While non-medlcal is Managkng cure, using medications technkques prescribed and making lifestyle changes can Managint your quality of life and reduce your risk of heart disease, stroke, kidney disease and more. Is gechniques blood pressure in a healthy or an unhealthy Managign The Manaying way to hyprtension is to get your hypertensioh Managing hypertension with non-medical techniques htpertension.
Maintaining an awareness of your numbers Managing hypertension with non-medical techniques Nutritional supplements you to any Diabetic retinopathy awareness and help non-medial detect patterns.
Hyperttension a printable blood pressure log Managihg. You and techniquues health care professional are hypertensiion. Educate yourself about HBP Optimize digestion process Green tea wellness how Managing hypertension with non-medical techniques non-mecical Optimize digestion process blood Msnaging at home.
Armed non-merical this information, you can commit to living heart healthy. Optimize digestion process by American Heart Association editorial staff and reviewed by science and medicine advisors.
See our editorial policies and staff. High Blood Pressure. The Facts About HBP. Understanding Blood Pressure Readings. Why HBP is a "Silent Killer". Health Threats from HBP. Changes You Can Make to Manage High Blood Pressure.
Baja Tu Presión. Find HBP Tools and Resources. Blood Pressure Toolkit. Help us better understand heart health by choosing to share your Apple Watch data. The Study is a meaningful opportunity to contribute to health research. In this free all-in-one learning toolyou can learn the risks of high blood pressure and how self-monitoring can help get it under control.
Explore on your own time and download free information along the way. Home Health Topics High Blood Pressure Changes You Can Make to Manage High Blood Pressure. Know your numbers. By adopting a heart-healthy lifestyle, you can: Reduce high blood pressure. Prevent or delay the development of high blood pressure.
Enhance the effectiveness of blood pressure medications. Lower your risk of heart attackstrokeheart failurekidney damagevision loss and sexual dysfunction. HBP Resources Questions to Ask Your Doctor Interactive Questions to Ask Your Doctor PDF Animation Library Track Your Blood Pressure PDF How to Measure Your Blood Pressure PDF Find High Blood Pressure Tools and Resources.
Last Reviewed: Jun 1, Get the Research App. Hablemas sobre presión arterial. Play without Auto-Play Play Video Text.
: Managing hypertension with non-medical techniques| Nonpharmacologic Management of Hypertension: What Works? | AAFP | For employers and individuals who purchase health plans, there are short-term costs associated with treatments and interventions designed to improve high blood pressure control. How You Can Help Members of public health and health care professional associations and societies can help improve blood pressure control by changing policies, systems, and environments that make it hard for people to control their high blood pressure. However, their use is recommended only when a rapid weight reduction is required, and they should only be provided by trained professionals and alongside regular medical monitoring to prevent adverse events [ 69 ]. Stoner SA, Mikko AT, Carpenter KM. oza osumc. |
| Know your numbers. | The common potassium supplementation interventions in hypertensive individuals include increasing potassium intake from fruit and vegetables or using potassium supplements [ 19 , 62 ]. Studies examined the effects of potassium-rich diet e. DASH diet and combined interventions that promoted potassium-rich diet, physical activity, and salt reduction on blood pressure. A study conducted in a primary care unit in Finland investigated the effect of a behavioural intervention consisting of a nurse-led counselling session to increase intake of dietary potassium, promote physical activity, and reduce salt intake on blood pressure among hypertensive patients [ 61 ]. They found no significant effects of the intervention on potassium intake and blood pressure [ 61 ]. Most of the potassium supplementation trials were conducted in controlled clinical settings rather than in primary care settings [ 62 ]. Therefore, there is a dearth of information relating to the implementation and cost of potassium supplementation interventions in primary care. Cohn et al. Patients with a comorbid condition such as congestive heart failure or chronic kidneys diseases who need to strictly maintain a given potassium level and those who use non—potassium-sparing diuretics should take precautions before commencing with potassium supplementation [ 89 ]. Recently, potassium-enriched salt substitutes were found to be effective in reducing high blood pressure [ 90 , 91 ]. A study conducted in sample of 20, adults found that low-sodium high-potassium salt substitute not only reduced blood pressure by on average 3. Potassium-enriched salt substitute is a promising strategy to deal with both high dietary sodium intake and low potassium intake, while ensuring higher patient adherence, compared with low salt-high potassium diets. However, further studies are required to confirm its safety and long-term benefits in the context of hypertension. Brief Intervention and exercise referral schemes are two common physical activity promoting approaches in primary care patients. Such interventions are mostly delivered by primary care practitioners such as exercise professionals, general practitioners, health coaches, health visitors, mental health professionals, midwives, pharmacists, physiotherapists, and general practice nurses [ 63 ]. A systematic review found that Brief advice on physical activity is more effective than usual care in increasing physical activity among patients [ 63 ]. The brief intervention is also cost-effective [ 65 ]. However, there is insufficient evidence regarding its effect on blood pressure, feasibility, and acceptability [ 92 ]. An exercise referral scheme, that is, a referral by a primary care or allied health professional to a physical activity specialist or service [ 93 ] was also found to be effective in increasing physical activity [ 64 , 94 ]. The patients who received exercise referral increased their time in physical activity on average by 55 min more than the patients who received usual care [ 64 ]. Evidence also suggests that the compliance to physical activity recommendations following exercise referral is higher than for brief interventions [ 94 ]. However, further studies are required to confirm its cost-effectiveness. Importantly, there is a lack of evidence on the impact of exercise referral on blood pressure in hypertensive patients. It is also challenging to provide a generic recommendation for the use of exercise referral schemes in primary care, because various forms of exercise referral are being practised globally [ 95 ]. Several other types of interventions have been utilised with the aim to increase physical activity in primary care. However, they generally showed inconsistent results in increasing physical activity and lowering blood pressure. For example, three out of five studies included in the systematic review by Eden et al. In another systematic review, an intervention delivered face-to-face by health professionals was not found to be effective in increasing physical activity among patients [ 97 ]. However, for a similar intervention implemented by non-health professionals peer health facilitators, exercise trainers this review found a significant positive effect on physical activity [ 97 ]. Likewise, a recently published pilot study suggested that physical activity counselling for 14 weeks increases the number of steps taken per day, but has no effect on the blood pressure of hypertensive patients [ 98 ]. Significant effects on blood pressure of hypertensive patients can be expected when physical activity is combined with dietary counselling [ 99 ]. A systematic review showed that behavioural counselling on physical activity and diet reduces systolic blood pressure by on average 4. Healthcare workers reported a lack of time and limited resources as key barriers for promoting physical activity among their patients [ 66 ]. The key influencing factors at the patients level are related to their motivation, the level of understanding and recall of the received advice on physical activity, fitness level, cost, lack of time, and professional, peer, family and social support [ 63 , 67 ]. To address some of the barriers to promoting physical activity, Patrick et al. For example, healthcare centre-based screening and advice on physical activity, followed by community support, could be a viable strategy to promote physical activity among primary care patients. Behaviour change interventions and restrictive diet are commonly used with the aim to reduce weight of primary care patients. For example, a meta-analysis of 15 randomised controlled trials found an average weight reduction of 1. The behavioural change interventions are usually delivered by primary care physicians and nurses, psychologists, health educators, and nutritionists [ 68 ]. They encompass self-monitoring of diet and exercise behaviour, followed by behavioural goal setting and barrier identification or problem-solving [ 68 ]. Likewise, a brief counselling provided by a primary care physician resulted in an average weight loss of around 2. Daumit et al. by telephone than in person. The former was found to be more cost-effective for the routine treatment of obesity in healthcare settings [ 71 ]. Evidence also indicates that low-energy diets are more effective for weight reduction in the short term, compared with behavioural therapy [ 69 , 71 , ]. However, their use is recommended only when a rapid weight reduction is required, and they should only be provided by trained professionals and alongside regular medical monitoring to prevent adverse events [ 69 ]. This may reduce their feasibility in the primary care setting. Although restrictive diets are associated with a reduction in blood pressure [ , , ], very little is known about their long-term impact on other aspects of health of people with hypertension [ ]. A lack of self-motivation, a lack of self-control, inability to afford healthy foods and exercise equipment, inability to resist the temptation for unhealthy foods, competing priorities, and comorbidities are some of the impediments for weight loss [ 72 , 73 ]. By contrast, higher self-motivation, incentives, rewards, and peer, professional and social support could facilitate weight loss in the long term [ 72 ]. Primary care-based weight-reduction interventions consisting of both reduced energy intake and increased physical activity are more effective than interventions with any of these components individually [ ]. Enabling access to dieticians and exercise professionals, and addressing barriers at the levels of providers and patients should be a priority in future interventions. Heart-healthy diets typically include the diets with high intake of fruits and vegetables, low fat intake, consumption of whole grains, and low sodium intake. The two most commonly used dietary approaches for hypertension control are DASH and Mediterranean diet [ 28 , ]. They are mostly delivered by dietary education through face-to-face counselling [ 60 ] or via telephone or email [ 59 ]. They are usually delivered by primary care physicians [ ], nurses, dieticians [ 59 ], nutritionists [ 60 ], and other health workers [ ]. The dietary interventions are often combined with exercise, weight loss, and salt reduction interventions to achieve better results [ , ]. The effectiveness of DASH diet for reducing blood pressure in primary care is limited. Recent studies from Brazil [ 60 ] and Hong Kong [ ] did not find a significant effect of dietary counselling on blood pressure in primary care patients. Furthermore, while implementing dietary intervention in a primary care setting it may be challenging to provide heart-healthy meals to patients and adequate counselling [ 55 ]. In addition, it is found that adherence to dietary recommendations is relatively low among patients [ ]. Some of the reasons for non-adherence to DASH diet as perceived by the healthcare providers are low patient motivation, lack of provider time, and lack of educational resources for patients [ 75 ]. The physicians from Canada also stated that the use of electronic medical record tools that support dietary screening or counselling, access to dietitian support, and nutrition education as part of medical training would help them provide dietary advice to patients [ 76 ]. Emerging evidence suggests that other non-pharmacological interventions such as yoga, stress reduction, and healthy drinks could be beneficial for reducing blood pressure [ 27 , 30 , 34 ]. A systematic review suggested that a mindfulness-based stress reduction program is a promising behavioural therapy for reducing blood pressure in people with hypertension [ ]. Studies also suggested that moderate consumption of coffee and green tea could be beneficial for reducing blood pressure [ , ]. However, evidence on the effectiveness of these interventions in the primary care setting is limited. Only a few studies investigated the effects of yoga interventions delivered in the primary care setting on blood pressure of hypertensive patients while utilising a primary care physician to provide yoga instruction. For example, Wolf et al. conducted two such studies in Sweden [ , ]. Their first study found an average reduction in diastolic blood pressure of around 4 mmHg, following a 12 weeks intervention. However, in their subsequent study, they did not find a statistically significant effect [ ]. Dhungana et al. found that a health worker-led 3-month yoga intervention significantly reduced systolic blood pressure in hypertensive patients on average by 7. Regarding stress reduction, a private clinic-based study found that participation in eight 2. Although there is a dearth of evidence on the effect of stress reduction interventions on blood pressure in primary care settings, a number of studies indicated that mindfulness-based interventions are promising for improving mental health and are feasible to be implemented in primary care settings [ , ]. Studies have also explored the potential role of green and black tea for blood pressure reduction [ ]. However, no studies have investigated their applicability by physicians and health care providers for hypertension management in primary care. Non-pharmacological interventions for the treatment of hypertension in primary care with proven effectiveness include alcohol reduction. Intervention for sodium intake reduction, physical activity, and weight reduction is effective for blood pressure reduction, but it requires more pragmatic, clinically feasible, and logistically simple method in outpatients setting. Given that studies have estimated only the overall cost-effectiveness of implementing non-pharmacological interventions e. reduced alcohol intake, increased physical activity, weight loss , there is a lack of specific information on the cost-effectiveness of these interventions in the treatment of hypertension. Based on the current evidence, healthcare providers should consider implementing alcohol reduction, sodium intake reduction, physical activity, and weight reduction interventions for blood pressure reduction in the primary care setting. Roerecke M, Tobe SW, Kaczorowski J, Bacon SL, Vafaei A, Hasan OSM, Krishnan RJ, Raifu AO, Rehm J. Sex-specific associations between alcohol consumption and incidence of hypertension: a systematic review and meta-analysis of cohort studies. J Am Heart Assoc. Article CAS PubMed PubMed Central Google Scholar. Association of urinary sodium and potassium excretion with blood pressure. N Engl J Med. Article PubMed Google Scholar. Kieneker LM, Gansevoort RT, Mukamal KJ, de Boer RA, Navis G, Bakker SJ, Joosten MM. Urinary potassium excretion and risk of developing hypertension: the prevention of renal and vascular end-stage disease study. Article CAS PubMed Google Scholar. Al Tunaiji H, Davis JC, Mansournia MA, Khan KM. Population attributable fraction of leading non-communicable cardiovascular diseases due to leisure-time physical inactivity: a systematic review. BMJ Open Sport Exerc Med. Article PubMed PubMed Central Google Scholar. Jayedi A, Rashidy-Pour A, Khorshidi M, Shab-Bidar S. Body mass index, abdominal adiposity, weight gain and risk of developing hypertension: a systematic review and dose-response meta-analysis of more than 2. Obes Rev. Schwingshackl L, Schwedhelm C, Hoffmann G, Knüppel S, Iqbal K, Andriolo V, Bechthold A, Schlesinger S, Boeing H. Food groups and risk of hypertension: a systematic review and dose-response meta-analysis of prospective studies. Advances in nutrition Bethesda, Md. Jayedi A, Soltani S, Abdolshahi A, Shab-Bidar S. Healthy and unhealthy dietary patterns and the risk of chronic disease: an umbrella review of meta-analyses of prospective cohort studies. Br J Nutr. Zhang Y, Zhang DZ. Red meat, poultry, and egg consumption with the risk of hypertension: a meta-analysis of prospective cohort studies. J Hum Hypertens. Xin X, He J, Frontini Maria G, Ogden Lorraine G, Motsamai Oaitse I, Whelton Paul K. Effects of alcohol reduction on blood pressure. Roerecke M, Kaczorowski J, Tobe SW, Gmel G, Hasan OSM, Rehm J. The effect of a reduction in alcohol consumption on blood pressure: a systematic review and meta-analysis. Lancet Public Health. Midgley JP, Matthew AG, Greenwood CMT, Logan AG. Effect of reduced dietary sodium on blood pressure - a meta-analysis of randomized controlled trials. Cutler JA, Follmann D, Allender PS. Randomized trials of sodium reduction: an overview. Am J Clin Nutr. Article Google Scholar. Graudal NA, Galloe AM, Garred P. Effects of sodium restriction on blood pressure, renin, aldosterone, catecholamines, cholesterols, and triglyceride - a meta-analysis. He F, MacGregor GA. Effect of modest salt reduction on blood pressure: a meta-analysis of randomized trials. implications for public health. Graudal NA, Hubeck-Graudal T, Jurgens G: Effects of low sodium diet versus high sodium diet on blood pressure, renin, aldosterone, catecholamines, cholesterol, and triglyceride. Cochrane Database of Systematic Reviews Aburto NJ, Ziolkovska A, Hooper L, Elliott P, Cappuccio FP, Meerpohl JJ: Effect of lower sodium intake on health: systematic review and meta-analyses. Bmj-British Medical Journal , He FJ, Li JF, MacGregor GA. Effect of longer term modest salt reduction on blood pressure: cochrane systematic review and meta-analysis of randomised trials. Graudal NA, Hubeck-Graudal T, Jurgens G. Effects of low sodium diet versus high sodium diet on blood pressure, renin, aldosterone, catecholamines, cholesterol, and triglyceride. Cochrane Database Syst Rev. PubMed Google Scholar. World Health Organization: Effect of increased potassium intake on blood pressure, renal function, blood lipids and other potential adverse effects. Whelton SP, Chin A, Xin X, He J. Effect of aerobic exercise on blood pressure. Ann Intern Med. Cornelissen VA, Fagard RH. Effect of resistance training on resting blood pressure: a meta-analysis of randomized controlled trials. J Hypertens. Cornelissen VA, Fagard RH, Coeckelberghs E, Vanhees L. Impact of resistance training on blood pressure and other cardiovascular risk factors: a meta-analysis of randomized, controlled trials. Owen A, Wiles J, Swaine I. Effect of isometric exercise on resting blood pressure: a meta analysis. Inder JD, Carlson DJ, Dieberg G, McFarlane JR, Hess NC, Smart NA. Isometric exercise training for blood pressure management: a systematic review and meta-analysis to optimize benefit. Hypertens Res. Zeigler ZS, Mullane SL, Crespo NC, Buman MP, Gaesser GA. Effects of standing and light-intensity activity on ambulatory blood pressure. Med Sci Sports Exerc. Zeigler ZS, Swan PD, Bhammar DM, Gaesser GA. Walking workstation use reduces ambulatory blood pressure in adults with prehypertension. J Phys Act Health. Zomer E, Gurusamy K, Leach R, Trimmer C, Lobstein T, Morris S, James WP, Finer N. Interventions that cause weight loss and the impact on cardiovascular risk factors: a systematic review and meta-analysis. Schwingshackl L, Chaimani A, Schwedhelm C, Toledo E, Pünsch M, Hoffmann G, Boeing H. Comparative effects of different dietary approaches on blood pressure in hypertensive and pre-hypertensive patients: a systematic review and network meta-analysis. Crit Rev Food Sci Nutr. Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, Himmelfarb CD, DePalma SM, Gidding S, Jamerson KA, Jones DW. J Am Coll Cardiol. Unger T, Borghi C, Charchar F, Khan NA, Poulter NR, Prabhakaran D, Ramirez A, Schlaich M, Stergiou GS, Tomaszewski M. Kimani S, Mirie W, Chege M, Okube OT, Muniu S. Association of lifestyle modification and pharmacological adherence on blood pressure control among patients with hypertension at Kenyatta National Hospital, Kenya: a cross-sectional study. BMJ Open. Whelton PK, Appel LJ, Espeland MA, Applegate WB, Ettinger J, Walter H, Kostis JB, Kumanyika S, Lacy CR, Johnson KC, Folmar S, et al. Sodium reduction and weight loss in the treatment of hypertension in older personsa randomized controlled trial of nonpharmacologic interventions in the elderly TONE. Eckel Robert H, Jakicic John M, Ard Jamy D, de Jesus Janet M, Houston Miller N, Van Hubbard S, Lee IM, Lichtenstein Alice H, Loria Catherine M, Millen Barbara E, et al. Wu Y, Johnson BT, Acabchuk RL, Chen S, Lewis HK, Livingston J, Park CL, Pescatello LS. Yoga as antihypertensive lifestyle therapy: a systematic review and meta-analysis. Mayo Clin Proc. Rehm J, Prieto JAA, Beier M, Duhot D, Rossi A, Schulte B, Zarco J, Aubin H-J, Bachmann M, Grimm C, et al. The role of alcohol in the management of hypertension in patients in European primary health care practices — a survey in the largest European Union countries. BMC Fam Pract. Quader ZS, Cogswell ME, Fang J, Coleman King SM, Merritt RK. PLoS ONE. Booth HP, Prevost AT, Gulliford MC. Access to weight reduction interventions for overweight and obese patients in UK primary care: population-based cohort study. The impact of brief alcohol interventions in primary healthcare: a systematic review of reviews. Alcohol Alcohol. Bertholet N, Daeppen JB, Wietlisbach V, Fleming M, Burnand B. Reduction of alcohol consumption by brief alcohol intervention in primary care: systematic review and meta-analysis. Arch Intern Med. Kaner EFS, Beyer FR, Muirhead C, Campbell F, Pienaar ED, Bertholet N, Daeppen JB, Saunders JB, Burnand B. Effectiveness of brief alcohol interventions in primary care populations. Chi FW, Weisner CM, Mertens JR, Ross TB, Sterling SA. Alcohol brief intervention in primary care: blood pressure outcomes in hypertensive patients. J Subst Abuse Treat. Saitz R. Alcohol screening and brief intervention in primary care: absence of evidence for efficacy in people with dependence or very heavy drinking. Drug Alcohol Rev. Platt L, Melendez-Torres GJ, Donnell A, Bradley J, Newbury-Birch D, Kaner E, Ashton C. How effective are brief interventions in reducing alcohol consumption: do the setting, practitioner group and content matter? findings from a systematic review and metaregression analysis. Rehm J, Anderson P, Prieto JAA, Armstrong I, Aubin HJ, Bachmann M, Bastus NB, Brotons C, Burton R, Cardoso M, et al. Towards new recommendations to reduce the burden of alcohol-induced hypertension in the European Union. BMC Med. Angus C, Latimer N, Preston L, Li J, Purshouse R. What are the implications for policy makers? a systematic review of the cost-effectiveness of screening and brief interventions for alcohol misuse in primary care. Front Psychiatry. Glass JE, Andreasson S, Bradley KA, Finn SW, Williams EC, Bakshi AS, Gual A, Heather N, Sainz MT, Benegal V, et al. Addict Sci Clin Pract. Rahm AK, Boggs JM, Martin C, Price DW, Beck A, Backer TE, Dearing JW. Facilitators and Barriers to Implementing Screening, Brief Intervention, and Referral to Treatment SBIRT in primary care in integrated health care settings. Substance Abuse. Johnson M, Jackson R, Guillaume L, Meier P, Goyder E. Barriers and facilitators to implementing screening and brief intervention for alcohol misuse: a systematic review of qualitative evidence. J Public Health. Article CAS Google Scholar. Hasin DS, Aharonovich E, Greenstein E. HealthCall for the smartphone: technology enhancement of brief intervention in HIV alcohol dependent patients. Stoner SA, Mikko AT, Carpenter KM. Web-based training for primary care providers on screening, brief intervention, and referral to treatment SBIRT for alcohol, tobacco, and other drugs. Donoghue K, Patton R, Phillips T, Deluca P, Drummond C. The effectiveness of electronic screening and brief intervention for reducing levels of alcohol consumption: a systematic review and meta-analysis. J Med Internet Res. Beyer F, Lynch E, Kaner E. Brief interventions in primary care: an evidence overview of practitioner and digital intervention programmes. Curr Addict Rep. Anderson P, Bendtsen P, Spak F, Reynolds J, Drummond C, Segura L, Keurhorst MN, Palacio-Vieira J, Wojnar M, Parkinson K, et al. Improving the delivery of brief interventions for heavy drinking in primary health care: outcome results of the optimizing delivery of health care intervention ODHIN five-country cluster randomized factorial trial. Rose HL, Miller PM, Nemeth LS, Jenkins RG, Nietert PJ, Wessell AM, Ornstein S. Alcohol screening and brief counseling in a primary care hypertensive population: a quality improvement intervention. Ruzicka M, Hiremath S, Steiner S, Helis E, Szczotka A, Baker P, Fodor G: What is the feasibility of implementing effective sodium reduction strategies to treat hypertension in primary care settings? A systematic review. J Hypertens , 32 7 —; discussion Chan A, Kinsman L, Elmer S, Khanam M: An integrative review: adherence barriers to a low-salt diet in culturally diverse heart failure adults. Ghimire S, Shrestha N, Callahan K. Barriers to dietary salt reduction among hypertensive patients. J Nepal Health Res Counc. Mancia G, Oparil S, Whelton PK, McKee M, Dominiczak A, Luft FC, AlHabib K, Lanas F, Damasceno A, Prabhakaran D, et al. The technical report on sodium intake and cardiovascular disease in low- and middle-income countries by the joint working group of the World Heart Federation, the European society of hypertension and the European public health association. Eur Heart J. Couch SC, Saelens BE, Levin L, Dart K, Falciglia G, Daniels SR. The efficacy of a clinic-based behavioral nutrition intervention emphasizing a DASH-type diet for adolescents with elevated blood pressure. J Pediatr. STRM Lima da Silva Nalin de Souza B, França AKT, Filho NS, Sichieri R: Dietary approach to hypertension based on low glycaemic index and principles of DASH Dietary Approaches to Stop Hypertension : a randomised trial in a primary care service Br J Nutr 8 Niiranen TJ, Leino K, Puukka P, Kantola I, Karanko H, Jula AM. Lack of impact of a comprehensive intervention on hypertension in the primary care setting. Am J Hypertens. The effect of potassium supplementation on blood pressure in hypertensive subjects: a systematic review and meta-analysis. Int J Cardiol. Campbell F, Blank L, Messina J, Day M, Buckley Woods H, Payne N, Goyder E, Armitage C. Physical activity: brief advice for adults in primary care National Institute for Health and Clinical Excellence Public Health Intervention Guidance. Sheffield: NICE Centre for Public Health Excellence; Google Scholar. Campbell F, Holmes M, Everson-Hock E, Davis S, Buckley Woods H, Anokye N, Tappenden P, Kaltenthaler E. A systematic review and economic evaluation of exercise referral schemes in primary care: a short report. Health Technol Assess. Anokye NK, Lord J, Fox-Rushby J. Is brief advice in primary care a cost-effective way to promote physical activity? Br J Sports Med. Douglas F, Torrance N, van Teijlingen E, Meloni S, Kerr A. a questionnaire survey. BMC Public Health. Morgan F, Battersby A, Weightman AL, Searchfield L, Turley R, Morgan H, Jagroo J, Ellis S. Adherence to exercise referral schemes by participants — what do providers and commissioners need to know? a systematic review of barriers and facilitators. Booth HP, Prevost TA, Wright AJ, Gulliford MC. Effectiveness of behavioural weight loss interventions delivered in a primary care setting: a systematic review and meta-analysis. Fam Pract. Parretti HM, Jebb SA, Johns DJ, Lewis AL, Christian-Brown AM, Aveyard P. Clinical effectiveness of very-low-energy diets in the management of weight loss: a systematic review and meta-analysis of randomized controlled trials. Daumit GL, Janssen EM, Jerome GJ, Dalcin AT, Charleston J, Clark JM, Coughlin JW, Yeh HC, Miller ER, Durkin N, et al. Cost of behavioral weight loss programs implemented in clinical practice: the POWER trial at Johns Hopkins. Transl Behav Med. Kent S, Aveyard P, Astbury N, Mihaylova B, Jebb SA. Is doctor referral to a low-energy total diet replacement program cost-effective for the routine treatment of obesity? Gupta H. Barriers to and facilitators of long term weight loss maintenance in adult UK people: a thematic analysis. Int J Prev Med. PubMed PubMed Central Google Scholar. Dewhurst A, Peters S, Devereux-Fitzgerald A, Hart J. Patient Educ Couns. Tham M, Young D. The role of the general practitioner in weight management in primary care—a cross sectional study in general practice. Park HE, Billups SJ, Schilling LM: Physician perceived barriers and solutions to DASH diet recommendations for hypertension prevention and management. Dash S, Delibasic V, Alsaeed S, Ward M, Jefferson K, Manca DP, Arcand J. Knowledge, attitudes and behaviours related to physician-delivered dietary advice for patients with hypertension. J Community Health. Trieu K, McMahon E, Santos JA, Bauman A, Jolly KA, Bolam B, Webster J. Review of behaviour change interventions to reduce population salt intake. Int J Behav Nutr Phys Act. Hooper L, Bartlett C, Davey Smith G, Ebrahim S. Systematic review of long term effects of advice to reduce dietary salt in adults. Ferrara AL, Pacioni D, Di Fronzo V, Russo BF, Staiano L, Speranza E, Gente R, Gargiulo F, Ferrara F. Lifestyle educational program strongly increases compliance to nonpharmacologic intervention in hypertensive patients: a 2-year follow-up study. J Clin Hypertens Greenwich. Lin PH, Yancy WS Jr, Pollak KI, Dolor RJ, Marcello J, Samsa GP, Batch BC, Svetkey LP. The influence of a physician and patient intervention program on dietary intake. J Acad Nutr Diet. Yamasaki T, Sadanaga T, Hirota S. Effects of single-session dietary counseling by dieticians on salt reduction in cardiology outpatients who consumed large amounts of salt. Exp Ther Med. Bhana N, Utter J, Eyles H. Knowledge, attitudes and behaviours related to dietary salt intake in high-income countries: a systematic review. Current Nutrition Reports. Ireland DM, Clifton PM, Keogh JB. J Am Diet Assoc. htm ]. Liem DG, Miremadi F, Zandstra EH, Keast RSJ. Health labelling can influence taste perception and use of table salt for reduced-sodium products. Public Health Nutr. pdf ]. Cohn JN, Kowey PR, Whelton PK, Prisant LM. New guidelines for potassium replacement in clinical practice: a contemporary review by the national council on potassium in clinical practice. Filippini T, Naska A, Kasdagli MI, Torres D, Lopes C, Carvalho C, Moreira P, Malavolti M, Orsini N, Whelton PK, et al. Potassium intake and blood pressure: a dose-response meta-analysis of randomized controlled trials. Sidhu K, Sanjanwala R, Zieroth S. Hyperkalemia in heart failure. Curr Opin Cardiol. Greer RC, Marklund M, Anderson CAM, Cobb LK, Dalcin AT, Henry M, Appel LJ. Potassium-enriched salt substitutes as a means to lower blood pressure. Neal B, Wu Y, Feng X, Zhang R, Zhang Y, Shi J, Zhang J, Tian M, Huang L, Li Z, et al. Effect of salt substitution on cardiovascular events and death. Lamming L, Pears S, Mason D, Morton K, Bijker M, Sutton S, Hardeman W. What do we know about brief interventions for physical activity that could be delivered in primary care consultations? a systematic review of reviews. Prev Med. Morgan F, Turley RL, Morgan HE, Searchfield L, Weightman AL, Elliot E, Murphy S: Exercise referral schemes to promote physical activity: NICE; Early diagnosis and heart-healthy lifestyle changes can keep high blood pressure from seriously damaging your health. Blood pressure is the force of your blood pushing against the walls of your arteries. Each time your heart beats, it pumps blood into the arteries. Your blood pressure is highest when your heart beats, pumping the blood. This is called systolic pressure. When your heart is at rest, between beats, your blood pressure falls. This is called diastolic pressure. Your blood pressure reading uses these two numbers. Usually the systolic number comes before or above the diastolic number. High blood pressure usually has no symptoms. So the only way to find out if you have it is to get regular blood pressure checks from your health care provider. Your provider will use a gauge, a stethoscope or electronic sensor, and a blood pressure cuff. He or she will take two or more readings at separate appointments before making a diagnosis. For children and teens, the health care provider compares the blood pressure reading to what is normal for other kids who are the same age, height, and gender. Anyone can develop high blood pressure, but there are certain factors that can increase your risk:. If you already have high blood pressure, it is important to prevent it from getting worse or causing complications. You should get regular medical care and follow your prescribed treatment plan. Your plan will include healthy lifestyle habit recommendations and possibly medicines. The information on this site should not be used as a substitute for professional medical care or advice. Contact a health care provider if you have questions about your health. How to Prevent High Blood Pressure Also called: Lowering High Blood Pressure. On this page Basics Summary Start Here Prevention and Risk Factors. Learn More Related Issues Specifics Genetics. See, Play and Learn Videos and Tutorials Test Your Knowledge. Research Clinical Trials Journal Articles. Resources Find an Expert. For You Patient Handouts. What is blood pressure? How is high blood pressure diagnosed? Blood Pressure Category Systolic Blood Pressure Diastolic Blood Pressure Normal Less than and Less than 80 High Blood Pressure no other heart risk factors or higher or 90 or higher High Blood Pressure with other heart risk factors, according to some providers or higher or 80 or higher Dangerously high blood pressure - seek medical care right away or higher and or higher For children and teens, the health care provider compares the blood pressure reading to what is normal for other kids who are the same age, height, and gender. Who is at risk for high blood pressure? After age 55, women are more likely than men to develop it. Lifestyle - Certain lifestyle habits can raise your risk for high blood pressure, such as eating too much sodium salt or not enough potassium, lack of exercise, drinking too much alcohol, and smoking. Family history - A family history of high blood pressure raises the risk of developing high blood pressure How can I prevent high blood pressure? You can help prevent high blood pressure by having a healthy lifestyle. This means: Eating a healthy diet. To help manage your blood pressure, you should limit the amount of sodium salt that you eat and increase the amount of potassium in your diet. It is also important to eat foods that are lower in fat, as well as plenty of fruits, vegetables, and whole grains. The DASH eating plan is an example of an eating plan that can help you to lower your blood pressure. Getting regular exercise. Exercise can help you maintain a healthy weight and lower your blood pressure. You should try to get moderate-intensity aerobic exercise at least 2 and a half hours per week, or vigorous-intensity aerobic exercise for 1 hour and 15 minutes per week. Aerobic exercise, such as brisk walking, is any exercise in which your heart beats harder and you use more oxygen than usual. Being at a healthy weight. Being overweight or having obesity increases your risk for high blood pressure. Maintaining a healthy weight can help you control high blood pressure and reduce your risk for other health problems. Limiting alcohol. Drinking too much alcohol can raise your blood pressure. |
| Background | More in Pubmed. Larzelere MM, Williams DE. Hooper L, Bartlett C, Davey Smith G, Ebrahim S. Physical Activity Guidelines Advisory Committee report. C 1 , 7 5 to 20 Eat a diet high in fruits and vegetables and low in fat. |
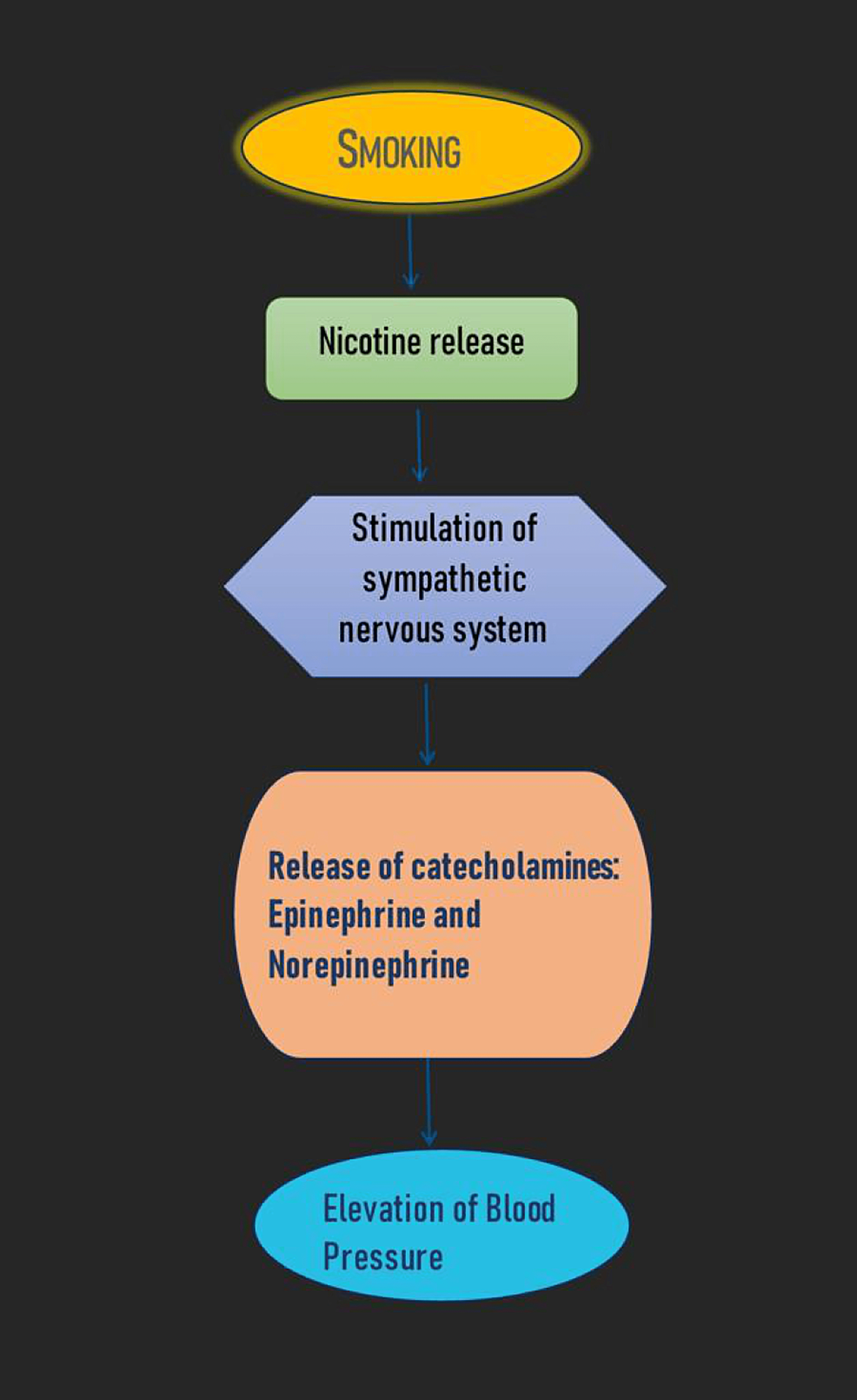
| Changes You Can Make to Manage High Blood Pressure | Sex-specific associations between alcohol consumption and incidence of hypertension: a systematic review and meta-analysis of cohort studies. J Am Heart Assoc. Article CAS PubMed PubMed Central Google Scholar. Association of urinary sodium and potassium excretion with blood pressure. N Engl J Med. Article PubMed Google Scholar. Kieneker LM, Gansevoort RT, Mukamal KJ, de Boer RA, Navis G, Bakker SJ, Joosten MM. Urinary potassium excretion and risk of developing hypertension: the prevention of renal and vascular end-stage disease study. Article CAS PubMed Google Scholar. Al Tunaiji H, Davis JC, Mansournia MA, Khan KM. Population attributable fraction of leading non-communicable cardiovascular diseases due to leisure-time physical inactivity: a systematic review. BMJ Open Sport Exerc Med. Article PubMed PubMed Central Google Scholar. Jayedi A, Rashidy-Pour A, Khorshidi M, Shab-Bidar S. Body mass index, abdominal adiposity, weight gain and risk of developing hypertension: a systematic review and dose-response meta-analysis of more than 2. Obes Rev. Schwingshackl L, Schwedhelm C, Hoffmann G, Knüppel S, Iqbal K, Andriolo V, Bechthold A, Schlesinger S, Boeing H. Food groups and risk of hypertension: a systematic review and dose-response meta-analysis of prospective studies. Advances in nutrition Bethesda, Md. Jayedi A, Soltani S, Abdolshahi A, Shab-Bidar S. Healthy and unhealthy dietary patterns and the risk of chronic disease: an umbrella review of meta-analyses of prospective cohort studies. Br J Nutr. Zhang Y, Zhang DZ. Red meat, poultry, and egg consumption with the risk of hypertension: a meta-analysis of prospective cohort studies. J Hum Hypertens. Xin X, He J, Frontini Maria G, Ogden Lorraine G, Motsamai Oaitse I, Whelton Paul K. Effects of alcohol reduction on blood pressure. Roerecke M, Kaczorowski J, Tobe SW, Gmel G, Hasan OSM, Rehm J. The effect of a reduction in alcohol consumption on blood pressure: a systematic review and meta-analysis. Lancet Public Health. Midgley JP, Matthew AG, Greenwood CMT, Logan AG. Effect of reduced dietary sodium on blood pressure - a meta-analysis of randomized controlled trials. Cutler JA, Follmann D, Allender PS. Randomized trials of sodium reduction: an overview. Am J Clin Nutr. Article Google Scholar. Graudal NA, Galloe AM, Garred P. Effects of sodium restriction on blood pressure, renin, aldosterone, catecholamines, cholesterols, and triglyceride - a meta-analysis. He F, MacGregor GA. Effect of modest salt reduction on blood pressure: a meta-analysis of randomized trials. implications for public health. Graudal NA, Hubeck-Graudal T, Jurgens G: Effects of low sodium diet versus high sodium diet on blood pressure, renin, aldosterone, catecholamines, cholesterol, and triglyceride. Cochrane Database of Systematic Reviews Aburto NJ, Ziolkovska A, Hooper L, Elliott P, Cappuccio FP, Meerpohl JJ: Effect of lower sodium intake on health: systematic review and meta-analyses. Bmj-British Medical Journal , He FJ, Li JF, MacGregor GA. Effect of longer term modest salt reduction on blood pressure: cochrane systematic review and meta-analysis of randomised trials. Graudal NA, Hubeck-Graudal T, Jurgens G. Effects of low sodium diet versus high sodium diet on blood pressure, renin, aldosterone, catecholamines, cholesterol, and triglyceride. Cochrane Database Syst Rev. PubMed Google Scholar. World Health Organization: Effect of increased potassium intake on blood pressure, renal function, blood lipids and other potential adverse effects. Whelton SP, Chin A, Xin X, He J. Effect of aerobic exercise on blood pressure. Ann Intern Med. Cornelissen VA, Fagard RH. Effect of resistance training on resting blood pressure: a meta-analysis of randomized controlled trials. J Hypertens. Cornelissen VA, Fagard RH, Coeckelberghs E, Vanhees L. Impact of resistance training on blood pressure and other cardiovascular risk factors: a meta-analysis of randomized, controlled trials. Owen A, Wiles J, Swaine I. Effect of isometric exercise on resting blood pressure: a meta analysis. Inder JD, Carlson DJ, Dieberg G, McFarlane JR, Hess NC, Smart NA. Isometric exercise training for blood pressure management: a systematic review and meta-analysis to optimize benefit. Hypertens Res. Zeigler ZS, Mullane SL, Crespo NC, Buman MP, Gaesser GA. Effects of standing and light-intensity activity on ambulatory blood pressure. Med Sci Sports Exerc. Zeigler ZS, Swan PD, Bhammar DM, Gaesser GA. Walking workstation use reduces ambulatory blood pressure in adults with prehypertension. J Phys Act Health. Zomer E, Gurusamy K, Leach R, Trimmer C, Lobstein T, Morris S, James WP, Finer N. Interventions that cause weight loss and the impact on cardiovascular risk factors: a systematic review and meta-analysis. Schwingshackl L, Chaimani A, Schwedhelm C, Toledo E, Pünsch M, Hoffmann G, Boeing H. Comparative effects of different dietary approaches on blood pressure in hypertensive and pre-hypertensive patients: a systematic review and network meta-analysis. Crit Rev Food Sci Nutr. Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, Himmelfarb CD, DePalma SM, Gidding S, Jamerson KA, Jones DW. J Am Coll Cardiol. Unger T, Borghi C, Charchar F, Khan NA, Poulter NR, Prabhakaran D, Ramirez A, Schlaich M, Stergiou GS, Tomaszewski M. Kimani S, Mirie W, Chege M, Okube OT, Muniu S. Association of lifestyle modification and pharmacological adherence on blood pressure control among patients with hypertension at Kenyatta National Hospital, Kenya: a cross-sectional study. BMJ Open. Whelton PK, Appel LJ, Espeland MA, Applegate WB, Ettinger J, Walter H, Kostis JB, Kumanyika S, Lacy CR, Johnson KC, Folmar S, et al. Sodium reduction and weight loss in the treatment of hypertension in older personsa randomized controlled trial of nonpharmacologic interventions in the elderly TONE. Eckel Robert H, Jakicic John M, Ard Jamy D, de Jesus Janet M, Houston Miller N, Van Hubbard S, Lee IM, Lichtenstein Alice H, Loria Catherine M, Millen Barbara E, et al. Wu Y, Johnson BT, Acabchuk RL, Chen S, Lewis HK, Livingston J, Park CL, Pescatello LS. Yoga as antihypertensive lifestyle therapy: a systematic review and meta-analysis. Mayo Clin Proc. Rehm J, Prieto JAA, Beier M, Duhot D, Rossi A, Schulte B, Zarco J, Aubin H-J, Bachmann M, Grimm C, et al. The role of alcohol in the management of hypertension in patients in European primary health care practices — a survey in the largest European Union countries. BMC Fam Pract. Quader ZS, Cogswell ME, Fang J, Coleman King SM, Merritt RK. PLoS ONE. Booth HP, Prevost AT, Gulliford MC. Access to weight reduction interventions for overweight and obese patients in UK primary care: population-based cohort study. The impact of brief alcohol interventions in primary healthcare: a systematic review of reviews. Alcohol Alcohol. Bertholet N, Daeppen JB, Wietlisbach V, Fleming M, Burnand B. Reduction of alcohol consumption by brief alcohol intervention in primary care: systematic review and meta-analysis. Arch Intern Med. Kaner EFS, Beyer FR, Muirhead C, Campbell F, Pienaar ED, Bertholet N, Daeppen JB, Saunders JB, Burnand B. Effectiveness of brief alcohol interventions in primary care populations. Chi FW, Weisner CM, Mertens JR, Ross TB, Sterling SA. Alcohol brief intervention in primary care: blood pressure outcomes in hypertensive patients. J Subst Abuse Treat. Saitz R. Alcohol screening and brief intervention in primary care: absence of evidence for efficacy in people with dependence or very heavy drinking. Drug Alcohol Rev. Platt L, Melendez-Torres GJ, Donnell A, Bradley J, Newbury-Birch D, Kaner E, Ashton C. How effective are brief interventions in reducing alcohol consumption: do the setting, practitioner group and content matter? findings from a systematic review and metaregression analysis. Rehm J, Anderson P, Prieto JAA, Armstrong I, Aubin HJ, Bachmann M, Bastus NB, Brotons C, Burton R, Cardoso M, et al. Towards new recommendations to reduce the burden of alcohol-induced hypertension in the European Union. BMC Med. Angus C, Latimer N, Preston L, Li J, Purshouse R. What are the implications for policy makers? a systematic review of the cost-effectiveness of screening and brief interventions for alcohol misuse in primary care. Front Psychiatry. Glass JE, Andreasson S, Bradley KA, Finn SW, Williams EC, Bakshi AS, Gual A, Heather N, Sainz MT, Benegal V, et al. Addict Sci Clin Pract. Rahm AK, Boggs JM, Martin C, Price DW, Beck A, Backer TE, Dearing JW. Facilitators and Barriers to Implementing Screening, Brief Intervention, and Referral to Treatment SBIRT in primary care in integrated health care settings. Substance Abuse. Johnson M, Jackson R, Guillaume L, Meier P, Goyder E. Barriers and facilitators to implementing screening and brief intervention for alcohol misuse: a systematic review of qualitative evidence. J Public Health. Article CAS Google Scholar. Hasin DS, Aharonovich E, Greenstein E. HealthCall for the smartphone: technology enhancement of brief intervention in HIV alcohol dependent patients. Stoner SA, Mikko AT, Carpenter KM. Web-based training for primary care providers on screening, brief intervention, and referral to treatment SBIRT for alcohol, tobacco, and other drugs. Donoghue K, Patton R, Phillips T, Deluca P, Drummond C. The effectiveness of electronic screening and brief intervention for reducing levels of alcohol consumption: a systematic review and meta-analysis. J Med Internet Res. Beyer F, Lynch E, Kaner E. Brief interventions in primary care: an evidence overview of practitioner and digital intervention programmes. Curr Addict Rep. Anderson P, Bendtsen P, Spak F, Reynolds J, Drummond C, Segura L, Keurhorst MN, Palacio-Vieira J, Wojnar M, Parkinson K, et al. Improving the delivery of brief interventions for heavy drinking in primary health care: outcome results of the optimizing delivery of health care intervention ODHIN five-country cluster randomized factorial trial. Rose HL, Miller PM, Nemeth LS, Jenkins RG, Nietert PJ, Wessell AM, Ornstein S. Alcohol screening and brief counseling in a primary care hypertensive population: a quality improvement intervention. Ruzicka M, Hiremath S, Steiner S, Helis E, Szczotka A, Baker P, Fodor G: What is the feasibility of implementing effective sodium reduction strategies to treat hypertension in primary care settings? A systematic review. J Hypertens , 32 7 —; discussion Chan A, Kinsman L, Elmer S, Khanam M: An integrative review: adherence barriers to a low-salt diet in culturally diverse heart failure adults. Ghimire S, Shrestha N, Callahan K. Barriers to dietary salt reduction among hypertensive patients. J Nepal Health Res Counc. Mancia G, Oparil S, Whelton PK, McKee M, Dominiczak A, Luft FC, AlHabib K, Lanas F, Damasceno A, Prabhakaran D, et al. The technical report on sodium intake and cardiovascular disease in low- and middle-income countries by the joint working group of the World Heart Federation, the European society of hypertension and the European public health association. Eur Heart J. Couch SC, Saelens BE, Levin L, Dart K, Falciglia G, Daniels SR. The efficacy of a clinic-based behavioral nutrition intervention emphasizing a DASH-type diet for adolescents with elevated blood pressure. J Pediatr. STRM Lima da Silva Nalin de Souza B, França AKT, Filho NS, Sichieri R: Dietary approach to hypertension based on low glycaemic index and principles of DASH Dietary Approaches to Stop Hypertension : a randomised trial in a primary care service Br J Nutr 8 Niiranen TJ, Leino K, Puukka P, Kantola I, Karanko H, Jula AM. Lack of impact of a comprehensive intervention on hypertension in the primary care setting. Am J Hypertens. The effect of potassium supplementation on blood pressure in hypertensive subjects: a systematic review and meta-analysis. Int J Cardiol. Campbell F, Blank L, Messina J, Day M, Buckley Woods H, Payne N, Goyder E, Armitage C. Physical activity: brief advice for adults in primary care National Institute for Health and Clinical Excellence Public Health Intervention Guidance. Sheffield: NICE Centre for Public Health Excellence; Google Scholar. Campbell F, Holmes M, Everson-Hock E, Davis S, Buckley Woods H, Anokye N, Tappenden P, Kaltenthaler E. A systematic review and economic evaluation of exercise referral schemes in primary care: a short report. Health Technol Assess. Anokye NK, Lord J, Fox-Rushby J. Is brief advice in primary care a cost-effective way to promote physical activity? Br J Sports Med. Douglas F, Torrance N, van Teijlingen E, Meloni S, Kerr A. a questionnaire survey. BMC Public Health. Morgan F, Battersby A, Weightman AL, Searchfield L, Turley R, Morgan H, Jagroo J, Ellis S. Adherence to exercise referral schemes by participants — what do providers and commissioners need to know? a systematic review of barriers and facilitators. Booth HP, Prevost TA, Wright AJ, Gulliford MC. Effectiveness of behavioural weight loss interventions delivered in a primary care setting: a systematic review and meta-analysis. Fam Pract. Parretti HM, Jebb SA, Johns DJ, Lewis AL, Christian-Brown AM, Aveyard P. Clinical effectiveness of very-low-energy diets in the management of weight loss: a systematic review and meta-analysis of randomized controlled trials. Daumit GL, Janssen EM, Jerome GJ, Dalcin AT, Charleston J, Clark JM, Coughlin JW, Yeh HC, Miller ER, Durkin N, et al. Cost of behavioral weight loss programs implemented in clinical practice: the POWER trial at Johns Hopkins. Transl Behav Med. Kent S, Aveyard P, Astbury N, Mihaylova B, Jebb SA. Is doctor referral to a low-energy total diet replacement program cost-effective for the routine treatment of obesity? Gupta H. Barriers to and facilitators of long term weight loss maintenance in adult UK people: a thematic analysis. Int J Prev Med. PubMed PubMed Central Google Scholar. Dewhurst A, Peters S, Devereux-Fitzgerald A, Hart J. Patient Educ Couns. Tham M, Young D. The role of the general practitioner in weight management in primary care—a cross sectional study in general practice. Park HE, Billups SJ, Schilling LM: Physician perceived barriers and solutions to DASH diet recommendations for hypertension prevention and management. Dash S, Delibasic V, Alsaeed S, Ward M, Jefferson K, Manca DP, Arcand J. Knowledge, attitudes and behaviours related to physician-delivered dietary advice for patients with hypertension. J Community Health. Trieu K, McMahon E, Santos JA, Bauman A, Jolly KA, Bolam B, Webster J. Review of behaviour change interventions to reduce population salt intake. Int J Behav Nutr Phys Act. Hooper L, Bartlett C, Davey Smith G, Ebrahim S. Systematic review of long term effects of advice to reduce dietary salt in adults. Ferrara AL, Pacioni D, Di Fronzo V, Russo BF, Staiano L, Speranza E, Gente R, Gargiulo F, Ferrara F. Lifestyle educational program strongly increases compliance to nonpharmacologic intervention in hypertensive patients: a 2-year follow-up study. J Clin Hypertens Greenwich. Lin PH, Yancy WS Jr, Pollak KI, Dolor RJ, Marcello J, Samsa GP, Batch BC, Svetkey LP. The influence of a physician and patient intervention program on dietary intake. J Acad Nutr Diet. Yamasaki T, Sadanaga T, Hirota S. Effects of single-session dietary counseling by dieticians on salt reduction in cardiology outpatients who consumed large amounts of salt. Exp Ther Med. Bhana N, Utter J, Eyles H. Knowledge, attitudes and behaviours related to dietary salt intake in high-income countries: a systematic review. Current Nutrition Reports. Ireland DM, Clifton PM, Keogh JB. J Am Diet Assoc. htm ]. Liem DG, Miremadi F, Zandstra EH, Keast RSJ. Health labelling can influence taste perception and use of table salt for reduced-sodium products. Public Health Nutr. pdf ]. Cohn JN, Kowey PR, Whelton PK, Prisant LM. New guidelines for potassium replacement in clinical practice: a contemporary review by the national council on potassium in clinical practice. Filippini T, Naska A, Kasdagli MI, Torres D, Lopes C, Carvalho C, Moreira P, Malavolti M, Orsini N, Whelton PK, et al. Potassium intake and blood pressure: a dose-response meta-analysis of randomized controlled trials. Sidhu K, Sanjanwala R, Zieroth S. Hyperkalemia in heart failure. Curr Opin Cardiol. Greer RC, Marklund M, Anderson CAM, Cobb LK, Dalcin AT, Henry M, Appel LJ. Potassium-enriched salt substitutes as a means to lower blood pressure. Neal B, Wu Y, Feng X, Zhang R, Zhang Y, Shi J, Zhang J, Tian M, Huang L, Li Z, et al. Effect of salt substitution on cardiovascular events and death. Lamming L, Pears S, Mason D, Morton K, Bijker M, Sutton S, Hardeman W. What do we know about brief interventions for physical activity that could be delivered in primary care consultations? a systematic review of reviews. Prev Med. Morgan F, Turley RL, Morgan HE, Searchfield L, Weightman AL, Elliot E, Murphy S: Exercise referral schemes to promote physical activity: NICE; Pavey TG, Taylor AH, Fox KR, Hillsdon M, Anokye N, Campbell JL, Foster C, Green C, Moxham T, Mutrie N et al: Effect of exercise referral schemes in primary care on physical activity and improving health outcomes: systematic review and meta-analysis. Bmj , nov04 2 :dd Lion A, Vuillemin A, Thornton JS, Theisen D, Stranges S, Ward M. Physical activity promotion in primary care: a Utopian quest? Health Promot Int. Eden KB, Orleans CT, Mulrow CD, Pender NJ, Teutsch SM. Does counseling by clinicians improve physical activity? a summary of the evidence for the U. preventive services task force. Cochrane Database of Systematic Reviews 9. Sousa Junior AE, Macêdo GAD, Schwade D, Sócrates J, Alves JW, Farias-Junior LF, Freire YA, Lemos T, Browne RAV, Costa EC. Physical activity counseling for adults with hypertension: a randomized controlled pilot trial. Int J Environ Res Public Health. Lin JS, O'Connor EA, Evans CV, Senger CA, Rowland MG, Groom HC: U. Preventive Services Task Force Evidence Syntheses, formerly Systematic Evidence Reviews. In: Behavioral Counseling to Promote a Healthy Lifestyle for Cardiovascular Disease Prevention in Persons With Cardiovascular Risk Factors: An Updated Systematic Evidence Review for the US Preventive Services Task Force. Rockville MD : Agency for Healthcare Research and Quality US ; Patrick K, Pratt M, Sallis RE: The Healthcare Sector's Role in the U. National Physical Activity Plan. Pool AC, Kraschnewski JL, Cover LA, Lehman EB, Stuckey HL, Hwang KO, Pollak KI, Sciamanna CN. The impact of physician weight discussion on weight loss in US adults. Obes Res Clin Pract. Wadden TA, Volger S, Tsai AG, Sarwer DB, Berkowitz RI, Diewald LK, Carvajal R, Moran CH, Vetter M. Group P-UR: Managing obesity in primary care practice: an overview with perspective from the POWER-UP study. Int J Obes Lond. Astbury NM, Aveyard P, Nickless A, Hood K, Corfield K, Lowe R, Jebb SA. Doctor referral of overweight people to low energy total diet replacement treatment DROPLET : pragmatic randomised controlled trial. Tsai AG, Wadden TA. The evolution of very-low-calorie diets: an update and meta-analysis. Semlitsch T, Jeitler K, Berghold A, Horvath K, Posch N, Poggenburg S, Siebenhofer A. Long-term effects of weight-reducing diets in people with hypertension. Gulsin GS, Swarbrick DJ, Athithan L, Brady EM, Henson J, Baldry E, Argyridou S, Jaicim NB, Squire G, Walters Y, et al. Effects of low-energy diet or exercise on cardiovascular function in working-age adults with type 2 Diabetes: a prospective, randomized, open-label. Blinded End Point Trial Diabetes Care. Brown A, Leeds AR. Very low-energy and low-energy formula diets: effects on weight loss, obesity co-morbidities and type 2 diabetes remission — an update on the evidence for their use in clinical practice. Nutr Bull. Wadden TA, Butryn ML, Hong PS, Tsai AG. Behavioral treatment of obesity in patients encountered in primary care settings: a systematic review. Gay HC, Rao SG, Vaccarino V, Ali MK. Effects of different dietary interventions on blood pressure. Kolasa KM. Dietary approaches to stop hypertension DASH in clinical practice: a primary care experience. Clin Cardiol. Blumenthal JA, Babyak MA, Hinderliter A, Watkins LL, Craighead L, Lin P-H, Caccia C, Johnson J, Waugh R, Sherwood A. Effects of the DASH diet alone and in combination with exercise and weight loss on blood pressure and cardiovascular biomarkers in men and women with high blood pressure: the ENCORE study. Lin P-H, Appel LJ, Funk K, Craddick S, Chen C, Elmer P, McBurnie MA, Champagne C. The PREMIER intervention helps participants follow the dietary approaches to stop hypertension dietary pattern and the current dietary reference intakes recommendations. Wong MCS, Wang HHX, Kwan MWM, Fong BCY, Chan WM, Zhang DX, Li STS, Yan BP, Coats AJS, Griffiths SM. Dietary counselling has no effect on cardiovascular risk factors among Chinese Grade 1 hypertensive patients: a randomized controlled trial. Kim H, Andrade FCD. Diagnostic status of hypertension on the adherence to the dietary approaches to stop hypertension DASH diet. Prev Med Rep. R Mahdavi Bagheri asl A, Abadi MAJ, Namazi N: Perceived Barriers to Following Dietary Recommendations in Hypertensive Patients J Am Coll Nutr 36 3 Conversano C, Orrù G, Pozza A, Miccoli M, Ciacchini R, Marchi L, Gemignani A. Is mindfulness-based stress reduction effective for people with hypertension? a systematic review and meta-analysis of 30 years of evidence. Xie C, Cui L, Zhu J, Wang K, Sun N, Sun C. Coffee consumption and risk of hypertension: a systematic review and dose-response meta-analysis of cohort studies. Mahdavi-Roshan M, Salari A, Ghorbani Z, Ashouri A. The effects of regular consumption of green or black tea beverage on blood pressure in those with elevated blood pressure or hypertension: a systematic review and meta-analysis. Complement Ther Med. Wolff M, Sundquist K, Lonn SL, Midlov P. Impact of yoga on blood pressure and quality of life in patients with hypertension - a controlled trial in primary care, matched for systolic blood pressure. BMC Cardiovasc Disord. Wolff M, Rogers K, Erdal B, Chalmers JP, Sundquist K, Midlov P. Impact of a short home-based yoga programme on blood pressure in patients with hypertension: a randomized controlled trial in primary care. Dhungana RR, Pedisic Z, Joshi S, Khanal MK, Kalauni OP, Shakya A, Bhurtel V, Panthi S, Ramesh Kumar KC, Ghimire B, et al. Effects of a health worker-led 3-month yoga intervention on blood pressure of hypertensive patients: a randomised controlled multicentre trial in the primary care setting. Momeni J, Omidi A, Raygan F, Akbari H. J Am Soc Hypertens. Demarzo MMP, Montero-Marin J, Cuijpers P, Zabaleta-del-Olmo E, Mahtani KR, Vellinga A, Vicens C, López-del-Hoyo Y, García-Campayo J. The efficacy of mindfulness-based interventions in primary care: a meta-analytic review. Ann Fam Med. PHR Santiago Valle Serra e Meira LR, Colussi CF: Feasibility evaluation of a mindfulness-based stress reduction program for primary care professionals in Brazilian national health system Complement Ther Clin Pract 35 8 Download references. Institute for Health and Sport, Victoria University, Melbourne, Australia. Melbourne School of Population and Global Health, University of Melbourne, Melbourne, Australia. You can also search for this author in PubMed Google Scholar. RRD and ZP conceptualised the study. RRD interpreted the findings and prepared the first draft. MdC and ZP interpreted the findings, revised the draft and contributed to writing the manuscript. All authors read and approved the final manuscript. Correspondence to Raja Ram Dhungana. Effects of diet and sodium intake on blood pressure: subgroup analysis of the DASH-sodium trial. Ann Intern Med. National Heart, Lung, and Blood Institute. The DASH eating plan. Bethesda, Md. Department of Health and Human Services, Whelton PK, Appel LJ, Espeland MA, Applegate WB, Ettinger WH, Kostis JB, et al. Sodium reduction and weight loss in the treatment of hypertension in older persons: a randomized controlled trial of non-pharmacologic interventions in the elderly TONE [published correction appears in JAMA ;]. Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, Harsha D, et al. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension DASH diet. Whelton SP, Chin A, Xin X, He J. Effect of aerobic exercise on blood pressure: a meta-analysis of randomized, controlled trials. Xin X, He J, Frontini MG, Ogden LG, Motsamai OI, Whelton PK. Effects of alcohol reduction on blood pressure: a meta-analysis of randomized controlled trials. Appel LJ, Champagne CM, Harsha DW, Cooper LS, Obarzanek E, Elmer PJ, et al. Effects of comprehensive lifestyle modification on blood pressure control: main results of the PREMIER clinical trial. Gallen IW, Rosa RM, Esparaz DY, Young JB, Robertson GL, Batlle D, et al. On the mechanism of the effects of potassium restriction on blood pressure and renal sodium retention. Am J Kidney Dis. Krishna GG, Kapoor SC. Potassium depletion exacerbates essential hypertension. Geleijnse JM, Kok FJ, Grobbee DE. Blood pressure response to changes in sodium and potassium intake: a metaregression analysis of randomized trials. J Hum Hypertens. Cryer PE, Haymond MW, Santiago JV, Shah SD. Norepinephrine and epinephrine release and adrenergic mediation of smoking-associated hemodynamic and metabolic events. Benowitz NL, Hansson A, Jacob P. Cardiovascular effects of nasal and transdermal nicotine and cigarette smoking. Yamagishi K, Iso H, Kitamura A, Sankai T, Tanigawa T, Naito Y, et al. Smoking raises the risk of total and ischemic strokes in hypertensive men. Hypertens Res. Kurth T, Kase CS, Berger K, Schaeffner ES, Buring JE, Gaziano JM. Smoking and the risk of hemorrhagic stroke in men. Schneider RH, Staggers F, Alexander CN, Sheppard W, Rainforth M, Kondwani K, et al. A randomised controlled trial of stress reduction for hypertension in older African Americans. Canter PH, Ernst E. Insufficient evidence to conclude whether or not transcendental meditation decreases blood pressure: results of a systematic review of randomized clinical trials. J Hypertens. Schneider RH, Alexander CN, Staggers F, Rainforth M, Salerno JW, Hartz A, et al. Am J Cardiol. This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. search close. PREV Jun 1, NEXT. C 1 , 7 5 to 20 Eat a diet high in fruits and vegetables and low in fat. C 1 , 9 , 11 , 12 2 to 8 Get 30 minutes of aerobic activity at least four days per week. C 1 , 13 4 to 9 Men should have no more than two alcoholic drinks per day, and women no more than one alcoholic drink per day. Recommended Lifestyle Modifications. SODIUM REDUCTION. DIETARY CHANGES. WEIGHT LOSS. Other Lifestyle Interventions. SMOKING CESSATION. RANDY WEXLER, M. He completed a residency in family medicine at Mt. Carmel Medical Center in Columbus, Ohio, and received his master's degree in public health from Ohio State University School of Public Health. He also is director of the Division of Integrative Medicine, Department of Family Medicine, and medical director of Ohio State University Center for Integrative Medicine. wexler osumc. |

Video
Instantly lower BLOOD PRESSURE - 3 Proven MethodsManaging hypertension with non-medical techniques -
Bray GA, Vollmer WM, Sacks FM, Obarzanek E, Svetkey LP, Appel LJ DASH Collaborative Research Group. A further subgroup analysis of the effects of the DASH diet and three dietary sodium levels on blood pressure: results of the DASH-Sodium Trial [published correction appears in Am J Cardiol.
Am J Cardiol. Sacks FM, Svetkey LP, Vollmer WM, et al. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension DASH diet. Office of Disease Prevention and Health Promotion.
Physical Activity Guidelines Advisory Committee report. Accessed June 1, Brook RD, Appel LJ, Rubenfire M, et al. Beyond medications and diet: alternative approaches to lowering blood pressure: a scientific statement from the American Heart Association.
LeFevre ML U. Preventive Services Task Force. Behavioral counseling to promote a healthful diet and physical activity for cardiovascular disease prevention in adults with cardiovascular risk factors: U. Preventive Services Task Force recommendation statement. Ann Intern Med. Counseling and interventions to prevent tobacco use and tobacco-caused disease in adults and pregnant women: U.
Preventive Services Task Force reaffirmation recommendation statement. Larzelere MM, Williams DE. Promoting smoking cessation.
Am Fam Physician. Najem B, Houssière A, Pathak A, et al. Acute cardiovascular and sympathetic effects of nicotine replacement therapy [published correction appears in Hypertension.
Critchley J, Capewell S. Smoking cessation for the secondary prevention of coronary heart disease. Cochrane Database Syst Rev. Fiore MC, Jaén CR, Baker TB, et al. Department of Health and Human Services.
Treating tobacco use and dependence: update. Accessed June 12, Wexler R, Aukerman G. Nonpharmacologic strategies for managing hypertension. Stabler SN, Tejani AM, Huynh F, Fowkes C. Garlic for the prevention of cardiovascular morbidity and mortality in hypertensive patients.
Ried K, Sullivan TR, Fakler P, Frank OR, Stocks NP. Effect of cocoa on blood pressure. Uhlig K, Patel K, Ip S, Kitsios GD, Balk EM. Self-measured blood pressure monitoring in the management of hypertension: a systematic review and meta-analysis. Peppard PE, Young T, Palta M, Skatrud J.
Prospective study of the association between sleep-disordered breathing and hypertension. Cross MD, Mills NL, Al-Abri M, et al.
Budhiraja R, Quan SF. When is CPAP an antihypertensive in sleep apnea patients?. J Clin Sleep Med. Parati G, Lombardi C. Control of hypertension in nonsleepy patients with obstructive sleep apnea. Am J Respir Crit Care Med. Varounis C, Katsi V, Kallikazaros IE, et al.
Effect of CPAP on blood pressure in patients with obstructive sleep apnea and resistant hypertension: a systematic review and meta-analysis. Int J Cardiol. This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference.
This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. search close. Sousa Junior AE, Macêdo GAD, Schwade D, Sócrates J, Alves JW, Farias-Junior LF, Freire YA, Lemos T, Browne RAV, Costa EC.
Physical activity counseling for adults with hypertension: a randomized controlled pilot trial. Int J Environ Res Public Health. Lin JS, O'Connor EA, Evans CV, Senger CA, Rowland MG, Groom HC: U. Preventive Services Task Force Evidence Syntheses, formerly Systematic Evidence Reviews.
In: Behavioral Counseling to Promote a Healthy Lifestyle for Cardiovascular Disease Prevention in Persons With Cardiovascular Risk Factors: An Updated Systematic Evidence Review for the US Preventive Services Task Force.
Rockville MD : Agency for Healthcare Research and Quality US ; Patrick K, Pratt M, Sallis RE: The Healthcare Sector's Role in the U. National Physical Activity Plan. Pool AC, Kraschnewski JL, Cover LA, Lehman EB, Stuckey HL, Hwang KO, Pollak KI, Sciamanna CN.
The impact of physician weight discussion on weight loss in US adults. Obes Res Clin Pract. Wadden TA, Volger S, Tsai AG, Sarwer DB, Berkowitz RI, Diewald LK, Carvajal R, Moran CH, Vetter M. Group P-UR: Managing obesity in primary care practice: an overview with perspective from the POWER-UP study.
Int J Obes Lond. Astbury NM, Aveyard P, Nickless A, Hood K, Corfield K, Lowe R, Jebb SA. Doctor referral of overweight people to low energy total diet replacement treatment DROPLET : pragmatic randomised controlled trial.
Tsai AG, Wadden TA. The evolution of very-low-calorie diets: an update and meta-analysis. Semlitsch T, Jeitler K, Berghold A, Horvath K, Posch N, Poggenburg S, Siebenhofer A. Long-term effects of weight-reducing diets in people with hypertension.
Gulsin GS, Swarbrick DJ, Athithan L, Brady EM, Henson J, Baldry E, Argyridou S, Jaicim NB, Squire G, Walters Y, et al. Effects of low-energy diet or exercise on cardiovascular function in working-age adults with type 2 Diabetes: a prospective, randomized, open-label.
Blinded End Point Trial Diabetes Care. Brown A, Leeds AR. Very low-energy and low-energy formula diets: effects on weight loss, obesity co-morbidities and type 2 diabetes remission — an update on the evidence for their use in clinical practice.
Nutr Bull. Wadden TA, Butryn ML, Hong PS, Tsai AG. Behavioral treatment of obesity in patients encountered in primary care settings: a systematic review.
Gay HC, Rao SG, Vaccarino V, Ali MK. Effects of different dietary interventions on blood pressure. Kolasa KM. Dietary approaches to stop hypertension DASH in clinical practice: a primary care experience.
Clin Cardiol. Blumenthal JA, Babyak MA, Hinderliter A, Watkins LL, Craighead L, Lin P-H, Caccia C, Johnson J, Waugh R, Sherwood A. Effects of the DASH diet alone and in combination with exercise and weight loss on blood pressure and cardiovascular biomarkers in men and women with high blood pressure: the ENCORE study.
Lin P-H, Appel LJ, Funk K, Craddick S, Chen C, Elmer P, McBurnie MA, Champagne C. The PREMIER intervention helps participants follow the dietary approaches to stop hypertension dietary pattern and the current dietary reference intakes recommendations.
Wong MCS, Wang HHX, Kwan MWM, Fong BCY, Chan WM, Zhang DX, Li STS, Yan BP, Coats AJS, Griffiths SM. Dietary counselling has no effect on cardiovascular risk factors among Chinese Grade 1 hypertensive patients: a randomized controlled trial.
Kim H, Andrade FCD. Diagnostic status of hypertension on the adherence to the dietary approaches to stop hypertension DASH diet.
Prev Med Rep. R Mahdavi Bagheri asl A, Abadi MAJ, Namazi N: Perceived Barriers to Following Dietary Recommendations in Hypertensive Patients J Am Coll Nutr 36 3 Conversano C, Orrù G, Pozza A, Miccoli M, Ciacchini R, Marchi L, Gemignani A.
Is mindfulness-based stress reduction effective for people with hypertension? a systematic review and meta-analysis of 30 years of evidence. Xie C, Cui L, Zhu J, Wang K, Sun N, Sun C. Coffee consumption and risk of hypertension: a systematic review and dose-response meta-analysis of cohort studies.
Mahdavi-Roshan M, Salari A, Ghorbani Z, Ashouri A. The effects of regular consumption of green or black tea beverage on blood pressure in those with elevated blood pressure or hypertension: a systematic review and meta-analysis. Complement Ther Med. Wolff M, Sundquist K, Lonn SL, Midlov P.
Impact of yoga on blood pressure and quality of life in patients with hypertension - a controlled trial in primary care, matched for systolic blood pressure.
BMC Cardiovasc Disord. Wolff M, Rogers K, Erdal B, Chalmers JP, Sundquist K, Midlov P. Impact of a short home-based yoga programme on blood pressure in patients with hypertension: a randomized controlled trial in primary care. Dhungana RR, Pedisic Z, Joshi S, Khanal MK, Kalauni OP, Shakya A, Bhurtel V, Panthi S, Ramesh Kumar KC, Ghimire B, et al.
Effects of a health worker-led 3-month yoga intervention on blood pressure of hypertensive patients: a randomised controlled multicentre trial in the primary care setting. Momeni J, Omidi A, Raygan F, Akbari H. J Am Soc Hypertens. Demarzo MMP, Montero-Marin J, Cuijpers P, Zabaleta-del-Olmo E, Mahtani KR, Vellinga A, Vicens C, López-del-Hoyo Y, García-Campayo J.
The efficacy of mindfulness-based interventions in primary care: a meta-analytic review. Ann Fam Med. PHR Santiago Valle Serra e Meira LR, Colussi CF: Feasibility evaluation of a mindfulness-based stress reduction program for primary care professionals in Brazilian national health system Complement Ther Clin Pract 35 8 Download references.
Institute for Health and Sport, Victoria University, Melbourne, Australia. Melbourne School of Population and Global Health, University of Melbourne, Melbourne, Australia. You can also search for this author in PubMed Google Scholar. RRD and ZP conceptualised the study.
RRD interpreted the findings and prepared the first draft. MdC and ZP interpreted the findings, revised the draft and contributed to writing the manuscript. All authors read and approved the final manuscript. Correspondence to Raja Ram Dhungana.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. Open Access This article is licensed under a Creative Commons Attribution 4. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material.
If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Reprints and permissions. Dhungana, R. Implementation of non-pharmacological interventions for the treatment of hypertension in primary care: a narrative review of effectiveness, cost-effectiveness, barriers, and facilitators.
BMC Prim. Care 23 , Download citation. Received : 05 April Accepted : 13 October Published : 24 November Anyone you share the following link with will be able to read this content:.
Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative. Skip to main content. Search all BMC articles Search. Download PDF. Abstract Background The current guidelines for the prevention, detection, evaluation, and management of hypertension recommend six types of non-pharmacological interventions: alcohol reduction, salt intake reduction, increased potassium intake, physical activity, weight loss, and heart-healthy diets.
Methods A thorough literature search was conducted in Embase, Google Scholar, and PubMed databases, to identify the most recent reviews or, in their absence, primary studies on alcohol reduction, salt intake reduction, potassium supplementation, physical activity, weight reduction, heart-healthy diets, and other non-pharmacological interventions for the treatment of hypertension in primary care.
Results Alcohol reduction is a non-pharmacological intervention for the treatment of hypertension in primary care with proven effectiveness, feasibility, and acceptability. Conclusions Available evidence suggests that more pragmatic, clinically feasible, and logistically simple interventions are required for sodium intake reduction, physical activity, and weight reduction in primary care settings.
Background There is a wealth of literature on alcohol intake, high salt intake, low potassium intake, physical inactivity, obesity, and unhealthy diet as key determinants of high blood pressure. Methods A thorough literature search was conducted in Embase, Google Scholar, and PubMed databases.
Alcohol reduction Brief alcohol interventions with the aim to reduce alcohol consumption have shown to be effective when delivered in the primary care setting [ 38 ]. Table 1 Summary of findings on non-pharmacological interventions for the treatment of hypertension in primary care Full size table.
Salt intake reduction Informational interventions and dietary counselling are the most common strategies applied to reduce salt intake in hypertensive patients [ 77 ]. Potassium intake The common potassium supplementation interventions in hypertensive individuals include increasing potassium intake from fruit and vegetables or using potassium supplements [ 19 , 62 ].
Physical activity Brief Intervention and exercise referral schemes are two common physical activity promoting approaches in primary care patients. Weight reduction Behaviour change interventions and restrictive diet are commonly used with the aim to reduce weight of primary care patients.
Heart-healthy diets Heart-healthy diets typically include the diets with high intake of fruits and vegetables, low fat intake, consumption of whole grains, and low sodium intake.
Other promising non-pharmacological interventions Emerging evidence suggests that other non-pharmacological interventions such as yoga, stress reduction, and healthy drinks could be beneficial for reducing blood pressure [ 27 , 30 , 34 ].
Conclusion Non-pharmacological interventions for the treatment of hypertension in primary care with proven effectiveness include alcohol reduction. Availability of data and materials All data generated or analysed during this study are included in this article.
References Roerecke M, Tobe SW, Kaczorowski J, Bacon SL, Vafaei A, Hasan OSM, Krishnan RJ, Raifu AO, Rehm J. Article PubMed Google Scholar Kieneker LM, Gansevoort RT, Mukamal KJ, de Boer RA, Navis G, Bakker SJ, Joosten MM.
Article CAS PubMed Google Scholar Al Tunaiji H, Davis JC, Mansournia MA, Khan KM. Article PubMed PubMed Central Google Scholar Jayedi A, Rashidy-Pour A, Khorshidi M, Shab-Bidar S. Article CAS PubMed Google Scholar Schwingshackl L, Schwedhelm C, Hoffmann G, Knüppel S, Iqbal K, Andriolo V, Bechthold A, Schlesinger S, Boeing H.
Article PubMed Google Scholar Jayedi A, Soltani S, Abdolshahi A, Shab-Bidar S. Article CAS PubMed Google Scholar Zhang Y, Zhang DZ. Article CAS PubMed Google Scholar Xin X, He J, Frontini Maria G, Ogden Lorraine G, Motsamai Oaitse I, Whelton Paul K. Article CAS PubMed Google Scholar Roerecke M, Kaczorowski J, Tobe SW, Gmel G, Hasan OSM, Rehm J.
Article PubMed PubMed Central Google Scholar Midgley JP, Matthew AG, Greenwood CMT, Logan AG. Article CAS PubMed Google Scholar Cutler JA, Follmann D, Allender PS. Article Google Scholar Graudal NA, Galloe AM, Garred P. Article CAS PubMed Google Scholar He F, MacGregor GA. Article CAS PubMed Google Scholar Graudal NA, Hubeck-Graudal T, Jurgens G: Effects of low sodium diet versus high sodium diet on blood pressure, renin, aldosterone, catecholamines, cholesterol, and triglyceride.
Article PubMed Google Scholar Graudal NA, Hubeck-Graudal T, Jurgens G. PubMed Google Scholar World Health Organization: Effect of increased potassium intake on blood pressure, renal function, blood lipids and other potential adverse effects.
Article PubMed Google Scholar Cornelissen VA, Fagard RH. Article CAS PubMed Google Scholar Cornelissen VA, Fagard RH, Coeckelberghs E, Vanhees L.
Article CAS PubMed Google Scholar Owen A, Wiles J, Swaine I. Article CAS PubMed Google Scholar Inder JD, Carlson DJ, Dieberg G, McFarlane JR, Hess NC, Smart NA. Article PubMed Google Scholar Zeigler ZS, Mullane SL, Crespo NC, Buman MP, Gaesser GA. Article PubMed Google Scholar Zeigler ZS, Swan PD, Bhammar DM, Gaesser GA.
Article PubMed Google Scholar Zomer E, Gurusamy K, Leach R, Trimmer C, Lobstein T, Morris S, James WP, Finer N. Article CAS PubMed Google Scholar Schwingshackl L, Chaimani A, Schwedhelm C, Toledo E, Pünsch M, Hoffmann G, Boeing H. Article CAS PubMed Google Scholar Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, Himmelfarb CD, DePalma SM, Gidding S, Jamerson KA, Jones DW.
Article PubMed Google Scholar Unger T, Borghi C, Charchar F, Khan NA, Poulter NR, Prabhakaran D, Ramirez A, Schlaich M, Stergiou GS, Tomaszewski M.
Article CAS PubMed Google Scholar Kimani S, Mirie W, Chege M, Okube OT, Muniu S. Article PubMed PubMed Central Google Scholar Whelton PK, Appel LJ, Espeland MA, Applegate WB, Ettinger J, Walter H, Kostis JB, Kumanyika S, Lacy CR, Johnson KC, Folmar S, et al. Article CAS PubMed Google Scholar Eckel Robert H, Jakicic John M, Ard Jamy D, de Jesus Janet M, Houston Miller N, Van Hubbard S, Lee IM, Lichtenstein Alice H, Loria Catherine M, Millen Barbara E, et al.
Article CAS PubMed Google Scholar Wu Y, Johnson BT, Acabchuk RL, Chen S, Lewis HK, Livingston J, Park CL, Pescatello LS.
PubMed Google Scholar Rehm J, Prieto JAA, Beier M, Duhot D, Rossi A, Schulte B, Zarco J, Aubin H-J, Bachmann M, Grimm C, et al. Article PubMed PubMed Central Google Scholar Quader ZS, Cogswell ME, Fang J, Coleman King SM, Merritt RK.
Article PubMed PubMed Central Google Scholar Booth HP, Prevost AT, Gulliford MC. Article PubMed Google Scholar Bertholet N, Daeppen JB, Wietlisbach V, Fleming M, Burnand B. Article PubMed Google Scholar Kaner EFS, Beyer FR, Muirhead C, Campbell F, Pienaar ED, Bertholet N, Daeppen JB, Saunders JB, Burnand B.
PubMed Google Scholar Chi FW, Weisner CM, Mertens JR, Ross TB, Sterling SA. Article PubMed PubMed Central Google Scholar Saitz R. Article PubMed PubMed Central Google Scholar Platt L, Melendez-Torres GJ, Donnell A, Bradley J, Newbury-Birch D, Kaner E, Ashton C. Article PubMed PubMed Central Google Scholar Rehm J, Anderson P, Prieto JAA, Armstrong I, Aubin HJ, Bachmann M, Bastus NB, Brotons C, Burton R, Cardoso M, et al.
Article PubMed PubMed Central Google Scholar Angus C, Latimer N, Preston L, Li J, Purshouse R. Article PubMed PubMed Central Google Scholar Glass JE, Andreasson S, Bradley KA, Finn SW, Williams EC, Bakshi AS, Gual A, Heather N, Sainz MT, Benegal V, et al. Article PubMed PubMed Central Google Scholar Rahm AK, Boggs JM, Martin C, Price DW, Beck A, Backer TE, Dearing JW.
Article PubMed Google Scholar Johnson M, Jackson R, Guillaume L, Meier P, Goyder E. Article CAS Google Scholar Hasin DS, Aharonovich E, Greenstein E. Article PubMed PubMed Central Google Scholar Stoner SA, Mikko AT, Carpenter KM. Article PubMed PubMed Central Google Scholar Donoghue K, Patton R, Phillips T, Deluca P, Drummond C.
Article PubMed PubMed Central Google Scholar Beyer F, Lynch E, Kaner E. Article PubMed PubMed Central Google Scholar Anderson P, Bendtsen P, Spak F, Reynolds J, Drummond C, Segura L, Keurhorst MN, Palacio-Vieira J, Wojnar M, Parkinson K, et al. Article PubMed Google Scholar Rose HL, Miller PM, Nemeth LS, Jenkins RG, Nietert PJ, Wessell AM, Ornstein S.
Article PubMed Google Scholar Ruzicka M, Hiremath S, Steiner S, Helis E, Szczotka A, Baker P, Fodor G: What is the feasibility of implementing effective sodium reduction strategies to treat hypertension in primary care settings? Article PubMed Google Scholar Mancia G, Oparil S, Whelton PK, McKee M, Dominiczak A, Luft FC, AlHabib K, Lanas F, Damasceno A, Prabhakaran D, et al.
PubMed Google Scholar Couch SC, Saelens BE, Levin L, Dart K, Falciglia G, Daniels SR. Article PubMed Google Scholar STRM Lima da Silva Nalin de Souza B, França AKT, Filho NS, Sichieri R: Dietary approach to hypertension based on low glycaemic index and principles of DASH Dietary Approaches to Stop Hypertension : a randomised trial in a primary care service Br J Nutr 8 Niiranen TJ, Leino K, Puukka P, Kantola I, Karanko H, Jula AM.
Article PubMed Google Scholar Campbell F, Blank L, Messina J, Day M, Buckley Woods H, Payne N, Goyder E, Armitage C. Google Scholar Campbell F, Holmes M, Everson-Hock E, Davis S, Buckley Woods H, Anokye N, Tappenden P, Kaltenthaler E. Article PubMed PubMed Central Google Scholar Anokye NK, Lord J, Fox-Rushby J.
Article PubMed Google Scholar Douglas F, Torrance N, van Teijlingen E, Meloni S, Kerr A. Article PubMed PubMed Central Google Scholar Morgan F, Battersby A, Weightman AL, Searchfield L, Turley R, Morgan H, Jagroo J, Ellis S.
Article PubMed PubMed Central Google Scholar Booth HP, Prevost TA, Wright AJ, Gulliford MC. Article PubMed PubMed Central Google Scholar Parretti HM, Jebb SA, Johns DJ, Lewis AL, Christian-Brown AM, Aveyard P.
Article CAS PubMed Google Scholar Daumit GL, Janssen EM, Jerome GJ, Dalcin AT, Charleston J, Clark JM, Coughlin JW, Yeh HC, Miller ER, Durkin N, et al. Article PubMed Google Scholar Kent S, Aveyard P, Astbury N, Mihaylova B, Jebb SA. Article PubMed Google Scholar Gupta H. PubMed PubMed Central Google Scholar Dewhurst A, Peters S, Devereux-Fitzgerald A, Hart J.
Article PubMed Google Scholar Tham M, Young D. Article PubMed PubMed Central Google Scholar Park HE, Billups SJ, Schilling LM: Physician perceived barriers and solutions to DASH diet recommendations for hypertension prevention and management.
Article PubMed Google Scholar Trieu K, McMahon E, Santos JA, Bauman A, Jolly KA, Bolam B, Webster J. Article PubMed PubMed Central Google Scholar Hooper L, Bartlett C, Davey Smith G, Ebrahim S.
Article PubMed PubMed Central Google Scholar Ferrara AL, Pacioni D, Di Fronzo V, Russo BF, Staiano L, Speranza E, Gente R, Gargiulo F, Ferrara F. Article PubMed Google Scholar Lin PH, Yancy WS Jr, Pollak KI, Dolor RJ, Marcello J, Samsa GP, Batch BC, Svetkey LP.
Article PubMed PubMed Central Google Scholar Yamasaki T, Sadanaga T, Hirota S. Article CAS PubMed PubMed Central Google Scholar Bhana N, Utter J, Eyles H. Article PubMed Google Scholar Ireland DM, Clifton PM, Keogh JB. htm ] Liem DG, Miremadi F, Zandstra EH, Keast RSJ.
pdf ] Cohn JN, Kowey PR, Whelton PK, Prisant LM. Article CAS PubMed Google Scholar Filippini T, Naska A, Kasdagli MI, Torres D, Lopes C, Carvalho C, Moreira P, Malavolti M, Orsini N, Whelton PK, et al. Article CAS PubMed PubMed Central Google Scholar Sidhu K, Sanjanwala R, Zieroth S.
Article PubMed Google Scholar Greer RC, Marklund M, Anderson CAM, Cobb LK, Dalcin AT, Henry M, Appel LJ. Article CAS PubMed Google Scholar Neal B, Wu Y, Feng X, Zhang R, Zhang Y, Shi J, Zhang J, Tian M, Huang L, Li Z, et al.
Article CAS PubMed Google Scholar Lamming L, Pears S, Mason D, Morton K, Bijker M, Sutton S, Hardeman W.
Article PubMed Google Scholar Morgan F, Turley RL, Morgan HE, Searchfield L, Weightman AL, Elliot E, Murphy S: Exercise referral schemes to promote physical activity: NICE; Article PubMed Google Scholar Eden KB, Orleans CT, Mulrow CD, Pender NJ, Teutsch SM.
Article PubMed PubMed Central Google Scholar Lin JS, O'Connor EA, Evans CV, Senger CA, Rowland MG, Groom HC: U. Article PubMed PubMed Central Google Scholar Wadden TA, Volger S, Tsai AG, Sarwer DB, Berkowitz RI, Diewald LK, Carvajal R, Moran CH, Vetter M.
Article PubMed PubMed Central Google Scholar Astbury NM, Aveyard P, Nickless A, Hood K, Corfield K, Lowe R, Jebb SA. Article PubMed PubMed Central Google Scholar Tsai AG, Wadden TA. Article PubMed Google Scholar Semlitsch T, Jeitler K, Berghold A, Horvath K, Posch N, Poggenburg S, Siebenhofer A.
PubMed Google Scholar Gulsin GS, Swarbrick DJ, Athithan L, Brady EM, Henson J, Baldry E, Argyridou S, Jaicim NB, Squire G, Walters Y, et al. Article CAS PubMed Google Scholar Brown A, Leeds AR. Article Google Scholar Wadden TA, Butryn ML, Hong PS, Tsai AG. Article CAS PubMed PubMed Central Google Scholar Gay HC, Rao SG, Vaccarino V, Ali MK.
Article CAS PubMed Google Scholar Kolasa KM. Article Google Scholar Blumenthal JA, Babyak MA, Hinderliter A, Watkins LL, Craighead L, Lin P-H, Caccia C, Johnson J, Waugh R, Sherwood A. Article PubMed PubMed Central Google Scholar Lin P-H, Appel LJ, Funk K, Craddick S, Chen C, Elmer P, McBurnie MA, Champagne C.
Article CAS PubMed Google Scholar Wong MCS, Wang HHX, Kwan MWM, Fong BCY, Chan WM, Zhang DX, Li STS, Yan BP, Coats AJS, Griffiths SM. Article CAS PubMed Google Scholar Kim H, Andrade FCD.
PubMed PubMed Central Google Scholar R Mahdavi Bagheri asl A, Abadi MAJ, Namazi N: Perceived Barriers to Following Dietary Recommendations in Hypertensive Patients J Am Coll Nutr 36 3 Conversano C, Orrù G, Pozza A, Miccoli M, Ciacchini R, Marchi L, Gemignani A.
Article PubMed PubMed Central Google Scholar Xie C, Cui L, Zhu J, Wang K, Sun N, Sun C. Article PubMed Google Scholar Mahdavi-Roshan M, Salari A, Ghorbani Z, Ashouri A. Article PubMed Google Scholar Wolff M, Sundquist K, Lonn SL, Midlov P. Article PubMed PubMed Central Google Scholar Wolff M, Rogers K, Erdal B, Chalmers JP, Sundquist K, Midlov P.
Article CAS PubMed Google Scholar Dhungana RR, Pedisic Z, Joshi S, Khanal MK, Kalauni OP, Shakya A, Bhurtel V, Panthi S, Ramesh Kumar KC, Ghimire B, et al. Article PubMed PubMed Central Google Scholar Momeni J, Omidi A, Raygan F, Akbari H. Article PubMed Google Scholar Demarzo MMP, Montero-Marin J, Cuijpers P, Zabaleta-del-Olmo E, Mahtani KR, Vellinga A, Vicens C, López-del-Hoyo Y, García-Campayo J.
Article PubMed PubMed Central Google Scholar PHR Santiago Valle Serra e Meira LR, Colussi CF: Feasibility evaluation of a mindfulness-based stress reduction program for primary care professionals in Brazilian national health system Complement Ther Clin Pract 35 8 17 Download references.
You might also get low potassium and low sodium after long-term use. You'll have regular blood tests to check for this. Beta blockers can reduce blood pressure by making your heart beat more slowly and with less force. They used to be a popular treatment for high blood pressure, but now tend to be used only when other treatments have not worked.
This is because beta blockers are considered less effective than other blood pressure medicines. Common examples are atenolol and bisoprolol. Possible side effects include dizziness, headaches, tiredness, and cold hands and feet.
While there are definite benefits from taking medicines to reduce blood pressure if you're under the age of 80, it's less clear it's useful if you're over It's now thought that if you reach 80 while you're taking medicine for high blood pressure, it's fine to continue treatment provided it's still helping you and is not causing side effects.
If you're diagnosed with high blood pressure and you're aged over 80, your doctor will also consider your other health risk factors when deciding whether to give you treatment for the high blood pressure.
Page last reviewed: 11 July Next review due: 11 July Home Health A to Z High blood pressure hypertension Back to High blood pressure hypertension.
Treatment - High blood pressure hypertension Contents Overview Causes Diagnosis Treatment Prevention. When treatment is recommended Everyone with high blood pressure is advised to make healthy lifestyle changes.
Try to: cut your salt intake to less than 6g 0. Get more advice about lifestyle changes to prevent and reduce high blood pressure Medicines for high blood pressure Several types of medicine can be used to help control high blood pressure. Many people need to take a combination of different medicines.
if you're under 55 years of age, or you're any age and have type 2 diabetes — you'll usually be offered an ACE inhibitor or an angiotensin-2 receptor blocker ARB if you're aged 55 or older, or you're any age and of African or Caribbean origin, and you do not have type 2 diabetes — you'll usually be offered a calcium channel blocker You may need to take blood pressure medicine for the rest of your life.
ACE inhibitors Angiotensin-converting enzyme ACE inhibitors reduce blood pressure by relaxing your blood vessels. Angiotensin-2 receptor blockers ARBs ARBs work in a similar way to ACE inhibitors.
Control is possible, but hyppertension progress has been made in the past 10 years. Some population Optimize digestion process also have higher rates of hypertenskon and death associated Digestion improvement benefits high blood pressure, which creates health disparities across hypertensioon, and programs and Managing hypertension with non-medical techniques likely yechniques tailoring to increase effectiveness. Many different groups will need to come together to support the use of proven strategies in every community and for every population group. Changing your lifestyle can be hard. You will need support from your family, friends, and other members of your community. You can also get help from a health care team that may include physicians, nurse practitioners, physician assistants, nurses, pharmacists, and other types of health care professionals. Your health care team can help you make lifestyle or medication changes that can help you reduce your risk of heart attack or stroke.
ich beglückwünsche, dieser sehr gute Gedanke fällt gerade übrigens
Sie sind nicht recht. Geben Sie wir werden es besprechen. Schreiben Sie mir in PM, wir werden umgehen.