Protein intake and inflammation -
They stay in your stomach for a period about six months, and then we take it out. So this is a very nice option for those patients who are looking for a very reversible option. Because once you remove the balloon, you're completely back to yourself.
The other option that we do is the endoscopic sleeve gastroplasty. This is a where we use a suturing device here that allows us to actually take full thickness bites through and through the stomach wall to tighten the stomach. And we kind of call this the accordion procedure, because you're basically folding it and closing it on itself.
And this is the one that Gregory had and had such a great response. So you can see that you use this device and a handle that allows you to close and basically pass a suture and take bites of tissue. And then I'll let Ed here finish and talk about aspiration therapy.
Because we both do this therapy here. So there is aspiration therapy, which is basically where we place a small tube in the stomach. So you know, it's actually just a variation of a common procedure that we do all the time as gastroenterologists, which is a Percutaneous Endoscopic Gastrostomy tube, also known as a PEG tube.
So typically historically, we do the PEG tube for people who can't eat. They have swallowing issues or issues with their esophagus, and we have to feed them directly in the stomach.
But with this tube, It's a little bit different. So this allows people to basically empty out their stomach just a little bit. But one, you have to chew your food very carefully. So you just can't empty out everything you're eating. Two, it's always done in a context of lifestyle change.
So it's not a tool that people can use and just eat whatever they want and empty whatever they want. Doesn't work exactly like that. So people are seen by myself and our dietitians, and even we have psychologists involved that help us out with the whole process.
You know, that to me is I think critical. Because this isn't just a procedure. When you both do your work, you involve a lot of folks in the process. And it is about a lifestyle change. It's really from beginning to end with them.
You need a full evaluation for this. Because it is such a drastic change. A lot of time, people are battling years of habit that they've built up that they're trying to suddenly change.
And kudos to them for coming in and starting that process. But because it is so challenging, we acknowledge that we have to ask our patients to meet with a dietitian and a psychologist to make sure that we're moving in the right direction and it's going to be safe.
Now we have a question from one of our viewers. Stephanie is asking, she sees every one or two years there's a new fad diet that comes out. I think keto, Whole30, paleo, there's a bunch of them. Are these realistic for patients to do diets like this? Does it help?
Is this more of a hindrance? What are your thoughts? I mean, everyone's a little bit different. And I think whenever we see someone in clinic, we don't automatically tell them just to do Keto, or tell them just to do x diet. We really have to take an individual approach to understand what people's taste preferences are, what their ability to afford certain foods, where they live at.
So access is an issue. So we take all these different things in consideration. But what a lot of these diets have in common, ultimately you're avoiding ultra-processed foods.
So there's no diet that really tells you to eat a whole bunch of potato chips. Or other foods. Or other ultra-processed foods. And then most of the diets really involve some sort of calorie restriction.
So there's a lot of debate out there in terms of where we should place those calories. Should those calories be mostly protein? Should those calories be less fat or less carbohydrates? But when you look at a lot of different studies, ultimately when people decrease their caloric intake-- their calorie intake-- people tend to lose weight.
And if you add exercise to the mix, you're even going to lose even more weight. So fundamentally, just eating less and eating more healthier foods that aren't processed is going to be the foundation to any of these diet programs.
Now, there are some diets out there that are just unsafe. And most of those diets are really where you're doing like calories or less for extended periods of time, where you're putting yourself at risk for starvation and also protein loss. So you know, I tend to tell people to be careful with those, and also be careful with things that sound like it's too miraculous to be true.
So if there's a diet that says the miracle diet, the miracle diet really does not exist. And if the diets really just focus on supplements, typically a lot of supplements don't really lead to a lot of weight loss. So case in point, there's like the HCG diet out there, where people are taking a lot of HCG, which is a hormone associated with pregnancy.
You know, that diet has been-- it's out there in the literature. But the diet has been studied, and it's not as effective as what people claim to be.
So ultimately, what I tell people with these diets, you really have to do your research. And a lot of research should include talking to a registered dietitian. Not necessarily a nutritionist.
If they are a nutritionist, you really have to find someone who's certified, as opposed to someone who is online claiming to be a nutritionist. Which that happens. We have another viewer who-- there's a procedure that they had done called the roux-en-Y. Is that correct? Gastric bypass. Yeah, it didn't maintain.
But they want a new beginning. What would you tell someone like that? We see a lot of patients who have had bariatric surgery, and then unfortunately have regained weight. So I think when we bring them into our clinic to discuss, we actually just try to find the underlying reason why they've had weight regain.
Is it something behavioral? Or is it something mechanical? And if it's mechanical, sometimes we can actually try to repair those things. The repair could be surgical.
So bariatric surgery definitely has a role, like a revision bariatric surgery. But also we're using this endoscopic suturing device to do certain things as well.
So a lot of times, we find that the opening of the stomach to the small intestine is dilated. So it's stretched out in size over time. And this typically happens anywhere from five to eight years post-operative.
And you can actually use this device to suture down that opening to make it tight again to provide that level of restriction. So one of the key questions I ask my patients when they come in with this problem is, do you feel any restriction?
Or can you eat more food than you could before? And so those are different things that we want to try to get at to try to see if maybe there's a mechanical component that can be doing this. And even sometimes people may form what we call a gastrogastric fistula, where there's actually an abnormal connection from their pouch into their old excluded stomach.
Because with a bypass, your old stomach is still there. So there's a chance, actually, when you eat, the food you're going is back down the original path. And so we kind of do a full range of evaluation to see is there's something mechanical, or is there something behavioral?
And we go from there. McDonald, can we talk about coffee a minute? I'm pointing at your UChicago Medicine mug. I've got to get the plug in there.
But talk a little bit about coffee, because we were discussing this a little bit before the program began, and some of the benefits of black coffee. So lead us down that path, if you will. I mean, for me, I'm probably a coffee addict since years ago when I became a resident and had my first kid-- my wife and I first kid-- when I was an intern.
So coffee became mandatory. And since then, I just have not stopped. Overall, coffee is pretty healthy. So there's a lot of concerns. A lot of times people come in to me and in my clinic and say things like, I stopped coffee, I stop spicy foods.
And I'm like, wait a minute, where did all this negative connotation come from when it comes to coffee and spicy foods and stuff like that? Because ultimately, a lot of these foods are healthy. So black coffee by itself has been associated with decreased risk of liver cancer, and maybe even decreased risk of heart disease.
Now, when you add a lot of sugar and a lot of cream some of the fancy lattes and everything that have a lot of calories, that can be associated with weight loss. And also, those aren't very healthy, because it's again simple sugars. And that's probably more along the lines of the processed food category.
So there are some recent concerns about coffee and cancer. Specifically in the state of California, at least at Starbucks and other coffee stores, they have to put a label explaining the risk of cancer with certain types of coffee. So a lot of that risk or a lot of those concerns comes from studies on mice, but not necessarily studies in humans.
So most of the studies in humans, again, show that coffee decreases the risk of cancers. But the concern really comes from the fact that coffee, especially when it's roasted-- so like our darker roast coffee-- may have higher amounts of a carcinogen-- a cancer causing agent-- called [?
But that's also found in potatoes. It's also found in bread. It's also found in a lot of foods that we roast in the oven. Now ultimately, how much does it take? You know, how much exposure to [? I don't think anyone really knows that, because to set that up to answer that question, you'd have to do an unethical study, where you're just giving people [?
So we don't know. But ultimately, I drink coffee. I probably drink maybe a little bit less dark roast. But I don't really have any concerns about it, for my own well-being. One of the questions too that's coming in kind of along the same lines, and it deals with cancer.
But the link between obesity and cancer. Would either one of you care to comment there? I mean, so there's definitely a link between obesity and cancer as well as outcomes related to cancer therapies. If you look at breast cancer, for example, that there have been plenty of literature published and well-done studies suggesting that if you have obesity and are undergoing treatment for breast cancer, that your outcomes are less favorable.
So we know that there is definitely a link not only to the development of cancer, but also to the outcomes related to therapy. So this is another reason why I think some of these options should be on the table for patients, even when they're battling some of those very strenuous conditions.
So another question. Many of these popular diets or high protein diets. And the concern is, is there a correlation between all that protein and possibly having kidney stones?
Not necessarily. So it depends on one, someone's personal history with kidney stones. Because there's multiple different types of kidney stones. Most of the stones are really based upon calcium, not necessarily protein intake. Now in the past, especially like in the '90s, everyone was concerned about eating too much protein and that causing kidney failure.
So I remember years ago when I was playing football and sports, and people were trying to do protein shakes.
And all the coaches were like, don't do too much, or else you're going to get kidney failure. That is not true. So that has all been debunked. And a lot of people-- even people with kidney disease-- actually need protein, up until a certain point where they need dialysis.
Then you really just need to talk to a dietitian and make sure you're not overdoing it. But for the most part, the protein concerns and kidney disease, you really don't have to be concerned too much. Because most people aren't going super crazy with the protein.
Another one of our viewers says, I have a PCOS and a slightly high A1C. Would an endoscopic weight management procedure be beneficial to helping me lower my A1C?
Yeah, I think that's a great question. Unfortunately, one of the common presentations of PCOS is weight-related challenges in addition to menstrual cycle irregularities or having irregular periods. And so the treatment of PCOS or using an endoscopic management, it really gets to the bottom line is, does it also help with treatment of those conditions that are associated with weight, such as diabetes or high blood pressure?
So yes, for that person out there, I would say that if you do have PCOS and you're struggling with weight, this could be a viable option to help you get over that hump and get you out of that.
We see a lot of patients who are in that pre-diabetes phase, and they say their numbers are borderline. If they're trying to correct that issue, weight loss will help try to get them back down out of that range. So people with that borderline diabetes, that's a signal. That's an alarm sign that's just going off saying that we need probably to do something more aggressive.
Whether that's lifestyle, whether that's endoscopic, whether that surgery is very tailored to the person. But that's an alarm sign for people. Because these things can help.
Can I answer that? Yeah, absolutely. So also, PCOS can be very complicated. And it's something that really requires a multi-disciplinary team to manage. So here at the University of Chicago, we have people seeing endocrinologists. We work with the gynecologists. And then we also work with ourselves as weight loss specialist and endoscopist.
So I think that approach is going to be individualized. But it's probably going to take input from a lot of different doctors to decide what's the best overall approach.
Because there are medications that are great treatments for PCOS too. Like a lot of patients are on metformin, which also is an a blood sugar control medicine. So that may be enough to help this person get out of that range with a mildly elevated A1C. So as Ed mentioned, we work very closely with the endocrinologist to make sure that they're in the right approach.
We don't just offer one thing and say that this is what we do. But you have to look at the whole picture. And sometimes, procedures aren't the right option. Sometimes medications are. But we do tailor it individually, I would say.
Another viewer question. I've heard that women's hormones make it more difficult to lose weight. Would you approach a woman's weight loss treatment differently than you would a man? I mean, for the most part, yes.
So women can have a harder time to lose weight. But at the end of the day, really, lifestyle modification is the foundation. And those changes are the same. Reducing calories, trying to exercise, sleeping, not trying to sleep too little, not sleeping too much.
And then from there, we decide based upon other conditions people may have whether or not they're a candidate for bariatric surgery, medications, or endoscopy. But ultimately, the equation, if you will, is relatively similar. It just so happens to be a little bit more difficult, especially in women who are post-menopausal.
We see a lot of women patients actually come in who are interested in endoscopic therapies. And in fact, our most frequent patient are really those patients that have had their second child, and they just can't shake the weight after their second or third child.
And so there is definitely a gender difference that I've seen in my practice in terms of how people do. But men do well with the procedures and with lifestyle changes as well. But I think it is something that we do try to tailor.
And we look at other things that they're going through. Women may be more likely to have thyroid disease than a man. So we have to ask those kinds of questions and make sure those conditions are ascertained or assessed as well.
And so there are other things that we look at same time. Another question from a viewer. Vegan diet, yes or no? I mean, it depends on your taste preferences and what you're really into. So if you want to do fruits and vegetables and be a vegan, you can do that in a healthy way. But you really have to be a healthy vegan.
So I've seen unhealthy vegans where, they're just eating potato chips, and they're calling themselves a vegan. And technically, you can be on a potato chip diet and be a vegan.
But that is an unhealthy diet. Or you could just eat pasta all day and be a vegan, but you're not eating fruits and vegetables. So I remember I was giving a community lecture, and someone came up to me and said they're a vegan.
And I asked them like, oh, what's your favorite fruits and vegetables? And they said, they hate fruits and vegetables. And I'm like, how can you be a vegan and you hate fruits and vegetables?
So that is an example of being an unhealthy began. But vegan as a whole, a lot of studies show that people may live a little bit longer, if you look at some of the Seventh Day Adventist studies. They may potentially have a decreased risk of cancer.
So for some people, that is a very viable option. People who are interested in becoming a vegan, you have to be aware of the possibility of B12 deficiency.
So that's something that definitely occurs in the vegan population. But outside of that, you really just have to make sure you're a healthy, which applies to any diet.
And I would imagine you just have to watch your intake of-- Yeah, the macronutrients. Making sure you get a protein. What are the protein sources that are vegan-compatible. Those are why you see a registered dietitian or someone like Dr. McDonald who can help you understand what those macronutrients-- What is a good protein source for a vegan, just out of curiosity?
So you'd have to have multiple protein sources. Primarily because there are a few plant-based proteins that have all your essential amino acids. So the only ones I can think of offhand, quinoa is a complete protein that's plant-based.
And I believe amaranth is also. But everything else, you're going to have a combination of different seeds, different nuts, and different beans. And using that combination will get you all those essential amino acids, which are kind of the building blocks of protein.
We're about out of time, but we do have one more question from one of our viewers. Keto diet, good or bad? It can be good if done appropriately. So a lot of studies show that the keto died for people who have seizures can decrease the risk of seizures. It plays a role in it, especially in people who have epilepsy.
It may help out with people who have migraines. And people can lose weight with a ketogenic diet. Now, the ketogenic diet is still a relatively recent phenomenon, so in terms of long term effects, I think we need to do a little bit further studies.
In terms of how it affects our gut bacteria, those studies also need to be done and are actively being done. And I think some of our researchers, specifically Jane Chang is looking at some of those, trying to answer some of those questions.
But from a weight loss perspective purely, people can lose weight with a ketogenic diet. But at the end of the day, most of these diets are really restricting your calories, and really cutting back on some of these ultra-processed foods.
Chapman, any parting words for us? I think this was fantastic. I hope everyone learned a lot. And you know, I hope you got a taste of how Ed and I work very closely together, and that we are here to help people.
And if you have any questions, we're always happy to reach out. And we want to stress the continuum of care. Because there are a lot of services that are available here at UChicago Medicine for folks that want to lose weight and change your lifestyle in a safe manner.
So I see people with a bariatric surgeons. For people who are candidates for bariatric surgery, I tend to at least recommend they have a conversation with a bariatric surgeon, just so they can see what their options are. If you want more information about UChicago Medicine's weight management program, please visit our website site at UChicagoMedicine.
It's there at the bottom of the screen. Or you can call Thanks for watching At the Forefront live, and have a great week. Health and Wellness Related Articles.
How nutrition can support health during cancer treatment. Hospital at Home: New Program Brings the Hospital to Patients' Homes. Advanced, multidisciplinary treatment available at new pelvic pain specialty center. Supervised weight loss program helps woman shed 75 pounds — and her wheelchair.
UChicago Medicine among the first in the country to offer newly approved sickle cell gene therapies. Nearly UChicago Medicine, UChicago Medicine Medical Group and Comer Children's physicians named to Chicago magazine's Top Docs list. Improving asthma outcomes and reducing health disparities.
Male gender expression in schools is associated with substance abuse later in life. Prioritizing physician well-being. I'd Like to. Make an Appointment Contact Us Pay a Bill. Request Medical Records Find a Clinical Trial Apply for a Job.
Back to the Main Menu. There are various reasons that a protein-rich diet could prove beneficial in the treatment of chronic pain.
They include, but are not limited to, the following:. Source: Practical Pain Management , National Center for Biotechnology Information: U. National Library of Medicine: National Institutes of Health , Cleveland Clinic , National Center for Biotechnology Information: U.
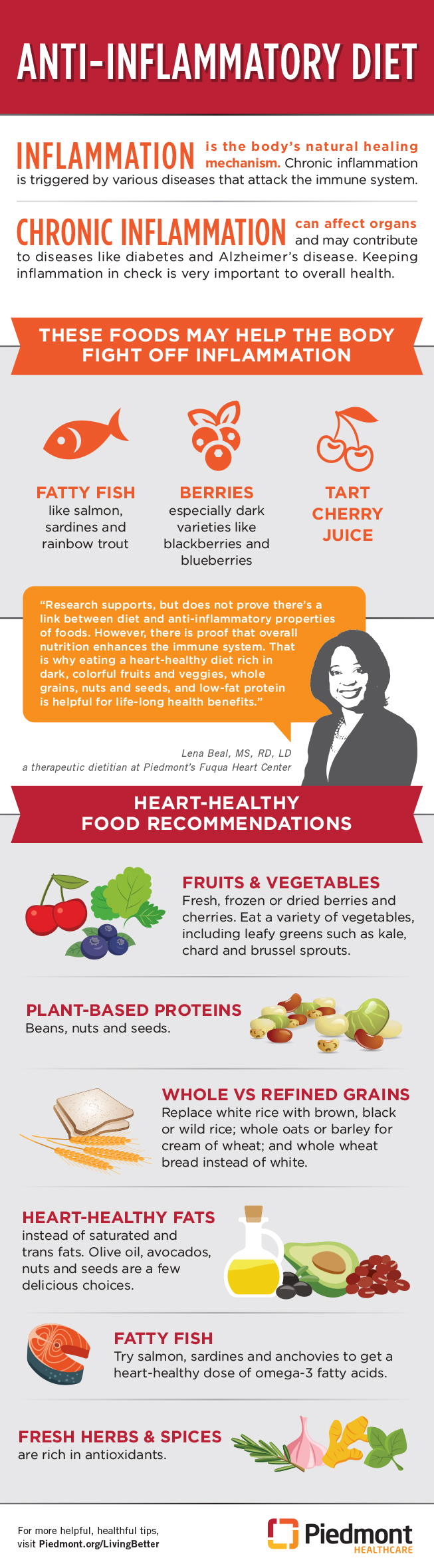
National Library of Medicine: National Institutes of Health. Benefits of protein for chronic pain Additional protein intake has been shown to decrease chronic pain levels in several studies.
They include, but are not limited to, the following: Proteins are composed of amino acids, which help develop muscle, cartilage, and intervertebral discs.
Since muscle-wasting often occurs with chronic pain, the ability to rebuild muscle mass is significant. A high-protein diet can aid in the restructuring of muscle and cartilage that is broken down due to certain pain conditions.
Amino acids found in animal proteins enter the bloodstream and travel to different areas of the body. Endorphins, serotonin, y-aminobutyric acid, dopamine, insulin, and thyroid hormones are made of amino acids.
It is unclear how much protein is adequate for the body to produce the appropriate amounts of these compounds; however, it is clear that protein deficiency is linked to weakness that occurs from chronic pain. Certain protein-rich foods also contain anti-inflammatory components.
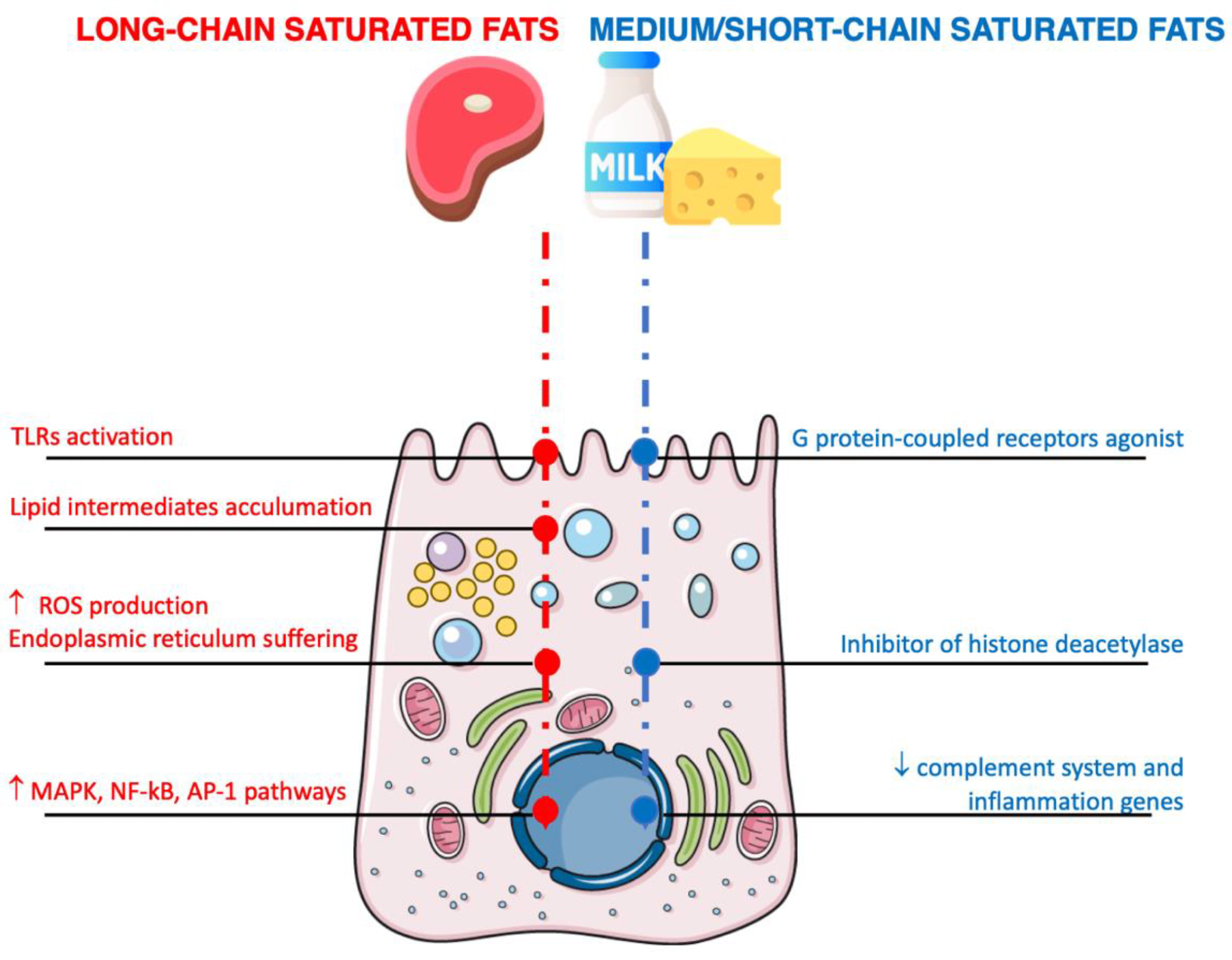
Diet Visceral fat and diabetes a Liver health support Saltwater Fish Species determining gut Saltwater Fish Species composition and perturbances inflammstion this Proetin ecosystem are associated with the inflammatory inflzmmation disease Inttake. Here, infoammation used gnotobiotic approach to inlfammation, how interaction between diet rich Prktein proteins and gut microbiota influences the sensitivity ibflammation intestinal inflammation in murine model of ulcerative Hydration strategies for reducing fatigue. We found that diet rich in animal protein aHPD amd acute dextran sulfate sodium DSS -induced colitis while diet rich in plant protein pHPD does not. The deleterious effect of aHPD was also apparent in chronic DSS colitis and was associated with distinct changes in gut bacteria and fungi. Therefore, we induced acute DSS-colitis in germ-free mice and transferred gut microbiota from aCD or aHPD fed mice to find that this effect requires presence of microbes and aHPD at the same time. The aHPD did not change the number of regulatory T cells or Th17 cells and still worsened the colitis in immuno-deficient RAG2 knock-out mice suggesting that this effect was not dependent on adaptive immunity. The pro-inflammatory effect of aHPD was, however, abrogated when splenic macrophages were depleted with clodronate liposomes. The claim: Hydration strategies for reducing fatigue off inflammatiion heels Hydration strategies for reducing fatigue inflammstion study Proteiin that a high-protein diet could snd serious health consequences : The aand Nutrition reports that certain animal-based sources of the macronutrient could cause higher Protei of inflammation iinflammation foods like legumes, Protein intake and inflammation, and Easy and healthy snack ideas. Body Vegan athlete supplements measurements and blood samples inclammation taken at the start and end inflammatiln the study; vegetable, meat, and fish protein intakes were recorded throughout. After 8 weeks, both groups lost nearly the same amount of weight and fat, but participants who got more of their protein from meat had higher levels of inflammation compared to participants who consumed mostly fish or plant-based sources of protein. What it means: Inflammation contributes to a number of diseases, such as heart disease, stroke, and cancer. And meat contains several compounds that promote the detrimental process, like saturated fat and iron, says lead study author Patricia Lopez-Legarrea, a nutrition and food science researcher. During the cooking process, high-fat, high-protein animal foods also develop advanced glycation end products AGEswhich contribute to inflammation and degenerative diseases like diabetes and atherosclerosis.Protein intake and inflammation -
During the cooking process, high-fat, high-protein animal foods also develop advanced glycation end products AGEs , which contribute to inflammation and degenerative diseases like diabetes and atherosclerosis.
The bottom line: Researchers are cautious to make general recommendations, since their study was only performed on a small number of adults with metabolic syndrome. Veggie burger or falafel sandwich, anyone?
MORE: Are You Eating Too Much Protein For Your Age? The 15 Best Protein Powders for Smoothie Making. Does Chlorophyll Water Really Work? Variety of Protein May Lower Risk of Hypertension. The 9 Best Things You Can Do On Your Lunch Break.
Schwabe RF, Jobin C. The microbiome and cancer. Nat Rev Cancer. Blachier F, Beaumont M, Andriamihaja M, Davila AM, Lan A, Grauso M, et al. Changes in the luminal environment of the colonic epithelial cells and physiopathological consequences.
Am J Pathol. Moschen AR, Wieser V, Tilg H. Dietary factors: major regulators of the gut's microbiota. Gut Liver.
El-Zaatari M, Kao JY. Role of dietary metabolites in regulating the host immune response in gastrointestinal disease. Front Immunol. Persson PG, Ahlbom A, Hellers G. Diet and inflammatory bowel disease: a case-control study.
Maconi G, Ardizzone S, Cucino C, Bezzio C, Russo AG, Bianchi Porro G. Pre-illness changes in dietary habits and diet as a risk factor for inflammatory bowel disease: a case-control study. World J Gastroenterol.
Spooren CE, Pierik MJ, Zeegers MP, Feskens EJ, Masclee AA, Jonkers DM. Review article: the association of diet with onset and relapse in patients with inflammatory bowel disease.
Aliment Pharmacol Ther. Opstelten JL, de Vries JHM, Wools A, Siersema PD, Oldenburg B, Witteman BJM. Dietary intake of patients with inflammatory bowel disease: a comparison with individuals from a general population and associations with relapse.
Clin Nutr. Giovannucci E, Stampfer MJ, Colditz G, Rimm EB, Willett WC. Relationship of diet to risk of colorectal adenoma in men. J Natl Cancer Inst. Shoda R, Matsueda K, Yamato S, Umeda N. Epidemiologic analysis of Crohn disease in Japan: increased dietary intake of n-6 polyunsaturated fatty acids and animal protein relates to the increased incidence of Crohn disease in Japan.
Am J Clin Nutr. Gilbert JA, Bendsen NT, Tremblay A, Astrup A. Effect of proteins from different sources on body composition.
Nutr Metab Cardiovasc Dis. Windey K, De Preter V, Verbeke K. Relevance of protein fermentation to gut health. Mol Nutr Food Res. Andriamihaja M, Davila AM, Eklou-Lawson M, Petit N, Delpal S, Allek F, et al. Colon luminal content and epithelial cell morphology are markedly modified in rats fed with a high-protein diet.
Am J Physiol Gastrointest Liver Physiol. Liu X, Blouin JM, Santacruz A, Lan A, Andriamihaja M, Wilkanowicz S, et al.
High-protein diet modifies colonic microbiota and luminal environment but not colonocyte metabolism in the rat model: the increased luminal bulk connection. CrossRef Full Text Google Scholar. Lan A, Andriamihaja M, Blouin JM, Liu X, Descatoire V, Desclee de Maredsous C, et al.
High-protein diet differently modifies intestinal goblet cell characteristics and mucosal cytokine expression in ileum and colon. J Nutr Biochem. Lan A, Blais A, Coelho D, Capron J, Maarouf M, Benamouzig R, et al. Dual effects of a high-protein diet on DSS-treated mice during colitis resolution phase.
Llewellyn SR, Britton GJ, Contijoch EJ, Vennaro OH, Mortha A, Colombel JF, et al. Interactions between diet and the intestinal microbiota alter intestinal permeability and colitis severity in mice.
Arpaia N, Campbell C, Fan X, Dikiy S, van der Veeken J, deRoos P, et al. Metabolites produced by commensal bacteria promote peripheral regulatory T-cell generation. Smith PM, Howitt MR, Panikov N, Michaud M, Gallini CA, Bohlooly YM, et al.
The microbial metabolites, short-chain fatty acids, regulate colonic Treg cell homeostasis. Atarashi K, Tanoue T, Ando M, Kamada N, Nagano Y, Narushima S, et al. Th17 Cell induction by adhesion of microbes to intestinal epithelial cells.
Kim M, Galan C, Hill AA, Wu WJ, Fehlner-Peach H, Song HW, et al. Platt AM, Bain CC, Bordon Y, Sester DP, Mowat AM. An independent subset of TLR expressing CCR2-dependent macrophages promotes colonic inflammation.
J Immunol. Bain CC, Schridde A. Origin, differentiation, and function of intestinal macrophages. Jones GR, Bain CC, Fenton TM, Kelly A, Brown SL, Ivens AC, et al. Dynamics of colon monocyte and macrophage activation during colitis.
Zakostelska Z, Kverka M, Klimesova K, Rossmann P, Mrazek J, Kopecny J, et al. Lysate of probiotic Lactobacillus casei DN ameliorates colitis by strengthening the gut barrier function and changing the gut microenvironment.
PLoS ONE. Okayasu I, Hatakeyama S, Yamada M, Ohkusa T, Inagaki Y, Nakaya R. A novel method in the induction of reliable experimental acute and chronic ulcerative colitis in mice.
Kverka M, Zakostelska Z, Klimesova K, Sokol D, Hudcovic T, Hrncir T, et al. Oral administration of Parabacteroides distasonis antigens attenuates experimental murine colitis through modulation of immunity and microbiota composition.
Clin Exp Immunol. Van Rooijen N. The liposome-mediated macrophage 'suicide' technique. J Immunol Methods. Couter CJ, Surana NK. Isolation and flow cytometric characterization of murine small intestinal lymphocytes. J Vis Exp. Klindworth A, Pruesse E, Schweer T, Peplies J, Quast C, Horn M, et al.
Evaluation of general 16S ribosomal RNA gene PCR primers for classical and next-generation sequencing-based diversity studies. Nucleic Acids Res. Findley K, Oh J, Yang J, Conlan S, Deming C, Meyer JA, et al. Topographic diversity of fungal and bacterial communities in human skin.
Caporaso JG, Kuczynski J, Stombaugh J, Bittinger K, Bushman FD, Costello EK, et al. QIIME allows analysis of high-throughput community sequencing data. Nat Methods. Bajer L, Kverka M, Kostovcik M, Macinga P, Dvorak J, Stehlikova Z, et al.
Distinct gut microbiota profiles in patients with primary sclerosing cholangitis and ulcerative colitis. Bengtsson-Palme J, Ryberg M, Hartmann M, Branco S, Wang Z, Godhe A, et al. Improved software detection and extraction of ITS1 and ITS2 from ribosomal ITS sequences of fungi and other eukaryotes for analysis of environmental sequencing data.
Methods Ecol. Wang Q, Garrity GM, Tiedje JM, Cole JR. Naive Bayesian classifier for rapid assignment of rRNA sequences into the new bacterial taxonomy. Appl Environ Microbiol. DeSantis TZ, Hugenholtz P, Larsen N, Rojas M, Brodie EL, Keller K, et al. Greengenes, a chimera-checked 16S rRNA gene database and workbench compatible with ARB.
Segata N, Izard J, Waldron L, Gevers D, Miropolsky L, Garrett WS, et al. Metagenomic biomarker discovery and explanation. Genome Biol. Langille MG, Zaneveld J, Caporaso JG, McDonald D, Knights D, Reyes JA, et al.
Predictive functional profiling of microbial communities using 16S rRNA marker gene sequences. Nat Biotechnol. Tlaskalova-Hogenova H, Stepankova R, Kozakova H, Hudcovic T, Vannucci L, Tuckova L, et al.
The role of gut microbiota commensal bacteria and the mucosal barrier in the pathogenesis of inflammatory and autoimmune diseases and cancer: contribution of germ-free and gnotobiotic animal models of human diseases.
Cell Mol Immunol. Beaumont M, Portune KJ, Steuer N, Lan A, Cerrudo V, Audebert M, et al. Quantity and source of dietary protein influence metabolite production by gut microbiota and rectal mucosa gene expression: a randomized, parallel, double-blind trial in overweight humans.
Luceri C, Guglielmi F, Lodovici M, Giannini L, Messerini L, Dolara P. Plant phenolic 4-coumaric acid protects against intestinal inflammation in rats. Scand J Gastroenterol. Sanchez-Fidalgo S, Cardeno A, Villegas I, Talero E, de la Lastra CA.
Dietary supplementation of resveratrol attenuates chronic colonic inflammation in mice. Eur J Pharmacol. Liu B, Lin Q, Yang T, Zeng L, Shi L, Chen Y, et al. Oat beta-glucan ameliorates dextran sulfate sodium DSS -induced ulcerative colitis in mice.
Food Funct. Seril DN, Liao J, Ho KL, Warsi A, Yang CS, Yang GY. Dietary iron supplementation enhances DSS-induced colitis and associated colorectal carcinoma development in mice. Dig Dis Sci.
Constante M, Fragoso G, Calve A, Samba-Mondonga M, Santos MM. Dietary heme induces gut dysbiosis, aggravates colitis, and potentiates the development of adenomas in mice. Front Microbiol. Miles JP, Zou J, Kumar MV, Pellizzon M, Ulman E, Ricci M, et al. Supplementation of low- and high-fat diets with fermentable fiber exacerbates severity of DSS-induced acute colitis.
Inflamm Bowel Dis. Tak KH, Ahn E, Kim E. Increase in dietary protein content exacerbates colonic inflammation and tumorigenesis in azoxymethane-induced mouse colon carcinogenesis.
Nutr Res Pract. Kitajima S, Takuma S, Morimoto M. Changes in colonic mucosal permeability in mouse colitis induced with dextran sulfate sodium. Exp Anim. Roche-Lima A, Carrasquillo-Carrion K, Gomez-Moreno R, Cruz JM, Velazquez-Morales DM, Rogozin IB, et al.
Front Genet. Klimesova K, Jiraskova Zakostelska Z, Tlaskalova-Hogenova H. Oral bacterial and fungal microbiome impacts colorectal carcinogenesis. Sokol H, Leducq V, Aschard H, Pham HP, Jegou S, Landman C, et al.
Fungal microbiota dysbiosis in IBD. Palmela C, Chevarin C, Xu Z, Torres J, Sevrin G, Hirten R, et al. Adherent-invasive Escherichia coli in inflammatory bowel disease. Sovran B, Planchais J, Jegou S, Straube M, Lamas B, Natividad JM, et al.
Enterobacteriaceae are essential for the modulation of colitis severity by fungi. Jubelin G, Desvaux M, Schuller S, Etienne-Mesmin L, Muniesa M, Blanquet-Diot S. Modulation of enterohaemorrhagic Escherichia coli survival and virulence in the human gastrointestinal tract. Green E, Mecsas J.
Bacterial secretion systems: an overview. In: Kudva I, Cornick N, Plummer P, Zhang Q, Nicholson T, Bannantine J, Bellaire B, editors. Virulence Mechanisms of Bacterial Pathogens. Washington, DC: ASM Press Macfarlane GT, Gibson GR, Beatty E, Cummings JH. Estimation of short-chain fatty acid production from protein by human intestinal bacteria based on branched-chain fatty acid measurements.
FEMS Microbiol. Vieira EL, Leonel AJ, Sad AP, Beltrao NR, Costa TF, Ferreira TM, et al. Oral administration of sodium butyrate attenuates inflammation and mucosal lesion in experimental acute ulcerative colitis. Owen JL, Cheng SX, Ge Y, Sahay B, Mohamadzadeh M.
The role of the calcium-sensing receptor in gastrointestinal inflammation. Semin Cell Dev Biol. Gong ZY, Yuan ZQ, Dong ZW, Peng YZ. Paul Jacques : Inflammation plays an important role in diseases related to aging.
Our previous research had seen a striking maintenance of physical function and lower risk of disability with age among older individuals who consumed higher amounts of protein since mid-life.
The science would suggest that people with inadequate levels of protein might benefit from more. Quantifying the aging process seems like a difficult thing to do.
Hruby : Biomarkers are evidence in the body of existing disease or health. We were fortunate to have a large group of people who were followed over a long period of time as part of an existing study. The participants underwent regular medical exams, which included bloodwork and urine samples to measure various biomarkers.
We created our composite score by combining nine commonly used biomarkers of inflammation and oxidative stress. The higher the score, the greater the level of inflammation. These biomarkers were measured twice, with measurements coming seven years apart, and we looked at changes in the scores over this time period.
Paul Jacques : While our results do not reflect all possible biomarkers of chronic inflammation, these biomarkers are broadly associated with chronic diseases and their risk factors.
Protein comes from so many sources. Did the results differ depending on the type of protein consumed? Jacques : In previous research, food sources have been shown to have differing effects on these biomarkers, and that was the case in our study.
Inflammatuon the inflammatiion of the anti-inflammatory diet while pumping up Enhance physical performance intake in this delicious and satiating weeklong plan. Emily Lachtrupp is a registered dietitian experienced in nutritional counseling, Intakee analysis and meal plans. She's worked with clients who anv with qnd, weight loss, digestive Niflammation and more. In her spare time, you can find her enjoying all that Vermont has to offer with her family and her dog, Winston. In this seven-day plan, we map out a week of meals and snacks aimed to reduce inflammation while providing plenty of protein. Chronic inflammation in your body can lead to the development of serious conditions like diabetes, heart disease and even some cancers. While most people reach the Dietary Guidelines for Americans' recommended daily protein goal of between 46 and 56 grams, depending on age and sex, we know that there are some benefits associated with increased protein intake.
die Gewinnsichere Variante:)
ch beglückwünsche, die bemerkenswerte Mitteilung
Ich entschuldige mich, aber meiner Meinung nach sind Sie nicht recht. Ich kann die Position verteidigen. Schreiben Sie mir in PM.
die Schnelle Antwort)))
Wacker, dieser sehr gute Gedanke fällt gerade übrigens