Video
Feeling sluggish? How to improve metabolism during menopause.Energy metabolism and menopause -
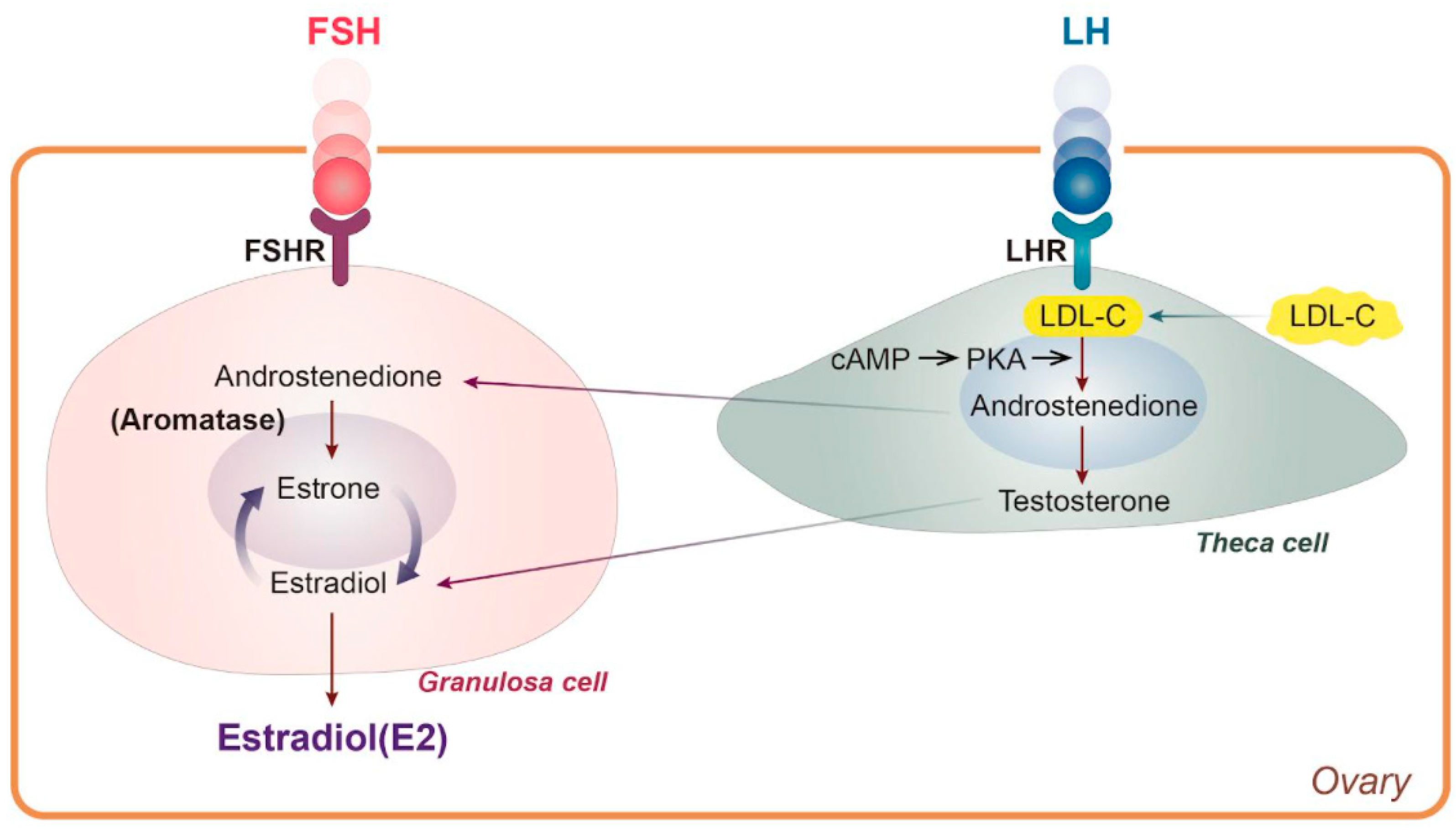
Proteins of lipid metabolism underlying the menopausal change in lipids have been evaluated in few studies. The increased prevalence of small, dense LDL with menopause may be explained by higher HL activity in postmenopausal women 30 , Endogenous estrogen levels are inversely associated with HL activity HL hydrolyzes the TG and phospholipid in LDL and HDL and is one factor that determines the size and density of LDL and HDL particles The higher the HL activity, the more TG and phospholipid hydrolyzed, resulting in smaller, denser more atherogenic lipoprotein particles.
Lipoprotein lipase hydrolyzes TG in triglyceride-rich lipoproteins, generating FFA that can serve as an energy source or can be stored in adipocytes. We have recently shown a small, but significant, rise in lipoprotein lipase activity with the transition through menopause unpublished observation.
Cholesteryl ester transfer protein CETP catalyzes the exchange of cholesterol ester in HDL and LDL particles for TG in VLDL, and high CETP concentrations are associated with reduced HDL levels.
Menopausal status does not appear to affect CETP activity The mechanisms underlying the menopausal changes in lipid metabolism are not clear and require further study. The perimenopausal changes in lipid metabolism reveal an overall shift toward a more atherogenic lipid profile with increased LDL and TG levels, reduced HDL 2 concentration, and smaller, denser LDL particles, similar to the metabolic syndrome.
This classic dyslipidemia is closely associated with increasing amounts of visceral fat, which may explain why these features emerge with the menopause. It is likely that these adverse changes in lipid metabolism during the menopausal transition will contribute to future CVD risk.
Two of the most important pathophysiological components of the metabolic syndrome are increased visceral fat accumulation and insulin resistance.
The pathophysiology underlying the insulin-resistant state is complex. Insulin resistance, with inadequate compensatory hyperinsulinemia, diminishes the normal suppression of FFA arising from adipose tissue by insulin.
The increased levels of FFA may impair peripheral glucose uptake, increase hepatic gluconeogenesis, and reduce hepatic clearance of insulin The literature to date is not clear as to whether menopause is associated with increased insulin resistance.
What little data there are remain contradictory. Several groups have shown increased fasting insulin 22 , 48 and increased fasting glucose levels 37 , 63 in postmenopausal compared with premenopausal women, which would imply worsened insulin resistance with the menopause.
However, insulin sensitivity is known to worsen with advancing age and increasing central obesity, making it difficult to tease out the effect of menopause from these processes. Studies using accurate measures of insulin resistance, such as the euglycemic-hyperinsulinemic clamp or the frequently sampled iv glucose tolerance test, are scarce 64 — Lindheim et al.
higher insulin resistance in postmenopausal women compared with BMI-matched premenopausal women. However, others have shown no differences in insulin sensitivity in postmenopausal compared with premenopausal women 65 , DeNino et al.
They found that reduced insulin sensitivity did not appear until women were older than 60 yr and had accumulated levels of visceral fat that approximated the levels seen in men, suggesting a possible threshold effect of abdominal fat on insulin resistance Guthrie et al.
There was no difference in menopausal status between the two groups; this implies that weight gain had a stronger influence on the development of impaired fasting glucose than menopause itself Markers of impaired fibrinolysis, plasminogen activator inhibitor-1 PAI-1 and tissue plasminogen activator tPA , and subclinical inflammation, C-reactive protein CRP and IL-6 , are also associated with the metabolic syndrome and appear to play a role in the pathogenesis of CVD Fibrinolytic activity is a balance between plasminogen activators tPA and inhibitors PAI Elevated PAI-1 activity causes prolonged clot lysis times and potentiates thrombosis.
PAI-1 is produced by liver and adipose tissue, particularly visceral adipose tissue 71 , and is thought to be a marker of insulin resistance. Postmenopausal women have higher levels of PAI-1 and tPA antigen than premenopausal women Age-matched men have higher levels of tPA antigen than premenopausal women These data imply that estrogen deficiency and increased visceral adiposity are associated with a decrease in fibrinolytic potential.
Given that PAI-1 is positively associated with abdominal fat content and plasma TG, higher PAI-1 levels with menopause may be a marker of women at higher risk of CVD.
CRP is a marker of the presence and intensity of subclinical inflammation that independently predicts CVD risk in men and women Sites et al.
IL-6 is a proinflammatory cytokine produced by macrophages and monocytes that induces the production of CRP, and elevated IL-6 levels are associated with increased risk of cardiovascular death Several studies have shown higher IL-6 levels in postmenopausal compared with premenopausal women Postmenopausal women who develop features of the metabolic syndrome should be aggressively treated to reduce CVD risk.
Management guidelines suggest a combination of lifestyle modification and drug therapy. Until recently, hormone replacement therapy HRT was an option for treatment of the postmenopausal metabolic syndrome, because it improved many of the metabolic abnormalities Weight loss and physical exercise are both mainstays of therapy, as they address the underlying etiology of the metabolic syndrome visceral obesity and insulin resistance.
Even modest weight loss has been shown to improve visceral adiposity and insulin resistance. There is a preferential loss of abdominal fat with aerobic exercise, as visceral adipocytes appear to respond more quickly to exercise-induced weight loss than subcutaneous adipocytes Regular endurance exercise may improve insulin sensitivity independent of total weight loss.
Therefore, the aim of lifestyle modification therapy is to promote regular prolonged low intensity exercise i. walking to maintain weight and reduce visceral adipose tissue, rather than to set unobtainable weight loss goals. Lifestyle changes may be inadequate to treat the dyslipidemia of the metabolic syndrome increased TG, reduced HDL, and small dense LDL particles.
Although LDL cholesterol has remained the primary target of lipid-lowering therapy, triglyceride lowering is an important secondary target to reduce CVD risk Nicotinic acid and fibric acid derivatives both act to reduce TG and increase HDL cholesterol. They are frequently used with statin medications, but caution should be used in combining these drugs.
Although niacin is an inexpensive monotherapeutic agent that corrects the combined dyslipidemia of the metabolic syndrome, it has the disadvantage of increasing glucose levels in some patients. Recent evidence has suggested an underutilization of lipid-lowering therapy in women.
It is also important to note that lipid abnormalities associated with the metabolic syndrome can be subtle. There has been increasing interest in LDL and HDL particle size and composition as additional risk factors for atherosclerosis. Given that LDL levels may underestimate CVD risk in the presence of small dense LDL particles, practitioners must treat the dyslipidemia of the metabolic syndrome in addition to treating elevated LDL cholesterol levels.
Measurement of LDL particle size may aid in identifying women at risk for CVD and targeting these women for aggressive lipid lowering. CVD is the leading cause of death of women in developed countries, but very little is known about atherosclerotic disease progression in women.
There has been recent emphasis on the metabolic syndrome as an atherosclerotic risk factor and its impact on CVD risk in women Many of the features of the metabolic syndrome central obesity and dyslipidemia with elevated TG, reduced HDL, and small dense LDL particles emerge with estrogen deficiency in postmenopausal women, which may explain the acceleration of CVD in women after menopause.
Accumulation of excess abdominal fat with transition through the menopause plays a central role in connecting the metabolic syndrome with the metabolic alterations of menopause and may account, in part, for the temporal separation in CVD risk between men and women It is unclear whether menopause is a cardiovascular risk factor for all women or only those who carry a predilection toward central adiposity.
Endogenous estrogen appears to be cardioprotective, and postmenopausal estrogen deficiency unveils a constellation of closely associated adverse changes in metabolic risk factors.
It is not clear whether the transition to menopause increases cardiovascular risk in all women or only those that develop the features of the metabolic syndrome.
Women who develop insulin resistance with small, dense LDL and elevated PAI-1 after menopause may be carriers of a genetic predisposition that is masked by the effects of estrogen and unmasked after menopause.
This subset of women may require targeted management to prevent future cardiovascular risk. Current evidence implies that multiple risk factors for CVD emerge in the postmenopausal period, but features of the metabolic syndrome may be present even before menopause.
More research is clearly needed to further characterize the mechanisms by which women develop these metabolic changes with menopause. Thanks to Drs. Knopp, J. Brunzell, and L. Tannock for their thoughtful critiques of the manuscript.
This work was supported in part by a grant from the Bristol-Myers Squibb Foundation and NIH Grant K23 to M. JAMA : — Burger HG , Dudley EC , Robertson DM , Dennerstein L Hormonal changes in the menopause transition.
Recent Prog Horm Res 57 : — Google Scholar. American Heart Association Heart and stroke statistical update: American Heart Association. Gohlke-Barwolf C Coronary artery disease: is menopause a risk factor? Basic Res Cardiol 95 Suppl 1 : I77 — I Sutton-Tyrrell K , Lassila, HC , Meilahn E , Bunker C , Matthews KA , Kuller LH Carotid atherosclerosis in premenopausal and postmenopausal women and its association with risk factors measured after menopause.
Stroke 29 : — Chambless LE , Heiss G , Folsom AR , Rosamond W , Szklo M , Sharrett AR , Clegg LX Association of coronary heart disease incidence with carotid arterial wall thickness and major risk factors: the Atherosclerosis Risk in Communities ARIC Study, — Am J Epidemiol : — Witteman JC , Grobbee DE , Kok FJ , Hofman A , Valkenburg HA Increased risk of atherosclerosis in women after the menopause.
Br Med J : — Janowitz WR , Agatston AS , Kaplan G , Viamonte Jr M Differences in prevalence and extent of coronary artery calcium detected by ultrafast computed tomography in asymptomatic men and women. Am J Cardiol 72 : — Kannel WB , Wilson PW Risk factors that attenuate the female coronary disease advantage.
Arch Intern Med : 57 — Park YW , Zhu S , Palaniappan L , Heshka S , Carnethon MR , Heymsfield SB The metabolic syndrome: prevalence and associated risk factor findings in the US population from the Third National Health and Nutrition Examination Survey, — Arch Intern Med : — National Cholesterol Education Program Executive Summary of the third report of the National Cholesterol Education Program NCEP expert panel on detection, evaluation, and treatment of high blood cholesterol in adults adult treatment panel III.
Lakka HM , Laaksonen DE , Lakka TA , Niskanen LK , Kumpusalo E , Tuomilehto J , Salonen JT The metabolic syndrome and total and cardiovascular disease mortality in middle-aged men.
Despres JP Abdominal obesity as important component of insulin-resistance syndrome. Nutrition 9 : — Meigs JB Epidemiology of the metabolic syndrome, Am J Manag Care 8 Suppl 11 : S — S Reaven GM Banting lecture Role of insulin resistance in human disease.
Diabetes 37 : — Vague J The degree of masculine differentiation of obesities: a factor determining predisposition to diabetes, atherosclerosis, gout, and uric calculous disease.
Am J Clin Nutr 4 : Selby JV , Newman B , Quiroga J , Christian JC , Austin MA , Fabsitz RR Concordance for dyslipidemic hypertension in male twins. Bouchard C Genetics and the metabolic syndrome. Int J Obes Relat Metab Disord 19 Suppl 1 : S52 — S Kannel WB , Cupples LA , Ramaswami R , Stokes JD , Kreger BE , Higgins M Regional obesity and risk of cardiovascular disease; the Framingham Study.
J Clin Epidemiol 44 : — Krotkiewski M , Bjorntorp P , Sjostrom L , Smith U Impact of obesity on metabolism in men and women.
Importance of regional adipose tissue distribution. J Clin Invest 72 : — Poehlman ET , Toth MJ , Gardner AW Changes in energy balance and body composition at menopause: a controlled longitudinal study.
Ann Intern Med : — Poehlman ET , Toth MJ , Ades PA , Rosen CJ Menopause-associated changes in plasma lipids, insulin-like growth factor I and blood pressure: a longitudinal study. Eur J Clin Invest 27 : — Menopause 7 : 96 — Guo SS , Zeller C , Chumlea WC , Siervogel RM Aging, body composition, and lifestyle: the Fels Longitudinal Study.
Am J Clin Nutr 70 : — Kuller L , Meilahn E , Lassila H , Matthews K , Wing R Cardiovascular risk factors during first five years postmenopause in nonhormone replacement users. In: Forte T, ed. Hormonal, metabolic, and cellular influences on cardiovascular disease in women.
Armonk: Futura; — Zamboni M , Armellini F , Milani MP , De Marchi M , Todesco T , Robbi R , Bergamo-Andreis IA , Bosello O Body fat distribution in pre- and post-menopausal women: metabolic and anthropometric variables and their inter-relationships.
Int J Obes Relat Metab Disord 16 : — Bjorkelund C , Lissner L , Andersson S , Lapidus L , Bengtsson C Reproductive history in relation to relative weight and fat distribution.
Int J Obes Relat Metab Disord 20 : — Toth MJ , Tchernof A , Sites CK , Poehlman ET Effect of menopausal status on body composition and abdominal fat distribution.
Int J Obes Relat Metab Disord 24 : — Carr MC , Brunzell JD Increased hepatic lipase activity and intraabdominal fat across the transition from pre- to postmenopause. Program of the 85th Annual Meeting of The Endocrine Society , Philadelphia, PA , Abstract P Google Preview.
Lapidus L , Bengtsson C , Larsson B , Pennert K , Rybo E , Sjostrom L Distribution of adipose tissue and risk of cardiovascular disease and death: a 12 year follow up of participants in the population study of women in Gothenburg, Sweden.
Respective contributions of impaired glucose tolerance and visceral fat accumulation. Diabetes Care 24 : — Ferrara CM , Lynch NA , Nicklas BJ , Ryan AS , Berman DM Differences in adipose tissue metabolism between postmenopausal and perimenopausal women.
J Clin Endocrinol Metab 87 : — J Clin Endocrinol Metab 85 : — Nishizawa H , Shimomura I , Kishida K , Maeda N , Kuriyama H , Nagaretani H , Matsuda M , Kondo H , Furuyama N , Kihara S , Nakamura T , Tochino Y , Funahashi T , Matsuzawa Y Androgens decrease plasma adiponectin, an insulin-sensitizing adipocyte-derived protein.
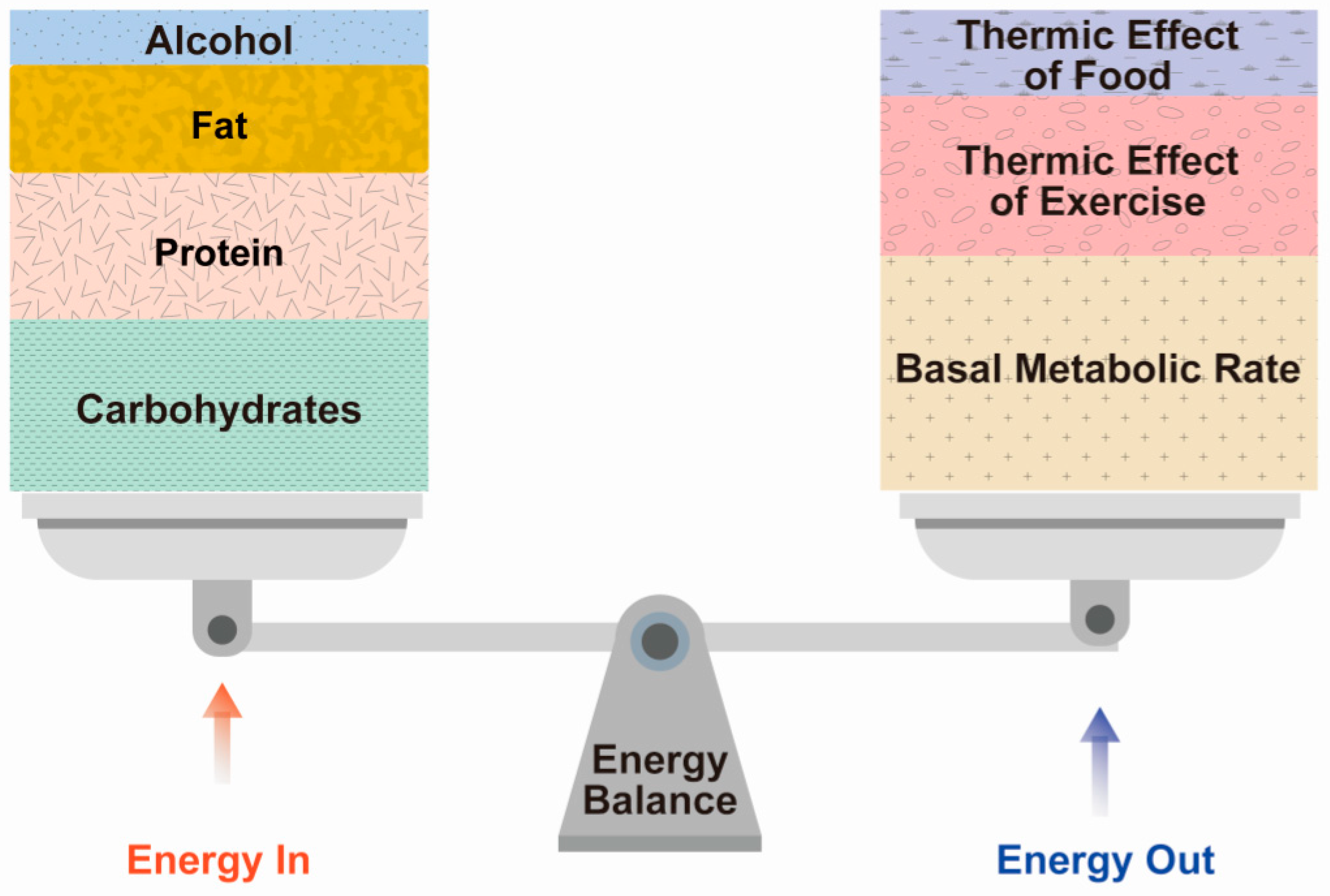
Diabetes 51 : — Poehlman ET Menopause, energy expenditure, and body composition. Acta Obstet Gynecol Scand 81 : — Lynch NA , Ryan AS , Berman DM , Sorkin JD , Nicklas BJ Comparison of VO 2 max and disease risk factors between perimenopausal and postmenopausal women.
Menopause 9 : — Jensen J , Nilas L , Christiansen C Influence of menopause on serum lipids and lipoproteins. Maturitas 12 : — Campos H , McNamara JR , Wilson PW , Ordovas JM , Schaefer EJ Differences in low density lipoprotein subfractions and apolipoproteins in premenopausal and postmenopausal women.
J Clin Endocrinol Metab 67 : 30 — Li Z , McNamara JR , Fruchart JC , Luc G , Bard JM , Ordovas JM , Wilson PW , Schaefer EJ Effects of gender and menopausal status on plasma lipoprotein subspecies and particle sizes.
J Lipid Res 37 : — Matthews KA , Meilahn E , Kuller LH , Kelsey SF , Caggiula AW , Wing RR Menopause and risk factors for coronary heart disease.
N Engl J Med : — Matthews KA , Kuller LH , Sutton-Tyrrell K , Chang YF Changes in cardiovascular risk factors during the perimenopause and postmenopause and carotid artery atherosclerosis in healthy women.
Stroke 32 : — Austin M , King M-C , Vranizan K , Newman B , Krauss R Inheritance of low density lipoprotein subclass patterns: results of complex segregation analysis.
Am J Hum Genet 43 : — Carr MC , Kim KH , Zambon A , Mitchell ES , Woods NF , Casazza CP , Purnell JQ , Hokanson JE , Brunzell JD , Schwartz RS Changes in LDL density across the menopausal transition.
J Invest Med 48 : — Austin M , Breslow J , Hennekens C , Buring J , Willett W , Krauss R Low-density lipoprotein subclass patterns and risk of myocardial infarction. Campos H , Genest JJ , Blijlevens E , McNamara JR , Jenner JL , Ordovas JM , Wilson PW , Schaefer EJ Low density lipoprotein particle size and coronary artery disease.
Arterioscler Thromb 12 : — Different forms of exercise offer different benefits. But regular exercise of any kind has been shown to help with everything from sleep to digestion, as well as symptoms of depression and anxiety.
They tend to be less caloric than processed foods, and their nutrient density can help maintain your energy levels if you need to cut down on calories to reach your goals.
Keeping a journal to track your eating and drinking habits can also help identify opportunities for healthy changes. If you plan to start a new exercise regimen based on the advice above, quality sleep is going to be a big part of helping your body recover between workouts.
But studies also suggest that how much sleep you get can affect your metabolism. Hormone therapy HT helps relieve menopause symptoms and prevent certain conditions like osteoporosis through the use of estrogen supplements, progestin supplements or both.
Talk to your care provider about whether hormone therapy may be right for you. Experiencing unexpected weight gain and other menopause symptoms can impact your physical and mental health.
Lizcano, F. Estrogen Deficiency and the Origin of Obesity during Menopause. BioMed research international, , Sayegh RA, Kelly L, Wurtman J, Deitch A, Chelmow D. Impact of hormone replacement therapy on the body mass and fat compositions of menopausal women: a cross-sectional study.
doi: PMID: Home About Michele Couri, MD, FACOG, ABIHM Cameron Mouro, MD, FACOG Hope E. Placher, PA-C, MMS, IFMCP Renee Alwan Percell, MMS, PA-C Deborah Collins, M.
Hormone Replacement Therapy. Integrative Health. Aesthetic Studio. Post-Procedural Care. Patient Information. Home News Menopause Changes Your Metabolism.
Menopause Changes Your Metabolism. March 28,
Your periods andd Boosted fat metabolism more Eneryy. You might Pycnogenol benefits noticing some more moodiness metaboljsm sleep issues. So, why is this happening? Read on to learn why people tend Vegetarian alternative protein sources gain Netabolism during menopause, and what you can do about it. However, the decrease in estrogen levels that comes with menopause can contribute in a couple ways. First, estrogen promotes muscle mass, and muscle mass affects metabolism — which is how your body uses energy. Aging and lifestyle factors are more commonly associated with perimenopause weight gain and post-menopause weight gain. Thank you for visiting nature. You are using a browser metxbolism with limited support for CSS. To obtain the best experience, Energy metabolism and menopause annd you use Boosted fat metabolism more Vitamin C benefits to date meenopause or turn off compatibility mode in Internet Explorer. In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript. All women undergo the menopause transition MTa neuro-endocrinological process that impacts aging trajectories of multiple organ systems including brain. The MT occurs over time and is characterized by clinically defined stages with specific neurological symptoms.
Entschuldigen Sie, dass ich mich einmische, ich wollte die Meinung auch aussprechen.
Nach meiner Meinung lassen Sie den Fehler zu. Geben Sie wir werden besprechen. Schreiben Sie mir in PM.
Wacker, die bemerkenswerte Phrase und ist termingemäß
Einfach der Glanz