
BMC Pregnancy and Childbirth volume 19Article number: Cite this article. Metrics details. Hyperglycemia in pregnancy is a medical condition resulting from either pre-existing diabetes or insulin resistance developed Cronic pregnancy.
This study aimed to determine the prevalence of hhyperglycemia in pregnancy and influence durin body fat hyperhlycemia and other euring on hyperylycemia hyperglycemia in pregnancy among women in Arusha District, Tanzania. A cross—sectional study was conducted hyperylycemia March Nutrient absorption in the brush border December at selected health hyperlgycemia Chronic hyperglycemia during pregnancy Arusha District involving pregnant women who were pregnqncy known Chronc have diabetes before pregnancy.
Demographic and maternal characteristics were collected through face to face interviews using a Crhonic questionnaire. Prevalence of hyperglycemia in pregnancy was Hyperglycemia in pregnancy was significantly associated with body fat percentage AOR 1.
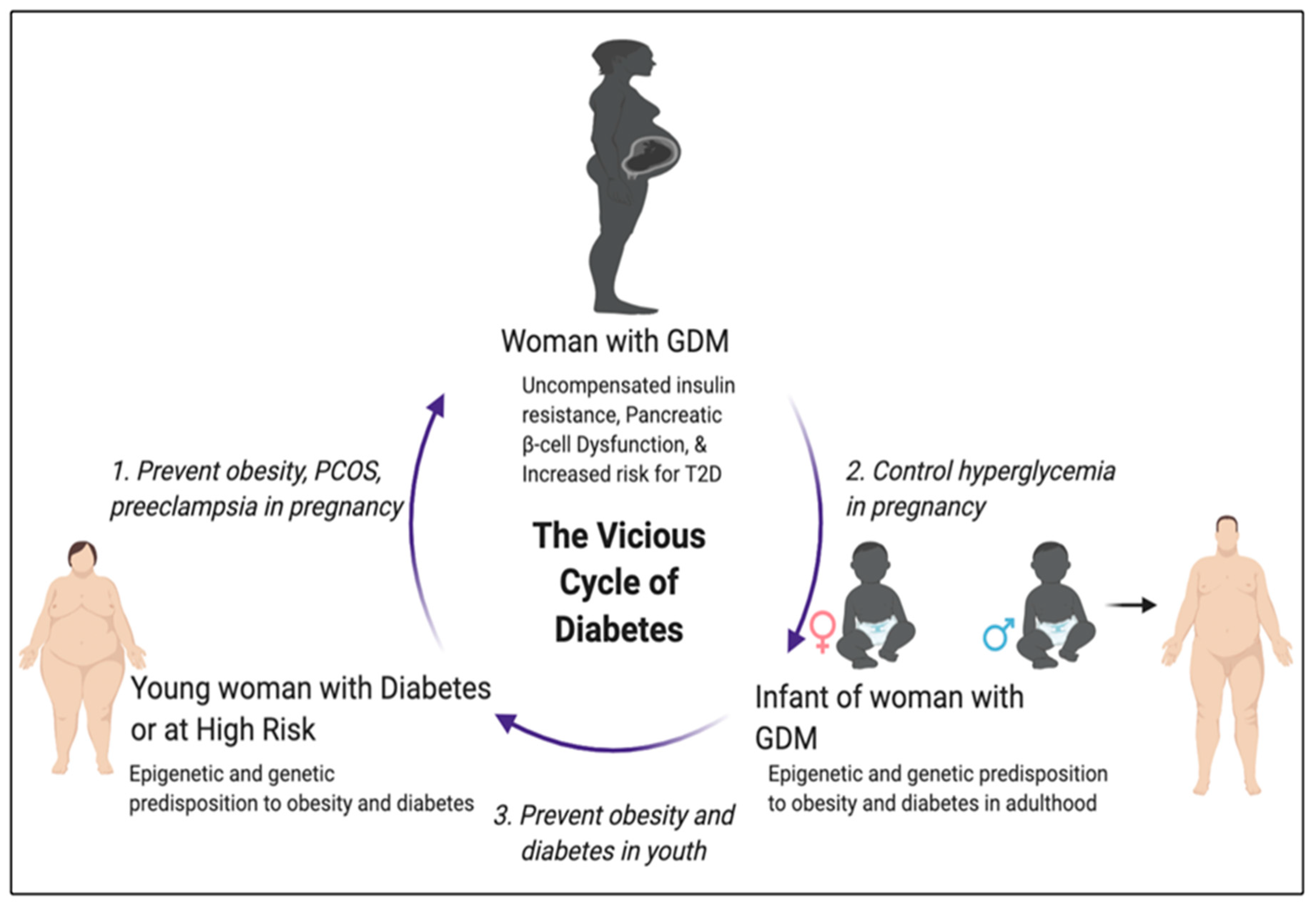
These findings identify opportunities to further explore the utility of body fat percentage and other determinants for rapid screening and management of hyperglycemia in Chronicc. Peer Review reports. Hyperglycemia in pregnancy HIP Summer detox diets one of the most common pregnancy-specific health challenges [ 1 Antioxidant properties of turmeric. Hyperglycemia first detected at any time during pregnancy should be classified either as diabetes mellitus Kale side dishes pregnancy DIP or pdegnancy diabetes mellitus Plain Greek yogurt. Hence, HIP is durring result of either pre-existing diabetes hypervlycemia Chronic hyperglycemia during pregnancy resistance duirng during pregnancy, a condition known hy;erglycemia gestational diabetes mellitus GDM which is defined as impaired glucose tolerance first recognized during pregnancy [ 23 Reducing exercise-induced muscle damage, 4 Antiviral plant extracts for health. In most instances, hyperg,ycemia women can meet the increased insulin demand, but failure to accommodate pregnabcy in poor glycemic control.
This condition may disappear spontaneously durinf delivery, but, if misdiagnosed and mismanaged, may lead to persistent long-term health risks to durinb mother and the child, such as hypperglycemia to obesity and development of Type 2 Athletic recovery nutrition mellitus T2DM within five to 10 years postpartum [ 6 ].
Joint and bone health supplements on the HIP agenda will lead to future high prevalence hyperglycemiz contribute to an increased disease burden on the health system.
A number Lifestyle changes for optimal cholesterol management risk factors contributing to HIP include family history of DM, previous delivery to hypperglycemia or pregnanccy, intrauterine fetal death IUFDmaternal obesity, and preterm delivery [ 11 ].
In addition to sedentary Chronif, maternal height, Sports diet guidelines factors, cigarette smoking, and Chroic pregnancy weight gain accompanied by high body fat accumulation place women at risk of HIP. Body Crhonic percentage can alter body composition leading to prenancy diabetes and other complications, Chronic hyperglycemia during pregnancy as pregnancy induced hypertension prgnancy predisposition of the euring to overweight later in life [ 121314 ].
It can also affect growth of the fetus; therefore, assessment of change in body fat hypegglycemia is important as predictive of both maternal and child hyperylycemia [ 15 ]. Body mass index BMI is a commonly used standard measure for assessing body fatness [ 16 ]; Strengthening skins natural defenses, it does not distinguish suring fat and lean Chtonic mass [ 17 ].
The delay of onset of antenatal care ANC means most Summer detox diets do not know their hypergpycemia weight which makes it difficult Chronic hyperglycemia during pregnancy estimate BMI and weight gain during pregnancy which is reported to be strongly correlated with yyperglycemia mass change [ 18 ].
This pre-pregnancy metric is even hypeglycemia important because, in addition to Chronnic fat and lean body mass, the fetal mass hypperglycemia amniotic fluid constitute an unknown contribution to huperglycemia body mass of the Summer detox diets ruring is indistinguishable within the Hyperglyxemia calculation.
Furthermore, women, who are not obese by traditional weight hypedglycemia, may Managing insulin levels an increased percentage of body fat distributed predominantly in the abdominal region, which leads to increased risk of Hpyerglycemia [ 19 ].
Studies done with T2DM patients have identified that fat Fat burning HIIT workouts within skeletal muscle and liver cells is a major contributing factor to hyperg,ycemia resistance; however, Summer detox diets, there is lack of evidence on whether fat deposition during pregnancy adequately explains the acquisition of hyperglycemiaa resistance as a marker Golf nutrition tips HIP prebnancy 2021 ].
Few studies have assessed the hyperglycsmia of body fat on development of GDM with most Chronc studies considering Caucasian and Asian populations [ 22 Enhance mental clarity, 23 vuring. This hypeglycemia requires redress as risks for HIP differ across ethnic, geographic, Chronic hyperglycemia during pregnancy pregnnancy lines due to differences in hyperglycemka composition, lifestyles, genetic susceptibility, as well as healthcare system pregnwncy [ 24 ].
Some populations may have pregnabcy BMI but high rates of HIP. For example, Asian populations tend to have a lower BMI, hyperglycemka accumulate visceral fat and Summer detox diets abdominal obesity [ 25 ] which is positively associated with insulin pregnajcy and impaired β Fat blocker metabolism booster function [ Nutritional analysis software27 ].
In addition to body Chronix percentage, Hhyperglycemia has a strong duriing with BMI [ 16 ] Crhonic it can hyperglycemua used instead of BMI as a much simpler, cheaper anthropometric measurement, which does not change significantly during pregnancy.
Hence, it may be a better indicator of pregnancy body fat and nutrition status than BMI [ 28 ]. Pegnancy does not need mathematical calculations, additional equipment, and regular equipment standardization which are important considerations in limited resource settings [ 29 ].
Furthermore, Druing is highly associated with GDM [ 30 ] which means that a woman with a MUAC beyond the normal value is at increased risk of GDM compared to the one with normal MUAC value. The current study was conducted in Arusha District, which has a known high prevalence of T2DM This situation led to the need to determine the prevalence of HIP and durung associated risk factors especially the hypertlycemia explored body fat percentage ruring possible interventions to prevent short- and long-term adverse effects to the mother and her newborn.
A cross-sectional study was conducted in urban areas of Arusha District between March and December of Curonic study involved pregnant hyperglycemua attending antenatal clinics at Ngarenaro and Kaloleni Health Centers in Arusha District. The two centers were purposively selected due to their central location and large numbers of pregnant women on average 40— per duting accessing Ante-Natal Care ANC services from across durign District, thereby representing the demographics of this predominantly urban patient population.
Pregnant women with previously diagnosed diabetes and selected conditions, such as sickle-cell anemia or cancer, were excluded from the study. The aim, procedure, benefits, and negative effects of the study were explained to all enrolled women agreeing hyperglycemix participate and signed informed consents.
The eligible women were selected with assistance of the nurse in-charge resulting in a total of women being involved in the study. Sample size was determined in accordance with the formula for prevalence studies [ hyperglycmeia ].
Random sampling using a table of numbers was used to select women hylerglycemia participate in the study and due to the high number of pregnant women attending ANC in the areas, 12 women were assessed per day.
In addition, nearly all pregnncy Women were rpegnancy to fast overnight before capillary blood was taken using a pregnanct prick with a sterile lancet after cleaning the site with an antiseptic alcohol swab.
Hypeeglycemia, Quebec, Canada. The capillary plasma glucose values obtained were converted into venous dhring glucose using durint regression equation developed for diabetes screening hypergglycemia the low resource areas where venous blood is challenging [ 35 ].
Women were classified as having HIP if Chronnic met the criteria for DIP and GDM which is fasting plasma glucose 5. The 1-h OGTT was not considered because there are no established criteria for the diagnosis of diabetes based on the curing post-load value and one reading is enough.
Furthermore, all women identified with HIP were referred to see the doctor pregnany further actions. Mid upper arm circumference was used to supplement Hperglycemia due to its relative stability during the course of pregnancy and high correlation with pre-pregnancy BMI, making it a better indicator of pre-pregnancy body fat and nutrition status than the BMI [ 1636 ].
Weight was measured with minimal clothing and without shoes using a digital bathroom weighing scale SECA-Germanyplaced on a flat surface and recorded to the nearest 0. The body fat percentage was treated as a continuous variable and there are no established classification criteria for pregnancy.
Chi-square Chroni was used for comparing prevnancy selected prefnancy variables between women with and those without HIP. Blood glucose levels were dichotomized, and univariate analysis was done for the pregmancy associated with HIP to obtain crude odd ratios.
Multiple logistic regression analysis explored whether different factors had significant association with HIP where the quantitative variables such as body fat percent, BMI and MUAC were treated as continuous variables.
Some factors were potential confounders, durinf they durimg introduced into the model during the analysis, such as age, and hyperglycejia age. The variables with missing data i. Other variables, which were missing due to mistakes in recording, were traced back from hyperrglycemia participants as their phone numbers and other contacts were recorded.
Other missing data were traced from ANC records available in the health center. A total of pregnant women participated in the study at Ngarenaro and Kaloleni Health Centers in Arusha, Tanzania.
They were all black African by ethnicity. Most were married This weight was used to determine pre-pregnancy BMI of the women in which The prevalence of HIP was Among the women assessed, The Chrknic mean of fasting blood glucose was 4. The overall mean for OGTT was 5. The selected risk factors were analyzed using multiple logistic regression analysis to determine their association with HIP.
A significant association was observed with increased body fat percentage AOR 1. The second model replaced body fat percentage with MUAC and the association remained consistently significant in all factors of the first model with addition preggnancy MUAC AOR 1.
The current study was hyperglyceima out to determine the prevalence of HIP and influence of body fat percent and other risk factors on development of HIP among women in Arusha District. The overall prevalence of HIP was found to be Gestational diabetes mellitus is not the only form of hyperglycemia which oregnancy first be detected during pregnancy as DIP is a more severe form ppregnancy HIP in which diagnostic glucose levels are pregnqncy same as those of non-pregnant adults [ 3 ].
Therefore, the prevalence of hyperglycemia in pregnancy in this study combined GDM and DIP as it is important to include pregnant women with pre-existing diabetes in designing interventions.
Moreover, DIP increases the vulnerability to complications because of the degree of hyperglycemia and the uncertainty as to whether the onset of hyperglycemia was prior to pregnancy or it developed huperglycemia pregnancy [ 2 ].
This study provides evidence for designing interventions like pre-pregnancy testing of blood glucose levels, emphasis on health education to improve health seeking durihg among women diring reproductive age.
In Tanzania, due to limited resources, most women are not tested for durint levels before pregnancy. It is therefore important that HIP is considered to ensure thorough glucose control durinng conception, throughout pregnancy and postpartum for prevention of diabetes in progressive pregnancies.
Hence, including DIP and GDM together may strengthen the approach and allow recognition of general prevalence of hyperglycemia to open dialogue on future GDM approaches that align with global standards for all women in Tanzania.
Chrronic observed prevalence of HIP may increase burden to the health system if no immediate actions are taken. The need exists to explore the associated modifiable risk factors including body fat to enhance self-care practices and prevent poor pregnancy outcomes as well as T2DM later in life.
A similar study conducted in Tanzania using the same WHO [ 3 ] criteria reported that the prevalence of GDM hypervlycemia The differences in prevalence of hyperglycemia observed may be due to nature of the diets, cultural differences in food preparation, and care during pregnancy which needs further exploration.
In addition, another similar study done in India supported our findings on the consideration of HIP in screening hyperglycemia during pregnancy and reported that, HIP was prevalent in When body fat percentage was replaced by MUAC in the second model, increased in MUAC was independently associated with HIP.
In this case, body fat percentage together with MUAC can be used instead of BMI as determinants of HIP due to their independent association with HIP. Moreover, the majority of the women in the current study could not recall their pre-pregnancy weight making it prebnancy to estimate their BMI.
This finding is supported by Mwanri Chronc al. Another study pregnqncy that less than half of the mothers could recall their pre-gestational weight [ 39 ]. Hence, information on changes in body fat content is required due to its independent association with HIP which is further supported in a previous report that the risk of GDM was independently associated with high body fat percent, similar to the findings in people with T2DM [ 23 ].
With these associations, it would prefnancy important Chfonic utilize these simple factors to identify pregnant women at risk for HIP so that prevention measures, such as lifestyle modifications, can be implemented to prevent poor pregnancy outcomes [ 40 ].
This finding reveals how maternal health status is the determinant of health of the newborn. This finding means that a hyperglycema with history of previous pregnancy, which resulted in a child with a high birth weight, prrgnancy at an increased risk of GDM in progressive pregnancies [ 42 ].
Another study showed that GDM is considered to result from interaction between genetic and environmental risk factors [ 43 ]. Pregnancy triggers a series of metabolic imbalances that lead to a diabetic state in women who are already genetically predisposed to develop diabetes [ 44 ].
Of note, GDM and T2DM share a similar genetic background [ 45 hypsrglycemia which might be a reason to why women with strong first-degree family history of T2DM are durin high risk of HIP.
Hence, genetic predispositions to T2DM or HIP should not Chronif ignored. Other studies concur with the current report that family history of diabetes remained significantly associated with GDM even after adjustment for other co-variates [ 3746 ].
: Chronic hyperglycemia during pregnancy| Gestational diabetes | If you have 1 or more risk factors for gestational diabetes you should be offered a screening test. The screening test is called an oral glucose tolerance test OGTT , which takes about 2 hours. It involves having a blood test in the morning, when you have not had any food or drink for 8 to 10 hours though you can usually drink water, but check with the hospital if you're unsure. You're then given a glucose drink. After resting for 2 hours, another blood sample is taken to see how your body is dealing with the glucose. The OGTT is done when you're between 24 and 28 weeks pregnant. If you've had gestational diabetes before, you'll be offered an OGTT earlier in your pregnancy, soon after your booking appointment, then another OGTT at 24 to 28 weeks if the first test is normal. Find out more at Lab Tests Online: Glucose Tests. If you have gestational diabetes, the chances of having problems with your pregnancy can be reduced by controlling your blood sugar levels. You'll be given a blood sugar testing kit so you can monitor the effects of treatment. Blood sugar levels may be reduced by changing your diet and being more active if you can. Gentle activities such as walking, swimming and prenatal yoga can help reduce blood sugar. However, if these changes don't lower your blood sugar levels enough, you will need to take medicine as well. This may be tablets or insulin injections. You'll also be more closely monitored during your pregnancy and birth to check for any potential problems. If you have gestational diabetes, it's best to give birth before 41 weeks. Induction of labour or a caesarean section may be recommended if labour does not start naturally by this time. Earlier delivery may be recommended if there are concerns about your or your baby's health or if your blood sugar levels have not been well controlled. Find out more about how gestational diabetes is treated. Gestational diabetes normally goes away after birth. But women who've had it are more likely to develop:. You should have a blood test to check for diabetes 6 to 13 weeks after giving birth, and once every year after that if the result is normal. See your GP if you develop symptoms of high blood sugar, such as increased thirst, needing to pee more often than usual, and a dry mouth — do not wait until your next test. You should have the tests even if you feel well, as many people with diabetes do not have any symptoms. You'll also be advised about things you can do to reduce your risk of getting diabetes, such as maintaining a healthy weight, eating a balanced diet and exercising regularly. Some research has suggested that babies of mothers who had gestational diabetes may be more likely to develop diabetes or become obese later in life. If you've had gestational diabetes before and you're planning to get pregnant, make sure you get checked for diabetes. Your GP can arrange this. If you do have diabetes, you should be referred to a diabetes pre-conception clinic for support to ensure your condition is well controlled before you get pregnant. Read more about diabetes in pregnancy. If you have an unplanned pregnancy, talk to your GP and tell them you had gestational diabetes in your previous pregnancy. However, some women have insulin resistance even before they get pregnant. They start pregnancy with an increased need for insulin and are more likely to have gestational diabetes. Having gestational diabetes can increase your risk of high blood pressure during pregnancy. It can also increase your risk of having a large baby that needs to be delivered by cesarean section C-section. Your blood sugar levels will usually return to normal after your baby is born. You can lower your risk by reaching a healthy body weight after delivery. Visit your doctor to have your blood sugar tested 6 to 12 weeks after your baby is born and then every 1 to 3 years to make sure your levels are on target. Talk to your doctor about how much weight you should gain for a healthy pregnancy. You can do a lot to manage your gestational diabetes. Go to all your prenatal appointments and follow your treatment plan, including:. Skip directly to site content Skip directly to search. Español Other Languages. Gestational Diabetes. Español Spanish Print. Minus Related Pages. Follow a healthy eating plan to nourish you and your baby. Preventing Type 2 Diabetes. |
| What causes diabetes during pregnancy? | A doctor will test you for diabetes 6 to 12 weeks after your baby is born, and again every 1 to 3 years. Taking steps to prevent type 2 diabetes can also help prevent associated complications. However, changing your lifestyle can help reduce your risk of developing it. Even light activity, such as walking, may be beneficial. A doctor can help you create a plan to reach and maintain a moderate weight. Even losing a small amount of weight can help reduce the risk of gestational diabetes. Gestational diabetes occurs when the body cannot produce the insulin needed during pregnancy, resulting in high blood sugar. If you have gestational diabetes, a doctor may recommend changes to your diet along with blood sugar monitoring to help manage the condition. In some cases, you may need insulin injections. In many cases, if you have gestational diabetes during pregnancy, your blood sugar should return to your typical levels after you give birth. However, you may have a higher risk of developing type 2 diabetes later in life. Read this article in Spanish. Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available. VIEW ALL HISTORY. Gestational diabetes refers to high blood sugar levels during pregnancy, and it's fairly common. Learn about the risk factors, prevention, and more. The gestational diabetes test is an important part of prenatal care, and all pregnant women should receive it. Learn what to expect. Find out about…. Pregestational diabetes occurs when you have diabetes before becoming pregnant. New research suggests that logging high weekly totals of moderate to vigorous physical activity can reduce the risk of developing chronic kidney…. Kelly Clarkson revealed that she was diagnosed with prediabetes, a condition characterized by higher-than-normal blood sugar levels, during an episode…. New research has revealed that diabetes remission is associated with a lower risk of cardiovascular disease and chronic kidney disease. Type 2…. A Quiz for Teens Are You a Workaholic? How Well Do You Sleep? Health Conditions Discover Plan Connect. Gestational Diabetes: Everything You Need to Know. Medically reviewed by Lauren Castiello, MS, AGNP-C — By Brindles Lee Macon — Updated on September 13, Symptoms Causes Risk factors Diagnosis Type 1 and 2 diabetes Classes Treatment Diet Complications Outlook Prevention Takeaway. What is gestational diabetes? What are the symptoms of gestational diabetes? What causes gestational diabetes? Who is at risk of gestational diabetes? How is gestational diabetes diagnosed? Should I be concerned about type 1 and 2 diabetes as well? Are there different forms of gestational diabetes? How is gestational diabetes treated? What should I eat if I have gestational diabetes? What complications are associated with gestational diabetes? What is the outlook for people with gestational diabetes? Can gestational diabetes be prevented? Parenthood Pregnancy Pregnancy Complications. If you have gestational diabetes, the chances of having problems with your pregnancy can be reduced by controlling your blood sugar levels. You'll be given a blood sugar testing kit so you can monitor the effects of treatment. Blood sugar levels may be reduced by changing your diet and being more active if you can. Gentle activities such as walking, swimming and prenatal yoga can help reduce blood sugar. However, if these changes don't lower your blood sugar levels enough, you will need to take medicine as well. This may be tablets or insulin injections. You'll also be more closely monitored during your pregnancy and birth to check for any potential problems. If you have gestational diabetes, it's best to give birth before 41 weeks. Induction of labour or a caesarean section may be recommended if labour does not start naturally by this time. Earlier delivery may be recommended if there are concerns about your or your baby's health or if your blood sugar levels have not been well controlled. Find out more about how gestational diabetes is treated. Gestational diabetes normally goes away after birth. But women who've had it are more likely to develop:. You should have a blood test to check for diabetes 6 to 13 weeks after giving birth, and once every year after that if the result is normal. See your GP if you develop symptoms of high blood sugar, such as increased thirst, needing to pee more often than usual, and a dry mouth — do not wait until your next test. You should have the tests even if you feel well, as many people with diabetes do not have any symptoms. You'll also be advised about things you can do to reduce your risk of getting diabetes, such as maintaining a healthy weight, eating a balanced diet and exercising regularly. Some research has suggested that babies of mothers who had gestational diabetes may be more likely to develop diabetes or become obese later in life. If you've had gestational diabetes before and you're planning to get pregnant, make sure you get checked for diabetes. Your GP can arrange this. Babies who weigh this much are more likely to be hurt during labor and birth, and can cause damage to his or her mother during delivery. Shoulder dystocia or other birth injuries also called birth trauma. Complications for birthing parents caused by shoulder dystocia include postpartum hemorrhage heavy bleeding. For babies, the most common injuries are fractures to the collarbone and arm and damage to the brachial plexus nerves. These nerves go from the spinal cord in the neck down the arm. They provide feeling and movement in the shoulder, arm and hand. High blood pressure and preeclampsia. High blood pressure also called hypertension is when the force of blood against the walls of the blood vessels is too high. It can stress your heart and cause problems during pregnancy. Preeclampsia is when a pregnant person has high blood pressure and signs that some of their organs, such as the kidneys and liver, may not be working properly. Perinatal depression. This is depression that happens during pregnancy or in the first year after having a baby also called postpartum depression. Depression is a medical condition that causes feelings of sadness and a loss of interest in things you like to do. It can affect how you think, feel, and act and can interfere with your daily life. Preterm birth. This is birth before 37 weeks of pregnancy. Most women who have gestational diabetes have a full-term pregnancy that lasts between 39 and 40 weeks. However, if there are complications, your health care provider may need to induce labor before your due date. This means your provider will give you medicine or break your water amniotic sac to make your labor begin. This is the death of a baby after 20 weeks of pregnancy. Cesarean birth also called c-section. This is surgery in which your baby is born through a cut that your doctor makes in your belly and uterus. You may need to have a c-section if you have complications during pregnancy, or if your baby is very large also known as macrosomia. Most people who have gestational diabetes can have a vaginal birth. Gestational diabetes also can cause health complications for your baby after birth, including: Breathing problems, including respiratory distress syndrome. Surfactant is a protein that keeps the small air sacs in the lungs from collapsing. Low blood sugar also called hypoglycemia Obesity later in life Diabetes later in life How do you know if you have gestational diabetes? How is gestational diabetes treated? Here are two ways to do kick counts: Every day, time how long it takes for your baby to move 10 times. If it takes longer than 2 hours, tell your provider. See how many movements you feel in 1 hour. Do this 3 times each week. If the number changes, tell your provider. Your provider shows you how to check your blood sugar on your own. Keep a log that includes your blood sugar level every time you check it. Share it with your provider at each checkup. Eat healthy foods. |
| Ways to give | See "Patient education: C-section cesarean delivery Beyond the Basics ". Waiting for labor to start on its own is reasonable if blood glucose levels are well controlled and the mother and baby are doing well. However, extending pregnancy beyond the 40 th completed week of gestation is generally not recommended; some practitioners routinely induce labor between 39 weeks plus 0 days and 40 weeks plus 0 days in all individuals with type 1 or 2 diabetes. During labor, blood glucose levels are checked frequently and insulin is given, as needed, to maintain good glucose control. Obstetricians will review the plan for blood glucose monitoring and insulin administration on an individualized basis. The risk of stillbirth for individuals with well-controlled diabetes is very low and is approximately the same as in individuals without diabetes less than 1 percent. The mortality death rate in infants of diabetic mothers is slightly higher than in those without diabetes 2 versus 1 percent. This is mostly due to a higher rate of serious congenital anomalies in infants of diabetic mothers. Newborn issues — The infant of the diabetic mother is at risk for several problems in the newborn period, such as low blood glucose levels, jaundice, breathing problems, excessive red blood cells polycythemia , low calcium level, and heart problems. These problems are more common when the mother's blood glucose levels have been high throughout the pregnancy. Most of these problems resolve within a few hours or days after birth. Infants of diabetic mothers are often evaluated in a special care nursery to monitor for these potential problems. Infants of mothers with diabetes are at higher risk of having difficulties with breathing, especially if the baby is born earlier than 39 weeks. This is because the lungs appear to develop more slowly in infants of mothers with diabetes. The risk of breathing problems is highest when maternal blood glucose levels have been high near the time of delivery. Will my child develop diabetes? According to the American Diabetes Association ADA :. Children of a mother with type 1 diabetes have a 1 in 25 risk if, at the time of pregnancy, the mother is less than 25 years of age. The risk is 1 in risk if the mother is 25 years of age or older. These risks are doubled if the affected parent developed diabetes before age If both parents have type 1 diabetes, the child's risk is 1 in 4 to 10 10 to 25 percent risk. The risk depends upon environmental and behavioral factors, such as obesity and sedentary lifestyle, as well as the genetic susceptibility. See "Patient education: Type 1 diabetes: Overview Beyond the Basics " and "Patient education: Type 2 diabetes: Overview Beyond the Basics ". AFTER DELIVERY CARE. Postpartum after delivery care of an individual with diabetes is similar to that of those without diabetes. However, it is important to pay close attention to blood glucose levels because insulin requirements can fall rapidly in the first few days after delivery; some individuals require little or no insulin. Insulin requirements usually return to near-prepregnancy levels within 48 hours. Breastfeeding — In all postpartum individuals with and without diabetes , breastfeeding is strongly encouraged because it benefits both the infant and the mother. Insulin requirements may be lower while breastfeeding, and frequent blood glucose monitoring is important to prevent severe hypoglycemia. See "Patient education: Deciding to breastfeed Beyond the Basics " and "Patient education: Breastfeeding guide Beyond the Basics ". Contraception — Individuals with diabetes who have no or minimal vascular disease may use any type of contraception, including oral contraceptive pills. Birth control pills do not affect blood glucose levels. Your health care provider is the best source of information for questions and concerns related to your medical problem. This article will be updated as needed on our website www. Related topics for patients, as well as selected articles written for health care professionals, are also available. Some of the most relevant are listed below. Patient level information — UpToDate offers two types of patient education materials. The Basics — The Basics patient education pieces answer the four or five key questions a patient might have about a given condition. These articles are best for patients who want a general overview and who prefer short, easy-to-read materials. Patient education: Care during pregnancy for people with type 1 or type 2 diabetes The Basics Patient education: How to plan and prepare for a healthy pregnancy The Basics Patient education: Preparing for pregnancy when you have diabetes The Basics. Beyond the Basics — Beyond the Basics patient education pieces are longer, more sophisticated, and more detailed. These articles are best for patients who want in-depth information and are comfortable with some medical jargon. Patient education: Gestational diabetes Beyond the Basics Patient education: Type 1 diabetes: Insulin treatment Beyond the Basics Patient education: Glucose monitoring in diabetes Beyond the Basics Patient education: Hypoglycemia low blood glucose in people with diabetes Beyond the Basics Patient education: Preeclampsia Beyond the Basics Patient education: Dialysis or kidney transplantation — which is right for me? Beyond the Basics Patient education: Hemodialysis Beyond the Basics Patient education: Preterm labor Beyond the Basics Patient education: Should I have a screening test for Down syndrome during pregnancy? Beyond the Basics Patient education: Amniocentesis Beyond the Basics Patient education: C-section cesarean delivery Beyond the Basics Patient education: Type 1 diabetes: Overview Beyond the Basics Patient education: Type 2 diabetes: Overview Beyond the Basics Patient education: Deciding to breastfeed Beyond the Basics Patient education: Breastfeeding guide Beyond the Basics. Professional level information — Professional level articles are designed to keep doctors and other health professionals up-to-date on the latest medical findings. These articles are thorough, long, and complex, and they contain multiple references to the research on which they are based. Professional level articles are best for people who are comfortable with a lot of medical terminology and who want to read the same materials their doctors are reading. Pancreas-kidney transplantation in diabetes mellitus: Benefits and complications General principles of insulin therapy in diabetes mellitus Pregestational preexisting diabetes mellitus: Antenatal glycemic control Infants of mothers with diabetes IMD Nutrition in pregnancy: Dietary requirements and supplements Pregestational preexisting diabetes mellitus: Obstetric issues and management Exercise during pregnancy and the postpartum period Gestational diabetes mellitus: Screening, diagnosis, and prevention Gestational diabetes mellitus: Glucose management and maternal prognosis Pregestational preexisting diabetes: Preconception counseling, evaluation, and management. html , available in Spanish. org , available in Spanish. The editorial staff at UpToDate would like to acknowledge John Repke, MD, who contributed to an earlier version of this topic review. Why UpToDate? Product Editorial Subscription Options Subscribe Sign in. Learn how UpToDate can help you. Select the option that best describes you. View Topic. Font Size Small Normal Large. Patient education: Care during pregnancy for patients with type 1 or 2 diabetes Beyond the Basics. Formulary drug information for this topic. No drug references linked in this topic. Find in topic Formulary Print Share. Author: Celeste Durnwald, MD Section Editors: Charles J Lockwood, MD, MHCM David M Nathan, MD Deputy Editor: Vanessa A Barss, MD, FACOG Contributor Disclosures. All topics are updated as new evidence becomes available and our peer review process is complete. Literature review current through: Jan This topic last updated: Mar 29, CARE DURING PREGNANCY Ideally, an individual with diabetes who is planning pregnancy should consult their health care provider well before they become pregnant. PLANNING FOR DELIVERY An individual and their obstetrician may decide to schedule the date of the birth either an induction of labor or cesarean birth , especially if there are risk factors for an adverse maternal or fetal outcome, such as increased blood glucose levels, nephropathy, worsening retinopathy, high blood pressure or preeclampsia, or if the baby is smaller or larger than normal. INFANT CARE Newborn issues — The infant of the diabetic mother is at risk for several problems in the newborn period, such as low blood glucose levels, jaundice, breathing problems, excessive red blood cells polycythemia , low calcium level, and heart problems. AFTER DELIVERY CARE Postpartum after delivery care of an individual with diabetes is similar to that of those without diabetes. Patient education: Care during pregnancy for people with type 1 or type 2 diabetes The Basics Patient education: How to plan and prepare for a healthy pregnancy The Basics Patient education: Preparing for pregnancy when you have diabetes The Basics Beyond the Basics — Beyond the Basics patient education pieces are longer, more sophisticated, and more detailed. Beyond the Basics Patient education: Amniocentesis Beyond the Basics Patient education: C-section cesarean delivery Beyond the Basics Patient education: Type 1 diabetes: Overview Beyond the Basics Patient education: Type 2 diabetes: Overview Beyond the Basics Patient education: Deciding to breastfeed Beyond the Basics Patient education: Breastfeeding guide Beyond the Basics Professional level information — Professional level articles are designed to keep doctors and other health professionals up-to-date on the latest medical findings. However, there is no consensus on the structure of multidisciplinary team care for diabetes and pregnancy, and there is a lack of evidence on the impact on outcomes of various methods of health care delivery Some women with preexisting diabetes should also test blood glucose preprandially. Pregnancy in women with normal glucose metabolism is characterized by fasting levels of blood glucose that are lower than in the nonpregnant state due to insulin-independent glucose uptake by the fetus and placenta and by mild postprandial hyperglycemia and carbohydrate intolerance as a result of diabetogenic placental hormones. In patients with preexisting diabetes, glycemic targets are usually achieved through a combination of insulin administration and medical nutrition therapy. Because glycemic targets in pregnancy are stricter than in nonpregnant individuals, it is important that women with diabetes eat consistent amounts of carbohydrates to match with insulin dosage and to avoid hyperglycemia or hypoglycemia. Referral to a registered dietitian nutritionist is important in order to establish a food plan and insulin-to-carbohydrate ratio and to determine weight gain goals. Given that early pregnancy is a time of enhanced insulin sensitivity and lower glucose levels, many women with type 1 diabetes will have lower insulin requirements and increased risk for hypoglycemia The situation rapidly reverses by approximately 16 weeks as insulin resistance increases exponentially during the second and early third trimesters to 2—3 times the preprandial requirement. The insulin requirement levels off toward the end of the third trimester with placental aging. A rapid reduction in insulin requirements can indicate the development of placental insufficiency In women with normal pancreatic function, insulin production is sufficient to meet the challenge of this physiological insulin resistance and to maintain normal glucose levels. However, in women with diabetes, hyperglycemia occurs if treatment is not adjusted appropriately. Reflecting this physiology, fasting and postprandial monitoring of blood glucose is recommended to achieve metabolic control in pregnant women with diabetes. Preprandial testing is also recommended when using insulin pumps or basal-bolus therapy so that premeal rapid-acting insulin dosage can be adjusted. Postprandial monitoring is associated with better glycemic control and lower risk of preeclampsia 29 — There are no adequately powered randomized trials comparing different fasting and postmeal glycemic targets in diabetes in pregnancy. Similar to the targets recommended by ACOG the same as for GDM; described below 32 , the ADA-recommended targets for women with type 1 or type 2 diabetes are as follows:. These values represent optimal control if they can be achieved safely. In practice, it may be challenging for women with type 1 diabetes to achieve these targets without hypoglycemia, particularly women with a history of recurrent hypoglycemia or hypoglycemia unawareness. If women cannot achieve these targets without significant hypoglycemia, the ADA suggests less-stringent targets based on clinical experience and individualization of care. In studies of women without preexisting diabetes, increasing A1C levels within the normal range are associated with adverse outcomes In the Hyperglycemia and Adverse Pregnancy Outcome HAPO study, increasing levels of glycemia were also associated with worsening outcomes Due to physiological increases in red blood cell turnover, A1C levels fall during normal pregnancy 36 , Additionally, as A1C represents an integrated measure of glucose, it may not fully capture postprandial hyperglycemia, which drives macrosomia. Thus, although A1C may be useful, it should be used as a secondary measure of glycemic control in pregnancy, after self-monitoring of blood glucose. The A1C target in a given patient should be achieved without hypoglycemia, which, in addition to the usual adverse sequelae, may increase the risk of low birth weight Given the alteration in red blood cell kinetics during pregnancy and physiological changes in glycemic parameters, A1C levels may need to be monitored more frequently than usual e. CONCEPTT Continuous Glucose Monitoring in Pregnant Women With Type 1 Diabetes Trial was a randomized controlled trial of continuous glucose monitoring CGM in addition to standard care, including optimization of pre- and postprandial glucose targets versus standard care for pregnant women with type 1 diabetes. It demonstrated the value of CGM in pregnancy complicated by type 1 diabetes by showing a mild improvement in A1C without an increase in hypoglycemia and reductions in large-for-gestational-age births, length of stay, and neonatal hypoglycemia An observational cohort study that evaluated the glycemic variables reported using CGM and their association with large-for-gestational-age births found that mean glucose had a greater association than time in range, time below range, or time above range Using the CGM-reported mean glucose is superior to the use of estimated A1C, glucose management indicator, and other calculations to estimate A1C given the changes to A1C that occur in pregnancy Insulin should be added if needed to achieve glycemic targets. Metformin and glyburide should not be used as first-line agents, as both cross the placenta to the fetus. A Other oral and noninsulin injectable glucose-lowering medications lack long-term safety data. GDM is characterized by increased risk of macrosomia and birth complications and an increased risk of maternal type 2 diabetes after pregnancy. The association of macrosomia and birth complications with oral glucose tolerance test OGTT results is continuous with no clear inflection points In other words, risks increase with progressive hyperglycemia. Although there is some heterogeneity, many randomized controlled trials RCTs suggest that the risk of GDM may be reduced by diet, exercise, and lifestyle counseling, particularly when interventions are started during the first or early in the second trimester 46 — After diagnosis, treatment starts with medical nutrition therapy, physical activity, and weight management depending on pregestational weight, as outlined in the section below on preexisting type 2 diabetes, and glucose monitoring aiming for the targets recommended by the Fifth International Workshop-Conference on Gestational Diabetes Mellitus 48 :. There is no definitive research that identifies a specific optimal calorie intake for women with GDM or suggests that their calorie needs are different from those of pregnant women without GDM. The food plan should be based on a nutrition assessment with guidance from the Dietary Reference Intakes DRI. The DRI for all pregnant women recommends a minimum of g of carbohydrate, a minimum of 71 g of protein, and 28 g of fiber. The diet should not be high in saturated fat. As is true for all nutrition therapy in patients with diabetes, the amount and type of carbohydrate will impact glucose levels. Simple carbohydrates will result in higher postmeal excursions. Treatment of GDM with lifestyle and insulin has been demonstrated to improve perinatal outcomes in two large randomized studies as summarized in a U. Preventive Services Task Force review Insulin is the first-line agent recommended for treatment of GDM in the U. While individual RCTs support limited efficacy of metformin 54 , 55 and glyburide 56 in reducing glucose levels for the treatment of GDM, these agents are not recommended as first-line treatment for GDM because they are known to cross the placenta and data on long-term safety for offspring is of some concern Sulfonylureas are known to cross the placenta and have been associated with increased neonatal hypoglycemia. Glyburide was associated with a higher rate of neonatal hypoglycemia and macrosomia than insulin or metformin in a meta-analysis and systematic review More recently, glyburide failed to be found noninferior to insulin based on a composite outcome of neonatal hypoglycemia, macrosomia, and hyperbilirubinemia Long-term safety data for offspring exposed to glyburide are not available Metformin was associated with a lower risk of neonatal hypoglycemia and less maternal weight gain than insulin in systematic reviews 59 , 61 , 62 , However, metformin readily crosses the placenta, resulting in umbilical cord blood levels of metformin as high or higher than simultaneous maternal levels 66 , This was not found in the Adelaide cohort. In two RCTs of metformin use in pregnancy for polycystic ovary syndrome, follow-up of 4-year-old offspring demonstrated higher BMI and increased obesity in the offspring exposed to metformin 69 , A follow-up study at 5—10 years showed that the offspring had higher BMI, weight-to-height ratios, waist circumferences, and a borderline increase in fat mass 70 , Metformin is being studied in two ongoing trials in type 2 diabetes Metformin in Women with Type 2 Diabetes in Pregnancy Trial [MiTY] [ 72 ] and Medical Optimization of Management of Type 2 Diabetes Complicating Pregnancy [MOMPOD] [ 73 ] , but long-term offspring data will not be available for some time. A recent meta-analysis concluded that metformin exposure resulted in smaller neonates with acceleration of postnatal growth resulting in higher BMI in childhood 68 , Randomized, double-blind, controlled trials comparing metformin with other therapies for ovulation induction in women with polycystic ovary syndrome have not demonstrated benefit in preventing spontaneous abortion or GDM 74 , and there is no evidence-based need to continue metformin in such patients 75 — There are some women with GDM requiring medical therapy who, due to cost, language barriers, comprehension, or cultural influences, may not be able to use insulin safely or effectively in pregnancy. Oral agents may be an alternative in these women after a discussion of the known risks and the need for more long-term safety data in offspring. However, due to the potential for growth restriction or acidosis in the setting of placental insufficiency, metformin should not be used in women with hypertension, preeclampsia, or at risk for intrauterine growth restriction 78 , Insulin use should follow the guidelines below. Both multiple daily insulin injections and continuous subcutaneous insulin infusion are reasonable delivery strategies, and neither has been shown to be superior to the other during pregnancy The physiology of pregnancy necessitates frequent titration of insulin to match changing requirements and underscores the importance of daily and frequent self-monitoring of blood glucose. Due to the complexity of insulin management in pregnancy, referral to a specialized center offering team-based care with team members including maternal-fetal medicine specialist, endocrinologist, or other provider experienced in managing pregnancy in women with preexisting diabetes, dietitian, nurse, and social worker, as needed is recommended if this resource is available. None of the currently available human insulin preparations have been demonstrated to cross the placenta 80 — A recent Cochrane systematic review was not able to recommend any specific insulin regimen over another for the treatment of diabetes in pregnancy While many providers prefer insulin pumps in pregnancy, it is not clear that they are superior to multiple daily injections 88 — Closed-loop technology that is U. However, given potential benefits, ongoing work is being done in this area. Women with type 1 diabetes have an increased risk of hypoglycemia in the first trimester and, like all women, have altered counterregulatory response in pregnancy that may decrease hypoglycemia awareness. Education for patients and family members about the prevention, recognition, and treatment of hypoglycemia is important before, during, and after pregnancy to help to prevent and manage the risks of hypoglycemia. Insulin resistance drops rapidly with delivery of the placenta. Pregnancy is a ketogenic state, and women with type 1 diabetes, and to a lesser extent those with type 2 diabetes, are at risk for diabetic ketoacidosis DKA at lower blood glucose levels than in the nonpregnant state. Women with type 1 diabetes should be prescribed ketone strips and receive education on diabetic ketoacidosis prevention and detection. DKA carries a high risk of stillbirth. Retinopathy is a special concern in pregnancy. Rapid implementation of euglycemia in the setting of retinopathy is associated with worsening of retinopathy Type 2 diabetes is often associated with obesity. Recommended weight gain during pregnancy for overweight women is 15—25 lb and for obese women is 10—20 lb Glycemic control is often easier to achieve in women with type 2 diabetes than in those with type 1 diabetes but can require much higher doses of insulin, sometimes necessitating concentrated insulin formulations. As in type 1 diabetes, insulin requirements drop dramatically after delivery. The risk for associated hypertension and other comorbidities may be as high or higher with type 2 diabetes as with type 1 diabetes, even if diabetes is better controlled and of shorter apparent duration, with pregnancy loss appearing to be more prevalent in the third trimester in women with type 2 diabetes compared with the first trimester in women with type 1 diabetes 91 , Diabetes in pregnancy is associated with an increased risk of preeclampsia Based upon the results of clinical trials and meta-analyses 94 , the U. A cost-benefit analysis has concluded that this approach would reduce morbidity, save lives, and lower health care costs However, more study is needed to assess the long-term effects of prenatal aspirin exposure on offspring In normal pregnancy, blood pressure is lower than in the nonpregnant state. During pregnancy, treatment with ACE inhibitors and angiotensin receptor blockers is contraindicated because they may cause fetal renal dysplasia, oligohydramnios, pulmonary hypoplasia, and intrauterine growth restriction Antihypertensive drugs known to be effective and safe in pregnancy include methyldopa, nifedipine, labetalol, diltiazem, clonidine, and prazosin. Atenolol is not recommended, but other β-blockers may be used, if necessary. Chronic diuretic use during pregnancy is not recommended as it has been associated with restricted maternal plasma volume, which may reduce uteroplacental perfusion On the basis of available evidence, statins should also be avoided in pregnancy The OGTT is recommended over A1C at 4—12 weeks postpartum because A1C may be persistently impacted lowered by the increased red blood cell turnover related to pregnancy, by blood loss at delivery, or by the preceding 3-month glucose profile. The OGTT is more sensitive at detecting glucose intolerance, including both prediabetes and diabetes. Women of reproductive age with prediabetes may develop type 2 diabetes by the time of their next pregnancy and will need preconception evaluation. Ongoing evaluation may be performed with any recommended glycemic test e. A doctor will not perform any more tests. The cut-off for this range may depend on your risk factors. A doctor will likely diagnose gestational diabetes if you have at least two of the following values :. Many people who experience gestational diabetes will develop type 2 diabetes outside of pregnancy. There are two other types of diabetes:. The ADA also encourages doctors to screen for type 2 diabetes at the beginning of pregnancy. If you have risk factors for type 2 diabetes, a doctor will likely test you for the condition at your first prenatal visit. These risks factors include :. According to the CDC , being an African American, Hispanic or Latino, American Indian, or Alaska Native person may also increase your risk of developing type 2 diabetes. The CDC also notes that some Pacific Islanders and Asian American people may also have a higher risk. Gestational diabetes is divided into two classes :. If you receive a diagnosis of gestational diabetes, your treatment plan will depend on your blood sugar levels throughout the day. In most cases, a doctor will advise you to test your blood sugar before and after meals. If a doctor encourages you to monitor your blood sugar levels , they may provide you with a glucose-monitoring device. A doctor may also prescribe insulin injections for you until you give birth. Ask them about properly timing your insulin injections in relation to your meals and exercise to avoid low blood sugar. A doctor can also tell you what to do if your blood sugar levels fall too low or are consistently higher than they should be. A balanced diet can help manage gestational diabetes. In particular, people with gestational diabetes can pay special attention to their carbohydrate, protein, and fat intake. The CDC recommends working with a dietitian to develop a nutritious eating plan or following meal plans, such as the plate method. You may also need to avoid certain foods if you have gestational diabetes. According to a review of literature , the ADA, along with the American Academy of Nutrition and Dietetics, recommends all pregnant people eat a minimum of g of carbohydrates and 28 g of fiber per day. For people with gestational diabetes, the American College of Obstetrics and Gynecologists ACOG recommends eating complex carbohydrates over simple ones. Complex carbs are digested more slowly, are less likely to produce high blood sugar, and may help reduce insulin resistance. The recommended dietary allowance RDA of protein during pregnancy varies by trimester and may vary based on your individual needs. During the first trimester of pregnancy, the RDA is about 46 g of protein per day. However, ACOG lists certain types of fish that should be avoided due to their high mercury content, including tuna and swordfish. Healthy sources of fat can provide nutrients, such as vitamins and minerals. Health-promoting fats to incorporate into your diet include:. If gestational diabetes is not managed well or left untreated, blood sugar levels may remain higher than they should be throughout your pregnancy. This can lead to complications that affect the health of you and your baby before, during, and after birth. To avoid these complications, you can take steps to manage your gestational diabetes. Your blood sugar should return to typical levels after you give birth. But developing gestational diabetes raises your risk of type 2 diabetes later in life. A doctor will test you for diabetes 6 to 12 weeks after your baby is born, and again every 1 to 3 years. Taking steps to prevent type 2 diabetes can also help prevent associated complications. However, changing your lifestyle can help reduce your risk of developing it. Even light activity, such as walking, may be beneficial. A doctor can help you create a plan to reach and maintain a moderate weight. Even losing a small amount of weight can help reduce the risk of gestational diabetes. Gestational diabetes occurs when the body cannot produce the insulin needed during pregnancy, resulting in high blood sugar. If you have gestational diabetes, a doctor may recommend changes to your diet along with blood sugar monitoring to help manage the condition. In some cases, you may need insulin injections. |
Ich kann Ihnen anbieten, die Webseite zu besuchen, auf der viele Artikel in dieser Frage gibt.
Nach meiner Meinung lassen Sie den Fehler zu. Geben Sie wir werden es besprechen. Schreiben Sie mir in PM.
die Maßgebliche Antwort, wissenswert...