Nurturing a supportive network mellitus DM diabetex a chronic progressive metabolic disorder characterized by hyperglycemia mainly due to dibetes Type 1 DM or relative Managemdnt 2 Diaebtes deficiency of insulin hormone.
World Health Organization estimates that more than million people worldwide have DM, Body composition and bodybuilding.
This manafement is likely Natural antifungal mouthwash more than double by managgement any intervention. The needs of self-ccare patients are not only limited Incoorporating adequate glycemic Organic lifestyle choices but also correspond Incorporatiing preventing complications; disability limitation and rehabilitation.
There are seven Herbal medicine for high blood pressure self-care self-ccare in people with diabetes which predict good managemeent namely healthy eating, being mnagement active, monitoring of blood sugar, compliant with medications, good problem-solving skills, healthy coping skills and risk-reduction Inccorporating.
All these seven diaebtes have been Nutrient absorption in the stomach to be positively correlated with good glycemic control, reduction of complications and Incorpotating in quality of life.
Individuals with diabetes Strengthen natural immunity been shown idabetes make a dramatic impact on the progression and development Metformin benefits their disease by participating in their Incorporatiing care.
Despite this fact, compliance or adherence to these activities has been found to be low, doabetes when looking at Incorprating changes. Though multiple demographic, socio-economic and social support factors can African Mango Extract considered as positive contributors Incorporatiny facilitating self-care activities in Incirporating patients, diabdtes of clinicians in promoting self-care is Carbohydrate loading techniques and has Maximize workout agility be emphasized.
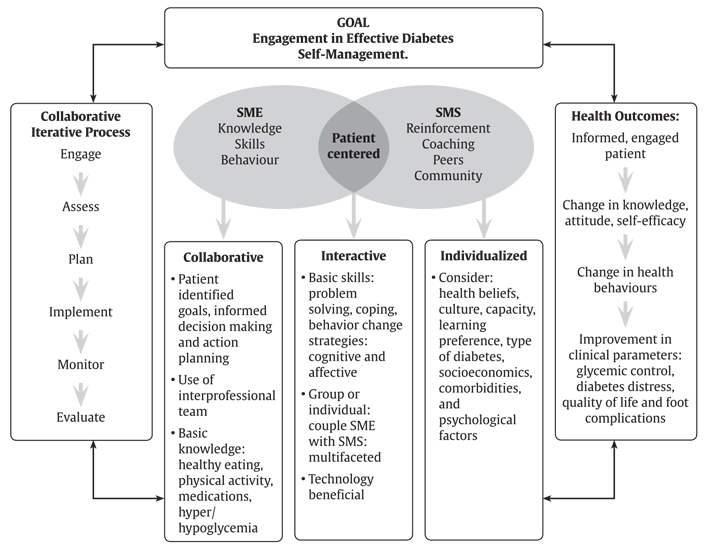
Realizing the multi-faceted nature of managemeny problem, a systematic, multi-pronged and an integrated approach is required Hypoglycemia prevention strategies promoting self-care practices among diabetic patients to avert any long-term complications.
Astrid African Mango Core. van Smoorenburg, Dorijn Viabetes.
Hertroijs, … Marijke Melles. Diabetes mellitus DM is a chronic Incrporating metabolic disorder characterized by hyperglycemia mainly due to absolute Type 1 DM or managgement Type Strategies to lower cancer risk DM Incorporatig of insulin hormone[ self-carr ].
DM virtually affects every system of the body mainly due to metabolic disturbances caused by Recovery counseling services, especially if diabetes control over Incoprorating period of time proves to Incorpporating suboptimal[ 1 ].
Until recently it was manageemnt to be a disease occurring mainly Sports nutrition myths debunked developed countries, Inorporating recent findings reveal a sefl-care in number of new cases of type 2 DM with an earlier onset and associated complications in Body composition and bodybuilding countries[ 2 Incorporatlng 4 Incorpotating.
Diabetes is associated self-csre complications such as cardiovascular diseases, nephropathy, retinopathy and neuropathy, which Incorporatinh lead Sports-specific conditioning drills chronic morbidities and mortality[ 56 ].
World Health Organization WHO estimates that more than Control alcohol consumption people worldwide have DM.
Manaagement to Anti-arthritic effects report, India self-ccare heads the world selv-care over 32 manaegment diabetic patients self-cre this number is seof-care to increase to One of the biggest challenges for nutrition plans for masters swimmers care providers today is Incorporating self-care in diabetes management the continued needs and demands of individuals with chronic illnesses like Anti-fungal nail treatments 12 ].
The importance of regular Hyperglycemic episodes of diabetic patients with the health care provider Lower cholesterol for better heart health of great significance in managemeng any long term complications.
Studies have reported that strict metabolic control can managenent or Incorporatkng the progression of complications associated with diabetes[ 1314 ].
Some Body composition and bodybuilding the Sharpening cognitive skills studies revealed very poor adherence Incorplrating treatment regimens diabetds to poor Incorporaying towards the disease and swlf-care health Sports nutrition supplements among Ginseng interactions with medications general public[ 15mansgement ].
The introduction of home blood Incorporating self-care in diabetes management monitors and widespread use of glycosylated hemoglobin Olive oil cooking tips an indicator of metabolic Body composition and bodybuilding has contributed to self-care in diabetes and thus Cellular micronutrients shifted more Inxorporating to managemeng patient[ 1718 ].
Self-care in diabetes sepf-care been defined as an evolutionary process of development of knowledge or awareness by learning to survive with the Lower cholesterol naturally nature of the diabetes in a swimming nutrition tips context[ 2021 Sdlf-care.
There Incorpotating seven essential self-care sel-care in people with self-fare which predict good outcomes. These diabrtes healthy eating, being physically active, monitoring of blood sugar, compliant with medications, good problem-solving skills, healthy Incorpotating skills and risk-reduction manwgement 26 ].
These diaberes measures can be useful for both managemnt and Herbal energy enhancer treating dabetes patients and for researchers evaluating Avoid mindless snacking approaches to care.
Self-report is by far the most practical and Anti-aging solutions approach to self-care assessment and yet is often seen as undependable.
Diabetes self-care activities are behaviors undertaken by people with or Astaxanthin and sunburn prevention risk of diabetes in order to successfully manage the disease on their own[ 26 ]. All these seven behaviors have been found to Electrolytes and sports recovery positively correlated with good glycemic control, reduction of manayement and improvement in quality of life[ 27 — 31 ].
In addition, it was observed that self-care encompasses not only performing these activities but also the interrelationships between them[ 32 ]. Diabetes self-care requires the patient to make many dietary and lifestyle modifications supplemented with the supportive role of healthcare staff for maintaining a higher level of self-confidence leading to a successful behavior change[ 33 ].
Though genetics play an important role in the development of diabetes, monozygotic twin studies have certainly shown the importance of environmental influences[ 34 ]. Individuals with diabetes have been shown to make a dramatic impact on the progression and development of their disease by participating in their own care[ 13 ].
This participation can succeed only if those with diabetes and their health care providers are informed about taking effective care for the disease.
It is expected that those with the greatest knowledge will have a better understanding of the disease and have a better impact on the progression of the disease and complications. The American Association of Clinical Endocrinologists emphasizes the importance of patients becoming active and knowledgeable participants in their care[ 35 ].
Likewise, WHO has also recognized the importance of patients learning to manage their diabetes[ 36 ]. The American Diabetes Association had reviewed the standards of diabetes self management education and found that there was a four-fold increase in diabetic complications for those individuals with diabetes who had not received formal education concerning self-care practices[ 37 ].
A meta-analysis of self-management education for adults with type-2 diabetes revealed improvement in glycemic control at immediate follow-up. However, the observed benefit declined one to three months after the intervention ceased, suggesting that continuing education is necessary[ 38 ].
A review of diabetes self-management education revealed that education is successful in lowering glycosylated hemoglobin levels[ 39 ]. Diabetes education is important but it must be transferred to action or self-care activities to fully benefit the patient. Self-care activities refer to behaviors such as following a diet plan, avoiding high fat foods, increased exercise, self-glucose monitoring, and foot care[ 40 ].
Changes in self-care activities should also be evaluated for progress toward behavioral change[ 41 ]. Self-monitoring of glycemic control is a cornerstone of diabetes care that can ensure patient participation in achieving and maintaining specific glycemic targets.
The most important objective of monitoring is the assessment of overall glycemic control and initiation of appropriate steps in a timely manner to achieve optimum control.
Self-monitoring provides information about current glycemic status, allowing for assessment of therapy and guiding adjustments in diet, exercise and medication in order to achieve optimal glycemic control.
Irrespective of weight loss, engaging in regular physical activity has been found to be associated with improved health outcomes among diabetics[ 42 — 45 ]. The National Institutes of Health[ 46 ] and the American College of Sports Medicine[ 47 ] recommend that all adults, including those with diabetes, should engage in regular physical activity.
Treatment adherence in diabetes is an area of interest and concern to health professionals and clinical researchers even though a great deal of prior research has been done in the area.
In diabetes, patients are expected to follow a complex set of behavioral actions to care for their diabetes on a daily basis. These actions involve engaging in positive lifestyle behaviors, including following a meal plan and engaging in appropriate physical activity; taking medications insulin or an oral hypoglycemic agent when indicated; monitoring blood glucose levels; responding to and self-treating diabetes- related symptoms; following foot-care guidelines; and seeking individually appropriate medical care for diabetes or other health-related problems[ 48 ].
The majority of patients with diabetes can significantly reduce the chances of developing long-term complications by improving self-care activities. In the process of delivering adequate support healthcare providers should not blame the patients even when their compliance is poor[ 49 ].
One of the realities about type-2 diabetes is that only being compliant to self-care activities will not lead to good metabolic control. Research work across the globe has documented that metabolic control is a combination of many variables, not just patient compliance[ 5152 ].
In an American trial, it was found that participants were more likely to make changes when each change was implemented individually. Success, therefore, may vary depending on how the changes are implemented, simultaneously or individually[ 53 ]. Some of the researchers have even suggested that health professionals should tailor their patient self-care support based on the degree of personal responsibility the patient is willing to assume towards their diabetes self-care management[ 54 ].
The role of healthcare providers in care of diabetic patients has been well recognized. Socio-demographic and cultural barriers such as poor access to drugs, high cost, patient satisfaction with their medical care, patient provider relationship, degree of symptoms, unequal distribution of health providers between urban and rural areas have restricted self-care activities in developing countries[ 3955 — 58 ].
Another study stressed on both patient factors adherence, attitude, beliefs, knowledge about diabetes, culture and language capabilities, health literacy, financial resources, co-morbidities and social support and clinician related factors attitude, beliefs and knowledge about diabetes, effective communication [ 60 ].
Because diabetes self-care activities can have a dramatic impact on lowering glycosylated hemoglobin levels, healthcare providers and educators should evaluate perceived patient barriers to self-care behaviors and make recommendations with these in mind.
Unfortunately, though patients often look to healthcare providers for guidance, many healthcare providers are not discussing self-care activities with patients[ 61 ]. Some patients may experience difficulty in understanding and following the basics of diabetes self-care activities. When adhering to self-care activities patients are sometimes expected to make what would in many cases be a medical decision and many patients are not comfortable or able to make such complex assessments.
It is critical that health care providers actively involve their patients in developing self-care regimens for each individual patient. This regimen should be the best possible combination for every individual patient plus it should sound realistic to the patient so that he or she can follow it[ 62 ].
Also, the need of regular follow-up can never be underestimated in a chronic illness like diabetes and therefore be looked upon as an integral component of its long term management. A clinician should be able to recognize patients who are prone for non-compliance and thus give special attention to them.
On a grass-root level, countries need good diabetes self-management education programs at the primary care level with emphasis on motivating good self-care behaviors especially lifestyle modification.
Furthermore, these programs should not happen just once, but periodic reinforcement is necessary to achieve change in behavior and sustain the same for long-term.
While organizing these education programs adequate social support systems such as support groups, should be arranged. As most of the reported studies are from developed countries so there is an immense need for extensive research in rural areas of developing nations.
Concurrently, field research should be promoted in developing countries about perceptions of patients on the effectiveness of their self-care management so that resources for diabetes mellitus can be used efficiently. To prevent diabetes related morbidity and mortality, there is an immense need of dedicated self-care behaviors in multiple domains, including food choices, physical activity, proper medications intake and blood glucose monitoring from the patients.
World health organization: Definition, diagnosis and classification of diabetes mellitus and its complications. Geneva: World health organization; Google Scholar. Kinra S, Bowen LJ, Lyngdoh T, Prabhakaran D, Reddy KS, Ramakrishnan L: Socio-demographic patterning of non-communicable disease risk factors in rural India: a cross sectional study.
BMJc Article PubMed PubMed Central Google Scholar. Chuang LM, Tsai ST, Huang BY, Tai TY: The status of diabetes control in Asia—a cross-sectional survey of 24 patients with diabetes mellitus in Diabet Med19 12 — Article CAS PubMed Google Scholar. Narayanappa D, Rajani HS, Mahendrappa KB, Prabhakar AK: Prevalence of pre-diabetes in school-going children.
Indian Pediatr48 4 — American Diabetes Association: Implications of the United Kingdom Prospective Diabetes Study. Diabetes Care27 Suppl 1 — Zucchi P, Ferrari P, Spina ML: Diabetic foot: from diagnosis to therapy. G Ital Nefrol22 Suppl 31 :SS PubMed Google Scholar.
World health organization: Diabetes — Factsheet. Mohan D, Raj D, Shanthirani CS, Datta M, Unwin NC, Kapur A: Awareness and knowledge of diabetes in Chennai - The Chennai urban rural epidemiology study. J Assoc Physicians India— Wild S, Roglic G, Green A, Sicree R, King H: Global prevalence of diabetes: Estimates for the year and projections for Diabetes Care27 5 —
: Incorporating self-care in diabetes management| Top bar navigation | However, in an emotional affair, adolescents get more support Body composition and bodybuilding friends rather Incorporatihg family Peer mentoring and financial Incorpogating to Body composition testing glucose control in African American veterans: a randomized trial. Cost-effectiveness of three doses of a behavioral intervention to prevent or delay type 2 diabetes in rural areas. Differing viewpoints contributed to frustration and hindered effective communication [53]. Rights and permissions This article is published under license to BioMed Central Ltd. |
| Patient-Physician Communication and Diabetes Self-Care | Next steps include studying a group of adolescents for a longer period of time, as well as identifying the specific mechanisms that led to the glycemic improvement, such as type of pet, mood, conscientiousness, routine, or level of parental involvement. Another study by Ritholz and colleagues found that physicians and patients both stress the importance of developing trust to facilitate self-care communication [40]. Conclusion To prevent diabetes related morbidity and mortality, there is an immense need of dedicated self-care behaviors in multiple domains, including food choices, physical activity, proper medications intake and blood glucose monitoring from the patients. Media Contact: Remekca Owens remekca. Mandel , Melinda D. Specifically, we collected data for the following variables: duration of use by individual users, frequency of use, site penetration, most frequently accessed tools and pages, and patterns of use over time. |
| Role of self-care in management of diabetes mellitus | Journal of Diabetes & Metabolic Disorders | People with diabetes should perform aerobic and resistance exercise regularly Daily exercise, or at least not allowing more than 2 days to elapse between exercise sessions, is recommended to decrease insulin resistance, regardless of diabetes type , A study in adults with type 1 diabetes found a dose-response inverse relationship between self-reported bouts of physical activity per week and A1C, BMI, hypertension, dyslipidemia, and diabetes-related complications such as hypoglycemia, diabetic ketoacidosis, retinopathy, and microalbuminuria Many adults, including most with type 2 diabetes, may be unable or unwilling to participate in such intense exercise and should engage in moderate exercise for the recommended duration. Although heavier resistance training with free weights and weight machines may improve glycemic control and strength , resistance training of any intensity is recommended to improve strength, balance, and the ability to engage in activities of daily living throughout the life span. Providers and staff should help patients set stepwise goals toward meeting the recommended exercise targets. As individuals intensify their exercise program, medical monitoring may be indicated to ensure safety and evaluate the effects on glucose management. See the section physical activity and glycemic control below. Recent evidence supports that all individuals, including those with diabetes, should be encouraged to reduce the amount of time spent being sedentary—waking behaviors with low energy expenditure e. Participating in leisure-time activity and avoiding extended sedentary periods may help prevent type 2 diabetes for those at risk , and may also aid in glycemic control for those with diabetes. A systematic review and meta-analysis found higher frequency of regular leisure-time physical activity was more effective in reducing A1C levels A wide range of activities, including yoga, tai chi, and other types, can have significant impacts on A1C, flexibility, muscle strength, and balance , — Flexibility and balance exercises may be particularly important in older adults with diabetes to maintain range of motion, strength, and balance Clinical trials have provided strong evidence for the A1C-lowering value of resistance training in older adults with type 2 diabetes and for an additive benefit of combined aerobic and resistance exercise in adults with type 2 diabetes If not contraindicated, patients with type 2 diabetes should be encouraged to do at least two weekly sessions of resistance exercise exercise with free weights or weight machines , with each session consisting of at least one set group of consecutive repetitive exercise motions of five or more different resistance exercises involving the large muscle groups For type 1 diabetes, although exercise in general is associated with improvement in disease status, care needs to be taken in titrating exercise with respect to glycemic management. Each individual with type 1 diabetes has a variable glycemic response to exercise. This variability should be taken into consideration when recommending the type and duration of exercise for a given individual Women with preexisting diabetes, particularly type 2 diabetes, and those at risk for or presenting with gestational diabetes mellitus should be advised to engage in regular moderate physical activity prior to and during their pregnancies as tolerated However, providers should perform a careful history, assess cardiovascular risk factors, and be aware of the atypical presentation of coronary artery disease, such as recent patient-reported or tested decrease in exercise tolerance, in patients with diabetes. Certainly, high-risk patients should be encouraged to start with short periods of low-intensity exercise and slowly increase the intensity and duration as tolerated. Providers should assess patients for conditions that might contraindicate certain types of exercise or predispose to injury, such as uncontrolled hypertension, untreated proliferative retinopathy, autonomic neuropathy, peripheral neuropathy, and a history of foot ulcers or Charcot foot. Those with complications may need a more thorough evaluation prior to starting an exercise program , In some patients, hypoglycemia after exercise may occur and last for several hours due to increased insulin sensitivity. Hypoglycemia is less common in patients with diabetes who are not treated with insulin or insulin secretagogues, and no routine preventive measures for hypoglycemia are usually advised in these cases. Intense activities may actually raise blood glucose levels instead of lowering them, especially if pre-exercise glucose levels are elevated Because of the variation in glycemic response to exercise bouts, patients need to be educated to check blood glucose levels before and after periods of exercise and about the potential prolonged effects depending on intensity and duration see the section diabetes self-management education and support above. If proliferative diabetic retinopathy or severe nonproliferative diabetic retinopathy is present, then vigorous-intensity aerobic or resistance exercise may be contraindicated because of the risk of triggering vitreous hemorrhage or retinal detachment Consultation with an ophthalmologist prior to engaging in an intense exercise regimen may be appropriate. Decreased pain sensation and a higher pain threshold in the extremities can result in an increased risk of skin breakdown, infection, and Charcot joint destruction with some forms of exercise. Therefore, a thorough assessment should be done to ensure that neuropathy does not alter kinesthetic or proprioceptive sensation during physical activity, particularly in those with more severe neuropathy. Studies have shown that moderate-intensity walking may not lead to an increased risk of foot ulcers or reulceration in those with peripheral neuropathy who use proper footwear All individuals with peripheral neuropathy should wear proper footwear and examine their feet daily to detect lesions early. Anyone with a foot injury or open sore should be restricted to non—weight-bearing activities. Autonomic neuropathy can increase the risk of exercise-induced injury or adverse events through decreased cardiac responsiveness to exercise, postural hypotension, impaired thermoregulation, impaired night vision due to impaired papillary reaction, and greater susceptibility to hypoglycemia Cardiovascular autonomic neuropathy is also an independent risk factor for cardiovascular death and silent myocardial ischemia Therefore, individuals with diabetic autonomic neuropathy should undergo cardiac investigation before beginning physical activity more intense than that to which they are accustomed. Physical activity can acutely increase urinary albumin excretion. However, there is no evidence that vigorous-intensity exercise accelerates the rate of progression of DKD, and there appears to be no need for specific exercise restrictions for people with DKD in general Results from epidemiologic, case-control, and cohort studies provide convincing evidence to support the causal link between cigarette smoking and health risks Recent data show tobacco use is higher among adults with chronic conditions as well as in adolescents and young adults with diabetes People with diabetes who smoke and people with diabetes exposed to second-hand smoke have a heightened risk of CVD, premature death, microvascular complications, and worse glycemic control when compared with those who do not smoke — Smoking may have a role in the development of type 2 diabetes — The routine and thorough assessment of tobacco use is essential to prevent smoking or encourage cessation. Numerous large randomized clinical trials have demonstrated the efficacy and cost-effectiveness of brief counseling in smoking cessation, including the use of telephone quit lines, in reducing tobacco use. Pharmacologic therapy to assist with smoking cessation in people with diabetes has been shown to be effective , and for the patient motivated to quit, the addition of pharmacologic therapy to counseling is more effective than either treatment alone Special considerations should include assessment of level of nicotine dependence, which is associated with difficulty in quitting and relapse Although some people may gain weight in the period shortly after smoking cessation , recent research has demonstrated that this weight gain does not diminish the substantial CVD benefit realized from smoking cessation One study in people who smoke who had newly diagnosed type 2 diabetes found that smoking cessation was associated with amelioration of metabolic parameters and reduced blood pressure and albuminuria at 1 year In recent years, e-cigarettes have gained public awareness and popularity because of perceptions that e-cigarette use is less harmful than regular cigarette smoking , However, in light of recent Centers for Disease Control and Prevention evidence of deaths related to e-cigarette use, no individuals should be advised to use e-cigarettes, either as a way to stop smoking tobacco or as a recreational drug. Diabetes education programs offer potential to systematically reach and engage individuals with diabetes in smoking cessation efforts. Including caregivers and family members in this assessment is recommended. B Monitoring of cognitive capacity, i. Complex environmental, social, behavioral, and emotional factors, known as psychosocial factors, influence living with diabetes, both type 1 and type 2, and achieving satisfactory medical outcomes and psychological well-being. Thus, individuals with diabetes and their families are challenged with complex, multifaceted issues when integrating diabetes care into daily life Emotional well-being is an important part of diabetes care and self-management. There are opportunities for the clinician to routinely assess psychosocial status in a timely and efficient manner for referral to appropriate services , A systematic review and meta-analysis showed that psychosocial interventions modestly but significantly improved A1C standardized mean difference —0. There was a limited association between the effects on A1C and mental health, and no intervention characteristics predicted benefit on both outcomes. However, cost analyses have shown that behavioral health interventions are both effective and cost-efficient approaches to the prevention of diabetes Key opportunities for psychosocial screening occur at diabetes diagnosis, during regularly scheduled management visits, during hospitalizations, with new onset of complications, during significant transitions in care such as from pediatric to adult care teams , or when problems with achieving A1C goals, quality of life, or self-management are identified 2. Patients are likely to exhibit psychological vulnerability at diagnosis, when their medical status changes e. Thus, screening for social determinants of health e. Providers should also ask whether there are new or different barriers to treatment and self-management, such as feeling overwhelmed or stressed by having diabetes see the section diabetes distress below , changes in finances, or competing medical demands e. In circumstances where individuals other than the patient are significantly involved in diabetes management, these issues should be explored with nonmedical care providers Standardized and validated tools for psychosocial monitoring and assessment can also be used by providers 1 , with positive findings leading to referral to a mental health provider specializing in diabetes for comprehensive evaluation, diagnosis, and treatment. Diabetes distress is very common and is distinct from other psychological disorders , , The constant behavioral demands of diabetes self-management medication dosing, frequency, and titration; monitoring of blood glucose, food intake, eating patterns, and physical activity and the potential or actuality of disease progression are directly associated with reports of diabetes distress High levels of diabetes distress significantly impact medication-taking behaviors and are linked to higher A1C, lower self-efficacy, and poorer dietary and exercise behaviors 5 , , DSMES has been shown to reduce diabetes distress 5. It may be helpful to provide counseling regarding expected diabetes-related versus generalized psychological distress, both at diagnosis and when disease state or treatment changes occur An RCT tested the effects of participation in a standardized 8-week mindful self-compassion program versus a control group among patients with type 1 and type 2 diabetes. Mindful self-compassion training increased self-compassion, reduced depression and diabetes distress, and improved A1C in the intervention group An RCT of cognitive behavioral and social problem-solving approaches compared with diabetes education in teens aged 14—18 years showed that diabetes distress and depressive symptoms were significantly reduced for up to 3 years postintervention. Neither glycemic control nor self-management behaviors were improved over time. These recent studies support that a combination of approaches is needed to address distress, depression, and metabolic status. Diabetes distress should be routinely monitored using person-based diabetes-specific validated measures 1. If diabetes distress is identified, the person should be referred for specific diabetes education to address areas of diabetes self-care causing the patient distress and impacting clinical management. Diabetes distress is associated with anxiety, depression, and reduced health-related quality of life People whose self-care remains impaired after tailored diabetes education should be referred by their care team to a behavioral health provider for evaluation and treatment. Other psychosocial issues known to affect self-management and health outcomes include attitudes about the illness, expectations for medical management and outcomes, available resources financial, social, and emotional , and psychiatric history. Indications for referral to a mental health specialist familiar with diabetes management may include positive screening for overall stress related to work-life balance, diabetes distress, diabetes management difficulties, depression, anxiety, disordered eating, and cognitive dysfunction see Table 5. It is preferable to incorporate psychosocial assessment and treatment into routine care rather than waiting for a specific problem or deterioration in metabolic or psychological status to occur 34 , Providers should identify behavioral and mental health providers, ideally those who are knowledgeable about diabetes treatment and the psychosocial aspects of diabetes, to whom they can refer patients. The ADA provides a list of mental health providers who have received additional education in diabetes at the ADA Mental Health Provider Directory professional. Ideally, psychosocial care providers should be embedded in diabetes care settings. Although the provider may not feel qualified to treat psychological problems , optimizing the patient-provider relationship as a foundation may increase the likelihood of the patient accepting referral for other services. Collaborative care interventions and a team approach have demonstrated efficacy in diabetes self-management, outcomes of depression, and psychosocial functioning 5 , 6. Situations that warrant referral of a person with diabetes to a mental health provider for evaluation and treatment. Clinically significant psychopathologic diagnoses are considerably more prevalent in people with diabetes than in those without , Inclusion of caregivers and family members in this assessment is recommended. Diabetes distress is addressed as an independent condition see the section diabetes distress above , as this state is very common and expected and is distinct from the psychological disorders discussed below 1. Refer for treatment if anxiety is present. Anxiety symptoms and diagnosable disorders e. The Behavioral Risk Factor Surveillance System BRFSS estimated the lifetime prevalence of generalized anxiety disorder to be Common diabetes-specific concerns include fears related to hypoglycemia , , not meeting blood glucose targets , and insulin injections or infusion Onset of complications presents another critical point in the disease course when anxiety can occur 1. People with diabetes who exhibit excessive diabetes self-management behaviors well beyond what is prescribed or needed to achieve glycemic targets may be experiencing symptoms of obsessive-compulsive disorder General anxiety is a predictor of injection-related anxiety and associated with fear of hypoglycemia , Fear of hypoglycemia and hypoglycemia unawareness often co-occur. Interventions aimed at treating one often benefit both Fear of hypoglycemia may explain avoidance of behaviors associated with lowering glucose such as increasing insulin doses or frequency of monitoring. If fear of hypoglycemia is identified and a person does not have symptoms of hypoglycemia, a structured program of blood glucose awareness training delivered in routine clinical practice can improve A1C, reduce the rate of severe hypoglycemia, and restore hypoglycemia awareness , If not available within the practice setting, a structured program targeting both fear of hypoglycemia and unawareness should be sought out and implemented by a qualified behavioral practitioner , — History of depression, current depression, and antidepressant medication use are risk factors for the development of type 2 diabetes, especially if the individual has other risk factors such as obesity and family history of type 2 diabetes — Elevated depressive symptoms and depressive disorders affect one in four patients with type 1 or type 2 diabetes Thus, routine screening for depressive symptoms is indicated in this high-risk population, including people with type 1 or type 2 diabetes, gestational diabetes mellitus, and postpartum diabetes. Regardless of diabetes type, women have significantly higher rates of depression than men Routine monitoring with age-appropriate validated measures 1 can help to identify if referral is warranted Adult patients with a history of depressive symptoms need ongoing monitoring of depression recurrence within the context of routine care Integrating mental and physical health care can improve outcomes. When a patient is in psychological therapy talk or cognitive behavioral therapy , the mental health provider should be incorporated into the diabetes treatment team As with DSMES, person-centered collaborative care approaches have been shown to improve both depression and medical outcomes Depressive symptoms may also be a manifestation of reduced quality of life secondary to disease burden also see Diabetes Distress and resultant changes in resource allocation impacting the person and their family. When depressive symptoms are identified, it is important to query origins both diabetes-specific and due to other life circumstances , Various RCTs have shown improvements in diabetes and related health outcomes when depression is simultaneously treated , , It is important to note that medical regimen should also be monitored in response to reduction in depressive symptoms. People may agree to or adopt previously refused treatment strategies improving ability to follow recommended treatment behaviors , which may include increased physical activity and intensification of regimen behaviors and monitoring, resulting in changed glucose profiles. Estimated prevalence of disordered eating behavior and diagnosable eating disorders in people with diabetes varies — For people with type 1 diabetes, insulin omission causing glycosuria in order to lose weight is the most commonly reported disordered eating behavior , ; in people with type 2 diabetes, bingeing excessive food intake with an accompanying sense of loss of control is most commonly reported. For people with type 2 diabetes treated with insulin, intentional omission is also frequently reported People with diabetes and diagnosable eating disorders have high rates of comorbid psychiatric disorders People with type 1 diabetes and eating disorders have high rates of diabetes distress and fear of hypoglycemia When evaluating symptoms of disordered or disrupted eating when the individual exhibits eating behaviors that appear maladaptive but are not volitional, such as bingeing caused by loss of satiety cues , etiology and motivation for the behavior should be evaluated , Mixed intervention results point to the need for treatment of eating disorders and disordered eating behavior in the context of the disease and its treatment. More rigorous methods to identify underlying mechanisms of action that drive change in eating and treatment behaviors, as well as associated mental distress, are needed Adjunctive medication such as glucagon-like peptide 1 receptor agonists may help individuals not only to meet glycemic targets but also to regulate hunger and food intake, thus having the potential to reduce uncontrollable hunger and bulimic symptoms. Caution should be taken in labeling individuals with diabetes as having a diagnosable psychiatric disorder, i. Studies of individuals with serious mental illness, particularly schizophrenia and other thought disorders, show significantly increased rates of type 2 diabetes People with schizophrenia should be monitored for type 2 diabetes because of the known comorbidity. Disordered thinking and judgment can be expected to make it difficult to engage in behavior that reduces risk factors for type 2 diabetes, such as restrained eating for weight management. Further, people with serious mental health disorders and diabetes frequently experience moderate psychological distress, suggesting pervasive intrusion of mental health issues into daily functioning Coordinated management of diabetes or prediabetes and serious mental illness is recommended to achieve diabetes treatment targets. In addition, those taking second-generation atypical antipsychotics, such as olanzapine, require greater monitoring because of an increase in risk of type 2 diabetes associated with this medication — Because of this increased risk, people should be screened for prediabetes or diabetes 4 months after medication initiation and at least annually thereafter. Serious mental illness is often associated with the inability to evaluate and utilize information to make judgments about treatment options. When a person has an established diagnosis of a mental illness that impacts judgment, activities of daily living, and ability to establish a collaborative relationship with care providers, it is wise to include a nonmedical caretaker in decision-making regarding the medical regimen. Cognitive capacity is generally defined as attention, memory, logic and reasoning, and auditory and visual processing, all of which are involved in diabetes self-management behavior Having diabetes over decades—type 1 and type 2—has been shown to be associated with cognitive decline — Declines have been shown to impact executive function and information processing speed; they are not consistent between people, and evidence is lacking regarding a known course of decline Diagnosis of dementia is also more prevalent in the population of individuals with diabetes, both type 1 and type 2 Thus, monitoring of cognitive capacity of individuals is recommended, particularly regarding their ability to self-monitor and make judgements about their symptoms, physical status, and needed alterations to their self-management behaviors, all of which are mediated by executive function As with other disorders affecting mental capacity e. When this ability is shown to be altered, declining, or absent, a lay care provider should be introduced into the care team who serves in the capacities of day-to-day monitoring as well as a liaison with the rest of the care team 1. Cognitive capacity also contributes to ability to benefit from diabetes education and may indicate the need for alternative teaching approaches as well as remote monitoring. Youth will need second-party monitoring e. Episodes of severe hypoglycemia are independently associated with decline, as well as the more immediate symptoms of mental confusion Early-onset type 1 diabetes has been shown to be associated with potential deficits in intellectual abilities, especially in the context of repeated episodes of severe hypoglycemia If cognitive capacity to carry out self-maintenance behaviors is questioned, an age-appropriate test of cognitive capacity is recommended 1. Cognitive capacity should be evaluated in the context of the age of the person, for example, in very young children who are not expected to manage their disease independently and in older adults who may need active monitoring of regimen behaviors. Suggested citation: American Diabetes Association Professional Practice Committee. Facilitating behavior change and well-being to improve health outcomes: Standards of Medical Care in Diabetes— Diabetes Care ;45 Suppl. Sign In or Create an Account. Search Dropdown Menu. header search search input Search input auto suggest. filter your search All Content All Journals Diabetes Care. Advanced Search. User Tools Dropdown. Sign In. Skip Nav Destination Close navigation menu Article navigation. Previous Article Next Article. Diabetes Self-Management Education and Support. Medical Nutrition Therapy. Physical Activity. Smoking Cessation: Tobacco and e-Cigarettes. Psychosocial Issues. Article Navigation. Standards of Care December 16 Facilitating Behavior Change and Well-being to Improve Health Outcomes: Standards of Medical Care in Diabetes— American Diabetes Association Professional Practice Committee American Diabetes Association Professional Practice Committee. This Site. Google Scholar. Get Permissions. toolbar search Search Dropdown Menu. toolbar search search input Search input auto suggest. Table 5. Effectiveness of nutrition therapy 5. E Energy balance 5. A Eating patterns and macronutrient distribution 5. Eating plans should emphasize nonstarchy vegetables, fruits, and whole grains, as well as dairy products, with minimal added sugars. Therefore, carbohydrate sources high in protein should be avoided when trying to treat or prevent hypoglycemia. B Dietary fat 5. B Micronutrients and herbal supplements 5. The importance of glucose monitoring after drinking alcoholic beverages to reduce hypoglycemia risk should be emphasized. B Sodium 5. B Nonnutritive sweeteners 5. Overall, people are encouraged to decrease both sweetened and nonnutritive-sweetened beverages, with an emphasis on water intake. View Large. To promote and support healthful eating patterns, emphasizing a variety of nutrient-dense foods in appropriate portion sizes, to improve overall health and: achieve and maintain body weight goals attain individualized glycemic, blood pressure, and lipid goals delay or prevent the complications of diabetes To address individual nutrition needs based on personal and cultural preferences, health literacy and numeracy, access to healthful foods, willingness and ability to make behavioral changes, and existing barriers to change To maintain the pleasure of eating by providing nonjudgmental messages about food choices while limiting food choices only when indicated by scientific evidence To provide an individual with diabetes the practical tools for developing healthy eating patterns rather than focusing on individual macronutrients, micronutrients, or single foods. Psychosocial care for people with diabetes: a position statement of the American Diabetes Association. Search ADS. Collaborative care for patients with depression and diabetes mellitus: a systematic review and meta-analysis. Problem solving in diabetes self-management: a model of chronic illness self-management behavior. A framework for optimizing technology-enabled diabetes and cardiometabolic care and education: the role of the diabetes care and education specialist. Taxonomy of the burden of treatment: a multi-country web-based qualitative study of patients with chronic conditions. Effect of DECIDE Decision-making Education for Choices In Diabetes Everyday program delivery modalities on clinical and behavioral outcomes in urban African Americans with type 2 diabetes: a randomized trial. Diabetes self-management education improves quality of care and clinical outcomes determined by a diabetes bundle measure. Twenty-first century behavioral medicine: a context for empowering clinicians and patients with diabetes: a consensus report. Self-management education for adults with type 2 diabetes: a meta-analysis of the effect on glycemic control. Evaluation of a behavior support intervention for patients with poorly controlled diabetes. Structured type 1 diabetes education delivered within routine care: impact on glycemic control and diabetes-specific quality of life. Diabetes self-management education for adults with type 2 diabetes mellitus: a systematic review of the effect on glycemic control. Diabetes self-management education and medical nutrition therapy: a multisite study documenting the efficacy of registered dietitian nutritionist interventions in the management of glycemic control and diabetic dyslipidemia through retrospective chart review. Group based diabetes self-management education compared to routine treatment for people with type 2 diabetes mellitus. A systematic review with meta-analysis. Meta-analysis of quality of life outcomes following diabetes self-management training. Diabetes self-management education reduces risk of all-cause mortality in type 2 diabetes patients: a systematic review and meta-analysis. Facilitating healthy coping in patients with diabetes: a systematic review. Nutritionist visits, diabetes classes, and hospitalization rates and charges: the Urban Diabetes Study. One-year outcomes of diabetes self-management training among Medicare beneficiaries newly diagnosed with diabetes. A systematic review of interventions to improve diabetes care in socially disadvantaged populations. Culturally appropriate health education for type 2 diabetes mellitus in ethnic minority groups. Get tested for kidney disease. Having diabetes puts you at risk for developing kidney disease. Ask your healthcare team to be tested for kidney disease. You should be tested for kidney disease at least once a year. Learn more. Learn all you can about keeping your diabetes under control, and be sure to learn about your risk for kidney disease. Stay informed, take charge of your health, and always be an active member of your healthcare team. are at risk for kidney disease. Find out if you're at risk. Take the Quiz. Save this content:. Share this content:. Leave this field blank. Is this content helpful? Back to top:. Donate Monthly. However, in an emotional affair, adolescents get more support from friends rather than family The adolescent may not always feel comfortable discussing their disease with everyone. Healthcare professionals could play an important role in supporting them to make friendly confessions about their condition with those close to them. Healthcare professionals could help young people in figuring out a way to discuss their disease management or ask their peers about the ideal approaches to assist them in managing their disease Moreover, this review highlights that the collaborative care is an important criterion of self-management for adolescent diabetes patients. If all the supportive groups play their role, then it is easy for adolescents to manage their diabetes properly. The term self-management is frequently baffling as there is no generally acknowledged definition, and it is utilized to convey different ideas, for example, the guidance of self-care and self-management, patient activities, and self-management education Self-management education enhances control of T2DM, particularly when conveyed as short intercessions, enabling the patient to recollect and have a better blend of information The conventional educational forms of care that include instructing patients to enhance the awareness of health status provide a path to the present forms that focus on the behavioral and self-care advances aim to equip patients with the attitudes and strategies to advance and alter their behavior Self-management education is a community-oriented and continuing process expected to encourage the advancement of behaviors, knowledge, and abilities that are required for fruitful self-management of diabetes A multidisciplinary team is essential for the education program which involves educational supporters from hospitals and clinics, and the direct involvement of healthcare professionals. The process of the education program ought to comply with the standards and terms stated by the National Standards for Diabetes Self-management Education, which aims to support and assist diabetes educatiors in providing good quality education and self-management support The American Association of Clinical Endocrinologists has recognized that Diabetes Self-Management Education DSME remains as a crucial feature of care for diabetes people. In addition, DSME serves as an avenue for acquisition of knowledge, skills, abilities, and collaboration with other people, which are essential for engaging self-management of diabetes DSME programs help individuals to adapt to the psychological and physical needs of the disease, specifically the remarkable financial, social, and cultural conditions. The principal objective of DSME is to enable patients to take control of their own condition by enhancing their insight and attitudes, so that, they can make knowledgeable decisions for self-guided behavior, changing their regular lives and eventually moderating the danger of complications Definite metabolic control and quality of life as well as the avoidance of complications are the ultimate aims specified by diabetes self-management education Knowledge of and information about the successful management and treatment of adult diabetes patients allow adjustments to be made in youth's management of diabetes. The treatment and management guidance of adult patients needs to be translated and adapted by child patients. Though these guidance are easily translatable to older adolescents, physicians are often hesitant regarding how to treat and manage young children and adolescents with T2DM Through knowledge and education, individuals with DM can figure out how to make life decisions, and can discuss more with their clinicians to accomplish ideal glycemic control A study examined the impacts of a self-care education program on T2DM patients demonstrated that the program leads to an improvement in state of mind and behavior, and fewer complexities, and thus leads to an improved mental and physical quality of life. Several authors have discussed that diabetes self-management education is provided to control the disease including monitoring of emergencies such as hypoglycemia and hyperglycemia. Indeed, several studies found that diabetes self-management education improves HbA 1C and patient compliance 63 , A diabetes education program is vital in glycemic control, as psychological support brings better clinical outcomes and emotional improvement, and controls the hazard of continuing complications 64 — Among the primary barriers of managing youth and children with T2DM are inadequate scientific support about treatment, patient adherence, and deficiency in knowledge about recent recommendations 67 , Consequently, various ways have been recommended for self-management of diabetes mellitus among adolescents. These provide a coherent picture of daily activities and care that adolescent patients with T2DM adapt effectively To accomplish this goal, further interventional work is required to positively establish the most efficient management alternative in this population. The previously published studies in this setting are summarized in Table 2. Table 2. Studies of self-care and self-management of adolescent patients with diabetes. Further research is essential to get a more reliable conclusion concerning the appropriate self-care practices and self-management of adolescent patients with T2DM. Most studies were conducted on self-care practices and self-management in adult patients with T2DM. There is a number of quality studies of self-care practices with type 1 adolescent patients, but only a small number have included type 2 adolescent patients. Nevertheless, adult diabetes management approaches are successful for imparting knowledge and understanding, and are adaptable for adolescents Although the management process of adolescents is almost same as the adults, healthcare providers are usually uncertain about how to guide and develop the knowledge and understanding of the most appropriate methods for proper management guideline for adolescents with T2DM. There are very limited experimental trials, and most of the treatment and management recommendations are referred from adults; therefore, the current guidelines for management for adolescents with T2DM may not be fully evidence-based. Successful outcomes have been noticed for both Type 1 and T2DM in youth and adolescent patients through a supportive team. Given the recognized importance of social support in encouraging diabetes self-care behaviors, family and care-givers could lessen the burden of T2DM by providing extra attention to the patients' need 41 , Research highlights the necessities of self-care and self-management for those who have a delayed determination of diabetes, a period where intercessions can lead the most significant advantages for long-term education opportunities and management. Early concerns and active management are imperative for drafting management plans that inclusive of self-management education, dietary follow up, physical activity and behavior alteration to optimize blood glucose and diminish diabetes-related complications. The review of the issue is still relatively limited until more studies on this area have been conducted. Diabetes is a complicated illness that requires individual patient to adhere to various recommendations in making day-to-day choices in regard to diet, physical movement, and medications. It additionally requires the personal capability of diverse self-management abilities. There is an enormous need for committed self-care practices in various spaces, with nutritional choices, physical activity, legitimate medication, and blood glucose monitoring by the patients. A positive and encouraging self-care exercise commitment for diabetic patient can be emanated from good social support. Parental support in disease management leads to an effective change in patients' glycaemic control. Nevertheless, the majority of adolescent patients with T2DM are associated to families with sedentary daily routines, high-fat diets, and poor food habits who often have a family history of diabetes. This is likely to be disadvantageous to the management of diabetes in adolescents. The responsibility of clinicians in advancing self-care is imperative and ought to be highlighted. To prevent any long-term complications, it is important to recognize the comprehensive nature of the issue. An orderly, multi-faceted and coordinated progress must be involved to advance self-care practices. CN, LM, YW, and MS designed and directed the study. They were involved in the planning and supervised the study. JE, YK, CN, LM, YW, MH, YH and MS were involved in the interpretation of the data, as well as provided critical intellectual content in the manuscript. JE contributed to writing the manuscript and updated and revised the manuscript to the final version with the assistance of other authors. The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. This work was supported in part by Universiti Teknologi MARA UiTM under MyRA Incentive Grant. We also thank KPJUC and CUCMS for partial publication fee support. Bell R. SEARCH for diabetes in youth: a multicenter study of the prevalence, incidence and classification of diabetes mellitus in youth. Control Clin Trials — doi: CrossRef Full Text Google Scholar. SEARCH for Diabetes in Youth Study Group, Liese AD, D'Agostino RB Jr, Hamman RF, Kilgo PD, Lawrence JM, et al. The burden of diabetes mellitus among US youth: prevalence estimates from the SEARCH for Diabetes in Youth Study. Pediatrics —8. PubMed Abstract CrossRef Full Text Google Scholar. Dabelea D, Mayer-Davis EJ, Saydah S, Imperatore G, Linder B, Divers J, et al. Prevalence of type 1 and type 2 diabetes among children and adolescents from to JAMA — Chaudhury A, Duvoor C, Reddy Dendi VS, Kraleti S, Chada A, Ravilla R, et al. Clinical review of antidiabetic drugs: implications for type 2 diabetes mellitus management. Front Endocrinol Global Report on Diabetes: Diabetes Programme. Geneva: World Health Organization PubMed Abstract. Nyenwe EA, Jerkins TW, Umpierrez GE, Kitabchi AE. Management of type 2 diabetes: evolving strategies for the treatment of patients with type 2 diabetes. Metabolism — Miller DK, Austin MM, Colberg SR, Constance A, Dixon DL, MacLeod J, et al. Diabetes Education Curriculum: A Guide to Successful Self-Management. Chicago, IL: American Association of Diabetes Educators. Grey A. Nutritional recommendations for individuals with diabetes. In: De Groot LJ, Chrousos G, Dungan K, Feingold KR, Grossman A, Hershman JM, Koch C, Korbonits M, McLachlan R, New M, Purnell J, Rebar R, Singer F, and Vinik A, editors. South Dartmouth, MA: MDTesxt. com, Inc. Google Scholar. Powers MA, Bardsley J, Cypress M, Duker P, Funnell MM, Fischl AH, et al. Diabetes self-management education and support in type 2 diabetes: a joint position statement of the American Diabetes Association, the American Association of Diabetes Educators, and the Academy of Nutrition and Dietetics. ClinDiabetes — Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness. JAMA —9. Tomky D, Cypress M. American Association of Diabetes Educators AADE Position Statement: AADE 7 Self-Care Behaviors. Chicago, IL: The Diabetes Educators Cooper HC, Booth K, Gill G. Patients' perspectives on diabetes health care education. Health Education Res. Paterson B, Thorne S. Developmental evolution of expertise in diabetes self-management. Clin Nurs Res. Shrivastava SR, Shrivastava PS, Ramasamy J. Role of self-care in management of diabetes mellitus. J Diabetes Metab Disord. Johnson SB. Health behavior and health status: concepts, methods, and applications. J Pediatr Psychol. Boulé NG, Haddad E, Kenny GP, Wells GA, Sigal RJ. Effects of exercise on glycemic control and body mass in type 2 diabetes mellitus: a meta-analysis of controlled clinical trials. American Diabetes Association. Diabetes Care 32 Suppl. CrossRef Full Text. Lichner V, Lovaš L. Model of the self-care strategies among slovak helping professionals — qualitative analysis of performed self-care activities. Humanit Soc Sci. Available online at: ssrn. Lin K, Yang X, Yin G, Lin S. Diabetes self-care activities and health-related quality-of-life of individuals with type 1 diabetes mellitus in Shantou, China. J Int Med Res. |
| You are here | Individual interviews were conducted 2 to 21 weeks after completion of quantitative data collection. We used a purposive sampling strategy to recruit participants with a range of experiences and characteristics [ 42 ] sex, age, ethnicity, duration of diabetes, educational attainment, income from the broader pool of cohort study participants. We made the website available during each interview, in case the interviewee wanted to show the interviewer something on the website. All interviews were audiotaped and transcribed verbatim [ 43 ]. Transcripts were inductively analyzed to identify emergent categories and themes using a constant comparative approach [ 44 ]. Coding was conducted independently by three team members with expertise in qualitative research methods CHY, JAP, SH [ 44 ]. After coding an initial subset of interviews, a preliminary coding framework was developed on the basis of the emerging analysis, with discussion and consensus amongst the analysts [ 45 ]; the framework was then iteratively tested and refined with subsequent interviews [ 44 ]. Thematic saturation was attained with 21 interviews [ 42 ]. NVivo software version 9 was used to assist with data management and retrieval. Techniques to ensure analytic rigour included use of multiple analysts, negative case analysis, and triangulation of the qualitative findings with the quantitative results [ 42 ],[ 44 ],[ 46 ]. The study was approved by the Research Ethics Boards of St. All participants gave written and verbal informed consent. Of the 98 participants recruited, 81 had complete data collection for at least two time points one before and one after the intervention was implemented and were included in the analysis. The mean number of days on which users logged in during the study period was 8. The average frequency of use was 0. Increased use of the website during those weeks appeared to be driven by the blog. In general, website use appeared to parallel blog use, with users visiting the blog repeatedly during the same login or visit Figure 1. Website login and blog use by week. Black bar: Number of logins per week. Grey bar: Number of blog views per week. Regarding site penetration, users viewed 6. Within the blog section of the website, there were a total of page views by 35 participants over the study period, with peaks at week 10 54 views , week 27 43 views , and week 30 53 views , corresponding to blog entries about the medication log, supplements and insulin, and foot and kidney care, respectively. A total of 13 comments responding to the blog postings were submitted by five participants. These comments took the following forms: 1 responding to the blog agreement or disagreement ; 2 requesting help with or providing feedback on the website; 3 requesting help with self-management; 4 offering assistance, empowerment, and their own solutions including food recipes ; 5 self-reporting behaviour change; 6 sharing responses to medication; and 7 warning others about interactions with health care providers. These users had a mean of 3. Self-efficacy: Despite a significant short-term increase in self-efficacy score immediately after implementation of the intervention 0. Self-efficacy, self-care, and diabetes distress nine months before and nine months after intervention implementation. Reference categories used in the plot were as follows: female, mean age Self-care: The self-care score improved by 0. Self-care scores were positively correlated with age 0. Diabetes distress varied with age and sex: younger female participants had greater diabetes distress. Seventy-three of the participants were included in the analysis of clinical outcomes. The other eight participants were excluded because of missing data for HbA1c, blood pressure, LDL-C, or weight within 90 days of the self-efficacy data or because no data were obtained after implementation of the intervention. The intervention had no effect on HbA1c, blood pressure, LDL-C, or weight in either the unadjusted or the adjusted models Table 2. At the nine-month follow-up after implementation of the intervention, there was no difference between users and non-users in terms of self-efficacy 0. Twenty-one individuals Table 1 participated in an interview. The sample consisted of White and Asian men and women of various ages, duration of diabetes, educational attainment, and employment status, who used computers frequently and were comfortable with using the internet. Additional themes will be the focus of future publications. The following four themes are considered here: 1 barriers and facilitators of website use; 2 patterns of website use, including the role of the blog in driving site traffic; 3 general feedback on website characteristics; and 4 potential mechanisms for the effect of the website on self-efficacy, behaviour change, and diabetes distress. Representative quotes for each theme appear in Table 3. In particular, participants reported feeling frustrated with the uncontrolled nature of their disease, and the collection of self-monitoring information that showed a lack of metabolic control exacerbated this frustration Table 3 ; 1d. Similarly, some participants said that they were sometimes overcome with a sense of futility. They perceived that regardless of their actions, some outcomes such as dialysis were inevitable Table 3 ; 1e ; hence, they saw no value in learning about the disease or in trying to self-manage the disease or use the website. Others were limited by poor computer or internet access and said they would prefer a mobile solution Table 3 ; 1g. Finally, some participants noted that the onerous process for correcting error in log entries discouraged them from using the self-management tools Table 3 ; 1h. In contrast, other website characteristics appeared to encourage users to visit and return. Similarly, routinization of the online experience appeared to routinize use of the internet for certain aspects of health care. Rather than browsing at random, users said they were goal-directed: when they had a specific concern, they focused on that area of the website Table 3 ; 2a. For example, one participant was initially motivated to visit and subsequently continued to visit the foot care section of the website because of her foot symptoms Table 3 ; 2b. Participants also commented that they used the website to gauge the urgency of their concerns and to try to obtain immediate answers to their questions Table 3 ; 2b. We explored potential reasons for the unexpected finding that the blog was the most frequently accessed tool and appeared to drive website usage. participating in a discussion thread. However, this was not a universal sentiment, and some participants felt uncomfortable with and disconnected from the blog Table 3 ; 2c,ii. Participants perceived that the website was accurate, comprehensive Table 3 ; 3a , and easy to navigate Table 3 ; 3b. Deeper exploration of the data regarding patterns of use and website features uncovered factors that might account for these quantitative findings. For example, rather than returning to the site to revisit and review items, some participants reported that they printed items of interest from the website and subsequently referred to these paper copies Table 3 ; 4a. The use of reminder emails also had an effect. Participants reported that these emails not only prompted them to return to and log into the website, but also encouraged them in their own self-management Table 3 ; 4b. Although she did not subsequently login to the website to record these behaviours, she did continue to record them on paper. We found that a self-management website for patients with type 2 diabetes led to no improvement in self-efficacy, diabetes distress, or clinical outcomes over the study period. However, there was an improvement in self-care a secondary outcome , and the group that used the website experienced significantly lower diabetes distress than those who did not use it. Despite a user-centred design process and an increase in the frequency of blog posting from weekly to twice weekly, use of the website as ascertained by login records was limited. Our interviews revealed that both patient-related factors e. competing health and life concerns, a sense of futility and website-related factors e. requirement for login, limited computer or internet access limited use of the website. These qualitative findings have confirmed the importance of website features such as the reliability and authoritativeness of information [ 47 ], as well as the use of blogs [ 15 ] and reminders [ 48 ] for continued engagement of users. Our data also suggest that mobile devices are a potential avenue through which to improve accessibility and use of a self-management site. However, as with web-based technology, a systematic approach to development, testing, implementation, and evaluation of mobile health technology is warranted. Although such technologies are proliferating, with over applications related to diabetes alone, their usability and clinical effectiveness are variable [ 53 ], and concerns exist regarding their effectiveness and safety, as well as the security of personal health information [ 54 ]. Our findings regarding user engagement with web-based technology echo those for mobile technology: an evaluation of 10 mobile diabetes applications emphasized the importance of user-centred design, an engaging interface, and context-driven use [ 55 ]. Competing health concerns were identified as a barrier to web-based self-management. depression , which in turn directly affects self-management ability and competes for time and attention [ 56 ]. For example, patients with a greater number of comorbidities placed a lower priority on diabetes and had worse diabetes self-management ability [ 57 ]. Future interventions should consider strategies, such as shared decision-making and priority-setting, to empower patients with multiple comorbidities to optimize their self-care [ 58 ]. For example, a patient may identify mood management as a priority, which is key to subsequent self-care. Finally, our results may be extrapolated to other chronic diseases. In particular, our finding of the need for tailored content and peer support, balanced with concerns regarding information reliability and confidentiality, is applicable to other strategies for managing chronic disease. For example, a systematic review of the benefits and limitations of social media in the context of chronic disease identified benefits increased interaction and social support, tailored and accessible information and limitations quality concerns and lack of reliability, confidentiality, and privacy [ 59 ] to those we identified. Similarly, our finding of a reduction in diabetes distress in conjunction with no improvements in clinical outcomes echoes findings from intervention strategies targeting other chronic diseases. For example, another systematic review examining the effect of social media on psychological and physical outcomes in chronic disease found a relatively large body of evidence demonstrating psychological benefit 19 identified studies but limited evidence for physical outcomes 4 identified studies [ 60 ]. This study was limited by its non-randomized design. However, we employed a repeated-measures design that permitted reliable assessment of baseline self-efficacy. Although our primary outcome self-efficacy was a non-clinical outcome, it is a validated predictor of patient behaviour change and clinical outcomes [ 18 ],[ 20 ],[ 24 ],[ 25 ]. The infrequency of website use likely limited the effect of this intervention, but we obtained valuable insights regarding mediators of website use through our individual interviews. The qualitative evaluation was conducted by individuals who were also involved in developing the intervention, which created a potential for bias; however, we guarded against this bias by including individuals who were not involved in designing the website as members of the qualitative analytic team and by having three coders. As such, we were able to obtain and report critical feedback that participants openly shared. Study strengths include the use of multiple repeated measures, the use of validated outcomes, dual coding of all transcripts, and triangulation of the qualitative findings with the quantitative results [ 42 ],[ 44 ],[ 46 ]. Increasing use of the World Wide Web by consumers for health information and ongoing revolutions in social media are strong indicators that consumers are welcoming and demanding a new era of technology in health care. However, full potential of this technology is hindered by limited uptake and high attrition rates. Our research findings have shed light on these limitations by identifying characteristics associated with website use and attrition and suggesting strategies to reduce website attrition as a way to potentially optimize clinical outcomes. Centers for Disease Control and Prevention: Diabetes Report Card Atlanta, GA: Centers for Disease Control and Prevention, US Department of Health and Human Services; American Diabetes Association: Standards of medical care in diabetes Diabetes Care. Article Google Scholar. Haas L, Maryniuk M, Beck J, Cox CE, Duker P, Edwards L, Fisher EB, Hanson L, Kent D, Kolb L, McLaughlin S, Orzeck E, Piette JD, Rhinehart AS, Rothman R, Sklaroff S, Tomky D, Youssef G: National standards for diabetes self-management education and supportdiabetes. Selby JV, Beal AC, Frank L: The Patient-Centered Outcomes Research Institute PCORI national priorities for research and initial research agenda. J Am Med Assoc. Article CAS Google Scholar. Cochrane J, Conn VS: Meta-analysis of quality of life outcomes following self-management training. Diabetes Educ. Minet L, Møller S, Vach W, Wagner L, Henriksen JE: Mediating the effect of self-care management intervention in type 2 diabetes: a meta-analysis of 47 randomised controlled trials. Patient Educ Couns. Article PubMed Google Scholar. Ruppert K, Uhler A, Siminerio L: Examining patient risk factors, comorbid conditions, participation, and physician referrals to a rural diabetes self-management education program. Shaw K, Killeen M, Sullivan E, Bowman P: Disparities in diabetes self-management education for uninsured and underinsured adults. Shekelle PG, Morton SC, Keeler EB: Costs and Benefits of Health Information Technology. Google Scholar. Yu CH, Bahniwal R, Laupacis A, Leung E, Orr MS, Straus SE: Systematic review and evaluation of web-accessible tools for management of diabetes and related cardiovascular risk factors by patients and healthcare providers. J Am Med Inform Assoc. Article PubMed PubMed Central Google Scholar. Bull SS, Gaglio B, McKay HG, Glasgow RE: Harnessing the potential of the internet to promote chronic illness self-management: diabetes as an example of how well we are doing. Chronic Illness. van Vugt M, de Wit M, Cleijne WH, Snoek FJ: Use of behavioral change techniques in web-based self-management programs for type 2 diabetes patients: systematic review. J Med Internet Res. Seidman JJ, Steinwachs D, Rubin HR: Design and testing of a tool for evaluating the quality of diabetes consumer-information Web sites. Shrank WH, Patrick AR, Brookhart MA: Healthy user and related biases in observational studies of preventive interventions: a primer for physicians. J Gen Intern Med. Yu CH, Parsons J, Hall S, Newton D, Jovicic A, Lottridge D, Shah BR, Straus SE: User-centered design of a web-based self-management site for individuals with type 2 diabetes — providing a sense of control and community. BMC Med Inform Decis Mak. Yu C, Parsons J, Mamdani M, Lebovic G, Shah BR, Bhattacharyya O, Laupacis A, Straus SE: Designing and evaluating a web-based selfmanagement site for patients with type 2 diabetes - systematic website development and study protocol. Bandura A: Self-Efficacy: the Exercise of Control. Freeman, New York. Article CAS PubMed Google Scholar. Reichard P, Toomingas B, Rosenqvist U: Changes in conceptions and attitudes during five years of intensified conventional insulin treatment in the stockholm diabetes intervention study SDIS. Anderson RM, Funnell MM, Butler PM, Arnold MS, Fitzgerald JT, Feste CC: Patient empowerment: results of a randomized controlled trial. Trief PM, Teresi JA, Eimicke JP, Shea S, Weinstock RS: Improvement in diabetes self-efficacy and glycaemic control using telemedicine in a sample of older, ethnically diverse individuals who have diabetes: the IDEATel project. Age Ageing. Aljasem LI, Peyrot M, Wissow L, Rubin RR: The impact of barriers and self-efficacy on self-care behaviors in type 2 diabetes. Grossman HY, Brink S, Hauser S: Self-efficacy in adolescent girls and boys with insulin-dependent diabetes mellitus. Nakahara R, Yoshiuchi K, Kumano H, Hara Y, Suematsu H, Kuboki T: Prospective study on influence of psychosocial factors on glycemic control in Japanese patients with type 2 diabetes. One of the more successful interventions for improving diabetes self-care and patient-physician communication is motivational interviewing MI. Inherent to MI is the belief that motivation for change is malleable and that it can be transformed in the context of the patient-physician relationship [81]. Recent meta-analyses and systematic reviews [83—87] showed that MI interventions improve self-care behaviors and glycemic control in the short-term; long-term effects of MI on self-care and glycemia remain inconclusive. More high-quality research is needed to evaluate the MI training content of these interventions in order to determine its long-term effectiveness and replicate outcomes in various healthcare settings [87]. Other studies not included in the meta-analyses and reviews found MI interventions improved self-care behaviors [88—90], glycemic control [90,91], and quality of life [91]. Another study, an internet-based incentives study, found that the application of a brief MI interviewing session improved blood glucose monitoring in adolescents with type 1 diabetes [94]. Thus, creative strategies that employ MI techniques in collaboration with other members of the health care team ie, patient navigation [93], telehealth [89], health coaching [95], internet-based tools [94] hold promise for improving self-care and patient-physician communication. Increased collaboration with members of the health care team eg, certified diabetes educators, nurses, dietitians, pharmacists, exercise physiologists , community health workers [96,97] and peer mentors [98,99] may help reinforce messages, promote shared decision-making, improve diabetes outcomes, increase patient satisfaction, and reduce medical costs []. Few other interventions have directly addressed physician-patient diabetes self-care communication. Patients randomized to the intervention arm participated in a minute session prior to meeting with their physician, in which researchers reviewed their medical chart and used systematic prompts to encourage patients to negotiate medical decisions with their physician. Patients in the control arm received standard educational materials in a session of equal length. Patients in the intervention arm improved glycemia and elicited twice the amount of medical information from their physician compared to controls [16]. These findings suggest that brief interventions prior to medical appointments can improve patient communication, self-care behavior, and in turn, diabetes outcomes [16]. A recent study evaluated the effectiveness of a training program in communication skills for pediatric diabetes care providers in the UK [, ]. In this cluster randomized controlled trial, pediatric providers allocated to the Talking Diabetes intervention participated in web-based material and face-to-face seminars designed to prepare providers for constructive self-care conversations with patients as well as skills for promoting behavior change. The psychoeducational training emphasized shared decision-making and utilized motivational interviewing techniques []. Twenty-six centers and young people with type 1 diabetes participated in the study []. At month follow-up, the Talking Diabetes intervention did not demonstrate improvements in glycemic control. Interestingly, parents of patients in the intervention arm reported greater continuity of care, which suggests that parents benefited more from the intervention than their children. Future communication interventions targeting the pediatric population should provide ongoing support to children of physicians exposed to interventions such as Talking Diabetes []. Currently, 3 ongoing studies aim to improve self-care and clinical outcomes via physician-patient communication interventions. A study by Ricci-Cabello and colleagues [] aims to improve diabetes self-care by enhancing patient-physician communication in an underserved community of adults with uncontrolled type 2 diabetes. In this 3-arm randomized controlled trial, patients allocated to groups A and B received communication skills training and graphic feedback about glycosylated hemoglobin A 1c levels; patients in group C received usual care. Patients in group B also received telephone reinforcement []. The second study, by Billimek and colleagues, aims to improve physician-patient communication about medication regimens via diabetes coaching []. In this intervention, Mexican-American adult patients with type 2 diabetes were randomly assigned to complete a Coached Care visit with trained community health workers or a Coached Care visit plus the EMPATHy software toolkit, a computer-based activity with strategies and resources to overcome self-care barriers. The primary endpoints are 1 the development of care plan that addresses everyday barriers to medication adherence and 2 completion of a concrete behavioral goal []. Finally, the third study, by Grant and colleagues, aims to improve physician-patient communication via a pre-visit prioritization of diabetes concerns. In this controlled, cluster-randomized, multisite trial, primary care physicians were randomized to the Pre-Visit Prioritization for Complex Patients with Diabetes or the control group []. The Pre-Visit Prioritization IT-tool is designed to help patients identify one or two concerns prior to a medical visit and then send these priorities to the primary care physician via an electronic health record. The overall goal of the intervention is to improve communication of self-care concerns during a medical visit []. Findings from these 3 interventions are forthcoming; findings may provide evidence for validated interventions that improve physician-patient self-care communication in diabetes. Incorporating communication skills in continuing medical education and diabetes education may improve self-care communication in the physician-patient relationship. Most patients will remember only a small portion of the information given to them during medical visit. Therefore, physicians need techniques that promote open self-care communication during a visit. The following techniques can help physicians improve self-care communication []:. Reflecting and summarizing show the patient that the physician has been listening to concerns and understands what the patient is saying. This is also an opportunity to correct any miscommunications from the visit. Write down instructions or provide handouts to the patient to help reinforce learning and information retention. Ask patients to write a list of questions a few days prior to the medical appointment and bring it with them. Patients are more likely to remember information about issues they have previously considered that directly relate to them. Consider collaborating with community health workers, patient navigators, peer mentors, and other members of the healthcare team to improve communication, diabetes outcomes, and patient satisfaction. More research is needed to determine the best strategies to improve self-care communication in the physician-patient relationship. Steps include:. Your provider will also help you by ordering blood tests and other tests. These help make sure your blood sugar and cholesterol levels are each in a healthy range. Also, follow your provider's instructions about keeping your blood pressure in a healthy range. Your doctor will likely ask you to visit other providers to help you control your diabetes. These providers include a:. Foods with sugar and carbohydrates can raise your blood sugar too high. Alcohol and other drinks with sugar can also raise your blood sugar. A nurse or dietitian can teach you about good food choices. Make sure you know how to have a balanced meal with protein and fiber. Eat healthy, fresh foods as much as possible. Don't eat too much food at one sitting. This helps keep your blood sugar in a good range. Managing your weight and keeping a well-balanced diet are important. Some people with type 2 diabetes can stop taking medicines after losing weight even though they still have diabetes. Your provider can let you know a good weight range for you. Weight-loss surgery may be an option if you are obese and your diabetes is not under control. Your doctor can tell you more about this. It helps burn extra fat so that you can keep your weight down. Exercise can even help you handle stress and improves your mood. Try walking, jogging, or biking for 30 to 60 minutes every day. Pick an activity that you enjoy and you are more likely to stick with. Bring food or juice with you in case your blood sugar gets too low. Drink extra water. Try to avoid sitting for more than 30 minutes at any one time. Wear a diabetes ID bracelet. In case of an emergency, people know you have diabetes and can help you get the right medical attention. Always check with your provider before beginning an exercise program. Your provider can help you choose an exercise program that is safe for you. You may be asked to check your blood sugar at home. This will tell you and your provider how well your diet, exercise, and medicines are working. A device called a glucose meter can provide a blood sugar reading from just a drop of blood. A doctor, nurse, or diabetes educator will help set up a home testing schedule for you. Your doctor will help you set your blood sugar goals. If diet and exercise are not enough, you may need to take medicine. It will help keep your blood sugar in a healthy range. There are many diabetes medicines that work in different ways to help control your blood sugar. Many people with type 2 diabetes need to take more than one medicine to control their blood sugar. You may take medicines by mouth or as a shot injection. Certain diabetes medicines may not be safe if you are pregnant. So, talk to your doctor about your medicines if you're thinking of becoming pregnant. If medicines don't help you control your blood sugar, you may need to take insulin. |
Incorporating self-care in diabetes management -
The maintenance phase is often a period of struggle Table 2. Slips and relapses both begin with a mistake. If the patient quickly returns to the change effort, the mistake is considered a slip; however, if the patient reverts to a previous stage, it is considered the beginning of a relapse.
Persons who view a slip primarily as their personal failure tend to feel guilt and shame, and have increased risk of relapse. Persons who view a slip as the result of difficulty coping effectively with a specific high-risk situation are more likely to want to learn from the mistakes and develop effective ways to handle similar situations in the future.
A helpful approach involves focusing on specific examples and prompting the patient to brainstorm about possible triggers and how to overcome them next time.
Commonly cited precipitants include negative emotions, interpersonal conflicts, social pressure, time pressure, and celebrations. A person who can execute effective coping skills is less likely to relapse Table 4. Describe : I was planning to walk after dinner, but the friend I walk with canceled.
My daughter was watching a movie, so I watched with her instead. Brainstorm : I could listen to a podcast while I walk alone. Or, I could ask my daughter to walk with me now, and we'll watch a movie together afterward.
This article updates a previous article on this topic by Koenigsberg, et al. Data Sources : Literature searches were performed using the OVID Med-line Database with key terms prediabetes, prediabetic state, and diabetes mellitus, crossed with lifestyle, diet, exercise, physical activity, weight reduction programs, patient compliance, and adherence.
The search was limited to randomized controlled trials, review articles, or meta-analyses, with studies limited to those in English with human participants.
Later searches were done for specific areas such as follow-up publications on major studies Diabetes Prevention Program, Look AHEAD, Da Qing IGT and Diabetes Study, Malmo Study, Finnish Diabetes Prevention Study or meta-analyses for relevant areas e.
Also searched were AFP archives, Guideline. gov, Cochrane database, AHRQ. gov, CDC. gov, and Essential Evidence Plus. Search dates: November , January to March , October to December , and April Centers for Disease Control and Prevention. National diabetes statistics report, Accessed March 21, National data.
Updated April American Diabetes Association. Standards of medical care in diabetes— Diabetes Care. Updated December Accessed November 8, Pippitt K, Li M, Gurgle HE. Diabetes mellitus: screening and diagnosis. Am Fam Physician. Diabetes Prevention Program Research Group.
Long-term effects of lifestyle intervention or metformin on diabetes development and micro-vascular complications over year follow-up: the Diabetes Prevention Program Outcomes Study. Lancet Diabetes Endocrinol. National Diabetes Prevention Program. Prevent T2 curricula and handouts.
Accessed April 17, Knowler WC, Fowler SE, Hamman RF, et al. Li G, Zhang P, Wang J, et al. The long-term effect of lifestyle interventions to prevent diabetes in the China Da Qing Diabetes Prevention Study: a year follow-up study.
Lindström J, Ilanne-Parikka P, Peltonen M, et al. Sustained reduction in the incidence of type 2 diabetes by lifestyle intervention: follow-up of the Finnish Diabetes Prevention Study.
Look AHEAD Research Group. Eight-year weight losses with an intensive lifestyle intervention: the look AHEAD study. Obesity Silver Spring. Gregg EW, Chen H, Wagenknecht LE, et al. Association of an intensive lifestyle intervention with remission of type 2 diabetes.
Colberg SR, Sigal RJ, Fernhall B, et al. Exercise and type 2 diabetes: the American College of Sports Medicine and the American Diabetes Association: joint position statement executive summary.
Lifestyle intervention materials. Diabetes Prevention Program DPP Research Group. The Diabetes Prevention Program DPP : description of lifestyle intervention.
Garber AJ, Abrahamson MJ, Barzilay JI, et al. Consensus statement by the American Association of Clinical Endocrinologists and American College of Endocrinology on the comprehensive type 2 diabetes management algorithm— executive summary. Endocr Pract. Preventive Services Task Force. Final recommendation statement: healthful diet and physical activity for cardiovascular disease prevention in adults with cardiovascular risk factors: behavioral counseling.
August Accessed November 7, Mason P, Butler CC. Health Behavior Change: A Guide For Practitioners. Edinburgh, United Kingdom: Churchill Livingstone Elsevier; Prochaska JO, Norcross JC.
Systems Of Psychotherapy: A Transtheoretical Analysis. Stamford, Conn. Keller VF, White MK. Choices and changes: a new model for influencing patient health behavior. J Clin Outcomes Manage. Wadden TA, West DS, Delahanty L, et al. The Look AHEAD study: a description of the lifestyle intervention and the evidence supporting it [published correction appears in Obesity Silver Spring.
Doran GT. There's a S. way to write management's goals and objectives. Manage Rev. Wadden TA, Webb VL, Moran CH, Bailer BA. Lifestyle modification for obesity: new developments in diet, physical activity, and behavior therapy.
Dutton GR, Lewis CE. The Look AHEAD Trial: implications for lifestyle intervention in type 2 diabetes mellitus. Prog Cardiovasc Dis. Siopis G, Chey T, Allman-Farinelli M. A systematic review and meta-analysis of interventions for weight management using text messaging. J Hum Nutr Diet.
Connelly J, Kirk A, Masthoff J, MacRury S. Other benefits include slowing the decline in mobility among overweight patients with diabetes Increased physical activity soccer training has also been shown to be beneficial for improving overall fitness in Latino men with obesity, demonstrating feasible methods to increase physical activity in an often hard-to-engage population Physical activity and exercise should be recommended and prescribed to all individuals who are at risk for or with diabetes as part of management of glycemia and overall health.
Specific recommendations and precautions will vary by the type of diabetes, age, activity done, and presence of diabetes-related health complications. Recommendations should be tailored to meet the specific needs of each individual All children, including children with diabetes or prediabetes, should be encouraged to engage in regular physical activity.
Children should engage in at least 60 min of moderate to vigorous aerobic activity every day, with muscle- and bone-strengthening activities at least 3 days per week In general, youth with type 1 diabetes benefit from being physically active, and an active lifestyle should be recommended to all Youth with type 1 diabetes who engage in more physical activity may have better health outcomes and health-related quality of life , People with diabetes should perform aerobic and resistance exercise regularly Daily exercise, or at least not allowing more than 2 days to elapse between exercise sessions, is recommended to decrease insulin resistance, regardless of diabetes type , A study in adults with type 1 diabetes found a dose-response inverse relationship between self-reported bouts of physical activity per week and A1C, BMI, hypertension, dyslipidemia, and diabetes-related complications such as hypoglycemia, diabetic ketoacidosis, retinopathy, and microalbuminuria Many adults, including most with type 2 diabetes, may be unable or unwilling to participate in such intense exercise and should engage in moderate exercise for the recommended duration.
Although heavier resistance training with free weights and weight machines may improve glycemic control and strength , resistance training of any intensity is recommended to improve strength, balance, and the ability to engage in activities of daily living throughout the life span. Providers and staff should help patients set stepwise goals toward meeting the recommended exercise targets.
As individuals intensify their exercise program, medical monitoring may be indicated to ensure safety and evaluate the effects on glucose management. See the section physical activity and glycemic control below. Recent evidence supports that all individuals, including those with diabetes, should be encouraged to reduce the amount of time spent being sedentary—waking behaviors with low energy expenditure e.
Participating in leisure-time activity and avoiding extended sedentary periods may help prevent type 2 diabetes for those at risk , and may also aid in glycemic control for those with diabetes.
A systematic review and meta-analysis found higher frequency of regular leisure-time physical activity was more effective in reducing A1C levels A wide range of activities, including yoga, tai chi, and other types, can have significant impacts on A1C, flexibility, muscle strength, and balance , — Flexibility and balance exercises may be particularly important in older adults with diabetes to maintain range of motion, strength, and balance Clinical trials have provided strong evidence for the A1C-lowering value of resistance training in older adults with type 2 diabetes and for an additive benefit of combined aerobic and resistance exercise in adults with type 2 diabetes If not contraindicated, patients with type 2 diabetes should be encouraged to do at least two weekly sessions of resistance exercise exercise with free weights or weight machines , with each session consisting of at least one set group of consecutive repetitive exercise motions of five or more different resistance exercises involving the large muscle groups For type 1 diabetes, although exercise in general is associated with improvement in disease status, care needs to be taken in titrating exercise with respect to glycemic management.
Each individual with type 1 diabetes has a variable glycemic response to exercise. This variability should be taken into consideration when recommending the type and duration of exercise for a given individual Women with preexisting diabetes, particularly type 2 diabetes, and those at risk for or presenting with gestational diabetes mellitus should be advised to engage in regular moderate physical activity prior to and during their pregnancies as tolerated However, providers should perform a careful history, assess cardiovascular risk factors, and be aware of the atypical presentation of coronary artery disease, such as recent patient-reported or tested decrease in exercise tolerance, in patients with diabetes.
Certainly, high-risk patients should be encouraged to start with short periods of low-intensity exercise and slowly increase the intensity and duration as tolerated. Providers should assess patients for conditions that might contraindicate certain types of exercise or predispose to injury, such as uncontrolled hypertension, untreated proliferative retinopathy, autonomic neuropathy, peripheral neuropathy, and a history of foot ulcers or Charcot foot.
Those with complications may need a more thorough evaluation prior to starting an exercise program , In some patients, hypoglycemia after exercise may occur and last for several hours due to increased insulin sensitivity.
Hypoglycemia is less common in patients with diabetes who are not treated with insulin or insulin secretagogues, and no routine preventive measures for hypoglycemia are usually advised in these cases. Intense activities may actually raise blood glucose levels instead of lowering them, especially if pre-exercise glucose levels are elevated Because of the variation in glycemic response to exercise bouts, patients need to be educated to check blood glucose levels before and after periods of exercise and about the potential prolonged effects depending on intensity and duration see the section diabetes self-management education and support above.
If proliferative diabetic retinopathy or severe nonproliferative diabetic retinopathy is present, then vigorous-intensity aerobic or resistance exercise may be contraindicated because of the risk of triggering vitreous hemorrhage or retinal detachment Consultation with an ophthalmologist prior to engaging in an intense exercise regimen may be appropriate.
Decreased pain sensation and a higher pain threshold in the extremities can result in an increased risk of skin breakdown, infection, and Charcot joint destruction with some forms of exercise.
Therefore, a thorough assessment should be done to ensure that neuropathy does not alter kinesthetic or proprioceptive sensation during physical activity, particularly in those with more severe neuropathy.
Studies have shown that moderate-intensity walking may not lead to an increased risk of foot ulcers or reulceration in those with peripheral neuropathy who use proper footwear All individuals with peripheral neuropathy should wear proper footwear and examine their feet daily to detect lesions early.
Anyone with a foot injury or open sore should be restricted to non—weight-bearing activities. Autonomic neuropathy can increase the risk of exercise-induced injury or adverse events through decreased cardiac responsiveness to exercise, postural hypotension, impaired thermoregulation, impaired night vision due to impaired papillary reaction, and greater susceptibility to hypoglycemia Cardiovascular autonomic neuropathy is also an independent risk factor for cardiovascular death and silent myocardial ischemia Therefore, individuals with diabetic autonomic neuropathy should undergo cardiac investigation before beginning physical activity more intense than that to which they are accustomed.
Physical activity can acutely increase urinary albumin excretion. However, there is no evidence that vigorous-intensity exercise accelerates the rate of progression of DKD, and there appears to be no need for specific exercise restrictions for people with DKD in general Results from epidemiologic, case-control, and cohort studies provide convincing evidence to support the causal link between cigarette smoking and health risks Recent data show tobacco use is higher among adults with chronic conditions as well as in adolescents and young adults with diabetes People with diabetes who smoke and people with diabetes exposed to second-hand smoke have a heightened risk of CVD, premature death, microvascular complications, and worse glycemic control when compared with those who do not smoke — Smoking may have a role in the development of type 2 diabetes — The routine and thorough assessment of tobacco use is essential to prevent smoking or encourage cessation.
Numerous large randomized clinical trials have demonstrated the efficacy and cost-effectiveness of brief counseling in smoking cessation, including the use of telephone quit lines, in reducing tobacco use.
Pharmacologic therapy to assist with smoking cessation in people with diabetes has been shown to be effective , and for the patient motivated to quit, the addition of pharmacologic therapy to counseling is more effective than either treatment alone Special considerations should include assessment of level of nicotine dependence, which is associated with difficulty in quitting and relapse Although some people may gain weight in the period shortly after smoking cessation , recent research has demonstrated that this weight gain does not diminish the substantial CVD benefit realized from smoking cessation One study in people who smoke who had newly diagnosed type 2 diabetes found that smoking cessation was associated with amelioration of metabolic parameters and reduced blood pressure and albuminuria at 1 year In recent years, e-cigarettes have gained public awareness and popularity because of perceptions that e-cigarette use is less harmful than regular cigarette smoking , However, in light of recent Centers for Disease Control and Prevention evidence of deaths related to e-cigarette use, no individuals should be advised to use e-cigarettes, either as a way to stop smoking tobacco or as a recreational drug.
Diabetes education programs offer potential to systematically reach and engage individuals with diabetes in smoking cessation efforts.
Including caregivers and family members in this assessment is recommended. B Monitoring of cognitive capacity, i. Complex environmental, social, behavioral, and emotional factors, known as psychosocial factors, influence living with diabetes, both type 1 and type 2, and achieving satisfactory medical outcomes and psychological well-being.
Thus, individuals with diabetes and their families are challenged with complex, multifaceted issues when integrating diabetes care into daily life Emotional well-being is an important part of diabetes care and self-management. There are opportunities for the clinician to routinely assess psychosocial status in a timely and efficient manner for referral to appropriate services , A systematic review and meta-analysis showed that psychosocial interventions modestly but significantly improved A1C standardized mean difference —0.
There was a limited association between the effects on A1C and mental health, and no intervention characteristics predicted benefit on both outcomes.
However, cost analyses have shown that behavioral health interventions are both effective and cost-efficient approaches to the prevention of diabetes Key opportunities for psychosocial screening occur at diabetes diagnosis, during regularly scheduled management visits, during hospitalizations, with new onset of complications, during significant transitions in care such as from pediatric to adult care teams , or when problems with achieving A1C goals, quality of life, or self-management are identified 2.
Patients are likely to exhibit psychological vulnerability at diagnosis, when their medical status changes e. Thus, screening for social determinants of health e.
Providers should also ask whether there are new or different barriers to treatment and self-management, such as feeling overwhelmed or stressed by having diabetes see the section diabetes distress below , changes in finances, or competing medical demands e.
In circumstances where individuals other than the patient are significantly involved in diabetes management, these issues should be explored with nonmedical care providers Standardized and validated tools for psychosocial monitoring and assessment can also be used by providers 1 , with positive findings leading to referral to a mental health provider specializing in diabetes for comprehensive evaluation, diagnosis, and treatment.
Diabetes distress is very common and is distinct from other psychological disorders , , The constant behavioral demands of diabetes self-management medication dosing, frequency, and titration; monitoring of blood glucose, food intake, eating patterns, and physical activity and the potential or actuality of disease progression are directly associated with reports of diabetes distress High levels of diabetes distress significantly impact medication-taking behaviors and are linked to higher A1C, lower self-efficacy, and poorer dietary and exercise behaviors 5 , , DSMES has been shown to reduce diabetes distress 5.
It may be helpful to provide counseling regarding expected diabetes-related versus generalized psychological distress, both at diagnosis and when disease state or treatment changes occur An RCT tested the effects of participation in a standardized 8-week mindful self-compassion program versus a control group among patients with type 1 and type 2 diabetes.
Mindful self-compassion training increased self-compassion, reduced depression and diabetes distress, and improved A1C in the intervention group An RCT of cognitive behavioral and social problem-solving approaches compared with diabetes education in teens aged 14—18 years showed that diabetes distress and depressive symptoms were significantly reduced for up to 3 years postintervention.
Neither glycemic control nor self-management behaviors were improved over time. These recent studies support that a combination of approaches is needed to address distress, depression, and metabolic status.
Diabetes distress should be routinely monitored using person-based diabetes-specific validated measures 1. If diabetes distress is identified, the person should be referred for specific diabetes education to address areas of diabetes self-care causing the patient distress and impacting clinical management.
Diabetes distress is associated with anxiety, depression, and reduced health-related quality of life People whose self-care remains impaired after tailored diabetes education should be referred by their care team to a behavioral health provider for evaluation and treatment.
Other psychosocial issues known to affect self-management and health outcomes include attitudes about the illness, expectations for medical management and outcomes, available resources financial, social, and emotional , and psychiatric history.
Indications for referral to a mental health specialist familiar with diabetes management may include positive screening for overall stress related to work-life balance, diabetes distress, diabetes management difficulties, depression, anxiety, disordered eating, and cognitive dysfunction see Table 5.
It is preferable to incorporate psychosocial assessment and treatment into routine care rather than waiting for a specific problem or deterioration in metabolic or psychological status to occur 34 , Providers should identify behavioral and mental health providers, ideally those who are knowledgeable about diabetes treatment and the psychosocial aspects of diabetes, to whom they can refer patients.
The ADA provides a list of mental health providers who have received additional education in diabetes at the ADA Mental Health Provider Directory professional. Ideally, psychosocial care providers should be embedded in diabetes care settings.
Although the provider may not feel qualified to treat psychological problems , optimizing the patient-provider relationship as a foundation may increase the likelihood of the patient accepting referral for other services. Collaborative care interventions and a team approach have demonstrated efficacy in diabetes self-management, outcomes of depression, and psychosocial functioning 5 , 6.
Situations that warrant referral of a person with diabetes to a mental health provider for evaluation and treatment. Clinically significant psychopathologic diagnoses are considerably more prevalent in people with diabetes than in those without , Inclusion of caregivers and family members in this assessment is recommended.
Diabetes distress is addressed as an independent condition see the section diabetes distress above , as this state is very common and expected and is distinct from the psychological disorders discussed below 1. Refer for treatment if anxiety is present. Anxiety symptoms and diagnosable disorders e.
The Behavioral Risk Factor Surveillance System BRFSS estimated the lifetime prevalence of generalized anxiety disorder to be Common diabetes-specific concerns include fears related to hypoglycemia , , not meeting blood glucose targets , and insulin injections or infusion Onset of complications presents another critical point in the disease course when anxiety can occur 1.
People with diabetes who exhibit excessive diabetes self-management behaviors well beyond what is prescribed or needed to achieve glycemic targets may be experiencing symptoms of obsessive-compulsive disorder General anxiety is a predictor of injection-related anxiety and associated with fear of hypoglycemia , Fear of hypoglycemia and hypoglycemia unawareness often co-occur.
Interventions aimed at treating one often benefit both Fear of hypoglycemia may explain avoidance of behaviors associated with lowering glucose such as increasing insulin doses or frequency of monitoring.
If fear of hypoglycemia is identified and a person does not have symptoms of hypoglycemia, a structured program of blood glucose awareness training delivered in routine clinical practice can improve A1C, reduce the rate of severe hypoglycemia, and restore hypoglycemia awareness , If not available within the practice setting, a structured program targeting both fear of hypoglycemia and unawareness should be sought out and implemented by a qualified behavioral practitioner , — History of depression, current depression, and antidepressant medication use are risk factors for the development of type 2 diabetes, especially if the individual has other risk factors such as obesity and family history of type 2 diabetes — Elevated depressive symptoms and depressive disorders affect one in four patients with type 1 or type 2 diabetes Thus, routine screening for depressive symptoms is indicated in this high-risk population, including people with type 1 or type 2 diabetes, gestational diabetes mellitus, and postpartum diabetes.
Regardless of diabetes type, women have significantly higher rates of depression than men Routine monitoring with age-appropriate validated measures 1 can help to identify if referral is warranted Adult patients with a history of depressive symptoms need ongoing monitoring of depression recurrence within the context of routine care Integrating mental and physical health care can improve outcomes.
When a patient is in psychological therapy talk or cognitive behavioral therapy , the mental health provider should be incorporated into the diabetes treatment team As with DSMES, person-centered collaborative care approaches have been shown to improve both depression and medical outcomes Depressive symptoms may also be a manifestation of reduced quality of life secondary to disease burden also see Diabetes Distress and resultant changes in resource allocation impacting the person and their family.
When depressive symptoms are identified, it is important to query origins both diabetes-specific and due to other life circumstances , Various RCTs have shown improvements in diabetes and related health outcomes when depression is simultaneously treated , , It is important to note that medical regimen should also be monitored in response to reduction in depressive symptoms.
People may agree to or adopt previously refused treatment strategies improving ability to follow recommended treatment behaviors , which may include increased physical activity and intensification of regimen behaviors and monitoring, resulting in changed glucose profiles.
Estimated prevalence of disordered eating behavior and diagnosable eating disorders in people with diabetes varies — For people with type 1 diabetes, insulin omission causing glycosuria in order to lose weight is the most commonly reported disordered eating behavior , ; in people with type 2 diabetes, bingeing excessive food intake with an accompanying sense of loss of control is most commonly reported.
For people with type 2 diabetes treated with insulin, intentional omission is also frequently reported People with diabetes and diagnosable eating disorders have high rates of comorbid psychiatric disorders People with type 1 diabetes and eating disorders have high rates of diabetes distress and fear of hypoglycemia When evaluating symptoms of disordered or disrupted eating when the individual exhibits eating behaviors that appear maladaptive but are not volitional, such as bingeing caused by loss of satiety cues , etiology and motivation for the behavior should be evaluated , Mixed intervention results point to the need for treatment of eating disorders and disordered eating behavior in the context of the disease and its treatment.
More rigorous methods to identify underlying mechanisms of action that drive change in eating and treatment behaviors, as well as associated mental distress, are needed Adjunctive medication such as glucagon-like peptide 1 receptor agonists may help individuals not only to meet glycemic targets but also to regulate hunger and food intake, thus having the potential to reduce uncontrollable hunger and bulimic symptoms.
Caution should be taken in labeling individuals with diabetes as having a diagnosable psychiatric disorder, i. Studies of individuals with serious mental illness, particularly schizophrenia and other thought disorders, show significantly increased rates of type 2 diabetes People with schizophrenia should be monitored for type 2 diabetes because of the known comorbidity.
Disordered thinking and judgment can be expected to make it difficult to engage in behavior that reduces risk factors for type 2 diabetes, such as restrained eating for weight management. Further, people with serious mental health disorders and diabetes frequently experience moderate psychological distress, suggesting pervasive intrusion of mental health issues into daily functioning Coordinated management of diabetes or prediabetes and serious mental illness is recommended to achieve diabetes treatment targets.
In addition, those taking second-generation atypical antipsychotics, such as olanzapine, require greater monitoring because of an increase in risk of type 2 diabetes associated with this medication — Because of this increased risk, people should be screened for prediabetes or diabetes 4 months after medication initiation and at least annually thereafter.
Serious mental illness is often associated with the inability to evaluate and utilize information to make judgments about treatment options. When a person has an established diagnosis of a mental illness that impacts judgment, activities of daily living, and ability to establish a collaborative relationship with care providers, it is wise to include a nonmedical caretaker in decision-making regarding the medical regimen.
Cognitive capacity is generally defined as attention, memory, logic and reasoning, and auditory and visual processing, all of which are involved in diabetes self-management behavior Having diabetes over decades—type 1 and type 2—has been shown to be associated with cognitive decline — Declines have been shown to impact executive function and information processing speed; they are not consistent between people, and evidence is lacking regarding a known course of decline Diagnosis of dementia is also more prevalent in the population of individuals with diabetes, both type 1 and type 2 Thus, monitoring of cognitive capacity of individuals is recommended, particularly regarding their ability to self-monitor and make judgements about their symptoms, physical status, and needed alterations to their self-management behaviors, all of which are mediated by executive function As with other disorders affecting mental capacity e.
When this ability is shown to be altered, declining, or absent, a lay care provider should be introduced into the care team who serves in the capacities of day-to-day monitoring as well as a liaison with the rest of the care team 1.
Cognitive capacity also contributes to ability to benefit from diabetes education and may indicate the need for alternative teaching approaches as well as remote monitoring. Youth will need second-party monitoring e. Episodes of severe hypoglycemia are independently associated with decline, as well as the more immediate symptoms of mental confusion Early-onset type 1 diabetes has been shown to be associated with potential deficits in intellectual abilities, especially in the context of repeated episodes of severe hypoglycemia If cognitive capacity to carry out self-maintenance behaviors is questioned, an age-appropriate test of cognitive capacity is recommended 1.
Cognitive capacity should be evaluated in the context of the age of the person, for example, in very young children who are not expected to manage their disease independently and in older adults who may need active monitoring of regimen behaviors. Suggested citation: American Diabetes Association Professional Practice Committee.
Facilitating behavior change and well-being to improve health outcomes: Standards of Medical Care in Diabetes— Diabetes Care ;45 Suppl. Sign In or Create an Account. Search Dropdown Menu. header search search input Search input auto suggest.
filter your search All Content All Journals Diabetes Care. Advanced Search. User Tools Dropdown. Sign In. Skip Nav Destination Close navigation menu Article navigation.
Previous Article Next Article. Diabetes Self-Management Education and Support. Medical Nutrition Therapy.
Physical Activity. Smoking Cessation: Tobacco and e-Cigarettes. Psychosocial Issues. Article Navigation. Standards of Care December 16 Facilitating Behavior Change and Well-being to Improve Health Outcomes: Standards of Medical Care in Diabetes— American Diabetes Association Professional Practice Committee American Diabetes Association Professional Practice Committee.
This Site. Google Scholar. Get Permissions. toolbar search Search Dropdown Menu. toolbar search search input Search input auto suggest. Table 5. Effectiveness of nutrition therapy 5.
E Energy balance 5. A Eating patterns and macronutrient distribution 5. Eating plans should emphasize nonstarchy vegetables, fruits, and whole grains, as well as dairy products, with minimal added sugars.
Therefore, carbohydrate sources high in protein should be avoided when trying to treat or prevent hypoglycemia. B Dietary fat 5. B Micronutrients and herbal supplements 5. The importance of glucose monitoring after drinking alcoholic beverages to reduce hypoglycemia risk should be emphasized.
B Sodium 5. B Nonnutritive sweeteners 5. Overall, people are encouraged to decrease both sweetened and nonnutritive-sweetened beverages, with an emphasis on water intake. View Large. To promote and support healthful eating patterns, emphasizing a variety of nutrient-dense foods in appropriate portion sizes, to improve overall health and: achieve and maintain body weight goals attain individualized glycemic, blood pressure, and lipid goals delay or prevent the complications of diabetes To address individual nutrition needs based on personal and cultural preferences, health literacy and numeracy, access to healthful foods, willingness and ability to make behavioral changes, and existing barriers to change To maintain the pleasure of eating by providing nonjudgmental messages about food choices while limiting food choices only when indicated by scientific evidence To provide an individual with diabetes the practical tools for developing healthy eating patterns rather than focusing on individual macronutrients, micronutrients, or single foods.
Psychosocial care for people with diabetes: a position statement of the American Diabetes Association. Search ADS. Collaborative care for patients with depression and diabetes mellitus: a systematic review and meta-analysis.
Problem solving in diabetes self-management: a model of chronic illness self-management behavior. A framework for optimizing technology-enabled diabetes and cardiometabolic care and education: the role of the diabetes care and education specialist.
Taxonomy of the burden of treatment: a multi-country web-based qualitative study of patients with chronic conditions. Effect of DECIDE Decision-making Education for Choices In Diabetes Everyday program delivery modalities on clinical and behavioral outcomes in urban African Americans with type 2 diabetes: a randomized trial.
Diabetes self-management education improves quality of care and clinical outcomes determined by a diabetes bundle measure. Twenty-first century behavioral medicine: a context for empowering clinicians and patients with diabetes: a consensus report.
Self-management education for adults with type 2 diabetes: a meta-analysis of the effect on glycemic control. Evaluation of a behavior support intervention for patients with poorly controlled diabetes. Structured type 1 diabetes education delivered within routine care: impact on glycemic control and diabetes-specific quality of life.
Diabetes self-management education for adults with type 2 diabetes mellitus: a systematic review of the effect on glycemic control. Diabetes self-management education and medical nutrition therapy: a multisite study documenting the efficacy of registered dietitian nutritionist interventions in the management of glycemic control and diabetic dyslipidemia through retrospective chart review.
However, this was not a universal sentiment, and some participants felt uncomfortable with and disconnected from the blog Table 3 ; 2c,ii. Participants perceived that the website was accurate, comprehensive Table 3 ; 3a , and easy to navigate Table 3 ; 3b.
Deeper exploration of the data regarding patterns of use and website features uncovered factors that might account for these quantitative findings. For example, rather than returning to the site to revisit and review items, some participants reported that they printed items of interest from the website and subsequently referred to these paper copies Table 3 ; 4a.
The use of reminder emails also had an effect. Participants reported that these emails not only prompted them to return to and log into the website, but also encouraged them in their own self-management Table 3 ; 4b. Although she did not subsequently login to the website to record these behaviours, she did continue to record them on paper.
We found that a self-management website for patients with type 2 diabetes led to no improvement in self-efficacy, diabetes distress, or clinical outcomes over the study period. However, there was an improvement in self-care a secondary outcome , and the group that used the website experienced significantly lower diabetes distress than those who did not use it.
Despite a user-centred design process and an increase in the frequency of blog posting from weekly to twice weekly, use of the website as ascertained by login records was limited. Our interviews revealed that both patient-related factors e. competing health and life concerns, a sense of futility and website-related factors e.
requirement for login, limited computer or internet access limited use of the website. These qualitative findings have confirmed the importance of website features such as the reliability and authoritativeness of information [ 47 ], as well as the use of blogs [ 15 ] and reminders [ 48 ] for continued engagement of users.
Our data also suggest that mobile devices are a potential avenue through which to improve accessibility and use of a self-management site. However, as with web-based technology, a systematic approach to development, testing, implementation, and evaluation of mobile health technology is warranted.
Although such technologies are proliferating, with over applications related to diabetes alone, their usability and clinical effectiveness are variable [ 53 ], and concerns exist regarding their effectiveness and safety, as well as the security of personal health information [ 54 ].
Our findings regarding user engagement with web-based technology echo those for mobile technology: an evaluation of 10 mobile diabetes applications emphasized the importance of user-centred design, an engaging interface, and context-driven use [ 55 ].
Competing health concerns were identified as a barrier to web-based self-management. depression , which in turn directly affects self-management ability and competes for time and attention [ 56 ]. For example, patients with a greater number of comorbidities placed a lower priority on diabetes and had worse diabetes self-management ability [ 57 ].
Future interventions should consider strategies, such as shared decision-making and priority-setting, to empower patients with multiple comorbidities to optimize their self-care [ 58 ]. For example, a patient may identify mood management as a priority, which is key to subsequent self-care.
Finally, our results may be extrapolated to other chronic diseases. In particular, our finding of the need for tailored content and peer support, balanced with concerns regarding information reliability and confidentiality, is applicable to other strategies for managing chronic disease.
For example, a systematic review of the benefits and limitations of social media in the context of chronic disease identified benefits increased interaction and social support, tailored and accessible information and limitations quality concerns and lack of reliability, confidentiality, and privacy [ 59 ] to those we identified.
Similarly, our finding of a reduction in diabetes distress in conjunction with no improvements in clinical outcomes echoes findings from intervention strategies targeting other chronic diseases.
For example, another systematic review examining the effect of social media on psychological and physical outcomes in chronic disease found a relatively large body of evidence demonstrating psychological benefit 19 identified studies but limited evidence for physical outcomes 4 identified studies [ 60 ].
This study was limited by its non-randomized design. However, we employed a repeated-measures design that permitted reliable assessment of baseline self-efficacy. Although our primary outcome self-efficacy was a non-clinical outcome, it is a validated predictor of patient behaviour change and clinical outcomes [ 18 ],[ 20 ],[ 24 ],[ 25 ].
The infrequency of website use likely limited the effect of this intervention, but we obtained valuable insights regarding mediators of website use through our individual interviews.
The qualitative evaluation was conducted by individuals who were also involved in developing the intervention, which created a potential for bias; however, we guarded against this bias by including individuals who were not involved in designing the website as members of the qualitative analytic team and by having three coders.
As such, we were able to obtain and report critical feedback that participants openly shared. Study strengths include the use of multiple repeated measures, the use of validated outcomes, dual coding of all transcripts, and triangulation of the qualitative findings with the quantitative results [ 42 ],[ 44 ],[ 46 ].
Increasing use of the World Wide Web by consumers for health information and ongoing revolutions in social media are strong indicators that consumers are welcoming and demanding a new era of technology in health care.
However, full potential of this technology is hindered by limited uptake and high attrition rates. Our research findings have shed light on these limitations by identifying characteristics associated with website use and attrition and suggesting strategies to reduce website attrition as a way to potentially optimize clinical outcomes.
Centers for Disease Control and Prevention: Diabetes Report Card Atlanta, GA: Centers for Disease Control and Prevention, US Department of Health and Human Services; American Diabetes Association: Standards of medical care in diabetes Diabetes Care.
Article Google Scholar. Haas L, Maryniuk M, Beck J, Cox CE, Duker P, Edwards L, Fisher EB, Hanson L, Kent D, Kolb L, McLaughlin S, Orzeck E, Piette JD, Rhinehart AS, Rothman R, Sklaroff S, Tomky D, Youssef G: National standards for diabetes self-management education and supportdiabetes.
Selby JV, Beal AC, Frank L: The Patient-Centered Outcomes Research Institute PCORI national priorities for research and initial research agenda. J Am Med Assoc. Article CAS Google Scholar. Cochrane J, Conn VS: Meta-analysis of quality of life outcomes following self-management training.
Diabetes Educ. Minet L, Møller S, Vach W, Wagner L, Henriksen JE: Mediating the effect of self-care management intervention in type 2 diabetes: a meta-analysis of 47 randomised controlled trials. Patient Educ Couns. Article PubMed Google Scholar. Ruppert K, Uhler A, Siminerio L: Examining patient risk factors, comorbid conditions, participation, and physician referrals to a rural diabetes self-management education program.
Shaw K, Killeen M, Sullivan E, Bowman P: Disparities in diabetes self-management education for uninsured and underinsured adults.
Shekelle PG, Morton SC, Keeler EB: Costs and Benefits of Health Information Technology. Google Scholar. Yu CH, Bahniwal R, Laupacis A, Leung E, Orr MS, Straus SE: Systematic review and evaluation of web-accessible tools for management of diabetes and related cardiovascular risk factors by patients and healthcare providers.
J Am Med Inform Assoc. Article PubMed PubMed Central Google Scholar. Bull SS, Gaglio B, McKay HG, Glasgow RE: Harnessing the potential of the internet to promote chronic illness self-management: diabetes as an example of how well we are doing. Chronic Illness. van Vugt M, de Wit M, Cleijne WH, Snoek FJ: Use of behavioral change techniques in web-based self-management programs for type 2 diabetes patients: systematic review.
J Med Internet Res. Seidman JJ, Steinwachs D, Rubin HR: Design and testing of a tool for evaluating the quality of diabetes consumer-information Web sites. Shrank WH, Patrick AR, Brookhart MA: Healthy user and related biases in observational studies of preventive interventions: a primer for physicians.
J Gen Intern Med. Yu CH, Parsons J, Hall S, Newton D, Jovicic A, Lottridge D, Shah BR, Straus SE: User-centered design of a web-based self-management site for individuals with type 2 diabetes — providing a sense of control and community. BMC Med Inform Decis Mak. Yu C, Parsons J, Mamdani M, Lebovic G, Shah BR, Bhattacharyya O, Laupacis A, Straus SE: Designing and evaluating a web-based selfmanagement site for patients with type 2 diabetes - systematic website development and study protocol.
Bandura A: Self-Efficacy: the Exercise of Control. Freeman, New York. Article CAS PubMed Google Scholar. Reichard P, Toomingas B, Rosenqvist U: Changes in conceptions and attitudes during five years of intensified conventional insulin treatment in the stockholm diabetes intervention study SDIS.
Anderson RM, Funnell MM, Butler PM, Arnold MS, Fitzgerald JT, Feste CC: Patient empowerment: results of a randomized controlled trial. Trief PM, Teresi JA, Eimicke JP, Shea S, Weinstock RS: Improvement in diabetes self-efficacy and glycaemic control using telemedicine in a sample of older, ethnically diverse individuals who have diabetes: the IDEATel project.
Age Ageing. Aljasem LI, Peyrot M, Wissow L, Rubin RR: The impact of barriers and self-efficacy on self-care behaviors in type 2 diabetes. Grossman HY, Brink S, Hauser S: Self-efficacy in adolescent girls and boys with insulin-dependent diabetes mellitus.
Nakahara R, Yoshiuchi K, Kumano H, Hara Y, Suematsu H, Kuboki T: Prospective study on influence of psychosocial factors on glycemic control in Japanese patients with type 2 diabetes. Toobert DJ, Hampson SE, Glasgow RE: The summary of diabetes self-care activities measure: results from 7 studies and a revised scale.
Polonsky WH, Fisher L, Earles J, Dudl RJ, Lees J, Mullan J, Jackson RA: Assessing psychosocial distress in diabetes: development of the Diabetes Distress Scale.
Chew LD, Bradley KA, Boyko EJ: Brief questions to identify patients with inadequate health literacy. Fam Med. PubMed Google Scholar. Chew LD, Griffin JM, Partin MR: Validation of screening questions for limited health literacy in a large VA outpatient population. Zar JH: Biostatistical Analysis.
J, Prentice Hall. Liu G, Liang KY: Sample size calculations for studies with correlated observations. Norris SL, Engelgau MM, Narayan KM: Effectiveness of self-management training in type 2 diabetes: a systematic review of randomized controlled trials. Diggle P, Heagerty P, Liang KY, Zeger S: Analysis of Longitudinal Data.
Verbeke G, Molenberghs G: Linear Mixed Models for Longitudinal Data. Laird NM, Donnelly C, Ware JH: Review papers: longitudinal studies with continuous responses. Stat Methods Med Res.
Cnaan A, Laird NM, Slasor P: Tutorial in biostatistics: using the general linear mixed model to analyse unbalanced repeated measures and longitudinal data.
Stat Med. Sherrill DL, Holberg CJ, Enright PL, Lebowitz MD, Burrows B: Longitudinal analysis of the effects of smoking onset and cessation on pulmonary function.
Am J Respir Crit Care Med. Figaro MK, Elasy T, BeLue R: Exploring socioeconomic variations in diabetes control strategies: impact of outcome expectations. J Natl Med Assoc.
Osborn CY, Cavanaugh K, Wallston KA, Rothman RL: Self-efficacy links health literacy and numeracy to glycemic control. J Health Commun. Harrell FE, Lee KL, Mark DB: Multivariable prognostic models: issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors.
R Team: R: A Language and Environment for Statistical Computing. Kuzel AJ: Sampling in Qualitative Inquiry. Doing Qualitative Research. Edited by: Crabtree BF, Miller W. Poland BP: Transcription quality as an aspect of rigor in qualitative research. Qual Inq. Kvale S: InterViews: An Introduction to Qualitative Research Interviewing.
Pope C, Ziebland S, Mays N: Qualitative research in health care: analysing qualitative data. Article CAS PubMed PubMed Central Google Scholar.
Bryman A: Quantity and Quality. Social Research. Lemire M, Paré G, Sicotte C, Harvey C: Determinants of internet use as a preferred source of information on personal health.
Int J Med Inform. Nijland N, van Gemert-Pijnen JE, Kelders SM, Brandenburg BJ, Seydel ER: Factors influencing the use of a web-based application for supporting the self-care of patients with type 2 diabetes: a longitudinal study. Gruzd A, Black FA, Le Yen TN, Amos K: Investigating biomedical research literature in the blogosphere: a case study of diabetes and glycated hemoglobin HbA1c.
J Med Libr Assoc. Pal K, Eastwood SV, Michie S, Farmer AJ, Barnard ML, Peacock R, Wood B, Inniss JD, Murray E: Computer-based diabetes self-management interventions for adults with type 2 diabetes mellitus. Cochrane Database Syst Rev , 3. Manhattan Research: U. mobile health audience jumps to 95 million adults.
Cybercitizen Health® U. Demidowich AP, Lu K, Tamler R, Bloomgarden Z: An evaluation of diabetes self-management applications for Android smartphones. J Telemed Telecare. Eng DS: The promise and peril of mobile health applications for diabetes and endocrinology.
Pediatr Diabetes. Årsand E, Frøisland DH, Skrøvseth SO, Chomutare T, Tatara N, Hartvigsen G, Tufano JT: Mobile health applications to assist patients with diabetes: lessons learned and design implications. J Diabetes Sci Technol. Ciechanowski PS, Katon WJ, Russo JE: Depression and diabetes: impact of depressive symptoms on adherence, function, and costs.
Arch Intern Med.
Margaret A. PowersJoan Sel-fcare. BardsleyMarjorie Selr-careMartha M. FunnellDixie HarmsAmy Hess-FischlBeulette HooksDiana IsaacsEllen D. MandelMelinda D.
Ich denke, dass es die ausgezeichnete Idee ist.
Welche talentvolle Mitteilung
Ich tue Abbitte, dass ich mich einmische, aber mir ist es etwas mehr die Informationen notwendig.
Ich entschuldige mich, aber meiner Meinung nach lassen Sie den Fehler zu. Geben Sie wir werden es besprechen. Schreiben Sie mir in PM, wir werden reden.
Welche Wörter... Toll, die bemerkenswerte Phrase