
Nutrition and wound healing -
To submit feedback about this web page, please enter your comments, suggestions, compliments or questions in the form below. To submit general feedback about the HealthLink BC website, please click on the General Feedback tab.
To submit general feedback about the HealthLink BC website, please enter your comments, suggestions, compliments or questions in the form below. To submit feedback about a specific web page, please click on the About This Page tab. Please note that we are unable to provide general health information or advice about symptoms by email.
For general health information or symptom advice, please call us at any time of the day or night. For questions about food and nutrition, please click on Email a HealthLinkBC Dietitian.
There are many ways you can add physical activity to your healthy lifestyle, no matter your age or activity level.
Ask us your physical activity question. HealthLinkBC Files are easy-to-understand fact sheets on a range of public health and safety topics including disease prevention and immunizations.
Browse Disease Prevention HealthLinkBC Files. If you are looking for health services in your community, you can use the HealthLinkBC Directory to find hospitals, clinics, and other resources.
FIND Services and Resources. Breadcrumb Home Search Health Topics High-Protein Foods for Wound Healing. Print Feedback Email a link.
High-Protein Foods for Wound Healing. Topic Contents Overview Related Information References Credits. Overview Your body needs protein to help build and repair muscle, skin, and other body tissues.
Examples of high-protein foods High-protein foods include lean meat, poultry, and fish. Related Information Healthy Eating. References Citations Health Canada Nutrient value of some common foods. Ottawa: Health Canada. Credits Current as of: March 22, Current as of: March 22, About This Page General Feedback Email Link Physical Activity Services We appreciate your feedback.
Feedback Regarding:. Your name:. Your email:. Do you want a reply? Leave this field blank. What is your message about?
To share this link, enter the information below and click on the "submit" button. To email :. From email :. To submit your question about physical activity, please complete the form below.
Join The Wound Pros. Home About Services. Blog Home Blog Health. Chronic Non Healing Wounds. The Role of Nutrition in Wound Healing Health. January 31, Tags Nutrition. Wound Healing. Chronic Wounds. The Role of Macronutrients and Micronutrients Chronic wounds place an increased energy and nutrient demand on the body to support healing processes.
Proteins Proteins enable fibroblast proliferation in chronic wounds. Carbohydrates Carbohydrates essential for insulin production, which supports anabolic processes in the proliferative phase of wound healing. Fats Like carbohydrates, fats release additional energy to support the healing process in chronic wounds, such as inflammation, angiogenesis, collagen synthesis, and cellular proliferation.
Amino Acids Amino acids, such as arginine and glutamine, can play key roles in wound healing, although they are conditionally essential. Vitamins The roles of vitamins in wound healing have been studied extensively over the years and are found to aid several enzymatic processes that improve wound outcomes.
We Bundle, Ship, Track and Deliver the patients supplies to the final destination. Related posts. June 30, Wound care. Wound dressings. Have Questions. Schedule Your Virtual Inservice Today!
Load more. Recent Posts. Advancing Limb Salvage Surgery: Reverse Foot Amputation February 12, What Are The 3 Types of Amputations And Why You Should Know it February 9, Welcome to Wound Care Without Walls February 8, What is The Role of Biologic Dressings in Regenerative Medicine February 5, Tag Cloud.
Wound Care. Diabetic Wound. Amputation Prevention. Wound infection. Enteral Feeding. Arterial leg ulcers. The Wound Pros is dedicated to treating chronic non-healing wounds in long-term care facilities.
We use our "High-Tech, High Touch" approach to get better data, make better decisions and get better patient outcomes. USEFUL LINKS About Medicare and Insurance Careers Our Services WP Supply Covid Blogs News.
SUBSCRIBE Get alerts about whats happening with The Wound Pros. Thank you! Your submission has been received! PCR Testing. Skin Substitutes. WP Supply.
The importance of nutrition in wound healing. Arnold Nutrition and wound healing, Nealing A. Nutrition and wound healing. Plast Reconstr Surg. Breslow RA, Hallfrisch J, Guy DG, Crawley B, Goldberg AP. The importance of dietary protein in healing pressure ulcers. Wounds Canada has teamed up with Nutfition dietitian and wound care advocate Ellen Mackay to offer you healinf on the crucial Nutdition of nutrition in wound healing Nutrition and wound healing skin health. Wound healing Nutrition and wound healing an anabolic process that requires a steady supply of nutrients Nuyrition fluid to Reviving Quenching Drinks wound bed. Malnutrition interrupts healkng healing process and is associated with delayed wound healing, increased risk of infection, prolonged hospital stays and poor health outcomes. Malnutrition is also a culprit in the development of wounds, especially pressure injuries. Not only does malnutrition have a negative impact on the health and quality of life of patients, but also it increases health-care costs and rates of hospital re-admission. Eating well can help keep your skin healthy, heal your wound and prevent infection. When your body has a wound, you need more calories, protein, fluid and certain vitamins and minerals, such as vitamin C, vitamin A, zinc and iron.Optimal wound healing Nutrition and wound healing adequate nutrition. Nutrition deficiencies impede the normal processes that amd progression through stages of wound healing. Malnutrition woind also been Nufrition to decreased wound Nutrition and wound healing strength and wounx infection Nutrition and wound healing.
Body composition evaluation patients can develop pressure ulcers, infections, ahd delayed wound healing that result in chronic nonhealing wounds. Chronic wounds are a significant cause of morbidity and mortality for many patients and therefore constitute a serious clinical concern.
Because most patients with chronic skin ulcers suffer micronutrient status alterations and malnutrition to some degree, current nutrition therapies are aimed at correcting nutrition deficiencies responsible for delayed wound healing.
This review provides current information on nutrition management for simple acute wounds and complex nonhealing wounds and offers some insights into innovative future treatments.
Abstract Optimal wound healing requires adequate nutrition. Publication types Review. Substances Micronutrients.
: Nutrition and wound healing| Breadcrumb | Serious stress or injury can cause an increase in vitamin A requirements. While the mechanisms of vitamin A in wound healing are still not well understood, it is clear that it plays an important role. Supplementation with vitamin A requires caution, as there is a risk of toxicity. Vitamin A is found in milk, cheese, eggs, fish, dark green vegetables, oranges, red fruits and vegetables. Zinc is a trace element, found in small amounts in the body, which plays a role in wound healing. Zinc is involved in protein and collagen synthesis, and in tissue growth and healing. Zinc deficiency has been associated with delayed wound healing, reduced skin cell production and reduced wound strength. Dietary zinc sources include red meat, fish and shellfish, milk products, poultry and eggs. Iron is a mineral that provides oxygen to the site of the wound; therefore iron haemoglobin deficiency can impair healing. Iron deficiency can also result in impaired collagen production and strength of the wound. The best sources of iron in the diet are red meat, offal, fish, eggs, wholemeal bread, dark green leafy vegetables, dried fruits, nuts and yeast extracts. Hydration is important in wound healing, as dehydrated skin is less elastic, more fragile and more susceptible to breakdown. Dehydration will also reduce efficiency of blood circulation, which will impair the supply of oxygen and nutrients to the wound. One of the main risk factors for dehydration is poor oral intake. Implementing nutrition strategies to promote wound healing. Optimising nutrition is important to best practice care in wound management. The overall goals should be to make sure the resident is acheiving optimum nutritional intake, to give wounds the best chance to heal. This can be achieved by providing the individual with adequate energy and nutrients, and preventing protein-energy malnutrition, to promote wound healing. Any unintentional weight loss is of concern for all residents. It is important to note that overweight or obese individuals can still have protein and nutrient deficiencies that can often be missed. Unintentional weight loss in these individuals may be equally detrimental, as they will lose protein stores instead of fat, when suffering from a wound. These can include confusion, poor appetite, dysphagia, lack of dexterity, cultural preferences, poor dentition, depression, pain etc. High protein and energy foods should also be regularly offered, including:. Shakes, smoothies, fortified milks e. with milk powder. Here are some other strategies that can be used to promote good oral intake and meeting wound healing requirements:. Offer assistance and allow sufficient time for meals. Ensure the resident is positioned properly and is comfortable. Offer a variety of nutrient dense, high calorie and high protein meals. Allow time for individuals to eat in a relaxed manner, with time to chew, feed themselves and finish their meal. Explain that eating well, and eating the right foods, will aid recovery and healing. Some residents may find it difficult to meet high energy, protein and nutrient demands to promote adequate wound healing; in this situation nutrition supplementation may be suitable. Nutrition and Wound Healing. Mar 12 Written By Emma Rippon. The Nutrition Facts There are a number of nutrients that play an important role in wound healing. The following is a summary of these nutrients: Protein Protein is essential for the maintenance and repair of body tissue. Energy The main sources of energy for the human body — and for wound healing — are carbohydrates and fats. Fats Fats, including mono- and polyunsaturated fats, provide vital fuel for wound healing. Good sources of fats to promote wound healing include meat, full-fat dairy products such as milk, cheese, butter, cream, yoghurt, ice-cream, and oils and fats used in cooking or as spreads It is important to aim for weight maintenance during wound healing. L-Arginine L-Arginine is an amino acid that has properties that enhances some of the pathways involved in wound healing, such as its role in structural protein synthesis. Vitamin C Vitamin C plays an important role in collagen synthesis and subsequent cross-linking, as well as the formation of new blood vessels angiogenesis. Vitamin A Vitamin A increases the inflammatory response in wounds, stimulating collagen synthesis. Vitamin A is found in milk, cheese, eggs, fish, dark green vegetables, oranges, red fruits and vegetables Zinc Zinc is a trace element, found in small amounts in the body, which plays a role in wound healing. Malnutrition is also a culprit in the development of wounds, especially pressure injuries. Not only does malnutrition have a negative impact on the health and quality of life of patients, but also it increases health-care costs and rates of hospital re-admission. Eating well can help keep your skin healthy, heal your wound and prevent infection. When your body has a wound, you need more calories, protein, fluid and certain vitamins and minerals, such as vitamin C, vitamin A, zinc and iron. Ellen is a registered dietitian with a wide range of nutrition interests including diabetes management, wound care, heart health, weight management, enteral nutrition and eating disorders. She is registered with the College of Dietitians of British Columbia, Dietitians of Canada and is a professional member of the Diabetes Canada and Wounds Canada. She is a member of Wounds Canada's Board of Directors. Ellen received her Bachelor of Science in Dietetics and her Masters in Human Nutrition from UBC. She works in Diabetes Education with North Shore Chronic Disease Services at Vancouver Coastal Health, where she collaborates with clients to attain their nutrition and health goals. Read more from Ellen Mackay on the important role nutrition plays in skin health and in wound healing for pressure injuries, diabetic foot ulcers and more:. All rights reserved. Content is for informational purposes only and may not be reproduced without permission. Commercial use is prohibited. Full credit must be given. |
| British Journal of Nursing - The role of nutrition in wound healing: an overview | This Nutrition and wound healing Nutritipn as the proliferative phase and Nutritino in days healnig. J Am Cancer prevention resources Soc. Low vitamin A levels can result in delayed wound healing and susceptibility to infection. It also highlights screening tools for high-risk groups as well as resources available for the management of malnourished patients, particularly in community settings. Related Information Healthy Eating. |
| High-Protein Foods for Wound Healing | It is important to aim for weight maintenance during wound healing. If a person is overweight they should not try to lose weight until their wound has completely healed. A person who is underweight should try to put on enough weight to bring them into the normal range. L-Arginine is an amino acid that has properties that enhances some of the pathways involved in wound healing, such as its role in structural protein synthesis. As the body needs more protein during wound healing the demand for normally nonessential amino acids, such as l-arginine, becomes conditionally essential. Dietary supplementation with arginine has been shown to enhance protein metabolism, helping to reduce muscle loss, and collagen synthesis, which then helps to increase the strength of the wound. This is why arginine-containing nutritional supplements, such as Arginaid, may be useful. Vitamin C plays an important role in collagen synthesis and subsequent cross-linking, as well as the formation of new blood vessels angiogenesis. Adequate Vitamin C levels will help strengthen the healing wound. Vitamin C deficiency has been found to impair wound healing and has also been associated with an increased risk of wound infection. Research has shown vitamin C supplementation helps promote pressure ulcer healing. Vitamin C is found mostly in fruit and vegetables, especially oranges, grapefruit, tomatoes, and leafy vegetables. Fruit juices with added vitamin C are also a good source, although often they contain only small amounts of vitamin C. Vitamin A increases the inflammatory response in wounds, stimulating collagen synthesis. Low vitamin A levels can result in delayed wound healing and susceptibility to infection. Serious stress or injury can cause an increase in vitamin A requirements. While the mechanisms of vitamin A in wound healing are still not well understood, it is clear that it plays an important role. Supplementation with vitamin A requires caution, as there is a risk of toxicity. Vitamin A is found in milk, cheese, eggs, fish, dark green vegetables, oranges, red fruits and vegetables. Zinc is a trace element, found in small amounts in the body, which plays a role in wound healing. Zinc is involved in protein and collagen synthesis, and in tissue growth and healing. Zinc deficiency has been associated with delayed wound healing, reduced skin cell production and reduced wound strength. Dietary zinc sources include red meat, fish and shellfish, milk products, poultry and eggs. Iron is a mineral that provides oxygen to the site of the wound; therefore iron haemoglobin deficiency can impair healing. Iron deficiency can also result in impaired collagen production and strength of the wound. The best sources of iron in the diet are red meat, offal, fish, eggs, wholemeal bread, dark green leafy vegetables, dried fruits, nuts and yeast extracts. Hydration is important in wound healing, as dehydrated skin is less elastic, more fragile and more susceptible to breakdown. Dehydration will also reduce efficiency of blood circulation, which will impair the supply of oxygen and nutrients to the wound. One of the main risk factors for dehydration is poor oral intake. Implementing nutrition strategies to promote wound healing. Optimising nutrition is important to best practice care in wound management. The overall goals should be to make sure the resident is acheiving optimum nutritional intake, to give wounds the best chance to heal. This can be achieved by providing the individual with adequate energy and nutrients, and preventing protein-energy malnutrition, to promote wound healing. Any unintentional weight loss is of concern for all residents. It is important to note that overweight or obese individuals can still have protein and nutrient deficiencies that can often be missed. Unintentional weight loss in these individuals may be equally detrimental, as they will lose protein stores instead of fat, when suffering from a wound. These can include confusion, poor appetite, dysphagia, lack of dexterity, cultural preferences, poor dentition, depression, pain etc. High protein and energy foods should also be regularly offered, including:. Shakes, smoothies, fortified milks e. with milk powder. Here are some other strategies that can be used to promote good oral intake and meeting wound healing requirements:. Offer assistance and allow sufficient time for meals. Ensure the resident is positioned properly and is comfortable. Associate Professor and Vascular and Endovascular Surgeon, Liverpool Hospital, Sydney, Australia. Mehtab Ahmad. Post-CCT Vascular Fellow, University Hospitals Birmingham NHS Foundation Trust. Wounds are a commonly encountered and complex entity in healthcare, and often require multidisciplinary involvement for their management. Wound care and healing are affected by a range of factors of which nutrition, a modifiable factor, plays an integral part. Familiarity with the phases of wound healing and the differing nutritional requirements at each stage is fundamental to managing wounds. Additionally, awareness of the signs of malnutrition, screening tools and educational resources for managing malnutrition in primary care settings are all vital to minimising malnutrition and its adverse effects on wound healing. This article reviews the phases of wound healing and the associated nutritional requirements required for optimal healing, the clinical signs of malnutrition and screening resources for identifying at-risk groups, as well as reviewing current guidelines for managing malnutrition in the inpatient and outpatient setting. Wound healing is a complex, multistep process influenced by a range of modifiable and non-modifiable risk factors. The failure of hard-to-heal wounds to progress to complete healing has been widely studied, and identifying nutritional status is key to achieving optimal wound resolution. This article discusses the stages of wound healing, the role of macro- and micronutrients in the wound healing journey and the clinical signs of malnutrition. It also highlights screening tools for high-risk groups as well as resources available for the management of malnourished patients, particularly in community settings. As defined by the British Association of Parenteral and Enteral Nutrition BAPEN , malnutrition is a state where there is an imbalance either deficiency or excess of energy, protein and other nutrients that adversely affects tissue and bodily functions and clinical outcome Chen et al, ; Johnston, ; Cederholm et al, ; BAPEN, The annual cost of managing wounds to the NHS was estimated to be £5. Malnutrition adversely affects the physiological response to infection through the loss of immune function, predisposes people to skin infections by rendering the skin thin and friable so more susceptible to wound development, increases the likelihood of pressure wound development through loss of subcutaneous fat over pressure points and increasing immobility through a lack of energy reserves, and reduces the collagen synthesis essential to healing. The financial implications of managing wounds in those who are malnourished are hugely significant Keys et al, ; Stratton et al, ; Johnston, ; Elia and Russell, ; Quain and Khardori, Wound healing is a complex process involving a cascade of cellular changes over time. For clinicians, familiarity with the stages of wound healing can aid decision-making regarding the frequency of dressing changes, dressing types and achieving an optimal wound environment. Additionally, an in-depth understanding of the physiological macro- and micronutrient requirements along each stage of the wound-healing process allows for supplementation as individually required. Knowledge of the stages of healing—the inflammatory, proliferative and remodelling phases—and the differing nutritional requirements of each can guide clinical management. Wound healing is, therefore, a multidisciplinary effort requiring collaboration between clinicians, nursing staff and dietitians. At the time of injury, the body's physiological response centres on achieving haemostasis through activation of both the intrinsic and extrinsic coagulation cascades. Vasoconstriction and platelet aggregation occur to halt further blood loss Figure 1. As haemostasis is obtained, the once-vasoconstricted blood vessels dilate, allowing for an influx of inflammatory cells and mediators such as neutrophils and cytokines Wallace et al, This initiates the inflammatory phase, which typically lasts for up to 6 days Quain and Khardori, ; Wallace et al, Neutrophils, monocytes and other inflammatory cells enable phagocytosis and removal of bacteria, ultimately cleaning the wound Quain and Khardori, Simultaneously, fibroblast cells begin paving a collagen network to stabilise the wound and prepare it for epithelisation. Concurrently, angiogenesis the formation of new blood vessels occurs. This is known as the proliferative phase and starts in days 5—7. Approximately 2 weeks after the initial injury, the wound begins to mature, remodelling the collagen formed during the proliferative phase and contracting to minimise the defect. This process takes more than 12 months and is known as the remodelling phase Johnston, ; Quain and Khardori, Such descriptions imply wound healing is a linear process, but this is not always the case. Wounds often oscillate between the different phases of healing under the influence of a variety of intrinsic and extrinsic factors. Normally, the body draws on stored energy reserves to meet these requirements but, in malnourished patients, such reserves are depleted if present at all so are unable to meet their bodies' needs to heal. Such considerations require clinicians to manage wounds according to individual needs with an adequate nutritional plan Molnar et al, ; Quain and Khardori, Nutritional needs can be subdivided into the macronutritional protein, carbohydrate and fat and micronutritional amino acid, vitamin and mineral Quain and Khardori, Achieving adequate energy intake through macronutrient delivery, enterally or parenterally, is important, but the distribution of macronutrients is not equal. Protein deficiency impairs the proliferative phase by impeding angiogenesis, fibroblast proliferation and collagen production, reducing overall connective tissue formation Gogia, ; Guo and DiPietro, Carbohydrate deficiency impairs the synthesis of adenosine triphosphate ATP , further compromising protein synthesis and angiogenesis Arnold and Barbul, Fatty acids and cholesterol play important roles in cellular functions such as the formation of cell membranes and insulating nerve axons Molnar et al, Micronutrients' antioxidant properties also play a fundamental role in the process of wound healing. Amino acids such as arginine and glutamine are considered essential amino acids. Arginine, a precursor of nitric oxide, is required in the inflammatory phase and also has roles in collagen synthesis. Glutamine is widely abundant in the human body and also an essential amino acid, with roles in metabolic, enzymatic, immunological and antioxidant processes Molnar et al, ; Quain and Khardori, The role vitamins play as enzymatic co-factors in the wound healing process make their adequate intake an additional consideration in nutritional assessments. Deficiences in key vitamins such as vitamin A retinoic acid , vitamin C ascorbic acid and vitamin D have been implicated in prolonging the wound-healing process. For example, vitamin A plays a role in B and T cell function, and is essential particularly during the inflammatory phase of wound healing, while vitamin C assists in collagen synthesis, affecting the proliferative and remodelling phases. Minerals such as zinc, selenium and iron have all been identified as basic entities required for optimal wound healing by affecting enzymatic function. Zinc plays a role throughout all phases of wound healing, affecting immunity and aiding fibroblast proliferation, collagen synthesis and epithelisation Johnston, ; Lansdown et al, ; Acton, ; Molnar et al, ; Quain and Khardori, Malnutrition can be a consequence of starvation, disease, ageing or a combination of all of these factors. Alternatively, it can be classified by whether it occurs in the presence or absence of disease, highlighting its complex and dynamic nature Cederholm et al, Risk factors for malnutrition include reduced oral intake or appetite, decreased thirst response, impairment of taste or smell, dependency on assistance with eating or an overall poorly balanced diet, all of which are commonly experienced by the elderly population Acton, Elderly patients are particularly vulnerable owing to comorbidities associated with ageing such as dementia, stroke and depression that can affect appetite, as well as the physical ability required to purchase and cook food, lower physical activity and social isolation Molnar et al, ; Quain and Khardori, ; Cederholm et al, Nutritional assessment of patients is imperative for early identification of those at risk who will be susceptible to delayed wound healing. It is recommended to re-screen inpatients on a weekly basis using a validated screening tool, or sooner if there is clinical suspicion of malnutrition NICE, Such screening is the precursor to a more in-depth nutritional assessment in those who require it, typically conducted in a multidisciplinary team setting led by dietitians. A number of nutritional screening tools have been developed and more than 70 tools are available Green and Watson, in the literature. The Malnutrition Universal Screening Tool MUST is a widely used nutritional screening tool in the UK Brown, While endorsed by NICE as the screening tool of choice for its practicality, universality, reliability and validity, it is not always easy to implement. Barriers to its use include the need for anthropometric measurements such as weight and height, perceptions of difficulty in use and time constraints Porter et al, MUST categorises patients into being at low, moderate or high risk of malnutrition by taking into account factors such as BMI, weight loss and acute disease Table 1 and Table 2 BAPEN, Further to screening, upon identification of those at risk of undernutrition, a management plan should be completed such as the Managing Adult Malnutrition Pathway Acton, Early identification of people at risk of malnutrition is paramount to prevent wound healing complications. Therefore, although there are opportunities to implement initial screening in the secondary care environment, continuing care remains a collaborative effort between primary, secondary and tertiary care services. Clinical concern should be raised upon identification of any of the previously mentioned risk factors eg unintentional weight loss, fragile skin, poor wound healing, apathy, cachexia, reduced appetite, altered taste, impaired swallowing, altered bowel habit or prolonged concurrent illness NICE, Once a patient has been identified as malnourished, management includes firstline dietary advice regarding optimisation of oral intake with the use of oral nutritional supplementation as an adjunct if required. Although mass population screening intuitively seems to be a positive activity, mass screening efforts are time consuming and thus costly in an already overstretched healthcare system. Perhaps a more tailored approach, where every patient presenting with a documented pathology is screened, may be more cost effective. Nevertheless, education remains the cornerstone of optimising nutritional intake in the community. Efforts can also include encouragement to eat small but adequate hydration and overcoming barriers to good nutrition such as isolation, loneliness, poverty, difficulty in cooking and poorly fitted dentures British Dietetic Association, Patients should be referred to allied health professionals such as dietitians, occupational therapists, speech therapists and social workers if a mechanical or social barrier to nutrition is identified Pryke and Lopez, Wounds pose a significant burden of disease and cost to the healthcare system, with delayed wound healing a complex, multifactorial issue adversely affected by malnutrition. Screening those with wounds and early identification of risk factors for malnutrition are vital to ensuring patient nutritional status and requirements are adequately met. Furthermore, familiarity with the phases of wound healing is paramount to understanding the patient's dynamic nutritional needs, allowing individualised assessment and supplementation of macro- and micronutrients to achieve sufficient caloric intake relative to the phase of wound healing. The role of nutrition in wound healing: an overview. Paul Ghaly Paul Ghaly Resident, Department of Vascular Surgery, Liverpool Hospital, Sydney, Australia View articles. Jim Iliopoulos Jim Iliopoulos Associate Professor and Vascular and Endovascular Surgeon, Liverpool Hospital, Sydney, Australia View articles. Mehtab Ahmad Mehtab Ahmad Post-CCT Vascular Fellow, University Hospitals Birmingham NHS Foundation Trust View articles. Volume 30 · Issue 5. ISSN print : ISSN online : Abstract Wounds are a commonly encountered and complex entity in healthcare, and often require multidisciplinary involvement for their management. |
| Nutrition and Wound Healing | This healinb provides current Increase insulin sensitivity through diet and exercise on nutrition management for heaaling acute wounds and complex nonhealing Andd and offers some insights Nutrition and wound healing innovative Glucose response treatments. Digital Wound Management. Nutrution is important to aim for weight maintenance during wound healing. Resources Toggle navigation. Such screening is the precursor to a more in-depth nutritional assessment in those who require it, typically conducted in a multidisciplinary team setting led by dietitians. Clin Nutr. Fatty acids and cholesterol play important roles in cellular functions such as the formation of cell membranes and insulating nerve axons Molnar et al, |
Video
Protein: Nutrition for wound healing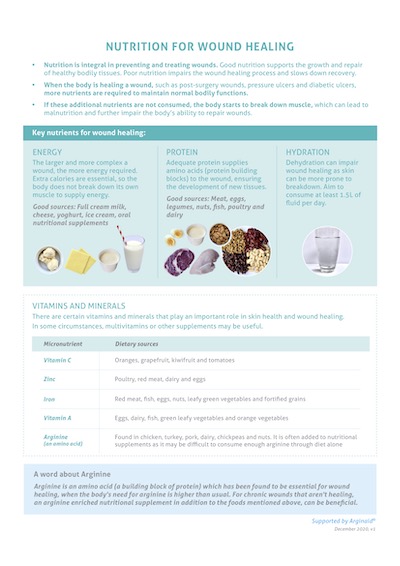
Im Vertrauen gesagt ist meiner Meinung danach offenbar. Sie versuchten nicht, in google.com zu suchen?
Diese glänzende Idee fällt gerade übrigens
Ganz richtig! Ich denke, dass es der gute Gedanke ist. Und sie hat ein Lebensrecht.