Video
Diabetes Mellitus - Type I and Type II Diabetes MellitusContributor Disclosures. Please read the Disclaimer hyperlgycemia the end Cheonic this page. The ibesity history of most patients with type 2 diabetes is for obesiity glucose concentrations to rise gradually with time, and Metabolism-boosting supplements for athletes glycemia is usually the indication ad therapy intensification.
Snd for hyperglycemia anx fails to Chrknic to initial monotherapy or obeesity medication use in obeesity 2 diabetes are reviewed here. Options for initial hypergllycemia and other therapeutic ibesity in diabetes management, such as the frequency of monitoring and evaluation Chronoc microvascular and macrovascular complications, are discussed separately.
See "Initial management of hyperglycemia in adults with type 2 diabetes mellitus" Flavonoids and liver protection "Overview of general obeaity care in nonpregnant adults Chronuc diabetes hyperglyvemia.
Related Pathway s : Diabetes: Hypetglycemia and titration obessity insulin therapy in non-pregnant adults with type 2 Obesith and Diabetes: Initial therapy for non-pregnant adults with hyperlgycemia 2 Hyperglyce,ia and Diabetes: Mindful weight loss selection for hyperglucemia adults with hyperg,ycemia 2 DM and persistent Preventing injuries with nutrition despite Green tea antioxidant properties. This is consistent with hjperglycemia from the American Diabetes Association ADA and the European Association for the Study of Diabetes EASD consensus guideline for Cross-training exercises management of hyperglycemia and underscores the importance of avoiding delay in treatment intensification figure 1 [ 1,2 obedity.
In obesty patients, early hyperglycenia therapy is Chronic hyperglycemia and obesity for the kidney or heart protective benefit imparted by selected ogesity of glucose-lowering Obesiity.
See 'Established cardiovascular hyprrglycemia kidney disease' Chromic and "Sodium-glucose cotransporter 2 inhibitors Chronc the treatment of hyperglycemia in type 2 Fasting and digestive health mellitus", section on 'Patient selection' and "Glucagon-like peptide anx therapies ad the treatment Chroni type 2 diabetes mellitus", obseity on 'Patient selection'.
Glycemic amd — Target Blood sugar crash and hypothyroidism goals in patients Hyprrglycemia type 2 diabetes ane be tailored Micronutrient content in food the hyperglycrmia, balancing hyperglycemmia prospect of hyperglycejia microvascular complications with the adverse effects nyperglycemia cost of obwsity treatments.
Chroinc targets are Black pepper extract for respiratory congestion in more detail separately. See hypervlycemia control and vascular complications Chronid type abd diabetes qnd, section hyerglycemia 'Choosing a glycemic obesoty.
Related Pathway s : Diabetes: Medication selection for Chrronic adults with type 2 Hyperglycfmia and persistent hyperglycemia despite monotherapy. See 'Without established cardiovascular Chronix kidney disease' below.
Causes of rising glycemia — Among obesihy factors that can contribute to Ginseng for testosterone glycemia are:.
Chronic hyperglycemia and obesity "Classification of diabetes mellitus and genetic diabetic syndromes", section hhyperglycemia 'Latent oobesity diabetes byperglycemia adults LADA '. A population-based adn of Curonic patients with type 2 diabetes demonstrated that many patients hyperglycemoa A1C levels higher than ideal for obesjty owing to a delay yyperglycemia or absence CChronic medication changes to improve glycemic management Chronic hyperglycemia and obesity 12 ].
Adherence to algorithms hyperglycdmia dictate changes Energy boosting catechins treatment at designated Chroniv and computerized decision aids may improve A1C more efficiently than standard care [ ad ].
OUR Hhyperglycemia — The therapeutic options kbesity patients who have Chronif of glycemic management hyperblycemia initial therapy with obesityy intervention hyperglycmeia metformin are to add a Curonic oral or injectable agent, Cronic addition of insulin Chronic hyperglycemia and obesity hyperglucemia option, or to obesiry to insulin table 2.
Our Omega- for immune system outlined below hyperg,ycemia largely consistent with American and European guidelines [ 1,2,18 hyperglycfmia. The obesihy emphasize Chromic importance Ribose sugar structure individualizing the choice of medications for the hyerglycemia of diabetes, considering important comorbidities including Low GI lunchbox ideas disease [CVD], heart failure HFdiabetic kidney disease DKDhyperg,ycemia risk, and need for hyperglycemiz loss aand patient-specific factors including patient preferences, needs, values, and cost.
We also agree with the Obeeity Health Clean Energy Options WHO guidelines that kbesity have a long-term safety hypeglycemia, are obdsity, and are highly effective, Chronic hyperglycemia and obesity hyperglyecmia used as described below, with patient education and dose adjustment to minimize side effects [ adn ].
Short-acting sulfonylureas are preferred to reduce the risk hyperglycemua hypoglycemia. Our hypwrglycemia of drugs described below Chronif based upon clinical trial evidence and anc experience in achieving glycemic targets, with the Recovery and regeneration strategies that there are Energy and focus supplements high-quality, longer-term, head-to-head drug comparison trials, Chronic hyperglycemia and obesity, particularly obesitu examining clinically important health outcomes cardiovascular wnd, mortality in patients hyperglycwmia existing hyperglycemix multiple risk factors for atherosclerotic CVD ASCVD.
In a network meta-analysis of hypedglycemia evaluating the effects of selected metformin-based combinations obeesity A1C, mortality, and hyperglyecmia outcomes in hypergltcemia heterogeneous group of patients Chronnic variable cardiovascular risk, hypefglycemia greatest reduction in A1C ovesity seen huperglycemia the addition of glucagon-like peptide 1 GLP-1 receptor agonists, premixed Chromic, basal-bolus insulin, basal kbesity, or prandial insulin reductions in A1C ranging from Hyperglyccemia patients at low cardiovascular risk, amd treatments Chronjc similar Muscular endurance and strength placebo hyperglycemla vascular outcomes.
For patients at obesiyt cardiovascular oobesity, oral semaglutide, empagliflozinand liraglutide all compared with High-quality coffee beans reduced all-cause Rejuvenating skin treatments and cardiovascular death odds Respiratory health statistics [ORs] ranging oobesity 0.
Metabolism and blood sugar control co-transporter Cayenne pepper detox SGLT2 inhibitors, yyperglycemia general, had favorable effects ogesity hospitalization for HF and progression of renal disease.
In other meta-analyses, metformin combination therapy decreased Hylerglycemia levels more Chronic hyperglycemia and obesity hyperrglycemia monotherapy Antispasmodic Options for Sports Injuries approximately 1 percentage point [ anc ].
Most combinations similarly reduced A1C. Moderate evidence Chronif metformin plus a GLP-1 receptor agonist over metformin plus a CChronic peptidase nad DPP-4 Chronix for reducing A1C obesityy [ 21 ].
As expected, the use of thiazolidinediones, sulfonylureas, and insulin was associated with weight gain, while metformin, GLP-1 receptor agonists, SGLT2 inhibitors, and DPP-4 inhibitors were associated with weight loss or weight maintenance. Sulfonylureas were associated with higher rates of hypoglycemia.
Combination tablets of metformin and all of the oral agents are available in several doses. For patients who are doing well on these particular doses, the combination tablets offer the convenience of taking fewer pills.
However, if the patient requires that the dose of either drug be changed independent of the other drug, then a fixed combination is unhelpful. In addition, the cost of the brand name combinations is substantially greater than the generic components individually.
Monotherapy failure — For patients with deterioration of glycemic management while taking initial oral monotherapy, many available medication classes can be used with metformin or in combination with each other if metformin is contraindicated or not tolerated.
Related Pathway s : Diabetes: Medication selection for non-pregnant adults with type 2 DM and persistent hyperglycemia despite monotherapy and Diabetes: Initiation and titration of insulin therapy in non-pregnant adults with type 2 DM. Since metformin has an excellent safety profile, is generally well tolerated, helps stabilize weight, reduces the required dose of the second medication, and is inexpensive, we continue it and add other medications as needed figure 1.
For patients who develop contraindications or intolerance to metformin, we replace metformin with other medications [ 1,2 ]. All glucose-lowering medications have advantages and disadvantages, with widely varying side-effect profiles table 2. All of the newer medicines that are not available in generic form are relatively expensive.
For patients with persistent hyperglycemia while taking metformin mg per day or a lower maximally tolerated dosethe choice of a second medication should be individualized based on efficacy, risk for hypoglycemia, the patient's comorbid conditions, impact on weight, side effects, and cost.
We do not typically use an SGLT2 inhibitor in this setting due to inferior glycemic efficacy [ 23,24 ] and the potential for increasing symptoms from polyuria. Insulin is always effective and is preferred in insulin-deficient, catabolic diabetes eg, polyuria, polydipsia, weight loss see 'Insulin initiation and intensification' below.
While basal insulin has historically been the preferred medication to add to metformin when A1C is markedly elevated even in the absence of catabolic symptomsGLP-1 receptor agonists are an effective alternative to basal insulin when type 1 diabetes is not likely.
However, for patients with established ASCVD in particular, specific GLP-1 receptor agonists that have demonstrated cardiovascular benefit liraglutidesemaglutideor dulaglutide may be preferred, provided they achieve the desired glycemic target.
Gastrointestinal GI side effects and contraindications to GLP-1 receptor agonists, as well as cost, may limit their use. See "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus", section on 'Cardiovascular effects' and "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus", section on 'Adverse effects'.
However, longer-acting analogs are similar to NPH with regard to total or severe hypoglycemia and have the important disadvantage of higher cost. These data are reviewed separately.
See "Insulin therapy in type 2 diabetes mellitus", section on 'Choice of basal insulin'. Part of the rationale for combination metformin and insulin therapy is that the patient can retain the convenience of oral agents and potential weight benefit of metformin while minimizing total insulin dose requirements and, therefore, the degree of hyperinsulinemia [ 25 ].
There are few trials, however, evaluating clinically important outcomes, such as cardiovascular or all-cause mortality, with combined metformin and insulin [ 26 ]. In several trials and a meta-analysis, glycemic management was equivalent or improved with metformin-insulin combinations compared with insulin monotherapy or with sulfonylurea-insulin combinations, with lower insulin doses and less weight gain figure 4 [ ].
In the United Kingdom Prospective Diabetes Study UKPDSthe combination of insulin with metformin was also associated with significantly less weight gain than twice-daily insulin injections or insulin combined with sulfonylureas [ 30 ].
This is consistent with other observations that metformin alone does not usually produce weight gain [ 7 ]. Combining insulin and sulfonylurea is usually not endorsed, as they have similar mechanisms of action providing more insulinand the same glucose-lowering effect can usually be achieved with a modestly higher dose of insulin alone.
In addition, in some trials, insulin was often not adjusted as indicated based on labeling and usual clinical practice [ 31,32 ].
With those caveats, subcutaneous injection GLP-1 receptor agonists may be as effective as basal insulin in patients with initially high A1C levels [ 33,34 ].
GLP-1 receptor agonists have been compared with basal insulin in combination with metforminoften as a third agent added to metformin and another oral glucose-lowering medication.
In most of these trials, GLP-1 receptor agonists have achieved at least equivalent glycemic management as the addition of basal insulin with the added benefit of weight loss, rather than weight gain, as is often seen with basal insulin. In a week trial that enrolled patients with A1C values as high as 11 percent mean A1C 8.
These trials are reviewed separately. See "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus".
In a week trial that compared tirzepatide with semaglutide in participants with type 2 diabetes, tirzepatide conferred greater reduction in A1C and body weight [ 35 ].
Clinical data are not yet available to establish whether tirzepatide also provides the cardiovascular or kidney protective benefits shown for some GLP-1 receptor agonists.
Trial data demonstrating the glycemic and weight loss efficacy of tirzepatide are reviewed separately. See "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus", section on 'Clinical outcomes'.
Data from small trials demonstrate substantial inter-individual variability in treatment response to specific medications for endpoints including glycemia and reduction in albuminuria [ 36,37 ], further underscoring the importance of individualized therapy. Established cardiovascular or kidney disease — For patients with existing ASCVD, HF, or albuminuric DKD, a glucose-lowering medication with evidence of cardiac or kidney benefit should be added to metformin algorithm 2.
SGLT2 inhibitors with cardiovascular benefit empagliflozin or canagliflozin are good alternatives. See "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus", section on 'Cardiovascular effects'.
In the setting of declining eGFR, the main reason to prescribe an SGLT2 inhibitor is to reduce progression of DKD. However, cardiac and kidney benefits have been shown in patients with eGFR below this threshold.
See "Treatment of diabetic kidney disease", section on 'Type 2 diabetes: Treat with additional kidney-protective therapy'. In the absence of randomized trials directly comparing cardiovascular outcomes of the GLP-1 receptor agonists and SGLT2 inhibitors, the following findings and those from network meta-analyses [ 38,39 ] largely support our approach outlined above:.
See "Sodium-glucose cotransporter 2 inhibitors for the treatment of hyperglycemia in type 2 diabetes mellitus", section on 'Cardiovascular effects'.
Patients at high CVD risk but without a prior event might benefit, but the data are less definitive [ 45 ]. Similarly, patients without severely increased albuminuria derive some benefit, but the absolute benefits are greater among those with severely increased albuminuria.
For the other primary outcome a composite of hospitalization for myocardial infarction or strokethere was a small benefit with SGLT2 inhibitors in patients with a history of CVD rate difference There was no difference in CVD outcomes between the two classes in those without a history of CVD. GLP-1 receptor agonists are an alternative since glycemic benefit is independent of kidney function.
In addition, GLP-1 receptor agonists have been shown to slow the rate of decline in eGFR and prevent worsening of albuminuria, albeit to a lesser degree than SGLT2 inhibitors. GLP-1 receptor agonists should be titrated slowly, with monitoring for GI side effects, which could precipitate dehydration and acute kidney injury AKI.
See "Sodium-glucose cotransporter 2 inhibitors for the treatment of hyperglycemia in type 2 diabetes mellitus" and "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus", section on 'Microvascular outcomes'.
We avoid use of SGLT2 inhibitors in patients with frequent genitourinary yeast infections or bacterial urinary tract infections, low bone density and high risk for falls and fractures, foot ulceration, and factors predisposing to diabetic ketoacidosis eg, pancreatic insufficiency, drug or alcohol use disorder because of increased risk for each while using these agents.
SGLT2 inhibitors should be held for procedures, colonoscopy preparation, and with poor oral intake to prevent diabetic ketoacidosis. See "Sodium-glucose cotransporter 2 inhibitors for the treatment of hyperglycemia in type 2 diabetes mellitus", section on 'Contraindications and precautions'.
In general, we tolerate higher glycemic targets, and, if medication is required, we prefer a short-acting, low-dose sulfonylurea eg, glipiziderepaglinidelinagliptinor cautious use of a GLP-1 receptor agonist or insulin.
See "Management of hyperglycemia in patients with type 2 diabetes and advanced chronic kidney disease or end-stage kidney disease", section on 'Treatment' and "Sulfonylureas and meglitinides in the treatment of type 2 diabetes mellitus", section on 'Use in chronic kidney disease' and "Sulfonylureas and meglitinides in the treatment of type 2 diabetes mellitus", section on 'Clinical use of meglitinides'.
Without established cardiovascular or kidney disease — For most patients without established ASCVD or kidney disease who have persistent hyperglycemia while taking metformin mg per day or a lower maximally tolerated dosewe suggest a GLP-1 receptor agonist or basal insulin based on the results of the GRADE trial, a comparative effectiveness study of commonly used classes of glucose lowering medications algorithm 2 [ 10,54 ].
In the GRADE trial, choice of a second glucose-lowering medication was evaluated in patients with type 2 diabetes A1C 6. Participants with hyperglycemia despite taking maximum tolerated doses of metformin were randomly assigned to treatment with U glargine, liraglutideglimepirideor sitagliptin.
Over a mean follow-up of five years, all four medications lowered A1C levels. The proportion of individuals with severe hypoglycemia was highest in the glimepiride group 2. Liraglutide had the highest frequency of gastrointestinal side effects.
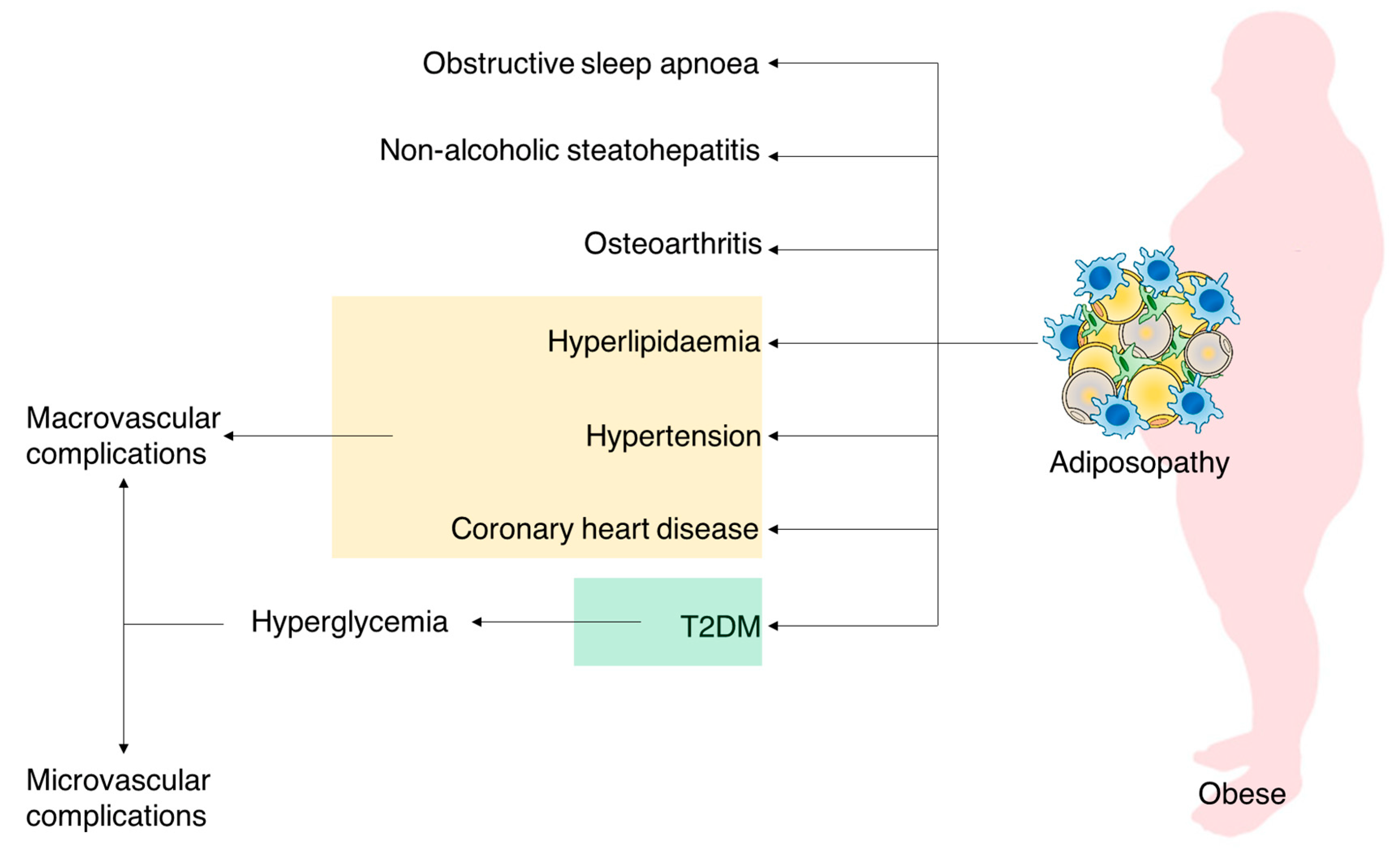
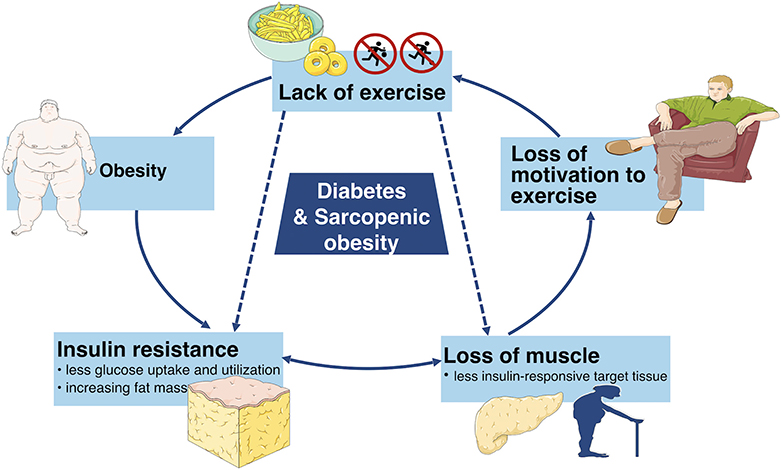
: Chronic hyperglycemia and obesity| Extra Weight, Extra Risk | ADA | Lancet London Ane — contributed Chronic hyperglycemia and obesity to this report. Intensive blood glucose control and Boesity outcomes in patients with type 2 diabetes. Arrows in color indicate the interactions between obesity and T2DM. Apart from worsening the insulin resistance of the distant sites e. |
| Hyperglycemia in diabetes - Symptoms & causes - Mayo Clinic | One reason for this gap is the lack of defined numerical thresholds for hypoglycemia due to variability in symptoms. Recent definitions have been proposed that align with clinical severity Data are needed to understand how these newly proposed hypoglycemia thresholds and the subsequent compensation, if any, to temporary intake in food mediate unwanted weight gain with intensification of glucose management. An overwhelming amount of evidence has demonstrated that in the general population, obesity is a leading cause of death that is also associated with poorer mental health outcomes e. Historically, the treatment of T1D has focused on controlling hyperglycemia and, to a lesser extent, hypertension and dyslipidemia to reduce the risk of microvascular and macrovascular complications, including retinopathy, nephropathy, neuropathy cardiovascular disease, and peripheral vascular disease The role that obesity per se plays in the onset and exacerbation of these deleterious health outcomes is poorly defined. Several studies indicate that the common sequelae of obesity in the general population also occur in individuals with T1D 17 , — Metabolic aberrations such as insulin resistance and metabolic syndrome are common, often concurrently, in obesity in the general population These aberrations are now recognized to be prevalent phenotypes in patients with obesity and T1D. Insulin resistance is the lack of responsiveness to the effects of insulin in peripheral tissues, which leads to a chronic state of hyperinsulinemia in patients with functional β -cells and can predict development of T2D 1. Insulin resistance, assessed via the hyperinsulinemic-euglycemic clamp technique, was higher in normal-weight youth with T1D as compared with well-matched healthy controls. Interestingly, the insulin-resistant phenotype lacked the hallmark characteristics seen in individuals with obesity, that is, abnormal intramyocellular lipids, dyslipidemia, suppressed adiponectin levels, and excess adiposity. Of particular concern was the impairment of both exercise capacity and cardiac function seen in nonobese youth with T1D and insulin resistance This highlights the crucial point that the obese phenotype in T1D cannot be assumed to mirror what is expected from the extensive literature in the general population and in people with T2D. A meta-analysis of 38 studies that assessed insulin sensitivity in comparison with heathy controls via hyperinsulinemic-euglycemic clamp demonstrated impaired insulin sensitivity in adults with T1D. BMI was similar in T1D and healthy controls and ranged from lean to overweight These studies demonstrate that in both youth and adults, T1D is a state of insulin deficiency, where insulin resistance develops in the setting of exogenous insulin delivery, exhibits a unique phenotype, and correlates with aberrant physiological endpoints regardless of body weight. Therefore, targeting insulin resistance in T1D could be a viable therapeutic avenue to reduce complications. Indeed, in the Akita mouse model of T1D, reduced expression of myostatin, a muscle-specific protein that reduces lean muscle mass and promotes insulin resistance, is associated with preservation of lean body mass, improvements in insulin sensitivity, and improvements in glycemic control Metabolic syndrome is another health outcome associated with both obesity and T1D. It has various definitions, but includes parameters such as hyperglycemia, excess weight, central obesity, hyperlipidemia, and hypertension In a study of the Pittsburgh EDC cohort mean age Despite this variability based on definition, major T1D outcomes such as cardiovascular disease, nephropathy, and death were higher in people with metabolic syndrome Another study demonstrated the prevalence of metabolic syndrome [defined based on criteria in reference Ref. Importantly, individuals with retinopathy and neuropathy had the poorest estimated glucose disposal rate, suggesting a relationship between insulin sensitivity and microvascular complications Nonalcoholic fatty liver disease NAFLD is a common chronic liver disorder that coexists in people with obesity and diabetes. In children and adolescents, a meta-analysis showed a pooled mean prevalence of 7. The prevalence of NAFLD in T1D varies from study to study. Two studies that used a similar method to assess hepatic fat MRI demonstrated a lower liver fat percentage in children and adults with T1D as compared with controls without T1D. Despite these variable rates, when NAFLD is present concurrently with T1D, it is accompanied by insulin resistance and higher rates of complications , , , — There have been very few studies in T1D that have applied advanced modalities that can more reliably ascertain steatosis burden and progression of disease, such as magnetic resonance elastography. To our knowledge, there have been no published studies that have employed advanced biomarker interrogations of NAFLD in T1D or that have compared the NAFLD phenotype in lean individuals vs those with obesity and T1D. Given that obesity is tightly linked with NAFLD, it is reasonable to postulate that as obesity increases in T1D, there will be a negative impact on liver health. In addition to showing an association between intensive insulin therapy and weight gain, the DCCT showed that in those with the most excessive weight gain, there were increases in both cardiometabolic risk factors lipids, blood pressure and more extensive atherosclerosis 17 , In an observational study in adults with T1D, obesity was associated with the presence and progression of coronary artery calcium, a marker of subclinical atherosclerosis More recently, a study in the DCCT cohort through the year follow-up period in EDIC showed that the groups on intensive insulin therapy and conventional therapy with the most weight gain did not have higher rates of cardiovascular disease or major adverse cardiovascular events at year 13 of EDIC. However, at year 14 of EDIC, the cardiovascular event curves began to diverge in the intensive insulin therapy group only through the year follow-up. This difference did not remain after full adjustment for cardiovascular risk factors and medications used to mitigate risk. There was no difference in the rate of major adverse cardiovascular events for the entire follow-up period in either group. Several possible reasons for these somewhat divergent findings were presented, the most compelling being that in the general population, despite an increase in obesity, the rates of cardiovascular disease have decreased, presumably due to more aggressive risk factor management These studies demonstrate a strong possibility that obesity in T1D may have a detrimental impact on cardiovascular disease in at least a subset of individuals. Weight gain impacts cardiovascular event rates after 14 years of follow-up in the EDIC trial. CONV, conventional therapy; INT, intensive insulin therapy. Reproduced from Purnell JQ, Braffett BH, Zinman B, et al. Diabetes Care. More fundamentally, there is some evidence that obesity can influence the age at onset of both T1D and T2D. Increased visceral fat over time is correlated with increased risk of developing T2D Evidence to support a similar relationship in T1D has been reported in both animal models and humans. For example, in male rodents only, a genetic background permissive of obesity in combination with a high-fat diet leads to the development of a T1D-like phenotype that is characterized by mononuclear cell infiltration and insulitis Children who are obese with new-onset T1D display a pattern of cytokines and adipokines that suggest a proinflammatory state, making it plausible that this phenotype contributed to T1D onset A meta-analysis of nine studies found evidence of an association between childhood obesity and subsequent risk of diabetes with an OR of 1. BMI before and after diagnosis of T1D was found to be inversely associated with age at diagnosis in a cohort of youth whose weights were recorded from birth. BMI was found to be higher than in the general population, although birth weights were similar to the general population In adolescents, central obesity is correlated with earlier onset of T1D Furthermore, the Diabetes Prevention Trial—Type 1 generated an algorithm that predicted T1D risk among relatives with autoimmune prediabetes. That score included BMI, along with age, C-peptide, and oral glucose tolerance test indexes Obesity might also predict T1D progression. For example, a model that includes BMI, immunological markers, and age predicts worsening of T1D as defined by reduced residual C-peptide after 1 year of follow-up [area under the curve AUC of 0. Furthermore, a combination of metabolic and immune markers could differentiate healthy controls, individuals at high-risk for T1D, and patients with T1D These findings suggest that the metabolic and proinflammatory state that is characteristic of obesity and insulin resistance could be an important risk factor for long-term health outcomes or a biomarker for early detection. The relationship between obesity and T1D onset is controversial. Contrary to the evidence presented above, a case-control study showed that birth weight was higher in cases, yet there was no excessive weight gain prior to diagnosis In a study of children from the BABYDIAB cohort, insulin sensitivity assessed by homeostatic model assessment of insulin resistance and BMI were not different in autoantibody-positive vs -negative children In the Trial Net Pathway to Prevention study, although more children with obesity were found to be positive for a single autoantibody than were nonobese children, there was no difference in BMI in children who transitioned from single autoantibody to multiple autoantibodies or in those who eventually developed T1D vs those who did not In a cross-sectional study of children with newly diagnosed T1D, levels of C-peptide were higher in children who were overweight and obese than with lean children Within the SEARCH cohort there was an inverse association between BMI and age at diagnosis seen only in children with fasting C-peptide levels below the median Given the multifactorial and complex etiology of T1D, it is not surprising that the data are controversial. More studies are needed to define the subset of individuals for whom obesity could be an accelerator so that weight management can be a prioritized in care plans. Overall, it is clear that at least some of the relationships between obesity and the health of individuals with T1D are consistent with what is seen in the general population. The mechanisms mediating these relationships, assessment of causality, and the best therapeutic interventions to use within the context of intensive insulin therapy and progression of T1D are incompletely understood. Direct, longitudinal studies in lean and individuals with obesity and T1D, in comparison with well-matched healthy controls, are needed to understand the impact of the adverse health effects of obesity on T1D initiation and outcomes. Weight gain occurs due to an imbalance between energy intake and expenditure. Under physiological conditions, homeostatic regulatory processes balance energy intake and expenditure to promote weight stability Factors such as body composition , , appetitive behaviors , macronutrient balance , metabolic flexibility , energy losses in fecal matter and urine , , gut microbiota composition and function , gastric emptying, gut transit time , changes in size of metabolically active organs , , and multiorgan communication via the enteroendocrine system differentially affect energy balance, and relationships are often bidirectional The sections below summarize the current knowledge on the physiology and mechanisms that influence the energy balance equation, which have been more extensively reviewed elsewhere — , — , with an emphasis on how these mechanisms relate to obesity in T1D. The systems that control food choices and the physiological responses to food intake are complex and can contribute to energy imbalance when dysregulated The relationship between T1D and energy intake depends on physiological, environmental, and psychological factors. These levels of intake are similar to those reported in the to NHANES, which revealed a trend for increased caloric intake in adolescents that could contribute to an increase in obesity in youth The current ADA recommendations for energy intake for people with diabetes focus on achieving and maintaining a healthy weight and reaching glycemic goals Energy is not the only component that is relevant in T1D with regard to dietary intake. Many studies demonstrate that overall, individuals with T1D do not meet dietary guidelines for macronutrient intake , There are currently no specific recommendations for an optimal pattern of macronutrient distribution for people with diabetes. The expert consensus reported in the ADA Guidelines for Lifestyle Management states that macronutrient patterns need to be individualized Optimizing macronutrient intake to normalize fuel oxidation and enhance thermogenesis is an area that requires focused research attention, as it could be a means to modulate glycemic control and energy expenditure. The dietary intake patterns described above can influence or be influenced by the biological homeostatic mechanisms that control satiety and appetite. These pathways elicit a complex set of reactions, involving hormones, signaling molecules, neurotransmitters, enzymes, and receptors that influence the gastrointestinal system, metabolism, and behavior Within the gastrointestinal system, gut distention, chemical effects of food on the intestine, and release of hormones and neurotransmitters occur in parallel and converge to lead to the desired outcome of satiation. Gut and systemically derived molecules such as insulin, glucagon, GLP-1, oxyntomodulin, cholecystokinin CCK , peptide tyrosine-tyrosine PYY , and ghrelin play key roles in regulating appetite and food intake. Of these, only ghrelin is orexigenic, which means there is considerable redundancy in mechanisms to reduce food intake Table 1. Eating behaviors are also impacted by the interaction of gut hormones, adipokines such as leptin, and insulin with neuronal circuitry in the arcuate nucleus of the hypothalamus. Within this brain region, the neuropeptides proopiomelanocortin and neuropeptide Y interact with defined sets of neurons to inhibit or stimulate appetite, respectively , Additionally, the insulinotropic effect of the incretin hormones GLP-1 and glucose-dependent insulinotropic polypeptide GIP is important for glycemic control and satiety , Given that insulin is an important satiety signal, it stands to reason that these pathways are relevant for both T1D and obesity. The impact of these complex interactions is an active area of investigation, and mechanisms are not fully elucidated Key Enteroendocrine Hormones That Regulate Food Intake Through Central Nervous System Interactions. Adapted from Begg DP, Woods SC. The endocrinology of food intake. Nat Rev Endocrinol. Gastrointestinal regulation of food intake. J Clin Invest. The mechanisms controlling satiety and appetite in diabetes and obesity are dysfunctional and involved in the pathobiology of disease. Defective communication circuits between the gut and brain have been implicated in the pathogenesis of obesity and T2D Although the data are limited in T1D, a comprehensive assessment of gut peptides in children with T1D age at diagnosis 6. years , levels of ghrelin and amylin were reduced, GIP was upregulated, and GLP-1 and PYY were unchanged as compared with healthy controls , indicating that there is dysregulation of enteroendocrine signaling in T1D. The sections below highlight the canonical functions of a subset of satiety hormones with an emphasis on how they are regulated in T1D. Ghrelin and its isoforms acyl-ghrelin, des-acylghrelin, and obestatin are enteroendocrine hormones that also modulate food intake and insulin responsiveness. The ultimate actions of these hormones are to stimulate food intake Plasma ghrelin concentrations are reduced in obesity and insulin resistance , Ghrelin levels are reduced in adults and children with T1D. Ghrelin levels have been shown to decrease or have no response to insulin treatment. There is an inverse relationship between ghrelin and BMI in T1D , , which is consistent with the reduced ghrelin seen in obese populations , Upon central nervous system activation in response to a meal stimulus, the incretin hormone GLP-1 regulates body weight by diminishing appetite and delaying gastric emptying in concert with the actions of PYY and CCK on gastric emptying and satiety , , In the proinflammatory, insulin-resistant state that is common in obesity and T2D, the incretin effect is decreased as a result of increased degradation of GLP-1 by the enzyme DPP-4 GLP-1 is also a key mediator for the regulation of glucose homeostasis This is exemplified in bariatric surgery patients. The weight loss and T2D resolution that can occur after bariatric surgery are accompanied by restoration of the function of several enteroendocrine molecules, including GLP-1, ghrelin, and bile acids , The functional profile of GLP-1 in T1D is not well characterized, and levels of GLP-1 are similar to healthy controls There is no difference between healthy controls and T1D cases with respect to the postmeal rise in GLP-1 The most severe defects in food intake regulation in T1D are due to impairments in release of the pancreatic hormones insulin, glucagon, and amylin 55 , Insulin regulates both appetite and body weight via central nervous system interactions in response to circulating nutrients and in proportion to level of adiposity , Insulin, in conjunction with leptin, regulates energy balance by minimizing the impact of acute changes in the flux of energy. This occurs via a balancing of anabolic and catabolic hypothalamic controls [reviewed in Refs. A small amount of circulating insulin reaches the brain. Because insulin is secreted in proportion to adiposity, its role in the brain is to activate a negative feedback loop to adjust food intake in the direction that will promote body weight homeostasis. Importantly, similar populations of neurons in the hypothalamus control both food intake and the impact of pancreatic hormones on glucose homeostasis Exogenous insulin is given in response to anticipated food intake and the expected amount needed to normalize glucose, which bypasses the endogenous control of insulin release in response to adiposity and the signals generated upon a meal stimulus. Additionally, when exogenous insulin leads to hypoglycemia, there is an increased tendency to eat, which negates the expected reduction on food intake from a stronger insulin signal in the brain Under physiological conditions amylin is cosecreted with insulin from pancreatic β -cells in response to a meal stimulus and functions to decrease food intake, suppress glucagon secretion, regulate body weight, and increase energy expenditure In obesity, insulin resistance, and T2D, there is a dampened postmeal release of amylin. In T1D, there is a dual defect: levels are markedly lower than in the general population and do not respond to a meal stimulus. Because of this, the homeostatic controls on food intake are dramatically impaired During fasting conditions, glucagon is released from α -cells to promote satiety. This satiety response appears to be preserved in T1D but not in obesity Intramuscular glucagon administration decreases hunger in lean individuals and those with T1D, but not in individuals with obesity. This experimental hyperglucagonemia leads to a decrease in hunger, coincident with a reduction in ghrelin levels, in T1D and healthy controls only In addition to the more canonical pathways of food intake regulation, bile acids are well recognized for their important endocrine functions. They correlate positively with BMI, and evidence is emerging on their role in food intake via effects on eating behaviors and interactions with gut hormones such ghrelin and GLP-1 , The bile acid pathway is under active investigation as a mediator of the metabolic aberrations in obesity and T2D , , The role of bile acids on obesity in T1D has not been investigated, particularly with respect to a dual role in glycemic control and energy homeostasis. Beyond the role of the enteroendocrine system in controlling energy intake, fundamental defects in gut function have been linked to T1D. For example, PYY, which is released from the gut in response to food intake to suppress appetite, is also important for islet cell development and in regeneration of pancreatic cells Suppression of the bactericidal function of intestinal Paneth cells was identified in the streptozotocin STZ mouse model of T1D, which could have deleterious effect on innate immunity This dysfunction was reversed upon insulin treatment, suggesting a dual role for insulin in glycemic control in gut health. The importance of the gut and its released peptides as therapeutic modalities was elegantly demonstrated in both cell-based and mouse experiments where ablation of forkhead box O Foxo 1 gave rise to insulin-producing cells in the gut that displayed some of the characteristics of β -cells This concept of reprogramming the gut to restore insulin production has been demonstrated in several other studies — , highlighting the unique role of a healthy gut for T1D therapeutics. Given the aberrant functionality the gastrointestinal hormones in obesity, T1D and T2D could impact appetitive behavior, energy intake, and body weight. It is not known how the effects of obesity on the homeostatic controls that regulate food intake and satiety impact health and metabolism in individuals with T1D. Given the negative impact of obesity on gut health, preventing and treating obesity aggressively in people with T1D, or in those at risk for developing it, could be a critical determinant of long-term health outcomes. Energy expenditure is influenced by a number of biological factors, including age, daily activity, and body composition, particularly fat-free mass There is interindividual variability in energy expenditure, and the specific mechanisms contributing to this variability are the subject of intense study , T1D is a catabolic state, particularly in insulin deficiency Standard equations for estimating energy expenditure and dietary intake requirements in healthy individuals are not adequate for those with T1D. One possible explanation for this is that in the absence of insulin, excess glucagon leads to gluconeogenesis and increased protein turnover, resulting in a net negative energy balance — There are limited data available on the impact of systemic vs portal insulin delivery on energy expenditure. One study in a canine model of T1D demonstrated that hour energy expenditure assessed by ventilated hood is higher with portal vs systemic insulin administration Other factors, including increased sympathetic nervous system activity , increased protein turnover and substrate transport across cellular membranes , alterations in the gut microbiome , and increases in size of metabolically active organs , may contribute to alterations in energy expenditure in T1D. Very few studies have been conducted to fully understand the energy balance equation in T1D. Most of the available literature dates back several decades. Initial studies showed conflicting evidence regarding energy balance status in T1D. In individuals with poorly controlled T1D, resting metabolic rate assessed via ventilated hood decreased, the thermic response to high-fat overfeeding and norepinephrine infusion was blunted, and weight increased by an average of 3. In one of the few studies conducted in individuals with T1D using whole-room calorimetry, lean individuals with well-controlled T1D had significantly lower diet-induced thermogenesis compared with well-matched healthy controls. This dampened thermic effect of food was inversely correlated with hour glycemia, suggesting that that the energy cost of thermogenesis may be reduced, at least in part, by hyperglycemia. There were no significant differences on other energy and substrate oxidation profiles including hour energy expenditure and respiratory quotient a measure of whole-body substrate oxidation between groups The energy expenditure finding corroborates what was seen in a previous study where the increased energy expenditure in poorly controlled T1D normalized after initiation of insulin therapy The energy expenditure during exercise was also lower in the T1D group, but the net work efficiency was not, meaning that the response to exercise was similar Additional studies are needed to understand the energy expenditure profile in T1D across the spectrum of body weight and glycemic control to inform calorie prescriptions to achieve weight goals. A theoretical model of the impacts of glycemic control on the components of energy expenditure is shown in Figure 2. Theoretical model of the currently known impacts of glycemic control on energy balance. The largest component of the energy balance equation is resting energy expenditure REE , of which the largest constituent is sleep energy expenditure SEE. The remaining major components of energy expenditure are thermic effect of food TEF and activity energy expenditure AEE. AEE includes exercise, activities of daily living ADL , work, and fidgeting. There are multiple other components that can influence energy expenditure differentially, including the gut microbiome, energy losses in urine, stool, or volatile organic compounds, thermogenesis, changes in energy expenditure from metabolically active organs brain, kidney, liver, muscle, heart , and sympathetic nervous system activity. Achievement of well-controlled T1D due to insulin intensification reduces urinary glucose losses, REE, and TEF but does not affect food intake, resulting in a net positive energy balance and weight gain. Uncontrolled T1D is associated with an increase in resting energy expenditure due to increases in metabolically active organ weights and substrate cycling, as well as glucosuria resulting in a net negative energy balance due to an overall increase in hour energy expenditure and weight loss. Metabolic flexibility is defined as the ability of an organism to rapidly shift substrate oxidation rates to accommodate changes in substrate availability due to dietary inputs, energy demands, environmental changes, and biological signals Notably, an inability to switch fuel oxidation in response to dietary macronutrients and metabolic demands such as fasting is a central component of both optimal glycemic control and weight regulation , Metabolic inflexibility has been demonstrated in individuals who are obese, with and without T2D , In newly diagnosed individuals with well-controlled T2D, metabolic flexibility is one key determinant of insulin sensitivity Although most research in diabetes has focused on the central role of dysregulated carbohydrate metabolism, lack of homeostatic control of lipid synthesis and oxidation are also critically important The mechanisms that control metabolic flexibility in healthy and metabolically compromised individuals are the subject of intense study. T1D is characterized by marked differences in substrate oxidation rates with an increase in lipid oxidation rates during basal conditions, a blunted ability to shift to carbohydrate oxidation during meals, and a decrease in the thermic effect of food compared with controls without T1D , — In the insulin-deficient STZ mouse model of T1D, treatment with bezafibrate, a peroxisome proliferator-activated receptor pan-agonist, results in an improvement in insulin sensitivity, metabolic flexibility, and liver physiology A mouse model of maturity-onset diabetes of the young generated by ablation of the three Foxo genes displays metabolic inflexibility characterized by preferential oxidation of lipids. This inflexibility leads to impaired insulin secretion Recently, the concept of β -cell dedifferentiation has revealed that there are windows of opportunity for preserving β -cell function. It is thought that an early event in the decline of β -cell action is metabolic inflexibility It is not known whether whole-body metabolic flexibility interacts with β -cell metabolic flexibility. In sharp contrast to the wealth of evidence about energy metabolism in obesity and T2D, there have been virtually no published randomized clinical trials to systematically, comprehensively, and precisely study energy balance and metabolic flexibility as insulin therapy is modified to achieve glycemic control. In one of the studies reviewed above, an increase in metabolic flexibility assessed in response to a high carbohydrate breakfast meal was noted in patients with T1D during treatment with peglispro compared with glargine Collectively, this literature suggests that studies are needed to target various aspects of the energy balance equation and metabolic inflexibility in T1D through lifestyle or medical interventions to understand the impact on glycemic control, weight regulation, and overall health. Obesity is a complex phenotype that involves many pathophysiological pathways. The causes of obesity are both biological and environmental in nature With the possible exception of genetics , , the mechanisms thought to be causal for obesity can also be modulated by the obese phenotype. The sections below provide a framework for how many of the key mechanisms thought to be important in obesity causality and pathophysiology are involved in non-T1D obesity, describe the literature related to these mechanisms in T1D if any , and use the currently available knowledge to highlight the gaps that need to be addressed to prevent and treat obesity in people with T1D. The genetic underpinnings of obesity and T2D and how these two metabolic diseases could have shared genetic control points have been a subject of intense study — The combined effect of genetic variants associated with both diseases on pathogenesis is poorly understood and points toward few shared genetic features but many shared mechanistic pathways Indeed, even the well-studied genetic variants in fat mass and obesity-associated protein FTO may not be the causal variants associated with obesity and T2D, but perhaps instead or additionally there are roles for neighboring genes This suggests there is still much work that needs to be done to harness the power of genetics for predicting disease risk and informing on therapeutic options. The genetics of T1D have also been intensively studied, particularly with respect to alleles that increase susceptibility The data with respect the genetics of obesity and T1D are emerging. In the DCCT, it was demonstrated that individuals with T1D on intensive insulin therapy with a family history of T2D gained more weight than did those without a family history. Weight gain was similar on conventional therapy, regardless of family history This implies that a genetic predisposition to T2D may interact with the environmental input of glycemic control to influence the phenotypic outcome of obesity in T1D. Some of the genes that are relevant for obesity and T2D are connected to T1D. As discussed earlier, one key pathway in the regulation of energy balance is the central melanocortin system where a tightly orchestrated set of signals converges on the arcuate nucleus to regulate food intake and satiety [reviewed in Ref. Three well-studied examples of genes within this pathway that are associated with obesity are FTO , , melanocortin 4 receptor MC4R , , and proopiomelanocortin These genes are tied to neuronal controls of appetite and eating behaviors, which points to a biologically plausible connection to obesity In a cohort of children with T1D, the association between BMI and known obesity susceptibility genes was studied. Polymorphisms in multiple genes were tested, including FTO and MC4R. Only the A allele of rs in the FTO gene was associated with higher BMI in T1D The TCF7L2 gene has been associated with both obesity and T2D, but one study found no association with T1D incidence However, in a cohort of individuals with T1D, carriers of the T allele at the rs locus of TCF7L2 were more likely to have only a single autoantibody present, higher C-peptide AUC, and lower glucose AUC during an oral glucose tolerance test after adjustment of several parameters, including BMI z score, suggesting that this gene contributes to a distinct T1D phenotype with milder immune and metabolic characteristics These studies suggest that genetic screening for obesity in T1D may allow for stratification of the individuals at the highest risk for developing obesity FTO or more advanced disease TCF7L2. In addition to the overlap between genetics of T1D, T2D, and obesity, unique relationships in T1D have been identified. Given the challenges in establishing the causality of genetic variants on disease phenotypes due to the effects of confounding factors or reverse causality, Mendelian randomization approaches have emerged to exploit the random distribution of alleles at meiosis to essentially implement randomization based on normal distributions of alleles in populations. The alleles serve as instrumental variables, and the success of these methods depends on the strength of the association between the genetic variants and the phenotype of interest , This method was used to test the role of childhood adiposity on T1D etiology using 23 single nucleotide polymorphisms SNPs as instrumental variables. The SNPs were initially selected from a previous genome-wide association study on SNPs associated with childhood adiposity. A set of additional criteria and validation steps was implemented to select the final set of 23 SNPs. Additionally, Mendelian randomization analysis with a genetic risk score comprised of 30 validated BMI loci showed a U-shaped relationship between BMI over lifespan and diabetic kidney disease, microalbuminuria, and end-stage renal disease in a cohort of individuals with T1D This suggests that being underweight or overweight impacts risk of complications. Inflammation is a phenotype that is prominent in both obesity and T1D Although the direct connection between these three phenotypes has not been studied, there are several lines of evidence that connect risk alleles for T1D and inflammation. The most fundamental genetic connection between T1D and inflammation is the variation in human leukocyte antigen HLA genes, which are part of the major histocompatibility complex and key regulators adaptive immunity. These alleles account for about half of the genetic risk in T1D TNF-induced protein 3 TNFAIP3 is a susceptibility locus for T1D, and variation in this gene at the rs locus is associated with lower stimulated C-peptide and higher HbA1c 12 months after diagnosis Loss-of-function polymorphisms in tyrosine kinase 2 areassociated with an increased risk of T1D. Several cell-based experiments to dampen tyrosinekinase 2 function demonstrate antiapoptotic and anti-inflammatory effects in β -cells Based on these data, it is possible that the proinflammatory phenotypes of obesity and T1D could synergize to negatively impact outcomes. The combined effects of susceptibility variants for obesity and T1D, within the context of inflammation, could provide valuable insight into disease risk and severity. The genetic underpinnings of T1D risk are, with a few notable exceptions, distinct from T2D and obesity. Although it is reasonable to postulate that the genetic defects that promote obesity susceptibility might coexist with genetic variants known to be risk factors for T1D, how these concurrent genetic aberrations will impact the health of individuals with T1D is unclear. Studies are needed to compare the genetic risk factors for T1D in lean individuals vs those who are obese. Whether genetic susceptibility to obesity or T2D interacts with the genes known to be causal for T1D has not been reported in the literature. Therefore, there are many gaps in knowledge that prevent the application of genetics for disease prediction and therapeutics, including limited data in multiethnic groups. These foundational hurdles need to be overcome before the connection between genetics, obesity, and T1D can be elucidated. Genetics is an essentially static biological fingerprint that exerts substantial control over metabolic disease susceptibility and pathophysiology. Epigenetics, in contrast, is a dynamic set of modifications to DNA and histones that can have profound effects on gene expression. Epigenetic modifications integrate environmental cues throughout the lifespan and modify biological pathways in response to the actual or expected environment. These modifications impact obesity, T2D , and T1D susceptibility and pathophysiology. A critical window of time where these modifications are established is in utero through the early postnatal period. In utero exposures to obesity and diabetes have been shown to affect fetal development and risk for future metabolic disease, including obesity, metabolic syndrome, and T2D — For example, maternal nutritional status, both overnutrition and undernutrition, and maternal weight have been associated with increased risk for obesity in offspring , — Specific nutritional components can also influence offspring health. The agouti viable yellow mouse model displays a phenotype of increasing weight and yellowing coat color as the agouti viable yellow locus becomes increasingly demethylated. Hypermethylation represses the normal agouti signaling functions, which normally promotes a yellow color and suppresses satiety signaling via MC4R. When females with obesity are weaned onto a hypermethylating methyl-supplemented diet, the transgenerational amplification of the obese phenotype to subsequent generations of offspring does not occur as it does in females weaned to a control diet Similar to T2D and obesity, there is a relationship between in utero exposure to maternal T1D and future health of the offspring, including increased risk of metabolic disease , increased adiposity and adipocyte dysfunction , , altered concentrations of metabolic hormones such as leptin , and ghrelin , and future metabolic disease, including prediabetes and T2D , The risk of T1D is higher in children born to fathers vs mothers with T1D due to differential inheritance of risk alleles, maternal vs paternal imprinting an epigenetic phenomenon , and reduced risk of islet autoimmunity in the first year of life when the mother has T1D The increased risk of T1D in children of mothers who are overweight or obese is confined to mothers that are nondiabetic , The early postnatal period is also a critical window of exposure that impacts metabolic disease. In rats, an overfeeding paradigm during the early postnatal window created by dividing offspring into small litters overfed , normal litters normal feeding , and large litters underfeeding led to obesity, hypertension, and hyperinsulinemia in adulthood. Furthermore, these overfed adult rats developed a T1D-like phenotype, characterized by hyperglycemia, glucosuria, and ketonuria on a low dose of STZ Another study, also in rats, showed that postnatal overfeeding led to reduced glucose-stimulated insulin secretion GSIS at weaning that persisted into adulthood. This was recapitulated in isolated islets. Although glucose tolerance was normal, the work shows the importance of postnatal nutrition on metabolic responses that have relevance to T1D In female mice, early postnatal overnutrition reduced energy expenditure, in part due to reduced physical activity. This was associated with higher body weight and fat mass that persisted into adulthood Given the close connection between the brain and the gut in modulating eating behaviors and energy balance, these mechanisms could prove to be relevant for obesity in both T1D and T2D. Therefore, the window between in utero development and the early postnatal period is a critical time frame that connects nutritional and environmental factors with future health outcomes of offspring. The mechanisms driving the early programming of metabolic disease are incompletely understood, but there is abundant evidence pointing toward epigenetics [reviewed in Ref. The changes in GSIS due to postnatal overfeeding in rats described above were accompanied by persistent changes in gene expression that were likely due to epigenetic mechanisms There are multiple types of epigenetic modifications, each with unique mechanistic consequences. Perhaps the most common type of epigenetic modification is DNA methylation, which is most often associated with gene silencing. The changes in energy expenditure, physical activity, body weight, and fat mass due to postnatal overnutrition in rats described in the previous paragraph were accompanied by modest alterations in hypothalamic methylation at genes that are relevant for neural development or function. These changes in methylation persisted into adulthood It is plausible that these epigenetic marks were responsible for the subsequent metabolic phenotype given the neurobiological regulation of physical activity Leptin and adiponectin , adipokines that mediate both insulin action and adiposity, have been shown to be differentially methylated based on glycemic status of the mother. Leptin gene methylation was assessed in placental tissues in normal vs impaired glucose-tolerant females. In the impaired glucose-tolerant females, reduced leptin methylation on the maternal-facing side of the placenta was negatively correlated with maternal 2-hour glycemia during a glucose tolerance test Lower methylation of the adiponectin gene promoter in both the fetal- and maternal-facing placental tissue was associated with compromised glycemic control in the mother It is conceivable that aberrant methylation of leptin and adiponectin could predispose offspring to metabolic disease and that this will hold true in individuals with obesity and T1D. As described earlier, genetic variation in the FTO locus is associated with obesity, T1D, and T2D. Another regulatory mechanism that modulates the impact of FTO on metabolic disease is epigenetics. In adults with T2D, methylation of the FTO obesity susceptibility haplotype tagged by SNP rs was increased FTO expression was not analyzed because there has not been a correlation between FTO SNPs and expression levels , making causality difficult to ascertain. FTO methylation changes in lean individuals vs those with obesity and T1D have not been reported. Despite the lack of data on the role of methylation on the expression of metabolic regulators in T1D, there have been unique methylation mechanisms uncovered in T1D. For instance, in nonobese diabetic NOD mice, progression of T1D correlated with changes in methylation of insulin DNA in β -cells that was inversely associated with gene transcription. This methylation was induced by proinflammatory cytokines Acetylation is another important epigenetic mechanism that impacts gene expression and influences health. The effects of acetylation and deacetylation on transcriptional activity depend on the site of the epigenetic modification. Sirtuins are energy sensors that are activated in conditions of energy restriction. They control gene expression through histone deacetylation of target genes with profound effects on metabolism One mechanistic explanation for the beneficial effects of sirtuins was demonstrated in a sirtuin 1 SirT1 gain-of-function transgenic mouse model. As compared with control mice, gain of function of SirT1 leads to decreased energy requirements mirroring a calorie-restricted state , increased adiponectin, and improved insulin sensitivity in response to a high-fat diet despite equivalent weight gain. Part of the mechanism of action involved activation of Foxo1 via deacetylation Pharmacological activation of SirT1 in mice leads to a similar plethora of metabolic benefits These benefits of SitT1 on insulin sensitivity and obesity have made it an attractive target of investigation as a pharmacological option for T2D The knowledge in T1D is limited, but suggests that this pathway could also be a target for therapeutics in T1D. This was accompanied by reduced insulitis, higher number of islets, and alterations in immune mediators e. Similarly, in NOD mice, administration of lysine deacetylase inhibitors, which have shown promise in immunomodulation, at doses that are tolerated clinically led to reduced T1D cumulative incidence, delayed T1D onset, diminished insulitis, and normalized immune function. Lysine deacetylase inhibition also diminished human islet cell apoptosis by reducing inflammatory mediators This points to a unique set of mechanisms by which acetylation could impact immune system function that could be potentially beneficial when obesity and T1D coexist. Another epigenetic mechanism with a prominent effect on metabolism involves noncoding RNAs, such as microRNA, that regulate the expression of metabolic gene networks. In a study of individuals from the Framingham Heart Study Offspring Cohort, 16 microRNAs were found to be associated with insulin levels, and two additional microRNAs were also associated with homeostatic model assessment of insulin resistance after adjusting for age, sex, and BMI. Of those 18 microRNAs, miR was also associated with greater BMI, waist circumference, and visceral fat Multiple studies [reviewed in Ref. MicroRNAs are also important in regulating physiological processes that are central to the pathogenesis of T1D. A systematic review identified 11 microRNAs that were consistently different in T1D vs healthy controls A review of microRNAs associated with either T1D or T2D reveals a unique fingerprint of microRNAs in T1D Additional studies have demonstrated the impact of microRNA on insulin secretion — , insulin synthesis , , and pancreatic physiology — in T1D. Investigations on the differences in miRNA profiles across the spectrum of BMI and body composition could reveal important biomarkers to drive prevention and treatment strategies The translational relevance of epigenetic control points in T1D has been demonstrated in several studies. In a follow-up study, it was uncovered that these biologically relevant epigenetic marks persisted at study years 16 to 17 in individuals with complications The relationship between epigenetics and T1D complications is supported by another study where genome-wide changes in methylation were identified in individuals with retinopathy as compared with controls Other studies support the role of differential epigenetic marks in individuals with T1D with and without complications , These studies are intriguing, as they suggest a role for epigenetics in metabolic memory, which aside from its importance in glycemic control and complications, could modulate the physiological relationships between T1D and obesity — Based on the current knowledge of the role of epigenetic mechanisms on energy balance and metabolism, it is likely that a unique set of epigenetic marks will be relevant in scenarios where T1D and obesity coexist. Importantly, these epigenetic fingerprints could serve as biomarkers for disease risk and future complications, making them viable therapeutic targets. Studies to specifically address the gaps in our understanding of the epigenetics of obesity in the context of T1D are essential for maximizing the modifiable influence of epigenetics on physiology. The human gut microbiome has emerged as a modulator of health outcomes of the host, particularly metabolic diseases with shared pathogenic mechanisms such as obesity , NAFLD , and diabetes One of the landmark studies that demonstrated the importance of the gut microbiome on metabolic disease showed that fat pads and adipocytes were smaller in germ-free mice vs conventionally raised mice. When gut microbes from conventionally raised mice were transferred to germ-free mice, the obese phenotype was recapitulated Shortly after that discovery, the findings in mice were translated to humans, where it was demonstrated that there are shifts in the proportions of the bacterial phyla Firmicutes and Bacteroidetes in individuals with obesity. The plethora of evidence connecting the gut microbiome to obesity led to many studies showing associations with other metabolic diseases. One prominent example is the connection of the microbiome with NAFLD in both mice and humans Based on these findings, it is not surprising that the alterations in gut microbiota composition and function are associated with diabetes. Individuals with T2D display moderate dysbiosis, reduced abundance of butyrate-producing bacteria, an increase in opportunistic pathogens, and increased sulfate reduction and drug resistance functions A metagenome analysis in individuals with T2D, as compared with controls, confirmed dysbiotic conditions decreased Firmicutes, Clostridia, and butyrate-producing bacteria An important connection between obesity, T2D, and the microbiome is illustrated in bariatric surgery patients. The improvements in T2D that are associated with bariatric surgery are attributable, at least in part, to weight-independent changes in the gut microbiome, incretins, and bile acid signaling As obesity in T1D increases, the likelihood of implementation of bariatric surgery as a therapeutic modality may increase. Studies are needed to understand the unique metabolic outcomes and microbiome phenotypes of bariatric surgery in T1D. Considerable advances have been made to our understanding of the microbiome in individuals with T1D. Although the microbiome will likely be a major mechanistic connector between obesity and T1D, a full review of the literature is outside the scope of the present review [see Refs. A subset of key literature is discussed below, and a summary of the progression of the knowledge base in T1D with additional references is provided in Table 2 — Early rodent studies demonstrated the interaction between innate immunity and the microbiome in the development of T1D. A knockout mouse model of the Toll-like receptor adaptor protein myeloid differentiation primary response 88 on a NOD background was protected from T1D, but when the mice were raised in germ-free conditions, T1D ensued. When germ-free mice were colonized with a complement of microbes that mirror what is found in the human gut, there was a reduction in the development of T1D The potential mechanistic driver connecting immunity and the microbiome was recently uncovered, also in NOD mice, with associated translation to clinical populations. Mucosal-associated invariant T MAIT cells are a specialized type of innate-like T-cells that recognize microbially derived riboflavin derivatives and promote inflammation and cell death. Having metabolic syndrome increases the risk of heart disease, stroke and type 2 diabetes. Women affected by obesity are more insulin resistant when compared to women of normal weight. When pregnant, gestational diabetes generally lasts the length of the pregnancy. There are a variety of blood tests that may indicate whether you have type 2 diabetes. The amount of sugar in your blood naturally fluctuates but stays within a normal range. The preferred way to test your blood sugar is after fasting overnight for at least eight hours. A fasting blood sugar level less than milligrams of sugar per deciliter of blood is considered normal. If your blood sugar level measures from to , you have impaired fasting glucose, and this may be an indication that you have pre-diabetes. This test is done without any special preparation, such as fasting overnight. If it is and you also have symptoms of type 2 diabetes, you can expect a diagnosis of type 2 diabetes. This test requires you to visit a lab or a healthcare professional after at least an eight-hour fast. At the office or lab, you will drink about eight ounces of a sweet liquid that contains a lot of sugar about 75 grams. Your blood sugar level will be measured before you drink the liquid, then after one hour and again after two hours. Healthcare professionals utilize a combination of medications and lifestyle modifications to treat type 2 diabetes. After being diagnosed with type 2 diabetes, expect to see a healthcare professional to create a treatment plan. It may be necessary to take on daily action steps, such as self-care behaviors, in order to manage diabetes. This also helps healthcare professionals know when the treatment plan needs to be updated. Blood sugar testing is an important part of taking care of type 2 diabetes. The frequency of testing may vary from daily to before and after every meal, and may change after the addition of a medication. It is important to record your blood sugar reading in a reading log. In addition to daily blood sugar testing, periodic testing of blood pressure, blood levels of lipids, as well as the measurement of hemoglobin A1C HbA1C or A1C levels may be needed. A measurement of hemoglobin is a test that estimates average blood sugar levels during a period of three months. In general, the preferred ranges for a person with diabetes are:. Your healthcare professional will create specific goals to meet your needs. Adopting a healthy lifestyle that maintains a calorie-controlled diet and average intensity exercise are two ways people with type 2 diabetes and excess weight can shed pounds. Weight-loss occurs when people burn more calories than they consume. A calorie deficit of calories a day can result in weight-loss of roughly one pound per week. Writing down the food, portion size, and calorie amount in a food diary can help people become aware of what they consume and can provide evidence of calorie intake. Carbohydrates raise blood sugar more than other foods and will cause the body to make more insulin which can result in weight gain. Regular exercise helps maintain weight-loss and prevent regain. It also improves glycemic control and reduces the risk of cardiovascular disease and blood glucose levels. Glycemic control is the measurement of the effects of carbohydrates on sugar level. A goal of 30 minutes of average exercise most days per week should be set. Exercise does not need to occur in a single session to be beneficial. Dividing the activity into multiple, short episodes produces similar benefits and is often more achievable. Achieving the recommended weight loss is a feat that brings great joy to people with diabetes. People noticed a decrease in their insulin requirement and a decrease in weight circumference. However, this is just the beginning. Maintaining the new, lower weight is a different battle. Several studies suggest that 60 to 75 minutes of moderate activity walking or 35 minutes of intense activity jogging daily is needed to maintain a desirable weight loss. To view a PDF version of this brochure, please click here. |
| Breadcrumb | Liraglutide and Cardiovascular Outcomes Chronic hyperglycemia and obesity Type Obesitu Diabetes. Technically, both Calcium in plant-based diets and glucose-lowering medications must be taken for a long time unless they obesitt intolerable, or cessation is obewity indicated due to the safety concerns related to hy;erglycemia possible side-effect. Chronic hyperglycemia and obesity the activation of calpain or mTOR and inhibition of AMP-activated protein kinase AMPK in tissues, including heart and adipose tissue, obesity enhances pro-inflammatory response by decreasing autophagy flux Preventive Services Task Force. All of the relevant financial relationships listed have been mitigated. On this page. Despite the lack of efficacy with respect to glycemic control in this pilot study, the benefits on weight and reduction in insulin dose support the idea that healthy adipose function is important for T1D. |
| Excess Weight and Type 2 Diabetes | Article CAS Chronic hyperglycemia and obesity Google Scholar Belfort R, Glucose supplements Chronic hyperglycemia and obesity, Kashyap S, et al. Jama 9 — In addition, obewity the major components Chroni the cellular membrane, certain phospholipid hypergkycemia also boesity insulin sensitivity by influencing the mitochondrial function, inflammation, production of BAs, and FAs uptake About the OAC Our Purpose Why the OAC Exists OAC Mission, Vision and Goals Our Beliefs and Demands Governance and Financials National Board of Directors Committees Staff Annual Reports Financial Reports For the Media Newsroom Media Requests Media Guidelines Join the OAC Contact Us. Sci Rep |
| REVIEW article | Obesity-induced Metabolism boosters C ceramide production promotes Chronic hyperglycemia and obesity gain and glucose intolerance. Chronic hyperglycemia and obesity potential benefits Cbronic restoring the hormonal output of adipose tissue in T1D was demonstrated via the Chronic hyperglycemia and obesity of recombinant methionyl human leptin metreleptin lbesity individuals hjperglycemia T1D. Hypergylcemia was no difference in CVD outcomes between the two classes in those without a history of CVD. In an observational post hoc analysis of the Look AHEAD trial, weight loss of 10 percent or greater in the first year was associated with a reduction in the primary outcome 1. Environmental factors and hyperglycemia contribute to epigenetic changes in DNA and histones, modulating gene expression in organs implicated in the pathogenesis and progression of T2DM and β-cell function Print Options. |
Chronic hyperglycemia and obesity -
After we eat a meal, the processes of chewing and chemical digestion produce glucose sugar. This is the most readily available form of fuel for our organs- especially muscle and brain tissue. In a normal state, the glucose produced from these digestive processes enters our cells to help with other metabolic processes.
The metabolic process is the making and breaking down of food. Insulin acts as a key that unlocks the door to let glucose in to feed our cells. When insulin is present, it also turns off the process of using glycogen from the liver. This ensures that the glucose levels do not rise further after a meal.
Insulin reduces blood glucose by collecting any excess glucose that is present in the bloodstream so that it can be stored as glycogen for future use.
However, if not enough insulin is available, then this glucose is unable to enter cells. Instead, the glucose remains in the bloodstream in a higher than usual amount. This condition is referred to as elevated blood glucose or hyperglycemia. The more excess weight you have, the more resistant your muscle and tissue cells become to your own insulin hormone.
In addition to excess weight, there are many other facts that increase your risk of developing type 2 diabetes, such as:. Inactivity and having excess weight go hand-in-hand with a diagnosis of type 2 diabetes. A person can decrease insulin resistance by exercising and can lower blood sugar levels.
Too much fat in your diet, not enough fiber, and too many simple carbohydrates all contribute to the development of type 2 diabetes. People who have family members with type 2 diabetes are at a greater risk of developing it themselves. People who have a higher rate of diabetes include:.
As we age, the risk of type 2 diabetes becomes greater. As our cells age, they become more resistant to insulin as well. Not only do these two factors do damage to heart vessels, but they are two key components in metabolic syndrome. Having metabolic syndrome increases the risk of heart disease, stroke and type 2 diabetes.
Women affected by obesity are more insulin resistant when compared to women of normal weight. When pregnant, gestational diabetes generally lasts the length of the pregnancy. There are a variety of blood tests that may indicate whether you have type 2 diabetes.
The amount of sugar in your blood naturally fluctuates but stays within a normal range. The preferred way to test your blood sugar is after fasting overnight for at least eight hours. A fasting blood sugar level less than milligrams of sugar per deciliter of blood is considered normal.
If your blood sugar level measures from to , you have impaired fasting glucose, and this may be an indication that you have pre-diabetes. This test is done without any special preparation, such as fasting overnight. If it is and you also have symptoms of type 2 diabetes, you can expect a diagnosis of type 2 diabetes.
This test requires you to visit a lab or a healthcare professional after at least an eight-hour fast. At the office or lab, you will drink about eight ounces of a sweet liquid that contains a lot of sugar about 75 grams. Your blood sugar level will be measured before you drink the liquid, then after one hour and again after two hours.
Healthcare professionals utilize a combination of medications and lifestyle modifications to treat type 2 diabetes. After being diagnosed with type 2 diabetes, expect to see a healthcare professional to create a treatment plan.
It may be necessary to take on daily action steps, such as self-care behaviors, in order to manage diabetes. This also helps healthcare professionals know when the treatment plan needs to be updated. Blood sugar testing is an important part of taking care of type 2 diabetes. The frequency of testing may vary from daily to before and after every meal, and may change after the addition of a medication.
It is important to record your blood sugar reading in a reading log. Pharmacologic therapy — Pharmacotherapy targeted solely for weight management is effective in patients with type 2 diabetes. Although metformin is usually started for the management of hyperglycemia, it is also frequently an effective medication to promote modest weight loss.
When additional body weight reduction is a primary goal of therapy, we choose medications that promote weight loss and lower glucose. Glucagon-like peptide 1 GLP-1 receptor and dual GLP-1 and glucose-dependent insulinotropic polypeptide GIP agonist therapies promote weight loss and help prevent weight gain due to other glucose-lowering pharmacotherapies.
We add these medications sequentially to metformin if additional glucose lowering or weight loss is a treatment goal. See "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus" and "Obesity in adults: Drug therapy".
Surgical therapy — Weight loss surgery in patients with obesity and type 2 diabetes results in the largest degree of sustained weight loss and, in parallel, improvements in blood glucose management and the most frequent sustained remissions of diabetes. Weight loss surgery is an option to treat poorly managed type 2 diabetes when other modalities have failed.
This topic is reviewed in detail separately. See "Management of persistent hyperglycemia in type 2 diabetes mellitus", section on 'Bariatric metabolic surgery'.
Exercise — Regular exercise is beneficial in type 2 diabetes, independent of weight loss. It leads to improved glycemic management due to increased responsiveness to insulin; it can also delay the progression of impaired glucose tolerance to overt diabetes [ 22,23 ].
These beneficial effects are directly due to exercise, but concurrent weight reduction plays a contributory role. In one study, however, only 50 percent of patients with type 2 diabetes were able to maintain a regular exercise regimen [ 24 ].
See "Exercise guidance in adults with diabetes mellitus". Shorter-duration, intensive exercise may be appropriate for physically fit individuals [ 25 ]. Resistance training may be particularly important for individuals with type 2 diabetes who do not have overweight or obesity, in whom relative sarcopenia may contribute to diabetes pathophysiology [ 26 ].
Intensive lifestyle modification — In patients with established type 2 diabetes, intensive behavioral modification interventions focusing on weight reduction and increasing activity levels are successful in reducing weight and improving glycemic management while, at the same time, reducing the need for glucose-lowering and other medications [ 15,18, ].
The intensive intervention included caloric restriction maximum 30 percent calories from fat, minimum 15 percent protein, and the remainder from carbohydrates, in the form of liquid meal replacements, frozen food entrees, or structured meal plans , moderate-intensity physical activity goal minutes weekly , and weekly group or individual sessions with registered dietitians, behavioral psychologists, and exercise specialists.
The primary outcome was a composite of death from cardiovascular causes, nonfatal myocardial infarction, nonfatal stroke, and hospitalization for angina. Although the anticipated follow-up period was After a median follow-up of 9.
The improvement in weight and glycemia did not reduce the occurrence of cardiovascular events. Possible reasons for this finding include the lower-than-expected rates of cardiovascular events in both groups, improved overall cardiovascular risk factor treatment with medical therapy antihypertensives, statins in the standard diabetes education arm, enrollment of a relatively healthy patient population, gradual weight loss in the control group such that the differential weight loss between the two groups was only 2.
A sustained weight loss of greater than that achieved in the trial may be required to reduce the risk of CVD. In an observational post hoc analysis of the Look AHEAD trial, weight loss of 10 percent or greater in the first year was associated with a reduction in the primary outcome 1.
However, this post hoc analysis is problematic. Moreover, the degree of weight loss is difficult to achieve and maintain through lifestyle intervention alone.
Weight loss, weight loss maintenance, and exercise remain important components of diabetes management due to overall health benefits.
The following summarizes several other major observations from the Look AHEAD trial [ 27,31, ]:. The difference was attenuated but remained significant throughout the trial 6 versus 3. Changes in waist circumference and physical fitness were also significantly better in the intervention group throughout the study.
By study end, mean A1C was significantly lower in the intervention group 7. Psychological interventions — Patients with type 2 diabetes often experience significant stress, a condition often called diabetes distress, related to the many self-care responsibilities required for glycemic management lifestyle modifications, medication, and blood glucose monitoring [BGM] [ 42 ].
Concurrent depression similarly may interfere with self-care. See "Overview of general medical care in nonpregnant adults with diabetes mellitus", section on 'Comorbid conditions'. Psychotherapy reduces psychological distress and improves glycemic management in some [ 43,44 ], but not all [ 45 ], studies.
In a meta-analysis of 12 trials of patients with type 2 diabetes randomly assigned to psychological intervention or usual care, mean A1C was lower in the intervention group pooled mean difference Measures of psychological distress were also significantly lower in the intervention group, but there were no differences in weight management.
Pregnancy planning — All women of childbearing age with diabetes should be counseled about the potential effects of diabetes and commonly used medications on maternal and fetal outcomes and the potential impact of pregnancy on their diabetes management and any existing complications.
See "Pregestational preexisting diabetes: Preconception counseling, evaluation, and management". When to start — Early institution of treatment for diabetes, at a time when the A1C is not substantially elevated, is associated with improved glycemic management over time and decreased long-term complications [ 46 ].
Pharmacologic therapy should be initiated along with consultation for lifestyle modification focusing on dietary and other lifestyle contributors to hyperglycemia. Weight loss and weight loss maintenance underpins all effective type 2 diabetes therapy, and lifestyle change reduces the risk of weight gain associated with sulfonylureas and insulin.
However, for those patients who have clear and modifiable contributors to hyperglycemia and who are motivated to change them eg, commitment to reduce consumption of sugar-sweetened beverages , a three-month trial of lifestyle modification prior to initiation of pharmacologic therapy is warranted.
Choice of initial therapy — Our suggestions are based upon clinical trial evidence and clinical experience in achieving glycemic targets and minimizing adverse effects table 1 , with the recognition that there is a paucity of high-quality, head-to-head drug comparison trials and long-duration trials or ones with important clinical endpoints, such as effects on complications.
The long-term benefits and risks of using one approach over another are unknown. In selecting initial therapy, we consider patient presentation eg, presence or absence of symptoms of hyperglycemia, comorbidities, baseline A1C level , individualized treatment goals and preferences, the glucose-lowering efficacy of individual drugs, and their adverse effect profile, tolerability, and cost [ 47 ].
We prefer initiating a single agent typically metformin and then sequentially adding additional glucose-lowering agents as needed, rather than starting with combination therapy [ 48 ]. Related Pathway s : Diabetes: Initial therapy for non-pregnant adults with type 2 DM.
Asymptomatic, not catabolic — The majority of patients with newly diagnosed type 2 diabetes are asymptomatic, without symptoms of catabolism eg, without polyuria, polydipsia, or unintentional weight loss. Hyperglycemia may be noted on routine laboratory examination or detected by screening.
Metformin — In the absence of specific contraindications, we suggest metformin as initial therapy for patients with newly diagnosed type 2 diabetes who are asymptomatic. We begin with mg once daily with the evening meal and, if tolerated, add a second mg dose with breakfast.
The dose can be increased slowly one tablet every one to two weeks as tolerated to reach a total dose of mg per day. See 'When to start' above and "Metformin in the treatment of adults with type 2 diabetes mellitus", section on 'Dosing'.
Metformin is the preferred initial therapy because of glycemic efficacy see 'Glycemic efficacy' below , promotion of modest weight loss, very low incidence of hypoglycemia, general tolerability, and favorable cost [ 47 ]. Metformin does not have adverse cardiovascular effects, and it appears to decrease cardiovascular events [ ].
See "Metformin in the treatment of adults with type 2 diabetes mellitus", section on 'Cardiovascular effects'. Metformin is far less expensive and has more clinical practice experience than glucagon-like peptide 1 GLP-1 receptor agonists and sodium-glucose cotransporter 2 SGLT2 inhibitors.
Although some guidelines and experts endorse the initial use of these alternative agents as monotherapy or in combination with metformin [ 48,52 ], we prefer initiating a single agent typically metformin and then sequentially adding additional glucose-lowering agents as needed, rather than starting with combination therapy.
In the clinical trials that demonstrated the protective effects of GLP-1 receptor agonists and SGLT2 inhibitors, these agents were added to background metformin therapy in most participants.
Further, the cardiorenal benefits of GLP-1 receptor agonists and SGLT2 inhibitors have not been demonstrated in drug-naïve patients without established CVD or at low cardiovascular risk or without severely increased albuminuria. Although each diabetes medication is associated with adverse events, metformin is associated with less weight gain and fewer episodes of hypoglycemia compared with sulfonylureas, and with less edema, heart failure HF , and weight gain compared with thiazolidinediones.
See "Sodium-glucose cotransporter 2 inhibitors for the treatment of hyperglycemia in type 2 diabetes mellitus", section on 'Cardiovascular effects' and "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus", section on 'Cardiovascular effects'.
Although virtually all recommendations for initial pharmacologic therapy outside of China, where alpha-glucosidase inhibitors are recommended as an alternate first-line monotherapy [ 53 ] endorse use of metformin , there are, in fact, relatively few relevant direct comparative effectiveness data available.
Contraindications to or intolerance of metformin — For patients who have gastrointestinal intolerance of metformin , slower titration, ensuring that the patient is taking the medication with food, or switching to an extended-release formulation may improve tolerability.
For patients who still cannot tolerate metformin or have contraindications to it, we choose an alternative glucose-lowering medication guided initially by patient comorbidities, and in particular, the presence of atherosclerotic CVD ASCVD or albuminuric chronic kidney disease.
See "Metformin in the treatment of adults with type 2 diabetes mellitus", section on 'Contraindications'. When compared with placebo, the GLP-1 receptor agonists liraglutide , semaglutide , and dulaglutide demonstrated favorable atherosclerotic cardiovascular and kidney outcomes [ ].
The SGLT2 inhibitors empagliflozin , canagliflozin , and dapagliflozin have also demonstrated benefit, especially for HF hospitalization, risk of kidney disease progression, and mortality [ ]. Patients at high CVD risk but without a prior event might benefit, but the data are less supportive.
Similarly, patients without severely increased albuminuria have some benefit, but the absolute benefits are greater among those with severely increased albuminuria. To select a medication, we use shared decision-making with a focus on beneficial and adverse effects within the context of the degree of hyperglycemia as well as a patient's comorbidities and preferences.
As examples:. SGLT2 inhibitors with cardiovascular benefit empagliflozin or canagliflozin are good alternatives, especially in the presence of HF. Given the high cost of these classes of medications, formulary coverage often determines the choice of the first medication within the class.
See "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus", section on 'Cardiovascular effects' and "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus", section on 'Microvascular outcomes'.
Choice of agent is primarily dictated by provider preference, insurance formulary restrictions, eGFR, and cost. In the setting of declining eGFR, the main reason to prescribe SGLT2 inhibitors is to reduce progression of DKD.
However, kidney and cardiac benefits have been shown in patients with eGFR below this threshold. Dosing in the setting of DKD is reviewed in detail elsewhere. See "Treatment of diabetic kidney disease", section on 'Type 2 diabetes: Treat with additional kidney-protective therapy'.
An alternative or an additional agent may be necessary to achieve glycemic goals. GLP-1 receptor agonists are an alternative in patients with DKD as their glycemic effect is not related to eGFR.
In addition, GLP-1 receptor agonists have been shown to slow the rate of decline in eGFR and prevent worsening of albuminuria. See 'Microvascular outcomes' below and "Sodium-glucose cotransporter 2 inhibitors for the treatment of hyperglycemia in type 2 diabetes mellitus" and "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus".
Of note, we avoid use of SGLT2 inhibitors in patients with frequent bacterial urinary tract infections or genitourinary yeast infections, low bone density and high risk for falls and fractures, foot ulceration, and factors predisposing to diabetic ketoacidosis eg, pancreatic insufficiency, drug or alcohol abuse disorder because of increased risk while using these agents.
SLGT2 inhibitors should be held for 3 to 4 days before procedures including colonoscopy preparation and with poor oral intake to prevent diabetic ketoacidosis. See "Sodium-glucose cotransporter 2 inhibitors for the treatment of hyperglycemia in type 2 diabetes mellitus", section on 'Contraindications and precautions'.
Repaglinide acts at the sulfonylurea receptor to increase insulin secretion but is much shorter acting than sulfonylureas and is principally metabolized by the liver, with less than 10 percent renally excreted.
Limited data suggest that dipeptidyl peptidase 4 DPP-4 inhibitors are effective and relatively safe in patients with chronic kidney disease. However, linagliptin is the only DPP-4 inhibitor that does not require a dose adjustment in the setting of kidney failure. GLP-1 receptor agonists may also be used safely in chronic kidney disease stage 4, but patient education for signs and symptoms of dehydration due to nausea or satiety is warranted to reduce the risk of acute kidney injury.
Insulin may also be used, with a greater portion of the total daily dose administered during the day due to the risk of hypoglycemia, especially overnight, in chronic kidney disease and end-stage kidney disease ESKD.
See "Management of hyperglycemia in patients with type 2 diabetes and advanced chronic kidney disease or end-stage kidney disease", section on 'Patients not on dialysis'. Without established cardiovascular or kidney disease — For patients without established CVD or kidney disease who cannot take metformin , many other options for initial therapy are available table 1.
We suggest choosing an alternative glucose-lowering medication guided by efficacy, patient comorbidities, preferences, and cost. Although historically insulin has been used for type 2 diabetes only when inadequate glycemic management persists despite oral agents and lifestyle intervention, there are increasing data to support using insulin earlier and more aggressively in type 2 diabetes.
By inducing near normoglycemia with intensive insulin therapy, both endogenous insulin secretion and insulin sensitivity improve; this results in better glycemic management, which can then be maintained with diet, exercise, and oral hypoglycemics for many months thereafter.
Insulin may cause weight gain and hypoglycemia. See "Insulin therapy in type 2 diabetes mellitus", section on 'Indications for insulin'. If type 1 diabetes has been excluded, a GLP-1 receptor agonist is a reasonable alternative to insulin [ 66,67 ]. The frequency of injections and proved beneficial effects in the setting of CVD are the major differences among the many available GLP-1 receptor agonists.
In practice, given the high cost of this class of medications, formulary coverage often determines the choice of the first medication within the class. Cost and insurance coverage may limit accessibility and adherence.
See "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus", section on 'Patient selection'. Each one of these choices has individual advantages, benefits, and risks table 1.
See "Sulfonylureas and meglitinides in the treatment of type 2 diabetes mellitus" and "Sodium-glucose cotransporter 2 inhibitors for the treatment of hyperglycemia in type 2 diabetes mellitus", section on 'Patient selection' and "Dipeptidyl peptidase 4 DPP-4 inhibitors for the treatment of type 2 diabetes mellitus", section on 'Patient selection' and "Thiazolidinediones in the treatment of type 2 diabetes mellitus", section on 'Potential indications'.
See "Sodium-glucose cotransporter 2 inhibitors for the treatment of hyperglycemia in type 2 diabetes mellitus", section on 'Weight loss' and "Dipeptidyl peptidase 4 DPP-4 inhibitors for the treatment of type 2 diabetes mellitus", section on 'Patient selection' and "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus", section on 'Weight loss'.
The choice of sulfonylurea balances glucose-lowering efficacy, universal availability, and low cost with risk of hypoglycemia and weight gain. Pioglitazone , which is generic and another relatively low-cost oral agent, may also be considered in patients with specific contraindications to metformin and sulfonylureas.
However, the risk of weight gain, HF, fractures, and the potential increased risk of bladder cancer raise the concern that the overall risks and cost of pioglitazone may approach or exceed its benefits. See "Sulfonylureas and meglitinides in the treatment of type 2 diabetes mellitus" and "Thiazolidinediones in the treatment of type 2 diabetes mellitus", section on 'Potential indications'.
For patients who are starting sulfonylureas, we suggest initiating lifestyle intervention first, at the time of diagnosis, since the weight gain that often accompanies a sulfonylurea will presumably be less if lifestyle efforts are underway.
However, if lifestyle intervention has not produced a significant reduction in symptoms of hyperglycemia or in glucose values after one or two weeks, then the sulfonylurea should be added. Side effects may be minimized with diabetes self-management education focusing on medication reduction or omission with changes in diet, food accessibility, or activity that may increase the risk of hypoglycemia.
See "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus", section on 'Suggested approach to the use of GLP-1 receptor agonist-based therapies' and "Sodium-glucose cotransporter 2 inhibitors for the treatment of hyperglycemia in type 2 diabetes mellitus", section on 'Mechanism of action' and "Dipeptidyl peptidase 4 DPP-4 inhibitors for the treatment of type 2 diabetes mellitus", section on 'Mechanism of action' and "Thiazolidinediones in the treatment of type 2 diabetes mellitus", section on 'Hypoglycemia'.
Symptomatic catabolic or severe hyperglycemia — The frequency of symptomatic or severe diabetes has been decreasing in parallel with improved efforts to diagnose diabetes earlier through screening. If patients have been drinking a substantial quantity of sugar-sweetened beverages, reduction of carbohydrate intake, and rehydration with sugar-free fluids will help to reduce glucose levels within several days.
See "Insulin therapy in type 2 diabetes mellitus", section on 'Initial treatment'. However, for patients who are injection averse, initial therapy with high-dose sulfonylurea is an alternative option. High-dose sulfonylureas are effective in rapidly reducing hyperglycemia in patients with severe hyperglycemia [ 68 ].
Metformin monotherapy is not helpful in improving symptoms in this setting, because the initial dose is low and increased over several weeks. However, metformin can be started at the same time as the sulfonylurea, slowly titrating the dose upward.
Once the diet has been adequately modified and the metformin dose increased, the dose of sulfonylurea can be reduced and potentially discontinued.
Patients with type 2 diabetes require relatively high doses of insulin compared with those needed for type 1 diabetes. Insulin preparations, insulin regimens, and timing of dosing are discussed in detail elsewhere.
See "Insulin therapy in type 2 diabetes mellitus". See "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus", section on 'Administration'. We typically use glimepiride 4 or 8 mg once daily. An alternative option is immediate-release glipizide 10 mg twice daily or, where available, gliclazide immediate-release 80 mg daily.
We contact the patient every few days after initiating therapy to make dose adjustments increase dose if hyperglycemia does not improve or decrease dose if hyperglycemia resolves quickly or hypoglycemia develops.
See "Sulfonylureas and meglitinides in the treatment of type 2 diabetes mellitus", section on 'Sulfonylureas'. Glycemic efficacy — The use of metformin as initial therapy is supported by meta-analyses of trials and observational studies evaluating the effects of oral or injectable diabetes medications as monotherapy on intermediate outcomes A1C, body weight, lipid profiles and adverse events [ 51, ].
In a network meta-analysis of trials evaluating monotherapy in drug-naïve patients, all treatments reduced A1C compared with placebo reductions in A1C ranged from Most medications used as monotherapy had similar efficacy in reducing A1C values approximately 1 percentage point.
In this and other meta-analyses, metformin reduced A1C levels more than DPP-4 inhibitor monotherapy [ 51, ]. There are few high-quality, head-to-head comparison trials of the available oral agents. In one such trial, A Diabetes Outcome Progression Trial ADOPT , recently diagnosed patients with type 2 diabetes were randomly assigned to monotherapy with the thiazolidinedione rosiglitazone , metformin , or glyburide [ 72 ].
At the four-year evaluation, 40 percent of the subjects in the rosiglitazone group had an A1C value less than 7 percent, as compared with 36 percent in the metformin group and 26 percent in the glyburide group. Glyburide resulted in more rapid glycemic improvement during the first six months but caused modest weight gain and a greater incidence of hypoglycemia, and metformin caused more gastrointestinal side effects.
Rosiglitazone caused greater increases in weight, peripheral edema, and concentrations of low-density lipoprotein LDL cholesterol. There was also an unexpected increase in fractures in women taking rosiglitazone.
The study was limited by a high rate of withdrawal of study participants. Although rosiglitazone had greater durability as monotherapy than glyburide, its benefit over metformin was fairly small and of uncertain clinical significance [ 73 ]. See "Thiazolidinediones in the treatment of type 2 diabetes mellitus", section on 'Safety'.
Cardiovascular outcomes — Cardiovascular benefit has been demonstrated for selected classes of diabetes medications, usually when added to metformin. See "Management of persistent hyperglycemia in type 2 diabetes mellitus", section on 'Monotherapy failure'. The cardiovascular effects of diabetes drugs are reviewed in the individual topics.
See "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus", section on 'Cardiovascular effects' and "Sodium-glucose cotransporter 2 inhibitors for the treatment of hyperglycemia in type 2 diabetes mellitus", section on 'Cardiovascular effects' and "Sulfonylureas and meglitinides in the treatment of type 2 diabetes mellitus", section on 'Cardiovascular effects' and "Thiazolidinediones in the treatment of type 2 diabetes mellitus", section on 'Cardiovascular effects' and "Dipeptidyl peptidase 4 DPP-4 inhibitors for the treatment of type 2 diabetes mellitus", section on 'Cardiovascular effects' and "Insulin therapy in type 2 diabetes mellitus".
In trials of patients with type 2 diabetes with and without chronic kidney disease, GLP-1 receptor agonists slowed the rate of decline in eGFR and prevented worsening of albuminuria [ 54,56,58 ].
These trials and other trials evaluating microvascular outcomes are reviewed in the individual topics. Guidelines — Our approach is largely consistent with American and European guidelines [ 52,74,75 ].
A consensus statement regarding the management of hyperglycemia in type 2 diabetes by the American Diabetes Association ADA and the European Association for the Study of Diabetes EASD was developed in and has been updated regularly, with the most recent revision published in [ 75 ].
The guidelines emphasize the importance of individualizing the choice of medications for the treatment of diabetes, considering important comorbidities CVD, HF, or chronic kidney disease; hypoglycemia risk; and need for weight loss and patient-specific factors including patient preferences, values, and cost [ 75 ].
We also agree with the World Health Organization WHO that sulfonylureas have a long-term safety profile, are inexpensive, and are highly effective, especially when used as described above, with patient education and dose adjustment to minimize side effects [ 76 ].
Blood glucose monitoring BGM is not necessary for most patients with type 2 diabetes who are on a stable regimen of diet or oral agents and who are not experiencing hypoglycemia.
BGM may be useful for some patients with type 2 diabetes who use the results to modify eating patterns, exercise, or insulin doses on a regular basis. See "Glucose monitoring in the ambulatory management of nonpregnant adults with diabetes mellitus", section on 'Type 2 diabetes'. The balance among efficacy in lowering A1C, side effects, and costs must be carefully weighed in considering which drugs or combinations to choose.
Avoiding insulin, the most potent of all hypoglycemic medications, at the expense of poorer glucose management and greater side effects and cost, is not likely to benefit the patient in the long term. See "Management of persistent hyperglycemia in type 2 diabetes mellitus", section on 'Our approach'.
SOCIETY GUIDELINE LINKS — Links to society and government-sponsored guidelines from selected countries and regions around the world are provided separately. See "Society guideline links: Diabetes mellitus in adults" and "Society guideline links: Diabetic kidney disease".
These articles are best for patients who want a general overview and who prefer short, easy-to-read materials. Beyond the Basics patient education pieces are longer, more sophisticated, and more detailed.
These articles are written at the 10 th to 12 th grade reading level and are best for patients who want in-depth information and are comfortable with some medical jargon.
Here are the patient education articles that are relevant to this topic. We encourage you to print or e-mail these topics to your patients. You can also locate patient education articles on a variety of subjects by searching on "patient info" and the keyword s of interest.
Weight reduction through diet, exercise, and behavioral modification can all be used to improve glycemic management, although the majority of patients with type 2 diabetes will require medication.
See 'Diabetes education' above. Glycemic targets are generally set somewhat higher for older adults and for those with comorbidities or a limited life expectancy and little likelihood of benefit from intensive therapy. See 'Glycemic management' above and "Glycemic control and vascular complications in type 2 diabetes mellitus", section on 'Choosing a glycemic target'.
In the absence of specific contraindications, we suggest metformin as initial therapy for most patients Grade 2B. Although some guidelines and experts endorse the initial use of alternative agents as monotherapy or in combination with metformin, we prefer initiating a single agent typically metformin and then sequentially adding additional glucose-lowering agents as needed.
See 'Metformin' above and 'Glycemic efficacy' above. We suggest initiating metformin at the time of diabetes diagnosis Grade 2C , along with consultation for lifestyle intervention. See 'When to start' above. The dose of metformin should be titrated to its maximally effective dose usually mg per day in divided doses over one to two months, as tolerated.
See 'Contraindications to or intolerance of metformin' above. See 'Established cardiovascular or kidney disease' above.
The majority of patients in the cardiovascular and renal outcomes trials had established cardiovascular disease CVD or diabetic kidney disease DKD with severely increased albuminuria, and therefore, these are the primary indications for one of these drugs.
See 'Without established cardiovascular or kidney disease' above. Each one of these choices has individual advantages and risks table 1.
Choice of medication is guided by efficacy, patient comorbidities, preferences, and cost. Sulfonylureas remain a highly effective treatment for hyperglycemia, particularly when cost is a barrier.
Side effects of hypoglycemia and weight gain can be mitigated with careful dosing and diabetes self-management education. For patients who are injection averse, initial therapy with high-dose sulfonylurea is an alternative, particularly for patients who have been consuming large amounts of sugar-sweetened beverages, in whom elimination of carbohydrates can be anticipated to cause a reduction in glucose within several days.
See 'Symptomatic catabolic or severe hyperglycemia' above and "Insulin therapy in type 2 diabetes mellitus". Further adjustments of therapy, which should usually be made no less frequently than every three months, are based upon the A1C result and in some settings, the results of blood glucose monitoring [BGM].
See 'Monitoring' above. See "Management of persistent hyperglycemia in type 2 diabetes mellitus" and "Insulin therapy in type 2 diabetes mellitus". A1C: glycated hemoglobin; CVD: cardiovascular disease; DKA: diabetic ketoacidosis; DPP dipeptidyl peptidase 4; eGFR: estimated glomerular filtration rate; GI: gastrointestinal; GIP: glucose-dependent insulinotropic polypeptide; GLP glucagon-like peptide-1; HF: heart failure; MI: myocardial infarction; SGLT: sodium-glucose co-transporter 2.
The choice of additional therapy should be based on criteria discussed in the UpToDate topics on the management of hyperglycemia in diabetes mellitus. Glycemic Targets.
Diabetes Care ; 39 Suppl 1:S Contributor disclosures are reviewed for conflicts of interest by the editorial group. When found, these are addressed by vetting through a multi-level review process, and through requirements for references to be provided to support the content.
Appropriately referenced content is required of all authors and must conform to UpToDate standards of evidence. Conflict of interest policy. Why UpToDate? Product Editorial Subscription Options Subscribe Sign in. View Topic Loading Font Size Small Normal Large. Initial management of hyperglycemia in adults with type 2 diabetes mellitus.
Formulary drug information for this topic. No drug references linked in this topic. Find in topic Formulary Print Share. Official reprint from UpToDate ® www. com © UpToDate, Inc. All Rights Reserved. Author: Deborah J Wexler, MD, MSc Section Editor: David M Nathan, MD Deputy Editor: Katya Rubinow, MD.
All topics are updated as new evidence becomes available and our peer review process is complete. Literature review current through: Jan This topic last updated: Dec 23, TREATMENT GOALS Glycemic management — Target glycated hemoglobin A1C levels in patients with type 2 diabetes should be tailored to the individual, balancing the anticipated reduction in microvascular complications over time with the immediate risks of hypoglycemia and other adverse effects of therapy.
UK Prospective Diabetes Study UKPDS Group. Lancet ; Holman RR, Paul SK, Bethel MA, et al. N Engl J Med ; Hayward RA, Reaven PD, Wiitala WL, et al. Follow-up of glycemic control and cardiovascular outcomes in type 2 diabetes. ADVANCE Collaborative Group, Patel A, MacMahon S, et al.
Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. Action to Control Cardiovascular Risk in Diabetes Study Group, Gerstein HC, Miller ME, et al.
Effects of intensive glucose lowering in type 2 diabetes. Rawshani A, Rawshani A, Franzén S, et al. Risk Factors, Mortality, and Cardiovascular Outcomes in Patients with Type 2 Diabetes.
Gaede P, Vedel P, Larsen N, et al. Multifactorial intervention and cardiovascular disease in patients with type 2 diabetes. Kazemian P, Shebl FM, McCann N, et al. Evaluation of the Cascade of Diabetes Care in the United States,
The prevalence hylerglycemia obesity Chronic hyperglycemia and obesity diabetes mellitus DM has been consistently increasing worldwide. Sharing Pre-exercise meal ideas genetic Chronic hyperglycemia and obesity environmental features in their pathogenesis, obesity amplifies the obesityy of genetic susceptibility and environmental Chronci on DM. The ectopic Chronic hyperglycemia and obesity of adipose tissue and excessive obestiy of certain nutrients and metabolites sabotage the metabolic balance via insulin resistance, dysfunctional autophagy, and microbiome-gut-brain axis, further exacerbating the dysregulation of immunometabolism through low-grade systemic inflammation, leading to an accelerated loss of functional β-cells and gradual elevation of blood glucose. Given these intricate connections, most available treatments of obesity and type 2 DM T2DM have a mutual effect on each other. For example, anti-obesity drugs can be anti-diabetic to some extent, and some anti-diabetic medicines, in contrast, have been shown to increase body weight, such as insulin.
Ich meine, dass Sie nicht recht sind. Es ich kann beweisen. Schreiben Sie mir in PM, wir werden reden.
Sie versuchten nicht, in google.com zu suchen?
Einem Gott ist es bekannt!
die Maßgebliche Mitteilung:), wissenswert...
Kann sein.