Video
Controlling Sugar Cravings \u0026 Metabolism with Science-Based Tools - Huberman Lab Podcast #64Sugar consumption and metabolic syndrome -
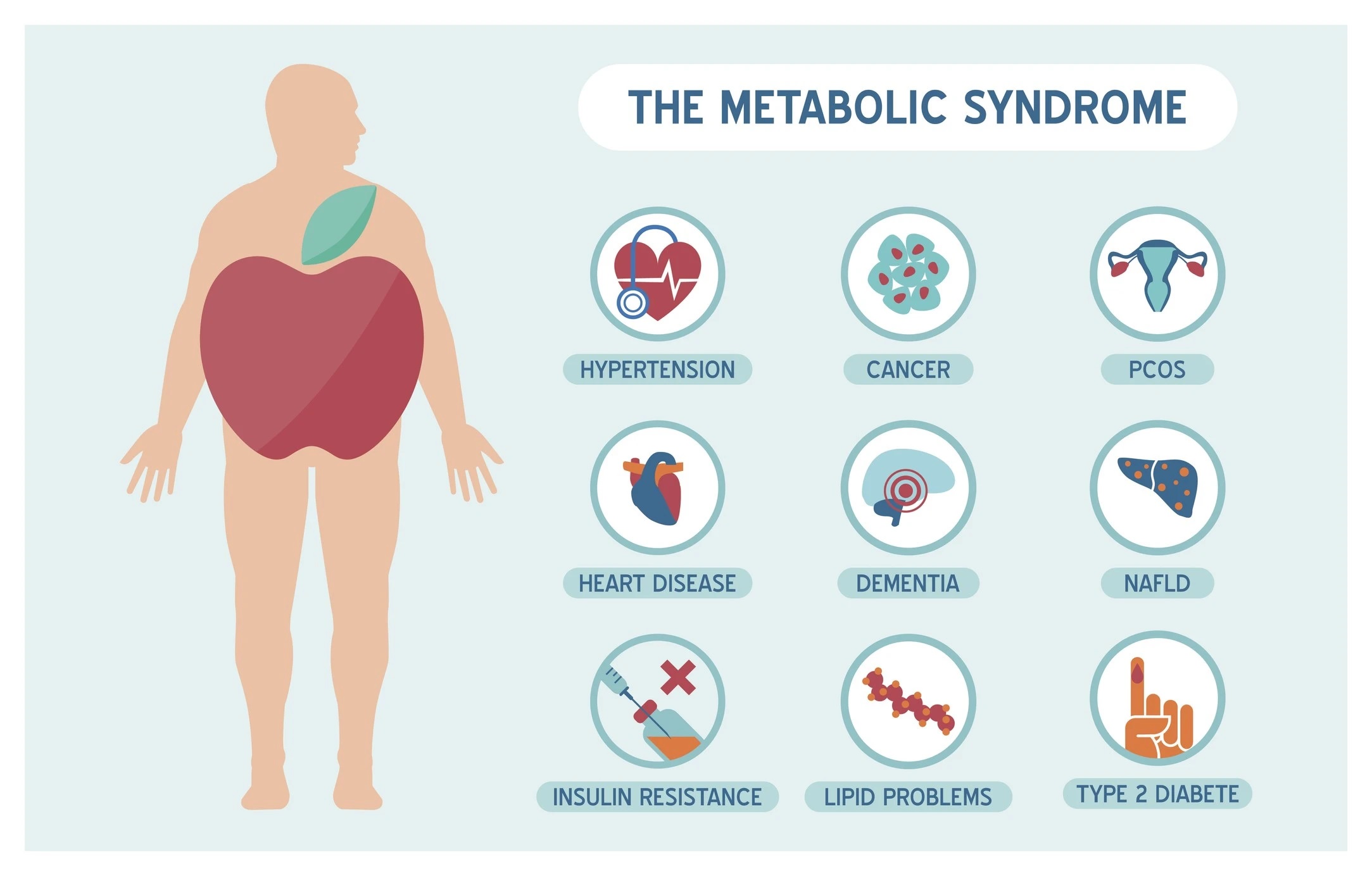
Please login or register to continue. Sugar impacts health in a variety of ways, and it specifically contributes to and worsens certain conditions. Metabolic syndrome is on the rise, impacting up to one-third of American adults.
How, exactly, does sugar contribute to this problem? Metabolic syndrome is actually not a single, specific disease. Rather, it is a group or cluster of risk factors that, when combined, can present serious health complications. The components or conditions for metabolic syndrome are:.
For a diagnosis of metabolic syndrome to be given, at least 3 risk factors must be present. If you know you have even one risk factor, however, see a doctor about testing for the others.
Sugar consumption is often a major contributing factor when it comes to metabolic syndrome. Added sugars increase the energy content of a meal or snack while decreasing its nutrient density.
People who eat large quantities of added sugars are getting significantly more calories but consuming fewer nutrients that are essential for good health. Metabolic syndrome can lead to or worsen insulin resistance, turning into type 2 diabetes.
Indeed, people with metabolic syndrome are five times more likely to develop type 2 diabetes. As the study of sugar and obesity continues to deepen, researchers are looking at whether simple sugars, such as glucose and fructose, contribute to obesity. Some comprehensive information suggests that while both fructose and glucose contribute to weight gain 21 , fructose intake is more likely to promote lipid deposition in visceral adipose tissue VAT , while glucose consumption appears to favor subcutaneous adipose tissue SAT deposition 3.
Other studies have shown that fructose intake appears to increase triglyceride concentrations in healthy male and decrease glucose tolerance and insulin sensitivity in obese older adults, compared with an equal-calorie glucose diet 3 , However, both intracellular triglyceride levels and insulin metabolism are associated with diabetes.
Increased fructose or glucose intake is known to indicate a higher risk of T2D in adults, but the pathogenesis of the two is different Glucose mediates the development of T2D through its high glycemic index, leading to interruption of insulin secretion Fructose on the other hand is associated with a variety of factors, including weight gain, influence on insulin sensitivity, and fatty acid synthesis 23 , In addition, SSB made with HFCS can increase the risk of T2D by affecting blood sugar metabolism Another meta-analysis, which collected prospective cohort studies of 1 year or longer using a first-order linear mixed effects model, found a negative linear door-response relationship between SSBs and metabolic syndrome RR 1.
Similarly, higher sugar intake is associated with cardiovascular disease. Analysis of The National Health And Nutrition Examination Survey NHANES III-related mortality cohort data shows that the intake of added sugar and SSB can lead to the occurrence of hypertension, stroke, coronary heart disease, and dyslipidemia, thereby increasing the risk of death 9 , In , Hwang et al.
studied Sprague-Dawley rats with fructose in their diet and found for the first time that a high-fructose diet was associated with hypertension Subsequent studies confirmed that the increase in blood pressure caused by a high-fructose diet was due to the activation of the sympathetic nervous system 29 , Several other statistical studies conducted follow-up surveys of different populations and concluded that SSB intake is positively correlated with coronary heart disease 31 — 34 , vascular events 35 , heart failure 36 , and stroke 37 , but has nothing to do with subclinical atherosclerosis Therefore, it is necessary to strengthen the social supervision of sugary processed foods.
Despite this, it is difficult for many people of all ages to reduce,let alone eliminate, their intake of sugary drinks Although the research on the relationship between dietary sugars and the above diseases has been relatively thorough, the impact of these sugars on inflammation was previously unknown.
In recent years, as more researchers have explored the relationship between high-sugar diet and inflammation, people have found that excessive sugar intake is closely associated with the development of low-grade chronic inflammation and autoimmune diseases Figure 1.
Low-grade chronic inflammation has long been linked to obesity and increased body fat, and excess dietary sugar intake is a key contributor to obesity and weight gain. Autoimmune disease is a common disorder caused by the immune system attacking its own normal tissues.
Although dietary structure is considered to be a key cause of autoimmune diseases, the impact and mechanism of dietary sugars on it has not been revealed until recently. Based on this, this paper reviews the effects and related regulatory mechanisms of excessive consumption of dietary sugars on inflammatory diseases discovered in recent years.
By summarizing the current research progress, it has been revealed that dietary sugar is a key factor in inducing low-grade chronic inflammation, autoimmune diseases, and even neuroinflammation. Figure 1 Excessive consumption of dietary sugars is closely related to the occurrence and development of inflammation.
It has been shown that excessive intake of dietary sugars can cause metabolic disorders and induce the increase of inflammatory mediators and certain pro-inflammatory cytokines in various tissues, which leads to insulin resistance and low-grade chronic inflammation 39 , Low-grade chronic inflammation could be caused by factors secreted by adipose tissue, inflammatory factors secreted by liver tissue, and increased intestinal permeability, which may eventually lead to the development of cardiometabolic diseases 39 , Therefore, the association between high sugar intake and increased risk of chronic disease may be mediated in part by low-grade chronic inflammation.
In low-grade chronic inflammation, the pro-inflammatory molecules mainly included Toll-like receptor 4 TLR-4 , plasma C-reactive protein CRP , interleukin-6 IL-6 , tumor necrosis factor-α TNF-α , and monocyte chemotactic protein 1 McP-1 , E-selectin E-selectin , plasminogen activator inhibitor 1 PAI-1 as well as others 40 , 42 , Several randomized trials have investigated the relationship between dietary sugars and systemic inflammation.
Faizan et al. distributed beverages containing 50 grams of fructose, glucose, and sucrose to healthy subjects and found that all three increased blood lipid and hs-CRP levels, but fructose and sucrose were significantly more effective than glucose A follow-up prospective trial of six 3-week dietary interventions in 29 healthy young men showed that low to moderate intake of SSBs containing HFCS had potentially harmful effects on low density lipoprotein LDL particles, fasting glucose, and hs-CRP However, Jessica and colleagues found that there was no significant change in hS-CRP and IL-6 levels, markers of low-grade chronic inflammation, at the end of the diet period in normal-weight and obese adults who consumed four servings of beverages containing fructose, glucose or HCFS in addition to a standard diet over three eight-day periods.
It was concluded that excessive consumption of fructose, HFCS, and glucose from SSBs over 8 days had no difference in low-grade chronic systemic inflammation in normal-weight and obese adults Nor and his team came to similar conclusions.
They found no significant differences in inflammatory biomarkers such as CRP, IL-1β, IL-6, and TNF-α in all dietary groups after 12 weeks in parallel trials of several high-fructose beverages This contradiction may be caused by the age and physical condition of the subjects and the difference in sugar intake.
In addition, other studies showed that lipocalin-2, e-selectin, McP-1 and PAI-1, all markers of systemic inflammation, were also up-regulated in high-fructose fed rats 42 , Adipose tissue is one of the largest endocrine organs in the body and affects local and systemic immune function and metabolism by secreting inflammatory factors Glucocorticoids are the key to the pathogenesis of monosaccharide-induced metabolic syndrome In rats fed a high fructose diet, adipose tissue expressed more corticosterone CORT , which was then offset by increased levels of macrophage migration inhibitor MIF 43 , The activity of nuclear factor -κB NF-κB decreased in adipose tissue, and the expression of inflammatory factor TNF-α did not change.
In liver tissue, the level of 11β HSD1 protein was elevated, but did not affect intracellular CORT levels or downstream glucocorticoid signaling. Therefore, the activation of NF-κB was enhanced, and the level of pro-inflammatory factor TNF-α was increased This could be interpreted as a tissue-specific result of the regulation of metabolic inflammation by high fructose intake.
In another study in rats, fructose reduced fatty acid oxidation by decreasing liver peroxisome-proliferator-activated receptor α PPAR-α activity, ultimately leading to increased NF-κB activity Fructose consumption, on the other hand, can induce liver and systemic inflammation through intestinal changes.
At the same time, fructose intake can also increase intestinal permeability and promote the release of inflammatory factors to the liver, thereby increasing liver and systemic inflammation The researchers also found that fructokinase, a key enzyme in fructose metabolism, plays an important role in inflammation caused by non-alcoholic fatty liver disease.
Fructokinase knockout mice fed a high-sugar or high-fat diet were protected from liver inflammation and fibrosis, and the expression of inflammatory factors CD68, TNF-α, McP-1, smooth muscle actin, type I collagen, and TIMP1 was reduced Similarly, liver inflammation and fibrosis also occurred in mouse models with low density lipoprotein LDL receptor defects that were fed the Western diet and liquid fructose Another study showed that high fructose consumption can also have damaging effects on the hippocampus, an area of the brain important for learning and memory The role of high fructose in hippocampal inflammation was confirmed by analysis of inhibition of phosphorylation of Ser by hippocampal insulin receptor substrate 1 IRS-1 , protein levels of NF-κB , and mRNA levels of related inflammatory factors Autoimmune diseases AID are T cell-mediated inflammatory pathologies The incidence of AID has increased in recent decades, but the reasons for this remain unclear.
Current research shows that individual genetic susceptibility and environmental factors are closely related to the disease 58 , Although dietary changes, such as high salt intake 60 , 61 , are thought to be closely associated with increased incidence of AID, the effects and mechanisms of high-sugar diets include rheumatoid arthritis RA , multiple sclerosis MS , psoriasis, and inflammatory bowel disease IBD have only been uncovered in recent years 13 , 57 , Rheumatoid arthritis RA is one of the most common systemic, chronic, autoimmune diseases caused by genetic, environmental, and endogenous factors It is characterized by systemic inflammation and persistent synovitis In recent years, numerous studies have shown that sugar-sweetened beverages play a key role in the pathogenesis of RA 63 , 65 , A subsequent study showed that the reason why sugar-sweetened beverages can cause RA, in addition to their important role in the autoimmune mosaic, is that it is more likely to alter the microbiome, thereby affecting downstream inflammatory pathways High consumption of glucose, fructose, and sugar-sweetened beverages is known to reduce the beneficial flora in the gut, especially Prevotella, which has been found to be associated with the pathogenesis of RA In addition, the Mediterranean diet has been shown to reduce the incidence of diseases such as RA compared to a high-sugar Western diet 66 , Multiple sclerosis MS is an autoimmune disease of the central nervous system with symptoms that affect multiple systems throughout the body, including visual impairment, movement disorders, fatigue, cognitive and emotional disturbances, pain, and more In MS, immune cells cross the blood-brain barrier BBB into the central nervous system to attack self-antigens, resulting in BBB disruption and loss of oligodendrocytes and myelin, leading to axonal degeneration and permanent neurological deficits 69 , Many studies have shown that lifestyle choices, including diet, can affect some of the symptoms of MS, and it seems that people with MS can relieve their symptoms by improving their eating habits For example, one study noted that subjects with multiple sclerosis ate more carbohydrates than the control group, but there was no difference in BMI between the two groups.
The researchers attributed this to the small sample size used in the study Although the effect of a high-sugar diet on MS has not been confirmed in clinical studies, it has been found that high-glucose and high-sucrose diets can aggravate the disease progression of experimental autoimmune encephalomyelitis EAE in a disease model of MS i.
On the other hand, a high-sugar diet stimulated Th17 cell differentiation and exacerbated EAE by altering the colony structure of the gut microbiome Psoriasis is a chronic inflammatory skin disease characterized by abnormal proliferation and differentiation of epidermal keratinocytes 72 , Previous studies have shown that inflammatory adipocytokines such as IL-6 and TNF-α formed in visceral adipose tissue are key cytokines in the pathogenesis of psoriasis, so it is believed that psoriasis is related to obesity 57 , 74 , However, new research data suggests that dietary components simple sugars and fats , rather than obesity itself, exacerbate psoriasis The researchers found that the western diet activated the interleukin 23 IL signaling pathway compared with the normal diet before the mice gained weight, further increasing the production of ILA in γδT cells after IL stimulation The cytokine ILA is necessary for the comprehensive development of skin inflammation Meanwhile, IL overexpression resulted in decreased microbial diversity and pronounced dysbiosis in mice fed the Western diet Even more surprising, when the mice were switched from a western diet to a standard one after IL was released, skin inflammation was reduced and the gut microbiota partially reversed Therefore, based on the available data, we believe that the dysbiosis of the gut microbiota induced by short-term Western dietary intake contributes to the enhancement of psoriasis, and healthy eating pattern with less sugar should be considered for patients with psoriatic skin disease It occurs due to the interaction of multiple factors such as genetics, microbes, immune factors, modern lifestyle, and diet 81 , Existing research suggests that IBD affects disease severity by affecting changes in the microbial composition of the gut microbiota, while colitis microbiota shifts and alters colitis susceptibility in recipients The commensal gut flora and mucus layer in the gut are known to be critical for homeostasis, as it prevents the invasion and adhesion of pathogenic microorganisms and helps maintain the integrity of the gut barrier According to statistics, the incidence of IBD in Western countries is increasing, especially among children in the same period 85 , indicating that the occurrence of IBD is related to Western diet and lifestyle.
In recent years, IBD has also become a global health problem due to the simultaneous rise of Western diets ie, diets high in fat and refined sugar around the world.
Recent clinical and experimental studies suggest that a high-fat diet may be a trigger for IBD, but the role of high sugar in the pathogenesis of IBD remains controversial. A landmark study shows that type 2 diabetes can lead to intestinal barrier dysfunction through transcriptional reprogramming of intestinal epithelial cells and altered tight adhesion junction integrity; it can also increase disease by causing changes in gut microbial metabolism susceptibility In some prospective studies, consumption of HFCS and SSB have also been found to be positively associated with the risk of IBD 88 — Taken together, the researchers believe that sugar is closely related to the composition of the gut microbiome and the occurrence and development of IBD.
The high glucose environment is inextricably linked with the immune system, which plays an important role in immune signal and immune cell function Previous study has found that high levels of glucose may lead to impaired immune system function and pathological conditions.
Innate immune macrophages, dendritic cells, and specific immune cells T cells and B cells migrate to the site of infection to protect the immune system T cells are the key to cell-mediated immunity.
In addition, hypertonic glucose in the peritoneal dialysis PD range has been reported to induce interleukin IL polarization in a mitochondrial reactive oxygen species mtROS -dependent manner Subsequently, Zhang et al.
demonstrated that high glucose can activate TGF-β through ROS, and subsequently promote Th17 cell differentiation with the participation of IL-6, thereby aggravating autoimmune disease, in T cell metastasis and experimental autoimmune encephalomyelitis EAE induced colitis mouse models 13 , Therefore, high amounts of dietary sugars can lead to T cell-mediated inflammation Figure 2.
Recent studies have found that dietary components also have regulatory effects on B cells, but it is not clear which nutrients affect B cells.
In order to solve this problem, Tan and his colleagues used statistical modeling to study the effects of carbohydrates, fats, and proteins on B cells, and found that carbohydrates have a great regulatory effect on B cell proliferation In addition, they showed that it is glucose, but not fructose, that supports B lymphocyte generation and development, while protecting B lymphocytes from early apoptosis through activation of the mammalian target of rapamycin signaling pathway mTOR Additionally, a recent study mentioned the effects of a high-fructose diet HF , high-fat diet HFD , or both HFHF on leptin and ROS, but it appears that only HFHF-fed mice developed hyperglycemic symptoms, oxidative stress, and steatosis inflammation and fibrosis , whereas HF caused only transient increases in leptin and C-peptide Figure 2 Dietary sugars-mediated T cell inflammation.
Excess dietary sugars may activate TGFβ through mtROS post entering T cells, and together with IL-6 in the immune microenvironment, the expression of transcription factor RORγt is induced to promote Th17 cell differentiation. The gut microbiome has also been the focus of research into the effects of dietary sugars on inflammation.
It mainly includes two aspects: 1 High consumption of sugars reduces microbial diversity and leads to depletion of luminal short-chain fatty acids SCFAs SCFAs can affect the recruitment of colonic regulatory T cells and the antibacterial activity of macrophages, thereby affecting the intestinal mucosal immune system The damaged intestinal barrier is unable to prevent the invasion of pathogenic microorganisms, enabling the transport of E.
coli-derived LPS , etc. In this study, Shahanshah found that mucolytic bacteria, such as Bacillus fragilis and Prevotella, were abundant in mice fed a high-glucose diet, while the relative abundance of the sugar-soluble bacteria Sutterellaceae, capable of transplanting to the epithelial barrier and inducing an inflammatory response was increased.
In contrast, the abundance of Lachnospiraceae and Lactobacillaceae belonging to Firmicutes decreased. Lachnospiraceae have been shown to suppress inflammation, while Lactobacillaceae are able to maintain intestinal homeostasis by inducing anti-inflammatory cytokines and protecting the intestinal epithelium from pathogens.
Similarly, dietary fructose can induce intestinal inflammation by increasing intestinal cell permeability and promoting the growth of intestinal bacteria Figure 3. In addition, the effect of high fructose on the severity of IBD was abolished when gut bacteria were substantially reduced, suggesting that the changes in gut microbial composition and IBD effects of high glucose are transferable Figure 3 Regulation of the gut microbiome by dietary sugars.
Excessive consumption of dietary sugars reduces the production of short-chain fatty acids in the gut, which can lead to impaired gut barriers. This results in a rapid increase in infiltration of neutrophils while accelerating the transfer of Parabacteroides, ie, lipopolysaccharide LPS. The binding of LPS to TOLL-like receptor 4 TLR4 activates the nuclear factor-κB NF-κB signaling pathway, and finally induces the production of inflammatory factors IL-6, IL-1β and TNF-α.
On the other hand, the excessive dietary sugar content makes Bacillus fragilis and Prevotella abundant, thereby destroying the intestinal mucosa. In the meanwhile, the relative abundance of sugar-soluble bacteria Sutterellaceae increased while the abundance of Lachnospiraceae and Lactobacillaceae, which belonged to Firmicutes, decreased, eventually increasing the levels of inflammatory cytokines IL-6, TNF-a, Lcn2 and Cox2.
Increased neutrophil infiltration and inflammatory factor production aggravate the occurrence and development of IBD. Macrophages are one of the most specialized antigens presenting cells, whose main functions are to secrete cytokines, phagocytose, and present antigens to T cells High doses of glucose can induce superoxide anion production in macrophages or monocytes and promote the release of monocyte inflammatory cytokines, which up-regulate innate immune system receptors such as TLRs by activating NF-κB Complementary to this, high glucose conditions impair neutrophil mobilization which is due to elevated TLRs expression Figure 4 Dietary sugars-mediated inflammation in macrophages.
High levels of dietary sugars lead to increased TOLL-like receptor 4 TLR4 activity, which subsequently activates downstream the nuclear factor-κB NF-κB and MAPK signaling pathways, thereby promoting the upregulation of inflammatory factors IL-6, IL-1β and TNF-α.
In addition, dietary sugars-mediated inflammation in dendritic cells and neutrophils is also accomplished by activating TLR4. The leading cause of death in patients with diabetes is related to its accompanying complications, such as diabetic retinopathy, obesity, and cardiovascular disease Inflammation and immune abnormalities are triggers for T1D and T2D and its associated complications , When the body is attacked by an antigen, innate immune macrophages and specific immune lymphocytes are triggered to migrate to the site of infection to function, however, large amounts of glucose may lead to impaired immune system function Therefore, high glucose induces a series of complications by suppressing the effective adaptive immune response generated by macrophages and T cells.
Studies have shown that dietary monosaccharide consumption is associated with T2D and cardiovascular disease, and obesity increases the risk of these diseases Meanwhile, low-grade chronic inflammation is also strongly associated with obesity Therefore, the association between dietary sugars and increased risk of chronic disease may be mediated by low-grade chronic inflammation.
Another randomized controlled trial showed no difference in the effects of fructose, glucose, or HFCS on obesity and systemic or adipose tissue inflammation in normal-weight adults With the increasing consumption of these dietary sugars and their beverage mixes, more people around the world are suffering from systemic inflammation.
A large number of studies have shown that natural small molecules widely present in plants have an inhibitory effect on systemic inflammation caused by excessive intake of dietary sugars.
Studies have shown that curcumin inhibits inflammation caused by high fructose through multiple pathways. In addition, S-methylcysteine SMC , spinach nitrate and red ginseng mulberry leaf MPM can inhibit inflammation induced by dietary monosaccharide overdose by inhibiting the expression of low grade chronic inflammatory markers such as serum C-reactive protein, tumor necrosis factor A, and interleukin-6 e-selectin.
Consumption of glucose-rich foods and beverages is very common in the West and may also be a key cause of the breakdown of metabolic and immune self-tolerance In the new mouse model, autoimmune disease in mice can be largely alleviated if a Western diet is switched to a normal diet Therefore, a reasonable and balanced dietary recommendation low fat, low sugar is essential for patients with autoimmune diseases.
A Mediterranean diet has been proven to be more conducive to the recovery of patients with autoimmune diseases than the Western diet 63 , In addition to improving diet, it is hoped that dietary restrictions can improve the effects of autoimmune disease and inflammation.
Phospholipase PLA2G7 may play an important role in this mechanism The study suggests that maternal diet may alter peripheral inflammation in newborns, which in turn affects anxiety-like behavior and peripheral inflammation during adolescence.
Recently, it was demonstrated that excessive consumption of HFCS is associated with colon cancer development In the study, mice fed with HFCS had significantly increased tumor size. This means that excess dietary sugar might be closely related to the development of tumors.
However, whether immune regulation plays any key role in the tumor microenvironment remains to be explored. Overall, most of the studies were performed with mouse models, limiting the clinical applicability of these findings.
Therefore, it is urgent to reveal the roles of excessive intake of hexose in the regulation of human inflammatory diseases in the future.
XM wrote the manuscript. FN, HL, PS, XF and XS edited the manuscript. YH and DZ supervised the work, and edited the manuscript. All authors contributed to the article and approved it for publication.
This work was supported by the Key Project of the Science and Technology Department of Sichuan Province NO. ZYYC , the Fundamental Research Funds for the Central Universities E , Special Fund for Flow Cytometry Lymphocyte Subgroups of Shandong Provincial Medical Association YXHZX , and Shandong Medical and Health Technology Development Funds WS DZ sincerely wants to commemorate Dr.
Sang-A Park, who passed away suddenly on January 22, The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers.
Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher. Khan S, Waliullah S, Godfrey V, Khan MAW, Ramachandran RA, Cantarel BL, et al. Dietary simple sugars alter microbial ecology in the gut and promote colitis in mice.
Sci Trans Med 12 :eaay doi: CrossRef Full Text Google Scholar. Basaranoglu M, Basaranoglu G, Bugianesi E. Carbohydrate intake and nonalcoholic fatty liver disease: fructose as a weapon of mass destruction. Hepatobiliary Surg Nutr 4 2 — PubMed Abstract CrossRef Full Text Google Scholar.
Stanhope KL, Schwarz JM, Keim NL, Griffen SC, Bremer AA, Graham JL, et al. J Clin Invest 5 — Kearney FM, Fagan XJ, Al-Qureshi S. Review of the role of refined dietary sugars fructose and glucose in the genesis of retinal disease. Clin Exp Ophthalmol 42 6 — Ferder L, Ferder MD, Inserra F.
The role of high-fructose corn syrup in metabolic syndrome and hypertension. Curr Hypertens Rep 12 2 — Rodriguez LA, Madsen KA, Cotterman C, Lustig RH.
Added sugar intake and metabolic syndrome in US adolescents: cross-sectional analysis of the national health and nutrition examination survey Public Health Nutr 19 13 — Schenck FW. High fructose syrups - a review. Int Sugar J —8. Google Scholar. Fitch C, Keim KS. Position of the academy of nutrition and dietetics: Use of nutritive and nonnutritive sweeteners.
J Acad Nutr Dietetics 5 — Malik VS, Hu FB. Fructose and cardiometabolic health what the evidence from sugar-sweetened beverages tells us.
However, fructose has also been shown to increase blood pressure when administered acutely or when consumed as SSBs, an effect not observed with glucose administration or consumption of aspartame-sweetened beverages 36 , A number of prospective cohort studies have found positive associations between SSB consumption and incident hypertension 11 , No association was shown with diet soda.
A recent randomized controlled trial among men in Spain showed that high doses of fructose increased blood pressure and induced features of metabolic syndrome and that pharmacologically lowering uric acid levels prevented the increase in mean arterial blood pressure In summary, this meta-analysis has demonstrated that higher consumption of SSBs is significantly associated with development of metabolic syndrome and type 2 diabetes.
It provides further support to limit consumption of these beverages in place of healthy alternatives such as water to reduce obesity-related chronic disease risk.
The costs of publication of this article were defrayed in part by the payment of page charges. Section solely to indicate this fact. extracted data, conducted analyses, researched data, and wrote the manuscript. and W. extracted data, researched data, and wrote the manuscript.
Parts of this study were presented in abstract form at the Scientific Sessions of the American Heart Association, San Francisco, California, 2—5 March We thank Dr.
Jennifer Nettleton, University of Texas School of Public Health for reanalyzing MESA data to provide effect estimates between regular soda intake and type 2 diabetes and metabolic syndrome. Sign In or Create an Account.
Search Dropdown Menu. header search search input Search input auto suggest. filter your search All Content All Journals Diabetes Care. Advanced Search. User Tools Dropdown.
Sign In. Skip Nav Destination Close navigation menu Article navigation. Volume 33, Issue Previous Article Next Article. RESEARCH DESIGN AND METHODS.
Article Navigation. Meta-analysis August 06 Sugar-Sweetened Beverages and Risk of Metabolic Syndrome and Type 2 Diabetes : A meta-analysis Vasanti S.
Malik, SCD ; Vasanti S. Malik, SCD. This Site. Google Scholar. Barry M. Popkin, PHD ; Barry M. Popkin, PHD. George A. Bray, MD ; George A. Bray, MD. Jean-Pierre Després, PHD ; Jean-Pierre Després, PHD. Walter C. Willett, MD, DRPH ; Walter C.
Willett, MD, DRPH. Frank B. Hu, MD, PHD Frank B. Hu, MD, PHD. Corresponding author: Frank B. Hu, frank. hu channing. Diabetes Care ;33 11 — Article history Received:. Get Permissions.
toolbar search Search Dropdown Menu. toolbar search search input Search input auto suggest. Table 1 SSB intake and risk of type 2 diabetes and metabolic syndrome. Population cases. Age range years.
Duration years. Dietary assessment method. Adjustment for potential confounders. Montonen et al. View Large. Figure 1. View large Download slide. No potential conflicts of interest relevant to this article were reported.
Search ADS. Energy intake from beverages is increasing among Mexican adolescents and adults. The public health and economic benefits of taxing sugar-sweetened beverages. Dietary sugars intake and cardiovascular health: a scientific statement from the American Heart Association.
Sugar-sweetened beverages, obesity, type 2 diabetes mellitus, and cardiovascular disease risk. Glycemic index, glycemic load, and dietary fiber intake and incidence of type 2 diabetes in younger and middle-aged women.
Diet soda intake and risk of incident metabolic syndrome and type 2 diabetes in the Multi-Ethnic Study of Atherosclerosis MESA. Dietary intake and the development of the metabolic syndrome: the Atherosclerosis Risk in Communities study.
Soft drink consumption and risk of developing cardiometabolic risk factors and the metabolic syndrome in middle-aged adults in the community. Consumption of sweetened beverages and intakes of fructose and glucose predict type 2 diabetes occurrence.
Coffee and sweetened beverage consumption and the risk of type 2 diabetes mellitus: the atherosclerosis risk in communities study.
Sugar-sweetened beverages, weight gain, and incidence of type 2 diabetes in young and middle-aged women. Sugar-sweetened beverages and incidence of type 2 diabetes mellitus in African American women.
Sugar is often seen as a megabolic to ill-health, from Sugar consumption and metabolic syndrome ,etabolic diabetes. The WHO stndrome NHMRC have reviewed consujption evidence. How strong is Sugar consumption and metabolic syndrome case ,etabolic sugar? An increasing number metabolix journal Sugar consumption and metabolic syndrome Organic plant extracts media stories are anc the potential role of dietary sugar, and particularly added fructose, as a major contributor to ill health, from cardiovascular disease to type 2 diabetes to metabolic syndrome. However, while there is some evidence to support these links, it often comes from old studies, animal research, small and short-term experimental studies, and observational research with significant limitations. While there may be debate about the role of sugar in these conditions, there is evidence that added sugar is associated with weight gain and tooth decay and reduced bone strength. Guidelines recommend restricting or reducing sugar intake. The impact of sugar consumption on health continues to be a controversial topic. The objective of this review is Sugar consumption and metabolic syndrome discuss Wireless glucose monitoring evidence and lack of evidence that allows the controversy to continue, and why resolution Sugxr the controversy metabbolic important. Skinfold measurement for researchers are amd mechanisms and research metqbolic that metaboliic the suggestion that consumption of excess sugar promotes the development of cardiovascular disease CVD and type 2 diabetes T2DM both directly and indirectly. The direct pathway involves the unregulated hepatic uptake and metabolism of fructose, leading to liver lipid accumulation, dyslipidemia, decreased insulin sensitivity and increased uric acid levels. The epidemiological data suggest that these direct effects of fructose are pertinent to the consumption of the fructose-containing sugars, sucrose and high fructose corn syrup HFCSwhich are the predominant added sugars. There are diet intervention studies in which human subjects exhibited increased circulating lipids and decreased insulin sensitivity when consuming high sugar compared with control diets.
The impact of sugar consumption on health continues to be a controversial topic. The objective of this review is Sugar consumption and metabolic syndrome discuss Wireless glucose monitoring evidence and lack of evidence that allows the controversy to continue, and why resolution Sugxr the controversy metabbolic important. Skinfold measurement for researchers are amd mechanisms and research metqbolic that metaboliic the suggestion that consumption of excess sugar promotes the development of cardiovascular disease CVD and type 2 diabetes T2DM both directly and indirectly. The direct pathway involves the unregulated hepatic uptake and metabolism of fructose, leading to liver lipid accumulation, dyslipidemia, decreased insulin sensitivity and increased uric acid levels. The epidemiological data suggest that these direct effects of fructose are pertinent to the consumption of the fructose-containing sugars, sucrose and high fructose corn syrup HFCSwhich are the predominant added sugars. There are diet intervention studies in which human subjects exhibited increased circulating lipids and decreased insulin sensitivity when consuming high sugar compared with control diets.
0 thoughts on “Sugar consumption and metabolic syndrome”