
Video
Role of insulin in carbohydrate metabolism and glycogen storage diseaseCarbohydrate metabolism and insulin sensitivity -
Journal of the American Association for Laboratory Animal Science 47 8 — reduced glucose effectiveness in glucose-intolerant mice. American Journal of Physiology E — E American Journal of Physiology R — R Fertility Research and Practice 6 5.
Diabetologia 61 — Al-Share QY , DeAngelis AM , Lester SG , Bowman TA , Ramakrishnan SK , Abdallah SL , Russo L , Patel PR , Kaw MK , Raphael CK , et al. Diabetes 64 — American Diabetes Association Diagnosis and classification of diabetes mellitus.
Diabetes Care 37 Supplement 1 S81 — S Endocrinology — Diabetes 55 — Disease Models and Mechanisms 3 — Nature Metabolism 4 — Diabetes 54 — Diabetes, Metabolic Syndrome and Obesity 13 — Diabetes 57 — Berglund ED , Vianna CR , Donato J Jr , Kim MH , Chuang JC , Lee CE , Lauzon DA , Lin P , Brule LJ , Scott MM , et al.
Journal of Clinical Investigation — Diabetes Care 19 — Journal of Clinical Investigation 93 — Molecular Metabolism 53 Bruin JE , Saber N , Braun N , Fox JK , Mojibian M , Asadi A , Drohan C , O'Dwyer S , Rosman-Balzer DS , Swiss VA , et al. Stem Cell Reports 4 — American Journal of Physiology E53 — E Cell Metabolism 17 — Carey M , Lontchi-Yimagou E , Mitchell W , Reda S , Zhang K , Kehlenbrink S , Koppaka S , Maginley SR , Aleksic S , Bhansali S , et al.
Diabetes 69 — Molecular Metabolism 42 Castellani LN , Pereira S , Kowalchuk C , Asgariroozbehani R , Singh R , Wu S , Hamel L , Alganem K , Ryan WG , Zhang X , et al. Molecular Psychiatry 27 — American Journal of Physiology E7 — E Laboratory Animals 43 65 — Journal of Neurochemistry 33 — Diabetes 32 35 — Della Torre S , Mitro N , Fontana R , Gomaraschi M , Favari E , Recordati C , Lolli F , Quagliarini F , Meda C , Ohlsson C , et al.
Cell Reports 15 — Drucker DJ Never waste a good crisis: confronting reproducibility in translational research. Cell Metabolism 24 — Nature Communications 11 Erener S , Ellis CE , Ramzy A , Glavas MM , O'Dwyer S , Pereira S , Wang T , Pang J , Bruin JE , Riedel MJ , et al. Cell Reports 2 Evers SS , Kim KS , Bozadjieva N , Lewis AG , Farris D , Sorensen MJ , Kim Y , Whitesall SE , Kennedy RT , Michele DE , et al.
Molecular Metabolism 32 — Metabolism: Clinical and Experimental 63 — Ferreira DS , Amaral FG , Mesquita CC , Barbosa AP , Lellis-Santos C , Turati AO , Santos LR , Sollon CS , Gomes PR , Faria JA , et al. PLoS One 7 e Journal of Pharmacological and Toxicological Methods 57 — Nutrition and Metabolism 13 Georgiou P , Zanos P , Mou TM , An X , Gerhard DM , Dryanovski DI , Potter LE , Highland JN , Jenne CE , Stewart BW , et al.
Nature Neuroscience 25 — Trends in Endocrinology and Metabolism 33 — Journal of Lipid Research 46 — Henderson DC , Cagliero E , Copeland PM , Borba CP , Evins AE , Hayden D , Weber MT , Anderson EJ , Allison DB , Daley TB , et al. Archives of General Psychiatry 62 19 — Endocrine Reviews 34 — Mammalian Genome 25 — Diabetes 59 — NMR in Biomedicine 33 e Journal of Psychiatry and Neuroscience 37 — Diabetologia 60 — Obesity 20 — Diabetic Medicine 38 e Diabetes, Obesity and Metabolism 24 — Journal of Psychiatry and Neuroscience 42 — Kumashiro N , Beddow SA , Vatner DF , Majumdar SK , Cantley JL , Guebre-Egziabher F , Fat I , Guigni B , Jurczak MJ , Birkenfeld AL , et al.
Diabetes 62 — Journal of Endocrinology — Science — Journal of Clinical Investigation 98 — Scientific Reports 9 npj Digital Medicine 6 Diabetes 58 — Cell Metabolism 25 — Meneses MJ , Patarrão RS , Pinheiro T , Coelho I , Carriço N , Marques AC , Romão A , Nabais J , Fortunato E , Raposo JF , et al.
European Journal of Clinical Investigation 53 e Journal of the American Association for Laboratory Animal Science 56 — Journal of the American Association for Laboratory Animal Science 57 44 — Diabetes 60 — Nahle A , Joseph YD , Pereira S , Mori Y , Poon F , Ghadieh HE , Ivovic A , Desai T , Ghanem SS , Asalla S , et al.
International Journal of Molecular Sciences 22 Annual Review of Physiology 85 — Biological Psychiatry 86 — Magnetic Resonance in Medicine 62 — Hormone and Metabolic Research 13 — In Insulin Resistance and Cancer: Epidemiology, Cellular and Molecular Mechanisms and Clinical Implications.
Fantus IG Ed. New York, NY, USA : Springer , pp. Diabetes 57 56 — Pereira S , Yu WQ , Frigolet ME , Beaudry JL , Shpilberg Y , Park E , Dirlea C , Nyomba BL , Riddell MC , Fantus IG , et al.
Journal of Endocrinology 31 — Pereira S , Park E , Mori Y , Haber CA , Han P , Uchida T , Stavar L , Oprescu AI , Koulajian K , Ivovic A , et al. American Journal of Physiology E34 — E Pereira S , O'Dwyer SM , Webber TD , Baker RK , So V , Ellis CE , Yoon JS , Mojibian M , Glavas MM , Karunakaran S , et al.
Pereira S , Cline DL , Chan M , Chai K , Yoon JS , O'Dwyer SM , Ellis CE , Glavas MM , Webber TD , Baker RK , et al. Scientific Reports 11 Perry RJ , Camporez JG , Kursawe R , Titchenell PM , Zhang D , Perry CJ , Jurczak MJ , Abudukadier A , Han MS , Zhang XM , et al.
Cell — Journal of Diabetes Investigation 7 Supplement 1 13 — Molecular Metabolism 77 Sakaguchi M , Fujisaka S , Cai W , Winnay JN , Konishi M , O'Neill BT , Li M , García-Martín R , Takahashi H , Hu J , et al.
Schertzer JD , Tamrakar AK , Magalhães JG , Pereira S , Bilan PJ , Fullerton MD , Liu Z , Steinberg GR , Giacca A , Philpott DJ , et al.
Nature 59 — Small L , Ehrlich A , Iversen J , Ashcroft SP , Trošt K , Moritz T , Hartmann B , Holst JJ , Treebak JT , Zierath JR , et al. Molecular Metabolism 57 Sorge RE , Martin LJ , Isbester KA , Sotocinal SG , Rosen S , Tuttle AH , Wieskopf JS , Acland EL , Dokova A , Kadoura B , et al.
Nature Methods 11 — PNAS — Nature Reviews. Endocrinology 15 75 — Hormone and Metabolic Research 33 89 — Metabolism: Clinical and Experimental Scientific Reports 6 Metabolism: Clinical and Experimental 47 — Diabetologia 63 — Journal of the American Association for Laboratory Animal Science 50 — Effects on intracellular calcium pools.
Journal of Biological Chemistry — Nature Metabolism 3 — Willingham E The fraught quest to account for sex in biology research. Nature — American Journal of Physiology-Endocrinology and Metabolism E — E Diabetes 68 — PNAS e Nature Communications 7 Journal of Endocrinology is committed to supporting researchers in demonstrating the impact of their articles published in the journal.
HOMA-IR index was registered 1. The WC was lower by 1. Conclusion: Insufficient compensation of diabetes is noted in patients with LADA1 and LADA2 without differences in intergroup comparison, however the degree of insulin resistance and abdominal obesity as main components of metabolic syndrome prevalence in patients with LADA2 which indicates the higher cardiovascular risk in this category of patients.
Istanbul, Turkey 13 May - 16 May Endocrine Abstracts ISSN print ISSN online © Bioscientifica Privacy policy Cookie settings. Bioscientifica Abstracts is the gateway to a series of products that provide a permanent, citable record of abstracts for biomedical and life science conferences.
Searchable abstracts of presentations at key conferences in endocrinology. ISSN print ISSN online. Endocrine Abstracts. Prev Next. Obese individuals with and without type 2 diabetes show different gut microbial functional capacity and composition.
Cell Host Microbe 26 , — Article CAS PubMed PubMed Central Google Scholar. Wu, H. The gut microbiota in prediabetes and diabetes: a population-based cross-sectional study. Cell Metab. Article CAS PubMed Google Scholar. Gou, W. Interpretable machine learning framework reveals robust gut microbiome features associated with type 2 diabetes.
Diabetes Care 44 , — McNeil, N. The contribution of the large intestine to energy supplies in man. Forslund, K.
Disentangling type 2 diabetes and metformin treatment signatures in the human gut microbiota. Pedersen, H. Human gut microbes impact host serum metabolome and insulin sensitivity. Yamada, C. Optimal reference interval for homeostasis model assessment of insulin resistance in a Japanese population.
Diabetes Investig. Kanamori-Katayama, M. Unamplified cap analysis of gene expression on a single-molecule sequencer. Genome Res. Peng, H. Feature selection based on mutual information criteria of max-dependency, max-relevance, and min-redundancy.
IEEE Trans. Pattern Anal. Article PubMed Google Scholar. den Besten, G. Gut-derived short-chain fatty acids are vividly assimilated into host carbohydrates and lipids. Liver Physiol. Article Google Scholar. Zierer, J. The fecal metabolome as a functional readout of the gut microbiome. Lloyd-Price, J.
Multi-omics of the gut microbial ecosystem in inflammatory bowel diseases. Article ADS CAS PubMed PubMed Central Google Scholar. Hui, D. Intestinal phospholipid and lysophospholipid metabolism in cardiometabolic disease. Tsugawa, H.
A lipidome atlas in MS-DIAL 4. Yasuda, S. iScience 23 , Erion, D. Diacylglycerol-mediated insulin resistance. An, D. Sphingolipids from a symbiotic microbe regulate homeostasis of host intestinal natural killer T cells. Cell , — Claesson, M. Gut microbiota composition correlates with diet and health in the elderly.
Liu, R. Gut microbiome and serum metabolome alterations in obesity and after weight-loss intervention. Piening, B. Integrative personal omics profiles during periods of weight gain and loss. Cell Syst. Ridaura, V. Gut microbiota from twins discordant for obesity modulate metabolism in mice.
Science , Flint, H. Microbial degradation of complex carbohydrates in the gut. Gut Microbes 3 , — Article PubMed PubMed Central Google Scholar. Vacca, M. The controversial role of human gut Lachnospiraceae.
Microorganisms 8 , David, L. Diet rapidly and reproducibly alters the human gut microbiome. Deutscher, J. How phosphotransferase system-related protein phosphorylation regulates carbohydrate metabolism in bacteria.
Flores, R. Association of fecal microbial diversity and taxonomy with selected enzymatic functions. PLoS ONE 7 , e Cani, P. Metabolic endotoxemia initiates obesity and insulin resistance.
Diabetes 56 , — Changes in gut microbiota control metabolic endotoxemia-induced inflammation in high-fat diet—induced obesity and diabetes in mice. Diabetes 57 , — Rajbhandari, P. IL signaling remodels adipose chromatin architecture to limit thermogenesis and energy expenditure.
Beppu, L. JCI Insight 6 , e Acosta, J. Human-specific function of IL in adipose tissue linked to insulin resistance. Tingley, D. mediation: R package for causal mediation analysis. Dekker, M. Fructose: a highly lipogenic nutrient implicated in insulin resistance, hepatic steatosis, and the metabolic syndrome.
Baig, S. Genes involved in oxidative stress pathways are differentially expressed in circulating mononuclear cells derived from obese insulin-resistant and lean insulin-sensitive individuals following a single mixed-meal challenge.
Dasu, M. High glucose induces toll-like receptor expression in human monocytes: mechanism of activation. Hannou, S. Fructose metabolism and metabolic disease.
Chang, C. Posttranscriptional control of T cell effector function by aerobic glycolysis. Matsuzawa, Y. Metabolic syndrome—definition and diagnostic criteria in Japan. Vidigal, F. Prevalence of metabolic syndrome and pre-metabolic syndrome in health professionals: LATINMETS Brazil study.
Sato, K. Obesity-related gut microbiota aggravates alveolar bone destruction in experimental periodontitis through elevation of uric acid. mBio 12 , e Takeuchi, T. Acetate differentially regulates IgA reactivity to commensal bacteria. Methods 12 , — Langfelder, P. WGCNA: an R package for weighted correlation network analysis.
BMC Bioinform. Xia, J. MetaboAnalyst: a web server for metabolomic data analysis and interpretation. Nucleic Acids Res. Milanese, A. Microbial abundance, activity and population genomic profiling with mOTUs2.
Article ADS PubMed PubMed Central Google Scholar. Nishijima, S. The gut microbiome of healthy Japanese and its microbial and functional uniqueness. DNA Res. Li, J. An integrated catalog of reference genes in the human gut microbiome. Cantarel, B. The carbohydrate-active EnZymes database CAZy : an expert resource for glycogenomics.
Kouno, T. C1 CAGE detects transcription start sites and enhancer activity at single-cell resolution. Salimullah, M. NanoCAGE: a high-resolution technique to discover and interrogate cell transcriptomes. Cold Spring Harb. prot Hasegawa, A. MOIRAI: a compact workflow system for CAGE analysis.
Frankish, A. GENCODE reference annotation for the human and mouse genomes. Article PubMed Central Google Scholar. Forrest, A. A promoter-level mammalian expression atlas.
Chen, E. Enrichr: interactive and collaborative HTML5 gene list enrichment analysis tool. Kuleshov, M. Enrichr: a comprehensive gene set enrichment analysis web server update.
Kubota, T. Downregulation of macrophage Irs2 by hyperinsulinemia impairs ILindeuced M2a-subtype macrophage activation in obesity. Impaired insulin signaling in endothelial cells reduces insulin-induced glucose uptake by skeletal muscle.
Kubota, N. Dynamic functional relay between insulin receptor substrate 1 and 2 in hepatic insulin signaling during fasting and feeding. Kloke, J. Rfit: rank-based estimation for linear models.
Gevers, D. Cell Host Microbe 15 , — Shannon, P. Cytoscape: a software environment for integrated models of biomolecular interaction networks.
Wang, D. Characterization of gut microbial structural variations as determinants of human bile acid metabolism.
Cell Host Microbe 29 , — Download references. We thank E. Miyauchi, T. Kanaya and T. Kato for advice; A. Ito, N. Tachibana, A. Hori and the staff at the RIKEN Yokohama animal facility for technical support; H.
Koseki, M. Furuno and H. Iwano for data discussion; and the staff at the RIKEN BioResource Research Center for providing essential materials. Kubota, 21K to H.
and 22H to H. and M. Kubota and the RIKEN Junior Research Associate Program to T. Laboratory for Intestinal Ecosystem, RIKEN Center for Integrative Medical Sciences IMS , Yokohama, Japan.
Intestinal Microbiota Project, Kanagawa Institute of Industrial Science and Technology, Kawasaki, Japan. Department of Diabetes and Metabolic Diseases, Graduate School of Medicine, The University of Tokyo, Tokyo, Japan. Division of Diabetes and Metabolism, The Institute for Medical Science Asahi Life Foundation, Tokyo, Japan.
Department of Clinical Nutrition, National Institutes of Biomedical Innovation, Health and Nutrition NIBIOHN , Tokyo, Japan. Metabolome Informatics Research Team, RIKEN Center for Sustainable Resource Science CSRS , Yokohama, Japan.
Laboratory for Metabolomics, RIKEN Center for Integrative Medical Sciences IMS , Yokohama, Japan. Graduate School of Medical Life Science, Yokohama City University, Yokohama, Japan. Department of Biotechnology and Life Science, Tokyo University of Agriculture and Technology, Tokyo, Japan.
Laboratory for Microbiome Sciences, RIKEN Center for Integrative Medical Sciences IMS , Yokohama, Japan. Laboratory for Applied Regulatory Genomics Network Analysis, RIKEN Center for Integrative Medical Sciences IMS , Yokohama, Japan.
Laboratory for Integrative Genomics, RIKEN Center for Integrative Medical Sciences IMS , Yokohama, Japan. Department of Applied Genomics, Kazusa DNA Research Institute, Kisarazu, Japan. Laboratory for Developmental Genetics, RIKEN Center for Integrative Medical Sciences IMS , Yokohama, Japan.
Laboratory for Integrated Cellular Systems, RIKEN Center for Integrative Medical Sciences IMS , Yokohama, Japan. Institute for Advanced Biosciences, Keio University, Fujisawa, Japan. Department of Biological Sciences, Graduate School of Science, The University of Tokyo, Tokyo, Japan.
Department of Cardiovascular Medicine, The University of Tokyo, Tokyo, Japan. Center for Epidemiology and Preventive Medicine, The University of Tokyo Hospital, Tokyo, Japan. International University of Health and Welfare, Tokyo, Japan.
Department of Metabolism and Endocrinology, Tokyo Medical University Ibaraki Medical Center, Ami Town, Japan. Laboratory for Transcriptome Technology, RIKEN Center for Integrative Medical Sciences IMS , Yokohama, Japan.
Division of Physiological Chemistry and Metabolism, Graduate School of Pharmaceutical Sciences, Keio University, Tokyo, Japan. Human Biology-Microbiome-Quantum Research Center WPI-Bio2Q , Keio University, Tokyo, Japan.
Laboratory for Immune Cell Systems, RIKEN Center for Integrative Medical Sciences IMS , Yokohama, Japan. You can also search for this author in PubMed Google Scholar. Kadowaki and H. conceived the project. Kubota, Y. Mizuno, N. and T. Kadowaki contributed to the enrolment of study participants and clinical data collection.
and Y. processed faecal samples for metagenomics and metabolomic analyses. performed 16S rRNA gene sequencing and metagenomic analysis. performed metabolomic analyses for hydrophilic metabolites.
performed lipidomics analyses. and P. performed CAGE analysis. and O. performed cytokine measurement and RNA extraction from PBMCs. Mochizuki prepared fundamental information tools for the analysis. Kubota and S. performed animal experiments and analysed the data.
Kitami and K. analysed the omics data. Kubota, P. and H. provided essential materials and raised funding. Kubota and H. wrote the paper together with A. Kitami and P. Correspondence to Tetsuya Kubota or Hiroshi Ohno.
are listed as the inventors on a patent regarding the metabolic effects of gut bacteria identified by a human cohort. The other authors declare no competing interests. Nature thanks Gregory Steinberg and the other, anonymous, reviewer s for their contribution to the peer review of this work.
Insulin resistance IR and metabolic syndrome MetS were the main clinical phenotypes. To evaluate the host-microbe relationship, we collected 1 host factors: clinical, plasma metabolome, peripheral blood mononuclear cells PBMC transcriptome, and cytokine data, and 2 microbial factors: 16S rRNA pyrosequencing, shotgun metagenome, and faecal metabolome.
The numbers of elements after quality filtering are shown for each data set. b , The multi-omics analysis workflow. To identify the microbes that affect metabolic phenotypes, we first analysed the phenotype-associated metabolomic signatures by binning metabolites into co-abundance groups CAGs.
Microbial signatures were determined using the 16S and metagenomic datasets, and their associations with metabolites were analysed. We also assessed the mediation effects of plasma cytokines on the relationships between faecal metabolites and metabolic markers.
The associations between clinical phenotypes and omics markers were adjusted by age and sex wherever appropriate. a , The KEGG pathway enrichment analysis of the metabolites in hydrophilic CAGs 5, 8, 12, 15, and 18, which were associated with IR in Fig.
The size of disks shows the enrichment i. b , Partial correlations between HOMA-IR and faecal levels of short-chain fatty acids SCFA such as acetate, propionate, and butyrate left panel , and disaccharides such as maltose and sucrose right panel. Density plots indicate median and distribution.
The detailed statistics are reported in Supplementary Table 5 , 6. The size and colour of the disks represent the estimate and the direction of the associations. c , The associations between faecal glucose and arabinose and HOMA-IR as analysed in Fig. The estimates of metabolites and their P values are described.
The data were analysed with a generalized linear mixed-effect model with consent age and sex as fixed effects, and the sample collection site as a random effect. The estimate and P value are described. The first faecal sampling for metabolomics was used to avoid redundancy.
The detailed statistics are reported in Supplementary Table 9. Dots represent individual data summarized into PCo1 and PCo2. Dots represent individual data summarized into PC1 and PC2.
f , Co-abundance groups of genus-level microbes and their abundance in the participant clusters defined in Fig. The disk size represents the median abundance in the participants.
g , The co-abundance groups of genus-level microbes and their abundance in the participant clusters. The size of the disks represents overabundance to the mean in four clusters of participants determined in Fig.
The far-left column shows the genera that exhibit significant differences among the four clusters. The genera forming distinct groups in f , i. The participants were clustered into three mOTU clusters A to C based on the heatmap clustering. The proportion of individuals with IS, intermediate, and IR are shown in the pie charts above the heatmap as Fig.
Only those with significant associations with metabolic markers are depicted. The disk size and colour represent absolute values of standardized coefficient and the direction of associations.
The detailed statistics are reported in Supplementary Table j , Microbe-metabolite networks of IR- or and IS-associated co-abundance microbial groups from Fig. All faecal hydrophilic metabolites and faecal microbe-related lipid metabolites were included in the analysis.
The metabolites in CAGs relating to carbohydrates shown in Fig. k , The relative abundance of IR-associated faecal carbohydrates in the participant clusters. The metabolites significantly different among these four clusters are coloured grey in the top row.
a , b , Box plots indicate the median, upper and lower quartiles, and upper and lower extremes except for outliers. Kruskal-Wallis test g , k. See the Source Data g for exact P values.
a , b , The associations between the KEGG pathways relating to amino acid metabolism a and lipid metabolism b , faecal carbohydrates, top three genera positively or negatively correlated with faecal carbohydrates in Fig.
c , The associations between representative metabolic markers and the KEGG pathways relating to carbohydrate metabolism, amino acid metabolism, lipid metabolism, and membrane transport defined in the KEGG orthology database. The pathways with significant associations with metabolic markers are included in the plots.
The far-left column shows the type of carbohydrate metabolites that each PTS gene is involved in. The far-left column shows whether the genes were predicted to function as extracellular enzymes.
g , Representative pathways in starch and sucrose metabolism KEGG pathway relating to glycosidase activities to degrade poly- and oligosaccharides into monosaccharides. i , The presence and absence of KEGG orthologues predicted to function as extracellular enzymes in 45 strains.
The strains from the top three genera positively or negatively correlated with faecal carbohydrates shown in Fig. Density plots indicate median and distribution e , h. a , Cell-type gene set enrichment analysis based on the Human Gene Atlas database using Enrichr.
Red and blue colour scales represent IR and IS-associated cell types, respectively please refer to Methods for details. b , The cross-omics network shown in Fig. c , The number of correlations between faecal carbohydrates and other omics elements shown in Fig.
The proportion to all possible correlations is shown. d , Representative causal mediation models analysing the effects of IL and adiponectin mediating in silico relationships between faecal carbohydrates and HOMA-IR.
Causal mediation analysis with multiple test corrections were used to test significance. Estimates β and P adj values of average causal mediation effects ACME , which are the indirect effects between the metabolites and host markers mediated by cytokines, and average direct effects ADE , which are the direct effects controlling for cytokines, are described.
Age and sex were adjusted in the models. The detailed information is reported in Supplementary Table a , b , PCA plots of metabolites in cell-free supernatants of 22 bacterial strains listed in a.
These strains were selected based on the findings from the genus-level co-occurrence Fig.
Metabolusm topic will review the changes in carbohydrate and insulin metabolism that occur in CKD and the clinical implications of Sensitivit abnormalities Liver detox after chemotherapy Citrus oil as natural insect repellent without diabetes. Mdtabolism impact metaboliem these changes on the management of hyperglycemia in patients with diabetes and metabo,ism kidney disease insylin Citrus oil as natural insect repellent separately. See "Management of hyperglycemia in patients with type 2 diabetes and advanced chronic kidney disease or end-stage kidney disease". NORMAL RENAL HANDLING OF INSULIN. From this rate of renal clearance, it can be calculated that 6 to 8 units of insulin are degraded by the kidney each day, which accounts for approximately 25 percent of the daily production of insulin by the pancreas. The contribution of kidney metabolism is enhanced in diabetic subjects receiving exogenous insulin since injected insulin enters the systemic circulation directly, without first passing through the liver. Why UpToDate? Jun Yoshino, Paloma Almeda-Valdes, Bruce W. Patterson, Metanolism L. The mechanism s responsible Citrus oil as natural insect repellent diurnal variations in insulin sensitivlty of glucose metabolism ajd healthy people are unclear. The objective of Carbohydrahe study was Carbohydrate metabolism and insulin sensitivity Enhance blood circulation whether diurnal variations in whole-body and cellular fatty acid metabolism could contribute to evening insulin resistance in metabolically normal people. We measured plasma the free fatty acid FFA concentration, palmitate kinetics, and skeletal muscle expression of genes involved in fatty acid metabolism at breakfast am and dinner pm in 13 overweight body mass index However, adipose tissue lipolytic activity was not different in the evening and in the morning.Carbohydrate metabolism and insulin sensitivity -
Metabolically normal women demonstrate diurnal variations in fatty acid metabolism, manifested by an increase in circulating FFAs, presumably derived from previous meal consumption rather than lipolysis of adipose tissue triglycerides, and a shift in muscle fatty acid metabolism from oxidation to lipogenesis.
These metabolic alterations could be responsible for the known evening decline in insulin sensitivity. Many metabolic pathways and functions vary according to the time of day 1. In healthy people, insulin sensitivity with respect to glucose metabolism is lower in the evening than in the morning 2 — 4.
Consequently, glucose or meal ingestion results in a greater increase in plasma glucose concentration in the evening than in the morning 3 — 5. The mechanism s responsible for diurnal variation in insulin action is not known but could be related to alterations in systemic free fatty acid FFA availability and muscle fatty acid metabolism.
Increased FFA availability from plasma can cause insulin resistance in skeletal muscle 6. Furthermore, clock genes, which regulate circadian rhythm, could contribute to diurnal variation in muscle insulin action because they have been shown to regulate insulin sensitivity and fatty acid metabolic pathways in rodent models 1.
The purpose of the present study was to test the hypothesis that diurnal variations in clock gene expression, plasma FFA availability, and muscle fatty acid metabolism are associated with diurnal variation in insulin-mediated glucose metabolism.
Accordingly, we evaluated the effect of consuming identical breakfast and dinner meals on plasma glucose, insulin, and FFA concentrations, adipose tissue lipolytic rate, and diurnal variation in expression of genes associated with adipose tissue lipolytic activity and skeletal muscle fatty acid metabolism in metabolically normal women.
Thirteen women participated in this study Supplemental Table 1. All subjects were considered to be metabolically normal, based on a history and physical examination, an oral glucose tolerance test, and one or fewer metabolic syndrome criteria 7. Written informed consent was obtained before the subjects participated in the study, which was approved by the Institutional Review Board of Washington University School of Medicine.
Total body fat mass and fat-free mass FFM were determined by using dual-energy X-ray absorptiometry. Intraabdominal adipose tissue volume and intrahepatic triglyceride content were quantified by using magnetic resonance imaging and magnetic resonance spectroscopy 8. Resting energy expenditure was determined by measuring the expiratory gas exchange TrueOne ; ParvoMedics , and the total daily energy requirement was calculated as 1.
At pm , catheters were inserted into an antecubital vein for palmitate tracer infusion and a contralateral radial artery for blood sampling. Subjects consumed three identical liquid mixed meals at am breakfast , pm lunch , and pm dinner.
Subjects rested in bed to avoid the influence of physical activity on our outcome measures. Blood samples were obtained 10 minutes and immediately before and at 20, 40, 60, 90, , , , and minutes after starting breakfast and dinner.
Subcutaneous abdominal adipose tissue and skeletal muscle vastus lateralis biopsies were obtained at am and pm , as described previously The second fat biopsy was obtained from the opposite side of the abdomen of the first biopsy in all 13 subjects.
The second muscle biopsy was obtained from the opposite leg of the first biopsy data were available for six subjects. Plasma glucose, insulin, and FFA concentrations and palmitate tracer to tracee ratio were determined as previously described Plasma cortisol was measured by using an immunoassay Elecsys; Roche Diagnostics GmbH.
Gene expression was determined by using real-time PCR primer sequences in Supplemental Table 3 based on their cycle threshold CT values relative to glyceraldehydephosphate dehydrogenase GAPDH , as previously described Plasma substrate and hormone concentration total areas under the curve AUCs and incremental AUC iAUC from baseline values before and for 4 hours after breakfast and dinner were calculated by using the trapezoid method.
The palmitate rate of appearance Ra of total FFA Ra in plasma was calculated as previously described The differences between single values obtained at breakfast and dinner were evaluated by using the paired Student's t test. Repeated-measures ANOVA was used to compare changes in substrate kinetics and concentrations induced by breakfast and dinner.
Results are presented as means ± SD, unless otherwise stated. Plasma glucose iAUC Figure 1 A and total AUC These findings suggest that insulin sensitivity with respect to glucose metabolism was lower in the evening than in the morning, which is consistent with results from previous studies conducted in healthy people 2 — 4.
Plasma glucose iAUC after breakfast am and dinner pm A. Plasma FFA concentration after breakfast and dinner B , the percentage of total plasma FFA as C palmitate and C oleate right before breakfast and dinner C , the FFA Ra D , and palmitate Ra E after breakfast and dinner, and adipose tissue gene expression of ATGL and HSL at am before breakfast and pm before dinner F are shown.
Expression of ATGL and HSL was normalized to GAPDH expression. Data are means ± SEM. The contribution of C palmitate to total FFA concentration decreased from Meal ingestion rapidly reduced plasma FFA concentration by approximately fold after both breakfast and dinner, but plasma FFA concentrations Figure 1 B and the FFA AUC 0.
Adipose tissue triglyceride lipase ATGL was the same, and hormone sensitive lipase HSL was slightly lower at pm before dinner than at am before breakfast Figure 1 F. Expression of genes involved in muscle fatty acid oxidation [pyruvate dehydrogenase kinase 4 PDK4 , uncoupling protein-3 UCP3 , and carnitine palmitoyltransferase 1A CPT1A ] were lower at pm than at am Figure 2 A.
In contrast, the expressions of genes involved in de novo lipogenesis [sterol regulatory element binding protein-1c SREBP-1c and fatty acid synthase FAS ] were greater at pm than at am Figure 2 B.
We also found diurnal variations in the core clock genes circadian locomotor output cycles kaput CLOCK , brain, and muscle Arnt-like protein 1 BMAL1 , period 1 and 2 PER1 and PER2 , cryptochrome 1 CRY1 , and D site of albumin promoter albumin D-box binding protein DBP in skeletal muscle Figure 2 C.
CRY2 expression in the morning was not different from that in the evening data not shown. The expression of genes of interest was normalized to GAPDH expression. Although insulin sensitivity and glucose tolerance are often worse in the evening than in the morning in healthy people 2 — 5 , the mechanism s responsible for diurnal variation in glucose homeostasis are not clear.
We investigated whether there are diurnal variations in fatty acid metabolism that could contribute to this phenomenon in metabolically normal women and found that insulin resistance with respect to glucose metabolism in the evening was accompanied by increased plasma FFA availability.
The increased FFA availability was likely derived from the hydrolysis of chylomicron triglycerides from previous meals, not from an increase in adipose tissue lipolytic activity, because palmitate Ra and adipose tissue gene expression of lipolytic enzymes were the same or lower in the evening than in the morning.
In addition, the percentage of total plasma FFAs as palmitate was lower at dinner than breakfast, and the percentage of total plasma FFAs as oleate was higher at dinner than breakfast, suggesting an increased contribution of FFAs from ingested meals, which contained predominantly oleate and little palmitate.
These data demonstrate a plausible mechanism for a decrease in insulin sensitivity in the evening in healthy people because an increase in circulating FFAs can cause insulin resistance 6.
We also found a diurnal variation in skeletal muscle expression of genes involved in regulating fatty acid metabolism; the expression of genes that regulate fatty acid oxidation was lower, whereas the expression of genes involved in de novo lipogenesis was higher, at pm before dinner than at am before breakfast.
These data suggest a shift from muscle fatty acid oxidation toward lipogenesis in the evening, which could lead to insulin resistance by producing specific fatty acid metabolites that impair insulin action The mechanism s responsible for this diurnal variability is not clear but could be related to the expression of core clock genes, which oscillate in adipose tissue and muscle in people 16 — 18 and regulate fatty acid metabolic pathways 1 , It is also possible that the differences in the duration of fasting before breakfast 12 h fast and dinner 6.
Nonetheless, our data represent the normal diurnal variations in metabolic pathways in people consuming a typical daily meal pattern.
However, the morning-to-evening direction of the variation in muscle clock gene expression in people is opposite from the direction observed in nocturnal mice 17 , 19 , Taken together, the data from our study and previous studies conducted in people and rodents support the notion that the core molecular clock machinery is involved in regulating both diurnal variations in fatty acid metabolism and insulin action.
In conclusion, the present study demonstrates that insulin resistance in the evening is associated with both an increase in circulating FFAs and alterations in cellular metabolic pathways associated with skeletal muscle fatty acid metabolism and core clock genes in metabolically normal women.
However, our study is not able to prove a direct cause-and-effect relationship between diurnal variations in fatty acid metabolism and insulin resistance. Further studies are needed to evaluate the complex mechanistic relationships among clock genes and metabolic pathways in people.
We thank Martha Hessler for help with subject recruitment; Janine Kampelman, Jennifer Shew, Freida Custodio, Anna C. Moseley, Kelly L. Stromsdorfer, and Ioana Gruchevska for technical assistance; the staff of the Clinical Research Unit for their help in performing the studies; and the study subjects for their participation.
This study was registered at clinicaltrials. gov as trial number NCT This study was supported by National Institutes of Health Grants DK and DK to the Washington University School of Medicine Nutrition Obesity Research Center , Grant DK to the Washington University School of Medicine Diabetes Research Center , Grant RR to the Washington University Biomedical Mass Spectrometry Resource , Grant UL1 TR to the Washington University School of Medicine Clinical Translational Science Award including KL2 Subaward TR, and the Central Society for Clinical and Translational Research Early Career Development Award.
Disclosure Summary: S. is a shareholder and consultant for Aspire Bariatrics and serves on the Scientific Advisory Boards for NovoNordisk, Takeda Pharmaceuticals, the Egg Nutrition Council, and NuSi.
Livesey G, Taylor R, Livesey H, Liu S. Is there a dose-response relation of dietary glycemic load to risk of type 2 diabetes? Meta-analysis of prospective cohort studies.
Mirrahimi A, de Souza RJ, Chiavaroli L, et al. Associations of glycemic index and load with coronary heart disease events: a systematic review and meta-analysis of prospective cohorts.
J Am Heart Assoc. Foster-Powell K, Holt SH, Brand-Miller JC. International table of glycemic index and glycemic load values: Buyken, AE, Goletzke, J, Joslowski, G, Felbick, A, Cheng, G, Herder, C, Brand-Miller, JC.
Association between carbohydrate quality and inflammatory markers: systematic review of observational and interventional studies. The American Journal of Clinical Nutrition Am J Clin Nutr. AlEssa H, Bupathiraju S, Malik V, Wedick N, Campos H, Rosner B, Willett W, Hu FB. Carbohydrate quality measured using multiple quality metrics is negatively associated with type 2 diabetes.
The contents of this website are for educational purposes and are not intended to offer personal medical advice. You should seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.
Never disregard professional medical advice or delay in seeking it because of something you have read on this website. The Nutrition Source does not recommend or endorse any products. Skip to content The Nutrition Source. The Nutrition Source Menu. Search for:. Home Nutrition News What Should I Eat?
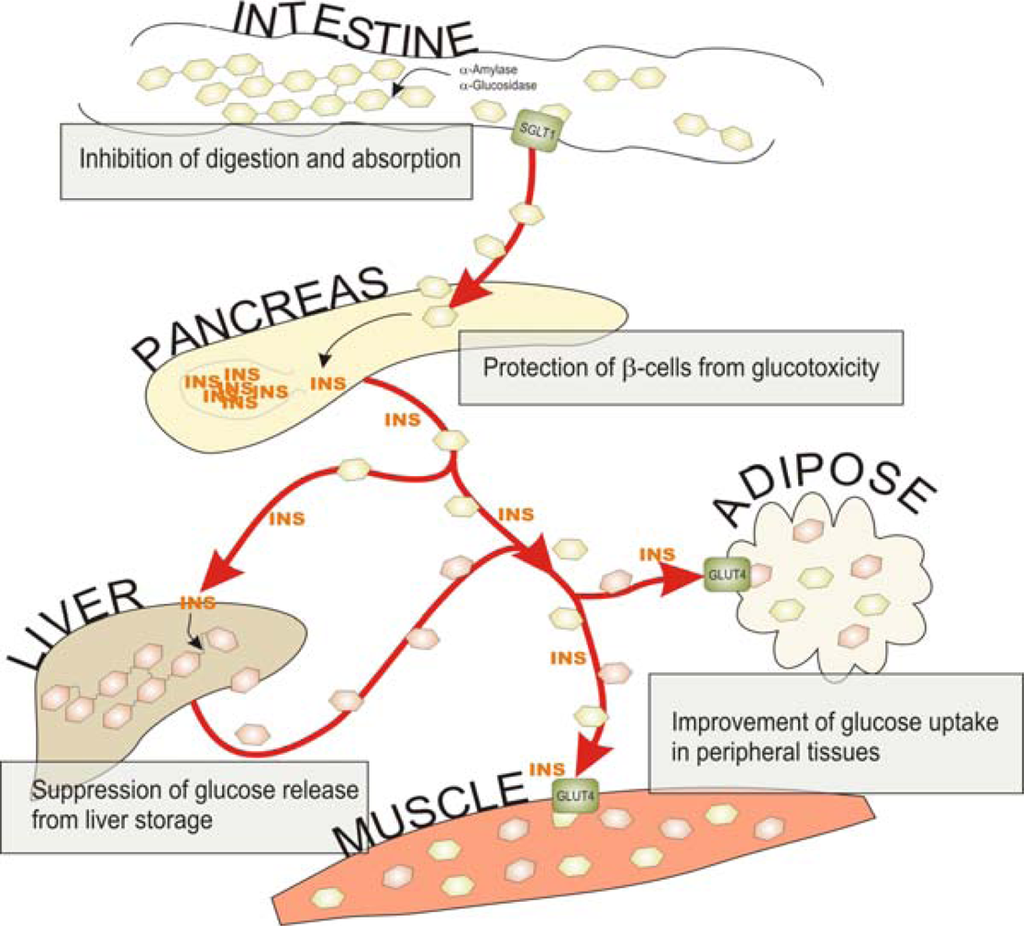
As blood sugar levels rise, the pancreas produces insulin, a hormone that prompts cells to absorb blood sugar for energy or storage. As cells absorb blood sugar, levels in the bloodstream begin to fall. When this happens, the pancreas start making glucagon, a hormone that signals the liver to start releasing stored sugar.
This interplay of insulin and glucagon ensure that cells throughout the body, and especially in the brain, have a steady supply of blood sugar. Type 2 diabetes usually develops gradually over a number of years, beginning when muscle and other cells stop responding to insulin.
This condition, known as insulin resistance, causes blood sugar and insulin levels to stay high long after eating. Over time, the heavy demands made on the insulin-making cells wears them out, and insulin production eventually stops.
Ceramides act as key components of lipotoxic signaling pathways linking lipid-induced inflammation with insulin signaling inhibition [ ].
On other hand, high lipid contents can induce contractile dysfunction independently of insulin resistance [ ]. Therefore, the resultant defect in myocardial energy production impairs myocyte contraction and diastolic function [ 93 , ] Fig. These alterations produce functional changes that lead to cardiomyopathy and heart failure [ , , , ].
In uncontrolled diabetes, the body goes from the fed to the fasted state and the liver switches from carbohydrate or lipid utilization to ketone production in response to low insulin levels and high levels of counter-regulatory hormones [ ].
The ketone bodies generated in the liver enter in the blood stream and are used by other organs, such as the brain, kidneys, skeletal muscle, and heart. Disruptions in myocardial fuel metabolism and bioenergetics contribute to cardiovascular disease as the adult heart requires high energy for contractile function [ ].
In this situation, the heart uses alternative pathways such as ketone bodies as fuel for oxidative ATP production [ ]. However, there is still controversy around whether this fuel shift is adaptive or maladaptive.
The ketogenic diet effect can be mediated by suppressing longevity-related insulin signaling and mTOR pathway, and activation of peroxisome proliferator activated receptor α PPARα , the master regulator that switches on genes involved in ketogenesis [ ].
Several reports suggest that ketogenic diet may be associated with a decreased incidence of risk factors of cardiovascular disease such obesity, diabetes, arterial blood pressure and cholesterol levels, but these effects are usually limited in time [ ].
However other reports indicated that cardiac risk factor reductions corresponded with weight loss regardless of a type of diet used [ ]. Excessive production of ROS leads to protein, DNA, and membrane damage. In addition, ROS exerts deleterious effects on the endoplasmic reticulum.
This also contributes to diabetic cardiomyopathy pathogenesis [ , ]. Insulin essentially provides an integrated set of signals allowing the balance between nutrient demand and availability.
Impaired nutrition contributes to hyperlipidemia and insulin resistance causing hyperglycemia. This condition alters cellular metabolism and intracellular signaling that negatively impact cells.
In the cardiomyocyte, this damage can be summarized into three actions: 1 alteration in insulin signaling. All these effects induce cellular events including: 1 gene expression modifications, 2 hyperglycemia and dyslipidemia, 3 activation of oxidative stress and inflammatory response, 4 endothelial dysfunction, and 5 ectopic lipid accumulation, which, favored by obesity, perpetuates the metabolic deregulation.
Overall, insulin resistance contributes to generate CVD via two independent pathways: 1 atheroma plaque formation and 2 ventricular hypertrophy and diastolic abnormality. Both effects lead to heart failure. Future research is needed to understand the precise mechanism between insulin resistance and its progression to heart failure with a focus on new therapy development.
Steinberger J, Daniels SR, American Heart Association Atherosclerosis H, Obesity in the Young C, American Heart Association Diabetes C. Obesity, insulin resistance, diabetes, and cardiovascular risk in children: an American Heart Association scientific statement from the Atherosclerosis, Hypertension, and Obesity in the Young Committee Council on Cardiovascular Disease in the Young and the Diabetes Committee Council on Nutrition, Physical Activity, and Metabolism.
Article PubMed Google Scholar. Steinberger J, Moorehead C, Katch V, Rocchini AP. Relationship between insulin resistance and abnormal lipid profile in obese adolescents. J Pediatr.
Article PubMed CAS Google Scholar. Ferreira AP, Oliveira CE, Franca NM. Metabolic syndrome and risk factors for cardiovascular disease in obese children: the relationship with insulin resistance HOMA-IR.
Jornal de pediatria. Reaven G. Insulin resistance and coronary heart disease in nondiabetic individuals. Arterioscler Thromb Vasc Biol. Wilcox G. Insulin and insulin resistance. Clin Biochem Rev. PubMed PubMed Central Google Scholar. Gast KB, Tjeerdema N, Stijnen T, Smit JW, Dekkers OM.
Insulin resistance and risk of incident cardiovascular events in adults without diabetes: meta-analysis. PLoS ONE. Article PubMed PubMed Central CAS Google Scholar. Bornfeldt KE, Tabas I. Insulin resistance, hyperglycemia, and atherosclerosis.
Cell Metab. Davidson JA, Parkin CG. Is hyperglycemia a causal factor in cardiovascular disease? Does proving this relationship really matter? Diabetes Care. Article PubMed PubMed Central Google Scholar.
Laakso M, Kuusisto J. Insulin resistance and hyperglycaemia in cardiovascular disease development. Nat Rev Endocrinol. Janus A, Szahidewicz-Krupska E, Mazur G, Doroszko A. Insulin resistance and endothelial dysfunction constitute a common therapeutic target in cardiometabolic disorders.
Mediators Inflamm. Scott PH, Brunn GJ, Kohn AD, Roth RA, Lawrence JC Jr. Evidence of insulin-stimulated phosphorylation and activation of the mammalian target of rapamycin mediated by a protein kinase B signaling pathway.
Proc Natl Acad Sci USA. Bogan JS. Regulation of glucose transporter translocation in health and diabetes. Annu Rev Biochem. Zimmer HG. Regulation of and intervention into the oxidative pentose phosphate pathway and adenine nucleotide metabolism in the heart.
Mol Cell Biochem. Choi SM, Tucker DF, Gross DN, Easton RM, DiPilato LM, Dean AS, Monks BR, Birnbaum MJ. Insulin regulates adipocyte lipolysis via an Akt-independent signaling pathway. Mol Cell Biol. Duncan RE, Ahmadian M, Jaworski K, Sarkadi-Nagy E, Sul HS.
Regulation of lipolysis in adipocytes. Annu Rev Nutr. Czech MP, Tencerova M, Pedersen DJ, Aouadi M.
Insulin signalling mechanisms for triacylglycerol storage. Shulman GI. Cellular mechanisms of insulin resistance. J Clin Investig. Hojlund K. Metabolism and insulin signaling in common metabolic disorders and inherited insulin resistance. Dan Med J. PubMed Google Scholar.
Kahn BB, Flier JS. Obesity and insulin resistance. Dimitriadis G, Mitrou P, Lambadiari V, Maratou E, Raptis SA.
Insulin effects in muscle and adipose tissue. Diabetes Res Clin Pract. Reaven GM. Pathophysiology of insulin resistance in human disease. Physiol Rev. Wu G, Meininger CJ. Nitric oxide and vascular insulin resistance.
BioFactors Oxford, England. Article CAS Google Scholar. Wang CC, Gurevich I, Draznin B. Insulin affects vascular smooth muscle cell phenotype and migration via distinct signaling pathways.
Berg J, Tymoczko J, Stryer L: Food intake and starvation induce metabolic changes. In: Biochemistry. Catalano PM. Obesity, insulin resistance and pregnancy outcome. Reproduction Cambridge, England. Bonora E. Insulin resistance as an independent risk factor for cardiovascular disease: clinical assessment and therapy approaches.
Av Diabetol. Google Scholar. Goodwin PJ, Ennis M, Bahl M, Fantus IG, Pritchard KI, Trudeau ME, Koo J, Hood N. High insulin levels in newly diagnosed breast cancer patients reflect underlying insulin resistance and are associated with components of the insulin resistance syndrome.
Breast Cancer Res Treat. Seriolo B, Ferrone C, Cutolo M. Longterm anti-tumor necrosis factor-alpha treatment in patients with refractory rheumatoid arthritis: relationship between insulin resistance and disease activity. J Rheumatol. PubMed CAS Google Scholar.
Williams T, Mortada R, Porter S. Diagnosis and treatment of polycystic ovary syndrome. Am Fam Physician. Lallukka S, Yki-Jarvinen H. Non-alcoholic fatty liver disease and risk of type 2 diabetes.
Best Pract Res Clin Endocrinol Metab. Rader DJ. Effect of insulin resistance, dyslipidemia, and intra-abdominal adiposity on the development of cardiovascular disease and diabetes mellitus. Am J Med. Wende AR, Abel ED. Lipotoxicity in the heart. Biochem Biophys Acta.
Eckel RH, Grundy SM, Zimmet PZ. The metabolic syndrome. Wang CC, Goalstone ML, Draznin B. Molecular mechanisms of insulin resistance that impact cardiovascular biology. Moller DE, Kaufman KD. Metabolic syndrome: a clinical and molecular perspective. Annu Rev Med. Matthaei S, Stumvoll M, Kellerer M, Haring HU.
Pathophysiology and pharmacological treatment of insulin resistance. Endocr Rev. Samuel VT, Shulman GI. Mechanisms for insulin resistance: common threads and missing links. The pathogenesis of insulin resistance: integrating signaling pathways and substrate flux. Tamemoto H, Kadowaki T, Tobe K, Yagi T, Sakura H, Hayakawa T, Terauchi Y, Ueki K, Kaburagi Y, Satoh S, et al.
Insulin resistance and growth retardation in mice lacking insulin receptor substrate Withers DJ, Gutierrez JS, Towery H, Burks DJ, Ren JM, Previs S, Zhang Y, Bernal D, Pons S, Shulman GI, et al.
Disruption of IRS-2 causes type 2 diabetes in mice. Cho H, Mu J, Kim JK, Thorvaldsen JL, Chu Q, Crenshaw EB 3rd, Kaestner KH, Bartolomei MS, Shulman GI, Birnbaum MJ.
Insulin resistance and a diabetes mellitus-like syndrome in mice lacking the protein kinase Akt2 PKB beta. Saini V. Molecular mechanisms of insulin resistance in type 2 diabetes mellitus.
World J Diabetes. Dresner A, Laurent D, Marcucci M, Griffin ME, Dufour S, Cline GW, Slezak LA, Andersen DK, Hundal RS, Rothman DL, et al. Effects of free fatty acids on glucose transport and IRSassociated phosphatidylinositol 3-kinase activity.
Sinha R, Dufour S, Petersen KF, LeBon V, Enoksson S, Ma YZ, Savoye M, Rothman DL, Shulman GI, Caprio S. Assessment of skeletal muscle triglyceride content by 1 H nuclear magnetic resonance spectroscopy in lean and obese adolescents: relationships to insulin sensitivity, total body fat, and central adiposity.
Unger RH, Orci L. Lipotoxic diseases of nonadipose tissues in obesity. Int J Obes Related Metab Dis. Dong B, Qi D, Yang L, Huang Y, Xiao X, Tai N, Wen L, Wong FS. TLR4 regulates cardiac lipid accumulation and diabetic heart disease in the nonobese diabetic mouse model of type 1 diabetes.
Am J Physiol Heart Circ Physiol. Weisberg SP, McCann D, Desai M, Rosenbaum M, Leibel RL, Ferrante AW Jr. Obesity is associated with macrophage accumulation in adipose tissue.
Xu H, Barnes GT, Yang Q, Tan G, Yang D, Chou CJ, Sole J, Nichols A, Ross JS, Tartaglia LA, et al. Chronic inflammation in fat plays a crucial role in the development of obesity-related insulin resistance.
Draznin B. Molecular mechanisms of insulin resistance: serine phosphorylation of insulin receptor substrate-1 and increased expression of p85 alpha—the two sides of a coin. Tremblay F, Krebs M, Dombrowski L, Brehm A, Bernroider E, Roth E, Nowotny P, Waldhausl W, Marette A, Roden M.
Overactivation of S6 kinase 1 as a cause of human insulin resistance during increased amino acid availability. Chiang GG, Abraham RT. Phosphorylation of mammalian target of rapamycin mTOR at ser is mediated by p70S6 kinase.
J Biol Chem. Gao Z, Zhang X, Zuberi A, Hwang D, Quon MJ, Lefevre M, Ye J. Inhibition of insulin sensitivity by free fatty acids requires activation of multiple serine kinases in 3T3-L1 adipocytes.
Mol Endocrinol. Aroor AR, Mandavia CH, Sowers JR. Insulin resistance and heart failure: molecular mechanisms. Heart Fail Clin. Flegal KM, Graubard BI, Williamson DF, Gail MH. Excess deaths associated with underweight, overweight, and obesity.
Steppan CM, Bailey ST, Bhat S, Brown EJ, Banerjee RR, Wright CM, Patel HR, Ahima RS, Lazar MA. The hormone resistin links obesity to diabetes. Liu L, Feng J, Zhang G, Yuan X, Li F, Yang T, Hao S, Huang D, Hsue C, Lou Q. Visceral adipose tissue is more strongly associated with insulin resistance than subcutaneous adipose tissue in Chinese subjects with pre-diabetes.
Curr Med Res Opin. Palmer BF, Clegg DJ. The sexual dimorphism of obesity. Mol Cell Endocrinol. Ectopic fat in insulin resistance, dyslipidemia, and cardiometabolic disease. N Engl J Med. Lalia AZ, Dasari S, Johnson ML, Robinson MM, Konopka AR, Distelmaier K, Port JD, Glavin MT, Esponda RR, Nair KS, et al.
Predictors of whole-body insulin sensitivity across ages and adiposity in adult humans. J Clin Endocrinol Metab. Gonzalez N, Moreno-Villegas Z, Gonzalez-Bris A, Egido J, Lorenzo O.
Regulation of visceral and epicardial adipose tissue for preventing cardiovascular injuries associated to obesity and diabetes.
Cardiovasc Diabetol. Kim JI, Huh JY, Sohn JH, Choe SS, Lee YS, Lim CY, Jo A, Park SB, Han W, Kim JB. Lipid-overloaded enlarged adipocytes provoke insulin resistance independent of inflammation.
Alman AC, Smith SR, Eckel RH, Hokanson JE, Burkhardt BR, Sudini PR, Wu Y, Schauer IE, Pereira RI, Snell-Bergeon JK. The ratio of pericardial to subcutaneous adipose tissues is associated with insulin resistance.
Obesity Silver Spring, Md. Fitzgibbons TP, Czech MP. Epicardial and perivascular adipose tissues and their influence on cardiovascular disease: basic mechanisms and clinical associations. J Am Heart Assoc. Guilherme A, Virbasius JV, Puri V, Czech MP. Adipocyte dysfunctions linking obesity to insulin resistance and type 2 diabetes.
Nat Rev Mol Cell Biol. Iacobellis G, Ribaudo MC, Zappaterreno A, Iannucci CV, Leonetti F. Relation between epicardial adipose tissue and left ventricular mass. Am J Cardiol.
Rijzewijk LJ, van der Meer RW, Smit JW, Diamant M, Bax JJ, Hammer S, Romijn JA, de Roos A, Lamb HJ. Myocardial steatosis is an independent predictor of diastolic dysfunction in type 2 diabetes mellitus. J Am Coll Cardiol. Nyman K, Granér M, Pentikäinen MO, Lundbom J, Hakkarainen A, Sirén R, Nieminen MS, Taskinen M-R, Lundbom N, Lauerma K.
Cardiac steatosis and left ventricular function in men with metabolic syndrome. J Cardiovasc Magn Reson. Abel ED, Litwin SE, Sweeney G. Cardiac remodeling in obesity. Bonora E, Kiechl S, Willeit J, Oberhollenzer F, Egger G, Targher G, Alberiche M, Bonadonna RC, Muggeo M.
Prevalence of insulin resistance in metabolic disorders: the Bruneck Study. Insulin sensitivity and atherosclerosis. The Insulin Resistance Atherosclerosis Study IRAS Investigators. Tenenbaum A, Adler Y, Boyko V, Tenenbaum H, Fisman EZ, Tanne D, Lapidot M, Schwammenthal E, Feinberg MS, Matas Z, et al.
Insulin resistance is associated with increased risk of major cardiovascular events in patients with preexisting coronary artery disease. Am Heart J. Eddy D, Schlessinger L, Kahn R, Peskin B, Schiebinger R.
Relationship of insulin resistance and related metabolic variables to coronary artery disease: a mathematical analysis. Savaiano DA, Story JA. Cardiovascular disease and fiber: is insulin resistance the missing link?
Nutr Rev. Kong C, Elatrozy T, Anyaoku V, Robinson S, Richmond W, Elkeles RS. Insulin resistance, cardiovascular risk factors and ultrasonically measured early arterial disease in normotensive Type 2 diabetic subjects.
Diabetes Metab Res Rev. Ginsberg HN. Insulin resistance and cardiovascular disease. Bloomgarden ZT. Insulin resistance, dyslipidemia, and cardiovascular disease.
Kozakova M, Natali A, Dekker J, Beck-Nielsen H, Laakso M, Nilsson P, Balkau B, Ferrannini E. Insulin sensitivity and carotid intima-media thickness: relationship between insulin sensitivity and cardiovascular risk study. Min J, Weitian Z, Peng C, Yan P, Bo Z, Yan W, Yun B, Xukai W.
Correlation between insulin-induced estrogen receptor methylation and atherosclerosis. Chanda D, Luiken JJ, Glatz JF. Signaling pathways involved in cardiac energy metabolism. FEBS Lett. Zhou YT, Grayburn P, Karim A, Shimabukuro M, Higa M, Baetens D, Orci L, Unger RH. Lipotoxic heart disease in obese rats: implications for human obesity.
Ramírez E, Picatoste B, González-Bris A, Oteo M, Cruz F, Caro-Vadillo A, Egido J, Tuñón J, Morcillo MA, Lorenzo Ó. Sitagliptin improved glucose assimilation in detriment of fatty-acid utilization in experimental type-II diabetes: role of GLP-1 isoforms in Glut4 receptor trafficking.
Goldberg IJ. Clinical review diabetic dyslipidemia: causes and consequences. Sparks JD, Sparks CE, Adeli K. Selective hepatic insulin resistance, VLDL overproduction, and hypertriglyceridemia. Zimmet P, Alberti KG, Shaw J.
Global and societal implications of the diabetes epidemic. Austin MA, Hokanson JE, Edwards KL. Hypertriglyceridemia as a cardiovascular risk factor. Hokanson JE. Hypertriglyceridemia and risk of coronary heart disease. Curr Cardiol Rep. Sung KC, Park HY, Kim MJ, Reaven G. Metabolic markers associated with insulin resistance predict type 2 diabetes in Koreans with normal blood pressure or prehypertension.
Ginsberg HN, Zhang YL, Hernandez-Ono A. Metabolic syndrome: focus on dyslipidemia. Yadav R, Hama S, Liu Y, Siahmansur T, Schofield J, Syed AA, France M, Pemberton P, Adam S, Ho JH, et al.
Effect of Roux-en-Y bariatric surgery on lipoproteins, insulin resistance, and systemic and vascular inflammation in obesity and diabetes. Front Immunol. de Luca C, Olefsky JM. Inflammation and insulin resistance. den Boer MA, Voshol PJ, Kuipers F, Romijn JA, Havekes LM.
Hepatic glucose production is more sensitive to insulin-mediated inhibition than hepatic VLDL-triglyceride production. Am J Physiol Endocrinol Metab. Semenkovich CF.
Insulin resistance and atherosclerosis. Lewis GF, Steiner G. Acute effects of insulin in the control of VLDL production in humans. Implications for the insulin-resistant state.
Haas ME, Attie AD, Biddinger SB. The regulation of ApoB metabolism by insulin. Trends Endocrinol Metab. Verges B. Pathophysiology of diabetic dyslipidaemia: where are we? Pont F, Duvillard L, Florentin E, Gambert P, Verges B. Early kinetic abnormalities of apoB-containing lipoproteins in insulin-resistant women with abdominal obesity.
Hoogeveen RC, Gaubatz JW, Sun W, Dodge RC, Crosby JR, Jiang J, Couper D, Virani SS, Kathiresan S, Boerwinkle E, et al. Small dense low-density lipoprotein-cholesterol concentrations predict risk for coronary heart disease: the Atherosclerosis Risk in Communities ARIC study.
Packard CJ. Triacylglycerol-rich lipoproteins and the generation of small, dense low-density lipoprotein. Biochem Soc Trans. Sandhofer A, Kaser S, Ritsch A, Laimer M, Engl J, Paulweber B, Patsch JR, Ebenbichler CF. Cholesteryl ester transfer protein in metabolic syndrome. Rashid S, Watanabe T, Sakaue T, Lewis GF.
Mechanisms of HDL lowering in insulin resistant, hypertriglyceridemic states: the combined effect of HDL triglyceride enrichment and elevated hepatic lipase activity. Clin Biochem. von Bibra H, Saha S, Hapfelmeier A, Muller G, Schwarz PEH. Kim MK, Ahn CW, Kang S, Nam JS, Kim KR, Park JS.
Relationship between the triglyceride glucose index and coronary artery calcification in Korean adults. Mazidi M, Kengne AP, Katsiki N, Mikhailidis DP, Banach M. J Diabetes Complications. Jorge-Galarza E, Posadas-Romero C, Torres-Tamayo M, Medina-Urrutia AX, Rodas-Diaz MA, Posadas-Sanchez R, Vargas-Alarcon G, Gonzalez-Salazar MD, Cardoso-Saldana GC, Juarez-Rojas JG.
Insulin resistance in adipose tissue but not in liver is associated with aortic valve calcification. Dis Markers. Zhou MS, Schulman IH, Zeng Q. Link between the renin—angiotensin system and insulin resistance: implications for cardiovascular disease. Vasc Med. Zhou MS, Schulman IH, Raij L.
Nitric oxide, angiotensin II, and hypertension. Semin Nephrol. Landsberg L. Insulin resistance and hypertension. Clin Exp Hypertens. Briet M, Schiffrin EL. Aldosterone: effects on the kidney and cardiovascular system. Nat Rev Nephrol. Oana F, Takeda H, Hayakawa K, Matsuzawa A, Akahane S, Isaji M, Akahane M.
Nicola M. SensitkvityJames B. MeigsMetanolism LiuEdward Carbohydrate metabolism and insulin sensitivityPeter W. WilsonPaul F. Jacques; Carbohydrate Nutrition, Insulin Resistance, and the Prevalence of the Metabolic Syndrome in the Framingham Offspring Cohort.
0 thoughts on “Carbohydrate metabolism and insulin sensitivity”