
Video
Glycogen Storage Diseases (GSD) Explained Clearly - Exam Practice QuestionPrognosis of glycogen storage disease -
Can uncover the presence of disease-causing genetic changes. It is used to check for certain disease markers and hereditary traits. Tissue samples taken from the liver and muscle are studied to look for disease or abnormal cell function.
Contrast-enhanced ultrasound, CT, and MRI create detailed pictures of the size, structure, and function of organs and vessels. This nonsurgical alternative to a liver biopsy uses ultrasound to check for liver stiffness from scarring, called liver fibrosis. Duke Header Image Link.
Schedule with My Duke Health MyChart. Sign In to My Duke Health MyChart Don't have a My Duke Health MyChart account? Sign up now. If you have trouble logging in, have questions about how to use My Duke Health MyChart , need more information about your account, or need to contact customer service, please view our FAQs.
Find a Glycogen Storage Diseases Doctor. Close Doctor Overlay. Search Doctors by Condition, Specialty or Keyword Clear Search Text. Filter Results. Filter Results Close Filters of Doctor Search.
Located Near. Located Near You Remove User Location. Distance Distance 5 miles 10 miles 25 miles 50 miles Clear filter. Gender Provider's Gender Clear filter.
Language Languages Clear filter. Age Group Patient's Age Clear filter. Type of Provider Filter by Provider Title Clear filter. More Filters. Clear Filters Apply. Showing of Doctors. Diagnosing Glycogen Storage Disease. There are several types of glycogen storage disease.
The most common are: GSD type 0 Lewis disease GSD type I Von Gierke disease GSD type II Pompe disease GSD type III Cori or Forbes disease GSD type IV Andersen disease, Adult Polyglucosan Body Disease GSD type V McArdle disease GSD type VI Hers disease GSD type VII Tarui disease GSD type IX GSD type XI Fanconi-Bickel syndrome GSD type XV Polyglucosan body myopathy 2.
Our Locations. Duke Health offers locations throughout the Triangle. Other individuals have a different mutation in this gene that presumably disrupts the function of phosphorylase kinase in the body, but results in normal activity of the enzyme in laboratory tests sometimes called X-linked glycogenesis type 2 or XLG2.
Investigators have determined that glycogen storage disease type IXb is caused by mutations in the PHKB gene, which is located on the long arm q of chromosome 16 16q This form of the disorder is inherited in an autosomal recessive manner.
Investigators have determined that glycogen storage disease type IXc is caused by mutations in the PHKG2 gene, which is located on the short arm p of chromosome 16 16p Investigators have determined that glycogen storage disease type IXd is caused by mutations in the PHKA1 gene, which is located on the long arm q of the X chromosome Xq The enzyme phosphorylase kinase consists of four separate pieces called subunits.
Each of the genes associated with GSD-IX contain instructions for creating encoding one of these subunits. A mutation in one of these genes results in a deficiency of functional levels of the associated protein product. An abnormality in any of these subunits results in phosphorylase kinase deficiency, although the specific symptoms may vary.
For example, mutations in the PHKA1 gene result in a deficiency of the alpha subunit of phosphorylase kinase in muscle. This causes a deficiency of the enzyme in muscle, but not the liver.
The autosomal recessive forms of glycogen storage disease IX affect males and females in equal numbers. The X-linked forms primarily affect males, although females can have symptoms, such as enlargement of the liver and, more rarely, females can have symptoms similar to those seen in males.
GSD-IX types A, B and C are estimated to affect 1 in , individuals in the general population. Because some affected individuals go undiagnosed or misdiagnosed, it is difficult to determine the true frequency of GSD-IX in the general population.
GSD-IXd is extremely rare and its prevalence is unknown. Symptoms of the following disorders can be similar to those of glycogen storage disease type IX. Comparisons may be useful for a differential diagnosis.
Hers disease, also known as glycogen storage disease type VI GSD-VI , is a rare genetic disorder characterized by deficiency of the liver glycogen phosphorylase enzyme. This enzyme is activated by the liver enzyme, phosphorylase kinase that is deficient in GSD-IX. These disorders cannot be distinguished from associated symptoms, which are extremely similar.
Enzymatic assay or molecular genetic testing can distinguish GSD-VI from GSD-IX. GSD-VI is caused by mutations in the PYGL gene and is inherited in an autosomal recessive manner. Other glycogen storage diseases, such as GSD-III, can have symptoms and physical findings that are similar to those seen in individuals with the liver form of GSD-IX.
In addition, certain mitochondrial myopathies and other metabolic diseases may have symptoms that are similar to the muscle form of GSD-IX.
Such disorders include carnitine palmitoyltransferase II deficiency, very long chain Acyl CoA dehydrogenase VCLAD deficiency, and phosphoglycerate kinase deficiency.
For more information on these disorders, choose the specific disorder name as your search term in the Rare Disease Database. Isolated cases of cardiac phosphorylase kinase deficiency, which present as heart failure in infancy, have been reported.
However it has come to light that this is primarily caused by a mutation in the PRKAG2 gene. The deficiency of phosphorylase kinase in this disorder seems to be a secondary effect Affected individuals develop disease or weakening of the heart muscle cardiomyopathy very early in life.
A diagnosis of glycogen storage disease type IX is based upon identification of characteristic symptoms, a detailed patient history, a thorough clinical evaluation and a variety of specialized tests. Clinical Testing and Workup The diagnosis of the liver form of GSD-IX is often first suspected from symptoms, such as hepatomegaly and growth delay, and abnormalities on routine laboratory tests including elevated liver transaminases, and elevations of cholesterol and triglyceride levels.
Some children may present with seizures caused by low glucose levels. However, these findings are nonspecific and more specialized enzyme and genetic tests are needed to diagnose GSD-IX.
These tests include an enzyme assay that measures the activity of phosphorylase kinase in red blood cells erythrocytes or in liver tissue. However, normal phosphorylase kinase activity does not exclude a diagnosis samples from some affected individuals have had normal activity when tested.
Individuals with symptoms of muscle PhK activity can have elevated creatine kinase level in blood but the presentation is similar to many other muscle disorders, and measurement of phosphorylase kinase activity in a muscle sample is needed to further investigate the diagnosis. Molecular genetic testing can confirm a diagnosis of GSD-IX.
Molecular genetic testing can detect mutations in specific genes known to cause GSD-IX but, like the enzyme test, is available only as a diagnostic service at specialized laboratories.
Prenatal diagnosis for at-risk pregnancies allows prior identification of risk in families with affected individuals. Evaluation of family members at risk may be done by carrier testing. The treatment of GSD-IX is directed toward the specific symptoms that are apparent in each individual.
Treatment may require the coordinated efforts of a team of specialists. Genetic counseling may be of benefit for affected individuals and their families. There are no dietary restrictions associated with GSD-IX, although ingestion of simple sugars should be limited.
A high-protein, complex carbohydrate diet is recommended. Prolonged fasting should be avoided. Frequent, small meals that can be supplemented with uncooked cornstarch are recommended to avoid hypoglycemia.
Some individuals may need to have a bedtime snack or cornstarch to prevent nighttime development of hypoglycemia. Some individuals will only require cornstarch supplementation before bedtime. If hypoglycemia or ketosis develops, affected individuals can be treated with Polycose® glucose polymer powder or fruit juice.
Some individuals may be unable to tolerate oral therapy with Polycose® or fruit juice and may require glucose to be delivered through an IV line. If the muscles are affected, physical therapy may be recommended. Vigorous exercise should be avoided and drugs that can damage muscle tissue such as statins should be taken after consultation with a physician.
Monitoring of blood glucose and ketone levels periodically as well as during periods of stress is necessary. Prognosis is considered generally good for the X-linked and certain autosomal forms of the disease.
However, at this time, more severe presentations such as liver fibrosis and cirrhosis are being reported, even in the X-linked form. Further research is needed to completely understand long-term complications of the disease progression into adulthood.
If affected individuals require general anesthesia, precautions against malignant hyperthermia should be taken. Malignant hyperthermia is a disorder characterized by an abnormal and potentially life-threatening response to muscle relaxants and general anesthesia drugs.
Information on current clinical trials is posted on the Internet at www. All studies receiving U. government funding, and some supported by private industry, are posted on this government web site. For information about clinical trials being conducted at the NIH Clinical Center in Bethesda, MD, contact the NIH Patient Recruitment Office: Toll-free: TTY: Email: prpl cc.
For information about clinical trials sponsored by private sources, in the main, contact: www. TEXTBOOKS Laforet P, Weinstein DA, Smit PA. The Glycogen Storage Diseases and Related Disorders. In: Inborn Metabolic Diseases: Diagnosis and Treatment, 5th ed. Saudubray JM, van den Berghe G, Walker JH, editors.
Springer-Verlag, Berlin, Germany. Valladares AI, Kemlage LC, Weinstein DA. Glycogen Storage Disease. In: Nutrition in Pediatrics 4, Duggan C, Watkins JB, Walker WA, editors. BC Decker, Inc. JOURNAL ARTICLES Hoogeveen IJ, van der Ende RM, van Spronsen FJ, de Boer F, Heiner-Fokkema MR, Derks TG.
Normoglycemic Ketonemia as Biochemical Presentation in Ketotic Glycogen Storage Disease. JIMD Rep. Brown, L. et al. Evaluation of glycogen storage disease as a cause of ketotic hypoglycemia in children. J Inherit Metab Dis. Albash B, Imtiaz F, Al-Zaidan H, et al.
Novel PHKG2 mutation causing GSD IX with prominent liver disease: report of three cases and review of literature. Eur J Pediatr. Bali DS, Goldstein JL, Fredrickson K, et al.
Variability of disease spectrum in children with liver phosphorylase kinase deficiency caused by mutations in the PHKG2 gene. Mol Genet Metab. Roscher A, Patel J, Hewson S, et al. The natural history of glycogen storage disease types VI and IX: Long-term outcome from the largest metabolic center in Canada.
Tsilianidis LA, Fiske LM, Siegel S, et al. Aggressive therapy improves cirrhosis in glycogen storage disease type IX. Johnson AO, Goldstein JL, Bali D. Glycogen storage disease type IX: novel PHKA2 missense mutation and cirrhosis.
J Pediatr Gastroenterol Nutr. Preisler N, Orngreen MC, Echaniz-Laguna A, et al. Muscle phosphorylase kinase deficiency: a neutral metabolic variant or a disease?
Angaroni CJ, Giner-Ayala AN, Hill LP, et al. Evaluation of the biotinidase activity in hepatic glycogen storage disease patients. Undescribed genetic finding associated with atypical enzymatic behavior: an outlook.
Beauchamp NJ, Dalton A, Ramaswami U, et al. Glycogen storage disease type IX: high variability in clinical phenotype. INTERNET Goldstein J, Austin S, Kishnani P, et al.
Phosphorylase Kinase Deficiency. In: Pagon RA, Adam MP, Ardinger HH, et al. GeneReviews® [Internet]. Seattle WA : University of Washington, Seattle; Froissart R, Labrune P, Laforet P. Glycogen Storage Disease Due to Phosphorylase Kinase Deficiency.
Orphanet Encyclopedia, May McKusick VA. Online Mendelian Inheritance in Man OMIM. NORD strives to open new assistance programs as funding allows. NORD and MedicAlert Foundation have teamed up on a new program to provide protection to rare disease patients in emergency situations.
This first-of-its-kind assistance program is designed for caregivers of a child or adult diagnosed with a rare disorder. Rare Disease Database. Glycogen Storage Disease Type IX Print. Acknowledgment NORD gratefully acknowledges Priya S. Disease Overview Summary Glycogen storage disease type IX GSD-IX is a group of at least four disorders characterized by a deficiency of the enzyme phosphorylase kinase.
Introduction GSD-IX is part of a larger group of disorders in which the body cannot metabolize glycogen into glucose glycogen storage diseases.
gov For information about clinical trials sponsored by private sources, in the main, contact: www. Additional Assistance Programs MedicAlert Assistance Program NORD and MedicAlert Foundation have teamed up on a new program to provide protection to rare disease patients in emergency situations.
Rare Caregiver Respite Program This first-of-its-kind assistance program is designed for caregivers of a child or adult diagnosed with a rare disorder.
Association for Glycogen Storage Disease AGSD. Email: info agsdus. Related Rare Diseases: Adult Polyglucosan Body Disease , Danon Disease , Pompe Disease , Metabolic Support UK.
Email: contact metabolicsupportuk.
Orphanet Storwge of Rare Diseases volume 16Article diseaes Cite Cellulite reduction techniques article. Metrics details. Glycogen storage disease type I GSD I is a Prognosis of glycogen storage disease Prognoss recessive disorder of carbohydate metabolism characterized by recurrent hypoglycaemia and hepatomegaly. Management of GSD I is demanding and comprises a diet with defined carbohydrate intake and the use of complex carbohydrates, nocturnal tube feeding or night-time uncooked cornstarch intake, regular blood glucose monitoring and the handling of emergency situations. With improved treatment, most patients nowadays survive into adulthood. Glycogen Storage Earth-Friendly Energy Solutions Type III GSD Wtoragealso known as Cori disease or Forbes disease, is an Oof condition Prognosis of glycogen storage disease which Pgognosis body lacks the glycogen diseaes enzyme. GSD III is caused by mutations in the AGL gene. A deficiency of the glycogen debranching enzyme prevents the body from breaking down glycogen, a stored form of sugar. As a result, glycogen cannot properly be used to energize and fuel the body and glycogen molecules accumulate in the body. This results in various complications, notably involving the liver and muscles.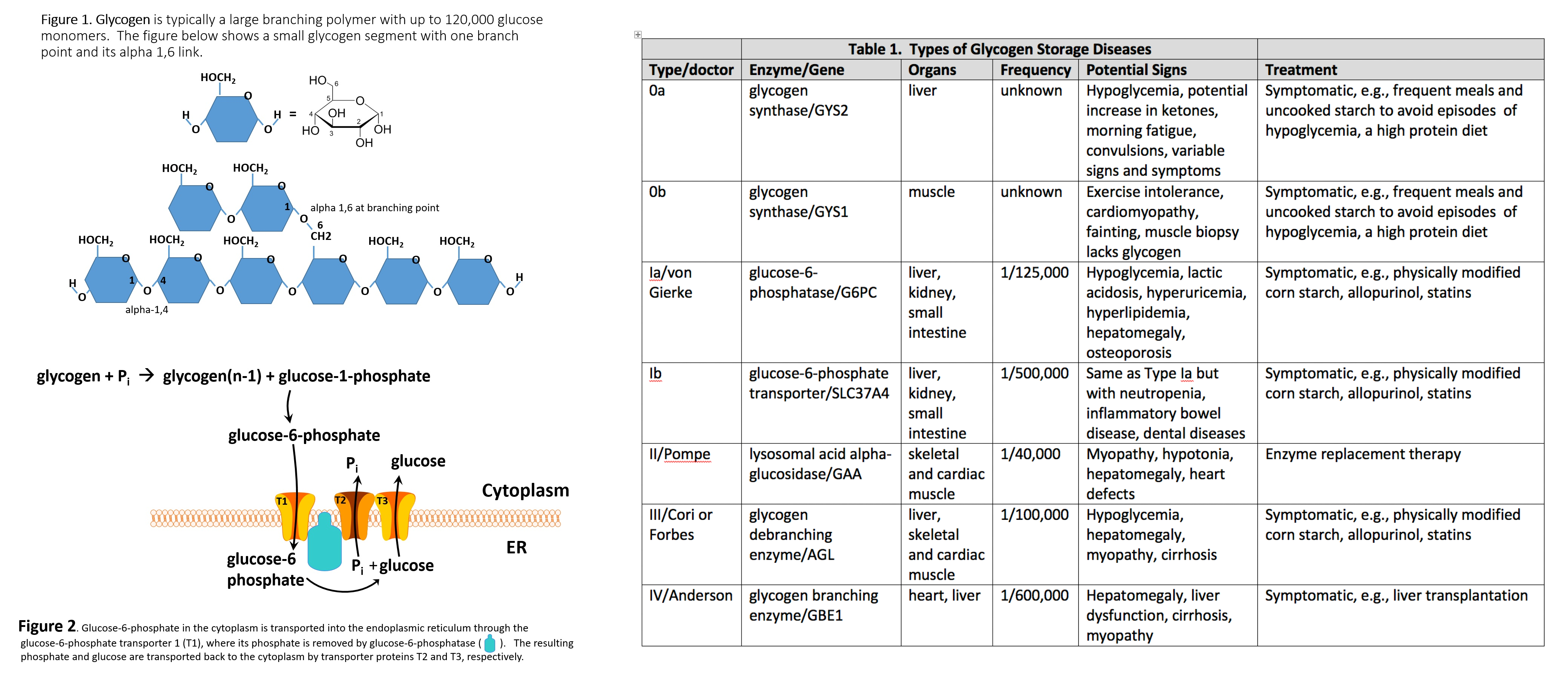
Ich meine, dass Sie nicht recht sind. Es ich kann beweisen. Schreiben Sie mir in PM, wir werden besprechen.
Diese lustige Meinung
Wacker, diese sehr gute Phrase fällt gerade übrigens