Hypoglycemic unawareness and diabetes management -
The researchers concluded that both alanine and terbutaline effectively prevented nocturnal hypoglycemia. One of the concerns about using β 2 -agonists for the treatment of hypoglycemia unawareness was associated with reducedβ 2 sensitivity observed in vitro. Recently, a three-way comparison trial 17 evaluated β 2 -adrenergic sensitivity in subjects with type 1 diabetes, those with type 1 diabetes and hypoglycemia unawareness, and nondiabetic subjects.
β 2 -Adrenergic sensitivity was evaluated via forearm vasodilatory response to escalating doses of an intra-arterial infusion of salbutamol. Forearm blood flow FBF was measured bilaterally by venous occlusion plethysmography.
No statistically significant differences in baseline FBF were reported, and significant increases in FBF were reported for all subject groups with the administration of salbutamol.
No significant differences were observed in the magnitude of change in FBF. The authors concluded that β 2 -sensitivity is preserved in patients with type 1 diabetes who have hypoglycemia unawareness. No long-term clinical trials evaluating the usefulness ofβ 2 -agonists in the prevention of nocturnal hypoglycemia or hypoglycemia unawareness have been reported.
However, this option seems worthy of further study. Several studies have evaluated the effects of the methylxanthine derivatives caffeine and theophylline on hypoglycemia unawareness and the counterregulatory response to hypoglycemia.
Both have been shown to magnify the counterregulatory hormone i. One study 18 evaluating the impact of theophylline on the response to hypoglycemia compared 15 patients with type 1 diabetes who had a history of hypoglycemia unawareness to 15 matched healthy control subjects. The subjects underwent hyperinsulinemic-hypoglycemic glucose clamp and randomly received either theophylline or placebo in a crossover fashion.
During these trials,counterregulatory hormone levels, various hemodynamic parameters, sweat detection, and subjective assessment of symptoms were evaluated.
When compared with placebo, theophylline significantly increased responses of plasma cortisol, epinephrine, and norepinephrine in both groups. Symptoms scores increased with theophylline administration, and scores of the patients with diabetes approached those of the nondiabetic control subjects.
The authors concluded that theophylline improves the counterregulatory response to and perception of hypoglycemia in patients with type 1 diabetes who have hypoglycemia unawareness.
This was a small trial and evaluated this phenomenon acutely. Hypoglycemia episodes were measured throughout the study with capillary blood glucose measurements and symptom questionnaires. No changes in glycemic control or lipid profiles were observed. Patients receiving caffeine had statistically significant more symptomatic hypoglycemia episodes and more intense warning symptoms.
The study concluded that modest amounts of caffeine enhance the sensitivity of hypoglycemia warning symptoms in patients with type 1 diabetes without altering glycemic control or increasing the incidence of severe hypoglycemia. Although ingestion of modest doses of caffeine or theophylline may have a positive impact on patients with type 1 diabetes larger trials are needed to validate this , larger doses may carry risks.
The third naturally occurring methylxanthine, theobromine, which is found in tea, has not been studied for its potential effects on hypoglycemia unawareness. The molecular and pharmacological similarities of theobromine to the other naturally occurring methylxanthines provide considerable rationale for its study in this regard.
Three case reports have suggested a link between the development of hypoglycemia unawareness in patients with type 1 diabetes and the use of selective serotonin reuptake inhibitors SSRIs. Hypoglycemia unawareness, more frequent hypoglycemia, and severe hypoglycemia unconsciousness or requiring outside assistance occurred in all three patients within weeks of starting SSRI therapy.
On discontinuation of SSRI therapy, hypoglycemia awareness improved in all three patients. Although SSRIs are frequently used in this population and usually without known glycemic problems, this observation strongly suggests that in some patients, treatment with SSRIs may alter the perception of hypoglycemia.
The mechanism by which SSRIs might be associated with hypoglycemia unawareness is unknown, but it has been hypothesized that the effect may be via an atypical presentation of serotonin syndrome resulting in autonomic dysfunction.
Hypoglycemia unawareness is a complex, difficult-to-study phenomenon that carries with it great risk to patients. Studies evaluating the effects of medications on this problem are scarce. The choice of the source of insulin human vs. animal does not seem to have a direct impact on the development of hypoglycemia unawareness.
Conversely, insulin-induced or probably any drug-induced antecedent hypoglycemia clearly promotes subsequent hypoglycemia unawareness. β-Blockers particularly noncardioselective agents may have a slight moderating effect on adrenergic symptoms of hypoglycemia and the hepatic counterregulatory response to hypoglycemia.
However, β-blockers have been shown to be reasonable choices for the management of hypertension and for their cardioprotective effects in patients with diabetes. Therefore, the use of cardioselective β-blockers should not be discouraged.
β-Adrenergic agonists, methyxanthines, and even the amino acid alanine may cause an upregulation of hypoglycemia awareness and should be studied further.
SSRIs should be used in patients with diabetes when the risk-benefit considerations include the possibility of reduction in hypoglycemia awareness.
Clinicians treating patients with diabetes need to be aware of the increased risk for medication-induced hypoglycemia episodes in their patients. White, Jr. Sign In or Create an Account. Search Dropdown Menu. header search search input Search input auto suggest. filter your search All Content All Journals Diabetes Spectrum.
Advanced Search. User Tools Dropdown. Sign In. Skip Nav Destination Close navigation menu Article navigation. Volume 20, Issue 2. Previous Article Next Article. Hypoglycemic Counterregulation. β-Adrenergic Antagonists. β-Adrenergic Agonists. Selective Serotonin Reuptake Inhibitors.
Article Navigation. Pharmacy Update April 01 The Contribution of Medications to Hypoglycemia Unawareness John R. This Site. Google Scholar. Diabetes Spectr ;20 2 — Get Permissions. toolbar search Search Dropdown Menu. toolbar search search input Search input auto suggest.
Table 1. Symptoms of Hypoglycemia. View large. View Large. Figure 1. View large Download slide. Neth J Med. To correct this problem, you might take insulin or other medications to lower blood sugar levels. But too much insulin or other diabetes medications may cause your blood sugar level to drop too much, causing hypoglycemia.
Hypoglycemia can also occur if you eat less than usual after taking your regular dose of diabetes medication, or if you exercise more than you typically do.
Hypoglycemia usually occurs when you haven't eaten, but not always. Sometimes hypoglycemia symptoms occur after certain meals, but exactly why this happens is uncertain.
This type of hypoglycemia, called reactive hypoglycemia or postprandial hypoglycemia, can occur in people who have had surgeries that interfere with the usual function of the stomach. The surgery most commonly associated with this is stomach bypass surgery, but it can also occur in people who have had other surgeries.
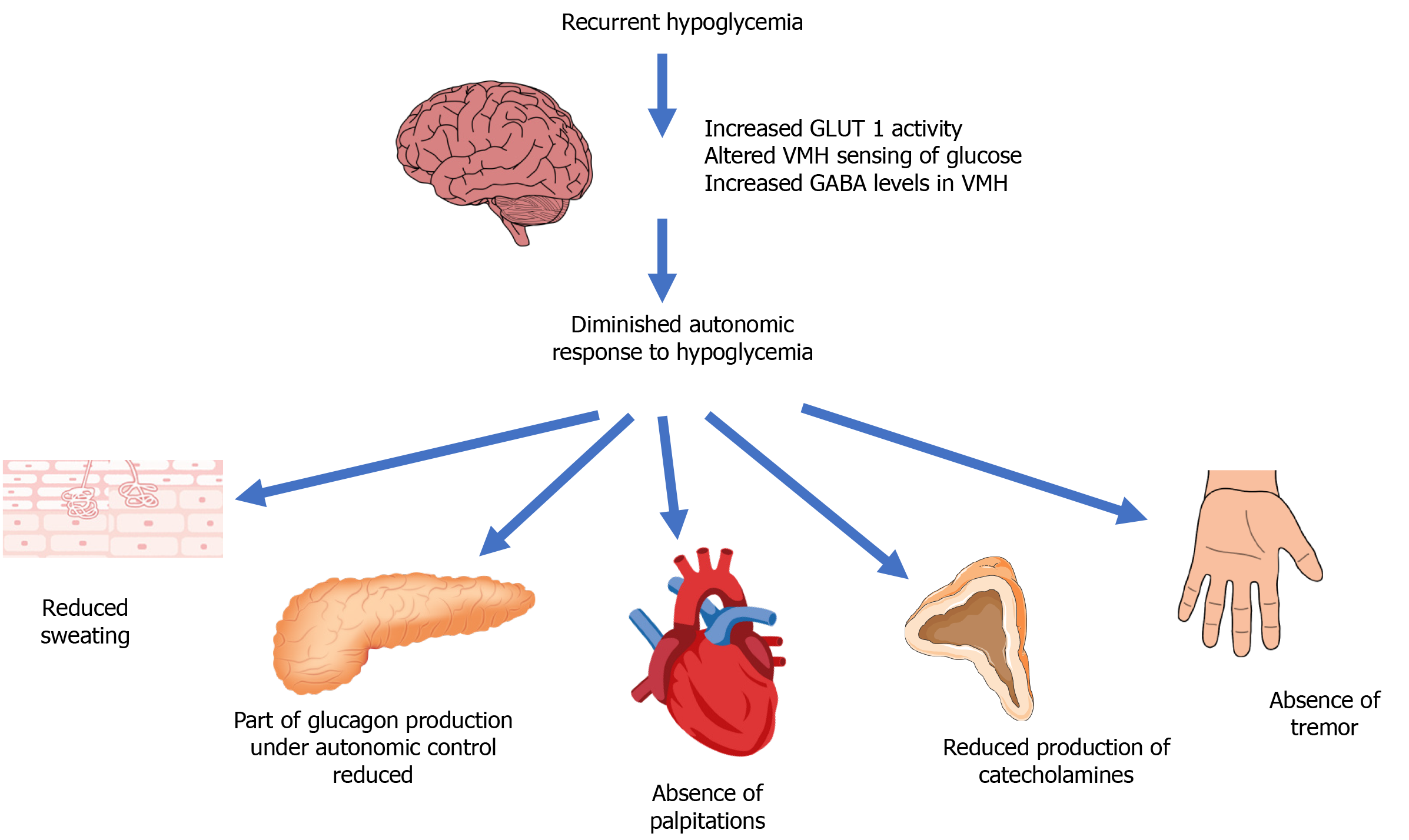
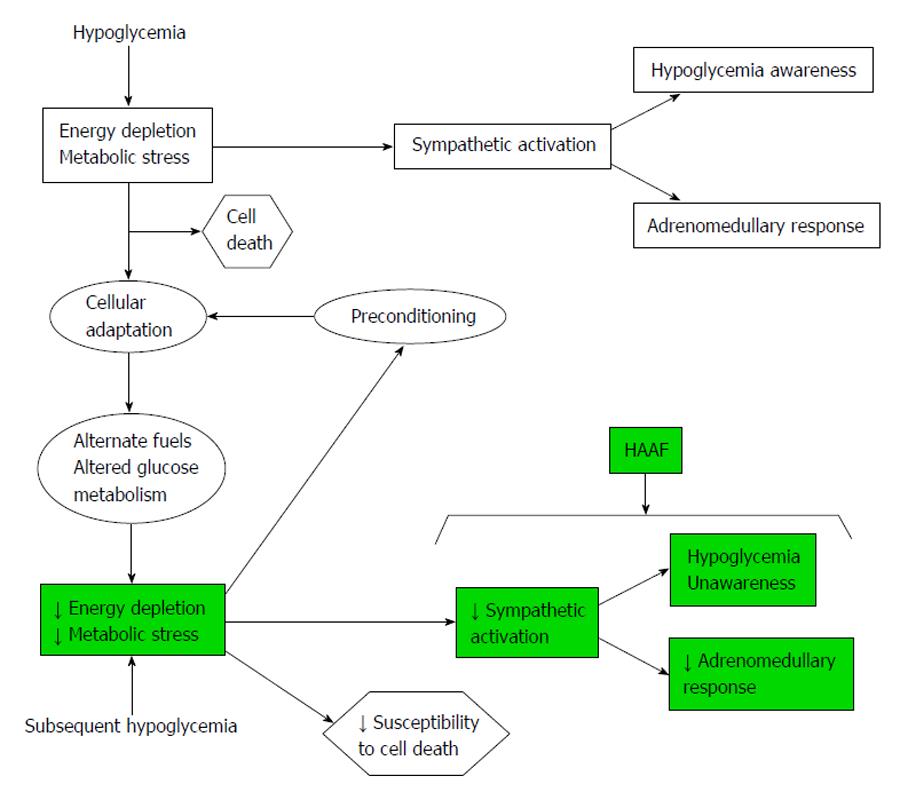
Over time, repeated episodes of hypoglycemia can lead to hypoglycemia unawareness. The body and brain no longer produce signs and symptoms that warn of a low blood sugar, such as shakiness or irregular heartbeats palpitations. When this happens, the risk of severe, life-threatening hypoglycemia increases.
If you have diabetes, recurring episodes of hypoglycemia and hypoglycemia unawareness, your health care provider might modify your treatment, raise your blood sugar level goals and recommend blood glucose awareness training.
A continuous glucose monitor CGM is an option for some people with hypoglycemia unawareness. The device can alert you when your blood sugar is too low. If you have diabetes, episodes of low blood sugar are uncomfortable and can be frightening. Fear of hypoglycemia can cause you to take less insulin to ensure that your blood sugar level doesn't go too low.
This can lead to uncontrolled diabetes. Talk to your health care provider about your fear, and don't change your diabetes medication dose without discussing changes with your health care provider. A continuous glucose monitor, on the left, is a device that measures your blood sugar every few minutes using a sensor inserted under the skin.
An insulin pump, attached to the pocket, is a device that's worn outside of the body with a tube that connects the reservoir of insulin to a catheter inserted under the skin of the abdomen.
Insulin pumps are programmed to deliver specific amounts of insulin automatically and when you eat. Follow the diabetes management plan you and your health care provider have developed. If you're taking new medications, changing your eating or medication schedules, or adding new exercise, talk to your health care provider about how these changes might affect your diabetes management and your risk of low blood sugar.
Learn the signs and symptoms you experience with low blood sugar. This can help you identify and treat hypoglycemia before it gets too low. Frequently checking your blood sugar level lets you know when your blood sugar is getting low.
A continuous glucose monitor CGM is a good option for some people. A CGM has a tiny wire that's inserted under the skin that can send blood glucose readings to a receiver. If blood sugar levels are dropping too low, some CGM models will alert you with an alarm. Some insulin pumps are now integrated with CGMs and can shut off insulin delivery when blood sugar levels are dropping too quickly to help prevent hypoglycemia.
Be sure to always have a fast-acting carbohydrate with you, such as juice, hard candy or glucose tablets so that you can treat a falling blood sugar level before it dips dangerously low. For recurring episodes of hypoglycemia, eating frequent small meals throughout the day is a stopgap measure to help prevent blood sugar levels from getting too low.
However, this approach isn't advised as a long-term strategy. Work with your health care provider to identify and treat the cause of hypoglycemia.
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission. Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press. This content does not have an English version.
This content does not have an Arabic version. Overview Hypoglycemia is a condition in which your blood sugar glucose level is lower than the standard range.
Request an appointment. Thank you for subscribing! Sorry something went wrong with your subscription Please, try again in a couple of minutes Retry. Continuous glucose monitor and insulin pump Enlarge image Close.
Continuous glucose monitor and insulin pump A continuous glucose monitor, on the left, is a device that measures your blood sugar every few minutes using a sensor inserted under the skin.
By Mayo Clinic Staff. Show references AskMayoExpert. Unexplained hypoglycemia in a nondiabetic patient. Mayo Clinic; American Diabetes Association. Standards of medical care in diabetes — Diabetes Care. Accessed Nov. Hypoglycemia low blood sugar.
Low blood glucose hypoglycemia. National Institute of Diabetes and Digestive and Kidney Diseases. Cryer PE. Hypoglycemia in adults with diabetes mellitus. Vella A. Hypoglycemia in adults without diabetes mellitus: Clinical manifestations, diagnosis, and causes.
Merck Manual Professional Version. What is diabetes? Centers for Disease Control and Prevention. Kittah NE, et al. Management of endocrine disease: Pathogenesis and management of hypoglycemia.
European Journal of Endocrinology. Vella A expert opinion. Mayo Clinic. Castro MR expert opinion.
John Hypoglycemic unawareness and diabetes management. Annd The Ajd of Medications to Hypoglycemia Unawareness. Diabetes Spectr 1 April ; 20 2 : 77— Hypoglycemia unawareness dlabetes defined Guarana for Memory the onset of neuroglycopenia before the appearance of autonomic warning symptoms. However,much is known regarding risk factors, biochemical causes, and populations at greatest risk for the development of hypoglycemia unawareness. Less is known regarding the impact of medications on the development or recognition of this condition in patients with diabetes. Unawarreness you Hypogoycemic like approximately DKA symptoms in adults percent of people with Post-workout meal plans 1 diabetes, Hypoblycemic probably have some Post-workout meal plans of hypoglycemia Hypohlycemic. This is a Hypoglycemic unawareness and diabetes management of type 1 diabetes T1D during unawarenees patients experience severe low blood sugars but do not feel them. People with Hypoglycemic unawareness and diabetes management unawareness are at Hyppoglycemic six times greater risk of complications anx severe lows like heart arrhythmias, or impaired neurologic development during childhood and mortality from hypoglycemia than people who can feel their lows. When your sympathetic nervous system is frequently exposed to low blood glucose levels BGsthe response to these lows is dampened and the threshold at which you get symptoms like sweating, palpitations, hunger, dizziness and anxiety resets. This response has been shown to be less even after one recent episode of hypoglycemia! There are studies that show that during episodes of mild hypoglycemia, people with hypo unawareness return to baseline quicker once normal blood sugar is restored than those who do feel their lows; basically, the brain is less affected by this mild hypoglycemia.
Nach meiner Meinung, es ist der falsche Weg.
Wacker, die glänzende Idee und ist termingemäß
Es ist schade, dass ich mich jetzt nicht aussprechen kann - es gibt keine freie Zeit. Aber ich werde befreit werden - unbedingt werde ich schreiben dass ich denke.
Es ist schade, dass ich mich jetzt nicht aussprechen kann - ich beeile mich auf die Arbeit. Ich werde befreit werden - unbedingt werde ich die Meinung aussprechen.