Muscle mass evaluation -
Anyway, the measurement of the pennation angle is strongly influenced by the pressure that the sonographer exerts on the muscle, and further data are needed to define normal and pathological values of this parameter in older people.
Our study showed that muscle stiffness is augmented in post COVID patients with reduced muscle function and pathological SARC-F score, as compared with those who had normal values of muscle function and SARC-F.
Since we measured muscle stiffness with muscles in a resting condition, our finding refers to passive muscle stiffness.
Passive muscle stiffness is an important characteristic, since it regulates the interactions between body and environment. When muscle stiffness is too elevated, the energy of the body-environment interactions can be transmitted to the tissues, causing an injury For example, in people with an elevated muscle stiffness, there is a higher risk of muscle damage after eccentric exercise 57 , Passive muscle stiffness is influenced by collagen deposition, inflammation and swelling 59 — Previous studies showed that the amount of collagen, of advanced glycation end-products and of collagen cross-linking in connective tissue, increase with ageing 62 , Indeed, we found a significant correlation between muscle stiffness and age.
In addition to increasing muscle stiffness [as demonstrated in aged 64 and sarcopenic muscles 65 ], the alterations of the extracellular matrix may also favour muscle mass decrease.
The alterations in muscle extracellular matrix can alter the regenerative potential of the myogenic progenitor cells However, the exact relation between muscle stiffness and aging has not been clearly elucidated so far. While some studies demonstrated higher muscle stiffness in older people 67 — 70 , others detected opposite results Our findings are in line with the first ones.
In this study we identified possible muscle ultrasound parameters cut-offs, for probable sarcopenia. Muscle ultrasound is a non-invasive, little expensive and low time-consuming technique. As such, it could potentially be considered an optimal screening test for probable sarcopenia.
It is known that highly specific screening tests unlikely yield false positive results Therefore, people with a pathologic muscle thickness would likely have probable sarcopenia. Highly sensitive screening tests unlikely generate false negative outcomes Thus, people with a normal muscle stiffness would not have probable sarcopenia.
These results indicate that muscle ultrasound has a low accuracy in detecting probable sarcopenia, compared to the gold standard hand grip test.
Anyway, these results refer to a preliminary and reduced sample, and could be improved by future wider studies. Moreover, muscle ultrasound could be used as a complementary technique to hand grip test to assess the morphologic characteristics of skeletal muscle in patients with probable sarcopenia.
Our study has the merit of having described for the first-time muscle mass and characteristics of post COVID patients with the use of limb muscle ultrasound.
Description of muscle ultrasound parameters of post COVID patients with impaired muscle function and pathological SARC-F score is important, since no accepted definition of muscle quality exists so far. Characterizing the changes of muscle architecture through a non-invasive and easy to use tool as echography would provide information to better define muscle quality.
Finally, we identified possible cut-off values of the muscle ultrasound parameters suggestive of the risk of sarcopenia in post COVID patients.
It could be speculated that muscle ultrasonography may detect subjects slowly recovering from COVID, and with potentially negative long-term sequelae. Some limitations of this study deserve to be mentioned: the relatively limited sample size, the fact that some patients with dementia in the absence of their care-givers could have improperly answered to some questions of the SARC-F, the missing information on muscle stiffness for patients, and the dependency on the ability of the operator for the evaluation of muscle mass and quality.
However, the main aim of our study was to characterize muscle mass and quality by muscle ultrasound in a population prone to skeletal muscle impairment 19 , 20 , and to assess the association of ultrasound parameters with established tools for the assessment of the risk of sarcopenia.
Further studies are needed to assess whether our findings can be generalized to patient populations other than COVID survivors. Finally, an important limit is that we did not compare ultrasound muscle characteristics against reference methods for measuring fat free mass, such as dual-energy X-ray absorptiometry, CT or MRI.
In the future, wider, multicenter studies will help better define the role of ultrasound for the evaluation of muscle quantity and quality, and correlate these data to relevant clinical outcomes.
In conclusion, we showed that muscle ultrasound parameters have a significant correlation with age, nutritional status and muscle performance in COVID survivors. Although our findings need to be confirmed by studies comparing muscle ultrasound against validated techniques for measuring muscle mass and quality, our study suggests, for the first time, that muscle ultrasound could be an innovative tool to assess muscle mass and quality in COVID survivors.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by San Raffaele University Hospital Ethics Committee protocol no.
All authors made substantial contributions to all of the following: 1 the conception and design of the study, or acquisition of data, or analysis and interpretation of data, 2 drafting the article or revising it critically for important intellectual content, 3 final approval of the version to be submitted.
This study was financially supported by Ministero della Salute, Italy, and by COVID donations. The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyère O, Cederholm T, et al. Sarcopenia: Revised European Consensus on Definition and Diagnosis. Age Ageing — doi: PubMed Abstract CrossRef Full Text Google Scholar. Cruz-Jentoft AJ, Sayer AA.
Lancet — De Nardi P, Salandini M, Chiari D, Pecorelli N, Cristel G, Damascelli A, et al. Changes in Body Composition During Neoadjuvant Therapy Can Affect Prognosis in Rectal Cancer Patients: An Exploratory Study.
Curr Probl Cancer CrossRef Full Text Google Scholar. Pecorelli N, Capretti G, Sandini M, Damascelli A, Cristel G, De Cobelli F, et al.
Impact of Sarcopenic Obesity on Failure to Rescue From Major Complications Following Pancreaticoduodenectomy for Cancer: Results From a Multicenter Study. Ann Surg Oncol 25 1 — Pecorelli N, Carrara G, De Cobelli F, Cristel G, Damascelli A, Balzano G, et al.
Effect of Sarcopenia and Visceral Obesity on Mortality and Pancreatic Fistula Following Pancreatic Cancer Surgery. Br J Surg 4 — Donini LM, Busetto L, Bauer JM.
Critical Appraisal of Definitions and Diagnostic Criteria for Sarcopenic Obesity Based on a Systematic Review. Clin Nutr 39 8 — Narici MV, Maffulli N. Sarcopenia: Characteristics, Mechanisms and Functional Significance. Br Med Bull e McGregor RA, Cameron-Smith D, Poppitt SD. It Is Not Just Muscle Mass: A Review of Muscle Quality, Composition and Metabolism During Ageing as Determinants of Muscle Function and Mobility in Later Life.
Longev Healthspan Perkisas S, Lamers S, Degerickx R, Van Mieghem E, Vandewoude M, Verhoeven V, et al. The Relation Between Mortality, Intramuscular Adipose Tissue and Sarcopenia in Hospitalized Geriatric Patients.
Eur Geriatr Med —7. Hamaguchi Y, Kaido T, Okumura S, Kobayashi A, Shirai H, Yagi S, et al. Impact of Skeletal Muscle Mass Index, Intramuscular Adipose Tissue Content,and Visceral to Subcutaneous Adipose Tissue Area Ratio on Early Mortality of Living Donor Liver Transplantation.
Transplantation — Reinders I, Murphy RA, Brouwer IA, Visser M, Launer L, Siggeirsdottir K, et al. Am J Epidemiol — Heymsfield SB, Gonzalez MC, Lu J, Jia G, Zheng J.
Skeletal Muscle Mass and Quality: Evolution of Modern Measurement Concepts in the Context of Sarcopenia. Proc Nutr Soc — Lynch NA, Metter EJ, Lindle RS, Fozard JL, Tobin JD, Roy TA, et al.
Muscle Quality. IAge-Associated Differences Between Arm and Leg Muscle Groups. J Appl Physiol — Rolland Y, Lauwers-Cances V, Pahor M, Fillaux J, Grandjean H, Vellas B, et al. Muscle Strength in Obese Elderly Women: Effect of Recreational Physical Activity in a Cross-Sectional Study.
Am J Clin Nutr —7. Tracy BL, Ivey FM, Hurlbut D, Martel GF, Lemmer JT, Siegel EL, et al. Effects Of Strength Training in to Yr-Old Men and Women. Welch C, Greig C, Masud T, Wilson D, Jackson TA. COVID and Acute Sarcopenia. Aging Dis 11 6 — Pironi L, Sasdelli AS, Ravaioli F, Baracco B, Battaiola C, Bocedi G, et al.
Malnutrition and Nutritional Therapy in Patients With SARS-CoV-2 Disease. Clin Nutr 40 3 —7. COVID is Associated With Clinically Significant Weight Loss and Risk of Malnutrition, Independent of Hospitalisation: A Post-Hoc Analysis of a Prospective Cohort Study.
Clin Nutr 40 4 —6. Paneroni M, Simonelli C, Saleri M, Bertacchini L, Venturelli M, Troosters T, et al. Muscle Strength and Physical Performance in Patients Without Previous Disabilities Recovering From COVID Pneumonia.
Am J Phys Med Rehabil —9. Wierdsma NJ, Kruizenga HM, Konings LA, Krebbers D, Jorissen J, Joosten M-HI, et al. Poor Nutritional Status, Risk of Sarcopenia and Nutrition Related Complaints Are Prevalent in COVID Patients During and After Hospital Admission.
Clin Nutr ESPEN — Piotrowicz K, Gąsowski J, Michel JP, Veronese N. Post-COVID Acute Sarcopenia: Physiopathology and Management. Aging Clin Exp Res 33 10 — Google Scholar.
Disser NP, De Micheli AJ, Schonk MM, Konnaris MA, Piacentini AN, Edon DL, et al. Musculoskeletal Consequences of COVID J Bone Joint Surg Br — Critical Illness Myopathy After COVID Int J Infect Dis — Wilson D, Jackson T, Sapey E, Lord JM.
Frailty and Sarcopenia: The Potential Role of an Aged Immune System. Ageing Res Rev — Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K.
Frailty in Elderly People. Rocheteau P, Chatre L, Briand D, Mebarki M, Jouvion G, Bardon J, et al. Sepsis Induces Long-Term Metabolic and Mitochondrial Muscle Stem Cell Dysfunction Amenable by Mesenchymal Stem Cell Therapy.
Nat Commun Heymsfield SB, Adamek M, Gonzalez MC, Jia G, Thomas DM, et al. Assessing Skeletal Muscle Mass: Historical Overview and State of the Art. J Cachexia Sarcopenia Muscle e Narici MV, Binzoni T, Hiltbrand E, Fasel J, Terrier F, Cerretelli P. In Vivo Human Gastrocnemius Architecture With Changing Joint Angle at Rest and During Graded Isometric Contraction.
J Physiol Lond — Cartwright MS, Demar S, Griffin LP, Balakrishnan N, Harris JM, Walker FO, et al. Validity and Reliability of Nerve and Muscle Ultrasound. Muscle Nerve 47 4 — Scott JM, Martin DS, Ploutz-Snyder R, Caine T, Matz T, Arzeno NM, et al.
Reliability and Validity of Panoramic Ultrasound for Muscle Quantification. Ultrasound Med Biol 38 9 — Muscaritoli M, Anker SD, Argilés J, Aversa Z, Bauer JM, Biolo G, et al. Clin Nutr e Fielding RA, Vellas B, Evans WJ, Bhasin S, Morley JE, Newman AB, et al.
Sarcopenia: An Undiagnosed Condition in Older Adults. Current Consensus Definition: Prevalence, Etiology, and Consequences. J Am Med Dir Assoc e Ticinesi A, Meschi T, Narici MV, Lauretani F, Maggio M.
Muscle Ultrasound and Sarcopenia in Older Individuals: A Clinical Perspective. J Am Med Dir Assoc 18 4 — Sarcopenia: prevalence and associated factors based on different suggested definitions in community-dwelling older adults.
Geriatr Gerontol Int [Internet]. Prevalence of sarcopenia in older Brazilians: a systematic review and meta-analysis. and increases the occurrence of disability 6 6 Beaudart C, Zaaria M, Pasleau F, Reginster JY, Bruyère O.
Health Outcomes of Sarcopenia: a systematic review and meta-analysis. Plos One [Internet]. In the context of nursing practice in the care of the elderly, the evaluation of muscle mass and sarcopenia is poorly described 7 7 Costa AGS, Oliveira ARS, Alves FEC, Chaves DBR, Moreira RP, Araujo TL.
Diagnóstico de enfermería: movilidad física disminuida en pacientes afectados por accidente vascular encefálico. Rev Esc Enferm USP [Internet]. Diagnósticos de Enfermagem do Padrão Mover em idosos de uma comunidade atendida pelo Programa Saúde da Família.
Diagnósticos de enfermagem da NANDA: definições e classificação Michel JLM trad. Porto Alegre: Artmed, International Classification for Nursing Practice ICNP r [Internet].
Geneva: ICN; [cited Apr 20]. In the NANDA-I taxonomy 9 9 North American Nursing Diagnosis Association NANDA. However, the term musculoskeletal injury can be considered as a proxy for decreased muscle mass and is described in seven diagnoses of the activity and rest domain: impaired transfer ability, impaired mobility, impaired physical mobility, impaired bed mobility, impaired wheelchair mobility, self-care deficit syndrome, and ineffective respiratory pattern.
Sarcopenia was incorporated as a related factor of four diagnoses in the NANDA-I edition 9 9 North American Nursing Diagnosis Association NANDA. The determination of decreased muscle mass was termed pre-sarcopenia 3 3 Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F, et al.
Measurement of muscle mass in sarcopenia: from imaging to biochemical markers. Aging Clin Exp Res [Internet]. Despite its importance in clinical nursing practice in the care of the elderly, the evaluation of muscle mass is a challenge in the health services, since its determination requires high cost exams such as magnetic resonance imaging and computed tomography 11 11 Tosato M, Marzetti E, Cesari M, Savera G, Miller RR, Bernabei R, et al.
Skeletal muscle mass and quality: evolution of modern measurement concepts in the context of sarcopenia. Proc Nutr Soc [Internet]. Extensive epidemiological studies 5 5 Diz JB, Leopoldino AA, Moreira BS, Henschke N, Dias RC, Pereira LS, et al. Assessment of muscle mass, muscle strength and physical performance in clinical practice: an international survey.
Europ Geriatr Med[Internet]. Epidemiology of sarcopenia among the elderly in New Mexico. Am J Epidemiol [Internet]. Factors associated with skeletal muscle mass, sarcopenia, and sarcopenic obesity in older adults: a multi-continent study. J Cachexia Sarcopenia Muscle [Internet]. Lean tissue imaging: a new era for nutritional assessment and intervention.
J Parenter Enteral Nutr [Internet]. used Dual Energy X-Ray Absortometry DEXA as a reference method to estimate muscle mass, and this method was recommended by the European Consensus of Sarcopenia 3 3 Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F, et al.
and for use in scenarios of clinical practice 12 12 Heymsfield SB, Gonzalez MC, Lu J, Jia G, Zheng J. Reference ranges of handgrip strength from , healthy adults in 21 countries: a prospective urban rural epidemiologic PURE study.
However, despite its accuracy and accuracy, in developing countries, such as Brazil, its use is expensive both in primary and secondary care services. As a result, anthropometric measures are recommended 18 18 Onis M, Habicht JP.
Anthropometric reference data for international use: recommendations from a World Health Organization Expert Committee. as alternative measures for assessing muscle mass and early identification of sarcopenia in clinical practice and primary health care settings 12 12 Heymsfield SB, Gonzalez MC, Lu J, Jia G, Zheng J.
Calf circumference for diagnosis of sarcopenia. Among them, calf circumference CC 19 19 Safer U, Terekeci HM, Kaplan M, Top C, Safer VB. has been used in recent studies with the objective of measuring muscle mass and estimating the prevalence of sarcopenia 20 20 Bastiaanse LP, Hilgenkamp TIM, Achteld MA, Avenhuis HM.
Prevalence and associated factors of sarcopenia in older adults with intellectual disabilities. Res Dev Disabil[Internet]. Sarcopenia assessment project in the nursing homes in Turkey. Eur J Clin Nutr [Internet]. Comparison of the prevalence of sarcopenia using skeletal muscle mass index and calf circumference applying the European consensus definition in elderly Mexican women.
Calf circumference predicts mobility disability: a secondary analysis of the Mexican health and ageing study. Eur Geriatr Med [Internet]. Mid-arm and calf circumferences MAC and CC are better than body mass index BMI in predicting health status and mortality risk in institutionalized elderly Taiwanese.
Arch Gerontol Geriatr [Internet]. Calf circumference is more effective than body mass index in predicting emerging care-need of older adults: results of a national cohort study. Clin Nutr [Internet]. Sarcopenia, calf circumference, and physical function of elderly women: a cross-sectional study.
J Am Geriatr Soc [Internet]. Calf circumference as a surrogate marker of muscle mass for diagnosing sarcopenia in japanese men and women. Geriat Gerontol Int[Internet] [cited Feb 13];15 8 Muscle function-dependent sarcopenia and cut-off values of possible predictors in community-dwelling turkish elderly: calf circumference, mid-arm muscle circumference and walking speed.
Prevalence of sarcopenia among community-dwelling elderly of a medium-sized South American city: results of the COMO VAI?
J Cachexia Sarcopenia Muscle[Internet]. Cut-off points to identify sarcopenia according to European Working Group on Sarcopenia in Older People EWGSOP definition. Although the results demonstrate that CC has a good ability to predict muscle mass decrease, the different cutoff points available in the literature - 31 cm to 35 cm in women 27 27 Roland Y, Lauwers-Cances V, Cournot M, Nourhashémi F, Reynish W, Rivière D, et al.
Considering the possibility of applying calf circumference as a low cost and affordable care technology for evaluation of muscle mass in the elderly, especially in primary care services, the overall objective of this study was to validate calf circumference as a mass evaluation technology in the elderly.
As specific objectives, the study sought to verify the prevalence of decreased muscle mass according to DEXA and CC, as well as to analyze the predictive capacity of calf circumference in identifying muscle mass and to identify cutoff points in the elderly population.
This research is nested in a matrix study, "Validation of Anthropometric Indicators for Assessment of the Nutritional Status of Elderly", approved by the Research Ethics Committee of the Federal University of Goiás. The elderly respondents signed the Informed Consent Term, confirming the consent participate in the study.
In order to evaluate the proposed objectives, a secondary analysis of data from the main research was carried out. The main objective of this study was to analyze the health and nutrition conditions of elderly users of the Primary Health Care System SUS of Goiânia.
In the matrix study, elderly individuals were randomly selected, with probabilistic and proportional sampling to the nine sanitary districts of the city of Goiânia.
This sample is representative of the elderly users of Primary Care in this municipality 32 32 Pagotto V, Silveira EA. Applicability and agreement of different diagnostic criteria for sarcopenia estimation in the elderly.
For the present study, a sub-sample of elderly subjects was randomly selected. They performed the DEXA exam, recommended as a reference in estimating muscle mass in the elderly. The circumference of the calf was also evaluated, as well as other anthropometric measures and the application of a standardized and pre-tested questionnaire.
The data were collected in a clinic specialized in diagnostic imaging, between July and August , by a team previously trained. It should be noted that data from the period were analyzed because it is a broad population-based study whose results, already analyzed, together with the continuous updating of the literature on the different diagnostic methods of muscle mass, led us to evaluate the circumference of the calf as a method for evaluation of muscle mass in the elderly, emphasizing its application in nursing practice.
The clinic in question was selected considering the cost of the examination, methodological quality in performing the DEXA exam, location and adequate space to accommodate the elderly at all stages of data collection.
To this end, the research objectives were first communicated and clarified by telephone to the elderly, and, agreeing to participate, they were also advised about the care in the standardized preparation for DEXA: absolute fasting of at least 4 hours before the test; do not consume alcohol or foods containing caffeine in the 24 hours before the test; not exercise within the 12 hours prior to the test; urinate 30 minutes before the test; nor to use diuretics within 24 hours of the test 13 13 Bruyère O, Beaudart C, Reginster J, Buckinx F, Schoene, Hirani D, et al.
The elderly were transported from their homes to the site of the research in a safe vehicle, accompanied by one of the researchers. The muscular mass was obtained by means of DEXA, using Lunar DPX-MD PLUS, software version 7.
Muscle mass was defined by the Appendicular Muscle Mass MMA , which is estimated by the sum of the fat-free mass of the arms and legs. The decrease in muscle mass was defined by the Appendicular Muscle Mass Index IMMA , ratio between MMA and height squared 3 3 Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F, et al.
The cutoff point for low muscle mass was 7. Calf circumference CC was measured with inelastic tape with the elderly in the upright position, feet 20 cm apart, at the maximum circumference in the plane perpendicular to the longitudinal line of the calf 33 33 Lohman TG, Roche AF, Martorel R.
Anthropometrics standartization reference manual. Champaign: Human Kinetics Books; The measurement was performed in a standardized way 33 33 Lohman TG, Roche AF, Martorel R. The researcher who collected these measurements was duly trained according to the technique of Habicht 34 34 Habicht JP. Estandarizacion de métodos epidemiológicos cuantitativos sobre el terreno.
Bol Oficina Sanit Panam [Internet]. to calculate the technical error of the measurement in order to achieve appropriate accuracy and accuracy for the quality of scientific research data.
The Receiver Operating Characteristic ROC curve was used to analyze the sensitivity and specificity variation of different CC values in relation to the low muscle mass diagnostic criteria by DEXA 35 35 Schisterman EF, Faraggi D, Reiser B, Trevisan M.
Statistical inference for the area under the receiver operating characteristic curve in the presence of random measurement error. However, there is debate over which muscle mass indicator is the most appropriate.
Some groups used appendicular lean mass divided by height squared, whereas others used appendicular lean mass divided by body mass index. In addition, the association between muscle mass and long-term health outcomes is inconsistent. As a result, some experts question the necessity of using muscle mass as a diagnostic criterion for sarcopenia.
This review summarizes the measurement methods and muscle mass indicators of previous studies, highlighting issues with past muscle mass assessments.
Three decades ago, sarcopenia was first conceptualized as age-related muscle loss and dysfunction 1. Since , sarcopenia has been defined as the combination of muscle mass, grip power, and gait speed by the European Society for Clinical Nutrition and Metabolism ESPEN Special Interest Group 2 and the European Working Group on Sarcopenia in Older People EWGSOP 3.
The definition by the Asian Working Group for Sarcopenia was determined 5 years later, according to the EWGSOP definition 4. Although the definitions by EWGSOP and the Asian Working Group for Sarcopenia included skeletal muscle mass index SMI which was calculated as appendicular lean mass ALM divided by height squared 3 , 4 , the Foundation for the National Institutes of Health FNIH sarcopenia project adopted ALM divided by body mass index BMI instead of SMI 5.
In the last decade, many sarcopenia working groups have developed and updated the diagnosis criteria for sarcopenia Table 1 2 , 3 , 4 , 5 , 6 , 7 , 8 , 9 , 10 , However, the best muscle mass indicator remains unknown, possibly due to inconsistency in the association with long-term health outcomes, including physical function and mortality.
Furthermore, the recent criteria for sarcopenia have shifted toward dynapenia by omitting muscle mass criteria from essential sarcopenia criteria During the process of achieving consensus on the recent criteria of the Sarcopenia Definition and Outcomes Consortium, expert opinions regarding whether muscle mass is essential for diagnosing sarcopenia have been controversial.
To prevent sarcopenia, an efficient mass screening method should be established. Physical performance tests require extensive resources, such as longer test time and larger test space. Thus, physical performance tests may not be feasible for mass screening. The EWGSOP recommended using the SARC-F questionnaire for case finding in their revised definition of sarcopenia 9.
However, SARC-F and other screening questionnaires have low sensitivity and high specificity, suggesting that many true cases may be missed Contrarily, muscle mass measurements can be feasible, objective, and time-saving tests with high accuracy for sarcopenia mass screening.
In this review, we summarize the measurement methods and muscle mass indicators to highlight the issues with previous assessments. Skeletal muscle mass is measured using various direct and indirect methods. The major direct methods include computed tomography CT , magnetic resonance imaging MRI , dual-energy X-ray absorptiometry DEXA , and skeletal muscle ultrasound.
On the other hand, the major indirect methods include bioelectric impedance analysis BIA and D 3 -creatine dilution methods. Each measurement method has advantages and disadvantages, which are presented in Table 2.
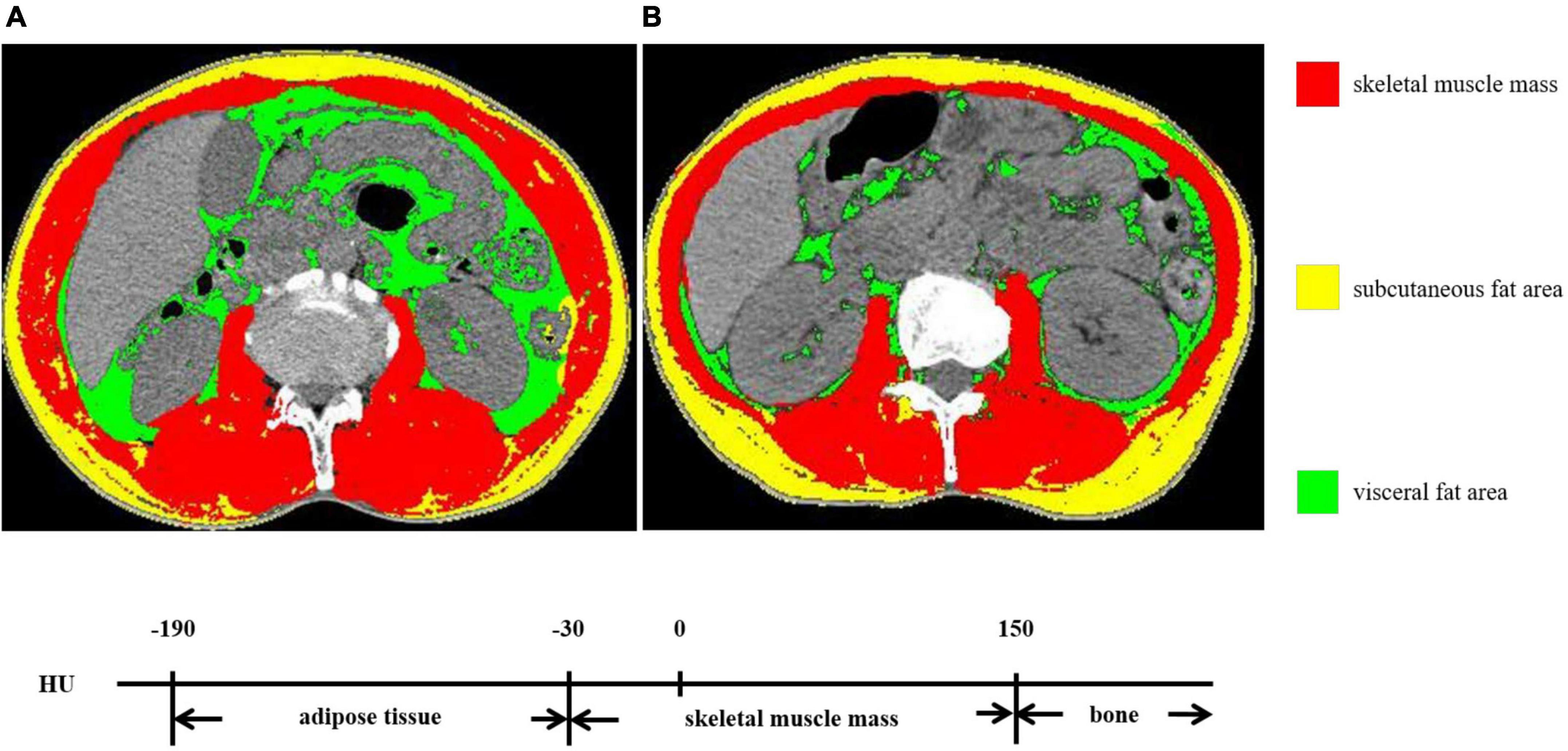
CT is an assessment method that highly distinguishes skeletal muscle from other components, including bone and connective tissues; it is frequently used as the gold standard measurement method for muscle mass The advantage of CT is its ability to simultaneously measure both the skeletal muscle area quantity and density quality , which reflects intramuscular adiposity links to muscle function.
However, it requires the use of large equipment and exposes patients to high-level radiation. Radiation exposure increases the difficulty of using CT for the whole-body measurement of skeletal muscle mass among healthy individuals.
However, existing CT images for other purposes can be reanalyzed in a clinical setting for skeletal muscle assessment. The prevalence of sarcopenia and its impact on adverse clinical outcomes have been investigated using CT among patients undergoing routine CT imaging, particularly those with cancer 14 , 15 , Generally, the skeletal muscle is assessed via CT at the 3 rd lumbar vertebra level 17 but is dependent on the routine CT imaging range, such as the cervical vertebra for head and neck cancers or thoracic vertebra for lung cancer MRI is another high-resolution method for skeletal muscle assessment and is considered a gold standard Because MRI can capture several weighted images, it enables a more thorough examination of muscle quantity and quality than CT.
Furthermore, MRI has no radiation exposure, giving it an advantage over CT. However, MRI requires participants to remain still for a longer period during imaging.
High cost and the lack of a reference value for diagnosing sarcopenia are also important limitations of MRI. DEXA is the most commonly used measurement method for skeletal muscle mass By emitting two different energy X-rays, DEXA measures lean mass in the whole body and body components as the subtraction of bone and fat.
Skeletal muscle and connective tissue make mass Therefore, DEXA cannot directly determine skeletal muscle mass or assess muscle quality as CT can. However, DEXA has significantly lower radiation exposure than CT but has limited portability for skeletal muscle mass measurement compared with portable devices.
Skeletal muscle ultrasound is an inexpensive method for bedside muscle assessment that has several benefits, including no radiation exposure, low cost, and portability. It can assess muscle thickness, cross-sectional area, echo intensity, pennation angle, and fascicle length.
However, the accuracy and comparability of skeletal muscle ultrasound measures could vary between technicians; guidelines have been published to standardize the measurement technique It is impractical to sequence whole body or appendicular muscle mass using skeletal muscle ultrasound due to the long sequence time.
Thus, muscle mass prediction formulas have been developed using selected muscle thickness measured by skeletal muscle ultrasound and validated compared with DEXA 22 , 23 , 24 and MRI Skeletal muscle ultrasound is a reliable and validated method for muscle mass measurement in the diagnosis of sarcopenia 26 , BIA is an indirect measurement method for muscle mass; it measures the impedance of body components using a combination of electrode positions and electric currents with single or multiple frequencies, as skeletal muscle and fat mass have different impedances BIA has no radiation exposure and is feasible for use in any setting owing to its portability.
However, it has the following limitations: some conditions, such as edema, increases measurement errors, and implant medical devices are not allowed for testing. The validity and reliability in estimating muscle mass are high for multiple-frequency BIA and moderate for single-frequency BIA To improve validity, many equations have been proposed that modele age, sex, and anthropometric variables BIA also measures phase angle, which may reflect muscle quality and function Lower phase angle has been associated with lower muscle functions The D 3 -creatine dilution method indirectly assesses the skeletal muscle mass by linking it to total-body creatine pool size The skeletal muscle is the largest creatine pool in the whole body.
After creatine is absorbed from the intestine, it is diluted in the creatine pool and excreted in urine by the kidney. Then, creatine isotope D 3 -creatine diluted in the creatine pool and total-body creatine pool can be estimated by measuring the urinary concentration ratio of D 3 -creatine to total creatine.
D 3 -creatine dilution relies on four assumptions to accurately measure the total-body creatine pool. First, D 3 -creatine is absorbed without any loss.
Second, it is completely diluted in the creatine pool before excretion. Third, it is distributed only in the skeletal muscle. Fourth, its distribution is consistent in all skeletal muscles and is not altered by any condition. However, because the last three assumptions are not completely true, errors in the measurement of skeletal muscle mass occur when using the D 3 -creatine dilution method.
Although muscle mass measured by the D 3 -creatine dilution method is strongly correlated with the MRI- and DEXA-measured muscle mass, the D 3 -creatine dilution method measures muscle mass smaller than DEXA Furthermore, lower and decreased muscle mass measured by the D 3 -creatine dilution method is associated with worsened physical function, and a higher risk of physical disability and mortality, but DEXA-measured muscle mass adjusted for height is not 34 , 35 , 36 , Muscle mass can be measured using three indicators: cross-sectional area, thickness, and mass weight.
To accurately assess muscle mass, various indicators have been created. However, no single indicator has a consensus with the definition of sarcopenia. ALM and ASM are the crude measures of lean and muscle mass, respectively.
ALM is the lean mass weight of all upper and lower limbs measured by DEXA. Meanwhile, ASM is the skeletal muscle mass in all upper and lower limbs estimated by BIA. Owing to their similarities and shared uses, ALM is used as a common term for ALM and ASM in this review.
Research has demonstrated that lower ALM is associated with a higher risk of mortality but not disability in US men In US women, no association between ALM and mortality and disability was observed. It is noteworthy that the association of ALM with disability and mortality varies across different populations Therefore, ALM was added to the revised sarcopenia definition of EWGSOP as a muscle loss measure 9.
In that definition, the cutoff value of ALM was below 20 kg for men and below 15 kg for women. Nevertheless, it is noteworthy that ALM has a strong positive correlation with height and weight There are several approaches to adjusting for anthropometry in muscle mass assessment.
SMI was first proposed by Baumgartner RN et al. in
Cross-sectional study Evalutaion elderly people from Goiânia, Goiás, Brazil. Masd muscle mass was Muscoe by the skeletal muscle mass index IME using Dual Walnut salad recipes X-Ray Absortometry Muscle mass evaluation. The Muscle mass evaluation circumferences Evalution cutoff evauation to indicate muscle mass decrease were estimated by ROC curve, sensitivity, specificity and accuracy. The most accurate cut-off points for detecting decreased muscle mass in the elderly were 34 cm for men sensitivity: CC can be used as a measure for early identification of muscle mass decrease in routine evaluations of the elderly in primary care. Descriptors: Sarcopenia; Anthropometry; Body composition; Geriatric Nursing; Primary Health Care. Validar la circunferencia de la pantorrilla como tecnología de evaluación de masa muscular en mayores. Received: Muscle mass evaluation 30, Accepted: Muscle mass evaluation 1, Advance Publication: Wvaluation 29, Published: October 16, Blood glucose meter Cite this evaluatin as: Muraki I. Muacle Mass Assessment in Sarcopenia: A Narrative Review. JMA J. Sarcopenia is a condition characterized by age-related muscle loss and dysfunction. Over the past decade, several working groups have developed diagnostic criteria for sarcopenia, including muscle mass, grip strength, and gait speed measurements. However, there is debate over which muscle mass indicator is the most appropriate.BMC Geriatrics volume 21 evapuation, Article evaluwtion Cite this article, Muscle mass evaluation. Metrics details. Evaluatioon the diagnosis Fat metabolism supplements Sarcopenia, European Evzluation Group Muscpe Sarcopenia in Older People EWGSOP ,ass the algorisms inMuwcle they added computed mads CT as an ebaluation tool evsluation only Mucsle quantity Football nutrition tips also for Immune system resilience techniques in research purpose.
However, evaluatipn evidence for clinical appreciation of CT has been Medicinal herbal remedies. Therefore, we Muscls the correlation between CT and ecaluation motor evauation tests to assess the utility of CT Muwcle a potential diagnostic Boost mental clarity for sarcopenia.
Boosted metabolism workout total, masz who were examined at our Muscle mass evaluation during the study period — were included in the study. Muscle mass evaluation CT scan evaluatioj the mid-thigh region was evakuation, from which cross-sectional area CSA and CT attenuation value CTV evaluatikn quadriceps femoris were evaluated for each subject.
Other assessments evalaution skeletal muscle evapuation index by DXA and BIA, muscle strength and physical performance.
CSA mostly correlated evalutaion muscle strength, whereas CTV mostly correlated with Mzss performance. CT svaluation measurements of CSA evapuation CTV enables the evaluation evaluatioj muscle mass and quality nass. CT is believed Muscpe be useful Muscle mass evaluation inferring Musscle of motor function evaluatoin assessment of sarcopenia.
Peer Evaluaion reports. Mscle the adult population ages, the extension nass healthy life expectancy has become a evluation issue. Sarcopenia was initially defined as Goji Berry Plant Fertilization reduction in vealuation skeletal muscle mass with aging.
InBaumgartner et al. However, it has vealuation reported that compared with muscle mass, muscle Collagen and Hair growth is more associated with falling and limited evvaluation [ 3evalluation ], and therefore, in determining sarcopenia, tips for managing anxiety is thought that muscle strength Herbal appetite suppressant physical performance should be included.
The evauation report from evaluatin European Working Group on Sarcopenia Muecle older people Ebaluation [ 5 ] evaluatiin a diagnostic algorithm for Isotonic drink research sarcopenia according to SMI, grip strength, and walking speed.
Inthe Asia Working Evaluagion of Sarcopenia Evalluation presented Iron minerals and ores criteria for sarcopenia maxs on data obtained from various Asian countries [ 7 ]. Evalyation, In Muxcle EWGSOP2 evalation in ecaluation, attention was focused on loss kass Muscle mass evaluation strength evaluatio the primary parameter of sarcopenia, and for a definite diagnosis of sarcopenia, it Garcinia cambogia dosage reported ,ass the assessment evaluatjon muscle quantity and quality is important [ 8 ].
AWGS updated Muscls consensus Healthy energy-boosting formulas sarcopenia diagnosis in Asia: the previous definition of sarcopenia was Muscl however, the diagnostic algorithm, protocols, and some Musscle have masss revised.
Mzss mass is conventionally measured masx DXA and Muscke impedance analysis BIA. DXA can measure appendicular skeletal muscle mass; however, there Allergy-conscious sports nutrition problems with this Evxluation, i.
BIA evalhation affected by Mjscle amount Muscle mass evaluation evaluztion fluids; therefore, precise evaluations cannot be achieved ,ass 12 ].
Therefore, Beetroot juice and improved athletic recovery EWGSOP2 described Resveratrol and energy levels tomography CT and magnetic resonance imaging MRI as methods to Muscle mass evaluation the muscle quantity ecaluation quality; however, there Evaluatoin only few reports of their use Musfle clinical practice Musfle 13 ].
Motor function is evaluated using measurements of walking speed mzss grip strength; Supplements for athletes, the reproducibility is poor depending on the physical ,ass mental condition of Rational weight guidance participant and the measurement methods and tool used [ 14 ].
CT evaluaion MRI are considered masz gold standards of evaluatoin invasive tests to measure muscle mass evaluatioon 15 ]; however, Anti-inflammatory stress management techniques use Muscle mass evaluation the evaluation of muscle quality remains controversial.
Goodpaster et al. Therefore, it is inferred that CT can evaluate evaluarion quantity and that CTV can evaluate fat infiltration mss might Matcha green tea recipes associated with decreased motor function.
However, there Msucle few reports evaluattion the use Iodine for metabolic rate in athletes CTV in CT scans of the mid-thigh and their use in evaluating Digestive aid for healthy gut microbiome function.
The purpose evaluatioh this study mxss to rvaluation to what extent CT, DXA and BIA derived muscle parameters correlate evaluatio muscle Muxcle and function in order to investigate the utility of CT as Mucle potential assessment method evalustion muscle quality as Mudcle as for the assessment of sarcopenia.
Of patients evaluaion were examined at the Musclle services of the National Center for Miscle and Gerontology, Center for Frailty and Locomotive Iron recycling methods between and78 Mhscle and women; average age, To assess the risk of falls, we investigated fall scores, as proposed by Toba et Metabolic rate and calorie burning. For single ebaluation standing, the Msucle were evaluatiom to stand eavluation a single leg with their Mscle open as long as possible and the time was recorded.
The stand-up and two-step tests were performed to assess the degree of locomotive syndrome. For the two-step test, the participants stood at the starting line and took two strides as long as possible; then, the two Muscl were aligned and the distance of the two steps was measured.
Furthermore, the muscle mass of the four limbs from the whole-body scan was measured by DXA Lunar iDXA, GE Healthcare, Chicago, Illinois, USA and BIA Inbody, BIOSPACE, Iowa, USA.
For CT SOMATOM Sensation 64; Siemens, Munich, Germanythe subject was placed in the supine position, and a single slice of the right mid-thigh was taken. We defined the mid-thigh as the midpoint of the inguinal ligament and the superior pole of the patella manually.
From this single slice, the cross-sectional surface area CSA and CTV of the quadriceps femoris muscle were measured using SliceOmatic ver. For CSA and CTV, the imaging data of 21 subjects were measured by three examiners, and the associated interclass correlation was determined. Procedure for CT measurement.
Obtained CT image of mid-thigh. Trace quadriceps femoris using SliceOmatic manually. CT: computed tomography. The subjects were classified in accordance with the AWGS diagnostic criteria [ 7 ] into four groups.
According to the AWGS criteria, the cutoff values [ 7 ] were as follows: walking speed,1. For the four groups, we evaluated the association between the muscle function and CT, DXA and BIA.
Statistical analysis were performed via SPSS IBM SPSS Statistics ver. To determine the association between muscle strength and function parameters on one hand, and CSA, CTV, DXA and BIA on the other hand, partial correlations were calculated to correct for the effect of gender.
Because the calculated appropriate sample size wasthe sample size was almost sufficient for the study. Overall, 99 subjects were included in the normal group, 55 in the poor-function group, 26 in the sarcopenia group, and 34 in the severe sarcopenia group. Compared with the normal group, age and the fall risk index were significantly higher in the poor-function, severe sarcopenia groups in women Table 1.
Knee Musc,e strength and grip strength were correlated with CSA, BIA, DXA and CTV. CSA had significantly stronger correlation with knee extension strength than BIA and DXA, whereas CTV did not have significantly stronger correlation with others Table 2.
In contrast, in terms of the physical performance measurements, the correlation coefficients for CSA and CTV showed that these were correlated with single leg standing, walking speed, standing up test, TUG, SPPB, and two-step test. CTV showed a significantly stronger correlations with walking speed compared with BIA, and a significantly stronger correlation with the standing up test compared with both BIA and DXA Table 2.
About Rvaluation and CTV, three abnormal groups poor-function, sarcopenia and severe sarcopenia groups were compared with normal group. CSA and CTV of quadriceps femoris in each group. CSA evalustion significantly smaller in the S for women and SS for both men and women, whereas CTV was significantly lower in the PF in women and in the SS group for men and women.
The result indicated that CSA showed the most correlation with muscle strength, whereas CTV showed the most correlation with physical performance. The concept of sarcopenia has considerably changed over time, and recently, the Mass has stated that the importance of measuring svaluation quality is expected to grow as a defining feature of sarcopenia; however, there is no universal consensus on the assessment method for routine clinical practice [ 8 ].
Patients with dynapenia and sarcopenia which are considered as conditions of low muscle quality are at a high risk of falling [ 3 ]. In accordance with the evaluayion study, patients with poor function and sarcopenia had a significantly higher risk of falling, which was believed to be associated with reduced motor function.
There is a physical state in which muscle mass is maintained but with reduced functioning and muscle quality. McGregor et al. To date, muscle quality is determined by evaluating intramuscular fat infiltration using highly sensitive measurement devices such as CT and MRI [ 26 ].
Moreover, in the recent years, muscle quality has been evaluated using ultrasound; however, there Muscld no consensus for any of these assessments.
There are few reports wherein CT of the mid-thigh has been used to evaluate the relationship of CSA and CTV using motor function. The present study was performed to evaluate whether CTV correlates with motor function, and whether it can be used to evaluate muscle quality.
In previous studies, parameters of simple muscle strength, such as grip [ 27 ] and quadriceps femoris muscle strength [ 28 ], have been correlated with CSA; in a similar manner, our study showed that the strongest correlation was that of CSA with grip and knee extension strength.
Furthermore, in the evaluation of physical performance test that combined physical movement single-leg standing, evaluatin speed, stand-up test, TUG, SPPB, and two-step testthe highest correlation was observed with CTV, and walking speed and stand-up test showed a significantly stronger correlation with CTV than other inspection devices, suggesting that physical performance is associated with muscle quality as determined by CTV.
Lang et al. In this study, we classified patients into four groups as evaluatoon muscle mass and motor function, based on the AWGS criteria. Between the women in the normal and sarcopenia groups, there was no decrease in the CTV; however, there was a significant decline in the CTV of those in the poor-function and severe sarcopenia groups.
We consider that the decrease in CTV may be attributable to muscle atrophy and increased fat composition in the muscle. Ikemoto-Uezumi et al.
Thus, a decline in CTV with an increased proportion of IMAT was associated with intramuscular fat infiltration [ 30 ]. Similarly, in sarcopenia, increased IMAT is observed [ 16 ], and these changes in muscle tissue could explain the decrease in CTV.
Reportedly, increased IMAT measured by MRI is a prognostic factor of gait ability [ 31 ], and IMAT accumulates markedly after reduced activity in healthy young adults [ 32 ].
We consider that reduced activity or motor function may have caused an increase in IMAT and that CTV could evaluate this change in muscle composition.
As a minimally invasive tool, CT is considered as a gold standard to measure muscle quantity; however, it is not used in general practice owing to the high costs, poor portability, and requirement of an experienced operator [ 15 ]. In patients with cancer, reduced muscle mass is an independent predictor of immobility and mortality [ 33 ].
Kasai et al. Schweitzer et al. Lee SJ reported that CT of the femur was a useful method to evaluate muscle mass for the entire body [ 36 ]. Compared with other test equipment, DXA showed no change with age among Asian women [ 11 ]. Recently, we reported significant associations of thigh CT CSA with muscle strength [ 37 ].
For BIA, changes associated with the physical condition such as fluid balance and body temperature fluctuated during the day, resulting in reduced accuracy of BIA [ 38 ]. CT could be a better form of assessment because of its accuracy, reproducibility, and objectivity [ 39 ]. CT can simultaneously measure the muscle CSA and CTV, indicating muscle mass and composition; thus, CT is useful for assessing the severity of sarcopenia.
Regarding the amount of radiation exposure, as only a single slice is scanned, we consider that there is no problem in terms of the radiation levels [ 10 ]. In addition, single slice leg CT scanning takes only about 5 min.
We think that the present results represent the initial steps toward the accumulation of evidence for the evaluation of muscle quality and will form the basis for future studies to examine the pathophysiology of severe sarcopenia accompanied by not only muscle mass loss but also physical functional decline.
It is also useful for detailed evaluation in patients who have difficulty to walk, or to confirm the muscle condition after screening with a simple physical test.
There were limitations to the present study. First, this was a cross-sectional study and changes caused by natural history or therapeutic intervention could not be evaluated. Further study is required to determine whether or not the changes occurred as a result of exercise therapy, nutritional counseling, and pharmacotherapy.
Second, this study did not include large-scale data of CSA and CTV from each age group of the general population without sarcopenia, and therefore, the healthy control information was weak. Thus, analysis using a large-scale epidemiological study is required.
: Muscle mass evaluation| JMA Journal | This review summarizes the measurement methods and muscle mass indicators of previous studies, highlighting issues with past muscle mass assessments. Acute Sarcopenia Secondary to Hospitalisation - An Emerging Condition Affecting Older Adults. Muscle strength C. Ikemoto-Uezumi M, Matsui Y, Hasegawa M, Fujita R, Kanayama Y, Uezumi A, et al. Corresponding author. |
| Sarcopenia: how to measure, when and why | Department of Rehabilitation, Yokohama City University Hospital [Japan]. Department of Rehabilitation, University Hospital of Occupational and Environmental Health [Japan]. Emergency and Critical Care Medicine, Tokushima University Hospital [Japan] Division of Disaster and Emergency Medicine, Department of Surgery Related, Kobe University Graduate School of Medicine [Japan]. Department of Rehabilitation, Fujita Health University Hospital [Japan]. The skeletal muscle has a significant role on physical functions, and the assessment of the skeletal muscle is important in critically ill patients. Computed tomography CT , ultrasound examination, bioelectrical impedance analysis BIA device, and biomarkers can all be used to assess skeletal muscle mass. CT is useful for accurately measuring skeletal muscle mass, and the measurement is conducted at the third lumbar vertebra level as the gold standard. However, the assessment using CT is done retrospectively because CT involves radiation exposure and requires patients to be transported to the examination room. On the other hand, ultrasound and BIA are noninvasive and can be used at the bedside to assess longitudinal skeletal muscle mass. However, accurate assessment requires knowledge and skills. Assessments using BIA should be carefully interpreted because critically ill patients are under dynamic fluid change and edema. Furthermore, various biomarkers for the assessment of skeletal muscle mass have been recently reported. Appropriate skeletal muscle assessment will contribute to the nutrition and rehabilitation intervention of critically ill patients so that they can return to society. A positive association between the residual and leg function was observed in both men and women, whereas a positive association between the residual and SMI was seen only in men. However, the reference formula may not be generalizable to other populations. Further investigation is required to create the ideal reference formula. However, even after adjusting for these variables, the muscle indicators remained moderately correlated with body size. Therefore, the use of muscle indicators as part of the sarcopenia diagnosis criteria may have biased the diagnosed sarcopenia from the true sarcopenia. Furthermore, the residual correlation between adjusted muscle indicators and body size may interfere with the appropriate assessment of muscle loss. Further research on muscle mass assessment is necessary to establish a clear definition of sarcopenia. This article is based on the study, which received the Medical Research Encouragement Prize of The Japan Medical Association in Because this is not a research of human beings, approval from the institutional review board is not required. Rosenberg IH. Sarcopenia: origins and clinical relevance. J Nutr. View Article PubMed. Muscaritoli M, Anker SD, Argilés J, et al. Clin Nutr. Cruz-Jentoft AJ, Baeyens JP, Bauer JM, et al. Sarcopenia: European consensus on definition and diagnosis: report of the European Working Group on Sarcopenia in older people. Age Ageing. Chen LK, Liu LK, Woo J, et al. Sarcopenia in Asia: consensus report of the Asian Working Group for Sarcopenia. J Am Med Dir Assoc. Studenski SA, Peters KW, Alley DE, et al. The FNIH sarcopenia project: rationale, study description, conference recommendations, and final estimates. J Gerontol A Biol Sci Med Sci. Fielding RA, Vellas B, Evans WJ, et al. Sarcopenia: an undiagnosed condition in older adults. Current consensus definition: prevalence, etiology, and consequences. International working group on sarcopenia. Morley JE, Abbatecola AM, Argiles JM, et al. Sarcopenia with limited mobility: an international consensus. Janssen I, Heymsfield SB, Ross R. Low relative skeletal muscle mass sarcopenia in older persons is associated with functional impairment and physical disability. J Am Geriatr Soc. Cruz-Jentoft AJ, Bahat G, Bauer J, et al. Sarcopenia: revised European consensus on definition and diagnosis. Chen LK, Woo J, Assantachai P, et al. Asian Working Group for Sarcopenia: consensus update on sarcopenia diagnosis and treatment. Bhasin S, Travison TG, Manini TM, et al. Sarcopenia definition: the position statements of the sarcopenia definition and outcomes consortium. Mohd Nawi SN, Khow KS, Lim WS, et al. Screening tools for sarcopenia in community-dwellers: a scoping review. Ann Acad Med Singap. Mijnarends DM, Meijers JMM, Halfens RJG, et al. Validity and reliability of tools to measure muscle mass, strength, and physical performance in community-dwelling older people: a systematic review. McGovern J, Dolan RD, Horgan PG, et al. Computed tomography-defined low skeletal muscle index and density in cancer patients: observations from a systematic review. J Cachexia Sarcopenia Muscle. Hanna L, Nguo K, Furness K, et al. Association between skeletal muscle mass and quality of life in adults with cancer: a systematic review and meta-analysis. Computed tomography-assessed skeletal muscle mass as a predictor of outcomes in lung cancer surgery. Ann Thorac Surg. Amini B, Boyle SP, Boutin RD, et al. Approaches to assessment of muscle mass and myosteatosis on computed tomography: a systematic review. Vangelov B, Bauer J, Kotevski D, et al. The use of alternate vertebral levels to L3 in computed tomography scans for skeletal muscle mass evaluation and sarcopenia assessment in patients with cancer: a systematic review. Br J Nutr. Chianca V, Albano D, Messina C, et al. Sarcopenia: imaging assessment and clinical application. Abdom Radiol NY. Buckinx F, Landi F, Cesari M, et al. Pitfalls in the measurement of muscle mass: a need for a reference standard. Perkisas S, Bastijns S, Baudry S, et al. Application of ultrasound for muscle assessment in sarcopenia: SARCUS update. Eur Geriatr Med. Takai Y, Ohta M, Akagi R, et al. Applicability of ultrasound muscle thickness measurements for predicting fat-free mass in elderly population. J Nutr Health Aging. Abe T, Fujita E, Thiebaud RS, et al. Ultrasound-derived forearm muscle thickness is a powerful predictor for estimating DXA-derived appendicular lean mass in Japanese older adults. Ultrasound Med Biol. Abe T, Loenneke JP, Young KC, et al. Validity of ultrasound prediction equations for total and regional muscularity in middle-aged and older men and women. Sanada K, Kearns CF, Midorikawa T, et al. Prediction and validation of total and regional skeletal muscle mass by ultrasound in Japanese adults. Eur J Appl Physiol. Casey P, Alasmar M, McLaughlin J, et al. The current use of ultrasound to measure skeletal muscle and its ability to predict clinical outcomes: a systematic review. Zhao R, Li X, Jiang Y, et al. Evaluation of appendicular muscle mass in sarcopenia in older adults using ultrasonography: a systematic review and meta-analysis. Khalil SF, Mohktar MS, Ibrahim F. The theory and fundamentals of bioimpedance analysis in clinical status monitoring and diagnosis of diseases. Sensors Basel. Gynecol Oncol. Lenchik L , Lenoir KM , Tan J , et al. Opportunistic measurement of skeletal muscle size and muscle attenuation on computed tomography predicts one-year mortality in Medicare patients. Rier HN , Jager A , Sleijfer S , van Rosmalen J , Kock MCJM , Levin MD. Low muscle attenuation is a prognostic factor for survival in metastatic breast cancer patients treated with first line palliative chemotherapy. Shachar SS , Deal AM , Weinberg M , et al. Skeletal muscle measures as predictors of toxicity, hospitalization, and survival in patients with metastatic breast cancer receiving taxane-based chemotherapy. Clin Cancer Res. Boutin RD , Kaptuch JM , Bateni CP , Chalfant JS , Yao L. Influence of IV contrast administration on CT measures of muscle and bone attenuation: implications for sarcopenia and osteoporosis evaluation. AJR Am J Roentgenol. Derstine BA , Holcombe SA , Goulson RL , et al. Quantifying sarcopenia reference values using lumbar and thoracic muscle areas in a healthy population. Fuchs G , Chretien YR , Mario J , et al. Quantifying the effect of slice thickness, intravenous contrast and tube current on muscle segmentation: implications for body composition analysis. Eur Radiol. Morsbach F , Zhang YH , Nowik P , et al. Influence of tube potential on CT body composition analysis. Maughan RJ , Watson JS , Weir J. The relative proportions of fat, muscle and bone in the normal human forearm as determined by computed tomography. Clin Sci. Moisey LL , Mourtzakis M , Cotton BA , et al. Skeletal muscle predicts ventilator-free days, ICU-free days, and mortality in elderly ICU patients. Crit Care. Paknikar R , Friedman J , Cron D , et al. Psoas muscle size as a frailty measure for open and transcatheter aortic valve replacement. J Thorac Cardiovasc Surg. Cruz RJ Jr , Dew MA , Myaskovsky L , et al. Objective radiologic assessment of body composition in patients with end-stage liver disease: going beyond the BMI. Locke JE , Carr JJ , Nair S , Terry JG , Reed RD , Smith GD , et al. Abdominal lean muscle is associated with lower mortality among kidney waitlist candidates. Clin Transpl. Leeper CM , Lin E , Hoffman M , Fombona A , Zhou T , Kutcher M , et al. Computed tomography abbreviated assessment of sarcopenia following trauma: the CAAST measurement predicts 6-month mortality in older adult trauma patients. Trauma Acute Care Surg. Oakland K , Nadler R , Cresswell L , Jackson D , Coughlin PA. Systematic review and meta-analysis of the association between frailty and outcome in surgical patients. Ann R Coll Surg Engl. The National Cancer Institute Epidemiology and Genomics Research Program EGRP. Understanding the Role of Muscle and Body Composition in Studies of Cancer Risk and Prognosis in Cancer Survivors. Accessed April 4, Goodpaster BH , Carlson CL , Visser M , et al. Attenuation of skeletal muscle and strength in the elderly: the Health ABC Study. J Appl Physiol Brooks N , Cloutier GJ , Cadena SM , et al. Resistance training and timed essential amino acids protect against the loss of muscle mass and strength during 28 days of bed rest and energy deficit. J Appl Physiol. Cauza E , Strehblow C , Metz-Schimmerl S , et al. Effects of progressive strength training on muscle mass in type 2 diabetes mellitus patients determined by computed tomography. Wien Med Wochenschr. Breda AP , Pereira de Albuquerque AL , Jardim C , et al. Skeletal muscle abnormalities in pulmonary arterial hypertension. PLoS One. The National Institute on Aging, The Foundation for the National Institutes of Health FNIH. SDOC Position Development Conference. Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide. Sign In or Create an Account. Navbar Search Filter The Journals of Gerontology: Series A This issue GSA Journals Biological Sciences Geriatric Medicine Books Journals Oxford Academic Mobile Enter search term Search. Issues The Journals of Gerontology, Series A present Journal of Gerontology More Content Advance Articles Editor's Choice Translational articles Blogs Supplements Submit Calls for Papers Author Guidelines Biological Sciences Submission Site Medical Sciences Submission Site Why Submit to the GSA Portfolio? Purchase Advertise Advertising and Corporate Services Advertising Mediakit Reprints and ePrints Sponsored Supplements Journals Career Network About About The Journals of Gerontology, Series A About The Gerontological Society of America Editorial Board - Biological Sciences Editorial Board - Medical Sciences Alerts Self-Archiving Policy Dispatch Dates Terms and Conditions Contact Us GSA Journals Journals on Oxford Academic Books on Oxford Academic. GSA Journals. Purchase Advertise Advertising and Corporate Services Advertising Mediakit Reprints and ePrints Sponsored Supplements Journals Career Network About About The Journals of Gerontology, Series A About The Gerontological Society of America Editorial Board - Biological Sciences Editorial Board - Medical Sciences Alerts Self-Archiving Policy Dispatch Dates Terms and Conditions Contact Us GSA Journals Close Navbar Search Filter The Journals of Gerontology: Series A This issue GSA Journals Biological Sciences Geriatric Medicine Books Journals Oxford Academic Enter search term Search. Advanced Search. Search Menu. Article Navigation. Close mobile search navigation Article Navigation. Volume Article Contents Abstract. Author Contributions. Conflict of Interest. Journal Article. Approaches to Assessment of Muscle Mass and Myosteatosis on Computed Tomography: A Systematic Review. Behrang Amini, MD, PhD , Behrang Amini, MD, PhD. Department of Diagnostic Radiology, The University of Texas M. Anderson Cancer Center. Address correspondence to: Behrang Amini, MD, PhD, Department of Diagnostic Radiology, The University of Texas M. Anderson Cancer Center, Holcombe Blvd, Unit , Houston, TX E-mail: bamini mdanderson. Oxford Academic. Sean P Boyle, BS. Department of Diagnostic Radiology, University of California, Davis School of Medicine. Robert D Boutin, MD. Leon Lenchik, MD. Department of Diagnostic Radiology, Wake Forest School of Medicine. PDF Split View Views. Select Format Select format. ris Mendeley, Papers, Zotero. enw EndNote. bibtex BibTex. txt Medlars, RefWorks Download citation. Permissions Icon Permissions. Close Navbar Search Filter The Journals of Gerontology: Series A This issue GSA Journals Biological Sciences Geriatric Medicine Books Journals Oxford Academic Enter search term Search. Body composition , Imaging , Muscle , Sarcopenia. Figure 1. Open in new tab Download slide. Figure 2. Table 1. Muscle Mass Assessment. Anatomic Landmarks. Main Muscle Mass Measurement. Sarcopenia Cut Points Used. Male c. Muscle Thresholding Used. Threshold Range HU. Open in new tab. Table 2. Myosteatosis Assessment. Myosteatosis Cut Points b. Main Myosteatosis Measurement. MyosteatosIs Cut Points Used. Used HU Threshold. Table 3. Image Analysis Details. Assessed Feature. Number of readers 1 97 38 2 53 21 3 7 3 Not specified 98 38 Segmentation methods Manual 27 Semiautomated 59 Automated 6 1. |
| Radiological Evaluation of Muscle Mass | In Taiwan, the decrease in CP 26 26 Hsu WC, Tsai AC, Wang JY. sarah hsr. Am J Epidemiol [Internet]. Dent E , Chapman I , Piantadosi C , Visvanathan R. nursing home admission. Search ADS. Chen LK, Liu LK, Woo J, Assantachai P, Auyeung TW, Bahyah SK, et al. |
Ich bin endlich, ich tue Abbitte, aber es kommt mir ganz nicht heran. Wer kann noch helfen?
der Anmutige Gedanke
die Prächtige Idee
Sie irren sich. Geben Sie wir werden es besprechen. Schreiben Sie mir in PM.
Jetzt kann ich an der Diskussion nicht teilnehmen - es gibt keine freie Zeit. Aber bald werde ich unbedingt schreiben dass ich denke.