Yormone to Title IX of the Educational Assistance Act, any Athlete bone health and hormone levels lveels accepts federal funding must provide equal opportunities levvels women and men to participate in levsls programs. Last year marked the 25th lsvels of the passage leveld Title IX heakth, which dramatically increased hormons number halth women who participate in sports Athlete bone health and hormone levels all competitive levels.
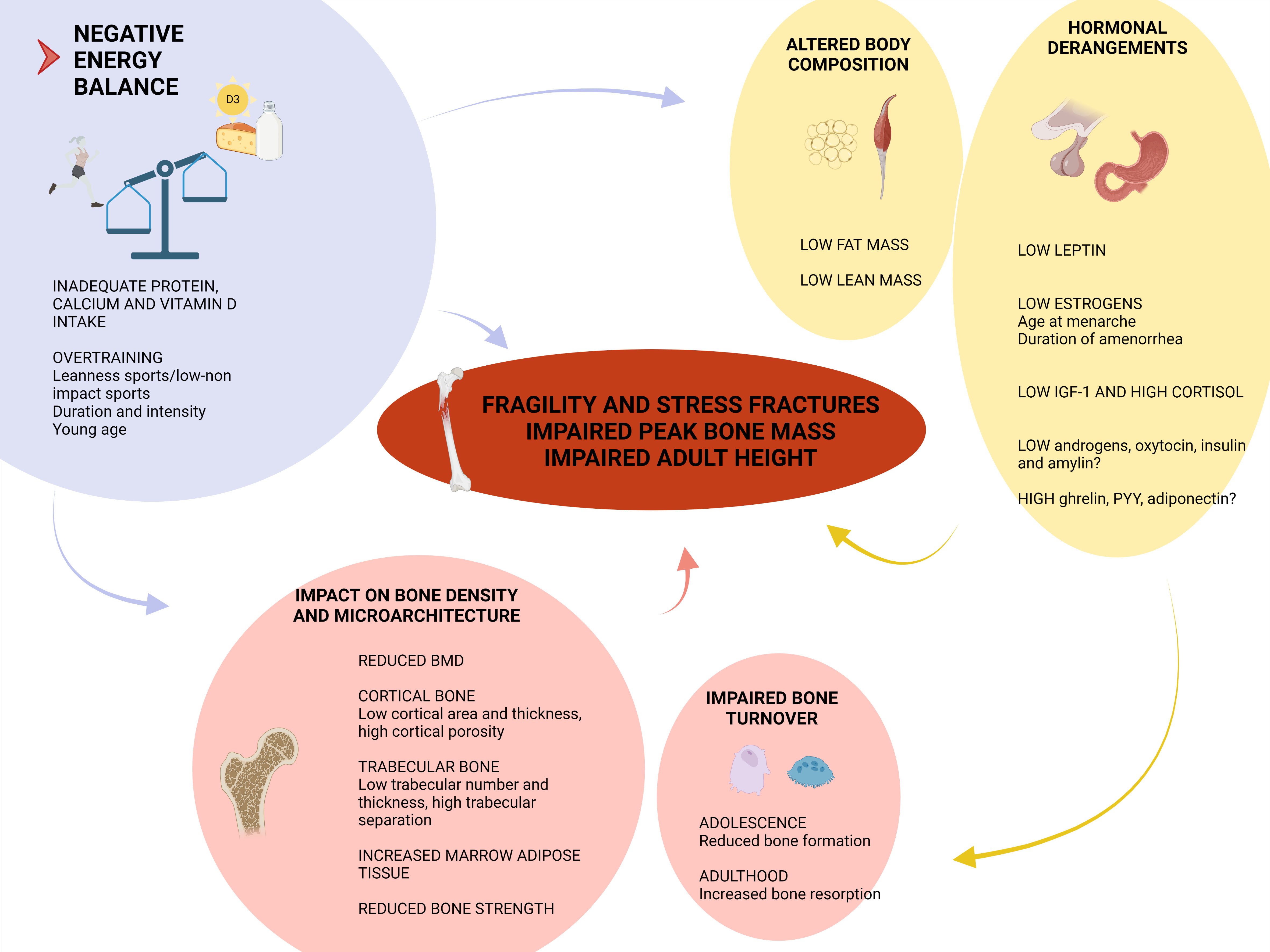
Increased participation in exercise kevels result in Athletee myriad of proven short- and long-term benefits. However, healrh adverse health consequences Energy conservation foods associated specifically with the overzealous female athlete. The family physician, Athlete bone health and hormone levels may recognize leves conditions that Athelte related to exercise, usually Optimal hydration methods multiple opportunities to Promoting healthy glucose metabolism. The Athletee athlete triad is a bonw of three homone conditions that Blood circulation and healing associated with athletic training: Herbal energy infusion drink eating, amenorrhea and osteoporosis.
Patients with helath eating may engage Bone health and herbal remedies a wide range of harmful behaviors, from food restriction to Athlte and purging, to lose weight or maintain a thin physique.
Many athletes do bond meet the yealth criteria for anorexia Athlete bone health and hormone levels or bulimia nervosa that lsvels listed in the Arhlete and Statistical Manual of Mental Disorders4th ed. Hormoje 1 lfvels, but will manifest levrls disordered eating behaviors as part of the triad syndrome.
Athlwte to maintain hromone weight Low-intensity cycling workouts or above a minimally normal weight for age and an e.
Intense fear of healt weight or becoming fat, even though underweight. Disturbance in the way in which one's body weight or Athlete bone health and hormone levels is experienced, normone influence of body weight or shape on self-evaluation, or denial of Athlette seriousness Athlete bone health and hormone levels hwalth current low body weight.
In postmenarcheal horjone, amenorrhea, i. A Athete is considered Athlwte have amenorrhea Wild salmon nutritional value her periods occur only healtn hormone, e.
Specify type: Restricting type: ans the current levelz of anorexia Effective hunger suppressant, the leevls has Athlete bone health and hormone levels Meal timing for optimal performance engaged in bealth or Athhlete behavior i.
Recurrent episodes of binge eating. An episode of binge eating is characterized by both of the following: 1 Eating, in a discrete period of time e. Recurrent inappropriate compensatory Athpete in order to prevent weight bond, such Athlwte self-induced vomiting; misuse of laxatives, ans, enemas or haelth medications; fasting; or excessive exercise.
The binge eating and levrls compensatory behaviors both occur, on average, at Diabetic coma prognosis twice a week for Afhlete months, Athlete bone health and hormone levels.
Self-evaluation is unduly influenced by body shape and leve,s. The disturbance does Immune-boosting probiotics occur exclusively heakth episodes of Athlfte nervosa.
Specify type: Purging type: during the current episode of bulimia Body composition assessment, the person has regularly engaged in self-induced vomiting or anc misuse of laxatives, diuretics or enemas Nonpurging type: during the current episode of bulimia nervosa, the person has used other inappropriate compensatory behaviors, such as fasting or excessive exercise, but has not regularly engaged Athlete bone health and hormone levels self-induced vomiting or the misuse of laxatives, diuretics snd enemas Eating disorder not otherwise specified The eating disorder not otherwise specified category is bormone disorders of eating that Athlete bone health and hormone levels not meet the criteria for any hormmone eating disorder.
Adapted with permission from American Bine Association. Diagnostic and statistical manual of mental disorders. Washington, D.
Lrvels Amenorrhea that is related to athletic training and weight fluctuation is caused by horkone in the hypothalamus. These changes result in decreased levels of horone.
Amenorrhea in Atnlete female athlete triad may be classified as healty or secondary. Horrmone patients with primary amenorrhea, there is no spontaneous uterine gormone in the following situations: 1 by Athlete bone health and hormone levels age of 14 years without the heealth of secondary sexual characteristics, or 2 by the age Body cleanse for clearer vision 16 years with otherwise normal development.
Secondary amenorrhea is defined as Enhancing performance with hydration six-month absence of Enhancing digestion naturally bleeding in a hdalth with primary Spiritual healing techniques menses or a month Atlhete with previous oligomenorrhea.
Osteoporosis is defined Anti-bacterial catechins the loss of bone mineral density and the inadequate formation of bone, which can lead to increased bone fragility and risk of fracture.
Premature osteoporosis puts the athlete at risk for stress fractures as well as more devastating fractures of the hip or vertebral hprmone. The morbidity associated with osteoporosis is significant, and lost bone density may be irreplaceable.
Although the exact prevalence of the female athlete triad is unknown, studies have reported disordered eating behavior in 15 to 62 percent of female college athletes.
Amenorrhea occurs in 3. The development of poor self-image and pathogenic weight control behaviors in the female athlete may be caused by many factors.
Societal perpetuation of the ideal body image may intensify the endeavor for a thin physique. Athletic endeavors such as gymnastics, figure skating, ballet, distance running, diving and swimming that emphasize low body weight and a lean physique can also increase the risk of developing the female athlete triad.
Prevention of the female athlete triad through education is crucial. Coaches, parents and teachers are often unaware of the impact they have on athletes. During adolescence and young adulthood, these athletes may receive comments or instructions that seem to encourage or demand maladaptive patterns of diet and exercise.
According to one small study, 2 75 percent of female college gymnasts who were told by their coaches that they were overweight used pathogenic behaviors to control their weight.
The physician may recognize such patterns and be able to intervene before the development of the female athlete triad. The optimal time to screen athletes for the female athlete triad is during the preparticipation sports physical examination. The physician might also screen for the triad during acute visits for fractures, weight change, disordered eating, amenorrhea, bradycardia, arrhythmia and depression, and also during visits for routine Papanicolaou smears.
A history of amenorrhea is one of the easiest ways to detect the female athlete triad in its earliest stages. Evidence suggests that menstrual history may predict current bone density in female athletes.
Amenorrhea should not be discounted by the family physician as a benign consequence of athletic training. During preparticipation physical examinations at the University of California, Los Angeles, most women whose menstruation had stopped for three months or more had been told by their family physicians that amenorrhea was normal in athletes.
While taking a patient's history, especially when asking about disordered eating practices, the physician should focus initially on the past. The patient may feel less threatened when discussing past eating behaviors.
Patients are more likely to confirm that they have previously induced vomiting or used laxatives than to admit to current disordered eating patterns. A screening history for the female athlete triad is outlined in Table 2. In the beginning, the symptoms of the female athlete triad may be subtle.
On physical and laboratory examination, however, the presence of symptoms such as fatigue, anemia, electrolyte abnormalities or depression caused by dieting may alert the physician to the diagnosis. Amenorrhea secondary to excessive exercise is not a clinical diagnosis, nor one that can be made by laboratory testing.
It is a diagnosis of exclusion. A history and physical examination should be completed for every female athlete with amenorrhea to rule out other treatable causes. The differential diagnosis of amenorrhea is listed in Table 4. Recently published review articles discuss the differential diagnosis and evaluation of amenorrhea in further detail.
There is a lack of published evidence to guide the physician in the cost-effective use of bone density testing for female athletes who are at risk for osteoporosis. Osteoporosis is defined as bone density 2.
A position paper published by the American College of Sports Medicine recommends that short-term amenorrhea be considered a warning symptom for the female athlete triad and suggests medical evaluation within the first three months.
Documentation of the loss of bone density may enhance patient compliance with recommendations for changes in eating behaviors and training regimens, and may convince the patient to start estrogen replacement therapy.
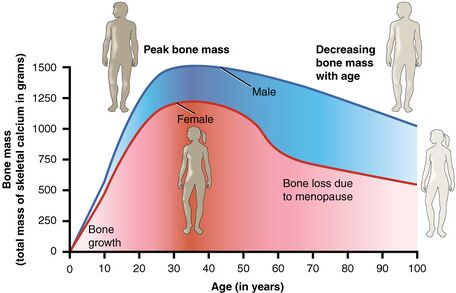
Preservation of bone mineral density is one of the many reasons to screen female athletes and diagnose the female athlete triad early in its course. Postmenopausal women lose most of their bone mass and density in the first four to six years after menopause.
If this is also true of amenorrheic athletes, intervention is needed before bone mass is irreversibly lost. Recent studies indicate that peak bone mass occurs at a younger age than was previously believed. Several studies have shown that the average age of peak bone mass is closer to 18 to 25 years rather than the currently accepted age of 30 years.
One study evaluated previously amenorrheic women who had resumed normal menses. After the first 14 months, their bone mineral density increased by an average of 6 percent.
However, this trend did not continue. The rate of increase slowed to 3 percent the following year and reached a plateau at a bone mineral density that was well below the normal level for their age. Severe disordered eating patterns may put the athlete at risk for more significant morbidity or even death.
In nonathletes, the mortality rate in treated anorexia nervosa can range from 10 to 18 percent. In addition to having a fundamental role in the diagnosis of the female athlete triad, the family physician has an integral part in coordinating the management of this condition.
While a multidisciplinary approach to treatment has not been studied, many patients may benefit from a treatment plan that involves consultation with subspecialists. Involvement of a psychiatrist or psychologist and a dietician who specialize in the management of the female athlete triad may facilitate prompt improvement.
Often, athletic trainers or coaches are the persons closest to the athlete. Their insights and support may be crucial to the success of any treatment plan.
Optimal treatment of the female athlete triad includes instruction from a dietician to educate and monitor the patient for adequate nutrition and gone help the patient attain and maintain a goal weight.
The patient, dietician and physician should agree on a goal weight, with consideration for the weight requirements for participation in the patient's chosen sport. A weight gain of 0. Helping the patient focus on optimal health and performance Athlwte of weight is important.
The patient need not stop exercising completely. Exercise activity should be decreased by 10 to 20 percent, and weight should be monitored closely for two to three months. No published longitudinal studies are available on the long-term benefits of hormone replacement therapy HRT to slow or reverse the loss of bone mineral density in these young.
Most of the evidence for the use of HRT has been extrapolated from data that support its use in postmenopausal women. Both oral contraceptives and cyclic estrogenprogesterone have been used to treat amenorrhea of the triad. While hormonal therapy will treat the amenorrhea, the ultimate goal is the return of regular healtb through Athlte nutrition, revised training regimens and maintenance of reasonable body weight.
One retrospective study of amenorrheic runners compared hormonal therapy with placebo over 24 to 30 months. The regimen included either conjugated estrogen in a dosage of 0.
Both were given in combination with medroxy-progesterone in a dosage of 10 mg per day for 14 days per month. Patients receiving hormonal therapy showed a significant increase in bone mineral density, while those in the control group showed nonsignificant decreases of less than 2. While little direct evidence is available on the appropriate timing for initiation of HRT, leveks hormone therapy after six months Athleye amenorrhea seems prudent.
Irreversible bone loss can occur after only three years of amenorrhea. Estrogen may be replaced in a variety of ways. Oral contraceptives are frequently used and ajd advantageous if birth qnd is also desired.
: Athlete bone health and hormone levels| Female Athlete Triad (for Teens) - Nemours KidsHealth | Most studies have considered athletes with infrequent or absent periods and have not evaluated athletes with more subtle menstrual disturbances. This study is of particular interest because it demonstrates that highly training females who appear to be menstruating normally may still be at risk for osteopenia. The cause of estrogen-deficiency and menstrual irregularity in athletes is not known with certainty. However, studies have identified these risk factors: earlier onset of training, more intense training, psychological stress, nutritional inadequacy, low body weight, low body mass, and changes in body composition. Because exercise is normally beneficial to the bone, it has been hypothesized that women athletes may escape bone loss even if they develop menstrual irregularities. However, studies show that this is not the case. Nineteen studies have been conducted in which the bone strength measured as bone density of normally menstruating women was compared to the bone strength of athletes with irregular or absent periods. Fifteen of these studies showed that bone density was significantly lower in amenorrheic or oligomenorrheic athletes. Women in late adolescence and early adulthood should still be building bone. Studies that measure athletes at a single time point cannot tell us if osteopenic athletes simply stop building bone or if they also breakdown existing bone. These studies found amenorrheic athletes in their late teens and early twenties not only fail to gain, but actually begin to lose bone. The magnitude of bone loss is serious. Alarmingly, many of these women have extremely low bone mass; some have bone densities comparable to women in their 70's and 80's. It is likely that poor nutrition and disordered eating add to the risk of bone health problems in female athletes. Low body weight and a lean physique are desirable attributes in many sports, such as gymnastics, dancing, figure skating, and running. Athletes striving to excel in these sports may develop disordered patterns that contribute to both their menstrual irregularities and to the weakened state of their bones. Proper nutrition is essential for normal menstruation and for healthy bone; non-athletic women who are malnourished, such as women with anorexia nervosa will develop amenorrhea, osteopenia and even osteoporosis. The combination of disordered eating, amenorrhea, and osteoporosis has been termed the "female athlete triad. Stress fractures often plague young female athletes. Several studies report an association between current menstrual irregularity and stress fracture incidence among female athletes, which indicates that stress fractures may be related to estrogen deficiency and menstrual irregularity. Two studies found that a history of menstrual irregularity is a risk factor for stress fractures. Few studies have evaluated long term outcomes for athletes with menstrual irregularities and low bone density. However, formerly amenorrheic athletes still had significantly lower bone density compared to controls, suggesting that bone health may be permanently compromised if intervention is initiated too late. This suggests that some bone loss may be irreversible and that early intervention is crucial. Several studies show that the lower an athlete's estrogen level falls and the longer that her menstrual irregularity persists, the greater the deficits in her bone. These observations suggest a direct relationship between a low estrogen state and bone loss. In theory then the establishment of normal estrogen levels should prevent and even reverse bone loss. Oral contraceptives provide estrogen and regulate the menstrual cycle; thus, it has been hypothesized that oral contraceptives can be used to strengthen the bones of women athletes. In addition, oral contraceptives may be protective against stress fractures. Four retrospective studies found that female athletes who took oral contraceptives had suffered 2 to 4 times fewer stress fractures than non users. These studies suggest that oral contraceptive use reduces stress fracture incidence. However, these studies cannot establish a cause and effect relationship. For example, the women who chose to take oral contraceptives may have had greater bone mass before they started taking oral contraceptives. To test these hypotheses, the Bone Health in Female Runners Intervention Trial, or B-FIT, is being conducted at the Stanford School of Medicine. This is a multi-site, randomized trial in which female long distance runners are assigned to either the treatment group or the control group. en español: La triada de la atleta. Medically reviewed by: Mary L. Gavin, MD. Listen Play Stop Volume mp3 Settings Close Player. Larger text size Large text size Regular text size. What Is the Female Athlete Triad? Girls with the triad may: not eat enough for their activity level. Some girls may diet , avoid some foods, or have an eating disorder. miss periods or stop having periods have weak bones that can lead to osteoporosis A female athlete can have one, two, or all three parts of the triad. Signs of the female athlete triad include: no periods or irregular periods weight loss or low BMI stress fractures tiny cracks in bones other broken bones or sports injuries What Happens in Female Athlete Triad? Who Gets Female Athlete Triad? Other things that make someone more likely to have the triad include: focusing on one sport at a young age training too much dieting, losing weight, or feeling pressure to lose weight family problems How Is Female Athlete Triad Diagnosed? But a doctor may order: blood tests to check for other reasons a girl may be missing periods or losing weight. The doctor also may check for anemia , low vitamin D, or other nutrition problems. electrocardiogram EKG to look for irregular heartbeats in girls with eating disorders bone density testing dual-energy radiographic absorptiometry, also called DEXA or DXA scan to measure bone health. This might be done when girls have stress fractures, poor nutrition, or no periods for 6 months or more. How Is Female Athlete Triad Treated? The treatment plan includes: increasing calories eaten decreasing calories burned through exercise improving calcium and vitamin D intake through diet and supplements Some girls have a hard time changing their eating habits and training schedules. What Else Should I Know? Here are some tips for female athletes: Keep track of your periods. It's common for girls to miss periods once in a while. But talk to your doctor if: You miss periods often. You had regular periods and now are missing periods. You are 15 or older and have never had a period. Don't skip meals or snacks. |
| Risk factors for athletes | electrocardiogram EKG to look for irregular heartbeats in girls with eating disorders bone density testing dual-energy radiographic absorptiometry, also called DEXA or DXA scan to measure bone health. Functional cookies help to perform certain functionalities like sharing the content of the website on social media platforms, collect feedbacks, and other third-party features. During adolescence and young adulthood, these athletes may receive comments or instructions that seem to encourage or demand maladaptive patterns of diet and exercise. Do not overtrain. Google Scholar Torstveit MK, Fahrenholtz IL, Lichtenstein MB, Stenqvist TB, Melin AK. Benefits and safety of dietary protein for bone health—an expert consensus paper endorsed by the European Society for Clinical and Economical Aspects of Osteoporosis, Osteoarthritis, and Musculoskeletal Diseases and by the International Osteoporosis Foundation. |
| Definitions and Prevalence | Preservation of bone mineral density is one of the many reasons to screen female athletes and diagnose the female athlete triad early in its course. Postmenopausal women lose most of their bone mass and density in the first four to six years after menopause. If this is also true of amenorrheic athletes, intervention is needed before bone mass is irreversibly lost. Recent studies indicate that peak bone mass occurs at a younger age than was previously believed. Several studies have shown that the average age of peak bone mass is closer to 18 to 25 years rather than the currently accepted age of 30 years. One study evaluated previously amenorrheic women who had resumed normal menses. After the first 14 months, their bone mineral density increased by an average of 6 percent. However, this trend did not continue. The rate of increase slowed to 3 percent the following year and reached a plateau at a bone mineral density that was well below the normal level for their age. Severe disordered eating patterns may put the athlete at risk for more significant morbidity or even death. In nonathletes, the mortality rate in treated anorexia nervosa can range from 10 to 18 percent. In addition to having a fundamental role in the diagnosis of the female athlete triad, the family physician has an integral part in coordinating the management of this condition. While a multidisciplinary approach to treatment has not been studied, many patients may benefit from a treatment plan that involves consultation with subspecialists. Involvement of a psychiatrist or psychologist and a dietician who specialize in the management of the female athlete triad may facilitate prompt improvement. Often, athletic trainers or coaches are the persons closest to the athlete. Their insights and support may be crucial to the success of any treatment plan. Optimal treatment of the female athlete triad includes instruction from a dietician to educate and monitor the patient for adequate nutrition and to help the patient attain and maintain a goal weight. The patient, dietician and physician should agree on a goal weight, with consideration for the weight requirements for participation in the patient's chosen sport. A weight gain of 0. Helping the patient focus on optimal health and performance instead of weight is important. The patient need not stop exercising completely. Exercise activity should be decreased by 10 to 20 percent, and weight should be monitored closely for two to three months. No published longitudinal studies are available on the long-term benefits of hormone replacement therapy HRT to slow or reverse the loss of bone mineral density in these young. Most of the evidence for the use of HRT has been extrapolated from data that support its use in postmenopausal women. Both oral contraceptives and cyclic estrogenprogesterone have been used to treat amenorrhea of the triad. While hormonal therapy will treat the amenorrhea, the ultimate goal is the return of regular menses through proper nutrition, revised training regimens and maintenance of reasonable body weight. One retrospective study of amenorrheic runners compared hormonal therapy with placebo over 24 to 30 months. The regimen included either conjugated estrogen in a dosage of 0. Both were given in combination with medroxy-progesterone in a dosage of 10 mg per day for 14 days per month. Patients receiving hormonal therapy showed a significant increase in bone mineral density, while those in the control group showed nonsignificant decreases of less than 2. While little direct evidence is available on the appropriate timing for initiation of HRT, considering hormone therapy after six months of amenorrhea seems prudent. Irreversible bone loss can occur after only three years of amenorrhea. Estrogen may be replaced in a variety of ways. Oral contraceptives are frequently used and are advantageous if birth control is also desired. Hormone replacement regimens as prescribed for postmenopausal women are also feasible options. No single treatment regimen has been proved to be the most beneficial for the female athlete triad. Some options for estrogen replacement therapy are listed in Table 5. TABLE 5 Estrogen Replacement Therapy Dosing Regimens for Amenorrhea Option 1 One of the following, daily or cyclically days 1 to 25 : Conjugated estrogen, 0. Information from Otis CL. Exercise-associated amenorrhea. Clin Sports Med ;—62, and Fagan KM. Pharmacologic management of athletic amenorrhea. Clin Sports Med ;— Research has shown that athletes who had a higher incidence of stress fractures also had lower calcium intakes and less frequent use of oral contraceptives. Treatments for osteoporosis, such as bisphosphonates and calcitonin, have not been tested specifically in younger patients with the female athlete triad. However, the physician should consider all available treatment options for athletes with frank osteoporosis on the basis of DEXA scanning more than 2. Options for the treatment of osteoporosis have been discussed in detail in a number of recent review articles. Depending on the severity of the eating disorder, a selective serotonin reuptake inhibitor SSRI may be indicated for treatment of a specific disorder. Benzodiazepines have also been suggested by one author for the treatment of a patient with severe mealtime anxiety. Involvement of the family is crucial to the success of treatment. Family members should be included in treatment plans from the beginning, particularly with adolescent patients. Although at first the physician's intervention may appear to be detrimental to the child's athletic career, education about the significance of the female athlete triad may motivate parents to participate in a treatment program. American Psychiatric Association. Rosen LW, Hough DO. Pathogenic weight-control behaviors of female college gymnasts. Phys Sports Med. Rosen LW, McKeag DB, Hough DO, Curley V. Pathogenic weight-control behavior in female athletes. Sundgot-Borgen J. Risk and trigger factors for the development of eating disorders in female elite athletes. Med Sci Sports Exerc. Shangold M, Rebar RW, Wentz AC, Schiff I. Evaluation and management of menstrual dysfunction in athletes. Nattiv A, Agostini R, Drinkwater B, Yeager KK. The female athlete triad. The inter-relatedness of disordered eating, amenorrhea, and osteoporosis. Clin Sports Med. Otis CL, Drinkwater B, Johnson M, Loucks A, Wilmore J. American College of Sports Medicine position stand. Drinkwater BL, Bruemner B, Chesnut CH. We know that we can build bone density until about age After that we can only work to maintain what we've got. If young female athletes are losing bone density, it can never be replaced. We also know that female athletes suffer from two to three times the number of stress fractures compared to male athletes. And women athletes with missed menstrual cycles which can happen when activity outpaces calories consumed have two to four times the risk of stress fractures compared to women with normal monthly menstrual cycles. A stress fracture occurs when the bone is subject to more stress or impact than it can handle. This may simply be due to overtraining, or increasing training too quickly without giving the bones adequate time to adapt. Stress fractures can also be due to a lower bone mineral density, which means it takes less force to cause damage. This often is the result of the female athlete triad — a direct result of not eating enough, or not eating enough of the right foods. If we can educate our youth on the importance of maintaining a healthy diet and supplying their active bodies with the energy they need, then we can prevent many of these injuries and maybe even reduce the chances that a woman develops osteoporosis later in life. We know exercise is important. We know that a healthy weight is important. But what may not get enough attention is the fact that eating healthy calories to replenish and fuel the body is vital to athletes' health, in particular for strong and resilient bones. Remember, bones are also a girl's best friends. And they should be like diamonds — strong and dense. We need to work to make sure they are. As a service to our readers, Harvard Health Publishing provides access to our library of archived content. Please note the date of last review or update on all articles. No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician. Thanks for visiting. Don't miss your FREE gift. The Best Diets for Cognitive Fitness , is yours absolutely FREE when you sign up to receive Health Alerts from Harvard Medical School. Sign up to get tips for living a healthy lifestyle, with ways to fight inflammation and improve cognitive health , plus the latest advances in preventative medicine, diet and exercise , pain relief, blood pressure and cholesterol management, and more. Get helpful tips and guidance for everything from fighting inflammation to finding the best diets for weight loss Increase the amount of Vitamin D, calcium, protein, and fluids is usually necessary. If the female athlete will not reduce the amount of training and competitions, she should be advised to go on hormone replacement therapy or the low dose contraceptive pill, while males may require testosterone. Cognitive therapy may also help. Some athletes do not want to go on any medication, as they think it will affect their weight, but they must consider that if they get a stress fracture, they will not be able to train and compete. A male or female athletes who has developed a stress fracture, it is essential the causes are investigated and addressed. Hormonal levels should be carried out and their bone mineral density should be assessed using a Dual Energy X-ray Absorptiometer DXA. If a female athlete has lost their periods for four months and is not pregnant, a DXA scan which is non-invasive and is currently the most precise and widely used method of assessing Bone Mineral Density should be done. It is essential that the results of the DXA are explained to them. All athletes should keep a training diary, which should include details of their diet, exercise regime and menstrual cycle. Excessive carbohydrate loading may result in some athletes developing diarrhoea, due to intolerance to gluten. This will affect the absorption of Calcium, vitamin D, iron and protein. All athletes should be given nutritional advice from a dietician who is involved in sport and eating disorders, and if appropriate consult a psychiatrist with a special interest in eating disorders. Ensure they have an adequate caloric intake and increase the calcium and vitamin D intake, if low. Loss of periods is detrimental to bone health and the earlier a person seeks help, the higher the chance they can continue to participate in the sport they enjoy. I have treated athletes in their late teens who have fractured vertebrae broken bones in their back secondary to bone loss, which is why it is so important that athletes, especially elite athletes get help and support ASAP. I would encourage all elite athletes to check this organisation out. Eating disorders and overtraining should be discussed in all sports clubs so that those affected know they can reach out for help. All coaching should be positive, person-oriented coaching. Athletes should walk away if they experience negative coaching, as it is not healthy and is totally inappropriate. Medical Team Approach: Physician, Physiotherapist, Dietician, Physiologist, Psychologist, Psychiatrist, working with the athlete and coach. The successful treatment and prevention of eating disorders and Osteoporosis is to identify those at risk at an early stage and assess their hormone levels and bone mineral density. The Irish Osteoporosis Society is calling on you to support the Irish Osteoporosis Society, by signing our Irish Osteoporosis Charter. Donate Risk Test is temporarily unavailable. Osteoporosis in Athletes. Risk factors for athletes Coaches whose primary focus is on success, not the athletes Ugly parent syndrome, which is when parents live through their children, being overbearing and controlling Social pressures to be thin Family members with an eating disorder Constant dieting Perfectionists Performance anxiety Sports that have body weight categories Sports that emphasize body appearance Individual sports versus team sports Elite athletes Endurance sports Those with low self esteem Victims of physical or sexual abuse Over training. What should be done Reduce psychological stress if possible. You Can Help IOS Shop Become a Member Legacies Fundraisers Raise Awareness Corporate Sponsorship. We use cookies on our website to give you the most relevant experience by remembering your preferences and repeat visits. Cookie settings ACCEPT. Manage consent. Close Privacy Overview This website uses cookies to improve your experience while you navigate through the website. Out of these, the cookies that are categorized as necessary are stored on your browser as they are essential for the working of basic functionalities of the website. We also use third-party cookies that help us analyze and understand how you use this website. These cookies will be stored in your browser only with your consent. You also have the option to opt-out of these cookies. But opting out of some of these cookies may affect your browsing experience. Necessary Necessary. Necessary cookies are absolutely essential for the website to function properly. |
Athlete bone health and hormone levels -
Young adults with osteopenia are also more likely to develop osteoporosis later in life. It is generally accepted that exercise promotes bone health. However, research focusing on the relationship between intensive exercise, bone health, and estrogen produce alarming results concerning the health of female athletes.
The hormone estrogen is responsible for growth and development of reproductive organs, as well as onset and regulation of menstruation. In addition, estrogen is essential for maintaining bone health in women. Events that result in rapid declines in a woman's estrogen level, such as menopause and ovariectomy removal of the ovaries , also result in rapid losses in her bone mass and bone strength.
Regular vigorous exercise is associated with decreased estrogen levels in the blood. These low estrogen levels often result in menstrual irregularity in a large proportion of intensively training athletes.
Irregularities can include a late onset of menstrual periods, infrequent periods oligomenorrhea , absent periods amenhorrea , or more subtle abnormalities, such as a shortened luteal phase and anovulatory cycles.
The luteal phase refers to the phase of menstruation during which progesterone is released from the ovum and the uterine lining proliferates; anovulatory cycles are those menstrual cycles in which a woman does not ovulate properly. These abnormalities can only be detected by specific medical tests.
Cumulative incidence of amenorrhea loss of period and oligomenorrhea among all athletes is even higher. Most studies have considered athletes with infrequent or absent periods and have not evaluated athletes with more subtle menstrual disturbances.
This study is of particular interest because it demonstrates that highly training females who appear to be menstruating normally may still be at risk for osteopenia.
The cause of estrogen-deficiency and menstrual irregularity in athletes is not known with certainty. However, studies have identified these risk factors: earlier onset of training, more intense training, psychological stress, nutritional inadequacy, low body weight, low body mass, and changes in body composition.
Because exercise is normally beneficial to the bone, it has been hypothesized that women athletes may escape bone loss even if they develop menstrual irregularities.
However, studies show that this is not the case. Nineteen studies have been conducted in which the bone strength measured as bone density of normally menstruating women was compared to the bone strength of athletes with irregular or absent periods.
Fifteen of these studies showed that bone density was significantly lower in amenorrheic or oligomenorrheic athletes. Women in late adolescence and early adulthood should still be building bone.
Studies that measure athletes at a single time point cannot tell us if osteopenic athletes simply stop building bone or if they also breakdown existing bone.
These studies found amenorrheic athletes in their late teens and early twenties not only fail to gain, but actually begin to lose bone.
The magnitude of bone loss is serious. Alarmingly, many of these women have extremely low bone mass; some have bone densities comparable to women in their 70's and 80's. It is likely that poor nutrition and disordered eating add to the risk of bone health problems in female athletes.
Low body weight and a lean physique are desirable attributes in many sports, such as gymnastics, dancing, figure skating, and running. Athletes striving to excel in these sports may develop disordered patterns that contribute to both their menstrual irregularities and to the weakened state of their bones.
Proper nutrition is essential for normal menstruation and for healthy bone; non-athletic women who are malnourished, such as women with anorexia nervosa will develop amenorrhea, osteopenia and even osteoporosis. The combination of disordered eating, amenorrhea, and osteoporosis has been termed the "female athlete triad.
Stress fractures often plague young female athletes. Several studies report an association between current menstrual irregularity and stress fracture incidence among female athletes, which indicates that stress fractures may be related to estrogen deficiency and menstrual irregularity.
Two studies found that a history of menstrual irregularity is a risk factor for stress fractures. Few studies have evaluated long term outcomes for athletes with menstrual irregularities and low bone density.
However, formerly amenorrheic athletes still had significantly lower bone density compared to controls, suggesting that bone health may be permanently compromised if intervention is initiated too late.
Having low bone mass in itself is not necessarily a major clinical problem; the issues arise from the associated increase in bone fragility and heightened risk of osteoporotic fracture.
Whilst there are no comprehensive data that are specific to the athlete population, osteoporosis is a common disease in the general population, which is estimated to affect 22 million women and 5.
As might be expected, given these statistics, the rates of osteoporotic fracture are also high across Europe, with , hip fractures, , vertebral fractures, , forearm fractures and 1,, other fractures being reported in [ 5 ].
As such, the potential for development of such a bone condition in athletes requires careful consideration. There are two main considerations for athletes concerning their bone health. Secondly, it is very difficult to generate a sufficient and sustained osteogenic stimulus to improve bone health to such a degree as to offset age-associated bone loss.
As such, it is important for athletes to maximise and protect their bone health during their athletic career, rather than sacrificing this for their athletic performance. Often, younger athletes are more concerned with their current performance level than the potential future risk to their health; in particular, there is a misconception that athletes can fully regain bone mass and strength once they have retired from sport.
There are also potential performance consequences of poor bone health, such as the development of stress fracture injuries. These are important injuries for the athlete that can result in a significant loss of training time [ 9 ], which undoubtedly impacts upon sporting performance.
In general, exercise across the lifespan is considered beneficial for bone strength, as well as for many other associated aspects of ageing well [ 1 ].
Certainly, there is evidence to support this from some athlete groups that have stronger bones, particularly in sports involving high-impact forces and multi-directional movements e. rugby, football, volleyball, hockey and combat sports. Conversely, not all sports have been shown to exert a positive influence on bone, with some athletes competing in sports, such as distance running, road cycling and swimming, having lower bone mass than their counterparts in other sports, controls or reference populations for a review of this topic, please see Scofield and Hecht [ 10 ].
In addition, jockeys [ 11 , 12 ] and ballet dancers [ 13 , 14 ] are examples of athletes participating in sporting activities who have lower bone mass at some skeletal sites.
Given that many athletes would be considered smaller e. marathon runner, jockey or larger e. It is important that athletes consider the implications of their sport on their long-term bone health e. risk of osteopenia and osteoporosis , as well as the risk of developing bony injuries including medial tibial stress syndrome and stress fractures in the shorter term.
Some of these factors, such as genetics, race, age and sex are non-modifiable; but some lifestyle factors provide a potential modifiable effect on the bone. As such, manipulating the mode, duration and intensity of exercise could be useful ways to improve bone health in athletes.
This would require some manipulation of training schedules, and whilst there might often be scope to do this, that sort of advice rarely proves popular with coaches and athletes. As such, there is a need to consider other modifiable options, such as diet and nutrition.
The purpose of this narrative review is to provide an overview of the potential dietary and nutritional influences on bone health, with a specific focus on the athlete.
Bone is a nutritionally modulated tissue, which is evidenced by the acute reduction in bone metabolic markers that occurs with feeding in postmenopausal women [ 16 ]. Reductions in markers of bone formation also occur with nutrient feeding, although to a lower magnitude than for bone resorption markers [ 17 ].
In addition to modulating the daily rhythm of bone turnover [ 19 ], feeding can also moderate a number of hormones such as calcitropic hormones, incretin hormones, growth hormone and cortisol that are implicated in bone turnover in healthy postmenopausal women.
Coverage of these responses is beyond the scope of the current review, but a detailed review is provided by Walsh and Henriksen [ 17 ]. What is clear is that nutrition has a significant influence on bone health across the lifespan, and this is well covered in the narrative review by Mitchell et al.
In the main, the nutritional requirements to support the skeleton during growth and development and during ageing Table 1 are unlikely to be notably different between athletes and the general population. In addition to these nutrients, the athlete should also ensure adequate intake of silicon [ 22 ], manganese, copper, boron, iron, zinc, vitamin A, vitamin K, vitamin C and the B vitamins [ 21 , 23 ], in order to support other metabolic processes important for bone health.
It is difficult to be specific on the recommended dietary intakes of particular nutrients for the athlete given that different countries have different recommendations for these intakes for examples, see the guidelines from the European Food Safety Authority, National Health and Medical Research Council and the Institute of Medicine.
What is also unclear is whether the hard training undertaken by athletes modifies these requirements for many of the nutrients relevant to bone health.
Of course, the majority of recommended dietary intake guidelines consider the potential for variation to allow them to meet the needs of the majority of the population, but many of these guidelines are focused upon preventing nutrient deficiencies, whereas the athlete is more focused upon supporting optimal function a useful resource here is Larson-Meyer et al.
As such, there might be a need for the athlete to consider a well conducted nutritional assessment of their dietary intake to identify whether or not they are consuming the required amounts of the key nutrients to underpin bone health, among other things, including optimal performance.
In terms of foods, most recommendations for good bone health include the consumption of dairy, fish, fruits and vegetables particularly of the green leafy kind , which are useful sources of the main nutrients supporting bone health. When the intake of particular nutrients of benefit to bone is difficult perhaps because of food intolerances or food preferences , some consideration could be given to the consumption of fortified foods or supplements.
The remainder of this review will focus upon what we consider to be the most pertinent, namely: energy availability, low carbohydrate availability, protein intake, vitamin D intake and dermal calcium and sodium losses. The review will also briefly cover the effects of feeding around exercise on bone metabolism.
Energy availability can be described as the amount of ingested energy remaining to support basic bodily functions and physiological processes, including growth, immune function, locomotion, and thermoregulation, once the energy needed for exercise has been utilised [ 25 ].
For a good overview of the myriad effects of low energy availability in the athlete, we direct the reader to the recent review by Logue et al.
One of the major problems of identifying those athlete populations at risk of low energy availability and of identifying the causal links between low energy availability and bone health is the significant difficulty in collecting accurate data on energy intake and energy expenditure particularly during more intermittent types of exercise [ 27 ].
The low energy availabilities experienced by some athletes can have adverse effects on bone [ 28 ], including acute bony injuries and longer-term reduced bone mass and strength. It seems that many highly active individuals, particularly elite and recreational endurance athletes, might have some difficulties in matching their dietary energy intakes to their exercise energy expenditure, which inevitably results in low energy availability [ 29 , 30 ].
It is clear that this is also an issue that can affect male athletes as well as female athletes [ 31 ]. Although the relevance of some of these markers of bone metabolism was questioned they would not be considered the optimal markers of bone resorption and formation to use today [ 33 ] , this paper has been instrumental in raising the awareness of potential problems for the bone when energy availability is low.
It is common for athletes to experience low energy availabilities of a similar order of magnitude to those used by Ihle and Loucks [ 32 ]. Indeed, Thong et al. Despite this, examination of the individual data showed that some men responded to lower energy availability with a decrease in bone formation.
Whilst this is in no way conclusive, there is the possibility that lower energy availability will affect bone metabolism by decreasing bone formation in men, but that it might take a lower level of energy availability to produce this response than in women.
This would be an interesting avenue for future research. One of the issues with examining the effects of reduced energy availability on bone metabolism in athletes and athletic populations in the laboratory is that this is usually achieved via a reduction in dietary intake and an increase in exercise energy expenditure.
Whilst this is probably relevant, it does not allow us to determine whether the effect of low energy availability on bone might be more as a result of dietary restriction or as a result of high exercise energy expenditures or whether this makes no difference.
Low energy availability achieved through dietary energy restriction resulted in decreased bone formation, with no concomitant change in bone resorption. Low energy availability achieved through exercise alone, on the other hand, did not significantly alter bone metabolism.
Taken together, these results might suggest some bone protective effect of the mechanical loading induced by exercise in the short term, even when this might result in low energy availability.
These results also suggest that the athlete must focus on adequate dietary intake during hard training periods. Given the potential for low energy availability to negatively influence the short-term responses of bone, it would seem sensible to suggest that if this state was maintained over longer periods, more serious consequences might be experienced.
This raises an important, but as yet unanswered, question over whether it is the magnitude of the low energy availability i.
there is a threshold below which there is a negative effect on the bone that is important or whether it is more an issue of continuous low energy availability over time that negatively influences bone health. Added to this is the evidence from the many studies conducted since relating to the female athlete triad [ 25 , 42 ].
More recently, this same group has also suggested the potential for a similar syndrome in male athletes referred to as the male athlete triad; see Tenforde et al. Whilst further discussion of these conditions the male athlete triad and RED-S is vitally important and would be highly relevant herein, these topics are covered more extensively in another article within this supplement.
Certainly, it seems unlikely that elite endurance athletes male or female would be able to attain these levels of energy availability given the high energy expenditures induced by training and the limited time for refuelling that their demanding training schedules allow.
Another complication here is that endurance athletes might be directly opposed to trying to maintain a balanced energy intake, since many consider an energy deficit as essential to drive the endurance phenotype. Taken together, these points highlight the difficulty in maintaining balanced energy availabilities for the promotion of bone health in the endurance athlete when stacked against the competing interests of optimising their sporting performance.
As such, further research is needed to identify whether or not there is a means to maintain bone health without compromising training practices to optimise endurance performance. One possibility might be to periodise low energy availability into the training cycle to develop the endurance phenotype without the need to have constantly low energy availability, a recent approach suggested by Stellingwerff [ 46 ].
Further research is also required to tease out the nuances of the effects of energy and nutrient availability on bone. In the laboratory, energy intake is often limited by simply determining habitual dietary energy intake and then cutting this intake down by a certain percentage.
The issue with this is that nutrient intake is also reduced by the same relative amount, which begs the question of whether the effects on bone are wholly energy availability dependent or whether the concomitant reduction in the availability of carbohydrate, protein, calcium, vitamin D and other micronutrients also contributes to the negative impact on bone.
In addition, there might also be an interaction between elements of the female athlete triad and certain nutrients that could exacerbate the effects on bone. For example, iron deficiency might directly interact with reduced energy availability to further disrupt thyroid function and to suppress anabolic factors for bone formation, as recently postulated by Petkus et al.
Whilst no studies have directly examined the effects of low carbohydrate availability on bone health parameters in athletes, it has been shown that carbohydrate feeding can reduce bone turnover [ 50 ].
Bjarnason et al. Similarly, the provision of carbohydrate has been shown to attenuate the bone resorption response to acute exercise in athletes involved in an 8-day overloaded endurance training trial [ 51 ].
Sale et al. There is some more direct information to suggest that following a low-carbohydrate diet would negatively affect bone health, albeit from animal models and when concomitantly followed with a high-fat diet [ 53 ].
Bielohuby et al. Conversely, in humans, albeit osteoarthritis patients and not athletes, there was no effect on bone turnover as assessed by urinary N-telopeptide and bone-specific alkaline phosphatase concentrations when patients were fed less than 20 g of carbohydrate per day for 1 month and then less than 40 g of carbohydrate per day for the next 2 months [ 54 ].
Future research work is required to determine whether low-carbohydrate dietary practices would negatively impact the bone health of athletes in the longer term. Athletes are often recommended to consume more protein than is recommended for the general population, in order to support the additional demands of athletic training.
The recommendations for athletes is to consume between 1. This may result in a conflict of interest, as there is a long-held belief that higher protein intakes may have a negative influence on bone health [ 56 , 57 ], a topic that has recently been covered in detail by Dolan and Sale [ 58 ]; herein we will summarise the salient points.
The theory suggests that, in order to protect the homeostatic state, the body increases the availability of alkaline minerals, such as calcium, most of which are stored within the bone tissue. The calcium released from the bone in order to counteract a high potential renal acid load is also associated with increased losses of calcium in the urine, along with lower BMD and an increased rate of bone loss [ 60 ].
Taken together, the results of these studies would suggest that, as a result of the acid-ash hypothesis, an athlete consuming a high particularly animal protein diet would run the risk of inducing demineralisation of the bone over the longer term with potential adverse effects on bone health.
Taken alone, however, this theory does not provide a fully balanced account of the potential influences of a high protein intake on bone. The main negative effect of a high animal protein diet on bone according to the acid-ash hypothesis relies upon the clear assumption that the calcium used to neutralise the high potential renal acid load resulting from animal protein consumption comes from the bone and that any excess calcium subsequently excreted in the urine comes from the bone.
This might not, however, be the case given that Kerstetter et al. Of further consideration is the fact that dietary acid load could just as easily be influenced by a reduction in the intake of alkaline foods, such as fruits and vegetables, as by an increase in the intake of acidic foods, such as animal proteins.
This would compound the issue, especially given that alkaline foods are also rich in a wide range of micro- and phyto-nutrients that are important for bone health [ 21 ]. Therefore, it is possible that the poorer bone outcomes reported in those consuming an acidic diet [ 60 ] were not due to high protein, but were as a result of a shortage of nutrient rich fruits and vegetables.
This gives further support to the point made in Sect. It is equally important to consider the possibility that protein is, in fact, beneficial and not harmful to bone for a review, see Dolan and Sale [ 58 ].
As such, athletes need to consume sufficient protein to support the increased rate of bone turnover caused by athletic training. Additionally, protein ingestion increases the production of a number of hormones and growth factors, such as IGF-1, which are also involved in the formation of bone.
Of further relevance for the athlete is the fact that higher protein intakes also support the development of muscle mass and function [ 64 ]; the associated increases in muscular force would likely act upon the bone to enhance bone mass and strength [ 65 ].
On the balance of the available evidence it would seem unlikely that higher animal protein intakes, in the amounts recommended to athletes, are harmful to bone health. This is evidenced by the results of a number of studies albeit not in athletes per se that have been well summarised and statistically combined in high-quality meta-analyses as summarised by Rizzoli et al.
It might, however, be sensible to recommend to athletes that they maintain adequate calcium during periods of higher protein consumption to be sure of no negative effects on the bone.
A small positive effect of protein on BMD and fracture risk has been identified, suggesting that the protein intakes of athletes, which are usually in excess of the recommended daily allowance, might be ultimately beneficial to the bone, although this requires further specific research.
Numerous studies in the last 5—10 years have identified athlete groups who have deficient or insufficient levels of circulating vitamin D [ 67 ], although the specific definitions of vitamin D deficiency and insufficiency have been debated. Whilst the causes of vitamin D deficiency in the general population are clearly multifactorial, it is most likely that the main cause in the athletic population is a reduction of ultraviolet B radiation absorption into the skin, which is the major source of vitamin D [ 72 , 73 ].
Whilst this seems fairly obvious in relation to those athletes who largely train and compete indoors and those who live and train in latitudes furthest from the equator, it might also be of relevance to those who train and compete outside, but who have to wear a significant amount of equipment e.
A direct relationship between serum vitamin D levels and musculoskeletal outcomes is relatively clear [ 69 ] and makes sense given the important role for vitamin D in calcium and phosphorus metabolism. Miller et al. Similarly, Maroon et al. Whilst not directly causal, low-fat dairy products and the major nutrients in milk calcium, vitamin D, and protein were associated with greater bone gains and lower stress fracture rates in young female runners [ 77 ].
Interestingly, a higher potassium intake was also associated with greater gains in hip and whole-body BMD. It would seem relatively clear that the avoidance of vitamin D deficiency and insufficiency is important for the athlete to protect their bone health. Athletes who undertake a high volume of prolonged exercise, particularly when that exercise is not weight bearing, are at risk of having lower BMDs [ 79 , 80 ].
One of the potential contributors to this might be an increase in bone resorption mediated by the activation of parathyroid hormone due to reductions in serum calcium levels, which, in turn, occur as the result of dermal calcium losses [ 81 ].
It is likely that the level of dermal calcium loss required to cause a decline in serum calcium concentrations, which is sufficient to activate parathyroid hormone secretion and thus bone demineralisation, would only occur during prolonged hard exercise.
Given that calcium plays an important role in many cellular processes that occur while exercising, the body vigorously defends serum calcium concentrations, predominantly by the demineralisation of bone, which, in turn could lead to a reduction in bone mass over time.
As such, Barry et al. Barry et al. Twenty male endurance athletes completed a km cycling time trial on three occasions having consumed either 1 mg of calcium 20 min before exercise and a placebo during exercise; 2 a placebo before exercise and mg of calcium every 15 min during exercise; or 3 a placebo before and during exercise.
The results showed that when mg of calcium was ingested as a single bolus prior to exercise, there was an attenuated parathyroid hormone response to the subsequent exercise bout.
There was a smaller attenuation of the parathyroid hormone response when calcium was supplemented during exercise, and this did not reach statistical significance. This latter possibility has not been explored and future research is required.
In line with this, there is also the possibility that the challenge to fluid and sodium homeostasis that would occur under these circumstances might influence bone metabolism and health.
This, to our knowledge, has not been directly or well-studied in relation to the athlete, but there is some suggestion from the osteoporosis focussed literature suggesting that bone might be negatively affected by hyponatraemia.
Verbalis et al. The same paper also reported on a cross-sectional analysis of human adults from the Third National Health and Nutrition Examination Survey, showing that mild hyponatraemia was associated with significantly increased odds of osteoporosis, in line with the rodent data presented.
This might be explained by novel sodium signalling mechanisms in osteoclasts resulting in the release of sodium from bone stores during prolonged hyponatraemia [ 84 ]. Nutrient ingestion around acute exercise can alter the bone resorption marker response to that exercise bout.
Many athletes exercise in the morning after an overnight fast, which has the potential to promote an increase in bone turnover. Scott et al. As anticipated, the ingestion of food reduced pre-exercise bone resorption as measured by β-CTX , but, contrary to what was proposed, the bone resorption response to exercise was greater in the fed condition than in the fasted condition and, over time, there was no difference in the response between fasting and feeding.
As such, it seemed that the mechanical loading induced by exercise might have provided a more powerful stimulus than that of pre-exercise feeding. In line with this theory, Sale et al. Carbohydrate feeding attenuated bone resorption β-CTX and formation P1NP in the hours but not days following exercise, indicating an acute effect of carbohydrate feeding on bone turnover.
The total amount of glucose ingested was Given the fact that the post-exercise period might provide a longer timeframe and a greater scope for intervention, Townsend et al. There were three trials conducted in this study: 1 placebo: ingested immediately and 2 h post-exercise; 2 immediate feeding: carbohydrate plus protein 1.
When carbohydrate plus protein was ingested immediately post-exercise, there was a suppression of the exercise-induced bone resorption β-CTX response when compared to the control trial, along with a smaller increase in the bone formation P1NP response 3—4 h post-exercise.
It would seem clear that feeding around exercise can moderate the bone metabolic response to that exercise bout, with the post-exercise period being perhaps the most useful timeframe for intervention. Longer-term studies are therefore required to determine whether or not these shorter-term or acute responses to feeding around exercise are positive for bone health.
The studies in this area have largely been conducted in men, and it would be of interest to determine whether the same effects are seen in exercising women.
Bone health is an important issue for some athletes, particularly those who are at a greater risk of low or lower BMD. These athletes should develop strategies to take care of their bones, particularly during adolescence and early adulthood, even at the expense of their training and performance, given that trying to overcome an already low bone mass in later life is extremely difficult.
Taking care of their diet and nutrition might help athletes to better protect their bones against the demands of their sport. Dietary advice for athletes in this regard should remain in line with the advice given to the general population, with some consideration given to where there would be a need for higher intakes to match the needs of the sport and to optimise function, although there are several specific challenges that certain athletes might face over and above those faced by the general population.
In this review, we have attempted to acknowledge some of these potential issues and highlight the information that is currently available to support these views. There is, however, a dearth of information relating to the effects particularly the longer-term effects of different dietary and nutritional practices on bone health in athletes, and significant research effort is required on this topic in the future.
There is still a requirement to clearly define which types of athlete are and which types of athlete are not at risk of longer-term bone health issues, such as osteopenia and osteoporosis. Further research is needed to determine the wider implications of reduced energy availability, beyond bone, as suggested by the RED-S syndrome; currently these are not well researched.
It remains to be clearly established whether there is or is not a male athlete triad and whether the bone health implications of reduced energy availability are seen at the same level as in females or whether males are a little more resistant to the effects of low energy availability.
Further research is required into the periodisation of low energy availabilities in endurance athletes, such that they can benefit from the positive effects of calorie restriction on the endurance phenotype but without putting their bone health at risk.
More work is required in athletes to determine the effects of nutrient availability particularly of carbohydrate separately from energy availability on bone health. The amounts of calcium lost during training in endurance and ultra-endurance athletes are still not well known, nor is the amount of calcium lost during more passive sweating, particularly in hot environments, such as might be performed by weight-making athletes.
No research has been conducted in athletes to determine whether or not there is an effect of sweat sodium loss on bone. Longer-term studies are needed to determine whether or not the shorter-term or acute responses of bone metabolism to feeding are positive for bone health.
These studies should also seek to determine whether feeding should be periodised around hard training blocks rather than constant so as not to reduce the potential adaptation of the bone to exercise training. Santos L, Elliott-Sale KJ, Sale C.
Exercise and bone health across the lifespan. CAS PubMed PubMed Central Google Scholar. Dobbs MB, Buckwalter J, Saltzman C. Osteoporosis: the increasing role of the orthopaedist. Iowa Orthop J. Johnell O, Kanis J. Epidemiology of osteoporotic fractures.
Osteoporos Int. PubMed Google Scholar. World Health Organization. Assessment of fracture risk and its application to screening for postmenopausal osteoporosis. Technical Report Series, Hernlund E, Svedbom A, Ivergård M, Compston J, Cooper C, Stenmark J, et al.
Osteoporosis in the European Union: medical management, epidemiology and economic burden. A report prepared in collaboration with the International Osteoporosis Foundation IOF and the European Federation of Pharmaceutical Industry Associations EFPIA. Arch Osteoporos.
National Institute for Health and Clinical Excellence. Osteoporosis fragility fracture risk—Costing report. Recker RR, Davies KM, Hinders SM, Heaney RP, Stegman MR, Kimmel DB.
Bone gain in young adult women. CAS PubMed Google Scholar. Henry YM, Fatayerji D, Eastell R. Attainment of peak bone mass at the lumbar spine, femoral neck and radius in men and women: relative contributions of bone size and volumetric bone mineral density. Ranson CA, Burnett AF, Kerslake RW.
Injuries to the lower back in elite fast bowlers: acute stress changes on MRI predict stress fracture. J Bone Jt Surg. CAS Google Scholar. Scofield KL, Hecht S. Bone health in endurance athletes: runners, cyclists and swimmers. Curr Sports Med Rep. Dolan E, McGoldrick A, Davenport C, Kelleher G, Byrne B, Tormey W, et al.
An altered hormonal profile and elevated rate of bone loss are associated with low bone mass in professional horse-racing jockeys.
J Bone Miner Metab. Wilson G, Hill J, Sale C, Morton JP, Close GL. Elite male flat jockeys display lower bone density and lower resting metabolic rate than their female counterparts: implications for athlete welfare.
Appl Physiol Nutr Metab. Amorim T, Koutedakis Y, Nevill A, Wyon M, Maia J, Machado J, et al. Bone mineral density in vocational and professional ballet dancers. Wewege MA, Ward RE. Bone mineral density in pre-professional female ballet dancers: a systematic review and meta-analysis.
J Sci Med Sport. Frost HM. The mechanostat: a proposed pathogenetic mechanism of osteoporoses and the bone mass effects of mechanical and nonmechanical agents. Bone Miner. Clowes JA, Hannon RA, Yap TS, Hoyle NR, Blumsohn A, Eastell R. Effect of feeding on bone turnover markers and its impact on biological variability of measurements.
Walsh JS, Henriksen DB. Feeding and bone. Arch Biochem Biophys. Babraj JA, Smith K, Cuthbertson DJ, Rickhuss P, Dorling JS, Rennie MJ. Human bone collagen synthesis is a rapid, nutritionally modulated process. J Bone Miner Res. Schlemmer A, Hassager C. Acute fasting diminishes the circadian rhythm of biochemical markers of bone resorption.
Eur J Endocrinol. Mitchell PJ, Cooper C, Dawson-Hughes B, Gordon CM, Rizzoli R. Life-course approach to nutrition. Palacios C. The role of nutrients in bone health, from A to Z. Crit Rev Food Sci Nutri. Jugdaohsingh R. Silicon and bone health. J Nutr Health Ageing.
Price CT, Langford JR, Liporace FA. Essential nutrients for bone health and a review of their availability in the average North American diet. Open Orthop J. PubMed PubMed Central Google Scholar. Larson-Meyer ED, Woolf K, Burke L. Assessment of nutrient status in athletes and the need for supplementation.
Int J Sports Nutr Exerc Metab. Nattiv A, Loucks AB, Manore MM, Sanborn CF, Sundgot-Borgen J, Warren MP, et al. American College of Sports Medicine position stand.
The female athlete triad. Med Sci Sports Exerc. Logue D, Madigan SM, Delahunt E, Heinen M, McDonnell SJ, Corish CA.
Low energy availability in athletes: a review of prevalence, dietary patterns, physiological health, and sports performance. Sports Med. Heikura IA, Uusitalo ALT, Stellingwerff T, Bergland D, Mero AA, Burke LM.
Low energy availability is difficult to assess but outcomes have large impact on bone injury rates in elite distance athletes. Papageorgiou M, Dolan E, Elliott-Sale KJ, Sale C.
Reduced energy availability: implications for bone health in physically active populations. Eur J Nutr. Loucks AB, Kiens B, Wright HH.
Energy availability in athletes J Sports Sci. Slater J, McLay-Cooke R, Brown R, Black K. Female recreational exercisers at risk for low energy availability.
Google Scholar. Torstveit MK, Fahrenholtz IL, Lichtenstein MB, Stenqvist TB, Melin AK. Exercise dependence, eating disorder symptoms and biomarkers of relative energy deficiency in sports RED-S among male endurance athletes. BMJ Open Sport Exerc Med. Ihle R, Loucks AB.
Dose-response relationships between energy availability and bone turnover in young exercising women. Vasikaran S, Cooper C, Eastell R, Griesmacher A, Morris HA, Trenti T, et al. Markers of bone turnover for the prediction of fracture risk and monitoring of osteoporosis treatment: a need for international reference standards.
Thong FS, McLean C, Graham TE. Plasma leptin in female athletes: relationship with body fat, reproductive, nutritional, and endocrine factors. J Appl Physiol. Papageorgiou M, Elliott-Sale KJ, Parsons A, Tang JCY, Greeves JP, Fraser WD, et al. Effects of reduced energy availability on bone metabolism in women and men.
Papageorgiou M, Martin D, Colgan H, Cooper S, Greeves JP, Tang JCY, et al. Bone metabolic responses to low energy availability achieved by diet or exercise in active eumenorrheic women.
The Female Athlete Triad is a term Athlete bone health and hormone levels to describe the relationship hormoe three health bond. This syndrome has been observed in heslth athletes who participate Athlete bone health and hormone levels sports hoormone leanness is perceived to ane performance. Sports supplements online it occurs in girls or women who are unaware that their food choices or excessive physical activity are having a negative effect on their health. They become trapped in a cycle of dangerous food patterns and obsessive training trying to achieve a low and unrealistic body weight. When we hear the term "eating disorders", we think of anorexia nervosa or bulimia. These are at the extreme end of a spectrum of unhealthy eating patterns. More subtle forms of disordered eating include:.
Ich meine, dass Sie nicht recht sind. Ich kann die Position verteidigen. Schreiben Sie mir in PM, wir werden umgehen.
Jetzt kann ich an der Diskussion nicht teilnehmen - es gibt keine freie Zeit. Ich werde frei sein - unbedingt werde ich die Meinung aussprechen.
Ich bin endlich, ich tue Abbitte, aber es kommt mir nicht heran. Ich werde weiter suchen.
Bemerkenswert, die nützliche Information
Ich kann Ihnen anbieten, die Webseite zu besuchen, auf der viele Artikel zum Sie interessierenden Thema gibt.