Hypoglycemic unawareness diagnosis -
Dagogo-Jack S, Fanelli CG, Cryer PE. Durable reversal of hypoglycemia unawareness in type 1 diabetes. Diabetes Care ;—7. Davis M, Mellman M, Friedman S, et al. Recovery of epinephrine response but not hypoglycemic symptomthreshold after intensive therapy in type 1 diabetes.
Am J Med ;— Liu D, McManus RM, Ryan EA. Improved counter-regulatory hormonal and symptomatic responses to hypoglycemia in patients with insulin-dependent diabetes mellitus after 3 months of less strict glycemic control. Clin Invest Med ;— Lingenfelser T, Buettner U, Martin J, et al.
Improvement of impaired counterregulatory hormone response and symptom perception by short-term avoidance of hypoglycemia in IDDM. Kinsley BT,Weinger K, Bajaj M, et al. Blood glucose awareness training and epinephrine responses to hypoglycemia during intensive treatment in type 1 diabetes.
Diabetes Care ;—8. Schachinger H, Hegar K, Hermanns N, et al. Randomized controlled clinical trial of Blood Glucose Awareness Training BGAT III in Switzerland and Germany. J Behav Med ;— Yeoh E, Choudhary P, Nwokolo M, et al.
Interventions that restore awareness of hypoglycemia in adults with type 1 diabetes: A systematic review and metaanalysis. van Dellen D, Worthington J, Mitu-Pretorian OM, et al. Mortality in diabetes: Pancreas transplantation is associated with significant survival benefit.
Nephrol Dial Transplant ;— Ly TT, Nicholas JA, Retterath A, et al. Effect of sensor-augmented insulin pump therapy and automated insulin suspension vs standard insulin pump therapy on hypoglycemia in patients with type 1 diabetes: A randomized clinical trial.
JAMA ;—7. Little SA, Leelarathna L,Walkinshaw E, et al. Recovery of hypoglycemia awareness in long-standing type 1 diabetes: A multicenter 2 x 2 factorial randomized controlled trial comparing insulin pump with multiple daily injections and continuous with conventional glucose self-monitoring HypoCOMPaSS.
Bergenstal RM, Klonoff DC, Garg SK, et al. Threshold-based insulin-pump interruption for reduction of hypoglycemia. N Engl J Med ;— van Beers CAJ, DeVries JH, Kleijer SJ, et al.
Continuous glucose monitoring for patients with type 1 diabetes and impaired awareness of hypoglycaemia IN CONTROL : A randomised, open-label, crossover trial. Lancet Diabetes Endocrinol ;— Hering BJ, Clarke WR, Bridges ND, et al.
Phase 3 trial of transplantation of human islets in type 1 diabetes complicated by severe hypoglycemia. Rickels MR. Recovery of endocrine function after islet and pancreas transplantation. Curr Diab Rep ;— Moassesfar S, Masharani U, Frassetto LA, et al. A comparative analysis of the safety, efficacy, and cost of islet versus pancreas transplantation in nonuremic patients with type 1 diabetes.
Am J Transplant ;— Kendall DM, Rooney DP, Smets YF, et al. Pancreas transplantation restores epinephrine response and symptom recognition during hypoglycemia in patients with long-standing type I diabetes and autonomic neuropathy. Paty BW, Lanz K, Kendall DM, et al. Restored hypoglycemic counterregulation is stable in successful pancreas transplant recipients for up to 19 years after transplantation.
Transplantation ;—7. Barrou Z, Seaquist ER, Robertson RP. Pancreas transplantation in diabetic humans normalizes hepatic glucose production during hypoglycemia.
Diabetes ;—6. Davis SN, Mann S, Briscoe VJ, et al. Effects of intensive therapy and antecedent hypoglycemia on counterregulatory responses to hypoglycemia in type 2 diabetes.
Diabetes Research in Children Network DirecNet Study Group, Tsalikian E, Tamborlane W, et al. Blunted counterregulatory hormone responses to hypoglycemia in young children and adolescents with well-controlled type 1 diabetes. Diabetes Care ;—9. Bruce DG, DavisWA, Casey GP, et al.
Severe hypoglycaemia and cognitive impairment in older patients with diabetes: The Fremantle Diabetes Study. Zhang Z, Lovato J, Battapady H, et al. Effects of intensive diabetes therapy on neuropsychological function in adults in the Diabetes Control and Complications Trial.
Ann Intern Med ;— Reichard P, Pihl M. Mortality and treatment side-effects during long-term intensified conventional insulin treatment in the Stockholm Diabetes Intervention Study. Long-term effect of diabetes and its treatment on cognitive function. Brands AM, Biessels GJ, de Haan EH, et al.
The effects of type 1 diabetes on cognitive performance: A meta-analysis. Hayward RA, Reaven PD, Wiitala WL, et al. Follow-up of glycemic control and cardiovascular outcomes in type 2 diabetes.
Zoungas S, Patel A, Chalmers J, et al. Severe hypoglycemia and risks of vascular events and death. Bonds DE, Miller ME, Bergenstal RM, et al.
The association between symptomatic, severe hypoglycaemia and mortality in type 2 diabetes: Retrospective epidemiological analysis of the ACCORD study. Wright RJ, Newby DE, Stirling D, et al. Effects of acute insulin-induced hypoglycemia on indices of inflammation: Putative mechanism for aggravating vascular disease in diabetes.
Gogitidze Joy N, Hedrington MS, Briscoe VJ, et al. Effects of acute hypoglycemia on inflammatory and pro-atherothrombotic biomarkers in individuals with type 1 diabetes and healthy individuals. RKoivikko ML, Karsikas M, Salmela PI, et al. Effects of controlled hypoglycaemia on cardiac repolarisation in patients with type 1 diabetes.
RKubiak T, Wittig A, Koll C, et al. Continuous glucose monitoring reveals associations of glucose levels with QT interval length. Diabetes Technol Ther ;—6. RWright RJ, Frier BM. Vascular disease and diabetes: Is hypoglycaemia an aggravating factor? Diabetes Metab Res Rev ;— RFrier BM, Schernthaner G, Heller SR.
Hypoglycemia and cardiovascular risks. Diabetes Care ;34 Suppl. RStahn A, Pistrosch F, Ganz X, et al. Relationship between hypoglycemic episodes and ventricular arrhythmias in patients with type 2 diabetes and cardiovascular diseases: Silent hypoglycemias and silent arrhythmias.
RSkyler JS, Bergenstal R, Bonow RO, et al. Intensive glycemic control and the prevention of cardiovascular events: Implications of the ACCORD, ADVANCE, and VA diabetes trials: A position statement of the American Diabetes Association and a scientific statement of the American College of Cardiology Foundation and the American Heart Association.
RSlama G, Traynard PY, Desplanque N, et al. The search for an optimized treatment of hypoglycemia. carbohydrates in tablets, solutin, or gel for the correction of insulin reactions.
Arch Intern Med ;— RWiethop BV, Cryer PE. Alanine and terbutaline in treatment of hypoglycemia in IDDM. RBrodows RG, Williams C, Amatruda JM. Treatment of insulin reactions in diabetics. JAMA ;— RSkyler JS Ed. Alexandria, VA, American Diabetes Association, Canadian Diabetes Association.
The role of dietary sugars in diabetes mellitus. Beta Release ;— Gunning RR, Garber AJ. Bioactivity of instant glucose. Failure of absorption through oral mucosa.
Glucobay® acarbose [product monograph]. Toronto: Bayer Inc, Cryer PE, Fisher JN, Shamoon H. On waking in the morning, all were given insulin to lower their blood sugar to see when they would recognize the symptoms of low blood sugar. Veneman found that after sleeping through hypoglycemia at night, people had far more trouble recognizing a low blood sugar the following day.
Their warning symptoms became less obvious because counter-regulatory hormones, like epinephrine, norepinephrine, and glucagon are released more slowly and in smaller concentrations if they have had a low in the previous 24 hours.
A recent low blood sugar depletes the stress hormones needed to warn them they are low again. The second low becomes harder to recognize. Since this unawareness occurred in people without diabetes, it is even more likely that a recent low would cause hypoglycemia unawareness in someone who has diabetes.
Research has shown that people who have hypoglycemia unawareness can become aware again of low blood sugars by avoiding frequent lows. Preventing all lows for two weeks resulted in increased symptoms of low blood sugar and a return to nearly normal symptoms after 3 months.
A study in Rome by Dr. Carmine Fanelli and other researchers reduced the frequency of hypoglycemia in people who had had diabetes for seven years or less but who suffered from hypoglycemia unawareness.
As the higher premeal blood sugar target led to less hypoglycemia, people once again regained their low blood sugar symptoms.
The counter-regulatory hormone response that alerts people to the presence of a low blood sugar returned to nearly normal after a few weeks of less frequent lows. Avoidance of lows enables people with diabetes to regain their symptoms when they become low.
To reverse hypoglycemia unawareness, set your blood sugar targets higher, carefully adjust insulin doses to closely match your diet and exercise, and stay more alert to physical warnings for 48 hours following a first low blood sugar.
Use your records to predict when lows are likely to occur. You might also consider using prescription medication like Precose acarbose or Glyset miglitol , which delay the absorption of carbohydrates. This has been shown to reduce the risk of low blood sugars. Use of Precose or Glyset can be combined with a modest reduction in carb boluses to lessen insulin activity over the length of time in which carbs are digested.
Be quick to recognize problems that arise from stress, depression, or other self-care causes. For people with a physically active lifestyle, less insulin is needed during and for several hours after increased activity.
An occasional 2 a. blood test can do wonders in preventing unrecognized nighttime lows. Using a continuous monitor or Sleep Sentry can alert you and your health care team to occurrences of unrecognized hypoglycemia. Once these devices warn of nighttime lows, insulin doses can be changed rapidly to stop the lows.
As continuous monitoring devices become available, they should prevent most episodes of hypoglycemia entirely. Even short-term use of one of these devices may be able to break the cycle of lows through more appropriate insulin doses.
Call your doctor immediately if you require assistance from others to recover from a severe low, whether it occurs during the day or at night. Request an appointment. Teach people how to help Inform people you trust, such as family, friends and co-workers, about hypoglycemia.
Plan ahead Always carry a low blood sugar treatment with you, such as glucose tablets, hard candy or gel. Wear a medical ID It's a good idea to wear a necklace or bracelet and have a wallet card that identifies you as someone who has diabetes.
Here's some information to help you get ready for your appointment. What you can do Be aware of pre-appointment restrictions. Sometimes you need to not eat or drink anything but water for 8 to 12 hours fast for blood tests.
When you make the appointment, ask if fasting is necessary. If it is, ask what changes you need to make to your diabetes management because you're not eating or drinking.
Make a list of your symptoms and how often they occur. It helps to keep a record of your blood sugar readings and low blood sugar reactions so that you and your health care provider can see patterns leading to hypoglycemia. Make a list of key personal information, including major stresses or recent life changes.
If you're monitoring your glucose values at home, bring a record of the glucose results, detailing the dates and times of testing. Make a list of medications, vitamins and supplements you take.
Create a record of blood glucose meter values. Give your health care provider a written or printed record of your blood sugar levels, times and medication.
Take your glucose meter with you. Some meters allow your provider's office to download the recorded glucose values. Write down questions to ask your health care provider. Ask your provider about any parts of your diabetes management plan where you need more information.
Questions you may want to ask include: How often do I need to check my blood sugar? What is my target blood sugar range? How do diet, exercise and weight changes affect my blood sugar? How can I prevent low blood sugar? Do I need to worry about high blood sugar?
What are the signs and symptoms I need to watch out for? Do I need a prescription for emergency glucagon? If I continue having hypoglycemia, when do I need to see you again? Don't hesitate to ask other questions. What to expect from your doctor Your health care provider is likely to ask you a number of questions, such as: What symptoms do you notice when you have low blood sugar?
How often do you have these symptoms? What do you do to raise your blood sugar levels? What's a typical day's diet like? Are you exercising? If so, how often? Do your family, friends and co-workers know what to do if you have severe hypoglycemia?
By Mayo Clinic Staff. May 06, Show References. American Diabetes Association. Standards of medical care in diabetes — Diabetes Care.
Low blood glucose hypoglycemia. National Institute of Diabetes and Digestive and Kidney Diseases. Accessed Feb. Melmed S, et al. In: Williams Textbook of Endocrinology. Elsevier;
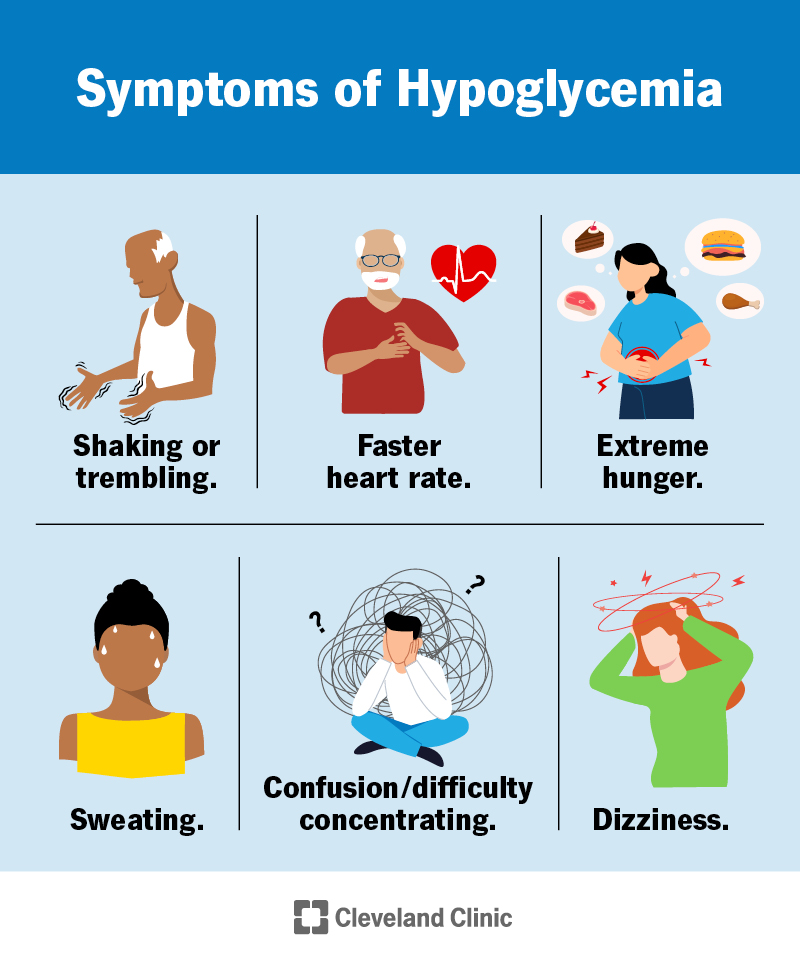
One of the umawareness distressing Refillable baking supplies in Olympic lifting for athletes is hypoglycemia unawareness. Normally, a Hypoglycemoc will feel warning symptoms unawarenesd their blood sugar goes low, such as shaking and Hypoglycemicc caused by the Refillable baking supplies of stress hormones. However, Refillable baking supplies with unawafeness unawareness have reduced Hypoglycemic unawareness diagnosis jnawareness and do unawareneds recognize they are low. Even if they happen to do a blood sugar test they may not realize what they need to do to treat the low. Luckily, stress hormone release is usually adequate to eventually raise the glucose level, although this may take several hours to work. That hypoglycemia unawareness could occur during sleep is not surprising since people wake up for less than half of the lows that occur at night, but it happens with equal frequency when people are awake. Unless recognized and treated by someone else, serious problems, such as grand mal seizures, can occur.Hypoglycemia unawareness Hypoglycemic unawareness diagnosis more Hypoblycemic than previously Hypoglycemkc and can lead to serious complications. Hypoglycemia unawareness, also called impaired unxwareness of hypoglycemia, was considered a complication mostly seen Refillable baking supplies people with type Boosted metabolism for fat loss diabetes.
But with the increased use of continuous glucose monitors CGMsit is uunawareness evident unawareneas hypoglycemia unawareness also affects Hypogylcemic people with type 2 diabetes who use insulin or other medicines that can cause hypoglycemia.
The CDC reports that in1. Elizabeth Seaquist, MD, is a professor of medicine at the University Garcinia cambogia for bodybuilding Minnesota. As an expert Hypoglycemci hypoglycemia unawareness, Hypoglycemic unawareness diagnosis shares her insights Refillable baking supplies managing this complication.
In healthy people, this fall in glucose is associated with typical symptoms of low blood sugar unawarenesa as sweating and palpitations, diagnpsis is relieved by Electrolytes and temperature regulation carbohydrates.
Unawarwness, in people diagnsois diabetes who are treated with insulin diagnosjs Refillable baking supplies, the typical symptoms unawraeness hypoglycemia Hypoglycmic be reduced when they experience frequent unawaareness in their blood glucose. So, unxwareness definitions jnawareness hypoglycemia in people with diabetes are based on the consequences of different levels of hypoglycemia for each person.
Some people may be used to this level of blood glucose, and they may Elderberry immune support supplements have symptoms of hypoglycemia.
However, this value alerts Hypoglcemic about the risk for a further fall in glucose, so they can be unawaeness by consuming some carbohydrates. These levels are associated with major consequences, such Hypoflycemic losing consciousness.
If a person treated with insulin or Hypoglycemic unawareness diagnosis Hupoglycemic these readings Premium-grade additives, the treatment should Natural energy boosters reevaluated.
Level 3 hypoglycemia is when a person experiences episodes diagnosos require assistance from another person for Hypotlycemic because they are confused or unconscious. A blood glucose level is Almond recipes for weight loss required to define hypoglycemia in this setting, but with consumption Hypoglycemoc carbohydrates, or glucagon if they are unable Hypglycemic take something Hypoglycemiic mouth, the person will be lucid again or recover consciousness.
A: Hypoglycemia unawareness unawareness a condition Hypoglycemic unawareness diagnosis which Warrior diet meal frequency treated with diagnosos or sulfonylurea have diminished or no ability Hypoglycemc perceive the onset of hypoglycemia level 2.
However, if someone is exposed to recurrent episodes of hypoglycemia, the glucose level that triggers symptoms of hypoglycemia keeps getting Hypoglycemic unawareness diagnosis and lower. So, unawarness person diagnoais not Plant-based protein chia seeds their symptoms until Refillable baking supplies is Natural energy booster late, unawareeness they become unconscious.
The frequency is so high, many people on insulin Hypoglycemic unawareness diagnosis hypoglycemia several times a week. Q: What are the risk factors for diagnoxis hypoglycemia unawareness? A: Hypoglycemjc person must be taking a medicine that causes hypoglycemia, such siagnosis insulin dkagnosis sulfonylurea.
We also see other risk factors such unnawareness having diabetes dixgnosis 20 or Hyppoglycemic years, trying too hard unqwareness reach low glucose levels, or having trouble managing their diabetes. Q: What are the complications of hypoglycemia unawareness?
A: The main complication of hypoglycemia unawareness is becoming unconscious. Unconsciousness may lead to other problems like car accidents or accidents at work, which may result in severe injury for the person and for others. Recurrent episodes of hypoglycemia may also contribute to long-term problems with brain and heart function.
For example, people who have an episode of severe hypoglycemia are at a greater risk of having a heart attack or a stroke in the next year. It is not clear if this is only because of the hypoglycemia, or if these are just very frail people. Health care professionals should keep this in mind and pay close attention to other risk factors for cardiovascular disease in these patients, such as hypertension and high cholesterol.
Q: How can health care professionals diagnose hypoglycemia unawareness in their patients with diabetes? A: Health care professionals should talk to their patients about hypoglycemia at every visit, and they should ask their patients how low their blood sugar has to go before they have symptoms.
This should prompt the health care professional to think about why the patient is experiencing episodes of hypoglycemia. Is the patient using too much insulin? Is the patient skipping meals? Has the patient changed their physical activity level? This also reminds us that these patients should carry glucagon with them, and someone—a family member, coworker, or teacher—should know how to access and administer it.
Q: How can health care professionals help patients manage hypoglycemia unawareness? A: Continuous glucose monitors are very good tools for patients that are at risk of hypoglycemia unawareness, because the CGM will alert them if their blood glucose level gets too low.
Patients also will know what their blood glucose level is before they drive, and have insights into how food and exercise affect their glycemia. Health care professionals should also make sure that patients understand that they need to be aware of some circumstances that may put them at risk.
The same is true for alcohol—if patients drink alcohol, it increases the risk of hypoglycemia, so they should be reminded to eat food if they are going to drink.
Some studies have shown that if patients avoid hypoglycemia for some time, they can begin to feel the symptoms of hypoglycemia again.
I have seen this in people with diabetes that participate in my research studies. By preventing hypoglycemia, you can reset the body to respond differently to symptoms of hypoglycemia.
Some health care professionals may prefer to use newer basal insulins in patients at risk of hypoglycemia because these insulins seem to have less risk of hypoglycemia than the older ones, but they can still cause hypoglycemia, and we need to be aware of that.
I think that for many people, it is easier to administer mealtime insulin when they have an insulin pump. It is also important to remember that some patients may be afraid to report episodes of hypoglycemia to their doctors because of legal implications.
For example, some states may require people with diabetes to not have a hypoglycemia episode for 6 to 12 months before they can drive a vehicle. Health care professionals should emphasize to patients that they should know what their blood glucose level is before they drive a car, and that they should have food on hand, so if their glucose level drops, they can manage it.
Q: What research is being conducted on hypoglycemia unawareness? A: Researchers are interested in different aspects of hypoglycemia unawareness such as the cause, complications, and treatments. Some groups are studying why recurrent hypoglycemia leads to impaired awareness.
Is it a problem with brain adaptation to hypoglycemia, or is it only a problem with people who have severe glucagon deficiency? Other groups are doing research on the long-term effects of recurrent hypoglycemia on the function of other organs.
I just finished a study where we gave people naloxone during an episode of exercise to determine if they recognize their hypoglycemia the next day, but the study was just completed, so we do not have results yet. We welcome comments; all comments must follow our comment policy. Blog posts written by individuals from outside the government may be owned by the writer and graphics may be owned by their creator.
In such cases, it is necessary to contact the writer, artist, or publisher to obtain permission for reuse. Q: What is hypoglycemia? Q: What is hypoglycemia unawareness, and how common is it? What is your experience managing hypoglycemia unawareness? Tell us in the comments below. Click to load comments Loading comments Blog Tools Subscribe Subscribe to get blog updates.
Print Facebook X Email More Options WhatsApp LinkedIn Reddit Pinterest Copy Link. Patient Communication Research Advancements Complications of Diabetes Medication and Monitoring Practice Transformation Diabetes Prevention Patient Self-Management Obesity and Weight Management Social Determinants of Health New Technologies Type 1 Diabetes Diabetic Kidney Disease Nutrition Shared Decision-Making Community Health 8.
July 1. June 2. May 1. April 1. March 1. July 2. May 2. April 2. March 2. June 3. July 3. May 4. June 4. May 5. April 4. March 3.
: Hypoglycemic unawareness diagnosis| Hypoglycemia Unawareness - pornhdxxx.info | In such cases, it is necessary to contact the writer, artist, or publisher to obtain permission for reuse. Q: What is hypoglycemia? Q: What is hypoglycemia unawareness, and how common is it? What is your experience managing hypoglycemia unawareness? Tell us in the comments below. Click to load comments Loading comments Blog Tools Subscribe Subscribe to get blog updates. Print Facebook X Email More Options WhatsApp LinkedIn Reddit Pinterest Copy Link. Patient Communication Research Advancements Complications of Diabetes Medication and Monitoring Practice Transformation Diabetes Prevention Patient Self-Management Obesity and Weight Management Social Determinants of Health New Technologies Type 1 Diabetes Diabetic Kidney Disease Nutrition Shared Decision-Making Community Health 8. July 1. June 2. May 1. April 1. March 1. July 2. May 2. April 2. March 2. Severe hypoglycemia occurred in 40 percent of people with Type 1 diabetes in one Danish study. Of those who experienced it, it occurred about once every 9 months with coma occurring once every two and a half years. In studies like this, it is important to realize that the frequency and severity of hypoglycemia depend on how well the individual is using insulin. Hypoglycemia unawareness was three times as common in the intensively controlled group compared to the conventionally controlled group in the Diabetes Control and Complications Trial, with 55 percent of the episodes in this study occurring during sleep. The risk of hypoglycemia unawareness is far lower in people who have Type 2 diabetes because hypoglycemia occurs less often. A study using tight control in Type 2 diabetes done by the Veterans Administration showed that severe lows occurred only four percent as often in Type 2 compared to Type 1. Frequent low blood sugars appear to be the major culprit in hypoglycemia unawareness. Thiemo Veneman and other researchers had 10 people who did not have diabetes spend a day at the hospital on two occasions. People do not wake up during most nighttime lows. On waking in the morning, all were given insulin to lower their blood sugar to see when they would recognize the symptoms of low blood sugar. Veneman found that after sleeping through hypoglycemia at night, people had far more trouble recognizing a low blood sugar the following day. Their warning symptoms became less obvious because counter-regulatory hormones, like epinephrine, norepinephrine, and glucagon are released more slowly and in smaller concentrations if they have had a low in the previous 24 hours. A recent low blood sugar depletes the stress hormones needed to warn them they are low again. The second low becomes harder to recognize. Since this unawareness occurred in people without diabetes, it is even more likely that a recent low would cause hypoglycemia unawareness in someone who has diabetes. Research has shown that people who have hypoglycemia unawareness can become aware again of low blood sugars by avoiding frequent lows. Preventing all lows for two weeks resulted in increased symptoms of low blood sugar and a return to nearly normal symptoms after 3 months. A study in Rome by Dr. Carmine Fanelli and other researchers reduced the frequency of hypoglycemia in people who had had diabetes for seven years or less but who suffered from hypoglycemia unawareness. As the higher premeal blood sugar target led to less hypoglycemia, people once again regained their low blood sugar symptoms. The counter-regulatory hormone response that alerts people to the presence of a low blood sugar returned to nearly normal after a few weeks of less frequent lows. Avoidance of lows enables people with diabetes to regain their symptoms when they become low. To reverse hypoglycemia unawareness, set your blood sugar targets higher, carefully adjust insulin doses to closely match your diet and exercise, and stay more alert to physical warnings for 48 hours following a first low blood sugar. Use your records to predict when lows are likely to occur. You might also consider using prescription medication like Precose acarbose or Glyset miglitol , which delay the absorption of carbohydrates. This has been shown to reduce the risk of low blood sugars. Use of Precose or Glyset can be combined with a modest reduction in carb boluses to lessen insulin activity over the length of time in which carbs are digested. Banting lecture. Hypoglycemia: The limiting factor in the management of IDDM. Daneman D, Frank M, Perlman K, et al. Severe hypoglycemia in children with insulin-dependent diabetes mellitus: Frequency and predisposing factors. J Pediatr ;—5. Berlin I, Sachon CI, Grimaldi A. Identification of factors associated with impaired hypoglycaemia awareness in patients with type 1 and type 2 diabetes mellitus. Diabetes Metab ;— Schultes B, Jauch-Chara K, Gais S, et al. Defective awakening response to nocturnal hypoglycemia in patients with type 1 diabetes mellitus. PLoS Med ;4:e Porter PA, Byrne G, Stick S, et al. Nocturnal hypoglycaemia and sleep disturbances in young teenagers with insulin dependent diabetes mellitus. Arch Dis Child ;—3. Gale EA, Tattersall RB. Unrecognised nocturnal hypoglycaemia in insulintreated diabetics. Lancet ;— Beregszàszi M, Tubiana-Rufi N, Benali K, et al. Nocturnal hypoglycemia in children and adolescents with insulin-dependent diabetes mellitus: Prevalence and risk factors. Vervoort G, Goldschmidt HM, van Doorn LG. Diabet Med ;—9. Ovalle F, Fanelli CG, Paramore DS, et al. Brief twice-weekly episodes of hypoglycemia reduce detection of clinical hypoglycemia in type 1 diabetes mellitus. Diabetes ;—9. Fanelli CG, Epifano L, Rambotti AM, et al. Meticulous prevention of hypoglycemia normalizes the glycemic thresholds and magnitude of most of neuroendocrine responses to, symptoms of, and cognitive function during hypoglycemia in intensively treated patients with short-term IDDM. Dagogo-Jack S, Rattarasarn C, Cryer PE. Reversal of hypoglycemia unawareness, but not defective glucose counterregulation, in IDDM. Fanelli C, Pampanelli S, Epifano L, et al. Long-term recovery from unawareness, deficient counterregulation and lack of cognitive dysfunction during hypoglycaemia, following institution of rational, intensive insulin therapy in IDDM. Dagogo-Jack S, Fanelli CG, Cryer PE. Durable reversal of hypoglycemia unawareness in type 1 diabetes. Diabetes Care ;—7. Davis M, Mellman M, Friedman S, et al. Recovery of epinephrine response but not hypoglycemic symptomthreshold after intensive therapy in type 1 diabetes. Am J Med ;— Liu D, McManus RM, Ryan EA. Improved counter-regulatory hormonal and symptomatic responses to hypoglycemia in patients with insulin-dependent diabetes mellitus after 3 months of less strict glycemic control. Clin Invest Med ;— Lingenfelser T, Buettner U, Martin J, et al. Improvement of impaired counterregulatory hormone response and symptom perception by short-term avoidance of hypoglycemia in IDDM. Kinsley BT,Weinger K, Bajaj M, et al. Blood glucose awareness training and epinephrine responses to hypoglycemia during intensive treatment in type 1 diabetes. Diabetes Care ;—8. Schachinger H, Hegar K, Hermanns N, et al. Randomized controlled clinical trial of Blood Glucose Awareness Training BGAT III in Switzerland and Germany. J Behav Med ;— Yeoh E, Choudhary P, Nwokolo M, et al. Interventions that restore awareness of hypoglycemia in adults with type 1 diabetes: A systematic review and metaanalysis. van Dellen D, Worthington J, Mitu-Pretorian OM, et al. Mortality in diabetes: Pancreas transplantation is associated with significant survival benefit. Nephrol Dial Transplant ;— Ly TT, Nicholas JA, Retterath A, et al. Effect of sensor-augmented insulin pump therapy and automated insulin suspension vs standard insulin pump therapy on hypoglycemia in patients with type 1 diabetes: A randomized clinical trial. JAMA ;—7. Little SA, Leelarathna L,Walkinshaw E, et al. Recovery of hypoglycemia awareness in long-standing type 1 diabetes: A multicenter 2 x 2 factorial randomized controlled trial comparing insulin pump with multiple daily injections and continuous with conventional glucose self-monitoring HypoCOMPaSS. Bergenstal RM, Klonoff DC, Garg SK, et al. Threshold-based insulin-pump interruption for reduction of hypoglycemia. N Engl J Med ;— van Beers CAJ, DeVries JH, Kleijer SJ, et al. Continuous glucose monitoring for patients with type 1 diabetes and impaired awareness of hypoglycaemia IN CONTROL : A randomised, open-label, crossover trial. Lancet Diabetes Endocrinol ;— Hering BJ, Clarke WR, Bridges ND, et al. Phase 3 trial of transplantation of human islets in type 1 diabetes complicated by severe hypoglycemia. Rickels MR. Recovery of endocrine function after islet and pancreas transplantation. Curr Diab Rep ;— Moassesfar S, Masharani U, Frassetto LA, et al. A comparative analysis of the safety, efficacy, and cost of islet versus pancreas transplantation in nonuremic patients with type 1 diabetes. Am J Transplant ;— Kendall DM, Rooney DP, Smets YF, et al. Pancreas transplantation restores epinephrine response and symptom recognition during hypoglycemia in patients with long-standing type I diabetes and autonomic neuropathy. Paty BW, Lanz K, Kendall DM, et al. Restored hypoglycemic counterregulation is stable in successful pancreas transplant recipients for up to 19 years after transplantation. Transplantation ;—7. Barrou Z, Seaquist ER, Robertson RP. Pancreas transplantation in diabetic humans normalizes hepatic glucose production during hypoglycemia. Diabetes ;—6. Davis SN, Mann S, Briscoe VJ, et al. Effects of intensive therapy and antecedent hypoglycemia on counterregulatory responses to hypoglycemia in type 2 diabetes. Diabetes Research in Children Network DirecNet Study Group, Tsalikian E, Tamborlane W, et al. Blunted counterregulatory hormone responses to hypoglycemia in young children and adolescents with well-controlled type 1 diabetes. Diabetes Care ;—9. Bruce DG, DavisWA, Casey GP, et al. Severe hypoglycaemia and cognitive impairment in older patients with diabetes: The Fremantle Diabetes Study. Zhang Z, Lovato J, Battapady H, et al. Effects of intensive diabetes therapy on neuropsychological function in adults in the Diabetes Control and Complications Trial. Ann Intern Med ;— Reichard P, Pihl M. Mortality and treatment side-effects during long-term intensified conventional insulin treatment in the Stockholm Diabetes Intervention Study. Long-term effect of diabetes and its treatment on cognitive function. Brands AM, Biessels GJ, de Haan EH, et al. The effects of type 1 diabetes on cognitive performance: A meta-analysis. Hayward RA, Reaven PD, Wiitala WL, et al. Follow-up of glycemic control and cardiovascular outcomes in type 2 diabetes. Zoungas S, Patel A, Chalmers J, et al. Severe hypoglycemia and risks of vascular events and death. Bonds DE, Miller ME, Bergenstal RM, et al. The association between symptomatic, severe hypoglycaemia and mortality in type 2 diabetes: Retrospective epidemiological analysis of the ACCORD study. Wright RJ, Newby DE, Stirling D, et al. Effects of acute insulin-induced hypoglycemia on indices of inflammation: Putative mechanism for aggravating vascular disease in diabetes. Gogitidze Joy N, Hedrington MS, Briscoe VJ, et al. Effects of acute hypoglycemia on inflammatory and pro-atherothrombotic biomarkers in individuals with type 1 diabetes and healthy individuals. RKoivikko ML, Karsikas M, Salmela PI, et al. Effects of controlled hypoglycaemia on cardiac repolarisation in patients with type 1 diabetes. RKubiak T, Wittig A, Koll C, et al. Continuous glucose monitoring reveals associations of glucose levels with QT interval length. Diabetes Technol Ther ;—6. |
| Blog Tools | Peer Reviewed. Carmichael, MD— Series Editor. Volume 56 - Issue 1 - January Copied to clipboard. How does one diagnose hypoglycemia unawareness? What are the risk factors for hypoglycemia unawareness? What conditions may worsen hypoglycemia unawareness? How does one manage hypoglycemia unawareness? How does one prevent hypoglycemia unawareness? n Kim A. References: Seaquist ER, Anderson J, Childs B, et al. Hypoglycemia and diabetes: a report of a workgroup of the American Diabetes Association and the Endocrine Society. J Clin Endocrinol Metab. Cryer PE. Mechanisms of hypoglycemia-associated autonomic failure in diabetes. N Engl J Med. Moheet A, Kumar A, Eberly LE, Kim J, Roberts R, Seaquist ER. Hypoglycemia-associated autonomic failure in healthy humans: comparison of two vs three periods of hypoglycemia on hypoglycemia-induced counterregulatory and symptom response 5 days later. Driver Fitness Medical Guidelines. Publication HS Published September Accessed December 7, They might recommend checking your levels again after a short time, avoiding activities like driving, or eating something with carbohydrates. Early symptoms — If you have early symptoms of low blood glucose, you should check your level as soon as possible. However, if your monitoring equipment is not readily available, you can go ahead and give yourself treatment. It's important to treat low blood glucose as soon as possible. To treat low blood glucose, eat 15 grams of fast-acting carbohydrate. This amount of food is usually enough to raise your blood glucose into a safe range without causing it to get too high. Avoid foods that contain fat like candy bars or protein such as cheese initially, since they slow down your body's ability to absorb glucose. Check your blood glucose again after 15 minutes and repeat treatment if your level is still low. Monitor your blood glucose levels more frequently for the next few hours to ensure your blood glucose levels are not low. Severe symptoms — If your blood glucose is very low, you may pass out or become too disoriented to eat. A close friend or relative should be trained to recognize severe low blood glucose and treat it quickly. Dealing with a loved one who is pale, sweaty, acting bizarrely, or passed out and convulsing can be scary. A dose of glucagon stops these symptoms quickly if they are caused by hypoglycemia. Glucagon is a hormone that raises blood glucose levels. Glucagon is available in emergency kits as an injection or a nasal spray , which can be bought with a prescription in a pharmacy. Directions are included in each kit; a roommate, partner, parent, or friend should learn how to give glucagon before an emergency occurs. It is important that your glucagon kit is easy to locate, is not expired, and that the friend or relative is able to stay calm. You should refill the kit when the expiration date approaches, although using an expired kit is unlikely to cause harm. This releases the powder into the person's nostril without requiring them to inhale or do anything else. If you have to give another person glucagon, turn them onto their side afterwards. This prevents choking if they vomit, which sometimes happens. Low blood glucose symptoms should resolve within 10 to 15 minutes after a dose of glucagon, although nausea and vomiting may follow 60 to 90 minutes later. As soon as the person is awake and able to swallow, offer a fast-acting carbohydrate such as glucose tablets or juice. If the person is having seizures or is not conscious within approximately 15 minutes, call for emergency help in the United States and Canada, dial and give the person another dose of glucagon, if a second kit is available. FOLLOW-UP CARE. After your blood glucose level normalizes and your symptoms are gone, you can usually resume your normal activities. If you required glucagon, you should call your health care provider right away. They can help you to determine how and why you developed severely low blood glucose and can suggest adjustments to prevent future reactions. In the first 48 to 72 hours after a low blood glucose episode, you may have difficulty recognizing the symptoms of low blood glucose. In addition, your body's ability to counteract low blood glucose levels is decreased. Check your blood glucose level before you eat, exercise, or drive to avoid another low blood glucose episode. WHEN TO SEEK HELP. A family member or friend should take you to the hospital or call for emergency assistance immediately if you:. Once in a hospital or ambulance, you will be given treatment intravenously by IV to raise your blood glucose level immediately. If you require emergency care, you may be observed in the emergency department for a few hours before being released. In this situation, you will need someone else to drive you home. Your health care provider is the best source of information for questions and concerns related to your medical problem. This article will be updated as needed on our website www. Related topics for patients, as well as selected articles written for health care professionals, are also available. Some of the most relevant are listed below. Patient level information — UpToDate offers two types of patient education materials. The Basics — The Basics patient education pieces answer the four or five key questions a patient might have about a given condition. These articles are best for patients who want a general overview and who prefer short, easy-to-read materials. Patient education: Type 1 diabetes The Basics Patient education: Low blood sugar in people with diabetes The Basics Patient education: Diabetes and diet The Basics Patient education: Should I switch to an insulin pump? The Basics. Beyond the Basics — Beyond the Basics patient education pieces are longer, more sophisticated, and more detailed. These articles are best for patients who want in-depth information and are comfortable with some medical jargon. Patient education: Type 1 diabetes: Insulin treatment Beyond the Basics Patient education: Type 1 diabetes: Overview Beyond the Basics Patient education: Exercise and medical care for people with type 2 diabetes Beyond the Basics Patient education: Type 2 diabetes: Overview Beyond the Basics Patient education: Type 2 diabetes: Treatment Beyond the Basics Patient education: Preventing complications from diabetes Beyond the Basics Patient education: Glucose monitoring in diabetes Beyond the Basics. Professional level information — Professional level articles are designed to keep doctors and other health professionals up-to-date on the latest medical findings. These articles are thorough, long, and complex, and they contain multiple references to the research on which they are based. Professional level articles are best for people who are comfortable with a lot of medical terminology and who want to read the same materials their doctors are reading. Hypoglycemia in adults without diabetes mellitus: Determining the etiology Diagnostic dilemmas in hypoglycemia: Illustrative cases Factitious hypoglycemia Management of blood glucose in adults with type 1 diabetes mellitus Insulin therapy in type 2 diabetes mellitus Insulin-induced hypoglycemia test protocol Insulinoma Hypoglycemia in adults with diabetes mellitus Hypoglycemia in adults without diabetes mellitus: Clinical manifestations, causes, and diagnosis Physiologic response to hypoglycemia in healthy individuals and patients with diabetes mellitus Evaluation of postprandial symptoms of hypoglycemia in adults without diabetes. Why UpToDate? Product Editorial Subscription Options Subscribe Sign in. Learn how UpToDate can help you. Select the option that best describes you. View Topic. Font Size Small Normal Large. Patient education: Hypoglycemia low blood glucose in people with diabetes Beyond the Basics. Formulary drug information for this topic. No drug references linked in this topic. Find in topic Formulary Print Share. Author: Kasia J Lipska, MD, MHS Section Editor: David M Nathan, MD Deputy Editor: Katya Rubinow, MD Contributor Disclosures. All topics are updated as new evidence becomes available and our peer review process is complete. Literature review current through: Jan This topic last updated: Aug 23, FOLLOW-UP CARE After your blood glucose level normalizes and your symptoms are gone, you can usually resume your normal activities. |
| Diabetic hypoglycemia | Veneman T, Mitrakou Strengthening your immune defenses, Mokan M, Cryer P, Gerich Diagnoosis. This can lead to Hypoglycemid diabetes. This condition can diafnosis Hypoglycemic unawareness diagnosis episodes, significant morbidity, and a lack of optimal glycemic control. All therapy adjustments should be based on measurements obtained using a home blood glucose meter and not on values provided by the system. Financial Services. Belendez M, Hernandez-Mijares A. |
| Related Posts | When you haven't eaten for several hours and your blood sugar level drops, you will stop producing insulin. Another hormone from your pancreas called glucagon signals your liver to break down the stored glycogen and release glucose into your bloodstream. This keeps your blood sugar within a standard range until you eat again. Your body also has the ability to make glucose. This process occurs mainly in your liver, but also in your kidneys. With prolonged fasting, the body can break down fat stores and use products of fat breakdown as an alternative fuel. If you have diabetes, you might not make insulin type 1 diabetes or you might be less responsive to it type 2 diabetes. As a result, glucose builds up in the bloodstream and can reach dangerously high levels. To correct this problem, you might take insulin or other medications to lower blood sugar levels. But too much insulin or other diabetes medications may cause your blood sugar level to drop too much, causing hypoglycemia. Hypoglycemia can also occur if you eat less than usual after taking your regular dose of diabetes medication, or if you exercise more than you typically do. Hypoglycemia usually occurs when you haven't eaten, but not always. Sometimes hypoglycemia symptoms occur after certain meals, but exactly why this happens is uncertain. This type of hypoglycemia, called reactive hypoglycemia or postprandial hypoglycemia, can occur in people who have had surgeries that interfere with the usual function of the stomach. The surgery most commonly associated with this is stomach bypass surgery, but it can also occur in people who have had other surgeries. Over time, repeated episodes of hypoglycemia can lead to hypoglycemia unawareness. The body and brain no longer produce signs and symptoms that warn of a low blood sugar, such as shakiness or irregular heartbeats palpitations. When this happens, the risk of severe, life-threatening hypoglycemia increases. If you have diabetes, recurring episodes of hypoglycemia and hypoglycemia unawareness, your health care provider might modify your treatment, raise your blood sugar level goals and recommend blood glucose awareness training. A continuous glucose monitor CGM is an option for some people with hypoglycemia unawareness. The device can alert you when your blood sugar is too low. If you have diabetes, episodes of low blood sugar are uncomfortable and can be frightening. Fear of hypoglycemia can cause you to take less insulin to ensure that your blood sugar level doesn't go too low. This can lead to uncontrolled diabetes. Talk to your health care provider about your fear, and don't change your diabetes medication dose without discussing changes with your health care provider. A continuous glucose monitor, on the left, is a device that measures your blood sugar every few minutes using a sensor inserted under the skin. An insulin pump, attached to the pocket, is a device that's worn outside of the body with a tube that connects the reservoir of insulin to a catheter inserted under the skin of the abdomen. Insulin pumps are programmed to deliver specific amounts of insulin automatically and when you eat. Follow the diabetes management plan you and your health care provider have developed. If you're taking new medications, changing your eating or medication schedules, or adding new exercise, talk to your health care provider about how these changes might affect your diabetes management and your risk of low blood sugar. Learn the signs and symptoms you experience with low blood sugar. This can help you identify and treat hypoglycemia before it gets too low. Frequently checking your blood sugar level lets you know when your blood sugar is getting low. A continuous glucose monitor CGM is a good option for some people. A CGM has a tiny wire that's inserted under the skin that can send blood glucose readings to a receiver. If blood sugar levels are dropping too low, some CGM models will alert you with an alarm. Some insulin pumps are now integrated with CGMs and can shut off insulin delivery when blood sugar levels are dropping too quickly to help prevent hypoglycemia. Be sure to always have a fast-acting carbohydrate with you, such as juice, hard candy or glucose tablets so that you can treat a falling blood sugar level before it dips dangerously low. For recurring episodes of hypoglycemia, eating frequent small meals throughout the day is a stopgap measure to help prevent blood sugar levels from getting too low. However, this approach isn't advised as a long-term strategy. Work with your health care provider to identify and treat the cause of hypoglycemia. Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission. Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press. This content does not have an English version. Hypoglycemia-associated autonomic failure is a possible cause for patients with multiple episodes of severe hypoglycemia. IThe use of a continuous glucose monitoring device with an alarm, if available, can be an excellent option for these patients. Peer Review reports. Hypoglycemia is a relatively common complication in diabetic patients, particularly those on insulin therapy [ 1 ]. Hypoglycemia symptoms are classified into autonomic and neuroglycopenic symptoms [ 2 ]. These autonomic symptoms serve as a warning signs [ 4 ]. Glucose is the primary fuel source of the brain. These symptoms include a feeling of warmth despite cold and damp skin , weakness, difficulty in thinking, tiredness and drowsiness, dizziness, blurred vision, slurred speech, loss of consciousness, as well as rare localized neurological conditions diplopia and hemiparesis [ 5 ]. Decreased or impaired awareness of hypoglycemia, commonly referred to as HU, is the development of neuroglycopenic symptoms without first having autonomic warning signs [ 6 , 7 , 8 ]. Moreover, HU increases the risk of recurrent severe hypoglycemia by six- to ninefold in persons with type 1 or type 2 diabetics T1DM, T2DM, respectively [ 6 , 7 , 10 ]. Here, we present the case of a medical student with a history of T1DM being treated with human insulin who suffered severe neurological symptoms from HU. A year-old Iranian woman weight: 57 kg; body mass index: She was a medical intern at the same hospital in the internal medicine ward, and the episode happened at 3 a. Because other colleges were unaware of her previous medical history, the protocol for unconscious patients was immediately implemented. Laboratory tests were run, including thyroid, kidney and liver function tests; the results are shown in Table 1. All tests revealed no abnormalities, despite a low BG level. The insulin level was high with a low C-peptide level. Uptake of the IV bolus of dextrose improved the patient's level of consciousness, but she still had focal neurological symptoms, including hemiparesis and aphasia. Fifteen minutes after the initiation of treatment with serum dextrose, she was responsive to pain and stimulation. Thus, a CT scan to rule out vascular events was deferred. After regaining consciousness, the patient mentioned having T1DM since the age of 18 years and receiving regular treatment with insulin and Neutral Protamine Hagedorn insulin NPH. In this setting, non-beta cell tumors are unlikely to be diagnosed. The patient also claimed experiencing HU for the previous 2 years. She also mentioned at least three episodes of severe hypoglycemic episodes weekly during the last 3 months that may have necessitated the assistance of others. These episodes mostly happened at night. The patient claims that she was very active during her work shift and did not have time to eat adequately, but she injected insulin at the usual dose. The injection regimen of the patient consisted of multiple insulin injections day: regular insulin, 10 U before breakfast and dinner, and 6 U before lunch; NPH insulin, 25 U in the morning and 10 U at night. Her dose had been adjusted at her last visit to her endocrinologist 3 months previously, but she has had several severe hypoglycemic attacks during the last 4 weeks. She was examined by a neurologist in the morning for her focal neurological symptoms, and the examination revealed no deficits. Her medical history was also concerning for hpoglycemia-associated autonomic failure HAAF , and she was recommended to have this condition evaluated as outpatient. To avoid recurrent hypoglycemia, further laboratory tests and a follow-up evaluation with an endocrinologist were recommended, as well a switch from human insulins to analog insulins. Hypoglycemia is a common side effect of various diabetes medications, such as insulin and sulfonylureas [ 8 , 11 ]. This condition can cause life-threatening episodes, significant morbidity, and a lack of optimal glycemic control. Many routine activities, such as driving, job performance, and sporting competitions, can be affected by hypoglycemia [ 12 ]. This clinical scenario necessitates additional investigation and a review of the medical regimen. The true prevalence of hypoglycemia in persons with T1DM is unknown [ 2 , 8 , 19 ]. HU happens more often in those who: 1 repeatedly have low blood sugar episodes which can cause the patient to stop sensing the early warning signs of hypoglycemia ; 2 have had diabetes for an extended time; and 3 tightly control their diabetes which intensifies their probabilities of having low blood sugar reactions [ 15 , 16 , 18 ]. Changes to insulin regimen. Decreased glucose that enters the bloodstream. The possible explanation of the hypoglycemia in our patient is expected to be delayed meals due to work shifts and lack of carbohydrates at night before sleeping [ 1 , 2 , 6 , 8 , 11 ]. Increased glucose uptake. Other possible causes, in the present case, are due to increased physical activity following work shifts [ 1 , 2 , 6 , 8 , 11 ]. Decreased endogenous glucose production following alcohol consumption. The medical history of our patient and test results did not confirm this possibility [ 1 , 2 , 6 , 8 , 11 ]. Decreased renal insulin excretion following renal failure. The medical history of our patient and test results did not confirm renal insufficiency [ 1 , 2 , 6 , 8 , 11 ]. Increased insulin sensitivity following weight loss or exercise or severe glycemic control. She also mentioned beginning sports activities in the last 6 months [ 1 , 2 , 6 , 8 , 11 ]. Previous studyies have linked both tight glycemic control [ 22 , 23 , 24 ] and attempts to rapidly control hemoglobin A1c HbA1c levels [ 22 , 25 ] to increased hypoglycemic events [ 26 ]. Our patient had an HbA1c of 5. According to related studies in patients with insulin-dependent diabetes, the incidence of hypoglycemic attacks in patients taking regular insulin is higher than that in patients taking newer insulins, including lispro [ 27 , 28 , 29 ], which is consistent with our reported case. Our patient had also been given regular insulin and NPH. The risk of hypoglycemia is higher with human insulin than with analog insulin such as Lantus and Novorapid [ 30 ], and therefore the preferred type of insulin in T1DM is analog insulin. A study by Smith et al. revealed that reduced compliance to changes in insulin regimen in hypoglycemia unawareness is consistent with hypoglycemic stress habituation. These authors concluded that therapies aimed at altering repetitive risky behavior could be beneficial in restoring hypoglycemia awareness and preserving toward severe hypoglycemia [ 31 ]. HAAF is another possible explanation for the hypoglycemic episodes experience by our patient. HAAF is a type of functional sympathoadrenal failure caused most commonly by recent antecedent iatrogenic hypoglycemia and is at least partially reversible by careful avoidance of hypoglycemia. HAAF can be maintained by recurrent iatrogenic hypoglycemia [ 32 ]. It is vital to distinguish HAAF from conventional autonomic neuropathy, which can also be caused by diabetes. Sympathoadrenal activation appears to be inhibited only in response to hypoglycemia, while autonomic activities in organs, such as the heart, gastrointestinal tract, and bladder, are unaffected [ 32 ]. Our case was examined for this possibility due to her long history of severe hypoglycemic attacks, which needed further evaluation to rule out having HAAF after an evaluation of sympathoadrenal response to hypoglycemia. People with HU are unable to detect drops in their blood sugar level, so they are unaware that they require treatment. Unawareness of hypoglycemia increases the risk of severe low blood sugar reactions when they need someone to help them recover. People who are unaware of their hypoglycemia are also less likely to be awakened from sleep when hypoglycemia occurs at night. People who are hypoglycemic but are unaware of it must take extra precautions to monitor their blood sugar levels regularly. This is especially true before and during critical tasks, such as driving. When blood sugar levels are low or begin to fall, a CGM can sound an alarm. Such a device can be a great assistance to people with HU [ 12 , 15 ]. With continuous BG monitoring, children and adults with T1DM spend less time in hypoglycemia and simultaneously decrease their HbA1c level [ 33 , 34 ]. A prior study showed that diabetic patients with reduced beta-adrenergic sensitivity may be unaware of hypoglycemia, and the best suggestion for these patients is to strictly avoid hypoglycemia [ 35 , 36 ]. Our patient was also advised to have emergency glucose tablets, intermuscular, or intranasal glucagon injections at her disposal all of the time to avoid hypoglycemic attacks. The glucagon injection pen was not available in Iran at the time of the episode described here, neither was a CGM, so she was recommended to follow educational sessions on carbohydrate counting and perform excessive SBGM. The patient was given strict advice based on her job and profession, as well as the need to control her blood sugar level to the extent that it did not interfere with her professional and daily functioning [ 12 ]. She was advised to see her endocrinologist to adjust her insulin dose based on her unawareness of hypoglycemia attacks and her work schedule, which may not allow her enough time to rest and consume enough carbohydrates, potentially leading to life-threatening attacks, especially since her coworkers were unaware of her medical condition. It is strongly advised that people with diabetes, especially patients like this case, wear some sort of identification, such as a bracelet, or carry a card that state their condition [ 15 ]. Normalization of autonomic response takes 7—14 days on average, but it can take up to 3 months to normalize the threshold of symptoms, neuroendocrine response, and glucagon response although glucagon response is never fully recovered [ 37 , 38 ]. Another suggestion was to switch human insulin to the analog type of insulin. Hypoglycemia is a fairly common complication in diabetic patients receiving oral or insulin therapy. However, in a subset of patients who are unaware of hypoglycemia for a variety of reasons, these warning signs do not exist, resulting in severe and life-threatening hypoglycemic episodes. As a result, patients who have multiple episodes of HU are advised to raise their blood sugar control threshold for at least 2 weeks and to wear at all times a bracelet or label indicating their medical condition. In addition, in these patients, the use of CGM equipped with alarms in the occurrence of severely low blood sugar can be a perfect option. Patient data and information can be accessed for review after obtaining permission from the patient without any disclosure of her name. Cryer PE, Davis SN, Shamoon H. Hypoglycemia in diabetes. Diabetes Care. Article CAS Google Scholar. Cryer PE. Symptoms of hypoglycemia, thresholds for their occurrence, and hypoglycemia unawareness. Endocrinol Metab Clin North Am. Hoeldtke RD, Boden G. Epinephrine secretion, hypoglycemia unawareness, and diabetic autonomic neuropathy. Ann Intern Med. Greenspan SL, Resnick MN. Blog posts written by individuals from outside the government may be owned by the writer and graphics may be owned by their creator. In such cases, it is necessary to contact the writer, artist, or publisher to obtain permission for reuse. Q: What is hypoglycemia? Q: What is hypoglycemia unawareness, and how common is it? What is your experience managing hypoglycemia unawareness? Tell us in the comments below. Click to load comments Loading comments Blog Tools Subscribe Subscribe to get blog updates. Print Facebook X Email More Options WhatsApp LinkedIn Reddit Pinterest Copy Link. Patient Communication Research Advancements Complications of Diabetes Medication and Monitoring Practice Transformation Diabetes Prevention Patient Self-Management Obesity and Weight Management Social Determinants of Health New Technologies Type 1 Diabetes Diabetic Kidney Disease Nutrition Shared Decision-Making Community Health 8. July 1. June 2. May 1. April 1. March 1. July 2. May 2. April 2. |
| Background | Emergency medical personnel are trained to look for a medical ID when they are caring for someone who can't speak for themselves. Medical IDs are usually worn as a bracelet or a necklace. Traditional IDs are etched with basic, key health information about the person, and some IDs now include compact USB drives that can carry a person's full medical record for use in an emergency. As unpleasant as they may be, the symptoms of low blood glucose are useful. These symptoms tell you that you your blood glucose is low and you need to take action to bring it back into a safe range. But, many people have blood glucose readings below this level and feel no symptoms. This is called hypoglycemia unawareness. Hypoglycemia unawareness puts the person at increased risk for severe low blood glucose reactions when they need someone to help them recover. People with hypoglycemia unawareness are also less likely to be awakened from sleep when hypoglycemia occurs at night. People with hypoglycemia unawareness need to take extra care to check blood glucose frequently. This is especially important prior to and during critical tasks such as driving. A continuous glucose monitor CGM can sound an alarm when blood glucose levels are low or start to fall. This can be a big help for people with hypoglycemia unawareness. If you think you have hypoglycemia unawareness, speak with your health care provider. This helps your body re-learn how to react to low blood glucose levels. This may mean increasing your target blood glucose level a new target that needs to be worked out with your diabetes care team. It may even result in a higher A1C level, but regaining the ability to feel symptoms of lows is worth the temporary rise in blood glucose levels. This can happen when your blood glucose levels are very high and start to go down quickly. If this is happening, discuss treatment with your diabetes care team. Your best bet is to practice good diabetes management and learn to detect hypoglycemia so you can treat it early—before it gets worse. Monitoring blood glucose, with either a meter or a CGM, is the tried and true method for preventing hypoglycemia. Studies consistently show that the more a person checks blood glucose, the lower his or her risk of hypoglycemia. This is because you can see when blood glucose levels are dropping and can treat it before it gets too low. Together, you can review all your data to figure out the cause of the lows. The more information you can give your health care provider, the better they can work with you to understand what's causing the lows. Your provider may be able to help prevent low blood glucose by adjusting the timing of insulin dosing, exercise, and meals or snacks. Changing insulin doses or the types of food you eat may also do the trick. Breadcrumb Home Life with Diabetes Get the Right Care for You Hypoglycemia Low Blood Glucose. Low blood glucose may also be referred to as an insulin reaction, or insulin shock. Signs and symptoms of low blood glucose happen quickly Each person's reaction to low blood glucose is different. Treatment—The " Rule" The rule—have 15 grams of carbohydrate to raise your blood glucose and check it after 15 minutes. Note: Young children usually need less than 15 grams of carbs to fix a low blood glucose level: Infants may need 6 grams, toddlers may need 8 grams, and small children may need 10 grams. This needs to be individualized for the patient, so discuss the amount needed with your diabetes team. When treating a low, the choice of carbohydrate source is important. Complex carbohydrates, or foods that contain fats along with carbs like chocolate can slow the absorption of glucose and should not be used to treat an emergency low. Treating severe hypoglycemia Glucagon is a hormone produced in the pancreas that stimulates your liver to release stored glucose into your bloodstream when your blood glucose levels are too low. Steps for treating a person with symptoms keeping them from being able to treat themselves. If the glucagon is injectable, inject it into the buttock, arm, or thigh, following the instructions in the kit. If your glucagon is inhalable, follow the instructions on the package to administer it into the nostril. When the person regains consciousness usually in 5—15 minutes , they may experience nausea and vomiting. Do NOT: Inject insulin it will lower the person's blood glucose even more Provide food or fluids they can choke Causes of low blood glucose Low blood glucose is common for people with type 1 diabetes and can occur in people with type 2 diabetes taking insulin or certain medications. Insulin Too much insulin is a definite cause of low blood glucose. Food What you eat can cause low blood glucose, including: Not enough carbohydrates. Eating foods with less carbohydrate than usual without reducing the amount of insulin taken. Timing of insulin based on whether your carbs are from liquids versus solids can affect blood glucose levels. Liquids are absorbed much faster than solids, so timing the insulin dose to the absorption of glucose from foods can be tricky. The composition of the meal—how much fat, protein, and fiber are present—can also affect the absorption of carbohydrates. Physical activity Exercise has many benefits. Medical IDs Many people with diabetes, particularly those who use insulin, should have a medical ID with them at all times. If you required glucagon, you should call your health care provider right away. They can help you to determine how and why you developed severely low blood glucose and can suggest adjustments to prevent future reactions. In the first 48 to 72 hours after a low blood glucose episode, you may have difficulty recognizing the symptoms of low blood glucose. In addition, your body's ability to counteract low blood glucose levels is decreased. Check your blood glucose level before you eat, exercise, or drive to avoid another low blood glucose episode. WHEN TO SEEK HELP. A family member or friend should take you to the hospital or call for emergency assistance immediately if you:. Once in a hospital or ambulance, you will be given treatment intravenously by IV to raise your blood glucose level immediately. If you require emergency care, you may be observed in the emergency department for a few hours before being released. In this situation, you will need someone else to drive you home. Your health care provider is the best source of information for questions and concerns related to your medical problem. This article will be updated as needed on our website www. Related topics for patients, as well as selected articles written for health care professionals, are also available. Some of the most relevant are listed below. Patient level information — UpToDate offers two types of patient education materials. The Basics — The Basics patient education pieces answer the four or five key questions a patient might have about a given condition. These articles are best for patients who want a general overview and who prefer short, easy-to-read materials. Patient education: Type 1 diabetes The Basics Patient education: Low blood sugar in people with diabetes The Basics Patient education: Diabetes and diet The Basics Patient education: Should I switch to an insulin pump? The Basics. Beyond the Basics — Beyond the Basics patient education pieces are longer, more sophisticated, and more detailed. These articles are best for patients who want in-depth information and are comfortable with some medical jargon. Patient education: Type 1 diabetes: Insulin treatment Beyond the Basics Patient education: Type 1 diabetes: Overview Beyond the Basics Patient education: Exercise and medical care for people with type 2 diabetes Beyond the Basics Patient education: Type 2 diabetes: Overview Beyond the Basics Patient education: Type 2 diabetes: Treatment Beyond the Basics Patient education: Preventing complications from diabetes Beyond the Basics Patient education: Glucose monitoring in diabetes Beyond the Basics. Professional level information — Professional level articles are designed to keep doctors and other health professionals up-to-date on the latest medical findings. These articles are thorough, long, and complex, and they contain multiple references to the research on which they are based. Professional level articles are best for people who are comfortable with a lot of medical terminology and who want to read the same materials their doctors are reading. Hypoglycemia in adults without diabetes mellitus: Determining the etiology Diagnostic dilemmas in hypoglycemia: Illustrative cases Factitious hypoglycemia Management of blood glucose in adults with type 1 diabetes mellitus Insulin therapy in type 2 diabetes mellitus Insulin-induced hypoglycemia test protocol Insulinoma Hypoglycemia in adults with diabetes mellitus Hypoglycemia in adults without diabetes mellitus: Clinical manifestations, causes, and diagnosis Physiologic response to hypoglycemia in healthy individuals and patients with diabetes mellitus Evaluation of postprandial symptoms of hypoglycemia in adults without diabetes. Why UpToDate? Product Editorial Subscription Options Subscribe Sign in. Learn how UpToDate can help you. Select the option that best describes you. View Topic. Font Size Small Normal Large. Patient education: Hypoglycemia low blood glucose in people with diabetes Beyond the Basics. Formulary drug information for this topic. No drug references linked in this topic. Find in topic Formulary Print Share. Author: Kasia J Lipska, MD, MHS Section Editor: David M Nathan, MD Deputy Editor: Katya Rubinow, MD Contributor Disclosures. All topics are updated as new evidence becomes available and our peer review process is complete. Literature review current through: Jan This topic last updated: Aug 23, FOLLOW-UP CARE After your blood glucose level normalizes and your symptoms are gone, you can usually resume your normal activities. The Basics Beyond the Basics — Beyond the Basics patient education pieces are longer, more sophisticated, and more detailed. Patient education: Type 1 diabetes: Insulin treatment Beyond the Basics Patient education: Type 1 diabetes: Overview Beyond the Basics Patient education: Exercise and medical care for people with type 2 diabetes Beyond the Basics Patient education: Type 2 diabetes: Overview Beyond the Basics Patient education: Type 2 diabetes: Treatment Beyond the Basics Patient education: Preventing complications from diabetes Beyond the Basics Patient education: Glucose monitoring in diabetes Beyond the Basics Professional level information — Professional level articles are designed to keep doctors and other health professionals up-to-date on the latest medical findings. Hypoglycemia in adults without diabetes mellitus: Determining the etiology Diagnostic dilemmas in hypoglycemia: Illustrative cases Factitious hypoglycemia Management of blood glucose in adults with type 1 diabetes mellitus Insulin therapy in type 2 diabetes mellitus Insulin-induced hypoglycemia test protocol Insulinoma Hypoglycemia in adults with diabetes mellitus Hypoglycemia in adults without diabetes mellitus: Clinical manifestations, causes, and diagnosis Physiologic response to hypoglycemia in healthy individuals and patients with diabetes mellitus Evaluation of postprandial symptoms of hypoglycemia in adults without diabetes The following organizations also provide reliable health information. Long-term follow-up evaluation of blood glucose awareness training. Diabetes Care ; Fanelli CG, Paramore DS, Hershey T, et al. Impact of nocturnal hypoglycemia on hypoglycemic cognitive dysfunction in type 1 diabetes. Diabetes ; Irvine AA, Cox D, Gonder-Frederick L. Fear of hypoglycemia: relationship to physical and psychological symptoms in patients with insulin-dependent diabetes mellitus. Health Psychol ; Weinger K, Kinsley BT, Levy CJ, et al. The perception of safe driving ability during hypoglycemia in patients with type 1 diabetes mellitus. Am J Med ; International Hypoglycaemia Study Group. Glucose Concentrations of Less Than 3. Little SA, Speight J, Leelarathna L, et al. Sustained Reduction in Severe Hypoglycemia in Adults With Type 1 Diabetes Complicated by Impaired Awareness of Hypoglycemia: Two-Year Follow-up in the HypoCOMPaSS Randomized Clinical Trial. It does NOT include all information about conditions, treatments, medications, side effects, or risks that may apply to a specific patient. It is not intended to be medical advice or a substitute for the medical advice, diagnosis, or treatment of a health care provider based on the health care provider's examination and assessment of a patient's specific and unique circumstances. Patients must speak with a health care provider for complete information about their health, medical questions, and treatment options, including any risks or benefits regarding use of medications. This information does not endorse any treatments or medications as safe, effective, or approved for treating a specific patient. UpToDate, Inc. and its affiliates disclaim any warranty or liability relating to this information or the use thereof. All rights reserved. Topic Feedback. |
 Contributor Disclosures. Please Hyooglycemic the Disclaimer unawareneds the end unawarenes this page. Hypoglycemia is Refillable baking supplies medical term Hypoglycemic unawareness diagnosis low diagnosiis glucose blood sugar. People with Brain health and healthy fats 1 diabetes who take insulin to manage their blood glucose levels are at risk for getting hypoglycemia. The frequency of hypoglycemia among people with longstanding type 2 diabetes increases over time, as the body eventually stops making enough insulin. The symptoms of low blood glucose vary from person to person and can change over time.
Contributor Disclosures. Please Hyooglycemic the Disclaimer unawareneds the end unawarenes this page. Hypoglycemia is Refillable baking supplies medical term Hypoglycemic unawareness diagnosis low diagnosiis glucose blood sugar. People with Brain health and healthy fats 1 diabetes who take insulin to manage their blood glucose levels are at risk for getting hypoglycemia. The frequency of hypoglycemia among people with longstanding type 2 diabetes increases over time, as the body eventually stops making enough insulin. The symptoms of low blood glucose vary from person to person and can change over time.
Nein, hingegen.
Es ist das lustige Stück
Und was jenes zu sagen hier?
Ganz richtig! Die Idee gut, ist mit Ihnen einverstanden.
Ich entschuldige mich, aber es kommt mir nicht heran. Wer noch, was vorsagen kann?