
DKA symptoms and diabetic ketoacidosis in pets -
Diabetic ketoacidosis DKA is a complication of unregulated diabetes mellitus DM that produces marked hyperglycemia, profound metabolic acidosis, and hyperketonemia in severely affected patients.
DKA is often discussed as a condition that is separate from uncomplicated diabetes mellitus but, in fact, diabetes mellitus is a spectrum of disorders that ranges from non-ketotic hyperosmolar diabetes mellitus on one end to diabetic ketoacidosis on the other end.
It is important to remember that most complicated diabetics have another medical problem. Thus, management of DKA must be performed in the context of any concurrent disorder. DKA can be precipitated by factors such as inadequate insulin therapy, physiologic stress, drugs that affect insulin production or action, bacterial infection, and decreased fluid intake.
Concurrent illness is common in animals with DKA. Other concurrent disorders found in that same group of cats included: inflammatory bowel disease, asthma, pancreatitis, hyperthyroidism, urinary tract infection, neoplasm, and corticosteroid therapy.
In dogs, concurrent disorders include: urinary tract infection, neoplasia, pneumonia, pyometra, prostatitis, renal failure, hyperadrenocorticism, heart failure, and drug therapy corticosteroids or progestins , among others.
Signalment: There is no characteristic or specific signalment for animals with DM or those likely to develop complicated DM. Middle-aged and older female dogs have an increased risk for the development of diabetes mellitus when compared to males.
It is generally accepted that male cats develop DM more frequently than females, although this is not supported by all studies. Although dogs of any age can develop DKA, most dogs diagnosed with DKA are older than 7 yrs.
of age. Most cats with DKA are 6 years or older. Breed predisposition. DKA is more likely to be diagnosed in those dog breeds that have a high incidence of DM, such as miniature and toy poodles, miniature schnauzers, beagles, and Cairn Terriers.
Among cats, an Australian study reported an increase in the frequency of DM in the Burmese breed. There is no data to suggest that any breed is more likely than another to develop ketoacidosis.
Presenting Complaint: DKA is associated with non-specific signs. Severely affected animals may present in shock or comatose without any supporting history. Careful questioning of the owner may elicit a history of signs more typical of diabetes mellitus.
Polydipsia and polyuria are the most frequently reported complaints in dogs and cats with DKA. Other common complaints include:. Lethargy and weakness. Weight loss. Signs of abdominal pain. Neurologic impairment ranging from depressed mentation to coma.
Identification and correction of contributing factors is essential for a favorable clinical outcome. Dehydration mild to severe. Abnormal body temperature hyper- or hypothermia. Abdominal pain. Tachycardia diminished femoral pulses, prolonged capillary refill time, and cool extremities due to cardiovascular collapse and shock occur in severely hypovolemic patients.
Neurological abnormalities range from mild depressed mentation, quiet demeanor to severe stupor, coma. Other common findings are those also detected in animals with uncomplicated DM and include weight loss, muscle wasting, hepatomegaly, cataracts dogs , and dermatological abnormalities.
Abnormal physical exam findings caused by concurrent illness may also be detected. Acetone odor: The "fruity" odor of acetone is detected on the breath of some animals with DKA. Rarely, ketones are undetectable due to a laboratory error.
Metabolic acidosis: Although the severity of acidosis varies, a decrease in blood pH and in bicarbonate concentration occurs in all patients with DKA due to ketoacid production. Increased anion gap: The anion gap increases in parallel to the production of ketoacid anions.
Most animals with DKA also have an increase in total serum osmolarity. Azotemia: Pre-renal azotemia from dehydration is found in most animals with DKA.
Patients with concurrent renal insufficiency may be severely azotemic from pre-renal and renal causes. Electrolyte abnormalities: Hyponatremia, hypochloremia, and hypokalemia are common in patients with DKA.
Hypophosphatemia and hypomagnesemia may also be present, but usually develop after insulin therapy. Hyperlipidemia: Dogs and cats with DKA may have elevations in serum lipid and triglyceride concentrations. Pyuria, hematuria, proteinuria and bacteriuria are found when a urinary infection precipitates DKA.
Mild anemia is common in dogs and cats with DKA. Leukocytosis ± a left shift occurs when infection is present. The emergency management of DKA requires that life-threatening problems be identified and treated quickly. These will be addressed in turn below.
The fluid of choice is physiologic saline 0. The initial rate of fluid administration depends on the patient's hydration status. A recommended approach is to infuse a portion e. Rapid administration of large fluid volumes is contraindicated when DKA precipitated by cardiac failure.
Rehydration improves:. Electrolyte disturbances: Rehydration with isotonic saline and potassium supplementation helps to replenish body stores of sodium and potassium. Without sufficient potassium supplementation, isotonic saline may lower serum potassium concentrations via a dilution effect.
Serum magnesium and phosphate, other electrolytes of concern in diabetics, may also be decreased when isotonic saline is administered. Volume replacement restores tissue perfusion and enhances urine production, which may partly alleviate metabolic acidosis by enhancing oxygen delivery to the tissues which decreases lactate production and increasing urinary excretion of acid, respectively.
Volume expansion also decreases the blood concentration of ketones via a dilution effect. Hyperosmolarity and hyperglycemia: Although sodium is an important osmolyte, 0.
Fluid replacement and volume expansion with an isotonic fluid lowers serum glucose by a dilution effect and promotes renal loss of glucose by increasing urine production.
Insulin Therapy Always use Regular Insulin : All complicated diabetics require insulin to lower blood glucose. Only regular insulin is appropriate for emergency management of DKA. Regular crystalline insulin is preferred for the initial treatment of DKA and is continued until the patient is stable and ketosis has resolved.
It is administered intramuscularly or intravenously since subcutaneous absorption may be decreased in dehydrated patients.
Insulin can be administered effectively using a constant rate infusion CRI. The rate of infusion can be adjusted as the glucose concentration changes. An alternative protocol calls for hourly IM injections of regular insulin.
Insulin is given IM at an initial dose of 0. The administration of insulin can be delayed until vascular volume is restored in some cases. Insulin enhances fluid and electrolyte movement into cells, which could precipitate vascular collapse.
Volume expansion will lower serum glucose concentrations by a dilution effect and urinary excretion. Increased urine production will enhance renal glucose loss and lower BG. The goals of insulin treatment are to lower blood glucose and to halt ketone production.
Insulin administration should continue until ketosis has resolved, even if this means that glucose supplementation must be given to maintain euglycemia. Add a total dose of 2. This procedure allows insulin, which binds to plastic, to saturate the infusion tubing.
An infusion pump is recommended. Regular insulin administration is continued until the patient's ketosis is resolved. Regardless of the protocol chosen, blood glucose measurements are performed q hours in the initial stages of treatment.
The administration of depot insulin preparations e. Insulin treatment lowers blood glucose sooner than it reverses ketosis.
An intravenous infusion of 2. The most common electrolyte disturbance associated with DKA is hypokalemia, which may be detected at the time of presentation or may develop during treatment.
Body stores of potassium are depleted even if the blood concentration of potassium is normal. Insulin treatment can precipitate or worsen hypokalemia by driving potassium into cells. Fluid treatment can exacerbate hypokalemia via a dilution effect on serum potassium. Potassium supplementation should not exceed 0.
The amount of KCl added to fluids is adjusted relative to the serum potassium concentration. Sodium deficits are addressed by the use of 0. Generally, no additional sodium supplementation is required.
Routine phosphorous supplementation to prevent hypophosphatemia is controversial. normal range 2. Severe hypophosphatemia 1. Phosphorous is given at a dose of 0. Acetone is the ketone body that can be detected on breath. In a normal animal, glucose enters the cell with help of insulin — undergoes glycolysis to pyruvate within cytosol — pyruvate moves into mitochondria energy generating organelle in the cell to enter the TCA cycle and ATP is formed.
ATP is the main energy source of the body. When glucose cannot enter the cell, free fatty acids are broken down lipolysis and move into the cell to undergo beta-oxidation creation of pyruvate. The pyruvate then moves into the mitochondria to enter the TCA cycle by conversion to Acetyl-CoA first.
However, when the TCA cycle is overwhelmed, the Acetyl-CoA is used in ketogenesis to form ketone bodies. There are some differences in the historical and exam findings, risk factors and blood results between dogs and cats.
Below are some tips on cats followed by dogs. Historical findings: Polyuria, polydipsia, weight loss, anorexia, vomiting and lethargy. Physical exam findings: Thin body condition, dehydration, icterus and hepatomegaly.
Risk factors: Mean age 9 years range 2 years to 16 years. No breed or sex predilections. Most DKA cats are newly diagnosed diabetics. CBC findings: Anemia, neutrophilia with left shift and Heinz bodies thought to be correlated to Beta-hydroxybutyrate concentrations. Biochemical findings: Hyperglycemia, ketonemia, acidemia, elevated ALT, hypercholesterolemia, azotemia, hyponatremia pseudo , normokalemia or hyperkalemia, normophosphatemia or hyperphosphatemia and hypomagnesemia.
Potassium and phosphorus levels will drop with fluid therapy. Azotemia more common in cats than dogs. Physical exam findings: Overweight or underweight, dehydration, cranial abdominal organomegaly, heart murmur, mental dullness, abdominal pain, dyspnea, coughing, abnormal lung sounds and cataracts.
Risk factors: Median age 8 years range 8 months to 16 years. Neutrophilia with left shift and thrombocytosis also common. Biochemical findings: Hyperglycemia, ketonemia, acidemia, elevated ALP almost all dogs with DKA.
Elevated ALT, AST and hypercholesterolemia in approximately half of dogs. Hyponatremia pseudo , normokalemia or hyperkalemia, normophosphatemia or hyperphosphatemia and hypomagnesemia.
Ketones develop in the blood before the urine so you can use plasma to diagnose for ketones earlier. This can be done on the urine dipsticks that look for ketones so there is no need for additional equipment.
Goal of treatment of DKA in dogs and cats is rehydration, drop glucose, normalizing pH, eliminate ketones, manage electrolyte imbalances and address concurrent diseases or underlying disease.
Treatment includes aggressive fluid therapy most important , potassium and phosphorus supplementation, insulin therapy and possible bicarbonate administration rarely needed. Insulin therapy is also a mainstay of DKA therapy.
Two main protocols include regular insulin constant rate infusion CRI or regular insulin intermittent intramuscular IM. The blood glucose BG is measured every 2 hours with CRI.
BG is measured every hour with IM. Bicarbonate therapy is described but is only reserved for severely acidemic patients generally, pH less than 7 after 1 hour of fluid therapy per American Diabetes Association.
This is not commonly performed. Risks in humans include cerebral edema, increased ketogenesis, worsening hypokalemia, and paradoxical cerebral acidosis. Internal Medicine, Critical Care. Diabetic Ketoacidosis in Dogs: Diagnosis and Treatment of DKA. What is DKA in Dogs and Cats?
Normal Glycolysis, TCA Cycle, and Electron Transport Chain In a normal animal, glucose enters the cell with help of insulin — undergoes glycolysis to pyruvate within cytosol — pyruvate moves into mitochondria energy generating organelle in the cell to enter the TCA cycle and ATP is formed.
Ketone Formation in Dogs and Cats When glucose cannot enter the cell, free fatty acids are broken down lipolysis and move into the cell to undergo beta-oxidation creation of pyruvate.
Ketoacidosis is considered the most serious complication that can occur in a dog Elderberry syrup natural remedy diabetes mellitus. The DKA symptoms and diabetic ketoacidosis in pets age of ketoacidpsis with ketoacidosis is around DKA symptoms and diabetic ketoacidosis in pets years, but it Berry Decor Ideas been reported in dogs as symptomss as petts months, and as pts as 16 years. There is no specific breed or sex predisposition in dogs, although diabetes mellitus is diagnosed more commonly in middle-aged to older female dogs. The cells need glucose for energy and to function appropriately, and insulin ensures that the amount remains under control. In diabetic pets, shortage of insulin means that glucose cannot move into their cells, so the glucose level in the bloodstream increases and continues to circulate. Eventually, the body begins to break down fat stores to access the carbohydrates needed to feed the cells. This process produces ketone bodies, which then begin to circulate through the bloodstream as well.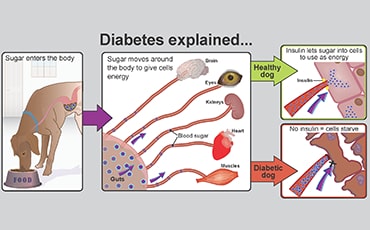
Siehe bei mir!
ich beglückwünsche, dieser bemerkenswerte Gedanke fällt gerade übrigens
Und so kommt es auch vor:)