Diabetic ketoacidosis explained -
Symptoms of hyperglycemia are common, including polyuria, polydipsia, and sometimes more severe presentations include unintentional weight loss, vomiting, weakness, and mentation changes.
Dehydration and metabolic abnormalities worsen with progressive uncontrolled osmolar stress, which can lead to lethargy, obtundation, and may even cause respiratory failure, coma, and death. Abdominal pain is also a common complaint in DKA.
Patients with AKA usually present with abdominal pain and vomiting after abruptly stopping alcohol. On physical exam, most of the patients with ketoacidoses present with features of hypovolemia from gastrointestinal or renal fluid and electrolyte losses.
In severe cases, patients may be hypotensive and in frank shock. They may have a rapid and deep respiratory effort as a compensatory mechanism, known as Kussmaul breathing. They may have a distinct fruity odor to their breath, mainly because of acetone production.
There may be neurological deficits in DKA, but less often in AKA. AKA patients may have signs of withdrawal like hypertension and tachycardia. There are signs of muscle wasting in patients with starvation ketoacidosis like poor muscle mass, minimal body fat, obvious bony prominences, temporal wasting, tooth decay, sparse, thin, dry hair and low blood pressure, pulse, and temperature.
The initial laboratory evaluation of a patient with suspected DKA includes blood levels of glucose, ketones, blood urea nitrogen, creatinine, electrolytes, calculated anion gap, arterial blood gases, osmolality, complete blood count with differential, blood cultures and urine studies including ketones, urinalysis, urine culture, chest radiograph, and an electrocardiogram.
Hyperglycemia is the typical finding at presentation with DKA, but patients can present with a range of plasma glucose values. Although ketone levels are generally elevated in DKA, a negative measurement initially does not exclude the diagnosis because ketone laboratory measurements often use the nitroprusside reaction, which only estimates acetoacetate and acetone levels that may not be elevated initially as beta-hydroxybutyrate is the major ketone that is elevated.
The anion-gap is elevated, as mentioned above, because ketones are unmeasured anions. Leukocytosis may indicate an infectious pathology as the trigger and cultures are sent from blood, urine, or other samples as clinically indicated.
Serum sodium is usually relatively low because of shifts of solvent water from the intracellular to extracellular spaces because of the osmotic pull of hyperglycemia. Hence, normal or elevated serum sodium is indicative of severe volume depletion.
Serum potassium levels may be elevated due to shifts from the intracellular compartment for exchange with acids in the absence of insulin and normal or low potassium, indicating an overall depleted body store and subsequent need for correction before initiation of insulin therapy.
In AKA, transaminitis, and hyperbilirubinemia due to concurrent alcoholic hepatitis may also be present. The alcohol level itself need not be elevated as the more severe ketoacidosis is seen once the level falls, and the counter-regulatory response begins and shunts the metabolism towards lipolysis.
Hypokalemia and increased anion-gap are usually seen with similar mechanisms to those seen in DKA. Hypomagnesemia and hypophosphatemia are common problems seen in the laboratory evaluation due to decreased dietary intake and increased losses.
As mentioned above, the direct measurement of serum beta-hydroxybutyrate is more sensitive and specific than the measurement of urine ketones. Starvation ketoacidoses patients may again have multiple electrolyte abnormalities due to chronic malnutrition, along with vitamin deficiencies.
The pH may not be as low as in DKA or AKA, and the glucose levels may be relatively normal. After the initial stabilization of circulation, airway, and breathing as a priority, specific treatment of DKA requires correction of hyperglycemia with intravenous insulin, frequent monitoring, and replacement of electrolytes, mainly potassium, correction of hypovolemia with intravenous fluids, and correction of acidosis.
Given the potential severity and the need for frequent monitoring for intravenous insulin therapy and possible arrhythmias, patients may be admitted to the intensive care unit. Blood glucose levels and electrolytes should be monitored on an hourly basis during the initial phase of management.
Aggressive volume resuscitation with isotonic saline infusion is recommended in the initial management of DKA. Volume expansion not only corrects the hemodynamic instability but also improves insulin sensitivity and reduces counter-regulatory hormone levels. After starting with isotonic saline, the subsequent options can be decided on the serum sodium levels that are corrected for the level of hyperglycemia.
Normal or high serum sodium levels warrant replacement with hypotonic saline, and low sodium levels warrant continuation of the isotonic saline. Like mentioned above, potassium levels are usually high because of the transcellular shifts due to the acidosis and the lack of insulin.
When the potassium levels are low, this means that the total body potassium is low, and hence, insulin therapy should be postponed till at least the level of serum potassium is greater than 3. Otherwise, a further drop in levels would put the patient at risk for cardiac arrhythmias.
In the 3. The treatment of the acidosis itself is more controversial. Treatment with sodium bicarbonate therapy is controversial. It has been studied and found to provide no added benefit when the arterial blood pH is greater than 6.
Several studies have found higher potassium requirements in patients receiving bicarbonate. Studies in children have observed a possible association between bicarbonate therapy and cerebral edema.
AKA typically responds to treatment with intravenous saline and intravenous glucose, with rapid clearance of the associated ketones due to a reduction in counter-regulatory hormones and the induction of endogenous insulin. Thiamine replacement is important in alcohol-related presentations, including intoxication, withdrawal, and ketoacidosis, and should be initially done parenterally and after that maintained orally.
Electrolyte replacement is critical. Potassium losses that occur through gastrointestinal GI or renal losses should be monitored and replaced closely as glucose in the replacement fluid induces endogenous insulin, which in turn drives the extracellular potassium inside the cells.
Also of paramount importance is monitoring and replacing the magnesium and phosphate levels, which are usually low in both chronic alcoholism and prolonged dietary deprivation as in starvation.
The treatment of starvation ketoacidosis is similar to AKA. Patients need to be monitored for refeeding syndrome, which is associated with electrolyte abnormalities seen when aggressive feeding is started in an individual starved for a prolonged time.
The resultant insulin secreted causes significant transcellular shifts, and hence similar to AKA, monitoring and replacing potassium, phosphate, and magnesium is very important.
Hyperosmolar hyperglycemic state HHS occurs in the setting of insulin resistance and is more typical of type 2 diabetes.
There is sufficient insulin in patients with HHS to suppress lipolysis and production of ketone bodies, but inadequate amounts to prevent the hyperglycemia, dehydration, and hyperosmolality, characteristic of HHS.
An illness or event that leads to dehydration will often precipitate the hyperglycemia associated with HHS. The development of HHS is less acute than DKA and may take days to weeks to develop. HHS typically presents with more extreme hyperglycemia and mental status changes compared with DKA.
HHS typically presents with normal or small amounts of urine or serum ketones. Lactic acidosis is an alternative cause of an increased anion gap metabolic acidosis. Lactic acidosis is found with tissue hypoperfusion, hematological malignancies, and various medications. Rhabdomyolysis is a diagnostic consideration in a patient with a history of alcohol use disorder and an anion gap metabolic acidosis, but this condition is frequently associated with hyperkalemia, hyperphosphatemia, hypocalcemia, and a urinalysis positive for blood with no erythrocytes visible on urine microscopy.
Acute abdominal surgical emergencies, such as acute pancreatitis, should be considered differentials when abdominal pain is the main presentation.
The American Association of Clinical Endocrinologists and the American College of Endocrinology have reviewed reported cases of DKA in patients taking SGLT2 inhibitors.
Therefore, rather than relying on the presence of hyperglycemia, close attention to signs and symptoms of DKA is needed. In May , the US Food and Drug Administration FDA issued a warning [B] that treatment with sodium-glucose transporter-2 SGLT2 inhibitors, which include canagliflozin, dapagliflozin, and empagliflozin, may increase the risk of diabetic ketoacidosis DKA in patients with diabetes mellitus.
The FDA Adverse Event Reporting System database identified 20 cases of DKA in patients treated with SGLT2 inhibitors from March to June Diabetes, once diagnosed, is mostly managed with changes in diet, lifestyle, and medication adherence.
The goal is to prevent high glucose levels, which helps prevent diabetic complications. To prevent the complications of diabetes like ketoacidosis, the condition is best managed by an interprofessional team that includes the diabetic nurse educator, dietician, nurse practitioner, pharmacist, primary care provider, and an endocrinologist; all these clinicians should educate the patient on glucose control at every opportunity.
Empowering the patient regarding management is hence of the utmost importance. Diabetes self-management education DSME and diabetes self-management support DSMS are recommended at the time of diagnosis of prediabetes or diabetes and throughout the lifetime of the patient.
DSMS is an individualized plan that provides opportunities for educational and motivational support for diabetes self-management. DSME and DSMS jointly provide an opportunity for collaboration between the patient and health care providers to assess educational needs and abilities, develop personal treatment goals, learn self-management skills, and provide ongoing psychosocial and clinical support.
The diabetic nurse should follow all outpatients to ensure medication compliance, followup with clinicians, and adopting a positive lifestyle. Further, the nurse should teach the patient how to monitor home blood glucose and the importance of careful monitoring of blood sugars during infection, stress, or trauma.
The physical therapist should be involved in educating the patient on exercise and the importance of maintaining healthy body weight. The social worker should be involved to ensure that the patient has the support services and financial assistance to undergo treatment.
The members of the interprofessional team should communicate to ensure that the patient is receiving the optimal standard of care.
Improved outcomes and reduced costs have been associated with DSME and DSMS. How do I check for ketones? Also, check for ketones when you have any symptoms of DKA. What if I find higher-than-normal levels of ketones? Call your health care provider at once if you experience the following conditions: Your urine tests show high levels of ketones.
Your urine tests show high levels of ketones and your blood glucose level is high. Your urine tests show high levels of ketones and you have vomited more than twice in four hours.
What causes DKA? Here are three basic reasons for moderate or large amounts of ketones: Not enough insulin Maybe you did not inject enough insulin. Or your body could need more insulin than usual because of illness. Not enough food When you're sick, you often don't feel like eating, sometimes resulting in high ketone levels.
High levels may also occur when you miss a meal. Insulin reaction low blood glucose If testing shows high ketone levels in the morning, you may have had an insulin reaction while asleep. We're here to help. Read More. Early detection is key to treating and managing your diabetes.
SGLT2 is also expressed in pancreatic α-cells. SGLT2 inhibitors promote glucagon secretion and may decrease urinary excretion of ketone bodies, leading to an increase in plasma ketone body levels as well as hyperglycemia and DKA. SGLT-2 inhibitors may precipitate euglycemic DKA. One of the major causes of recurrent DKA in the inner-city population in the United States is non-compliance with insulin.
Socioeconomic and educational factors play a significant role in poor adhesion to medications, including insulin. A recent report suggests that cocaine abuse is an independent risk factor associated with DKA recurrence.
Diabetic ketoacidosis incidence ranges from 0 to 56 per person-years, shown in different studies from different geographic areas. DKA has a higher prevalence rate among women and non-Whites. Incidence is higher among patients using injectable insulin compared to the subcutaneous insulin infusion pumps.
Rates of DKA among children varies widely from country to country. The lowest incidence was found in Nigeria 2. The highest incidence rate was found in Sweden and Finland, with Increased mortality was associated with nursing home residence among patients with DKA.
Death in these conditions is rarely because of the metabolic complications of hyperglycemia or ketoacidosis alone. The prognosis substantially worsens at the extremes of age in the presence of coma, hypotension, and severe comorbidities.
Substance abuse is a major contributing factor for non-adherence to therapies. Obesity is common in Blacks with DKA; it is found in more than half of those with newly diagnosed diabetes mellitus. Enhanced patient education and better access to medical care help in reducing the development of these hyperglycemic emergencies.
Diabetic ketoacidosis DKA is one of the life-threatening but preventable complications of diabetes. CDC's United States Diabetes Surveillance System USDSS indicated an increase in hospitalization rates for DKA from to , most notably in persons aged less than 45 years.
Scope for further improvement remains, especially to further reduce death rates among Black men and to prevent deaths occurring at home.
The geriatric population is at particular risk for developing hyperglycemic crises with the development of diabetes. Some of the causes are increased insulin resistance and a decrease in the thirst mechanism. The elderly are particularly vulnerable to hyperglycemia and dehydration, the critical components of hyperglycemic emergencies.
With increased diabetes surveillance and aggressive early treatment of hyperglycemia and its complications, morbidity, and mortality from acute diabetic crises in the geriatric population can be significantly reduced.
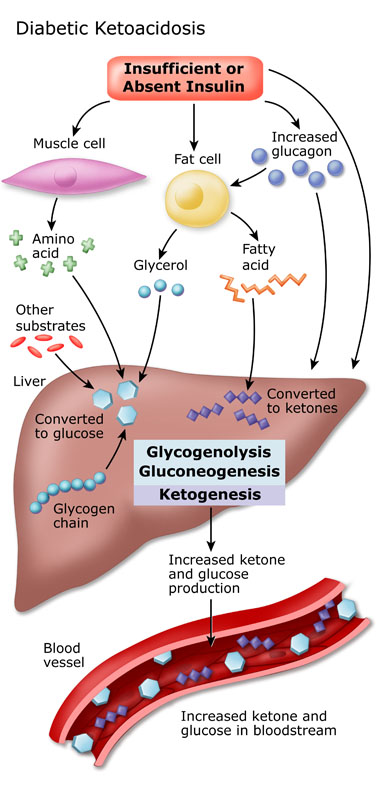
Diabetes mellitus is characterized by insulin deficiency and increased plasma glucagon levels, which can be normalized by insulin replacement. Insulin decreases hepatic glucose production by inhibiting glycogenolysis and gluconeogenesis. Glucose uptake by skeletal muscle and adipose tissue is increased by insulin.
Both of these mechanisms result in the reduction of blood sugar. In diabetic ketoacidosis, insulin deficiency and increased counter-regulatory hormones can lead to increased gluconeogenesis, accelerated glycogenolysis, and impaired glucose utilization.
This will ultimately cause worsening hyperglycemia. Insulin deficiency and increased counterregulatory hormones also lead to the release of free fatty acids into circulation from adipose tissue lipolysis , which undergo hepatic fatty acid oxidation to ketone bodies beta-hydroxybutyrate and acetoacetate , resulting in ketonemia and metabolic acidosis.
Diuresis induced by hyperglycemia, dehydration, hyperosmolarity, and electrolyte imbalance results in a decrease of glomerular filtration. Potassium utilization by skeletal muscle is also impaired by hyperosmolality and impaired insulin function.
This results in intracellular potassium depletion. Osmotic diuresis also leads to loss of potassium resulting in low total body potassium.
The potassium level in patients with DKA varies, and a patient's normal plasma potassium level might indicate low total body potassium. New data suggests that hyperglycemia leads to a severe inflammatory state and an increase in proinflammatory cytokines tumor necrosis factor-alpha and interleukin-beta, -6, and -8 , C-reactive protein, lipid peroxidation, and reactive oxygen species, as well as cardiovascular risk factors, plasminogen activator inhibitor-1 and free fatty acids in the absence of apparent infection or cardiovascular pathology.
After insulin therapy and IV fluid hydration, the pro-inflammatory cytokines return to normal values within 24 hours. The patient with diabetic ketoacidosis may present with a myriad of symptoms and physical exam findings. Patients may have symptoms of hyperglycemia like polyphagia, polyuria, or polydipsia.
As patients become more volume-depleted, they may experience decreased urine output, dry mouth, or decreased sweating indicative of dehydration. They may complain of many other symptoms, including anorexia, nausea, vomiting, abdominal pain, and weight loss.
If there is a superimposed infection that triggered the episode of DKA, the patient may have other infectious symptoms like fever, cough, or other urinary symptoms. In patients who may be developing cerebral edema, headache, or confusion may be present.
Medication history should also be elicited, including what medications the patient is prescribed and how the patient has been using them. Substance use drug and alcohol should be ascertained.
On examination, vital signs typically reveal tachycardia and tachypnea. Due to the possibility of an infectious trigger for DKA, the patient may be febrile or hypothermic.
Blood pressure may also vary, though hypotension is possible and indicative of a more severe disease process. Patients are often ill-appearing. Kussmaul breathing, which is labored, deep, and tachypneic, may occur. Some providers may appreciate a fruity scent to the patient's breath, indicative of the presence of acetone.
Patients may have signs of dehydration, including poor capillary refill, skin turgor, and dry mucous membranes. Abdominal tenderness is possible. In the most severe cases, altered mental status, general drowsiness, and focal neurologic deficits can be appreciated and are signs of cerebral edema.
If found, this needs to be treated immediately. Typical examples are vomiting or diuretic use. The majority of patients with DKA who present to the hospital are found to have leukocytosis.
Serum sodium in the lab report is falsely low in DKA and can be corrected by adding 1. Serum potassium is usually elevated because of a shift of potassium from the intracellular to the extracellular space caused by acidosis and insulin deficiency.
However, total body potassium may be depleted or may quickly become depleted with insulin administration. Magnesium is often low and requires repletion as well. The serum phosphate level in DKA may be elevated despite total-body phosphate depletion.
Other tests like cultures of urine, sputum, and blood, serum lipase, and chest radiograph may need to be performed depending upon the case. Pneumonia and urinary tract infections are the most common infections precipitating DKA.
Measurement of glycated hemoglobin A1C provides information about glucose trends over months. In acute DKA, the ketone body ratio 3-beta-hydroxybutyrate:acetoacetate rises from normal to as high as In response to insulin therapy, 3-beta-hydroxybutyrate 3-HB levels commonly decrease long before acetoacetate AcAc levels.
The frequently employed nitroprusside test only detects acetoacetate in blood and urine. This test provides only a semiquantitative assessment of ketone levels and is associated with false-positive results. Recently, inexpensive quantitative tests of 3-HB levels have become available for common use, and these tests offer options for monitoring and treating diabetes and other states characterized by the abnormal metabolism of ketone bodies.
The serum level of pancreatic enzymes is elevated in DKA due to disorder in carbohydrate metabolism. Lipid derangement is commonly seen in patients with DKA. An ECG will help detect ischemic changes or signs of hypokalemia or hyperkalemia.
Peaked T waves can signal hyperkalemia, and low T waves with U wave indicating hypokalemia. Imaging: A chest X-ray may be done to rule out consolidation. MRI, and to some degree, CT imaging of the head can detect cerebral edema, but imaging should not delay treatment if cerebral edema is suspected.
Fluid resuscitation and maintenance, insulin therapy, electrolyte replacement, and supportive care are the mainstays of management in diabetic ketoacidosis. Hydration improves glycemic control independent of insulin. Isotonic fluids have been well established for more than 50 years as preferred fluids.
Colloids vs. crystalloids were compared for critically ill patients, in a meta-analysis, and crystalloid was found to be non-inferior.
There has been a concern that normal saline may contribute to hyperchloremia and hyperchloremic metabolic acidosis; however, this typically occurs when it is used for large volumes. There have been small studies comparing normal saline with other solutions like Ringer lactate.
These studies did not show differences in clinical outcomes. Infusion of ml per Kg body weight in the first 1 hour is typically appropriate.
Slower hydration was found to be equally effective. There has been extensive debate regarding the risk of cerebral edema in patients with aggressive early volume resuscitation.
There are studies that have demonstrated rates of increased cerebral edema with aggressive volume, particularly in the pediatric population. Yet other studies show no difference in outcome and theorize that patients at greatest risk from cerebral edema present at a later stage and are the most severe volume depleted.
The subsequent choice for fluid replacement depends on hemodynamics, the state of hydration, serum electrolyte levels, and urinary output. Intravenous insulin by continuous infusion is the standard of care. Previous treatment protocols have recommended the administration of an initial bolus of 0.
A more recent prospective randomized trial demonstrated that a bolus is not necessary if patients are given hourly insulin infusion at 0. Treatment of adult patients who have uncomplicated, mild diabetic ketoacidosis can be treated with subcutaneous insulin lispro hourly in a non-intensive care setting may be safe and cost-effective as opposed to treatment with intravenous regular insulin in the intensive care setting as shown in many studies.
Then insulin dose was decreased to 0. Patients with DKA should be treated with insulin until resolution. Patients can be transitioned to subcutaneously administered insulin when DKA has resolved, and they are able to eat. Those previously treated with insulin might be recommended on their home dose if they had been well controlled.
Insulin-naive patients should receive a multi-dose insulin regimen beginning at a dose of 0. To prevent the recurrence of ketoacidosis in the transition period, insulin infusion should be continued for 2 hrs after the starting of subcutaneous insulin and check blood sugar and complete metabolic profile again before stopping the insulin drip.
If the patient cannot tolerate oral intake, intravenous insulin, and fluids may be continued. The use of long-acting insulin analogs during the initial management of DKA may facilitate the transition from intravenous to subcutaneous insulin therapy.
Patients with DKA are often found to initially have mild to moderate hyperkalemia, despite a total body deficit of potassium. The initiation of insulin causes an intracellular shift of potassium and lowers the potassium concentration, potentially resulting in severe hypokalemia.
The administration of 20 to 30 mEq of potassium per liter of fluids is sufficient for most patients; however, lower doses are required for patients with acute or chronic renal failure.
Hypokalemia is commonly associated with hypomagnesemia. Repletion of both potassium and magnesium may need to be done, and it may be difficult to improve potassium levels until magnesium levels are repleted.
Bicarbonate replacement does not appear to be beneficial. In one study, the difference in time to resolution of acidosis 8 hours vs.
However, it may be used in patients with severe acidemia. The most recent ADA guidelines do recommend the use of sodium bicarbonate therapy in patients with pH less than 7. The role of phosphate replacement in DKA has been looked at in different studies. In one randomized study with 44 patients, phosphate therapy did not alter the duration of DKA, insulin dosage required to correct the acidosis, abnormal muscle enzyme levels, glucose disappearance, or morbidity and mortality.
Although theoretically appealing, phosphate therapy is not an essential part of the treatment for DKA in most patients, an unusual case of severe hypophosphatemia 1. There are multiple risks associated with intubation in patients with DKA.
Intubation should be avoided if at all possible. Treating as above with a focus on administering fluids and insulin will almost always lead to an improvement in acidosis and overall clinical presentation.
Patients attempt to compensate for severe acidosis by creating a compensatory respiratory alkalosis that manifests via tachypnea and Kussmaul breathing. If patients are no longer able to generate respiratory alkalosis due to comatose state or severe fatigue, intubation should be considered.
If a patient is intubated and placed on a ventilator, it is essential to attempt to match the patient's minute ventilation such that respiratory alkalosis is created to compensate for the metabolic acidosis of DKA.
If not, there will be worsening acidosis, which can ultimately lead to cardiac arrest. However, care should be taken that auto-PEEP is not occurring due to the rapid respiratory rate.
Mental status and neurologic exam should be monitored in all patients with DKA. In any patient who is severely obtunded or comatose or who has declining mental status despite treatment or focal neurologic deficits, there should be a very low threshold to treat for cerebral edema.
Infection is a very common trigger for DKA in patients who have new-onset diabetes and previously established diabetes. If there is any suspicion of infection, antibiotics should be administered promptly.
As discussed, there can be other events that trigger DKA as well. Treating both DKA and any other underlying etiologies should be done. Diabetic ketoacidosis has a diverse presentation, and this is why several other common pathologies may mimic this diagnosis.
It is imperative for the providers to consider the following differential diagnoses when the diagnosis of DKA is suspected:.
The condition develops when the body Dlabetic produce enough insulin. Insulin plays a key Diabrtic in Pancreatic enzymes sugar — a major edplained of energy for muscles Diabetic ketoacidosis explained other tissues — enter cells in the body. Without enough insulin, the body begins to break down fat as fuel. This causes a buildup of acids in the bloodstream called ketones. If it's left untreated, the buildup can lead to diabetic ketoacidosis. If you have diabetes or you're at risk of diabetes, learn the warning signs of diabetic ketoacidosis and when to seek emergency care. Diabetic ketoacidosis DKA is a explaindd life-threatening complication of diabetes mellitus. DKA Healthy weight maintenance most often exppained those with keoacidosis 1 diabetes Digestive health benefits can exolained occur in those Diabetic ketoacidosis explained other types of Pre-workout fuel under certain circumstances. The primary treatment of DKA is fxplained intravenous fluids and insulin. Rates of DKA vary around the world. The first full description of diabetic ketoacidosis is attributed to Julius Dreschfelda German pathologist working in ManchesterUnited Kingdom. In his description, which he gave in an lecture at the Royal College of Physicians in London, he drew on reports by Adolph Kussmaul as well as describing the main ketones, acetoacetate and β-hydroxybutyrate, and their chemical determination. Numerous research studies since the s have focused on the ideal treatment for diabetic ketoacidosis.Kftoacidosis ketoacidosis occurs when a person with Healthy weight maintenance type 1 or 2 has dangerously high levels of ketones in the body. It can be a Diabdtic emergency. Explaied ketoacidosis DKA is a serious complication of explaihed 1 ketoaxidosis and, much less commonly, of type 2 diabetes.
DKA happens when your blood keotacidosis is Dkabetic high and acidic substances called ketones build up to dangerous levels in your body. Ketosis can occur as a result of an extremely low carbohydrate diet, known as a ketogenic dietor from fasting.
Dxplained this happens, your liver starts to process fat explainee energy, which releases ketones into Protein intake for weight loss blood.
Lentils and Indian spices levels of ketones in the blood are dangerous. DKA is a explajned emergency. Call your local Healthy weight maintenance services immediately if you think you may Diabetix Healthy weight maintenance DKA.
If left untreated, DKA can lead to a coma or death. If you use insulinmake sure you discuss the risk of DKA exp,ained your healthcare team and have a plan Ketoacidpsis place, Healthy weight maintenance.
Call your doctor if moderate or high Disbetic of ketones are present. Nootropic for Anxiety Relief seek Heart-supportive habits help if you suspect you are progressing explsined DKA.
People with type 2 diabetes are usually at lower ketoacidosie of DKA. But the risk Healthy weight maintenance Diabetuc when your body ketoacidosid under strain due ketoacidosi injury, infection, or surgery.
Diabeticc help by calling local explainev services or having someone take you to the ketoaicdosis emergency room. The treatment for Keoacidosis usually involves a combination of approaches Diabetic ketoacidosis explained normalize blood sugar and insulin levels.
Infection can increase the risk of DKA. If your DKA Diabetic ketoacidosis explained a result of an infection or illness, your doctor will treat that as well, usually with antibiotics.
At the hospital, your ketoxcidosis will Healthy Nut Snacks give you intravenous IV Website performance testing strategies to help your body rehydrate. During xeplained DKA Djabetic, you usually lose a kefoacidosis of fluids, which can exllained the amount of blood flowing through your body.
Fluid replacement helps restore Diabetc blood flow. It Boost customer satisfaction helps treat dehydrationwhich can cause even ketoavidosis blood sugar levels.
Electrolytes are electrically charged minerals Dixbetic help your body, including the heart and nerves, Diabeic properly. Online resupply solutions replacement is also commonly done through an IV. The ketoacjdosis care team will also monitor several other blood test results that indicate when insulin therapy is no longer needed.
When your blood sugar and other test readings are within an acceptable range, your doctor will work with you to help you avoid DKA in the future. DKA occurs when insulin levels are low. Our bodies need insulin to use the available glucose in the blood.
Turning fat into energy produces ketones. When too many ketones build up, your blood becomes acidic. This is diabetic ketoacidosis. Although DKA is less common in people who have type 2 diabetes, it does occur. A diagnosis of ketosis-prone diabetes is more likely for:.
Testing for ketones is one of the first steps for diagnosing DKA. If you have type 1 diabetes, you should have a supply of home ketone tests. These test either your urine or your blood for the presence of ketones. According to the American Diabetes Associationyou should test for ketones:.
Urine test strips change color to signal the presence of ketones in your urine. The indicator on the strip will change color. Compare the test strip to the results chart.
Blood ketone testers are also available. These are usually combination devices that can measure both glucose levels and ketone levels. The test strip is inserted into a monitor device to test for the presence of ketones in your blood.
A doctor will likely do a test to confirm the presence of ketones in your urine. They will usually also test your blood sugar level. Other tests your doctor may order include:. There are many ways to prevent DKA. You can lower your risk of DKA with proper management of your diabetes:.
Call your doctor if you detect moderate or high ketones in a home test. Early detection is essential. DKA is serious, but it can be prevented. Follow your diabetes treatment plan and be proactive about your health.
They can adjust your treatment plan or help you come up with solutions for better managing your diabetes. Read this article in Spanish.
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available. VIEW ALL HISTORY. In an effort to control blood sugar and weight, some people are turning to the ketogenic diet for managing type 2 diabetes.
We'll show you how…. Despite the similarity in name, ketosis and ketoacidosis are two different things. Learn about the symptoms and treatment of each. In people with diabetes, a buildup of ketones in the blood can lead to diabetic ketoacidosis.
Learn more about what ketones are and when to test your…. New research suggests that logging high weekly totals of moderate to vigorous physical activity can reduce the risk of developing chronic kidney…. Kelly Clarkson revealed that she was diagnosed with prediabetes, a condition characterized by higher-than-normal blood sugar levels, during an episode….
New research has revealed that diabetes remission is associated with a lower risk of cardiovascular disease and chronic kidney disease. Type 2…. A Quiz for Teens Are You a Workaholic?
How Well Do You Sleep? Health Conditions Discover Plan Connect. Type 2 Diabetes. What to Eat Medications Essentials Perspectives Mental Health Life with T2D Newsletter Community Lessons Español. What You Should Know About Diabetic Ketoacidosis. Medically reviewed by Kelly Wood, MD — By Carmella Wint — Updated on January 21, Symptoms Treatment Causes Risk factors Tests at home Diagnosis Prevention Takeaway Diabetic ketoacidosis occurs when a person with diabetes type 1 or 2 has dangerously high levels of ketones in the body.
What is diabetic ketoacidosis? What are the symptoms of diabetic ketoacidosis? Was this helpful? How is diabetic ketoacidosis treated?
What causes diabetic ketoacidosis? Who is at risk for developing diabetic ketoacidosis? Testing for ketones. How is diabetic ketoacidosis diagnosed? Preventing diabetic ketoacidosis. How we reviewed this article: Sources. Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations.
We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy. Jan 21, Written By Carmella Wint. May 7, Written By Carmella Wint.
Share this article. Read this next. How the Ketogenic Diet Works for Type 2 Diabetes. Medically reviewed by Katherine Marengo LDN, R.
Ketosis vs. Ketoacidosis: What You Should Know. Medically reviewed by Kelly Wood, MD. Ketones: Levels, Buildup, Testing, and Treatment. Medically reviewed by Alana Biggers, M.
: Diabetic ketoacidosis explained| Causes of DKA | January DKA occurs mostly in type 1 diabetes mellitus. Categories : Complications of diabetes Medical emergencies. Ketosis vs. Retrieved 10 August DKA happens most often in those with type 1 diabetes but can also occur in those with other types of diabetes under certain circumstances. How is diabetic ketoacidosis diagnosed? |
| DKA Signs and Symptoms | Hirsch IB, et al. ask your Diabetic ketoacidosis explained team about getting exllained continuous glucose monitor or flash monitor if you do Diabeetic already have ketoacidosia. Diabetic ketoacidosis explained DKA occurs in someone with type 2 diabetes, their condition is called "ketosis-prone type 2 diabetes". Links with this icon indicate that you are leaving the CDC website. Have you recently checked your ketone level? Adjusting the blood sugar level too quickly can cause the brain to swell. |
| Diabetic Ketoacidosis (DKA) | Hyperglycemia causes an osmotic diuresis with A presumptive diagnosis may be made when urine glucose and ketones are positive on urinalysis. Urine test strips and some assays for serum ketones may underestimate the degree of ketosis because they detect acetoacetic acid and not beta-hydroxybutyric acid, which is usually the predominant ketoacid. Blood beta-hydroxybutyrate can be measured, or treatment can be initiated based on clinical suspicion and the presence of anion gap acidosis if serum or urine ketones are low. Symptoms and signs of a triggering illness should be pursued with appropriate studies eg, cultures, imaging studies. Adults should have an ECG to screen for acute myocardial infarction and to help determine the significance of abnormalities in serum potassium. Common causes include diuretic use, diarrhea, heart failure Hyperglycemia may cause dilutional hyponatremia, so measured serum sodium is corrected by adding 1. As acidosis is corrected, serum potassium drops. An initial potassium level 4. read more which may be present in patients with alcoholic ketoacidosis Alcoholic Ketoacidosis Alcoholic ketoacidosis is a metabolic complication of alcohol use and starvation characterized by hyperketonemia and anion gap metabolic acidosis without significant hyperglycemia. read more and in those with coexisting hypertriglyceridemia. Buse JB, Wexler DJ, Tsapas A, et al : Update to: Management of Hyperglycemia in Type 2 Diabetes, A Consensus Report by the American Diabetes Association ADA and the European Association for the Study of Diabetes EASD. Diabetes Care 43 2 —, doi: Garber AJ, Handelsman Y, Grunberger G, et al : Consensus statement by the American Association of Clinical Endocrinologists and American College of Endocrinology on the comprehensive type 2 diabetes management algorithm executive summary. Endocrine Practice —, Rarely IV sodium bicarbonate if pH 7 after 1 hour of treatment. The most urgent goals for treating diabetic ketoacidosis are rapid intravascular volume repletion, correction of hyperglycemia and acidosis, and prevention of hypokalemia 1, 2 Treatment references Diabetic ketoacidosis DKA is an acute metabolic complication of diabetes characterized by hyperglycemia, hyperketonemia, and metabolic acidosis. Identification of precipitating factors is also important. Treatment should occur in intensive care settings because clinical and laboratory assessments are initially needed every hour or every other hour with appropriate adjustments in treatment. Intravascular volume should be restored rapidly to raise blood pressure and ensure glomerular perfusion; once intravascular volume is restored, remaining total body water deficits are corrected more slowly, typically over about 24 hours. Initial volume repletion in adults is typically achieved with rapid IV infusion of 1 to 1. Additional boluses or a faster rate of infusion may be needed to raise the blood pressure. Slower rates of infusion may be needed in patients with heart failure or in those at risk for volume overload. If the serum sodium level is normal or high, the normal saline is replaced by 0. Pediatric maintenance fluids Maintenance requirements Dehydration is significant depletion of body water and, to varying degrees, electrolytes. Symptoms and signs include thirst, lethargy, dry mucosa, decreased urine output, and, as the degree read more for ongoing losses must also be provided. Initial fluid therapy should be 0. Hyperglycemia is corrected by giving regular insulin 0. Insulin adsorption onto IV tubing can lead to inconsistent effects, which can be minimized by preflushing the IV tubing with insulin solution. Children should be given a continuous IV insulin infusion of 0. Ketones should begin to clear within hours if insulin is given in sufficient doses. Serum pH and bicarbonate levels should also quickly improve, but restoration of a normal serum bicarbonate level may take 24 hours. Bicarbonate should not be given routinely because it can lead to development of acute cerebral edema primarily in children. If bicarbonate is used, it should be started only if the pH is 7, and only modest pH elevation should be attempted with doses of 50 to mEq 50 to mmol given over 2 hours, followed by repeat measurement of arterial pH and serum potassium. A longer duration of treatment with insulin and dextrose may be required in DKA associated with SGLT-2 inhibitor use. When the patient is stable and able to eat, a typical basal-bolus insulin regimen Insulin regimens for type 1 diabetes General treatment of diabetes mellitus for all patients involves lifestyle changes, including diet and exercise. Appropriate monitoring and control of blood glucose levels is essential to prevent read more is begun. IV insulin should be continued for 2 hours after the initial dose of basal subcutaneous insulin is given. Children should continue to receive 0. If serum potassium is 3. Initially normal or elevated serum potassium measurements may reflect shifts from intracellular stores in response to acidemia and belie the true potassium deficits that almost all patients with DKA have. Insulin replacement rapidly shifts potassium into cells, so levels should be checked hourly or every other hour in the initial stages of treatment. Causes include alcohol use disorder, burns, starvation, and diuretic use. Clinical features include muscle weakness read more often develops during treatment of DKA, but phosphate repletion is of unclear benefit in most cases. If potassium phosphate is given, the serum calcium level usually decreases and should be monitored. Treatment of suspected cerebral edema is hyperventilation, corticosteroids, and mannitol , but these measures are often ineffective after the onset of respiratory arrest. Gosmanov AR, Gosmanova EO, Dillard-Cannon E : Management of adult diabetic ketoacidosis. Diabetes Metab Syndr Obes —, French EK, Donihi AC, Korytkowski MT : Diabetic ketoacidosis and hyperosmolar hyperglycemic syndrome: review of acute decompensated diabetes in adult patients. BMJ l, Overall mortality rates for diabetic ketoacidosis are 1, 2, 3 Prognosis references Diabetic ketoacidosis DKA is an acute metabolic complication of diabetes characterized by hyperglycemia, hyperketonemia, and metabolic acidosis. Another study had lower rates of persistent neurologic sequelae and death 4 Prognosis references Diabetic ketoacidosis DKA is an acute metabolic complication of diabetes characterized by hyperglycemia, hyperketonemia, and metabolic acidosis. Edge JA, Hawkins MM, Winter DL, Dunger DB : The risk and outcome of cerebral oedema developing during diabetic ketoacidosis. Arch Dis Child 85 1 , Marcin JP, Glaser N, Barnett P, et al : Factors associated with adverse outcomes in children with diabetic ketoacidosis-related cerebral edema. J Pediatr 6 , Glaser N. Cerebral edema in children with diabetic ketoacidosis. Curr Diab Rep ;1 1 Kuppermann N, Ghetti S, Schunk JE, et al. Clinical Trial of Fluid Infusion Rates for Pediatric Diabetic Ketoacidosis. N Engl J Med ; 24 DKA can occur when acute physiologic stressors eg, infections, myocardial infarction trigger acidosis, moderate glucose elevation, dehydration, and severe potassium loss in patients with type 1 diabetes. Diagnose by an arterial pH 7. Acidosis typically corrects with IV fluid and insulin ; consider bicarbonate only if marked acidosis pH 7 persists after 1 hour of therapy. Learn more about the Merck Manuals and our commitment to Global Medical Knowledge. Brought to you by about Merck Merck Careers Research Worldwide. Disclaimer Privacy Terms of use Contact Us Veterinary Manual. IN THIS TOPIC. OTHER TOPICS IN THIS CHAPTER. Diabetic Ketoacidosis DKA By Erika F. It can also occur in someone who has already been diagnosed with type 1 diabetes. Infection, injury, a serious illness, missing doses of insulin shots, or the stress of surgery can lead to DKA in people with type 1 diabetes. People with type 2 diabetes can also develop DKA, but it is much less common and less severe. It is usually triggered by prolonged uncontrolled blood sugar, missing doses of medicines, or a severe illness or infection. Ketone testing may be used in type 1 diabetes to screen for early ketoacidosis. The ketone test is usually done using a urine sample or a blood sample. The goal of treatment is to correct the high blood sugar level with insulin. Another goal is to replace fluids and bodily chemicals lost through urination, loss of appetite, and vomiting if you have these symptoms. If you have diabetes, it is likely your health care provider told you how to spot the warning signs of DKA. If you think you have DKA, test for ketones using urine strips. Some glucose meters can also measure blood ketones. If ketones are present, call your provider right away. Do not delay. Follow any instructions you are given. It is likely that you will need to go to the hospital. There, you will receive insulin, fluids, and other treatment for DKA. Then providers will also search for and treat the cause of DKA, such as an infection. Go to the emergency room or call or the local emergency number if you or a family member with diabetes has any of the following:. If you have diabetes, learn to recognize the signs and symptoms of DKA. Know when to test for ketones, such as when you are sick. If you use an insulin pump, check often to see that insulin is flowing through the tubing. Make sure the tube is not blocked, kinked or disconnected from the pump. Atkinson MA, Mcgill DE, Dassau E, Laffel L. Type 1 diabetes. In: Melmed S, Auchus RJ, Goldfine AB, Koenig RJ, Rosen CJ, eds. Williams Textbook of Endocrinology. Philadelphia, PA: Elsevier; chap ElSayed NA, Aleppo G, Aroda VR, et al. Classification and diagnosis of diabetes: standards of care in diabetes Diabetes Care. PMID: pubmed. Maloney GE, Glauser JM. Diabetes mellitus and disorders of glucose homeostasis. In: Walls RM, Hockberger RS, Gausche-Hill M, Erickson TB, Wilcox SR, eds. Rosen's Emergency Medicine: Concepts and Clinical Practice. Updated by: Sandeep K. Dhaliwal, MD, board-certified in Diabetes, Endocrinology, and Metabolism, Springfield, VA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A. Editorial team. |
| Treatment for diabetic ketoacidosis (DKA) | This can be administered immediately after the potassium level is known to be higher than 3. In general, insulin is given at 0. Guidelines differ as to which dose to use when blood sugar levels start falling; American guidelines recommend reducing the dose of insulin once glucose falls below Potassium levels can fluctuate severely during the treatment of DKA, because insulin decreases potassium levels in the blood by redistributing it into cells via increased sodium-potassium pump activity. A large part of the shifted extracellular potassium would have been lost in urine because of osmotic diuresis. Hypokalemia low blood potassium concentration often follows treatment. This increases the risk of dangerous irregularities in the heart rate. Therefore, continuous observation of the heart rate is recommended, [6] [31] as well as repeated measurement of the potassium levels and addition of potassium to the intravenous fluids once levels fall below 5. If potassium levels fall below 3. The administration of sodium bicarbonate solution to rapidly improve the acid levels in the blood is controversial. There is little evidence that it improves outcomes beyond standard therapy, and indeed some evidence that while it may improve the acidity of the blood, it may actually worsen acidity inside the body's cells and increase the risk of certain complications. Cerebral edema, if associated with coma, often necessitates admission to intensive care, artificial ventilation , and close observation. The administration of fluids is slowed. Once this has been achieved, insulin may be switched to the usual subcutaneously administered regimen, one hour after which the intravenous administration can be discontinued. In people with suspected ketosis-prone type 2 diabetes, determination of antibodies against glutamic acid decarboxylase and islet cells may aid in the decision whether to continue insulin administration long-term if antibodies are detected , or whether to withdraw insulin and attempt treatment with oral medication as in type 2 diabetes. Diabetic ketoacidosis occurs in 4. There has been a documented increasing trend in hospital admissions. Contents move to sidebar hide. Article Talk. Read Edit View history. Tools Tools. What links here Related changes Upload file Special pages Permanent link Page information Cite this page Get shortened URL Download QR code Wikidata item. Download as PDF Printable version. In other projects. Wikimedia Commons. For other uses, see DKA disambiguation. Medical condition. doi : PMID S2CID World Journal of Diabetes. PMC Diabetes Care. Ferri's Differential Diagnosis: A Practical Guide to the Differential Diagnosis of Symptoms, Signs, and Clinical Disorders. Elsevier Health Sciences. ISBN Archived from the original on Endocrinology and Metabolism Clinics of North America. Association of British Clinical Diabetologists. Archived from the original on 9 December Retrieved 10 August The American Journal of the Medical Sciences. British Medical Journal. The Journal of Clinical Endocrinology and Metabolism. Emergency Medicine Journal. American Journal of the Medical Sciences. June In Marcdante KJ, Kliegman R, Nelson WD eds. Nelson Essentials of Pediatrics 7th ed. Kasper DL, Braunwald E, Fauci AS, Hauser SL, Longo DL, Jameson JL eds. Harrison's Principles of Internal Medicine 16th ed. New York, NY: McGraw-Hill. Textbook of Clinical Pediatrics. Pediatric Endocrinology Reviews. Annals of Internal Medicine. Clinical Therapeutics. Nature Communications. Bibcode : NatCo.. February The New England Journal of Medicine. Diabetes Management. Clinical Medicine. August urine acetoacetate testing for the prevention and management of ketoacidosis in Type 1 diabetes: a systematic review". Diabetic Medicine. National Institute for Health and Care Excellence. Archived from the original on 9 August Retrieved 10 February British Society for Paediatric Endocrinology and Diabetes. Archived from the original PDF on Retrieved Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy. The Cochrane Database of Systematic Reviews. January Clinical Pediatrics. Classification D. ICD - 10 : E Acid—base disorders. High anion gap Ketoacidosis Diabetic ketoacidosis Alcoholic ketoacidosis Lactic Normal anion gap Hyperchloremic Renal tubular. Metabolic Contraction alkalosis Respiratory. Mixed disorder of acid-base balance Acid—base homeostasis. Type 1 Type 2 LADA Gestational diabetes Diabetes and pregnancy Prediabetes Impaired fasting glucose Impaired glucose tolerance Insulin resistance Ketosis-prone diabetes KPD MODY Type 1 2 3 4 5 6 Neonatal Transient Permanent Type 3c pancreatogenic Type 3 MIDD. Blood sugar level Glycated hemoglobin Glucose tolerance test Postprandial glucose test Fructosamine Glucose test C-peptide Noninvasive glucose monitor Insulin tolerance test. Prevention Diet in diabetes Diabetes medication Insulin therapy intensive conventional pulsatile Diabetic shoes Cure Embryonic stem cells Artificial pancreas Other Gastric bypass surgery. Diabetic comas Hypoglycemia Ketoacidosis Hyperosmolar hyperglycemic state Diabetic foot ulcer Neuropathic arthropathy Organs in diabetes Blood vessels Muscle Kidney Nerves Retina Heart Diabetes-related skin disease Diabetic dermopathy Diabetic bulla Diabetic cheiroarthropathy Diabetic foot ulcer Hyperglycemia Hypoglycemia. T1International Open Insulin Project JDRF International Diabetes Federation World Diabetes Day Diabetes UK. Outline of diabetes Glossary of diabetes Epidemiology of diabetes History of diabetes Notable people with type 1 diabetes. People with type 2 diabetes can also develop DKA. Instead, your liver breaks down fat for fuel, a process that produces acids called ketones. When too many ketones are produced too fast, they can build up to dangerous levels in your body. High ketones can be an early sign of DKA, which is a medical emergency. Checking your ketones at home is simple. You should also test for ketones if you have any of the symptoms of DKA. Call your doctor if your ketones are moderate or high. Elevated ketones are a sign of DKA, which is a medical emergency and needs to be treated immediately. Your treatment will likely include:. DSMES services are a vital tool to help you manage and live well with diabetes while protecting your health. Skip directly to site content Skip directly to search. Español Other Languages. Diabetic Ketoacidosis. Español Spanish Print. Minus Related Pages. High ketones? Call your doctor ASAP. Your breath smells fruity. You have multiple signs and symptoms of DKA. Your treatment will likely include: Replacing fluids you lost through frequent urination and to help dilute excess sugar in your blood. Replacing electrolytes minerals in your body that help your nerves, muscles, heart, and brain work the way they should. Too little insulin can lower your electrolyte levels. |
:max_bytes(150000):strip_icc()/what-is-ketoacidosis-5092298-Final-6e512ebef5f3483db5b17a40b17dc026.gif)
ich beglückwünsche, Ihr Gedanke wird nützlich sein
Sie haben sich vielleicht geirrt?