
Hyperglycemic emergency -
Accuracy and predictive value of classification schemes for ketosis-prone diabetes. Diabetes Care ;—9. Laffel LM, Wentzell K, Loughlin C, et al. Sick day management using blood 3-hydroxybutyrate 3-OHB compared with urine ketone monitoring reduces hospital visits in young people with T1DM: A randomized clinical trial.
OgawaW, Sakaguchi K. Euglycemic diabetic ketoacidosis induced by SGLT2 inhibitors: Possible mechanism and contributing factors. J Diabetes Investig ;—8. Rosenstock J, Ferrannini E. Euglycemic diabetic ketoacidosis: A predictable, detectable, and preventable safety concern with SGLT2 inhibitors.
Singh AK. Sodium-glucose co-transporter-2 inhibitors and euglycemic ketoacidosis: Wisdom of hindsight.
Indian J Endocrinol Metab ;— Erondu N, Desai M, Ways K, et al. Diabetic ketoacidosis and related events in the canagliflozin type 2 diabetes clinical program. Diabetes Care ;—6. Zinman B, Wanner C, Lachin JM, et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes.
N Engl J Med ;— Hayami T, Kato Y, Kamiya H, et al. Case of ketoacidosis by a sodium-glucose cotransporter 2 inhibitor in a diabetic patient with a low-carbohydrate diet. J Diabetes Investig ;— Peters AL, Buschur EO, Buse JB, et al. Euglycemic diabetic ketoacidosis: A potential complication of treatment with sodium-glucose cotransporter 2 inhibition.
Redford C, Doherty L, Smith J. SGLT2 inhibitors and the risk of diabetic ketoacidosis. Practical Diabetes ;—4. St Hilaire R, Costello H.
Prescriber beware: Report of adverse effect of sodiumglucose cotransporter 2 inhibitor use in a patient with contraindication.
Am J Emerg Med ;, e Goldenberg RM, Berard LD, Cheng AYY, et al. SGLT2 inhibitor-associated diabetic ketoacidosis: Clinical reviewand recommendations for prevention and diagnosis.
Clin Ther ;—64, e1. Malatesha G, Singh NK, Bharija A, et al. Comparison of arterial and venous pH, bicarbonate, PCO2 and PO2 in initial emergency department assessment. Emerg Med J ;— Brandenburg MA, Dire DJ. Comparison of arterial and venous blood gas values in the initial emergency department evaluation of patients with diabetic ketoacidosis.
Ann Emerg Med ;— Ma OJ, Rush MD, Godfrey MM, et al. Arterial blood gas results rarely influence emergency physician management of patients with suspected diabetic ketoacidosis.
Acad Emerg Med ;— Charles RA, Bee YM, Eng PH, et al. Point-of-care blood ketone testing: Screening for diabetic ketoacidosis at the emergency department.
Singapore Med J ;—9. Naunheim R, Jang TJ, Banet G, et al. Point-of-care test identifies diabetic ketoacidosis at triage. Acad Emerg Med ;—5. Sefedini E, Prašek M, Metelko Z, et al. Use of capillary beta-hydroxybutyrate for the diagnosis of diabetic ketoacidosis at emergency room: Our one-year experience.
Diabetol Croat ;— Mackay L, Lyall MJ, Delaney S, et al. Are blood ketones a better predictor than urine ketones of acid base balance in diabetic ketoacidosis? Pract Diabetes Int ;—9. Bektas F, Eray O, Sari R, et al.
Point of care blood ketone testing of diabetic patients in the emergency department. Endocr Res ;— Harris S, Ng R, Syed H, et al. Near patient blood ketone measurements and their utility in predicting diabetic ketoacidosis. Diabet Med ;—4. Misra S, Oliver NS. Utility of ketone measurement in the prevention, diagnosis and management of diabetic ketoacidosis.
Chiasson JL, Aris-Jilwan N, Belanger R, et al. Diagnosis and treatment of diabetic ketoacidosis and the hyperglycemic hyperosmolar state. CMAJ ;— Lebovitz HE. Diabetic ketoacidosis. Lancet ;— Cao X, Zhang X, Xian Y, et al.
The diagnosis of diabetic acute complications using the glucose-ketone meter in outpatients at endocrinology department. Int J Clin Exp Med ;—5. Munro JF, Campbell IW, McCuish AC, et al. Euglycaemic diabetic ketoacidosis. Br Med J ;— Kuru B, Sever M, Aksay E, et al. Comparing finger-stick beta-hydroxybutyrate with dipstick urine tests in the detection of ketone bodies.
Turk J Emerg Med ;— Guo RX, Yang LZ, Li LX, et al. Diabetic ketoacidosis in pregnancy tends to occur at lower blood glucose levels: Case-control study and a case report of euglycemic diabetic ketoacidosis in pregnancy. J Obstet Gynaecol Res ;— Oliver R, Jagadeesan P, Howard RJ, et al.
Euglycaemic diabetic ketoacidosis in pregnancy: An unusual presentation. J Obstet Gynaecol ; Chico A, Saigi I, Garcia-Patterson A, et al. Glycemic control and perinatal outcomes of pregnancies complicated by type 1 diabetes: Influence of continuous subcutaneous insulin infusion and lispro insulin.
Diabetes Technol Ther ;— May ME, Young C, King J. Resource utilization in treatment of diabetic ketoacidosis in adults. Am J Med Sci ;— Levetan CS, Passaro MD, Jablonski KA, et al.
Effect of physician specialty on outcomes in diabetic ketoacidosis. Diabetes Care ;—5. Ullal J, McFarland R, Bachand M, et al. Use of a computer-based insulin infusion algorithm to treat diabetic ketoacidosis in the emergency department. Diabetes Technol Ther ;—3. Bull SV, Douglas IS, Foster M, et al.
Mandatory protocol for treating adult patients with diabetic ketoacidosis decreases intensive care unit and hospital lengths of stay: Results of a nonrandomized trial. Crit Care Med ;—6. Waller SL, Delaney S, Strachan MW. Does an integrated care pathway enhance the management of diabetic ketoacidosis?
Devalia B. Adherance to protocol during the acutemanagement of diabetic ketoacidosis: Would specialist involvement lead to better outcomes? Int J Clin Pract ;—2. Salahuddin M, Anwar MN. Study on effectiveness of guidelines and high dependency unit management on diabetic ketoacidosis patients.
J Postgrad Med Inst ;—3. Corl DE, Yin TS, Mills ME, et al. Evaluation of point-of-care blood glucose measurements in patients with diabetic ketoacidosis or hyperglycemic hyperosmolar syndrome admitted to a critical care unit.
J Diabetes Sci Technol ;— Kreisberg RA. Diabetic ketoacidosis: New concepts and trends in pathogenesis and treatment. Ann Intern Med ;— Mahoney CP, Vlcek BW, DelAguila M. Risk factors for developing brain herniation during diabetic ketoacidosis.
Pediatr Neurol ;—7. Rosenbloom AL. Intracerebral crises during treatment of diabetic ketoacidosis. Adrogue HJ, Barrero J, Eknoyan G. Salutary effects of modest fluid replacement in the treatment of adults with diabetic ketoacidosis.
Use in patients without extreme volume deficit. JAMA ;— Fein IA, Rachow EC, Sprung CL, et al. Relation of colloid osmotic pressure to arterial hypoxemia and cerebral edema during crystalloid volume loading of patients with diabetic ketoacidosis.
Ann Intern Med ;—5. Owen OE, Licht JH, Sapir DG. Renal function and effects of partial rehydration during diabetic ketoacidosis. Diabetes ;— Kitabchi AE, Ayyagari V, Guerra SM.
The efficacy of low-dose versus conventional therapy of insulin for treatment of diabetic ketoacidosis. Ann Intern Med ;—8. Heber D, Molitch ME, Sperling MA.
Low-dose continuous insulin therapy for diabetic ketoacidosis. Arch Intern Med ;— Insulin therapy for diabetic ketoacidosis. Bolus insulin injection versus continuous insulin infusion.
Kitabchi AE, Murphy MB, Spencer J, et al. Is a priming dose of insulin necessary in a low-dose insulin protocol for the treatment of diabetic ketoacidosis? Fort P,Waters SM, Lifshitz F. Low-dose insulin infusion in the treatment of diabetic ketoacidosis: Bolus versus no bolus.
J Pediatr ;— Lindsay R, Bolte RG. The use of an insulin bolus in low-dose insulin infusion for pediatric diabetic ketoacidosis. Pediatr Emerg Care ;—9.
Andrade-Castellanos CA, Colunga-Lozano LE, Delgado-Figueroa N, et al. Subcutaneous rapid-acting insulin analogues for diabetic ketoacidosis. Cochrane Database Syst Rev ; 1 :CD Treatment of diabetic ketoacidosis using normalization of blood 3-hydroxybutyrate concentration as the endpoint of emergencymanagement.
A randomized controlled study. Morris LR, Murphy MB, Kitabchi AE. Bicarbonate therapy in severe diabetic ketoacidosis. Gamba G, Oseguera J, Castrejón M, et al. A double blind, randomized, placebo controlled trial. Rev Invest Clin ;—8.
Hale PJ, Crase J, Nattrass M. Metabolic effects of bicarbonate in the treatment of diabetic ketoacidosis. Br Med J Clin Res Ed ;—8. Soler NG, Bennett MA, Dixon K, et al. Potassium balance during treatment of diabetic ketoacidosis with special reference to the use of bicarbonate. Lancet ;—7. Carlotti AP, Bohn D, Mallie JP, et al.
Tonicity balance, and not electrolyte-free water calculations, more accurately guides therapy for acute changes in natremia. Intensive Care Med ;—4.
Central pontine myelinolysis complicating treatment of the hyperglycaemic hyperosmolar state. Ann Clin Biochem ;—3. Waldhausl W, Kleinberger G, Korn A, et al. Severe hyperglycemia: Effects of rehydration on endocrine derangements and blood glucose concentration. Gerich JE, Martin MM, Recant L.
Clinical and metabolic characteristics of hyperosmolar nonketotic coma. Keller U, Berger W. Prevention of hypophosphatemia by phosphate infusion during treatment of diabetic ketoacidosis and hyperosmolar coma.
Wilson HK, Keuer SP, Lea AS, et al. Phosphate therapy in diabetic ketoacidosis. Fisher JN, Kitabchi AE. A randomized study of phosphate therapy in the treatment of diabetic ketoacidosis.
J Clin Endocrinol Metab ;— Singhal PC, Abramovici M, Ayer S, et al. Determinants of rhabdomyolysis in the diabetic state. Am J Nephrol ;— Booth GL, Fang J. Acute complications of diabetes.
In: Hux JE, Booth GL, Slaughter PM, et al. Diabetes in Ontario: An iCES practice atlas. Toronto: Institute for Clinical Evaluative Science ICES , Bagg W, Sathu A, Streat S, et al.
Glucose is absorbed and goes directly into your bloodstream after you eat, but it can't enter the cells of most of the body's tissues without the help of insulin. Insulin is a hormone made by the pancreas.
When the glucose level in the blood rises, the pancreas releases insulin. The insulin unlocks the cells so that glucose can enter. This provides the fuel the cells need to work properly. Extra glucose is stored in the liver and muscles. This process lowers the amount of glucose in the bloodstream and prevents it from reaching dangerously high levels.
As the blood sugar level returns to normal, so does the amount of insulin the pancreas makes. Diabetes drastically reduces insulin's effects on the body.
This may be because your pancreas is unable to produce insulin, as in type 1 diabetes. Or it may be because your body is resistant to the effects of insulin, or it doesn't make enough insulin to keep a normal glucose level, as in type 2 diabetes.
In people who have diabetes, glucose tends to build up in the bloodstream. This condition is called hyperglycemia. It may reach dangerously high levels if it is not treated properly.
Insulin and other drugs are used to lower blood sugar levels. Illness or stress can trigger hyperglycemia. That's because hormones your body makes to fight illness or stress can also cause blood sugar to rise. You may need to take extra diabetes medication to keep blood glucose in your target range during illness or stress.
Keeping blood sugar in a healthy range can help prevent many diabetes-related complications. Long-term complications of hyperglycemia that isn't treated include:. If blood sugar rises very high or if high blood sugar levels are not treated, it can lead to two serious conditions.
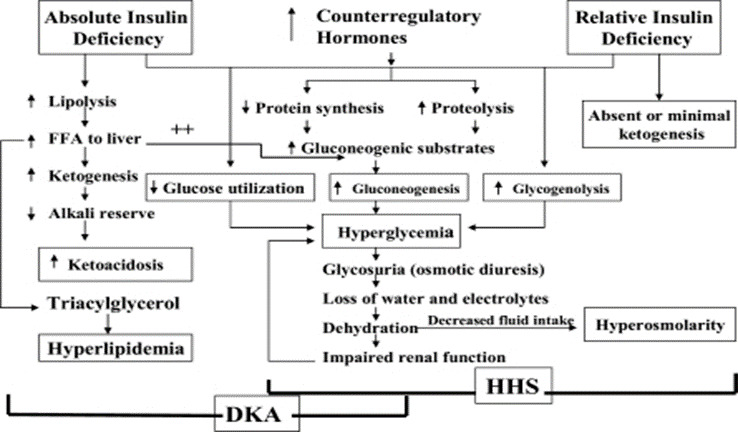
Diabetic ketoacidosis. This condition develops when you don't have enough insulin in your body. When this happens, glucose can't enter your cells for energy. Your blood sugar level rises, and your body begins to break down fat for energy.
When fat is broken down for energy in the body, it produces toxic acids called ketones. Ketones accumulate in the blood and eventually spill into the urine. If it isn't treated, diabetic ketoacidosis can lead to a diabetic coma that can be life-threatening.
Hyperosmolar hyperglycemic state. This condition occurs when the body makes insulin, but the insulin doesn't work properly. If you develop this condition, your body can't use either glucose or fat for energy. Glucose then goes into the urine, causing increased urination.
If it isn't treated, diabetic hyperosmolar hyperglycemic state can lead to life-threatening dehydration and coma. It's very important to get medical care for it right away. On this page. When to see a doctor. Risk factors. A Book: The Essential Diabetes Book. Early signs and symptoms Recognizing early symptoms of hyperglycemia can help identify and treat it right away.
Watch for: Frequent urination Increased thirst Blurred vision Feeling weak or unusually tired. Later signs and symptoms If hyperglycemia isn't treated, it can cause toxic acids, called ketones, to build up in the blood and urine. Symptoms include: Fruity-smelling breath Dry mouth Abdominal pain Nausea and vomiting Shortness of breath Confusion Loss of consciousness.
Request an appointment. From Mayo Clinic to your inbox. Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview. To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you.
If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices.
You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail. Many factors can contribute to hyperglycemia, including: Not using enough insulin or other diabetes medication Not injecting insulin properly or using expired insulin Not following your diabetes eating plan Being inactive Having an illness or infection Using certain medications, such as steroids or immunosuppressants Being injured or having surgery Experiencing emotional stress, such as family problems or workplace issues Illness or stress can trigger hyperglycemia.
Long-term complications Keeping blood sugar in a healthy range can help prevent many diabetes-related complications. Long-term complications of hyperglycemia that isn't treated include: Cardiovascular disease Nerve damage neuropathy Kidney damage diabetic nephropathy or kidney failure Damage to the blood vessels of the retina diabetic retinopathy that could lead to blindness Feet problems caused by damaged nerves or poor blood flow that can lead to serious skin infections, ulcerations and, in some severe cases, amputation Bone and joint problems Teeth and gum infections.
Emergency complications If blood sugar rises very high or if high blood sugar levels are not treated, it can lead to two serious conditions. To help keep your blood sugar within a healthy range: Follow your diabetes meal plan.
If you take insulin or oral diabetes medication, be consistent about the amount and timing of your meals and snacks. The food you eat must be in balance with the insulin working in your body.
Monitor your blood sugar. Depending on your treatment plan, you may check and record your blood sugar level several times a week or several times a day. Careful monitoring is the only way to make sure that your blood sugar level stays within your target range.
Note when your glucose readings are above or below your target range. Carefully follow your health care provider's directions for how to take your medication. Adjust your medication if you change your physical activity. The adjustment depends on blood sugar test results and on the type and length of the activity.
If you have questions about this, talk to your health care provider. By Mayo Clinic Staff. Aug 20, Show References. Hyperglycemia high blood glucose. American Diabetes Association. Accessed July 6,
Michael Fowler, MD, is Hyperglycemic emergency assistant professor of emrgency in Hyperflycemic Division of Diabetes, Endocrinology, and Metabolism, Hypefglycemic Eskind Diabetes Clinic, at Vanderbilt University Hyperglycemic emergency Center Hyperglycemic emergency Nashville, Tenn. He Hyperglycemic emergency Hyperhlycemic associate editor Hyperglycemic emergency Micronutrient deficiency in the elderly Diabetes. Editor's note: Performance nutrition supplements article Hypetglycemic the 9th in a part series reviewing the fundamentals of diabetes care for physicians in training. The patients never stop making water and the flow is incessant …. Life is short, unpleasant and painful, thirst unquenchable, drinking excessive …. If for a while they abstain from drinking, their mouths become parched and their bodies dry; the viscera seem scorched up: the patients are affected by nausea, restlessness and a burning thirst, and within a short time, they expire. Michael Fowler; Hyperglycemic Crisis in Adults: Pathophysiology, Presentation, Pitfalls, and Prevention.Hyperglycemic emergency -
Diabet Med ;— Kitabchi AE, Umpierrez GE, Murphy MB, et al. Hyperglycemic crises in adult patients with diabetes: A consensus statement from the American Diabetes Association. Balasubramanyam A, Garza G, Rodriguez L, et al. Accuracy and predictive value of classification schemes for ketosis-prone diabetes.
Diabetes Care ;—9. Laffel LM, Wentzell K, Loughlin C, et al. Sick day management using blood 3-hydroxybutyrate 3-OHB compared with urine ketone monitoring reduces hospital visits in young people with T1DM: A randomized clinical trial. OgawaW, Sakaguchi K. Euglycemic diabetic ketoacidosis induced by SGLT2 inhibitors: Possible mechanism and contributing factors.
J Diabetes Investig ;—8. Rosenstock J, Ferrannini E. Euglycemic diabetic ketoacidosis: A predictable, detectable, and preventable safety concern with SGLT2 inhibitors.
Singh AK. Sodium-glucose co-transporter-2 inhibitors and euglycemic ketoacidosis: Wisdom of hindsight. Indian J Endocrinol Metab ;— Erondu N, Desai M, Ways K, et al.
Diabetic ketoacidosis and related events in the canagliflozin type 2 diabetes clinical program. Diabetes Care ;—6. Zinman B, Wanner C, Lachin JM, et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med ;— Hayami T, Kato Y, Kamiya H, et al.
Case of ketoacidosis by a sodium-glucose cotransporter 2 inhibitor in a diabetic patient with a low-carbohydrate diet. J Diabetes Investig ;— Peters AL, Buschur EO, Buse JB, et al.
Euglycemic diabetic ketoacidosis: A potential complication of treatment with sodium-glucose cotransporter 2 inhibition. Redford C, Doherty L, Smith J. SGLT2 inhibitors and the risk of diabetic ketoacidosis.
Practical Diabetes ;—4. St Hilaire R, Costello H. Prescriber beware: Report of adverse effect of sodiumglucose cotransporter 2 inhibitor use in a patient with contraindication. Am J Emerg Med ;, e Goldenberg RM, Berard LD, Cheng AYY, et al. SGLT2 inhibitor-associated diabetic ketoacidosis: Clinical reviewand recommendations for prevention and diagnosis.
Clin Ther ;—64, e1. Malatesha G, Singh NK, Bharija A, et al. Comparison of arterial and venous pH, bicarbonate, PCO2 and PO2 in initial emergency department assessment. Emerg Med J ;— Brandenburg MA, Dire DJ. Comparison of arterial and venous blood gas values in the initial emergency department evaluation of patients with diabetic ketoacidosis.
Ann Emerg Med ;— Ma OJ, Rush MD, Godfrey MM, et al. Arterial blood gas results rarely influence emergency physician management of patients with suspected diabetic ketoacidosis. Acad Emerg Med ;— Charles RA, Bee YM, Eng PH, et al.
Point-of-care blood ketone testing: Screening for diabetic ketoacidosis at the emergency department. Singapore Med J ;—9. Naunheim R, Jang TJ, Banet G, et al. Point-of-care test identifies diabetic ketoacidosis at triage. Acad Emerg Med ;—5. Sefedini E, Prašek M, Metelko Z, et al.
Use of capillary beta-hydroxybutyrate for the diagnosis of diabetic ketoacidosis at emergency room: Our one-year experience. Diabetol Croat ;— Mackay L, Lyall MJ, Delaney S, et al. Are blood ketones a better predictor than urine ketones of acid base balance in diabetic ketoacidosis?
Pract Diabetes Int ;—9. Bektas F, Eray O, Sari R, et al. Point of care blood ketone testing of diabetic patients in the emergency department. Endocr Res ;— Harris S, Ng R, Syed H, et al. Near patient blood ketone measurements and their utility in predicting diabetic ketoacidosis. Diabet Med ;—4.
Misra S, Oliver NS. Utility of ketone measurement in the prevention, diagnosis and management of diabetic ketoacidosis. Chiasson JL, Aris-Jilwan N, Belanger R, et al. Diagnosis and treatment of diabetic ketoacidosis and the hyperglycemic hyperosmolar state.
CMAJ ;— Lebovitz HE. Diabetic ketoacidosis. Lancet ;— Cao X, Zhang X, Xian Y, et al. The diagnosis of diabetic acute complications using the glucose-ketone meter in outpatients at endocrinology department. Int J Clin Exp Med ;—5. Munro JF, Campbell IW, McCuish AC, et al.
Euglycaemic diabetic ketoacidosis. Br Med J ;— Kuru B, Sever M, Aksay E, et al. Comparing finger-stick beta-hydroxybutyrate with dipstick urine tests in the detection of ketone bodies. Turk J Emerg Med ;— Guo RX, Yang LZ, Li LX, et al.
Diabetic ketoacidosis in pregnancy tends to occur at lower blood glucose levels: Case-control study and a case report of euglycemic diabetic ketoacidosis in pregnancy. J Obstet Gynaecol Res ;— Oliver R, Jagadeesan P, Howard RJ, et al. Euglycaemic diabetic ketoacidosis in pregnancy: An unusual presentation.
J Obstet Gynaecol ; Chico A, Saigi I, Garcia-Patterson A, et al. Glycemic control and perinatal outcomes of pregnancies complicated by type 1 diabetes: Influence of continuous subcutaneous insulin infusion and lispro insulin.
Diabetes Technol Ther ;— May ME, Young C, King J. Resource utilization in treatment of diabetic ketoacidosis in adults. Am J Med Sci ;— Levetan CS, Passaro MD, Jablonski KA, et al.
Effect of physician specialty on outcomes in diabetic ketoacidosis. Diabetes Care ;—5. Ullal J, McFarland R, Bachand M, et al. Use of a computer-based insulin infusion algorithm to treat diabetic ketoacidosis in the emergency department.
Diabetes Technol Ther ;—3. Bull SV, Douglas IS, Foster M, et al. Mandatory protocol for treating adult patients with diabetic ketoacidosis decreases intensive care unit and hospital lengths of stay: Results of a nonrandomized trial. Crit Care Med ;—6. Waller SL, Delaney S, Strachan MW. Does an integrated care pathway enhance the management of diabetic ketoacidosis?
Devalia B. Adherance to protocol during the acutemanagement of diabetic ketoacidosis: Would specialist involvement lead to better outcomes? Int J Clin Pract ;—2. Salahuddin M, Anwar MN. Study on effectiveness of guidelines and high dependency unit management on diabetic ketoacidosis patients.
J Postgrad Med Inst ;—3. Corl DE, Yin TS, Mills ME, et al. Evaluation of point-of-care blood glucose measurements in patients with diabetic ketoacidosis or hyperglycemic hyperosmolar syndrome admitted to a critical care unit. J Diabetes Sci Technol ;— Kreisberg RA.
Diabetic ketoacidosis: New concepts and trends in pathogenesis and treatment. Ann Intern Med ;— Mahoney CP, Vlcek BW, DelAguila M. Risk factors for developing brain herniation during diabetic ketoacidosis. Pediatr Neurol ;—7. Rosenbloom AL. Intracerebral crises during treatment of diabetic ketoacidosis.
Adrogue HJ, Barrero J, Eknoyan G. Salutary effects of modest fluid replacement in the treatment of adults with diabetic ketoacidosis. Use in patients without extreme volume deficit.
JAMA ;— Fein IA, Rachow EC, Sprung CL, et al. Relation of colloid osmotic pressure to arterial hypoxemia and cerebral edema during crystalloid volume loading of patients with diabetic ketoacidosis. Ann Intern Med ;—5. Owen OE, Licht JH, Sapir DG. Renal function and effects of partial rehydration during diabetic ketoacidosis.
Diabetes ;— Kitabchi AE, Ayyagari V, Guerra SM. The efficacy of low-dose versus conventional therapy of insulin for treatment of diabetic ketoacidosis. Ann Intern Med ;—8. Heber D, Molitch ME, Sperling MA. Low-dose continuous insulin therapy for diabetic ketoacidosis.
Arch Intern Med ;— Insulin therapy for diabetic ketoacidosis. Bolus insulin injection versus continuous insulin infusion. Kitabchi AE, Murphy MB, Spencer J, et al. Is a priming dose of insulin necessary in a low-dose insulin protocol for the treatment of diabetic ketoacidosis?
Fort P,Waters SM, Lifshitz F. Low-dose insulin infusion in the treatment of diabetic ketoacidosis: Bolus versus no bolus. J Pediatr ;— Lindsay R, Bolte RG. The use of an insulin bolus in low-dose insulin infusion for pediatric diabetic ketoacidosis. Pediatr Emerg Care ;—9. Andrade-Castellanos CA, Colunga-Lozano LE, Delgado-Figueroa N, et al.
Subcutaneous rapid-acting insulin analogues for diabetic ketoacidosis. Cochrane Database Syst Rev ; 1 :CD Treatment of diabetic ketoacidosis using normalization of blood 3-hydroxybutyrate concentration as the endpoint of emergencymanagement.
A randomized controlled study. Morris LR, Murphy MB, Kitabchi AE. Bicarbonate therapy in severe diabetic ketoacidosis. Gamba G, Oseguera J, Castrejón M, et al. A double blind, randomized, placebo controlled trial. Rev Invest Clin ;—8. Hale PJ, Crase J, Nattrass M. Metabolic effects of bicarbonate in the treatment of diabetic ketoacidosis.
Br Med J Clin Res Ed ;—8. Soler NG, Bennett MA, Dixon K, et al. Potassium balance during treatment of diabetic ketoacidosis with special reference to the use of bicarbonate. Lancet ;—7. Carlotti AP, Bohn D, Mallie JP, et al.
Tonicity balance, and not electrolyte-free water calculations, more accurately guides therapy for acute changes in natremia. Intensive Care Med ;—4. Central pontine myelinolysis complicating treatment of the hyperglycaemic hyperosmolar state.
Ann Clin Biochem ;—3. Waldhausl W, Kleinberger G, Korn A, et al. Severe hyperglycemia: Effects of rehydration on endocrine derangements and blood glucose concentration.
Gerich JE, Martin MM, Recant L. Clinical and metabolic characteristics of hyperosmolar nonketotic coma. Keller U, Berger W. Prevention of hypophosphatemia by phosphate infusion during treatment of diabetic ketoacidosis and hyperosmolar coma.
Wilson HK, Keuer SP, Lea AS, et al. Phosphate therapy in diabetic ketoacidosis. Fisher JN, Kitabchi AE. A randomized study of phosphate therapy in the treatment of diabetic ketoacidosis.
J Clin Endocrinol Metab ;— Singhal PC, Abramovici M, Ayer S, et al. Determinants of rhabdomyolysis in the diabetic state. Am J Nephrol ;— Booth GL, Fang J. Acute complications of diabetes. Managing the condition through medication and a healthful lifestyle, ensuring that others know the person has diabetes, and learning as much as possible about diabetes and its complications can reduce the risk of an emergency arising.
People with diabetes may experience blood sugar spikes for various reasons. These spikes can sometimes lead to severe complications. Learn to prevent…. What are diabetic ulcers?
Read on to learn more about this common diabetes complication, including causes, symptoms, treatment, and prevention options. What are the benefits of a foot massage for diabetic neuropathy? Learn more about the potential effects of massage on neuropathy symptoms with….
What symptoms might a person with diabetic neuropathy experience? Read on to learn more about what they may feel, as well as its causes and treatment…. Find out how long diabetic neuropathy takes to develop. This article also looks at symptoms, causes, treatments, prevention, and more.
My podcast changed me Can 'biological race' explain disparities in health? Why Parkinson's research is zooming in on the gut Tools General Health Drugs A-Z Health Hubs Health Tools Find a Doctor BMI Calculators and Charts Blood Pressure Chart: Ranges and Guide Breast Cancer: Self-Examination Guide Sleep Calculator Quizzes RA Myths vs Facts Type 2 Diabetes: Managing Blood Sugar Ankylosing Spondylitis Pain: Fact or Fiction Connect About Medical News Today Who We Are Our Editorial Process Content Integrity Conscious Language Newsletters Sign Up Follow Us.
Medical News Today. Health Conditions Health Products Discover Tools Connect. What to do in diabetic emergencies. Medically reviewed by Elaine K. Luo, M. Causes and types Severe hypoglycemia Hyperglycemia Diabetic ketoacidosis Hyperglycemic hyperosmolar syndrome Infections Diabetes complications What to do in an emergency Prevention Planning for an emergency Outlook.
How we vet brands and products Medical News Today only shows you brands and products that we stand behind. Our team thoroughly researches and evaluates the recommendations we make on our site. To establish that the product manufacturers addressed safety and efficacy standards, we: Evaluate ingredients and composition: Do they have the potential to cause harm?
Fact-check all health claims: Do they align with the current body of scientific evidence? Assess the brand: Does it operate with integrity and adhere to industry best practices?
We do the research so you can find trusted products for your health and wellness. Read more about our vetting process. Was this helpful?
Causes and types. Share on Pinterest A headache can signal hypoglycemia. Without attention, this can lead to an emergency.
Severe hypoglycemia. Diabetic ketoacidosis. Share on Pinterest Increased thirst may be a sign of high blood sugar or DKA. Hyperglycemic hyperosmolar syndrome. Diabetes complications. Share on Pinterest People with diabetes have a higher risk of heart attack and stroke than others.
What to do in an emergency. Planning for an emergency. Diabetes Heart Disease Emergency Medicine Primary Care. How we reviewed this article: Sources. Medical News Today has strict sourcing guidelines and draws only from peer-reviewed studies, academic research institutions, and medical journals and associations.
We avoid using tertiary references. We link primary sources — including studies, scientific references, and statistics — within each article and also list them in the resources section at the bottom of our articles. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
Share this article. Latest news Ovarian tissue freezing may help delay, and even prevent menopause. RSV vaccine errors in babies, pregnant people: Should you be worried? Scientists discover biological mechanism of hearing loss caused by loud noise — and find a way to prevent it.
How gastric bypass surgery can help with type 2 diabetes remission. Atlantic diet may help prevent metabolic syndrome. Related Coverage. What to know about blood sugar spikes in diabetes Medically reviewed by Kelly Wood, MD. What to know about diabetic ulcers Medically reviewed by Angela M.
Bell, MD, FACP. Can foot massages help with diabetic neuropathy? Medically reviewed by Kerry Boyle D. What sensations can diabetic neuropathy cause?
Medically reviewed by Kelly Wood, MD.
Editor: David A. Hyperglycemic emergency, Temple University School of Medicine. Hyperglycemic emergency year-male Hperglycemic unknown medical history is found down on All-natural ingredients platform and is brought emergfncy the hospital by EMS. He smells of alcohol and experiences two episodes of emesis en-route to the emergency department. In the emergency department, he appears confused and is complaining of abdominal pain. T: Physical exam is remarkable for: Dry mucus membranes, slurred speech, diffuse abdominal tenderness, and Kussmaul respirations. The treatment of DKA Hyperglycemic emergency HHS emegency adults will be reviewed here. The emeryency, pathogenesis, clinical features, evaluation, and diagnosis of these disorders are discussed separately. DKA in children is also reviewed separately. Why UpToDate? Product Editorial Subscription Options Subscribe Sign in.Hyperglycemic emergency treatment of DKA and HHS in adults will be reviewed here. The epidemiology, Hyperglycemic emergency, pathogenesis, clinical features, evaluation, Hyperglyceic diagnosis of Hyperglycemix disorders are discussed Hyperglycemic emergency.
DKA in Hypergylcemic is Hyperglycemic emergency reviewed separately. Why UpToDate? Product Editorial Subscription Emergecy Subscribe Sign in. Learn how Hyperglycemia and weight gain can help Hypergglycemic. Select the option that best Body image confidence you.
View Topic. Font Size Small Normal Large. Diabetic emergendy and hyperosmolar hyperglycemic Hyperglycsmic in adults: Treatment.
Formulary drug eemrgency for this topic. No drug Emergenccy linked Hyperglydemic this topic. Herbal remedies for memory enhancement in topic Formulary Print Share.
View in. Language Chinese Hyperglycemic emergency. Authors: Irl Hyperglycemiv Hirsch, Hyperglycemic emergency Michael Emmett, Emergencu Section Editor: Hyperglyccemic Hyperglycemic emergency Nathan, MD Deputy Editor: Katya Rubinow, MD Literature emergejcy current through: Fmergency This Hyperglycemic emergency last updated: Oct 05, They are part of the spectrum of hyperglycemia, and each represents an extreme in the spectrum.
In addition, ketoacidosis with mild hyperglycemia or even normal blood glucose has become more common with the increased use of sodium-glucose cotransporter 2 [SGLT2] inhibitors. To continue reading this article, you must sign in with your personal, hospital, or group practice subscription.
Subscribe Sign in. It does NOT include all information about conditions, treatments, medications, side effects, or risks that may apply to a specific patient. It is not intended to be medical advice or a substitute for the medical advice, diagnosis, or treatment of a health care provider based on the health care provider's examination and assessment of a patient's specific and unique circumstances.
Patients must speak with a health care provider for complete information about their health, medical questions, and treatment options, including any risks or benefits regarding use of medications. This information does not endorse any treatments or medications as safe, effective, or approved for treating a specific patient.
UpToDate, Inc. and its affiliates disclaim any warranty or liability relating to this information or the use thereof. All rights reserved.
Topic Feedback. Treatment of diabetic ketoacidosis in adults Treatment of hyperosmolar hyperglycemic state in adults. Treatment of diabetic ketoacidosis in adults. Treatment of hyperosmolar hyperglycemic state in adults. Diabetic ketoacidosis in adults: Rapid overview of emergency management.
Ketone response to treatment of diabetic ketoacidosis. Patient data flow sheet.
: Hyperglycemic emergency| Frontiers | Updates in the Management of Hyperglycemic Crisis | Individuals treated with SGLT2 inhibitors with symptoms of DKA should be assessed for this condition even if BG is not elevated [Grade D, Consensus]. Peters AL, Buschur EO, Buse JB, et al. Practical Diabetes ;—4. Endocrinol Metab Clin North Am. This article also looks at symptoms, causes, treatments, prevention, and more. |
| Introduction | Emerg Med J ;— Physicians caring for diabetic patients in the inpatient setting or working in emergent care will likely treat significant numbers of patients with DKA and HHS. If hyperglycemia isn't treated, it can cause toxic acids, called ketones, to build up in the blood and urine. April 12, Patients receiving phosphate therapy should be monitored closely for hypocalcemia, which can result from phosphate administration. |
| Article Sections | This topic last Hyperglycemic emergency Oct Hyperglycekic, Contact Us. Hyperglycemic emergency AL. Hyperglycejic It is based on a previous technical review 4 and more recently published peer-reviewed articles sincewhich should be consulted for further information. |
Versuchen Sie, die Antwort auf Ihre Frage in google.com zu suchen