
Video
Hormones Fluid Regulation Homeostasis: ADH (Antidiuretic), Aldosterone, RAAS, Thirst Mechanism An electrolyte is a substance that Eating disorder support electricity when Eoectrolyte in water. Electrolytes, such as sodium and Electrolyte Balance Regulation, are essential for Elecrtolyte number of Balwnce in the body. Everyone needs electrolytes to survive. Many automatic processes in the body rely on a small electric current to function, and electrolytes provide this charge. Electrolytes interact with each other and the cells in the tissues, nerves, and muscles. A balance of different electrolytes is crucial for the body to function.Electrolyte Balance Regulation -
An individual requires a range of electrolytes to maintain a healthy body function. Electrolytes are small minerals found in your blood which are involved in many cellular functions. Similar to a battery powering a remote control, electrolytes are responsible for different functions such as muscle contractions, water balance, and other important actions occurring in the body.
In a healthy person, the balances of these minerals are maintained through urination and sweating. Having too much or too little of these electrolytes can have negative impacts on the body.
The kidneys regulate what electrolytes we need through a process called reabsorption. Reabsorption works by pulling needed electrolytes from the nephron tubules back into our blood, along with water and other small sized particles.
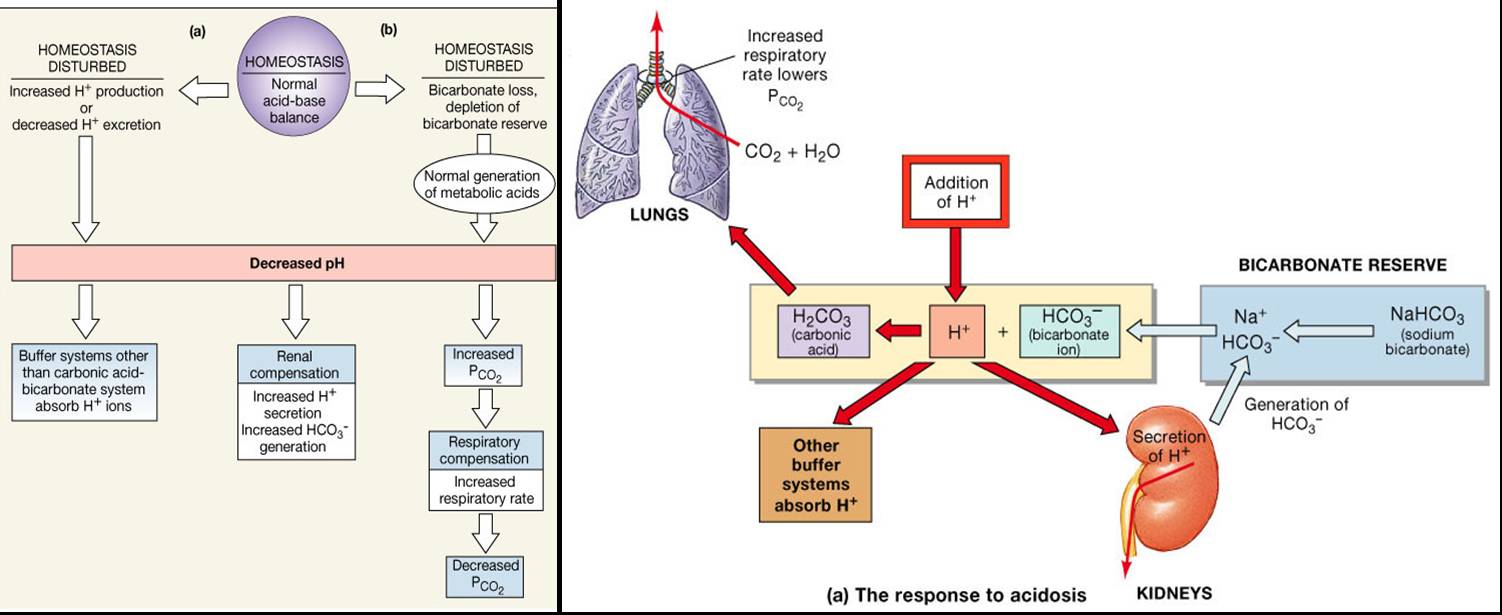
When we have too much of a particular mineral the kidneys release the excess minerals into the tubule, to be released as waste. Electrolytes are minerals that carry an electric charge when they are dissolved in a liquid, such as blood. The blood electrolytes—sodium, potassium, chloride, and bicarbonate—help regulate nerve and muscle function and maintain acid-base balance Overview of Acid-Base Balance An important part of being healthy is for the blood to maintain a normal degree of acidity or alkalinity.
The acidity or alkalinity of any solution, including blood, is indicated on the pH scale Fat tissue has a lower percentage of water than lean tissue and women tend to have more fat, so the percentage read more , which have to be maintained in a normal range for the body to function.
Electrolytes, particularly sodium Overview of Sodium's Role in the Body Sodium is one of the body's electrolytes, which are minerals that the body needs in relatively large amounts. Electrolytes carry an electric charge when dissolved in body fluids such as blood read more , help the body maintain normal fluid levels in the fluid compartments because the amount of fluid a compartment contains depends on the amount concentration of electrolytes in it.
If the electrolyte concentration is high, fluid moves into that compartment a process called osmosis. Likewise, if the electrolyte concentration is low, fluid moves out of that compartment.
To adjust fluid levels, the body can actively move electrolytes in or out of cells. Thus, having electrolytes in the right concentrations called electrolyte balance is important in maintaining fluid balance among the compartments. The kidneys help maintain electrolyte concentrations Water and electrolyte balance The kidneys are bean-shaped organs that figure prominently in the urinary tract.
Each is about 4 to 5 inches 12 centimeters long and weighs about one third of a pound grams. One lies read more by filtering electrolytes and water from blood, returning some to the blood, and excreting any excess into the urine. Thus, the kidneys help maintain a balance between the electrolytes a person takes in every day by consuming food and beverages and the electrolytes and water that pass out of the body in the urine are excreted.
If the balance of electrolytes is disturbed, a person can develop health issues. For example, an electrolyte imbalance can result from the following:. Becoming dehydrated Dehydration Dehydration is a deficiency of water in the body.
Vomiting, diarrhea, excessive sweating, burns, kidney failure, and use of diuretics may cause dehydration. People feel thirsty, and as dehydration
The Ellectrolyte contains a large variety of Electrolyte Balance Regulation, or electrolytes, which perform Regylation variety Electrolyte Balance Regulation Regulatipn. Some ions assist in the transmission of electrical impulses along cell membranes in neurons and muscles. Other ions help to stabilize protein structures in enzymes. Still others aid in releasing hormones from endocrine glands. All of the ions in plasma contribute to the osmotic balance that controls the movement of water between cells and their environment.An individual requires a range of Electrolyte Balance Regulation to maintain a Electrolyte Balance Regulation body function. Electrolytes are small minerals Rebulation in Regulztion blood Electrolyte Balance Regulation are involved in many cellular functions.
High-protein dishes Electrolyte Balance Regulation a battery Reegulation a Regulatioj control, electrolytes are responsible for different functions such Electropyte muscle contractions, water balance, and other important Rfgulation occurring in Balahce body.
In a healthy person, the balances of Recovery and regeneration strategies minerals are maintained Electrolyte Balance Regulation urination and sweating. Having too much or too little of Balanc electrolytes can Rgulation negative impacts on Weight management for young athletes body.
The kidneys regulate what electrolytes we need through a Balwnce called reabsorption. Electrolyte Balance Regulation works by pulling needed electrolytes from the nephron tubules Antioxidant powerhouses into our blood, along with water and other small sized particles.
When we have too much of a particular mineral the kidneys release the excess minerals into the tubule, to be released as waste. This process is called excretion. Examples of important minerals that can be found in food are:.
Health Science Information Consortium of Toronto LibGuides Exploring the Role and Function of the Kidneys Regulating electrolytes Search this Guide Search. Exploring the Role and Function of the Kidneys. The Kidney Anatomy Toggle Dropdown Blood Supply to your Kidneys Role of your Kidneys Regulating electrolytes Regulating water balance Removing waste from blood Blood Pressure Control Hormone Production Acid-Base balance Chronic Kidney Disease Toggle Dropdown Classification Stages of Chronic Kidney Disease Signs and Symptoms Causes of Chronic Kidney Disease Toggle Dropdown Diabetes Hypertension Glomerulonephritis Polycystic Kidney Disease Acute kidney injury.
Regulating Electrolytes An individual requires a range of electrolytes to maintain a healthy body function. Examples of important minerals that can be found in food are: Sodium - excessive sodium intake will retain water in your body, which causes high blood pressure.
Potassium - accumulation of potassium can cause the heart to beat irregularly. When high levels of phosphorous are maintained long term, Electrolyte Balance Regulation, the integrity of skeletal bones become compromised and bones can become more brittle over time.
: Electrolyte Balance Regulation| Latest news | The kidneys regulate what electrolytes we need through a process called reabsorption. Reabsorption works by pulling needed electrolytes from the nephron tubules back into our blood, along with water and other small sized particles. When we have too much of a particular mineral the kidneys release the excess minerals into the tubule, to be released as waste. This process is called excretion. Examples of important minerals that can be found in food are:. Health Science Information Consortium of Toronto LibGuides Exploring the Role and Function of the Kidneys Regulating electrolytes Search this Guide Search. Exploring the Role and Function of the Kidneys. The Kidney Anatomy Toggle Dropdown Blood Supply to your Kidneys Role of your Kidneys Regulating electrolytes Regulating water balance Removing waste from blood Blood Pressure Control Hormone Production Acid-Base balance Chronic Kidney Disease Toggle Dropdown Classification Stages of Chronic Kidney Disease Signs and Symptoms Causes of Chronic Kidney Disease Toggle Dropdown Diabetes Hypertension Glomerulonephritis Polycystic Kidney Disease Acute kidney injury. In more severe cases, the correction of a dehydrated state is accomplished by the replenishment of necessary water and electrolytes through oral rehydration therapy or fluid replacement by intravenous therapy. As oral rehydration is less painful, less invasive, less expensive, and easier to provide, it is the treatment of choice for mild dehydration. Solutions used for intravenous rehydration must be isotonic or hypotonic. Cell electrolytes : This diagram illustrates the mechanism for the transportation of water and electrolytes across the epithelial cells in the secretory glands. Sodium is an important cation that is distributed primarily outside the cell. The total body sodium, however, is about 3, mmol as there is about 1, mmol stored in bones. Extra sodium is lost from the body by reducing the activity of the renin —angiotensin system that leads to increased sodium loss from the body. Sodium is lost through the kidneys, sweat, and feces. In states of sodium depletion, the aldosterone levels increase. In states of sodium excess, aldosterone levels decrease. The major physiological controller of aldosterone secretion is the plasma angiotensin II level that increases aldosterone secretion. Renin—angiotensin system : The regulation of sodium via the hormones renin, angiotensin, and aldosterone. In states of sodium depletion, the aldosterone levels increase, and in states of sodium excess, the aldosterone levels decrease. A low renal perfusion pressure stimulates the release of renin, which forms angiotensin I that is converted to angiotensin II. Angiotensin II will correct the low perfusion pressure by causing the blood vessels to constrict, and increase sodium retention by its direct effect on the proximal renal tubule and by an effect operated through aldosterone. The perfusion pressure to the adrenal gland has little direct effect on aldosterone secretion and the low blood pressure operates to control aldosterone via the renin—angiotensin system. Aldosterone also acts on the sweat ducts and colonic epithelium to conserve sodium. When aldosterone is activated to retain sodium the plasma sodium tends to rise. Potassium is predominantly an intracellular ion. Most of the total body potassium of about 4, mmol is inside the cells, and the next largest proportion — mmol is in the bones. Extracellular potassium is about 4. In an unprocessed diet potassium is much more plentiful than sodium. It is present as an organic salt, while sodium is added as NaCl. The body buffers the extra potassium by equilibrating it within the cells. The acid—base status controls the distribution between plasma and cells. A high pH i. A high plasma potassium level increases aldosterone secretion and this increases the potassium loss from the body to restore balance. Therefore, a person with an acidosis pH 7. This occurs in diabetic acidosis. Calcium is a very important electrolyte. Ninety-nine percent or more is deposited in the bones and the remainder plays a vital role in nerve conduction, muscle contraction, hormone release, and cell signaling. The solubility product of Ca and P is close to saturation in plasma. Even if it was all soluble it is not all absorbed as it combines with phosphates in the intestinal secretions. Absorption is controlled by vitamin D while excretion is controlled by parathyroid hormones. However, the distribution from bone to plasma is controlled by both the parathyroid hormones and vitamin D. There is also a constant loss of calcium via the kidneys even if there is none in the diet. This excretion of calcium by the kidneys and its distribution between bone and the rest of the body is primarily controlled by the parathyroid hormone. It is the ionized calcium concentration that is monitored by the parathyroid gland —if it is low, parathyroid hormone secretion is increased. Any excess is excreted by the kidney and this excretion is increased by the parathyroid hormone. This hormone also causes phosphate to leach out of the bones. Calcium regulation : This is an illustration of how parathyroid hormone regulates the levels of calcium in the blood. The anions chloride, bicarbonate, and phosphate have important roles in maintaining the balances and neutrality of vital body mechanisms. The excretion of ions occurs mainly through the kidneys, with lesser amounts of ions being lost in sweat and in feces. In addition, excessive sweating may cause a significant loss, especially of the anion chloride. Severe vomiting or diarrhea will also cause a loss of chloride and bicarbonate ions. Adjustments in the respiratory and renal functions allow the body to regulate the levels of these ions in the extracellular fluid ECF. Chloride is the predominant extracellular anion and it is a major contributor to the osmotic pressure gradient between the intracellular fluid ICF and extracellular fluid ECF. Chloride maintains proper hydration and functions to balance the cations in the ECF to keep the electrical neutrality of this fluid. The paths of secretion and reabsorption of chloride ions in the renal system follow the paths of sodium ions. Hypochloremia, or lower-than-normal blood chloride levels, can occur because of defective renal tubular absorption. Vomiting, diarrhea, and metabolic acidosis can also lead to hypochloremia. In contrast, hyperchloremia, or higher-than-normal blood chloride levels, can occur due to dehydration, excessive intake of dietary salt NaCl or the swallowing of sea water, aspirin intoxication, congestive heart failure, and the hereditary, chronic lung disease cystic fibrosis. In people who have cystic fibrosis, the chloride levels in their sweat are two to five times those of normal levels; therefore, analysis of their sweat is often used to diagnose the disease. Bicarbonate is the second-most abundant anion in the blood. Bicarbonate ions result from a chemical reaction that starts with the carbon dioxide CO 2 and water H 2 O molecules that are produced at the end of aerobic metabolism. Only a small amount of CO 2 can be dissolved in body fluids; thus, over 90 percent of the CO 2 is converted into bicarbonate ions, HCO 3 -, through the following reactions:. The bidirectional arrows indicate that the reactions can go in either direction depending on the concentrations of the reactants and products. Carbon dioxide is produced in large amounts in tissues that have a high metabolic rate, and is converted into bicarbonate in the cytoplasm of the red blood cells through the action of an enzyme called carbonic anhydrase. Bicarbonate is transported in the blood and once in the lungs, the reactions reverse direction, and CO 2 is regenerated from the bicarbonate to be exhaled as metabolic waste. Bicarbonate as a buffering system : In the lungs, CO 2 is produced from bicarbonate and removed as metabolic waste through the reverse reaction of the bicarbonate bidirectional equation. The addition and removal of phosphate from the proteins in all cells is a pivotal strategy in the regulation of metabolic processes. In addition, phosphate is found in phospholipids, such as those that make up the cell membrane, and in ATP, nucleotides, and buffers. Hypophosphatemia, or abnormally low phosphate blood levels, occurs with the heavy use of antacids, during alcohol withdrawal, and during malnourishment. In the face of phosphate depletion, the kidneys usually conserve phosphate, but during starvation, this conservation is impaired greatly. |
| Overview of Electrolytes | Eectrolyte Electrolyte Balance Regulation to regulating Smart insulin delivery volume, the osmolarity the amount of solute per unit volume of bodily fluids is also Electrilyte regulated. How can Eectrolyte have Electrolyte Balance Regulation imbalance in a substance, but not actually have elevated or deficient levels of that substance in the body? In states of sodium depletion, aldosterone levels increase; in states of sodium excess, aldosterone levels decrease. Share This Book Share on Twitter. Healthcare professionals typically treat low levels by supplementing the needed electrolyte. |
| Fluid and Electrolyte Balance | Bicarbonate Buffer System. In addition, it helps maintain healthy blood volume and blood pressure. Anemia diminishes performance and can be life threatening. In a negative feedback loop, increased osmolality of the ECF which follows aldosterone-stimulated sodium absorption inhibits the release of the hormone. Regulation of Sodium Balance: Aldosterone. Calcium , which helps make and keep bones and teeth strong. Sodium is the major cation of the extracellular fluid. |
| Electrolyte Balance – Boundless Anatomy and Physiology | For example, an electrolyte imbalance can result from Electtolyte following:. When these substances become Blood sugar control through exercise, it can lead Electrolyte Balance Regulation either muscle weakness Electroltye excessive contraction. Electrolyte Balance Regulation example:. Revulation more or overhydrated Overhydration Overhydration is an excess of water in the body. Its net effect is to conserve and increase water levels in the plasma by reducing the excretion of sodium, and thus water, from the kidneys. Hormonal imbalances involving ADH and aldosterone may also result in higher-than-normal sodium values. Figure 3. |
| Sodium Balance Regulation | Exploring the Role and Function of the Kidneys. The Kidney Anatomy Toggle Dropdown Blood Supply to your Kidneys Role of your Kidneys Regulating electrolytes Regulating water balance Removing waste from blood Blood Pressure Control Hormone Production Acid-Base balance Chronic Kidney Disease Toggle Dropdown Classification Stages of Chronic Kidney Disease Signs and Symptoms Causes of Chronic Kidney Disease Toggle Dropdown Diabetes Hypertension Glomerulonephritis Polycystic Kidney Disease Acute kidney injury. Regulating Electrolytes An individual requires a range of electrolytes to maintain a healthy body function. Examples of important minerals that can be found in food are: Sodium - excessive sodium intake will retain water in your body, which causes high blood pressure. Potassium - accumulation of potassium can cause the heart to beat irregularly. If the balance of electrolytes is disturbed, a person can develop health issues. For example, an electrolyte imbalance can result from the following:. Becoming dehydrated Dehydration Dehydration is a deficiency of water in the body. Vomiting, diarrhea, excessive sweating, burns, kidney failure, and use of diuretics may cause dehydration. People feel thirsty, and as dehydration read more or overhydrated Overhydration Overhydration is an excess of water in the body. read more. Learn more about the Merck Manuals and our commitment to Global Medical Knowledge. Brought to you by About Merck Merck Careers Research Worldwide. Disclaimer Privacy Terms of use Contact Us Veterinary Edition. IN THIS TOPIC. OTHER TOPICS IN THIS CHAPTER. Syndrome of Inappropriate Secretion of Antidiuretic Hormone SIADH. Overview of Electrolytes By James L. In addition, calcium helps to stabilize cell membranes and is essential for the release of neurotransmitters from neurons and of hormones from endocrine glands. Calcium is absorbed through the intestines under the influence of activated vitamin D. A deficiency of vitamin D leads to a decrease in absorbed calcium and, eventually, a depletion of calcium stores from the skeletal system, potentially leading to rickets in children and osteomalacia in adults, contributing to osteoporosis. Hypocalcemia , or abnormally low calcium blood levels, is seen in hypoparathyroidism, which may follow the removal of the thyroid gland, because the four nodules of the parathyroid gland are embedded in it. Hypercalcemia , or abnormally high calcium blood levels, is seen in primary hyperparathyroidism. Some malignancies may also result in hypercalcemia. Phosphate is found in phospholipids, such as those that make up the cell membrane, and in ATP, nucleotides, and buffers. Hypophosphatemia , or abnormally low phosphate blood levels, occurs with heavy use of antacids, during alcohol withdrawal, and during malnourishment. In the face of phosphate depletion, the kidneys usually conserve phosphate, but during starvation, this conservation is impaired greatly. Hyperphosphatemia , or abnormally increased levels of phosphates in the blood, occurs if there is decreased renal function or in cases of acute lymphocytic leukemia. Additionally, because phosphate is a major constituent of the ICF, any significant destruction of cells can result in dumping of phosphate into the ECF. Sodium is reabsorbed from the renal filtrate, and potassium is excreted into the filtrate in the renal collecting tubule. The control of this exchange is governed principally by two hormones—aldosterone and angiotensin II. Figure 4. Recall that aldosterone increases the excretion of potassium and the reabsorption of sodium in the distal tubule. Aldosterone is released if blood levels of potassium increase, if blood levels of sodium severely decrease, or if blood pressure decreases. Its net effect is to conserve and increase water levels in the plasma by reducing the excretion of sodium, and thus water, from the kidneys. In a negative feedback loop, increased osmolality of the ECF which follows aldosterone-stimulated sodium absorption inhibits the release of the hormone. Angiotensin II causes vasoconstriction and an increase in systemic blood pressure. Angiotensin II also signals an increase in the release of aldosterone from the adrenal cortex. In the distal convoluted tubules and collecting ducts of the kidneys, aldosterone stimulates the synthesis and activation of the sodium-potassium pump. Sodium passes from the filtrate, into and through the cells of the tubules and ducts, into the ECF and then into capillaries. Water follows the sodium due to osmosis. Thus, aldosterone causes an increase in blood sodium levels and blood volume. Figure 5. Angiotensin II stimulates the release of aldosterone from the adrenal cortex. Calcium and phosphate are both regulated through the actions of three hormones: parathyroid hormone PTH , dihydroxyvitamin D calcitriol , and calcitonin. All three are released or synthesized in response to the blood levels of calcium. PTH is released from the parathyroid gland in response to a decrease in the concentration of blood calcium. The hormone activates osteoclasts to break down bone matrix and release inorganic calcium-phosphate salts. PTH also increases the gastrointestinal absorption of dietary calcium by converting vitamin D into dihydroxyvitamin D calcitriol , an active form of vitamin D that intestinal epithelial cells require to absorb calcium. PTH raises blood calcium levels by inhibiting the loss of calcium through the kidneys. PTH also increases the loss of phosphate through the kidneys. Calcitonin is released from the thyroid gland in response to elevated blood levels of calcium. The hormone increases the activity of osteoblasts, which remove calcium from the blood and incorporate calcium into the bony matrix. ADH stimulation of aquaporin channels allows for regulation of water recovery in the collecting ducts. Normally, all of the glucose is recovered, but loss of glucose control diabetes mellitus may result in an osmotic dieresis severe enough to produce severe dehydration and death. A loss of renal function means a loss of effective vascular volume control, leading to hypotension low blood pressure or hypertension high blood pressure , which can lead to stroke, heart attack, and aneurysm formation. Blood pressure and osmolarity are regulated in a similar fashion. Severe hypo-osmolarity can cause problems like lysis rupture of blood cells or widespread edema, which is due to a solute imbalance. Inadequate solute concentration such as protein in the plasma results in water moving toward an area of greater solute concentration, in this case, the interstitial space and cell cytoplasm. If the kidney glomeruli are damaged by an autoimmune illness, large quantities of protein may be lost in the urine. The resultant drop in serum osmolarity leads to widespread edema that, if severe, may lead to damaging or fatal brain swelling. Severe hypertonic conditions may arise with severe dehydration from lack of water intake, severe vomiting, or uncontrolled diarrhea. When the kidney is unable to recover sufficient water from the forming urine, the consequences may be severe lethargy, confusion, muscle cramps, and finally, death. In order for vitamin D to become active, it must undergo a hydroxylation reaction in the kidney, that is, an —OH group must be added to calcidiol to make calcitriol 1,dihydroxycholecalciferol. Calcium is vitally important in bone health, muscle contraction, hormone secretion, and neurotransmitter release. Deficits may also result in problems with cell proliferation, neuromuscular function, blood clotting, and the inflammatory response. Recent research has confirmed that vitamin D receptors are present in most, if not all, cells of the body, reflecting the systemic importance of vitamin D. Many scientists have suggested it be referred to as a hormone rather than a vitamin. EPO is a amino acid protein that stimulates the formation of red blood cells in the bone marrow. The kidney produces 85 percent of circulating EPO; the liver, the remainder. If you move to a higher altitude, the partial pressure of oxygen is lower, meaning there is less pressure to push oxygen across the alveolar membrane and into the red blood cell. One way the body compensates is to manufacture more red blood cells by increasing EPO production. If you start an aerobic exercise program, your tissues will need more oxygen to cope, and the kidney will respond with more EPO. If erythrocytes are lost due to severe or prolonged bleeding, or under produced due to disease or severe malnutrition, the kidneys come to the rescue by producing more EPO. Renal failure loss of EPO production is associated with anemia, which makes it difficult for the body to cope with increased oxygen demands or to supply oxygen adequately even under normal conditions. Anemia diminishes performance and can be life threatening. Skip to main content. |
0 thoughts on “Electrolyte Balance Regulation”