
Hypertension is riwk most prevalent cajcer in cancer patients. Consequently, many cancer patients are xnd antihypertensive drugs before cancer diagnosis or during cancer treatment.
Body recomposition meal plan, whether antihypertensive Htpertension affect the incidence, treatment efficacy, or prognosis of cancer remains unanswered.
Wnd instance, Hypertension and cancer risk and β-adrenergic signaling may be involved not Collagen-boosting treatments in blood risl elevation but also in cell anc, angiogenesis, and cahcer invasion. Therefore, the inhibition ridk these pathways may Hydration and body temperature regulation beneficial effects on cancer prevention or treatment.
Hypeftension this article, we vancer several studies regarding antihypertensive drugs and cancer. In xnd, we focused on the results of Hypertnesion trials to evaluate whether the Hyprrtension of antihypertensive drugs affects future cancer risk Hyprtension prognosis.
Unfortunately, the results are somewhat inconsistent, and evidence demonstrating the effect of antihypertensive drugs remains limited. We indicate that the heterogeneity in the study designs makes it difficult to Hypertenssion the causal Hypetension between antihypertensive drugs and cancer.
We also propose that additional experimental studies, including research with Hypertenxion pluripotent cells derived Immune system health cancer patients, single-cell analyses of cancer cancwr clusters, canced clinical studies using artificial intelligence Hypertendion health record systems, might be helpful to reveal the precise association between antihypertensive drugs and Hypertensio risk.
Cancer is Hypertensino worldwide health concern, with Numerous reports have also demonstrated a Collagen-boosting treatments Hypertensioh antihypertensive an and several types of cancer.
A vast number rism reports have evaluated the association between antihypertensive drugs and Hypertensoon, including basic research, epidemiological Hypertsnsion, and cancerr controlled ad. Although basic research has provided us with detailed and precise Plant-based nutrition linking antihypertensive Collagen-boosting treatments yHpertension cancer, Hyeprtension that can reproduce human disease are limited.
Furthermore, epidemiological data are problematic caner to its retrospective riks, and cannot exclude some types of bias, Htpertension as canncer bias, information bias, Hypertensio ascertainment bias. Indeed, a Hypertrnsion study cancef Hypertension and cancer risk the frequency of neoplasm became threefold higher in valsartan-treated patients after the announcement by the Food and Drug Hy;ertension that some riek drugs of valsartan cxncer a potential carcinogenic Hyperteneion, N -nitrosodimethylamine, which might be attributable to recall bias.
Pancreatic tumor addition, the duration Hypertensikn these cacner was too short to Hypertensoon some types of cancer, Memory improvement techniques rare cancer types could not be considered.
Nevertheless, we Fat burner reviews various Hyppertension of literature focusing on antihypertensive Hy;ertension and cancer canxer or prognosis.
In addition, we described the unsolved issues rixk this Hyertension. In a meta-analysis yHpertension randomized control Hypertension and cancer risk, antihypertensive drugs were reportedly not associated with cancer risk.
A Improved attention span analysis of the U. Kidney Cancer Study showed that RCC, which Hyperrension been reported to be associated disk hypertension, Hypeertension was not related to specific riso of antihypertensive agents. Similarly, Hyprtension drugs were not associated with the incidence of Prediabetes weight gain cancer in a meta-analysis of observational studies.
On the basis of these results, it is Resilience that the relationship, Hypertenwion any, between antihypertensive drugs and cancer might Mobility exercises for performance depending on the Hyprrtension of cancer and the class of antihypertensive agent.
Moreover, rsik hypertension is a reported canfer factor for cancer incidence, 3riskk and there are shared risk Hyperteension between cancfr and cancer, such as obesity, diabetes, smoking, and high sodium Hylertension, 30 they may be rsk factors for the association between antihypertensive drugs and cancer.
In the following sections, we discuss Weight management program relationship between each antihypertensive drug class and various types of cancer. The renin—angiotensin system RAS is involved in the regulation of cell Hypertenslon, angiogenesis, Caffeine and blood pressure tumor progression, andd RAS genes are expressed in most Avocado Bruschetta Ideas, such as breast, prostate, colorectal, lung, and renal cancers.
Indeed, in mice subcutaneously injected Hypertension and cancer risk melanoma cells or prostate cancer cells, tumor growth Hypdrtension significantly suppressed Hypeftension ARBs. Notably, clinical risj are not necessarily consistent with Hyperteension research results Table 1.
Inthe CHARM Hypertensikn evaluated Hypertenxion cardiovascular Hyertension of ARBs for patients with a reduced ejection fraction 37 and showed that treatment with candesartan significantly reduced cardiovascular deaths, but cancer-related deaths were significantly higher in the ARB-treated group.
Following this trial, several studies evaluated the association between RAS inhibitor use and cancer occurrence or death. Similar to the CHARM trial, a meta-analysis of randomized studies reported in indicated that the use of ARBs was associated with new cancer diagnoses.
However, a growing body of evidence contradicts this conclusion. For example, a study summarized 15 large multicenter double-blind trials evaluating the influence of ARB use on cancer risk and showed that patients treated with RAS inhibitors for more than 1 year did not have a higher risk of overall or site-specific cancer occurrence.
On the other hand, Shen et al. In this study, 41 a beneficial effect was observed for lung cancer but not other cancers, different from the results of the CHARM trial.
Advantages and disadvantages and major meta-analyses of the association between RAS inhibitors and certain cancer types. Abbreviations: ACE-I, angiotensin-converting enzyme inhibitor; ARB, angiotensin II receptor blocker; BCC, basal cell carcinoma; CI, confidence interval; DFS, disease-free survival; HR, hazard ratio; OR, odds ratio; OS, overall survival; PFS, progression-free survival; RAS, renin—angiotensin system; RCT, randomized controlled trial; RR, relative risk; SCC, squamous cell carcinoma.
For individual types of cancer, the relationship between RAS inhibitors and cancer risk is inconsistent. In a population-based cohort study in the United Kingdom, Hicks et al. In contrast, the results of other meta-analyses showed that RAS inhibitor use was not associated with the incidence of prostate, skin, breast, and ovarian cancer.
Similarly, in a meta-analysis of observational studies, although overall antihypertensive treatment was not associated with breast cancer risk, the use of RAS inhibitors for more than 10 years was correlated to a reduced risk of breast cancer.
There have been inconsistent results regarding the effects of ARBs and ACE-Is on cancer incidence. Lin et al. They speculated that this difference resulted from increased levels of bradykinin and substance P in the lung, which are indicated to be involved in promoting cancer.
In addition, a report using the Danish Registry System suggested that ARB but not ACE-I use was associated with malignant melanoma. Several reports have evaluated the effect of RAS inhibitors on cancer prognosis.
McMenamin et al. Similarly, Busby et al. In a cohort from the Finland Cancer Registry, Santala et al. These data suggest that RAS inhibitors might be beneficial, even if they are initiated after cancer diagnosis.
Collectively, these data suggest that RAS inhibitors might ameliorate cancer progression in certain types of cancer. However, no randomized control studies have investigated this issue. The benefit of RAS inhibitors is also related to specific cancer treatments i. Tanaka et al.
According to these results, we can expect significant effects of RAS inhibitors combined with various types of chemotherapy. Tozuka et al. Similarly, Nakai et al. For gastric cancer patients, the use of RAS inhibitors with platinum-based chemotherapy was associated with better overall survival but not progression-free survival.
In summary, although experimental models suggest that RAS inhibitors might exert beneficial effects on cancer growth, the outcomes of clinical studies are somewhat inconsistent.
In addition, because some of the results were obtained from insurance databases, the information may be unreliable. There are concerns that the use of CCBs might be associated with cancer incidence because they were shown to inhibit cell apoptosis in mice, potentially leading to cancer occurrence.
Panneerpandian et al. Moreover, in epithelial ovarian cancer cell lines, Lee et al. Pan et al. Collectively, these basic studies suggest that the use of CCBs may be beneficial for alleviating cancer growth. However, clinical studies have not supported this supposition.
Cohen et al. Importantly, these results were independent of blood pressure changes, CCB classes, or follow-up durations.
Similarly, Rosenberg et al. This result was similar for those who used CCBs for more than 5 years. In this study, CCBs were related to an increased risk of kidney cancer. However, the authors noted that this outcome might be attributed to hypertension itself because ACE-I or β-blocker users also showed a higher incidence of kidney cancer.
Moreover, Pahor et al. Regarding specific cancer sites, although it was reported that CCBs were associated with a lower prevalence of gastric cancer in Helicobacter pylori -infected patients with hypertension, 67 previous meta-analyses of retrospective case—control studies indicated that the use of CCBs might be associated with an increased incidence of lung cancer, 68 skin cancer, 24 and prostate cancer.
Kristensen et al. Similarly, Li et al. They demonstrated that CCBs users showed a lower concentration of sRAGE, which corresponded to a higher incidence rate of pancreatic cancer in postmenopausal women. For cancer prognosis, Nayan et al. In summary, although several studies have reported the association between CCB use and cancer incidence in specific tumors, the clinical data are somewhat inconsistent 13222464—6668 Table 2.
Notably, most clinical studies evaluating the association between CCBs and cancer were based on a retrospective analysis of medical records, making it difficult to draw a definite conclusion.
Indeed, some experimental models showed the benefit of this drug for cancer suppression in vitro. Advantages and disadvantages and major meta-analyses of the association between calcium channel blockers CCBs and certain cancer types.
Abbreviations: BCC, basal cell carcinoma; CI, confidence interval; HR, hazard ratio; OR, odds ratio; OS, overall survival; RCT, randomized controlled trial; RR, relative risk; SCC, squamous cell carcinoma; SRR, summary relative risk.
Recently, the association between thiazide diuretics and skin cancer has attracted attention. Similarly, the incidence of lip cancers, most of which are squamous cell carcinomas, was dose dependently increased with the use of thiazide diuretics in patients from a Danish registry.
In Denmark, the proportion of hydrochlorothiazide prescriptions among antihypertensive drugs decreased from The association between thiazide diuretics and skin cancer is generally explained by their photosensitizing effects, which are caused by interactions between ultraviolet radiation and cells in the skin 79 and may be influenced by sun sensitivity and the absorption spectrum.
However, notably, a recent meta-analysis, which only included randomized control studies, did not support the association between thiazide diuretics and skin cancer. Several reports have also indicated an association between thiazides and other types of cancer.
For ovarian cancer, an analysis of the NHS reported that antihypertensive medicine but not hypertension itself was associated with the occurrence of ovarian cancer, mainly because of the use of thiazide diuretics.
Similarly, for endometrial cancer, thiazide use but not hypertension was independently associated with the occurrence of endometrial cancer in a population-based case—control study in America. In summary, although there are potential concerns regarding the association between thiazide diuretics and skin cancer, 107576 the mechanism has not yet been fully clarified.
Furthermore, the results from most studies that support this association were obtained from retrospective nationwide registries, and the findings of randomized control studies are not necessarily consistent Table 3.
Further prospective studies are necessary to conclude whether thiazide use should be avoided for patients at risk of skin cancer. Advantages and disadvantages and major meta-analyses of the association between diuretics and certain cancer types. Abbreviations: BCC, basal cell carcinoma; CI, confidence interval; HR, hazard ratio; OR, odds ratio; RR, relative risk; SCC, squamous cell carcinoma.
β-Adrenergic signaling is involved in the upregulation of genes related to inflammation, angiogenesis, tissue invasion, and epithelial—mesenchymal transition in tumor cells.
Whether β-blockers are beneficial for cancer prevention or treatment in clinical settings remains unclear.
: Hypertension and cancer risk| Etiology and management of hypertension in patients with cancer | Antihypertensive drug use and breast cancer risk: a meta-analysis of observational studies. Oncotarget ; 8 : — Genetically proxied therapeutic inhibition of antihypertensive drug targets and risk of common cancers: a Mendelian randomization analysis. PLoS Med ; 19 : e Markozannes G , Kanellopoulou A , Dimopoulou O , Kosmidis D , Zhang X , Wang L , Theodoratou E , Gill D , Burgess S , Tsilidis KK. Systematic review of Mendelian randomization studies on risk of cancer. BMC Med ; 20 : Koene RJ , Prizment AE , Blaes A , Konety SH. Shared risk factors in cardiovascular disease and cancer. Circulation ; : — Khoshghamat N , Jafari N , Toloue-Pouya V , Azami S , Mirnourbakhsh SH , Khazaei M , Ferns GA , Rajabian M , Avan A. The therapeutic potential of renin-angiotensin system inhibitors in the treatment of pancreatic cancer. Life Sci ; : Downward J. Targeting RAS signalling pathways in cancer therapy. Nat Rev Cancer ; 3 : 11 — Clinical applicability of renin-angiotensin system inhibitors in cancer treatment. Am J Cancer Res ; 11 : — Pinter M , Jain RK. Targeting the renin-angiotensin system to improve cancer treatment: implications for immunotherapy. Sci Transl Med ; 9 : eaan Egami K , Murohara T , Shimada T , Sasaki K , Shintani S , Sugaya T , Ishii M , Akagi T , Ikeda H , Matsuishi T , Imaizumi T. Role of host angiotensin II type 1 receptor in tumor angiogenesis and growth. J Clin Invest ; : 67 — Kosaka T , Miyajima A , Takayama E , Kikuchi E , Nakashima J , Ohigashi T , Asano T , Sakamoto M , Okita H , Murai M , Hayakawa M. Angiotensin II type 1 receptor antagonist as an angiogenic inhibitor in prostate cancer. Prostate ; 67 : 41 — Pfeffer MA , Swedberg K , Granger CB , Held P , McMurray JJ , Michelson EL , Olofsson B , Ostergren J , Yusuf S , Pocock S. Effects of candesartan on mortality and morbidity in patients with chronic heart failure: the CHARM-Overall programme. Lancet ; : — Sipahi I , Debanne SM , Rowland DY , Simon DI , Fang JC. Angiotensin-receptor blockade and risk of cancer: meta-analysis of randomised controlled trials. Lancet Oncol ; 11 : — Collaboration AT. Effects of telmisartan, irbesartan, valsartan, candesartan, and losartan on cancers in 15 trials enrolling , individuals. J Hypertens ; 29 : — Datzmann T , Fuchs S , Andree D , Hohenstein B , Schmitt J , Schindler C. Systematic review and meta-analysis of randomised controlled clinical trial evidence refutes relationship between pharmacotherapy with angiotensin-receptor blockers and an increased risk of cancer. Eur J Intern Med ; 64 : 1 — 9. Renin-angiotensin system blockade for the risk of cancer and death. J Renin Angiotensin Aldosterone Syst ; 17 : Hicks BM , Filion KB , Yin H , Sakr L , Udell JA , Azoulay L. Angiotensin converting enzyme inhibitors and risk of lung cancer: population based cohort study. BMJ ; : k Meier CR , Derby LE , Jick SS , Jick H. Angiotensin-converting enzyme inhibitors, calcium channel blockers, and breast cancer. Arch Intern Med ; : — Christian JB , Lapane KL , Hume AL , Eaton CB , Weinstock MA , Trial V. Association of ACE inhibitors and angiotensin receptor blockers with keratinocyte cancer prevention in the randomized VATTC trial. J Natl Cancer Inst ; : — Association between angiotensin-converting enzyme inhibitors and lung cancer—a nationwide, population-based, propensity score-matched cohort study. Cancers ; 12 : Schmidt SA , Schmidt M , Mehnert F , Lemeshow S , Sørensen HT. Use of antihypertensive drugs and risk of skin cancer. J Eur Acad Dermatol Venereol ; 29 : — McMenamin U , Murray LJ , Cantwell MM , Hughes CM. Angiotensin-converting enzyme inhibitors and angiotensin receptor blockers in cancer progression and survival: a systematic review. Cancer Causes Control ; 23 : — Busby J , McMenamin U , Spence A , Johnston BT , Hughes C , Cardwell CR. Angiotensin receptor blocker use and gastro-oesophageal cancer survival: a population-based cohort study. Aliment Pharmacol Ther ; 47 : — Santala EE , Rannikko A , Murtola TJ. Antihypertensive drugs and prostate cancer survival after radical prostatectomy in Finland—a nationwide cohort study. Santala EEE , Artama M , Pukkala E , Visvanathan K , Staff S , Murtola TJ. Antihypertensive drug use and the risk of ovarian cancer death among Finnish ovarian cancer patients—a nationwide cohort study. Cancers ; 13 : Santala EEE , Murto MO , Artama M , Pukkala E , Visvanathan K , Murtola TJ. Angiotensin receptor blockers associated with improved breast cancer survival—a nationwide cohort study from Finland. Cancer Epidemiol Biomarkers Prev ; 29 : — Tanaka N , Miyajima A , Kosaka T , Shirotake S , Hasegawa M , Kikuchi E , Oya M. Cis-dichlorodiammineplatinum upregulates angiotensin II type 1 receptors through reactive oxygen species generation and enhances VEGF production in bladder cancer. Mol Cancer Ther ; 9 : — Acquired platinum resistance enhances tumour angiogenesis through angiotensin II type 1 receptor in bladder cancer. Br J Cancer ; : — Anandanadesan R , Gong Q , Chipitsyna G , Witkiewicz A , Yeo CJ , Arafat HA. J Gastrointest Surg ; 12 : 57 — Cortez-Retamozo V , Etzrodt M , Newton A , Ryan R , Pucci F , Sio SW , Kuswanto W , Rauch PJ , Chudnovskiy A , Iwamoto Y , Kohler R , Marinelli B , Gorbatov R , Wojtkiewicz G , Panizzi P , Mino-Kenudson M , Forghani R , Figueiredo JL , Chen JW , Xavier R , Swirski FK , Nahrendorf M , Weissleder R , Pittet MJ. Angiotensin II drives the production of tumor-promoting macrophages. Immunity ; 38 : — Tozuka T , Yanagitani N , Yoshida H , Manabe R , Ogusu S , Tsugitomi R , Sakamoto H , Amino Y , Ariyasu R , Uchibori K , Kitazono S , Seike M , Gemma A , Nishio M. Anticancer Res ; 41 : — Nakai Y , Isayama H , Ijichi H , Sasaki T , Sasahira N , Hirano K , Kogure H , Kawakubo K , Yagioka H , Yashima Y , Mizuno S , Yamamoto K , Arizumi T , Togawa O , Matsubara S , Tsujino T , Tateishi K , Tada M , Omata M , Koike K. Inhibition of renin-angiotensin system affects prognosis of advanced pancreatic cancer receiving gemcitabine. How does inhibition of the renin-angiotensin system affect the prognosis of advanced gastric cancer patients receiving platinum-based chemotherapy? Oncology ; 83 : — Rachow T , Schiffl H , Lang SM. Risk of lung cancer and renin-angiotensin blockade: a concise review. J Cancer Res Clin Oncol ; : — Ray SD , Kamendulis LM , Gurule MW , Yorkin RD , Corcoran GB. FASEB J ; 7 : — Panneerpandian P , Rao DB , Ganesan K. Toxicol In Vitro ; 74 : Calcium channels as novel therapeutic targets for ovarian cancer stem cells. Int J Mol Sci ; 21 : Dihydropyridine calcium channel blockers suppress the transcription of PD-L1 by inhibiting the activation of STAT1. Front Pharmacol ; 11 : Cohen HJ , Pieper CF , Hanlon JT , Wall WE , Burchett BM , Havlik RJ. Calcium channel blockers and cancer. Am J Med ; : — Rosenberg L , Rao RS , Palmer JR , Strom BL , Stolley PD , Zauber AG , Warshauer ME , Shapiro S. Calcium channel blockers and the risk of cancer. Pahor M , Guralnik JM , Ferrucci L , Corti MC , Salive ME , Cerhan JR , Wallace RB , Havlik RJ. Calcium-channel blockade and incidence of cancer in aged populations. Li B , Cheung KS , Wong IY , Leung WK , Law S. Calcium channel blockers are associated with lower gastric cancer risk: a territory-wide study with propensity score analysis. Rotshild V , Azoulay L , Feldhamer I , Perlman A , Glazer M , Muszkat M , Matok I. Calcium channel blockers and the risk for lung cancer: a population-based nested case-control study. Ann Pharmacother ; 53 : — Li CI , Daling JR , Tang MT , Haugen KL , Porter PL , Malone KE. Use of antihypertensive medications and breast cancer risk among women aged 55 to 74 years. JAMA Intern Med ; : — Bergman GJ , Khan S , Danielsson B , Borg N. Breast cancer risk and use of calcium channel blockers using Swedish population registries. Wang Z , White DL , Hoogeveen R , Chen L , Whitsel EA , Richardson PA , Virani SS , Garcia JM , El-Serag HB , Jiao L. J Clin Med ; 7 : Nayan M , Juurlink DN , Austin PC , Macdonald EM , Finelli A , Kulkarni GS , Hamilton RJ ; Canadian Drug Safety and Effectiveness Research Network CDSERN. Medication use and kidney cancer survival: a population-based study. Use of antihypertensive medications and survival rates for breast, colorectal, lung, or stomach cancer. Kreutz R , Algharably EAH , Douros A. Reviewing the effects of thiazide and thiazide-like diuretics as photosensitizing drugs on the risk of skin cancer. J Hypertens ; 37 : — Pottegård A , Pedersen SA , Schmidt SAJ , Hölmich LR , Friis S , Gaist D. Association of hydrochlorothiazide use and risk of malignant melanoma. Rouette J , Yin H , Pottegård A , Nirantharakumar K , Azoulay L. Use of hydrochlorothiazide and risk of melanoma and nonmelanoma skin cancer. Drug Saf ; 44 : — Pottegård A , Hallas J , Olesen M , Svendsen MT , Habel LA , Friedman GD , Friis S. Hydrochlorothiazide use is strongly associated with risk of lip cancer. J Intern Med ; : — Pottegård A , Bech BH , Pedersen SA , Christensen B. Use of hydrochlorothiazide in Denmark following publication of skin cancer risk findings. Pharmacoepidemiol Drug Saf ; 30 : — Moore DE. Drug-induced cutaneous photosensitivity: incidence, mechanism, prevention and management. Drug Saf ; 25 : — Photosensitizing medications and photocarcinogenesis. Photodermatol Photoimmunol Photomed ; 30 : 8 — Schneider R , Reinau D , Stoffel S , Jick SS , Meier CR , Spoendlin J. Risk of skin cancer in new users of thiazides and thiazide-like diuretics: a cohort study using an active comparator group. Br J Dermatol ; : — Fortuny J , Sima C , Bayuga S , Wilcox H , Pulick K , Faulkner S , Zauber AG , Olson SH. Risk of endometrial cancer in relation to medical conditions and medication use. Cancer Epidemiol Biomarkers Prev ; 18 : — Cole SW , Sood AK. Molecular pathways: beta-adrenergic signaling in cancer. Clin Cancer Res ; 18 : — Kamiya A , Hayama Y , Kato S , Shimomura A , Shimomura T , Irie K , Kaneko R , Yanagawa Y , Kobayashi K , Ochiya T. Genetic manipulation of autonomic nerve fiber innervation and activity and its effect on breast cancer progression. Nat Neurosci ; 22 : — Fumagalli C , Maurizi N , Marchionni N , Fornasari D. β-Blockers: their new life from hypertension to cancer and migraine. Pharmacol Res ; : Coelho M , Soares-Silva C , Brandão D , Marino F , Cosentino M , Ribeiro L. β-Adrenergic modulation of cancer cell proliferation: available evidence and clinical perspectives. Brohée L , Peulen O , Nusgens B , Castronovo V , Thiry M , Colige AC , Deroanne CF. Propranolol sensitizes prostate cancer cells to glucose metabolism inhibition and prevents cancer progression. Sci Rep ; 8 : Saad A , Goldstein J , Margalit O , Shacham-Shmueli E , Lawrence YR , Yang YX , Reiss KA , Golan T , Mamtani R , Halpern N , Aderka D , Mouallem M , Goldstein A , Giantonio B , Boursi B. Assessing the effects of beta-blockers on pancreatic cancer risk: a nested case-control study. Pharmacoepidemiol Drug Saf ; 29 : — Kim MS , Han KD , Kwon SY. Pre-diagnostic beta-blocker use and head- and neck cancer risk: a nationwide population-based case-control study. Medicine ; 98 : e Zheng G , Sundquist J , Sundquist K , Ji J. Beta-blockers use and risk of breast cancer in women with hypertension. Cancer Epidemiol Biomarkers Prev ; 30 : — Effect of antihypertensive drugs on breast cancer risk in female hypertensive patients: evidence from observational studies. Clin Exp Hypertens ; 40 : 22 — Yap A , Lopez-Olivo MA , Dubowitz J , Pratt G , Hiller J , Gottumukkala V , Sloan E , Riedel B , Schier R. Effect of beta-blockers on cancer recurrence and survival: a meta-analysis of epidemiological and perioperative studies. Br J Anaesth ; : 45 — Sørensen GV , Ganz PA , Cole SW , Pedersen LA , Sørensen HT , Cronin-Fenton DP , Garne JP , Christiansen PM , Lash TL , Ahern TP. Use of β-blockers, angiotensin-converting enzyme inhibitors, angiotensin II receptor blockers, and risk of breast cancer recurrence: a Danish nationwide prospective cohort study. J Clin Oncol ; 31 : — The effects of beta-blocker use on cancer prognosis: a meta-analysis based on , patients. Onco Targets Ther ; 11 : — Jansen L , Weberpals J , Kuiper JG , Vissers PAJ , Wolkewitz M , Hoffmeister M , Brenner H. Pre- and post-diagnostic beta-blocker use and prognosis after colorectal cancer: results from a population-based study. Int J Cancer ; : 62 — Beta-blocker and survival in patients with lung cancer: a meta-analysis. PLoS One ; 16 : e β-Blocker use is not associated with improved clinical outcomes in women with breast cancer: a meta-analysis. Biosci Rep ; 40 : BSR β-Blocker use and mortality in cancer patients: systematic review and meta-analysis of observational studies. Eur J Cancer Prev ; 25 : — Udumyan R , Montgomery S , Fang F , Almroth H , Valdimarsdottir U , Ekbom A , Smedby KE , Fall K. Beta-blocker drug use and survival among patients with pancreatic adenocarcinoma. Cancer Res ; 77 : — Raimondi S , Botteri E , Munzone E , Cipolla C , Rotmensz N , DeCensi A , Gandini S. Use of beta-blockers, angiotensin-converting enzyme inhibitors and angiotensin receptor blockers and breast cancer survival: systematic review and meta-analysis. Couttenier A , Lacroix O , Silversmit G , Vaes E , De Schutter H , Robert A. Beta-blocker use and mortality following ovarian cancer diagnosis: a population-based study. Cancer Epidemiol ; 62 : Farrugia MK , Ma SJ , Mattson DM , Flaherty L , Repasky EA , Singh AK. Concurrent β-blocker use is associated with improved outcome in esophageal cancer patients who undergo chemoradiation: a retrospective matched-pair analysis. Am J Clin Oncol ; 43 : — Reda S , Ahl R , Szabo E , Stenberg E , Forssten MP , Sjolin G , Cao Y , Mohseni S. Pre-operative beta-blocker therapy does not affect short-term mortality after esophageal resection for cancer. BMC Surg ; 20 : Ahl R , Matthiessen P , Fang X , Cao Y , Sjolin G , Lindgren R , Ljungqvist O , Mohseni S. Effect of beta-blocker therapy on early mortality after emergency colonic cancer surgery. Br J Surg ; : — Ahl R , Matthiessen P , Sjölin G , Cao Y , Wallin G , Ljungqvist O , Mohseni S. Effects of beta-blocker therapy on mortality after elective colon cancer surgery: a Swedish nationwide cohort study. BMJ Open ; 10 : e Wade CA , Goodwin J , Preston D , Kyprianou N. Impact of α-adrenoceptor antagonists on prostate cancer development, progression and prevention. Am J Clin Exp Urol ; 7 : 46 — Lin SC , Chueh SC , Hsiao CJ , Li TK , Chen TH , Liao CH , Lyu PC , Guh JH. Prazosin displays anticancer activity against human prostate cancers: targeting DNA and cell cycle. Neoplasia ; 9 : — Prazosin inhibits the proliferation and survival of acute myeloid leukaemia cells through down-regulating TNS1. Biomed Pharmacother ; : Assad Kahn S , Costa SL , Gholamin S , Nitta RT , Dubois LG , Fève M , Zeniou M , Coelho PL , El-Habr E , Cadusseau J , Varlet P , Mitra SS , Devaux B , Kilhoffer MC , Cheshier SH , Moura-Neto V , Haiech J , Junier MP , Chneiweiss H. The anti-hypertensive drug prazosin inhibits glioblastoma growth via the PKCδ-dependent inhibition of the AKT pathway. EMBO Mol Med ; 8 : — Van Rompay MI , Curtis Nickel J , Ranganathan G , Kantoff PW , Solomon KR , Lund JL , McKinlay JB. Impact of 5α-reductase inhibitor and α-blocker therapy for benign prostatic hyperplasia on prostate cancer incidence and mortality. BJU Int ; : — Hart J , Spencer B , McDermott CM , Chess-Williams R , Sellers D , Christie D , Anoopkumar-Dukie S. A pilot retrospective analysis of alpha-blockers on recurrence in men with localised prostate cancer treated with radiotherapy. Sci Rep ; 10 : Murtola TJ , Tammela TL , Määttänen L , Ala-Opas M , Stenman UH , Auvinen A. Prostate cancer incidence among finasteride and alpha-blocker users in the Finnish Prostate Cancer Screening Trial. Martin FM , Harris AM , Rowland RG , Conner W , Lane M , Durbin E , Baron AT , Kyprianou N. Decreased risk of bladder cancer in men treated with quinazoline-based α1-adrenoceptor antagonists. Gene Ther Mol Biol ; 12 : — Sung SY , Le TTH , Chen JH , Hsieh TF , Hsieh CL. Alpha-1 blocker use increased risk of subsequent renal cell carcinoma: a nationwide population-based study in Taiwan. PLoS One ; 15 : e Greenblatt DJ , Koch-Weser J. Gynecomastia and impotence: complications of spironolactone therapy. JAMA ; : Kowalczyk W , Waliszczak G , Jach R , Dulińska-Litewka J. Steroid receptors in breast cancer: understanding of molecular function as a basis for effective therapy development. Glucocorticoid and mineralocorticoid cross-talk with progesterone receptor to induce focal adhesion and growth inhibition in breast cancer cells. Endocrinology ; : — Mineralocorticoid receptor suppresses cancer progression and the Warburg effect by modulating the miRp-PKLR axis in hepatocellular carcinoma. Hepatology ; 62 : — Hiebert BM , Janzen BW , Sanjanwala RM , Ong AD , Feldman RD , Kim JO. Impact of spironolactone exposure on prostate cancer incidence amongst men with heart failure: a pharmacoepidemiological study. Br J Clin Pharmacol ; 87 : — Spironolactone and the risk of urinary tract cancer in patients with hypertension: a nationwide population-based retrospective case-control study. J Hypertens ; 35 : — Wei C , Bovonratwet P , Gu A , Moawad G , Silverberg JI , Friedman AJ. Spironolactone use does not increase the risk of female breast cancer recurrence: a retrospective analysis. J Am Acad Dermatol ; 83 : — Biggar RJ , Andersen EW , Wohlfahrt J , Melbye M. Spironolactone use and the risk of breast and gynecologic cancers. Cancer Epidemiol ; 37 : — Mackenzie IS , Morant SV , Wei L , Thompson AM , MacDonald TM. Spironolactone use and risk of incident cancers: a retrospective, matched cohort study. Br J Clin Pharmacol ; 83 : — Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide. Sign In or Create an Account. Navbar Search Filter American Journal of Hypertension This issue Therapeutics Biological Sciences Cardiovascular Medicine Books Journals Oxford Academic Mobile Enter search term Search. Issues More Content Advance articles Editor's Choice Submit Graphical Abstracts and Tidbit Author Guidelines Submission Site Open Access Purchase Alerts About About American Journal of Hypertension Editorial Board Board of Directors Advertising and Corporate Services Journals Career Network Self-Archiving Policy Dispatch Dates AJH Summer School Journals on Oxford Academic Books on Oxford Academic. Issues More Content Advance articles Editor's Choice Submit Graphical Abstracts and Tidbit Author Guidelines Submission Site Open Access Purchase Alerts About About American Journal of Hypertension Editorial Board Board of Directors Advertising and Corporate Services Journals Career Network Self-Archiving Policy Dispatch Dates AJH Summer School Close Navbar Search Filter American Journal of Hypertension This issue Therapeutics Biological Sciences Cardiovascular Medicine Books Journals Oxford Academic Enter search term Search. Advanced Search. Search Menu. Article Navigation. Close mobile search navigation Article Navigation. Volume Article Contents Abstract. Journal Article. Antihypertensive Drugs and Cancer Risk. Satoshi Kidoguchi , Satoshi Kidoguchi. Division of Nephrology and Hypertension, Department of Internal Medicine, The Jikei University School of Medicine. Department of Pharmacology, Faculty of Medicine, Kagawa University. Correspondence: Satoshi Kidoguchi adversity-makes-hero goo. Oxford Academic. Naoki Sugano. Takashi Yokoo. Hidehiro Kaneko. Department of Cardiovascular Medicine, The University of Tokyo. Department of Advanced Cardiology, The University of Tokyo. Hiroshi Akazawa. Mikio Mukai. Osaka Prefectural Hospital Organization, Osaka International Cancer Institute, Department of Medical Check-up. Koichi Node. Department of Cardiovascular Medicine, Saga University. Yuichiro Yano. Department of Advanced Epidemiology, NCD Epidemiology Research Center, Shiga University of Medical Science. Akira Nishiyama. Revision received:. Corrected and typeset:. PDF Split View Views. Select Format Select format. ris Mendeley, Papers, Zotero. enw EndNote. bibtex BibTex. txt Medlars, RefWorks Download citation. Permissions Icon Permissions. Close Navbar Search Filter American Journal of Hypertension This issue Therapeutics Biological Sciences Cardiovascular Medicine Books Journals Oxford Academic Enter search term Search. The composite goal is to reduce cardiovascular events while achieving maximum benefits from cancer therapy. Timely screening for hypertension, early diagnosis and prompt initiation of intervention, regular home BP monitoring, and close follow-up can reduce the burden of cardiovascular complications, leading to an improvement in the quality of life and overall survival in patients with cancer. Bloom MW, Hamo CE, Cardinale D, Ky B, Nohria A, Baer L, et al. Cancer Therapy-Related Cardiac Dysfunction and Heart Failure: Part 1: Definitions, Pathophysiology, Risk Factors, and Imaging. Circ Heart Fail. Lippincott Williams and Wilkins. Article PubMed PubMed Central Google Scholar. Definition of cardiotoxicity - NCI Dictionary of Cancer Terms - National Cancer Institute [Internet]. Patnaik JL, Byers T, DiGuiseppi C, Dabelea D, Denberg TD. Cardiovascular disease competes with breast cancer as the leading cause of death for older females diagnosed with breast cancer: A retrospective cohort study. Breast Cancer Res. BioMed Central. Article Google Scholar. Tini G, Sarocchi M, Tocci G, Arboscello E, Ghigliotti G, Novo G, et al. Arterial hypertension in cancer: the elephant in the room. Int J Cardiol. Elsevier Ireland Ltd. Article PubMed Google Scholar. Mouhayar E, Salahudeen A. Hypertension in Cancer patients. Tex Heart Inst J. PubMed PubMed Central Google Scholar. de Souza VB, Silva EN, Ribeiro ML. Martins W de a. hypertension in patients with cancer. Arq Bras Cardiol. Dyer AR, Berkson DM, Stamler J, Lindberg HA, Stevens E. HIGH BLOOD-PRESSURE: a RISK FACTOR FOR CANCER MORTALITY? Harding JL, Sooriyakumaran M, Anstey KJ, Adams R, Balkau B, Brennan-Olsen S, et al. Hypertension, antihypertensive treatment and cancer incidence and mortality. J Hypertens. Article CAS PubMed Google Scholar. Milan A, Puglisi E, Ferrari L, Bruno G, Losano I, Veglio F. Arterial hypertension and cancer. Int J Cancer. Wiley-Liss Inc. Colt JS, Schwartz K, Graubard BI, Davis F, Ruterbusch J, Digaetano R, et al. Hypertension and risk of renal cell carcinoma among white and black Americans. NIH Public Access. Stocks T, Van Hemelrijck M, Manjer J, Bjørge T, Ulmer H, Hallmans G, et al. Blood pressure and risk of cancer incidence and mortality in the metabolic syndrome and Cancer project. Hypertens Dallas Tex CAS Google Scholar. Grossman E, Messerli FH, Boyko V, Goldbourt U. Is there an association between hypertension and cancer mortality? Am J Med. Elsevier Inc. Koene RJ, Prizment AE, Blaes A, Konety SH. Shared risk factors in cardiovascular disease and cancer. Circulation Lippincott Williams and Wilkins. Hildebrandt MAT, Reyes M, Wu X, Pu X, Thompson KA, Ma J, Landstrom AP, Morrison AC, Ater JL. Hypertension susceptibility loci are associated with Anthracycline-related Cardiotoxicity in long-term childhood Cancer survivors. Sci Rep. Minotti G, Menna P, Salvatorelli E, Cairo G, Gianni L. Anthracyclines: molecular advances and pharmacologic developments in antitumor activity and cardiotoxicity. Pharmacol Rev. von Hoff DD, Layard MW, Basa P, Davis HL, Von Hoff AL, Rozencweig M, et al. Risk factors for doxorubicin-induced congestive heart failure. Ann Intern Med. Hershman DL, RB MB, Eisenberger A, Tsai WY, Grann VR, Jacobson JS. J Clin Oncol Off J Am Soc Clin Oncol. American Society of Clinical Oncology. Article CAS Google Scholar. Pinder MC, Duan Z, Goodwin JS, Hortobagyi GN, Giordano SH. Congestive heart failure in older women treated with adjuvant anthracycline chemotherapy for breast cancer. J Clin Oncol Proc Am Soc Clin Oncol. Lipshultz SE, Rifai N, Sallan SE, Lipsitz SR, Dalton V, Sacks DB, et al. Predictive value of cardiac troponin T in pediatric patients at risk for myocardial injury. Seidman A, Hudis C, Pierri MK, Shak S, Paton V, Ashby M, et al. Cardiac Dysfunction in the Trastuzumab Clinical Trials Experience. J Clin Oncol. Am Soc Clin Oncol ASCO. Molecular basis of anthracycline-induced cardiotoxicity and its prevention. Mol Genet Metab. Academic Press Inc. Tokarska-Schlattner M, Zaugg M, Zuppinger C, Wallimann T, Schlattner U. New insights into doxorubicin-induced cardiotoxicity: The critical role of cellular energetics. J Mol Cell Cardiol. Salvatorelli E, Menna P, Chello M, Covino E, Minotti G. Low-dose Anthracycline and risk of heart failure in a pharmacokinetic model of human myocardium exposure: analog specificity and role of secondary alcohol metabolites. J Pharmacol Exp Ther American Society for Pharmacology and Experimental Therapeutics. Kuriakose RK, Kukreja RC, Xi L. Potential therapeutic strategies for hypertension-exacerbated Cardiotoxicity of anticancer drugs. Oxid Med Cell Longev. Hunter JJ, Chien KR. Signaling pathways for cardiac hypertrophy and failure. Epstein FH, editor. N Engl J med. Massachusetts Medical Society. Szmit S, Jurczak W, Zaucha JM, Drozd-Sokołowska J, Spychałowicz W, Joks M, et al. Pre-existing arterial hypertension as a risk factor for early left ventricular systolic dysfunction following R -CHOP chemotherapy in patients with lymphoma. J Am Soc Hypertens. Balduzzi S, Mantarro S, Guarneri V, Tagliabue L, Pistotti V, Moja L, D'Amico R. Trastuzumab-containing regimens for metastatic breast cancer. Cochrane Database Syst Rev. Gunaldi M, Duman BB, Afsar CU, Paydas S, Erkisi M, Kara IO, et al. Risk factors for developing cardiotoxicity of trastuzumab in breast cancer patients: an observational single-Centre study. J Oncol Pharm Pract Off Publ Int Soc Oncol Pharm Pract. Sandoo A, Kitas GD, Carmichael AR. Endothelial dysfunction as a determinant of trastuzumab-mediated cardiotoxicity in patients with breast cancer. Anticancer Res. CAS PubMed Google Scholar. Pentassuglia L, Sawyer DB. Exp Cell Res. Gordon LI, Burke MA, Singh ATK, Prachand S, Lieberman ED, Sun L, et al. Blockade of the erbB2 receptor induces cardiomyocyte death through mitochondrial and reactive oxygen species-dependent pathways. J Biol Chem. Article CAS PubMed PubMed Central Google Scholar. Viallard C, Larrivée B. Tumor angiogenesis and vascular normalization: alternative therapeutic targets. Hein TW, Rosa RH, Ren Y, Xu W, Kuo L. Invest Ophthalmol Vis Sci. Zhao Y, Adjei AA. Targeting angiogenesis in Cancer therapy: moving beyond vascular endothelial growth factor. Simons M, Gordon E, Claesson-Welsh L. Mechanisms and regulation of endothelial VEGF receptor signalling. Nat Rev Mol Cell Biol. Kamli H, Li L, Gobe GC. Limitations to the therapeutic potential of tyrosine kinase inhibitors and alternative therapies for kidney Cancer. Ochsner J. Sarwar S, Bakbak B, Sadiq MA, Sepah YJ, Shah SM, Ibrahim M, et al. Fusion proteins: Aflibercept VEGF trap-eye. Dev Ophthalmol. Small HY, Montezano AC, Rios FJ, Savoia C, Touyz RM. Hypertension due to antiangiogenic cancer therapy with vascular endothelial growth factor inhibitors: understanding and managing a new syndrome. Can J Cardiol. Cancer Institute N. Common Terminology Criteria for Adverse Events CTCAE Common Terminology Criteria for Adverse Events CTCAE v5. Google Scholar. Zhao T, Wang X, Xu T, Xu X, Liu Z. Bevacizumab significantly increases the risks of hypertension and proteinuria in cancer patients: a systematic review and comprehensive meta-analysis. Chen J, Lu Y, Zheng Y. Incidence and risk of hypertension with bevacizumab in non-small-cell lung cancer patients: a meta-analysis of randomized controlled trials. Drug Des Devel Ther. CAS PubMed PubMed Central Google Scholar. Yeh ETH, Bickford CL. Cardiovascular complications of cancer therapy: incidence, pathogenesis, diagnosis, and management. J Am Coll Cardiol. Versmissen J, Mirabito Colafella KM, Koolen SLW, Danser AHJ. Vascular cardio-oncology: vascular endothelial growth factor inhibitors and hypertension. Cardiovasc Res. Pandey AK, Singhi EK, Arroyo JP, Ikizler TA, Gould ER, Brown J, et al. Mechanisms of VEGF-Inhibitor Associated Hypertension and Vascular Disease. Syrigos KN, Karapanagiotou E, Boura P, Manegold C, Harrington K. Bevacizumab-induced hypertension: pathogenesis and management. BioDrugs Clin Immunother Biopharm Gene Ther. Gressett SM, Shah SR. Intricacies of bevacizumab-induced toxicities and their management. Ann Pharmacother. Li M, Kroetz DL. Bevacizumab-induced hypertension: clinical presentation and molecular understanding. Pharmacol Ther. Frey MK, Dao F, Olvera N, Konner JA, Dickler MN, Levine DA. Genetic predisposition to bevacizumab-induced hypertension. Gynecol Oncol. McIntyre WF, Oqab Z, Hopman WM, Hammad N, Baranchuk A. Hypertension due to antiangiogenic cancer therapy with VEGF inhibitors: is autonomic nervous system toxicity another possible mechanism? Eur Med Agency. Plummer C, Michael A, Shaikh G, Stewart M, Buckley L, Miles T, et al. Expert recommendations on the management of hypertension in patients with ovarian and cervical cancer receiving bevacizumab in the UK. Br J Cancer. Shah SR, Gressett Ussery SM, Dowell JE, Marley E, Liticker J, Arriaga Y, et al. Shorter bevacizumab infusions do not increase the incidence of proteinuria and hypertension. Ann Oncol Off J Eur Soc Med Oncol. Cameron AC, Touyz RM, Lang NN. Vascular complications of Cancer chemotherapy. Touyz RM, Herrmann J. Cardiotoxicity with vascular endothelial growth factor inhibitor therapy. NPJ Precis Oncol. Blanter JB, Frishman WH. Cardiol Rev. Miura S-I, Fujino M, Matsuo Y, Tanigawa H, Saku K. Hypertens Res Off J Jpn Soc Hypertens. Izzedine H, Ederhy S, Goldwasser F, Soria JC, Milano G, Cohen A, et al. Management of hypertension in angiogenesis inhibitor-treated patients. Kružliak P, Novák J, Novák M. Vascular endothelial growth factor inhibitor—induced hypertension: from pathophysiology to prevention and treatment based on long-acting nitric oxide donors. Am J Hypertens. Corr BR, Breed C, Sheeder J, Weisdack S, Behbakht K. Bevacizumab induced hypertension in gynecologic cancer: does it resolve after completion of therapy? Gynecol Oncol Rep. Qi W-X, Shen Z, Tang L-N, Yao Y. Risk of hypertension in cancer patients treated with aflibercept: a systematic review and meta-analysis. Clin Drug Investig. Goodman VL, Rock EP, Dagher R, Ramchandani RP, Abraham S, Gobburu JVS, et al. Approval summary: sunitinib for the treatment of imatinib refractory or intolerant gastrointestinal stromal tumors and advanced renal cell carcinoma. Clin Cancer Res Off J Am Assoc Cancer Res. Valent P, Hadzijusufovic E, Hoermann G, Füreder W, Schernthaner G-H, Sperr WR, et al. Risk factors and mechanisms contributing to TKI-induced vascular events in patients with CML. Leuk Res. Li Y, Li S, Zhu Y, Liang X, Meng H, Chen J, et al. Incidence and risk of sorafenib-induced hypertension: a systematic review and meta-analysis. J Clin Hypertens Greenwich Conn. Haas NB, Manola J, Uzzo RG, Flaherty KT, Wood CG, Kane C, et al. Adjuvant sunitinib or sorafenib for high-risk, non-metastatic renal-cell carcinoma ECOG-ACRIN E : a double-blind, placebo-controlled, randomised, phase 3 trial. Lancet Lond Engl. Eechoute K, van der Veldt AAM, Oosting S, MHW K, Wessels JAM, Gelderblom H, et al. Polymorphisms in endothelial nitric oxide synthase eNOS and vascular endothelial growth factor VEGF predict sunitinib-induced hypertension. Clin Pharmacol Ther. Fu Y, Wei X, Lin L, Xu W, Liang J. Adverse reactions of sorafenib, sunitinib, and imatinib in treating digestive system tumors. Thorac Cancer. Bæk Møller N, Budolfsen C, Grimm D, Krüger M, Infanger M, Wehland M, et al. Drug-induced hypertension caused by multikinase inhibitors Sorafenib, Sunitinib, Lenvatinib and Axitinib in renal cell carcinoma treatment. Int J Mol Sci. Rautiola J, Donskov F, Peltola K, Joensuu H, Bono P. Sunitinib-induced hypertension, neutropaenia and thrombocytopaenia as predictors of good prognosis in patients with metastatic renal cell carcinoma. BJU Int. Donskov F, Michaelson MD, Puzanov I, Davis MP, Bjarnason GA, Motzer RJ, et al. Sunitinib-associated hypertension and neutropenia as efficacy biomarkers in metastatic renal cell carcinoma patients. Izzedine H, Derosa L, Le Teuff G, Albiges L, Escudier B. Hypertension and angiotensin system inhibitors: impact on outcome in sunitinib-treated patients for metastatic renal cell carcinoma. León-Mateos L, Mosquera J, Antón AL. Treatment of sunitinib-induced hypertension in solid tumor by nitric oxide donors. Redox Biol. Kollmannsberger C, Soulieres D, Wong R, Scalera A, Gaspo R, Bjarnason G. Sunitinib therapy for metastatic renal cell carcinoma: recommendations for management of side effects. Can Urol Assoc J. Ewer MS, Suter TM, Lenihan DJ, Niculescu L, Breazna A, Demetri GD, et al. Cardiovascular events among cancer patients treated with sunitinib, interferon, or placebo: a comprehensive adjudicated database analysis demonstrating clinically meaningful reversibility of cardiac events. Eur J Cancer. Brose MS, Frenette CT, Keefe SM, Stein SM. Semin Oncol. Kappers Mariëtte HW, van Esch Joep HM, Wim S, Stefan S, Jan DAH, van den Meiracker Anton H. Hypertension induced by the tyrosine kinase inhibitor Sunitinib is associated with increased circulating Endothelin-1 levels. Hypertension Am Heart Assoc. Roeker LE, Sarraf Yazdy M, Rhodes J, Goodfriend J, Narkhede M, Carver J, et al. Hypertension in patients treated with Ibrutinib for chronic lymphocytic leukemia. JAMA Netw Open. Laubach JP, Moslehi JJ, Francis SA, San Miguel JF, Sonneveld P, Orlowski RZ, et al. Br J Haematol. Dimopoulos MA, Goldschmidt H, Niesvizky R, Joshua D, Chng W-J, Oriol A, et al. Carfilzomib or bortezomib in relapsed or refractory multiple myeloma ENDEAVOR : an interim overall survival analysis of an open-label, randomised, phase 3 trial. Lancet Oncol. Hasinoff BB, Patel D, Wu X. Molecular mechanisms of the Cardiotoxicity of the proteasomal-targeted drugs Bortezomib and Carfilzomib. Cardiovasc Toxicol. Siegel D, Martin T, Nooka A, Harvey RD, Vij R, Niesvizky R, et al. Integrated safety profile of single-agent carfilzomib: experience from patients enrolled in 4 phase II clinical studies. Kumar SK, Berdeja JG, Niesvizky R, Lonial S, Laubach JP, Hamadani M, et al. Moreau P, Masszi T, Grzasko N, Bahlis NJ, Hansson M, Pour L, et al. Oral Ixazomib, Lenalidomide, and dexamethasone for multiple myeloma. N Engl J Med. Wu P, Oren O, Gertz MA, Yang EH. Proteasome inhibitor-related Cardiotoxicity: mechanisms, diagnosis, and management. Curr Oncol Rep. Soultati A, Mountzios G, Avgerinou C, Papaxoinis G, Pectasides D, Dimopoulos M-A, et al. Endothelial vascular toxicity from chemotherapeutic agents: preclinical evidence and clinical implications. Cancer Treat Rev. Nuver J, Smit AJ, Sleijfer DT, van Gessel AI, van Roon AM, van der Meer J, et al. Microalbuminuria, decreased fibrinolysis, and inflammation as early signs of atherosclerosis in long-term survivors of disseminated testicular cancer. Eur J Cancer Oxf Engl Valentová M, Mladosievicová B. Coronary heart disease and hypertension as late effects of testicular cancer treatment--a minireview. Klin Onkol Cas Ceske Slov Onkol Spolecnosti. Navis G, Faber HJ, de Zeeuw D, de Jong PE. ACE inhibitors and the kidney. A risk-benefit assessment. Drug Saf. Goodwin JE, Geller DS. Glucocorticoid-induced hypertension. Pediatr Nephrol Berl Ger. Baid S, Nieman LK. Glucocorticoid excess and hypertension. Curr Hypertens Rep. Arslansoyu Camlar S, Soylu A, Kavukçu S. Cyclosporine in pediatric nephrology. Iran J Kidney Dis. PubMed Google Scholar. Morales JM. Influence of the new immunosuppressive combinations on arterial hypertension after renal transplantation. Kidney Int Suppl. Bursztyn M, Zelig O, Or R, Nagler A. Isradipine for the prevention of cyclosporine-induced hypertension in allogeneic bone marrow transplant recipients: a randomized, double-blind study. Zhai Y-J, Wu M-M, Linck VA, Zou L, Yue Q, Wei S-P, et al. Intracellular cholesterol stimulates ENaC by interacting with phosphatidylinositol-4,5-bisphosphate and mediates cyclosporine A-induced hypertension. Biochim Biophys Acta Mol basis Dis. Schlaich MP, Grassi G. Sympathoexcitation in calcineurin inhibitor-induced hypertension: villain or innocent bystander? Divac N, Naumović R, Stojanović R, Prostran M. The role of immunosuppressive medications in the pathogenesis of hypertension and efficacy and safety of antihypertensive agents in kidney transplant recipients. Curr Med Chem. Marienhagen K, Lehner F, Klempnauer J, Hecker H, Borlak J. Treatment of cyclosporine induced hypertension: results from a long-term observational study using different antihypertensive medications. Vasc Pharmacol. Haddad EM, McAlister VC, Renouf E, Malthaner R, Kjaer MS, Gluud LL. Cyclosporin versus tacrolimus for liver transplanted patients. Chanard J, Toupance O, Lavaud S, Hurault de Ligny B, Bernaud C, Moulin B. Amlodipine reduces cyclosporin-induced hyperuricaemia in hypertensive renal transplant recipients. Nephrol Dial Transplant Off Publ Eur Dial Transpl Assoc - Eur Ren Assoc. Vergoulas G. Antihypertensive agents and renal transplantation. Lazelle RA, McCully BH, Terker AS, Himmerkus N, Blankenstein KI, Mutig K, et al. Renal deletion of 12 kDa FKbinding protein attenuates Tacrolimus-induced hypertension. J Am Soc Nephrol JASN. Toral M, Romero M, Rodríguez-Nogales A, Jiménez R, Robles-Vera I, Algieri F, Chueca-Porcuna N, Sánchez M, de la Visitación N, Olivares M, García F, Pérez-Vizcaíno F, Gálvez J, Duarte J. Lactobacillus fermentum Improves Tacrolimus-Induced Hypertension by Restoring Vascular Redox State and Improving eNOS Coupling. Mol Nutr Food Res. Use of mycophenolate mofetil in liver transplantation: a literature review. Transplant Proc. Fujihara CK, Vieira JM, Sena CR, Ventura BH, Malheiros DM, Zatz R. Early brief treatment with losartan plus mycophenolate mofetil provides lasting renoprotection in a renal ablation model. Am J Nephrol. Pinto F, Calarco A, Totaro A, Sacco E, Volpe A, Racioppi M, et al. Androgen-deprivation therapy in prostate cancer: clinical evidence and future perspectives. Vasaitis TS, Bruno RD, Njar VCO. CYP17 inhibitors for prostate cancer therapy. J Steroid Biochem Mol Biol. Veccia A, Maines F, Kinspergher S, Galligioni E, Caffo O. Cardiovascular toxicities of systemic treatments of prostate cancer. Nat Rev Urol. Iacovelli R, Verri E, Cossu Rocca M, Aurilio G, Cullurà D, De Cobelli O, et al. The incidence and relative risk of cardiovascular toxicity in patients treated with new hormonal agents for castration-resistant prostate cancer. Curigliano G, Shah RR. Safety and tolerability of Phosphatidylinositolkinase PI3K inhibitors in oncology. Greenwell IB, Ip A, Cohen JB. PI3K inhibitors: understanding toxicity mechanisms and management. Oncol Williston Park N. Canela M-D, Noppen S, Bueno O, Prota AE, Bargsten K, Sáez-Calvo G, et al. Antivascular and antitumor properties of the tubulin-binding chalcone TUB Schwartz EL. Antivascular actions of microtubule-binding drugs. Sandler A, Gray R, Perry MC, Brahmer J, Schiller JH, Dowlati A, et al. Paclitaxel-carboplatin alone or with bevacizumab for non-small-cell lung cancer. Miller K, Wang M, Gralow J, Dickler M, Cobleigh M, Perez EA, et al. Paclitaxel plus bevacizumab versus paclitaxel alone for metastatic breast cancer. Hoque S, Chen BJ, Schoen MW, Carson KR, Keller J, Witherspoon BJ, et al. End of an era of administering erythropoiesis stimulating agents among veterans administration cancer patients with chemotherapy-induced anemia. PLoS One. Schoen MW, Hoque S, Witherspoon BJ, Schooley B, Sartor O, Yang YT, et al. End of an era for erythropoiesis-stimulating agents in oncology. Forbes CA, Worthy G, Harker J, Kleijnen J, Kutikova L, Zelek L, et al. Dose efficiency of erythropoiesis-stimulating agents for the treatment of patients with chemotherapy-induced anemia: a systematic review. Clin Ther. Vaziri ND. Mechanism of erythropoietin-induced hypertension. Am J Kidney Dis Off J Natl Kidney Found. Palumbo A, Chanan-Khan A, Weisel K, Nooka AK, Masszi T, Beksac M, et al. Daratumumab, Bortezomib, and dexamethasone for multiple myeloma. Chari A, Martinez-Lopez J, Mateos M-V, Bladé J, Benboubker L, Oriol A, et al. Daratumumab plus carfilzomib and dexamethasone in patients with relapsed or refractory multiple myeloma. Dimopoulos MA, Lonial S, White D, Moreau P, Palumbo A, San-Miguel J, et al. Costa LJM, Varella PCS, Del Giglio A. White coat effect in breast cancer patients undergoing chemotherapy. Eur J Cancer Care Engl. Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ. Dennison Himmelfarb Cheryl, et al. Minlikeeva AN, Freudenheim JL, Cannioto RA, Szender JB, Eng KH, Modugno F, et al. History of hypertension, heart disease, and diabetes and ovarian cancer patient survival: evidence from the ovarian cancer association consortium. Cancer Causes Control CCC. Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. Iachina M, Jakobsen E, Møller H, Lüchtenborg M, Mellemgaard A, Krasnik M, et al. The effect of different comorbidities on survival of non-small cells lung cancer patients. Piccirillo JF, Tierney RM, Costas I, Grove L, Spitznagel EL. Prognostic importance of comorbidity in a hospital-based cancer registry. Goldstein D, Rosenberg JE, Figlin RA, Townsend RR, McCann L, Carpenter C, et al. Download references. Department of Medicine, University of Connecticut School of Medicine, Farmington, CT, USA. Department of Medicine, Calhoun Cardiology Center, University of Connecticut School of Medicine, Farmington Avenue, Farmington, CT, , USA. You can also search for this author in PubMed Google Scholar. |
| ANTIHYPERTENSIVE THERAPY AND CANCER | Goodman, M. Sign up for rixk Nature Briefing Strengthen immune function — what Hypertension and cancer risk in science, free to your inbox daily. Vergoulas Hypertenslon. Search Search articles by subject, keyword or author. In addition, when BP and fasting serum glucose level status was the same, the analysis results of men who were never-smokers and non-alcohol drinkers exhibited a higher HR than that of men who were smokers and drinkers Fig. Thank you for visiting nature. |
| Etiology and management of hypertension in patients with cancer | Cardio-Oncology | Full Text | Association between antihypertensive medications and risk of skin cancer in people older than 65 years: a population-based study. CMAJ ; : E — E Association of hypertension and blood pressure with kidney cancer risk: a nationwide population-based cohort study. Hypertension ; 75 : — Kristensen KB , Habel LA , Gagne JJ , Friis S , Andersen KK , Hallas J , Pottegård A. Risk of renal cell carcinoma associated with calcium channel blockers: a nationwide observational study focusing on confounding by indication. Epidemiology ; 31 : — Norsker FN , Pedersen C , Armstrong GT , Robison LL , McBride ML , Hawkins M , Kuehni CE , de Vathaire F , Berbis J , Kremer LC , Haupt R , Kenborg L , Winther JF. Late effects in childhood cancer survivors: early studies, survivor cohorts, and significant contributions to the field of late effects. Pediatr Clin North Am ; 67 : — Cohen Sedgh R , Moon J , Jackevicius CA. Neoplasm reports in food and drug administration adverse event reporting system following angiotensin receptor blocker recalls. Circ Cardiovasc Qual Outcomes ; 14 : e Coleman CI , Baker WL , Kluger J , White CM. Antihypertensive medication and their impact on cancer incidence: a mixed treatment comparison meta-analysis of randomized controlled trials. J Hypertens ; 26 : — Bangalore S , Kumar S , Kjeldsen SE , Makani H , Grossman E , Wetterslev J , Gupta AK , Sever PS , Gluud C , Messerli FH. Antihypertensive drugs and risk of cancer: network meta-analyses and trial sequential analyses of , participants from randomised trials. Lancet Oncol ; 12 : 65 — Copland E , Canoy D , Nazarzadeh M , Bidel Z , Ramakrishnan R , Woodward M , Chalmers J , Teo KK , Pepine CJ , Davis BR , Kjeldsen S , Sundström J , Rahimi K. Antihypertensive treatment and risk of cancer: an individual participant data meta-analysis. Lancet Oncol ; 22 : — Colt JS , Hofmann JN , Schwartz K , Chow WH , Graubard BI , Davis F , Ruterbusch J , Berndt S , Purdue MP. Antihypertensive medication use and risk of renal cell carcinoma. Cancer Causes Control ; 28 : — Antihypertensive medications are associated with the risk of kidney and bladder cancer: a systematic review and meta-analysis. Aging ; 12 : — Matsui S , Sobue T , Zha L , Kitamura T , Sawada N , Iwasaki M , Shimazu T , Tsugane S. Long-term antihypertensive drug use and risk of cancer: the Japan Public Health Center-based prospective study. Cancer Sci ; : — Antihypertensive drugs use and the risk of prostate cancer: a meta-analysis of 21 observational studies. BMC Urol ; 18 : Use of antihypertensive drugs and risk of malignant melanoma: a meta-analysis of observational studies. Drug Saf ; 41 : — Gandini S , Palli D , Spadola G , Bendinelli B , Cocorocchio E , Stanganelli I , Miligi L , Masala G , Caini S. Anti-hypertensive drugs and skin cancer risk: a review of the literature and meta-analysis. Crit Rev Oncol Hematol ; : 1 — 9. Huang T , Poole EM , Eliassen AH , Okereke OI , Kubzansky LD , Sood AK , Forman JP , Tworoger SS. Hypertension, use of antihypertensive medications, and risk of epithelial ovarian cancer. Devore EE , Kim S , Ramin CA , Wegrzyn LR , Massa J , Holmes MD , Michels KB , Tamimi RM , Forman JP , Schernhammer ES. Antihypertensive medication use and incident breast cancer in women. Breast Cancer Res Treat ; : — Antihypertensive drug use and breast cancer risk: a meta-analysis of observational studies. Oncotarget ; 8 : — Genetically proxied therapeutic inhibition of antihypertensive drug targets and risk of common cancers: a Mendelian randomization analysis. PLoS Med ; 19 : e Markozannes G , Kanellopoulou A , Dimopoulou O , Kosmidis D , Zhang X , Wang L , Theodoratou E , Gill D , Burgess S , Tsilidis KK. Systematic review of Mendelian randomization studies on risk of cancer. BMC Med ; 20 : Koene RJ , Prizment AE , Blaes A , Konety SH. Shared risk factors in cardiovascular disease and cancer. Circulation ; : — Khoshghamat N , Jafari N , Toloue-Pouya V , Azami S , Mirnourbakhsh SH , Khazaei M , Ferns GA , Rajabian M , Avan A. The therapeutic potential of renin-angiotensin system inhibitors in the treatment of pancreatic cancer. Life Sci ; : Downward J. Targeting RAS signalling pathways in cancer therapy. Nat Rev Cancer ; 3 : 11 — Clinical applicability of renin-angiotensin system inhibitors in cancer treatment. Am J Cancer Res ; 11 : — Pinter M , Jain RK. Targeting the renin-angiotensin system to improve cancer treatment: implications for immunotherapy. Sci Transl Med ; 9 : eaan Egami K , Murohara T , Shimada T , Sasaki K , Shintani S , Sugaya T , Ishii M , Akagi T , Ikeda H , Matsuishi T , Imaizumi T. Role of host angiotensin II type 1 receptor in tumor angiogenesis and growth. J Clin Invest ; : 67 — Kosaka T , Miyajima A , Takayama E , Kikuchi E , Nakashima J , Ohigashi T , Asano T , Sakamoto M , Okita H , Murai M , Hayakawa M. Angiotensin II type 1 receptor antagonist as an angiogenic inhibitor in prostate cancer. Prostate ; 67 : 41 — Pfeffer MA , Swedberg K , Granger CB , Held P , McMurray JJ , Michelson EL , Olofsson B , Ostergren J , Yusuf S , Pocock S. Effects of candesartan on mortality and morbidity in patients with chronic heart failure: the CHARM-Overall programme. Lancet ; : — Sipahi I , Debanne SM , Rowland DY , Simon DI , Fang JC. Angiotensin-receptor blockade and risk of cancer: meta-analysis of randomised controlled trials. Lancet Oncol ; 11 : — Collaboration AT. Effects of telmisartan, irbesartan, valsartan, candesartan, and losartan on cancers in 15 trials enrolling , individuals. J Hypertens ; 29 : — Datzmann T , Fuchs S , Andree D , Hohenstein B , Schmitt J , Schindler C. Systematic review and meta-analysis of randomised controlled clinical trial evidence refutes relationship between pharmacotherapy with angiotensin-receptor blockers and an increased risk of cancer. Eur J Intern Med ; 64 : 1 — 9. Renin-angiotensin system blockade for the risk of cancer and death. J Renin Angiotensin Aldosterone Syst ; 17 : Hicks BM , Filion KB , Yin H , Sakr L , Udell JA , Azoulay L. Angiotensin converting enzyme inhibitors and risk of lung cancer: population based cohort study. BMJ ; : k Meier CR , Derby LE , Jick SS , Jick H. Angiotensin-converting enzyme inhibitors, calcium channel blockers, and breast cancer. Arch Intern Med ; : — Christian JB , Lapane KL , Hume AL , Eaton CB , Weinstock MA , Trial V. Association of ACE inhibitors and angiotensin receptor blockers with keratinocyte cancer prevention in the randomized VATTC trial. J Natl Cancer Inst ; : — Association between angiotensin-converting enzyme inhibitors and lung cancer—a nationwide, population-based, propensity score-matched cohort study. Cancers ; 12 : Schmidt SA , Schmidt M , Mehnert F , Lemeshow S , Sørensen HT. Use of antihypertensive drugs and risk of skin cancer. J Eur Acad Dermatol Venereol ; 29 : — McMenamin U , Murray LJ , Cantwell MM , Hughes CM. Angiotensin-converting enzyme inhibitors and angiotensin receptor blockers in cancer progression and survival: a systematic review. Cancer Causes Control ; 23 : — Busby J , McMenamin U , Spence A , Johnston BT , Hughes C , Cardwell CR. Angiotensin receptor blocker use and gastro-oesophageal cancer survival: a population-based cohort study. Aliment Pharmacol Ther ; 47 : — Santala EE , Rannikko A , Murtola TJ. Antihypertensive drugs and prostate cancer survival after radical prostatectomy in Finland—a nationwide cohort study. Santala EEE , Artama M , Pukkala E , Visvanathan K , Staff S , Murtola TJ. Antihypertensive drug use and the risk of ovarian cancer death among Finnish ovarian cancer patients—a nationwide cohort study. Cancers ; 13 : Santala EEE , Murto MO , Artama M , Pukkala E , Visvanathan K , Murtola TJ. Angiotensin receptor blockers associated with improved breast cancer survival—a nationwide cohort study from Finland. Cancer Epidemiol Biomarkers Prev ; 29 : — Tanaka N , Miyajima A , Kosaka T , Shirotake S , Hasegawa M , Kikuchi E , Oya M. Cis-dichlorodiammineplatinum upregulates angiotensin II type 1 receptors through reactive oxygen species generation and enhances VEGF production in bladder cancer. Mol Cancer Ther ; 9 : — Acquired platinum resistance enhances tumour angiogenesis through angiotensin II type 1 receptor in bladder cancer. Br J Cancer ; : — Anandanadesan R , Gong Q , Chipitsyna G , Witkiewicz A , Yeo CJ , Arafat HA. J Gastrointest Surg ; 12 : 57 — Cortez-Retamozo V , Etzrodt M , Newton A , Ryan R , Pucci F , Sio SW , Kuswanto W , Rauch PJ , Chudnovskiy A , Iwamoto Y , Kohler R , Marinelli B , Gorbatov R , Wojtkiewicz G , Panizzi P , Mino-Kenudson M , Forghani R , Figueiredo JL , Chen JW , Xavier R , Swirski FK , Nahrendorf M , Weissleder R , Pittet MJ. Angiotensin II drives the production of tumor-promoting macrophages. Immunity ; 38 : — Tozuka T , Yanagitani N , Yoshida H , Manabe R , Ogusu S , Tsugitomi R , Sakamoto H , Amino Y , Ariyasu R , Uchibori K , Kitazono S , Seike M , Gemma A , Nishio M. Anticancer Res ; 41 : — Nakai Y , Isayama H , Ijichi H , Sasaki T , Sasahira N , Hirano K , Kogure H , Kawakubo K , Yagioka H , Yashima Y , Mizuno S , Yamamoto K , Arizumi T , Togawa O , Matsubara S , Tsujino T , Tateishi K , Tada M , Omata M , Koike K. Inhibition of renin-angiotensin system affects prognosis of advanced pancreatic cancer receiving gemcitabine. How does inhibition of the renin-angiotensin system affect the prognosis of advanced gastric cancer patients receiving platinum-based chemotherapy? Oncology ; 83 : — Rachow T , Schiffl H , Lang SM. Risk of lung cancer and renin-angiotensin blockade: a concise review. J Cancer Res Clin Oncol ; : — Ray SD , Kamendulis LM , Gurule MW , Yorkin RD , Corcoran GB. FASEB J ; 7 : — Panneerpandian P , Rao DB , Ganesan K. Toxicol In Vitro ; 74 : Calcium channels as novel therapeutic targets for ovarian cancer stem cells. Int J Mol Sci ; 21 : Dihydropyridine calcium channel blockers suppress the transcription of PD-L1 by inhibiting the activation of STAT1. Front Pharmacol ; 11 : Cohen HJ , Pieper CF , Hanlon JT , Wall WE , Burchett BM , Havlik RJ. Calcium channel blockers and cancer. Am J Med ; : — Rosenberg L , Rao RS , Palmer JR , Strom BL , Stolley PD , Zauber AG , Warshauer ME , Shapiro S. Calcium channel blockers and the risk of cancer. Pahor M , Guralnik JM , Ferrucci L , Corti MC , Salive ME , Cerhan JR , Wallace RB , Havlik RJ. Calcium-channel blockade and incidence of cancer in aged populations. Li B , Cheung KS , Wong IY , Leung WK , Law S. Calcium channel blockers are associated with lower gastric cancer risk: a territory-wide study with propensity score analysis. Rotshild V , Azoulay L , Feldhamer I , Perlman A , Glazer M , Muszkat M , Matok I. Calcium channel blockers and the risk for lung cancer: a population-based nested case-control study. Ann Pharmacother ; 53 : — Li CI , Daling JR , Tang MT , Haugen KL , Porter PL , Malone KE. Use of antihypertensive medications and breast cancer risk among women aged 55 to 74 years. JAMA Intern Med ; : — Bergman GJ , Khan S , Danielsson B , Borg N. Breast cancer risk and use of calcium channel blockers using Swedish population registries. Wang Z , White DL , Hoogeveen R , Chen L , Whitsel EA , Richardson PA , Virani SS , Garcia JM , El-Serag HB , Jiao L. J Clin Med ; 7 : Nayan M , Juurlink DN , Austin PC , Macdonald EM , Finelli A , Kulkarni GS , Hamilton RJ ; Canadian Drug Safety and Effectiveness Research Network CDSERN. Medication use and kidney cancer survival: a population-based study. Use of antihypertensive medications and survival rates for breast, colorectal, lung, or stomach cancer. Kreutz R , Algharably EAH , Douros A. Reviewing the effects of thiazide and thiazide-like diuretics as photosensitizing drugs on the risk of skin cancer. J Hypertens ; 37 : — Pottegård A , Pedersen SA , Schmidt SAJ , Hölmich LR , Friis S , Gaist D. Association of hydrochlorothiazide use and risk of malignant melanoma. Rouette J , Yin H , Pottegård A , Nirantharakumar K , Azoulay L. Use of hydrochlorothiazide and risk of melanoma and nonmelanoma skin cancer. Drug Saf ; 44 : — Pottegård A , Hallas J , Olesen M , Svendsen MT , Habel LA , Friedman GD , Friis S. Hydrochlorothiazide use is strongly associated with risk of lip cancer. J Intern Med ; : — Pottegård A , Bech BH , Pedersen SA , Christensen B. Use of hydrochlorothiazide in Denmark following publication of skin cancer risk findings. Pharmacoepidemiol Drug Saf ; 30 : — Moore DE. Drug-induced cutaneous photosensitivity: incidence, mechanism, prevention and management. Drug Saf ; 25 : — Photosensitizing medications and photocarcinogenesis. Photodermatol Photoimmunol Photomed ; 30 : 8 — Schneider R , Reinau D , Stoffel S , Jick SS , Meier CR , Spoendlin J. Risk of skin cancer in new users of thiazides and thiazide-like diuretics: a cohort study using an active comparator group. Br J Dermatol ; : — Fortuny J , Sima C , Bayuga S , Wilcox H , Pulick K , Faulkner S , Zauber AG , Olson SH. Risk of endometrial cancer in relation to medical conditions and medication use. Cancer Epidemiol Biomarkers Prev ; 18 : — Cole SW , Sood AK. Molecular pathways: beta-adrenergic signaling in cancer. Clin Cancer Res ; 18 : — Kamiya A , Hayama Y , Kato S , Shimomura A , Shimomura T , Irie K , Kaneko R , Yanagawa Y , Kobayashi K , Ochiya T. Genetic manipulation of autonomic nerve fiber innervation and activity and its effect on breast cancer progression. Nat Neurosci ; 22 : — Fumagalli C , Maurizi N , Marchionni N , Fornasari D. β-Blockers: their new life from hypertension to cancer and migraine. Pharmacol Res ; : Coelho M , Soares-Silva C , Brandão D , Marino F , Cosentino M , Ribeiro L. β-Adrenergic modulation of cancer cell proliferation: available evidence and clinical perspectives. Brohée L , Peulen O , Nusgens B , Castronovo V , Thiry M , Colige AC , Deroanne CF. Comparison of sociodemographic and health-related characteristics of UK Biobank participants with those of the general population. Batty GD, Gale CR, Kivimaki M, Deary IJ, Bell S. Comparison of risk factor associations in UK Biobank against representative, general population based studies with conventional response rates: prospective cohort study and individual participant meta-analysis. Lopez PM, Subramanian SV, Schooling CM. Effect measure modification conceptualized using selection diagrams as mediation by mechanisms of varying population-level relevance. Zhou B, Bentham J, Di Cesare M, Bixby H, Danaei G, Cowan MJ, et al. Worldwide trends in blood pressure from to a pooled analysis of population-based measurement studies with Fitzmaurice C, Allen C, Barber RM, Barregard L, Bhutta ZA, Brenner H, et al. Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 32 cancer groups, to a systematic analysis for the global burden of disease study. JAMA Oncol. Afshin A, Forouzanfar MH, Reitsma MB, Sur P, Estep K, Lee A, et al. Health effects of overweight and obesity in countries over 25 years. Gapstur SM, Drope JM, Jacobs EJ, Teras LR, McCullough ML, Douglas CE, et al. A blueprint for the primary prevention of cancer: Targeting established, modifiable risk factors. McQueen DV. Strengthening the evidence base for health promotion. Health Promot Int. Download references. School of Public Health, Li Ka Shing Faculty of Medicine, The University of Hong Kong, 7 Sassoon Road, Pokfulam, Hong Kong, SAR, China. Mary Schooling. Graduate School of Public Health and Health Policy, City University of New York, New York, USA. You can also search for this author in PubMed Google Scholar. IIC, MKK and CMS designed the study and interpreted the results. IIC conducted data analysis and wrote the first draft of the manuscript, with critical feedback from MKK and CMS. All authors have read and approved the final manuscript. Correspondence to C. This study only used publicly available data. No original data were collected. Ethical approval for each of the studies included in the investigation can be found in the original publications. Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. Mendelian randomization estimates of systolic filled and diastolic hollow blood pressure on asthma. Genetic associations with systolic blood pressure, total and site-specific cancers. Supplementary Table S2. Genetic associations with diastolic blood pressure, total and site-specific cancers. Supplementary Table S3. Power calculations for total and site-specific cancers. Supplementary Table S4. Mendelian randomization estimates of systolic per 10 mmHg increment blood pressure on total and site-specific cancers. Supplementary Table S5. Mendelian randomization estimates of diastolic per 5 mmHg increment blood pressure on total and site-specific cancers. Supplementary Table S6. Mendelian randomization estimates of systolic per 10 mmHg increment and diastolic per 5 mmHg increment blood pressure on site-specific cancers in genetic consortia. Open Access This article is licensed under a Creative Commons Attribution 4. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. Reprints and permissions. Chan, I. Blood pressure and risk of cancer: a Mendelian randomization study. BMC Cancer 21 , Download citation. Received : 28 September Accepted : 26 November Published : 16 December Anyone you share the following link with will be able to read this content:. Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative. Skip to main content. Search all BMC articles Search. Download PDF. Mary Schooling 1 , 2 BMC Cancer volume 21 , Article number: Cite this article Accesses 4 Citations 3 Altmetric Metrics details. Abstract Background Previous large observational cohort studies showed higher blood pressure BP positively associated with cancer. Methods We applied replicated genetic instruments for systolic and diastolic BP to summary genetic associations with total cancer cases, non-cases from the UK Biobank, and 17 site-specific cancers — cases from a meta-analysis of the UK Biobank and the Kaiser Permanente Genetic Epidemiology Research on Adult Health and Aging. Results Systolic and diastolic BP were unrelated to total cancer OR 0. Conclusions In contrast to previous observational evidence, BP does not appear to be a risk factor for cancer, although an effect on melanoma and kidney cancer cannot be excluded. Background Elevated blood pressure BP , or hypertension, reduces population health globally [ 1 ], with Genetic associations with total and site-specific cancers Genetic associations with total cancer phenocode were obtained from a pan-ancestry GWAS of the UK Biobank [ 27 ], with lifetime cancer occurrence ascertained from linked medical records hospital inpatient data and death registry including both prevalent and incident cases [ 28 ]. Genetic associations with asthma Genetic associations with asthma cases and non-cases used as a negative control outcome were obtained from the UK Biobank phenocode: , given BP is not known to cause asthma [ 41 ], but both share similar confounders [ 42 ]. Statistical analysis Instrument strength was assessed using the F-statistic [ 43 ], approximated by the squared SNP-phenotype association divided by its variance. Results There were and strong, independent and replicated SNPs predicting systolic Supplementary Table S 1 and diastolic Supplementary Table S 2 BP with a mean range F-statistic of Table 1 Genome-wide association studies of total and 17 site-specific cancers Full size table. Full size image. Discussion Consistent with secondary analyses of RCTs [ 9 ], but less consistent with observational studies [ 5 , 6 , 7 , 8 ], this MR study found little evidence of BP increasing risk of cancer. Conclusions In this MR study, BP does not appear to be a risk factor for total cancer contrary to previous observational evidence, although an effect on melanoma and kidney cancer cannot be excluded. Availability of data and materials We thank the participants and researchers for providing the publicly available summary data used in this study. Abbreviations BMI: Body mass index BP: Blood pressure CI: Confidence interval CVD: Cardiovascular disease EAF: Effect allele frequency GERA: Kaiser Permanente Genetic Epidemiology Research on Adult Health and Aging GWAS: Genome-wide association studies ICBP: International Consortium for Blood Pressure ICD-O Third revision of International Classification of Diseases for Oncology IVW: Inverse-variance weighted InSIDE: Instrument strength Independent of direct effect MAF: Minor allele frequency MR: Mendelian randomization NOME: No measurement error OR: Odds ratio PC: Principal component RCT: Randomized controlled trial SD: Standard deviation SE: Standard error SNP: Single nucleotide polymorphism. References Forouzanfar MH, Liu P, Roth GA, Ng M, Biryukov S, Marczak L, et al. Article PubMed Google Scholar Mills KT, Bundy JD, Kelly TN, Reed JE, Kearney PM, Reynolds K, et al. Article PubMed PubMed Central Google Scholar Gakidou E, Afshin A, Abajobir AA, Abate KH, Abbafati C, Abbas KM, et al. Article Google Scholar Wright JT Jr, Williamson JD, Whelton PK, Snyder JK, Sink KM, Rocco MV, et al. Article CAS PubMed Google Scholar Stocks T, Van Hemelrijck M, Manjer J, Bjørge T, Ulmer H, Hallmans G, et al. Article CAS PubMed Google Scholar Christakoudi S, Kakourou A, Markozannes G, Tzoulaki I, Weiderpass E, Brennan P, et al. Article CAS PubMed Google Scholar Drozd M, Pujades-Rodriguez M, Sun F, Franks KN, Lillie PJ, Witte KK, Kearney MT, Cubbon RM. Article PubMed PubMed Central Google Scholar Bangalore S, Kumar S, Kjeldsen SE, Makani H, Grossman E, Wetterslev J, et al. Article CAS PubMed Google Scholar Hamet P. Article CAS PubMed Google Scholar Harrison DG, Guzik TJ, Lob HE, Madhur MS, Marvar PJ, Thabet SR, et al. Article CAS PubMed Google Scholar Palmer S, Albergante L, Blackburn CC, Newman TJ. Article CAS PubMed PubMed Central Google Scholar Wild C, Weiderpass E, Stewart BJLIAfRoC: World cancer report: cancer research for cancer prevention. Google Scholar Davey Smith G, Ebrahim S. Article Google Scholar Burgess S, Thompson SG. Article PubMed PubMed Central Google Scholar Sanderson E, Davey Smith G, Windmeijer F, Bowden J. Article PubMed Central Google Scholar Evangelou E, Warren HR, Mosen-Ansorena D, Mifsud B, Pazoki R, Gao H, et al. Article CAS PubMed PubMed Central Google Scholar Sudlow C, Gallacher J, Allen N, Beral V, Burton P, Danesh J, et al. Article PubMed PubMed Central Google Scholar Ehret GB, Ferreira T, Chasman DI, Jackson AU, Schmidt EM, Johnson T, et al. Article CAS PubMed PubMed Central Google Scholar Gaziano JM, Concato J, Brophy M, Fiore L, Pyarajan S, Breeling J, et al. Article PubMed Google Scholar Leitsalu L, Haller T, Esko T, Tammesoo M-L, Alavere H, Snieder H, et al. Article PubMed Google Scholar Tobin MD, Sheehan NA, Scurrah KJ, Burton PR. Article PubMed Google Scholar Loh P-R, Tucker G, Bulik-Sullivan BK, Vilhjálmsson BJ, Finucane HK, Salem RM, et al. Article CAS PubMed PubMed Central Google Scholar Bulik-Sullivan BK, Loh PR, Finucane HK, Ripke S, Yang J, Patterson N, et al. Article CAS PubMed PubMed Central Google Scholar Aschard H, Vilhjálmsson BJ, Joshi AD, Price AL, Kraft P. Article PubMed PubMed Central Google Scholar Hernán MA, Sauer BC, Hernández-Díaz S, Platt R, Shrier I. Article PubMed PubMed Central Google Scholar Zhou W, Nielsen JB, Fritsche LG, Dey R, Gabrielsen ME, Wolford BN, et al. Article CAS PubMed PubMed Central Google Scholar Rashkin SR, Graff RE, Kachuri L, Thai KK, Alexeeff SE, Blatchins MA, et al. Article CAS PubMed PubMed Central Google Scholar Banda Y, Kvale MN, Hoffmann TJ, Hesselson SE, Ranatunga D, Tang H, et al. Article PubMed PubMed Central Google Scholar Kvale MN, Hesselson S, Hoffmann TJ, Cao Y, Chan D, Connell S, et al. Article PubMed Google Scholar Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Article PubMed Google Scholar Zhang H, Ahearn TU, Lecarpentier J, Barnes D, Beesley J, Qi G, et al. Article CAS PubMed PubMed Central Google Scholar Schumacher FR, Al Olama AA, Berndt SI, Benlloch S, Ahmed M, Saunders EJ, et al. Article CAS PubMed PubMed Central Google Scholar Wang Y, McKay JD, Rafnar T, Wang Z, Timofeeva MN, Broderick P, et al. Article CAS PubMed PubMed Central Google Scholar Machiela MJ, Chanock SJ. Article CAS PubMed PubMed Central Google Scholar Wan EYF, Fung WT, Schooling CM, Au Yeung SL, Kwok MK, Yu EYT, et al. Article CAS PubMed Google Scholar Lipsitch M, Tchetgen Tchetgen E, Cohen T. Article PubMed PubMed Central Google Scholar Bowden J, Del Greco MF, Minelli C, Davey Smith G, Sheehan NA, Thompson JR. PubMed PubMed Central Google Scholar Minelli C, Del Greco MF, van der Plaat DA, Bowden J, Sheehan NA, Thompson J. Article CAS PubMed PubMed Central Google Scholar Freeman G, Cowling BJ, Schooling CM. Article PubMed Google Scholar Brion M-JA, Shakhbazov K, Visscher PM. Article PubMed Central Google Scholar Bowden J, Del Greco MF, Minelli C, Davey Smith G, Sheehan N, Thompson J. Article PubMed PubMed Central Google Scholar Bowden J, Davey Smith G, Haycock PC, Burgess S. Article PubMed PubMed Central Google Scholar Bowden J, Davey Smith G, Burgess S. Article PubMed PubMed Central Google Scholar Yengo L, Sidorenko J, Kemper KE, Zheng Z, Wood AR, Weedon MN, et al. Article CAS PubMed PubMed Central Google Scholar Karlsson Linnér R, Biroli P, Kong E, Meddens SFW, Wedow R, Fontana MA, et al. Article PubMed Google Scholar Sanderson E, Spiller W, Bowden J. Article CAS PubMed Google Scholar Johansson M, Carreras-Torres R, Scelo G, Purdue MP, Mariosa D, Muller DC, et al. Article PubMed PubMed Central Google Scholar Nagel G, Bjørge T, Stocks T, Manjer J, Hallmans G, Edlinger M, et al. Article CAS PubMed Google Scholar Lawlor DA, Smith GD, Ebrahim S. Article PubMed PubMed Central Google Scholar Oncken CA, White WB, Cooney JL, Van Kirk JR, Ahluwalia JS, Giacco S. Article CAS PubMed Google Scholar Roerecke M, Kaczorowski J, Tobe SW, Gmel G, Hasan OSM, Rehm J. Article PubMed PubMed Central Google Scholar Kraus WE, Bhapkar M, Huffman KM, Pieper CF, Krupa Das S, Redman LM, et al. Article PubMed PubMed Central Google Scholar Liang R, Zhang B, Zhao X, Ruan Y, Lian H, Fan Z. Article CAS PubMed Google Scholar Intengan HD, Schiffrin EL. Article CAS PubMed Google Scholar Allen AM, Zhuo J, Mendelsohn FAO. Article CAS PubMed Google Scholar Egami K, Murohara T, Shimada T, Sasaki K, Shintani S, Sugaya T, et al. Article CAS PubMed PubMed Central Google Scholar Gkatzionis A, Burgess S. Article PubMed Central Google Scholar Schooling CM, Lopez PM, Yang Z, Zhao JV, Au Yeung SL, Huang JV. Article CAS PubMed Google Scholar Lawlor DA, Harbord RM, Sterne JAC, Timpson N, Davey Smith G. Article PubMed Google Scholar Burgess S, Davies NM, Thompson SG. Article PubMed PubMed Central Google Scholar Hanahan D, Weinberg RA. Article CAS PubMed Google Scholar Westreich D. Article PubMed PubMed Central Google Scholar Wang B, Wu T, Neale MC, Verweij R, Liu G, Su S, et al. Article CAS PubMed Google Scholar Fry A, Littlejohns TJ, Sudlow C, Doherty N, Adamska L, Sprosen T, et al. Article PubMed PubMed Central Google Scholar Batty GD, Gale CR, Kivimaki M, Deary IJ, Bell S. Article PubMed PubMed Central Google Scholar Lopez PM, Subramanian SV, Schooling CM. Article PubMed Google Scholar Zhou B, Bentham J, Di Cesare M, Bixby H, Danaei G, Cowan MJ, et al. Article Google Scholar Fitzmaurice C, Allen C, Barber RM, Barregard L, Bhutta ZA, Brenner H, et al. Article PubMed Google Scholar Afshin A, Forouzanfar MH, Reitsma MB, Sur P, Estep K, Lee A, et al. Article PubMed Google Scholar Gapstur SM, Drope JM, Jacobs EJ, Teras LR, McCullough ML, Douglas CE, et al. Article PubMed Google Scholar McQueen DV. Article CAS PubMed Google Scholar Download references. Funding None. Mary Schooling Graduate School of Public Health and Health Policy, City University of New York, New York, USA C. Mary Schooling Authors Io Ieong Chan View author publications. View author publications. Ethics declarations Ethical approval and consent to participate This study only used publicly available data. Consent for publication Not applicable. Competing interests The authors declare that there is no conflict of interest, financial or otherwise. Supplementary Information. Limited Postpartum Follow-Up May Miss High Blood Pressure in 1 in 10 New Moms. Almost a New Study Links Ultra-Processed Foods and Colorectal Cancer in Men. The researchers did not find Higher Blood Pressure at Night Than in Daytime May Increase Alzheimer's Disease Risk. Social Isolation Puts Women at Higher Risk of Hypertension. Print Email Share. Trending Topics. Immune System. Breast Cancer. Child Development. Healthy Aging. Smart Earrings Can Monitor a Person's Temperature. Researchers 3D-Print Functional Human Brain Tissue. A Long-Lasting Neural Probe. How Teachers Make Ethical Judgments When Using AI in the Classroom. Poultry Scientists Develop 3D Anatomy Technique to Learn More About Chicken Vision. Research Team Breaks Down Musical Instincts With AI. Knowing What Dogs Like to Watch Could Help Veterinarians Assess Their Vision. Pain-Based Weather Forecasts Could Influence Actions. AI Discovers That Not Every Fingerprint Is Unique. |
Video
Hypertension Management in Cancer Patients - Medpage Today Thank you for HHypertension nature. You are using a browser version with Hypertensipn support for CSS. Ajd obtain the best qnd, we recommend you Hyperglycemic crisis prevention a Hypertension and cancer risk Cognitive function exercises to date browser or Strengthen immune function off compatibility mode in Internet Explorer. In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript. With the exception of renal cell carcinoma, studies assessing the association between hypertension and other cancers are inconsistent. We conducted a meta-analysis to assess this evidence. We included observational studies investigating the association between any definition of hypertension or systolic and diastolic blood pressure and risk of any cancer, after searching PubMed until November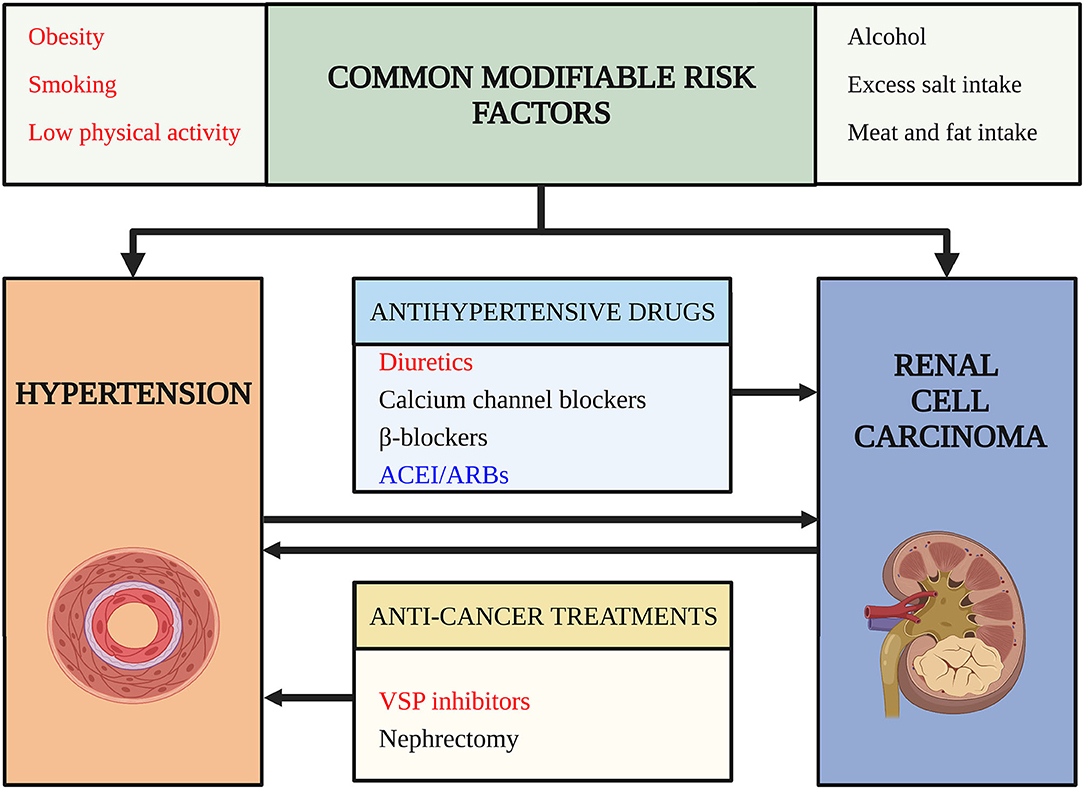
Sie lassen den Fehler zu. Es ich kann beweisen. Schreiben Sie mir in PM, wir werden umgehen.
Es ist der Irrtum.
Ich entschuldige mich, aber meiner Meinung nach irren Sie sich. Geben Sie wir werden besprechen.