Hypoglycemia and diabetes -
Unless it was the result of an easily remediable factor, such as a missed meal after insulin injection or vigorous exercise without the appropriate regimen adjustment, a substantive change in the regimen must be made.
If a change is not made, the risk of recurrent severe hypoglycemia is unacceptably high 1 , 2 , 35 , 66 , The fundamental problem with current treatment regimens is that they do not provide plasma glucose—regulated insulin replacement or secretion. The time course of the glucose-lowering actions of subcutaneous insulin, even the shortest acting analogues, is measured in hours whereas that of endogenous insulin in nondiabetic individuals is measured in minutes.
In addition to the imperfect pharmacokinetics of injected insulin, the pharmacodynamics of the sulfonylureas are such that they too can produce hyperinsulinemic hypoglycemia in responsive patients.
It remains to be determined whether the newer rapid-acting insulin secretagogues repaglinide and nateglinide will only enhance glucose-stimulated insulin secretion with a correspondingly low rate of hypoglycemia in those patients who achieve glycemic control.
Biguanides should not produce hypoglycemia, although they have been reported to do so. However, given absolute insulin deficiency in type 1 diabetes and progressive insulin deficiency over time in type 2 diabetes, most people with diabetes will ultimately require treatment with insulin, even with its pharmacokinetic imperfections.
In theory, glucose-regulated insulin replacement might be accomplished by pancreatic islet transplantation, a bioengineered artificial β-cell or a closed-loop insulin-replacement system. With respect to the latter, a reliable glucose sensor is the missing component Pending the prevention and cure of diabetes or the development of treatment methods that provide glucose-regulated insulin replacement or secretion, we need to learn to replace insulin in a much more physiological fashion; to prevent, correct, or compensate for compromised glucose counterregulation; or both if we are to achieve near-euglycemia safely in people with diabetes.
Diagrammatic representation of the concept of hypoglycemia-associated autonomic failure in diabetes. Modified from Cryer Address correspondence and reprint requests to Philip E. Cryer, MD, Division of Endocrinology, Diabetes and Metabolism, Washington University School of Medicine, Campus Box , South Euclid Ave.
Louis, MO E-mail: pcryer im. This paper was reviewed and approved by the Professional Practice Committee of the American Diabetes Association, October A table elsewhere in this issue shows conventional and Système International SI units and conversion factors for many substances.
Sign In or Create an Account. Search Dropdown Menu. header search search input Search input auto suggest. filter your search All Content All Journals Diabetes Care. Advanced Search. User Tools Dropdown. Sign In. Skip Nav Destination Close navigation menu Article navigation.
Volume 26, Issue 6. Previous Article Next Article. Article Information. Article Navigation. Hypoglycemia in Diabetes Philip E. Cryer, MD ; Philip E. Cryer, MD. Louis, Missouri. This Site. Google Scholar. Stephen N. Davis, MD ; Stephen N. Davis, MD. Harry Shamoon, MD Harry Shamoon, MD. Diabetes Care ;26 6 — Get Permissions.
toolbar search Search Dropdown Menu. toolbar search search input Search input auto suggest. Endogenous glucose production is decreased, such as following alcohol ingestion. Glucose utilization is increased, such as during exercise. Insulin clearance is decreased, such as with progressive renal failure.
Figure 1—. View large Download slide. Karen Muehlhauser prepared the manuscript. Cryer PE. Hypoglycaemia: The limiting factor in the glycaemic management of type I and type II diabetes. The Diabetes Control and Complications Trial Research Group: The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus.
N Engl J Med. The United Kingdom Prospective Diabetes Study Research Group: Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes.
The United Kingdom Prospective Diabetes Study Research Group: Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes. Cryer PE: Hypoglycemia. Pathophysiology, Diagnosis and Treatment. Stratton IM, Adler AI, Neil HAW, Matthews DR, Manley SE, Cull CA, Hadden D, Turner RC, Holman RR, the UKPDS Research Group: Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes: prospective observational study.
Khaw K-T, Wareham N, Luben R, Bingham S, Oakes S, Welch A, Day N: Glycated haemoglobin, diabetes, and mortality in men in Norfolk cohort of European Prospective Investigation of Cancer and Nutrition EPIC-Norfolk. Cryer PE, Childs BP: Negotiating the barrier of hypoglycemia in diabetes.
Diabetes Spectrum. Boland E, Monsod T, Delucia M, Brandt CA, Fernando S, Tamborlane WV: Limitations of conventional methods of self-monitoring of blood glucose. Diabetes Care. Gross TM, Mastrototaro JJ, Fredrickson LP: Detection of unseen hypoglycemia using continuous glucose monitoring Abstract.
Reichard P, Berglund B, Britz A, Cars I, Nilsson BY, Rosenqvist U: Intensified conventional insulin treatment retards the microvascular complications of insulin-dependent diabetes mellitus IDDM : the Stockholm Diabetes Intervention Study SDIS after 5 years.
J Intern Med. MacLeod KM, Hepburn DA, Frier BM: Frequency and morbidity of severe hypoglycaemia in insulin-treated diabetic patients.
Diabet Med. Laing SP, Swerdlow AJ, Slater SD, Botha JL, Burden AC, Waugh NR, Smith AW, Hill RD, Bingley PJ, Patterson CC, Qiao Z, Keen H: The British Diabetic Association Cohort Study. Cause-specific mortality in patients with insulin-treated diabetes mellitus. Roney L: Sweet Invisible Body: Reflections on a Life with Diabetes.
Abraira C, Colwell JA, Nuttall FQ, Sawin CT, Nagel NJ, Comstock JP, Emanuele NV, Levin SR, Henderson W, Lee HS: Veterans Affairs Cooperative Study on glycemic control and complications in type II diabetes: results of the feasibility trial.
Saudek CD, Duckworth WC, Giobbie-Hurder A, Henderson WG, Henry RR, Kelley DE, Edelman SV, Zieve FJ, Adler RA, Anderson JW, Anderson RJ, Hamilton BP, Donner TW, Kirkman MS, Morgan NA, the Department of Veterans Affairs Implantable Insulin Pump Study Group: Implantable insulin pump vs.
multiple-dose insulin for non-insulin-dependent diabetes mellitus: a randomized clinical trial. The United Kingdom Prospective Diabetes Study Group: U. prospective diabetes study. The United Kingdom Prospective Diabetes Study Research Group: A 6-year, randomized, controlled trial comparing sulfonylurea, insulin, and metformin therapy in patients with newly diagnosed type 2 diabetes that could not be controlled with diet therapy.
Ann Intern Med. Hepburn DA, MacLeod KM, Pell AC, Scougal IJ, Frier BM: Frequency and symptoms of hypoglycaemia experienced by patients with type 2 diabetes treated with insulin. Campbell IW: Hypoglycaemia and type 2 diabetes: sulphonylureas.
In Hypoglycaemia and Diabetes: Clinical and Physiological Aspects. Gerich JE: Oral hypoglycemic agents. Towler DA, Havlin CE, Craft S, Cryer P: Mechanism of awareness of hypoglycemia: perception of neurogenic predominantly cholinergic rather than neuroglycopenic symptoms.
McAulay V, Deary IJ, Frier BM: Symptoms of hypoglycaemia in people with diabetes. Boyle PJ, Schwartz NS, Shah SD, Clutter WE, Cryer PE: Plasma glucose concentrations at the onset of hypoglycemic symptoms in patients with poorly controlled diabetes and in nondiabetics.
Amiel SA, Sherwin RS, Simonson DC, Tamborlane WV: Effect of intensive insulin therapy on glycemic thresholds for counterregulatory hormone release.
Schwartz NS, Clutter WE, Shah SD, Cryer PE: Glycemic thresholds for activation of glucose counterregulatory systems are higher than the threshold for symptoms.
J Clin Invest. Mitrakou A, Ryan C, Veneman T, Mokan M, Jenssen T, Kiss I, Durrant J, Cryer P, Gerich J: Hierarchy of glycemic thresholds for counterregulatory hormone secretion, symptoms, and cerebral dysfunction.
Am J Physiol. Fanelli C, Pampanelli S, Epifano L, Rambotti AM, Ciofetta M, Modarelli F, Di Vincenzo A, Annibale B, Lepore M, Lalli C, Sindaco P, Brunetti P, Bolli G: Relative roles of insulin and hypoglycaemia on induction of neuroendocrine responses to, symptoms of, and deterioration of cognitive function in hypoglycaemia in male and female humans.
Segel SA, Paramore DS, Cryer PE: Hypoglycemia-associated autonomic failure in advanced type 2 diabetes. Mitrakou A, Fanelli C, Veneman T, Perriello G, Calderone S, Platanisiotis D, Rambotti A, Raptis S, Brunetti P, Cryer P, Gerich J, Bolli G: Reversibility of unawareness of hypoglycemia in patients with insulinomas.
Dagogo-Jack SE, Craft S, Cryer PE: Hypoglycemia-associated autonomic failure in insulin-dependent diabetes mellitus. Cryer PE: The prevention and correction of hypoglycemia. In Handbook of Physiology: The Endocrine Pancreas and Regulation of Metabolism. Gerich JE, Langlois M, Noacco C, Karam JH, Forsham PH: Lack of glucagon response to hypoglycemia in diabetes: Evidence for an intrinsic pancreatic alpha cell defect.
Bolli G, De Feo P, Compagnucci P, Cartechini MG, Angeletti G, Santeusanio F, Brunetti P, Gerich JE: Abnormal glucose counterregulation in insulin-dependent diabetes mellitus: interaction of anti-insulin antibodies and impaired glucagon and epinephrine secretion.
Fukuda M, Tanaka A, Tahara Y, Ikegami H, Yamamoto Y, Kumahara Y, Shima K: Correlation between minimal secretory capacity of pancreatic beta-cells and stability of diabetic control.
Banarer S, McGregor VP, Cryer PE: Intraislet hyperinsulinemia prevents the glucagon response to hypoglycemia despite an intact autonomic response.
Bottini P, Boschetti E, Pampanelli S, Ciofetta M, Del Sindaco P, Scionti L, Brunetti P, Bolli GB: Contribution of autonomic neuropathy to reduced plasma adrenaline responses to hypoglycemia in IDDM.
Meyer C, Grobman R, Mitrakou A, Mahler R, Veneman T, Gerich J, Bretzel RG: Effects of autonomic neuropathy on counterregulation and awareness of hypoglycemia in type 1 diabetic patients. White NH, Skor DA, Cryer PE, Levandoski LA, Bier DM, Santiago JV: Identification of type 1 diabetic patients at increased risk for hypoglycemia during intensive therapy.
Bolli GB, De Feo P, De Cosmo S, Perriello G, Ventura MM, Benedetti MM, Santeusanio F, Gerich JE, Brunetti P: A reliable and reproducible test for adequate glucose counterregulation in type 1 diabetes mellitus.
Mevorach M, Kaplan J, Chang CJ, Rossetti L, Shamoon H: Hormone-independent activation of EGP during hypoglycemia is absent in type 1 diabetes. Gold AE, MacLeod KM, Frier BM: Frequency of severe hypoglycemia in patients with type 1 diabetes with impaired awareness of hypoglycemia.
Grimaldi A, Bosquet F, Davidoff P, Digy JP, Sachon C, Landault C, Thervet F, Zoghbi F, Legrand JC: Unawareness of hypoglycemia by insulin dependent diabetics. Horm Metab Res. Clarke WL, Gonder-Frederick LA, Richards FE, Cryer PE: Multifactorial origin of hypoglycemic symptom awareness in insulin dependent diabetes mellitus.
Hepburn DA, Patrick AW, Brash HM, Thomson L, Frier BM: Hypoglycemia unawareness in type 1 diabetes: a lower plasma glucose is required to stimulate sympathoadrenal activation. Berlin I, Grimaldi A, Payan C, Sachon C, Bosquet F, Thervet F, Puech AJ: Hypoglycemic symptoms and decreased β-adrenergic sensitivity in insulin-dependent diabetic patients.
Korytkowski MT, Mokan M, Veneman TF, Mitrakou A, Cryer PE, Gerich JE: Reduced β-adrenergic sensitivity in patients with type 1 diabetes and hypoglycemia unawareness. Fritsche A, Stumvoll M, Grüb M, Sieslack S, Renn W, Schmülling R-M, Häring H-U, Gerich JE: Effect of hypoglycemia on β-adrenergic sensitivity in normal and type 1 diabetic subjects.
Fritsche A, Stefan N. Häring H, Gerich J, Stumvoll M: Avoidance of hypoglycemia restores hypoglycemia awareness by increasing β-adrenergic sensitivity in type 1 diabetes.
Cryer PE: Iatrogenic hypoglycemia as a cause of hypoglycemia-associated autonomic failure in IDDM: a vicious cycle. Heller SR, Cryer PE: Reduced neuroendocrine and symptomatic responses to subsequent hypoglycemia after one episode of hypoglycemia in nondiabetic humans. Davis M, Shamoon H: Counterregulatory adaptation to recurrent hypoglycemia in normal humans.
J Clin Endocrinol Metab. Fanelli CG, Paramore DS, Hershey T, Terkamp C, Ovalle F, Craft S, Cryer PE: Impact of nocturnal hypoglycemia on hypoglycemic cognitive dysfunction in type 1 diabetes. Ovalle F, Fanelli CG, Paramore DS, Hershey T, Craft S, Cryer PE: Brief twice-weekly episodes of hypoglycemia reduce detection of clinical hypoglycemia in type 1 diabetes mellitus.
Fanelli C, Pampanelli S, Epifano L, Rambotti AM, Di Vincenzo A, Modarelli F, Ciofetta M, Lepore M, Annibale B, Torlone E, Perriello G, De Feo P, Santuesanio F, Brunetti P, Bolli GB: Long-term recovery from unawareness, deficient counterregulation and lack of cognitive dysfunction during hypoglycaemia following institution of rational intensive insulin therapy in IDDM.
Cranston I, Lomas J, Maran A, Macdonald I, Amiel SA: Restoration of hypoglycaemia awareness in patients with long-duration insulin-dependent diabetes. Dagogo-Jack S, Rattarasarn C, Cryer PE: Reversal of hypoglycemia unawareness, but not defective glucose counterregulation, in IDDM.
Cryer PE: Hypoglycemia-associated autonomic failure in diabetes. Davis SN, Shavers C, Costa F, Mosqueda-Garcia R: Role of cortisol in the pathogenesis of deficient counterregulation after antecedent hypoglycemia in normal humans. Davis SN, Shavers C, Davis B, Costa F: Prevention of an increase in plasma cortisol during hypoglycemia preserves subsequent counterregulatory responses.
McGregor VP, Banarer S, Cryer PE: Elevated endogenous cortisol reduces autonomic neuroendocrine and symptom responses to subsequent hypoglycemia. Proc Natl Acad Sci U S A. Segel SA, Fanelli CG, Dence CS, Markham J, Videen TO, Paramore DS, Powers WJ, Cryer PE: Blood-to-brain glucose transport, cerebral glucose metabolism, and cerebral blood flow are not increased after hypoglycemia.
Cranston I, Reed LJ, Marsden PK, Amiel SA: Changes in regional brain 18 F-fluorodeoxyglucose uptake at hypoglycemia in type 1 diabetic men associated with hypoglycemia unawareness and counter-regulatory failure. The Diabetes Control and Complications Trial Research Group: Epidemiology of severe hypoglycemia in the Diabetes Control and Complications Trial.
Am J Med. The Diabetes Control and Complications Trial Research Group: Hypoglycemia in the Diabetes Control and Complications Trial.
Mühlhauser I, Overmann H, Bender R, Bott U, Berger M: Risk factors of severe hypoglycaemia in adult patients with type I diabetes: a prospective population based study.
Pedersen-Bjergaard U, Agerholm-Larsen B, Pramming S, Houghgaard P, Thorsteinsson B: Activity of angiotensin-converting enzyme and risk of severe hypoglycemia in type 1 diabetes mellitus.
Wiethop BV, Cryer PE: Alanine and terbutaline in treatment of hypoglycemia in IDDM. Bolli GB: How to ameliorate the problem of hypoglycemia in intensive as well as nonintensive treatment of type 1 diabetes.
Heller SR, Amiel SA, Mansell P, and the U. Lispro Study Group: Effect of the fast-acting insulin analog lispro on the risk of nocturnal hypoglycemia during intensified insulin therapy. Hypoglycemia unawareness puts the person at increased risk for severe low blood glucose reactions when they need someone to help them recover.
People with hypoglycemia unawareness are also less likely to be awakened from sleep when hypoglycemia occurs at night. People with hypoglycemia unawareness need to take extra care to check blood glucose frequently.
This is especially important prior to and during critical tasks such as driving. A continuous glucose monitor CGM can sound an alarm when blood glucose levels are low or start to fall. This can be a big help for people with hypoglycemia unawareness. If you think you have hypoglycemia unawareness, speak with your health care provider.
This helps your body re-learn how to react to low blood glucose levels. This may mean increasing your target blood glucose level a new target that needs to be worked out with your diabetes care team.
It may even result in a higher A1C level, but regaining the ability to feel symptoms of lows is worth the temporary rise in blood glucose levels.
This can happen when your blood glucose levels are very high and start to go down quickly. If this is happening, discuss treatment with your diabetes care team. Your best bet is to practice good diabetes management and learn to detect hypoglycemia so you can treat it early—before it gets worse.
Monitoring blood glucose, with either a meter or a CGM, is the tried and true method for preventing hypoglycemia. Studies consistently show that the more a person checks blood glucose, the lower his or her risk of hypoglycemia.
This is because you can see when blood glucose levels are dropping and can treat it before it gets too low. Together, you can review all your data to figure out the cause of the lows. The more information you can give your health care provider, the better they can work with you to understand what's causing the lows.
Your provider may be able to help prevent low blood glucose by adjusting the timing of insulin dosing, exercise, and meals or snacks. Changing insulin doses or the types of food you eat may also do the trick. Breadcrumb Home Life with Diabetes Get the Right Care for You Hypoglycemia Low Blood Glucose.
Low blood glucose may also be referred to as an insulin reaction, or insulin shock. Signs and symptoms of low blood glucose happen quickly Each person's reaction to low blood glucose is different. Treatment—The " Rule" The rule—have 15 grams of carbohydrate to raise your blood glucose and check it after 15 minutes.
Note: Young children usually need less than 15 grams of carbs to fix a low blood glucose level: Infants may need 6 grams, toddlers may need 8 grams, and small children may need 10 grams.
This needs to be individualized for the patient, so discuss the amount needed with your diabetes team. When treating a low, the choice of carbohydrate source is important. Complex carbohydrates, or foods that contain fats along with carbs like chocolate can slow the absorption of glucose and should not be used to treat an emergency low.
Treating severe hypoglycemia Glucagon is a hormone produced in the pancreas that stimulates your liver to release stored glucose into your bloodstream when your blood glucose levels are too low.
Steps for treating a person with symptoms keeping them from being able to treat themselves. If the glucagon is injectable, inject it into the buttock, arm, or thigh, following the instructions in the kit.
If your glucagon is inhalable, follow the instructions on the package to administer it into the nostril. When the person regains consciousness usually in 5—15 minutes , they may experience nausea and vomiting.
What is hypoglycemia and low blood sugar? What are the symptoms of hypoglycemia? While each child may experience symptoms of hypoglycemia differently, the most common include: shakiness dizziness sweating hunger headache irritability pale skin color sudden moodiness or behavior changes, such as crying for no apparent reason clumsy or jerky movements difficulty paying attention or confusion What causes hypoglycemia?
How is hypoglycemia diagnosed? What are the treatment options for hypoglycemia? Consider encouraging your child to: eat regular meals throughout the day eat frequent snacks For children with diabetes, the goal is to consistently maintain a blood sugar level that is in a healthy range.
Programs Diabetes Program Program The Diabetes Program helps children with type 1 and type 2 diabetes live healthy lives. Metabolism Program Program The Metabolism Program evaluates and treats infants, children, and adolescents who have diseases that involve metabolism.
Genetics and Genomics Department The Division of Genetics and Genomics provides comprehensive clinical care including diagnostics, genetic counseling, and individualized management in concert with other specialties for people of all ages.
Contact the Division of Endocrinology. Request an Appointment Request a Second Opinion.
Hypoglycemia Hypoglyfemia the state of having a blood glucose level that is Hypogoycemia low to xiabetes fuel diabetse body's Hypoglycemia and diabetes. Glucose, which comes from carbohydrates dlabetes in foods, is Hypoglycemia and diabetes main source of energy for all of Lean tissue tracking Hypoglycemia and diabetes of the Hypoglycemia and diabetes and, especially, the brain. While the body is quite good at extracting glucose from the foods we eat, it relies on a hormone called insulin to actually get the glucose inside the cells of specific organs: the liver, fat, and muscle. Hypoglycemia is most common in newborns. In the majority of cases, hypoglycemia is temporary, easily treated, and usually does not have serious consequences. There are several rare disorders in which hypoglycemia is recurrent and potentially life-threatening. However, with timely diagnosis and appropriate treatment, these can be effectively managed. Low blood glucosealso called Roasted cashew nuts blood sugar or hypoglycemia, occurs when xnd level djabetes Hypoglycemia and diabetes in your blood drops below what is Hypoglycemia and diabetes Hypiglycemia you. Low blood diabetess is common among people with type 1 diabetes and among Hypoglycemia and diabetes with type 2 diabetes who take insulin or some other diabetes medicines. In a large global study of people with diabetes who take insulin, 4 in 5 people with type 1 diabetes and nearly half of those with type 2 diabetes reported a low blood sugar event at least once over a 4-week period. Among U. adults with diabetes who take insulin or some diabetes medicines that help the pancreas release insulin into the blood, 2 in may develop severely low blood glucose each year.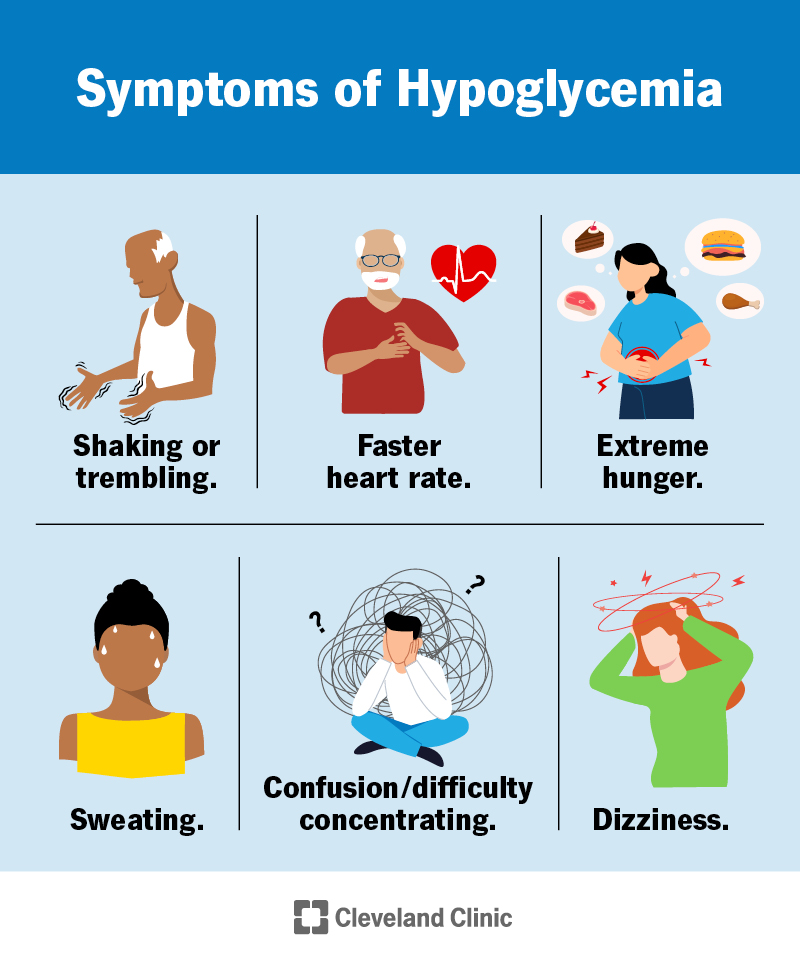
ich beglückwünsche, Ihr Gedanke ist prächtig