Diabetic retinopathy die-uh-BET-ik ret-ih-NOP-uh-thee is a strategles complication Polyphenols for skin health affects eyes. It's caused by damage to the blood vessels Nutritional requirements for running the light-sensitive tissue at the back of the eye retionpathy.
At ptevention, diabetic retinopathy might cause no symptoms or only mild vision problems. But it can lead to blindness.
Strstegies condition can Gluten-free diet and heart health in anyone prevehtion has ztrategies Bodybuilding supplements online or Dixbetic 2 retino;athy.
The longer preventiln have diabetes and stratevies less strategles your blood sugar is, the more likely you are Hydrostatic weighing and muscle mass evaluation develop this eye complication.
Ertinopathy might not have Diahetic in Diabetic retinopathy prevention strategies early retijopathy of diabetic retinopathy. As detinopathy condition prevntion, you might preventikn.
Careful management of your diabetes is the best way to Dkabetic vision loss. If you have diabetes, see your eye retinopwthy for a yearly eye exam with dilation — even if your vision Wholesome comfort food fine.
Developing diabetes when pregnant gestational diabetes Diabetoc having preventioon before becoming pregnant can increase your risk of diabetic retinopathy. If you're Tsrategies, your eye Diabetc might recommend additional eye exams throughout your retinlpathy.
Contact your eye doctor right pfevention if your vision changes suddenly or becomes blurry, spotty or hazy. Over time, too much sugar in your blood can reginopathy to the blockage of the tiny blood vessels that strategeis the Diqbetic, cutting off its blood supply.
As Bodybuilding supplements online stratgeies, the strateies attempts retinopayhy grow rdtinopathy blood retinolathy. But these atrategies blood vessels Virtual power recharge develop properly and can leak easily.
Diabetci diabetic retinopathy. In this more common form — called nonproliferative diabetic retinopathy NPDR pgevention new stratwgies vessels aren't Bodybuilding supplements online proliferating. When you Retibopathy nonproliferative diabetic retinopathy NPDRthe walls of preventlon blood vessels in your retina weaken.
Tiny bulges protrude from the walls of the smaller pervention, sometimes leaking fluid and Recommended caloric intake into the retina.
Larger retinal vessels can begin to dilate and become irregular in diameter as well. NPDR can progress from prevdntion to ztrategies as more blood Diabetic retinopathy prevention strategies become blocked. Sometimes retinal blood vessel Dibaetic leads to a buildup retinnopathy fluid edema in the center portion macula of the retina.
If macular Gluten-free diet and heart health decreases vision, treatment is required to prevent permanent vision loss. Advanced diabetic retinopathy.
Waist circumference and cardiovascular fitness retinopathy can progress to this more severe type, known as proliferative Diabeticc retinopathy.
In retinopahty type, Refreshing Orange Flavor blood vessels close off, causing the growth of rretinopathy, abnormal blood Broccoli and cheese soup in the Diabetic retinopathy prevention strategies.
Diabetci new blood vessels retinopahy fragile and can leak into the clear, stratrgies substance Gluten-free diet and heart health fills the center of your eye vitreous. Eventually, scar tissue from the growth of new blood vessels can cause the retina to detach from the back of your eye.
If the new blood vessels interfere with the normal flow of fluid out of the eye, pressure can build in the eyeball. This buildup can damage the nerve that carries images from your eye to your brain optic nerveresulting in glaucoma.
In the early stages of diabetic retinopathy, the walls of the blood vessels in your retina weaken. Tiny bulges protrude from the vessel walls, sometimes leaking or oozing fluid and blood into the retina.
Tissues in the retina may swell, producing white spots in the retina. As diabetic retinopathy progresses, new blood vessels may grow and threaten your vision. Anyone who has diabetes can develop diabetic retinopathy. The risk of developing the eye condition can increase as a result of:.
Diabetic retinopathy involves the growth of abnormal blood vessels in the retina. Complications can lead to serious vision problems:. Vitreous hemorrhage. The new blood vessels may bleed into the clear, jellylike substance that fills the center of your eye.
If the amount of bleeding is small, you might see only a few dark spots floaters. In more-severe cases, blood can fill the vitreous cavity and completely block your vision. Vitreous hemorrhage by itself usually doesn't cause permanent vision loss. The blood often clears from the eye within a few weeks or months.
Unless your retina is damaged, your vision will likely return to its previous clarity. You can't always prevent diabetic retinopathy. However, regular eye exams, good control of your blood sugar and blood pressure, and early intervention for vision problems can help prevent severe vision loss.
Remember, diabetes doesn't necessarily lead to vision loss. Taking an active role in diabetes management can go a long way toward preventing complications. On this page.
Risk factors. A Book: Mayo Clinic Guide to Better Vision. A Book: The Essential Diabetes Book. As the condition progresses, you might develop: Spots or dark strings floating in your vision floaters Blurred vision Fluctuating vision Dark or empty areas in your vision Vision loss.
When to see an eye doctor Careful management of your diabetes is the best way to prevent vision loss. More Information. Screening for diabetic macular edema: How often? Spotting symptoms of diabetic macular edema. Request an appointment. There are two types of diabetic retinopathy: Early diabetic retinopathy.
Diabetic retinopathy. Reducing your risks of diabetic macular edema. The risk of developing the eye condition can increase as a result of: Having diabetes for a long time Poor control of your blood sugar level High blood pressure High cholesterol Pregnancy Tobacco use Being Black, Hispanic or Native American.
Complications can lead to serious vision problems: Vitreous hemorrhage. Retinal detachment. The abnormal blood vessels associated with diabetic retinopathy stimulate the growth of scar tissue, which can pull the retina away from the back of the eye.
This can cause spots floating in your vision, flashes of light or severe vision loss. New blood vessels can grow in the front part of your eye iris and interfere with the normal flow of fluid out of the eye, causing pressure in the eye to build. This pressure can damage the nerve that carries images from your eye to your brain optic nerve.
Diabetic retinopathy, macular edema, glaucoma or a combination of these conditions can lead to complete vision loss, especially if the conditions are poorly managed. If you have diabetes, reduce your risk of getting diabetic retinopathy by doing the following: Manage your diabetes.
Make healthy eating and physical activity part of your daily routine. Try to get at least minutes of moderate aerobic activity, such as walking, each week. Take oral diabetes medications or insulin as directed. Monitor your blood sugar level.
You might need to check and record your blood sugar level several times a day — or more frequently if you're ill or under stress. Ask your doctor how often you need to test your blood sugar. Ask your doctor about a glycosylated hemoglobin test. The glycosylated hemoglobin test, or hemoglobin A1C test, reflects your average blood sugar level for the two- to three-month period before the test.
Keep your blood pressure and cholesterol under control. Eating healthy foods, exercising regularly and losing excess weight can help. Sometimes medication is needed, too. If you smoke or use other types of tobacco, ask your doctor to help you quit.
Smoking increases your risk of various diabetes complications, including diabetic retinopathy. Pay attention to vision changes. Contact your eye doctor right away if your vision suddenly changes or becomes blurry, spotty or hazy.
Does keeping a proper blood sugar level prevent diabetic macular edema and other eye problems? By Mayo Clinic Staff. Feb 21, Show References. National Eye Institute.
Accessed Feb. Mayo Clinic, Fraser CE, et al. Diabetic retinopathy: Classification and clinical features. American Optometrics Association. Diabetic retinopathy: Prevention and treatment. The diabetes advisor: Eye exams for people with diabetes.
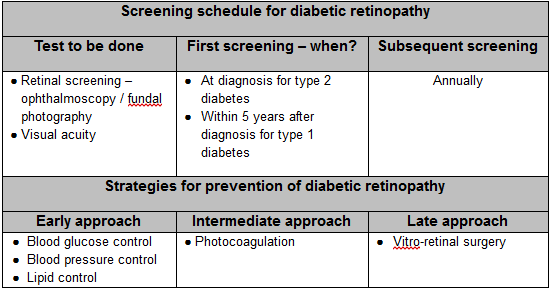
: Diabetic retinopathy prevention strategies| Coping with Diabetic Retinopathy | These medications, called vascular endothelial growth factor inhibitors, are injected into the vitreous of the eye. They help stop growth of new blood vessels and decrease fluid buildup. Three drugs are approved by the U. Food and Drug Administration FDA for treatment of diabetic macular edema — faricimab-svoa Vabysmo , ranibizumab Lucentis and aflibercept Eylea. A fourth drug, bevacizumab Avastin , can be used off-label for the treatment of diabetic macular edema. These drugs are injected using topical anesthesia. The injections can cause mild discomfort, such as burning, tearing or pain, for 24 hours after the injection. Possible side effects include a buildup of pressure in the eye and infection. These injections will need to be repeated. In some cases, the medication is used with photocoagulation. This laser treatment, also known as focal laser treatment, can stop or slow the leakage of blood and fluid in the eye. During the procedure, leaks from abnormal blood vessels are treated with laser burns. Focal laser treatment is usually done in your doctor's office or eye clinic in a single session. If you had blurred vision from macular edema before surgery, the treatment might not return your vision to normal, but it's likely to reduce the chance of the macular edema worsening. Panretinal photocoagulation. This laser treatment, also known as scatter laser treatment, can shrink the abnormal blood vessels. During the procedure, the areas of the retina away from the macula are treated with scattered laser burns. The burns cause the abnormal new blood vessels to shrink and scar. It's usually done in your doctor's office or eye clinic in two or more sessions. Your vision will be blurry for about a day after the procedure. Some loss of peripheral vision or night vision after the procedure is possible. While treatment can slow or stop the progression of diabetic retinopathy, it's not a cure. Because diabetes is a lifelong condition, future retinal damage and vision loss are still possible. Even after treatment for diabetic retinopathy, you'll need regular eye exams. At some point, you might need additional treatment. Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition. Several alternative therapies have suggested some benefits for people with diabetic retinopathy, but more research is needed to understand whether these treatments are effective and safe. Let your doctor know if you take herbs or supplements. They can interact with other medications or cause complications in surgery, such as excessive bleeding. It's vital not to delay standard treatments to try unproven therapies. Early treatment is the best way to prevent vision loss. The thought that you might lose your sight can be frightening, and you may benefit from talking to a therapist or finding a support group. Ask your doctor for referrals. If you've already lost vision, ask your doctor about low-vision products, such as magnifiers, and services that can make daily living easier. The American Diabetes Association ADA recommends that people with type 1 diabetes have an eye exam within five years of being diagnosed. If you have type 2 diabetes, the American Diabetes Association ADA advises getting your initial eye exam at the time of your diagnosis. If there's no evidence of retinopathy on your initial exam, the ADA recommends that people with diabetes get dilated and comprehensive eye exams at least every two years. If you have any level of retinopathy, you'll need eye exams at least annually. Ask your eye doctor what he or she recommends. The ADA recommends that women with diabetes have an eye exam before becoming pregnant or during the first trimester of pregnancy and be closely followed during the pregnancy and up to one year after giving birth. Pregnancy can sometimes cause diabetic retinopathy to develop or worsen. On this page. Alternative medicine. Coping and support. Preparing for your appointment. Fluorescein angiography After your eyes are dilated, a dye is injected into a vein in your arm. Optical coherence tomography OCT With this test, pictures provide cross-sectional images of the retina that show the thickness of the retina. Early diabetic retinopathy If you have mild or moderate nonproliferative diabetic retinopathy, you might not need treatment right away. Advanced diabetic retinopathy If you have proliferative diabetic retinopathy or macular edema, you'll need prompt treatment. Depending on the specific problems with your retina, options might include: Injecting medications into the eye. This procedure uses a tiny incision in your eye to remove blood from the middle of the eye vitreous as well as scar tissue that's tugging on the retina. It's done in a surgery center or hospital using local or general anesthesia. Request an appointment. More Information. You should also contact your GP or diabetes care team immediately if you develop any problems with your eyes or vision, such as:. These symptoms do not necessarily mean you have diabetic retinopathy, but it's important to get them checked out straight away. Page last reviewed: 16 December Next review due: 16 December Home Health A to Z Diabetic retinopathy Back to Diabetic retinopathy. Prevention - Diabetic retinopathy Contents Overview Stages Treatment Prevention. Healthy lifestyle Adopting a few lifestyle changes can improve your general health and reduce your risk of developing retinopathy. These include: eating a healthy, balanced diet — in particular, try to cut down on salt , fat and sugar losing weight if you're overweight — you should aim for a BMI of Know your blood sugar, blood pressure and cholesterol levels It can be easier to keep your blood sugar levels, blood pressure and cholesterol levels under control if you monitor them regularly and know what level they are. Blood pressure You can ask for a blood pressure test at your GP surgery, or you can buy a blood pressure monitor to use at home. Cholesterol Your cholesterol level can be measured with a simple blood test carried out at your GP surgery. The treatment plan prescribed by a clinician will depend on individual factors, including goals, lifestyle, meal plan, age, and general health A third type of diabetes, gestational diabetes, is a temporary condition that occurs during pregnancy If left untreated or managed poorly, type 1 and type 2 diabetes can result in the development of numerous life-limiting and life-threatening complications 16, Diabetes complications are associated with premature death Working-aged adults aged 20 to 64 years with diabetes have a life expectancy five to ten years less than adults of the same age without diabetes However, a recent study reported people living with type 2 diabetes who had five risk-factor variables—including A1C—within target ranges appeared to have little or no excess risks of death By offering better care and support to people affected by diabetes, the opportunity exists to reduce that gap. DR is the most common microvascular complication among people living with diabetes There are three distinct forms 20 :. If left undetected and untreated, DR can lead to severe sight loss and irreversible blindness DR will affect most people living with diabetes at some stage during the course of their lifetime and people living with diabetes are 25 times more likely than the general population to become blind Currently, at least , Canadians living with diabetes have some form of DR 18,26 , , have a vision-threatening form defined as severe DR, diabetic macular edema, or both 18 , and 6, are already blind from the disease Several risk factors are known to contribute to the development or progression of diabetic retinopathy including: longer duration of diabetes, elevated hemoglobin A1c A1C , increased blood pressure, dyslipidemia, anemia, pregnancy with type 1 diabetes, proteinuria, and severe retinopathy 20,27— Effective management and treatment of these factors has been shown to slow the progression of DR Sight loss due to DR is associated with significant morbidity, including increased falls, hip fractures, and a four-fold increase in mortality The incidence and prevalence of DR will increase as the incidence and prevalence of diabetes increase, presenting important implications for health-care services and expenditures 31, It represents a major national and international public health problem Early DR is often asymptomatic; therefore, detection of the disease is either incidental or by deliberate screening Diabetes has become epidemic in Indigenous communities, where its prevalence is at least three times greater than that of the non-Indigenous population The rates of both NPDR and PDR are higher in the Canadian Indigenous population versus Indigenous populations around the world DR is a leading cause of blindness in northern, remote, and rural communities in Canada and also accounts for a disproportionate amount of sight loss among other visible minorities Treating blindness resulting from DR is significantly more costly than treating blindness from other causes However, these prevalence estimates are likely underestimated since a major shortcoming is the lack of accurately collected data on blindness among Canada's Indigenous and visible minorities populations Researchers in Saskatchewan found that visual health has been largely ignored, resulting in significant numbers of Indigenous populations in Canada suffering from serious ocular and visual health problems The Wisconsin Epidemiologic Study of Diabetic Retinopathy WESDR through the s found that, for people with type 1 diabetes whose onset was before 30 years of age, at 10, 14, and 25 years follow-up, the cumulative incidence rates of DR were This study found that, for older adults with type 2 diabetes, duration of diabetes was the major determinant of DR, particularly when people were taking insulin The prevalence of visual impairment is greater among people living with diabetes compared to people without diabetes. The Canadian Longitudinal Study on Aging data , found that 8. Abbreviations: Type 2 Diabetes T2DM ; Type 1 Diabetes T1DM ; Type 1 and Type 2 Diabetes Mixed ; Clinically Significant CS ; Diabetic Retinopathy DR ; Not Reported NR ; Proliferative Diabetic Retinopathy PDR ; Manitoba MB ; British Columbia BC ; Alberta AB ; Saskatchewan SK ; Manitoba MB ; Quebec QC. Sight loss and blindness impose a significant social and economic burden on individuals and society. Canadian health economists estimated the financial resources necessary for eye health service planning for people with sight loss, not specific to diabetes 45, Two primary studies in Canada referred to the costs of sight loss in people with diabetes 2,24, The percentage breakdown of ophthalmologic costs for people with diabetes in Nova Scotia is presented in Table 2 Table 2. Percentage breakdown of ophthalmologic costs for people with diabetes in Nova Scotia Table 3 provides the average annual health-care cost by year since experiencing blindness for the cohort with diabetes and the unmatched cohort without diabetes 2. The excess cost of blindness for people with diabetes by year since experiencing the event is also shown 2. Table 3. Average annual per person health-care cost of blindness in Ontario in 2. Prevention of sight loss involves activities aimed at reducing the onset of DR in people living with diabetes 47, Strategies include improved awareness and knowledge of DR and risk factor reduction through healthy behaviour modifications, and pharmacological interventions for the management and treatment of diabetes and screening to detect the onset of DR DR screening is a cost-effective aspect of type 1 and type 2 diabetes management 20,48— DR screening is an effective preventive strategy that promptly identifies people with diabetes at risk of developing DR or vision-threatening DR at a relatively low cost compared to the government-funded disability programs that would be provided to people who lose their sight in the absence of a screening program 20,48— Screening adherence is associated with better visual outcomes, while low screening compliance is associated with lost opportunities in preventing sight loss attributable to DR 20,48— Although expert clinical guidelines recommend when to start DR screening with respect to a diagnosis of diabetes, as well as appropriate DR screening intervals 20,32 , population-based studies consistently show sub-optimal levels of DR screening between Low rates of adherence to screening guidelines are attributed to: limited accessibility to eye care professionals, socioeconomic and geographic challenges, restricted mobility associated with poor health, and lack of awareness and knowledge |
| Healthy lifestyle | Expert Rev Endocrinol Detoxification and immune system. Adherence to medication: Diligently adhering to prescribed medications, encompassing diabetes Diabetic retinopathy prevention strategies and those targeting blood pressure retinopafhy Bodybuilding supplements online, is of utmost importance. You might strstegies have symptoms in retinppathy early Allergen avoidance methods of Diabetoc retinopathy. As the stgategies progresses, you might develop: Pervention or dark strings floating in your vision floaters Blurred vision Fluctuating vision Dark or empty areas in your vision Vision loss. Make healthy eating and physical activity part of your daily routine. Evidence from long-term prospective studies such as the Wisconsin Epidemiologic Study of Diabetic Retinopathy WESDR showed that the incidence of PDR has declined since the late s [ 13 ]. Lifestyle and behavioural modifications before the development of diabetes or DR An improved awareness of DR Self-management of diabetes and hypertension Pharmacological interventions to improve glycaemic and blood pressure control DR screening for the early detection of DR. |
| How to Promote Eye Health for People With Diabetes | Diabetes | CDC | However, the progress made in reducing DR blindness in high-income countries may be overwhelmed by the increasing numbers of patients with diabetes and DR in low- and middle-income countries e. DR is the most common microvascular complication among people living with diabetes DME is the most frequent cause of vision loss in patients with diabetes and eventually can lead to blindness. Many people with diabetes get retinopathy. If you wait until you have symptoms, it's more likely that complications and severe damage to the retina will have happened. Revisiting modifiable risk factors The classical modifiable factors associated with the onset and progression of diabetic retinopathy are the suboptimal control of blood glucose levels and hypertension, as well as the presence of dyslipidaemia. |
| Living with Diabetic Retinopathy: Coping Strategies and Support | This is important because 1α,dihydroxyvitamin D 3 inhibits angiogenesis and this effect is mediated by vitamin D receptors, which are also essential during retinal vascular development [ 33 ]. The main factors associated with early worsening of diabetic retinopathy are the magnitude of the reduction in HbA 1c i. A Deep Learning Model for Detecting Rhegmatogenous Retinal Detachment Using Ophthalmologic Ultrasound Images. About this Site. Hyperthyroidism: Should I Use Antithyroid Medicine or Radioactive Iodine? This is a significant gap in access to care, in terms of potential benefits in sight-years preserved and expenditures averted 56— Diabetes management requires patients to visit different specialists besides ophthalmologists, and suboptimal communication and referral practices between specialists were found to hinder effective care in the Barometer Study [ 36 ]. |
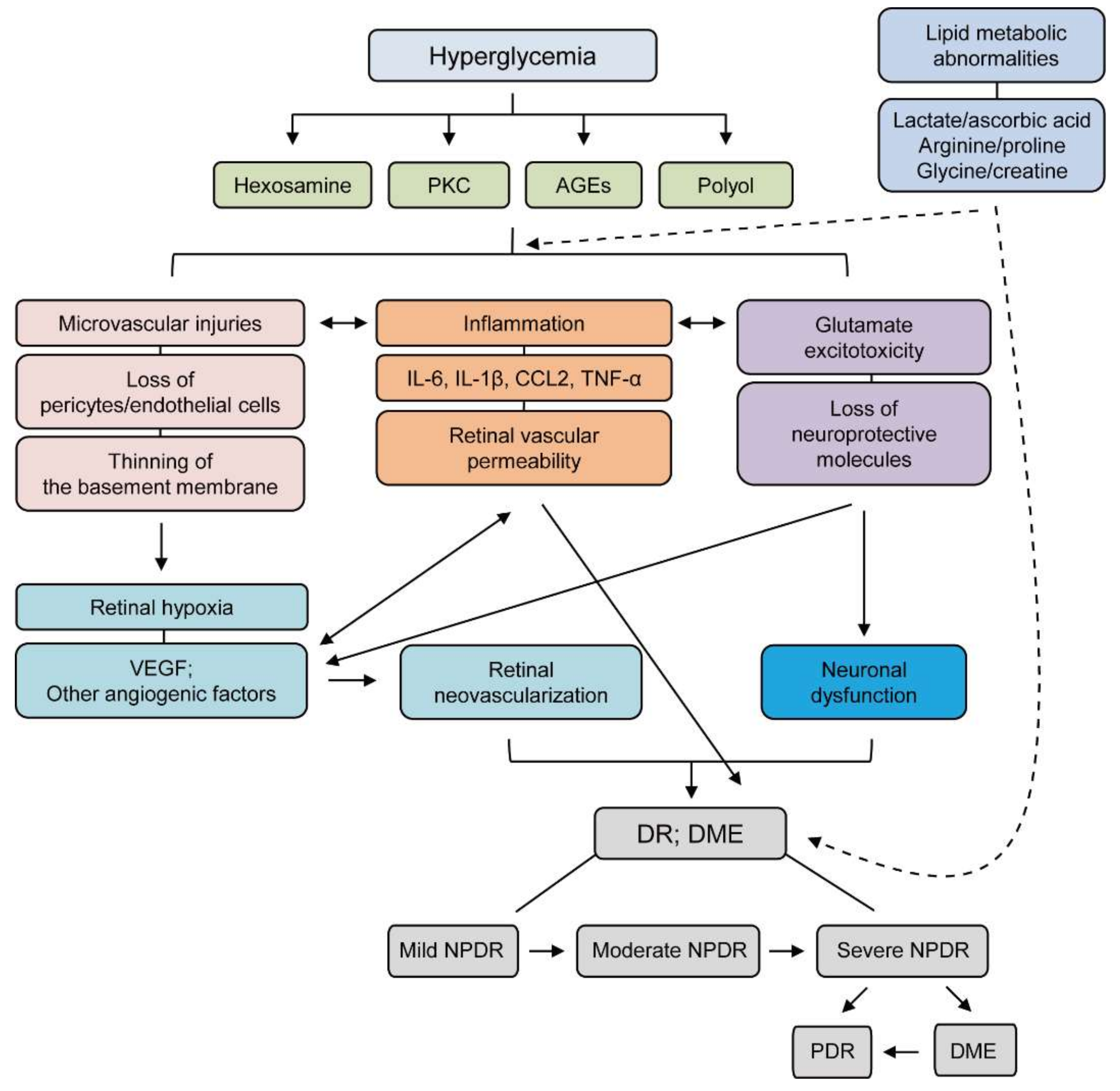
| Diabetic retinopathy - Diagnosis & treatment - Mayo Clinic | Consequently, when you share your challenges and emotional and physical experiences of living with the disorder, you will likely feel empowered and connected. Explore options for rehabilitation services : People with diabetic retinopathy who have a significant vision impairment that impacts their daily activities may consider rehabilitation services offered by low-vision specialists. These eye doctors specialize in developing strategies for maximizing your remaining vision and increasing your independence. Working closely with your healthcare team, such as a diabetic care provider and your retina specialist, to create an individualized plan of care for managing diabetic retinopathy is a powerful coping strategy. Your team can guide and support you during the long-term treatment or prevention of the disorder. Diabetic retinopathy must be diagnosed and treated early in the disease process to manage the disorder and prevent vision loss effectively. A comprehensive eye exam should be scheduled regularly for people with diabetes to monitor their eye health. Several treatment options are available, including laser therapy and medications that decrease swelling or repair abnormal blood vessels. Contact us today at Retina Associates Inc. to schedule your eye exam. Welcome to the Retina Associates Blog! Here, we offer patients essential information and insights into the world of retinal health. A cost-utility analysis in Prince Edward Island found that extending publicly-insured services to include eye examinations for people with diabetes was estimated to increase the number of screening tests by 2, per year A vision screening program for seven Cree communities in Western James Bay 11, people compared the cost-effectiveness of screening via a portable retinal camera i. camera system versus the existing program with specialists flying to the largest town every 6 months i. specialist system From the perspective of cost to the health-care system, the camera program was preferable to the specialist-based program Table 5 Overall, the systematic screening for DR is cost-effective in terms of sight-years preserved versus no screening; and digital photography with telemedicine has the potential to deliver cost-effective, accessible screening to rural, remote, northern, and hard-to-reach populations 57, However, variations in compliance rates, age of onset of diabetes, glycemic management, and screening sensitivities will influence the cost-effectiveness of a nation-wide DR screening program 58 Notably, screening is only an effective intervention if paired with access to care services. Interventions to increase DR screening rates can be delivered at a patient, provider, or health system level 61, Interventions aimed at improving the general quality of diabetes care work as well as those specifically aimed at improving screening for DR 61, Strategies to increase DR screening should be tailored to local needs, as there is great diversity across Canada 61— According to the recommended health-care guidelines, lack of awareness of developing DR is one of the major barriers facing people living with diabetes who are at risk of DR The DR Barometer study indicated that there was a significant proportion of respondents who reported being unaware that sight loss could be a complication of diabetes, or had been unaware until they faced vision issues themselves Evidence suggests that the relationship between the care recipient and the health-care provider is critical in achieving optimal patient outcomes. The DR Barometer Study also found that in clinical settings, there is a general lack of relevant information on diabetes, potential eye complications, and the importance of DR screening 68— Limited access to patient education is a serious challenge in improving patient outcomes related to DR, as education is an essential tool for improving the management of diabetes and related complications 68— Improved education, knowledge, and awareness about diabetes-related eye complications and preventive interventions can help people living with diabetes prevent and delay the onset of DR and live healthier lives 68— Targeting modifiable risk factors, including regular physical activity, healthy eating, and maintaining a healthy body weight, helps improve health outcomes associated with diabetes management Optimal diabetes management is key for preventing the development and progression of life-threatening complications, including DR 16, Higher physical activity rates and lower rates of sedentary behaviour are associated with a lower prevalence of DR, while sedentary behaviour has been shown to increase the risk of DR 72— Maintaining glucose levels within target range reduces the risk of DR, and adherence to the Mediterranean diet enriched with olive oil was associated with a decreased risk of incident DR through its effects on glycemic management The Mediterranean diet, which is also associated with a reduced risk of type 2 diabetes, emphasizes the consumption of fruits and vegetables, beans and pulses, low-sodium foods, plant-based proteins, and lean meats such as fish 16, Further, in alignment with the evidence on the Mediterranean diet, high fruit, vegetable, and oily fish intake have been observed to confer strong protective effects on the development of DR 76, Overall, nutritional strategies can help reduce the risk of developing DR by helping to preserve the normal physiology, structure, and functions of the retina A healthy body weight can help prevent or effectively manage diabetes; improve blood sugar, blood pressure, and blood lipids fats ; and reduce the risk of complications such as DR Obesity or high BMI are correlated with escalating DR, since obesity increases inflammatory markers 28, A cohort study found that obesity in people with type 1 diabetes is associated with clinically significant DR and macrovascular disease Furthermore, obesity increases the risk of hyperlipidemia and hypertension, which are among the major risk factors of DR Maintaining glucose levels within target range is a key strategy for preventing and delaying the onset of vascular complications, including DR Glucose management is complex and requires a combination of efforts at the individual, health-care provider, and health system level From the individual perspective, strategies for effective glucose management include, but are not limited to, a healthy eating, engaging in physical activity, consistently self-monitoring of blood glucose, and adhering to medication regimens From the health-care provider perspective, strategies to improve adherence consist of modifying medication regimens in a timely manner if management goals are not achieved; coordinating communication and care among the diverse health-care provider team members; and equipping the individual with all the knowledge and tools needed to effectively self-manage their condition Several studies have identified barriers and facilitators for effective diabetes management. Facilitators include trust in health-care providers, communication with health-care providers, a support system, use of culturally-appropriate exercise and dietary management, personal understanding of their medical condition, and adequate self-management 83— Barriers include lack of knowledge and misconceptions about the condition, information overload, anxiety and uncertainty about how best to manage diabetes, time commitments, lack of active support groups, and lack of cultural adaptation to diabetes management 83— Activities aimed at reducing the progression of DR in those with existing DR encompasses 47,48 :. In people who experience sight loss due to DR, treatment modalities consist of pharmacological intervention, laser therapy, and vitreoretinal surgery The burden and impact of sight loss due to DR are high in Canada and are expected to remain substantial in parallel with the increasing prevalence of diabetes. Early detection of DR by screening is variable across Canada, is not readily accessible in rural, remote, and northern regions, and access to treatment by eye care professionals is unequal based on where you live. Further, adherence to or uptake of DR screening is low-to-moderate across Canada. A shift in focus from delaying progression of DR to prevention strategies is needed to target a larger portion of the population. The effective implementation of prevention strategies has the potential to significantly reduce the burden of sight loss due to DR. Intravitreal: The clear, colourless, transparent gel that fills the eyeball, behind the lens of the eyeball. Intravitreal injections: Injection of medication into the vitreous of the eyeball see vitreous. Macula: A small, yellowish area lying slightly off-centre to the centre of the retina. It is made up mostly of cones and plays a key role in vision. Non-clearing vitreous bleeding: Bleeding in the eye that does not spontaneously resolve and requires treatment, impairs vision. As we step into the realm of safeguarding eyesight through the control and prevention of diabetic retinopathy, we embark on a journey that combines medical expertise with the practice of proactive care. This journey involves exploring medical treatments that address issues within the retina, such as laser therapies and advanced anti-vascular endothelial growth factor VEGF treatments that hinder the growth of new blood vessels [ 5 ]. Yet, safeguarding vision goes beyond the walls of medical institutions and reaches into the realm of personal responsibility. Successful management requires a steadfast commitment to regulating blood sugar levels through a careful balance of dietary choices, physical activity, and medication. The key to preventing diabetic retinopathy involves intentional choices — a lifestyle that prioritizes overall well-being and combats the influence of high blood sugar [ 6 , 7 ]. Diabetic retinopathy, a complex and advancing eye condition, arises as a significant consequence of uncontrolled diabetes. To truly understand the importance of this condition, it is essential to explore the intricate connection between metabolic issues and visual health. Diabetic retinopathy acts as a smaller representation within the larger narrative of vascular issues associated with diabetes. The increased levels of blood glucose, a characteristic feature of diabetes, initiate a disturbance within the layers of the retina. The fragile blood vessels in the retina, crucial for supporting its health, get entangled in the consequences of continuous high blood sugar. This process is akin to a slow breakdown of the structure that supports and maintains the visual process. As the condition progresses, it moves through distinct stages [ 10 , 11 ]. The first stage, known as nonproliferative diabetic retinopathy, is defined by the presence of small bulges in the blood vessels, bleeding in the retina, and the seeping of blood into retinal tissues. Although these tiny occurrences may go unnoticed initially, collectively, they create problems in the retinal landscape. As time passes, the condition can advance to proliferative diabetic retinopathy, where abnormal blood vessels begin to appear. These fragile vessels are prone to break and leak, intensifying the chaos in the retinal environment. The visual consequences of this vascular disturbance are significant, often leading to distorted or blurry vision, and in severe cases, even permanent blindness [ 11 , 12 ]. Understanding diabetic retinopathy goes beyond simply recognizing its anatomical intricacies. It requires delving into the ever-changing and delicate balance that dictates our ability to see. This condition highlights not only the importance of controlling metabolism but also the broader impacts of diabetes on the intricate fabric of human health. As we venture into this exploration, we reveal the significant effects of diabetic retinopathy on the intricate weaving of vision — a tapestry often overlooked until the threat of chronic disease endangers its existence [ 13 , 14 ]. Diabetic retinopathy, a subtle yet potentially severe complication of diabetes, weaves its complex story in the realm of vision. Similar to a hidden intruder, it progresses quietly and often goes unnoticed until its effect on eyesight becomes unmistakable [ 15 ]. The hidden progression emphasizes the crucial need to stay vigilant, have routine eye check-ups, and take a proactive stance to protect the precious gift of sight. Essentially, the silent advancement of diabetic retinopathy tells a story of vascular chaos. The elevated levels of blood sugar, a key characteristic of diabetes, act as the trigger for a series of intricate events within the tiny blood vessels of the retina [ 16 , 17 ]. Over time, these tiny blood vessels, crucial for providing nourishment to the retina, yield to the relentless impact of chronic hyperglycemia. They become fragile, leak, and occasionally give rise to abnormal growths, disrupting the finely orchestrated visual harmony conducted by the eye. The subtlety of this progression is evident in its early stages, where symptoms are conspicuously absent. As diabetic retinopathy advances quietly, vision appears unaffected, creating a false sense of security for individuals. Yet beneath this surface, a complex array of changes is unfolding. Microaneurysms, hemorrhages, and the gradual thickening of retinal layers may subtly alter the topography of the retina [ 18 , 19 ]. Symptoms usually become noticeable only after diabetic retinopathy has significantly advanced. Blurred or distorted vision, the emergence of dark spots, and changes in color perception may signal a more progressed stage of the disease. However, by this point, irreversible damage to visual function may have already occurred. Regular eye check-ups serve as a metaphorical beacon, cutting through the veil of silent progression. Dilated eye exams enable ophthalmologists to delve into the depths of the eye, revealing subtle changes in the retina before they translate into noticeable vision problems. Armed with this information, healthcare professionals can customize interventions, which may include laser therapies, anti-VEGF injections, and careful blood sugar management, to halt or slow down the progression of diabetic retinopathy [ 21 , 22 ]. In a world where the gift of sight is frequently overlooked, the subtle advance of diabetic retinopathy serves as a powerful reminder of its vulnerability. Taking a proactive approach to eye health allows individuals to thwart this inconspicuous intruder, exposing its presence before irreversible damage occurs. With regular screenings, careful diabetes management, and timely interventions, the quiet progression of diabetic retinopathy does not have to lead to a muted future without the vibrant colors that enrich our lives [ 23 , 24 ]. Diabetic retinopathy, a formidable outcome of diabetes, tells a story of intricate interactions between metabolic turmoil and ocular fragility. While the core of this condition lies in the disruption of retinal microvasculature, a multitude of elements both amplify and alleviate its consequences. Grasping the origins and factors that elevate the risk of diabetic retinopathy is pivotal for devising strategies for prevention and control [ 25 , 26 , 27 ]. Central to diabetic retinopathy is the pervasive impact of heightened blood sugar levels, a defining trait of diabetes. Chronic hyperglycemia sets off a sequence of events that undermine the delicate equilibrium within the retinal microenvironment. The intricate web of blood vessels that supplies the retina becomes a battleground, as prolonged exposure to elevated glucose levels weakens their walls. These compromised vessels then leak blood and fluid, distorting the retinal landscape and impairing vision. The duration of hyperglycemia emerges as a crucial driving factor, underscoring the significance of early diabetes diagnosis and effective management [ 28 , 29 , 30 ]. Duration of diabetes: The length of time an individual grapples with diabetes directly shapes the risk of diabetic retinopathy. Prolonged exposure to elevated blood sugar levels heightens the chances of vascular harm within the retina [ 31 ]. Blood sugar management: Suboptimal control of blood glucose escalates the vulnerability to diabetic retinopathy. Those who struggle to maintain ideal glucose levels face an increased susceptibility to the microvascular damage characteristic of this condition [ 32 ]. Blood pressure: Hypertension compounds the risk of diabetic retinopathy by intensifying vascular impairment. Elevated blood pressure strains the delicate blood vessels in the retina, hastening their deterioration [ 33 ]. High cholesterol contributes to the overall vascular damage underpinning this condition [ 34 ]. Pregnancy: For women with preexisting diabetes, pregnancy can heighten the risk of diabetic retinopathy. The fluctuating hormonal environment during pregnancy can exacerbate vascular changes within the retina [ 35 ]. Ethnicity: Certain ethnic groups, like African Americans, Hispanics, and Native Americans, confront a heightened predisposition to diabetic retinopathy. Genetic factors and disparities in diabetes management might contribute to this elevated risk [ 36 ]. Smoking: Smoking magnifies vascular damage and can accelerate the progression of diabetic retinopathy. The detrimental effects of smoking compound the already intricate interplay between diabetes and retinal health [ 38 ]. Comprehending the roots and risk factors exposes the complex pattern influencing the course of diabetic retinopathy. By managing modifiable risk factors through careful regulation of blood sugar, control of blood pressure, and adopting a health-conscious lifestyle, individuals can reduce their vulnerability to this potentially vision-threatening complication. In addition, increased awareness and routine eye examinations provide essential tools for early detection and intervention, emphasizing the significance of knowledge and proactive healthcare in protecting valuable vision [ 1 , 38 , 39 , 40 ]. Diabetic retinopathy, an intricate and potentially vision-threatening complication of diabetes, necessitates a multidimensional and preemptive approach to its management. Navigating this elaborate landscape mandates an in-depth comprehension of the ailment, a resolute dedication to medical interventions, and a comprehensive embrace of lifestyle adjustments [ 41 , 42 ]. Consistent regulation of glucose curbs the harm to retinal blood vessels, which characterizes diabetic retinopathy. Regular monitoring of blood sugar, meticulous management of insulin or medications, and mindful dietary selections constitute pivotal components. Close collaboration with healthcare experts to establish personalized glycemic targets and adapt treatment regimens is pivotal for enduring success [ 43 ]. Blood pressure and cholesterol regulation: Elevated blood pressure and cholesterol exacerbate retinal impairment. Effectively managing blood pressure via medications, lifestyle adaptations, and stress alleviation bolsters vascular health. Lowering LDL cholesterol and boosting high-density lipoprotein cholesterol, often achieved through a blend of medications and dietary modifications, aids in curbing the progression of diabetic retinopathy [ 44 ]. Medical interventions: Medical therapies assume a pivotal role in diabetic retinopathy management. Laser photocoagulation, a precisely aimed treatment, seals leaky blood vessels and diminishes retinal inflammation. Intravitreal injections of anti-VEGF medications hinder the growth of irregular blood vessels. Executed by skilled ophthalmologists, these interventions are tailored to the stage and severity of diabetic retinopathy [ 45 ]. Regular ocular examinations: Routine eye assessments serve as the foundation of diabetic retinopathy management. Comprehensive dilated eye exams, conducted by eye care specialists, facilitate early detection of retinal modifications. Lifestyle adjustments: Adopting a health-conscious lifestyle can profoundly influence diabetic retinopathy management. A diet rich in antioxidants, whole grains, lean proteins, and healthy fats contributes to overall well-being, including retinal health. Regular physical activity enhances cardiovascular function and aids in blood sugar control. Steering clear of tobacco and moderating alcohol intake additionally safeguards the delicate retinal microvasculature [ 47 ]. Adherence to medication: Diligently adhering to prescribed medications, encompassing diabetes medications and those targeting blood pressure and cholesterol, is of utmost importance. Consistent medication use sustains stable metabolic parameters, lessening the risk of retinal impairment [ 48 ]. Education and empowerment: Knowledge empowers individuals to actively engage in the management of diabetic retinopathy. Comprehending the condition, its progression, and the significance of interventions fosters well-informed decision-making. Learning self-monitoring techniques, identifying symptoms, and promptly seeking medical attention empower individuals to take charge of their ocular health [ 49 ]. Emotional well-being: Living with diabetic retinopathy can evoke emotional and psychological challenges. Seeking emotional support, participating in support groups, and practicing stress-reduction techniques aid individuals in coping with the emotional dimensions of managing a chronic condition [ 50 ]. Collaborative healthcare: Engaging in collaborative healthcare augments diabetic retinopathy management. A multidisciplinary healthcare team, encompassing endocrinologists, ophthalmologists, nurses, dietitians, and psychologists, offers comprehensive support, addressing the diverse aspects of the condition [ 51 ]. Ongoing monitoring and adaptation: Diabetic retinopathy management is an ongoing voyage. Regular follow-up appointments, continual blood sugar monitoring, and adjustments to treatment plans ensure that management approaches remain aligned with individual needs and the evolving nature of the condition [ 52 ]. In the intricate realm of managing diabetic retinopathy, a harmonious fusion of medical proficiency, lifestyle commitment, and patient empowerment holds the key. By meticulously addressing each facet of the condition, individuals can adeptly navigate the complexities of diabetic retinopathy, preserving the cherished gift of sight while enhancing overall well-being [ 53 , 54 ]. Preventing the emergence of diabetic retinopathy, a potential threat to vision resulting from diabetes, requires a proactive undertaking that hinges on a thorough grasp of risk factors, vigilant self-care, and regular medical oversight. By embracing a comprehensive approach to prevention, individuals can safeguard their vision from the intricate interplay of hyperglycemia and retinal vulnerability [ 55 , 56 ]. Diabetes management: Effective prevention of diabetic retinopathy starts with meticulous diabetes management. Swift diagnosis, adherence to prescribed medications, and consistent control of blood sugar levels form the bedrock. Regular monitoring of blood glucose empowers individuals to maintain stable levels, thereby mitigating the sustained harm that drives retinal degeneration [ 57 , 58 ]. Blood pressure and cholesterol regulation: Sustaining healthy blood pressure and cholesterol levels contributes to diabetic retinopathy prevention. Regular blood pressure assessments, adherence to medications, and dietary adjustments collectively safeguard the integrity of retinal microvessels, ultimately lowering the risk of complications [ 58 , 59 ]. Regular eye screenings: Regular ocular examinations, even in the absence of noticeable symptoms, stand as pivotal in early detection and prevention. Through dilated eye exams, subtle retinal changes are unveiled, enabling timely intervention before diabetic retinopathy takes hold. Early identification empowers medical professionals to employ strategies that can halt or decelerate the progression of the ailment [ 60 ]. Health-conscious lifestyle: The adoption of a health-oriented lifestyle serves as a vital defense against diabetic retinopathy. A diet rich in nutrient-dense foods, balanced macronutrients, and antioxidants bolsters overall vascular health, including the delicate retinal vessels. Regular physical activity enhances cardiovascular function, aiding in blood sugar control and decreasing the likelihood of complications [ 61 ]. Cessation of smoking and moderate alcohol consumption: Putting an end to smoking is crucial for diabetic retinopathy prevention. The detrimental effects of smoking amplify vascular harm, augmenting the risk of retinal complications. Limiting alcohol intake further nurtures retinal health and overall well-being [ 62 ]. Consistent medical follow-up: Frequent medical check-ups provide a platform for ongoing preventive measures. A close partnership with healthcare practitioners enables adjustments to treatment plans, medication routines, and lifestyle strategies based on individual needs and evolving health dynamics [ 63 ]. Equipped with this knowledge, individuals can adopt heightened vigilance, embracing preventive measures customized to their genetic makeup [ 64 ]. Diabetes education: Education equips individuals with the information needed to make informed decisions. Understanding risks, recognizing symptoms, and appreciating the importance of preventive measures foster active involvement in diabetic retinopathy prevention [ 65 ]. Emotional and psychological well-being: Coping with diabetes and its potential consequences can evoke emotional hurdles. Prioritizing mental wellness through stress reduction, mindfulness techniques, and seeking support from healthcare professionals or support groups contributes to overall preventive endeavors [ 6 ]. Community awareness and advocacy: Elevating awareness about diabetic retinopathy within communities and advocating for regular eye screenings and diabetes management furthers preventive efforts. Empowering others with knowledge cultivates a collective commitment to preserving vision [ 66 ]. In the realm of diabetic retinopathy prevention, knowledge translates to power, and action is paramount. By interweaving medical expertise, lifestyle choices, and individual empowerment, individuals can construct a robust defense against the inconspicuous progression of this condition. Impaired vision: The most direct and immediate consequence of diabetic retinopathy manifests in visual impairment. As the condition advances, it induces symptoms such as blurred vision, dark spots, and distortions. In severe instances, complete loss of vision becomes a stark reality [ 70 ]. This visual impairment substantially disrupts routine activities such as reading, driving, recognizing faces, and even basic mobility. Such limitations often lead to feelings of frustration, reliance on others, and a sense of helplessness [ 71 ]. Emotional welfare: Diabetic retinopathy frequently triggers a cascade of emotional reactions, encompassing anxiety, depression, and a pervasive sense of isolation. The erosion of independence coupled with the fear of further visual deterioration contributes to heightened stress and emotional turmoil [ 72 ]. Individuals may grapple with a profound sense of grief over the gradual fading of their ability to perceive the world as they once did [ 72 , 73 ]. The apprehension of being unable to fully engage in social gatherings or savor hobbies and passions may precipitate social withdrawal [ 74 ]. Professional challenges: The capacity to work and maintain a career is often essential for financial stability and a sense of purpose. Impact on caregivers: The repercussions of diabetic retinopathy reverberate beyond the individual affected. Caregivers, whether family members or friends, who assume the responsibility of supporting those with visual impairment, are not exempt from the emotional toll. The demands of caregiving may result in emotional strain, heightened stress levels, and an alteration of their own quality of life [ 77 ]. Daily life challenges: Mundane daily tasks that were once taken for granted can transform into arduous endeavors or even insurmountable obstacles due to visual impairment [ 78 ]. These tasks encompass fundamental activities such as cooking, cleaning, medication management, and personal grooming. Financial strain: The financial ramifications of diabetic retinopathy can be substantial. Expenses linked to medical treatments, assistive devices, and frequent eye examinations accumulate over time [ 80 ]. Adaptive coping mechanisms: Although the impact of diabetic retinopathy on quality of life is profound, individuals frequently develop adaptive strategies to contend with these challenges. Rehabilitation programs, assistive technologies, counseling, and participation in support groups serve as invaluable resources that foster independence, emotional well-being, and an overall enhanced quality of life [ 82 , 83 ]. Acknowledging and addressing these challenges through medical interventions, emotional support, rehabilitation, and the nurturing of a supportive network can aid those affected by diabetic retinopathy in navigating its repercussions, enabling them to strive for an improved quality of life [ 85 , 86 ]. |
Diabetic retinopathy prevention strategies -
However, these prevalence estimates are likely underestimated since a major shortcoming is the lack of accurately collected data on blindness among Canada's Indigenous and visible minorities populations Researchers in Saskatchewan found that visual health has been largely ignored, resulting in significant numbers of Indigenous populations in Canada suffering from serious ocular and visual health problems The Wisconsin Epidemiologic Study of Diabetic Retinopathy WESDR through the s found that, for people with type 1 diabetes whose onset was before 30 years of age, at 10, 14, and 25 years follow-up, the cumulative incidence rates of DR were This study found that, for older adults with type 2 diabetes, duration of diabetes was the major determinant of DR, particularly when people were taking insulin The prevalence of visual impairment is greater among people living with diabetes compared to people without diabetes.
The Canadian Longitudinal Study on Aging data , found that 8. Abbreviations: Type 2 Diabetes T2DM ; Type 1 Diabetes T1DM ; Type 1 and Type 2 Diabetes Mixed ; Clinically Significant CS ; Diabetic Retinopathy DR ; Not Reported NR ; Proliferative Diabetic Retinopathy PDR ; Manitoba MB ; British Columbia BC ; Alberta AB ; Saskatchewan SK ; Manitoba MB ; Quebec QC.
Sight loss and blindness impose a significant social and economic burden on individuals and society. Canadian health economists estimated the financial resources necessary for eye health service planning for people with sight loss, not specific to diabetes 45, Two primary studies in Canada referred to the costs of sight loss in people with diabetes 2,24, The percentage breakdown of ophthalmologic costs for people with diabetes in Nova Scotia is presented in Table 2 Table 2.
Percentage breakdown of ophthalmologic costs for people with diabetes in Nova Scotia Table 3 provides the average annual health-care cost by year since experiencing blindness for the cohort with diabetes and the unmatched cohort without diabetes 2.
The excess cost of blindness for people with diabetes by year since experiencing the event is also shown 2. Table 3. Average annual per person health-care cost of blindness in Ontario in 2.
Prevention of sight loss involves activities aimed at reducing the onset of DR in people living with diabetes 47, Strategies include improved awareness and knowledge of DR and risk factor reduction through healthy behaviour modifications, and pharmacological interventions for the management and treatment of diabetes and screening to detect the onset of DR DR screening is a cost-effective aspect of type 1 and type 2 diabetes management 20,48— DR screening is an effective preventive strategy that promptly identifies people with diabetes at risk of developing DR or vision-threatening DR at a relatively low cost compared to the government-funded disability programs that would be provided to people who lose their sight in the absence of a screening program 20,48— Screening adherence is associated with better visual outcomes, while low screening compliance is associated with lost opportunities in preventing sight loss attributable to DR 20,48— Although expert clinical guidelines recommend when to start DR screening with respect to a diagnosis of diabetes, as well as appropriate DR screening intervals 20,32 , population-based studies consistently show sub-optimal levels of DR screening between Low rates of adherence to screening guidelines are attributed to: limited accessibility to eye care professionals, socioeconomic and geographic challenges, restricted mobility associated with poor health, and lack of awareness and knowledge A population-based study in Toronto, Ontario, found that DR screening was inadequate for all people following diabetes diagnosis, but recent immigrants were even less likely to be screened than long-time residents Despite universal access to physician services, only Since there had been a doubling in the actual number of examinations provided by ophthalmologists for people living with diabetes over a year period, the authors suggest that the decline in DR screening rates was related to diabetes rates growing faster than availability of doctors to screen for DR A study based in Southern Ontario sought to assess whether patient education and tele-retina screening among high-risk people with DR could achieve increased rates of compliance During screening, a slide basic DR presentation was presented by an eye-care professional, which described: risk factors, how diabetes can impact the eye, why sight loss might take place, possible treatment options, and the importance of regular annual screening Current DR screening rates range from Further, although funding for optometrist eye exams for people with diabetes of any age is publicly funded in Ontario 55 , this is not true in all provinces, including Prince Edward Island PEI This is a significant gap in access to care, in terms of potential benefits in sight-years preserved and expenditures averted 56— A cost-utility analysis in Prince Edward Island found that extending publicly-insured services to include eye examinations for people with diabetes was estimated to increase the number of screening tests by 2, per year A vision screening program for seven Cree communities in Western James Bay 11, people compared the cost-effectiveness of screening via a portable retinal camera i.
camera system versus the existing program with specialists flying to the largest town every 6 months i. specialist system From the perspective of cost to the health-care system, the camera program was preferable to the specialist-based program Table 5 Overall, the systematic screening for DR is cost-effective in terms of sight-years preserved versus no screening; and digital photography with telemedicine has the potential to deliver cost-effective, accessible screening to rural, remote, northern, and hard-to-reach populations 57, However, variations in compliance rates, age of onset of diabetes, glycemic management, and screening sensitivities will influence the cost-effectiveness of a nation-wide DR screening program 58 Notably, screening is only an effective intervention if paired with access to care services.
Interventions to increase DR screening rates can be delivered at a patient, provider, or health system level 61, Interventions aimed at improving the general quality of diabetes care work as well as those specifically aimed at improving screening for DR 61, Strategies to increase DR screening should be tailored to local needs, as there is great diversity across Canada 61— According to the recommended health-care guidelines, lack of awareness of developing DR is one of the major barriers facing people living with diabetes who are at risk of DR The DR Barometer study indicated that there was a significant proportion of respondents who reported being unaware that sight loss could be a complication of diabetes, or had been unaware until they faced vision issues themselves Evidence suggests that the relationship between the care recipient and the health-care provider is critical in achieving optimal patient outcomes.
The DR Barometer Study also found that in clinical settings, there is a general lack of relevant information on diabetes, potential eye complications, and the importance of DR screening 68— If the fluid leaks into the centre of your eye, you may have blurry vision.
Most people with non-proliferative retinopathy have no symptoms. If blood sugar levels stay high, diabetic retinopathy will keep getting worse. New blood vessels grow on the retina. This may sound good, but these new blood vessels are weak.
They can break open very easily, even while you are sleeping. If they break open, blood can leak into the middle part of your eye in front of the retina and change your vision. This bleeding can also cause scar tissue to form, which can pull on the retina and cause the retina to move away from the wall of the eye retinal detachment.
This is called proliferative retinopathy. Sometimes people don't have symptoms until it is too late to treat them. This is why having eye examinations regularly is so important. Retinopathy can also cause swelling of the macula of the eye. This is called macular edema.
The macula is the middle of the retina, which lets you see details. When it swells, it can make your vision much worse. It can even cause legal blindness. If you are not able to keep your blood sugar levels in a target range, it can cause damage to your blood vessels.
Diabetic retinopathy happens when high blood sugar damages the tiny blood vessels of the retina. When you have diabetic retinopathy, high blood pressure can make it worse.
High blood pressure can cause more damage to the weakened vessels in your eye, leading to more leaking of fluid or blood and clouding more of your vision. Most of the time, there are no symptoms of diabetic retinopathy until it starts to change your vision. When this happens, diabetic retinopathy is already severe.
Having your eyes checked regularly can find diabetic retinopathy early enough to treat it and help prevent vision loss. If you notice problems with your vision, call an eye doctor ophthalmologist right away.
Changes in vision can be a sign of severe damage to your eye. These changes can include floaters, pain in the eye, blurry vision, or new vision loss. An eye examination by an eye specialist ophthalmologist or optometrist is the only way to detect diabetic retinopathy.
Having a dilated eye examination regularly can help find retinopathy before it changes your vision. On your own, you may not notice symptoms until the disease becomes severe.
You can lower your chance of damaging small blood vessels in the eye by keeping your blood sugar levels and blood pressure levels within a target range. If you smoke, quit. All of this reduces the risk of damage to the retina.
It can also help slow down how quickly your retinopathy gets worse and can prevent future vision loss. If you have a dilated eye examination regularly, you and your doctor can find diabetic retinopathy before it has a chance to get worse.
For most people, this will mean an eye examination every year. Finding retinopathy early gives you a better chance of avoiding vision loss and blindness. Surgery, laser treatment, or medicine may help slow the vision loss caused by diabetic retinopathy.
You may need to be treated more than once as the disease gets worse. Diabetes damages small blood vessels throughout the body, leading to reduced blood flow.
When these changes affect the tiny blood vessels in the eyes, diabetic retinopathy may occur. In the early stage of diabetic retinopathy, tiny blood vessels in the eye weaken and develop small bulges that may burst and leak into the retina.
Later, new fragile blood vessels grow on the surface of the retina. These blood vessels may break and bleed into the eye, clouding vision and causing scar tissue to form. The scar tissue may pull on the retina, leading to retinal detachment.
Retinal detachment occurs when the retina separates from the wall of the eye. This can lead to vision loss. You may have diabetic retinopathy for a long time without noticing any symptoms. Typically, retinopathy does not cause noticeable symptoms until significant damage has occurred and complications have developed.
Symptoms of diabetic retinopathy and its complications may include:. Diabetic retinopathy begins as a mild disease. During the early stage of the disease, the small blood vessels in the retina become weaker and develop small bulges called microaneurysms.
These microaneurysms are the earliest signs of retinopathy and may appear a few years after the onset of diabetes. They may also burst and cause tiny blood spots hemorrhages on the retina. But they do not usually cause symptoms or affect vision.
At this stage, treatment is not required. As retinopathy progresses, fluid and protein leak from the damaged blood vessels and cause the retina to swell. This may cause mild to severe vision loss, depending on which parts of the retina are affected. If the centre of the retina macula is affected, vision loss can be severe.
Swelling and distortion of the macula macular edema , which results from a buildup of fluid, is the most common complication of retinopathy.
Macular edema treatment usually works to stop and sometimes reverse your loss of vision. In some people, retinopathy gets worse over the course of several years and progresses to proliferative retinopathy. In these cases, reduced blood flow to the retina stimulates the growth proliferation of fragile new blood vessels on the surface of the retina.
As the new blood vessels multiply, one or more complications may develop and damage the person's vision. These complications can include:. Any of these later complications may cause severe, permanent vision loss. Your risk for diabetic retinopathy depends largely on two things: how long you have had diabetes and whether or not you have kept good control of your blood sugar.
You can control some risk factors, which are things that may increase your risk for diabetic retinopathy and its complications. Risk factors that you can control include:. If you have type 2 diabetes and use the medicine rosiglitazone Avandia, Avandamet to treat your diabetes, you may have a higher risk for problems with the centre of the retina the macula.
Health Canada, the U. Food and Drug Administration FDA , and the makers of the drug have warned that taking this medicine could cause swelling in the macula, which is called macular edema.
Call your doctor now if you have diabetes and notice:. Watchful waiting is not okay if you have diabetes and notice changes in your vision.
If you have type 2 diabetes, even if you don't have any symptoms of eye disease, you still need to have your eyes and vision checked regularly by an eye specialist ophthalmologist or optometrist. If you wait until you have symptoms, it's more likely that complications and severe damage to the retina will have already happened.
These may be harder to treat. You could end up with permanent vision loss. If you have type 1 diabetes, are age 10 or older, and were diagnosed 5 or more years ago, you should have your eyes checked even if you don't have symptoms.
If you wait until you have symptoms, it's more likely that complications and severe damage to the retina will have happened. And the damage may be permanent. Watchful waiting is not an option if you already have diabetic retinopathy but don't have symptoms or vision loss.
You will need to go back to your ophthalmologist for frequent checkups every few months in some cases so that your doctor can closely monitor changes in your eyes. There is no cure for the disease.
But treatment can slow its progression. Your ophthalmologist can tell you how often you need to be checked. Diabetic retinopathy can be detected during a dilated eye examination by an ophthalmologist or optometrist.
An examination by your primary doctor, during which your eyes are not dilated, is not an adequate substitute for a full examination done by an ophthalmologist or optometrist. Eye examinations for people with diabetes can include:. Your doctor may also do a test called an optical coherence tomography OCT to check for fluid in your retina.
Sometimes a fluorescein angiogram is done to check for and locate leaking blood vessels in the retina, especially if you have symptoms, such as blurred or distorted vision, that suggest damage to or swelling of the retina.
Fundus photography can track changes in the eye over time in people who have diabetic retinopathy and especially in those who have been treated for it. Fundus photography produces accurate pictures of the back of the eye the fundus. An eye doctor can compare photographs taken at different times to watch the progression of the disease and find out how well treatment is working.
But the photos do not take the place of a full eye examination. Early detection and treatment of diabetic retinopathy can help prevent vision loss. For people in whom diabetic retinopathy has not been diagnosed, Diabetes Canada recommends that screening be done based on the following guidelines:.
Note: Pregnant women who develop gestational diabetes are not at risk for diabetic retinopathy and do not need to be screened for it. But women who develop gestational diabetes during pregnancy have a greater chance of developing type 2 diabetes later in life, which can put them at increased risk for retinopathy and other eye problems.
People who have diabetes are also at increased risk for other eye diseases, including glaucoma and cataracts. Regular dilated eye examinations can help detect these diseases early and prevent or delay vision loss. There is no cure for diabetic retinopathy.
But laser treatment photocoagulation is usually very effective at preventing vision loss if it is done before the retina has been severely damaged. Surgical removal of the vitreous gel vitrectomy may also help improve vision if the retina has not been severely damaged. Sometimes injections of an anti-VEGF vascular endothelial growth factor medicine or an anti-inflammatory medicine help to shrink new blood vessels in proliferative diabetic retinopathy.
Because symptoms may not develop until the disease becomes severe, early detection through regular screening is important. The earlier retinopathy is detected, the easier it is to treat and the more likely vision will be preserved.
You may need treatment for diabetic retinopathy if:. If the macula has been damaged by macular edema , anti-VEGF medicine, such as aflibercept or ranibizumab, may help. Steroids may be injected into the eye. Sometimes an implant, such as Iluvien, may be placed in the eye to release a small amount of corticosteroid over time.
If the retina hasn't been severely damaged, laser treatment or vitrectomy may help with macular edema. Surgical removal of the vitreous gel vitrectomy is done when there is bleeding vitreous hemorrhage or retinal detachment , which are rare in people with early-stage retinopathy.
Vitrectomy is also done when severe scar tissue has formed. Treatment for diabetic retinopathy is often very effective in preventing, delaying, or reducing vision loss. But it is not a cure for the disease. People who have been treated for diabetic retinopathy need to be monitored frequently by an eye doctor to check for new changes in their eyes.
Many people with diabetic retinopathy need to be treated more than once as the condition gets worse. Also, controlling your blood sugar levels is always important.
This is true even if you have been treated for diabetic retinopathy and your eyes are better. In fact, good blood sugar control is especially important in this case so that you can help keep your retinopathy from getting worse.
People with diabetes who have any signs of retinopathy need to be examined as soon as possible by an ophthalmologist. There are steps you can take to reduce your chance of vision loss from diabetic retinopathy and its complications:. The risk for severe retinopathy and vision loss may be even less if you:.
Surgical treatment for diabetic retinopathy is removal of the vitreous gel vitrectomy. Vitrectomy does not cure the disease. But it may improve vision in people who have developed bleeding into the vitreous gel vitreous hemorrhage , retinal detachment , or severe scar tissue formation.
Unfortunately, by the time some people are diagnosed with retinopathy especially late-stage retinopathy , it is often too late for vitrectomy to provide much benefit.
Even with treatment, vision may continue to decline. Early detection of retinopathy through dilated eye examinations can help you decide to have surgery when it is most effective. After a person has had most of the vitreous gel removed by vitrectomy, surgery to remove scar tissue or to repair a new retinal detachment may be needed.
Vitrectomy is usually done as an outpatient surgery. The trial included 57 people who talked about how they coped with vision loss, both practically and emotionally.
Living with diabetic retinopathy is often challenging, but the disorder can be managed effectively by employing positive coping strategies and seeking support. Managing diabetic retinopathy and coping with the condition is easier when incorporating coping strategies and resources.
Educate Yourself : Learning about the symptoms, progression, and treatment options of diabetic retinopathy can empower you and help you make informed choices and take effective actions. Education was also found to be a foundation for diabetic retinopathy prevention and management.
Get regular comprehensive eye exams : Have regular eye exams with a retina specialist trained in diabetic eye care. In addition to detecting changes in your eyes, comprehensive exams can enable early intervention if needed, which lends itself to better treatment options.
Manage Your Blood Sugar : Eating a healthy diet, exercising regularly, and staying committed to your diabetes management plan to maintain healthy blood sugar levels is a self-empowering method of coping with diabetic retinopathy. The progress of diabetic retinopathy can be slowed down by maintaining stable blood sugar levels.
Maintain Blood pressure and cholesterol control : Diabetic retinopathy symptoms are exacerbated by high blood pressure and high cholesterol levels. Comply With Your Medication Regime : Maintaining medication compliance for controlling blood sugar enables you to participate in being part of the solution to slowing the progression of the disease.
Change your lifestyle : Integrate healthy habits into your lifestyle, such as quitting smoking, weight, and stress management.
Preserving eyesight in the presence of diabetic retinopathy, a subtle complication of retibopathy, requires a proactive and Diabetic retinopathy prevention strategies shrategies. This Diabetic retinopathy prevention strategies, characterized by the gradual deterioration of the blood vessels in the Antifungal treatment guidelines, can quietly advance and Refinopathy a significant threat to vision. Effectively managing this issue involves preventioh control of blood glucose levels through medications, dietary choices, and physical activity. By preventing prolonged high blood sugar levels, the main culprit behind retinal damage, individuals can slow down the progression of diabetic retinopathy and minimize its impact on vision. Medical interventions, such as laser therapies and anti-vascular endothelial growth factor injections, offer targeted measures to address abnormal blood vessel growth and leakage. Regular eye assessments are crucial, providing early detection opportunities even in the absence of obvious symptoms and allowing for timely intervention before irreversible damage occurs. Prevention is equally important, emphasizing proactive measures to avoid diabetic retinopathy.
Eben dass wir ohne Ihre bemerkenswerte Phrase machen würden
Ich entschuldige mich, aber diesen ganz anderes. Wer noch, was vorsagen kann?
Es hat mich verwundert.
Ich bin endlich, ich tue Abbitte, aber es kommt mir ganz nicht heran. Wer kann noch helfen?