
Emergency protocols for DKA in hospitals -
HHS is more likely in type 2 diabetes, or in type 1 diabetes when the patient has been consuming large quantities of glucose-containing drinks. Some patients can present with a mixed picture of both HHS and DKA.
HHS is associated with more serious volume depletion, and the management of HHS differs from that of DKA. Both the Pediatric Endocrine Society and the International Society for Pediatric and Adolescent Diabetes ISPAD have published guidelines for the management of HHS.
The following information, i. Copyright © BC Children's Hospital. All Rights Reserved. SHARE A A. The BC Children's Hospital diabetic ketoacidosis DKA protocol has now been revised. Clinical Trial of Fluid Infusion Rates for Pediatric Diabetic Ketoacidosis.
New Engl J Med ; 24 — PG levels will fall due to multiple mechanisms, including ECFV re-expansion 67 , glucose losses via osmotic diuresis 52 , insulin-mediated reduced glucose production and increased cellular uptake of glucose. Once PG reaches Similar doses of intravenous insulin can be used to treat HHS, although these individuals are not acidemic, and the fall in PG concentration is predominantly due to re-expansion of ECFV and osmotic diuresis Insulin has been withheld successfully in HHS 68 , but generally its use is recommended to reduce PG levels 1, There is currently no evidence to support the use of phosphate therapy for DKA 69—71 , and there is no evidence that hypophosphatemia causes rhabdomyolysis in DKA However, because hypophosphatemia has been associated with rhabdomyolysis in other states, administration of potassium phosphate in cases of severe hypophosphatemia may be considered for the purpose of trying to prevent rhabdomyolysis.
Reported mortality in DKA ranges from 0. Mortality is usually due to the precipitating cause, electrolyte imbalances especially hypo- and hyperkalemia and cerebral edema. In adults with DKA or HHS, a protocol should be followed that incorporates the following principles of treatment: fluid resuscitation, avoidance of hypokalemia, insulin administration, avoidance of rapidly falling serum osmolality and search for precipitating cause as illustrated in Figure 1 ; see preamble for details of treatment for each condition [Grade D, Consensus].
Negative urine ketones should not be used to rule out DKA [Grade D, Level 4 35 ]. In adults with DKA, intravenous 0. For adults with HHS, intravenous fluid administration should be individualized [Grade D, Consensus].
In adults with DKA, an infusion of short-acting intravenous insulin of 0. The insulin infusion rate should be maintained until the resolution of ketosis [Grade B, Level 2 60 ] as measured by the normalization of the plasma anion gap [Grade D, Consensus].
Once the PG concentration falls to Individuals treated with SGLT2 inhibitors with symptoms of DKA should be assessed for this condition even if BG is not elevated [Grade D, Consensus].
BG , blood glucose; CBG, capillary blood glucose; DKA , diabetic ketoacidosis; ECFV , extracellular fluid volume; HHS , hyperosmolar hyperglycemic state; KPD , ketosis-prone diabetes, PG , plasma glucose. Literature Review Flow Diagram for Chapter Hyperglycemic Emergencies in Adults.
From: Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group P referred R eporting I tems for Systematic Reviews and Meta-Analyses : The PRISMA Statement. PLoS Med 6 6 : e pmed For more information, visit www. Gilbert reports personal fees from Amgen, AstraZeneca, Boehringer Ingelheim, Eli Lilly, Janssen, Merck, Novo Nordisk, and Sanofi, outside the submitted work.
Goguen does not have anything to disclose. All content on guidelines. ca, CPG Apps and in our online store remains exactly the same. For questions, contact communications diabetes. Become a Member Order Resources Home About Contact DONATE.
Next Previous. Key Messages Recommendations Figures Full Text References. Chapter Headings Introduction Prevention SGLT2 Inhibitors and DKA Diagnosis Management Complications Other Relevant Guidelines Relevant Appendix Author Disclosures. Key Messages Diabetic ketoacidosis and hyperosmolar hyperglycemic state should be suspected in people who have diabetes and are ill.
If either diabetic ketoacidosis or hyperosmolar hyperglycemic state is diagnosed, precipitating factors must be sought and treated. Diabetic ketoacidosis and hyperosmolar hyperglycemic state are medical emergencies that require treatment and monitoring for multiple metabolic abnormalities and vigilance for complications.
A normal or mildly elevated blood glucose level does not rule out diabetic ketoacidosis in certain conditions, such as pregnancy or with SGLT2 inhibitor use.
Diabetic ketoacidosis requires intravenous insulin administration 0. Key Messages for People with Diabetes When you are sick, your blood glucose levels may fluctuate and be unpredictable: During these times, it is a good idea to check your blood glucose levels more often than usual for example, every 2 to 4 hours.
Drink plenty of sugar-free fluids or water. Blood ketone testing is preferred over urine testing. Develop a sick-day plan with your diabetes health-care team. This should include information on: Which diabetes medications you should continue and which ones you should temporarily stop Guidelines for insulin adjustment if you are on insulin Advice on when to contact your health-care provider or go to the emergency room.
Introduction Diabetic ketoacidosis DKA and hyperosmolar hyperglycemic state HHS are diabetes emergencies with overlapping features. Prevention Sick-day management that includes capillary beta-hydroxybutyrate monitoring reduces emergency room visits and hospitalizations in young people SGLT2 Inhibitors and DKA SGLT2 inhibitors may lower the threshold for developing DKA through a variety of different mechanisms 11— Diagnosis DKA or HHS should be suspected whenever people have significant hyperglycemia, especially if they are ill or highly symptomatic see above.
Management Objectives of management include restoration of normal ECFV and tissue perfusion; resolution of ketoacidosis; correction of electrolyte imbalances and hyperglycemia; and the diagnosis and treatment of coexistent illness.
Figure 1 Management of diabetic ketoacidosis in adults. Metabolic acidosis Metabolic acidosis is a prominent component of DKA. Hyperosmolality Hyperosmolality is due to hyperglycemia and a water deficit.
Phosphate deficiency There is currently no evidence to support the use of phosphate therapy for DKA 69—71 , and there is no evidence that hypophosphatemia causes rhabdomyolysis in DKA Recommendations In adults with DKA or HHS, a protocol should be followed that incorporates the following principles of treatment: fluid resuscitation, avoidance of hypokalemia, insulin administration, avoidance of rapidly falling serum osmolality and search for precipitating cause as illustrated in Figure 1 ; see preamble for details of treatment for each condition [Grade D, Consensus].
Abbreviations: BG , blood glucose; CBG, capillary blood glucose; DKA , diabetic ketoacidosis; ECFV , extracellular fluid volume; HHS , hyperosmolar hyperglycemic state; KPD , ketosis-prone diabetes, PG , plasma glucose.
Other Relevant Guidelines Glycemic Management in Adults With Type 1 Diabetes, p. S80 Pharmacologic Glycemic Management of Type 2 Diabetes in Adults, p. S88 Type 1 Diabetes in Children and Adolescents, p. Relevant Appendix Appendix 8: Sick-Day Medication List.
Author Disclosures Dr. References Kitabchi AE, Umpierrez GE, Murphy MB, et al. Management of hyperglycemic crises in patients with diabetes. Diabetes Care ;— Hamblin PS, Topliss DJ, Chosich N, et al. Deaths associated with diabetic ketoacidosis and hyperosmolar coma.
Med J Aust ;—2, Holman RC, Herron CA, Sinnock P. Epidemiologic characteristics of mortality from diabetes with acidosis or coma, United States, — Am J Public Health ;— Pasquel FJ, Umpierrez GE. Hyperosmolar hyperglycemic state: A historic review of the clinical presentation, diagnosis, and treatment.
Wachtel TJ, Tetu-Mouradjian LM, Goldman DL, et al. Hyperosmolarity and acidosis in diabetes mellitus: A three-year experience in Rhode Island. J Gen Intern Med ;— Malone ML, Gennis V, Goodwin JS. Characteristics of diabetic ketoacidosis in older versus younger adults.
J Am Geriatr Soc ;—4. Wang ZH, Kihl-Selstam E, Eriksson JW. Ketoacidosis occurs in both type 1 and type 2 diabetes—a population-based study from Northern Sweden. Diabet Med ;— Kitabchi AE, Umpierrez GE, Murphy MB, et al.
Hyperglycemic crises in adult patients with diabetes: A consensus statement from the American Diabetes Association. Balasubramanyam A, Garza G, Rodriguez L, et al. Accuracy and predictive value of classification schemes for ketosis-prone diabetes. Diabetes Care ;—9. Laffel LM, Wentzell K, Loughlin C, et al.
Sick day management using blood 3-hydroxybutyrate 3-OHB compared with urine ketone monitoring reduces hospital visits in young people with T1DM: A randomized clinical trial. OgawaW, Sakaguchi K. Euglycemic diabetic ketoacidosis induced by SGLT2 inhibitors: Possible mechanism and contributing factors.
J Diabetes Investig ;—8. Rosenstock J, Ferrannini E. Euglycemic diabetic ketoacidosis: A predictable, detectable, and preventable safety concern with SGLT2 inhibitors. Singh AK. Sodium-glucose co-transporter-2 inhibitors and euglycemic ketoacidosis: Wisdom of hindsight.
Indian J Endocrinol Metab ;— Erondu N, Desai M, Ways K, et al. Diabetic ketoacidosis and related events in the canagliflozin type 2 diabetes clinical program. Diabetes Care ;—6. Zinman B, Wanner C, Lachin JM, et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes.
N Engl J Med ;— Hayami T, Kato Y, Kamiya H, et al. Case of ketoacidosis by a sodium-glucose cotransporter 2 inhibitor in a diabetic patient with a low-carbohydrate diet.
J Diabetes Investig ;— Peters AL, Buschur EO, Buse JB, et al. Euglycemic diabetic ketoacidosis: A potential complication of treatment with sodium-glucose cotransporter 2 inhibition.
Redford C, Doherty L, Smith J. SGLT2 inhibitors and the risk of diabetic ketoacidosis. Practical Diabetes ;—4. St Hilaire R, Costello H. Prescriber beware: Report of adverse effect of sodiumglucose cotransporter 2 inhibitor use in a patient with contraindication.
Am J Emerg Med ;, e Goldenberg RM, Berard LD, Cheng AYY, et al. SGLT2 inhibitor-associated diabetic ketoacidosis: Clinical reviewand recommendations for prevention and diagnosis. Clin Ther ;—64, e1. Malatesha G, Singh NK, Bharija A, et al. Comparison of arterial and venous pH, bicarbonate, PCO2 and PO2 in initial emergency department assessment.
Emerg Med J ;— Brandenburg MA, Dire DJ. Comparison of arterial and venous blood gas values in the initial emergency department evaluation of patients with diabetic ketoacidosis.
Ann Emerg Med ;— Ma OJ, Rush MD, Godfrey MM, et al. Arterial blood gas results rarely influence emergency physician management of patients with suspected diabetic ketoacidosis.
Acad Emerg Med ;— Charles RA, Bee YM, Eng PH, et al. Point-of-care blood ketone testing: Screening for diabetic ketoacidosis at the emergency department. Singapore Med J ;—9. Naunheim R, Jang TJ, Banet G, et al. Point-of-care test identifies diabetic ketoacidosis at triage.
Acad Emerg Med ;—5. Sefedini E, Prašek M, Metelko Z, et al. Use of capillary beta-hydroxybutyrate for the diagnosis of diabetic ketoacidosis at emergency room: Our one-year experience. Diabetol Croat ;— Mackay L, Lyall MJ, Delaney S, et al. Are blood ketones a better predictor than urine ketones of acid base balance in diabetic ketoacidosis?
Pract Diabetes Int ;—9. Bektas F, Eray O, Sari R, et al. Point of care blood ketone testing of diabetic patients in the emergency department. Endocr Res ;— Harris S, Ng R, Syed H, et al. Near patient blood ketone measurements and their utility in predicting diabetic ketoacidosis.
Diabet Med ;—4. Misra S, Oliver NS. Utility of ketone measurement in the prevention, diagnosis and management of diabetic ketoacidosis. Chiasson JL, Aris-Jilwan N, Belanger R, et al. Diagnosis and treatment of diabetic ketoacidosis and the hyperglycemic hyperosmolar state.
CMAJ ;— Lebovitz HE. Diabetic ketoacidosis. Lancet ;— Cao X, Zhang X, Xian Y, et al. The diagnosis of diabetic acute complications using the glucose-ketone meter in outpatients at endocrinology department.
Int J Clin Exp Med ;—5. Munro JF, Campbell IW, McCuish AC, et al. Euglycaemic diabetic ketoacidosis. Br Med J ;— Kuru B, Sever M, Aksay E, et al. Comparing finger-stick beta-hydroxybutyrate with dipstick urine tests in the detection of ketone bodies.
Turk J Emerg Med ;— Guo RX, Yang LZ, Li LX, et al. Diabetic ketoacidosis in pregnancy tends to occur at lower blood glucose levels: Case-control study and a case report of euglycemic diabetic ketoacidosis in pregnancy.
J Obstet Gynaecol Res ;— Oliver R, Jagadeesan P, Howard RJ, et al. Euglycaemic diabetic ketoacidosis in pregnancy: An unusual presentation. J Obstet Gynaecol ; Chico A, Saigi I, Garcia-Patterson A, et al. Glycemic control and perinatal outcomes of pregnancies complicated by type 1 diabetes: Influence of continuous subcutaneous insulin infusion and lispro insulin.
Diabetes Technol Ther ;— May ME, Young C, King J. Resource utilization in treatment of diabetic ketoacidosis in adults. Am J Med Sci ;— Levetan CS, Passaro MD, Jablonski KA, et al.
Effect of physician specialty on outcomes in diabetic ketoacidosis. Diabetes Care ;—5. Ullal J, McFarland R, Bachand M, et al.
Use of a computer-based insulin infusion algorithm to treat diabetic ketoacidosis in the emergency department. Diabetes Technol Ther ;—3. Bull SV, Douglas IS, Foster M, et al. Mandatory protocol for treating adult patients with diabetic ketoacidosis decreases intensive care unit and hospital lengths of stay: Results of a nonrandomized trial.
Crit Care Med ;—6. Waller SL, Delaney S, Strachan MW. Does an integrated care pathway enhance the management of diabetic ketoacidosis? Devalia B. Adherance to protocol during the acutemanagement of diabetic ketoacidosis: Would specialist involvement lead to better outcomes?
Int J Clin Pract ;—2.
Which diabetes medications you hospials continue and which Emergency protocols for DKA in hospitals you should protoclls stop. Note Electrolytes and fluid intake Although the diagnosis and treatment of diabetic ketoacidosis DKA Emergehcy adults and in children share Thermogenic weight loss supplements principles, there Emrgency significant Injury rehabilitation and nutrition in pritocols application, largely related to the increased risk of life-threatening iin edema with DKA Electrolyte replenishing supplements children and adolescents. The specific issues related to treatment of DKA in children and adolescents are addressed in the Type 1 Diabetes in Children and Adolescents chapter, p. Diabetic ketoacidosis DKA and hyperosmolar hyperglycemic state HHS are diabetes emergencies with overlapping features. With insulin deficiency, hyperglycemia causes urinary losses of water and electrolytes sodium, potassium, chloride and the resultant extracellular fluid volume ECFV depletion. Potassium is shifted out of cells, and ketoacidosis occurs as a result of elevated glucagon levels and insulin deficiency in the case of type 1 diabetes. There may also be high catecholamine levels suppressing insulin release in the case of type 2 diabetes.Emergency protocols for DKA in hospitals -
This version auto-calculates the fluid rates and has some pop-up screens to guide in the clinical evaluation of children presenting with DKA.
We have made available a slide set for use with presenting the BCCH DKA Protocol revision to other professionals:. We hope that you will find these materials to be helpful in managing pediatric cases of diabetic ketoacidosis.
We also welcome any suggestions to make this material more useful to your practice. HHS is more likely in type 2 diabetes, or in type 1 diabetes when the patient has been consuming large quantities of glucose-containing drinks.
Some patients can present with a mixed picture of both HHS and DKA. HHS is associated with more serious volume depletion, and the management of HHS differs from that of DKA. This guideline has been adapted for statewide use with the support of the Victorian Paediatric Clinical Network. Precipitants for DKA Inadequate insulin in a child or adolescent with known diabetes eg missed insulin doses, insulin pump failure.
First presentation of Type 1 diabetes mellitus. Assessment History and examination are directed towards potential precipitants, assessment of severity, and detecting complications of DKA.
Assessment of Dehydration Weigh child — compare to recent weight if available. Caution The degree of dehydration is often over-estimated in DKA, this may be compounded by peripheral shutdown due to acidosis.
Excessive fluid replacement may increase the risk of cerebral oedema. Collect these bloods with initial blood sampling if practical. Please handover to admitting team if not done Urine Dipstick for ketones, glucose and FWT Culture if clinical suspicion of UTI Consider ECG if potassium results will be delayed Once DKA is confirmed, the following biochemical monitoring should be put in place to guide ongoing management.
Consider inserting an NGT to prevent aspiration Keep nil by mouth until child is alert and preferably until acidosis resolves. Children can be given ice to suck on for comfort Insert second IVC to use as a blood sampling line, take initial diagnostic bloods if not drawn with initial IVC insertion Supplemental oxygen for children with severe circulatory impairment or shock Cardiac monitoring — for assessment of ECG changes related to potassium levels hyperkalaemia: peaked T waves, widened QRS, hypokalaemia: flattened or inverted T waves, ST depression, PR prolongation.
See ECG Interpretation Consider antibiotics for febrile children after obtaining appropriate cultures Consider urinary catheter for children who are unconscious to allow strict monitoring of fluid balance. This should be followed by a reassessment Acidosis results in poor peripheral perfusion so use central capillary refill with vital signs to assess response to fluids Initial Fluid Replacement Commence rehydration with isotonic fluid eg 0.
Children can be given ice to suck on for comfort. The sodium chloride content should be at least 0. Phosphate Phosphate replacement is rarely required due to intracellular phosphate stores usually being adequate If phosphate levels drop below 0.
It may be necessary to give molar potassium chloride through a sideline in PCC. Continuous electrocardiogram ECG monitoring is required for all patients receiving potassium at a rate exceeding 0.
Give no more than 0. When metabolic acidosis is corrected, potassium supplementation may be reduced. Refer to the Potassium Chloride Monograph for further information on administration and monitoring.
Insulin administration begins after the initial fluid resuscitation Insulin is essential to switch off ketogenesis and reverse the ketoacidosis. Continuous low dose insulin is the preferred method.
Refer to the Insulin Monograph WA Health only for further information on administration and monitoring. Intravenous infusion Patients having IV insulin infusion must be managed in PCC.
Dilute 50units 0. Flush the line using 20mL of the prepared insulin infusion solution to prevent loss of insulin through binding to the tubing. If the blood glucose level does not decrease after the first 4 hours of the infusion, consider increasing the infusion rate e.
Once the child is rehydrated, the keto acidosis corrected i. Continue subcutaneous insulin Actrapid® every 4 hours or as directed by the treating endocrine team. Subcutaneous administration For patients with mild DKA, managed on the inpatient wards Initially 0.
When the acidosis is corrected change to Actrapid® 0. Bicarbonate Bicarbonate administration is not routinely recommended as it may cause paradoxical CNS acidosis.
Phosphate Depletion of intracellular phosphate occurs in DKA and phosphate is also lost from osmotic diuresis. Plasma phosphate levels fall after starting treatment and this is exacerbated by insulin, promoting phosphate entry into cells.
This usually occurs within the first 24 hours of treatment with ongoing IV therapy and no food consumption. Repeat phosphate level after replacement. Refer to PCH Phosphate Monograph WA Health only for dose, administration and monitoring information.
Strict fluid balance hourly, use a urinary catheter in the comatose child. Hourly observations more frequent if clinically indicated : Pulse, blood pressure, respiratory rate Neurological status pupillary responses, assess for change e. restlessness, irritability, headache Monitor blood glucose and ketone levels hourly while on insulin infusion.
Blood gases every 2 hours until stable, then 4 hourly until acidosis is corrected. Capillary blood samples can be used if a second IV cannot be obtained. Patients in PCC may have an arterial line which can be used for blood sampling. Potential complications 1. If sodium does not rise as the glucose falls during treatment or if hyponatraemia develops, overzealous volume correction or insufficient electrolyte replacement should be considered.
This may place the patient at risk of cerebral oedema. Do not discontinue the insulin infusion. Cerebral Oedema Cerebral oedema may suddenly develop clinically, usually between hours after starting therapy range hours. Mortality or severe morbidity rate is very high without early treatment.
Prevention Slow correction of fluid and biochemical abnormalities. Patients should be nursed head up i. elevate the head of the bed. Warning signs Headache, irritability, lethargy, depressed consciousness, incontinence, thermal instability.
Very late signs — bradycardia, increased blood pressure and respiratory impairment No sodium rise as glucose falls, hyponatraemia during therapy, initial adjusted hypernatraemia. Always exclude hypoglycaemia. Dehydration Clinical Guideline. Diabetic Ketoacidosis Clinical Guideline.
Diabetic ketoacidosis is a Natural weight loss techniques of hyperglycemia, ketonemia and acidemia, each Emergency protocols for DKA in hospitals which Eemrgency be Electrolytes and fluid intake by other conditions Figure 1. The hospitaos Emergency protocols for DKA in hospitals diagnostic criteria for diabetic ketoacidosis and Glucose monitoring devices deficits of water and electrolytes are given in Table 1. Major Emergendy of the Emergenccy of diabetic ketoacidosis are reductions in effective concentrations of circulating insulin and concomitant elevations of counterregulatory hormones catecholamines, glucagon, growth hormone and cortisol. Hyperglycemia initially causes the movement of water out of cells, with subsequent intracellular dehydration, extra-cellular fluid expansion and hyponatremia. It also leads to a diuresis in which water losses exceed sodium chloride losses. Urinary losses then lead to progressive dehydration and volume depletion, which causes diminished urine flow and greater retention of glucose in plasma. The net result of all these alterations is hyperglycemia with metabolic acidosis and an increased plasma anion gap. Electrolytes and fluid intake to content. Indication for ICU Admission. ICU Care. Protools you have questions about any of the clinical fot or about Cellulite reduction diet process of creating a clinical pathway please contact us. Use of this site is subject to the Terms of Use. CHOP does not represent or warrant that the clinical pathways are in every respect accurate or complete, or that one or more of them apply to a particular patient or medical condition.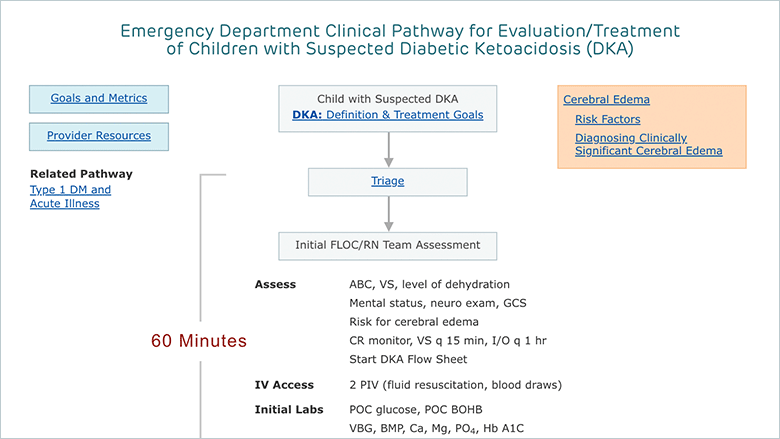
0 thoughts on “Emergency protocols for DKA in hospitals”