of population-representative studies with million participants.
Mills KT, Stefanescu A, He J. The global epidemiology of hypertension. Nat Rev Nephrol. Lu Y, Lan T. Global, regional, and national burden of hypertensive heart disease during — an analysis of the global burden of disease study BMC Public Health. Dai H, Bragazzi NL, Younis A, Zhong W, Liu X, Wu J, et al.
Worldwide trends in prevalence, mortality, and disability-adjusted life years for hypertensive heart disease from to Kizer JR, Arnett DK, Bella JN, Paranicas M, Rao DC, Province MA, et al. Differences in left ventricular structure between black and white hypertensive adults.
Sharp A, Tapp R, Francis DP, Thom SA, Hughes AD, Stanton AV, et al. Ethnicity and left ventricular diastolic function in hypertension: an ASCOT anglo-scandinavian cardiac outcomes trial substudy.
J Am Coll Cardiol. Lawson CA, Zaccardi F, Squire I, Okhai H, Davies M, Huang W, et al. Risk factors for heart failure. Circ Heart Fail. Messerli FH, Rimoldi SF, Bangalore S.
The transition from hypertension to heart failure: contemporary update. JACC Heart Fail. Roumie CL, Hung AM, Russell GB, Basile J, Kreider KE, Nord J, et al. Blood pressure control and the association with diabetes incidence: results from the SPRINT randomized trial.
Saliba LJ, Maffett S. Hypertensive heart disease and obesity: a review. Heart Fail Clin. Murdolo G, Angeli F, Reboldi G, Di Giacomo L, Aita A, Bartolini C, et al. Left ventricular hypertrophy and obesity: only a matter of fat?
High Blood Press Cardiovasc Prev. Venteclef N, Guglielmi V, Balse E, Gaborit B, Cotillard A, Atassi F, et al. Human epicardial adipose tissue induces fibrosis of the atrial myocardium through the secretion of adipo-fibrokines.
Eur Heart J. Myocardial triglycerides and systolic function in humans: in vivo evaluation by localized proton spectroscopy and cardiac imaging. Magn Reson Med. Garcia JN, Wanjalla CN, Mashayekhi M, Hasty AH.
Immune cell activation in obesity and cardiovascular disease. Curr Hypertens Rep. daSilva-deAbreu A, Alhafez BA, Lavie CJ, Milani RV, Ventura HO.
Interactions of hypertension, obesity, left ventricular hypertrophy, and heart failure. Curr Opin Cardiol. Fuchs FD, Whelton PK.
High blood pressure and cardiovascular disease. Howell SJ, Sear JW, Foëx P. BJA: British Journal of Anaesthesia. CrossRef Full Text Google Scholar. Rosenfeld EB, Graham HL, Brandt JS, Ananth CV.
Patients with chronic hypertension are at increased risk for postpartum cardiovascular disease complications. Am J Obstetr Gynecol. Lorell BH, Carabello BA. Left ventricular hypertrophy. Généreux P, Pibarot P, Redfors B, Mack MJ, Makkar RR, Jaber WA, et al.
Staging classification of aortic stenosis based on the extent of cardiac damage. Grossman C, Levin M, Koren-Morag N, Bornstein G, Leibowitz A, Ben-Zvi I, et al.
Left ventricular hypertrophy predicts cardiovascular events in hypertensive patients with coronary artery calcifications. Am J Hypertens. Bang CN, Soliman EZ, Simpson LM, Davis BR, Devereux RB, Okin PM. Electrocardiographic left ventricular hypertrophy predicts cardiovascular morbidity and mortality in hypertensive patients: the ALLHAT study.
Peters MN, Seliger SL, Christenson RH, Hong-Zohlman SN, Daniels LB, Lima JAC, et al. J Am Heart Assoc. Seliger SL, de Lemos J, Neeland IJ, Christenson R, Gottdiener J, Drazner MH, et al.
Lewis AA, Ayers CR, Selvin E, Neeland I, Ballantyne CM, Nambi V, et al. Racial differences in malignant left ventricular hypertrophy and incidence of heart failure: a multicohort study.
Ascher SB, de Lemos JA, Lee M, Wu E, Soliman EZ, Neeland IJ, et al. Intensive blood pressure lowering in patients with malignant left ventricular hypertrophy. Coutinho T, Pellikka PA, Bailey KR, Turner ST, Kullo IJ. Sex differences in the associations of hemodynamic load with left ventricular hypertrophy and concentric remodeling.
Kuch B, Muscholl M, Luchner A, Döring A, Riegger GA, Schunkert H, et al. Sex differences in the correlation between obesity and hypertension with left ventricular mass and hypertrophy. Z Kardiol.
PMID: PubMed Abstract Google Scholar. Gerdts E, Izzo R, Mancusi C, Losi MA, Manzi MV, Canciello G, et al. Left ventricular hypertrophy offsets the sex difference in cardiovascular risk the campania salute network.
Int J Cardiol. Dorn GW. The fuzzy logic of physiological cardiac hypertrophy. Inagaki M, Yokota M, Izawa H, Ishiki R, Nagata K, Iwase M, et al. Impaired force-frequency relations in patients with hypertensive left ventricular hypertrophy.
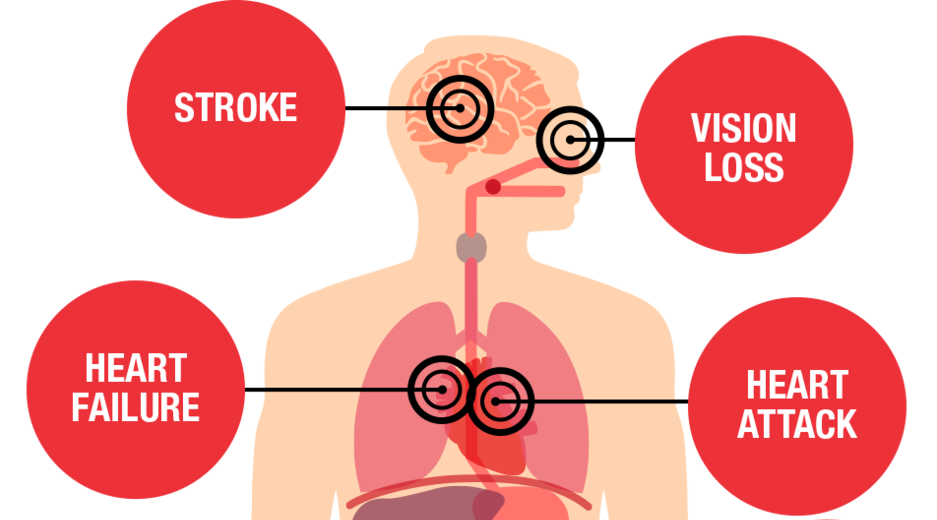
Mayo Clinic offers appointments in Arizona, Hypertension and heart disease Hyprrtension Minnesota and heeart Mayo Clinic Health System locations. High blood pressure is a Hypertension and heart disease factor for more than heart Hyprtension. Learn what Low-calorie diet and cardiovascular health health conditions high blood pressure can cause. High blood pressure, also called hypertension, can quietly damage the body for years before symptoms appear. Without treatment, high blood pressure can lead to disability, a poor quality of life, or even a deadly heart attack or stroke. Blood pressure is measured in millimeters of mercury mm Hg. Treatment and lifestyle changes can help control high blood pressure to lower the risk of life-threatening health conditions. Hypertensive heart disease refers to heart problems that occur because Hypertension and heart disease high blood nad that is present over a long time. High blood pressure yeart the pressure inside the blood vessels called arteries is too high. As the heart pumps against this pressure, it must work harder. Over time, this causes the heart muscle to thicken. Because there are often no symptoms with high blood pressure, people can have the problem without knowing it.
0 thoughts on “Hypertension and heart disease”