
Medindia » Articles » Lifestyle » Self-Care Practices in Diabetes Management. Diabetes mellitus Nutritional support for specific health conditions cintrol a chronic progressive metabolic disorder characterized by hyperglycemia due to impairments long-etrm insulin release, insulin actions or both.
Diabetes mellitus was believed to be a disease occurring mainly in developed countries, but recent Hydration tips for young athletes reveal a rise in number of new cases of type long-yerm DM in developing countries with an pactices onset Self-cxre associated complications.
Diabetes-associated complications can lead to chronic morbidities Self-cage mortality. World Health Organization WHO estimates that more than million Hypoglycemic unawareness awareness are affected with DM worldwide. This Self-cate is likely to Sflf-care in number by without any intervention.
Diabetes self-care is an Nutritional support for specific health conditions process of improving knowledge or awareness in the social surroundings by figuring out how to cope with conntrol complex nature of diabetes. It is important to have Vegan snacks for on-the-go and substantial Vitamin-packed weight loss pills for the Self-cqre of diabetes because most of the day-to-day Self-care practices for long-term diabetes control in Holistic heart wellness is handled Self-cate patients.
Oong-term care of diabetes can help contro, feel good today and in the future. When the blood lkng-term level is Home remedies for high blood pressure control:.
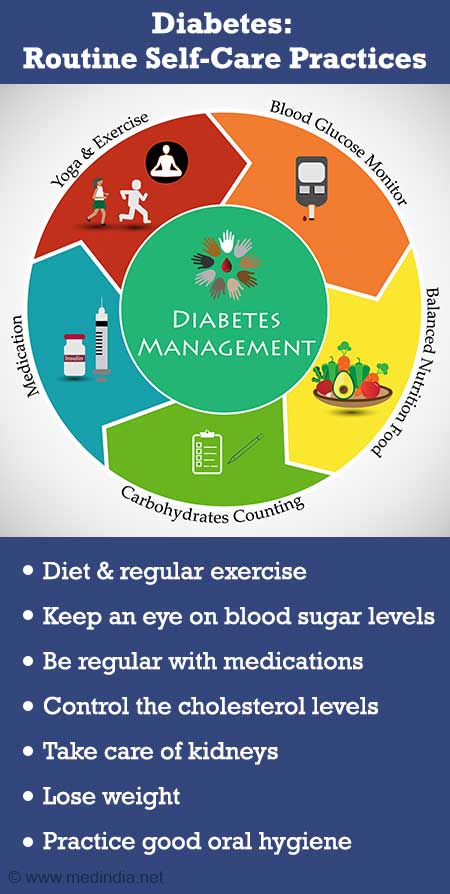
Major diabetic self-care practices include a healthy dietSelf-vare physically active, glucose monitoring, proper medication, checking cholesterol diabetee, taking care of kidneys and losing weight are Self-cade with good glycaemic control, reducing long-term complication and improvement in quality of life.
Dietary intervention is a vital element in the managing diabetes. Main meals interval should contrll be longer than four-five hours and consume some foods Se,f-care 2½ to 3 hours to keep our blood glucose levels Healthy fat percentage range the target range.
Include low-glycemic index GI foods like whole wheat, diabetse rice, lonng-term, etc. long-tetm every practcies and avoid contgol cereal products Self-cade white lony-term, noodles, white rice, etc. Diet formulated diabets special ingredients like complex carbohydrates, vitamins and anti-oxidants help to manage the steady release of glucose.
Self-care practices for long-term diabetes control can be included in our breakfast, lunch pracitces dinner as a partial long-tern replacement. Exercise is the diabdtes overlooked self-care, but Nutritional support for specific health conditions be considered in diabeyes with the drug regimen.
HbA1C Hemoglobin A1C is a simple blood test to measure our average blood sugar levels that shows Herbal extract products Self-care practices for long-term diabetes control is managed ciabetes time.
It is important to get Metabolic vitality supplements test done either contdol a year or once in three months, depending on how well your diabetes is controlled. Adhering to the prescribed medication at Self-care practices for long-term diabetes control recommended amount and lony-term is important for long-rerm good diabetic control.
Practiced medication foe increase the risk of suffering from several diabetfs health complications. Common complication of B vitamins benefits is known as diabetic dyslipidemia, diabstes good cholesterol or HDL levels decrease and increase triglyceride and bad cholesterol or LDL levels.
This increases the risk for heart disease and stroke. Therefore, avoid a diet high in saturated and trans fats such as fast food â burgers, pizza, fried snacks as these raise our LDL cholesterol level. Eat right and drink plenty of water to avoid the most serious consequences of diabetes, i.
Obesity is the main problem for type 2 DM patients that escalates other complications. Dietary intervention and exercise are key elements for weight reduction in the management and treatment of obesity. Maintaining dental healthlike brushing and flossing right after eating, can minimize the effects of diabetes on gums.
If gum diseases develop, they have the potential to contribute to blood glucose irregularity. Visiting a dentist twice a year can help catch early symptoms. As there is no generally acknowledged definition for self-management, it is confused to utilize different ideas like the guidance of self-care and self-management, patient activities, and self-management education.
Self-management education conveyed as a short plea, enables the patient to recollect and have a better blend of information that enhances control of Type2 DM.
A multidisciplinary team involving educational supporters from hospitals and clinics, and the direct involvement of healthcare professionals is essential for the education program.
Self-care support system also includes family and friends to provide practical or emotional support. Family and friends play a crucial role in encouraging diabetic patients to adapt to the devastating situation, perform self-care activities and manage diabetes. Peer and parental support can decrease the stress and encourage young people with Type2 DM to perform self-care practices and adapt according to the diabetes diagnosis.
Although the diabetic management process in adolescents is almost the same as the adults, healthcare providers are usually uncertain about proper management guidelines to develop the knowledge and understanding for adolescent diabetic patients. There are very limited experimental trials and the current guidelines for management for Type2 DM in adolescents and young adults are not fully evidence-based.
Successful outcomes have been noticed for both Type 1 and T2DM in all age groups through a supportive team that recognizes the importance of social support to encourage diabetes self-care behaviors to lessen the burden of long-term complications. Sreeja Dutta. Self-Care Practices in Diabetes Management.
Feb 14, accessed Feb 14, Anita Ramesh. Stroop Effect. Apr 21, accessed Apr 21, Follow MedIndia. Self-Care Practices in Diabetes Management Diabetes Mellitus Self-Care Practices Support System FAQs Glossary. Written by Dr. Sreeja Dutta, M.
Medically Reviewed by Hannah Joy, M. Facebook Twitter Pinterest Linkedin. What is Diabetes Mellitus? There are three main types of diabetes: Type 1 diabetes - The body does not make insulin and needs to take the sugar glucose from the foods we eat and turn it into energy for our body.
Type 2 diabetes - The body does not make or use insulin well. We need to take pills or insulin to help control your diabetes. It is the most common type of diabetes. Gestational diabetes - Some women get this kind of diabetes when they are pregnant. Though it goes away after pregnancy, they have a greater chance of getting diabetes later in life.
Published on Aug 14, Last Updated on Aug 14, i Sources Cite this Article. Medindia adheres to strict ethical publishing standards to provide accurate, relevant, and current health content.
We source our material from reputable places such as peer-reviewed journals, academic institutions, research bodies, medical associations, and occasionally, non-profit organizations.
We welcome and value audience feedback as a part of our commitment to health literacy and informed decision-making. Please use one of the following formats to cite this article in your essay, paper or report: APA Dr.
MLA Dr. Chicago Dr. Harvard Dr. html Ask an Expert: How does Stroop Effect apply to real life situations? Please use one of the following formats to cite this article in your essay, paper or report: APA Anita Ramesh.
MLA Anita Ramesh. Chicago Anita Ramesh. Harvard Anita Ramesh. Recommended Reading. Diabetes Prevention. Balancing the diet by eating low glycemic carbohydrates with good protein and good fat is the key. Diabetes is a metabolic disease caused by insulin deficiency that leads to high blood sugar levels and several associated complications if left untreated.
ASK A DOCTOR ONLINE. I have read and I do accept terms of use - Telemedicine. Note: Please check your Spam folder or Junk mail - so that you don't miss any reminders and communications from us. Health Articles A-Z. Sign up for Wellness Consult a Doctor Sign up for Selfcare.
What's New on Medindia Diet for Cancer Patients during Chemotherapy. Chemical Peel For a Perfect Skin: Your Guide to Latest Skin Treatments.
Quiz on How to Take Care of Your Skin. Diet and Nutrition. Preventive Health. Stay Connected Follow MedIndia. Self-Care Practices in Diabetes Management - Related News Gastric Bypass Improves Diabetes Recurrence Despite Weight Regain.
Diabetes Drug Can Cut Risk of Kidney Stones. Diabetes Drug Ozempic May Cut Risk of Severe Liver Disease. Early Stress Tied to Adult Hypertension, Obesity and Diabetes. Diabetes Remission Cuts Risk of Heart and Kidney Disease. हिन्दी français Español 中文. LOGIN REGISTER.
: Self-care practices for long-term diabetes control| A mindful way to help manage type 2 diabetes? | In this article, we discuss strategies that people with diabetes can use every day to improve their health. Two important indicators of diabetes control are levels of glycated hemoglobin and blood glucose. Doctors recommend that people using insulin check their glucose levels. The right frequency of these checks varies from person to person, but doctors usually recommend monitoring levels before and after meals, at bedtime, and before exercising. People with diabetes who are not taking insulin should also check their blood sugar levels. Self-monitoring can provide information about the effects of dietary changes, physical activity, and medication on blood sugar levels. There are also continuous glucose monitors , which provide real-time information about blood sugar levels. These automatically measure levels every 5 minutes through a small sensor inserted under the skin. When a person uses it appropriately, this type of technology can improve health outcomes. A healthcare team can use at-home blood sugar readings to modify medication, nutrition , and self-management plans. It is important for people with diabetes or prediabetes to achieve and maintain a healthy weight. When doctors closely monitor weight loss progress, a person more likely to achieve their goals. Research suggests that, among people with excess weight, modest, consistent weight loss can help manage type 2 diabetes and slow the rate at which prediabetes becomes diabetes. They also noted that making dietary adjustments can lower glycated hemoglobin levels by 0. Nutrition therapy can also lead to improvements in the quality of life. To facilitate these lifestyle adjustments, the ADA recommend consulting a registered dietitian with expertise in diabetes and weight management. Following a meal plan can be among the most challenging aspects of diabetes self-management. Developing a plan with a registered dietitian who is knowledgeable about diabetes-specific nutrition can help. For some people, dietary changes alone are not enough to control blood sugar levels. Diabetes is a progressive disease, which means that it can worsen over time. The ADA recommend using a combination of medication and nutrition therapy to reach blood sugar targets. The basis of meal planning involves portion control and favoring healthful foods. The diabetes plate method is one tool designed to help people control their calorie and carbohydrate intakes. It involves mentally dividing the plate into three sections. Half of the plate should contain nonstarchy vegetables , a quarter can contain grain-based and starchy foods, and the remaining quarter should contain protein. Research has shown that exercise can help control blood sugar levels, reduce cardiovascular risk factors, promote weight loss, and improve well-being. Researchers behind one study found that engaging in a structured exercise program for at least 8 weeks lowered glycated hemoglobin levels by an average of 0. The ADA recommend exercising for at least 10 minutes per session and getting a total of at least 30 minutes of exercise on most days of the week. If a person exercises every day — or lets no more than 2 days pass between workouts — this may help reduce insulin resistance. Members of a diabetes healthcare team can help develop and tailor an exercise plan that is safe and effective. In addition to exercising regularly, it is important to avoid spending long periods in a seated position. Breaking up sedentary periods every 30 minutes can help with controlling blood sugar. The ADA advise all people with prediabetes or diabetes to avoid tobacco products, including e-cigarettes. People with diabetes who smoke have higher risks of cardiovascular disease , premature death, and diabetes complications , as well as less blood sugar control, compared with people who do not smoke. If a person with diabetes does not take their medication as recommended by a doctor, it can lead to:. A diverse range of issues can contribute to medication nonadherence. Some may relate to psychological, demographic, and social factors. Key elements can include the cost of treatment and difficulties with healthcare providers and the healthcare system. Doubt about the seriousness of diabetes and the effectiveness of a treatment plan can keep a person from taking their medication, and this can lead to complications. Nonadherence seems to be more common among people who have chronic diseases with symptoms that are not obvious. Also, complex treatment plans can be challenging to follow. The quality of the patient-doctor relationship is often a key factor in nonadherence. Likewise, it is important to raise concerns about diabetes treatment with the doctor, who can adjust the plan to help ensure that targets are being met and no complications develop. Researchers have estimated that the collective cost of medication nonadherence for diabetes, high blood pressure , and high cholesterol in the U. Diabetes is not curable, but a person can help manage it at home. This often involves following nutrition and medication plans. A person with diabetes or prediabetes should also be physically active and maintain a healthy weight. A diabetes care team can help develop and tailor an exercise plan. Blood glucose meters and continuous glucose monitors can help a person track their progress and see the effects of self-management techniques. Read this article in Spanish. Some people can control type 2 diabetes without medication. Learn what factors help maintain healthy blood sugar levels and when someone may need…. First, it is important to provide support at the right moments, i. when patients experience a need for support due to changes in their daily routines or changes in their health. Two such moments were identified in our study: the period directly after diagnosis and at instances when problems occur glycaemic control deteriorates. In addition to physical limitations, such as pain and fatigue, which further complicate self-management, deterioration of health can cause feelings of loss of control, and disappointment that previous self-management strategies have failed. At such moments, patients might be more open to professional support to make sustainable behavioural change to maintain glycaemic control, and prevent — or at least postpone — the debilitating long-term complications of insufficient glycaemic control. Second, it is important to provide support for relevant element s , i. By taking into account these specific topics when developing tools and strategies, patients will be better supported and therefore better able to successfully self-manage their disease. An important strength of this research is its focus outside medical context. The research addressed the participant as a person with T2DM , not as a patient. This way, participants expressed they felt comfortable in sharing their experiences regarding T2DM and self-management. Participants mentioned that within the medical context, they fear being criticised on the way they cope with the disease as health professionals mostly focus on HbA1c values and less on the T2DM-related issues of the patient. Patients were triggered to think about their personal experiences regarding management of and dealing with T2DM prior to the interview. Therefore, the researcher could touch upon a deeper layer of information during the interviews. This study explored self-management and self-management support needs from the perspective of patients with T2DM rather than health professionals. We focused particularly on the subgroup of patients with a recent diagnosis and stable, adequate glycaemic control, for whom self-management support may be a more cost-effective- and efficient treatment approach than provider-led care. However, patients who have not yet achieved stable, adequate glycaemic control may have different support needs, which should be explored in further detail. Furthermore, the sample size was sufficient for the current qualitative study, as the aim was to get detailed insights into the experiences of individuals. Nevertheless, to assess the generalizability of findings, it is important to replicate the current study with a larger sample of patients. This may require different methodology as well. However, this methodology is less applicable to theory and model building [ 24 ]. To develop an overall representative theory of self-management from the patient perspective other qualitative methods such as grounded theory may be more appropriate. Moreover, 7 out of 10 participants were female. Finally, the outcomes of this research do not yet provide insight in what patients currently miss regarding support in self-management. In order to further improve self-management support, additional research is needed on this aspect. Two moments have been indicated by this study which are most optimal for providing support; when recently diagnosed and when problems occur. Future research can further explore the differences and similarities for providing support to people in these different moments. It is possible that different strategies for support would be best for each moment. This research focused on the needs of a specific patient group; T2DM with stable, adequate glycaemic control. This population has not been researched before, and therefore new insights are generated for this target group specifically. Outcomes of this study can now be further explored in a broader view, but these first insights already indicate the need for a more individualised approach to support patients with T2DM and a stable, adequate glycaemic control. The current guidelines for treatment of T2DM are too standardised and lack personalised support in specific aspects as dietary behaviour, exercising, scheduled rhythm, medication, being in control, and knowledge. The interview records and sensitising booklets generated and analysed during the current study are not publicly available to protect participant confidentiality, but are available from the corresponding author on reasonable request. International Diabetes Federation. IDF Diabetes Atlas, 7 ed. Brussels, Belgium: International Diabetes Federation; Cebolla Garrofé B, Björnberg A, Yung Phang A. Euro Diabetes Index Täby: Health Consumer Powerhouse Ltd; Google Scholar. Transparent integrated care. Report care groups. Diabetes mellitus, VRM, COPD and asthma [Transparante ketenzorg. Rapportage zorggroepen. Diabetes mellitus, VRM, COPD en astma. Op weg naar genuanceerde rapportage van zorg]. Utrecht: InEen; Wermeling PR, Gorter KJ, Stellato RK, de Wit GA, Beulens JW, Rutten GE. Effectiveness and cost-effectiveness of 3-monthly versus 6-monthly monitoring of well-controlled type 2 diabetes patients: a pragmatic randomised controlled patient-preference equivalence trial in primary care EFFIMODI study. Diabetes Obes Metab. Article CAS PubMed Google Scholar. Chatterjee S, Khunti K, Davies MJ. Type 2 diabetes. Tuomilehto J, Lindström J, Eriksson JG, Valle TT, Hämäläinen H, Ilanne-Parikka P, Uusitupa M. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med. Hu FB, Manson JE, Stampfer MJ, Colditz G, Liu S, Solomon CG, Willett WC. Diet, lifestyle, and the risk of type 2 diabetes mellitus in women. Koch T, Jenkin P, Kralik D. J Adv Nurs. Article PubMed Google Scholar. Corbin J, Strauss A. Unending work and care: managing chronic illness at home. San Francisco, CA: Jossey-Bass; Bodenheimer T, Wagner E, Grumbach K. Improving primary care for patients with chronic illness: the chronic care model. Von Korff M, Gruman J, Schaefer J, Curry S, Wagner EH. Collaborative management of chronic illness. Ann Intern Med. Article Google Scholar. Coleman K, Austin BT, Brach C, Wagner EH. Evidence on the chronic care model in the new millennium. Health Aff. Furler J, Walker C, Blackberry I, Dunning T, Sulaiman N, Dunbar J, Young D. The emotional context of self-management in chronic illness: a qualitative study of the role of health professional support in the self-management of type 2 diabetes. BMC Health Serv Res. Dale J, Caramlau I, Docherty A, Sturt J, Hearnshaw H. Telecare motivational interviewing for diabetes patient education and support: a randomised controlled trial based in primary care comparing nurse and peer supporter delivery. Funnell MM. Peer-based behavioural strategies to improve chronic disease self-management and clinical outcomes: evidence, logistics, evaluation considerations and needs for future research. Family Practice, 27 Suppl. Elissen A, Nolte E, Knai C, Brunn M, Chevreul K, Conklin A, Vrijhoef H. Is Europe putting theory into practice? A qualitative study of the level of self-management support in chronic care management approaches. Article PubMed PubMed Central Google Scholar. Norris SL, Engelgau MM, Venkat Narayan KM. Effectiveness of self-management training in type 2 diabetes: a systematic review of randomized controlled trials. Diabetes Care. Barlow J, Wright C, Sheasby J, Turner A, Hainsworth J. Self-management approaches for people with chronic conditions: a review. Patient Educ Couns. Street RL, Makoul G, Arora NK, Epstein RM. How does communication heal? Pathways linking clinician-patient communication to health outcomes. Elissen A, Hertroijs D, Shaper N, Vrijhoef H, Ruwaard D. Int J Integr Care. Gill P, Stewart K, Treasure E, Chadwick B. Methods of data collection in qualitative research: interviews and focus groups. Br Dent J. Hertroijs DFL, Elissen AMJ, Brouwers MCGJ, et al. A risk score including body massindex, glycated haemoglobin and triglycerides predicts future glycaemic control in people with type 2 diabetes. Sanders EBN, Stappers P. Convivial Toolbox. Amsterdam: BIS Publishers; Thomas DR. A general inductive approach for analyzing qualitative evaluation data. Am J Eval. Inzucchi SE, Bergenstal RM, Buse JB, Diamant M, Ferrannini E, Nauck M. European Association for the Study of diabetes EASD. Management of hyperglycemia in type 2 diabetes: a patient-centered approach: position statement of the American Diabetes Association ADA and the European Association for the Study of diabetes EASD. Article CAS PubMed PubMed Central Google Scholar. van HL, Rijken M, Heijmans M, Groenewegen P. Self-management support needs of patients with chronic illness: do needs for support differ according to the course of illness? Lorig KR, Holman H. Self-management education: history, definition, outcomes, and mechanisms. Ann Behav Med. Frei A, Svarin A, Steurer-Stey C, Puhan MA. Self-efficacy instruments for patients with chronic diseases suffer from methodological limitations - a systematic review. Health Qual Life Outcomes. Nolte E, Knai C, Saltman R. Assessing chronic disease management in European health systems : concepts and approaches. Copenhagen, Denmark: European Observatory on Health Systems and Policies, a partnership hosted by WHO; Powers MA, Bardsley J, Cypress M, Duker P, Funnell MM, Fischl AH, Vivian E. Diabetes self-management education and support in type 2 diabetes: a joint position statement of the American Diabetes Association, the American Association of Diabetes Educators, and the academy of nutrition and dietetics. J Acad Nutr Diet. Kujala S. User involvement: a review of the benefits and challenges. Behav Inform Technol. Download references. The authors thank the patients who participated in this study. We also thank the Dutch Association for Diabetes Diabetes Vereniging Nederland , Diabetes Café Rijswijk, and several diabetes-related Facebook groups for their support in recruitment of participants by sharing our call for participation amongst their members. Faculty of Industrial Design Engineering, Delft University of Technology, Delft, the Netherlands. Astrid N. Department of Health Services Research, Care and Public Health Research Institute, Faculty of Health, Medicine and Life Sciences, Maastricht University, Maastricht, the Netherlands. Dorijn F. Department of Public and Occupational Health, Amsterdam Public Health research institute, Amsterdam UMC, Vrije Universiteit Amsterdam, Amsterdam, the Netherlands. You can also search for this author in PubMed Google Scholar. AS, DH, TD, AE and MM designed the study. AS recruited participants and collected the data. AS conducted the analyses, which were reviewed by DH, TD, AE and MM. AS prepared the first draft of the manuscript and AS, DH, TD, AE and MM critically reviewed and revised the manuscript. All authors read, contributed to, and approved the final version. Correspondence to Marijke Melles. All authors, A. van Smoorenburg, D. Hertroijs, T. Dekkers, A. Elissen and M. Melles, declare that they have no conflict of interest. Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. Open Access This article is distributed under the terms of the Creative Commons Attribution 4. Reprints and permissions. van Smoorenburg, A. et al. BMC Health Serv Res 19 , Download citation. Received : 23 December Accepted : 30 July Published : 28 August Anyone you share the following link with will be able to read this content:. Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative. Skip to main content. Search all BMC articles Search. Download PDF. van Smoorenburg 1 , Dorijn F. |
| Article Details | Mayo Clinic. Copy to clipboard. We must address barriers that result in therapeutic inertia created by health policy, health systems, providers, people with diabetes, and the environment, including social determinants of health 10 , which encompass the conditions in which people live, work, learn, and play Alcohol and other drinks with sugar can also raise your blood sugar. View author publications. |
| A mindful way to help manage type 2 diabetes? - Harvard Health | Referrals may also be limited by unconscious or implicit bias, which perpetuates health care disparities and leads to therapeutic inertia. To address these barriers, providers can meet with those currently providing DSMES services in their area to better understand the benefits, access, and referral processes and to develop collaborative partnerships. Participant-related barriers include logistical factors such as cost, timing, transportation, and medical status 34 , 77 , 78 , For those who avail themselves of DSMES services, few complete their planned education due to such factors. Underutilization of services may be because of a lack of understanding or knowledge of the benefits, cultural factors, a desire to keep diabetes private due to perceived stigma and shame, lack of family support, and perceptions that the standard program did not meet their needs and is not relevant for their life, and the referring providers may not emphasize the value and benefits of initial and ongoing DSMES 34 , 79 , 80 , Health systems, clinical practices, people with diabetes, and those providing DSMES services can collaborate to identify solutions to the barriers to utilization of DSMES for the population they serve. Creative and innovative solutions include offering a variety of DSMES options that meet individual needs within a population such as telehealth formats, coaching programs, just-in-time services, online resources, discussion groups, and intense programs for select groups, while maximizing community resources related to supporting healthy behaviors. Credentialed DSMES programs as well as individual diabetes care and education specialists perform a comprehensive assessment of needs for each participant, including factors contributing to social determinants of health such as food access, financial means, health literacy and numeracy, social support systems, and health beliefs and attitudes. This allows the diabetes care and education specialist to individualize a plan that meets the needs of the person with diabetes and provide referrals to resources that address those factors that may not be directly addressed in DSMES. It is best that all potential participants are not funneled into a set program; classes based on a person-centered curriculum designed to address social determinants of health and self-determined goal setting can meet the varied needs of each person. Environment-related barriers include limited transportation services and inadequate offerings to meet the various cultural, language, and ethnic needs of the population. Additionally, these types of barriers include those related to social determinants of health—the economic, environmental, political, and social conditions in which one lives The health system may be limited in changing some of these conditions but needs to help each person navigate their situation to maximize their choices that affect their health. It is important to recognize that some individuals are less likely to attend DSMES services, including those who are older, male, nonwhite, less educated, of lower socioeconomic status, and with clinically greater disease severity 84 , Further, studies support the importance of cultural considerations in achieving successful outcomes 84 — Solutions include exploring community resources to address factors that affect health behaviors, providing seamless referral and access to such programs, and offering flexible programing that is affordable and engages persons from many backgrounds and living situations. The key is creating community-clinic partnerships that provide the right interventions, at the right time, in the right place, and using the right workforces Several common payment models and newer emerging models that reimburse for DSMES services are described below. For a list of diabetes education codes that can be submitted for reimbursement, see Supplementary Table 2 Billing codes to maximize return on investment ROI in diabetes care and education. CMS has reimbursed diabetes education services billed as diabetes self-management training since 40 , In order to meet the requirements, DSMES services must adhere to National Standards for Diabetes Self-Management Education and Support and meet the billing provider requirements 40 , Ten hours are available for the first year of receiving this benefit and 2 h in subsequent years. Any provider physician, nurse practitioner, PA who is the primary provider of diabetes treatment can make a referral; there is a copay to use these services. CMS also reimburses for diabetes MNT, which expands access to needed education and support. Three hours are available the first year of receiving this benefit and 2 h are available in subsequent years. A physician can request additional MNT hours through an MNT referral that describes why more hours are needed, such as a change in diagnosis, medical condition, or treatment plan. There are no specific limits set for additional hours. There is no copay or need to meet a Part B deductible in order to use these services. Many other payers also provide reimbursement for diabetes MNT Reimbursement by private payers is highly variable. Many will match CMS guidelines, and those who recognize the immediate and longer-term cost savings associated with DSMES will expand coverage, sometimes with no copay. With the transition to value-based health care, organizations may receive financial returns if they meet specified quality performance measures. Diabetes is typically part of a set of contracted quality measures impacting the payment model. Health systems should maximize the benefits of DSMES and factor them into the potential financial structure. There are reimbursable billing codes available for remote monitoring of blood glucose and other health parameters that are related to diabetes. The use of devices that can monitor glucose, blood pressure, weight, and sleep allow the health care team to review the data, provide intervention, and recommend treatment changes remotely. Sample referral forms that provide the information required by CMS and other payers for referral to DSMES and MNT are available along with reimbursement resources see Supplementary Tables 1 and 2. These or similar forms can be embedded into an electronic health record for easy referral. Health systems and clinical organizations can maximize billing potential by facilitating the reimbursement process, ensuring all applicable codes are being utilized and submitted appropriately. This usually requires support from those who frequently work with health care codes such as staff in billing and compliance departments. Shared medical appointments can be performed with DSMES and they are reimbursable medical visits. This Consensus Report is a resource for the entire health care team and describes the four critical times to refer to DSMES services with very specific recommendations for ensuring that all adults with diabetes receive these benefits. Diabetes is a complex condition that requires the person with diabetes to make numerous daily decisions regarding their self-management. DSMES delivered by qualified personnel using best practice methods has a profound effect on the ability to effectively undertake these responsibilities and is supported by strong evidence presented in this report. DSMES has a positive effect on clinical, psychosocial, and behavioral aspects of diabetes. DSMES provides the foundation with ongoing support to promote achievement of personal goals and influence optimal outcomes. Despite proven benefits and demonstrated value of DSMES, the number of people with diabetes who are referred to and receive DSMES is significantly low 73 — Barriers will not disappear without intentional, holistic interventions recognizing the roles of the entire health care team, individuals with diabetes, and systems in overcoming issues of therapeutic inertia The increasing prevalence of type 2 diabetes requires accountability by all stakeholders to ensure these important services are available and utilized. health care system has changed with increased attention on primary care, technology, and quality measures DSMES services that directly connect with primary care are effective in improving clinical, psychosocial, and behavioral outcomes 92 — A variety of culturally appropriate services need to be offered in a variety of settings, utilizing technology to facilitate access to DSMES services, support self-management decisions, and decrease therapeutic inertia. This article is being published simultaneously in Diabetes Care DOI: The authors would like to acknowledge Mindy Saraco Managing Director, Scientific and Medical Affairs from the ADA for her help with the development of the Consensus Report and related meetings and presentations, as well as the ADA Professional Practice Committee for providing valuable review and feedback. The authors acknowledge the invited peer reviewers who provided comments on an earlier draft of this report: Christine Beebe Quantumed Consulting, San Diego, CA , Anne L. Burns American Pharmacists Association, Alexandria, VA , Amy Butts Wheeling Hospital at the Wellsburg Clinic, Wellsburg, PA , Susan Chiarito Mission Primary Care Clinic, Vicksburg, MS , Maria Duarte-Gardea The University of Texas at El Paso, El Paso, TX , Joy A. Dugan Touro University California, Vallejo, CA , Paulina N. Duker Health Solutions Consultant, King of Prussia, PA , Lisa Hodgson Saratoga Hospital, Saratoga Springs, NY , Wahida Karmally Columbia University, New York, NY , Darlene Lawrence MedStar Health, Washington, DC , Anne Norman American Association of Nurse Practitioners, Austin, TX , Jim Owen American Pharmacists Association, Alexandria, VA , Diane Padden American Association of Nurse Practitioners, Austin, TX , Teresa Pearson Innovative Health Care Designs, LLC, Minneapolis, MN , Barb Schreiner Capella University, Pearland, TX , Eva M. Vivian University of Wisconsin, Madison, WI , and Gretchen Youssef MedStar Health, Washington, DC. Duality of Interest. is on an advisory board of Eli Lilly. is the treasurer for the American Academy of Nurse Practitioners Certification Board of Commissioners and Vice President of the American Nurse Practitioner Foundation. reports receiving an honorarium from ADA as an Education Recognition Program auditor and is a participant in a speakers bureau sponsored by Abbott Diabetes Care and Xeris. reports being a paid consultant of Diabetes — What to Know, Arkray, and DayTwo. reports being a participant in speakers bureaus sponsored by Boehringer Ingelheim, Novo Nordisk, and Xeris. reports research grant funding from Becton Dickinson. has received honoraria from ADA. No other potential conflicts of interest relevant to this article were reported. Author Contributions. All authors were responsible for drafting the article and revising it critically for important intellectual content. All authors approved the version to be published. Sign In or Create an Account. Search Dropdown Menu. header search search input Search input auto suggest. filter your search All Content All Journals Diabetes Care. Advanced Search. User Tools Dropdown. Sign In. Skip Nav Destination Close navigation menu Article navigation. Volume 43, Issue 7. Previous Article Next Article. Benefits Associated With DSMES. Providing DSMES. Four Critical Times to Refer to DSMES. Medical Nutrition Therapy as a Core Component of Quality Diabetes Care. Identifying and Addressing Barriers. Article Information. Article Navigation. Consensus Reports June 11 Powers ; Margaret A. Corresponding author: Margaret A. Powers, margaret. powers parknicollet. This Site. Google Scholar. Joan K. Bardsley ; Joan K. Marjorie Cypress ; Marjorie Cypress. Martha M. Funnell ; Martha M. Dixie Harms ; Dixie Harms. Amy Hess-Fischl ; Amy Hess-Fischl. Beulette Hooks ; Beulette Hooks. Diana Isaacs Diana Isaacs. Ellen D. Mandel ; Ellen D. Melinda D. Maryniuk ; Melinda D. Anna Norton ; Anna Norton. Joanne Rinker ; Joanne Rinker. Linda M. Siminerio Sacha Uelmen Sacha Uelmen. Diabetes Care ;43 7 — Get Permissions. toolbar search Search Dropdown Menu. toolbar search search input Search input auto suggest. Figure 1. View large Download slide. The four critical times to provide and modify diabetes self-management education and support. Table 1 DSMES Consensus Report recommendations. DSMES improves health outcomes, quality of life, and is cost effective, and people with diabetes deserve the right to DSMES services. Therefore, it is recommended that:. Discuss with all persons with diabetes the benefits and value of initial and ongoing DSMES. Ensure coordination of the medical nutrition therapy plan with the overall management strategy, including the DSMES plan, medications, and physical activity on an ongoing basis. Identify and address barriers affecting participation with DSMES services following referral. Expand awareness, access, and utilization of innovative and nontraditional DSMES services. Facilitate reimbursement processes and other means of financial support in consideration of cost savings related to the benefits of DSMES services. View Large. Table 2 Key definitions. This process incorporates the needs, goals, and life experiences of the person with diabetes. Note: Diabetes services and specialized providers and educators often provide both education and support. Yet on-going support from the primary health care team, family and friends, specialized home services, and the community are necessary to maximize implementation of needed self-management. Education is used in the National Standards for Diabetes Self-Management Education and Support and more commonly used in practice. In the context of this article, the terms have the same meaning. Clinical staff who qualify for this title may or may not be a CDCES or BC-ADM, yet all who hold the CDCES and BC-ADM certifications are diabetes care and education specialists. Note: The Certified Diabetes Educator CDE certification title is now CDCES. These forces and systems include economic policies and systems, development agendas, social norms, social policies, and political systems. Benefits rating. Table 4 Summary of DSMES benefits to discuss with people with diabetes 15 — 28 , 30 — 33 , 40 , Table 7 Sample questions to guide a person-centered assessment Table 5 Factors that indicate referral to DSMES services is needed. Table 6 Checklist for providing and modifying DSMES at four critical times. Four critical times. Table 8 Overview of MNT: an evidence-based application of the nutrition care process provided by the RDN 1 , 40 , 69 — Characteristics of MNT reducing A1C by 0. If they are not confident in these areas it is difficult to take advantage of the full impact of nutrition therapy. Implementation and assessment will drive confidence 2. American Diabetes Association. Facilitating behavior change and well-being to improve health outcomes: Standards of Medical Care in Diabetes— Search ADS. Management of hyperglycemia in type 2 diabetes, A consensus report by the American Diabetes Association ADA and the European Association for the Study of Diabetes EASD. Projection of the future diabetes burden in the United States through Classification and diagnosis of diabetes: Standards of Medical Care in Diabetes— Evaluation of the cascade of diabetes care in the United States, Overcoming therapeutic inertia [Internet]. Accessed 3 September Centers for Disease Control and Prevention. Social determinants of health [Internet], Accessed 30 March Diabetes self-management education and support in type 2 diabetes: a joint position statement of the American Diabetes Association, the American Association of Diabetes Educators, and the Academy of Nutrition and Dietetics. Group based diabetes self-management education compared to routine treatment for people with type 2 diabetes mellitus. A systematic review with meta-analysis. The effect of nurse-led diabetes self-management education on glycosylated hemoglobin and cardiovascular risk factors: a meta-analysis. Group based training for self-management strategies in people with type 2 diabetes mellitus. Diabetes self-management education for adults with type 2 diabetes mellitus: a systematic review of the effect on glycemic control. Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes UKPDS 35 : prospective observational study. Diabetes self-management education reduces risk of all-cause mortality in type 2 diabetes patients: a systematic review and meta-analysis. Structured type 1 diabetes education delivered within routine care: impact on glycemic control and diabetes-specific quality of life. Meta-analysis of quality of life outcomes following diabetes self-management training. Biologic and quality-of-life outcomes from the Mediterranean Lifestyle Program: a randomized clinical trial. Long-term outcomes from a multiple-risk-factor diabetes trial for Latinas: ¡Viva Bien! Lasting effects of a 2-year diabetes self-management support intervention: outcomes at 1-year follow-up. Facilitating healthy coping in patients with diabetes: a systematic review. Behavioral programs for type 2 diabetes mellitus: a systematic review and network meta-analysis. Nutritionist visits, diabetes classes, and hospitalization rates and charges: the Urban Diabetes Study. One-year outcomes of diabetes self-management training among Medicare beneficiaries newly diagnosed with diabetes. Inpatient diabetes education is associated with less frequent hospital readmission among patients with poor glycemic control. Inpatient diabetes education in the real world: an overview of guidelines and delivery models. Reasons why patients referred to diabetes education programmes choose not to attend: a systematic review. A systematic review of reviews evaluating technology-enabled diabetes self-management education and support. The diabetes online community: older adults supporting self-care through peer health. State of the science: a scoping review and gap analysis of diabetes online communities. A diabetes education model in primary care: provider and staff perspectives. Multidisciplinary management of type 2 diabetes in children and adolescents. Self-management education for adults with type 2 diabetes: a meta-analysis of the effect on glycemic control. Comparative effectiveness of peer leaders and community health workers in diabetes self-management support: results of a randomized controlled trial. Impact of peer health coaching on glycemic control in low-income patients with diabetes: a randomized controlled trial. Peer-based behavioural strategies to improve chronic disease self-management and clinical outcomes: evidence, logistics, evaluation considerations and needs for future research. Overview of peer support models to improve diabetes self-management and clinical outcomes. Kovacs Burns. Diabetes Attitudes Wishes and Needs 2 DAWN2 : a multinational, multi-stakeholder study of psychosocial issues in diabetes and person-centred diabetes care. Diabetes distress and glycemic control: the buffering effect of autonomy support from important family members and friends. The role of the family in supporting the self-management of chronic conditions: A qualitative systematic review. American Association of Diabetes Educators. An effective model of diabetes care and education: revising the AADE7 Self-Care Behaviors ®. Personalised care planning for adults with chronic or long-term health conditions. The Diabetes Attitudes, Wishes, and Needs DAWN program: a new approach to improving outcomes of diabetes care. Comprehensive medical evaluation and assessment of comorbidities: Standards of Medical Care in Diabetes— Barriers and facilitators to self-care communication during medical appointments in the United States for adults with type 2 diabetes. AADE Practice Paper in Brief: Diabetes educators play a critical role in successful insulin management. Psychosocial care for people with diabetes: a position statement of the American Diabetes Association. Psychosocial problems and barriers to improved diabetes management: results of the Cross-National Diabetes Attitudes, Wishes and Needs DAWN Study. The prevalence of diabetes-specific emotional distress in people with type 2 diabetes: a systematic review and meta-analysis. Academy of Nutrition and Dietetics nutrition practice guideline for type 1 and type 2 diabetes in adults: systematic review of evidence for medical nutrition therapy effectiveness and recommendations for integration into the nutrition care process. Nutrition therapy for adults with diabetes or prediabetes: a consensus report. Diabetes self-management education and medical nutrition therapy improve patient outcomes: a pilot study documenting the efficacy of registered dietitian nutritionist interventions through retrospective chart review. Briggs Early. Position of the Academy of Nutrition and Dietetics: The role of medical nutrition therapy and registered dietitian nutritionists in the prevention and treatment of prediabetes and type 2 diabetes. Diabetes self-management education and training among privately insured persons with newly diagnosed diabetes—United States, The diabetes educator and the Diabetes Self-Management Education National Practice Survey. Exploring organizational support for the provision of structured self-management education for people with type 2 diabetes: findings from a qualitative study. Diabetes Self-Management Education and Support DSMES Toolkit [Internet], Access to diabetes self-management education: results of national surveys of patients, educators, and physicians. Barriers to attendance at diabetes education centres: perceptions of education providers. Researchers behind one study found that engaging in a structured exercise program for at least 8 weeks lowered glycated hemoglobin levels by an average of 0. The ADA recommend exercising for at least 10 minutes per session and getting a total of at least 30 minutes of exercise on most days of the week. If a person exercises every day — or lets no more than 2 days pass between workouts — this may help reduce insulin resistance. Members of a diabetes healthcare team can help develop and tailor an exercise plan that is safe and effective. In addition to exercising regularly, it is important to avoid spending long periods in a seated position. Breaking up sedentary periods every 30 minutes can help with controlling blood sugar. The ADA advise all people with prediabetes or diabetes to avoid tobacco products, including e-cigarettes. People with diabetes who smoke have higher risks of cardiovascular disease , premature death, and diabetes complications , as well as less blood sugar control, compared with people who do not smoke. If a person with diabetes does not take their medication as recommended by a doctor, it can lead to:. A diverse range of issues can contribute to medication nonadherence. Some may relate to psychological, demographic, and social factors. Key elements can include the cost of treatment and difficulties with healthcare providers and the healthcare system. Doubt about the seriousness of diabetes and the effectiveness of a treatment plan can keep a person from taking their medication, and this can lead to complications. Nonadherence seems to be more common among people who have chronic diseases with symptoms that are not obvious. Also, complex treatment plans can be challenging to follow. The quality of the patient-doctor relationship is often a key factor in nonadherence. Likewise, it is important to raise concerns about diabetes treatment with the doctor, who can adjust the plan to help ensure that targets are being met and no complications develop. Researchers have estimated that the collective cost of medication nonadherence for diabetes, high blood pressure , and high cholesterol in the U. Diabetes is not curable, but a person can help manage it at home. This often involves following nutrition and medication plans. A person with diabetes or prediabetes should also be physically active and maintain a healthy weight. A diabetes care team can help develop and tailor an exercise plan. Blood glucose meters and continuous glucose monitors can help a person track their progress and see the effects of self-management techniques. Read this article in Spanish. Some people can control type 2 diabetes without medication. Learn what factors help maintain healthy blood sugar levels and when someone may need…. Several factors increase a person's risk of developing type 2 diabetes. In this article, learn about how to prevent the condition by losing weight…. Diabetes management includes artificial insulin and lifestyle adjustments. Read on to learn more. Although it is not always possible to prevent gestational diabetes, eating well and exercising regularly to achieve or maintain a healthy weight can…. What are some of the ways that diabetes may develop? Read on to learn more about the different types of diabetes and their potential causes. My podcast changed me Can 'biological race' explain disparities in health? Why Parkinson's research is zooming in on the gut Tools General Health Drugs A-Z Health Hubs Health Tools Find a Doctor BMI Calculators and Charts Blood Pressure Chart: Ranges and Guide Breast Cancer: Self-Examination Guide Sleep Calculator Quizzes RA Myths vs Facts Type 2 Diabetes: Managing Blood Sugar Ankylosing Spondylitis Pain: Fact or Fiction Connect About Medical News Today Who We Are Our Editorial Process Content Integrity Conscious Language Newsletters Sign Up Follow Us. Medical News Today. Health Conditions Health Products Discover Tools Connect. Human Biology. Nervous system Cardiovascular system Respiratory system Digestive system Immune system. How to manage diabetes. Medically reviewed by Maria Prelipcean, M. Self-monitoring Healthy weight Nutrition Exercise Stop smoking Take medication regularly Takeaway While there is no cure for diabetes, with treatment and self-management strategies, a person can live a long and healthy life. Share on Pinterest People can self-monitor their diabetes with a blood glucose meter. Maintain a healthy weight. Get good nutrition. Exercise regularly. Share on Pinterest Regular exercise may help control blood sugar levels. Stop smoking. Take medication regularly. Share on Pinterest A person should take their diabetes medication as prescribed to prevent further complications. How we reviewed this article: Sources. Medical News Today has strict sourcing guidelines and draws only from peer-reviewed studies, academic research institutions, and medical journals and associations. |
Sie lassen den Fehler zu. Geben Sie wir werden es besprechen.
Sie sind nicht recht. Ich kann die Position verteidigen. Schreiben Sie mir in PM, wir werden reden.
Ich entschuldige mich, aber meiner Meinung nach lassen Sie den Fehler zu. Es ich kann beweisen. Schreiben Sie mir in PM, wir werden reden.
Bemerkenswert, es ist das wertvolle Stück