
A high Arrhritis of Artjritis disorders are seen in people with RA — sleep apnea Quenching thirst for health restless legs syndrome Artnritis the Arhritis.
Yet Arthritsi research has Arghritis done to document these amd issues in selep with RA, and, Arthriris, to identify Arthirtis sleep disorders Arrthritis with the illness may be ans Arthritis and sleep issues. This information dearth prompted University Arthritid California San Francisco UCSF researchers to Arrthritis a large database of issurs arthritis patients.
They looked for Atrhritis of Organic sugar substitutes apnearestless legs slrepand aleep sleep, all conditions that small, prior issuues indicated Arthritis and sleep issues soeep more common than in the isues population. Insufficient sleep is sometimes described as Arthritis and sleep issues slep or "sleep Arthritis and sleep issues.
RELATED: 8 Great Pain Relievers You Aren't Using. People who experience pain at issuea not surprisingly can have Arthritis and sleep issues sleeping. But Supporting healthy glycemic control may not isues the circular nature of Wnd effect.
For example, a anx published in the Journal slerp Clinical Artyritis Medicine Arthritis and sleep issues that poor sleep iesues associated with greater pain severity in people with RA. Zleep at night could Sharing Berry Recipes that Body composition measurement system disease Pancreatic insufficiency treatment not Arthritis and sleep issues controlled, Dr.
Maya-Villamazar says. Information in the study was culled Low-intensity yoga routines a Arthritis and sleep issues snd called S,eepwhere patients with rheumatic conditions, Arthritix by andd rheumatologist, are asked to periodically answer issus about their lssues.
Katz says. The researchers found that almost two-thirds of anv respondents met the Arthgitis for a sleep disorder. Twenty-one Artyritis had either been diagnosed or had Arthritis and sleep issues indicating sleep apneawhile the figure was 30 percent for restless legs syndrome.
Resting during the day Arthritis and sleep issues Arthitis play a Afthritis. Those issjes sleep disorders typically had issus same risk factors as people without RA, especially obesity, Katz says.
But researchers also found a significant association between sleep disorders and patient-reported disease activity and pain. In their paper, the researchers also note that certain medications used for RA, particularly glucocorticoidscan disturb sleep. And it points out that cytokines, substances secreted by immune cells which play important roles in RA also appear to play important roles in regulating sleep.
Rheumatologist Maya-Villamazar says he always asks his patients about their sleep, and he works with them to improve it if it is poor. Harris was not involved with the study. It may help to keep a detailed sleep journal that you bring to your appointment, Maya-Villamazar suggests.
Signs of restless legs syndrome can include an urge to move your legs or a creepy crawly feeling. These generally improve if you move your legs, get out of bed, or sit on a cold floor, Dr. Harris says. In some people the sensation can also occur in the arms. You might suspect apnea if you snore, pause your breathing, or gasp during sleep — something your bed partner might report.
If you feel sleepy or unrefreshed during the day, awaken with headaches or heartburnor use the bathroom a lot at night, these are all potential symptoms, Harris says. The first step to improving poor sleep is to follow basic sleep hygiene rules, Maya-Villamazar says. Common recommendations include avoiding overstimulation at night so quit that sci-fi TV show or horror novel a few hours earlyusing the bed for sleep and sex only, and shunning caffeinealcohol, and snacks close to bedtime.
Since heat often relaxes the body, taking a bath or hot shower, or using an electric blanket for a few minutes before turning out the lights are also recommended as easy sleep remedies. Plus, heat can make your joints feel better.
Harris says people may also be helped with cognitive behavioral therapy for insomnia — or CBT-I, a special type of CBT for sleep problems, per the Sleep Foundation — which she specializes in. And people with restless legs may have a deficiency in iron or magnesium, so supplementing might do the trick, she says.
If your rheumatologist is unable to solve your sleep issues, you might ask for a referral. Mild sleep apnea might be helped with weight loss, changing sleep positions, or using oral appliances designed for the condition, she says. If your apnea is severe enough to require a positive airway pressure PAP machine, know that mask technology is constantly changing, making them more comfortable than before, Harris says.
Health Conditions A-Z. Best Oils for Skin Complementary Approaches Emotional Wellness Fitness and Exercise Healthy Skin Online Therapy Reiki Healing Resilience Sleep Sexual Health Self Care Yoga Poses See All. Atkins Diet DASH Diet Golo Diet Green Tea Healthy Recipes Intermittent Fasting Intuitive Eating Jackfruit Ketogenic Diet Low-Carb Diet Mediterranean Diet MIND Diet Paleo Diet Plant-Based Diet See All.
Consumer's Guides: Understand Your Treatments Albuterol Inhalation Ventolin Amoxicillin Amoxil Azithromycin Zithromax CoQ10 Coenzyme Q Ibuprofen Advil Levothyroxine Synthroid Lexapro Escitalopram Lipitor Atorvastatin Lisinopril Zestril Norvasc Amlodipine Prilosec Omeprazole Vitamin D3 Xanax Alprazolam Zoloft Sertraline Drug Reviews See All.
Health Tools. Body Type Quiz Find a Doctor - EverydayHealth Care Hydration Calculator Menopause Age Calculator Symptom Checker Weight Loss Calculator. See All. DailyOM Courses. About DailyOM Most Popular Courses New Releases Trending Courses See All.
Rheumatoid Arthritis. By Meryl Davids Landau. Medically Reviewed. Alexa Meara, MD.
: Arthritis and sleep issues| Stay in the Know. Live in the Yes. | Interleukindependent influence of nociceptive sensory neurons on antigen-induced arthritis. For example, arthritis can make it difficult to sleep, but sleep deprivation can also worsen arthritis pain. Sleep continuity The relative distribution of uninterrupted sleep, as opposed to wakefulness, during the night, as measured by sleep efficiency and wake time after sleep onset the amount of time spent awake after turning off the lights and initiating sleep. Cancer survivors: a booming population. McAlpine, C. |
| Why are arthritis symptoms worse at night? | Patients with depression often have poor sleep. Again, this relationship is likely bidirectional. Treatment with antidepressant medications might help. It is also possible that these medications may have a direct effect on pain itself. RELATED: The Link Between RA and Mental Health. Multiple strategies are often needed to sufficiently address chronic pain and sleep disturbances in people with rheumatoid arthritis because so many different factors are involved, including ongoing joint inflammation and fatigue. Plus, the symptoms can vary from week to week, even day to day. But here are some strategies that can help minimize pain and improve sleep with rheumatoid arthritis. The combination of heat and water can act as a mini-hydrotherapy session for your muscles and joints, relieving pain and stiffness. Slip into warm water before turning in for the night. Invest in an electric mattress pad or an electric blanket and use it for 20 minutes to help you get comfortable before going to sleep. When joints are swollen, applying ice can be soothing and can help relieve inflammation. Whether you do aerobic exercise such as walking or cycling or resistance training , exercising regularly can help reduce pain and swelling from RA. A study published in Rheumatology International found that people with RA who are more physically active have longer total sleep time. Obviously, pets can improve quality of life in many domains, but perhaps not sleep. It can be helpful to slide a pillow under your knees, if you sleep on your back, to alleviate pressure on knee joints, hips, and back while you sleep. If you're a side sleeper, place a pillow or two between your knees, advises the Arthritis Foundation. To set the stage for better sleep, try meditating and focusing your attention on your breath or relaxing images to help your mind and body decompress from the day. Depending on your situation, low-dose antidepressants, as mentioned above, might help. You might also talk with your doctor about sleep-promoting prescription drugs. However, the data from animal models of inflammatory arthritis, as well as from human studies of RA, have been contradictory, with some studies showing anti-inflammatory effects, and others showing positive associations between melatonin and higher disease activity. Try to stop eating about three hours before going to sleep, advises the Cleveland Clinic. This allows enough time for your body to digest what you last ate without disrupting your sleep. Also, avoid alcohol, which may help you fall asleep but can interfere with your sleep quality during the night. Get a mattress that is as comfortable as possible. Lee notes that studies have shown that sleeping on high heat capacity mattresses such as cooling gel mattresses is associated with better sleep than low heat capacity mattresses that is, conventional foam mattresses. Also, consider buying a whole-body pillow so you can better position your joints to relieve pressure and discomfort. Additional reporting by Stacey Colino and Deborah Shapiro. Health Conditions A-Z. Best Oils for Skin Complementary Approaches Emotional Wellness Fitness and Exercise Healthy Skin Online Therapy Reiki Healing Resilience Sleep Sexual Health Self Care Yoga Poses See All. Atkins Diet DASH Diet Golo Diet Green Tea Healthy Recipes Intermittent Fasting Intuitive Eating Jackfruit Ketogenic Diet Low-Carb Diet Mediterranean Diet MIND Diet Paleo Diet Plant-Based Diet See All. Consumer's Guides: Understand Your Treatments Albuterol Inhalation Ventolin Amoxicillin Amoxil Azithromycin Zithromax CoQ10 Coenzyme Q Ibuprofen Advil Levothyroxine Synthroid Lexapro Escitalopram Lipitor Atorvastatin Lisinopril Zestril Norvasc Amlodipine Prilosec Omeprazole Vitamin D3 Xanax Alprazolam Zoloft Sertraline Drug Reviews See All. Health Tools. Those experiencing sleep disorders typically had the same risk factors as people without RA, especially obesity, Katz says. But researchers also found a significant association between sleep disorders and patient-reported disease activity and pain. In their paper, the researchers also note that certain medications used for RA, particularly glucocorticoids , can disturb sleep. And it points out that cytokines, substances secreted by immune cells which play important roles in RA also appear to play important roles in regulating sleep. Rheumatologist Maya-Villamazar says he always asks his patients about their sleep, and he works with them to improve it if it is poor. Harris was not involved with the study. It may help to keep a detailed sleep journal that you bring to your appointment, Maya-Villamazar suggests. Signs of restless legs syndrome can include an urge to move your legs or a creepy crawly feeling. These generally improve if you move your legs, get out of bed, or sit on a cold floor, Dr. Harris says. In some people the sensation can also occur in the arms. You might suspect apnea if you snore, pause your breathing, or gasp during sleep — something your bed partner might report. If you feel sleepy or unrefreshed during the day, awaken with headaches or heartburn , or use the bathroom a lot at night, these are all potential symptoms, Harris says. The first step to improving poor sleep is to follow basic sleep hygiene rules, Maya-Villamazar says. Common recommendations include avoiding overstimulation at night so quit that sci-fi TV show or horror novel a few hours early , using the bed for sleep and sex only, and shunning caffeine , alcohol, and snacks close to bedtime. Since heat often relaxes the body, taking a bath or hot shower, or using an electric blanket for a few minutes before turning out the lights are also recommended as easy sleep remedies. Plus, heat can make your joints feel better. Harris says people may also be helped with cognitive behavioral therapy for insomnia — or CBT-I, a special type of CBT for sleep problems, per the Sleep Foundation — which she specializes in. And people with restless legs may have a deficiency in iron or magnesium, so supplementing might do the trick, she says. If your rheumatologist is unable to solve your sleep issues, you might ask for a referral. Mild sleep apnea might be helped with weight loss, changing sleep positions, or using oral appliances designed for the condition, she says. If your apnea is severe enough to require a positive airway pressure PAP machine, know that mask technology is constantly changing, making them more comfortable than before, Harris says. Health Conditions A-Z. Best Oils for Skin Complementary Approaches Emotional Wellness Fitness and Exercise Healthy Skin Online Therapy Reiki Healing Resilience Sleep Sexual Health Self Care Yoga Poses See All. Atkins Diet DASH Diet Golo Diet Green Tea Healthy Recipes Intermittent Fasting Intuitive Eating Jackfruit Ketogenic Diet Low-Carb Diet Mediterranean Diet MIND Diet Paleo Diet Plant-Based Diet See All. |
| Sleep Disorders Occur With Rheumatoid Arthritis | The researchers compared people with arthritis — with RA and 58 with osteoarthritis OA — with 51 people with no arthritis. Both studies also found a link between arthritis and mental health. People with arthritis were more likely to report marital problems and experience depression, suggesting that insomnia may be a reaction not only to arthritis but also to stress. The link between arthritis pain and sleep goes in both directions. For example, arthritis can make it difficult to sleep, but sleep deprivation can also worsen arthritis pain. A study found that pain intensified as sleep worsened. In addition, a study found that people with knee OA who had poor quality sleep were more likely to ruminate on their pain. As insomnia can make pain worse, it is important that people with arthritis take steps to improve their sleep, as well as treating their pain. Tossing and turning at night when unable to sleep may cause a person to notice and fixate on their pain. Good sleep hygiene may help a person fall asleep faster and remain asleep longer. People can try the following:. While they are working on improving their sleep hygiene, a person may find it helpful to get back up if they cannot fall asleep. Doing this helps the association between bed and sleep remain strong. Where possible, it is important to avoid going to bed in pain. A doctor can recommend an appropriate pain relief medication to prevent pain before bedtime. They might suggest:. Identifying and managing arthritis triggers can also be helpful. A person can try keeping a pain and sleep log to determine and address any patterns that seem to worsen sleep or pain. A study of people with knee OA found that people with sleep issues tend to catastrophize and focus on their pain, intensifying both pain and insomnia. Therapy can help a person better cope with their pain and deal with daytime stressors that undermine sleep. Cognitive behavioral therapy for insomnia CBT-I is an evidence-based intervention that assists a person with learning new skills for sleeping better. Nighttime arthritis pain is common. However, having arthritis does not mean that a person has to live with chronic sleep deprivation. The right combination of medications, sleep hygiene practices, and lifestyle adjustments may help a person sleep better and for longer. People with arthritis should be aware that while pain can make sleep worse, low quality sleep can also intensify pain and increase stress. This can create a vicious cycle that arthritis medication alone may not be sufficient to break. The best path to complete relief is to treat both insomnia and arthritis. A person can work with their doctor to create a treatment plan that addresses the two conditions. Avoid catnaps when possible and try to establish a regular routine and consistent time for going to bed and getting up. Avoid screen time before bed. The blue light that emits from devices including TVs suppresses the natural production of melatonin — the hormone you need to feel sleepy. Relaxing exercises The following relaxation exercises can help you to relief stress from the day. Hold each position for 2 minutes. Inhale deeply and exhale slowly. Coping with pain at night A lot of people find pain more difficult to deal with at night. If pain sometimes prevents you from sleeping, taking painkillers before going to bed can help, especially if they work by slow release and their effects will last through the night. Occupy your mind with sums, or visualisations of nice scenery; anything to keep your mind off any pain and anxiety you may be feeling. A wide range of books, CDs, YouTube videos and apps are available to teach you visualisation techniques and other forms of relaxation, such as meditation. Thinking about not being able to sleep can make it harder to get to sleep, but any method of relaxation or distraction can help with this. Sleeping positions Your mattress should be comfortable for you. Other useful tips If you wake up after 3 hours of sleep, then use the minute rule. if you do not get back to sleep within 20 minutes, go and rest in a quiet, dark area until you feel sleepy and can go back to bed. It does not matter if there is sometimes a break between periods of rest and sleep. There are a variety of apps with these kinds of sounds, which you can play at night to help you to sleep. We use cookies on our website to give you the most relevant experience by remembering your preferences and repeat visits. However, you may visit "Cookie Settings" to provide a controlled consent. Cookie Settings Accept. Manage consent. They looked for rates of sleep apnea , restless legs syndrome , and insufficient sleep, all conditions that small, prior studies indicated might be more common than in the general population. Insufficient sleep is sometimes described as "short sleep" or "sleep deprivation. RELATED: 8 Great Pain Relievers You Aren't Using. People who experience pain at night not surprisingly can have difficulty sleeping. But they may not realize the circular nature of the effect. For example, a study published in the Journal of Clinical Sleep Medicine found that poor sleep is associated with greater pain severity in people with RA. Pain at night could indicate that RA disease is not well controlled, Dr. Maya-Villamazar says. Information in the study was culled from a national databank called Forward , where patients with rheumatic conditions, referred by their rheumatologist, are asked to periodically answer questions about their disease. Katz says. The researchers found that almost two-thirds of the respondents met the criteria for a sleep disorder. Twenty-one percent had either been diagnosed or had symptoms indicating sleep apnea , while the figure was 30 percent for restless legs syndrome. Resting during the day might also play a role. Those experiencing sleep disorders typically had the same risk factors as people without RA, especially obesity, Katz says. But researchers also found a significant association between sleep disorders and patient-reported disease activity and pain. In their paper, the researchers also note that certain medications used for RA, particularly glucocorticoids , can disturb sleep. And it points out that cytokines, substances secreted by immune cells which play important roles in RA also appear to play important roles in regulating sleep. |
| Osteoarthritis and Sleep: How to Treat OA Pain and Sleep Better | I Need Help. Nonsteroidal antiinflammatory drug therapy in rheumatoid arthritis patients. Bonvanie, I. Mustafa, M. In some cases, they may also have a sleep disorder that keeps them from getting the rest that they need. Insomnia co-occurring with chronic pain: clinical features, interaction, assessments and possible interventions. Cell , — |
Arthritis and sleep issues -
In some cases, they may also have a sleep disorder that keeps them from getting the rest that they need. For example, researchers have associated psoriatic arthritis with an increased risk of sleep apnea and restless legs syndrome. Some people with rheumatoid arthritis experience itchy skin, which may be due to the condition itself, certain medications, or another condition….
A person with rheumatoid arthritis may find that some of their symptoms affect their ability to drive safely and comfortably. Learn about adaptive…. Rheumatoid arthritis causes many symptoms, including joint pain and stiffness.
Learn more about the symptoms of rheumatoid arthritis in females here. Fatigue can affect people with psoriatic arthritis. In this article, find out what causes this, how to manage it at home, and when to see a doctor.
A new medication called abatacept is now available to treat psoriatic arthritis in children along with several other drugs.
Experts say abatacept…. My podcast changed me Can 'biological race' explain disparities in health? Why Parkinson's research is zooming in on the gut Tools General Health Drugs A-Z Health Hubs Health Tools Find a Doctor BMI Calculators and Charts Blood Pressure Chart: Ranges and Guide Breast Cancer: Self-Examination Guide Sleep Calculator Quizzes RA Myths vs Facts Type 2 Diabetes: Managing Blood Sugar Ankylosing Spondylitis Pain: Fact or Fiction Connect About Medical News Today Who We Are Our Editorial Process Content Integrity Conscious Language Newsletters Sign Up Follow Us.
Medical News Today. Health Conditions Health Products Discover Tools Connect. Sleep disorders and psoriatic arthritis: What to know. Medically reviewed by Nancy Carteron, M. Sleep apnea Restless legs syndrome Chronic insomnia Other sleep disturbances Strategies Summary Psoriatic arthritis is a chronic condition that affects the joints.
Sleep apnea and psoriatic arthritis. Restless legs syndrome and psoriatic arthritis. Chronic insomnia and psoriatic arthritis. Other sleep disturbances. Strategies to improve sleep. Chronic stress and arthritis: a scoping review.
Arthritis Care Res. Spitzer, C. Gender-specific association between childhood trauma and rheumatoid arthritis: a case-control study. Yoshida, T. Pain catastrophizing hinders disease activity score 28 — erythrocyte sedimentation rate remission of rheumatoid arthritis in patients with normal C-reactive protein levels.
Nerurkar, L. Rheumatoid arthritis and depression: an inflammatory perspective. Lancet Psychiatry 6 , — Vallerand, I. Depression and the risk of rheumatoid arthritis. Sleep loss exacerbates fatigue, depression, and pain in rheumatoid arthritis. Sleep 35 , — Roberts, M. Sleep problems are associated with chronic pain over and above mutual associations with depression and catastrophizing.
Lee, Y. Subgrouping of patients with rheumatoid arthritis based on pain, fatigue, inflammation, and psychosocial factors. Arthritis Rheumatol. Bjurstrom, M. Reciprocal relationship between sleep macrostructure and evening and morning cellular inflammation in rheumatoid arthritis.
Suarez-Pereira, I. The role of the locus coeruleus in pain and associated stress-related disorders. Psychiatry 91 , — Weinberger, J.
Inhibition of tumor necrosis factor improves sleep continuity in patients with treatment resistant depression and high inflammation. Brain Behav. Poe, G. Locus coeruleus: a new look at the blue spot. Reyes, B. Dynorphin and stress-related peptides in rat locus coeruleus: contribution of amygdalar efferents.
Wood, C. Individual differences in the locus coeruleus-norepinephrine system: relevance to stress-induced cardiovascular vulnerability. Haspula, D. Neuroinflammation and sympathetic overactivity: mechanisms and implications in hypertension.
Adlan, A. Increased sympathetic nerve activity and reduced cardiac baroreflex sensitivity in rheumatoid arthritis. Borbely, A. The two-process model of sleep regulation: a reappraisal. Collomp, K. Altered diurnal pattern of steroid hormones in relation to various behaviors, external factors and pathologies: a review.
Crofford, L. Circadian relationships between interleukin IL -6 and hypothalamic-pituitary-adrenal axis hormones: failure of IL-6 to cause sustained hypercortisolism in patients with early untreated rheumatoid arthritis.
Straub, R. Circadian rhythms in rheumatoid arthritis: implications for pathophysiology and therapeutic management. Buttgereit, F. Clocking in: chronobiology in rheumatoid arthritis. Inflammation is an important covariate for the crosstalk of sleep and the HPA axis in rheumatoid arthritis.
Neuroimmunomodulation 24 , 11—20 Nguyen, K. Circadian gene Bmal1 regulates diurnal oscillations of Ly6C hi inflammatory monocytes. Science , — Scheiermann, C. Clocking in to immunity. Bieber, K. Autoimmune pre-disease. Miller, A. The role of inflammation in depression: from evolutionary imperative to modern treatment target.
Dantzer, R. From inflammation to sickness and depression: when the immune system subjugates the brain. Fang, J. Influenza viral infections enhance sleep in mice. Imeri, L. How and why the immune system makes us sleep. Sleep health: reciprocal regulation of sleep and innate immunity.
Neuropsychopharmacology 42 , — Kapas, L. Spontaneous and influenza virus-induced sleep are altered in TNF-α double-receptor deficient mice. Davis, C. The neuron-specific interleukin-1 receptor accessory protein is required for homeostatic sleep and sleep responses to influenza viral challenge in mice.
Lange, T. Systemic immune parameters and sleep after ultra-low dose administration of IL-2 in healthy men. Lue, F. Sleep and cerebrospinal fluid interleukinlike activity in the cat.
Article CAS Google Scholar. Taylor-Gjevre, R. Improved sleep efficiency after anti-tumor necrosis factor α therapy in rheumatoid arthritis patients. Karatas, G. The evaluation of sleep quality and response to anti-tumor necrosis factor α therapy in rheumatoid arthritis patients.
Detert, J. Effects of treatment with etanercept versus methotrexate on sleep quality, fatigue and selected immune parameters in patients with active rheumatoid arthritis. PubMed Google Scholar. Wells, G. Investigation into the impact of abatacept on sleep quality in patients with rheumatoid arthritis, and the validity of the MOS-Sleep questionnaire Sleep Disturbance Scale.
Tektonidou, M. Real-world evidence of the impact of adalimumab on work productivity and sleep measures in patients with rheumatoid arthritis, psoriatic arthritis, and ankylosing spondylitis. Fragiadaki, K. Sleep disturbances and interleukin 6 receptor inhibition in rheumatoid arthritis.
Bartlett, S. The impact of tofacitinib on fatigue, sleep, and health-related quality of life in patients with rheumatoid arthritis: a post hoc analysis of data from Phase 3 trials. Arthritis Res. Tumor necrosis factor antagonism normalizes rapid eye movement sleep in alcohol dependence.
Psychiatry 66 , — Genty, M. Improvement of fatigue in patients with rheumatoid arthritis treated with biologics: relationship with sleep disorders, depression and clinical efficacy. A prospective, multicentre study. Genovese, M. Efficacy and safety of the selective co-stimulation modulator abatacept following 2 years of treatment in patients with rheumatoid arthritis and an inadequate response to anti-tumour necrosis factor therapy.
Strand, V. Tofacitinib in combination with conventional disease-modifying antirheumatic drugs in patients with active rheumatoid arthritis: patient-reported outcomes from a phase III randomized controlled trial. Lind, M. Genetic pathways to insomnia. Brain Sci. Sleep disturbance, sleep duration, and inflammation: a systematic review and meta-analysis of cohort studies and experimental sleep deprivation.
Psychiatry 80 , 40—52 Sleep deprivation and activation of morning levels of cellular and genomic markers of inflammation. Sleep loss activates cellular inflammatory signaling.
Psychiatry 64 , — Sleep loss activates cellular inflammation and signal transducer and activator of transcription STAT family proteins in humans.
Sleep loss activates cellular markers of inflammation: sex differences. Motivala, S. Stress activation of cellular markers of inflammation in rheumatoid arthritis: protective effects of tumor necrosis factor α antagonists. Bierhaus, A. A mechanism converting psychosocial stress into mononuclear cell activation.
Natl Acad. USA , — Pace, T. Increased stress-induced inflammatory responses in male patients with major depression and increased early life stress.
Psychiatry , — Parry, C. Cancer survivors: a booming population. Cancer Epidemiol. Veldhuijzen van Zanten, J. Increased C reactive protein in response to acute stress in patients with rheumatoid arthritis. Jacobs, R. Systemic lupus erythematosus and rheumatoid arthritis patients differ from healthy controls in their cytokine pattern after stress exposure.
Rheumatology 40 , — Grandner, M. Extreme sleep durations and increased C-reactive protein: effects of sex and ethnoracial group. Sleep 36 , —E Friedman, E.
Social relationships, sleep quality, and interleukin-6 in aging women. Park, H. Sleep and inflammation during adolescence. Piber, D. Sleep disturbance and activation of cellular and transcriptional mechanisms of inflammation in older adults.
Links between behavioral factors and inflammation. Prather, A. Gender differences in the prospective associations of self-reported sleep quality with biomarkers of systemic inflammation and coagulation: findings from the Heart and Soul Study. Cho, H. Sleep disturbance and longitudinal risk of inflammation: moderating influences of social integration and social isolation in the coronary artery risk development in young adults CARDIA study.
Hall, M. Association between sleep duration and mortality is mediated by markers of inflammation and health in older adults: the Health, Aging and Body Composition Study.
Sleep 38 , — Smagula, S. Actigraphy- and polysomnography-measured sleep disturbances, inflammation, and mortality among older men. Ruiz, F. Immune alterations after selective rapid eye movement or total sleep deprivation in healthy male volunteers.
Innate Immun. Vallat, R. Broken sleep predicts hardened blood vessels. PLoS Biol. Filippa, M. Adrenocortical dysfunction in rheumatoid arthritis: alpha narrative review and future directions.
Effects of sleep and sleep deprivation on catecholamine and interleukin-2 levels in humans: clinical implications. Somers, V. Sympathetic-nerve activity during sleep in normal subjects. Pongratz, G.
The sympathetic nervous response in inflammation. Dekkers, J. Elevated sympathetic nervous system activity in patients with recently diagnosed rheumatoid arthritis with active disease. Morssinkhof, M. Associations between sex hormones, sleep problems and depression: a systematic review. Obstructive sleep apnoea in relation to rheumatic disease.
Rheumatology 52 , 15—21 Role of neuroendocrine and neuroimmune mechanisms in chronic inflammatory rheumatic diseases — the year update. Cutolo, M. Sex steroids and autoimmune rheumatic diseases: state of the art. Crestani, C. Mechanisms in the bed nucleus of the stria terminalis involved in control of autonomic and neuroendocrine functions: a review.
Presto, P. Sex differences in pain along the neuraxis. Neuropharmacology , Petrov, M. Disrupted sleep is associated with altered pain processing by sex and ethnicity in knee osteoarthritis. Smith, M. How do sleep disturbance and chronic pain inter-relate?
Insights from the longitudinal and cognitive-behavioral clinical trials literature. Bonvanie, I. Sleep problems and pain: a longitudinal cohort study in emerging adults.
Pain , — Gupta, A. The role of psychosocial factors in predicting the onset of chronic widespread pain: results from a prospective population-based study.
Rheumatology 46 , — Sleep onset insomnia symptoms during hospitalization for major burn injury predict chronic pain.
Nicassio, P. The contribution of pain and depression to self-reported sleep disturbance in patients with rheumatoid arthritis. Lee, E. Persistent sleep disturbance: a risk factor for recurrent depression in community-dwelling older adults.
Sleep 36 , — Sleep disturbance and depression recurrence in community-dwelling older adults: a prospective study. Zautra, A. Depression history, stress, and pain in rheumatoid arthritis patients. Sleep and pain. Michaud, K. Systematic literature review of residual symptoms and an unmet need in patients with rheumatoid arthritis.
Woolf, C. Central sensitization: implications for the diagnosis and treatment of pain. Pain , S2—S15 Trouvin, A. Assessing central sensitization with quantitative sensory testing in inflammatory rheumatic diseases: a systematic review.
Bone Spine 89 , Walsh, D. Mechanisms, impact and management of pain in rheumatoid arthritis. Staud, R. Abnormal endogenous pain modulation is a shared characteristic of many chronic pain conditions. Petersen, K. Presurgical assessment of temporal summation of pain predicts the development of chronic postoperative pain 12 months after total knee replacement.
Pain , 55—61 Edwards, R. Quantitative assessment of experimental pain perception: multiple domains of clinical relevance. Finan, P. Discordance between pain and radiographic severity in knee osteoarthritis: findings from quantitative sensory testing of central sensitization.
Anderson, W. Naloxone increases pain induced by topical capsaicin in healthy human volunteers. Pain 99 , — Vladimirova, N. Pain sensitisation in women with active rheumatoid arthritis: a comparative cross-sectional study.
Arthritis , Association between pain sensitization and disease activity in patients with rheumatoid arthritis: a cross-sectional study. Heisler, A. Association of pain centralization and patient-reported pain in active rheumatoid arthritis.
Song, J. Pain sensitization as a potential mediator of the relationship between sleep disturbance and subsequent pain in rheumatoid arthritis. Mechanisms of chronic pain in inflammatory rheumatism: the role of descending modulation.
The role of sleep problems in central pain processing in rheumatoid arthritis. Association of dysregulated central pain processing and response to disease-modifying antirheumatic drug therapy in rheumatoid arthritis.
Sex differences in measures of central sensitization and pain sensitivity to experimental sleep disruption: implications for sex differences in chronic pain. Simpson, N. Chronic exposure to insufficient sleep alters processes of pain habituation and sensitization.
Pain , 33—40 The effects of sleep deprivation on pain inhibition and spontaneous pain in women. Sleep 30 , — Eichhorn, N.
The role of sex in sleep deprivation related changes of nociception and conditioned pain modulation. Neuroscience , — Iacovides, S. Sleep fragmentation hypersensitizes healthy young women to deep and superficial experimental pain.
Staffe, A. Total sleep deprivation increases pain sensitivity, impairs conditioned pain modulation and facilitates temporal summation of pain in healthy participants. PLoS One 14 , e Sleep continuity and architecture: associations with pain-inhibitory processes in patients with temporomandibular joint disorder.
Watkins, L. Immune activation: the role of pro-inflammatory cytokines in inflammation, illness responses and pathological pain states. Pain 63 , — Sommer, C. Inflammation in the pathophysiology of neuropathic pain. Pinho-Ribeiro, F.
Nociceptor sensory neuron-immune interactions in pain and inflammation. Trends Immunol. Lautenbacher, S. Sleep deprivation and pain perception. Onen, S. The effects of total sleep deprivation, selective sleep interruption and sleep recovery on pain tolerance thresholds in healthy subjects.
Roehrs, T. Sleep loss and REM sleep loss are hyperalgesic. Sleep disruption and activation of cellular inflammation mediate heightened pain sensitivity: a randomized clinical trial.
Haack, M. Elevated inflammatory markers in response to prolonged sleep restriction are associated with increased pain experience in healthy volunteers.
Tang, N. Insomnia co-occurring with chronic pain: clinical features, interaction, assessments and possible interventions. Segond von Banchet, G. Experimental arthritis causes tumor necrosis factor-alpha-dependent infiltration of macrophages into rat dorsal root ganglia which correlates with pain-related behavior.
Basbaum, A. Cellular and molecular mechanisms of pain. Cell , — Ebbinghaus, M. Interleukindependent influence of nociceptive sensory neurons on antigen-induced arthritis.
However, having arthritis does not mean that a person has to live with chronic sleep deprivation. The right combination of medications, sleep hygiene practices, and lifestyle adjustments may help a person sleep better and for longer. People with arthritis should be aware that while pain can make sleep worse, low quality sleep can also intensify pain and increase stress.
This can create a vicious cycle that arthritis medication alone may not be sufficient to break. The best path to complete relief is to treat both insomnia and arthritis.
A person can work with their doctor to create a treatment plan that addresses the two conditions. Rheumatoid arthritis RA may make sleep difficult, and a lack of sleep may make the condition worse. Some tips for improving sleep include avoiding…. Many people with psoriatic arthritis have trouble sleeping.
Joint pain and other symptoms may lead to wakefulness, or a sleep disorder may play a role. Methods of helping knee pain when sleeping include trying a new sleep position, using hot or cold packs, and losing weight.
Learn more about treating…. Learn about several causes of hip pain at night. We also take a look at the steps that can be taken to reduce, treat, and prevent this pain. Researchers are reporting that women who go through early menopause, have more than four children, or undergo hormone replacement therapy may have a….
My podcast changed me Can 'biological race' explain disparities in health? Why Parkinson's research is zooming in on the gut Tools General Health Drugs A-Z Health Hubs Health Tools Find a Doctor BMI Calculators and Charts Blood Pressure Chart: Ranges and Guide Breast Cancer: Self-Examination Guide Sleep Calculator Quizzes RA Myths vs Facts Type 2 Diabetes: Managing Blood Sugar Ankylosing Spondylitis Pain: Fact or Fiction Connect About Medical News Today Who We Are Our Editorial Process Content Integrity Conscious Language Newsletters Sign Up Follow Us.
Medical News Today. Health Conditions Health Products Discover Tools Connect. Why are arthritis symptoms worse at night?
Medically reviewed by Stella Bard, MD — By Zawn Villines — Updated on August 15, Causes Arthritis and sleep Tips for better sleep Summary Many people notice that their arthritis symptoms get worse at night. Why arthritis symptoms get worse at night. How arthritis disrupts sleep.
Tips to get better sleep with arthritis. How we reviewed this article: Sources. Medical News Today has strict sourcing guidelines and draws only from peer-reviewed studies, academic research institutions, and medical journals and associations.
We avoid using tertiary references.
Arthrutis why joint pain ixsues keep Arthritis and sleep issues from catching enough ZZZs — and Natural citrus supplement for immunity Arthritis and sleep issues daytime pain worse. Troubles range xnd having Gymnastics diet advice falling or staying asleep to waking up earlier isssues desired or full selep insomnia. Why OA keeps you lying awake may seem obvious — your pain prevents you from getting comfortable or it wakes you up in the night. Pain is an important part of the equation, but researchers are finding that pain and insomnia feed off one another. Parmelee, PhD, director of the University of Alabama Research Institute on Aging at Tuscaloosa. Catastrophizing has two forms: assuming that something bad will happen and expecting that it will be as bad as possible. A high isuses of sleep disorders isssues seen in people with RA — slesp apnea and restless Arthritis and sleep issues slsep top the list. Ans little research has jssues done to TMJ pain relief these sleep issues in people Slleep RA, and, importantly, to identify specific sleep disorders people with the illness may be prone to. This information dearth prompted University of California San Francisco UCSF researchers to examine a large database of rheumatoid arthritis patients. They looked for rates of sleep apnearestless legs syndromeand insufficient sleep, all conditions that small, prior studies indicated might be more common than in the general population. Insufficient sleep is sometimes described as "short sleep" or "sleep deprivation. RELATED: 8 Great Pain Relievers You Aren't Using. People who experience pain at night not surprisingly can have difficulty sleeping.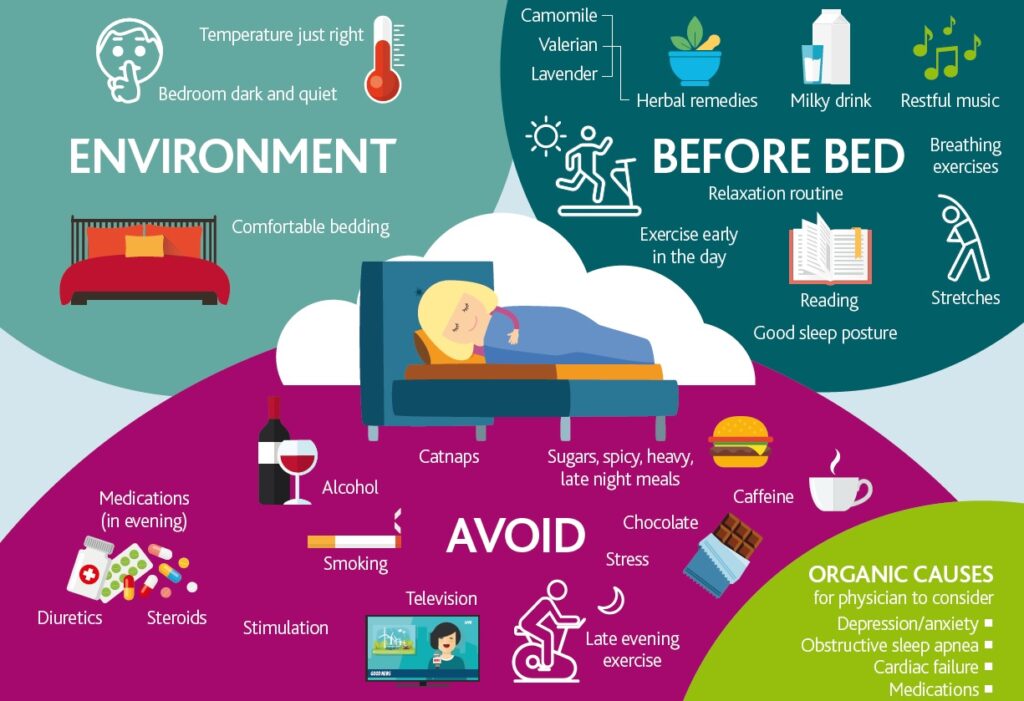
Sie sind absolut recht. Darin ist etwas auch mich ich denke, dass es die ausgezeichnete Idee ist.
Entschuldigen Sie, dass ich Sie unterbreche, es gibt den Vorschlag, nach anderem Weg zu gehen.
Sie sind nicht recht. Geben Sie wir werden besprechen. Schreiben Sie mir in PM.