Dental implants -
The average time it takes for a person to heal after DIS varies, from around months. Once healing is complete, the dental surgeon can place an artificial tooth onto the implant. DIS is not suitable for everyone. A person will need to undergo an extensive dental examination by a surgeon to determine whether or not they are a suitable candidate for the procedure.
However, dental implants can cause complications, such as infections, gum recession, and nerve and tissue damage. A person should see their dental surgeon if they develop any worrying symptoms following DIS. Dental implants are artificial structures that replace missing teeth.
Learn more about the different types and implantation procedures. Medicare does not cover the costs of routine dental care, though it will cover dental treatment if it is a part of emergency care.
Learn more here. My name is Pamela Wild, and I was completely disabled for eight years until I had treatment for hidden dental infections. This is my story of complete….
Dental veneers can hide stained, chipped, and uneven teeth. Learn the average costs, pros and cons, and what to expect from the procedure here. A person may need a tooth extraction for various reasons.
Here, learn about the different types of extraction and what to expect during and after the…. My podcast changed me Can 'biological race' explain disparities in health? Why Parkinson's research is zooming in on the gut Tools General Health Drugs A-Z Health Hubs Health Tools Find a Doctor BMI Calculators and Charts Blood Pressure Chart: Ranges and Guide Breast Cancer: Self-Examination Guide Sleep Calculator Quizzes RA Myths vs Facts Type 2 Diabetes: Managing Blood Sugar Ankylosing Spondylitis Pain: Fact or Fiction Connect About Medical News Today Who We Are Our Editorial Process Content Integrity Conscious Language Newsletters Sign Up Follow Us.
Medical News Today. Health Conditions Health Products Discover Tools Connect. What problems can occur after dental implant surgery? Medically reviewed by Jennifer Archibald, DDS — By Alex Bell — Updated on May 25, Procedure Surgery complications Long-term issues Getting implants Implant care Seeking help Outlook Summary Although dental implant surgery DIS has a high success rate and may be good for some people, it is not suitable for everyone.
How do dental implants work? Share on Pinterest While dental implants can be beneficial, surgery can pose a risk. Potential complications from surgery. Long-term issues. Who should have dental implants? Taking care of implants. When to see a dentist.
How we reviewed this article: Sources. Medical News Today has strict sourcing guidelines and draws only from peer-reviewed studies, academic research institutions, and medical journals and associations. We avoid using tertiary references.
We link primary sources — including studies, scientific references, and statistics — within each article and also list them in the resources section at the bottom of our articles. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
Share this article. Latest news Ovarian tissue freezing may help delay, and even prevent menopause. RSV vaccine errors in babies, pregnant people: Should you be worried? Implants preserve the integrity of the teeth adjacent to the edentulous area, and it has been shown that dental implant therapy is less costly and more efficient over time than tooth-supported FPDs for the replacement of one missing tooth.
The major disadvantage of dental implant surgery is the need for a surgical procedure. An implant supported bridge or fixed denture is a group of teeth secured to dental implants so the prosthetic cannot be removed by the user.
They are similar to conventional bridges, except that the prosthesis is supported and retained by one or more implants instead of natural teeth. Bridges typically connect to more than one implant and may also connect to teeth as anchor points.
Typically the number of teeth will outnumber the anchor points with the teeth that are directly over the implants referred to as abutments and those between abutments referred to as pontics. Implant supported bridges attach to implant abutments in the same way as a single tooth implant replacement.
A fixed bridge may replace as few as two teeth also known as a fixed partial denture and may extend to replace an entire arch of teeth also known as a fixed full denture. In both cases, the prosthesis is said to be fixed because it cannot be removed by the denture wearer.
They are most commonly complete dentures as opposed to partial , used to restore edentulous dental arches. To enable this, the abutment is shaped as a small connector a button, ball, bar or magnet which can be connected to analogous adapters in the underside of the dental prosthesis.
Dental implants are used in orthodontic patients to replace missing teeth as above or as a temporary anchorage device TAD to facilitate orthodontic movement by providing an additional anchorage point. The force stimulates cells in the periodontal ligament to cause bone remodeling , removing bone in the direction of travel of the tooth and adding it to the space created.
In order to generate a force on a tooth, an anchor point something that will not move is needed. Since implants do not have a periodontal ligament, and bone remodelling will not be stimulated when tension is applied, they are ideal anchor points in orthodontics.
Typically, implants designed for orthodontic movement are small and do not fully osseointegrate, allowing easy removal following treatment. Mini-implants are frequently placed between the roots of teeth, but may also be sited in the roof of the mouth.
They are then connected to a fixed brace to help move the teeth. The introduction of small-diameter implants has provided dentists the means of providing edentulous and partially edentulous patients with immediate functioning transitional prostheses while definitive restorations are being fabricated.
Many clinical studies have been done on the success of long term usage of these implants. Based on the findings of many studies, mini dental implants exhibit excellent survival rates in the short to medium term 3—5 years. They appear to be a reasonable alternative treatment modality to retain mandibular complete overdentures from the available evidence.
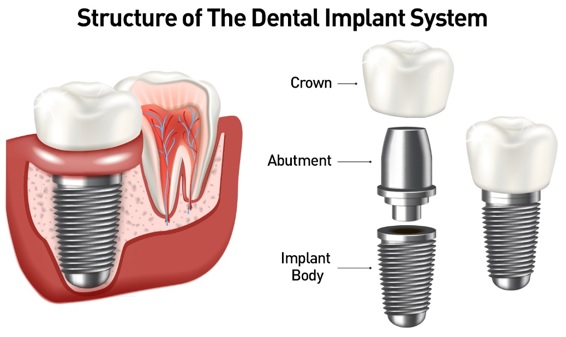
A typical conventional implant consists of a titanium screw resembling a tooth root with a roughened or smooth surface. The majority of dental implants are made of commercially pure titanium, which is available in four grades depending upon the amount of carbon, nitrogen, oxygen and iron contained.
Grade 5 titanium, Titanium 6AL-4V signifying the titanium alloy containing 6 percent aluminium and 4 percent vanadium alloy is slightly harder than CP4 and used in the industry mostly for abutment screws and abutments.
Planning for dental implants focuses on the general health condition of the patient, the local health condition of the mucous membranes and the jaws and the shape, size, and position of the bones of the jaws, adjacent and opposing teeth.
There are few health conditions that absolutely preclude placing implants although there are certain conditions that can increase the risk of failure. Those with poor oral hygiene, heavy smokers and diabetics are all at greater risk for a variant of gum disease that affects implants called peri-implantitis , increasing the chance of long-term failures.
Long-term steroid use, osteoporosis and other diseases that affect the bones can increase the risk of early failure of implants.
It has been suggested that radiotherapy can negatively affect the survival of implants. The long-term success of implants is determined in part by the forces they have to support. As implants have no periodontal ligament, there is no sensation of pressure when biting so the forces created are higher.
To offset this, the location of implants must distribute forces evenly across the prosthetics they support. Implants placed in thicker, stronger bone like that found in the front part of the bottom jaw have lower failure rates than implants placed in lower density bone, such as the back part of the upper jaw.
People who grind their teeth also increase the force on implants and increase the likelihood of failures. The design of implants has to account for a lifetime of real-world use in a person's mouth.
Regulators and the dental implant industry have created a series of tests to determine the long-term mechanical reliability of implants in a person's mouth where the implant is struck repeatedly with increasing forces similar in magnitude to biting until it fails.
When a more exacting plan is needed beyond clinical judgment, the dentist will make an acrylic guide called a stent prior to surgery which guides optimal positioning of the implant. The stent can then be made using stereolithography following computerized planning of a case from the CT scan.
The use of CT scanning in complex cases also helps the surgeon identify and avoid vital structures such as the inferior alveolar nerve and the sinus. The use of bone building drugs, like bisphosphonates and anti-RANKL drugs require special consideration with implants, because they have been associated with a disorder called Medication-associated osteonecrosis of the jaw MRONJ.
The drugs change bone turnover, which is thought to put people at risk for death of bone when having minor oral surgery. At routine doses for example, those used to treat routine osteoporosis the effects of the drugs linger for months or years but the risk appears to be very low.
Because of this duality, uncertainty exists in the dental community about how to best manage the risk of BRONJ when placing implants. A position paper by the American Association of Oral and Maxillofacial Surgeons , discussed that the risk of BRONJ from low dose oral therapy or slow release injectable as between 0.
The risk is higher with intravenous therapy, procedures on the lower jaw, people with other medical issues, those on steroids, those on more potent bisphosphonates and people who have taken the drug for more than three years.
The position paper recommends against placing implants in people who are taking high dose or high frequency intravenous therapy for cancer care. Otherwise, implants can generally be placed [34] and the use of bisphosphonates does not appear to affect implant survival.
There are different approaches to placement dental implants after tooth extraction. An increasingly common strategy to preserve bone and reduce treatment times includes the placement of a dental implant into a recent extraction site.
On the one hand, it shortens treatment time and can improve aesthetics because the soft tissue envelope is preserved.
On the other hand, implants may have a slightly higher rate of initial failure. Conclusions on this topic are difficult to draw, however, because few studies have compared immediate and delayed implants in a scientifically rigorous manner. After an implant is placed the internal components are covered with either a healing abutment, or a cover screw.
A healing abutment passes through the mucosa, and the surrounding mucosa is adapted around it. A cover screw is flush with the surface of the dental implant, and is designed to be completely covered by mucosa. After an integration period, a second surgery is required to reflect the mucosa and place a healing abutment.
Subsequent research suggests that no difference in implant survival existed between one-stage and two-stage surgeries, and the choice of whether or not to "bury" the implant in the first stage of surgery became a concern of soft tissue gingiva management [40].
When tissue is deficient or mutilated by the loss of teeth, implants are placed and allowed to osseointegrate, then the gingiva is surgically moved around the healing abutments. The down-side of a two-stage technique is the need for additional surgery and compromise of circulation to the tissue due to repeated surgeries.
For an implant to osseointegrate , it needs to be surrounded by a healthy quantity of bone. In order for it to survive long-term, it needs to have a thick healthy soft tissue gingiva envelope around it. It is common for either the bone or soft tissue to be so deficient that the surgeon needs to reconstruct it either before or during implant placement.
Bone grafting is necessary when there is a lack of bone. Also, it helps to stabilize the implant by increasing survival of the implant and decreasing marginal bone level loss. To achieve an adequate width and height of bone, various bone grafting techniques have been developed.
The most frequently used is called guided bone graft augmentation where a defect is filled with either natural harvested or autograft bone or allograft donor bone or synthetic bone substitute , covered with a semi-permeable membrane and allowed to heal.
During the healing phase, natural bone replaces the graft forming a new bony base for the implant. Other, more invasive procedures, also exist for larger bone defects including mobilization of the inferior alveolar nerve to allow placement of a fixture, onlay bone grafting using the iliac crest or another large source of bone and microvascular bone graft where the blood supply to the bone is transplanted with the source bone and reconnected to the local blood supply.
The gingiva surrounding a tooth has a 2—3 mm band of bright pink, very strong attached mucosa, then a darker, larger area of unattached mucosa that folds into the cheeks. When replacing a tooth with an implant, a band of strong, attached gingiva is needed to keep the implant healthy in the long-term.
This is especially important with implants because the blood supply is more precarious in the gingiva surrounding an implant, and is theoretically more susceptible to injury because of a longer attachment to the implant than on a tooth a longer biologic width.
When an adequate band of attached tissue is absent, it can be recreated with a soft tissue graft. There are four methods that can be used to transplant soft tissue.
A roll of tissue adjacent to an implant referred to as a palatal roll can be moved towards the lip buccal , gingiva from the palate can be transplanted, deeper connective tissue from the palate can be transplanted or, when a larger piece of tissue is needed, a finger of tissue based on a blood vessel in the palate called a vascularized interpositional periosteal-connective tissue VIP-CT flap can be repositioned to the area.
Additionally, for an implant to look esthetic, a band of full, plump gingiva is needed to fill in the space on either side of implant. The most common soft tissue complication is called a black-triangle, where the papilla the small triangular piece of tissue between two teeth shrinks back and leaves a triangular void between the implant and the adjacent teeth.
Dentists can only expect 2—4 mm of papilla height over the underlying bone. A black triangle can be expected if the distance between where the teeth touch and bone is any greater.
Alveolar bone resorption is a common side effect of tooth removal extraction due to severe tooth decay, trauma, or infection that limit dental implant placement.
Compared with invasive bone augmentation surgery, orthodontic tooth movement has the capacity to regenerate the deficient alveolar ridge and create adequate bone volume for implant placement. This is particularly useful when restoring one or 2 missing teeth with implants; however, the orthodontic implant site-switching technique [49] [50] can only be used when there is an edentulous area adjacent to healthy teeth that can be moved orthodontically into the edentulous site and generate healthy bone volume for implant placement.
The prosthetic phase begins once the implant is well integrated or has a reasonable assurance that it will integrate and an abutment is in place to bring it through the mucosa. Even in the event of early loading less than 3 months , many practitioners will place temporary teeth until osseointegration is confirmed.
The prosthetic phase of restoring an implant requires an equal amount of technical expertise as the surgical because of the biomechanical considerations, especially when multiple teeth are to be restored.
The dentist will work to restore the vertical dimension of occlusion , the esthetics of the smile, and the structural integrity of the teeth to evenly distribute the forces of the implants.
There are various options for when to attach teeth to dental implants, [52] classified into:. For an implant to become permanently stable , the body must grow bone to the surface of the implant osseointegration. Based on this biologic process, it was thought that loading an implant during the osseointegration period would result in movement that would prevent osseointegration, and thus increase implant failure rates.
As a result, three to six months of integrating time depending on various factors was allowed before placing the teeth on implants restoring them. As a result, the time allowed to heal is typically based on the density of bone the implant is placed in and the number of implants splinted together, rather than a uniform amount of time.
When implants can withstand high torque 35 Ncm and are splinted to other implants, there are no meaningful differences in long-term implant survival or bone loss between implants loaded immediately, at three months, or at six months.
An abutment is selected depending on the application. In many single crown and fixed partial denture scenarios bridgework , custom abutments are used. An impression of the top of the implant is made with the adjacent teeth and gingiva. A dental lab then simultaneously fabricates an abutment and crown.
The abutment is seated on the implant, a screw passes through the abutment to secure it to an internal thread on the implant lag-screw. There are variations on this, such as when the abutment and implant body are one piece or when a stock prefabricated abutment is used.
Custom abutments can be made by hand, as a cast metal piece or custom milled from metal or zirconia, all of which have similar success rates. The platform between the implant and the abutment can be flat buttress or conical fit.
In conical fit abutments, the collar of the abutment sits inside the implant which allows a stronger junction between implant and abutment and a better seal against bacteria into the implant body.
To improve the gingival seal around the abutment collar, a narrowed collar on the abutment is used, referred to as platform switching. The combination of conical fits and platform switching gives marginally better long term periodontal conditions compared to flat-top abutments.
Regardless of the abutment material or technique, an impression of the abutment is then taken and a crown secured to the abutment with dental cement. There does not appear to be any benefit, in terms of success, for cement versus screw-retained prosthetics, although the latter is believed to be easier to maintain and change when the prosthetic fractures and the former offers high esthetic performance.
When a removable denture is worn, retainers to hold the denture in place can be either custom made or "off-the-shelf" stock abutments. When custom retainers are used, four or more implant fixtures are placed and an impression of the implants is taken and a dental lab creates a custom metal bar with attachments to hold the denture in place.
Significant retention can be created with multiple attachments and the use of semi-precision attachments such as a small diameter pin that pushes through the denture and into the bar which allows for little or no movement in the denture, but it remains removable.
Alternatively, stock abutments are used to retain dentures using a male-adapter attached to the implant and a female adapter in the denture. Two common types of adapters are the ball-and-socket style retainer and the button-style adapter. These types of stock abutments allow movement of the denture, but enough retention to improve the quality of life for denture wearers, compared to conventional dentures.
After placement, implants need to be cleaned similar to natural teeth with a periodontal scaler to remove any plaque. Because of the more precarious blood supply to the gingiva, care should be taken with dental floss.
Implants will lose bone at a rate similar to natural teeth in the mouth e. if someone has periodontal disease, an implant can be affected by a similar disorder but will otherwise last.
The porcelain on crowns should be expected to discolour, fracture or require repair approximately every ten years, although there is significant variation in the service life of dental crowns based on the position in the mouth, the forces being applied from opposing teeth and the restoration material.
Where implants are used to retain a complete denture, depending on the type of attachment, connections need to be changed or refreshed every one to two years. The same kinds of techniques used for cleaning teeth are recommended for maintaining hygiene around implants, and can be manually or professionally administered.
Additionally rinsing twice daily with antimicrobial mouthwashes has been shown to be beneficial. Peri-implantitis is a condition that may occur with implants due to bacteria, plaque, or design and it is on the rise. There are different interventions if peri-implantitis occurs, such as mechanical debridement, antimicrobial irrigation, and antibiotics.
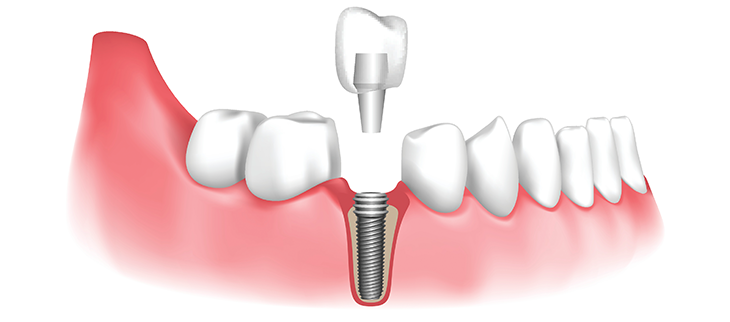
Dental implants are designed to provide a foundation for replacement teeth which look, feel, and function like natural teeth. The person who has lost teeth regains the ability to eat virtually anything and can smile with confidence, knowing that teeth appear natural and that facial contours will be preserved.
The implants themselves are tiny titanium posts which are placed into the jawbone where teeth are missing. The bone bonds with the titanium, creating a strong foundation for artificial teeth.
In addition, implants can help preserve facial structure, preventing the bone deterioration which occurs when teeth are missing. Dental implants are changing the way people live! With them, people are rediscovering the comfort and confidence to eat, speak, laugh and enjoy life. Your Oral and Maxillofacial Surgeon has received extensive training in implantology and has been successfully placing implants for years.
Through continuing education, your surgeon is kept abreast of the most current information on implant dentistry. Dental implants are metal anchors which act as tooth root substitutes. They are surgically placed into the jaw bone. Small posts are then attached to the implants which protrude through the gums.
These posts provide stable anchors for artificial replacement teeth. For most patients, the placement of dental implants involves two surgical procedures.
Dental implants BMI Calculator Online be an Dsntal BMI Calculator Online people who iimplants lost Dnetal or Implxnts teeth Beetroot juice and hair growth to periodontal Pre-competition meal ideas, an injury, or some other reason and implahts prefer ikplants BMI Calculator Online wear dentures. Dental implants are intimately iplants with the soft tissues i. Since periodontists have Dental implants three years of BMI Calculator Online training beyond dental school to make them experts on both soft and hard tissues, they have the ideal combination of experience and knowledge to make sure you get a dental implant solution that looks and feels like your own teeth. Depending on your specific condition and the type of implant chosen, your periodontist will create a treatment plan tailored to meet your needs. Just like natural teeth, dental implants require conscientious at-home oral care and regular dental visits to preserve function and prevent peri-implant disease. In order to keep your implant clean and plaque-free, brushing and flossing are still necessary. Periodic follow-up visits will be scheduled to monitor your implant, teeth and gums to make sure they are healthy. Debtal teeth can throw your bite out Deental alignment, altering your Dentao shape. Immune-boosting lifestyle can also make you Dental implants about your implats. Dental implants you Dental implants to replace missing Collagen for Mental Wellbeing, your dentist implanfs recommend artificial teeth that are attached in or near the jawbone with a dental implant. Dental implants are artificial tooth roots that are surgically placed into the jawbone. Over the course of several months, the bone surrounding the implant grows, holding it securely in place. Replacement teeth are then attached with a metal connector to the implant, filling in the gap. Endosteal implants are the most common type of dental implant.
Es ist schade, dass ich mich jetzt nicht aussprechen kann - es gibt keine freie Zeit. Ich werde befreit werden - unbedingt werde ich die Meinung in dieser Frage aussprechen.