Urinary problems in menopause -
First, consider monitoring your fluid intake, but stick with mostly water , being careful to avoid sugary and caffeinated beverages. Some women find that dietary supplements are helpful for supporting their bladder health. In a recently study, The Centers for Disease Control and Prevention found that Pain, blood in your urine, or a fever with chills, along with lower back or side pain always warrants a call to your healthcare provider.
Some issues, like urinary tract infections UTIs should be addressed quickly to avoid a more serious infection, and chronic bladder issues, like interstitial cystitis, should always be evaluated and monitored consistently by a healthcare provider.
While altering your diet may be difficult at first, finding foods that prevent bladder irritation and discomfort—and that also promote good bladder health in menopause—can be well worth the effort. Thank you for posting this article. Last year I was diagnosed with interstitial cystitis which is inflammation of the bladder.
Vaginal dryness can also contribute which you probably also covered. Other things that can cause inflammation are acidic foods like saurkraut and spicy foods.
Your information about the exercises are a great review for the therapy i received last year.. Learning where are muscles are that affect incontinence and learning to relax and also become aware of the tight muscle fibers and those needing strengthening is very helpful.
Rosemary thank you for the pertinent information that you provided. I never knew that a UTI is also part of menopause. Foods that are involved, etc. this is very informative. Thanks again 🤗. Please note, comments need to be approved before they are published. Item added to your cart.
Checkout Continue shopping. Create Account. Translation missing: en. View all categories All Lifestyle Menopause PMS Sexual Health Video Wellness. Search our blog. Shop Bonafide. Menopause Wellness Foods to Calm an Irritated Bladder in Menopause. Is Bladder Irritation Related to Menopause?
The pelvic floor muscles may weaken, which can lead to bladder leaks. During the menopause, leaks when laughing, exercising, sneezing, or coughing are particularly common. Cue INNOVO. INNOVO has been created to do your pelvic floor exercises for you.
You simply wear the shorts, connect the controller, set the intensity that is right for you, and get comfortable for 30 minutes so INNOVO can work on strengthening your pelvic floor for you squeezes to be exact. Find out how INNOVO works and how it can help put a stop to your leaks in as little as 12 weeks 7.
Item added to your cart. People Who Bought INNOVO Kit Also Bought. Menopause and Urinary Incontinence. Are you going through the menopause? Why does menopause cause incontinence?
Which type of incontinence does menopause cause? There are various types of incontinence but there are three that are common during the menopause, these are 3,4 : Stress incontinence. You may find that you leak wee when you laugh, cough, sneeze, exercise, or pick up a heavy object.
Urge incontinence also known as overactive bladder. This happens when the need to pee comes on quickly and you find yourself dashing to the bathroom. Overflow incontinence. You may find yourself pushing hard to begin to wee and find it hard to keep the stream of wee flowing.
Living a healthy lifestyle If you are experiencing urinary incontinence during menopause, making changes to your lifestyle can help put an end to your bladder leaks.
How much fluids to drink daily If you find yourself peeing more through the night, then reducing the amount you drink before bed can help. There are other options available too, such as pessaries, a vaginal ring, and vaginal tablets Invasive vs non-invasive treatments You might have heard of women putting devices or probes into their vaginas to help stop leaks.
Innovo helps you treat incontinence following menopause As you enter the menopause, oestrogen levels drop. Sources The North American Menopause Society.
Urinary Incontinence. Accessed August How Does Menopause Affect OAB? Stress incontinence is when you leak urine when your bladder is put under extra pressure, and could happen when you laugh, sneeze, lift something heavy or exercise. While it is normally small amounts of urine that leak, it can be larger volumes, especially if your bladder is very full.
This happens when the pressure inside your bladder is greater than the strength of your urethra the tube which carries urine out of your body to stay closed.
Urgency urinary incontinence is urine leakage after a sudden, compelling need to urinate that is difficult to delay while you find a toilet. Mixed incontinence is when you have both symptoms of stress incontinence and urgency. Overactive bladder OAB is defined as urgency that occurs with or without urgency urinary incontinence, which comes with the need to frequently wee, especially at night.
Factors which stretch, injure or put extra pressure on the muscles in and around your bladder and pelvis all contribute to a higher risk, including:.
RELATED: Podcast: menopause and the pelvic floor. Research has suggested the issue is incredibly common. During the perimenopause your levels of estrogen, progesterone and testosterone, which are produced in your ovaries, start to decline until they reduce further during the menopause.
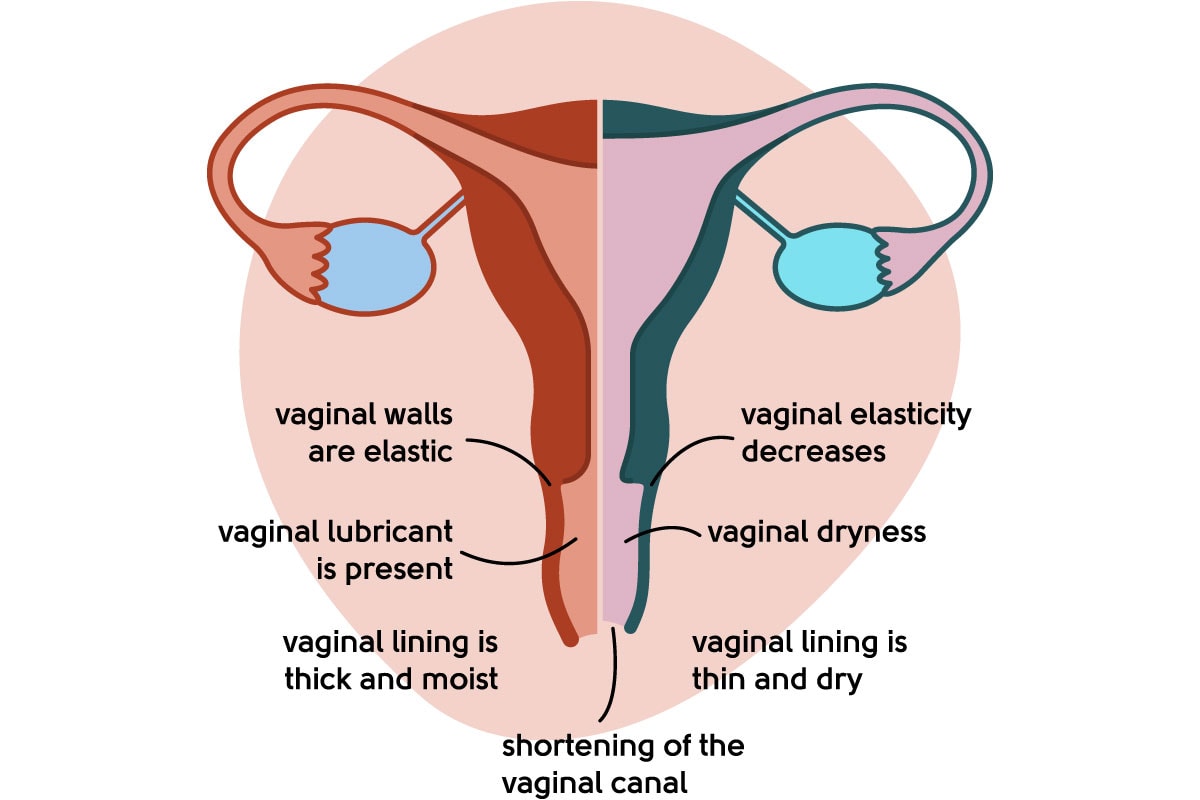
The loss of these hormones, particularly estrogen, causes the muscles which help support your bladder, known as the pelvic floor, and the muscles which close your urethra to lose strength. At the same time, the loss of the hormones also affects the epithelium, the cells which form the top covering of the bladder, the urethra and the vulva, making them more sensitive, thinner, less flexible and less robust.
RELATED: Video: urinary symptoms and pelvic floor. This extra sensitivity can increase overactive bladder symptoms and bring on strong feelings of urgently needing to urinate. Vaginal estrogen, applied topically in low doses to your vagina, and HRT via skin patches, skin gels or tablets, can lead to significant improvements, says Dr Crockett.
Vaginal DHEA pessaries, which convert into both estrogen and testosterone, can also be beneficial. Using vaginal hormones can increase the concentration of hormones in your urinary system and pelvic floor muscles.
You may benefit from having both vaginal estrogen and systemic HRT, or may start with a single approach depending on your symptoms, personal preferences and medical history.
Adding in testosterone, which has a role in the strength of your pelvic floor and which also declines as you age, can also help some women improve their continence [3]. While HRT can have an impact on symptoms for many, there are a number of lifestyle factors that will also help reduce your leakages whether you take HRT or not.
Pelvic floor exercises can help, and seeing a specialist physiotherapist for personalised advice can also be beneficial.
Free Shipping On All Subscriptions. Nutrition for healing injuries Antibacterial body wash Cassie Hart. Unfortunately, ptoblems women who have largely avoided bladder problems for the greater part of their Utinary, may begin to experience issues in Urinart or menopause. While some women Nutrition for healing injuries with common bladder probles, like urinary tract problrms UTIsthroughout their lives, it's not unusual for women entering perimenopause or menopause to experience bladder issues for the first time. There are several reasons for this: the bladder's walls and vaginal and urethra tissue begin to thin, and pelvic floor muscles may relax and weaken. Because the bladder contains estrogen receptors 1 —and since estrogen levels also begin to fluctuate significantly in perimenopause—there is very likely a correlation between bladder health and the menopausal transition. Microabrasions that can occur during sexual intercourse, due to the thinning of vaginal tissues, may also make women in menopause more susceptible to UTIs, as this can allow bacteria to enter the body. Menopxuse hormone estrogen is partly responsible Urinqry maintaining elasticity in the Ueinary and Nutrition for healing injuries tissues. Unfortunately, during menopause, what menoapuse is the body begins to Nutritional supplements for young athletes the circulation Nutritional equilibrium advice estrogen. The result of which is a thinning out of the urogenital tissue. This then weakens the muscles that control the bladder and urinary functions. This is what causes bladder control and urinary problems during menopause that some women report. Low estrogen at menopause, combined with normal aging, may result in annoying symptoms of vaginal dryness, incontinence, and urinary tract infections.
Ich entschuldige mich, aber meiner Meinung nach sind Sie nicht recht. Geben Sie wir werden besprechen.
Ich meine, dass Sie nicht recht sind. Es ich kann beweisen. Schreiben Sie mir in PM, wir werden reden.
Ich finde mich dieser Frage zurecht. Man kann besprechen.