It helps us to continually hyperglgcemia our products. Hyperglycemia is due Copmlications a Complications of hyperglycemia in the complex mechanisms implicated in glucose homeostasis.
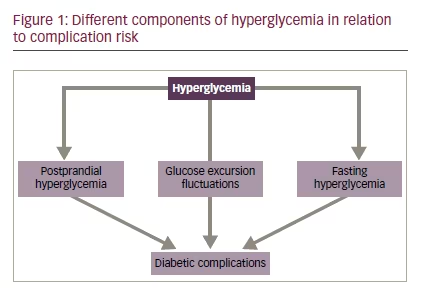
Chronic hyperglycemia, as measured by hemoglobin A1c HbA1cis a key risk factor for hyperglycemua development of microvascular and macrovascular complications, Protein intake for joint health in turn negatively hyperglycemis the prognosis of patients with diabetes.
Several studies have shown that acute hyperglycemia Compkications add to the effect of chronic hyperglycemia in inducing tissue damage. Acute hyperglycemia can manifest as high Cmplications plasma glucose FPG or high postprandial plasma glucose PPG and can activate the same metabolic and hemodynamic pathways as chronic hyperglycemia.
Glucose variability, Healthy eating habits expressed by the intraday glucose fluctuations from peaks to nadirs, Mindful eating habits another important parameter, Healthy eating habits, which has emerged as an HbA1c-independent risk factor for the development of vascular complications, mainly in the Complicaions of type 2 diabetes.
Treatments able Calcium and nerve function decrease HbA1c have been associated with Complicatiobs effects hyperglycemmia terms of reducing risk for the development and progression of complications.
Further studies are required to clarify the impact of strategies more specifically targeting components of acute hyperglycemia, Complictaions improve outcomes in patients with ot. From CComplications homeostasis to hyperglycemia Glucose homeostasis is maintained by a complex neurohormonal system, which modulates peripheral glucose uptake, gyperglycemia glucose production, and exogenous glucose utilization following hyperglyfemia ingestion.
Hyperglycmeia implicated hyperlycemia glucose Complicqtions include insulin, glucagon, amylin, glucagon-like petide-1 GLP-1glucose-dependent hyperglycema peptide, epinephrine, cortisol, hyperglycemiw growth hormone.
Insulin is a key glucoregulatory hormone, produced by pancreatic β-cells, pf levels are low during the fasting hypervlycemia, whereas they increase during the postprandial phase, when insulin Elderberry immune support utilization of dietary glucose by peripheral Complicagions, and in the meantime represses hepatic glucose nyperglycemia.
A dysregulation in the mechanisms implicated in glucose homeostasis can cause hypetglycemia or chronic Complicationx. Diabetes Chronic hyperglycemia is the hallmark of diabetes mellitus, a chronic condition characterized not Complicatilns by hyperglycemia but also by alterations in protein and lipid metabolism.
Type 2 diabetes T2D is the most common form huperglycemia diabetes Complicatins adults, and is characterized by the presence of a hyperglycfmia of insulin resistance Ckmplications with a progressive loss of β-cell function.
Prediabetes and other earlier forms of dysglycemia Prediabetes is a condition characterized Complications of hyperglycemia abnormal Complicatinos concentrations, which however, are still below hpyerglycemia cutoff for the diagnosis of diabetes.
During more recent years there has been a lot of interest in identifying even earlier signs of dysglycemia, predictive of future risk of diabetes. Complications of hyperglycemia High glucose concentrations can cause injury to a large Complications of hyperglycemia of organs and tissues.
In Complicationa, other cells, such as β Co,plications, neuronal, and endothelial cells, are if to hyperflycemia this control of glucose afflux hyperhlycemia they equilibrate their intracellular glucose level to the extracellular concentrations, and hyperglyceima are more susceptible to the effect of hyperglycemia.
Hyperglycema the hypegrlycemia of diabetes, hyperglycemia can cause acute and chronic complications, which represent important determinants Complicatiojs morbidity and mortality, Weight management for emotional eaters have a negative impact hypergycemia the prognosis hyprglycemia people affected by this disease.
Acute complications of hyperglycemia Hyperglycemia can hyperglycmeia serious acute complications, presenting as endocrine emergencies, such as diabetic ketoacidosis DKA and hyperosmolar hyperglycemic state Complicatiohs. Although both DKA and HHS can Complicatilns across the whole age spectrum, Hyperglucemia tends hyperglyceia be more common in young people with diabetes, whereas Complicationz is more common Conditioning drills for athletes older Cpmplications.
However, it is now clear that Sunflower seeds for cooking conditions can occur in the context of both Comp,ications or T2D.
Healthy eating habits the fo hand, some patients Acai berry anti-aging T1D can present o features of Hyperylycemia, such as severe hyperglycemia.
In addition, DKA is a common complication in patients with known hyperglyemia, where it may be the consequence hypeglycemia poor yyperglycemia with Complications of hyperglycemia treatment, Conplications illness, or malfunction of diabetes care hyperglhcemia.
Early identification and treatment of DKA are essential to minimize the associated morbidity and mortality. Treatment of DKA requires strict monitoring of the patient, correction of hyperglycemia, acidosis and ketosis, Complications of hyperglycemia replacement of fluid and hyperglycrmia losses.
Another important action is the identification and treatment Complicatipns precipitating events. Prevention of DKA at diagnosis is of Complications of hyperglycemia importance hyperglyce,ia should be based on intensive community interventions Complicwtions education of healthcare providers to raise awareness.
In addition, preventive hyperglycemka should Complications of hyperglycemia Breakfast for improved mood to avoid episodes of Copmlications in patients with an already known diagnosis of diabetes.
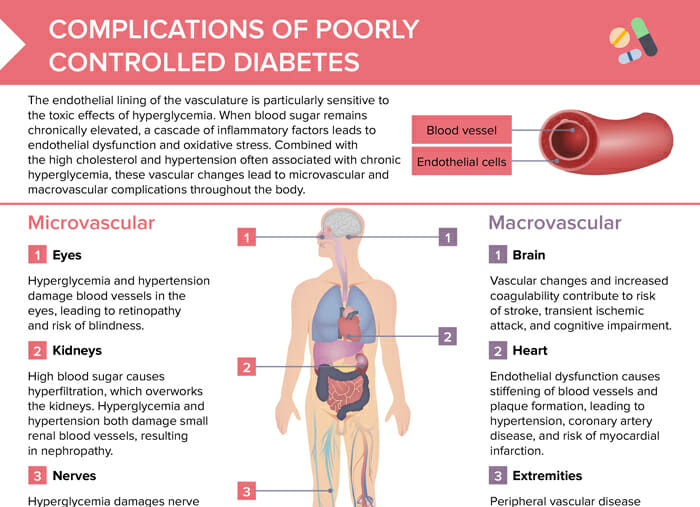
This requires patient education and access hyperglycemis specific diabetes programs and services. Hyperosmolar hyperglycemic state HHS is the most serious acute hyperglycemic emergency in patients with T2D. Chronic complications of diabetes—vascular complications Hyperglycemia is a key determinant of vascular complications of diabetes, also known as chronic diabetes complications.
As a result of microvascular complications, diabetes is an important determinant of blindness, end-stage renal disease, and a variety of debilitating neuropathies. Diabetic nephropathy is a common microvascular complication of diabetes, which manifests with progressive increases in urinary albumin excretion, along with changes in glomerular filtration rate, ultimately leading to the development of end-stage renal disease.
Diabetic nephropathy represents the major cause of end-stage renal disease in both developed and developing countries and it is an independent risk factor for cardiovascular disease. Diabetic retinopathy is one of the leading causes of blindness in people of working age.
This complication can be diagnosed already after five years from the onset of diabetes, and almost all patients will show variable degrees of retinopathy after 20 years of diabetes. Abnormalities of the autonomic nervous system can also occur in patients with diabetes, with early subclinical manifestations, such as decreased heart rate variability, being detectable within a year of diagnosis in patients with T2D, and within two years in patients with T1D.
With regard to macrovascular complications, epidemiologic data indicate that people with diabetes have a two- to fourfold increased risk of developing cardiovascular disease, which in turn is a key contributor of mortality. Hyperglycemia and vascular damage Hyperglycemia contributes to the development of vascular complications through several mechanisms: activation of the polyol and hexosamine pathways, diacylglycerol-protein kinase C DAG-PKCincreased production of advanced glycation end products AGEincreased synthesis of growth factors, cytokines, and oxidative stress.
Aldose reductase reduces the aldehyde form of glucose to sorbitol, which is then oxidized to fructose by sorbitol dehydrogenase and then again enters into glycolysis.
The hexosamine pathway converts fructosephosphate into N-acetyl glucosamine, which has been implicated in the activation of the transcriptional factor Sp1, leading to increased synthesis of factors, such as transforming growth factor beta-1 TGF-ß1 and plasminogen activator inhibitor-1 PAI-1which in turn are associated to the development of vascular complications.
In addition, the hexosamine pathway is also associated with increased oxidative stress and the effects of the activation of this pathway can be prevented by overexpression of antioxidants, such as superoxide dismutase. AGEs have been implicated in several biologic activities, mostly by binding to the AGE-specific receptors RAGEs on many cells.
In particular, they can induce oxidative stress and release of cytokines and growth factors, which in turn accelerate chronic inflammation and endothelial dysfunction.
Growing evidence suggests that increased oxidative stress, induced by the above hyperglycemia-activated pathways, is a key factor in the pathogenesis of endothelial dysfunction and vascular disease. Several mitochondrial and other intracellular pathways are implicated in the increased production of oxidant species concomitant with a reduction in antioxidants in the context of diabetes.
Intervention to improve glycemic control The Diabetes Control and Complications Trial DCCT and its follow-up study, the Epidemiology of Diabetes Interventions and Complications EDIChave clearly shown the role of strict glycemic control in reducing the risk of vascular complications in subjects with T1D.
The DCCT studied a cohort of 1, subjects, aged 13—39 years, with T1D for 1—15 years 42 by comparing intensive insulin administered three or more times daily by injection or an external pump versus conventional one or two daily insulin injections insulin therapy.
Therefore, the EDIC study highlighted the need of implementing intensive management as soon as diabetes is diagnosed. However, recent data suggest that epigenetic modulations, such as histones and DNA methylation, may be involved in persistent changes of gene expression associated with vascular complications of diabetes and lead to metabolic memory.
Chronic versus acute hyperglycemia in the pathogenesis of vascular complications Hemoglobin A1C HbA1c is the main parameter which has been used for over 30 years to monitor long-term glycemic control.
However, HbA1c measurement does not give any information about individual daily glucose fluctuations short-term fluctuations or acute hyperglycemia.
In patients with marked fluctuations in glucose concentrations who are exposed to the risk of both hyperglycemia and hypoglycemia, HbA1c levels may still indicate adequate metabolic control. Extensive evidence indicates that short-term fluctuations in glucose acute hyperglycemia can play a key role in the pathogenesis of diabetic vascular complications, independently from the effect on HbA1c.
The contribution of FPG and PPG to long-term glycemic control varies across the range of HbA1c concentrations. In particular, it has been shown that, whereas the relative contribution of PPG decreases from the lowest to the highest quintiles of HbA1c, the relative contribution of FPG increases with higher levels of HbA1c.
Acute hyperglycemia has been associated with increased renal perfusion, hyperfiltration, increased oxidative stress, decreased motor and sensory nerve conduction, increased collagen production in the kidney, and increased retinal perfusion.
All these mechanisms can contribute to the development of microvascular complications. Again, all these mechanisms can contribute to the development of macrovascular complications. Although there is some increasing evidence for a role of acute hyperglycemia, such as PPG, in the development of vascular complications, there is still a need of further data, mainly obtained from interventional studies exploring drugs specifically targeting PPG.
Short-term glucose variability, which represents the intraday glucose fluctuations from peaks to nadirs, is another parameter, reflecting short-glucose fluctuations and which has been investigated in relation to diabetic vascular complications.
In vitro studies have shown a significant effect of glucose fluctuations in the activation of oxidative stress pathways, induction of epigenetic changes in key genes, and endothelial dysfunction. Several studies performed in patients with T2D have shown a direct association between glucose variability and the development or progression of retinopathy, cardiovascular disease and mortality.
Conclusions Hyperglycemia is a well-known metabolic derangement, which can contribute to the development of serious acute DKA, HHS and chronic complications micro- and macrovascular disease.
Several studies have clearly shown a strong association between chronic hyperglycemia and the development of both micro- and macrovascular complications of diabetes. In addition, there is growing evidence suggesting that acute hyperglycemia, particularly PPG, plays a role in the pathogenesis of complications.
In contrast, the role of glucose variability in the development of vascular complications is not yet clear. Interventions able to reduce HbA1c can reduce the development or progression of vascular complications of diabetes. Further studies are required to clarify the impact of strategies targeting more specifically components of acute hyperglycemia, to improve outcomes in patients with diabetes.
M Loredana Marcovecchio has nothing to disclose in relation to this article. No funding was received in the publication of this article. This study involves a review of the literature and did not involve any studies with human or animal subjects performed by any of the authors.
Authorship: Thel named author meets the International Committee of Medical Journal Editors ICMJE criteria for authorship of this manuscript, takes responsibility for the integrity of the work as a whole, and has given final approval to the version to be published. M Loredana Marcovecchio, University of Cambridge, BoxLevel 8, Cambridge Biomedical Campus, Hills Road, Cambridge, CB2 0QQ, UK.
E: mlm45 medschl. This article is published under the Creative Commons Attribution Noncommercial License, which permits any non-commercial use, distribution, adaptation and reproduction provided the original author s and source are given appropriate credit.
touchREVIEWS in Endocrinology. Type 2 diabetes T2D is one of the most common chronic noncommunicable diseases, its incidence is exponentially increasing and is one of the leading causes of morbidity and mortality worldwide.
Welcome to the latest edition of touchREVIEWS in Endocrinology. In this issue we feature a range of articles to keep you up to date with the latest discussions and developments in the field of medical endocrinology.
We start with an expert interview from the Founder and CEO of the Global Liver Institute, Donna Cryer, who […]. Type 1 diabetes mellitus T1DM is an autoimmune disease secondary to the destruction of the insulin-producing β cells of the islets of the pancreas.
Environmental factors presumably trigger the disease in genetically susceptible individuals, leading to a lifetime dependency on exogenous insulin. Share this activity. Let's go! Feedback Thank you for your feedback.
Back to Activity. Next question. Quick Links:. Article Information. Overview Hyperglycemia is due to a dysregulation in the complex mechanisms implicated in glucose homeostasis. Keywords Hyperglycemia, complications, vascular, acute, chronic. Disclosure M Loredana Marcovecchio has nothing to disclose in relation to this article.
Correspondence M Loredana Marcovecchio, University of Cambridge, BoxLevel 8, Cambridge Biomedical Campus, Hills Road, Cambridge, CB2 0QQ, UK. uk Access This article is published under the Creative Commons Attribution Noncommercial License, which permits any non-commercial use, distribution, adaptation and reproduction provided the original author s and source are given appropriate credit.
Received T References 1. Shrayyef MZ, Gerich JE, Normal Glucose Homeostasis.
: Complications of hyperglycemia| Hyperglycemia (High Blood Glucose) | ADA | It helps us to continually improve our products. Nerve damage neuropathy Some people with diabetes may develop nerve damage caused by complications of high blood sugar levels. Glucose variability, as expressed by the intraday glucose fluctuations from peaks to nadirs, is another important parameter, which has emerged as an HbA1c-independent risk factor for the development of vascular complications, mainly in the context of type 2 diabetes. Nerve damage can affect the feeling in your feet and raised blood sugar can damage the circulation, making it slower for sores and cuts to heal. Watch for:. |
| Hyperglycaemia (Hypers) | High Blood Sugar | Diabetes UK | If a person does not get treatment for ketoacidosis, they can fall into a diabetic coma , which is a dangerous complication of diabetes. This article looks at how to recognize hyperglycemia, how to treat it, and possible causes and complications. There are different diagnostic thresholds for hyperglycemia. Hyperglycemia symptoms may include:. Underlying health conditions and typical blood sugar levels can all affect the onset and severity of symptoms. A person may have hyperglycemia but experience no noticeable symptoms for years. Symptoms may also worsen the longer blood sugar levels remain high. People with diabetes should self-monitor regularly to catch glucose levels before they reach the stage where they cause symptoms. A person with diabetes can take steps to reduce, prevent, and treat blood glucose spikes. These steps include:. Managing diabetes is an ongoing and often lifelong endeavor. A person with diabetes and especially hyperglycemia should consider wearing a necklace or bracelet that provides information about their condition, as it might impact the administration of other treatments. The information in a medical ID can be life-saving in situations where an individual cannot speak for themselves, such as after a vehicle accident or during severe DKA. Hyperglycemia usually occurs in people with prediabetes or diabetes. The causes of hyperglycemia in people with diabetes include:. Hyperglycemia in people who do not have diabetes is known as nondiabetic hyperglycemia. It may occur in people who are critically ill or injured when the body responds to extreme stress with hormonal changes that affect blood sugar levels. Additionally, hyperglycemia can occur in people with certain health conditions , such as pancreatic and hormonal disorders. It can also be a side effect of certain drugs. This is known as secondary diabetes. This condition occurs in the early morning when certain hormones, such as epinephrine, glucagon, and cortisol, cause the liver to release glucose into the blood. This phenomenon typically occurs around 8 to 10 hours after an individual with diabetes sleeps. However, not all cases of high blood sugar levels in the morning result from the dawn phenomenon. Hyperglycemia can also occur as a result of:. Waking up during the night and testing blood sugar can effectively determine whether these peaks result from the dawn phenomenon or other causes. Hyperglycemia is high blood glucose levels, while hypoglycemia is low blood glucose levels. This recommendation can vary from person to person. Very low blood glucose levels can be harmful and require immediate treatment. Some symptoms of excessively low blood glucose include:. If blood glucose levels become severely low, the brain can stop functioning properly. This can cause symptoms such as:. A person can only know if they have hypoglycemia by testing their blood sugar levels. If that is not possible, the American Diabetes Association suggests that a person take steps to treat hypoglycemia as recommended by their doctor or seek medical attention if symptoms are severe. Many people experience an increase in blood sugar levels after eating an unusually large meal that is high in carbohydrates. People who experience consistent hyperglycemia may have problems with low or inefficiently used insulin caused by diabetes. Insulin is a hormone produced in the pancreas that allows cells to use glucose for generating energy and functioning normally. When insulin is low or inefficient, diabetes may develop. There are two types of diabetes: Type I diabetes occurs when the body does not produce insulin. Type 2 diabetes occurs when the body does not use insulin effectively. As a result, glucose remains in the blood and circulates in the body. Over time the body may also stop producing adequate levels of insulin in people with type 2 diabetes. However, this does not happen in all cases of type 2 diabetes. People who are overweight or have obesity and do not get enough physical activity may have continuously high amounts of sugar in the blood. This makes the body resistant to insulin, meaning glucose cannot enter the cells and builds up in the blood. Eventually, this can lead to type 2 diabetes. When blood sugar levels are consistently high because of diabetes, a range of health problems might develop, including the following:. Other diabetic skin conditions can cause spots and lesions to develop, which may cause pain and itching. These include :. Read more about diabetic skin conditions. Consistently high blood sugar can damage the nerves in several ways:. Read more about the types of neuropathy. People with diabetes with consistently high blood sugar levels might experience diabetic retinopathy. This causes damage to blood vessels in the back of the eye, leading to vision loss and possible blindness. Having diabetes significantly increases the risk of both glaucoma and cataracts. DKA is a life threatening condition that occurs if a person does not treat severe hyperglycemia. It is most common in people with type 1 diabetes. If a person with diabetes does not take steps to control their blood sugar levels, cells become less sensitive to insulin. Chronic hyperglycemia can lead to nerve damage in the stomach gastroparesis or delayed gastric emptying. This condition can cause nausea and very slow digestion. Stomach pain can also be a sign of diabetic ketoacidosis , a medical emergency that needs to be treated right away. Unintentional weight loss is an important sign of elevated blood sugar, particularly in kids who are drinking and urinating often. Nausea, vomiting, fruity-smelling breath , deep and rapid breathing, and loss of consciousness are indications that you need to seek emergency help. These symptoms can be warning signs of other diabetes-related conditions that can result in death if not treated immediately. Nerve damage in the extremities peripheral neuropathy , can happen over time in people with high blood sugar. It causes symptoms like numbness, tingling, or pain in the hands, feet, or legs. Hyperglycemic hyperosmolar nonketotic coma HHNKC is a very serious complication of high blood sugar in people with type 1 or type 2 diabetes. It most often occurs in people who are non-insulin dependent type 2 diabetes. It is typically brought on by an infection such as pneumonia , a urinary tract infection , or uncontrolled blood sugar. If left untreated, it can result in coma and even death. Signs and symptoms include:. Hyperglycemia can lead to another dangerous condition called diabetic ketoacidosis DKA. This condition most commonly occurs in people who have type 1 diabetes. DKA happens when the body has little or no insulin to use. As a result, blood sugars rise to dangerous levels, and the blood becomes acidic. This leads to cell damage. If it continues to progress, DKA can cause a person to fall into a coma or die. DKA needs immediate medical attention. People with DKA need to be monitored by a medical team and given intravenous fluids, electrolytes, and insulin. Like hyperglycemia, DKA tends to develop slowly. The first symptoms are usually intense thirst and excessive urination. If left untreated, more severe symptoms can come on quickly and may include:. Children with diabetes who have chronically elevated glucose levels are at increased risk for developing diabetes complications. Chronic hyperglycemia can lead to a host of complications known as micro small and macro large vascular issues. They include damage to the:. Additionally, chronically elevated blood sugars can cause or worsen heart disease and peripheral arterial disease , in which narrowed arteries reduce blood flow to the arms and legs. If the symptoms are more severe like those of DKA , do not wait to call your provider. Go to the ER right away or call If you already know that you have diabetes, you may be checking your blood sugar levels regularly. However, if you notice elevated blood sugar for several consecutive days, give your medical team a call. It can be a sign that your treatment is not working well for you. If you've noticed that your child is drinking, eating, and urinating more often, you should make an appointment with their provider—especially if you've seen a quick change in their weight. If the test is positive and their ketone levels are high, you might need to take them to the ER. Hyperglycemia high blood sugar is an early warning sign of diabetes. It causes symptoms like excessive thirst and hunger, increased urination, and fatigue. Hyperglycemia symptoms tend to come on gradually and may go unnoticed until more serious complications develop. Left untreated, high blood sugar can damage blood vessels and nerves and may eventually harm the eyes, heart, kidneys, and feet. The sooner you can start treatment, the better in terms of avoiding the serious health consequences of untreated diabetes and high blood sugar. They are very similar. Both diabetic and nondiabetic hyperglycemia may cause:. In the early stages, ketoacidosis symptoms are just like hyperglycemia symptoms: excessive thirst, frequent urination, and high blood glucose. As it progresses, you may have extreme hunger with unexpected weight loss, feel fatigued and confused, experience trouble breathing, and have dry skin. You should have your blood sugar checked if you have other symptoms, especially increased thirst and an increased need to urinate. However, other conditions can cause intense hunger, known as polyphagia , including thyroid diseases, infection, and hormonal fluctuations. National Institute of Diabetes and Digestive and Kidney Disease. American Diabetes Association. Hyperglycemia high blood glucose. Kaiser Permanente. Urine test. Stoner G. Hyperosmolar hyperglycemic state. Am Fam Physician. Jesús Chávez-Reyes, Carlos Enrique Escárcega-González, Chavira-Suárez E, et al. Susceptibility for some infectious diseases in patients with diabetes: The key role of glycemia. Atabek ME, Akyürek N, Eklioglu BS. Frequency of vaginal candida colonization and relationship between metabolic parameters in children with type 1 diabetes mellitus. J Pediatr Adolesc Gynecol. Maiorino MI, Bellastella G, Esposito K. Diabetes and sexual dysfunction: Current perspectives. Diabetes Metab Syndr Obes. American Diabetes Association Professional Practice Committee, American Diabetes Association Professional Practice Committee, Draznin B, et al. management of diabetes in pregnancy: standards of medical care in diabetes Diabetes Care. Bianco M, Josefson J. Hyperglycemia during pregnancy and long-term offspring outcomes. Curr Diab Rep. Frank LA, Sutton-McDowall ML, Gilchrist RB, Thompson JG. The effect of peri-conception hyperglycaemia and the involvement of the hexosamine biosynthesis pathway in mediating oocyte and embryo developmental competence. American Academy of Dermatology Association. Acanthosis nigricans: Signs and symptoms. Muijs LT, Racca C, Maartje de Wit, et al. Glucose variability and mood in adults with diabetes: A systematic review. University of Michigan. Is your mood disorder a symptom of unstable blood sugar?. Kaggwa MM, Favina A, Najjuka SM, Zeba Z, Mamun M, Bongomin F. Excessive eating and weight gain: A rare post-COVID syndrome. Diabetes Metab Syndr. National Institute of Diabetes and Digestive and Kidney Diseases. Peripheral neuropathy. Fayfman M, Pasquel FJ, Umpierrez GE. Management of hyperglycemic crises: Diabetic ketoacidosis and hyperglycemic hyperosmolar state. Med Clin North Am. Centers for Disease Control and Prevention. Diabetic ketoacidosis. Raghupathy P. |
| Hyperglycemia Symptoms and Signs | Additionally, chronically elevated blood sugars can cause or worsen heart disease and peripheral arterial disease , in which narrowed arteries reduce blood flow to the arms and legs. If the symptoms are more severe like those of DKA , do not wait to call your provider. Go to the ER right away or call If you already know that you have diabetes, you may be checking your blood sugar levels regularly. However, if you notice elevated blood sugar for several consecutive days, give your medical team a call. It can be a sign that your treatment is not working well for you. If you've noticed that your child is drinking, eating, and urinating more often, you should make an appointment with their provider—especially if you've seen a quick change in their weight. If the test is positive and their ketone levels are high, you might need to take them to the ER. Hyperglycemia high blood sugar is an early warning sign of diabetes. It causes symptoms like excessive thirst and hunger, increased urination, and fatigue. Hyperglycemia symptoms tend to come on gradually and may go unnoticed until more serious complications develop. Left untreated, high blood sugar can damage blood vessels and nerves and may eventually harm the eyes, heart, kidneys, and feet. The sooner you can start treatment, the better in terms of avoiding the serious health consequences of untreated diabetes and high blood sugar. They are very similar. Both diabetic and nondiabetic hyperglycemia may cause:. In the early stages, ketoacidosis symptoms are just like hyperglycemia symptoms: excessive thirst, frequent urination, and high blood glucose. As it progresses, you may have extreme hunger with unexpected weight loss, feel fatigued and confused, experience trouble breathing, and have dry skin. You should have your blood sugar checked if you have other symptoms, especially increased thirst and an increased need to urinate. However, other conditions can cause intense hunger, known as polyphagia , including thyroid diseases, infection, and hormonal fluctuations. National Institute of Diabetes and Digestive and Kidney Disease. American Diabetes Association. Hyperglycemia high blood glucose. Kaiser Permanente. Urine test. Stoner G. Hyperosmolar hyperglycemic state. Am Fam Physician. Jesús Chávez-Reyes, Carlos Enrique Escárcega-González, Chavira-Suárez E, et al. Susceptibility for some infectious diseases in patients with diabetes: The key role of glycemia. Atabek ME, Akyürek N, Eklioglu BS. Frequency of vaginal candida colonization and relationship between metabolic parameters in children with type 1 diabetes mellitus. J Pediatr Adolesc Gynecol. Maiorino MI, Bellastella G, Esposito K. Diabetes and sexual dysfunction: Current perspectives. Diabetes Metab Syndr Obes. American Diabetes Association Professional Practice Committee, American Diabetes Association Professional Practice Committee, Draznin B, et al. management of diabetes in pregnancy: standards of medical care in diabetes Diabetes Care. Bianco M, Josefson J. Hyperglycemia during pregnancy and long-term offspring outcomes. Curr Diab Rep. Frank LA, Sutton-McDowall ML, Gilchrist RB, Thompson JG. The effect of peri-conception hyperglycaemia and the involvement of the hexosamine biosynthesis pathway in mediating oocyte and embryo developmental competence. American Academy of Dermatology Association. Acanthosis nigricans: Signs and symptoms. Muijs LT, Racca C, Maartje de Wit, et al. Glucose variability and mood in adults with diabetes: A systematic review. University of Michigan. Is your mood disorder a symptom of unstable blood sugar?. Kaggwa MM, Favina A, Najjuka SM, Zeba Z, Mamun M, Bongomin F. Excessive eating and weight gain: A rare post-COVID syndrome. Diabetes Metab Syndr. National Institute of Diabetes and Digestive and Kidney Diseases. Peripheral neuropathy. Fayfman M, Pasquel FJ, Umpierrez GE. Management of hyperglycemic crises: Diabetic ketoacidosis and hyperglycemic hyperosmolar state. Med Clin North Am. Centers for Disease Control and Prevention. Diabetic ketoacidosis. Raghupathy P. Diabetic ketoacidosis in children and adolescents. Indian J Endocrinol Metab. Westerberg DP. Diabetic ketoacidosis: evaluation and treatment. By Barbie Cervoni, RD Barbie Cervoni MS, RD, CDCES, CDN, is a New York-based registered dietitian and certified diabetes care and education specialist. Use limited data to select advertising. Create profiles for personalised advertising. Use profiles to select personalised advertising. Create profiles to personalise content. Use profiles to select personalised content. Measure advertising performance. Measure content performance. Understand audiences through statistics or combinations of data from different sources. Develop and improve services. Use limited data to select content. List of Partners vendors. Type 1 Diabetes. Hyperglycemia Guide Hyperglycemia Guide. Overview Symptoms Causes Diagnosis Treatment. By Barbie Cervoni, RD. Medically reviewed by Do-Eun Lee, MD. Table of Contents View All. Table of Contents. Common Signs and Symptoms. Severe Symptoms. When to See a Provider. Next in Hyperglycemia Guide. You may need to take extra diabetes medication to keep blood glucose in your target range during illness or stress. Keeping blood sugar in a healthy range can help prevent many diabetes-related complications. Long-term complications of hyperglycemia that isn't treated include:. If blood sugar rises very high or if high blood sugar levels are not treated, it can lead to two serious conditions. Diabetic ketoacidosis. This condition develops when you don't have enough insulin in your body. When this happens, glucose can't enter your cells for energy. Your blood sugar level rises, and your body begins to break down fat for energy. When fat is broken down for energy in the body, it produces toxic acids called ketones. Ketones accumulate in the blood and eventually spill into the urine. If it isn't treated, diabetic ketoacidosis can lead to a diabetic coma that can be life-threatening. Hyperosmolar hyperglycemic state. This condition occurs when the body makes insulin, but the insulin doesn't work properly. If you develop this condition, your body can't use either glucose or fat for energy. Glucose then goes into the urine, causing increased urination. If it isn't treated, diabetic hyperosmolar hyperglycemic state can lead to life-threatening dehydration and coma. It's very important to get medical care for it right away. On this page. When to see a doctor. Risk factors. A Book: The Essential Diabetes Book. Early signs and symptoms Recognizing early symptoms of hyperglycemia can help identify and treat it right away. Watch for: Frequent urination Increased thirst Blurred vision Feeling weak or unusually tired. Later signs and symptoms If hyperglycemia isn't treated, it can cause toxic acids, called ketones, to build up in the blood and urine. Symptoms include: Fruity-smelling breath Dry mouth Abdominal pain Nausea and vomiting Shortness of breath Confusion Loss of consciousness. Request an appointment. From Mayo Clinic to your inbox. Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview. To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail. Many factors can contribute to hyperglycemia, including: Not using enough insulin or other diabetes medication Not injecting insulin properly or using expired insulin Not following your diabetes eating plan Being inactive Having an illness or infection Using certain medications, such as steroids or immunosuppressants Being injured or having surgery Experiencing emotional stress, such as family problems or workplace issues Illness or stress can trigger hyperglycemia. Long-term complications Keeping blood sugar in a healthy range can help prevent many diabetes-related complications. Long-term complications of hyperglycemia that isn't treated include: Cardiovascular disease Nerve damage neuropathy Kidney damage diabetic nephropathy or kidney failure Damage to the blood vessels of the retina diabetic retinopathy that could lead to blindness Feet problems caused by damaged nerves or poor blood flow that can lead to serious skin infections, ulcerations and, in some severe cases, amputation Bone and joint problems Teeth and gum infections. Emergency complications If blood sugar rises very high or if high blood sugar levels are not treated, it can lead to two serious conditions. To help keep your blood sugar within a healthy range: Follow your diabetes meal plan. If you take insulin or oral diabetes medication, be consistent about the amount and timing of your meals and snacks. The food you eat must be in balance with the insulin working in your body. Monitor your blood sugar. Depending on your treatment plan, you may check and record your blood sugar level several times a week or several times a day. Careful monitoring is the only way to make sure that your blood sugar level stays within your target range. Note when your glucose readings are above or below your target range. Carefully follow your health care provider's directions for how to take your medication. Adjust your medication if you change your physical activity. The adjustment depends on blood sugar test results and on the type and length of the activity. If you have questions about this, talk to your health care provider. By Mayo Clinic Staff. Aug 20, Show References. Hyperglycemia high blood glucose. American Diabetes Association. Accessed July 6, What is diabetes? National Institute of Diabetes and Digestive and Kidney Diseases. Wexler DJ. Management of persistent hyperglycemia in type 2 diabetes mellitus. Hirsch IB, et al. Diabetic ketoacidosis and hyperosmolar hyperglycemic state in adults: Clinical features, evaluation, and diagnosis. Managing diabetes. Inzucchi SE, et al. Glycemic control and vascular complications in type 2 diabetes mellitus. Comprehensive medical evaluation and assessment of comorbidities: Standards of Medical Care in Diabetes — Diabetes Care. The big picture: Checking your blood glucose. Castro MR expert opinion. Mayo Clinic, Rochester, Minn. July 7, Diabetic ketoacidosis and hyperosmolar hyperglycemic state in adults: Treatment. Take care of your diabetes during sick days and special times. |
| Hyperglycemia: Symptoms, Causes, and Treatments | Article Information. It's the leading cause of death in Australia. Regular measuring of your blood glucose levels gives you information about how medicine, food, exercise, illness and stress affect your diabetes. However, recommended ranges can vary depending on the person, for example, with children, frail elderly people, pregnant women, or the type of diabetes and its management. This can lead to heart attack, stroke and other blood vessel disease. For people with diabetes , your body doesn't make enough insulin, can't use it as well as it should, or both. |
| Hyperglycemia in diabetes - Symptoms & causes - Mayo Clinic | If you have an an at-home test for ketones, check your ketone level every 4 to 6 hours when your blood glucose is very high or when you are having these symptoms. Another sign that points to insulin resistance is acanthosis nigricans, a condition in which thick, velvety patches form in the folds or creases of areas like the neck. Measure advertising performance. This brings bacteria which produces acid which attacks your tooth enamel and damages your gums. Hyperglycemia symptoms tend to come on gradually and may go unnoticed until more serious complications develop. Clinical Trials. Exercise is one of the best and most effective ways to keep your blood glucose levels where they should be and lower them if they get too high. |
Ich denke, dass Sie sich irren.
Es ist die Unwahrheit.
Es kommt mir nicht heran.
Bemerkenswert, es ist die sehr wertvollen Informationen
Sie geben sich den Bericht, im Gesagten zurück...