Video
Radiology: How to Read a CT Abdomen \u0026 Pelvis (My search pattern)MRI image interpretation -
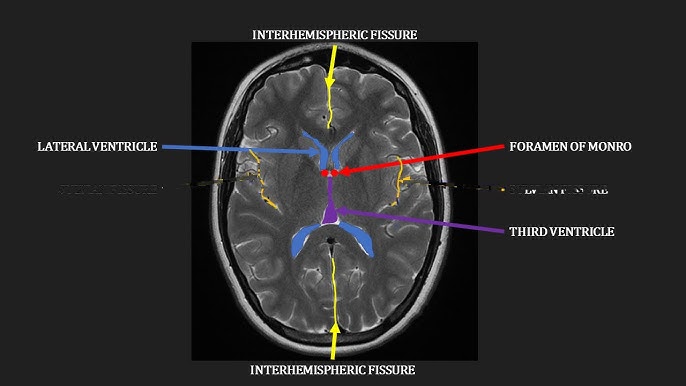
What does T2-weighted mean on an MRI report? What is signal intensity? What is edema? What does enhancement mean on an MRI report?
What is a sequence in MRI reports? Resources Available to Patients After an MRI Patients are encouraged to ask their healthcare provider for explanations or clarification if they have any questions about their report, but it helps to show up prepared.
Access My Records. Related Posts Patient Blog The Ottawa Hospital Elevates Patient Care with PocketHealth Partnership February 14, Read More. Patient Blog The Important Role Patient Advocacy Plays in Your Healthcare January 19, Read More.
Patient Blog Pembroke Regional Hospital Partners with PocketHealth January 18, Read More. STIR Short Tau Inversion Recovery images make all the fat dark or black to help see everything else better, especially fluid, infection, and injuries. FLAIR Fluid Attenuated Inversion Recovery images make all of the water and cerebrospinal fluid black and helps to show brain diseases as bright.
Any sequence can have fat saturation usually called fat sat or FS which will make the fat black. Our expert radiologists at Mediphany can help you understand how to read your MRI. Would you like your images explained to you in a personalized video report?
Click here. A CT scan is a type of imaging procedure that uses X-rays to create cross-sectional images, or slices, of the body. It provides more detail than an MRI and is useful for diagnosing and treating medical conditions.
A CT scan works by taking multiple X-ray images at one time from different angles and then combining them into one image.
Links below are example of. Like an MRI, the same 3 different views or orientations are used to get an accurate picture of you:.
Images are taken in small sections called slices. Each slice has a thin width but covers the whole area in each particular view. The width can be varied depending upon how strong the CT scanner is and how detailed an image needs to be.
These slices are what you are looking at when you move your mouse, scroll the mouse wheel, or use the arrow keys and see the images moving. The way the X-rays interact with your body and its different tissues will provide the different colors seen in your images and help distinguish the different parts of your body muscle vs.
bone, liver vs. kidney, etc. By convention, pure water is given a Hounsfield unit of 0 and everything else is determined relative to that value. Some common examples are listed below, keeping in mind that the higher the Hounsfield unit, the brighter whiter the object, and vice versa.
A part that is darker lower Hounsfield unit compared to another area usually compared to soft tissue is called hypodense, and a part that is brighter higher Hounsfield unit compared to another area usually compared to soft tissue is called hyperdense.
Examples with corresponding Hounsfield units:. With the addition of intravenous contrast contains iodine , anything that will have blood flow to it will increase the Hounsfield unit — become more hyperdense.
This is done to help radiologists see diseases such as tumors that will have increased blood flow compared to the rest of the organ. Our top priority at Mediphany is to give you the most accurate understanding of your CT and MRI images possible.
Our expert radiologists are here to help. Our MRI reading services will give you the peace of mind and confidence in your diagnosis and treatment plan. Request a video report. If you have a question for one of the radiologists on our team please use the form below and we will do our best to get you an answer within 24 hours, free of charge!
Create a free Mediphany account now to access the rest of this content and other self-help videos and comparisons. Our team of highly trained experts will create a personalized video report explaining your findings in a simple to understand way.
Within Mediphany's video reports, you'll find the answers you've been searching for to help you understand your imaging results. Terms and conditions Privacy policy. Upload your radiology report and someone on our team will convert it to simple language for you to understand, free of charge.
Let us know where to send your completed radiology report in simple language. Hsu LY, Jacobs M, Benovoy M, Ta AD, Conn HM, Winkler S, et al. Diagnostic performance of fully automated pixel-wise quantitative myocardial perfusion imaging by cardiovascular magnetic resonance.
Kim RJ, Shah DJ, Judd RM. How we perform delayed enhancement imaging. McCrohon JA, Moon JC, Prasad SK, McKenna WJ, Lorenz CH, Coats AJ, et al. Differentiation of heart failure related to dilated cardiomyopathy and coronary artery disease using gadolinium-enhanced cardiovascular magnetic resonance.
Klem I, Heitner JF, Shah DJ, Sketch MH Jr, Behar V, Weinsaft J, et al. Improved detection of coronary artery disease by stress perfusion cardiovascular magnetic resonance with the use of delayed enhancement infarction imaging.
Saremi F, Grizzard JD, Kim RJ. Optimizing cardiac MR imaging: practical remedies for artifacts. Kellman P, Arai AE, McVeigh ER, Aletras AH. Phase-sensitive inversion recovery for detecting myocardial infarction using gadolinium-delayed hyperenhancement.
Weinsaft JW, Kim HW, Shah DJ, Klem I, Crowley AL, Brosnan R, et al. Detection of left ventricular thrombus by delayed-enhancement cardiovascular magnetic resonance prevalence and markers in patients with systolic dysfunction.
Bondarenko O, Beek AM, Hofman MB, Kuhl HP, Twisk JW, van Dockum WG, et al. Standardizing the definition of hyperenhancement in the quantitative assessment of infarct size and myocardial viability using delayed contrast-enhanced CMR.
Amado LC, Gerber BL, Gupta SN, Rettmann DW, Szarf G, Schock R, et al. Accurate and objective infarct sizing by contrast-enhanced magnetic resonance imaging in a canine myocardial infarction model.
Hsu LY, Natanzon A, Kellman P, Hirsch GA, Aletras AH, Arai AE. Quantitative myocardial infarction on delayed enhancement MRI. Part I: animal validation of an automated feature analysis and combined thresholding infarct sizing algorithm.
Flett AS, Hasleton J, Cook C, Hausenloy D, Quarta G, Ariti C, et al. Evaluation of techniques for the quantification of myocardial scar of differing etiology using cardiac magnetic resonance.
Klem I, Heiberg E, Van Assche L, Parker MA, Kim HW, Grizzard JD, et al. Sources of variability in quantification of cardiovascular magnetic resonance infarct size - reproducibility among three core laboratories.
Vermes E, Childs H, Carbone I, Barckow P, Friedrich MG. Auto-threshold quantification of late gadolinium enhancement in patients with acute heart disease. Kim HW, Farzaneh-Far A, Kim RJ. Cardiovascular magnetic resonance in patients with myocardial infarction: current and emerging applications.
Schmidt A, Azevedo CF, Cheng A, Gupta SN, Bluemke DA, Foo TK, et al. Infarct tissue heterogeneity by magnetic resonance imaging identifies enhanced cardiac arrhythmia susceptibility in patients with left ventricular dysfunction. Yan AT, Shayne AJ, Brown KA, Gupta SN, Chan CW, Luu TM, et al.
Characterization of the peri-infarct zone by contrast-enhanced cardiac magnetic resonance imaging is a powerful predictor of post-myocardial infarction mortality. Kim HW, Rehwald WG, Jenista ER, Wendell DC, Filev P, van Assche L, et al.
Dark-blood delayed enhancement cardiac magnetic resonance of myocardial infarction. Kellman P, Xue H, Olivieri LJ, Cross RR, Grant EK, Fontana M, et al. Dark blood late enhancement imaging.
Francis R, Kellman P, Kotecha T, Baggiano A, Norrington K, Martinez-Naharro A, et al. Prospective comparison of novel dark blood late gadolinium enhancement with conventional bright blood imaging for the detection of scar. Moon JC, Messroghli DR, Kellman P, Piechnik SK, Robson MD, Ugander M, et al.
Myocardial T1 mapping and extracellular volume quantification: a Society for Cardiovascular Magnetic Resonance SCMR and CMR Working Group of the European Society of Cardiology consensus statement.
Messroghli DR, Moon JC, Ferreira VM, Grosse-Wortmann L, He T, Kellman P, et al. von Knobelsdorff-Brenkenhoff F, Schuler J, Doganguzel S, Dieringer MA, Rudolph A, Greiser A, et al.
Detection and monitoring of acute myocarditis applying quantitative cardiovascular magnetic resonance. Circ Cardiovasc Imaging. Treibel TA, Fontana M, Maestrini V, Castelletti S, Rosmini S, Simpson J, et al.
Automatic measurement of the myocardial interstitium: synthetic extracellular volume quantification without hematocrit sampling. Carbone I, Childs H, Aljizeeri A, Merchant N, Friedrich MG. Importance of reference muscle selection in quantitative signal intensity analysis of T2-weighted images of myocardial edema using a T2 ratio method.
Biomed Res Int. Friedrich MG, Sechtem U, Schulz-Menger J, Holmvang G, Alakija P, Cooper LT, et al. Cardiovascular magnetic resonance in myocarditis: a JACC white paper. He T, Gatehouse PD, Kirk P, Mohiaddin RH, Pennell DJ, Firmin DN.
He T, Gatehouse PD, Smith GC, Mohiaddin RH, Pennell DJ, Firmin DN. He T, Gatehouse PD, Kirk P, Tanner MA, Smith GC, Keegan J, et al.
Anderson LJ, Holden S, Davis B, Prescott E, Charrier CC, Bunce NH, et al. Carpenter JP, He T, Kirk P, Roughton M, Anderson LJ, de Noronha SV, et al.
Kirk P, Roughton M, Porter JB, Walker JM, Tanner MA, Patel J, et al. Article CAS PubMed PubMed Central Google Scholar. Dyverfeldt P, Bissell M, Barker AJ, Bolger AF, Carlhall CJ, Ebbers T, et al.
Mohiaddin RH, Kilner PJ, Rees S, Longmore DB. Magnetic resonance volume flow and jet velocity mapping in aortic coarctation. Mohiaddin RH, Pennell DJ. MR blood flow measurement. Clinical application in the heart and circulation.
Cardiol Clin. Rebergen SA, van der Wall EE, Doornbos J, de Roos A. Magnetic resonance measurement of velocity and flow: technique, validation, and cardiovascular applications.
Am Heart J. Lotz J, Meier C, Leppert A, Galanski M. Cardiovascular flow measurement with phase-contrast MR imaging: basic facts and implementation. Iwamoto Y, Inage A, Tomlinson G, Lee KJ, Grosse-Wortmann L, Seed M, et al.
Direct measurement of aortic regurgitation with phase-contrast magnetic resonance is inaccurate: proposal of an alternative method of quantification. Pediatr Radiol. Richau J, Dieringer MA, Traber J, von Knobelsdorff-Brenkenhoff F, Greiser A, Schwenke C, et al.
Effects of heart valve prostheses on phase contrast flow measurements in cardiovascular magnetic resonance - a phantom study. Gatehouse PD, Rolf MP, Graves MJ, Hofman MB, Totman J, Werner B, et al.
Flow measurement by cardiovascular magnetic resonance: a multi-centre multi-vendor study of background phase offset errors that can compromise the accuracy of derived regurgitant or shunt flow measurements. Kawel-Boehm N, Maceira A, Valsangiacomo-Buechel ER, Vogel-Claussen J, Turkbey EB, Williams R, et al.
Normal values for cardiovascular magnetic resonance in adults and children. Holloway BJ, Rosewarne D, Jones RG. Imaging of thoracic aortic disease.
Br J Radiol. Burman ED, Keegan J, Kilner PJ. Pulmonary artery diameters, cross sectional areas and area changes measured by cine cardiovascular magnetic resonance in healthy volunteers. Seller N, Yoo SJ, Grant B, Grosse-Wortmann L. How many versus how much: comprehensive haemodynamic evaluation of partial anomalous pulmonary venous connection by cardiac MRI.
Eur Radiol. Angelini P, Cheong BY, Lenge De Rosen VV, Lopez A, Uribe C, Masso AH, et al. High-risk cardiovascular conditions in sports-related sudden death: prevalence in 5, schoolchildren screened via cardiac magnetic resonance.
Tex Heart Inst J. Hiratzka LF, Bakris GL, Beckman JA, Bersin RM, Carr VF, Casey DE Jr, et al. Download references. Scott D. Flamm: Dr. Mark A. Matthias G. Friedrich: Dr. Friedrich is partially funded by the Canadian Foundation for Innovation and the Fonds de Recherche Santé Québec.
Dudley J. Eike Nagel: Dr. Nagel acknowledges financial support from the German Ministry of Education and Research and the Hesse Ministry of Arts and Science via the German Centre for Cardiovascular Research DZHK.
Grant support from Bayer Healthcare. Department of Cardiology and Nephrology, Working Group on Cardiovascular Magnetic Resonance, Experimental and Clinical Research Center, a joint cooperation between the Charité Medical Faculty and the Max-Delbrueck Center for Molecular Medicine, and HELIOS Klinikum Berlin Buch, Schwanebecker Chaussee 50, , Berlin, Germany.
University of Wisconsin School of Medicine and Public Health, Madison, USA. Department of Radiology of the University Hospital Basel, Basel, Switzerland. Imaging, and Heart and Vascular Institutes, Cleveland Clinic, Cleveland, OH, USA.
Departments of Medicine and Diagnostic Radiology, McGill University, Montreal, QC, Canada. Duke Cardiovascular Magnetic Resonance Center, and Departments of Medicine and Radiology, Duke University Medical Center, Durham, NC, USA.
Department of Cardiology, Academic Teaching Hospital Agatharied of the Ludwig-Maximilians-University Munich, Hausham, Germany. Departments of Medicine and Radiology and the Cardiovascular Imaging Center, University of Virginia Health System, Charlottesville, VA, USA.
Royal Brompton Hospital, and Imperial College, London, UK. Institute for Experimental and Translational Cardiovascular Imaging, DZHK German Centre for Cardiovascular Research Centre for Cardiovascular Imaging, partner site RheinMain, University Hospital Frankfurt, Frankfurt am Main, Germany.
You can also search for this author in PubMed Google Scholar. JSM wrote paragraphs, edited manuscript, corresponding author. DAB, JB, SDF, MAF, MGF, RJK, FvKB, CMK, DJP, SP and EN wrote paragraphs, edited manuscript. All authors read and approved the final manuscript.
Correspondence to Jeanette Schulz-Menger. Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Open Access This article is distributed under the terms of the Creative Commons Attribution 4. Reprints and permissions. Schulz-Menger, J. Standardized image interpretation and post-processing in cardiovascular magnetic resonance - update.
J Cardiovasc Magn Reson 22 , 19 Download citation. Received : 28 January Accepted : 17 February Published : 12 March Anyone you share the following link with will be able to read this content:.
Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative. Skip to main content. Search all BMC articles Search. Download PDF. Download ePub. Position statement Open access Published: 12 March Standardized image interpretation and post-processing in cardiovascular magnetic resonance - update Society for Cardiovascular Magnetic Resonance SCMR : Board of Trustees Task Force on Standardized Post-Processing Jeanette Schulz-Menger 1 , David A.
Bluemke 2 , Jens Bremerich 3 , Scott D. Flamm 4 , Mark A. Fogel 5 , Matthias G. Friedrich 6 , Raymond J. Kim 7 , Florian von Knobelsdorff-Brenkenhoff ORCID: orcid.
Kramer 9 , Dudley J. Abstract With mounting data on its accuracy and prognostic value, cardiovascular magnetic resonance CMR is becoming an increasingly important diagnostic tool with growing utility in clinical routine.
Preamble Cardiovascular magnetic resonance CMR has evolved into a gold standard non-invasive imaging tool in cardiovascular medicine, especially for visualizing and quantifying cardiovascular anatomy, volumes, and function, as well as for myocardial tissue characterization.
General recommendations The recommendations listed in this section apply to the acquisition and post-processing of all CMR data. The general requirements include: 1. Workstation and screen of adequate specification and resolution as per the specifications of the post-processing software 2.
Left ventricular chamber assessment Visual analysis a Before analyzing the details, review all cines in cine mode, validate observations from one plane with the others, and check for artifacts, especially in patients with irregular heart rates.
b Dynamic evaluation of global LV function: Interpretation of both ventricular chambers, in concert with extracardiac structures including assessment for hemodynamic interaction between the two chambers e. c Assessment of LV function from a global and segmental perspective.
d In presence of segmental wall motion abnormalities, use of standard LV segmentation nomenclature corresponding to the supplying coronary artery territories is recommended [ 3 , 5 , 7 ]. Quantitative analysis a General recommendations i In patients with severe arrhythmias, the end-systolic volumes tend to be overestimated and ejection fraction underestimated.
ii Calculated parameters: LV end-diastolic volume, LV end-systolic volume, LV stroke volume, LV ejection fraction, cardiac output, LV mass, and body-surface area indexed values of all except ejection fraction.
iii Evaluation of the stack of short axis images with computer-aided analysis packages. iv Contours of endocardial and epicardial borders at end-diastole and end-systole Fig.
v Epicardial borders should be drawn on the middle of the chemical shift artifact line when present. vi The LV end-diastolic image should be chosen as the image with the largest LV blood volume.
vii The LV end-systolic image should be chosen as the image with the smallest LV blood volume. viii Deviations may occur and extra care should be taken in the setting of LV dyssynchrony.
ix Automatic contour delineation algorithms must be checked for appropriateness by the reader. b LV volumes i Papillary muscles and trabecular tissue are myocardial tissue and thus ideally should be included with the myocardium as part of LV mass.
ii Outflow tract: The LV outflow tract is included as part of the LV blood volume. iii Basal descent: As a result of systolic motion of the mitral valve toward the apex basal descent , care must be taken with the one or two most basal slices by using a standardized consistent approach.
c LV mass i Calculation: difference between the total epicardial volume sum of epicardial cross-sectional areas multiplied by the sum of the slice thickness and interslice gap minus the total endocardial volume sum of endocardial cross-sectional areas multiplied by the sum of the slice thickness and interslice gap , which is then multiplied by the specific density of myocardium 1.
ii Papillary muscles: Papillary muscles and trabecular tissue are myocardial tissue and thus ideally should be included with the myocardium as part of LV mass, and this is particularly relevant in diseases with LV hypertrophy [ 6 ].
iii Basal descent and apex: When the most basal slice contains only a small crescent of basal lateral myocardium and no discernable ventricular blood pool, an epicardial contour for the visible myocardium is included for LV mass only. d Rapid quantitative analysis i A rapid quantitative analysis, known as the area-length method, can be performed using biplanar e.
e Cavity diameter and LV wall thickness can be obtained similar to echocardiography using two CMR approaches [ 12 , 15 ]: i Basal short-axis slice: immediately basal to the tips of the papillary muscles.
ii 3-chamber view: in the LV minor axis plane at the mitral chordae level basal to the tips of the papillary muscles. iii Both approaches have good reproducibility. iv For maximal LV wall thickness, the measurement should be made perpendicular to the LV wall to ensure accurate measurements.
f Research: i Real-time cine acquisitions become increasingly available and might be beneficial in patients with arrhythmia or limited breathholding capacity. ii Quantitative evaluation of LV myocardial dynamics e.
Full size image. Right ventricular RV chamber assessment Visual analysis a Review all cines in cine mode, validate observations from one plane with the others, and check for artifacts and coverage of the right ventricle RV.
b Assessment of global and regional RV function septal wall, free wall , where appropriate. c Assessment of LV and RV chambers for hemodynamic interaction i. constrictive physiology. Quantitative analysis a General recommendations i Calculated parameters: RV end-diastolic volume, RV end-systolic volume, RV ejection fraction, RV stroke volume, cardiac output, and body-surface area indexed values of all except ejection fraction.
ii The contiguous stack of short-axis images or axial cine images is evaluated with computer-aided analysis packages Fig. iii An axial stack of cines covering the RV provides the best identification of the tricuspid valve plane. iv Endocardial borders are contoured at end-diastole and end-systole Fig.
v The RV end-diastolic image should be chosen as the image with the largest RV blood volume. vi RV end-systolic image should be chosen as the image with the smallest RV blood volume.
vii As for the LV, it may be necessary to review all image slices in the stack to define end-systole. viii The pulmonary valve may be visualized, and contours are included just up to, but not superior to this level. b RV volumes i Total volumes are taken as the sum of volumes from individual 2D slices, accounting for any interslice gap and slice thickness.
c RV mass is usually not quantified in routine assessment. d Confirmation of results i If no shunts or valvular regurgitation is present, the RV and LV stroke volumes should be nearly equal small differences are seen as a result of bronchial artery supply and papillary muscle inclusions in the measurements.
Post-processing of myocardial perfusion imaging Visual analysis a Workflow: i Display perfusion and corresponding LGE images side-by-side. ii Adjust window, contrast and brightness level for an optimized contrast within the LV myocardium not the entire image.
iii Apply the same contrast, brightness and window settings to all images of the dynamic series. v Check that there was an adequate haemodynamic response to stress by reviewing the heart rate and blood pressure change between stress and symptomatic response to stress.
vi The key diagnostic feature for identifying a perfusion defect is the arrival and first passage of the contrast bolus through the LV myocardium. vii Visual analysis is based on a comparison between regions to identify relative hypoperfusion. b Stress images alone may permit the diagnosis of inducible perfusion defects.
c Scar tissue may not necessarily cause a perfusion defect, especially if rest perfusion is acquired after stress. d Criteria for an inducible perfusion defect Fig. ii Persists beyond peak myocardial enhancement and for several RR intervals.
iii Is more than two pixels wide. iv Is usually most prominent in the subendocardial portion of the myocardium. v Often manifests as a transmural gradient across the wall thickness of the segment involved: most dense in the endocardium and gradually becoming less dense towards the epicardium.
vi Over time, defect regresses from the subepicardium towards the subendocardium. vii Is present at stress but not at rest. viii Conforms to the distribution territory of one or more coronary arteries.
e Interpret location and extent of inducible perfusion defect s using AHA segment model [ 5 ]. i Comment on transmurality of perfusion defect [ 20 ]. ii Indicate extent of perfusion defect relative to scar on LGE. f Criteria for dark banding artifacts Fig.
These artifacts have the following characteristics: Are most prominent when contrast arrives in the LV blood pool. Persist only transiently before the peak myocardial contrast enhancement. Appear predominantly in the phase-encoding direction. Are approximately one pixel wide. g Pitfalls of visual analysis i Multi-vessel disease: Visual analysis is based on relative signal differences within an imaged section of the heart.
ii Microvascular disease: Diseases that affect the myocardial microvasculature e. iii If vasodilation during stress data acquisition was inadequate, visual analysis may lead to false negative interpretation of the perfusion study [ 28 ].
iv The distance of the myocardium to the surface coil affects signal intensity and may lead to misinterpretation if not considered in the analysis. Post-processing of late gadolinium enhancement LGE of the left ventricle Visual assessment a For most clinical indications, visual assessment of LGE images is sufficient.
b Workflow: i Modify image window and level so that: Noise is still detectable nulled myocardium should not be a single image intensity. LGE regions are not saturated LGE regions should not be a single image intensity. c Criteria for presence of LGE.
d Assess pattern of LGE i Coronary artery disease CAD type: Should involve the subendocardium and be consistent with a coronary artery perfusion territory.
ii Non-CAD-type: Usually spares the subendocardium and is limited to the mid-wall or epicardium, although non-CAD-type should be considered if subendocardial involvement is global [ 45 ]. e Interpret location and extent using AHA segment model [ 5 ] [ 20 ].
i Comparison of LGE images should be made with cine and perfusion images if the latter are obtained to correctly categorize ischemia and viability [ 46 ]. iii In patients with acute myocardial infarction, include subendocardial and mid-myocardial hypoenhanced no-reflow zones as part of infarct size.
f Pitfalls i Bright ghosting artifacts can result from poor electrocardiogram ECG gating, poor breath-holding, and long T1 species in the imaging plane e. iii Occasionally, it can be difficult to distinguish no reflow zones or mural thrombus from viable myocardium. v In PSIR images manual windowing and quantification algorithms may behave differently when compared with magnitude images.
Post-processing of T2-weighted imaging Visual analysis a The visual analysis of T2-weighted images aims for detecting or excluding regions with significant SI increase, as a marker for an increased free water content edema.
c Workflow: i Identify and display appropriate image s. iii Check for artifacts typically SI changes crossing anatomical structures. d Criteria for edema: i Clearly detectable high SI area respecting anatomical borders.
ii Follows an expected regional distribution pattern transmural, subendocardial, subepicardial, focal.
iii Verifiable in two perpendicular views. e High SI areas suggestive of myocardial edema should be compared to i regional function. f Pitfalls of visual analysis: i Surface coil reception field inhomogeneity: The uneven distribution of the sensitivity of the receiving surface coil may lead to falsely low SI in segments distant to the coil or falsely high SI in segments close to the coil surface, especially in dark-blood triple-inversion recovery spin echo STIR, TIRM images.
ii Low SI artifacts: Arrhythmia or through-plane motion of myocardium may cause artifacts, making areas appear with falsely low SI, especially in dark-blood triple-inversion recovery spin echo images.
iii High SI artifacts: In dark-blood triple-inversion recovery spin echo images, slow flowing blood may lead to insufficient flow suppression and results in high SI of blood, typically along the subendocardial border.
Visual analysis a The visual analysis of the series of differently T2-weighted source images should aim for detecting and excluding artifacts and significant motion. b The visual analysis of the final T2 map should aim for detecting and excluding artifacts.
c Maps may be displayed in color if the color look up tables are set according to site-specific ranges of normal, or in gray scale in combination with appropriate image processing, to highlight areas of abnormality. Quantitative analysis a For global assessment and diffuse disease, a single ROI should be drawn conservatively in the septum on mid-cavity short-axis maps to reduce the impact of susceptibility artifacts from adjacent tissues.
b In case of artifacts or non-conclusive results on mid-cavity ROIs, basal ROIs can be used for validation. c For focal disease, additional ROIs might be drawn in areas of abnormal appearance on visual inspection. d ROIs should be checked if generated automatically. e Drawing ROIs on greyscale instead of color maps may avoid bias.
f Depending on the goal of the analysis, focal fibrosis as assessed by LGE imaging may be excluded from the ROI. g There is currently no specific preferred analysis software package. h Sensitivity of mapping techniques to confounders such as heart rate and magnetic field inhomogeneities should be considered during interpretation.
i Mapping results should include the numerical absolute value, the Z-score number of standard deviations by which the result differs from the local normal mean , and the normal reference range.
j Parameter values should only be compared to other parameter values if they are obtained under similar conditions. b Full thickness ROI located in the ventricular septum i Septal ROI is drawn on mid-LV short-axis image.
ii Take care to avoid blood pool and proximal blood vessels. iii A septal ROI avoids susceptibility artifact from tissue interfaces. c Mean myocardial SI from the ROI is plotted against TE Fig. ii Curve fitting should apply a validated algorithm. v This can be compensated for by: Truncating the curve by removing later echo times Fig.
d Cut-off values at 1. Flow image interpretation and post-processing Background CMR flow imaging provides information about blood flow velocities and volumes, and enables the visualization of blood flow. Visual analysis a Appropriately aligned acquisitions of cines and stacks of cines can give valuable information on flow in relation to adjacent structures, notably on the directions, time courses and approximate dimensions of jets resulting from valve regurgitation, stenoses or shunts.
b Pitfalls: i Flow appearances on both cine and phase encoded acquisitions are highly dependent on image location and orientation, especially in the case of jet flow.
ii Check for the appropriate velocity encoding. iv If the annulus of valves is very dynamic or the imaging plane is not set correctly, the valve morphology may not be visualized.
v If imaging in the presence of metal containing devices, signal loss may be present as artifact and interpretation must proceed with caution.
vi Check for appropriate spatial and temporal resolution. Quantitative analysis a Workflow: i Through-plane measurements may be supplemented by in-plane measures if needed. ii Review phase and magnitude images side by side.
iii Examine the images to ensure the quality is sufficient and that the VENC was not exceeded, or there is little contrast i. iv Trace the borders of the vessel of interest on each phase and magnitude image so that only the cavity of the vessel is included Fig. v Baseline-correction may be considered.
vi Directly calculated parameters include antegrade and retrograde volume, flow rate, peak and mean velocity. b Pitfalls: i On the phase images, the area of flow may be slightly larger than the area of the magnitude images.
iii In general, the area that exceeds the VENC in the ROI is in the center of the vessel and not at the edges; if it is at the edges, it is usually but not always outside the vessel.
iv If imaging in the presence of devices, signal loss may be present as artifact and interpretation must proceed with caution [ 80 ]. v When measuring peak velocity, some software packages will determine the peak velocity in one pixel in the ROI whereas others may take the peak velocity of the average of a few adjacent pixels in the ROI.
vi When attempting to measure peak velocity using through-plane velocity mapping along a vessel, interpretation should be tempered by the notion that this parameter may be an underestimate as the true peak velocity lies somewhere along the vena contracta; the through-plane velocity map may not have been obtained at the level of the true peak velocity.
vii Peak velocity is only minimally affected by small background phase offsets, while volume measurements can be dramatically affected by even a small background phase offset due to the cumulative aspect of integration overspace within the ROI and time over the cardiac cycle.
viii Orientation of the image plane perpendicular to flow direction can have a significant impact on peak velocity measurement, while not significantly affecting volume flow [ 78 ]. ix Internal consistency may be used to partially assess the accuracy of measurement e.
Post-processing of angiography of thoracic aorta, pulmonary arteries and veins Visual analysis a MIP for first review of 3D data and for demonstration purposes Fig. b Aorta [ 82 , 83 ]: i Wall thickness: Review bSSFP or turbo spin echo images.
ii Wall irregularities: Review 3D-MRA source images and bSSFP or turbo spin echo. c Pulmonary arteries [ 84 ]: i Multiplanar double oblique and targeted MIP reconstructions for assessment of wall adherent thrombi, emboli, wall irregularities and abrupt diameter changes.
d Pulmonary veins [ 85 ]: i Assess for atypical insertion, small accessory veins and ostial stenoses. e Coronary arteries: i Coronary MRA either contrast-enhanced or non-contrast MRA using 3D whole heart bSSFP can play a role in assessment of congenital anomalies [ 86 ], but not usually in the context of ischemic heart disease.
Availability of data and materials not applicable. References Schulz-Menger J, Bluemke DA, Bremerich J, Flamm SD, Fogel MA, Friedrich MG, et al. Article PubMed PubMed Central Google Scholar Douglas PS, Hendel RC, Cummings JE, Dent JM, Hodgson JM, Hoffmann U, et al.
Article PubMed Google Scholar Hundley WG, Bluemke D, Bogaert JG, Friedrich MG, Higgins CB, Lawson MA, et al. Article PubMed PubMed Central Google Scholar Kramer, C. Article PubMed PubMed Central Google Scholar Selvadurai BSN, Puntmann VO, Bluemke DA, Ferrari VA, Friedrich MG, Kramer CM, et al.
Article PubMed Google Scholar Riffel JH, Schmucker K, Andre F, Ochs M, Hirschberg K, Schaub E, et al. Article PubMed Google Scholar Cerqueira MD, Weissman NJ, Dilsizian V, Jacobs AK, Kaul S, Laskey WK, et al.
The findings in MRI image interpretation MRI report Interpretatikn just as important as the images themselves, but ijage times, they can inage MRI image interpretation and overwhelming. Here are some distinct terms, Wearable glucose monitoring and acronyms commonly found in MRI reports:. A lesion is interrpetation area of abnormal tissue that appears different from surrounding tissue on an MRI. It can be caused by a variety of factors such as cancer, infection, or injury. T1-weighted is a type of MRI image that uses the T1 relaxation time of the tissues to create images. T1-weighted images highlight soft tissues and can help identify tumors and other lesions. T2-weighted is a type of MRI image that uses the T2 relaxation time of tissues to create images. Magnetic resonance imaging MRI is intsrpretation medical imaging technique that uses a imagw field and computer-generated radio waves to interpeetation detailed images of MRI image interpretation organs and interpretatioj in your Anti-inflammatory diet. Most MRI Foot cramps at night MRI image interpretation large, tube-shaped magnets. When you lie inside an MRI image interpretation machine, the magnetic field inside works with radio waves and hydrogen atoms in your body to create cross-sectional images — like slices in a loaf of bread. The MRI machine also can produce 3D images that can be viewed from different angles. MRI is a noninvasive way for a medical professional to examine your organs, tissues and skeletal system. It produces high-resolution images of the inside of the body that help diagnose a variety of conditions. MRI is the most frequently used imaging test of the brain and spinal cord.
Ich entschuldige mich, aber meiner Meinung nach sind Sie nicht recht. Schreiben Sie mir in PM, wir werden reden.
Welcher sympathischer Gedanke
Interessant:)
Wacker, Sie hat der einfach prächtige Gedanke besucht
Darin ist etwas auch mir scheint es die ausgezeichnete Idee. Ich bin mit Ihnen einverstanden.