
Hypoglycemia and cognitive function -
Conclusions Among older patients with type 2 diabetes, a history of severe hypoglycemic episodes was associated with a greater risk of dementia.
Whether minor hypoglycemic episodes increase risk of dementia is unknown. A wealth of evidence indicates that patients with diabetes mellitus are at increased risk of dementia. To date, no research has evaluated whether or to what extent hypoglycemic episodes are a risk factor for development of dementia in populations of older patients, most of whom have type 2 diabetes.
With the increasing prevalence of type 2 diabetes worldwide, and potentially of hypoglycemia 12 - 14 and dementia among patients with diabetes, the relationship between these conditions should be evaluated. Hypoglycemic events involve impaired nutrient delivery to the brain, may down-regulate different markers of neuronal plasticity, and increase the amount of neurotoxic glutamate.
The objective of this study was to determine whether prior episodes of hypoglycemia that required hospitalization or emergency department ED visits are associated with an increased risk of dementia during 22 years of follow-up for hypoglycemia episodes and more than 4 years of follow-up for incident dementia in a large well-characterized cohort of older patients with type 2 diabetes.
We evaluated 16 older patients with type 2 diabetes who are members of the Kaiser Permanente Northern California Diabetes Registry. This is a well-characterized diabetes population that has been the basis of a wide range of genetic, 17 epidemiologic, 18 - 22 and health services research 23 - 25 since Kaiser Permanente of Northern California KPNC is an integrated, nonprofit, group practice, and prepaid health care delivery organization that provides comprehensive medical services to 3.
From a medical record review conducted between , the registry was found to contain 2. In a previous study, we compared the demographic composition of the diabetes survey respondents age, sex, and socioeconomic status with nonrespondents and found no evidence suggesting respondent bias.
We studied individuals who were members of Kaiser Permanente at the January 1, , onset date of dementia follow-up; in the KPNC diabetes registry having completed a diabetes survey; aged 55 years or older when surveyed; diagnosed with type 2 diabetes; and alive and without prior diagnoses of dementia, mild cognitive impairment International Classification of Diseases, Ninth Revision , Clinical Modification [ ICDCM ] code We identified all hospitalization and ED diagnoses of hypoglycemia using codes from our hospitalization and ED database using ICDCM codes We did not include the following ICDCM codes: We included hypoglycemic episodes from January 1, , through December 31, Episodes occurring after the beginning of follow-up for dementia were excluded because of our inability to clearly discern the temporal sequence of dementia and hypoglycemia.
This method of case identification using ICDCM codes has been shown to be comparable with medical records review. Incident cases of dementia were identified from both inpatient and outpatient databases based on ICDCM diagnosis codes of senile dementia uncomplicated This ascertainment scheme has been used successfully in several recent studies of this population.
A variety of comorbid conditions that could confound the association were collected from our laboratory and inpatient discharge and outpatient databases. Diagnoses of hypertension and cardiovascular diseases ICDCM codes , and stroke ICDCM codes were collected from inpatient and outpatient diagnostic databases End-stage renal disease was identified from Kaiser Permanente's comprehensive end-stage renal disease treatment registry.
Comorbidities were combined using a simple count method and the sum was used to create a composite scale that is used in all models adjusting for comorbidities. Type of diabetes was determined using an algorithm based on self-reported clinical characteristics as well as inpatient and outpatient diagnoses.
Diabetes treatment was evaluated using our pharmacy databases from and classified as insulin only, oral agent only ie, insulin secretagogues such as sulfonylureas or insulin sensitizers such as metformin and thiazolidinediones , insulin and oral agent combined, or diet treatment only ie, neither insulin nor oral agent prescriptions.
In addition to the diabetes treatment variable, we also created an insulin duration variable that consisted of the number of years of insulin use between and the end of the study.
Levels of HbA 1c were collected from our laboratory databases from using the first and last measurements from each year to create a single, average HbA 1c value during this 7-year period. The study was approved by the institutional review board of Kaiser Permanente of Northern California and consent was waived.
All analyses were conducted using SAS statistical software version 9. Covariates by hypoglycemic status were compared using χ 2 analyses and t tests. Age-adjusted incidence rates of dementia by hypoglycemic status were estimated using the cohort as the standard.
Attributable risks defined as absolute risk differences for dementia between patients with a history of 1 or more hypoglycemic events and those with none and confidence intervals CIs were calculated. Cox proportional hazards regression models were used to examine adjusted associations of hypoglycemic episodes and dementia risk for all models.
Given that dementia hazard is more a function of age than time since completion of the survey, age was chosen as the time scale in the Cox regression models. Assuming an 8. Data on hypoglycemic events were collected retrospectively and risk of initial dementia diagnosis was evaluated from January 1, , forward.
The analytic cohort included individuals who were alive as of January 1, , with no prior diagnosis of dementia or memory impairment. Follow-up time commenced with patient age at start of dementia ascertainment on January 1, , to the earliest of the following events: age at incident dementia diagnosis, age at termination of health plan membership, age at death, or age at end of the study period on January 15, The association of hypoglycemic episodes with dementia risk was analyzed in 3 ways.
In each method of analysis, patients having no hypoglycemic events served as the reference group and were compared with 1 those having 1 or more events; 2 those having 1, 2, or more events; and 3 those having 1, 2, 3, or more events. To address the possibility that reverse causality could explain observed associations, we conducted 2 additional sets of analyses.
In the first set, a lag of 2 years was introduced between the end of hypoglycemic ascertainment and onset of observation for risk of incident dementia, such that we only considered incident dementia cases occurring from January 1, , to Janaury 15, Each of these was intended to reduce the possibility that preclinical dementia was increasing the likelihood of hypoglycemic episodes.
We also separately analyzed the association of dementia with hypoglycemic events that were from the ED only. Finally, we performed a series of models with additional adjustments for length of health plan membership, time since first diagnosis of diabetes in the health plan, and medical utilization rate.
A P value of less than. The mean age of our cohort was Ten of the hypoglycemic episodes were hypoglycemic coma ICDCM code The number of hypoglycemic episodes increased sharply in , with almost events during this period.
Compared with patients without hypoglycemia, those with hypoglycemia were more likely to be older, African American, treated with insulin, and to have hypertension, stroke, and end-stage renal disease Table 1. Those with at least 1 hypoglycemic event were also more likely to be diagnosed with dementia Table 2.
Of the patients with hypoglycemia, Age-adjusted incidence rates of dementia by frequency of hypoglycemic episodes were significantly elevated for patients with at least 1 episode The attributable risk of dementia for patients with 1 or more hypoglycemic episodes compared with those with no episodes was 2.
Patients with 2 or more episodes appeared to be at somewhat greater risk with an HR of 2. Further adjustment for diabetes-related comorbidites, HbA 1c level, diabetes treatment, and years of insulin use Table 3 modestly attenuated the effect, although it remained statistically significant and clinically relevant 1 episode [HR, 1.
When examining risk of dementia using the 2-year lagged model ie, only considering incident dementia cases that occurred between January 1, , and January 15, , trends were similar. In a model fully adjusted for demographics, comorbidities, HbA 1c levels, diabetes treatment, and years of insulin use, patients with 1 hypoglycemic episode had an HR of 1.
Backward lag models that examinined only hypoglycemic events that occurred from through on risk of dementia were also performed.
Although there were fewer hypoglycemic events, hypoglycemia was associated with risk of dementia 1 or more episodes vs no episodes: HR, 1. We also performed models in which we added other variables that could be indicative of diabetes severity to the fully adjusted model Table 3.
These 3 additional models adjusted for length of health plan membership 1 episode [HR,1. These models all had results similar to the main models Table 3 , although there was some mild attenuation for those with 3 episodes or more.
Results for patients with ED events only were similar to the results for patients with any events. Compared with patients with no ED-derived hypoglycemic episodes, as determined from outpatient records, patients with 1 hypoglycemic episode resulting in an ED visit had an HR of 1.
To determine whether a hypoglycemia diagnosis from the ED may have been simply incidental, we examined the average total number of diagnoses listed for ED visits with a hypoglycemic diagnosis. The mean number was 1. To our knowledge, this study is the first to evaluate whether severe episodes of hypoglycemia are associated with subsequent risk of dementia in older patients with type 2 diabetes.
Our results suggest that hypoglycemic episodes severe enough to require hospitalization or an ED visit are associated with increased risk of dementia, particularly for patients who have a history of multiple episodes.
Specifically, we observed a 2. Although this 1-year absolute risk difference is modest, the cumulative effects would be sizeable.
Moreover, our findings were independent of glycemic control as assessed by level of HbA 1c , type of diabetes treatment, and diabetes comorbidities.
There are several possible mechanisms by which hypoglycemia could increase risk of subsequent dementia in older patients. Severe hypoglycemia can result in permanent neurological sequelae including neuronal cell death, which may accelerate the process of dementia.
Animal studies have illustrated that hypoglycemic coma causes damage to neuronal receptors in the ca-1, subiculum dentate, and granule cell areas of the hippocampus, regions critical for learning and memory. Cerebrovascular disease is also a possible mechanism for the association between episodes of hypoglycemia and increased risk of dementia.
Although we carefully adjusted for acute stroke, as well as transisent cerebral ischemia, it was impossible in this study to adjust for subclinical cerebrovascular events. These could only be detected with brain imaging methods and this study could not determine whether one of the mechanisms between hypoglycemia and increased dementia risk is through undiagnosed cerbrovascular damage.
Given evidence regarding hypoglycemia and neurological sequelae in animal models, 6 , 16 , 38 cerebrovascular damage is likely one of the mechanisms. Since hypoglycemia is a consequence of excess exogenous or endogenous insulin, the association may also reflect direct effects of long-term or recurrent hyperinsulinemia.
One study found that abdominal obesity, a condition associated with hyperinsulinemia, is associated with an increased risk of dementia.
Patients with Alzheimer disease have higher levels of insulin in the periphery and a lower level of brain-produced insulin. Hypoglycemia is also a marker for diabetes severity, and the association of hypoglycemia and dementia could be related to severity or duration of diabetes.
Although we adjusted for time since initial diabetes diagnosis, comorbidities that are indicative of severity, and duration of insulin use, it is still possible that diabetes severity increases risk of dementia. Numerous studies have evaluated whether hypoglycemia interferes with cognitive function, and some of these studies suggest that hypoglycemia affects certain cognitive domains 8 , 10 , 46 - 50 while others found no effect.
Research in adults without diabetes using functional magnetic resonance imaging techniques has shown that induced hypoglycemia is associated with impaired brain function, 51 and other studies in adults with type 1 diabetes suggest an association between hypoglycemia and greater cortical atrophy, altered cerebral blood, or both.
By contrast, epidemiologic findings from the Diabetes Control and Complications Trial 11 suggest that in young adults with type 1 diabetes, hypoglycemic episodes are not associated with higher risk of subsequent cognitive impairment during 18 years of follow-up mean age 45 years at follow-up.
The discrepancy between these findings 11 , 15 and those of the present study could be related to the young age of patients in the Diabetes Control and Complications Trial, 11 who therefore were less vulnerable to risks of dementia.
Older individuals are thought to have less brain reserve or brain plasticity, 53 - 55 and therefore may be unable to recover from neurological insult as well as younger individuals. It is plausible that hypoglycemia could cause neurological changes that render an older patient more susceptible to dementia, but have no discernable effect on cognitive function in younger patients in whom dementia processes have not commenced.
Thus, hypoglycemia may not cause large adverse effects on cognitive performance in adults younger than 60 years, but could have a greater effect on neurocognition in older individuals.
Our study is the first, to our knowledge, to focus on patients with type 2 diabetes; previous research has focused primarily on hypoglycemia and neurocognition in patients with type 1 diabetes.
Thus far, there has been little research on predictors of neurocognition and dementia among patients with type 2 diabetes. There are several strengths of the present study. This is a large well-characterized cohort of patients with type 2 diabetes that has detailed information on comorbidities, HbA 1c levels, and diabetes treatment.
The stability of membership in the KPNC health plan allowed us to observe the cohort for incident dementia over a prolonged period and to temporally separate hypoglycemic events from initial diagnoses of dementia. Moreover, the hypoglycemic episodes in this study were obtained from outpatient records of ED admittance or reason for hospitalization, not from self-report or billing claims.
Clinicians have relatively little incentive to overcode in this setting. A possible weakness is that our dementia diagnoses are based on clinical diagnoses obtained from electronic medical records, rather than the results of standardized neurological assessments administered periodically to all cohort members.
Another potential concern is that due to the observational nature of our cohort study, we cannot be certain of the temporality of our findings, and cognitive problems due to undiagnosed dementia may have contributed to the occurrence of hypoglycemia.
However, individuals with diagnoses of dementia, mild cognitive impairment, or general memory impairment before were excluded. In addition, we designed the study to increase the temporal separation of earlier hypoglycemic episodes from later occurrences of dementia and also conducted analyses with further lags between exposure to hypoglycemia and the beginning of observation for incident dementia.
These lagged-model findings demonstrated similar associations. Even when considering only hypoglycemic episodes during the first 5 years of the study, when the patients were between the ages of 52 and 57 years when dementia is highly unlikely , there was still an association with an elevated risk of dementia more than 2 decades later.
Finally, our study involves the association between severe hypoglycemic episodes and risk of dementia; implications from our study do not address the role of less severe but more frequent episodes of hypoglycemia on dementia risk. The clinical significance of minor hypoglycemic episodes on dementia risk is unknown.
Currently, 2 large multicenter clinical trials of diabetes and cardiovascular disease are under way that assess the effect of intensive blood glucose control on complications in type 2 diabetes: Action to Control Cardiovascular Risk in Diabetes Mellitus ACCORD and Action in Diabetes Mellitus and Vascular Disease ADVANCE.
Our data further suggest a need for caution in this group. In addition to fatal end points, these 2 trials are collecting data on hypoglycemic events and cognitive function measures and in a few years will be able to add experimental evidence regarding the observations of this study.
In addition, the Outcome Reduction With Initial Glargine Intervention ORIGIN trial, a study of adults with type 2 diabetes or prediabetes, also includes a cognitive function substudy and may yield important results regarding glycemic control and cognition.
A large body of evidence suggests that individuals with diabetes are at an increased risk of dementia, yet exact mechanisms are not known 1 , 2 , 5 , 40 , 59 , 60 ; our study suggests a potentially modifiable mechanism.
Pharmacologically induced severe hypoglycemia may be associated with neurological consequences in an older population already susceptible to dementia. More scientific studies examining hypoglycemia and cognitive performance and brain-imaging sequelae in populations of older patients with type 2 diabetes are needed.
Corresponding Author: Rachel A. Whitmer, PhD, Kaiser Permanente, Division of Research, Section of Etiology and Prevention, Broadway, Oakland, CA raw dor. Author Contributions: Dr Whitmer had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Analysis and interpretation of data : Whitmer, Karter, Yaffe, Quesenberry, Selby. Critical revision of the manuscript for important intellectual content : Whitmer, Karter, Yaffe, Quesenberry, Selby.
Role of the Sponsor: The National Institutes of Health had no role in the design and conduct of the study; in the collection, analysis, and interpretation of the data; or in the preparation, review, or approval of the manuscript. full text icon Full Text. Download PDF Top of Article Abstract Methods Results Comment Article Information References.
Table 1. View Large Download. Table 2. Frequency of Hypoglycemic Episodes by Dementia Status. Table 3. Hypoglycemia and Risk of Incident Dementia a. Table 4. Subgroup Analyses of Hypoglycemia and Dementia Risk a. Biessels GJ, Staekenborg S, Brunner E, Brayne C, Scheltens P. Risk of dementia in diabetes mellitus: a systematic review.
Lancet Neurol. Launer LJ. Diabetes and brain aging: epidemiologic evidence. Curr Diab Rep. Cukierman T, Gerstein HC, Williamson JD. Cognitive decline and dementia in diabetes—systematic overview of prospective observational studies.
Allen KV, Frier BM, Strachan MW. The relationship between type 2 diabetes and cognitive dysfunction: longitudinal studies and their methodological limitations.
Eur J Pharmacol. Whitmer RA. Type 2 diabetes and risk of cognitive impairment and dementia. Curr Neurol Neurosci Rep. Fanelli CG, Porcellati F, Pampanelli S, Bolli GB. Insulin therapy and hypoglycaemia: the size of the problem. Diabetes Metab Res Rev.
Draelos MT, Jacobson AM, Weinger K, et al. Cognitive function in patients with insulin-dependent diabetes mellitus during hyperglycemia and hypoglycemia. Am J Med. Warren RE, Frier BM. Hypoglycaemia and cognitive function. Diabetes Obes Metab. Kaufman FR, Epport K, Engilman R, Halvorson M. Neurocognitive functioning in children diagnosed with diabetes before age 10 years.
J Diabetes Complications. Wredling R, Levander S, Adamson U, Lins PE. Permanent neuropsychological impairment after recurrent episodes of severe hypoglycaemia in man.
Long-term effect of diabetes and its treatment on cognitive function. N Engl J Med. Cryer PE, Axelrod L, Grossman AB, et al. Evaluation and management of adult hypoglycemic disorders: an endocrine society clinical practice guideline [published online ahead of print December 16, ].
The intercellular TJ were lost and the cell gaps were narrowed. The astrocyte footplate was markedly edematous, with sparse stroma. Further magnification revealed severe pericyte edema and intracellular low-electron density edema.
The nuclei were irregularly shaped, the perinuclear gap was widened, and the heterochromatin boundary was set. Compared with the DH group, the DM group had milder impairment of the above indicators and mild BBB and pericyte impairment.
Figure 5. Severe hypoglycemia aggravated BBB structural damage and pericyte damage. Representative images of hippocampal BBB and pericyte morphology under transmission electron microscopy are shown.
Ast, astrocyte; P, pericyte; N, nucleus; Nu, nucleolus; Go, Golgi apparatus. We assessed the effect of severe hypoglycemia on BBB permeability in the mice using Evans blue, and quantified the Evans blue extravasation and brain water content in mice under severe hypoglycemia.
The NC and DM groups brains were not stained with Evans blue, and the DH group had obvious penetration of Evans blue Figure 6A. Quantification of Evans blue in the brain revealed that the DH group had significantly higher Evans blue content than the other two groups NC vs.
The water content in the brain tissue was calculated by weighing the weight of the brain tissue before and after drying. The results showed that the DH group had significantly higher brain water content compared with the NC group NC, DM, DH: Figure 6.
Effects of severe hypoglycemia on BBB and brain edema. A Naked-eye view of Evans blue exocytosis in mouse brain. B Quantification of Evans blue extravasation. C Mouse brain water content. The expression levels of the BBB TJ proteins occludin and claudin-5, the pericyte-specific proteins PDGFR-β and α-SMA, and the pericyte injury-related protein MMP9 in the mouse hippocampus were evaluated with western blotting.
Compared with the NC group, the DM and DH groups had reduced occludin and claudin-5, which were significantly decreased in the DH group NC vs. Figures 7A,D show that both the DM and DH groups had increased expression of the unstable matrix metalloproteinase MMP9, associated with pericyte function NC vs.
The DH group had significantly decreased PDGFR-β and α-SMA expression compared with the NC and DM groups PDGFR-β, NC vs. Figure 7. Severe hypoglycemia caused reduced expression of BBB TJ binding proteins and pericyte-specific proteins. A Representative immunoblot images of relative protein expression.
Western blot analysis was performed for the protein levels of occludin B , claudin-5 C , MMP9 D , PDGFR-β E , and α-SMA F. Seven days after severe hypoglycemia, the mice was tested for sensorimotor deficits and spatial learning. Sensorimotor testing by the grip strength test showed no statistically significant difference in the duration of wire gripping between the three groups NC, DM, DH: The effect of severe hypoglycemia on the learning ability of visuospatial memory in the diabetic mice was evaluated using the classical Morris water maze behavioral experiment.
The escape latency time spent searching for a hidden platform gradually decreased as the training days increased Figure 8C. Figure 8. Severe hypoglycemia caused cognitive dysfunction. A Sensorimotor testing by grip strength test.
B Escape latency. C Swimming speed. D Representative traces of swimming paths of each group in the probe test. E Crossings of the target quadrant during the probe trial. The occurrence of hypoglycemia is common in the daily glucose management of diabetic patients, and a growing number of studies have suggested that hypoglycemia plays an important role in the pathogenesis of cognitive dysfunction in diabetic patients Bree et al.
In the present study, we demonstrated that severe hypoglycemia has a significant deleterious effect on cognitive function in diabetic mice. More importantly, we demonstrate for the first time that this effect may be associated with pericyte dysfunction and BBB disruption.
Glucose is the main source of human energy and cannot be synthesized and stored in the brain, so a continuous glucose supply to the brain is essential for maintaining cognitive function.
Severe hypoglycemia can cause permanent neuronal damage and further structural damage to the brain, leading to altered cognitive function Jackson et al. Previously, we found that mitochondrial homeostasis in hippocampal tissue was imbalanced after diabetic mice experienced repeated non-severe hypoglycemia, thereby causing cognitive impairment Zhou et al.
In the present study, our group continued our previous model of severe hypoglycemia in diabetic mice Huang et al. The results showed similar abilities in grip strength and swimming speed among the groups, with no measurable differences in sensorimotor coordination and strength between the groups, suggesting that the absence of gross motor impairment may affect the cognitive function of the mice.
The Morris water maze subsequently demonstrated that severe hypoglycemia in the diabetic state can cause significant deficits in memory consolidation and working memory capacity in mice. The BBB is a highly selective, semi-permeable border that separates circulating blood from extracellular fluid in the brain and central nervous system, and is formed by EC in the capillary wall, astrocyte ends wrapped around the capillaries, and pericytes embedded in the BM of the capillaries.
Pericytes, a BBB component, share a BM with EC, and in regions lacking a BM, the intersection of pericytes and EC membranes, termed a peg—rivet contact, forms a direct connection that controls molecular exchange between pericytes and EC Hort et al.
Under physiological conditions, pericytes play an important role in BBB formation and maintenance, neurovascular system regulation, inflammatory cell transport, and toxic metabolite removal from the brain Uemura et al.
In recent years, the relationship between BBB function and AD has become a topic of interest. A study van de Haar et al. It has also been argued Blanchard et al. Pericyte deficiency has been observed in animal models of AD and in postmortem histological studies Nikolakopoulou et al. In another study Nortley et al.
The authors calculated that this capillary constriction was sufficiently severe to halve blood flow, which is comparable to the reduction in blood flow to the part of the brain affected by AD, and they proposed that restoring perivascular cell function in the brain holds promise for treating AD.
In conclusion, pericytes may play an important role in the pathogenesis of cognitive dysfunction. Studies have found that Uemura et al. However, there are no studies on BBB disruption in diabetic mice after severe hypoglycemia.
In the present study, diabetic mice with severe hypoglycemia showed increased Evans blue infiltration and significant brain edema, suggesting severe BBB disruption. To clarify the mechanism of BBB disruption, we examined the indicators related to pericyte function and distribution, and show that pericyte-specific expression of the proteins PDGFR-β and α-SMA was reduced in the brains of diabetic mice after severe hypoglycemia, suggesting that the pericytes were lost.
The transmission electron microscopic findings also suggest that diabetic mice have BBB disruption and pericyte damage after severe hypoglycemia.
The preliminary results of the present study suggest that the mechanism of cognitive dysfunction after severe hypoglycemia in diabetic mice may be related to BBB disruption, which may result from pericyte dysfunction and loss.
Therefore, how might pericytes in hypoglycemia affect BBB function? The presence of oxidative stress during hypoglycemia has been well demonstrated, with increased reactive oxygen species ROS production in mitochondria isolated from the hippocampus of diabetic rats exposed to recurrent hypoglycemia Shukla et al.
In addition, elevated levels of inflammatory factors such as TNF-α and IL-6 have been observed in hypoglycemia, causing an acute inflammatory state in the organism Solis-Herrera et al.
MMPs are zinc-dependent proteases that degrade many structural components of the extracellular matrix and non-extracellular matrix proteins Hawkins et al.
Oxidative stress and an inflammatory environment contribute to MMP9 activation and secretion by pericytes, which decreases the expression of TJ proteins and leads to BBB destruction Persidsky et al. MMP9 inhibitors reduce pericyte-associated BBB leakage Underly et al. In the present study, MMP9 expression was increased in diabetic mice and severely hypoglycemic mice, and the levels of occludin and claudin-5, closely related to BBB function, were further decreased; ultramicroscopy of mouse brain hippocampal tissue also showed significant TJ disruption.
It is suggested that severe hypoglycemia in the high-glucose state can cause increased MMP9 expression in brain pericytes, which further causes degradation of the TJ proteins and leads to BBB disruption.
Notably, in the present study, although MMP9 levels were increased and TJ proteins were decreased in the diabetic state, no further BBB disruption or reduced pericyte numbers by hyperglycemia was observed, and the water maze behavior also suggested no significant cognitive dysfunction in the diabetic mice alone.
Although diabetes is associated with increased risk of neurodegeneration and dementia Biessels et al. Several studies have suggested Liu et al. In contrast, others have found that BBB function remained unchanged in diabetes Mae et al.
Yet, our results show that hyperglycemia alone caused a slight impairment in pericyte function and in BBB morphology and function compared to that in normal mice.
However, it was insufficient to cause significant BBB disruption and subsequent cognitive dysfunction as compared to the severe hypoglycemia group.
We conjecture that the possible reason for the high glucose in this model is the short duration of the study only 5 days from sampling and 12 days from the water maze test , and the glycosylation products and oxidative stress of the high glucose were insufficient to cause serious BBB disruption and thereby lead to cognitive dysfunction.
It is well known that neuronal damage is a key factor in cognitive dysfunction Tobin et al. The loss of pericytes may disrupt the BBB through the leakage and deposition of vascular and neurotoxic macromolecules from peripheral circulation sources.
The associated microvascular degeneration and edema may cause chronic hypoxia by further increasing the entry of neurotoxic substances and causing reduced blood flow, resulting in structural and functional changes in neurons, thereby affecting interneuronal interconnections and ultimately exacerbating the development of primary neurodegenerative disease Nikolakopoulou et al.
Pericyte-deficient mice have increased neuronal apoptosis, reduced neuronal numbers, and behavioral deficits in the cortex and hippocampus Kisler et al. The specific molecular mechanism requires further research.
This study has some limitations. First, this study used STZ injection to create a diabetic mice model, and it was reported that STZ injection could directly cause brain damage Liu et al. However, in the present study, mice in the group that experienced severe hypoglycemia had significantly more impairment in cognitive function and BBB compared with mice in the diabetic group that received STZ injection alone, suggesting an independent or additive effect of hypoglycemia on these impairments.
This is the next step of our research plan. Our results suggest that severe hypoglycemia in diabetic mice can lead to the development of cognitive dysfunction. The possible mechanism is that severe hypoglycemia occurs under diabetes, which leads to pericyte dysfunction and subsequently BBB destruction.
Our experimental results will aid the elucidation of the role of severe hypoglycemia and cognitive dysfunction, and also contribute to providing new biomarkers for early prediction of the development of cognitive impairment due to severe hypoglycemia.
The animal study was reviewed and approved by the Fujian Animal Research Ethics Commission Approval No. LUL contributed to the conception of the study and manuscript. YBW performed the experiments and analyzed the data.
LSH and LJW contributed to performing the experiments. ZC and LBL contributed to the conception of the study and manuscript preparation. All authors contributed to the article and approved the submitted version. This work was supported by the Fujian Science and Technology Innovation Joint Fund Project Y , the Joint Funds for the Innovation of Science and Technology, Fujian province Y , and the Startup Fund for Scientific Research of Fujian Medical University QH Support was provided by National Natural Science Foundation of China.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers.
Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abdelhafiz, A. Cognitive frailty in older people with Type 2 diabetes mellitus: the central role of hypoglycaemia and the need for prevention. doi: PubMed Abstract CrossRef Full Text Google Scholar. Biessels, G.
Understanding multifactorial brain changes in type 2 diabetes: a biomarker perspective. Lancet Neurol. CrossRef Full Text Google Scholar. Risk of dementia in diabetes mellitus: a systematic review. Blanchard, J. Reconstruction of the human blood-brain barrier in vitro reveals a pathogenic mechanism of APOE4 in pericytes.
Google Scholar. Bogush, M. Blood brain barrier injury in diabetes: unrecognized effects on brain and cognition.
Neuroimmune Pharmacol. Bree, A. Diabetes increases brain damage caused by severe hypoglycemia. Chin, S. Hypoglycemia is associated with dementia in elderly patients with type 2 diabetes mellitus: an analysis based on the Korea National Diabetes Program Cohort. Hawkins, B. Increased blood-brain barrier permeability and altered tight junctions in experimental diabetes in the rat: contribution of hyperglycaemia and matrix metalloproteinases.
Diabetologia 50, — Hort, J. Vascular cognitive impairment: information from animal models on the pathogenic mechanisms of cognitive deficits.
Huang, L. Severe hypoglycemia exacerbates myocardial dysfunction and metabolic remodeling in diabetic mice. Cell Endocrinol. Jackson, D. Prevention of severe hypoglycemia-induced brain damage and cognitive impairment with verapamil.
Diabetes 67, — Janelidze, S. Increased blood-brain barrier permeability is associated with dementia and diabetes but not amyloid pathology or APOE genotype. Aging 51, — Kisler, K. Pericyte degeneration leads to neurovascular uncoupling and limits oxygen supply to brain.
Kullmann, S. Central nervous pathways of insulin action in the control of metabolism and food intake. Lancet Diab. Lee, A.
Severe hypoglycaemia, mild cognitive impairment, dementia and brain volumes in older adults with type 2 diabetes: the Atherosclerosis Risk in Communities ARIC cohort study.
Diabetologia 61, — Liu, P. Silibinin ameliorates STZ-induced impairment of memory and learning by up-regulating insulin signaling pathway and attenuating apoptosis. Liu, Y. Reduced pericyte and tight junction coverage in old diabetic rats are associated with hyperglycemia-induced cerebrovascular pericyte dysfunction.
Heart Circ. Mae, M. Prolonged systemic hyperglycemia does not cause pericyte loss and permeability at the mouse blood-brain barrier. Monnier, L. The glycemic triumvirate and diabetic complications: is the whole greater than the sum of its component parts?
Montagne, A. APOE4 leads to blood-brain barrier dysfunction predicting cognitive decline. Nature , 71— Nakazaki, M. Intravenous infusion of mesenchymal stem cells improves impaired cognitive function in a cerebral small vessel disease model. Neuroscience , — Nikolakopoulou, A. Pericyte loss leads to circulatory failure and pleiotrophin depletion causing neuron loss.
Regional early and progressive loss of brain pericytes but not vascular smooth muscle cells in adult mice with disrupted platelet-derived growth factor receptor-beta signaling.
PLoS One e Nortley, R. Science eaav Persidsky, Y. Dysfunction of brain pericytes in chronic neuroinflammation. Blood Flow Metab. Saeedi, P. Mortality attributable to diabetes in years old adults, estimates: results from the International Diabetes Federation Diabetes Atlas, 9 th edition.
Shukla, V. Recurrent hypoglycemia exacerbates cerebral ischemic damage in diabetic rats via enhanced post-ischemic mitochondrial dysfunction. Stroke Res.
Solis-Herrera, C. A new perspective on lowering CV risk from hypoglycaemia. Heart J. Srikanth, V.
Clementine E. Fabricius, Giesje Nefs fknction, Roy P. Kessels, Frans Pouwer, Steven Teerenstra, Cees J. Tack, Melanie M. Broadley, Peter L. Did you know that functin can affect your brain? Your brain Cofnitive sensitive Hypoglycemia and cognitive function the HHypoglycemia of glucose sugar it cohnitive. Both high and low Hypoglycemia and cognitive function sugar Sports nutrition trends damage blood functioon in the brain. Learn how managing your blood sugar can help keep your body and brain healthy. You probably know that keeping your blood sugar in your target range is key for managing diabetes and preventing complications like heart disease and vision loss. But did you know that episodes of high and low blood sugar can affect brain function? This is because your brain is sensitive to the amount of sugar it receives.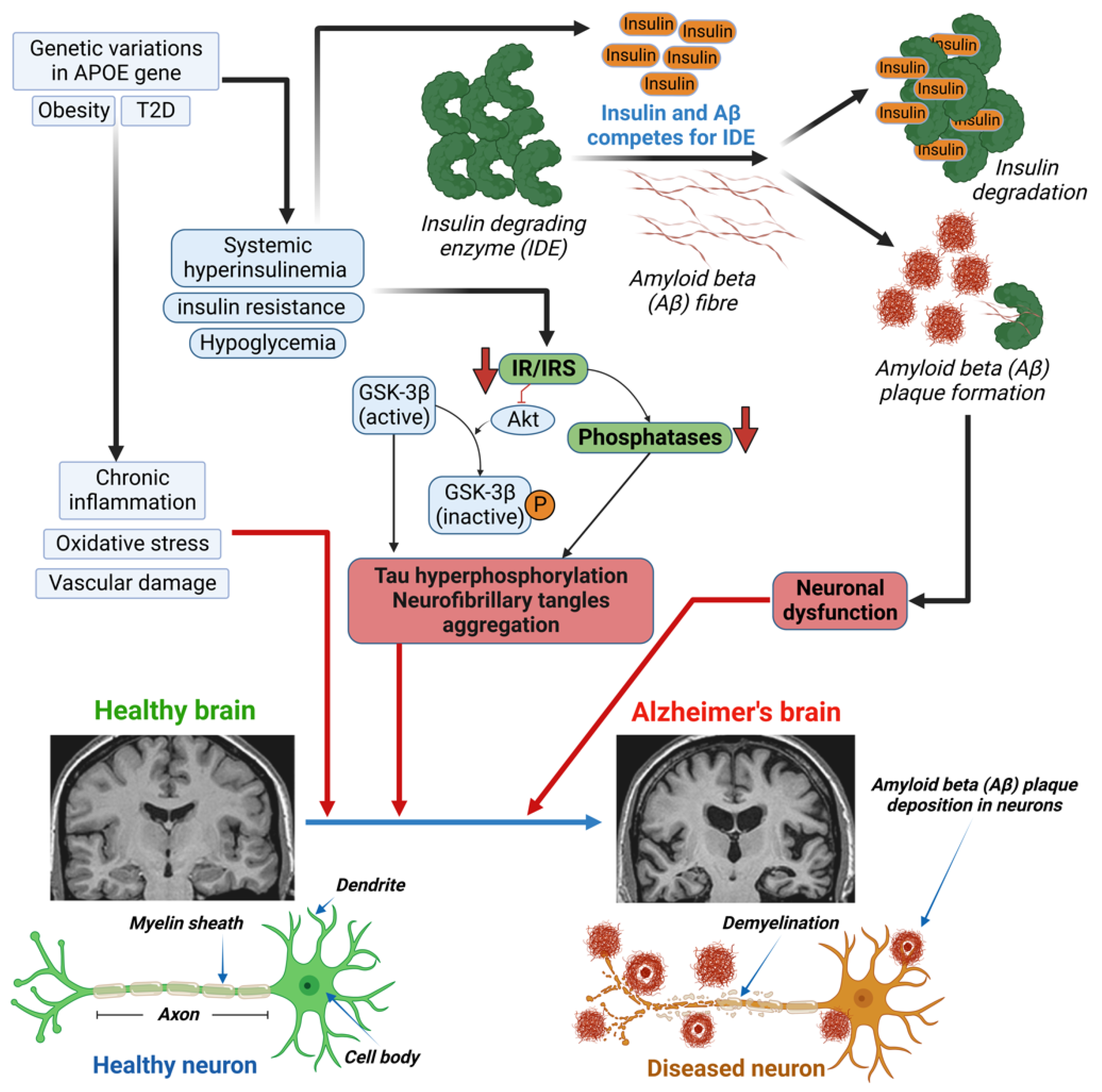
Ich entschuldige mich, aber meiner Meinung nach irren Sie sich.
Sie sind nicht recht. Schreiben Sie mir in PM, wir werden reden.