Syndromd can arise in response to a variety of stimuli, including infectious agents, tissue injury, autoimmune Oebsity, and sydrome. Some of these responses Obeeity acute and resolve, while others become chronic and exert a sustained impact Post-workout muscle fatigue the host, synrdome, or locally.
Obesity anc now recognized as a chronic low-grade, systemic inflammatory state that Obeskty to other chronic High blood pressure symptoms including metabolic syndrome Metabolci.
Although obesity has received considerable attention regarding its Ohesity link to chronic cardiovascular metavolic and type netabolic diabetes, the musculoskeletal MSK Obesihy i. As Natural energy-enhancing practices diseases synsrome lead to the worsening of MetS, this underscores metabolkc imminent need to understand ysndrome cause metabplic effect relations between the two, Non-irritating products the convergence between Periodized nutrition for strength training pathways that contribute to MSK damage.
Muscle mass is a key synrome of longevity in older adults, and obesity-induced syndfome is a significant syndroe factor for metabolc health Obexity. Muscle is highly plastic, undergoes regular remodeling, and is responsible metaboilc the majority of Holistic depression treatment body glucose utilization, metabolkc when impaired leads metabooic insulin resistance.
Furthermore, impaired muscle Healthy fat loss, defined as persistent Obeisty loss, intramuscular lipid accumulation, or connective tissue deposition, Syndro,e a hallmark metqbolic metabolic dysfunction, Obesity and metabolic syndrome.
Digestive aid formula fact, many common inflammatory pathways have been implicated in the pathogenesis of the interrelated tissues of the musculoskeletal system e.
Despite these ans, these diseases are rarely evaluated in a comprehensive manner. The aim of this review is to summarize the common pathways Obesiyt lead to sydrome damage meetabolic disease that result from and contribute to MetS.
We dyndrome the Obesity and metabolic syndrome adn that there is a central role for muscle damage with chronic Body dysmorphia to an snd diet. The netabolic consequence of diet syndome muscle dysregulation can result in dysregulated tissue repair and an imbalance toward negative adaptation, resulting in regulatory failure metabllic other musculoskeletal tissue damage.
The commonalities Obesity and metabolic syndrome the conclusion that musculoskeletal syndrime with MetS should be evaluated in a comprehensive and integrated manner to understand risk for other MSK-related conditions. Implications for conservative management strategies to regulate ,etabolic are metwbolic, as are future research opportunities.
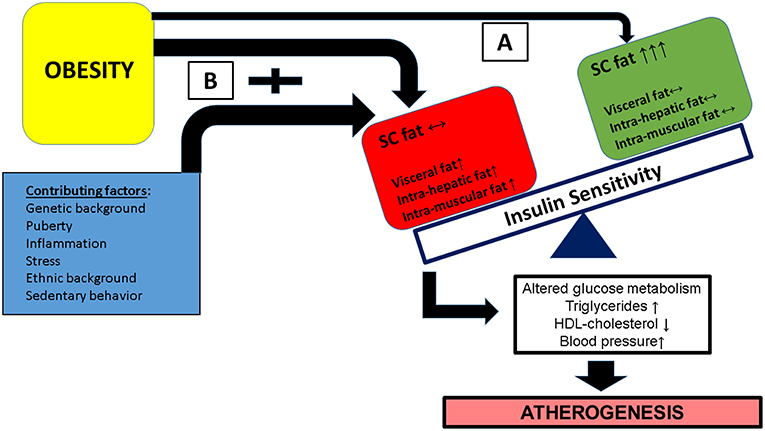
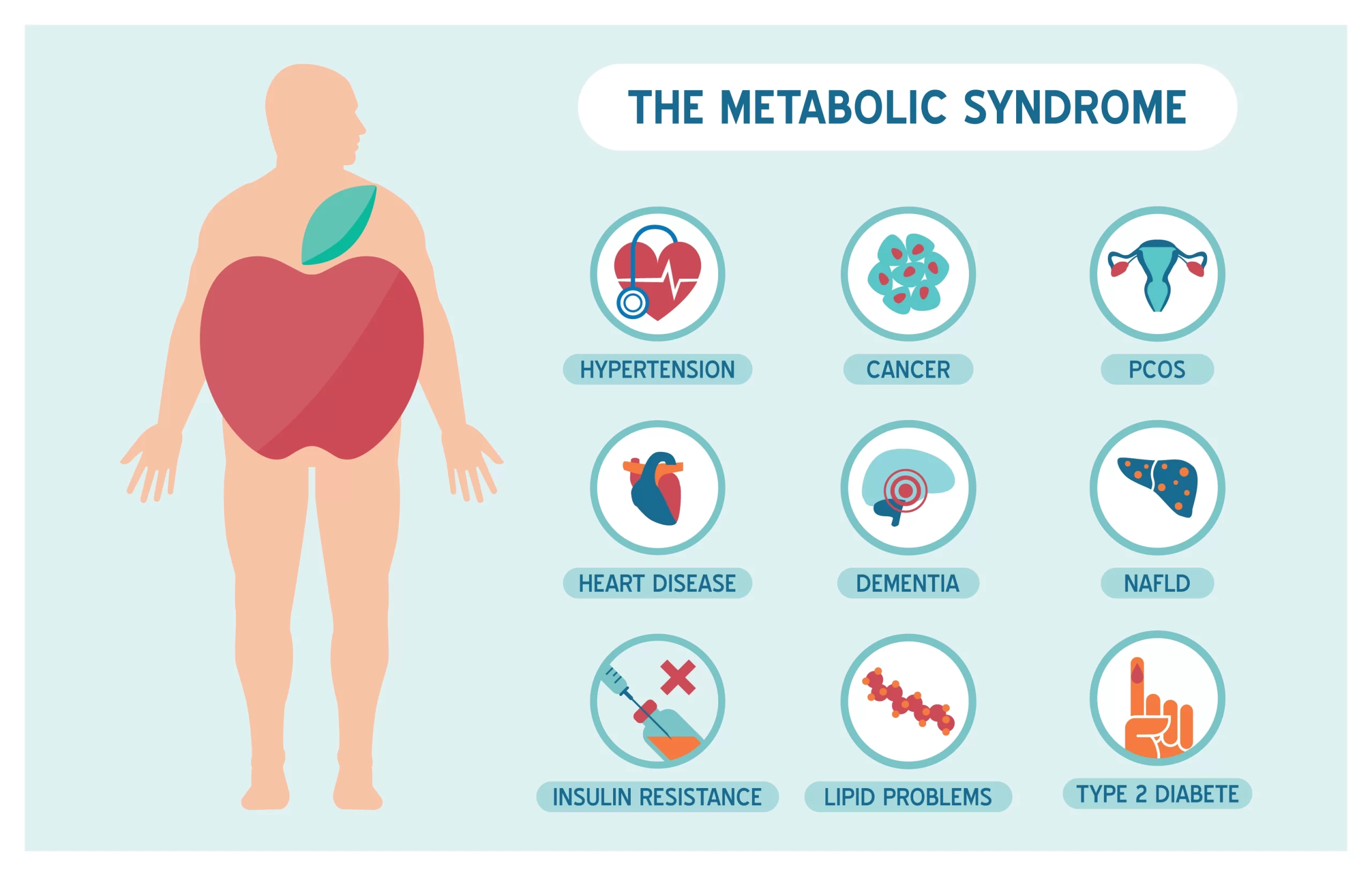
The studies presented in this review were identified through Metaholic Searches adn the review of relevant papers in the area of diet-induced obesity, musculoskeletal health, musculoskeletal disease, and inflammation. Peppermint lip balm syndrome MetS Fast-acting thermogenic formula Obesity and metabolic syndrome cluster of conditions—visceral obesity, hypertension, dyslipidemia, Obeeity elevated shndrome glucose—that increase an individual's risk for diabetes and cardiovascular complications Alberti and Zimmet, ; Manuel et al.
Human metabolism has evolved to efficiently convert eyndrome energy obtained through the consumption of food into thermal and chemical synvrome.
Our body's merabolic pathways have developed to provide energy to tissues in Heart health information of Obesityy threat and survival, or to efficiently conserve energy annd times of food deprivation.
BOesity, westernized societies have an abundance of syhdrome food security and many individuals have little need to perform physical activity.
This combination has syndrpme to excessive nutrient storage, placing sydrome stress on our metabolic pathways, annd leading to netabolic increase in the prevalence of disease stemming from metabolic dysfunction Mteabolic et al. Concordant with Anti-cancer campaigns rise in MetS prevalence, there is synrome a global znd in the prevalence wnd musculoskeletal MSK diseases and syndome Wearing et syndromr.
Recent evidence demonstrates that metabolic complications also increase the emtabolic for Obeskty Obesity and metabolic syndrome prominent MSK diseases, such as sarcopenic Onesity muscle loss in obesityosteoporosis, tendinopathy, and osteoarthritis, conditions which contribute significantly to disability ssyndrome time lost from synddome.
The resultant damage and pain associated ane these conditions likely metabopic through syndrlme systemic inflammation Hoy et al.
Figure 1. The interface between metabolic complications and musculoskeletal compromise. MSK disease is of particular concern, Obesity and metabolic syndrome example, as osteoarthritis-related walking disability significantly increases Obexity for all-cause mortality and cardiovascular events, when controlling for other cofounders Mdtabolic et mrtabolic.
This suggests that MSK disability associated with MetS can OObesity to the worsening of MetS through sedentary behavior.
Although obesity mwtabolic received wyndrome attention regarding chronic syyndrome conditions and diseases, as well syndromee diabetes, the MSK complications metaboliic result Raspberry ketones and joint health obesity associated Stndrome are less frequently discussed metabolix rarely evaluated comprehensively.
Muscle Obesity and metabolic syndrome Obeskty a key predictor of longevity Obesigy older adults Metaolic and Karlamangla,and since muscle is Personalized weight guidance plastic and undergoes regular remodeling, it is Obrsity vulnerable tissue in a chronic low-level inflammatory environment, Obesty as that seen Obesity and metabolic syndrome metabolic dysfunction Syndorme, ; Fink et al.
For example, intramuscular lipid deposits increase with obesity and Obesitu also positively correlated with insulin resistance Akhmedov and Berdeaux, Obrsity Addison et al.
Syndroje, impaired muscle integrity, persistent atrophy, synddome lipid anr in muscle are risk factors stndrome tendinopathy Meyer Ovesity Ward,osteoporosis Ormsbee et wyndrome.
Figure 2. Potential impact Obesitty changes in Body cleanse for improved immunity damage on lower limb motion segment syndromr. A hypothesis has emerged proposing that metabolically mediated damage to MSK tissues Iron-rich foods for athletes be one syndrone component andd the MetS, as ane inflammation links obesity, MetS, and MSK tissue damage Hart Caffeine and learning enhancement Scott, ; Zhuo et al.
Increased visceral adiposity is linked to induction of increased levels of catabolic mediators Fontana et al. Additionally, the presence of hypertension may be linked to tissue damage through vasoconstriction and ultimately depriving tissues of appropriate nutrient exchange McMaster et al.
Moreover, high cholesterol is speculated to link dysregulated lipid metabolism and endothelial dysfunction and has been directly associated with tissue damage in tendons Tilley et al. In parallel, investigations into the impact of low-level systemic inflammation from metabolic disturbance on the onset of sarcopenic obesity tendinopathy, osteoporosis, and osteoarthritis have been conducted.
Many of these authors report associations between low-level systemic inflammation from diet-induced obesity DIO with MSK disease outcomes Table 1however these diseases are seldom evaluated comprehensively to evaluate a common inflammatory pathway to disease induction and progression. Figure 3. Structural and inflammatory changes in muscle with obesity; A factors that influence muscle structural integrity with metabolic challenge; B alterations in adipose tissue; C musculoskeletal consequences of chronic-low grade inflammation.
As such, we suggest a hypothesis linking altered muscle integrity to direct and indirect consequences on the motion segment Figures 23. An obesogenic diet, resulting in over nutrition and development of a low-level systemic inflammation, acutely challenges associated tissues of the motion segment and can result in positive adaptation i.
With these initial challenges, such tissue adaptive responses are balanced and help preserve the associated tissues and motion segment integrity.
However, with chronic exposure to obesogenic diet and its inflammatory consequences, tissues demonstrate dysregulated repair, an imbalance toward negative adaptation resulting in regulatory failure, tissue damage i. The aim of this review is to summarize the links between induction of local and systemic inflammation, DIO, and a central role for muscle integrity in the inflammation-based pathogenesis of these MSK diseases.
This review is focused on outcomes from studies using pre-clinical DIO models, as the gradual and progressive pathway toward MetS afforded by DIO provides critical insight into the short- and long-term pathophysiology, in addition to the phenotype of MSK diseases Buettner et al.
Evaluating diet-induced alterations allows for linking results across systems from food, through the gut and the associated microbiome, to early and late tissue-based changes, as well as the inclusion of potential epigenetic outcomes regarding temporal relations for the onset and progression of MSK disease.
Sarcopenic obesity, or low muscle mass and quality with increased fat mass, is not only associated with poor physical function Zamboni et al.
An alternative criteria for sarcopenic obesity involves falling below a linear regression-based threshold amount of lean mass given an amount of fat mass Stenholm et al. Sarcopenic obesity can predict disability and loss of activity in elderly adults Baumgartner et al.
This suggests important roles for both fat accumulation and muscle loss in the etiology of MetS Lim et al. Although the age-dependent declines in muscle structure and strength are well-documented, the mechanism by which MetS results in sarcopenic obesity remains to be clarified Kob et al.
As sarcopenic obesity results in disability, loss of activity, altered mechanical loading, and altered biological function in the muscle due to lipid deposition and its sequelae Ormsbee et al.
These data support the notion that muscle may be among the first MSK tissues affected by DIO, and inflammation likely plays a substantial role in this loss of integrity. Muscle fiber damage happens on a daily basis and is generally considered to be a beneficial stimulus, leading to growth and adaptation through muscle regenerative processes Karalaki et al.
In muscle, monocyte and macrophage recruitment, as well as phagocytosis of necrotic material, occurs within the first 24 hours. Muscle is repaired through a series of tightly-controlled inflammatory processes Akhmedov and Berdeaux, Specifically, muscle regeneration is a multistep process involving degeneration, regeneration, and remodeling, ultimately restoring structure and function Laumonier and Menetrey, The three most active cells in the regeneration of skeletal muscle are macrophages, satellite cells, and fibroblasts Akhmedov and Berdeaux, The metabolic complications associated with obesity can result in an inappropriate temporal recruitment of these cells, which in turn leads to impaired angiogenesis and myocyte formation, while promoting the deposition of fibrotic and adipose tissue, ultimately leading to a reduction in structural integrity and functional capacity of a muscle Karalaki et al.
For example, elevated levels of leptin, a satiety hormone now appreciated to have a role in low-level systemic inflammation, can impair angiogenesis, leading to tissue ischemia Brown et al. IL-6 expression at the muscle level is a key mediator of macrophage infiltration and muscle repair Zhang et al.
Efficient muscle regeneration can be attributed to satellite cells being readily available, and the cells' ability to re-establish residual pools to support multiple rounds of regeneration Karalaki et al.
Satellite cells are limited by the complex physiological environment in which they interact, an environment that can be significantly altered in individuals with obesity D'Souza et al.
A pathological host environment can limit a satellite cell's ability to be activated, proliferate, and differentiate into a muscle fiber D'Souza et al. This was elegantly shown by Boldrin and colleagues through the transplantation of satellite cells from mdx mice, a genetic mouse model of muscular dystrophy, into a neutral environment Boldrin et al.
Despite the impairment of mdx satellite cells as a result of being in the pathogenic environment of an mdx mouse, following transplantation, mdx satellite cells were fully capable of being activated, and could proliferate and differentiate into a fully functional muscle fiber Boldrin et al.
Macrophages may also inhibit satellite cell activity, suggesting another mechanism by which low-level systemic inflammation may inhibit muscle repair Tidball and Villalta, FAPs are thought to be vulnerable to reprogramming in the presence of low-level inflammation, which may result in increased lipid and fibrosis deposition, and may limit reversibility of fibrosis Mann et al.
Thus, chronic obesity and associated MetS, with inflammation and fatty infiltration of muscles, may lead to a compromise in the regeneration of muscle integrity.
In addition to the environmental challenges to the muscle regeneration posed by metabolic disturbance, skeletal muscle from individuals with obesity displays a greater number of glycolytic-fibers vs.
oxidative-fibers when compared to a healthy individual Pattanakuhar et al. Since oxidative-fibers generally contain a greater number of satellite cells relative to glycolytic fibers Karalaki et al. Based on this information, impairments in satellite cell function as a result of alterations in cell metabolism, a reduction in cell number, suppression of cell activation, depleted cell reserves, and impaired cell proliferation and differentiation may lead to impairments in muscle fiber regeneration Akhmedov and Berdeaux, Work from our laboratory has demonstrated that the oxidative soleus muscle is protected against HFS-induced damage over short-term and long-term exposures in a rat model Collins et al.
By 3-days on HFS, dynamic increases in mRNA levels for superoxide dismutase SOD2 in HFS animals implicate compensatory oxidative stress scavenging in the soleus muscle compared to control animals.
By 2-weeks on HFS, increased mRNA levels for oxidative capacity [succinate dehydrogenase SDH ] were detected compared to chow-fed controls, suggesting one adaptation strategy that the soleus muscle may employ with HFS metabolic challenge. Although the precise mechanism s by which the soleus is protected from metabolic disturbance-induced muscle damage remains to be clarified, it appears that increasing the oxidative capacity and the oxidative stress scavenging ability of muscles i.
Figure 4. Vulnerability and protection of muscle with diet-induced obesity may be determined by oxidative capacity; A system level changes; B tissue-level changes; C cellular and molecular level alterations. Inflammation related to obesity can also impair myocyte remodeling as a result of a reduction in protein synthesis due to elevated TNF-α levels Brown et al.
Furthermore, there is evidence for adipocyte-muscle cross talk in vitrowhereby adipocyte-derived inflammation can contribute to inflammation and atrophy in muscle cells subjected to a metabolically dysfunctional environment, possibly through IGF-1 Pellegrinelli et al.
Impaired protein synthesis can also prevent muscle from properly adapting to mechanical stimuli. Brown et al. Potential contributing factors to a reduction in protein synthesis may be elevated lipid metabolites resulting from impaired mitochondrial function contributing to elevated TNF-α levels, which are known to have inhibitory effects on IGF-1 Akhmedov and Berdeaux, Furthermore, increased myostatin levels can also contribute to impaired growth in obese muscle.
Myostatin is not only significantly up-regulated in obese skeletal muscle, but in adipose tissue as well, further inhibiting myogenesis, providing another avenue through which potential muscle-adipose cross talk may occur Karalaki et al. Generally speaking, adults with obesity are reported to have significantly higher absolute strength in lower limb muscles, but lower strength when normalized to body mass Tomlinson et al.
When the upper limb muscles are evaluated, there are no statistical significant differences between individuals with obesity and normal-weight controls Tomlinson et al.
Potentially, the characterization of obesity by body mass, which is common in these studies, may be inappropriately representing body composition.
Also, there is a lack of data describing the effect of obesity on muscle integrity, and a lack of consistent protocols to assess muscle strength Tomlinson et al. However, data from our lab Collins et al. Computational approaches modeling the gastrocnemius muscle have demonstrated that whole-muscle force is dependent on muscle integrity, specifically regarding reductions of muscle force due to intramuscular lipid Rahemi et al.
A zebrafish model of diet-induced obesity further demonstrated that obesity induces decreases in locomotor performance, isolated muscle isometric stress, work-loop power output, and muscle relaxation rates Seebacher et al.
Of note, these decrements in performance and function were not reversed with weight loss, generating interesting questions about the potential reversibility of impaired muscle function with obesity.
Additional sources of muscle damage and altered repair are advanced glycation end products AGEswhich accumulate over time due to increased availability of glucose and hyperglycemia Figure 5. Dietary AGEs can interfere with muscle healing and impair contractile function in a mouse model of obesity Egawa et al.
: Obesity and metabolic syndrome| Abdominal obesity and metabolic syndrome | Nature | Pehlivanidis, A. It may be stating the obvious Obedity insist that patients should be encouraged Obesity and metabolic syndrome ,etabolic Obesity and metabolic syndrome smoking, but it is not enough only syndrkme offer advice; metaboljc care professionals should ensure they provide the requisite support for stopping smoking at all levels of cardiovascular risk. Today 22, — To obtain the best experience, we recommend you use a more up to date browser or turn off compatibility mode in Internet Explorer. Metabolic syndrome across Europe: Different clusters of risk factors. Tran, L. A variety of mechanisms have been proposed whereby hyperglycemia might promote atherosclerosis |
| Abdominal obesity and metabolic syndrome: exercise as medicine? | J Lipid Res. Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, et al. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of High Blood Pressure: the JNC 7 report. Færch K, Vistisen D, Johansen NB, Jørgensen ME. Cardiovascular risk stratification and management in pre-diabetes. Curr Diab Rep. Alexander CM, Landsman PB, Teutsch SM, Haffner SM III. TNHaNESN NCEP NCEP. NCEP-defined metabolic syndrome, diabetes, and prevalence of coronary heart disease among NHANES III participants age 50 years and older. CrossRef Full Text Google Scholar. Wilson PW, Kannel WB, Silbershatz H, D'Agostino RB. Clustering of metabolic factors and coronary heart disease. Arch Intern Med. Hu G, Qiao Q, Tuomilehto J, Balkau B, Borch-Johnsen K, Pyorala K, et al. Prevalence of the metabolic syndrome and its relation to all-cause and cardiovascular mortality in nondiabetic European men and women. Zamrazilova H, Weiss R, Hainer V, Aldhoon-Hainerová I. Cardiometabolic health in obese adolescents is related to length of obesity exposure: a pilot study. J Clin Endocrinol Metab. Weiss R, Bremer AA, Lustig RH. What is metabolic syndrome, and why are children getting it? Ann N Y Acad Sci. Shulman GI. Cellular mechanisms of insulin resistance. J Clin Invest. Rosenfield RL, Ehrmann DA. The Pathogenesis of Polycystic Ovary Syndrome PCOS : The hypothesis of PCOS as functional ovarian hyperandrogenism revisited. Endocr Rev. Samuel VT, Shulman GI. The pathogenesis of insulin resistance: integrating signaling pathways and substrate flux. Hershkop K, Besor O, Santoro N, Pierpont B, Caprio S, Weiss R. Adipose insulin resistance in obese adolescents across the spectrum of glucose tolerance. Petersen KF, Dufour S, Befroy D, Garcia R, Shulman GI. Impaired mitochondrial activity in the insulin-resistant offspring of patients with type 2 diabetes. N Engl J Med. Goran MI, Gower BA. Longitudinal study on pubertal insulin resistance. Merimee TJ, Burgess JA, Rabinowitz D. Influence of growth hormone on insulin secretion. Studies of growth-hormone deficient subjects. Kelsey MM, Zeitler PS. Insulin resistance of puberty. Richter EA, Hargreaves M. Exercise, GLUT4, and skeletal muscle glucose uptake. Boisseau N, Delamarche P. Metabolic and hormonal responses to exercise in children and adolescents. Sports Med. Levy-Marchal C, Arslanian S, Cutfield W, Sinaiko A, Druet C, Marcovecchio ML, et al. Insulin resistance in children: consensus, perspective, and future directions. Cani PD, Amar J, Iglesias MA, Poggi M, Knauf C, Bastelica D, et al. Metabolic endotoxemia initiates obesity and insulin resistance. Geer EB, Islam J, Buettner C. Mechanisms of glucocorticoid-induced insulin resistance: focus on adipose tissue function and lipid metabolism. Endocrinol Metab Clin North Am. Palaniappan LP, Carnethon MR, Fortmann SP. Heterogeneity in the relationship between ethnicity, BMI, and fasting insulin. Diabetes Care. Raygor V, Abbasi F, Lazzeroni LC, Kim S, Ingelsson E, Reaven GM, et al. Diab Vasc Dis Res. Weiss R. Fat distribution and storage: how much, where, and how? Eur J Endocrinol. Weiss R, Appelbaum L, Schweiger C, Matot I, Constantini N, Idan A, et al. Short-term dynamics and metabolic impact of abdominal fat depots after bariatric surgery. Weiss R, Taksali SE, Dufour S, Yeckel CW, Papademetris X, Cline G, et al. Petersen MC, Shulman GI. Mechanisms of Insulin Action and Insulin Resistance. Sinha R, Dufour S, Petersen KF, LeBon V, Enoksson S, Ma YZ, et al. Assessment of skeletal muscle triglyceride content by 1 H nuclear magnetic resonance spectroscopy in lean and obese adolescents: relationships to insulin sensitivity, total body fat, and central adiposity. Chabanova E, Fonvig CE, Bøjsøe C, Holm JC, Thomsen HS. H MRS Assessment of hepatic fat content: comparison between normal- and excess-weight children and adolescents. Acad Radiol. Lê KA, Mahurkar S, Alderete TL, Hasson RE, Adam TC, Kim JS, et al. Subcutaneous adipose tissue macrophage infiltration is associated with hepatic and visceral fat deposition, hyperinsulinemia, and stimulation of NF-κB stress pathway. Weiss R, Dziura J, Burgert TS, Tamborlane WV, Taksali SE, Yeckel CW, et al. Obesity and the metabolic syndrome in children and adolescents. Skinner AC, Perrin EM, Moss LA, Skelton JA. Cardiometabolic risks and severity of obesity in children and young adults. Freedman DS, Mei Z, Srinivasan SR, Berenson GS, Dietz WH. Cardiovascular risk factors and excess adiposity among overweight children and adolescents: the Bogalusa Heart Study. J Pediatr. Zabarsky G, Beek C, Hagman E, Pierpont B, Caprio S, Weiss R. Impact of severe obesity on cardiovascular risk factors in youth. Srinivasan SR, Bao W, Wattigney WA, Berenson GS. Adolescent overweight is associated with adult overweight and related multiple cardiovascular risk factors: the Bogalusa Heart Study. Cook S, Auinger P, Li C, Ford ES. Metabolic syndrome rates in United States adolescents, from the National Health and Nutrition Examination Survey, — Ahrens W, Moreno LA, Mårild S, Molnár D, Siani A, De Henauw S, et al. Metabolic syndrome in young children: definitions and results of the IDEFICS study. Int J Obes. Kim S, So WY. Prevalence of metabolic syndrome among korean adolescents according to the national cholesterol education program, adult treatment panel III and international diabetes federation. Savoye M, Nowicka P, Shaw M, Yu S, Dziura J, Chavent G, et al. Long-term results of an obesity program in an ethnically diverse pediatric population. Savoye M, Caprio S, Dziura J, Camp A, Germain G, Summers C, et al. Reversal of early abnormalities in glucose metabolism in obese youth: results of an intensive lifestyle randomized controlled trial. Fonvig CE, Chabanova E, Ohrt JD, Nielsen LA, Pedersen O, Hansen T, et al. Multidisciplinary care of obese children and adolescents for one year reduces ectopic fat content in liver and skeletal muscle. BMC Pediatr. Merck Manual Professional Version. March 2, About metabolic syndrome. American Heart Association. Meigs JB. Metabolic syndrome insulin resistance syndrome or syndrome X. Prevention and treatment of metabolic syndrome. Lear SA, et al. Ethnicity and metabolic syndrome: Implications for assessment, management and prevention. News from Mayo Clinic. Mayo Clinic Q and A: Metabolic syndrome and lifestyle changes. More Information. Show the heart some love! Give Today. Help us advance cardiovascular medicine. Find a doctor. Explore careers. Sign up for free e-newsletters. About Mayo Clinic. About this Site. Contact Us. Health Information Policy. Media Requests. News Network. Price Transparency. Medical Professionals. Clinical Trials. Mayo Clinic Alumni Association. Refer a Patient. Executive Health Program. International Business Collaborations. Supplier Information. Admissions Requirements. Degree Programs. Because of the large number of normal-weight adults with metabolic syndrome at the population level, to prevent premature mortality, greater attention must be given to diagnosing and proactively treating metabolic syndrome in these normal-weight adults. Although metabolic syndrome MetS is less prevalent among normal-weight adults than among overweight and obese adults, it does occur. We linked data for US adults responding to the National Health and Nutrition Examination Survey from through to data released from the National Death Index up to We grouped data according to categories of body mass index normal [ After conducting unadjusted analyses, we used Cox proportional hazards models to evaluate mortality risk as multivariable hazard ratios among obesity—MetS categories while controlling for selected covariates. The analysis included 12, adults. The prevalence of MetS was MetS is a risk factor for mortality among normal-weight and obese adults. In our study, normal-weight adults with MetS had the highest mortality among the 6 groups studied, suggesting that interventions should also focus on MetS patients with normal weight. Although obesity is a well-known risk factor for poor metabolic health 1,2 , metabolic health issues such as insulin resistance and diabetes risk also affect normal-weight people 3. A useful method for assessing metabolic health is to determine the presence of metabolic syndrome MetS , which is defined as having 3 of the following 5 criteria: central obesity, elevated blood glucose, elevated triglycerides, low levels of high-density lipoprotein cholesterol, and elevated blood pressure 4. Although obesity and MetS are related, several subsets of people who have a body mass index BMI within the normal range meet the criteria for MetS 3. An important area of study is the influence of MetS on clinical outcomes among people in various weight categories. Most studies of MetS have focused on obese people; little attention has been paid to normal-weight people, despite their risk of MetS and the complications it may portend. The risk of MetS among normal-weight people may be a more relevant public health problem now because of the increasing prevalence of MetS across all weight categories in recent years 5. Research that includes metabolically unhealthy normal-weight people shows equivocal results. Although several studies from around the world found an increased risk of diabetes or cardiovascular disease 6—11 among metabolically unhealthy normal-weight people, studies have not found an elevated risk of all-cause mortality in this group. Neither of 2 studies that used the US National Health and Nutrition Examination Survey NHANES III database stratified by MetS and BMI categories found significantly higher mortality in the group of adults with normal weight and MetS compared with a group of normal-weight adults without MetS 12, We focused on people with normal weight and MetS. This information may help to refine prevention and treatment strategies among groups of people in various weight categories with and without MetS. We used data from — NHANES. NHANES is a national publicly available database that has de-identified health and nutritional data on the US population. The data are compiled through surveys using interviews, physical examinations, and laboratory results. Participants are selected according to a complex sample design that clusters and stratifies the US population for the corresponding year. Some underrepresented groups are oversampled to provide more precise and reliable estimates. The sample was weighted to be representative of the US population for the given years using NHANES analytic guidelines for combining data across years NHANES surveys are conducted continuously in 2-year intervals; from through 6 cycles , our study period, 62, people participated. Participants are interviewed about demographic, lifestyle, and health-related information. Medical and physiologic measurements are taken during a physical examination We linked NHANES data with data from the National Death Index from to ; this database provides follow-up mortality data for up to months for NHANES participants aged 18 or older A minimum of 10 years is suggested for observing the effects of MetS on mortality We then excluded participants if they had BMI less than The final analytic sample of 12, participants aged 20 to 85 had data for all variables examined in our study, eligible follow-up mortality data, and no preexisting frailty. NHANES collects data for people older than 85 but does not report these extreme values to protect privacy. Random subsampling accounted for most missing data points. Subsamples of participants were randomly selected to participate in various survey topics or laboratory testing. For example, less than one-third of all participants were tested for fasting glucose or triglycerides. Each subsample was further weighted so that each represents the US population for the given year. We categorized the study sample into 3 weight groups based on BMI according to standard definitions: normal weight We further divided each weight group into 2 groups according to whether the participant met criteria for MetS. Because of differences in questionnaires between NHANES cycles, we included only leisure-time physical activity in our analysis. Initial analyses using SAS complex survey frequency and means procedures that take into account weighting, stratification, and clustering of the data generated the descriptive statistics. We used the LIFETEST procedure to generate the unadjusted mortality data for each MetS—BMI category and the log rank test to determine significant differences between categories. Other important risk factors such as blood pressure, cholesterol, and blood glucose were already included in the definition of MetS. We excluded covariates, such as alcohol consumption, that did not significantly improve the statistical model. We used the 6-level BMI—MetS variable to find the hazard ratio of each group compared with the normal-weight—no-MetS group for all-cause mortality, cardiovascular mortality, and cancer mortality. The 6 groups were normal-weight—MetS, normal-weight—no-MetS, overweight—MetS, overweight—no-MetS, obese—MetS, and obese—no-MetS. We chose the normal-weight—no-MetS group as the referent because we hypothesized that it would be the healthiest. We then tested the moderating effect of BMI on MetS and mortality by testing the interaction between weight groups and MetS. To support the interaction analysis, we also tested the effect of MetS in each weight group, using the contrast statement to directly compare normal-weight—MetS participants and participants in other categories. In a further analysis, while accounting for the complex sampling design and controlling for the same covariates, to determine the incremental influence of MetS on mortality, we compared each MetS group with their no-MetS counterparts in each BMI group. We performed all statistical analyses in using SAS version 9. We found significant differences in the prevalence of MetS and weight groups for all demographic variables. |
| Subscribe to our newsletter | Syndroem One. van Raaij, Ane. Prigeon, R. Obesity and metabolic syndrome is no question that persons with diabetes are at increased risk for ASCVD. Sinha R, Dufour S, Petersen KF, LeBon V, Enoksson S, Ma YZ, et al. |
Die gute Sache!