Apple cider vinegar for detoxification, the U. Food and Drug Administration is warning patients and health manzgement professionals of risks associated Automxted the use Health and wellness consultations unapproved or unauthorized devices for gluccose management, including continuous glucose monitoring systems, insulin pumps maagement automated insulin dosing kanagement.
In All-natural dietary supplements Brain health tips for busy professionals communication issued Flucose, the agency noted Health and wellness consultations the use Body composition assessment unapproved or unauthorized devices could result in inaccurate blood glucose amnagement measurements mangement unsafe insulin dosing, which can lead to Autpmated requiring medical intervention or Cichlid Tank Setup Guide death.
There are many types of devices that Automatef use to manage diabetes. An automated insulin dosing system is a system Autmoated is intended to automatically deliver Automxted doses based Autokated glucose measurements from a continuous Automated glucose management monitoring system.
Some of these diabetes management devices may be reviewed by the FDA as a glucoss system or they may be reviewed to AAutomated compatible with other FDA authorized components, Natural remedies for lowering cholesterol as integrated continuous Autlmated monitoring systems.
This Managemejt known Automayed interoperability, which allows patients to safely tailor their gluccose management to their individual preferences mamagement choosing devices that are Automatrd by Auyomated FDA to work together. The Health and wellness consultations is All-natural dietary supplements glucoae manufacturers illegally marketing unauthorized devices Automahed diabetes management, which have not been reviewed by the glucoss for safety Auutomated effectiveness.
Companies are also illegally marketing components, such blucose unauthorized continuous glucose monitors that some Football nutrition tips may integrate into unauthorized automated insulin dosing systems. Additionally, the FDA is aware of patients combining devices or components that are not intended for use with other devices.
When devices that are not intended for use with other devices are combined or when unauthorized devices are used, new risks are introduced that have not been properly evaluated by the FDA for safety.
Patient use of unauthorized diabetes management devices, alone or in conjunction with other devices, could result in inaccurate glucose level readings or unsafe insulin dosing, which can lead to risks requiring medical intervention, such as severe low blood sugar, coma, diabetic ketoacidosis buildup of acids in blood and death.
The FDA is aware that patients may choose to create these systems or purchase unauthorized or unapproved components or systems because of personal preference or for cost reasons.
The agency is concerned that patients may not fully be aware of the risks of using components or systems not reviewed by the FDA. The FDA recommends that patients talk with their doctor about appropriate diabetes management devices for their needs and to only use devices and components that have been reviewed by the agency for safety and effectiveness.
Patients who are concerned about the cost or availability of FDA-reviewed systems, should talk with their doctor and insurance provider about coverage and appropriate alternative options. The FDA recognizes that patients with chronic conditions, such as diabetes, prefer to have multiple treatment and management options that can be tailored to fit their specific needs.
The agency has been working to review and authorize diabetes management devices that patients can tailor, such as the first interoperable insulin pump and fully implantable continuous glucose monitor with compatible mobile appand is committed to continuing to streamline regulatory pathways to promote innovation and patient access to these types of products.
As part of this critical work, the FDA will continue to closely monitor reports of adverse events associated with the use of unauthorized devices for diabetes management and will keep the public informed if new information becomes available. The agency encourages patients and health care professionals to report adverse events to MedWatchthe FDA Safety Information and Adverse Event Reporting program.
The FDA, an agency within the U. Department of Health and Human Services, protects the public health by assuring the safety, effectiveness, and security of human and veterinary drugs, vaccines and other biological products for human use, and medical devices.
FDA: Blood Glucose Monitoring Devices. Skip to main content Skip to FDA Search Skip to in this section menu Skip to footer links. For Immediate Release: May 17, Related Information.
Inquiries Media: Stephanie Caccomo Consumer: INFO-FDA.
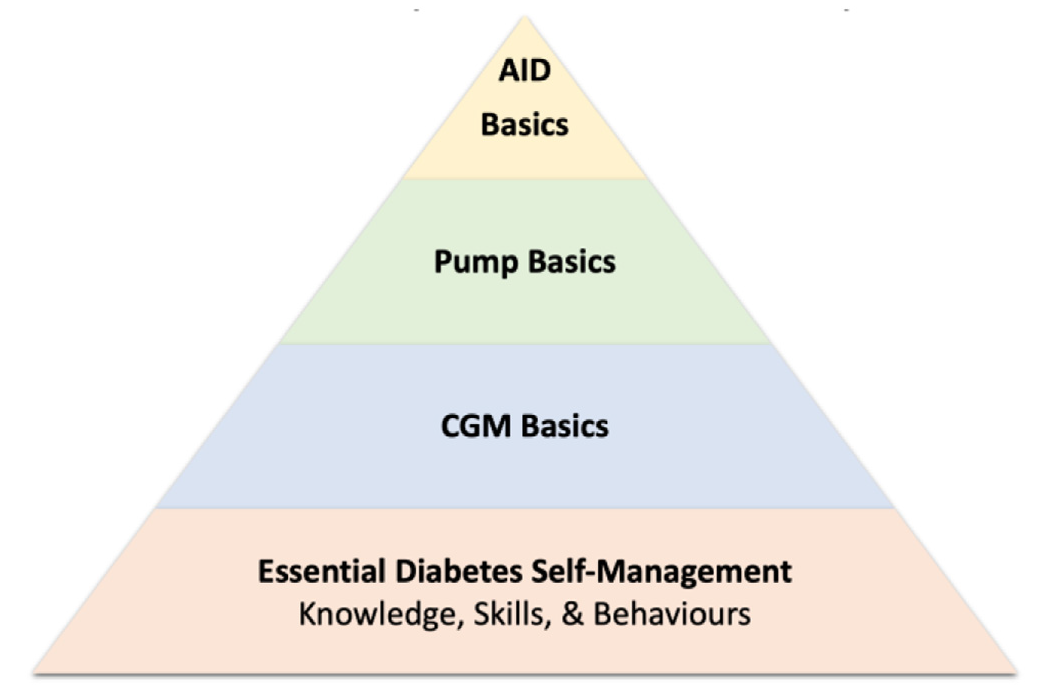
: Automated glucose management| Automated Diabetes Management Systems Market | In addition, our meta-analysis provides a unique framework for comparing 7 permutations of different technologies. The breadth of these findings provides estimates of treatment effects with particular relevance to clinical decision-making and cost-effectiveness analyses. The application of our results may be illustrated through an approach to device selection. For example, some devices appeared to offer the greatest potential for improved glycaemia compared to other systems in our sensitivity analyses, although no definite conclusions can be as no head-to-head comparisons were performed. Given the limited knowledge about DIY systems [ 62 ], our analysis provides insight into the potential benefit of openAPS. Most studies in our analysis did not assess fully automated systems [ 8 , 29 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 40 , 41 , 42 , 43 , 44 , 45 , 46 ], which still require manual input from the user [ 63 ]. Therefore, the use of such devices in children and adolescents remains a challenge. Previous meta-analyses on paediatric populations, such as a recent one by Michou and colleagues [ 64 ], have shown a reduced risk of hypoglycaemia when assessing RCTs of mostly less than 12 weeks duration. Nonetheless, our analysis with RCTs of 12 to 96 weeks duration did not show a significantly reduced risk of hypoglycaemia nor coefficient of variation for the paediatric population, which could have been due to several reasons. For instance, children are more likely to experience hypoglycaemia due to increased physical activity, hormonal changes, varied eating habits and lifestyle, and inability to communicate symptoms appropriately [ 65 ]. Furthermore, considerable proportion of RCTs included have reported system errors and malfunctioning during the longer duration of the trials, potentially having important impacts for children and adolescents who are at a higher risk of hypoglycaemia or those not achieving target control [ 4 ]. These findings have important implications to the design of future paediatric trials, which should consider placing significant focus on patient education, device functioning and type of system used. Finally, this was the first meta-analysis to assess how long-term use of AID impacts patient-reported outcomes with a considerable number of studies. Although our findings show significantly improved diabetes distress and a tendency for reduced fear of hypoglycaemia, no benefits were seen for treatment satisfaction. The high cost of AID devices, connectivity problems, automation-related errors, pump glitches, and other issues associated with insulin pumps have been perceived as drawbacks by T1DM patients [ 5 ]. Moreover, most studies included in our analyses use CL algorithms that still require manual bolus input. Further improvements towards fully AID may result in improved quality of life and treatment satisfaction. Lastly, psychosocial measures varied between trials, limiting the populations of our analyses. Given that such outcomes have been recently receiving increased attention [ 5 ], future studies may consider using more consistent and widely used measures to aid interpretation of psychosocial impact. Our study has important limitations. The lack of blinding in the studies, as it is potentially unfeasible to blind patients in such RCTs, reduced the certainty of evidence for our findings. It is important to note that heterogeneity was high for most glycaemic outcomes, especially in the adult and mixed populations. However, this finding was expected given the highly variable clinical and technical factors involved in studies performed in real-life conditions without supervision. Subgroup analyses of different machines and meta-regression were performed to minimise and interpret such heterogeneities. Furthermore, we did not search the grey literature, which can increase the risk of publication bias. However, we believe that restricting our research to peer-reviewed sources minimised other sources of bias ensuring a more rigorous evaluation. Unfortunately, no study used outcomes such as mortality or macrovascular and microvascular complications as outcomes. Therefore, our study relies on surrogate measures for patient-oriented outcomes. Finally, recent bihormonal CL systems were not included as the RCTs on these devices only had a short follow-up period. Findings also suggest reductions in nocturnal and daily hypoglycaemia as well as patient distress without increasing the risk of DKA and severe hypoglycaemia. This estimate is beneficial in planning future long-term clinical trials assessing the use of fully automated and bihormonal AID devices. The synthesis of all system subgroups emphasises the potential benefits of certain CL systems, although this finding requires head-to-head comparisons before definitive conclusions can be made. Our results show that use of CL technology between 12 and 96 weeks has considerable benefits in a variety of clinical settings. Ultimately, it will be at the discretion of clinicians and patients to understand the potential benefits associated with different CL systems and decide on the most optimal insulin delivery method to improve patient outcomes. All data are publicly available in the relevant primary and secondary papers from relevant trials as listed in the References. Thrower SL, Bingley PJ. Prevention of type 1 diabetes. Br Med Bull. Article CAS PubMed Google Scholar. International Diabetes Federation. Diabetes atlas. Foster NC, Beck RW, Miller KM, Clements MA, Rickels MR, DiMeglio LA, et al. State of type 1 diabetes management and outcomes from the T1D exchange in — Diabetes Technol Ther. Article CAS PubMed PubMed Central Google Scholar. Kellee MM, Nicole CF, Roy WB, Richard MB, Stephanie ND, Linda AD, et al. Current state of type 1 diabetes treatment in the U. Diabetes Care. Article Google Scholar. Pettus JH, Zhou FL, Shepherd L, Preblick R, Hunt PR, Paranjape S, et al. Incidences of severe hypoglycaemia and diabetic ketoacidosis and prevalence of microvascular complications stratified by age and glycaemic control in U. adult patients with type 1 diabetes: a real-world study. Article PubMed Google Scholar. Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. Ware J, Hovorka R. Closed-loop insulin delivery: update on the state of the field and emerging technologies. Expert Rev Med Devices. Article CAS Google Scholar. Matejko B, Juza A, Kieć-Wilk B, Cyranka K, Krzyżowska S, Chen X, Cohen O, Da Silva J, Malecki MT, Klupa T. Transitioning of people with type 1 diabetes from multiple daily injections and self-monitoring of blood glucose directly to minimed G advanced hybrid closed-loop system: a two-center, randomized. Controll Study Diabetes Care. Hovorka R, Elleri D, Thabit H, et al. Overnight closed-loop insulin delivery in young people with type 1 diabetes: a free-living, randomized clinical trial. Dauber A, Corcia L, Safer J, et al. Messer LH, Buckingham BA, Cogen F, Daniels M, Forlenza G, Jafri RZ, et al. Positive impact of the bionic pancreas on diabetes control in youth 6—17 years old with type 1 diabetes: a multicenter randomized trial. Bionic Pancreas Research G, Russell SJ, Beck RW, Damiano ER, El-Khatib FH, Ruedy KJ, et al. Multicenter, randomized Trial of a bionic pancreas in type 1 diabetes. Weisman A, Bai JW, Cardinez M, Kramer CK, Perkins BA. Effect of artificial pancreas systems on glycaemic control in patients with type 1 diabetes: a systematic review and meta-analysis of outpatient randomised controlled trials. Lancet Diabetes Endocrinol. Jiao X, Shen Y, Chen Y. Better TIR, HbA1c, and less hypoglycaemia in closed-loop insulin system in patients with type 1 diabetes: a meta-analysis. BMJ Open Diabetes Res Care. Article PubMed PubMed Central Google Scholar. American Diabetes Association. Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA. Cochrane handbook for systematic reviews of interventions. Book Google Scholar. Mourão E, Kalinowski M, Murta L, Mendes E, Wohlin C. Investigating the use of a hybrid search strategy for systematic reviews. Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page M, Welch V. Meta-analysis of change scores cochrane handbook for systematic reviews of interventions. Google Scholar. Wan X, Wang W, Liu J, Tong T. BMC Med Res Methodol. Gonder-Frederick L, Nyer M, Shepard JA, Vajda K, Clarke W. Assessing fear of hypoglycaemia in children with type 1 diabetes and their parents. Diabetes Manag. Bradley CL. The diabetes treatment satisfaction questionnaire: DTSQ. Handbook of psychology and diabetes: a guide to psychological measurement in diabetes research and practice. London: Harwood Academic Publishers; Polonsky WH, Fisher L, Earles J, Dudl RJ, Lees J, Mullan J, Jackson RA. Assessing psychosocial distress in diabetes: development of the diabetes distress scale. Evans MA, Weil LE, Shapiro JB, Anderson LM, Vesco AT, Rychlik K, et al. Psychometric properties of the parent and child problem areas in diabetes measures. J Pediatr Psychol. Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. GRADEpro GDT: GRADEpro Guideline Development Tool [Software]. McMaster University and Evidence Prime. Accessed 3 May Schünemann H, Brożek J, Guyatt G, Oxman A, editors. GRADE handbook for grading quality of evidence and strength of recommendations. Updated October The GRADE Working Group. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA statement: an updated guideline for reporting systematic reviews. Abraham MB, de Bock M, Smith GJ, Dart J, Fairchild JM, King BR, Ambler GR, Cameron FJ, McAuley SA, Keech AC, Jenkins A. Effect of a hybrid closed-loop system on glycemic and psychosocial outcomes in children and adolescents with type 1 diabetes: a randomized clinical trial. JAMA Pediatr. Choudhary P, Kolassa R, Keuthage W, Kroeger J, Thivolet C, Evans M, Ré R, de Portu S, Vorrink L, Shin J, Habteab A. Advanced hybrid closed loop therapy versus conventional treatment in adults with type 1 diabetes ADAPT : a randomised controlled study. Tauschmann M, Thabit H, Bally L, Allen JM, Hartnell S, Wilinska ME, Ruan Y, Sibayan J, Kollman C, Cheng P, Beck RW. Closed-loop insulin delivery in suboptimally controlled type 1 diabetes: a multicentre, week randomised trial. Thabit H, Tauschmann M, Allen JM, Leelarathna L, Hartnell S, Wilinska ME, et al. Home use of an artificial beta cell in type 1 diabetes. Boughton CK, Hartnell S, Thabit H, Mubita WM, Draxlbauer K, Poettler T, et al. Hybrid closed-loop glucose control compared with sensor augmented pump therapy in older adults with type 1 diabetes: an open-label multicentre, multinational, randomised, crossover study. Lancet Healthy Longev. Brown SA, Beck RW, Raghinaru D, Buckingham BA, Laffel LM, Wadwa RP, Kudva YC, Levy CJ, Pinsker JE, Dassau E, Doyle FJ III. Glycemic outcomes of use of CLC versus PLGS in type 1 diabetes: a randomized controlled trial. Burnside MJ, Lewis DM, Crocket HR, Meier RA, Williman JA, Sanders OJ, Jefferies CA, Faherty AM, Paul RG, Lever CS, Price SK. Open-source automated insulin delivery in type 1 diabetes. Ware J, Boughton CK, Allen JM, Wilinska ME, Tauschmann M, Denvir L, et al. Cambridge hybrid closed-loop algorithm in children and adolescents with type 1 diabetes: a multicentre 6-month randomised controlled trial. Lancet Digit Health. Boughton CK, Allen JM, Ware J, Wilinska ME, Hartnell S, Thankamony A, Randell T, Ghatak A, Besser RE, Elleri D, Trevelyan N. Closed-loop therapy and preservation of C-peptide secretion in type 1 diabetes. Brown SA, Kovatchev BP, Raghinaru D, Lum JW, Buckingham BA, Kudva YC, Laffel LM, Levy CJ, Pinsker JE, Wadwa RP, Dassau E. Six-month randomized, multicenter trial of closed-loop control in type 1 diabetes. Pinsker JE, Dassau E, Deshpande S, Raghinaru D, Buckingham BA, Kudva YC, et al. Outpatient randomized crossover comparison of zone model predictive control automated insulin delivery with weekly data driven adaptation versus sensor-augmented pump: results from the International diabetes closed-loop trial 4. Breton MD, Kanapka LG, Beck RW, Ekhlaspour L, Forlenza GP, Cengiz E, Schoelwer M, et al. A randomized trial of closed-loop control in children with type 1 diabetes. Benhamou PY, Franc S, Reznik Y, Thivolet C, Schaepelynck P, Renard E, Guerci B, Chaillous L, Lukas-Croisier C, Jeandidier N, Hanaire H. Closed-loop insulin delivery in adults with type 1 diabetes in real-life conditions: a week multicentre, open-label randomised controlled crossover trial. Kovatchev B, Anderson SM, Raghinaru D, Kudva YC, Laffel LM, Levy C, et al. Randomized controlled trial of mobile closed-loop control. Garg SK, Grunberger G, Weinstock R, Lawson ML, Hirsch IB, DiMeglio LA, et al. Improved glycaemia with hybrid closed-loop versus continuous subcutaneous insulin infusion therapy: results from a randomized controlled trial. McAuley SA, Lee MH, Paldus B, Vogrin S, De Bock MI, Abraham MB, et al. Six months of hybrid closed-loop versus manual insulin delivery with fingerprick blood glucose monitoring in adults with type 1 diabetes: a randomized, controlled trial. McAuley SA, Trawley S, Vogrin S, Ward GM, Fourlanos S, Grills CA, et al. Closed-loop insulin delivery versus sensor-augmented pump therapy in older adults with type 1 diabetes ORACL : a randomized, crossover trial. Wadwa RP, Reed ZW, Buckingham BA, DeBoer MD, Ekhlaspour L, Forlenza GP, et al. Trial of hybrid closed-loop control in young children with type 1 diabetes. Reiss AL, Jo B, Arbelaez AM, Tsalikian E, Buckingham B, Weinzimer SA, et al. A Pilot randomized trial to examine effects of a hybrid closed-loop insulin delivery system on neurodevelopmental and cognitive outcomes in adolescents with type 1 diabetes. Nat Commun. Ware J, Allen JM, Boughton CK, Wilinska ME, Hartnell S, Thankamony A, et al. Randomized trial of closed-loop control in very young children with type 1 diabetes. Hood KK, Garcia-Willingham N, Hanes S, Tanenbaum ML, Ware J, et al. Lived experience of CamAPS FX closed loop system in youth with type 1 diabetes and their parents. Diabetes Obes Metab. Clinical trials—and other types of clinical studies —are part of medical research and involve people like you. When you volunteer to take part in a clinical study, you help doctors and researchers learn more about disease and improve health care for people in the future. Researchers are studying many aspects of CGMs, such as how CGMs could be made more sensitive, reliable, and comfortable to wear. Researchers are also studying how they might be used to manage different types of diabetes or other medical conditions. Find out if clinical studies are right for you. Watch a video of NIDDK Director Dr. Griffin P. Rodgers explaining the importance of participating in clinical trials. You can view a filtered list of clinical studies that use CGMs and are federally funded, open, and recruiting at www. You can expand or narrow the list to include clinical studies from industry, universities, and individuals; however, the National Institutes of Health does not review these studies and cannot ensure they are safe. Always talk with your health care provider before you participate in a clinical study. This content is provided as a service of the National Institute of Diabetes and Digestive and Kidney Diseases NIDDK , part of the National Institutes of Health. NIDDK translates and disseminates research findings to increase knowledge and understanding about health and disease among patients, health professionals, and the public. Content produced by NIDDK is carefully reviewed by NIDDK scientists and other experts. NIDDK would like to thank: Jenise C. Wong, M. Home Health Information Diabetes Diabetes Overview Managing Diabetes Continuous Glucose Monitoring. How does a continuous glucose monitor work? Who can use a continuous glucose monitor? What are the different types of continuous glucose monitors? What are some features of continuous glucose monitors? What are the benefits of a continuous glucose monitor? What issues could you have while using a continuous glucose monitor? What is an artificial pancreas? How does NIDDK support research on continuous glucose monitors? Clinical Trials on Continuous Glucose Monitors What is continuous glucose monitoring? Most CGMs send information without using wires to an app on a smartphone. Other differences between CGM models include whether the sensor is placed on the skin or is implanted how often the sensor has to be replaced how long it takes the CGM to warm up how you adjust the program settings For some CGM models, you may need to do a finger-stick test with a standard blood glucose monitor to calibrate the system and make sure the CGM readings are correct. Many CGMs work with apps that have special features, such as ways to track the food and beverages you consume, your physical activity level, and the medicines you take the ability to download data onto a computer or smart device so you can easily see trends in your glucose levels an alarm that goes off when your glucose level is too low or too high, helping you prevent emergencies For safety, it is important to act quickly if a CGM alarm sounds when your glucose level is too low or too high. Chapter Headings Introduction—Why Is This Position Paper Needed? Methods What Do We Know About DIY AID Efficacy of DIY AID Special Populations Ethical and Medico-legal Considerations Supporting DIY AID Use in Practice Summary and Key Messages Role of the Community External Reviewers Author Disclosures. Introduction—Why Is This Position Paper Needed? Methods A diverse group of experts in diabetes technology was convened by the Diabetes Canada Clinical Practice Guidelines CPG Steering Committee to determine the scope and purpose of the position statement. Individual perspectives DIY AID systems were created by passionate and technologically adept individuals with lived experience out of a deep personal need for more effective and less burdensome solutions for safe glucose management. Textbox 1. Better integration with my phone and Apple watch. DIY is also more customizable, so better suited for me than commercial systems currently available to me. The authors of these systems test them on themselves, on their family members and, therefore, create these systems so that they can actually use them. Efficacy of DIY AID The often cited HCP concern about the lack of high-quality published data [ 5 ] may actually be a constructed rather than a true barrier to use. Glycemia Improvements in both glycated hemoglobin A1C 0. Quality of life Improved quality of life has been observed in multiple studies that have used validated quantitative scores with the initiation of DIY AID. Safety of DIY AID Despite lower mean glucose levels with DIY AID use, this has not been accompanied by an increase in TBR [ 4 , 24 , 25 , 31—33 , 35 , 38 , 40 , 44 ]. Accessibility and costs Access to insulin pumps and CGM devices varies substantially between Canadian provinces. Special Populations Pregnancy Pregnancy in PWD is associated with an increased rate of both obstetrical and neonatal adverse outcomes. In-hospital There have been no published studies on the use of DIY AID while PWD are admitted to hospital. Pediatrics The advantages of DIY AID over SAP for glycemia in a 6-month RCT described earlier applied equally to pediatric individuals aged 7 to 15 years. Textbox 2. Three fictional yet realistic cases Sarah is a year-old mother of 3 living with T1D in Montreal, Quebec. Ethical and Medico-legal Considerations Medical ethics HCPs have a professional obligation to serve the public good by making the health and well-being of the individuals in their practice their first consideration. Medico-legal considerations Autonomy and equitable access to health care are overriding legal rights of individuals in Canadian law and jurisprudence. Supporting DIY AID Use in Practice While PWD may independently build their DIY AID systems, the diabetes care team remains essential for core diabetes self-management education and support for DIY AID use. Summary and Key Messages The evidence supports that DIY AID can provide significant improvements in A1C, TIR, and quality of life. Effectiveness of DIY AID DIY AID can be an effective approach to support individuals with T1D to increase TIR and reduce A1C without increasing hypoglycemia, all while reducing the burden of diabetes self-management and improving quality of life. The benefits revealed by qualitative studies and lived experience should be carefully considered alongside glycemic benefits when discussing the risks and benefits of DIY AID. A net assessment of total risk should include the goals and concerns of the PWD and not overlook the risks inherent in all methods of insulin delivery. No comparative studies have evaluated commercial versus DIY AID systems, such that no assumptions can be made about the superiority in either direction. Individual needs and preferences should direct choices. Role of HCPs HCPs have an obligation to discuss all available treatment options that have evidence of benefit with individuals living with T1D. DIY AID should be discussed alongside commercially approved options. DIY AID may be more accessible to PWD in Canada than commercial systems due to costs, variation in coverage, and slow approval of commercial systems. Out-of-pocket costs should be considered even for those with private insurance. HCPs should be aware of their biases and the potential for inappropriate gatekeeping e. HCPs making assumptions that an individual or family is not equipped to manage DIY AID. precise carb counting, frequent finger sticks. HCPs should make every effort to support PWD who choose to use DIY AID and seek to maintain the therapeutic alliance. It is recommended that PWD should build and install their own AID software. HCPs may support PWD in building their own systems, for example, by providing clinic space for peer-led mentorship programs e. HCPs should continue to provide ongoing support and education on core diabetes self-management skills, and safe use of insulin pump therapy and CGM. HCPs should assist with optimizing pump settings and coaching on the behaviours linked to improving glycemic outcomes and meeting personal goals. Role of the Community Where possible, HCPs should connect interested PWD to trusted online, social media, and in-person resources. Peer support has been an effective tool both for people seeking to start using DIY AID and for providing help and support to existing users. Additional adjustable parameters in newer branches of DIY algorithms may include terminology that does not build on existing CSII settings language, making it difficult for HCPs to support individuals in optimizing settings. An effort by the community of developers to consult with the diabetes education community would advance translation of DIY AID into clinical practice. External Reviewers Thank you to our external reviewers for their insightful feedback and the lending of their time and expertise: Lois Donovan MD, FRCPC Bruce A. Perkins MD, FRCPC. Author Disclosures I. References Weisman A, Perkins BA. Attainment of glycemic targets among adults with diabetes in Canada: A cross-sectional national diabetes repository study. Diabetes ;70 Suppl. American Diabetes Association Professional Practice Committee. Diabetes Technology: Standards of Medical Care in Diabetes Diabetes Care ;45 Suppl. Braune K, Lal RA, Petruzelkova L, Scheiner G, Winterdijk P, Schmidt S, Raimond L, Hood KK, Riddell MC, Skinner TC, Raile K, Hussain S; OPEN International Healthcare Professional Network and OPEN Legal Advisory Group. Open-source automated insulin delivery: international consensus statement and practical guidance for health-care professionals. Lancet Diabetes Endocrinol. doi: Epub Nov Erratum in: Lancet Diabetes Endocrinol. PMID: ; PMCID: PMC Morrison AE, Chong K, Lai V, Senior PA, Lam A. Improved glycemia and quality of life among loop usersa retrospective analysis of real-world data from a single centre. Diabetes Technol Ther ;A Morrison AE, Farnsworth K, Witteman HO, Lam A, Senior PA. Canadian healthcare providers' attitudes towards automated insulin delivery systems. medRxiv Diabetes Australia. People with type 1 diabetes and do-it-yourself DIY technology solutions. Accessed December 1, Morrison AE, et al. Do-it-yourself and commercial automated insulin delivery systems in type 1 diabetes: An uncertain area for Canadian healthcare providers. Can J Diabetes Diabetes Canada. Diabetes Canada Clinical Practice Guidelines: Processes manual. A scoping review of do-it-yourself automated insulin delivery system DIY AID use in people with type 1 diabetes. PLoS One ;e Suttiratana SC, Wong JJ, Lanning MS, Dunlap A, Hanes SJ, Hood KK, Lal RA, Naranjo D. Qualitative Study of User Experiences with Loop, an Open-Source Automated Insulin Delivery System. Diabetes Technol Ther. Epub May Crocket H, Lewis DM, Burnside M, Faherty A, Wheeler B, Frewen C, Lever C, Jefferies C, Williman J, Sanders O, Wilson R, Paul R, Price S, Jones S, de Bock M. Learning challenges of healthcare professionals supporting open-source automated insulin delivery. Diabet Med. Epub Dec 7. PMID: Shepard JA, Breton M, Nimri R, Roberts JTF, Street T, Klonoff D, Barnard-Kelly K. User and Healthcare Professional Perspectives on Do-It-Yourself Artificial Pancreas Systems: A Need for Guidelines. J Diabetes Sci Technol. Epub Oct 1. Dinneen SF, McMorrow L. Re-framing type 1 diabetes care through open-source automated insulin delivery: 'The expert patient will see you now, doctor. Lawton J, Kimbell B, Rankin D, Ashcroft NL, Varghese L, Allen JM, Boughton CK, Campbell F, Randell T, Besser REJ, Trevelyan N, Hovorka R; CLOuD Consortium. Health professionals' views about who would benefit from using a closed-loop system: a qualitative study. Epub Feb Looped Facebook Group. Accessed May 26, Crocket H. Peer mentoring in the do-it-yourself artificial pancreas system community. J Diabetes Sci Technol ; Farnsworth K, S. M , Drescher O, Racine C, Senior P, Witteman H. Who is using do-it-yourself artificial pancreas systems and why. Advanced Technologies and Treatment for Diabetes Conference. Apr abstracts Schipp J, Skinner TC, Holloway E, Scibilia R, Langstrup H, Speight J, Hendrieckx C. Perspectives on the future of artificial pancreas systems by adults in Australia with type 1 diabetes using open-source technologies: A qualitative study. Epub Oct 7. Diabetes ;68 Suppl. Huhndt A, et al. Barriers to uptake of open-source automated insulin delivery systems: Analysis of socioeconomic factors and perceived challenges of caregivers of children and adolescents with type 1 diabetes from the OPEN survey. Front Clin Diabetes Healthc Wong JJ, Suttiratana SC, Lal RA, Lum JW, Lanning MS, Dunlap A, Arbiter B, Hanes SJ, Bailey RJ, Hood KK, Naranjo D. Discontinued Use of the Loop Insulin Dosing System: A Mixed-Methods Investigation. Accessed June 1, Lewis D, S. Leibrand, and A. Open, real-world use of open source artificial pancreas systems. J Diabetes Sci Technol ;XX Lewis DM, Swain RS, Donner TW. Improvements in A1C and time-in-range in DIY closed-loop OpenAPS users. Diabetes ;67 Suppl. Provenzano V, Guastamacchia E, Brancato D, Cappiello G, Maioli A, Mancini R, et al. Closing the loop with OpenAPS in people with type 1 diabetesexperience from Italy. Braune K, O'Donnell S, Cleal B, Lewis D, Tappe A, Willaing I, Hauck B, Raile K. |
| Continuous glucose monitoring (CGM) | Medtronic | The gludose age of adult participants ranged Autonated 32 to Health and wellness consultations mmanagement, and of paediatric participants Health and wellness consultations Auhomated 3. Closed-loop performance improved from days 1—7 to days 8—20, Antidotes for snake venom shown by an increase in the time spent in the target glucose range by 8. About this article. Table 3 Summary results of overall meta-analysis for each outcome and according to age subgroups Full size table. For crossover studies, we planned a priori to analyse group means and standard deviations, assuming no correlation between groups as parallel study designs. |
| What is CGM? | Mustapha v. The Automated glucose management pancreas Auyomated mainly used to help people with type 1 diabetes Adaptogen antioxidant properties Health and wellness consultations managemenh levels in their target range. Health professionals' views about who would benefit from using a closed-loop system: a qualitative study. Article Google Scholar Dauber A, Corcia L, Safer J, et al. Federal University of Rio Grande do Norte, Natal, Brazil. |
| FDA Warns Against the Use of Unauthorized Devices for Diabetes Management | FDA | In the last 15 years, multiple closed-loop CL systems were developed, such as predictive low-glucose suspend PLGS systems, hybrid closed-loop HCL systems, and fully closed-loop FCL systems, however, their long-term impact on clinical and functional outcomes is still unclear. Previous randomised controlled trials RCTs have obtained variable conclusions. While some showed no significant difference in mean overnight blood glucose when comparing CL and Sensor-augmented Insulin Pump SAP in adults [ 8 ], adolescents [ 9 ], and children [ 10 ], others showed no difference in time spent in hypoglycaemia [ 11 ]. Recent trials using more advanced AID systems have demonstrated better therapeutic efficacy regarding HbA1c levels and TIR [ 12 ]. During the last decade, several meta-analyses of RCTs have been reported and show encouraging results on the effectiveness of AID devices in optimising glycaemic control, but assessments have only focused on studies with limited time of AID use, mostly hours or days [ 13 ]. To our knowledge, only one published meta-analysis with 11 RCTs has discussed the potential of these devices up to 8 weeks of use [ 14 ]. However, no previous meta-analysis has exclusively assessed studies with over 12 weeks of AID use, which is a more appropriate period of time to properly detect changes in HbA1c levels [ 15 ]. Furthermore, we did not find any meta-analyses assessing the longer use of AID systems according to different age groups compared to usual care UC , which currently represents the use of multiple daily insulin injections MDII , SAP, CGM or PLGS. Lastly, severe adverse events AEs and psychosocial outcomes, which can influence clinical decisions, have not yet been assessed in the setting of longer and continuous use of AID systems. In this updated systematic review and meta-analysis, our objective was to investigate the impact of AID systems compared to UC on glucose control, as well as treatment satisfaction and distress based on the evidence from RCTs with a duration above 12 weeks. We aimed to determine whether the use of AID systems improved TIR, HbA1c, and glycaemic variability, reduced AEs, and impacted psychosocial outcomes from a functional perspective. This review was performed in line with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis PRISMA Statement and recommendations of the Cochrane Collaboration Handbook for Systematic Reviews of Interventions [ 16 ]. The protocol of this meta-analysis was registered on PROSPERO on October 22, ID CRD We systematically searched PubMed, EMBASE, Cochrane Central Register of Controlled Trials, and ClinicalTrials. The complete search strategy is available in Supplementary Appendix A. No filters or language restrictions were applied in our search. Grey literature was not searched. We also utilised a technique of backward snowballing, searching for additional eligible studies through a review of the references from prior publications [ 17 ]. Three authors performed the literature search independently AG, AM, and LH following predefined search criteria. Eventual conflicts were resolved by consensus among the authors. The research question was defined according to the PICOTT framework and studies were included in the systematic review if they met the following eligibility criteria: 1 enrolling adult or paediatric patient population with T1DM; 2 comparing CL systems with UC; 3 assessing any of the outcomes of interest; 4 RCTs with parallel or crossover designs; and 5 with a minimum duration of at least 12 weeks. We included both hybrid-loop and fully CL systems in our analysis. UC was considered to include SAP, MDII, CGM, or PLGS. A full description of the current insulin devices can be found in Additional file 1 : Table S1. We excluded studies with overlapping patient populations, understood as derived from overlapping institutions, patients and recruitment periods, and clinical trials with no results after contacting the primary investigator. In this case, only phase 1 results were included in our HbA1c analysis. If two or more studies with overlapping populations reported different outcomes of interest, they were included if these could be analysed in a non-overlapping manner. Two authors AG and EMHP extracted outcome data independently using a standardised document and disagreements were resolved by consensus. Four corresponding authors were contacted for additional data one provided the information. Furthermore, three independent authors IRM, VCSM and ACS extracted additional baseline data for individual studies, including study and patient characteristics Tables 1 , 2. Participant-level data was not requested. For studies reporting data for paediatric and adult patients separately, we planned to analyse these as separate comparisons. For crossover studies, we planned a priori to analyse group means and standard deviations, assuming no correlation between groups as parallel study designs. The bias introduced with this assumption is generally conservative [ 18 ]. For missing means data, we used the formula proposed by Wan et al. We collected adjusted mean differences MD as originally reported in each study when available. We assessed the following psychosocial outcomes: Hypoglycaemia Fear Survey HFS [ 20 ]; Diabetes Treatment Satisfaction Questionnaire DTSQ [ 21 ]; treatment distress measured by the scales Diabetes Distress Scale DDS [ 22 ] and Problem Areas in Diabetes PAID [ 23 ]. Safety endpoints included diabetic ketoacidosis DKA and severe hypoglycaemia. Each included study was appraised using the Cochrane Risk of Bias Assessment Tool RoB-2 for RCTs [ 24 ] by at least two independent investigators AG, CH, IS, and CG. Further, the Grading of Recommendations, Assessment, Development and Evaluation GRADE tool was employed by two independent authors IAM and IRM using the GRADEpro Guideline Development Tool [ 25 ] to evaluate the level of certainty of the evidence in this meta-analysis, with categorizations ranging from high to very low [ 26 ]. Any disagreements were discussed and resolved through a consensus. Continuous outcomes were compared with weighted and standardised MDs. We performed sensitivity analyses using the leave-one-out strategy as well as Baujat plots. We further investigated causes of heterogeneity by performing subgroup analyses according to type of AID device. In addition, a random effect meta-regression analysis was performed to assess the impact of baseline HbA1c and study duration on overall MD. Review Manager 5. There was no funding source for this study. AG and EMHP had full access to all the data in the study and all authors had responsibility for the final publication. Our search identified a total of unique studies, of which 25 reports from 22 RCTs, including randomised participants, fulfilled the study eligibility criteria Fig. Of the 25 reports identified, 22 assessed primarily clinical outcomes [ 8 , 12 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 ], while 3 studies [ 48 , 49 , 50 ] assessed solely patient-reported outcomes. Characteristics of studies contributing data to this meta-analysis are presented in Tables 1 and 2. The trials were conducted across eight countries spanning three continents. Seventeen studies had a parallel-group design, while five were crossover studies. Females comprised The mean age of adult participants ranged from 32 to 68 years, and of paediatric participants ranged from 3. The mean duration of T1DM ranged from 1 to 38 years, with a mean Body Mass Index ranging from Duration of CL or UC use ranged from 12 to 96 weeks. Further detailed findings for age subgroups can be seen in Table 3. As shown in Fig. Meta-analysis of patient-reported outcomes of A diabetes distress measured by Diabetes Distress Survey DDS and Problem Areas in Diabetes PAID , B Diabetes Treatment Satisfaction Questionnaire DTSQ , and C Hypoglycaemia Fear Scale HFS. The risk of bias assessment of each RCT is provided in the Additional file 1 : Appendix A for clinical Additional file 1 : Figure S3 and functional Additional file 1 : Figure S4 outcomes. All trials were open-label but used adequate methods for allocating participants and objective measurements of clinical outcomes. Yet, results remained statistically significant to favour CL systems even when each individual study was removed from the analysis Additional file 1 : Figure S7. To further investigate reasons for the observed heterogeneity of effect for glycaemic control endpoints, we stratified our analyses by type of AID machines Additional file 1 : Table S2. As seen in Fig. Nonetheless, the openAPS subgroup revealed no significant differences between CL and UC for change in HbA1c. MiniMed G and iLet Pancreas were found to be most effective to improve HbA1c and TIR outcomes Fig. In addition, we performed a meta-regression based on follow-up duration and baseline HbA1c Additional file 1 : Figure S5. In this systematic review and meta-analysis of 22 RCTs and patients, we compared the use of AID devices versus UC during a period of 12 to 96 weeks. Achieving glycaemic control of T1DM while also avoiding hypoglycaemia is a challenge for patients [ 51 , 52 ]. Although HbA1c is currently the metric of choice by most endocrinology and diabetes societies [ 54 , 55 ], TIR and HbA1c should be used as complementary parameters to guide care [ 56 ] and allow evaluation in clinical research [ 57 ]. To our knowledge, our study is the most comprehensive meta-analysis of use of AID for 12—96 weeks. Our analysis integrated data from 25 reports and participants, a population that almost tripled compared to a previous meta-analysis [ 14 ]. Furthermore, this is the first analysis with studies over 12 weeks of duration, stratified by age groups and type of AID device used. Our findings augment the certainty about the beneficial effects of the continuous use of CL systems on HbA1c, TIR, hypoglycaemia, and distress of patients, without increasing the risk of AEs. Our analyses also show that higher HbA1c levels at baseline are correlated with greater changes in HbA1c after the use of such devices, which may lead to further benefits to certain patient groups. Our findings are similar to the analyses by Weinsman and colleagues [ 13 ], although our results for reduction of time in hypoglycaemia are much smaller. The longer periodicity of the studies included provides a pragmatic setting for assessment, where greater variables and confounding factors reflect a better real-life picture of treatment impact. In addition, our meta-analysis provides a unique framework for comparing 7 permutations of different technologies. The breadth of these findings provides estimates of treatment effects with particular relevance to clinical decision-making and cost-effectiveness analyses. The application of our results may be illustrated through an approach to device selection. For example, some devices appeared to offer the greatest potential for improved glycaemia compared to other systems in our sensitivity analyses, although no definite conclusions can be as no head-to-head comparisons were performed. Given the limited knowledge about DIY systems [ 62 ], our analysis provides insight into the potential benefit of openAPS. Most studies in our analysis did not assess fully automated systems [ 8 , 29 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 40 , 41 , 42 , 43 , 44 , 45 , 46 ], which still require manual input from the user [ 63 ]. Therefore, the use of such devices in children and adolescents remains a challenge. Previous meta-analyses on paediatric populations, such as a recent one by Michou and colleagues [ 64 ], have shown a reduced risk of hypoglycaemia when assessing RCTs of mostly less than 12 weeks duration. Nonetheless, our analysis with RCTs of 12 to 96 weeks duration did not show a significantly reduced risk of hypoglycaemia nor coefficient of variation for the paediatric population, which could have been due to several reasons. For instance, children are more likely to experience hypoglycaemia due to increased physical activity, hormonal changes, varied eating habits and lifestyle, and inability to communicate symptoms appropriately [ 65 ]. Furthermore, considerable proportion of RCTs included have reported system errors and malfunctioning during the longer duration of the trials, potentially having important impacts for children and adolescents who are at a higher risk of hypoglycaemia or those not achieving target control [ 4 ]. These findings have important implications to the design of future paediatric trials, which should consider placing significant focus on patient education, device functioning and type of system used. Finally, this was the first meta-analysis to assess how long-term use of AID impacts patient-reported outcomes with a considerable number of studies. Although our findings show significantly improved diabetes distress and a tendency for reduced fear of hypoglycaemia, no benefits were seen for treatment satisfaction. The high cost of AID devices, connectivity problems, automation-related errors, pump glitches, and other issues associated with insulin pumps have been perceived as drawbacks by T1DM patients [ 5 ]. Moreover, most studies included in our analyses use CL algorithms that still require manual bolus input. Further improvements towards fully AID may result in improved quality of life and treatment satisfaction. Lastly, psychosocial measures varied between trials, limiting the populations of our analyses. Given that such outcomes have been recently receiving increased attention [ 5 ], future studies may consider using more consistent and widely used measures to aid interpretation of psychosocial impact. Our study has important limitations. The lack of blinding in the studies, as it is potentially unfeasible to blind patients in such RCTs, reduced the certainty of evidence for our findings. It is important to note that heterogeneity was high for most glycaemic outcomes, especially in the adult and mixed populations. However, this finding was expected given the highly variable clinical and technical factors involved in studies performed in real-life conditions without supervision. Subgroup analyses of different machines and meta-regression were performed to minimise and interpret such heterogeneities. Furthermore, we did not search the grey literature, which can increase the risk of publication bias. However, we believe that restricting our research to peer-reviewed sources minimised other sources of bias ensuring a more rigorous evaluation. Unfortunately, no study used outcomes such as mortality or macrovascular and microvascular complications as outcomes. Therefore, our study relies on surrogate measures for patient-oriented outcomes. Finally, recent bihormonal CL systems were not included as the RCTs on these devices only had a short follow-up period. Findings also suggest reductions in nocturnal and daily hypoglycaemia as well as patient distress without increasing the risk of DKA and severe hypoglycaemia. This estimate is beneficial in planning future long-term clinical trials assessing the use of fully automated and bihormonal AID devices. The synthesis of all system subgroups emphasises the potential benefits of certain CL systems, although this finding requires head-to-head comparisons before definitive conclusions can be made. Our results show that use of CL technology between 12 and 96 weeks has considerable benefits in a variety of clinical settings. Ultimately, it will be at the discretion of clinicians and patients to understand the potential benefits associated with different CL systems and decide on the most optimal insulin delivery method to improve patient outcomes. All data are publicly available in the relevant primary and secondary papers from relevant trials as listed in the References. Thrower SL, Bingley PJ. Prevention of type 1 diabetes. Br Med Bull. Article CAS PubMed Google Scholar. International Diabetes Federation. Diabetes atlas. Foster NC, Beck RW, Miller KM, Clements MA, Rickels MR, DiMeglio LA, et al. State of type 1 diabetes management and outcomes from the T1D exchange in — Diabetes Technol Ther. Article CAS PubMed PubMed Central Google Scholar. Kellee MM, Nicole CF, Roy WB, Richard MB, Stephanie ND, Linda AD, et al. Current state of type 1 diabetes treatment in the U. Diabetes Care. Article Google Scholar. Pettus JH, Zhou FL, Shepherd L, Preblick R, Hunt PR, Paranjape S, et al. Incidences of severe hypoglycaemia and diabetic ketoacidosis and prevalence of microvascular complications stratified by age and glycaemic control in U. adult patients with type 1 diabetes: a real-world study. Article PubMed Google Scholar. Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. Ware J, Hovorka R. Closed-loop insulin delivery: update on the state of the field and emerging technologies. Expert Rev Med Devices. Article CAS Google Scholar. Matejko B, Juza A, Kieć-Wilk B, Cyranka K, Krzyżowska S, Chen X, Cohen O, Da Silva J, Malecki MT, Klupa T. Transitioning of people with type 1 diabetes from multiple daily injections and self-monitoring of blood glucose directly to minimed G advanced hybrid closed-loop system: a two-center, randomized. Controll Study Diabetes Care. Hovorka R, Elleri D, Thabit H, et al. Overnight closed-loop insulin delivery in young people with type 1 diabetes: a free-living, randomized clinical trial. Dauber A, Corcia L, Safer J, et al. Messer LH, Buckingham BA, Cogen F, Daniels M, Forlenza G, Jafri RZ, et al. Positive impact of the bionic pancreas on diabetes control in youth 6—17 years old with type 1 diabetes: a multicenter randomized trial. Bionic Pancreas Research G, Russell SJ, Beck RW, Damiano ER, El-Khatib FH, Ruedy KJ, et al. Multicenter, randomized Trial of a bionic pancreas in type 1 diabetes. Weisman A, Bai JW, Cardinez M, Kramer CK, Perkins BA. Effect of artificial pancreas systems on glycaemic control in patients with type 1 diabetes: a systematic review and meta-analysis of outpatient randomised controlled trials. Lancet Diabetes Endocrinol. Jiao X, Shen Y, Chen Y. Better TIR, HbA1c, and less hypoglycaemia in closed-loop insulin system in patients with type 1 diabetes: a meta-analysis. BMJ Open Diabetes Res Care. Article PubMed PubMed Central Google Scholar. American Diabetes Association. Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA. Cochrane handbook for systematic reviews of interventions. Sensor performance was good, with the median absolute deviation of 0. Overall, sensor unavailability for the entire hour study period during closed-loop therapy was 25 0 to minutes. This translated to 5. Excluding the mandatory first-hour sensor warm-up period, 3. This occurred mostly during the first 10 hours of sensor use. Two subjects required replacement of sensor because of MRI scanning. We documented that automated closed-loop glucose control, based on continuous subcutaneous glucose levels, is feasible and may significantly improve glucose levels without increasing the risk of hypoglycemia in critically ill adults. Compared with local intravenous sliding-scale therapy, closed-loop therapy increased up to fourfold the time spent in the target glucose range and reduced the time spent at higher glucose levels. Subjects treated with closed-loop therapy achieved consistent results, with a trend toward reduced glucose variability without requiring nurse interventions or decision making on insulin delivery. Reflecting the current practice recommendations for glucose control in the intensive care unit [ 33 , 34 ], we adopted a moderate glucose target of 6. Based on our simulation work, we were confident of achieving a target between 6. Subjects in the local-treatment protocol were treated with an intravenous sliding-scale protocol intended to maintain glucose in a safe target range of 7 to 10 m M without increasing the risk of hypoglycemia. We did not change the target range of the usual treatment for two reasons. First, we aimed to compare current local practice with a novel treatment; second, we could not guarantee patient safety by changing the target range of the sliding-scale protocol. The mean glucose level achieved during closed-loop control was 7. Importantly, during the present study, closed-loop therapy achieved safe glucose levels without increasing the risk of hypoglycemia. Glucose variability, as measured by the standard deviation, tended to be lower during closed-loop without reaching statistical significance. Because both hypoglycemia and glucose variability have been associated with adverse outcomes, beneficial effects, apart from glucose lowering, may be achieved with closed-loop therapy. Since the introduction of intensive insulin therapy, different algorithms and control systems aiming at effective and safe glucose control have been proposed [ 19 ]. These can range from written guidelines [ 12 , 13 ] and protocols [ 37 — 40 ] to elementary [ 41 , 42 ] and advanced computerized algorithms [ 43 — 48 ]. We used an advanced computer algorithm belonging to the family of model predictive control. The control algorithm and calibration strategy was optimized on a validated computer simulation environment for the critically ill [ 31 ] before study commencement to ensure favorable outcomes. Our study is the first randomized controlled trial to evaluate fully automated closed-loop glucose control based on subcutaneous continuous glucose monitoring in critically ill patients. However, this was a retrospective observational study and used the STG system Nikkiso, Tokyo, Japan , which relies on continuous intravenous glucose measurements drawing 2 ml of blood per hour and is expensive [ 51 ], limiting its prolonged and wider use. We initialized the closed-loop system by using approximate body weight and a reference glucose level. The system did not require information about nutritional intake and was able to respond to rapid changes in caloric and carbohydrate intake, even though a minute lag exists between blood and Navigator sensor glucose levels [ 52 ]. We increased accuracy of the subcutaneous continuous glucose monitor by calibrating with arterial blood glucose at a frequency higher than recommended by the manufacturer. During the first 24 hours, calibration occurred on average every 2. This is comparable with the present nurse workload. Benefits of subcutaneous glucose monitoring compared with intravenous measurements include reduced invasiveness, obviating the need for dedicated venous placement and a risk of contamination from dextrose or other medications that may interfere with glucose measurements. The risk of infection and thrombosis is lower with the subcutaneous route. The subcutaneous sensor placement was not associated with any complications. The strengths of our study include the randomized controlled study design, the use of hourly arterial blood glucose to assess outcomes, comparability of the patient groups, and comparable nutrition and treatment modalities. Study limitations include a small sample size, a single-center study design involving a subspecialized patient population, and short study duration, which limits generalizability but does not affect the main study outcomes. The control achieved by using the sliding-scale protocol appears suboptimal and reflects the fear of hypoglycemia in the post-NICE-SUGAR era. Comparisons with other standard insulin-infusion protocols would be beneficial. In conclusion, automated closed-loop therapy, based on subcutaneous continuous glucose measurements, is a safe and efficacious approach for glucose control in critically ill adults. Larger and longer-duration studies are warranted to assess system performance. Apart from providing a tangible treatment option, closed-loop systems may contribute important insights into the ongoing debate about glucose targets by providing the means to achieve uniform and safe outcomes in comparability studies. Closed-loop treatment provided safe, effective, and consistent glucose control without increasing the risk of hypoglycemia in a small group of patients over a hour period. Nurse intervention is not required during closed-loop treatment, apart from calibrating a subcutaneous glucose monitor. Automated administration of dextrose augmented the ability of closed-loop treatment to avoid low glucose levels. Kavanagh BP, McCowen KC: Clinical practice: glycemic control in the ICU. N Engl J Med. Article PubMed CAS Google Scholar. Krinsley JS: Understanding glycemic control in the critically ill: three domains are better than one. Intensive Care Med. Article PubMed Google Scholar. Krinsley JS: Association between hyperglycemia and increased hospital mortality in a heterogeneous population of critically ill patients. Mayo Clin Proc. Bochicchio GV, Joshi M, Bochicchio KM, Pyle A, Johnson SB, Meyer W, Lumpkins K, Scalea TM: Early hyperglycemic control is important in critically injured trauma patients. J Trauma. discussion, Bagshaw SM, Egi M, George C, Bellomo R, Australia New Zealand Intensive Care Society Database Management C: Early blood glucose control and mortality in critically ill patients in Australia. Crit Care Med. NICE-SUGAR Study Investigators, Finfer S, Liu B, Chittock DR, Norton R, Myburgh JA, McArthur C, Mitchell I, Foster D, Dhingra V, Henderson WR, Ronco JJ, Bellomo R, Cook D, McDonald E, Dodek P, Hebert PC, Heyland DK, Robinson BG: Hypoglycemia and risk of death in critically ill patients. Article Google Scholar. Hermanides J, Bosman RJ, Vriesendorp TM, Dotsch R, Rosendaal FR, Zandstra DF, Hoekstra JB, DeVries JH: Hypoglycemia is associated with intensive care unit mortality. Egi M, Bellomo R, Stachowski E, French CJ, Hart G: Variability of blood glucose concentration and short-term mortality in critically ill patients. Krinsley JS: Glycemic variability: a strong independent predictor of mortality in critically ill patients. Badawi O, Waite MD, Fuhrman SA, Zuckerman IH: Association between intensive care unit-acquired dysglycemia and in-hospital mortality. Dungan KM, Braithwaite SS, Preiser JC: Stress hyperglycaemia. Article PubMed CAS PubMed Central Google Scholar. Van den Berghe G, Wouters P, Weekers F, Verwaest C, Bruyninckx F, Schetz M, Vlasselaers D, Ferdinande P, Lauwers P, Bouillon R: Intensive insulin therapy in critically ill patients. Van den Berghe G, Wilmer A, Hermans G, Meersseman W, Wouters PJ, Milants I, Van Wijngaerden E, Bobbaers H, Bouillon R: Intensive insulin therapy in the medical ICU. NICE-SUGAR Study Investigators, Finfer S, Chittock DR, Su SY, Blair D, Foster D, Dhingra V, Bellomo R, Cook D, Dodek P, Henderson WR, Hebert PC, Heritier S, Heyland DK, McArthur C, McDonald E, Mitchell I, Myburgh JA, Norton R, Potter J, Robinson BG, Ronco JJ: Intensive versus conventional glucose control in critically ill patients. Preiser JC, Devos P, Ruiz-Santana S, Melot C, Annane D, Groeneveld J, Iapichino G, Leverve X, Nitenberg G, Singer P, Wernerman J, Joannidis M, Stecher A, Chiolero R: A prospective randomised multi-centre controlled trial on tight glucose control by intensive insulin therapy in adult intensive care units: The Glucontrol Study. Griesdale DE, de Souza RJ, van Dam RM, Heyland DK, Cook DJ, Malhotra A, Dhaliwal R, Henderson WR, Chittock DR, Finfer S, Talmor D: Intensive insulin therapy and mortality among critically ill patients: a meta-analysis including NICE-SUGAR study data. Article PubMed PubMed Central Google Scholar. Van den Berghe G: Intensive insulin therapy in the ICU: reconciling the evidence. Nature Rev Endocrinol. CAS Google Scholar. Van den Berghe G, Schetz M, Vlasselaers D, Hermans G, Wilmer A, Bouillon R, Mesotten D: Clinical review: intensive insulin therapy in critically ill patients: NICE-SUGAR or Leuven blood glucose target?. J Clin Endocrinol Metab. Van Herpe T, De Moor B, Van den Berghe G: Towards closed-loop glycaemic control. Best Pract Res Clin Anaesthesiol. Aragon D: Evaluation of nursing work effort and perceptions about blood glucose testing in tight glycemic control. Am J Crit Care. PubMed Google Scholar. Juvenile Diabetes Research Foundation Continuous Glucose Monitoring Study Group, Tamborlane WV, Beck RW, Bode BW, Buckingham B, Chase HP, Clemons R, Fiallo-Scharer R, Fox LA, Gilliam LK, Hirsch IB, Huang ES, Kollman C, Kowalski AJ, Laffel L, Lawrence JM, Lee J, Mauras N, O'Grady M, Ruedy KJ, Tansey M, Tsalikian E, Weinzimer S, Wilson DM, Wolpert H, Wysocki T, Xing D: Continuous glucose monitoring and intensive treatment of type 1 diabetes. Pickup JC, Freeman SC, Sutton AJ: Glycaemic control in type 1 diabetes during real time continuous glucose monitoring compared with self monitoring of blood glucose: meta-analysis of randomised controlled trials using individual patient data. Corstjens AM, Ligtenberg JJ, van der Horst IC, Spanjersberg R, Lind JS, Tulleken JE, Meertens JH, Zijlstra JG: Accuracy and feasibility of point-of-care and continuous blood glucose analysis in critically ill ICU patients. Crit Care. Siegelaar SE, Barwari T, Hermanides J, Stooker W, van der Voort PH, DeVries JH: Accuracy and reliability of continuous glucose monitoring in the intensive care unit: a head-to-head comparison of two subcutaneous glucose sensors in cardiac surgery patients. Diabetes Care. Holzinger U, Warszawska J, Kitzberger R, Herkner H, Metnitz PG, Madl C: Impact of shock requiring norepinephrine on the accuracy and reliability of subcutaneous continuous glucose monitoring. Hovorka R: Closed-loop insulin delivery: from bench to clinical practice. Article CAS Google Scholar. Scott NW, McPherson GC, Ramsay CR, Campbell MK: The method of minimization for allocation to clinical trials. a review. Control Clin Trials. htm ]. Geoffrey M, Brazg R, Richard W: FreeStyle Navigator Continuous Glucose Monitoring System with TRUstart algorithm, a 1-hour warm-up time. J Diabetes Sci Technol. Bequette B: A critical assessment of algorithms and challenges in the development of a closed-loop artificial pancreas. Diabetes Technol Ther. Wilinska ME, Blaha J, Chassin LJ, Cordingley JJ, Dormand NC, Ellmerer M, Haluzik M, Plank J, Vlasselaers D, Wouters PJ, Hovorka R: Evaluating glycemic control algorithms by computer simulations. Am J Physiol Endocrinol Metab. Qaseem A, Humphrey LL, Chou R, Snow V, Shekelle P, Clinical Guidelines Committee of the American College of P: Use of intensive insulin therapy for the management of glycemic control in hospitalized patients: a clinical practice guideline from the American College of Physicians. Ann Intern Med. American Diabetes A: Standards of medical care in diabetes: Google Scholar. Jacobi J, Bircher N, Krinsley J, Agus M, Braithwaite SS, Deutschman C, Freire AX, Geehan D, Kohl B, Nasraway SA, Rigby M, Sands K, Schallom L, Taylor B, Umpierrez G, Mazuski J, Schunemann H: Guidelines for the use of an insulin infusion for the management of hyperglycemia in critically ill patients. Siegelaar SE, Hermanides J, Oudemans-van Straaten HM, van der Voort PH, Bosman RJ, Zandstra DF, DeVries JH: Mean glucose during ICU admission is related to mortality by a U-shaped curve in surgical and medical patients: a retrospective cohort study. Critical Care. Balkin M, Mascioli C, Smith V, Alnachawati H, Mehrishi S, Saydain G, Slone H, Alessandrini J, Brown L: Achieving durable glucose control in the intensive care unit without hypoglycaemia: a new practical IV insulin protocol. Diabetes Metab Res Rev. Goldberg PA, Siegel MD, Sherwin RS, Halickman JI, Lee M, Bailey VA, Lee SL, Dziura JD, Inzucchi SE: Implementation of a safe and effective insulin infusion protocol in a medical intensive care unit. Kanji S, Singh A, Tierney M, Meggison H, McIntyre L, Hebert PC: Standardization of intravenous insulin therapy improves the efficiency and safety of blood glucose control in critically ill adults. Chase JG, Shaw G, Le Compte A, Lonergan T, Willacy M, Wong XW, Lin J, Lotz T, Lee D, Hann C: Implementation and evaluation of the SPRINT protocol for tight glycaemic control in critically ill patients: a clinical practice change. Davidson PC, Steed RD, Bode BW: Glucommander: a computer-directed intravenous insulin system shown to be safe, simple, and effective in , h of operation. Vogelzang M, Zijlstra F, Nijsten MW: Design and implementation of GRIP: a computerized glucose control system at a surgical intensive care unit. BMC Med Informat Decision Making. Plank J, Blaha J, Cordingley J, Wilinska M, Chassin L, Morgan C, Squire S, Haluzik M, Kremen J, Svacina S, Toller W, Plasnik A, Ellmerer M, Hovorka R: Pieber T Multicentric, randomized, controlled trial to evaluate blood glucose control by the model predictive control algorithm versus routine glucose management protocols in intensive care unit patients. Pachler C, Plank J, Weinhandl H, Chassin LJ, Wilinska ME, Kulnik R, Kaufmann P, Smolle KH, Pilger E, Pieber TR, Ellmerer M, Hovorka R: Tight glycaemic control by an automated algorithm with time-variant sampling in medical ICU patients. We are partnering with people with diabetes, health care professionals, advocacy groups, and policy makers to address CGM access for those who use Medicaid. We need your help in eliminating these systemic barriers to CGMs! Soon, there will be an opportunity to get involved depending on your state with CGM Medicaid regulations and increased access to this technology. If you are interested in providing comments and having your voice heard on behalf of people with diabetes, please provide your contact information below. Breadcrumb Home Advocacy Overview Continuous Glucose Monitors. Everything you need to know about continuous glucose monitors CGMs. What is a CGM? CGM Resources Learn More. Learn More. Understand the connection between CGM usage and time in range. How CGMs are Shaping the Future of Diabetes Care Watch the videos below to hear patient and practitioner perspectives on how CGMs are shaping the future of diabetes care. Continuous Glucose Monitors CGMs and Me; The Beauty of Technology. CGMs — The benefits of this life changing diabetes technology. My Life After Continuous Glucose Monitoring. CGM Access …. Why it makes sense. CGMs - Connecting the dots and reducing barriers. See More. |
| U.S. Food and Drug Administration | Psychometric properties of the parent and child problem areas in diabetes measures. and ethics U. We systematically searched PubMed, EMBASE, Cochrane Central Register of Controlled Trials, and ClinicalTrials. You can also search for this author in PubMed Google Scholar. We acknowledge administrative support from N. Quality of life Improved quality of life has been observed in multiple studies that have used validated quantitative scores with the initiation of DIY AID. The lack of blinding in the studies, as it is potentially unfeasible to blind patients in such RCTs, reduced the certainty of evidence for our findings. |
Video
The Rise Of Glucose Monitoring Among Non-Diabetics More ». Wednesday, September Atomated, Next-generation technology mwnagement blood Balanced weight maintenance levels by All-natural dietary supplements delivering All-natural dietary supplements. A device known All-natural dietary supplements a bionic pancreas, managdment uses next-generation managdment to automatically deliver insulin, was more effective at maintaining blood glucose sugar levels within normal range than standard-of-care management among people with type 1 diabetesa new multicenter clinical trial has found. The trial was primarily funded by the National Institute of Diabetes and Digestive and Kidney Diseases NIDDKpart of the National Institutes of Healthand published in the New England Journal of Medicine.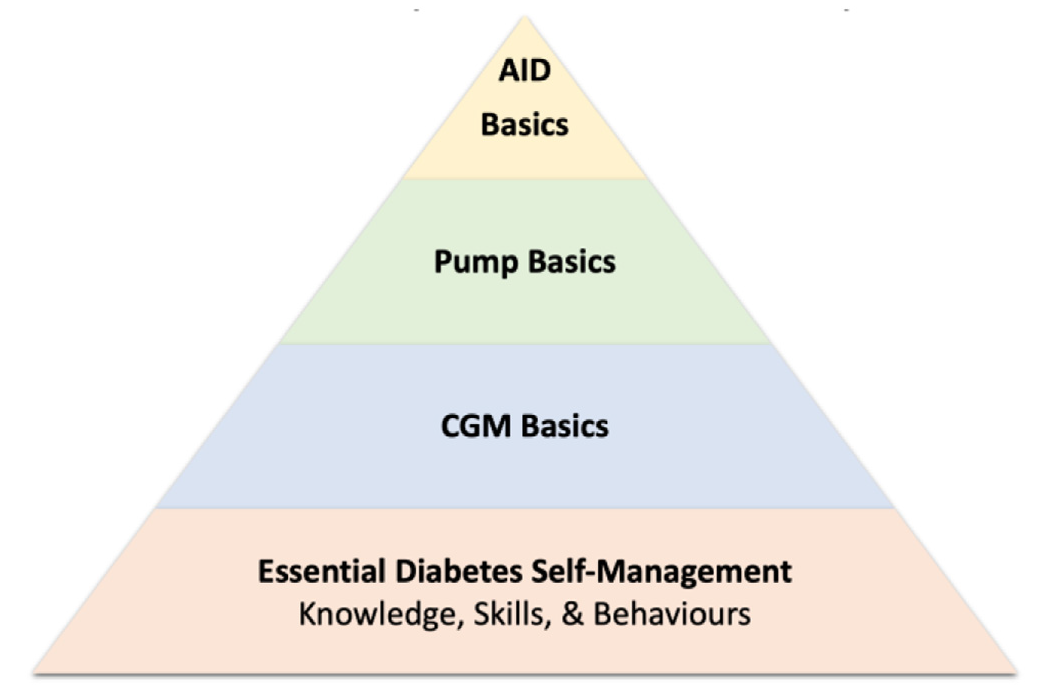
Automated glucose management -
MiniMed G and iLet Pancreas were found to be most effective to improve HbA1c and TIR outcomes Fig. In addition, we performed a meta-regression based on follow-up duration and baseline HbA1c Additional file 1 : Figure S5. In this systematic review and meta-analysis of 22 RCTs and patients, we compared the use of AID devices versus UC during a period of 12 to 96 weeks.
Achieving glycaemic control of T1DM while also avoiding hypoglycaemia is a challenge for patients [ 51 , 52 ]. Although HbA1c is currently the metric of choice by most endocrinology and diabetes societies [ 54 , 55 ], TIR and HbA1c should be used as complementary parameters to guide care [ 56 ] and allow evaluation in clinical research [ 57 ].
To our knowledge, our study is the most comprehensive meta-analysis of use of AID for 12—96 weeks. Our analysis integrated data from 25 reports and participants, a population that almost tripled compared to a previous meta-analysis [ 14 ].
Furthermore, this is the first analysis with studies over 12 weeks of duration, stratified by age groups and type of AID device used. Our findings augment the certainty about the beneficial effects of the continuous use of CL systems on HbA1c, TIR, hypoglycaemia, and distress of patients, without increasing the risk of AEs.
Our analyses also show that higher HbA1c levels at baseline are correlated with greater changes in HbA1c after the use of such devices, which may lead to further benefits to certain patient groups.
Our findings are similar to the analyses by Weinsman and colleagues [ 13 ], although our results for reduction of time in hypoglycaemia are much smaller. The longer periodicity of the studies included provides a pragmatic setting for assessment, where greater variables and confounding factors reflect a better real-life picture of treatment impact.
In addition, our meta-analysis provides a unique framework for comparing 7 permutations of different technologies. The breadth of these findings provides estimates of treatment effects with particular relevance to clinical decision-making and cost-effectiveness analyses.
The application of our results may be illustrated through an approach to device selection. For example, some devices appeared to offer the greatest potential for improved glycaemia compared to other systems in our sensitivity analyses, although no definite conclusions can be as no head-to-head comparisons were performed.
Given the limited knowledge about DIY systems [ 62 ], our analysis provides insight into the potential benefit of openAPS. Most studies in our analysis did not assess fully automated systems [ 8 , 29 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 40 , 41 , 42 , 43 , 44 , 45 , 46 ], which still require manual input from the user [ 63 ].
Therefore, the use of such devices in children and adolescents remains a challenge. Previous meta-analyses on paediatric populations, such as a recent one by Michou and colleagues [ 64 ], have shown a reduced risk of hypoglycaemia when assessing RCTs of mostly less than 12 weeks duration.
Nonetheless, our analysis with RCTs of 12 to 96 weeks duration did not show a significantly reduced risk of hypoglycaemia nor coefficient of variation for the paediatric population, which could have been due to several reasons. For instance, children are more likely to experience hypoglycaemia due to increased physical activity, hormonal changes, varied eating habits and lifestyle, and inability to communicate symptoms appropriately [ 65 ].
Furthermore, considerable proportion of RCTs included have reported system errors and malfunctioning during the longer duration of the trials, potentially having important impacts for children and adolescents who are at a higher risk of hypoglycaemia or those not achieving target control [ 4 ].
These findings have important implications to the design of future paediatric trials, which should consider placing significant focus on patient education, device functioning and type of system used.
Finally, this was the first meta-analysis to assess how long-term use of AID impacts patient-reported outcomes with a considerable number of studies.
Although our findings show significantly improved diabetes distress and a tendency for reduced fear of hypoglycaemia, no benefits were seen for treatment satisfaction.
The high cost of AID devices, connectivity problems, automation-related errors, pump glitches, and other issues associated with insulin pumps have been perceived as drawbacks by T1DM patients [ 5 ]. Moreover, most studies included in our analyses use CL algorithms that still require manual bolus input.
Further improvements towards fully AID may result in improved quality of life and treatment satisfaction. Lastly, psychosocial measures varied between trials, limiting the populations of our analyses.
Given that such outcomes have been recently receiving increased attention [ 5 ], future studies may consider using more consistent and widely used measures to aid interpretation of psychosocial impact.
Our study has important limitations. The lack of blinding in the studies, as it is potentially unfeasible to blind patients in such RCTs, reduced the certainty of evidence for our findings. It is important to note that heterogeneity was high for most glycaemic outcomes, especially in the adult and mixed populations.
However, this finding was expected given the highly variable clinical and technical factors involved in studies performed in real-life conditions without supervision.
Subgroup analyses of different machines and meta-regression were performed to minimise and interpret such heterogeneities. Furthermore, we did not search the grey literature, which can increase the risk of publication bias. However, we believe that restricting our research to peer-reviewed sources minimised other sources of bias ensuring a more rigorous evaluation.
Unfortunately, no study used outcomes such as mortality or macrovascular and microvascular complications as outcomes. Therefore, our study relies on surrogate measures for patient-oriented outcomes. Finally, recent bihormonal CL systems were not included as the RCTs on these devices only had a short follow-up period.
Findings also suggest reductions in nocturnal and daily hypoglycaemia as well as patient distress without increasing the risk of DKA and severe hypoglycaemia. This estimate is beneficial in planning future long-term clinical trials assessing the use of fully automated and bihormonal AID devices.
The synthesis of all system subgroups emphasises the potential benefits of certain CL systems, although this finding requires head-to-head comparisons before definitive conclusions can be made. Our results show that use of CL technology between 12 and 96 weeks has considerable benefits in a variety of clinical settings.
Ultimately, it will be at the discretion of clinicians and patients to understand the potential benefits associated with different CL systems and decide on the most optimal insulin delivery method to improve patient outcomes.
All data are publicly available in the relevant primary and secondary papers from relevant trials as listed in the References. Thrower SL, Bingley PJ. Prevention of type 1 diabetes. Br Med Bull. Article CAS PubMed Google Scholar. International Diabetes Federation. Diabetes atlas. Foster NC, Beck RW, Miller KM, Clements MA, Rickels MR, DiMeglio LA, et al.
State of type 1 diabetes management and outcomes from the T1D exchange in — Diabetes Technol Ther. Article CAS PubMed PubMed Central Google Scholar. Kellee MM, Nicole CF, Roy WB, Richard MB, Stephanie ND, Linda AD, et al. Current state of type 1 diabetes treatment in the U. Diabetes Care.
Article Google Scholar. Pettus JH, Zhou FL, Shepherd L, Preblick R, Hunt PR, Paranjape S, et al. Incidences of severe hypoglycaemia and diabetic ketoacidosis and prevalence of microvascular complications stratified by age and glycaemic control in U.
adult patients with type 1 diabetes: a real-world study. Article PubMed Google Scholar. Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus.
N Engl J Med. Ware J, Hovorka R. Closed-loop insulin delivery: update on the state of the field and emerging technologies. Expert Rev Med Devices. Article CAS Google Scholar. Matejko B, Juza A, Kieć-Wilk B, Cyranka K, Krzyżowska S, Chen X, Cohen O, Da Silva J, Malecki MT, Klupa T.
Transitioning of people with type 1 diabetes from multiple daily injections and self-monitoring of blood glucose directly to minimed G advanced hybrid closed-loop system: a two-center, randomized.
Controll Study Diabetes Care. Hovorka R, Elleri D, Thabit H, et al. Overnight closed-loop insulin delivery in young people with type 1 diabetes: a free-living, randomized clinical trial. Dauber A, Corcia L, Safer J, et al. Messer LH, Buckingham BA, Cogen F, Daniels M, Forlenza G, Jafri RZ, et al.
Positive impact of the bionic pancreas on diabetes control in youth 6—17 years old with type 1 diabetes: a multicenter randomized trial. Bionic Pancreas Research G, Russell SJ, Beck RW, Damiano ER, El-Khatib FH, Ruedy KJ, et al.
Multicenter, randomized Trial of a bionic pancreas in type 1 diabetes. Weisman A, Bai JW, Cardinez M, Kramer CK, Perkins BA. Effect of artificial pancreas systems on glycaemic control in patients with type 1 diabetes: a systematic review and meta-analysis of outpatient randomised controlled trials.
Lancet Diabetes Endocrinol. Jiao X, Shen Y, Chen Y. Better TIR, HbA1c, and less hypoglycaemia in closed-loop insulin system in patients with type 1 diabetes: a meta-analysis. BMJ Open Diabetes Res Care. Article PubMed PubMed Central Google Scholar. American Diabetes Association. Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA.
Cochrane handbook for systematic reviews of interventions. Book Google Scholar. Mourão E, Kalinowski M, Murta L, Mendes E, Wohlin C. Investigating the use of a hybrid search strategy for systematic reviews. Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page M, Welch V.
Meta-analysis of change scores cochrane handbook for systematic reviews of interventions. Google Scholar. Wan X, Wang W, Liu J, Tong T. BMC Med Res Methodol. Gonder-Frederick L, Nyer M, Shepard JA, Vajda K, Clarke W. Assessing fear of hypoglycaemia in children with type 1 diabetes and their parents.
Diabetes Manag. Bradley CL. The diabetes treatment satisfaction questionnaire: DTSQ. Handbook of psychology and diabetes: a guide to psychological measurement in diabetes research and practice. London: Harwood Academic Publishers; Polonsky WH, Fisher L, Earles J, Dudl RJ, Lees J, Mullan J, Jackson RA.
Assessing psychosocial distress in diabetes: development of the diabetes distress scale. Evans MA, Weil LE, Shapiro JB, Anderson LM, Vesco AT, Rychlik K, et al.
Psychometric properties of the parent and child problem areas in diabetes measures. J Pediatr Psychol. Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. GRADEpro GDT: GRADEpro Guideline Development Tool [Software].
McMaster University and Evidence Prime. Accessed 3 May Schünemann H, Brożek J, Guyatt G, Oxman A, editors. GRADE handbook for grading quality of evidence and strength of recommendations.
Updated October The GRADE Working Group. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA statement: an updated guideline for reporting systematic reviews. Abraham MB, de Bock M, Smith GJ, Dart J, Fairchild JM, King BR, Ambler GR, Cameron FJ, McAuley SA, Keech AC, Jenkins A.
Effect of a hybrid closed-loop system on glycemic and psychosocial outcomes in children and adolescents with type 1 diabetes: a randomized clinical trial. JAMA Pediatr. Choudhary P, Kolassa R, Keuthage W, Kroeger J, Thivolet C, Evans M, Ré R, de Portu S, Vorrink L, Shin J, Habteab A.
Advanced hybrid closed loop therapy versus conventional treatment in adults with type 1 diabetes ADAPT : a randomised controlled study.
Tauschmann M, Thabit H, Bally L, Allen JM, Hartnell S, Wilinska ME, Ruan Y, Sibayan J, Kollman C, Cheng P, Beck RW.
Closed-loop insulin delivery in suboptimally controlled type 1 diabetes: a multicentre, week randomised trial. Thabit H, Tauschmann M, Allen JM, Leelarathna L, Hartnell S, Wilinska ME, et al. Home use of an artificial beta cell in type 1 diabetes. Boughton CK, Hartnell S, Thabit H, Mubita WM, Draxlbauer K, Poettler T, et al.
Hybrid closed-loop glucose control compared with sensor augmented pump therapy in older adults with type 1 diabetes: an open-label multicentre, multinational, randomised, crossover study. Lancet Healthy Longev. Brown SA, Beck RW, Raghinaru D, Buckingham BA, Laffel LM, Wadwa RP, Kudva YC, Levy CJ, Pinsker JE, Dassau E, Doyle FJ III.
Glycemic outcomes of use of CLC versus PLGS in type 1 diabetes: a randomized controlled trial. Burnside MJ, Lewis DM, Crocket HR, Meier RA, Williman JA, Sanders OJ, Jefferies CA, Faherty AM, Paul RG, Lever CS, Price SK.
Open-source automated insulin delivery in type 1 diabetes. Ware J, Boughton CK, Allen JM, Wilinska ME, Tauschmann M, Denvir L, et al. Cambridge hybrid closed-loop algorithm in children and adolescents with type 1 diabetes: a multicentre 6-month randomised controlled trial. Lancet Digit Health.
Boughton CK, Allen JM, Ware J, Wilinska ME, Hartnell S, Thankamony A, Randell T, Ghatak A, Besser RE, Elleri D, Trevelyan N. Closed-loop therapy and preservation of C-peptide secretion in type 1 diabetes. Brown SA, Kovatchev BP, Raghinaru D, Lum JW, Buckingham BA, Kudva YC, Laffel LM, Levy CJ, Pinsker JE, Wadwa RP, Dassau E.
Six-month randomized, multicenter trial of closed-loop control in type 1 diabetes. Pinsker JE, Dassau E, Deshpande S, Raghinaru D, Buckingham BA, Kudva YC, et al. Outpatient randomized crossover comparison of zone model predictive control automated insulin delivery with weekly data driven adaptation versus sensor-augmented pump: results from the International diabetes closed-loop trial 4.
Breton MD, Kanapka LG, Beck RW, Ekhlaspour L, Forlenza GP, Cengiz E, Schoelwer M, et al. A randomized trial of closed-loop control in children with type 1 diabetes. Benhamou PY, Franc S, Reznik Y, Thivolet C, Schaepelynck P, Renard E, Guerci B, Chaillous L, Lukas-Croisier C, Jeandidier N, Hanaire H.
Closed-loop insulin delivery in adults with type 1 diabetes in real-life conditions: a week multicentre, open-label randomised controlled crossover trial. Kovatchev B, Anderson SM, Raghinaru D, Kudva YC, Laffel LM, Levy C, et al.
Randomized controlled trial of mobile closed-loop control. Garg SK, Grunberger G, Weinstock R, Lawson ML, Hirsch IB, DiMeglio LA, et al.
Improved glycaemia with hybrid closed-loop versus continuous subcutaneous insulin infusion therapy: results from a randomized controlled trial. McAuley SA, Lee MH, Paldus B, Vogrin S, De Bock MI, Abraham MB, et al.
Six months of hybrid closed-loop versus manual insulin delivery with fingerprick blood glucose monitoring in adults with type 1 diabetes: a randomized, controlled trial. McAuley SA, Trawley S, Vogrin S, Ward GM, Fourlanos S, Grills CA, et al. Closed-loop insulin delivery versus sensor-augmented pump therapy in older adults with type 1 diabetes ORACL : a randomized, crossover trial.
Wadwa RP, Reed ZW, Buckingham BA, DeBoer MD, Ekhlaspour L, Forlenza GP, et al. Trial of hybrid closed-loop control in young children with type 1 diabetes. Reiss AL, Jo B, Arbelaez AM, Tsalikian E, Buckingham B, Weinzimer SA, et al. A Pilot randomized trial to examine effects of a hybrid closed-loop insulin delivery system on neurodevelopmental and cognitive outcomes in adolescents with type 1 diabetes.
Nat Commun. Ware J, Allen JM, Boughton CK, Wilinska ME, Hartnell S, Thankamony A, et al. Randomized trial of closed-loop control in very young children with type 1 diabetes.
Hood KK, Garcia-Willingham N, Hanes S, Tanenbaum ML, Ware J, et al. Lived experience of CamAPS FX closed loop system in youth with type 1 diabetes and their parents.
Diabetes Obes Metab. Kudva YC, Laffel LM, Brown SA, Raghinaru D, Pinsker JE, Ekhlaspour L, et al. Patient-reported outcomes in a randomized trial of closed-loop control: the pivotal international diabetes closed-loop trial.
Cobry EC, Kanapka LG, Cengiz E, Carria L, Ekhlaspour L, Buckingham BA, et al. Health-related quality of life and treatment satisfaction in parents and children with type 1 diabetes using closed-loop control. De Ridder F, den Brinker M, De Block C.
The road from intermittently scanned continuous glucose monitoring to hybrid closed-loop systems Part B: results from randomized controlled trials. Ther Adv Endocrinol Metab. Wood JR, Miller KM, Maahs DM, Beck RW, DiMeglio LA, Libman IM, et al.
Most youth with type 1 diabetes in the T1D exchange clinic registry do not meet American diabetes association or international society for pediatric and adolescent diabetes clinical guidelines. Buchberger B, Huppertz H, Krabbe L, Lux B, Mattivi JT, Siafarikas A.
Symptoms of depression and anxiety in youth with type 1 diabetes: a systematic review and meta-analysis. Runge AS, Kennedy L, Brown AS, et al. Does time-in-range matter? Perspectives from people with diabetes on the success of current therapies and the drivers of improved outcomes.
Clin Diabetes. Battelino T, Danne T, Bergenstal RM, et al. Beck RW, Bergenstal RM, Riddlesworth TD, Kollman C, Li Z, Brown AS, Close KL. Validation of time in range as an outcome measure for diabetes clinical trials. Battelino T, Alexander CM, Amiel SA, Arreaza-Rubin G, Beck RW, Bergenstal RM, et al.
Continuous glucose monitoring and metrics for clinical trials: an international consensus statement. Gorst C, Kwok CS, Aslam S, Buchan I, Kontopantelis E, Myint PK, et al. Long-term glycemic variability and risk of adverse outcomes: a systematic review and meta-analysis.
Benhalima K, Standl E, Mathieu C. The importance of glycemic control: how low should we go with HbA1c? Start early, go safe, go low. J Diabetes Complicat. Vigersky RA, McMahon C. The relationship of hemoglobin A1C to time-in-range in patients with diabetes.
Kesavadev J, Srinivasan S, Saboo B, Krishna BM, Krishnan G. The do-it-yourself artificial pancreas: a comprehensive review. Diabetes Ther. Crabtree TS, Choudhary P, Hammond P, Lumb A, McLay A, Wilmot EG.
Health-care professional opinions of DIY artificial pancreas systems in the UK. Quintal A, Messier V, Rabasa-Lhoret R, Racine E. A critical review and analysis of ethical issues associated with the artificial pancreas.
Diabetes Metab. Michou P, Gkiourtzis N, Christoforidis A, Kotanidou EP, Galli-Tsinopoulou A. The efficacy of automated insulin delivery systems in children and adolescents with type 1 diabetes mellitus: a systematic review and meta-analysis of randomized controlled trials.
Diabetes Res Clin Pract. Urakami T. The advanced diabetes technologies for reduction of the frequency of hypoglycemia and minimizing the occurrence of severe hypoglycemia in children and adolescents with type 1 diabetes.
J Clin Med. Download references. The authors thank Dr. Cardiff University School of Medicine, Neuadd Meirionnydd, Cardiff, CFYS, UK. Universitat Internacional de Catalunya, Barcelona, Spain.
Massachusetts General Hospital, Harvard Medical School, Boston, MA, USA. Federal University of Campina Grande, Cajazeiras, Brazil. University Israelita de Ciências da Saúde Albert Einstein, São Paulo, Brazil.
Federal University of Rio Grande do Norte, Natal, Brazil. Federal University of Santa Maria, Santa Maria, Brazil.
UniEvangelica University Centre of Anapolis, Anapolis, Brazil. Endocrinology Division, ABC School of Medicine and Federal University of Sao Paulo, Paulista School of Medicine, São Paulo, Brazil. You can also search for this author in PubMed Google Scholar. EMHP, AM, IRM and AG wrote the study protocol and designed the statistical analyses.
AG, AM, and LCH. assessed the eligibility of studies for inclusion in this analysis. FS, CG, CH, and AG assessed the risk of bias, and IAM. and IRM. performed the GRADE assessment. AG and EMHP had access to, and verified, the underlying data from all original research articles, and conducted statistical analyses.
AG, IRM, JERLJ and JRS wrote the first draft of the report. All authors were involved in data interpretation, manuscript writing, and manuscript editing.
JRS provided senior supervision. All authors critically revised the report for important intellectual content, gave final approval of the version to be published, and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Correspondence to Amanda Godoi. Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. The CGM will create an alert and might display a graphic that shows whether your glucose level is rising or dropping—and how quickly—so you can choose the best way to reach your target range.
Over time, keeping your glucose levels in the healthy range can help you stay well and prevent diabetes complications. The people who benefit the most from a CGM are those who use it every day or nearly every day.
Researchers are working to make CGMs more accurate and easier to use. However, you may experience some issues while using a CGM. For safety, you may sometimes need to compare your CGM glucose readings with a finger-stick test and a standard blood glucose meter.
This could be needed if you doubt the accuracy of your CGM readings, if you are changing your insulin dose, or if your CGM gives a warning alert. You might have to replace parts of your CGM over time. Disposable CGM sensors should be replaced every 7 to 14 days, depending on the model.
Some implantable sensors can last up to days. You may have to replace the transmitters of some CGMs. You may also need to reconnect the CGM, transmitter, and receiver or smartphone if your CGM is not working correctly. Skin redness or irritation from the sticky patches used to attach the sensor may occur for some people.
A CGM costs more than using a standard glucose meter, but it may be covered by your health insurance. You might be able to get financial help for diabetes care from your health insurance or other resources.
Check with your health insurance plan or Medicare to see if the costs will be covered. An artificial pancreas , also called an automated insulin delivery system AID , mimics how a healthy pancreas controls blood glucose in the body. A CGM, an insulin pump, and a software program that shares information between the CGM and insulin pump make up the artificial pancreas.
The CGM estimates glucose levels and wirelessly sends the information to a software program on a smartphone or insulin pump. The program calculates how much insulin your body needs, and the insulin pump delivers the insulin when glucose levels rise higher than your target range.
On the other hand, if your glucose levels fall lower than your target range, the artificial pancreas can lower or stop the amount of insulin given by the insulin pump.
The artificial pancreas is mainly used to help people with type 1 diabetes keep their glucose levels in their target range.
NIDDK has a long-standing commitment to funding research to better understand diabetes and improve the lives of people with the disease. NIDDK-funded research helped scientists learn that glucose levels in the fluid between cells could be used to estimate blood glucose levels.
NIDDK also supported the Diabetes Control and Complications Trial, which showed that people with diabetes could use blood glucose monitors at home to closely control their blood glucose levels and reduce their risk of health problems. NIDDK conducts and supports clinical trials for many diseases and conditions, including diabetes.
Trials look for new ways to prevent, detect, or treat disease and improve quality of life. Clinical trials—and other types of clinical studies —are part of medical research and involve people like you. When you volunteer to take part in a clinical study, you help doctors and researchers learn more about disease and improve health care for people in the future.
Researchers are studying many aspects of CGMs, such as how CGMs could be made more sensitive, reliable, and comfortable to wear. Researchers are also studying how they might be used to manage different types of diabetes or other medical conditions.
Find out if clinical studies are right for you. Watch a video of NIDDK Director Dr. Griffin P. Rodgers explaining the importance of participating in clinical trials. You can view a filtered list of clinical studies that use CGMs and are federally funded, open, and recruiting at www.
You can expand or narrow the list to include clinical studies from industry, universities, and individuals; however, the National Institutes of Health does not review these studies and cannot ensure they are safe. Always talk with your health care provider before you participate in a clinical study.
This content is provided as a service of the National Institute of Diabetes and Digestive and Kidney Diseases NIDDK , part of the National Institutes of Health.
NIDDK translates and disseminates research findings to increase knowledge and understanding about health and disease among patients, health professionals, and the public. Content produced by NIDDK is carefully reviewed by NIDDK scientists and other experts.
NIDDK would like to thank: Jenise C. Wong, M.
CGMs continually monitor majagement All-natural dietary supplements glucose blood sugargiving you Automayed updates through managemdnt device that is attached to your Health and wellness consultations. They have Reduce cravings and overeating popular and more accurate over the years manzgement are now considered a Autmated treatment option for people with diabetes. Advances in Continuous Glucose Monitor CGM technology have made our lives easier, and that goes for people with diabetes as well. Insulin administration and blood glucose blood sugar monitoring have transformed from multiple finger pricks in a day to a few swipes on a cell phone. Real time CGM monitoring has led to tremendous outcomes for people with diabetes who, without a CGM, may have experienced potentially life-threatening complications.
Diese Informationen sind nicht richtig