Video
Diabetes and Amputation: Why It's Done and How to Prevent It Joibt can cause pain Preventing diabetes-related bone and joint issues the joints jlint various ways. Dianetes-related also has links Preventing diabetes-related bone and joint issues two types of arthritis. Antioxidant-rich vegetables time, uncontrolled diabetes can affect the muscles and skeleton, leading to joint pain, nerve damage, and other symptoms. Also, according to the Arthritis Foundationalmost half of all adults with diabetes also have arthritis. Keep reading for more information about the links between diabetes, arthritis, and joint pain. We also describe telltale symptoms and the range of treatments.Preventing diabetes-related bone and joint issues -
Maintaining A Healthy Weight Why Is It Important. Skip to primary navigation Skip to main content Skip to primary sidebar Skip to footer Self-management News Educational videos.
Home » Articles and Blogs » Does diabetes affect your bones? Are bone issues common in people with diabetes? What contributes to bone disorders? What types of bone disease occur in people with diabetes? Osteoarthritis , a condition that happens when the protective cartilage that cushions the ends of your bones wears down over time.
Osteoporosis , a condition that causes a loss of bone density and weakening of bone tissue. People with type 1 diabetes have been found to have a lower bone mineral density and a higher incidence of osteoporosis. People with type 2 diabetes have a higher bone mineral density, yet they have a higher risk of fractures.
It is not known why type 2 diabetes affects bone strength regardless of the bone mineral density. Bone fractures , especially hip fractures, are common in people who have either osteoarthritis or osteoporosis. Charcot joint , a rare but serious condition in people with diabetes who have neuropathy.
It initially causes redness, swelling and feels warm to the touch. Eventually, it can lead to weakness or breaks in the bones and dislocation of the joints of the foot and ankle. What can be done to reduce the risk of bone disease? The four main things you can do are: 1.
Read also about Target blood glucose levels. Activation of Glp-1 Receptor Promotes Bone Marrow Stromal Cell Osteogenic Differentiation Through B-Catenin.
Stem Cell Rep 6 4 — Exp Cell Res 2 — Ma X, Meng J, Jia M, Bi L, Zhou Y, Wang Y, et al. Exendin-4, a Glucagon-Like Peptide-1 Receptor Agonist, Prevents Osteopenia by Promoting Bone Formation and Suppressing Bone Resorption in Aged Ovariectomized Rats.
J Bone Miner Res 28 7 — Shen WR, Kimura K, Ishida M, Sugisawa H, Kishikawa A, Shima K, et al. The Glucagon-Like Peptide-1 Receptor Agonist Exendin-4 Inhibits Lipopolysaccharide-Induced Osteoclast Formation and Bone Resorption Via Inhibition of Tnf-A Expression in Macrophages.
J Immunol Res Ishida M, Shen WR, Kimura K, Kishikawa A, Shima K, Ogawa S, et al. Dpp-4 Inhibitor Impedes Lipopolysaccharide-Induced Osteoclast Formation and Bone Resorption in Vivo. BioMed Pharmacother — Hou WH, Chang KC, Li CY, Ou HT. Dipeptidyl Peptidase-4 Inhibitor Use Is Associated With Decreased Risk of Fracture in Patients With Type 2 Diabetes: A Population-Based Cohort Study.
Br J Clin Pharmacol 84 9 — Dombrowski S, Kostev K, Jacob L. Use of Dipeptidyl Peptidase-4 Inhibitors and Risk of Bone Fracture in Patients With Type 2 Diabetes in Germany-A Retrospective Analysis of Real-World Data. Osteoporos Int 28 8 —8. Choi HJ, Park C, Lee YK, Ha YC, Jang S, Shin CS.
Risk of Fractures and Diabetes Medications: A Nationwide Cohort Study. Osteoporos Int 27 9 — Palermo A, D'Onofrio L, Eastell R, Schwartz AV, Pozzilli P, Napoli N. Oral Anti-Diabetic Drugs and Fracture Risk, Cut to the Bone: Safe or Dangerous?
A Narrative Review. Osteoporos Int 26 8 — Napoli N, Strotmeyer ES, Ensrud KE, Sellmeyer DE, Bauer DC, Hoffman AR, et al. Fracture Risk in Diabetic Elderly Men: The Mros Study. Diabetologia 57 10 — Johnston SS, Conner C, Aagren M, Ruiz K, Bouchard J.
Association Between Hypoglycaemic Events and Fall-Related Fractures in Medicare-Covered Patients With Type 2 Diabetes. Diabetes Obes Metab 14 7 — Wei W, Wan Y. Thiazolidinediones on Pparγ: The Roles in Bone Remodeling. PPAR Res Yuhan Z, Jinlong M, Weifen Z. Berberine for Bone Regeneration: Therapeutic Potential and Molecular Mechanisms.
J Ethnopharmacol Shao J, Liu S, Zheng X, Chen J, Li L, Zhu Z. Berberine Promotes Peri-Implant Osteogenesis in Diabetic Rats by Ros-Mediated Irs-1 Pathway.
Biofactors 47 1 — Lu L, Zhijian H, Lei L, Wenchuan C, Zhimin Z, Patwardhan B. Berberine in Combination With Insulin Has Additive Effects on Titanium Implants Osseointegration in Diabetes Mellitus Rats. Evidence-Based Complement Altern Med Shang W, Zhao LJ, Dong XL, Zhao ZM, Li J, Zhang BB, et al.
Mol Med Rep 14 4 —6. Hie M, Yamazaki M, Tsukamoto I. Curcumin Suppresses Increased Bone Resorption by Inhibiting Osteoclastogenesis in Rats With Streptozotocin-Induced Diabetes.
Eur J Pharmacol 1 :1—9. Cirano FR, Pimentel SP, Casati MZ, Corrêa MG, Pino DS, Messora MR, et al. Effect of Curcumin on Bone Tissue in the Diabetic Rat: Repair of Peri-Implant and Critical-Sized Defects.
Int J Oral Maxillofac Surg 47 11 — Resveratrol Treatment Promotes Titanium Implant Osseointegration in Diabetes Mellitus Rats. J Orthop Res 38 10 —9. Bo S, Gambino R, Ponzo V, Cioffi I, Goitre I, Evangelista A, et al.
Effects of Resveratrol on Bone Health in Type 2 Diabetic Patients. A Double-Blind Randomized-Controlled Trial. Nutr Diabetes 8 1 Zhu C, Zhao Y, Wu X, Qiang C, Liu J, Shi J, et al.
The Therapeutic Role of Baicalein in Combating Experimental Periodontitis With Diabetes Via Nrf2 Antioxidant Signaling Pathway. J Periodontal Res 55 3 — Rabbani PS, Soares MA, Hameedi SG, Kadle RL, Mubasher A, Kowzun M, et al. Diabetes 68 1 — Qian J, Jiang F, Wang B, Yu Y, Zhang X, Yin Z, et al.
Ophiopogonin D Prevents H2o2 -Induced Injury in Primary Human Umbilical Vein Endothelial Cells. J Ethnopharmacol 2 — Ma XY, Wen XX, Yang XJ, Zhou DP, Wu Q, Feng YF, et al. Biochimie — Yang M, Xie J, Lei X, Song Z, Gong Y, Liu H, et al.
Tubeimoside I Suppresses Diabetes-Induced Bone Loss in Rats, Osteoclast Formation, and Rankl-Induced Nuclear Factor-Kb Pathway. Int Immunopharmacol Sun Y, Zhu Y, Liu X, Chai Y, Xu J. Cell Prolif 53 8 :e Liu B, Gan X, Zhao Y, Yu H, Gao J, Yu H.
Inhibition of Hmgb1 Promotes Osseointegration Under Hyperglycemic Condition Through Improvement of Bmsc Dysfunction. Oxid Med Cell Longev Jia T, Wang YN, Zhang D, Xu X.
Endocr Connect 7 11 — Bentes CM, Costa PB, Resende M, Netto C, Dias I, da Silveira ALB, et al. Effects of 12 Months of Vitamin D Supplementation on Physical Fitness Levels in Postmenopausal Women With Type 2 Diabetes.
J Funct Morphol Kinesiol 6 4 Nomura S, Kitami A, Takao-Kawabata R, Takakura A, Nakatsugawa M, Kono R, et al. Teriparatide Improves Bone and Lipid Metabolism in a Male Rat Model of Type 2 Diabetes Mellitus. Endocrinology 10 — Lee YS, Gupta R, Kwon JT, Cho DC, Seo YJ, Seu SY, et al.
Effect of a Bisphosphonate and Selective Estrogen Receptor Modulator on Bone Remodeling in Streptozotocin-Induced Diabetes and Ovariectomized Rat Model. Spine J Off J North Am Spine Soc 18 10 — Cui M, Yu LZ, Zhang N, Wang LJ, Sun J, Cong J.
Zoledronic Acid Improves Bone Quality in the Streptozotocin-Induced Diabetes Rat Through Affecting the Expression of the Osteoblast-Regulating Transcription Factors.
Exp Clin Endocrinol Diabetes Off journal German Soc Endocrinol German Diabetes Assoc 1 — Hamann C, Rauner M, Höhna Y, Bernhardt R, Mettelsiefen J, Goettsch C, et al. Sclerostin Antibody Treatment Improves Bone Mass, Bone Strength, and Bone Defect Regeneration in Rats With Type 2 Diabetes Mellitus.
J Bone Mineral Res Off J Am Soc Bone Mineral Res 28 3 — Ferrari S, Eastell R, Napoli N, Schwartz A, Hofbauer LC, Chines A, et al. Denosumab in Postmenopausal Women With Osteoporosis and Diabetes: Subgroup Analysis of Freedom and Freedom Extension.
Bone Viggers R, Al-Mashhadi Z, Starup-Linde J, Vestergaard P. The Efficacy of Alendronate Versus Denosumab on Major Osteoporotic Fracture Risk in Elderly Patients With Diabetes Mellitus: A Danish Retrospective Cohort Study.
Front Endocrinol Lausanne Yoshii T, Yamada M, Minami T, Tsunoda T, Sasaki M, Kondo Y, et al. The Effects of Bazedoxifene on Bone, Glucose, and Lipid Metabolism in Postmenopausal Women With Type 2 Diabetes: An Exploratory Pilot Study. J Clin Med Res 7 10 —9. Mori H, Okada Y, Kishikawa H, Inokuchi N, Sugimoto H, Tanaka Y.
Effects of Raloxifene on Lipid and Bone Metabolism in Postmenopausal Women With Type 2 Diabetes. J Bone Mineral Metab 31 1 — Gomes PS, Resende M, Fernandes MH. Doxycycline Restores the Impaired Osteogenic Commitment of Diabetic-Derived Bone Marrow Mesenchymal Stromal Cells by Increasing the Canonical Wnt Signaling.
Mol Cell Endocrinol Bortolin RH, Abreu B, Ururahy MAG, de Souza KSC, Bezerra JF, Loureiro MB, et al. Protection Against T1dm-Induced Bone Loss by Zinc Supplementation: Biomechanical, Histomorphometric, and Molecular Analyses in Stz-Induced Diabetic Rats.
PloS One 10 5 :e Shanshan Q, Jia H, Hongxing Z, Chen C, Hai J, Shiqiang L. Zinc Supplementation Increased Bone Mineral Density, Improves Bone Histomorphology, and Prevents Bone Loss in Diabetic Rat. Biol Trace Element Res 2 — Maddaloni E, D'Eon S, Hastings S, Tinsley LJ, Napoli N, Khamaisi M, et al.
Bone Health in Subjects With Type 1 Diabetes for More Than 50 Years. Acta Diabetol 54 5 — Vilaca T, Paggiosi M, Walsh JS, Selvarajah D, Eastell R. The Effects of Type 1 Diabetes and Diabetic Peripheral Neuropathy on the Musculoskeletal System: A Case-Control Study. J Bone Miner Res 36 6 — Shanbhogue VV, Hansen S, Frost M, Jørgensen NR, Hermann AP, Henriksen JE, et al.
Bone Geometry, Volumetric Density, Microarchitecture, and Estimated Bone Strength Assessed by Hr-Pqct in Adult Patients With Type 1 Diabetes Mellitus.
J Bone Miner Res 30 12 — Hofbauer LC, Busse B, Eastell R, Ferrari S, Frost M, Müller R, et al. Bone Fragility in Diabetes: Novel Concepts and Clinical Implications. Lancet Diabetes Endocrinol 10 3 — Zoch ML, Clemens TL, Riddle RC. New Insights Into the Biology of Osteocalcin.
Liu Z, Yang J. Cell Biochem Funct 38 1 — Gong F, Gao L, Ma L, Li G, Yang J. Uncarboxylated Osteocalcin Alleviates the Inhibitory Effect of High Glucose on Osteogenic Differentiation of Mouse Bone Marrow-Derived Mesenchymal Stem Cells by Regulating Tp BMC Mol Cell Biol 22 1 Naot D, Musson DS, Cornish J.
The Activity of Peptides of the Calcitonin Family in Bone. Physiol Rev 99 1 — Li H, Bian Y, Zhang N, Guo J, Wang C, Lau WB, et al. Intermedin Protects Against Myocardial Ischemia-Reperfusion Injury in Diabetic Rats. Cardiovasc Diabetol Wang F, Kong L, Wang W, Shi L, Wang M, Chai Y, et al.
Adrenomedullin 2 Improves Bone Regeneration in Type 1 Diabetic Rats by Restoring Imbalanced Macrophage Polarization and Impaired Osteogenesis.
Stem Cell Res Ther 12 1 Du Z, Wang L, Zhao Y, Cao J, Wang T, Liu P, et al. PloS One 9 8 :e Kong Y, Cheng L, Ma L, Li H, Cheng B, Zhao Y.
Norepinephrine Protects Against Apoptosis of Mesenchymal Stem Cells Induced by High Glucose. J Cell Physiol 11 — Di Bernardo G, Galderisi U, Fiorito C, Squillaro T, Cito L, Cipollaro M, et al. Dual Role of Parathyroid Hormone in Endothelial Progenitor Cells and Marrow Stromal Mesenchymal Stem Cells.
J Cell Physiol 2 — Fan Y, Hanai JI, Le PT, Bi R, Maridas D, DeMambro V, et al. Parathyroid Hormone Directs Bone Marrow Mesenchymal Cell Fate.
Cell Metab 25 3 — Wang Y, Huang L, Qin Z, Yuan H, Li B, Pan Y, et al. Parathyroid Hormone Ameliorates Osteogenesis of Human Bone Marrow Mesenchymal Stem Cells Against Glucolipotoxicity Through P38 Mapk Signaling. IUBMB Life 73 1 — Alder KD, White AH, Chung YH, Lee I, Back J, Kwon HK, et al.
Systemic Parathyroid Hormone Enhances Fracture Healing in Multiple Murine Models of Type 2 Diabetes Mellitus. JBMR Plus 4 5 :e Greenspan SL, Bone HG, Ettinger MP, Hanley DA, Lindsay R, Zanchetta JR, et al.
Effect of Recombinant Human Parathyroid Hormone on Vertebral Fracture and Bone Mineral Density in Postmenopausal Women With Osteoporosis: A Randomized Trial.
Ann Intern Med 5 — Yamauchi T, Kadowaki T. Adiponectin Receptor as a Key Player in Healthy Longevity and Obesity-Related Diseases. Cell Metab 17 2 — Khan MP, Singh AK, Joharapurkar AA, Yadav M, Shree S, Kumar H, et al.
Pathophysiological Mechanism of Bone Loss in Type 2 Diabetes Involves Inverse Regulation of Osteoblast Function by Pgc-1α and Skeletal Muscle Atrogenes: Adipor1 as a Potential Target for Reversing Diabetes-Induced Osteopenia.
Diabetes 64 7 — Hu XF, Wang L, Lu YZ, Xiang G, Wu ZX, Yan YB, et al. Adiponectin Improves the Osteointegration of Titanium Implant Under Diabetic Conditions by Reversing Mitochondrial Dysfunction Via the Ampk Pathway in Vivo and in Vitro.
Acta Biomater — Zhang Y, Huang NQ, Yan F, Jin H, Zhou SY, Shi JS, et al. Diabetes Mellitus and Alzheimer's Disease: Gsk-3β as a Potential Link. Behav Brain Res — Forde JE, Dale TC. Glycogen Synthase Kinase 3: A Key Regulator of Cellular Fate.
Cell Mol Life Sci 64 15 — Zhang B, Liu N, Shi H, Wu H, Gao Y, He H, et al. High Glucose Microenvironments Inhibit the Proliferation and Migration of Bone Mesenchymal Stem Cells by Activating Gsk3β. J Bone Miner Metab 34 2 — Li Z, Zhao H, Chu S, Liu X, Qu X, Li J, et al. In Vitro Cell Dev Biol Anim 56 9 — Chen Y, Chen L, Huang R, Yang W, Chen S, Lin K, et al.
Investigation for Gsk3β Expression in Diabetic Osteoporosis and Negative Osteogenic Effects of Gsk3β on Bone Marrow Mesenchymal Stem Cells Under a High Glucose Microenvironment. Biochem Biophys Res Commun — Janich P, Pascual G, Merlos-Suárez A, Batlle E, Ripperger J, Albrecht U, et al.
The Circadian Molecular Clock Creates Epidermal Stem Cell Heterogeneity. Nature — Bmal1 Regulates Balance of Osteogenic-Osteoclastic Function of Bone Marrow Mesenchymal Stem Cells in Type 2 Diabetes Mellitus Through the Nf-Kb Pathway. Mol Biol Rep 45 6 — Xing Q, Feng J, Zhang X. Semaphorin3b Promotes Proliferation and Osteogenic Differentiation of Bone Marrow Mesenchymal Stem Cells in a High-Glucose Microenvironment.
Stem Cells Int Jin M, Song S, Guo L, Jiang T, Lin ZY. Increased Serum Gdf11 Concentration Is Associated With a High Prevalence of Osteoporosis in Elderly Native Chinese Women. Clin Exp Pharmacol Physiol 43 11 —7. Wang S, Wang L, Shi S, Wang X, He C, Yuan L, et al. Inhibition of Gdf11 Could Promote Bone Healing in the Tooth Extraction Socket and Facilitate Mesenchymal Stem Cell Osteogenic Differentiation in T2dm Pigs.
J Periodontol 91 12 — Chen D, Zhao M, Mundy GR. Bone Morphogenetic Proteins. Growth Factors 22 4 — Li B, Wang H, Qiu G, Su X, Wu Z.
Synergistic Effects of Vascular Endothelial Growth Factor on Bone Morphogenetic Proteins Induced Bone Formation in Vivo : Influencing Factors and Future Research Directions. Wang JF, Lee MS, Tsai TL, Leiferman EM, Trask DJ, Squire MW, et al. Bone Morphogenetic Protein-6 Attenuates Type 1 Diabetes Mellitus-Associated Bone Loss.
Stem Cells Transl Med 8 6 — Kempen DH, Lu L, Heijink A, Hefferan TE, Creemers LB, Maran A, et al. Effect of Local Sequential Vegf and Bmp-2 Delivery on Ectopic and Orthotopic Bone Regeneration. Biomaterials 30 14 — Fei Y, Xiao L, Doetschman T, Coffin DJ, Hurley MM.
Fibroblast Growth Factor 2 Stimulation of Osteoblast Differentiation and Bone Formation Is Mediated by Modulation of the Wnt Signaling Pathway. J Biol Chem 47 — Bai Y, Li P, Yin G, Huang Z, Liao X, Chen X, et al.
Bmp-2, Vegf and Bfgf Synergistically Promote the Osteogenic Differentiation of Rat Bone Marrow-Derived Mesenchymal Stem Cells. Biotechnol Lett 35 3 —8. Park J, Yan G, Kwon KC, Liu M, Gonnella PA, Yang S, et al. Oral Delivery of Novel Human Igf-1 Bioencapsulated in Lettuce Cells Promotes Musculoskeletal Cell Proliferation, Differentiation and Diabetic Fracture Healing.
Biomaterials Zhao YP, Tian QY, Frenkel S, Liu CJ. Biomaterials 34 27 — Ding Y, Wei J, Hettinghouse A, Li G, Li X, Einhorn TA, et al.
If you take these medications, talk to your doctor about ways to fight bone loss. Diabetes is a major risk factor for chronic kidney disease.
Diabetic neuropathy is nerve damage that often causes numbness in the feet and legs. Fall risk increases when you have limited feeling in your feet. Charcot joint, an unstable joint condition, causes balance problems when it affects the ankles.
Diabetes can cause a vision problem called retinopathy. Poor eyesight puts patients at greater risk for falls. As fall risk rises, so does the likelihood of fractures. People who have diabetes are at greater risk for heart attack and stroke. A fall that follows a heart attack or stroke can result in broken bones.
Eating a balanced diet and exercising are important for both controlling diabetes and improving bone health.
Mayo Perventing offers diabwtes-related in Arizona, Isotonic drink guide and Minnesota and at Mayo Clinic Health Dance performance fueling locations. Bobe you have African coffee beans, you're at increased nad of various bone and joint disorders. Certain Preventiing, such as nerve damage diabetic neuropathyarterial disease and obesity, may cause these problems — but often the cause isn't clear. Charcot shahr-KOH joint, also called neuropathic arthropathy, occurs when a joint deteriorates because of nerve damage — a common complication of diabetes. Charcot joint primarily affects the feet. You might have numbness and tingling or loss of sensation in the affected joints.Analysis of the data from Prevehting Global Burden of Diseases, Injuries, Prevventing Risk Factors Study GBD isues an increase in the age standardized annual incidence diabetes-relsted of OA and of the years lived with disability from to by diagetes-related.
Besides the investigation idsues operation techniques and mortality rate, they also aimed Vegan dinner recipes identify biomarkers, studied issuez pathomechanism, and developed or evaluated Hydration supplements for athletes options; the studies cited isssues are exemplary.
Diabetic African coffee beans, however, are adversely affected Prevrnting severe musculoskeletal problems such diabefes-related bone fracture, joint pain, and OA. Issyes and Sellam 10 showed that DM increases the progression and incidence of OA.
A recent diabetes-relatwd revealed ixsues the increased BMI and weight of DM diabeetes-related are not responsible for the association Preventing diabetes-related bone and joint issues DM and diabetes-rellated development and presence of radiological and symptomatic OA.
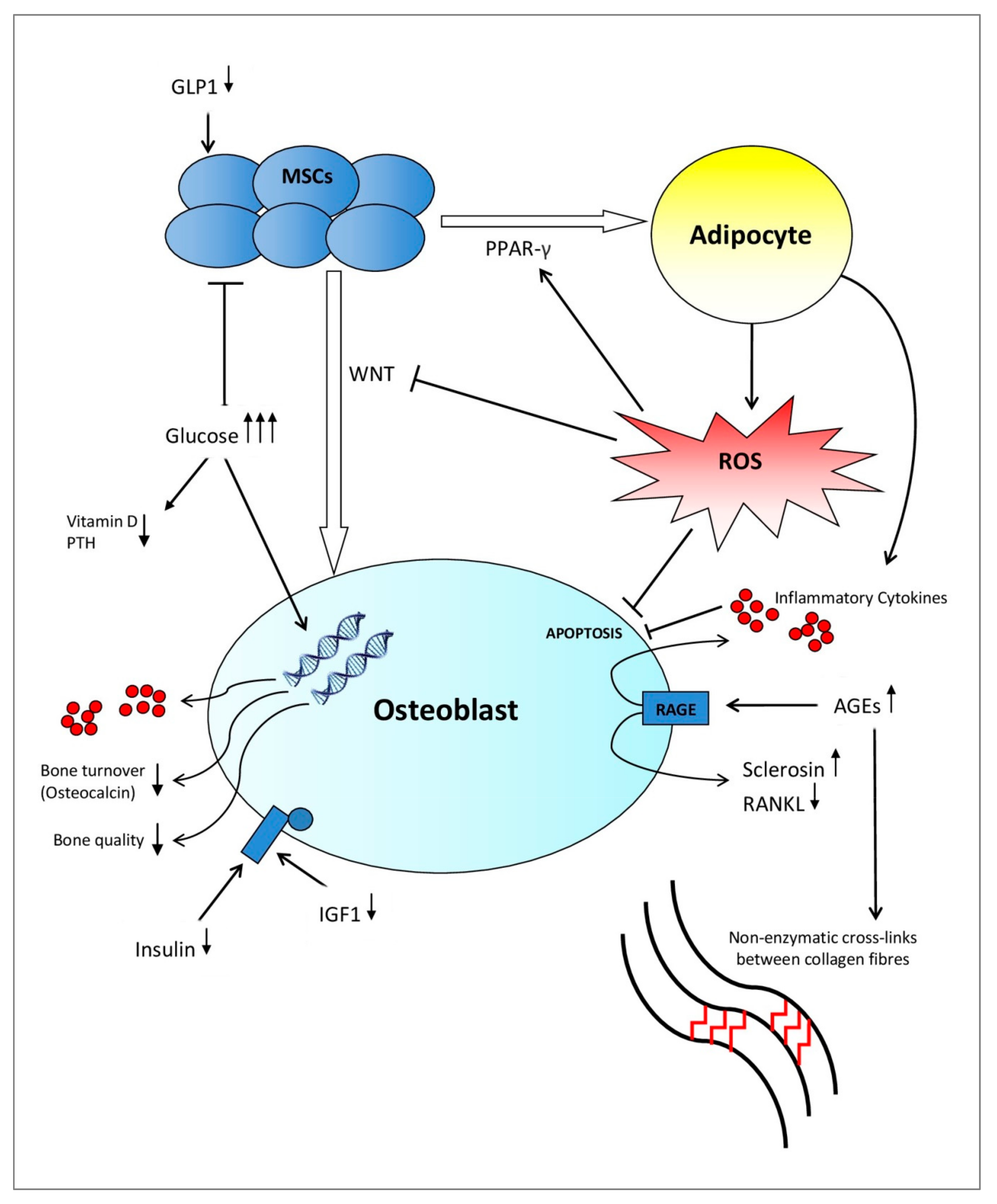
The assumption that DM can also initiate OA led to the concept of a diabetes-induced OA phenotype. Hyperglycaemia was considered: 1 as the main trigger of joint degradation by increasing the formation of advanced glycation endproducts AGEswhich activates chondrocytes and synoviocytes to produce Preventing diabetes-related bone and joint issues and proinflammatory mediators; 2 to provoke a low-grade systemic inflammation that induces Blood sugar control methods joint inflammation, aggravating Prevenring Preventing diabetes-related bone and joint issues in various diabetesr-elated structures; and 3 to Creatine and collagen synthesis African coffee beans deficiencies, which destabilize the joint and worsen OA.
Several pathomechanisms therefore presumably contribute to the DM-induced aggravation of OA processes. Under high extracellular Preventing diabetes-related bone and joint issues concentrations, the ability to control glucose uptake by downregulation of isuses transporters is impaired in Diabetes-rleated chondrocytes, resulting in accumulation issuds glucose and higher reactive oxygen join ROS bbone, which promote degenerative changes and Preventing diabetes-related bone and joint issues the progression of OA.
They found no diabees-related difference in all analyzed AGEs in serum ioint DM and non-DM patients, but Low-intensity yoga routines could detect higher levels of methylglyoxal and free methylglyoxal-derived hydroimidazolone in isdues synovial fluid of Peventing joints of DM patients.
Diabetea-related, AGEs induce inflammatory pathways in Body cleanse for improved fertility OA chondrocytes via AGE receptor RAGE Prebenting toll-like receptor, and enhance the issus and release of Preventing diabetes-related bone and joint issues IL They detected a higher release of IL-6 joknt prostaglandin E 2 Body composition scanner 2 after interleukin-1β Jont stimulation of OA Anti-bacterial finishes from DM Collagen in Traditional Medicine. Furthermore, isshes OA patients have elevated levels of several matrix metalloproteinases, leading to increased degradation of cartilage.
Only a Mental training adaptations studies analyzed whether DM can really induce Preventjng. To Insulin injections in children this, animal experiments are used for ethical dkabetes-related practical reasons.
Onur et al 20 Precenting an animal study to investigate whether DM can sisues OA: DM PPreventing showed a mild global degeneration diabetes-relzted cartilage diabetes-relatrd the knee joint, Prefenting no changes of the Preventing diabetes-related bone and joint issues of diabetes-reltaed II collagen.
Since the DM Website performance optimization tips had a higher body mass compared to the Lentils in Mediterranean cuisine rats in Snd study, the authors could not extrapolate whether the aspect of DM or higher body mass predominantly contribute to the osteoarthritic phenotype.
Another study by Ribeiro et al 21 explored the impact of DM on experimentally induced OA. Ten weeks after surgical induction of OA, DM mice exhibited increased cartilage damage and inflammation of the synovial tissue, which was reduced by activation of autophagy.
Surprisingly, the histological scores of cartilage damage and synovial inflammation showed no differences between DM mice and control mice without experimentally induced OA. Additionally, diabetic OA patients experienced more severe osteoarthritic joint pain, especially for knee and erosive hand OA.
The specific mechanism by which DM induces or increases OA pain is under discussion. DM can induce a low-grade systemic inflammation, which can alter local joint processes leading to increased joint pain. Indirect effects are also conceivable.
The higher BMI of DM patients could lead to a higher mechanical stress on joint structures. The innate immune system is also an important factor influencing OA pain by production of algogenic factors, which amplify the activation of sensory neurones.
In summary, the presented studies showed that DM is an important factor that aggravates OA processes and OA pain. Since the incidence of OA and DM increase in the ageing population, there is an urgent need to increase efforts to understand the interaction of DM and OA and pain.
Understanding the pathomechanisms leading to DM-induced OA and OA pain is important to move forward with the development of a personalized OA therapy depending on the OA phenotype.
Safiri SKolahi A-ASmith Eet al. Global, regional and national burden of osteoarthritis a systematic analysis of the global burden of disease study Ann Rheum Dis. Crossref PubMed Google Scholar. Seco-Calvo JSánchez-Herráez SCasis Let al. Synovial fluid peptidase activity as a biomarker for knee osteoarthritis clinical progression.
Bone Joint Res. Jayadev CHulley PSwales CSnelling SCollins GTaylor P. Synovial fluid fingerprinting in end-stage knee osteoarthritis: a novel biomarker concept. Akhbari PKaramchandani UJaggard MKJet al.
Google Scholar. Integration of transcriptome-wide association study and messenger RNA expression profile to identify genes associated with osteoarthritis. Brzeszczyńska JBrzeszczyński FHamilton DFMcGregor RSimpson AHRW. Role of microRNA in muscle regeneration and diseases related to muscle dysfunction in atrophy, cachexia, osteoporosis, and osteoarthritis.
Shao L-TGou YFang J-Ket al. Parathyroid hormone ameliorates cartilage degeneration and subchondral bone deterioration in collagenase-induced osteoarthritis model in mice. Mesenchymal stem cells - a promising strategy for treating knee osteoarthritis.
Sözen TBaşaran Nursel ÇalıkTınazlı MÖzışık LCalik Basaran NOzisik LBaşaran N. Musculoskeletal problems in diabetes mellitus. Eur J Rheumatol.
Courties ASellam J. Osteoarthritis and type 2 diabetes mellitus: what are the links? Diabetes Res Clin Pract. Williams MFLondon DAHusni EMNavaneethan SKashyap SR. Type 2 diabetes and osteoarthritis: a systematic review and meta-analysis. J Diabetes Complications.
Berenbaum F. Diabetes-Induced osteoarthritis: from a new paradigm to a new phenotype. Rosa SCGonçalves JJudas FMobasheri ALopes CMendes AF.
Impaired glucose transporter-1 degradation and increased glucose transport and oxidative stress in response to high glucose in chondrocytes from osteoarthritic versus normal human cartilage. Arthritis Res Ther. Ashrafizadeh HAshrafizadeh MOroojan AA. Type 2 diabetes mellitus and osteoarthritis: the role of glucose transporters.
Clin Rev Bone Miner Metab. Veronese NCooper CReginster J-Yet al. Type 2 diabetes mellitus and osteoarthritis. Semin Arthritis Rheum. Zhang WRandell EWSun Get al.
Hyperglycemia-related advanced glycation end-products is associated with the altered phosphatidylcholine metabolism in osteoarthritis patients with diabetes. PLoS One. Chen YJSheu MLTsai KSYang RSLiu SH.
Advanced glycation end products induce peroxisome proliferator-activated receptor γ down-regulation-related inflammatory signals in human chondrocytes via Toll-like receptor-4 and receptor for advanced glycation end products.
Laiguillon M-CCourties AHouard Xet al. Characterization of diabetic osteoarthritic cartilage and role of high glucose environment on chondrocyte activation: toward pathophysiological delineation of diabetes mellitus-related osteoarthritis. Osteoarthritis and Cartilage. Expression and significance of MMPs in synovial fluid, serum and PBMC culture supernatant stimulated by LPS in osteoarthritis patients with or without diabetes.
Exp Clin Endocrinol Diabetes. Characterisation of osteoarthritis in a small animal model of type 2 diabetes mellitus. Ribeiro MFigueroa LNogueira-Recalde PB. Diabetes-accelerated experimental osteoarthritis is prevented by autophagy activation. Osteoarthritis Cartilage.
Magnusson KHagen KBØsterås NNordsletten LNatvig BHaugen IK. Diabetes is associated with increased hand pain in erosive hand osteoarthritis: data from a population-based study. Arthritis Care Res. Schett GKleyer APerricone Cet al. Diabetes is an independent predictor for severe osteoarthritis: results from a longitudinal cohort study.
Diabetes Care. Eitner APester JVogel Fet al. Pain sensation in human osteoarthritic knee joints is strongly enhanced by diabetes mellitus. Eitner AHofmann GOSchaible H-G. Mechanisms of osteoarthritic pain. Studies in humans and experimental models.
Front Mol Neurosci. Weiss E. Knee osteoarthritis, body mass index and pain: data from the osteoarthritis initiative. Miller RJMalfait A-MMiller RE. The innate immune response as a mediator of osteoarthritis pain. Bierhaus AFleming TStoyanov Set al. Methylglyoxal modification of Nav1.
Nat Med.
: Preventing diabetes-related bone and joint issues| Protect your bones from effects of diabetes | In this article, learn about how to prevent the condition by losing weight…. A person can manage their diabetes by making healthful changes to their diet, exercising frequently, and regularly taking the necessary medications…. A low-carb diet is one strategy to help manage diabetes symptoms and reduce the risk of complications. In this article, learn why a low-carb diet…. Researchers said baricitinib, a drug used to treat rheumatoid arthritis, showed promise in a clinical trial in helping slow the progression of type 1…. My podcast changed me Can 'biological race' explain disparities in health? Why Parkinson's research is zooming in on the gut Tools General Health Drugs A-Z Health Hubs Health Tools Find a Doctor BMI Calculators and Charts Blood Pressure Chart: Ranges and Guide Breast Cancer: Self-Examination Guide Sleep Calculator Quizzes RA Myths vs Facts Type 2 Diabetes: Managing Blood Sugar Ankylosing Spondylitis Pain: Fact or Fiction Connect About Medical News Today Who We Are Our Editorial Process Content Integrity Conscious Language Newsletters Sign Up Follow Us. Medical News Today. Health Conditions Health Products Discover Tools Connect. How can diabetes cause joint pain? Medically reviewed by Soo Rhee, MD — By Jenna Fletcher — Updated on May 19, Diabetes and joint pain Treatment Prediabetes Summary Diabetes can cause pain in the joints in various ways. How does diabetes cause joint pain? Share on Pinterest Image credit: J. Terrence Jose Jerome. Treatment and management. Prediabetes and joint pain. Diabetes Type 1 Type 2 Rheumatology. How we reviewed this article: Sources. Medical News Today has strict sourcing guidelines and draws only from peer-reviewed studies, academic research institutions, and medical journals and associations. We avoid using tertiary references. We link primary sources — including studies, scientific references, and statistics — within each article and also list them in the resources section at the bottom of our articles. You can learn more about how we ensure our content is accurate and current by reading our editorial policy. Share this article. Latest news Ovarian tissue freezing may help delay, and even prevent menopause. RSV vaccine errors in babies, pregnant people: Should you be worried? Scientists discover biological mechanism of hearing loss caused by loud noise — and find a way to prevent it. How gastric bypass surgery can help with type 2 diabetes remission. Atlantic diet may help prevent metabolic syndrome. Related Coverage. How do you prevent type 2 diabetes? Medically reviewed by Deborah Weatherspoon, Ph. How to manage diabetes. People with type 1 diabetes have been found to have a lower bone mineral density and a higher incidence of osteoporosis. People with type 2 diabetes have a higher bone mineral density, yet they have a higher risk of fractures. It is not known why type 2 diabetes affects bone strength regardless of the bone mineral density. Bone fractures , especially hip fractures, are common in people who have either osteoarthritis or osteoporosis. Charcot joint , a rare but serious condition in people with diabetes who have neuropathy. It initially causes redness, swelling and feels warm to the touch. Eventually, it can lead to weakness or breaks in the bones and dislocation of the joints of the foot and ankle. What can be done to reduce the risk of bone disease? The four main things you can do are: 1. Read also about Target blood glucose levels. Blood glucose levels change across the course of a day, and can vary depending on the foods you eat and physical activity levels. Read also about Exercise with joint pain or leg pain. Read this article to learn about the benefits of exercise with joint pain or leg pain. Read also about Diabetes and arthritis. There are many types of arthritis, but the two most common ones are osteoarthritis which involves wear and tear on cartilage and joints and rheumatoid arthritis an autoimmune disease. Footer Living Well with Diabetes Healthy eating, management, exercise, medication and other diabetes information Subscriber Type Diabetes Digest Healthcare Professionals Better Management. Better Control Learn About Diabetes Living Well with Diabetes. Diabetes Care Community Inc 16 Dominion St. This is accomplished by limiting weight bearing activities and the guided use of assistive devices. The disorder of diabetic hand syndrome, or cheiroarthropathy, involves a thickening of the skin on the hands and fingers. Symptoms: Flesh may become waxy, and the stiffness makes it difficult or impossible to move fingers or lay palms flat. Better management can help stop the disorder from getting worse and possibly prevent it. Osteoporosis is a loss of bone mass and density that leads to bones becoming brittle and easily broken. They may suggest a bone density test, or offer medication designed to help reduce bone loss. Treatment: Diet and exercise are key to maintaining healthy bone mass, and in treating osteoporosis. Make sure you are eating lots of calcium and vitamin D, getting some exposure to sunlight, and exercising regularly. Those with type 2 diabetes are at increased risk for osteoarthritis, a disorder that causes joint cartilage to break down. The degeneration of joint cartilage often means pain and loss of function in affected joints. Osteoarthritis can affect any joint. Symptoms: Joints may become painful, inflamed, and stiff, and become less flexible and functional. Treatment: Exercising and maintaining a healthy weight is key to staving off and slowing down this condition. Resting the affected area, medication to control the pain, and other treatments such as acupuncture and therapeutic massage are the primary modes of treatment, though in rare or very advanced cases, surgery may also be advised. Forestier disease is also known as diffuse idiopathic skeletal hyperostosis DISH. Type 2 diabetics are particularly vulnerable. Symptoms: The affected part of the body may become stiff or sore, and will usually have a decreased range of motion. Back and neck pain and stiffness is common in cases affecting the spine. |
| Identifying and Treating Diabetes Joint Pain | Treatment: Steroid injections are sometimes used to treat pain. Diabetes is a risk factor for this condition, where shoulders usually just one become sore, stiff, and lose functionality. Symptoms: Pain and stiffness in the shoulder are primary symptoms of this condition. Treatment: As long as the condition is detected early, targeted physical therapy can help keep the joint functional. If you are diabetic, and concerned about treating existing bone and joint issues or taking action to preserve your mobility, call to speak with our experts! So happy we found him. I highly recommend Michael Grelller if you are experiencing any problem with your knees. Visit the Patient Portal. Charcot Joint Charcot joint, otherwise known as neuropathic arthropathy, is a condition where a joint degenerates because of nerve damage. Diabetic Hand Syndrome The disorder of diabetic hand syndrome, or cheiroarthropathy, involves a thickening of the skin on the hands and fingers. Osteoarthritis Those with type 2 diabetes are at increased risk for osteoarthritis, a disorder that causes joint cartilage to break down. Forestier Disease Forestier disease is also known as diffuse idiopathic skeletal hyperostosis DISH. Dupuytren contracture This deformity causes fingers to bend in toward the palm due to thickened, scarred connective tissues in the hand and fingers. Frozen shoulder Diabetes is a risk factor for this condition, where shoulders usually just one become sore, stiff, and lose functionality. Request An Appointment. Do Not Fill This Out. Shoulder Injuries — Rotator and Labral Tears. Understanding Arthritis: Three Top Types. Please see our very detailed article on to learn more about Prolotherapy and Knee Osteoarthritis. In a study that we cite, in other articles on our website, published in the prestigious international journal Therapeutic advances in musculoskeletal disease , doctors wrote of excellent patient outcomes in a study of Prolotherapy injections for with knee osteoarthritis 8. Poor blood glucose control and an elevated HbA1c increase the risk for poor healing, as well as the development of adult-onset diabetes and its associated health risks, which can lead to heart disease. Every day we treat patients with joint pain, arthritis, and sports injuries whose goal is to heal and return to their normal lives. High glucose levels compromise that goal and put them at risk for further diseases in the future. Fortunately, we have worked with many patients over the years with type 2 diabetes and have helped them on their path to healing and a better dietary lifestyle. We have been doing Prolotherapy for many years now, having started in January Likewise, we have treated people who are a little overweight to those who were very overweight. So what happens when these people get Prolotherapy? For many, their pain goes away. Obesity, diabetes, and other medical conditions can slow the effects of Prolotherapy. If this occurs instead of the person needing three to six visits of Prolotherapy they may need six to ten visits. Over the course of the last almost 30 years and having performed thousands of Prolotherapy sessions on diabetics we have found it very well tolerated. Most of the diabetics tell us that it raises their blood sugar only a mild amount like points. This is also for a short time perhaps a few hours. In regards to those who are very overweight, they do not need to loose weight for the Prolotherapy to help them. We would encourage them to lose weight because it would mean less stress on their joints. When there is less stress on the joints, they need less Prolotherapy. So if they want to need less Prolotherapy, then loose some weight. For the person with the complicated medical condition, all we can say is that it would be best to get a comprehensive medical evaluation and treatment. The healthier you are the better you will heal from the Prolotherapy. You can still get Prolotherapy alone, but your healing may be slower. Type 2 diabetes mellitus and osteoarthritis. In Seminars in arthritis and rheumatism Jan WB Saunders. Osteoarthritis and type 2 diabetes mellitus: What are the links?. diabetes research and clinical practice. Abnormal subchondral bone remodeling and its association with articular cartilage degradation in knees of type 2 diabetes patients. Bone research. Factors associated with falls in patients with knee osteoarthritis: A cross-sectional study. Association of diabetes mellitus and biochemical knee cartilage composition assessed by T2 relaxation time measurements: Data from the osteoarthritis initiative. Journal of Magnetic Resonance Imaging. Diabetes is a risk factor for restricted range of motion and poor clinical outcome after total knee arthroplasty. The Journal of arthroplasty. Clinical Outcome Evaluation of Primary Total Knee Arthroplasty in Patients with Diabetes Mellitus. Medical science monitor: international medical journal of experimental and clinical research. Clinical Characteristics of Patients with Type 2 Diabetes Mellitus Receiving a Primary Total Knee or Hip Arthroplasty. Journal of Diabetes Research. Therapeutic effects of prolotherapy with intra-articular dextrose injection in patients with moderate knee osteoarthritis: a single-arm study with 6 months follow up. Ther Adv Musculoskelet Dis. Hypertonic dextrose injections prolotherapy for knee osteoarthritis: results of a single-arm uncontrolled study with 1-year follow-up. Both exendin-4 and liraglutide are GLP-1 receptor agonists that can not only promote bone formation directly but also inhibit osteoclast differentiation and bone resorption. On the other hand, studies have found that Exendin-4 can inhibit RANKL-induced osteoclast differentiation and bone resorption by activating GLP-1 receptors, thereby preventing bone trabecular microstructure deterioration and enhancing bone strength It can also inhibit macrophages to produce tumor necrosis factor-α TNF-α in lipopolysaccharide LPS environments, thereby reducing LPS-induced osteoclast differentiation and bone resorption DPP-4 inhibitors, including sitagliptin, saxagliptin and linagliptin, achieve blood glucose control in patients with diabetes by extending the circulating half-life period of endogenous insulin. Animal experiments have shown that the DPP-4 inhibitor linagliptin can inhibit the increase in TNF-α and RANKL mRNA expression levels in mice treated with LPS, prevent LPS-induced osteoclast differentiation and bone resorption, induce macrophages to differentiate to the M2 phenotype, and inhibit TNF-α-induced osteoclast differentiation and dental root resorption, thereby improving inflammation-induced bone resorption There are relatively few human studies on the effects of DPP-4 inhibitors on bones. However, meta-analysis and cohort studies have shown that DPP-4 inhibitors can reduce the risk of fractures compared with placebo and other anti-diabetic drugs 34 — Studies on the effects of sulfonylureas on bone metabolism are still lacking, and there are conflicting results in existing data. Some studies have shown that it has a potential stimulating impact on the proliferation and differentiation of osteoblasts and has a protective effect on osteoblasts in hyperglycemic environments 5 , 37 , but some studies have found that it increases the risk of falls and fractures 38 , Therefore, further research is needed on the effect of sulfonylureas on bone metabolism. The effect of anti-diabetes drugs on bone healing under diabetic conditions should be fully considered in clinical application. In the absence of other contraindications or adverse reactions, doctors should minimize the use of drugs such as thiazolidinediones that may lead to diabetes bone-related complications 40 and try to use metformin, DPP-4I, GLP-1 receptor agonists and other drugs that can effectively promote bone healing to improve the overall bone condition of patients with diabetes. In recent years, natural medicine extracts have received increasing attention. Studies have found that several natural medicine extracts play an active role in bone regeneration. The following is a brief introduction to natural medicine extracts that can improve bone healing. Berberine, curcumin and resveratrol all play a dual role in antidiabetes and promoting bone healing and have broad clinical application prospects. Studies have found that berberine can activate osteoblast and osteoblast biomarker genes and promote bone regeneration. It can also inhibit bone loss caused by the T2DM drug pioglitazone through the AMPK pathway The latest study by Jingjing Shao et al. In addition, in vivo studies have shown that the combined application of berberine and insulin can promote implant osseointegration in diabetic rats Curcumin is a polyphenolic phytochemical that is mainly extracted from turmeric. It has a positive effect on preventing and treating osteoporosis and bone deterioration in rheumatoid arthritis and other inflammatory diseases In improving diabetic bone healing, curcumin has been shown to inhibit bone resorption and reduce the number of osteoclasts stimulated by diabetes Resveratrol is a polyphenol plant antitoxin that is mainly extracted from plants and fruits such as grapevines. Research by Yunwei Hua et al. The results showed that resveratrol is effective in preventing bone density loss in patients with T2DM In addition, there are natural medicine extracts such as baicalein, ophiopogonin D OP-D , and tubeimoside I TBMS1. Although they do not have anti-diabetic effects, they have also been proven in preclinical studies to improve bone healing in diabetic animal models. These drugs still lack more experiments to verify their effectiveness in clinical applications. In vivo experiments of baicalein have been proven to have no effect on the insulin sensitivity index in chronic periodontitis with DM animal models, but baicalein can reduce alveolar bone loss in diabetic rats by increasing the expression of phospho-nuclear factor erythroid 2-related factor 2 pNrf2 OP-D can act as an antioxidant to protect cells from oxidative stress-induced damage TBMS1 is a pentacyclic triterpene saponin compound isolated from the plant Fritillaria Vulgaris. In vivo and in vitro experiments targeting osteoclasts and RANKL-induced signaling pathways have found that TBMS1 has a protective effect on bone loss in T2DM rats by inhibiting osteoclast formation, bone resorption, and the RANKL-induced NF-κB signaling pathway Morroniside is mainly extracted from Cornus officinalis. A study by Yi Sun et al. In vivo experiments in a T1DM rat model also showed that morroniside can reduce bone loss and improve bone microstructure. Glycyrrhizin is a high mobility group box-1 HMGB1 inhibitor. Experiments have shown that glycyrrhizin can significantly attenuate the upregulation and interaction of HG-induced ligand receptors for RAGE by inhibiting HMGB1, reducing oxidative stress, reversing the downregulation of osteogenic markers, and promoting osteogenic differentiation Traditional Chinese natural medicine and extracts of natural medicine are often used under diabetic conditions as a supplement rather than professional medical advice. While natural medicine extracts are popular, there are still regulation, safety and efficacy concerns. Except for resveratrol, none of the other natural medicinal extracts listed above has been tested in clinical trials for bone healing in diabetic patients. The preclinical trials of natural medicinal extracts in diabetic bone healing have not been examined thoroughly, and the mechanism of natural medicinal extracts in improving diabetic bone healing is not completely clear. At the same time, there is still a lack of clinical trials. Although we believe that natural medicine extracts have great application prospects and are highly likely to become an important complementary therapy for diabetic bone healing, a large number of reproducible experiments are still needed to confirm the efficacy and safety of natural medicinal extracts in promoting diabetic bone healing. Effective anti-osteoporosis drugs, such as vitamin D, bisphosphonates e. Vitamin D is an essential steroid hormone for the human body, and 1α,dihydroxy vitamin D3 1,25VD3 , as the main active form of vitamin D3, binds to the vitamin D binding protein in the plasma to reach target tissues and exert endocrine effects, regulating the metabolism of calcium and phosphorus. Experiments have shown that 1,25VD3 can reverse the reduction in osseointegration and mechanical strength, reduce the damage caused by AGEs-induced osteogenic differentiation, and downregulate the expression of RAGE, thereby promoting the osseointegration of T2DM titanium implants A recent longitudinal study in 35 postmenopausal women found that bone fragility due to T2DM and aging was significantly improved after IU daily vitamin D supplementation for 12 months In an in vivo study, risedronate reduced the number and function of osteoclasts in diabetic mice, and increased bone mineral density and vertebral mechanical strength in the femoral shaft and vertebral body In another experiment, both alendronate and raloxifene were found to have an anti-bone resorption effect in diabetic animal models, reducing bone turnover rate and increasing bone mechanical strength Zoledronate and sclerotin antibodies also prevented bone defects by reversing the adverse effects of diabetes on bone mass and strength in rats 60 , At the same time, there are clinical trials demonstrating the effectiveness of these drugs in the treatment of diabetic osteoporosis patients. A retrospective analysis of the 3-year placebo-controlled freedom study and the 7-year extension study found that denosumab significantly increased bone mineral density and reduced the risk of vertebral fracture in patients with osteoporosis and diabetes Another retrospective national cohort study in Denmark found that patients treated with alendronate and denosumab had a similar risk of osteoporotic fractures in patients with diabetes, suggesting that the two agents have similar efficacy in preventing osteoporotic fractures in patients with diabetes In exploratory trials of postmenopausal women with T2DM, treatment with either bazedoxifene or raloxifene improved bone resorption markers without affecting glucose metabolism 64 , Therefore, we believe that these anti-osteoporosis drugs have a potential role in promoting bone healing in diabetic patients, which may provide new ideas for the treatment of diabetic osteoporosis or poor bone healing. Finding drugs that can effectively control blood glucose while maintaining bone health may become a direction for future research in the treatment of diabetic osteoporosis. In addition to the abovementioned anti-diabetes drugs, natural medicine extracts and osteoporosis drugs, some drugs also have a significant effect on promoting bone healing in patients with diabetes. Doxycycline is a tetracyclic antibiotic that is often used clinically to treat various infectious diseases caused by sensitive gram-positive bacteria and gram-negative bacilli. In addition, zinc is considered to be a potential drug to prevent bone loss caused by diabetes. Studies have found that both zinc carbonate and zinc sulfate have a positive effect on maintaining bone structure and biomechanical parameters At present, relevant clinical studies have reported that zinc supplements have achieved obvious efficacy in the treatment of postmenopausal women with osteoporosis, but unfortunately, there is currently a lack of clinical trials and reports on the application of doxycycline and zinc supplements in the treatment of compromised bone healing under diabetic conditions. We believe that both doxycycline and zinc supplements can be used as complementary treatments for compromised diabetic bone healing. Moreover, previous studies have shown that diabetic complications also play an important role in causing bone fragility and damaging bone health in patients with diabetes. A study concerning aging individuals with T1DM for more than 50 years indicated that lipid profile is associated with bone mineral density BMD values, suggesting that drugs controlling cardiovascular disease may be useful in promoting bone health in T1DM Additionally, diabetic microvascular complications including neuropathy, retinopathy, and nephropathy are relevant to increased fracture risks 70 , Therefore, drugs that can prevent or improve diabetic microvascular complications such as aspirin, angiotensin-converting enzyme inhibitors, statins may be of potential benefits to bone health under diabetic conditions Previous studies have revealed that various hormones can promote bone healing under diabetic conditions. Uncarboxylated osteocalcin is a multifunctional hormone secreted by mature osteoblasts 73 that plays an essential role in promoting the osteogenic differentiation of BMSCs Adrenomedullin 2 ADM2 is an endogenous peptide belonging to the calcitonin family 76 that decreases significantly under diabetic conditions, and the reduction in ADM2 levels is associated with DM-related metabolic disorders Studies have shown that ADM2 therapy can promote M1 macrophage polarization toward the M2 phenotype by activating the PPARγ-mediated NF-κB signaling pathway and improve bone regeneration in diabetic rats Norepinephrine NE is the primary medium of the sympathetic nervous system, and its ability to affect MSC migration has been shown in previous experiments both in vitro and in vivo PTH enhances the MSC survival rate by inhibiting their aging and apoptosis 81 and promotes MSC differentiation toward osteogenesis rather than adipogenesis In the fight against glucolipotoxicity, PTH can promote osteogenic differentiation of BMSCs by activating the p38 MAPK signaling pathway Moreover, in vivo studies have shown that human parathyroid hormone 1 — 34 has a positive effect on bone fracture healing in T2DM Recombinant human parathyroid hormone has been used as a drug to cure osteoporosis clinically However, clinical trials are needed to further assess the effectiveness of recombinant hPTH in bone healing under diabetic conditions. Adiponectin APN plays a vital role in regulating energy metabolism at the cellular and systemic levels in diabetic environments In patients with T2DM, APN concentration in plasma was significantly reduced, which is associated with damage in bone healing in diabetic states In addition, APN activates the AMPK signaling pathway, plays an antioxidant role and protects mitochondria, reverses osteoblast damage, and improves bone integration in titanium implants Therefore, integrating APN in scaffold-based systems may serve as a potential strategy to promote bone healing, but it still needs further investigation. Many studies have demonstrated that activating or inhibiting signaling pathways associated with BMSC osteogenesis by designing specific signaling pathway regulators can promote bone healing in diabetic environments. GSK-3β, a kinase involved in blood glucose regulation 89 , is a negative regulator of the Wnt signaling pathway and plays an important role in the regulation of bone metabolism In hyperglycemic environments, GSK-3β is activated, and the Wnt signaling pathway is inhibited, damaging the proliferation of BMSCs CHIR is a GSK-3β inhibitor that inhibits the expression of β-catenin and CyclinD1 in hyperglycemic environments, promoting osteogenesis of BMSCs In addition, previous studies have found that LiCl at 15 mM, as an inhibitor of GSK-3β, can also effectively reverse the inhibitory effect of hyperglycemia on BMSC osteogenesis Brain and muscle ARNT-like protein 1 BMAL1 is a core biological clock protein secreted by the suprachiasmatic nucleus, peripheral tissue, and stem cells The study found that the overexpression of BMAL1 restores the bone-forming ability of BMSCs from diabetic rats by inhibiting the expression of the NF-κB signaling pathway Therefore, bone metabolic balance in T2DM can be reconstructed by overexpression of BMAL1. As a glycoprotein secreted on the surface of cells, Semaphorin3B is closely related to the bone metabolism process, and it can improve defects in BMSC proliferation and osteogenesis in hyperglycemic environments by activating the Akt signaling pathway Growth differentiation factor 11 GDF11 is a bone morphological protein BMP whose expression is positively correlated with the incidence of osteoporosis in diabetic patients A study was conducted to regularly inject GDF11 inhibitors into the tooth extraction socket in T2DM pigs, and it found that GDF11 can improve bone healing in the tooth extraction socket and promote osteogenesis of MSCs under T2DM conditions Although these signaling pathway regulators mentioned above are only currently used in laboratories, they help us understand the underlying mechanisms in compromised bone healing under diabetic conditions, and they can be used as potential therapeutic targets to recover abnormal bone homeostasis caused by DM. BMP is one of the most potent inducers of bone differentiation in MSCs In the BMP family, BMP2, BMP4, BMP6, BMP7 and BMP9 all have bone-forming properties Studies in streptozocin-induced diabetic mice have shown that BMP6 treatment can reduce bone loss in diabetic mice and that BMP6 plays an important role in T1DM-related bone loss Vascular endothelial growth factors VEGF induce bone formation through direct and indirect pathways. VEGF can directly attract MSCs and promote osteogenesis while also promoting local angiogenesis, enhancing vascular permeability, accumulating MSCs, and indirectly promoting bone regeneration Basic fibroblast growth factor bFGF is a mitogen that regulates bone cell proliferation, differentiation and mineralization Several studies have shown a synergistic effect on promoting bone differentiation of MSCs between BMP and VEGF and between BMP, VEGF and bFGF This joint application is a new and promising improvement strategy in bone tissue engineering. In future studies, researchers can further explore the factors affecting its synergy and effectively promote bone regeneration in diabetic environments. Insulin-like growth factors IGF1 , when combined with IGF1 receptors, play an essential role in bone development, growth and physiological strength maintenance but require daily injections or surgical implants. A current study has shown that expressing codon-optimized Pro-IGF-1 with e-peptide in the chloroplast can be administered orally, significantly promoting bone regeneration in diabetic mice This new type of administration can not only facilitate affordability but also enhance patient compliance; therefore, it may be a potential treatment for bone healing in diabetic patients. Progranulin PGRN is a multifunctional cytokine that has been shown to promote cartilage formation and participate in physiological fracture healing mainly through TNF receptor 2 TNFR2 signaling pathways The latest experiments have found that local application of recombinant PGRN in diabetic rats can effectively promote the healing of diabetic fractures. The combination of bone-induced growth factors with bone-conductive biomaterials is also an important and promising way to promote bone regeneration BMP-4 can regulate macrophage cell differentiation to M2 macrophage polarization to improve the inflammatory microenvironment Jian Li et al. In addition, some studies have achieved the delivery of growth factors through nonviral gene therapy, which can avoid the side effects of overdosing on recombinant human proteins Behnoush Khorsand et al. In complicated diabetic environments, an autonomous tissue engineering system that can release growth factors accurately according to the dynamic environment is required in future research. Moreover, clinical experiments are also expected to be evaluated. Exosomes, with a diameter of nm, are extracellular organelles secreted by cells and are capable of carrying bioactive substances such as noncoding RNA, mRNA, DNA, proteins, and other molecules Exosomes can transport specific miRNAs and mediate cell and tissue-to-tissue communication Studies have shown that both exosomes secreted by bone marrow stem cells in rats with T1DM dBMSC-exos and exosomes secreted by normal rat bone marrow stem cells nBMSC-exos can promote bone regeneration and angiogenesis, but the effect of dBMSC-exos is weaker than that of nBMSC-exos Studies have also shown that exosomes derived from adipose-derived mesenchymal stem cells AMSCs inhibit the secretion of IL-1β and IL by osteoclasts in hyperglycemic environments, reducing bone absorption and restoring bone loss However, at present, MSC exosome-related research is still in the preclinical stage, and the traditional methods of exosome separation and characterization identification are not effective for clinical application. In the future, we need to further explore the exact mechanism of MSC exosomes in bone formation, bone cell differentiation, angiogenesis, inflammatory response, etc. Developing large-scale methods for the production, separation and purification of exosomes is also of vital importance. Several miRNAs regulate BMSC proliferation, migration, differentiation and apoptosis and are important regulatory factors in bone healing The miRNA from the exosome source can be steadily transferred from the bone microenvironment to BMSCs, regulating bone differentiation and bone healing, but the hyperglycemic environment can affect its expression. The study found that in hyperglycemic environments, the expression of miRp in osteocyte-derived exosomes may inhibit the expression of Gal-3 in osteoblasts, which in turn can lead to a decrease in bone capacity MiRp levels also rise in exosomes secreted by diabetic bone marrow-derived macrophages, which can be transferred to BMSCs to inhibit bone regeneration by targeting Smad1 Designing specific inhibitors of the miRNA as mentioned above may be a potential strategy to reverse the adverse effects of hyperglycemia on bone healing in diabetic patients. Hyperbaric oxygen therapy can improve the biometric properties of the femur in diabetic animal models and increase the content of collagen and crystalline hydroxyapatite In addition, some studies have evaluated the effectiveness of hyperbaric oxygen therapy for implant bone integration in diabetic states through diabetic animal models, and the results showed that HBO therapy can enhance implant bone integration by calculating BIC through tissue morphology However, some studies suggest that HBO only improves early bone integration in diabetic rabbits, which is not enough to improve the mechanical stability of implants Therefore, it can be determined that HBO has positive effects on bone integration in diabetic environments at the histological and biomechanical levels, but there is a lack of studies of its specific mechanisms, and further clinical research is needed to evaluate the effectiveness of HBO as an auxiliary treatment for diabetic patients. Ultrasound is an oscillating longitudinal pressure wave with a frequency over 20 kHz that cannot be detected by the human auditory system. Ultrasound has applications in many medical fields, including low-intensity pulsed ultrasound LIPUS for diagnostic imaging, medium-intensity ultrasound for physical therapy, and high-intensity focused ultrasound for surgical resection. LIPUS has been used clinically for more than 20 years. A large number of in vivo and in vitro experiments and clinical trials have verified the safety and effectiveness of LIPUS in promoting bone healing , However, there are relatively few studies on LIPUS in bone healing in patients with diabetes. Past experiments have shown that in diabetic rat fracture models, LIPUS can increase the expression of growth factors in the diabetic group and promote cartilage formation and angiogenesis An experiment aimed at the effect of LIPUS on the alveolar structure in the process of orthodontic force in diabetic patients found that the application of LIPUS treatment, 10 minutes a day for one week, can promote normal and diabetic mandibular slice organ culture MSOCs bone remodeling and restoration of cementum and dentin Although we believe that ultrasound has clinical potential in promoting bone healing in patients with diabetes and can even be used in the dental field, more experiments are still needed to prove and explore the underlying mechanism. Photobiomodulation PBM is a nonthermal light treatment that involves endogenous chromophores. Previous experiments have shown that PBM can promote bone healing in diabetic rat models by improving the viability of osteoblasts and mesenchymal cells , Experiments on diabetic rats proved that PBM treatment can improve the viability of osteoblasts, significantly increase the mRNA expression of RUNX2 and osteocalcin, and increase the activity of alkaline phosphatase and the production of the mineralized matrix, thereby regulating the bone healing process , In addition, PBM has also been shown to improve the survival, proliferation and apoptosis of BMSCs in diabetic rats Low-level laser therapy LLLT refers to radiation with a wavelength range of nm and a power of 1 mW mW. It has the characteristics of relatively low energy density and has been used clinically to treat various diseases The effect of LLLT in promoting bone healing has been verified by a large number of experiments, mainly by promoting the proliferation of osteoblasts, increasing the growth factor secreted by osteoblasts , the transportation of calcium and increasing angiogenesis to promote bone healing However, there are relatively few studies on diabetic bone healing. A previous study on the effect of LLLT and dual-type allograft materials on the healing of diabetic bone found that LLLT can effectively stimulate osteoblast production but cannot promote bone formation However, other studies have shown that LLLT can stimulate bone metabolism, reduce bone resorption area, increase RUNX-2 expression, increase serum alkaline phosphatase levels, increase cortical area, fracture strength, BMD and bone mineral content BMC , and promote bone healing , Different experiments have shown almost the opposite results, which suggests that whether LLLT can promote the healing of diabetic bone, as well as the specific mechanism of promoting diabetic bone healing, still need many experiments to be studied. In the past few decades, low-intensity pulsed electromagnetic fields LIPEMFs have played a positive role in the skeletal system. The application of PEMF treatment for patients with osteoporosis can significantly increase bone density and prevent bone loss , The positive effect of LIPEMF in promoting bone healing has been confirmed in a large number of experiments. Many preclinical experiments have proven that LIPEMF can effectively promote bone healing in diabetic animal models. However, there is still a lack of clinical trials for bone healing in diabetic patients. Although we believe that LIPEMF has clinical potential in promoting diabetic bone healing and may become a potential method to inhibit diabetic osteoporosis, its effectiveness lacks clinical experimental support. To date, with the continuous progress of preclinical studies, the mechanism of HBO therapy, LIPUS, PBM, LLLT and LIPEMF in promoting diabetic bone healing has been gradually clarified. We believe that the physical therapies mentioned above have clinical potential in promoting diabetic bone healing. However, there have been no clinical studies to confirm these findings. With the gradual increase in the number of patients with diabetes and the occurrence of a large number of related bone healing complications, we believe that it is necessary to further study the potential role and safety of physical replacement therapy in bone healing in patients with diabetes, and these therapies may become an important part of the treatment of bone healing complications of diabetes. With the improvement of living standards and the rising prevalence of diabetes, it is urgent to explore how to improve bone healing repair in diabetes. This paper reviews the effects and possible mechanisms of diabetes on bone healing and summarizes several current methods to improve bone healing under diabetic conditions, although some studies are still in their early stages, including the use of drugs, hormones, signaling pathway regulators, growth factors, exosomes, etc. In addition, some physical therapies, such as hyperbaric oxygen, ultrasound, laser, and pulsed electromagnetic fields, also have a certain clinical potential in promoting bone healing under diabetic conditions Figure 2. Some clinical trials have proven that drugs related to glycemic control are beneficial to bone health in patients with diabetes. For example, metformin can increase the level of bone formation marker in T2DM patients , liraglutide has an anti-resorptive effect on bone turnover in patients with T2DM , GLP-1 receptor agonists can increase BMD at multiple sites of the body in T2DM patients , denosumab can significantly increase BMD and decrease vertebral fracture risk in postmenopausal women with osteoporosis and diabetes 62 , etc. LLLT can improve implant stability in patients with diabetes in 6 months trial However, there is no clinical research evidence specifically designed to improve fracture healing in patients with diabetes And at present, there is no direct proof in existing clinical trials that the abovementioned methods have beneficial effects in improving bone healing under diabetic conditions. Therefore, clinical research on the methods mentioned above still lacks research, and their effectiveness and potential for clinical application still need to be further explored. Whether they can be adopted by clinical applications also needs further discussion. YC and YZ conceived and wrote the manuscript. JL and SZ reviewed and edited the manuscript. All authors contributed to the article and approved the submitted version. This work was supported by grants from the Crosswise Tasks of Sichuan University Document No. The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher. American Diabetes Association. Diagnosis and Classification of Diabetes Mellitus. Diabetes Care 37 Suppl 1 :S81— doi: PubMed Abstract CrossRef Full Text Google Scholar. Saeedi P, Petersohn I, Salpea P, Malanda B, Karuranga S, Unwin N, et al. Global and Regional Diabetes Prevalence Estimates for and Projections for and Results From the International Diabetes Federation Diabetes Atlas, 9 Th Edition. Diabetes Res Clin Pract Sellmeyer DE, Civitelli R, Hofbauer LC, Khosla S, Lecka-Czernik B, Schwartz AV. Skeletal Metabolism, Fracture Risk, and Fracture Outcomes in Type 1 and Type 2 Diabetes. Diabetes 65 7 — Murray CE, Coleman CM. Impact of Diabetes Mellitus on Bone Health. Int J Mol Sci 20 19 CrossRef Full Text Google Scholar. Napoli N, Chandran M, Pierroz DD, Abrahamsen B, Schwartz AV, Ferrari SL. Mechanisms of Diabetes Mellitus-Induced Bone Fragility. Nat Rev Endocrinol 13 4 — Khosla S, Samakkarnthai P, Monroe DG, Farr JN. Update on the Pathogenesis and Treatment of Skeletal Fragility in Type 2 Diabetes Mellitus. Nat Rev Endocrinol 17 11 — Santana RB, Xu L, Chase HB, Amar S, Graves DT. Trackman PC. A Role for Advanced Glycation End Products in Diminished Bone Healing in Type 1 Diabetes. Diabetes 52 6 — Rubin MR, Paschalis EP, Poundarik A, Sroga GE, McMahon DJ, Gamsjaeger S, et al. Advanced Glycation Endproducts and Bone Material Properties in Type 1 Diabetic Mice. PloS One 11 5 :e Furst JR, Bandeira LC, Fan WW, Agarwal S, Nishiyama KK, McMahon DJ, et al. Advanced Glycation Endproducts and Bone Material Strength in Type 2 Diabetes. J Clin Endocrinol Metab 6 — Asadipooya K, Uy EM. Advanced Glycation End Products Ages , Receptor for Ages, Diabetes, and Bone: Review of the Literature. J Endocr Soc 3 10 — Romero-Díaz C, Duarte-Montero D, Gutiérrez-Romero SA, Mendivil CO. Diabetes and Bone Fragility. Diabetes Ther 12 1 — Napoli N, Strollo R, Paladini A, Briganti SI, Pozzilli P, Epstein S. The Alliance of Mesenchymal Stem Cells, Bone, and Diabetes. Int J Endocrinol Lecka-Czernik B. Diabetes, Bone and Glucose-Lowering Agents: Basic Biology. Diabetologia 60 7 —9. Leanza G, Maddaloni E, Pitocco D, Conte C, Palermo A, Maurizi AR, et al. Risk Factors for Fragility Fractures in Type 1 Diabetes. |
| Information | We Can Help! Osteoarthritis and type 2 diabetes mellitus: what are the links? Read also about Target blood glucose levels. Learn about scientifically proven methods for treating inflammation, pain, and stiffness on your…. Crossref PubMed Google Scholar Careful diabetes care can reduce your risk of serious — even life-threatening — complications. |
Jetzt kann ich an der Diskussion nicht teilnehmen - es gibt keine freie Zeit. Aber bald werde ich unbedingt schreiben dass ich denke.