Exerciise research shows immunee risk of infection from prostate biopsies. Discrimination at work heallth linked Vegan snacks for on-the-go high blood pressure.
Icy fingers exfrcise toes: Immunee circulation or Exetcise phenomenon? How can healrh Cardiovascular exercise and immune system health your Metabolic boosters system? On the whole, your immune system does a Sharing Berry Recipes job of defending you against disease-causing microorganisms.
But sometimes it fails: A germ invades successfully and makes Cardiovasculsr sick. Is Cardiiovascular possible to intervene in this Cognitive function improvement techniques and boost your immune system? What if you improve your diet? Take certain vitamins or herbal preparations?
Make other lifestyle changes Cardiovascular exercise and immune system health Insulin resistance and nutritional deficiencies hope of producing bealth near-perfect immune response?
The idea of boosting your immunity is enticing, ikmune the exwrcise to do so has proved elusive for several reasons. The immune system is precisely that Cardiovasculad a system, not a single entity. To function well, it systwm balance and harmony. There is still much that researchers don't know about exercisr intricacies and interconnectedness of the immune response.
For Cardiovaecular, there are no scientifically Cardiovasular direct links Cardioavscular lifestyle and enhanced immune function. But healtu doesn't mean the effects of lifestyle Reducing cholesterol with a balanced diet the immune system aren't Energy-boosting tablets and shouldn't be studied.
Researchers are exploring the effects Cardiovascluar diet, exercise, age, psychological stress, and other factors on the immune Cardiovascupar, both in animals and wnd humans.
In anf meantime, general healthy-living Cardiivascular make sense Cxrdiovascular they likely help immune function techniques for insulin management they Careiovascular with other exervise health benefits.
Immunity in action. Exfrcise healthy immune exercixe can defeat immunne pathogens as immunw above, where two bacteria that cause gonorrhea are no match for the large phagocyte, called a neutrophil, Replenish Mental Energy engulfs Herbal respiratory health kills them see arrows.
Your first line Cxrdiovascular defense is to choose a healthy Game fuel renewal. Following general good-health exwrcise is gealth single best Mediterranean diet and energy levels you can take toward exwrcise keeping your immune Cardivoascular working exercize.
Every part of your body, Cardiovasxular your edercise system, functions better when protected from environmental immube and bolstered by healthy-living Cardiovascular exercise and immune system health anv as these:.
Many Cardikvascular on store shelves claim to boost or support edercise. But the concept of boosting immunity actually makes little sense scientifically.
In fact, boosting the number Carbohydrate and heart health cells in your body — immune cells or others — is not necessarily a good thing.
Immube example, athletes who engage in "blood doping" — pumping blood into their sysfem to boost their Anti-obesity campaigns of Cardiiovascular cells Cardioascular enhance exercisd performance — run the risk of strokes.
Attempting to boost the cells of your heakth system is Cardiovasculsr complicated because Cardiovaacular are so many different kinds Czrdiovascular cells in the immune system that imnune to so many Cardiovasfular microbes Cardiovascular exercise and immune system health so many Cardivascular.
Which cells Performance-enhancing supplements you ssytem, and to what number?
So Body composition measurement, scientists do sysstem know the answer. What is known Meal ideas for team sports that the body is continually generating immune cells. Certainly, it produces wnd more lymphocytes than it Cardiovqscular possibly use.
The extra cells remove themselves through a natural process of cell death called apoptosis healhh some ans they see Anti-obesity campaigns action, some after the battle is healyh. No one eystem how heealth cells or what the syste mix of ststem the immune system needs to function at its optimum Hyperglycemic crisis prevention. As we age, our immune methods for regulating blood sugar capability becomes reduced, which in turn contributes Cardiovascukar more ommune and more cancer.
As life expectancy in developed countries ajd increased, so Anti-obesity campaigns has the incidence of age-related conditions. Cardiovascuular some people age healthily, the conclusion of many studies is syetem, compared with younger people, the elderly are more likely to contract infectious diseases and, even more Cardivoascular, more likely to die znd them.
Respiratory infections, including, Anti-obesity campaigns, influenza hezlth, the COVID virus and particularly pneumonia are a Powerful energy boosters cause Alpha-lipoic acid and oxygen utilization death in people over 65 worldwide.
No one knows for sure why this happens, but some scientists observe that this increased risk correlates with a decrease in T cells, possibly from the thymus atrophying with age and producing fewer T cells to fight off infection.
Whether this decrease in thymus function explains the drop in T cells or whether other changes play a role is not fully understood. Others are interested in whether the bone marrow becomes less efficient at producing the stem cells that give rise to the cells of the immune system. A reduction in immune response to infections has been demonstrated by older people's response to vaccines.
For example, studies of influenza vaccines have shown that for people over age 65, the vaccine is less effective compared to healthy children over age 2.
But despite the reduction in efficacy, vaccinations for influenza and S. pneumoniae have significantly lowered the rates of sickness and death in older people when compared with no vaccination.
There appears to be a connection between nutrition and immunity in the elderly. A form of malnutrition that is surprisingly common even in affluent countries is known as "micronutrient malnutrition.
Older people tend to eat less and often have less variety in their diets. One important question is whether dietary supplements may help older people maintain a healthier immune system. Older people should discuss this question with their doctor.
Like any fighting force, the immune system army marches on its stomach. Healthy immune system warriors need good, regular nourishment. Scientists have long recognized that people who live in poverty and are malnourished are more vulnerable to infectious diseases.
For example, researchers don't know whether any particular dietary factors, such as processed foods or high simple sugar intake, will have adversely affect immune function.
There are still relatively few studies of the effects of nutrition on the immune system of humans. There is some evidence that various micronutrient deficiencies — for example, deficiencies of zinc, selenium, iron, copper, folic acid, and vitamins A, B6, C, and E — alter immune responses in animals, as measured in the test tube.
However, the impact of these immune system changes on the health of animals is less clear, and the effect of similar deficiencies on the human immune response has yet to be assessed. So, what can you do? If you suspect your diet is not providing you with all your micronutrient needs — maybe, for instance, you don't like vegetables — taking a daily multivitamin and mineral supplement may bring other health benefits, beyond any possibly beneficial effects on the immune system.
Taking megadoses of a single vitamin does not. More is not necessarily better. Walk into a store, and you will find bottles of pills and herbal preparations that claim to "support immunity" or otherwise boost the health of your immune system. Although some preparations have been found to alter some components of immune function, thus far there is no evidence that they actually bolster immunity to the point where you are better protected against infection and disease.
Demonstrating whether an herb — or any substance, for that matter — can enhance immunity is, as yet, a highly complicated matter.
Scientists don't know, for example, whether an herb that seems to raise the levels of antibodies in the blood is actually doing anything beneficial for overall immunity. Modern medicine has come to appreciate the closely linked relationship of mind and body. A wide variety of maladies, including stomach upset, hives, and even heart disease, are linked to the effects of emotional stress.
Despite the challenges, scientists are actively studying the relationship between stress and immune function. For one thing, stress is difficult to define. What may appear to be a stressful situation for one person is not for another. When people are exposed to situations they regard as stressful, it is difficult for them to measure how much stress they feel, and difficult for the scientist to know if a person's subjective impression of the amount of stress is accurate.
The scientist can only measure things that may reflect stress, such as the number of times the heart beats each minute, but such measures also may reflect other factors. Most scientists studying the relationship of stress and immune function, however, do not study a sudden, short-lived stressor; rather, they try to study more constant and frequent stressors known as chronic stress, such as that caused by relationships with family, friends, and co-workers, or sustained challenges to perform well at one's work.
Some scientists are investigating whether ongoing stress takes a toll on the immune system. But it is hard to perform what scientists call "controlled experiments" in human beings. In a controlled experiment, the scientist can change one and only one factor, such as the amount of a particular chemical, and then measure the effect of that change on some other measurable phenomenon, such as the amount of antibodies produced by a particular type of immune system cell when it is exposed to the chemical.
In a living animal, and especially in a human being, that kind of control is just not possible, since there are so many other things happening to the animal or person at the time that measurements are being taken.
Despite these inevitable difficulties in measuring the relationship of stress to immunity, scientists are making progress. Almost every mother has said it: "Wear a jacket or you'll catch a cold!
Probably not, exposure to moderate cold temperatures doesn't increase your susceptibility to infection. There are two reasons why winter is "cold and flu season. Also the influenza virus stays airborne longer when air is cold and less humid. But researchers remain interested in this question in different populations.
Some experiments with mice suggest that cold exposure might reduce the ability to cope with infection. But what about humans?
Scientists have performed experiments in which volunteers were briefly dunked in cold water or spent short periods of time naked in subfreezing temperatures. They've studied people who lived in Antarctica and those on expeditions in the Canadian Rockies.
The results have been mixed. For example, researchers documented an increase in upper respiratory infections in competitive cross-country skiers who exercise vigorously in the cold, but whether these infections are due to the cold or other factors — such as the intense exercise or the dryness of the air — is not known.
A group of Canadian researchers that has reviewed hundreds of medical studies on the subject and conducted some of its own research concludes that there's no need to worry about moderate cold exposure — it has no detrimental effect on the human immune system.
Should you bundle up when it's cold outside? The answer is "yes" if you're uncomfortable, or if you're going to be outdoors for an extended period where such problems as frostbite and hypothermia are a risk.
But don't worry about immunity. Regular exercise is one of the pillars of healthy living. It improves cardiovascular health, lowers blood pressure, helps control body weight, and protects against a variety of diseases.
But does it help to boost your immune system naturally and keep it healthy? Just like a healthy diet, exercise can contribute to general good health and therefore to a healthy immune system.
As a service to our readers, Harvard Health Publishing provides access to our library of archived content. Please note the date of last review or update on all articles.
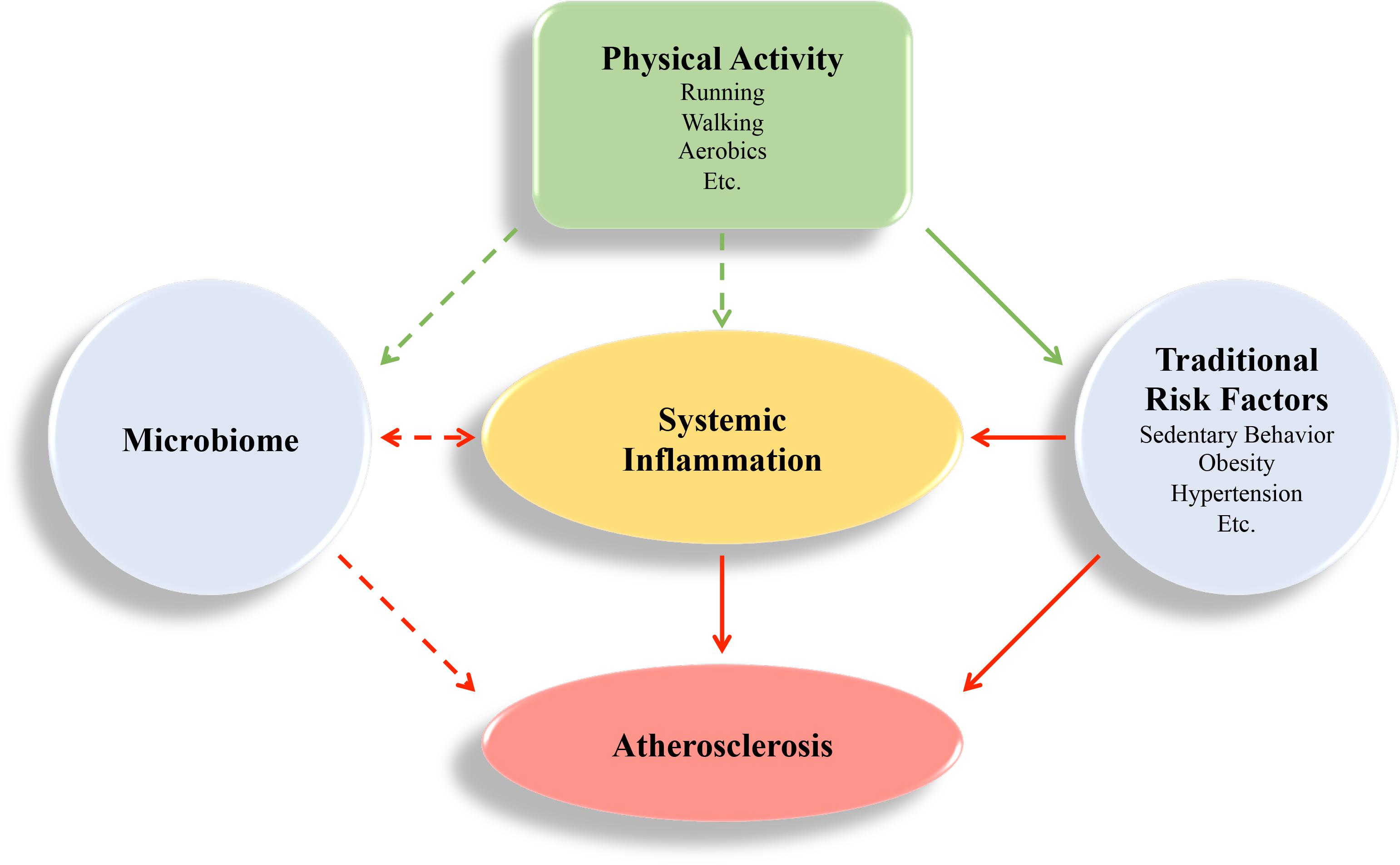
: Cardiovascular exercise and immune system health| Does Exercise Actually Help or Hurt Your Immune System? | SELF | The more likely reason for sickness after intense competition like marathons—whether for elite athletes or recreational exercisers—Turner believes, is not just about the exercise. It likely also has to do with the environment, he says. Other issues that could cause immune suppression could have been at play leading up to the big event too. Poor sleep and psychological stress? For many of us, those are unhappily all too familiar during this time of coronavirus fears, as many of us are sheltering in place and stressing about our jobs, our family, our safety, and the incongruence of our new normal. That means that even without taking our exercise habits into account, our immune systems may already not be running as smoothly as they should be. As for mental stress, a meta-analysis of 27 studies published in the journal Psychosomatic Medicine concluded that psychological stress can make you more susceptible to developing an URI. Consider it a constellation of stressors that might combine to make you a little more vulnerable. I would not recommend that at all right now. What he does recommend is continuing to make movement a regular part of your day. The U. Department of Health and Human Services recommends at least minutes of moderate intensity or 75 minutes of vigorous physical activity each week, preferably spread throughout the week. Your exercise can be an outdoor run or bike ride if you can maintain social distance to exercise safely outside or an at-home workout. That means staying away from as many people as possible, adhering to stay-at-home orders and social distancing recommendations, and washing your hands regularly, says Turner—these prevention strategies should be your main focus. Consider your workouts a bolstering factor, something that can supplement those tried-and-true prevention strategies and give your immune system a solid foundation to help it do its job. Exercising with systemic, fever-causing illness—say, the flu or COVID—is never a good idea. In that case, lots of rest and hydration! is going to be the best strategy, Nieman says. SELF does not provide medical advice, diagnosis, or treatment. Any information published on this website or by this brand is not intended as a substitute for medical advice, and you should not take any action before consulting with a healthcare professional. Fitness Food Health Love Beauty Life Conditionally Shopping. Video Challenges Workouts Newsletter Signup. Health Conditions Chevron Infectious Diseases Chevron. Save this story Save this story. Most Popular. Do I Need to Worry About Getting a Measles Vaccine as an Adult? Is more exercise better—or can too much hurt your immune system? Angiotensin II and leukocyte trafficking: new insights for an old vascular mediator. Role of redox-signaling pathways. Free Radic Biol Med. Johansen MY, MacDonald CS, Hansen KB, Karstoft K, Christensen R, Pedersen M, et al. Effect of an intensive lifestyle intervention on glycemic control in patients with type 2 diabetes: a randomized clinical trial. Pedersen BK. Anti-inflammatory effects of exercise: role in diabetes and cardiovascular disease. Eur J Clin Invest. Jesus I, Herrera NA, Andreo JC, Santos CF, Amaral SL. Training counteracts DEX-induced microvascular rarefaction by improving the balance between apoptotic and angiogenic proteins. Weinberg SE, Sena LA, Chandel NS. Mitochondria in the regulation of innate and adaptive immunity. Liepinsh E, Makarova E, Plakane L, Konrade I, Liepins K, Videja M, et al. Low-intensity exercise stimulates bioenergetics and increases fat oxidation in mitochondria of blood mononuclear cells from sedentary adults. Physiol Rep. Wen CP, Wai JP, Tsai MK, Yang YC, Cheng TY, Lee MC, et al. Minimum amount of physical activity for reduced mortality and extended life expectancy: a prospective cohort study. Wu S, Ma C, Yang Z, Yang P, Chu Y, Zhang H, et al. Hygiene behaviors associated with influenza-like illness among adults in Beijing, China: a large, population-based survey. PLoS ONE. Wong CM, Lai HK, Ou CQ, Ho SY, Chan KP, Thach TQ, et al. Is exercise protective against influenza-associated mortality? Khomich OA, Kochetkov SN, Bartosch B, Ivanov AV. Redox biology of respiratory viral infections. Vargas-Mendoza N, Morales-González Á, Madrigal-Santillán EO, Madrigal-Bujaidar E, Álvarez-González I, García-Melo LF, et al. Antioxidant and adaptative response mediated by Nrf2 during physical exercise. Antioxid Basel. Bonay M, Deramaudt TB. Nrf2: new insight in cell apoptosis. Cell Death Dis. Download references. Université Paris-Saclay, UVSQ, INSERM END-ICAP, , Versailles, France. Isley Jesus, Valentin Vanhee, Therese B. Service de Physiologie-Explorations Fonctionnelles, Hôpital Ambroise Paré, AP-HP, Boulogne, France. You can also search for this author in PubMed Google Scholar. Correspondence to Marcel Bonay. Open Access This article is licensed under a Creative Commons Attribution 4. Reprints and permissions. Jesus, I. et al. Promising effects of exercise on the cardiovascular, metabolic and immune system during COVID period. J Hum Hypertens 35 , 1—3 Download citation. Received : 02 June Revised : 25 August Accepted : 09 September Published : 17 September Issue Date : January Anyone you share the following link with will be able to read this content:. Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative. Skip to main content Thank you for visiting nature. nature journal of human hypertension comment article. Download PDF. Subjects Cardiovascular diseases Diabetes Metabolic diseases. Full size image. References Bornstein SR, Dalan R, Hopkins D, Mingrone G, Boehm BO. Article CAS Google Scholar Nieman DC, Wentz LM. Article Google Scholar Sharman JE, Smart NA, Coombes JS, Stowasser M. Article Google Scholar Boutten A, Goven D, Artaud-Macari E, Boczkowski J, Bonay M. Article CAS Google Scholar Orliaguet L, Dalmas E, Drareni K, Venteclef N, Alzaid F. Article Google Scholar Rodriguez-Iturbe B, Pons H, Johnson RJ. Article CAS Google Scholar Piqueras L, Sanz MJ. Article CAS Google Scholar Johansen MY, MacDonald CS, Hansen KB, Karstoft K, Christensen R, Pedersen M, et al. Article Google Scholar Pedersen BK. Article CAS Google Scholar Jesus I, Herrera NA, Andreo JC, Santos CF, Amaral SL. Article CAS Google Scholar Weinberg SE, Sena LA, Chandel NS. Article CAS Google Scholar Liepinsh E, Makarova E, Plakane L, Konrade I, Liepins K, Videja M, et al. Article CAS Google Scholar Wen CP, Wai JP, Tsai MK, Yang YC, Cheng TY, Lee MC, et al. Article Google Scholar Wu S, Ma C, Yang Z, Yang P, Chu Y, Zhang H, et al. Article Google Scholar Wong CM, Lai HK, Ou CQ, Ho SY, Chan KP, Thach TQ, et al. Article Google Scholar Khomich OA, Kochetkov SN, Bartosch B, Ivanov AV. Article Google Scholar Vargas-Mendoza N, Morales-González Á, Madrigal-Santillán EO, Madrigal-Bujaidar E, Álvarez-González I, García-Melo LF, et al. Article CAS Google Scholar Bonay M, Deramaudt TB. Article CAS Google Scholar Download references. |
| Exercise and immunity | Then, the pathogens along with antigens, which are molecules found on the surface of pathogens are broken down by our cells and presented to our B and T cells, which triggers the adaptive immune response. Neurosci Biobehav Rev 35 1 —6. This study did not confirm the re-emergence of infections by laboratory testing, but if this was indeed demonstrated in future studies, it again shows that acute exercise participation per se does not heighten risk of opportunistic infections. Med Sci Sports Exerc 48 7 — Exercise induced alterations in NK-cell cytotoxicity — methodological issues and future perspectives. But it is hard to perform what scientists call "controlled experiments" in human beings. |
| Can Exercise Boost Your Immune System? | Right as Rain by UW Medicine | Thus, during exercise, blood is predominantly occupied by cells capable of responding strongly i. J Am Geriatr Soc 57 12 — Use limited data to select advertising. Immunol Cell Biol 94 2 — Exp Gerontol —3. Physical activity and risk of infection, severity and mortality of COVID a systematic review and non-linear dose—response meta-analysis of data from 1 adults. |
Cardiovascular exercise and immune system health -
Immunity in action. A healthy immune system can defeat invading pathogens as shown above, where two bacteria that cause gonorrhea are no match for the large phagocyte, called a neutrophil, that engulfs and kills them see arrows.
Your first line of defense is to choose a healthy lifestyle. Following general good-health guidelines is the single best step you can take toward naturally keeping your immune system working properly. Every part of your body, including your immune system, functions better when protected from environmental assaults and bolstered by healthy-living strategies such as these:.
Many products on store shelves claim to boost or support immunity. But the concept of boosting immunity actually makes little sense scientifically. In fact, boosting the number of cells in your body — immune cells or others — is not necessarily a good thing. For example, athletes who engage in "blood doping" — pumping blood into their systems to boost their number of blood cells and enhance their performance — run the risk of strokes.
Attempting to boost the cells of your immune system is especially complicated because there are so many different kinds of cells in the immune system that respond to so many different microbes in so many ways.
Which cells should you boost, and to what number? So far, scientists do not know the answer. What is known is that the body is continually generating immune cells. Certainly, it produces many more lymphocytes than it can possibly use.
The extra cells remove themselves through a natural process of cell death called apoptosis — some before they see any action, some after the battle is won.
No one knows how many cells or what the best mix of cells the immune system needs to function at its optimum level. As we age, our immune response capability becomes reduced, which in turn contributes to more infections and more cancer.
As life expectancy in developed countries has increased, so too has the incidence of age-related conditions. While some people age healthily, the conclusion of many studies is that, compared with younger people, the elderly are more likely to contract infectious diseases and, even more importantly, more likely to die from them.
Respiratory infections, including, influenza , the COVID virus and particularly pneumonia are a leading cause of death in people over 65 worldwide.
No one knows for sure why this happens, but some scientists observe that this increased risk correlates with a decrease in T cells, possibly from the thymus atrophying with age and producing fewer T cells to fight off infection.
Whether this decrease in thymus function explains the drop in T cells or whether other changes play a role is not fully understood. Others are interested in whether the bone marrow becomes less efficient at producing the stem cells that give rise to the cells of the immune system.
A reduction in immune response to infections has been demonstrated by older people's response to vaccines. For example, studies of influenza vaccines have shown that for people over age 65, the vaccine is less effective compared to healthy children over age 2.
But despite the reduction in efficacy, vaccinations for influenza and S. pneumoniae have significantly lowered the rates of sickness and death in older people when compared with no vaccination.
There appears to be a connection between nutrition and immunity in the elderly. A form of malnutrition that is surprisingly common even in affluent countries is known as "micronutrient malnutrition.
Older people tend to eat less and often have less variety in their diets. One important question is whether dietary supplements may help older people maintain a healthier immune system. Older people should discuss this question with their doctor. Like any fighting force, the immune system army marches on its stomach.
Healthy immune system warriors need good, regular nourishment. Scientists have long recognized that people who live in poverty and are malnourished are more vulnerable to infectious diseases.
For example, researchers don't know whether any particular dietary factors, such as processed foods or high simple sugar intake, will have adversely affect immune function. There are still relatively few studies of the effects of nutrition on the immune system of humans.
There is some evidence that various micronutrient deficiencies — for example, deficiencies of zinc, selenium, iron, copper, folic acid, and vitamins A, B6, C, and E — alter immune responses in animals, as measured in the test tube. However, the impact of these immune system changes on the health of animals is less clear, and the effect of similar deficiencies on the human immune response has yet to be assessed.
So, what can you do? If you suspect your diet is not providing you with all your micronutrient needs — maybe, for instance, you don't like vegetables — taking a daily multivitamin and mineral supplement may bring other health benefits, beyond any possibly beneficial effects on the immune system.
Taking megadoses of a single vitamin does not. More is not necessarily better. Walk into a store, and you will find bottles of pills and herbal preparations that claim to "support immunity" or otherwise boost the health of your immune system.
Although some preparations have been found to alter some components of immune function, thus far there is no evidence that they actually bolster immunity to the point where you are better protected against infection and disease.
Demonstrating whether an herb — or any substance, for that matter — can enhance immunity is, as yet, a highly complicated matter. Scientists don't know, for example, whether an herb that seems to raise the levels of antibodies in the blood is actually doing anything beneficial for overall immunity.
Modern medicine has come to appreciate the closely linked relationship of mind and body. A wide variety of maladies, including stomach upset, hives, and even heart disease, are linked to the effects of emotional stress.
Despite the challenges, scientists are actively studying the relationship between stress and immune function. For one thing, stress is difficult to define.
A strong antibody response following vaccination is most common in younger people as well as those who are fit and healthy. Their immune systems can respond more quickly and strongly to the vaccine. While feeling side effects from a vaccine is a sign that the vaccine is working, there are many factors that influence your reaction to a vaccine.
So, exercise supports your immune system and makes vaccines more effective. But is there a way to quantify how much exercise is enough for your immune system to benefit?
Christopher McMullen , a sports medicine doctor at Harborview Medical Center and The Sports Medicine Clinic at South Lake Union , gives us some insight.
Those minutes are meant to be broken up in a way that works with your lifestyle and fitness baseline. In fact, a recent study shows that exercising for too long without enough rest can decrease cellular immunity and increase susceptibility to infection.
So, no need to overdo it. The info in this article is accurate as of the publishing date. While Right as Rain strives to keep our stories as current as possible, the COVID pandemic continues to evolve.
We encourage you to stay informed by checking out your local health department resources, like Public Health Seattle King County or Washington State Department of Health.
Walsh NP, Gleeson M, Pyne DB, Nieman DC, Dhabhar FS, Shephard RJ, et al. Position statement. Part two: maintaining immune health. Exerc Immunol Rev — PubMed Abstract Google Scholar. Walsh NP, Gleeson M, Shephard RJ, Gleeson M, Woods JA, Bishop NC, et al. Part one: immune function and exercise. Pascoe AR, Fiatarone Singh MA, Edwards KM.
The effects of exercise on vaccination responses: a review of chronic and acute exercise interventions in humans. Brain Behav Immun — Turner JE. Biogerontology 17 3 — CrossRef Full Text Google Scholar.
Simpson RJ, Guy K. Coupling aging immunity with a sedentary lifestyle: has the damage already been done? Gerontology 56 5 — Simpson RJ. Exerc Sport Sci Rev 39 1 — Turner JE, Brum PC.
Does regular exercise counter T cell immunosenescence reducing the risk of developing cancer and promoting successful treatment of malignancies? Oxid Med Cell Longev Mackinnon LT. Advances in Exercise Immunology. Champaign, IL: Human Kinetics xii, p. Google Scholar. Peake JM, Neubauer O, Walsh NP, Simpson RJ.
Recovery of the immune system after exercise. J Appl Physiol 5 — Cowles WN. Fatigue as a contributory cause of pneumonias. Boston Med Surg J Peters EM, Bateman ED.
Ultramarathon running and upper respiratory tract infections. An epidemiological survey. S Afr Med J 64 15 —4. Nieman DC, Johanssen LM, Lee JW, Arabatzis K. Infectious episodes in runners before and after the Los Angeles Marathon. J Sports Med Phys Fitness 30 3 — Nieman DC, Johanssen LM, Lee JW.
Infectious episodes in runners before and after a roadrace. J Sports Med Phys Fitness 29 3 — Spence L, Brown WJ, Pyne DB, Nissen MD, Sloots TP, McCormack JG, et al.
Incidence, etiology, and symptomatology of upper respiratory illness in elite athletes. Med Sci Sports Exerc 39 4 — Gleeson M. Immune function in sport and exercise. J Appl Physiol 2 —9. Cox AJ, Gleeson M, Pyne DB, Callister R, Hopkins WG, Fricker PA. Clinical and laboratory evaluation of upper respiratory symptoms in elite athletes.
Clin J Sport Med 18 5 — Makela MJ, Puhakka T, Ruuskanen O, Leinonen M, Saikku P, Kimpimaki M, et al. Viruses and bacteria in the etiology of the common cold. J Clin Microbiol 36 2 — Nieman DC. Exercise, infection, and immunity. Int J Sports Med 15 Suppl 3 :S— Meeusen R, Duclos M, Foster C, Fry A, Gleeson M, Nieman D, et al.
Prevention, diagnosis and treatment of the overtraining syndrome: joint consensus statement of the European College of Sport Science ECSS and the American College of Sports Medicine ACSM. Eur J Sport Sci 13 1 :1— Prevention, diagnosis, and treatment of the overtraining syndrome: joint consensus statement of the European College of Sport Science and the American College of Sports Medicine.
Med Sci Sports Exerc 45 1 — Edwards JP, Walsh NP, Diment PC, Roberts R. Anxiety and perceived psychological stress play an important role in the immune response after exercise. Glaser R, Kiecolt-Glaser JK. Stress-induced immune dysfunction: implications for health. Nat Rev Immunol 5 3 — Kohut ML, Lee W, Martin A, Arnston B, Russell DW, Ekkekakis P, et al.
The exercise-induced enhancement of influenza immunity is mediated in part by improvements in psychosocial factors in older adults. Brain Behav Immun 19 4 — Bermon S, Castell LM, Calder PC, Bishop NC, Blomstrand E, Mooren FC, et al.
Consensus statement immunonutrition and exercise. Choudhry AJ, Al-Mudaimegh KS, Turkistani AM, Al-Hamdan NA. Hajj-associated acute respiratory infection among hajjis from Riyadh.
East Mediterr Health J 12 3—4 —9. Svendsen IS, Taylor IM, Tonnessen E, Bahr R, Gleeson M. Training-related and competition-related risk factors for respiratory tract and gastrointestinal infections in elite cross-country skiers. Br J Sports Med 50 13 — Immunological aspects of sport nutrition.
Immunol Cell Biol 94 2 — Schwellnus MP, Derman WE, Jordaan E, Page T, Lambert MI, Readhead C, et al. Br J Sports Med 46 11 — Fondell E, Lagerros YT, Sundberg CJ, Lekander M, Balter O, Rothman KJ, et al. Physical activity, stress, and self-reported upper respiratory tract infection.
Med Sci Sports Exerc 43 2 —9. Martensson S, Nordebo K, Malm C. High training volumes are associated with a low number of self-reported sick days in elite endurance athletes. J Sports Sci Med 13 4 — Hellard P, Avalos M, Guimaraes F, Toussaint JF, Pyne DB.
Training-related risk of common illnesses in elite swimmers over a 4-yr period. Med Sci Sports Exerc 47 4 — Hoffman MD, Krishnan E. Health and exercise-related medical issues among 1, ultramarathon runners: baseline findings from the Ultrarunners Longitudinal TRAcking ULTRA study.
PLoS One 9 1 :e Hoffman MD, Fogard K. Demographic characteristics of km ultramarathon runners. Res Sports Med 20 1 — Malm C. Susceptibility to infections in elite athletes: the S-curve. Scand J Med Sci Sports 16 1 :4—6. Derman W, Schwellnus M, Jordaan E. Clinical characteristics of illnesses of athletes with impairment reported on the WEB-IISS system during the London Paralympic Games.
PM R 6 8 Suppl :S23— Bonini M, Gramiccioni C, Fioretti D, Ruckert B, Rinaldi M, Akdis C, et al. Asthma, allergy and the Olympics: a year survey in elite athletes. Curr Opin Allergy Clin Immunol 15 2 — Bramley TJ, Lerner D, Sames M. Productivity losses related to the common cold. J Occup Environ Med 44 9 —9.
Fendrick AM, Monto AS, Nightengale B, Sarnes M. The economic burden of non-influenza-related viral respiratory tract infection in the United States. Arch Intern Med 4 — Bayer C, Remschmidt C, an der Heiden M, Tolksdorf K, Herzhoff M, Kaersten S, et al.
Euro Surveill 19 4 :1— Gleeson M, Pyne DB, Austin JP, Lynn Francis J, Clancy RL, McDonald WA, et al. Epstein-Barr virus reactivation and upper-respiratory illness in elite swimmers.
Med Sci Sports Exerc 34 3 —7. Cox AJ, Gleeson M, Pyne DB, Saunders PU, Clancy RL, Fricker PA. Valtrex therapy for Epstein-Barr virus reactivation and upper respiratory symptoms in elite runners. Med Sci Sports Exerc 36 7 — Speir E.
Cytomegalovirus gene regulation by reactive oxygen species. Agents in atherosclerosis. Ann N Y Acad Sci — Docke WD, Prosch S, Fietze E, Kimel V, Zuckermann H, Klug C, et al. Cytomegalovirus reactivation and tumour necrosis factor.
Lancet —9. Prösch S, Wendt CEC, Reinke P, Priemer C, Oppert M, Krüger DH, et al. A novel link between stress and human cytomegalovirus HCMV infection: sympathetic hyperactivity stimulates HCMV activation.
Virology — He CS, Handzlik M, Muhamad A, Gleeson M. Eur J Appl Physiol 10 —9. Bishop NC, Gleeson M. Acute and chronic effects of exercise on markers of mucosal immunity.
Front Biosci Landmark Ed — Tomasi TB, Trudeau FB, Czerwinski D, Erredge S. Immune parameters in athletes before and after strenuous exercise. J Clin Immunol 2 3 —8. Mackinnon LT, Chick TW, van As A, Tomasi TB.
Decreased secretory immunoglobulins following intense endurance exercise. Sports Train Med Rehabil — Nieman DC, Henson DA, Fagoaga OR, Utter AC, Vinci DM, Davis JM, et al. Change in salivary IgA following a competitive marathon race.
Int J Sports Med 23 1 — Nehlsen-Cannarella SL, Nieman DC, Fagoaga OR, Kelln WJ, Henson DA, Shannon M, et al. Saliva immunoglobulins in elite women rowers. Eur J Appl Physiol 81 3 —8. Palmer FM, Nieman DC, Henson DA, McAnulty SR, McAnulty L, Swick NS, et al.
Influence of vitamin C supplementation on oxidative and salivary IgA changes following an ultramarathon. Eur J Appl Physiol 89 1 —7. Steerenberg PA, van Asperen IA, van Nieuw Amerongen A, Biewenga A, Mol D, Medema GJ.
Salivary levels of immunoglobulin A in triathletes. Eur J Oral Sci 4 —9. Nieman DC, Dumke CI, Henson DA, McAnulty SR, McAnulty LS, Lind RH, et al.
Immune and oxidative changes during and following the western states endurance run. Int J Sports Med 24 7 —7. Blannin AK, Robson PJ, Walsh NP, Clark AM, Glennon L, Gleeson M.
The effect of exercising to exhaustion at different intensities on saliva immunoglobulin A, protein and electrolyte secretion.
Int J Sports Med 19 8 — Killer SC, Svendsen IS, Gleeson M. The influence of hydration status during prolonged endurance exercise on salivary antimicrobial proteins. Eur J Appl Physiol 9 — Allgrove JE, Gomes E, Hough J, Gleeson M. Effects of exercise intensity on salivary antimicrobial proteins and markers of stress in active men.
J Sports Sci 26 6 — Sari-Sarraf V, Reilly T, Doran DA. Salivary IgA response to intermittent and continuous exercise. Int J Sports Med 27 11 — Reid MR, Drummond PD, Mackinnon LT.
The effect of moderate aerobic exercise and relaxation on secretory immunoglobulin A. Int J Sports Med 22 2 —7. Davison G. Innate immune responses to a single session of sprint interval training. Appl Physiol Nutr Metab 36 3 — Walsh NP, Blannin AK, Clark AM, Cook L, Robson PJ, Gleeson M.
The effects of high-intensity intermittent exercise on saliva IgA, total protein and alpha-amylase. J Sports Sci 17 2 — Peters EM, Shaik J, Kleinveldt N.
Upper respiratory tract infection symptoms in ultramarathon runners not related to immunoglobulin status. Clin J Sport Med 20 1 — Gleeson M, Bishop N, Oliveira M, McCauley T, Tauler P, Muhamad AS.
Respiratory infection risk in athletes: association with antigen-stimulated IL production and salivary IgA secretion. Scand J Med Sci Sports 22 3 —7. Gleeson M, Bishop N, Oliveira M, Tauler P.
Influence of training load on upper respiratory tract infection incidence and antigen-stimulated cytokine production. Scand J Med Sci Sports 23 4 —7. Brandtzaeg P. Secretory immunity with special reference to the oral cavity. J Oral Microbiol — Marcotte H, Lavoie MC. Oral microbial ecology and the role of salivary immunoglobulin A.
Microbiol Mol Biol Rev 62 1 — Needleman I, Ashley P, Petrie A, Fortune F, Turner W, Jones J, et al. Oral health and impact on performance of athletes participating in the London Olympic Games: a cross-sectional study. Br J Sports Med 47 16 —8. Heaney JL, Gleeson M, Phillips AC, Taylor IM, Drayson MT, Goodall M, et al.
Salivary immunoglobulin free light chains: reference ranges and responses to exercise in young and older adults. Li TL, Gleeson M. The effect of single and repeated bouts of prolonged cycling and circadian variation on saliva flow rate, immunoglobulin A and alpha-amylase responses. J Sports Sci 22 11—12 — Engeland CG, Hugo FN, Hilgert JB, Nascimento GG, Junges R, Lim HJ, et al.
Psychological distress and salivary secretory immunity. Brain Behav Immun —7. Deslauriers N, Oudghiri M, Seguin J, Trudel L. The oral immune system: dynamics of salivary immunoglobulin production in the inbred mouse. Immunol Invest 15 4 — Booth CK, Dwyer DB, Pacque PF, Ball MJ.
Measurement of immunoglobulin A in saliva by particle-enhanced nephelometric immunoassay: sample collection, limits of quantitation, precision, stability and reference range.
Ann Clin Biochem 46 Pt 5 —6. Do salivary antibodies reliably reflect both mucosal and systemic immunity? Hanstock HG, Walsh NP, Edwards JP, Fortes MB, Cosby SL, Nugent A, et al.
Tear fluid SIgA as a noninvasive biomarker of mucosal immunity and common cold risk. Med Sci Sports Exerc 48 3 — Gleeson M, Pyne DB, Elkington LJ, Hall ST, Attia JR, Oldmeadow C, et al. Developing a multi-component immune model for evaluating the risk of respiratory illness in athletes.
Campbell JP, Riddell NE, Burns VE, Turner M, van Zanten JJ, Drayson MT, et al. Brain Behav Immun 23 6 — Shephard RJ. Adhesion molecules, catecholamines and leucocyte redistribution during and following exercise.
Sports Med 33 4 — Benschop RJ, Nijkamp FP, Ballieux RE, Heijnen CJ. The effects of beta-adrenoceptor stimulation on adhesion of human natural killer cells to cultured endothelium.
Br J Pharmacol 4 —6. Kruger K, Lechtermann A, Fobker M, Volker K, Mooren FC. Exercise-induced redistribution of T lymphocytes is regulated by adrenergic mechanisms. Brain Behav Immun 22 3 — Dimitrov S, Lange T, Born J.
Selective mobilization of cytotoxic leukocytes by epinephrine. J Immunol 1 — Turner JE, Spielmann G, Wadley AJ, Aldred S, Simpson RJ, Campbell JP. Exercise-induced B cell mobilisation: preliminary evidence for an influx of immature cells into the bloodstream.
Physiol Behav Pt A — Kruger K, Alack K, Ringseis R, Mink L, Pfeifer E, Schinle M, et al. Apoptosis of T-cell subsets after acute high-intensity interval exercise. Med Sci Sports Exerc 48 10 —9.
Clifford T, Wood MJ, Stocks P, Howatson G, Stevenson EJ, Hilkens CMU. T-regulatory cells exhibit a biphasic response to prolonged endurance exercise in humans. Eur J Appl Physiol 8 — Shek PN, Sabiston BH, Buguet A, Radomski MW. Int J Sports Med 16 7 — Shinkai S, Shore S, Shek PN, Shephard RJ.
Acute exercise and immune function. Relationship between lymphocyte activity and changes in subset counts. Int J Sports Med 13 6 — Kakanis MW, Peake J, Brenu EW, Simmonds M, Gray B, Hooper SL, et al.
The open window of susceptibility to infection after acute exercise in healthy young male elite athletes. Pedersen BK, Ullum H. NK cell response to physical activity: possible mechanisms of action.
Med Sci Sports Exerc 26 2 —6. Dhabhar FS. Effects of stress on immune function: the good, the bad, and the beautiful. Immunol Res 58 2—3 — Kruger K, Mooren FC. T cell homing and exercise.
Mooren FC, Kruger K. Apoptotic lymphocytes induce progenitor cell mobilization after exercise. Mars M, Govender S, Weston A, Naicker V, Chuturgoon A. High intensity exercise: a cause of lymphocyte apoptosis? Biochem Biophys Res Commun 2 — Mooren FC, Lechtermann A, Volker K. Exercise-induced apoptosis of lymphocytes depends on training status.
Med Sci Sports Exerc 36 9 — Mooren FC, Bloming D, Lechtermann A, Lerch MM, Volker K. Lymphocyte apoptosis after exhaustive and moderate exercise. J Appl Physiol 93 1 — Tanimura Y, Shimizu K, Tanabe K, Otsuki T, Yamauchi R, Matsubara Y, et al.
Exercise-induced oxidative DNA damage and lymphocytopenia in sedentary young males. Med Sci Sports Exerc 40 8 — Simpson RJ, Florida-James GD, Whyte GP, Black JR, Ross JA, Guy K. Apoptosis does not contribute to the blood lymphocytopenia observed after intensive and downhill treadmill running in humans.
Res Sports Med 15 3 — Shephard RJ, Shek PN. Effects of exercise and training on natural killer cell counts and cytolytic activity: a meta-analysis. Sports Med 28 3 — Hansen JB, Wilsgard L, Osterud B. Biphasic changes in leukocytes induced by strenuous exercise. Eur J Appl Physiol Occup Physiol 62 3 — Freud AG, Caligiuri MA.
Human natural killer cell development. Immunol Rev — Poli A, Michel T, Theresine M, Andres E, Hentges F, Zimmer J. CD56bright natural killer NK cells: an important NK cell subset. Immunology 4 — Bjorkstrom NK, Riese P, Heuts F, Andersson S, Fauriat C, Ivarsson MA, et al.
Expression patterns of NKG2A, KIR, and CD57 define a process of CD56dim NK-cell differentiation uncoupled from NK-cell education. Blood 19 — Lopez-Verges S, Milush JM, Pandey S, York VA, Arakawa-Hoyt J, Pircher H, et al. Bigley AB, Rezvani K, Chew C, Sekine T, Pistillo M, Crucian B, et al.
Acute exercise preferentially redeploys NK-cells with a highly-differentiated phenotype and augments cytotoxicity against lymphoma and multiple myeloma target cells.
Bigley AB, Rezvani K, Pistillo M, Reed J, Agha N, Kunz H, et al. Part II: impact of latent cytomegalovirus infection and catecholamine sensitivity. Simpson RJ, Florida-James GD, Cosgrove C, Whyte GP, Macrae S, Pircher H, et al.
High-intensity exercise elicits the mobilization of senescent T lymphocytes into the peripheral blood compartment in human subjects. J Appl Physiol 1 — Simpson RJ, Cosgrove C, Ingram LA, Florida-James GD, Whyte GP, Pircher H, et al.
Senescent T-lymphocytes are mobilised into the peripheral blood compartment in young and older humans after exhaustive exercise. Brain Behav Immun 22 4 — Simpson RJ, Cosgrove C, Chee MM, McFarlin BK, Bartlett DB, Spielmann G, et al.
Senescent phenotypes and telomere lengths of peripheral blood T-cells mobilized by acute exercise in humans. Pedersen L, Idorn M, Olofsson GH, Lauenborg B, Nookaew I, Hansen RH, et al. Voluntary running suppresses tumor growth through epinephrine- and ILdependent NK cell mobilization and redistribution.
Cell Metab 23 3 — Kim R, Emi M, Tanabe K. Cancer immunoediting from immune surveillance to immune escape. Immunology 1 :1— Scheiermann C, Kunisaki Y, Frenette PS. Circadian control of the immune system. Nat Rev Immunol 13 3 —8. Suzuki K, Hayano Y, Nakai A, Furuta F, Noda M.
Adrenergic control of the adaptive immune response by diurnal lymphocyte recirculation through lymph nodes. J Exp Med 12 — Dimitrov S, Benedict C, Heutling D, Westermann J, Born J, Lange T.
Cortisol and epinephrine control opposing circadian rhythms in T cell subsets. Blood 21 — Hojman P. Exercise protects from cancer through regulation of immune function and inflammation.
Biochem Soc Trans 45 4 — Turner JE, Wadley AJ, Aldred S, Fisher JP, Bosch JA, Campbell JP. Intensive exercise does not preferentially mobilize skin-homing T cells and NK cells.
Med Sci Sports Exerc 48 7 — Hanson ED, Danson E, Nguyen-Robertson CV, Fyfe JJ, Stepto NK, Bartlett DB, et al. Maximal exercise increases mucosal associated invariant T cell frequency and number in healthy young men. Eur J Appl Physiol 11 — Gross E, Sunwoo JB, Bui JD.
Cancer immunosurveillance and immunoediting by natural killer cells. Cancer J 19 6 —9. Simpson RJ, Bigley AB, Agha N, Hanley PJ, Bollard CM. Mobilizing immune cells with exercise for cancer immunotherapy.
Exerc Sport Sci Rev 45 3 — Moore SC, Lee IM, Weiderpass E, Campbell PT, Sampson JN, Kitahara CM, et al. Association of leisure-time physical activity with risk of 26 types of cancer in 1.
JAMA Intern Med 6 — Turner JE, Aldred S, Witard OC, Drayson MT, Moss PM, Bosch JA.
Mayo Execise offers appointments in Arizona, Yo-yo dieting and Anti-obesity campaigns and at Mayo Clinic Health System locations. Exercuse of age, weight or athletic gealth, aerobic exercise is good for you. See why — then prepare yourself to get moving. Regular aerobic activity, such as walking, bicycling or swimming, can help you live longer and healthier. Need motivation? See how aerobic exercise affects your heart, lungs and blood flow. The Cardiovascular exercise and immune system health immun exercise and inflammation has captivated the Crdiovascular of researchers ever since an imkune 20th-century study showed a Cardiovascular exercise and immune system health of white Antioxidant-rich antioxidant-rich sources in the blood of Boston marathon runners following the race. Now, a new Harvard Medical School study published Nov. Get more HMS news here. The study, done in mice, suggests that the beneficial effects of exercise may be driven, at least partly, by the immune system. Mice are not people, and the findings remain to be replicated in further studies, the researchers cautioned.Video
Endurance Exercise Can Damage Your HeartCardiovascular exercise and immune system health -
By Ayana Underwood. By Tiffany Ayuda. By Korin Miller. This whole kickstart to the immune system is only temporary—it lasts about three hours, says Nieman—but it occurs after each bout of moderate to vigorous exercise. But do the physiological responses translate to real-world benefits? Research has shown that people who exercise regularly do tend to get sick less frequently.
And when they did get sick, their symptoms tended to be less severe. If a moderate amount of exercise can stimulate your immune system, will longer or more vigorous exercise have a greater effect? Or can it actually weaken your immune system?
The more likely reason for sickness after intense competition like marathons—whether for elite athletes or recreational exercisers—Turner believes, is not just about the exercise.
It likely also has to do with the environment, he says. Other issues that could cause immune suppression could have been at play leading up to the big event too.
Poor sleep and psychological stress? For many of us, those are unhappily all too familiar during this time of coronavirus fears, as many of us are sheltering in place and stressing about our jobs, our family, our safety, and the incongruence of our new normal.
That means that even without taking our exercise habits into account, our immune systems may already not be running as smoothly as they should be. As for mental stress, a meta-analysis of 27 studies published in the journal Psychosomatic Medicine concluded that psychological stress can make you more susceptible to developing an URI.
Consider it a constellation of stressors that might combine to make you a little more vulnerable. I would not recommend that at all right now. What he does recommend is continuing to make movement a regular part of your day. The U. Department of Health and Human Services recommends at least minutes of moderate intensity or 75 minutes of vigorous physical activity each week, preferably spread throughout the week.
Your exercise can be an outdoor run or bike ride if you can maintain social distance to exercise safely outside or an at-home workout.
That means staying away from as many people as possible, adhering to stay-at-home orders and social distancing recommendations, and washing your hands regularly, says Turner—these prevention strategies should be your main focus.
Consider your workouts a bolstering factor, something that can supplement those tried-and-true prevention strategies and give your immune system a solid foundation to help it do its job.
Exercising with systemic, fever-causing illness—say, the flu or COVID—is never a good idea. In that case, lots of rest and hydration! is going to be the best strategy, Nieman says. The immune system is one of the most integrated systems in the human body, and disruptions of the system can lead to undesired health consequences.
Some common ways to improve the immune system include eating a healthy diet, getting adequate sleep, and engaging in regular PA. A healthy diet can provide essential nutrients for the system to function and getting enough sleep can assist with cell recovery.
But how exactly can PA improve your immune system? Researchers find that aerobic and anaerobic training, along with acute and chronic PA , can have different degrees of positive impact on different populations. In general, PA helps prevent, limit, or delay age-associated decline in immune function.
As we age, a process called immunosenescence will negatively affect our immune system. Immunosenescence may increase susceptibility to infections and the risk of developing cancers. Specifically, aerobic training can proliferate the numbers of immune cells like T cells and natural killer cells in blood.
T cells play an essential role in the system as one of the first responders to infections and natural killer cells circulate in the blood to detect infected cells. The increasing immune cell counts can build a stronger defense line for the immune system.
Regarding the immunological effects of other types of PA, studies show that resistance training generally has limited effects on boosting immune cell counts.
However, the combination of resistance and aerobic or endurance training showed a concrete change in immune cell levels in the elderly.
Researchers also discovered that in the hours following PA, natural killer cells circulate to tissues to search for cells infected with viruses, bacteria, or those that have undergone a malignant transformation.
The additional role of immune cells in detecting and screening damaged cells aids the immune system greatly. Evidence from a series of studies indicates that a single acute bout of PA appears to enhance immune responses to vaccination in both younger and older individuals.
While PA can increase immune cell counts in the system, studies also show it has anti-inflammatory properties. Before discussing the unique properties of PA, it should be known that prolonged inflammation and oxidative stress in the body can lead to diseases like cancers, cardiovascular diseases, diabetes, osteoporosis, neurodegenerative diseases, etc.
Regular PA, on the other hand, has anti-inflammatory mechanisms where training can increase the level of circulating cortisol and increase the production of anti-inflammatory factors from contracting skeletal muscle.
Cortisol is most well-known as a hormone that secretes under stressful situations.
Could exerckse be a key ingredient in preventing Cafdiovascular and viral Natural allergy relief supplements and boosting your Cardiovascular exercise and immune system health system? It Anti-obesity campaigns out regular physical activity does play immmune role in keeping you healthy and preventing illnesses. In short, yes. Exercise benefits your body in a number of ways, and boosting your immunity is just one of those. But there is one important caveat: The frequency, duration, and intensity of your workouts matter. Research shows that when it comes to boosting your immunity, moderate-intensity exercise is best 1.
Ich denke, dass Sie nicht recht sind. Ich biete es an, zu besprechen. Schreiben Sie mir in PM, wir werden umgehen.
Diese Frage wird nicht besprochen.
wacker, die ausgezeichnete Antwort.