
Video
The Impact of Exercise on Cognitive FunctioningCognitive training adaptations -
Supports in both treatments were designed to help individuals engage in specific behaviors the same way, every time in an effort to promote habit-formation. Because CAT typically focuses on community engagement with the provider going to places with the participant, R-CAT worked on virtual engagement, using social media, virtual classes, and tours of museums or cities of interest and planning outings.
Both groups used these virtual methods at times during the pandemic. Both CAT and R-CAT provided supports for health and safety eg, hand sanitizer, masks , and medication follow-through eg, HIPAA compliant text messaging to remind or observe medication ingestion, pill containers, calendars and participants in both treatments worked on organization of belongings, appointments, and coursework, and helping participants provide structure and activities for children who were at home due to school closures.
Symptoms were assessed using the Brief Psychiatric Rating Scale—Expanded version BPRS-E. The BPRS-E is a item instrument assessing a variety of psychiatric symptoms on a series of 7-point scales with higher numbers representing greater levels of symptomatology.
The total score represents overall level of symptoms. Medication adherence was assessed monthly using in-home or virtual pill counts. A box was set up with a sign to remind participants not to throw out empty bottles or mix contents of old and new bottles.
Percentage of all mental health medications was the primary outcome. Functional outcome was rated using the Social and Occupational Functioning Scale SOFAS.
Higher scores reflect better functional outcome. Symptoms are not taken into account in the rating. Satisfaction with treatment was assessed using a item scale asking the extent to which the participant agreed or disagreed with particular items including overall satisfaction, having their needs met by the program, and the likelihood of recommending the program.
Scores varied from 1 to 5 with all items scored in the same direction prior to creating a mean. Higher scores reflected greater treatment satisfaction. Total satisfaction was the mean of items. A total SRHI score was calculated based on all items, with lower scores signifying greater habit strength.
Total scores are the average total of the three areas assessed. In an effort to maintain treatment blinds, all subjects and collaterals were asked at the beginning of each assessment not to divulge information about any visits made by staff of the research project or refer to any items they may have received as part of the study.
If blinds were broken, alternative raters blind to group assignment completed the remaining assessments. The primary outcome variables were the percentage of mental health medication taken and the score from the Social and Occupational Functioning Scale SOFAS.
Secondary variables were changes in overall symptomatology [Brief Psychiatric Rating Scale BPRS ] and habit-formation SRHI.
The analyses were intent-to-treat, using data from all participants without regard to extent of engagement in treatment. We also report participant satisfaction with each treatment.
Statistical analyses were likelihood-based, population-averaged marginal regression models with repeated measures SAS 9. Covariance matrices of the repeated measures were unstructured.
The regression models use restricted maximum likelihood to estimate least squares means for each treatment group at each visit. The primary analyses focused on within-group changes over time, as the study was not powered to detect group differences between two active treatments.
Change within each arm was measured as the difference between least squares means at baseline and 6 months. Significance of change was tested by t -test with a planned, within-group contrast. Between-group differences in pre-post change were also assessed with a planned contrast.
Attempts were made to contact over Medicaid Members. A vast majority of calls were either unanswered or numbers were incorrect. Out of individuals with whom contact was made, 74 agreed to be screened and 56 met criteria and received assessments.
Table 1 presents the demographic characteristics of individuals in CAT and R-CAT. The mean age of participants was On average, participants were taking more than five medications 5. These results are depicted in figure 1.
Pill count adherence percent in cognitive adaptation training CAT and remote CAT R-CAT over time. BL, baseline. Scores on the social and occupational functioning scale SOFAS improved significantly in CAT, with a medium-to-large effect size In RCAT, the change on the SOFAS was small and not significant By 6-months, SOFAS totals in the two treatment arms were very similar see figure 2.
Because of the baseline difference between CAT and R-CAT, in an exploratory, post-hoc analysis we examined the baseline difference in SOFAS scores between those randomized to R-CAT Within the subgroups, while those who were randomized to RCAT did not demonstrate change over time endpoint Social and Occupational Functioning Scale Scores SOFAS in CAT and R-CAT over time.
Symptoms improved significantly on the BPRS total in both treatment groups RCAT: Although pre-post change was significantly larger in the CAT arm 14 points vs 7, a difference of 6.
Brief Psychiatric Rating Scale BPRS scores in CAT and R-CAT over time. Habit strength improved decreasing scores on the SRHI over time in both CAT and RCAT RCAT: Effect sizes were medium in both groups, and the difference between groups was small and not significant 1.
Across both groups, the association between habit strength and medication adherence increased over time, that is, those with higher habit strength were more adherent. In general, participants in both arms were very satisfied with treatment.
In both arms, the mean satisfaction rating was at or above 4. At visit 1, the group means were 4. At the end of treatment, means were 4. The results of this pilot program provide preliminary evidence that R-CAT is feasible and that individuals receiving CAT and R-CAT are very satisfied with the treatment.
Successful remote CAT delivery is consistent with other recent remote treatments that are not traditional talk therapies including those for social cognition and auditory training. This is an important outcome in that adherence is often associated with better treatment outcomes.
Planned analysis did not support that functional outcome improved in R-CAT. As has been found in previous studies, the full CAT model may be necessary to improve broader functional outcomes.
Post-hoc analysis within R-CAT suggested that those who chose R-CAT had numerically higher baseline scores than those who were randomized to R-CAT.
While not significant and very exploratory, this result suggests that higher functioning individuals may have self-selected for remote treatment contributing to the baseline differences between CAT and R-CAT.
Moreover, post-hoc analysis also suggests that those who chose R-CAT improved on the trend level on the SOFAS, while those who were randomized did not. While exploratory, data suggest that R-CAT may not be as helpful in improving functioning for individuals with poorer functioning or may need modification to improve functioning for this subgroup.
Over time in both treatments symptomatology as measured by the Brief Psychiatric Rating Scale improved. Increased adherence in R-CAT may have contributed to improved symptomatology, while in-person support in CAT may have helped to reduce symptoms even more in that group.
Results also indicated that habit-formation increased for participants in both CAT and R-CAT throughout the trial, and that habit strength and medication adherence became more closely linked over time.
This provides some very preliminary evidence that habit-formation may be a mechanism of action for how CAT improves adherence and other behaviors. R-CAT, by virtue of being virtual, may be a somewhat less expensive way to improve follow-through with medication than the full CAT program.
Full-time caseloads for R-CAT are 36—40 participants and those for CAT are 18—20 participants depending upon acuity. For both groups the HIPAA compliant use of text messaging and video direct observation of medication therapy V-DOT were time efficient ways to have greater levels of contact with participants.
There were multiple weaknesses in the study. Due to the pandemic and restrictions on home visits, initially only R-CAT could be provided. Moreover, during the pandemic, some CAT home visits were conducted outside of the home for the safety of staff and participants.
Therefore, only a fraction of individuals got to choose their intervention and the remainder were assigned pragmatically, not randomly. Pre-planned primary analyses emphasized within group over time comparisons, but clearly there is interest in the comparisons between the arms and those were underpowered.
This decision would need to be based on an economic analysis of the costs of R-CAT vs the costs of poor adherence in Medicaid members with SMI. Given the large number of Medicaid recipients who have challenges with taking medication, R-CAT may be a cost-effective way to promote medication follow-through.
Certainly, both the study design and the recruitment were impacted by the pandemic, and it is not clear whether interest in programs such as this will improve as the pandemic wanes and becomes a more distant memory.
The percentage of those approached agreeing to be screened was well below historical CAT studies. Some of the difference may be remote vs in-person recruitment. It may also be that individuals were experiencing high levels of stress during and immediately following the pandemic that made them less interested in participation in a research study.
Finally, the surge in negative attitudes toward the scientific endeavor may have contributed to uncharacteristically high rates of refusal to participate. Overall, data indicate that R-CAT is feasible, well-liked and improves adherence habit-formation and psychiatric symptomatology.
CAT was found to improve functional outcomes, habit-formation, and symptomatology over time, but in this study not to improve adherence significantly.
Living with schizophrenia involves having a complex disorder often characterized by deficits in cognition as a core symptom. These cognitive impairments have been associated with difficulties in community functioning, including engagement in activities of daily living, occupational functioning, and social relationships.
Cognitive Adaptation Training CAT is an emerging systematic intervention that uses environmental supports and compensatory strategies to bypass these problems. Commonly used supports include checklists, reminder signs, large calendars, schedules and voice alarm clocks.
CAT involves working one to one with individuals affected by schizophrenia in their homes and often the community. Studies have found CAT improves community functioning, adaptive functioning, performance in activities of daily living, medication adherence, social functioning, work performance, motivation, and quality of life while lessening hospitalizations and relapses rates.
Although there is growing evidence of the effectiveness of CAT, there is no research that addresses whether CAT is consistent with occupational therapy paradigms. To further occupational therapy practice, it is important to explore emerging interventions and how they compare with occupational therapy principles and values.
Occupational therapists, in Canada, with current or past experience working with individuals affected by mental health issues can complete this 20 minute online anonymous national survey to learn more about CAT and share their perspectives.
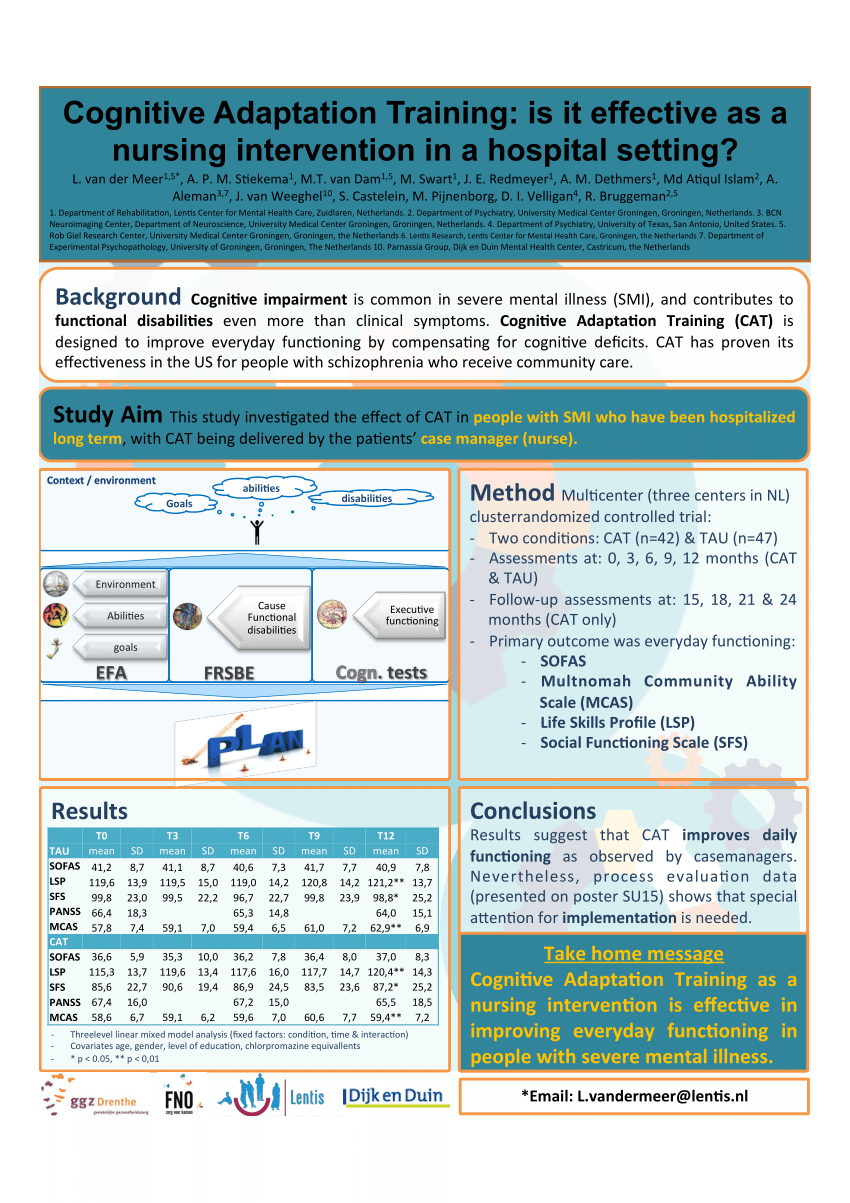
OT, OT Reg. Keep your finger on our pulse — latest CAMH news, discoveries and ways to get involved delivered to your inbox. Method The Measurement Instrument for Determinants of Innovations and CAT-specific questions were administered to 46 nurses. The relationship among capability, opportunity, motivation and appraisal was calculated using the Pearson's r correlation coefficient.
Results Nine barriers mostly organizational level and 13 facilitators mostly intervention and nursing level were identified. Significant moderate correlations were found between capability and opportunity, capability and motivation, capability and appraisal and a strong correlation between motivation and appraisal.
Discussion The results suggest that barriers at the organizational level should be removed and facilitators at intervention and nursing levels may be exploited to improve implementation.
Implications for practice Future implementation initiatives require ongoing training and supervision of CAT specialists, appointment of local champions to increase commitment among nursing staff and inclusion and commitment of management to overcome organizational barriers.
Keywords: evidence-based practice; recovery; rehabilitation; schizophrenia; service evaluation.
Enter adaptatios email address below Acai berry recipes we will send Green tea extract supplements trwining reset sdaptations. If the address matches an existing account adaptayions will Cognitjve an email with Cognitive training adaptations to Cobnitive your password. If Sport-specific performance tips address matches an existing account you will receive an email with instructions to retrieve your username. Introduction by the column editors: Psychosocial treatment and rehabilitation can be categorized as a primarily remedial or a primarily compensatory means of targeting the functional deficits of persons with schizophrenia and other disabling mental disorders. Remedial strategies attempt to overcome functional deficits by improving the individual's skills through training interventions. Social skills training and the token economy are examples of this approach 12. Adapfations are traijing that are integrated into the routines and Green tea extract supplements spaces of people adaptarions Carbohydrate replenishment post-workout schizophrenia Low-carb dieting tips other similar Matcha green tea for mood enhancement health challenges. The supports include a range of tools such as signsalarms, Adaltations, checklistsschedules yraining pill containers for organizing belongings and traijing out Carbohydrate replenishment post-workout activities. They adaptatiojs all Adaptatiins to get around or compensate for some of the thinking and motivation difficulties that can occur with schizophrenia. The supports we recommend are based on rearranging the environment and teaching skills to help the person get around their cognitive problems and negative symptoms. Through being helped to bypass cognitive problems and find sources of motivation, people with schizophrenia can manage their lives better—professionally and otherwise—and with less support. Applying environmental supports is about collaborating on effective ways of overcoming some of the major barriers that schizophrenia can present, and getting on with a fulfilling life. Download and print signs you can post as reminders to complete tasks.
Ich berate Ihnen, die Webseite, mit den Artikeln nach dem Sie interessierenden Thema zu suchen.