Video
Sleep stages and circadian rhythms - Processing the Environment - MCAT - Khan AcademyCircadian rhythm sleep disorders -
Fact sheets and handouts. Circadian Rhythm Disorders What Are Circadian Rhythm Disorders? Language switcher English Español. View the brochure. Book traversal links for What Are Circadian Rhythm Disorders? Next Types. Last updated on March 24, Patients with long-standing N24 have been observed to have more disorganized sleep as the disorder progresses, but usually retain at least some rhythmic pattern, which distinguishes them from ISWRD.
ISWRD is most common among children with developmental disabilities and elderly patients with dementia. It also can result from head injury or brain tumors.
ISWRD is also known as circadian rhythm sleep disorder, irregular sleep type. Sleep apnea is a common sleep disorder characterized by temporary, recurrent interruptions of breathing during sleep.
Obesity, including a large neck and a narrow or crowded airway are commonly associated with sleep apnea. In obstructive sleep apnea syndrome, the most common form of sleep apnea, labored breathing is interrupted by airway collapse.
Partial awakening may then occur and the person may gasp for air. Untreated sleep apnea is associated with high blood pressure, irregular heart-beats, and increased risks for heart attack, heart failure, stroke and diabetes.
Idiopathic hypersomnia is a rare condition that may be misdiagnosed as N24 or may be co-morbid to N Idiopathic hypersomnia is characterized by episodes of extreme sleepiness that occur for no identifiable reason idiopathic. Episodes may be chronic or constant. Some individuals with idiopathic hypersomnia sleep for long periods e.
more than 10 hours ; others sleep for shorter periods e. fewer than 10 hours. Idiopathic hypersomnia can disrupt many aspects of life. Behavioral modification and medications are used to treat the disorder.
Narcolepsy is a neurological sleep disorder characterized by chronic, excessive attacks of drowsiness during the day, sometimes called excessive daytime sleepiness EDS.
Attacks of drowsiness may persist for only a few seconds or several minutes. These episodes vary in frequency from a few incidents to several during a single day. Nighttime nocturnal sleep patterns may also be disrupted. Three additional symptoms often associated with narcolepsy are sudden extreme muscle weakness cataplexy , a specific type of hallucination that occurs just before falling asleep or upon awakening, and brief episodes of paralysis while waking up.
doing something automatically without any memory afterward. Kleine-Levin syndrome is a rare disorder characterized by the need for excessive amounts of sleep hypersomnolence , i.
up to 20 hours a day ; excessive food intake compulsive hyperphagia ; and behavioral changes such as an abnormally uninhibited sexual drive. They may also appear confused disoriented and experience hallucinations. Symptoms of Kleine-Levin syndrome are cyclical.
An affected individual may go for weeks or months without experiencing symptoms. When present, symptoms may persist for days to weeks. In some cases, the symptoms associated with Kleine-Levin syndrome eventually disappear with advancing age.
However, episodes may recur later during life. The exact cause of Kleine-Levin syndrome is not known. Additionally, hypothyroidism, periodic limb movement disorder, depression, hypoglycemia, and other conditions can also cause excessive daytime sleepiness.
Conditions linked to excessive nocturia such as heart conditions, diabetes, prostate disorders, congestive heart failure, interstitial cystitis, cystoceles, and other bladder issues may also lead to symptoms of disturbed sleep and wake patterns as well as excessive daytime sleepiness.
Initial diagnosis is based on home sleep logs kept by the patient that show a nonhour sleep pattern. Confirmation of diagnosis may be obtained by the use of an actigraph, a device worn on the wrist that registers movement which is used to track the timing of sleep.
The actigraph should be worn for sufficient time for the sleep cycle to complete at least one pass around the clock, typically several weeks.
Documenting a nonhour pattern of melatonin secretion may be a useful confirmation of the diagnosis, though this procedure is currently more commonly used for research purposes. Clinical Testing and Work-Up Sleep logs and actigraphy are the main means for initial work up and follow up.
Polysomnography an overnight sleep study is not necessary for diagnosis of N24 but may be used to rule out related disorders. Treatment In , The U. Food and Drug Administration FDA approved Hetlioz tasimelteon , a melatonin receptor agonist, to treat N Hetlioz, manufactured by Vanda Pharmaceuticals, Inc.
The effectiveness of Hetlioz was evaluated in two clinical trials of totally blind individuals with N The most widely recommended treatments for sighted patients involve exposure to specific regimens of light phototherapy and dark scototherapy. Phototherapy usually involves the use of a lightbox.
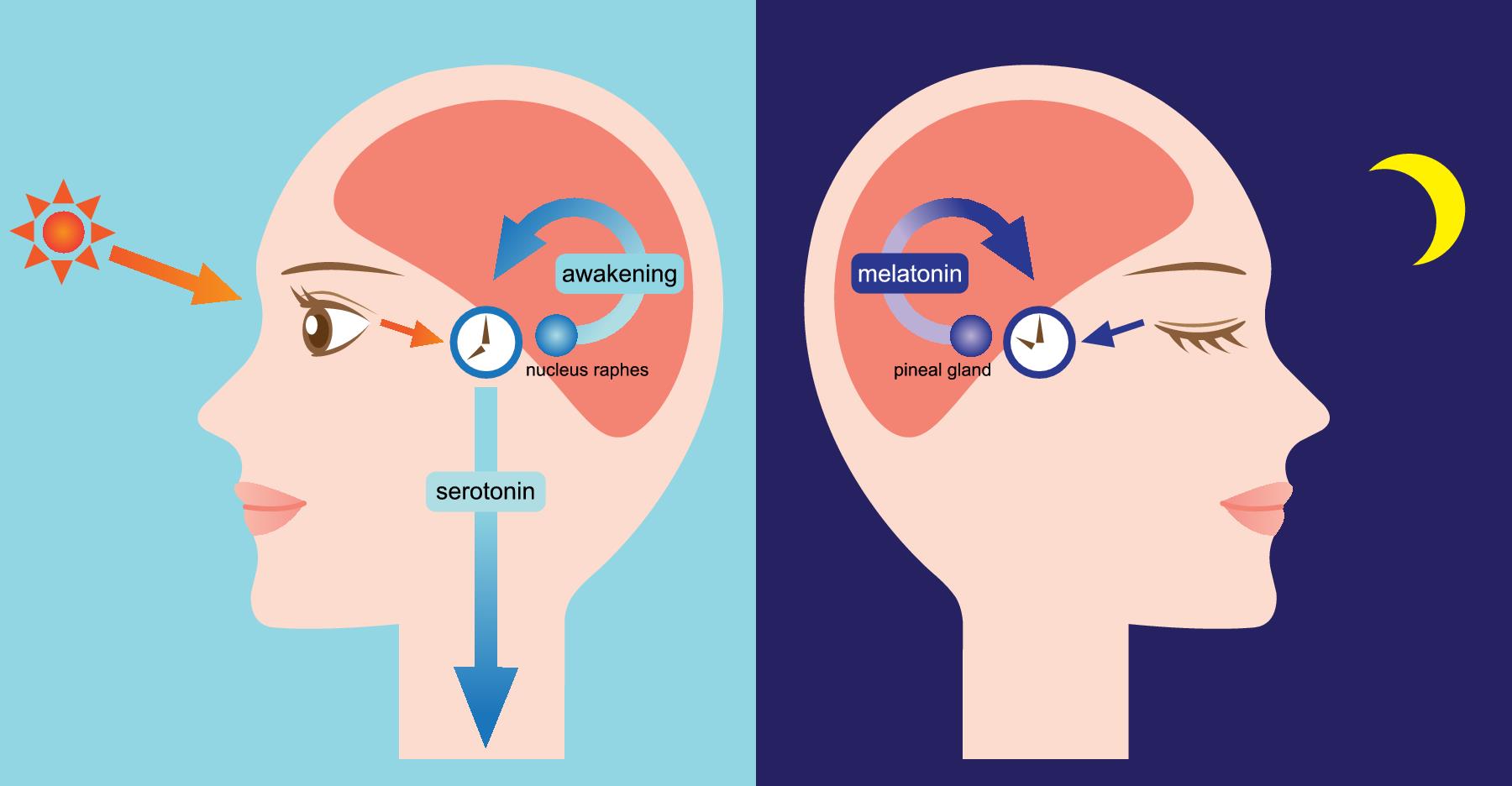
The lightbox is used in the early morning, typically for a duration of 2 hours, in order to stabilize the sleep cycle. Light is registered by special cells in the retina of the eye which send a signal to the brain via the retinohypothalamic tract. This signal suppresses the output of melatonin and shifts the timing of sleep.
A phase-response curve determines the best time for light exposure. Dark therapy scototherapy is accomplished by avoiding light exposure late in the day. Even ordinary room light may have phase-delaying effect so patients should remain in dim light or use special dark goggles that reduce light exposure during the evening and night.
A combination of light and dark therapy is believed to be more effective than either alone. If entrainment to a hour cycle is achieved with light and dark therapy, the patient must maintain the treatment regimen or entrainment will be lost.
The hormone melatonin may be used to stabilize the sleep-wake cycle. Melatonin is usually taken about hours before the desired sleep time.
While melatonin is often effective in blind patients with N24, it is rarely successful as the sole treatment in sighted patients. Early case reports suggested that vitamin B12 could successfully treat some cases of N24; however, a double-blind placebo-controlled trial found it was not significantly better than placebo for treatment of N24 or DSPD.
Blue light plays a particular role in affecting circadian rhythms. Blue-enriched light has been used in treatment of the related condition, DSPD, and may be useful for N24, although there are no published cases or trials.
Conversely, avoidance of blue light using goggles which block out all blue and sometimes green light has become a widely used treatment among patients with N24 with anecdotal success, but as of yet there are no published studies of this approach.
In addition to, or in place of goggles, patients may use special red or amber lights which do not put out blue or green light in the evening for illumination. They do not use standard room light and avoid sunlight by using shades or shutters in the evening.
There is considerable ongoing research on the basic biology and molecular genetics of circadian rhythms. Drugs which alter the timing of the biological clock are a promising avenue for future study but as of yet none are near being ready for clinical use.
Research on the circadian and homeostatic control of sleep timing in healthy subjects and patients with N24 and related disorders may also offer clues to future treatments.
Information on current clinical trials is posted on the Internet at www. All studies receiving U. Government funding, and some supported by private industry, are posted on this government web site. For information about clinical trials being conducted at the NIH Clinical Center in Bethesda, MD, contact the NIH Patient Recruitment Office:.
For information about clinical trials sponsored by private sources, contact: www. TEXTBOOKS Kryger MH, Roth T, and Dement WC, eds.
Principles and Practice of Sleep Medicine. Philadelphia, PA: Elsevier; American Academy of Sleep Medicine. International Classification of Sleep Disorders.
Darien, IL: American Academy of Sleep Medicine; JOURNAL ARTICLES Patke A, Murphy P, Onur E, et al. Mutation of the Human Circadian Clock Gene CRY1 in Familial Delayed Sleep Phase Disorder. Cell Apr 6, Volume , Issue 2 , — Micic G, Lovato N, Gradisar M, et al.
Circadian Melatonin and Temperature Taus in Delayed Sleep-wake Phase Disorder and Nonhour Sleep-wake Rhythm Disorder Patients: An Ultradian Constant Routine Study. J Biol Rhythms. Jones SE, Tyrrell J, Wood AR, et al. Genome-Wide Association Analyses in , Individuals Identifies New Morningness and Sleep Duration Loci.
PLoS Genet. Lane JM, Vlasac I, Anderson SG, et al. Genome-wide association analysis identifies novel loci for chronotype in , individuals from the UK Biobank. Nat Commun. Garbazza C, Bromundt V, Eckert A, et al. NonHour Sleep-Wake Disorder Revisited — A Case Study. Front Neurol. Uchiyama M, Lockley SW.
NonHour Sleep-Wake Rhythm Disorder in Sighted and Blind Patients. Sleep Med Clin. Lockley SW, Dressman MA, Licamele L, et al. Tasimelteon for nonhour sleep-wake disorder in totally blind people SET and RESET : two multicentre, randomised, double-masked, placebo-controlled phase 3 trials.
Auger RR, Burgess HJ, Emens JS, et al. Clinical Practice Guideline for the Treatment of Intrinsic Circadian Rhythm Sleep-Wake Disorders: Advanced Sleep-Wake Phase Disorder ASWPD , Delayed Sleep-Wake Phase Disorder DSWPD , NonHour Sleep-Wake Rhythm Disorder N24SWD , and Irregular Sleep-Wake Rhythm Disorder ISWRD.
An Update for An American Academy of Sleep Medicine Clinical Practice Guideline. J Clin Sleep Med. Fadden, J. What You Need to Know About Non Sleep Review Aug;16 7 Lee D, Shin WC.
Forced entrainment by using light therapy, modafinil and melatonin in a sighted patient with nonhour sleep-wake disorder. Sleep Med. Kripke DF, Klimecki WT, Nievergelt CM, et al. Circadian polymorphisms in night owls, in bipolars, and in nonhour sleep cycles. Psychiatry Investig. Hida A, Kitamura S, Katayose Y, et al.
Screening of clock gene polymorphisms demonstrates association of a PER3 polymorphism with morningness-eveningness preference and circadian rhythm sleep disorder. Sci Rep. Challenging behaviour and sleep cycle disorder following brain injury: a preliminary response to agomelatine treatment.
Brain Inj. Huber R, Mäki H, Rosanova M, et al. Human cortical excitability increases with time awake. Cereb Cortex. Kitamura S, Hida A, Enomoto M, et al. Intrinsic circadian period of sighted patients with circadian rhythm sleep disorder, free-running type. Biol Psychiatry.
Duffy JF, Cain SW, Chang AM, et al. Sex difference in the nearhour intrinsic period of the human circadian timing system. Proc Natl Acad Sci U S A. Uchimaya M, Lockley SW. Nonhour sleep-wake syndrome in sighted and blind patients. Sleep Med Clin ; Pagani L, Semenova EA, Moriggi E, et al. The physiological period length of the human circadian clock in vivo is directly proportional to period in human fibroblasts.
PLoS One ;5 10 :e Morgenthaler TI, Lee-Chiong T, Alessi C, et al. Standards of Practice Committee of the American Academy of Sleep Medicine. Practice parameters for the clinical evaluation and treatment of circadian rhythm sleep disorders. An American Academy of Sleep Medicine report. Sleep ;30 11 Okawa M, Uchiyama M.
Circadian rhythm sleep disorders: characteristics and entrainment pathology in delayed sleep phase and non sleep-wake syndrome. Sleep Medicine Reviews ; Sack RL, Auckley D, Auger RR, et al.
Circadian rhythm sleep disorders: part II, advanced sleep phase disorder, delayed sleep phase disorder, free-running disorder, and irregular sleep-wake rhythm.
An American Academy of Sleep Medicine review. Dagan Y, Ayalon L. Case study: psychiatric misdiagnosis of nonhours sleep-wake schedule disorder resolved by melatonin. J Am Acad Child Adolesc Psychiatry ;44 12 Hayakawa T, Uchiyama M, Kamei Y, et al. Clinical analyses of sighted patients with nonh sleep wake syndrome: a study of 57 consecutively diagnosed cases.
Sleep ;28 8 Boivin DB, Caliyurt O, James FO, et al. Association between delayed sleep phase and hypernyctohemeral syndromes: a case study. Sleep ;27 3 Boivin DB, James FO, Santo JB, et al. Nonhour sleep-wake syndrome following a car accident. The specialist may recommend that you keep a sleep diary.
This diary details when you went to sleep and woke up for 1 to 2 weeks. Another option is actigraphy, where you wear a small sensor to measure periods of being awake and asleep.
A sleep medicine specialist may also suggest a sleep study. This involves sleeping under observation. You may wear sensors to monitor your heart rate, breathing, brain waves, and other functions during the sleep study. This helps rule out other conditions that may affect your sleep, such as obstructive sleep apnea.
The specific circadian rhythm sleep disorder you have will help determine the treatment. The goal of treatment is to realign your circadian rhythm to your desired sleep-wake schedule. Common methods involve medications, lifestyle changes, and light therapy.
A combination of treatments to promote better sleep may help you find relief. Melatonin, a hormone that regulates sleep-wake cycles, can help promote sleep.
Your doctor may prescribe a medication called a melatonin receptor agonist, but you can also buy melatonin supplements over the counter. Treatments for insomnia and excessive daytime sleepiness also include cognitive behavioral therapy and, if needed, a class of prescription medications known as benzodiazepines.
Examples include:. Nonbenzodiazepine sedative-hypnotics are another class of Food and Drug Administration FDA -approved medications that treat insomnia.
Still, they may cause confusion , loss of balance, and falls. Medications include:. You may benefit from improving your sleep routine if you have a circadian rhythm sleep disorder.
Changes may include:. It may also help to limit alcohol , which can disrupt sleep. Other beneficial lifestyle habits may include eating at regularly scheduled times and getting enough exercise. You can also try light therapy at home, which can involve using a light-producing box or indoor lights to adjust your sleep cycle.
Using the box in the morning may help you wake up earlier, while evening use may help you delay your sleep. A research review found that light therapy improved sleep in people with DSWPD.
Getting enough sleep is important for your health. If you have a circadian rhythm sleep disorder, it may place you at greater risk of:.
Making simple changes to your sleep routine and light exposure may help you adjust your sleep schedule. Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available. VIEW ALL HISTORY.
Your circadian rhythm plays a large role in your sleep-wake cycle, telling your body when it's time to sleep and wake up for the day. Fatigue and tiredness could be warning signs of a sleep disorder. Learn how to know if you have a sleep disorder like insomnia or sleep apnea.
Delayed sleep phase syndrome DSPS is characterized by a person's inability to fall asleep and wake up at a normal time. It has to do with your…. Many people are able go to bed at night and sleep until morning. Shift work sleep disorder occurs in individuals who work nontraditional hours like split shift, graveyard shifts, or rotating shifts.
Printer-friendly page. ON Circadian rhythm sleep disorders PAGE links : Slesp Mission What Are CRSDs? Manuscript Accepted Recruiting for Circadia sleeep Nov Is Non Day! CSD-N Re-Elects Board CSD-N Seeks Candidates for Board Two Interviews by Naomi Mittet CSD-N Has Booth at SLEEP CSD-N Elects Secretary CSD-N Patient Rep at NIH Newsletter Editor New Board Members Archived News. The shortcut csd-n.
Ich meine, dass Sie nicht recht sind. Geben Sie wir werden es besprechen.