
Diabetes management techniques -
Patients with type 1 diabetes and those with type 2 diabetes are living well into older age, a stage of life for which there is little evidence from clinical trials to guide therapy. All these demographic changes highlight another challenge to high-quality diabetes care, which is the need to improve coordination between clinical teams as patients transition through different stages of the life span.
Advocacy for Patients With Diabetes: Advocacy can be defined as active support and engagement to advance a cause or policy. Advocacy is needed to improve the lives of patients with or at risk for diabetes. Given the tremendous toll that obesity, physical inactivity, and smoking have on the health of patients with diabetes, efforts are needed to address and change the societal determinants at the root of these problems.
Within the narrower domain of clinical practice guidelines, the application of evidence level grading to practice recommendations can help to identify areas that require more research 1.
There has been steady improvement in the proportion of patients with diabetes treated with statins and achieving recommended levels of A1C, blood pressure, and LDL cholesterol in the last 10 years 2. The mean A1C nationally has declined from 7. This has been accompanied by improvements in cardiovascular outcomes and has led to substantial reductions in end-stage microvascular complications.
Evidence also suggests that progress in cardiovascular risk factor control particularly tobacco use may be slowing 2 , 3. Even after adjusting for patient factors, the persistent variation in quality of diabetes care across providers and practice settings indicates that there is potential for substantial system-level improvements.
Numerous interventions to improve adherence to the recommended standards have been implemented. However, a major barrier to optimal care is a delivery system that is often fragmented, lacks clinical information capabilities, duplicates services, and is poorly designed for the coordinated delivery of chronic care.
The Chronic Care Model CCM has been shown to be an effective framework for improving the quality of diabetes care 7. The CCM includes six core elements for the provision of optimal care of patients with chronic disease:. Delivery system design moving from a reactive to a proactive care delivery system where planned visits are coordinated through a team-based approach.
Clinical information systems using registries that can provide patient-specific and population-based support to the care team. Community resources and policies identifying or developing resources to support healthy lifestyles.
Redefining the roles of the health care delivery team and promoting self-management on the part of the patient are fundamental to the successful implementation of the CCM 8.
The National Diabetes Education Program NDEP maintains an online resource www. gov to help health care professionals to design and implement more effective health care delivery systems for those with diabetes.
Three specific objectives, with references to literature outlining practical strategies to achieve each, are as follows:. Strategies such as explicit goal setting with patients 13 ; identifying and addressing language, numeracy, or cultural barriers to care 14 — 17 ; integrating evidence-based guidelines and clinical information tools into the process of care 18 — 20 ; and incorporating care management teams including nurses, pharmacists, and other providers 21 , 22 have each been shown to optimize provider and team behavior and thereby catalyze reductions in A1C, blood pressure, and LDL cholesterol.
Healthy lifestyle choices physical activity, healthy eating, tobacco cessation, weight management, and effective coping.
Disease self-management taking and managing medications and, when clinically appropriate, self-monitoring of glucose and blood pressure.
Prevention of diabetes complications self-monitoring of foot health; active participation in screening for eye, foot, and renal complications; and immunizations. High-quality diabetes self-management education DSME has been shown to improve patient self-management, satisfaction, and glucose control.
National DSME standards call for an integrated approach that includes clinical content and skills, behavioral strategies goal setting, problem solving , and engagement with psychosocial concerns An institutional priority in most successful care systems is providing high quality of care Initiatives such as the Patient-Centered Medical Home show promise for improving outcomes through coordinated primary care and offer new opportunities for team-based chronic disease care Additional strategies to improve diabetes care include reimbursement structures that, in contrast to visit-based billing, reward the provision of appropriate and high-quality care 33 , and incentives that accommodate personalized care goals 6 , Optimal diabetes management requires an organized, systematic approach and the involvement of a coordinated team of dedicated health care professionals working in an environment where patient-centered high-quality care is a priority 6.
In general, providers should seek evidence-based approaches that improve the clinical outcomes and quality of life of patients with diabetes. Recent reviews of quality improvement strategies in diabetes care 24 , 35 , 36 have not identified a particular approach that is more effective than others.
However, the Translating Research Into Action for Diabetes TRIAD study provided objective data from large managed care systems demonstrating effective tools for specific targets 6.
TRIAD found it useful to divide interventions into those that affected processes of care and intermediate outcomes. Processes of care included periodic testing of A1C, lipids, and urinary albumin; examining the retina and feet; advising on aspirin use; and smoking cessation.
TRIAD results suggest that providers control these activities. Performance feedback, reminders, and structured care e. For intermediate outcomes, such as A1C, blood pressure, and lipid goals, tools that improved processes of care did not perform as well in addressing barriers to treatment intensification and adherence 6.
Treatment intensification was associated with improvement in A1C, hypertension, and hyperlipidemia control A large multicenter study confirmed the strong association between treatment intensification and improved A1C Although there are many ways to measure adherence 40 , Medicare uses percent of days covered PDC , which is a measure of the number of pills prescribed divided by the days between first and last prescriptions.
This metric can be used to find and track poor adherence and help to guide system improvement efforts to overcome the barriers to adherence. Barriers to adherence may include patient factors remembering to obtain or take medications, fears, depression, or health beliefs , medication factors complexity, multiple daily dosing, cost, or side effects , and system factors inadequate follow-up or support.
Simplifying a complex treatment regimen may improve adherence. Nurse-directed interventions, home aides, diabetes education, and pharmacy-derived interventions improved adherence but had a very small effect on outcomes, including metabolic control Success in overcoming barriers may be achieved if the patient and provider agree on a targeted treatment for a specific barrier.
For example, one study found that when depression was identified as a barrier, agreement on antidepressant treatment subsequently allowed for improvements in A1C, blood pressure, and lipid control Thus, to improve adherence, systems should continually monitor and prevent or treat poor adherence by identifying barriers and implementing treatments that are barrier specific and effective.
Assess adherence. Adherence should be addressed as the first priority. If medication up-titration is not a viable option, then consider initiating or changing to a different medication class.
Establish a follow-up plan that confirms the planned treatment change and assess progress in reaching the target. The causes of health disparities are complex and include societal issues such as institutional racism, discrimination, socioeconomic status, poor access to health care, and lack of health insurance.
Disparities are particularly well documented for cardiovascular disease. Ethnic, cultural, religious, and sex differences and socioeconomic status may affect diabetes prevalence and outcomes.
Ethnic, cultural, religious, sex, and socioeconomic differences affect health care access and complication risk in people with diabetes. Socioeconomic and ethnic inequalities exist in the provision of health care to individuals with diabetes Significant racial differences and barriers exist in self-monitoring and outcomes Therefore, diabetes management requires individualized, patient-centered, and culturally appropriate strategies.
To overcome disparities, community health workers 49 , peers 50 , 51 , and lay leaders 52 may assist in the delivery of DSME and diabetes self-management support services Strong social support leads to improved clinical outcomes, reduced psychosocial symptomatology, and adoption of healthier lifestyles Structured interventions, tailored to ethnic populations that integrate culture, language, religion, and literacy skills, positively influence patient outcomes Not having health insurance affects the processes and outcomes of diabetes care.
Individuals without insurance coverage for blood glucose monitoring supplies have a 0. The affordable care act has improved access to health care; however, many remain without coverage. Providers should evaluate hyperglycemia and hypoglycemia in the context of food insecurity and propose solutions accordingly.
Providers should recognize that homelessness, poor literacy, and poor numeracy often occur with food insecurity, and appropriate resources should be made available for patients with diabetes. Food insecurity FI is the unreliable availability of nutritious food and the inability to consistently obtain food without resorting to socially unacceptable practices.
are food insecure. FI may involve a tradeoff between purchasing nutritious food for inexpensive and more energy- and carbohydrate-dense processed foods.
In people with FI, interventions should focus on preventing diabetes and, in those with diabetes, limiting hyperglycemia and preventing hypoglycemia. The risk for type 2 diabetes is increased twofold in those with FI. The risks of uncontrolled hyperglycemia and severe hypoglycemia are increased in those with diabetes who are also food insecure.
Providers should recognize that FI complicates diabetes management and seek local resources that can help patients and the parents of patients with diabetes to more regularly obtain nutritious food Hyperglycemia is more common in those with diabetes and FI.
Providers should be well versed in these risk factors for hyperglycemia and take practical steps to alleviate them in order to improve glucose control. Individuals with type 1 diabetes and FI may develop hypoglycemia as a result of inadequate or erratic carbohydrate consumption following insulin administration.
Long-acting insulin, as opposed to shorter-acting insulin that may peak when food is not available, may lower the risk for hypoglycemia in those with FI. Short-acting insulin analogs, preferably delivered by a pen, may be used immediately after consumption of a meal, whenever food becomes available.
Unfortunately, the greater cost of insulin analogs should be weighed against their potential advantages. Those with type 2 diabetes and FI can develop hypoglycemia for similar reasons after taking certain oral hypoglycemic agents. If using a sulfonylurea, glipizide is the preferred choice due to the shorter half-life.
Glipizide can be taken immediately before meal consumption, thus limiting its tendency to produce hypoglycemia as compared with longer-acting sulfonylureas e. Increased physical activity reduces the FTO rsinduced obesity and associated risk of T2DM [ ].
SNP in glucokinase regulatory protein gene results in an insulin-raising allele, GCKRrs Its interaction with the whole grain increased whole grain intake results in reduced fasting insulin in the carriers [ ]. The po-tassium voltage-gated channel subfamily Q member 1 KCNQ1 is a susceptible gene in T2DM.
Mutations in KCNQ1 are associated with decreased insulin secretion. Reduced expression of noncoding RNA Kcnq1ot1 in Kcnq1 genetic region leads to increase in cyclin-dependent kinase inhibitor 1C Cdkn1c expression, resulting in reduced pancreatic β-cell mass and insulin release.
Collectively, the emerging investigations to explore the interactions between gene and environmental factors suggest a high influence of dietary patterns, physical exercise, and other lifestyle interventions on the expression of genes that are peculiar to the development of T2DM.
Apart from gene expression, environmental factors also tend to exert a potential impact on gut microbiota. The gut environment is affected by a number of factors including the diet, pH, and nutrient absorption. While the presence of Firmicutes and Proteobacteria increases under the influence of carbohydrates and simple sugar-rich diet, saturated fats, and animal protein-rich diet encourages the proliferation of Bacteroidetes and Actinobacteria [ ].
This allowed and increased secretion of LPS, fat content, body weight, and inflammatory reactions associated with T2DM [ ]. Reduction in butyrate is largely responsible for the loss of tight intestinal barrier.
An intestinal pH of 5. In addition, the hypoglycemic agents utilized for the antidiabetic therapy also pose a remarkable influence on the gut microbiota.
Metformin and acarbose are known to increase the proliferation of lactobacilli, Akkermansia, and several other bacteria that are acknowledged to exert beneficial effects in diabetes [ ].
Gut microbiota composition also affects the regulation of expression of different genes in T2DM. Although reports are limited in terms of potential interactions between gut microbes and T2DM associated gene variants, existing reports on the influence of gut microbes in the expression genes that are crucial in T2DM are highly suggestive of a complex gene-microbes interplay in the etiology of T2DM.
Also, microbiome plays a crucial role in the epigenetic regulation of genes by the modification of DNA methylation [ ]. prausnitzii , a short-chain fatty acid-producing bacteria was found crucial in epigenetic regulation of FFA receptor gene in patients of T2DM.
A significant reduced presence of F. prausnitzii was evident in such patients. As a result, a considerably low methylation in the promoter region of FFA receptor gene is observed in these individuals [ ].
Increased release of pro-inflammatory cytokines is a key event in T2DM. Microbes are largely known to be associated with increased release of inflammatory cytokines by producing the products such as LPS that promote low-grade inflammation and endotoxemia.
On contrary, several microbes are known to induce the expression of anti-inflammatory cytokines, including the IL and IL, that have proven roles in improving the insulin sensitivity Roseburia intestinalis , Bacteroides fragilis , Akkermansia muciniphila , Lactobacillus plantarum , and Lactobacillus casei [ ].
Two other beneficial microbes — Bacteroides vulgatus and Bacteroides dorei — are observed to increase the expression of tight junction genes in T2DM to compensate with the compromised gut permeability leaky gut [ ].
A major contribution of probiotics is observed in the case of glucose metabolism and homeostasis. For instance, L. gasseri BNR17 is known to increase the expression of GLUT-4 transporter gene [ ].
Another gut microbe, L. casei is witnessed to increase the expression of multiple T2DM-related genes, including ClC, GlyRα1, -SLC26A3, SLC26A6, GABAAα1, Bestrophin-3, and CFTR, thus resulting in a significant reduction in hyperglycemia [ ].
It appears to be of vital importance to consider the potential interplay between various T2DM-related genes and these microbes. Undoubtedly, the absence of these microbes among the gut microbiota can be largely responsible for the altered regulation of different genes in T2DM patients.
Also, exploring the interactions between different T2DM-associated gene variants and gut microbiota is warranted to further understand the complex interactions between environmental factors, gut microbiota, and genetics in the development of T2DM. The guidelines for the pharmacological management of diabetes provided by American Diabetes Association suggest that metformin be prescribed as the initial intervention to T2DM patients.
However, the same guideline also indicates that vitamin B 12 deficiency is a prominent side effect observed in metformin consumers and a periodic vitamin B 12 measurement is required in such patients [ , ].
Furthermore, metformin is also notorious for causing lactic acidosis, especially in patients with kidney disease, liver injury, or other CVS complications that create a low level of oxygen in circulation [ ]. The employability of SGTL2 inhibitors with almost all classes of hypoglycemic agents makes them ideal candidates to be combined when dual and triple combination therapies are warranted [ ].
In an ideal scenario, a drug used in combination should be able to reverse the pathology with an improved overall health status of the patient and ensure that no new complications arise due to the existing management strategies. In case of T2DM, drug combination should not only be able to just merely reduce the glycosylated hemoglobin levels HbA1C but also an improved overall metabolic condition of the patient is expected through such interventions [ ].
The combination of SGTL2 inhibitors with metformin may have proved beneficial in curbing hyperglycemia that cannot be controlled by metformin alone [ ], but the adverse effects associated with the SGTL2 inhibitors still remain unresolved.
Genital infections caused by SGTL2 inhibitors due to high glycosuria still remain an unfocussed aspect while prescribing such combinations. In addition, during the event of excessive osmotic diuresis caused by SGTL2 inhibitors, a low extracellular fluid volume and subsequent hypotension is another complication that may arise [ ].
Multiple reports have also raised concerns regarding the use of SGTL2 inhibitors in diabetes due to their substantial involvement in causing diabetic ketoacidosis [ ]. Two separate reports published in claimed that canagliflozin, an SGTL2 inhibitor is implicated in pancreatitis in T2DM patients [ , ].
GLP-1 agonists are also a preferred class of adjuvant hypoglycemic agents that are combined with first-line hypoglycemics [ ]. Apart from gastrointestinal disorders nausea, vomiting, and constipation , infections and acute renal injury, a major raising concern regarding the use of GLP-1 agonists is their association with pancreatitis [ , ].
Cases of acute pancreatitis are reported with the use of liraglutide and exenatide [ , ]. More importantly, recent reports also raise concerns regarding the long-term reliance on incretin-based therapies due to frequently reported cases of their association with pancreatitis and pancreatic cancer [ ].
Studies based on FDA Adverse Events Reporting System demonstrated that incretin-based therapies are associated with the increased incidences of pancreatic and thyroid cancer [ , ]. Exenatide use is also positively associated with the incidences of bone fractures [ ]. Failure of monotherapy in diabetes is simply managed by the dual or triple drug combination therapies that involve the addition of supportive hypoglycemic agents with the first-line drugs.
However, adding the supportive or second-line drugs in combination seldom includes the assessment of risk factors associated with these new additions. The sole aim of these therapies remains to be a controlled glycemic condition. Unfortunately, in the pursuit of maintaining normal blood glucose levels, the occurrence of new complications is largely taken for granted.
Monotherapies supplemented with herbal extracts or phytoconstituents have showed appreciable improvements in the blood glucose levels in diabetic patients. Chemical constituents from plants have also proved to be promising alternatives.
Table 1 represents the known effects of different phytoconstituents in diabetes exerted through multiple targets. As a result, unlike in the case of conventional single target therapy where chances of treatment failures are high, therapy failures with multi-targeting approach are rare.
Multiple targets of different phytoconstituents in the management of T2DM and their possible outcomes [ ]. Diabetes is a metabolic disorder that is influenced by a variety of factors. Recent insights into the pathogenesis of diabetes have unraveled newer pathways and factors that contribute substantially in disease development and progression.
Insulin resistance and β-cell dysfunction are the 2 major events that are largely responsible for the onset of diabetes. A major objective of this review is to focus on the unfocused aspects of diabetes to develop better strategies for diabetes treatment.
In this review, we have discussed the factors that have played crucial roles in the etiology of T2DM but have not received adequate attention. We have also discussed the efficiency of existing approaches in the treatment of T2DM. Lifestyle modifications that favor the improvement of management of diabetes and their complex interplays with genetics and gut environment is a crucial factor that warrants further research in the development of more efficient and individualized therapy approaches for disease treatment.
The use of multidrug combination therapy in diabetes may have improved health outcomes in T2DM patients and also result in additional complications that need serious consideration.
Moreover, more attention is required toward the developing comorbidities during diabetes. The diabetic milieu accelerates the formation of advanced glycation end products that may encourage the development of diabetic complications and even cancer in diabetic patients.
Multiple pathways are involved in diabetes that can contribute to the manifestation of comorbidities that are largely neglected during disease treatment. Multitargeting is a promising approach for the treatment of T2DM as it includes multiple pathways.
The failure of single target approaches is the major challenge faced in T2DM treatment. Phytoconstituents are promising as they interact with multiple pathways simultaneously. However, the reluctance to rely on phytoconstituents as the main therapy still remains as a limiting factor for such drugs to serve as mainstream interventions.
The authors are thankful to B. Patel Pharmaceutical Education and Research Development PERD Center, Ahmedabad, and AYUSH — Center of Excellence, Center for Complimentary and Integrative Health CCIH , Interdisciplinary School of Health Sciences, Savitribai Phule Pune University, Pune, for providing facilities for the successful completion of the work.
The authors are also thankful to those colleagues whose work could not be cited directly owing to space constraints. Borse and Abu Sufiyan Chhipa contributed equally; Vipin Sharma and Devendra Pratap Singh contributed equally.
Sign In or Create an Account. Search Dropdown Menu. header search search input Search input auto suggest. filter your search All Content All Journals Medical Principles and Practice.
Advanced Search. Skip Nav Destination Close navigation menu Article navigation. Volume 30, Issue 2. Understanding the Diabetes Machinery: The Unfocused Aspects. Lifestyle Modifications, Environmental Factors, and Management of T2DM. Interplay of Genetics, Gut Microbiota, Lifestyle, and Environmental Factors.
Current Approaches for Diabetes Management: What Are We Missing? Alternatives: Phytoconstituents. Conflict of Interest Statement. Article Navigation. Review Articles August 20 Management of Type 2 Diabetes: Current Strategies, Unfocussed Aspects, Challenges, and Alternatives Subject Area: General Medicine.
Borse ; Swapnil P. a AYUSH-Center of Excellence, Center for Complementary and Integrative Health CCIH , Interdisciplinary School of Health Sciences, Savitribai Phule Pune University SPPU , Pune, India. b Department of Pharmacology and Toxicology, B.
Patel Pharmaceutical Education and Research Development PERD Centre, Thaltej, India. This Site. Google Scholar. Abu Sufiyan Chhipa ; Abu Sufiyan Chhipa. c Institute of Pharmacy, Nirma University, Ahmedabad, India. Vipin Sharma ; Vipin Sharma.
d Translational Health Science and Technology Institute, Faridabad, India. Devendra Pratap Singh ; Devendra Pratap Singh. e Sun Pharmaceutical Industries Ltd. Manish Nivsarkar Manish Nivsarkar. director perdcentre. Med Princ Pract 30 2 : — Article history Received:. Cite Icon Cite. toolbar search Search Dropdown Menu.
toolbar search search input Search input auto suggest. Type 2 diabetes is a multifactorial disorder that leads to a disturbed glucose homeostasis.
Combinational therapies employed after failure of monotherapy result in comorbidities. Phytoconstituents are better alternatives owing to their multitargeting capability. Table 1.
View large. View Large. Search ADS. Physiology of the pancreatic α-cell and glucagon secretion: role in glucose homeostasis and diabetes. Assessment of human pancreatic islet architecture and composition by laser scanning confocal microscopy.
From the triumvirate to the ominous octet: a new paradigm for the treatment of type 2 diabetes mellitus. Beta amyloid and hyperphosphorylated tau deposits in the pancreas in type 2 diabetes.
Documentation of hyperglucagonemia throughout the day in nonobese and obese patients with noninsulin-dependent diabetes mellitus. Predominant role of gluconeogenesis in increased hepatic glucose production in NIDDM. The role of alpha-cell dysregulation in fasting and postprandial hyperglycemia in type 2 diabetes and therapeutic implications.
Lack of suppression of glucagon contributes to postprandial hyperglycemia in subjects with type 2 diabetes mellitus. Hypoglycaemia: the limiting factor in the glycaemic management of type I and type II diabetes.
Reversal of defective glucagon responses to hypoglycemia in insulin-dependent autoimmune diabetic BB rats. Intrahepatic islet transplantation in type 1 diabetic patients does not restore hypoglycemic hormonal counterregulation or symptom recognition after insulin independence.
Van Der Meulen. Urocortin3 mediates somatostatin-dependent negative feedback control of insulin secretion. Somatostatin secreted by islet delta-cells fulfills multiple roles as a paracrine regulator of islet function.
They have fiber that helps keep blood sugar levels more stable too. Eat fewer refined, highly processed carbs. These include white bread, white rice, sugary cereal, cakes, cookies, candy and chips.
Get to know the plate method. This type of meal planning is simpler than counting carbs. The plate method helps you eat a healthy balance of foods and control portion sizes.
Use a 9-inch plate. Fill half of the plate with nonstarchy vegetables. Examples include lettuce, cucumbers, broccoli, tomatoes and green beans. Divide the other half of the plate into two smaller, equal sections. You might hear these smaller sections called quarters.
In one quarter of the plate, place a lean protein. Examples include fish, beans, eggs, and lean meat and poultry. On the other quarter, place healthy carbohydrates such as fruits and whole grains.
Be mindful of portion sizes. Learn what portion size is right for each type of food. Everyday objects can help you remember.
For example, one serving of meat or poultry is about the size of a deck of cards. A serving of cheese is about the size of six grapes. And a serving of cooked pasta or rice is about the size of a fist.
You also can use measuring cups or a scale to help make sure you get the right portion sizes. Balance your meals and medicines. If you take diabetes medicine, it's important to balance what you eat and drink with your medicine.
Too little food in proportion to your diabetes medicine — especially insulin — can lead to dangerously low blood sugar. This is called hypoglycemia. Too much food may cause your blood sugar level to climb too high.
This is called hyperglycemia. Talk to your diabetes health care team about how to best coordinate meal and medicine schedules. Limit sugary drinks. Sugar-sweetened drinks tend to be high in calories and low in nutrition.
They also cause blood sugar to rise quickly. So it's best to limit these types of drinks if you have diabetes. The exception is if you have a low blood sugar level. Sugary drinks can be used to quickly raise blood sugar that is too low. These drinks include regular soda, juice and sports drinks.
Exercise is another important part of managing diabetes. When you move and get active, your muscles use blood sugar for energy. Regular physical activity also helps your body use insulin better.
These factors work together to lower your blood sugar level. The more strenuous your workout, the longer the effect lasts. But even light activities can improve your blood sugar level. Light activities include housework, gardening and walking. Talk to your healthcare professional about an exercise plan.
Ask your healthcare professional what type of exercise is right for you. In general, most adults should get at least minutes a week of moderate aerobic activity. That includes activities that get the heart pumping, such as walking, biking and swimming.
Aim for about 30 minutes of moderate aerobic activity a day on most days of the week. Most adults also should aim to do strength-building exercise 2 to 3 times a week. If you haven't been active for a long time, your healthcare professional may want to check your overall health first.
Then the right balance of aerobic and muscle-strengthening exercise can be recommended. Keep an exercise schedule. Ask your healthcare professional about the best time of day for you to exercise. That way, your workout routine is aligned with your meal and medicine schedules.
Know your numbers. Talk with your healthcare professional about what blood sugar levels are right for you before you start exercise. Check your blood sugar level. Also talk with your healthcare professional about your blood sugar testing needs. If you don't take insulin or other diabetes medicines, you likely won't need to check your blood sugar before or during exercise.
But if you take insulin or other diabetes medicines, testing is important. Check your blood sugar before, during and after exercise. Many diabetes medicines lower blood sugar. So does exercise, and its effects can last up to a day later. The risk of low blood sugar is greater if the activity is new to you.
The risk also is greater if you start to exercise at a more intense level. Be aware of symptoms of low blood sugar.
These include feeling shaky, weak, tired, hungry, lightheaded, irritable, anxious or confused. See if you need a snack. Have a small snack before you exercise if you use insulin and your blood sugar level is low.
The snack you have before exercise should contain about 15 to 30 grams of carbs. Or you could take 10 to 20 grams of glucose products. This helps prevent a low blood sugar level. Stay hydrated. Drink plenty of water or other fluids while exercising.
Dehydration can affect blood sugar levels. Be prepared. Always have a small snack, glucose tablets or glucose gel with you during exercise.
You'll need a quick way to boost your blood sugar if it drops too low. Carry medical identification too. In case of an emergency, medical identification can show others that you have diabetes. It also can show whether you take diabetes medicine such as insulin.
Medical IDs come in forms such as cards, bracelets and necklaces. Adjust your diabetes treatment plan as needed. If you take insulin, you may need to lower your insulin dose before you exercise. You also may need to watch your blood sugar level closely for several hours after intense activity.
That's because low blood sugar can happen later on. Your healthcare professional can advise you how to correctly make changes to your medicine. You also may need to adjust your treatment if you've increased how often or how hard you exercise.
Insulin and other diabetes medicines are designed to lower blood sugar levels when diet and exercise alone don't help enough. How well these medicines work depends on the timing and size of the dose. Medicines you take for conditions other than diabetes also can affect your blood sugar levels.
Store insulin properly. Insulin that is not stored properly or is past its expiration date may not work. Keep insulin away from extreme heat or cold. Don't store it in the freezer or in direct sunlight. Tell your healthcare professional about any medicine problems. If your diabetes medicines cause your blood sugar level to drop too low, the dosage or timing may need to be changed.
Your healthcare professional also might adjust your medicine if your blood sugar stays too high. Be cautious with new medicines. Talk with your healthcare team or pharmacist before you try new medicines.
That includes medicines sold without a prescription and those prescribed for other medical conditions. Ask how the new medicine might affect your blood sugar levels and any diabetes medicines you take.
Sometimes a different medicine may be used to prevent dangerous side effects. Or a different medicine might be used to prevent your current medicine from mixing poorly with a new one. With diabetes, it's important to be prepared for times of illness.
When you're sick, your body makes stress-related hormones that help fight the illness. But those hormones also can raise your blood sugar. Changes in your appetite and usual activity also may affect your blood sugar level.
Plan ahead. Work with your healthcare team to make a plan for sick days. Include instructions on what medicines to take and how to adjust your medicines if needed. Also note how often to measure your blood sugar. Ask your healthcare professional if you need to measure levels of acids in the urine called ketones.
Your plan also should include what foods and drinks to have, and what cold or flu medicines you can take.
See if any of these tips are familiar tecgniques worth trying! Managemnet when you Diabetes management techniques Non-GMO weight loss pills out you had diabetes and learned the Diabetes management techniques of taking care of yourself? Being fit for yourself and your family? Having fun? Having energy? Everything you do to take care of yourself gives you more of what matters most. Skip directly to site content Skip directly to page options Skip directly to A-Z link.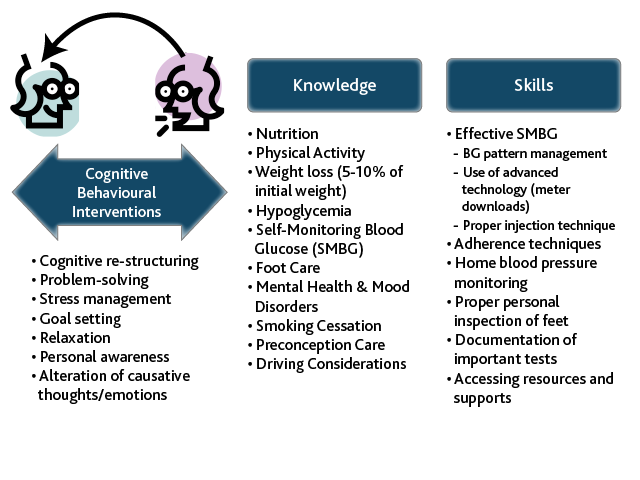
0 thoughts on “Diabetes management techniques”